
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C. S. PRASAD
CASE OF KULDEEP SINGH V/S APOLLO MUNICH HEALTH INSU. CO LTD.
COMPLAINT REF: NO: NOI-H-003-1920-0115
1.
Name & Address of the Complainant
KULDEEP SINGH
H.NO- 214 , II FLOOR , SECTOR -22
GAUTAM BUDH NAGAR
U.P.- 201301
2.
Policy No:
Type of Policy
Duration of policy/Policy period
110102/00021/AA00354313
HEALTH
3.
Name of the insured
Name of the policyholder
Kuldeep Singh
Kuldeep Singh
4.
Name of the insurer
APOLLO MUNICH HEALTH INSURANCE CO.
5.
Date of Rejection
3-07-2019
6.
Reason for rejection
Policy out of free look period
7.
Date of receipt of the Complaint
10-07-2019
8.
Nature of complaint
Repudiation for non disclosure of pre existing disease
9.
Amount of Claim
2,22,374.00
10.
Date of Partial Settlement
nil
11.
Amount of relief sought
12.
Complaint registered under
IOB rules
yes
13.
Date of hearing/place
18-12-2019/ NOIDA
14.
Representation at the hearing
a) For the Complainant
Mr. Kuldeep Singh
b) For the insurer
Dr. Mohd. Danish
15
Complaint how disposed
Award
16
Date of Award/Order
27.12.2019
17 . Brief Facts of the case : The complainant Mr. Kuldeep Singh purchased a health policy on 27-01-2016 for Rs.
5,00,000/- . He had submitted the claim papers of kidney transplant in January 2019 for settlement of the claim. The insurer
has rejected the claim on 3/07/2019 with the reason “Non disclosure and concealment of facts of previous illness of the
claimant”. On 10/07/2019 complainant has approached Ombudsman office for settlement of the claim.
18. Cause of the complaint:
A. Complainant argument : Complainant is having a policy with the insurer since January 2016. In January 2019
he got kidney transplant from AIIMS and submitted bills to the insurer. The insurer repudiated the claim stating that
his hospital treatment papers show that he is a known case of craniotomy( surgery of Brain) and neurocystcercosis (
by Larwa of tape worm of Taenia Solium Which travelled to brain ) in Year 2001. He does not have the record of
20 year old treatment. Complainant urges the operation was done 18 years back for removal of larva of tape worm in
brain and after removal of the same the problem never reoccured. He wants payment of the claim to be made by
Insurer.
B. Insurer’s argument : The policy was taken in 2016 and complainant had submitted bills for kidney transplant in
Jan 2019 for which treatment was given from last two years. In the discharge summary of AIIMS there was mention
of craniotomy and neurocysticercosis in 2001 and insurer has repudiated the claim for non disclosure of the previous
disease.
19. Reason for Registration of Complaint:
Repudiation of claim for non disclosure of previous health problem.
20. Following documents were placed for perusal:
1. Complaint letter.
2. medical treatment papers
3. SCN
21. Observation and conclusion :
Both the parties appeared for personal hearing and reiterated their submissions. The complainant Mr. Kuldeep Singh
had kidney problem from last two years and he got the kidney transplant in January 2019 from AIIMS, and
submitted the claim papers of that treatment to the insurer which have been rejected on account of the fact that the
insured had brain surgery in 2001 for removal of tape worm and he did not disclose it in the proposal form The
complainant stated that he never had any problem related to this after the operation and he did not preserve the
papers of treatment.
I have examined the documents exhibited as evidence and oral submissions made by both the parties, it is noticed
that removal of tape worm from brain by operation was done 18 years back and there is no nexus of between tape
worm larwa removal and the kidney transplant. Hence the insurer is directed to release the claim to the complainant
and reinstate the policy cover excluding pre- existing disease.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the Insurance company is directed to settle
the claim as per the conditions of the policy , and reinstate the policy cover excluding the
pre-existing disease.
The complaint is treated as closed accordingly.

22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 27.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C. S. PRASAD
CASE OF RAKESH KOHLI V/S APOLLO MUNICH HEALTH INSU. CO LTD.
COMPLAINT REF: NO: NOI-H-003-1920-0114
AWARD NO:
1.
Name & Address of the Complainant
RAKESH KOHLI
A-51 , SECTOR-2 NOIDA
U.P.- 201301
2.
Policy No:
Type of Policy
Duration of policy/Policy period
515732201903
HEALTH
12-05-2018
3.
Name of the insured
Name of the policyholder
Rakesh Kohli
Rakesh Kohli
4.
Name of the insurer
Apollo Munich Health Insurance Co.
5.
Date of Rejection
13-02-2019
6.
Reason for rejection
Repudiation for non disclosure of pre existing disease
7.
Date of receipt of the Complaint
13-05-2019
8.
Nature of complaint
repudiation
9.
Amount of Claim
75708.00
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Settlement of medical Bill and reinstatement of policy
12.
Complaint registered under
IOB rules
Yes
13.
Date of hearing/place
18-12-2019/ NOIDA
14.
Representation at the hearing
c) For the Complainant
Mr. Rakesh Kohli
d) For the insurer
Dr. Mohd. Danish
15
Complaint how disposed
Award
16
Date of Award/Order
30.12.2019
17 . Brief Facts of the case :
The policy holder had Health policy from Oriental insurance since 2010. One insurance broker approached the
complainant and advised him to port his policy to Apollo Munich and a new policy was issued to the complainant by
porting the health policy of Oriental Insurance Company in May 2018. On 29-08-2018 the assured was admitted to Noida
Medical Center Hospital and discharged on 31-08-2018. He submitted the bills for settlement of the claim . The insurer
rejected the claim for non disclosure of material facts . On 13-05-2019, complainant has approached Ombudsman Office
for settlement of the claim.
18. Cause of the complaint:
A. Complainant argument :
The complainant was under medical cover of a Health policy with Oriental Insurance company since 2010. One
Insurance broker advised him to port his policy to Apollo Munich Health policy and complainant got his policy
ported. All previous insurance policy papers were given to the broker with premium for new policy. He was
hospitalized for treatment on 28 to 31 August in Noida Medical Center hospital. He submitted his claim to the
insurer. The insurer had rejected the claim stating that The complainant was treated for tongue cancer in April 2013.
As per porting form submitted by complainant the policy details is given for three years only. Complainant has
stated he had given all papers since inception of policy and he did not had any health problem in last three years.
He has also submitted the certificate of doctor of treating hospital that in August 2018 the complainant got seizure
all of sudden. He wants his claim to be paid.
B. Insurer’s argument :
The complainant had purchased the policy on 12-05-2018. He submitted his claim for hospitalization from 29 to 31
August 2018. From treatment papers and discharge summary, it was revealed that the complainant was operated for
cancer of tongue in 2013. As per porting form of policy from Oriental Insurance to Apollo Munich, the details of 3
years policy was mentioned. There was no claim during in three years. The operation in 2013 is before the period
mentioned in the policy so this comes under the clause of non disclosure of materiel facts. Hence the insurer has
rejected the claim
19. Reason for Registration of Complaint:
Repudiation of claim for non disclosure of previous health problem.
20. Following documents were placed for perusal:
1. Complaint letter.
2. Medical treatment papers
3. SCN
21. Observation and conclusion -
Both the parties appeared for personal hearing and reiterated their submissions. The complainant Mr. Rakesh Kohli
was insured with Oriental Insurance company since 2009. An agent of Apollo Munich approached the complainant

for porting his policy to Apollo Munich Insurance. The assured gave all papers related to the existing policy. The
assured was hospitalized for treatment from 29
th
to 31st August 2018 for sudden onset of seizure due to neuro
problem. The insurer has rejected the claim stating that the insured had history of Carcinoma of Palate in 2013. In
the policy porting available with the insurer showing details of previous 3 years , which means assured was insured
with previous insurer for three years only. Hence as per insurer , history of Ca palate in 2013 is a non disclosure of
old disease and insurer has rejected the claim. The complainant stated that no form was signed by him at the time of
porting . He had given only a cheque of premium amount to the agent. The claim in the year 2013 was paid to the
complainant by the Oriental Insurance company.
I have examined the documents exhibited as evidence and oral submissions made by both the parties, I find that the
insured did not sign the porting forms as signature on the form is prima- facie, different from the signature done at
the court attendance . The alleged non disclosure can not be attributed to him and it would also be unfair to make
him bear its consequences. The claim payment details of Ca palate were available with Oriental insurance and the
same was to be checked by the insurer while porting the policy. Insured is not at fault. This fact is admitted by the
insurer. Hence, the insurer is directed to pay the claim of the complainant and renew the policy with exclusion of
pre existing disease.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the Insurance company is directed to pay the
claim amount to the complainant and reinstate the policy number 515732201903 by
excluding pre existing disease.
The complaint is treated as closed accordingly.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 30.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C. S. PRASAD
CASE OF AMIT SRIVASTAVA V/S APOLLO MUNICH HEALTH INSU. CO LTD.
COMPLAINT REF: NO: NOI-H-003-1920-0135
1.
Name & Address of the Complainant
AMIT SRIVASTAVA
FLAT NO- 304 , LILY TOWER , DIVINE
MEADOWS APTT. SECTOR- 108
GAUTAM BUDH NAGAR
U.P.- 201304
2.
Policy No:
Type of Policy
Duration of policy/Policy period
`110100/11121/AA00904629
HEALTH
3.
Name of the insured
Name of the policyholder
Ritu Aali Srivastava
Amit Srivastava
4.
Name of the insurer
APOLLO MUNICH HEALTH INSURANCE CO.
5.
Date of Rejection
3-07-2019
6.
Reason for rejection
Non disclosure of pre existing disease
7.
Date of receipt of the Complaint
30-07-2019
8.
Nature of complaint
Repudiation
9.
Amount of Claim
2,63,294.00
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
12.
Complaint registered under
IOB rules
Yes
13.
Date of hearing/place
18-12-2019/ NOIDA
14.
Representation at the hearing
e) For the Complainant
Mr. Amit Srivasatva
f) For the insurer
Dr. Mohd. Danish
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17 . Brief Facts of the case :
The complainant Mr. Amit Srivastava purchased a health insurance policy on 7-09-2018 for Rs. 5,00,000/- for him and his
wife Mrs. Ritu Aali Srivastava. He had submitted the claim papers of Mrs. Ritu who was hospitalized on 9-02-2019, for
settlement of the claim. The insurer has rejected the claim on 15-05-2019, with the reason “Non disclosure of the disease
Rheumatoid Arthritis while taking the policy”. On 30/07/2019 complainant has approached Ombudsman Office for
settlement of the claim.
18. Cause of the complaint:
A. Complainant argument :

The Complainant purchased this policy on 7-09-2018. On 09-02-2019, the complainant’s wife Mrs. Ritu Aali
Srivastava was taken to Jaypee Hospital with the complaint of drowsiness. The doctor in emergency ward,
informed them that drowsiness is due to deficiency of sodium & potassium. She was admitted in the Hospital. She
was given treatment there for 10 days for drowsiness and anemia. On 21-02-2019, she died of Septic Shock. Insurer
rejected the claim, with the reason of non disclosure of pre-insurance existing disease rheumatoid Arthritis .The
complainant has enclosed the doctors certificate that assured died of septic shock not Arthritis. He has also
submitted that patient was not having active rheumatoid Arthritis , duration of this illness was only 3-4 days. The
complainant wants payment of the claim by Insurer.
B. Insurer’s argument :
The policy was purchased by the complainant on 7-09-2018. Insured Mrs. Ritu was admitted in hospital on 9-02-
2019. On reviewing the treatment papers of assured Mrs. Ritu, it was observed that she was admitted with the
complaint of drowsiness. In discharge summary it is mentioned that patient was the known case of HTN from last 12
Years. She was also suffering from rheumatoid Arthritis since 2015 and was on medicines. The complainant did not
disclose the pre existing disease rheumatoid Arthritis, which is one of the cause of death. Hence, claim is not
payable by the insurer.
19. Reason for Registration of Complaint:
Repudiation of claim for non disclosure of previous health problem.
20. Following documents were placed for perusal:
1. Complaint letter.
2. Medical treatment papers
3. SCN
21. Observation and conclusion :
Both the parties appeared for personal hearing and reiterated their submissions. It is observed by reviewing the
discharge summary of Jaypee Hospital, where she was admitted with the problem of drowsiness and generalized
weakness, that she was diagnosed refractory nonconvusive epilepticus and Severe Septic shock. It was also
mentioned that hypertension and rheumatoid arthritis were comorbid illnesses. The complainant has produced the
certificate dated 17-05-2019 from the treating Doctor, that Life assured died of septic shock. The Rheumatoid
Arthritis was not the cause of death.
I have examined the documents exhibited as evidence and oral submissions made by both the parties. The certificate
by the treating Doctor of Jaypee Hospital, produced by the complainant clearly proves that the assured died of Septic
shock . The insurer’s decision to repudiate the claim because the insured did not disclose the previous existing
disease , Rheumatoid Arthritis is incorrect and unreasonable. Hence, claim is payable to the complainant.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the death of life assured was not due to
Rheumatic Arthritis, but it was due to septic shock . Hence, the Insurance company is
directed to pay the claim amount Rs. 2,63,294/- to the complainant.
The complaint is treated as closed accordingly.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. SAMIR AGARWAL V/S BAJAJ ALLIANZ GENERAL INSURANCE CO. LTD.
COMPLAINT REF. NO. : NOI-H- 005-1920-0124
1.
Name & Address of the Complainant
Sh. Samir Agarwal
B-5, Sector-27,
Noida, U.P.201301
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Sum Insured
OG-18-1105-8416-00000058
Extra Care Health Insurance Policy
12.06.2017 to 11.06.2018
Rs.15,00,000/-
3.
Name of the insured
Name of the policyholder
Ms. Monica Agarwal, Spouse
Sh. Samir Agarwal
4.
Name of the insurer
Bajaj Allianz General Ins. Co. Ltd.
5.
Date of Repudiation
14.12.2017
6.
Reason for repudiation
Non disclosure of PED
7.
Date of receipt of the Complaint
24.06.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
N.A.

10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Sum Insured Rs.15,00,000/- + 24% interest
Rs.7,20,000/- + harassment Rs.1,00,000/- +
Rs.1,00,000/- penalty Total Rs.24,20,000/- as per
Annex VI A
12.
Complaint registered under
Rule no: of IOB rules, 2017
13 (1)(b)
13.
Date of hearing/place
13.11.2019 / NOIDA
14.
Representation at the hearing
g) For the Complainant
Sh. Samir Agarwal
h) For the insurer
Sh. Angee Sharma, Dy. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
12.12.2019
17) Brief Facts of the Case : Sh. Samir Agarwal had taken a Extra Care Health Insurance Policy No.OG-18-1105-
8416-00000058 for the period from 12.06.2017 to 11.06.2018, Sum Insured of Rs.15,00,000/-. Claim of wife of
the Complainant was rejected by the Insurance Company. Aggrieved, he requested the insurer including its GRO
to reconsider the claim but failed to get any relief. Thereafter, he preferred a complaint to this office for
resolution of his grievance.
18) Cause of Complaint:
a) Complainant’s argument : The Complainant stated that he had taken Extra Care Health Insurance Policy
No.OG-18-1105-8416-00000058 for the period from 12.06.2017 to 11.06.2018 for the Sum Insured of
Rs.15,00,000/- from Bajaj Allianz General Ins. Co. Ltd. by paying the premium of Rs.9,459/-. He was already
having Health policy with the National Insurance Co. for Sum Insured of Rs.5,00,000/- and the policy given by
the Bajaj Allianz was over and above the existing policy of NIC.
During the year 2009, his wife got admitted to Bombay Hospital and Medical Research Centre where she was
diagnosed with the Spinocerebellar Ataxia (It is one of the group of disorders characterizes by slowly
progressive in coordination of gait and is often associated with poor coordination of hands, speech and eye
movement) and Acoustic Neuroma (It is a non-cancerous growth that develops on eight cranial nerve, also
known as Vestibulocochlear Nerve, it connects the inner ear with brain and has two different parts. One part is
involved in transmitting sound and other send balance information from the inner ear to brain). She was
operated for acoustic neuroma
On 04.11.2016, almost after 7 year, his wife was admitted to Max Hospital Delhi after the complaint of
Aspiration Pneumonia with type 1 respiratory failure and she was discharged on 13.11.2016. Claim of this
hospitalization in Max Hospital Delhi for Rs.1,20,000/- was given by the NIC.
Again on 30.12.2016, his wife was admitted to Kailash Hospital, Noida upon the same complaint of aspiration
pneumonia and severe breathlessness and was discharged after being in stable condition.
The complainant’s wife was again admitted on 22.02.2017 in Kailash hospital for the same problem i.e.
pneumonitis with sepsis and was discharged on 25.02.2017 whereupon the Bajaj paid the hospital bill amounting
to Rs.1,87,954/- only in September 2017 as the total Sum Insured of NIC was exhausted.
On 23.07.2017, his wife was suffering from acute loose motions with nausea and high fever and immediately had
to be taken to Kailash Hospital. After understanding the seriousness of the condition, the complainant preferred
to take her to Sir Ganga Ram Hospital which is better equipped than the Kailash Hospital in well equipped
ambulance on 25.07.2017 and discharged on 06.09.2017. The bill for the hospitalization in Kailash Hospital for
23.07.2017 to 25.07.2017 was paid by the NIC.
After exhausting the Sum Insured of NIC in the year 2017, the claim of Rs.14,01,747/- after deducting
Rs.5,00,000/- as per policy terms and conditions was filed with the Bajaj, though, the total bill amount for
admission in Sir Ganga Ram Hospital, Delhi was for Rs.19,01,747/-. The Bajaj Allianz were informed about the
admission on 28.09.2017. Thereafter, the Bajaj kept on asking for documents and bills and proofs which were
supplied to them within the time frame.
On 14.12.2017, the Bajaj repudiated his claim on ground that the verification of claim documents reveal that his
wife was suffering from Spinocerebellar Ataxia since 2009 which was pre-existing to the policy and has not been
disclosed on the proposal form.
b) Insurers’ argument: The Insurance Company stated in their SCN that it was found that the complainant’s
patient was admitted to Sir Ganga Ram Hospital, New Delhi on 25.07.2017 with a diagnosis or perforative
peritonitis s/p PEG tube re-insertion in a follow up case of Spinocerebellar ataxia and the insured was discharged
on 06.09.2017. The insured was also admitted prior to this treatment with Kailash Hospital, Noida on
30.12.2016 and was discharged on 25.01.2017. The case summary on the discharge summary for the said
treatment record explicitly confirms that the insured namely Monica Aggarwal was suffering from
spinocerebellar ataxia since 2009.
Although the Health Policy was held by the complainant since 2013 with the Bajaj but the illness
Spinocerebellar ataxia is a pre-existing disease to the policy starting with Bajaj which has not been disclosed in
the proposal form submitted at the time of taking the policy. The complainant had taken a policy from them in
the year 2013 and was aware of the pre-existing disease but the complainant deliberately chose not to mention
and misrepresented the same in the proposal form submitted to the Insurer.
On the history of illness and non disclosure of the same in the proposal form at the time of taking the policy, the
claim for the treatment of the insured was duly repudiated under the terms and conditions no.13 of the policy.

19) Reason for Registration of Complaint:- Rejection of Mediclaim.
20) The following documents were placed for perusal.
a) SCN.
b) Annexure VI A
c) Complaint copy
d) Discharge summary.
21) Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. The Complainant stated that
the Insurance Company had paid his claim for the same disease in 2017 because the amount was less. But
when, her wife was again hospitalized for the same disease and the hospital bill was huge, the Insurance
Company rejected his claim. The Insurance Company stated that the insured namely Monica Aggarwal was
suffering from spinocerebellar ataxia since 2009 and though, the Health Policy was held by the complainant
since 2013 with the Bajaj, the illness Spinocerebellar ataxia is a pre-existing disease to the policy starting with
Bajaj which has not been disclosed in the proposal form submitted at the time of taking the policy.
I have closely examined the documents exhibited and oral submissions made by both the parties during
personal hearing. The insurer has repudiated the claim of the complainant in December 2017 on the ground of
PED i.e. Spinocerebellar Ataxia to the policy.
The facts of the case in chronological order are given in the preceding pages which have not been assailed by
the insurer. It is observed that the complainant’s wife Ms. Monica Aggarwal was admitted in Max Hospital on
04.11.2016 and discharged on 13.11.2016. The Discharge summary of this hospital clearly mentions “Patient is
known case of Spinocerebellar ataxia and operated for Acoustic Neuroma under follow up of Neurologist for
last 7 years”.
Subsequently, the patient Ms. Monica Aggarwal was admitted in Kailash Hospital on 30.12.2016 and
discharged on 25.01.2017. The Discharge summary again mentions that the patient “ Monica Aggarwal age 51
year Female, operated for CP angle Tumour (Acoustic Neuroma) in 2019 in Mumbai with Spinocerebellar
Ataxia, unable to walk since 2009, unable to speak since 4-6 months and swallowing disorder. Presented with
severe breathlessness, Aspiration Pneumonia”.
Again the discharge summary of Kailash Hospital for Ms. Aggarwal Hospitalization from 22.02.2017 to
25.02.2017 clearly underlines the fact that she suffered from Spinocerebellar Ataxia and had a past history of
Acoustic Neuroma (Operated). The same illness is mentioned in the Discharge summary of Kailash Hospital
for the hospitalisation of Ms. Aggarwal from 23.07.2017 to 25.07.2017.
Notwithstanding the plethora of evidence about the pre-existing disease of Ms. Aggarwal, the insurer has
chosen to repudiate the claim on the basis of Sir Ganga Ram Hospital Discharge summary (for hospitalisation
from 25.07.2017-06.09.2017). Does it say anything new? No. It says
“Diagnosis: Perforative peritonitis s/p PEG tube re-insertion in a follow up case of Spinocerebellar Ataxia”
“History: 52 yrs. Old female with diagnosis of Spinocerebellar Ataxia status surgery for Acoustic Neuroma
restricted to bed on percuteneous gastronomy developed fever with loose stools. She was evaluated at Kailash
Hospital with diagnosis of Intra Abdominal Abscess ( Perforation) now admitted for further management”.
To conclude, the insurer was fully aware of the medical conditions of Ms, Monica Aggarwal as every details
were mentioned in several Discharge certificates of different hospitals. In fact, they had paid the claim of the
complainant amounting to Rs. 1,87,954/- in September 2017. Therefore, it is not understood as to why they
have invoked the issue of PED this time to repudiate the claim in just 2 months in December 2017. This office
is inclined to agree with the claimant that this was done because the claim amount is much more than the one
paid by them in September 2017. The repudiation order of the insurer is arbitrary, totally unjustified, and is set
aside. Hence, the insurance company is directed to settle the entire claim excluding the deductions as per
policy terms and conditions to the complainant.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 12.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by both the parties during the course of hearing, the Insurance Company is directed to
settle the entire claim excluding deductions as per policy’s terms and conditions to the
Complainant.
The complaint is treated as disposed off accordingly.

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. TANMAY SHARMA V/S HDFC ERGO General Insurance Co. Ltd.
COMPLAINT REF. NO.: NOI-H-018-1920-0061
1.
Name & Address of the Complainant
Sh.Tanmay Sharma
S/O Sh.Shiv Prasad Sharma
503,Ganpati Dham,Mathura Road Agra,
Sikander Fatehpur,Agra,
U.P.282007.
Phone No.09871586754
2.
Policy No:
Type of Policy
Duration of policy/Policy period
S.I.
2825202227852400000
Health Suraksha Policy
03.06.2018 to 02.06.2019
Rs.7,50,000/-
3.
Name of the insured
Name of the policyholder
Sh.Tanmay Sharma
Sh.Tanmay Sharma
4.
Name of the insurer
HDFC ERGO General Insurance Co. Ltd.
5.
Date of Repudiation/Partial Settlement
N.A.
6.
Reason for repudiation/Partial Settlement
N.A.
7.
Date of receipt of the Complaint
06.06.2019
8.
Nature of complaint
Policy cancelled due to non-disclosure of PED
9.
Amount of Claim
N.A.
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
N.A.
12.
Complaint registered under
Rule no. of IOB rules,2017
13(1)f
13.
Date of hearing/place
13.11.2019 / NOIDA
14.
Representation at the hearing
i) For the Complainant
Tanmay Sharma, Self
j) For the insurer
Shweta Pokhriyal, AM-Legal
15
Complaint how disposed
Award
16
Date of Award/Order
11.12.2019
17) Brief Facts of the Case:-. Sh.Tanmay Sharma, the Complainant had taken Health Suraksha Policy
No.2825202227852400000 from HDFC Ergo for the period from 03.06.2018 to 02.06.2019 for the S.I. of
Rs.7,50,000/-. His policy was cancelled at the time of renewal due to non disclosure of Pre Existing Disease.
Aggrieved, he requested the Insurer including its GRO to reconsider the renewal of his policy but failed to
get any relief. Thereafter, he preferred a complaint to this office for resolution of his grievance.
18) Cause of Complaint:
a) Complainant’s argument : The Complainant stated in his complaint that he got his Insurance Policy
no.218301/48/2018/035 from The Oriental Insurance Co. Ltd.. In this policy, a PED of Ca Rectum was
clearly mentioned, but at the time of porting this policy to HDFC policy number 2825202227852400000,
they did not mention his PED. The complainant said that he was not asked to fill any proposal form and
the agent told him that all the details would be taken from the previous policy. But in 2019, when the
complainant was renewing the policy, he noticed that PED was not mentioned in his policy and when he
asked the customer care team, they told him that it is a fraud done by him and they are cancelling his
policy. The complainant raised grievance but he got in the reply that his policy stands cancelled due to
non disclosure of facts, but the complainant's question is that he had disclosed everything and he provided
the Oriental policy at the time of portability, so how he has not disclosed all the facts. The complainant
further stated that his policy is claim free for the last 3 years and now the Insurer is cancelling the policy
because of their mistake and even denying coverage to his family who were also a part of this family
floater policy.
b) Insurers’ argument: The insurer stated in their SCN that in the month of June, 2018, the complainant
approached the Company for porting his health insurance policy from The Oriental Insurance Co.Ltd.to
HDFC Ergo and submitted a copy of his previous policy bearing no.218301/48/2018/035 along with the
proposal form. The complainant did not disclose about the pre-existing disease (PED) while porting the
policy to HDFC Ergo. Accordingly, relying upon the representations and details mentioned in the
proposal form and the previous insurance policy, the company issued the policy vide Policy
No.2825202227852400000. The complainant claims that the proposer's PED (Ca Rectum) was disclosed
in the previous policy with The Oriental Insurance, the copy of the policy submitted by the complainant
states "N/A” against the PED column. On receipt of renewal request from the complainant, the Company
renewed the above mentioned policy vide Policy bearing No.2825202227852401000 effective from
03.06.2019 to 02.06.2020. It was only, at the time of renewal of the policy, when the complainant chose
to disclose the proposer's PED. The complainant's act of disclosing the PED, at the time of renewal, lend
to "Non-disclosure of material facts” and therefore the Company was constrained to cancel the policy and
refund the premium. It may also be mentioned that, had the complainant disclosed the PED at the time of
porting the policy to HDFC Ergo, the company would have declined to issue the policy. The complainant
concealed material facts during the term of the first ported policy with HDFC Ergo in June, 2018 and
continued to enjoy the benefits under the said policy. By concealing the material facts, the complainant
has breached the terms and conditions and therefore the renewal policy was cancelled as per condition
no.10 r (ii) ab initio and the total premium amount of Rs.15,976/- was refunded by the Company.

19) Reason for Registration of Complaint:- Policy cancelled due to non-disclosure of PED
20) The following documents were placed for perusal.
a) Policy with terms and conditions.
b) Complaint copy
c) SCN
d) Annex VI A
21) Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. The Insurance Company
reiterated that the Insured had approached the insurer in the month of June, 2018 to port his 2 years old policy
of The Oriental Insurance Company Ltd.. At the time of porting the policy, he did not disclose his PED (Ca
Rectum) to the Insurance Company. Accordingly, relying upon the representations and details mentioned in
the proposal form and the previous insurance policy, the company issued the policy. On the other hand, the
Complainant reiterated that PED of Ca Rectum was clearly mentioned in his policy of The Oriental Insurance
Co. Ltd.., but at the time of porting this policy to HDFC, they did not mention his PED. The complainant
said that at the time of renewing the policy, he noticed that PED was not mentioned in his policy and when he
asked the customer care team, they told him that it was a fraud done by him and they are cancelling his
policy. The complainant stated that he had disclosed everything and he provided the Oriental policy at the
time of portability. The complainant further stated that his policy is claim free for the last 3 years. The
Insurer is cancelling the policy because of their own mistake and even denying coverage to his family who
were also a part of this family floater policy.
The Insurance Company stated that the proposer's PED (Ca Rectum) was not disclosed in the copy of the
policy submitted by the complainant to them. The policy states "N/A” against the PED column. On receipt
of renewal request from the complainant, the Company renewed the policy. After the renewal, the
complainant chose to disclose the proposer's PED. The complainant's act of disclosing the PED, at the time
of renewal, warrants to "Non-disclosure of material facts” and therefore the Company was constrained to
cancel the policy and refund the premium. It may also be mentioned that, had the complainant disclosed the
PED at the time of porting the policy to HDFC Ergo, the company would have declined to issue the policy.
I have examined the documents exhibited and oral submissions made by both the parties. It is observed that
the Complainant himself pointed out the discrepancy in the policy regarding his PED. During the course of
hearing on 13.11.2019, the insurer requested for time to verify the previous policies from the Oriental
Insurance Co. Ltd. which was acceded to.
On 09.12.2019, we received the mail from the Insurer wherein they have clarified that they have re-verified
the documents as filed by the customer. During re-verification of documents, it was found by the Insurer that
the previous year policy schedule as provided by the customer did not disclose the PED. At the time of
hearing, it was directed to the HDFC Ergo that they would verify the previous policies from the previous
Insurer i.e. The Oriental Insurance Company but HDFC Ergo has failed to do the same. The copy of the
policy of Oriental Insurance Company, submitted by the HDFC Ergo does not have the signature and seal of
Oriental Insurance Company whereas the copy of the same policy submitted by the complainant bears the
seal and signature of the Oriental Insurance Co. and the mention of PED also. Hence, insurer’s decision to
cancel the policy is not justified and is set aside. The Insurer is directed to restore the policy with continuity
benefits.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 11.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C. S. PRASAD
CASE OF RANJITA KRISHNA V/S MAX BUPA HEALTH INSU. CO LTD.
COMPLAINT REF: NO: NOI-H-003-1920-0136
1.
Name & Address of the Complainant
RANJITA KRISHNA
104-C , SUPER MIG FLATS
EXPRESS WAY APARTMENTS , SECTOR -93
NOIDA U.P.-201304
AWARD
Taking into account the facts and the submissions made by the insurer during the course
of hearing, the insurer is directed to restore the policy with continuity benefits.
The complaint is treated as disposed off accordingly.

2.
Policy No:
Type of Policy
Duration of policy/Policy period
30537024201802
HEALTH
3.
Name of the insured
Name of the policyholder
Ranjita Krishna
Sushila Krishna
4.
Name of the insurer
MAX BUPA HEALTH INSURANCE CO.
5.
Date of Rejection
18-03-2019
6.
Reason for rejection
Repudiation for non disclosure of pre existing disease
7.
Date of receipt of the Complaint
3-07-2019
8.
Nature of complaint
Reudiation
9.
Amount of Claim
56700.00
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Settlement of medical Bill and reinstatement of policy
12.
Complaint registered under
IOB rules
Yes
13.
Date of hearing/place
18-12-2019/ NOIDA
14.
Representation at the hearing
k) For the Complainant
Ms. Ranjita Krishna
l) For the insurer
Mr. Bhuwan Bhaskar
15
Complaint how disposed
Award
16
Date of Award/Order
30.12.2019
17 . Brief Facts of the case :
The policy holder Sushila Krishna purchased a health policy on 16-06-2016 for Rs. 30,00,000/ for herself and her
three daughters. On 16/02/2019 Ranjita was taken to hospital with complaint of pain in abdomen on and off. She
was admitted to hospital , and on the same day she was operated for cholelithiasis, and after post operative care,
she was discharged on 17-02-2019. The complainant submitted the Bill for payment but the insurer rejected the
claim stating the assured is known case of Diabetis and colloid nodule since 2015. The complainant has approached
Ombudsman Office on 3-07-2019 for settlement of claim.
18. Cause of the complaint:
A. Complainant’s argument :The complainant says that she was covered for insurance since June 2016. The
complainant went to AIIMS on 18-12-2018 for abdomen pain and was diagnosedwith 10 mm stone in her gall
bladder. She got herself admitted in Yatharth Hospital on 16 February 2019 for Gall Bladder removal and after
operation she was discharged on 17 February 2019. The investigating officer of Max Bupa stated in his report that
complainant was suffering from Diabetes Mellitus II and colloid Nodule since 2015. The insurance policy is
maintained by policy holder since 2016. The Insurer rejected the claim stating that the pre existing disease was not
disclosed to the insurer .The complainant says she did not have such disease in 2015 . Hence she wants payment of
the claim.
B. Insurer’s argument : Policy was running since 2016 . The complainant had submitted a bill for her treatment in
Yatharth Hospital from 16/02/2019 to 17/02/2019 for cholecystectomy. While reviewing the treatment papers it was
observed that Complainant went to AIIMS on 18/12/2018 for problem of abdomen pain related to Gall bladder. At
that time it was revealed that complainant was suffering from DM II and colloid nodule since 2015 . On the basis on
non disclosures of material facts, the claim was rejected by the insurer.
19. Reason for Registration of Complaint:
Repudiation of claim for non disclosure of previous health problem.
20. Following documents were placed for perusal:
1. Complaint letter.
2. Medical treatment papers
3. SCN
21. Observation and conclusion :
Both the parties appeared for personal hearing and reiterated their submissions. The complainant, Ms Ranjita
Krishna was admitted to Yatharth Hospital on 16-02-2019. When claim was submitted to the insurer, they had
rejected the claim stating that treatment papers of AIIMS of 18-12-2018 show that the complainant was suffering
from DM II and colloid Nodule since 2015 and policy was purchased in 2016. On reviewing again it was clear that
period of DM II was after two years of policy issued to assured. The insured reviewed the case again and
confirmed that a mistake was done on their part. The insurer agreed to release the payment and to reinstate the
policy.
The insurer is directed to release the claim amount under request No 405460 and reinstate the policy as agreed
during th hearing on 18-12-2019.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the Insurance company is directed to pay the
claim amount to the complainant and reinstate the policy number 30537024201802..
The complaint is disposed accordingly.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 30.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C. S. PRASAD
CASE OF NEERAJ PRAKASH V/S MAX BUPA HEALTH INS. CO LTD.
COMPLAINT REF: NO: NOI-H-003-1920-0134
1.
Name & Address of the Complainant
NEERAJ PRAKASH
FLAT NO-114, PATRAK AR PARISAR, SECOTR-5
VASUNDHARA GHAZIABAD
U.P.-201012
2.
Policy No:
Type of Policy
Duration of policy/Policy period
515732201903
HEALTH
3.
Name of the insured
Name of the policyholder
Divyansh Srivastava
Angika Kumari
4.
Name of the insurer
MAX BUPA HEALTH INSURANCE CO.
5.
Date of Rejection
5-09-2019
6.
Reason for rejection
Repudiation for non disclosure of pre existing disease
7.
Date of receipt of the Complaint
13-09-2019
8.
Nature of complaint
Repudiation
9.
Amount of Claim
46870.00
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Settlement of claim and reinstatement of policy
12.
Complaint registered under
IOB rules
Yes
13.
Date of hearing/place
18-12-2019/ NOIDA
14.
Representation at the hearing
m) For the Complainant
Mr. Neeraj Prakash
n) For the insurer
Mr. Bhuwas Bhaskar
15
Complaint how disposed
Award
16
Date of Award/Order
30.12.2019
17 . Brief Facts of the case : The policy holder Angika Kumari purchased health policy in March 2016 for Rs.
5,00,000/ for herself and her husband Mr. Neeraj Prakash. Their son “Divyansh ” was born on 28/11/2016 and they
got him added in their policy in year 2018-19. Their son was patient of down’s syndrome since birth but it was not
recorded in the policy. On 21-04-2019 Divyansh fell ill and was taken to hospital and was admitted with problem of
bilateral pneumonia. He was discharged after 4 days in stable condition on 25-04-2019. The Complainant submitted
papers to the insurer for settlement of claim but insurer has rejected the claim for non disclosure of material facts.
On 15-07-2019, complainant has approached Ombudsman Office for settlement of the claim.
18. Cause of the complaint:
A. Complainant argument : Complainant got added the name of their son “Divyansh” ( born on 28-11-2016) in
their old running policy with Max Bupa in year 2018-19. The child was suffering with down’s syndrome since birth.
Complainant says that they had given papers of Divyansh health problem to the agent but insurer says that no such
paper was submitted by insured. On 21-04-2019 Divyansh was admitted to hospital with problem of bilateral
pneumonia and complainant has submitted certificate from treating Doctor that pneumonia does not have any
connection to the old health problem. The Insurer rejected the claim stating that the pre existing disease down’s
syndrome was not disclosed to the insurer. The complainant wants payment of the claim.
B. Insurer’s argument : Policy was running since 2016 and the name of policy holder’s son Divyansh was added
to the policy in 2018. The insurer says that the complainant had willfully not disclosed the existing medical
condition of their child while including him in the subject policy. The cashless facility was denied by the insurer on
the basis of adverse medical condition down’s syndrome. The grievance cell also rejected the claim as this is a major
problem which was to be disclosed earlier.
19. Reason for Registration of Complaint:
Repudiation of claim for non disclosure of previous health problem.
20. Following documents were placed for perusal:
1. Complaint letter.
2. Medical treatment papers
3. SCN
21. Observation and conclusion :
Both the parties appeared for personal hearing and reiterated their submissions. The complainant Mr. Neeraj Prakash
stated the name of their son Divyansh was included in their pre-existing in the 2018-19. The papers of down’s
syndrome disease of their son were given to the agent. As per insurer no such paper was submitted by the agent.
During the hearing the insured submitted the e-mail dated 26-03-2018, the date of renewal of policy, sent to the
agent M D Sharma, giving him details of his son’s condition. The conversation between M D Sharma and the
complainant , brought by the complainant was also heard during the hearing , by which it is clear that the
complainant had given papers to the agent and the agent had forwarded the same to the insurer.
I have examined the documents exhibited as evidence and oral submissions made by both the parties. It is clear that
the papers of insured’s disease were given to the agent , who has been giving service to their policy since 2016.
The complainant is advised to submit the claim reimbursement papers to the insurer within a week . The insurer
shall settle the claim and review the cancellation of policy favorably.

AWARD
Taking into account the facts and circumstances of the case and the submissions made by both the parties
during the course of hearing, the Insurance company is directed to pay the claim amount to the complainant
and consider to reinstate the policy number 30515732201903.
The complaint is treated as closed accordingly.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 30.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C. S. PRASAD
CASE OF VARUN BANSAL V/S MAX BUPA HEALTH INSU. CO LTD.
COMPLAINT REF: NO: NOI-H-003-1920-0136
1.
Name & Address of the Complainant
VARUN BANSAL
271/6 THAPAR NAGAR
NEAR ARYA SAMAJ MANDIR , MEERUT
U.P. - 250002
2.
Policy No:
Type of Policy
Duration of policy/Policy period
30106392201806
HEALTH
12-06-2012
3.
Name of the insured
Name of the policyholder
Ajay Kumar
Ajay Kumar
4.
Name of the insurer
MAX BUPA HEALTH INSURANCE CO.
5.
Date of Rejection
10-09-2019
6.
Reason for rejection
Repudiation for non disclosure of pre existing disease
7.
Date of receipt of the Complaint
23-09-2019
8.
Nature of complaint
Repudiation
9.
Amount of Claim
10,00,000/-
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
10,33,084/-
12.
Complaint registered under
IOB rules
Yes
13.
Date of hearing/place
18-12-2019/ NOIDA
14.
Representation at the hearing
o) For the Complainant
Mr. Varun Bansal
p) For the insurer
Mr. Bhuwan Bhaskar
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17 . Brief Facts of the case : The complainant’s father, late Sh. Ajay Kumar had purchased the health policy from Max
Bupa Health Insurance Company on 12-06-2012, with insurance cover of Rs. 25 lacs, annual premium Rs. 77983/- for him
and his wife. He had maintained the policy by regular payment of premium. Mr. Ajay Kumar was admitted to Medanta
Hospital for installation of ICD-D instrument in September 2018. He had submitted his treatment Bill of Medanta Hospital
to Insurance company for settlement of the claim. The insurer has rejected the claim stating that Mr. Ajay Kumar was
suffering from HTN and CAD from last 8-10 years. The Complainant says that there was no such medical history of HTN
and CAD 8-10 years back. The complainant has approached the Ombudsman Office on 23-8-2019 for settlement of the
claim.
18. Cause of the complaint:
A. Complainant’s argument :
The complainant urged that his father, the policy holder Mr. Ajay Kumar had this policy with Max Bupa Insurance
Company since 2012. In September 2018, the assured suffered from chest pain sweating and weakness. He was
admitted to Jaswant Rai Hospital, Meerut, and after treatment for 3 days he was discharged. The Insurer settled the
claim and paid Rs. 45,000/- to the insured. After 4 days of discharge, he had a major health problem and was
referred to Medanta Hospital. Mr. Ajay Kumar was admitted to hospital of 28
th
September and after installation of
AICD device, discharged on 3
rd
October2018. The cost of this instrument was around 10 lacs. This time the claim
was rejected by the insurer stating that the assured had HTN and CAD for the last 8-10 years. The complainant has
alleged that the claim of Rs. 45,000/- was paid by insurer for heart related problem but for payment of Bill above
Rs. 10 lacs the insurer is giving false excuses. The claim is pending from last one year. The complainant informed
that the assured Mr. Ajay Kumar expired on 12-06-2019.
B. Insurer’s argument :
Insurer has stated in their SCN that assured Mr. Ajay Kumar was under medical cover with Max Bupa Company
since June 2012 for Rs. 25 lacs . The complainant had submitted the Bill for treatment of Mr. Ajay Kumar from 28-
09-2018 to 3-10-2018 and the insurer has rejected the claim stating that assured was suffering from HTN for 8-10
Years, CAD for 11 Years. The insurer has attached the report of Prakash Neuroroly Center which is showing HT
since 8-10 Years. Insurer has also submitted papers of his Visit to Center for sight where HTN is shown since 8-10
Years. The insurer has rejected the claim for non disclosure of HTN and CAD before purchasing policy.

19. Reason for Registration of Complaint:
Repudiation of claim for non disclosure of previous health problem.
20. Following documents were placed for perusal:
1. Complaint letter.
2. Medical treatment papers
3. SCN
21. Observation and conclusion :
Both the parties appeared for personal hearing and reiterated their submissions. The policy was purchased by the life
assured in the year 2012. In September 2018, the assured was admitted to Medanta Hospial for installation of Pace
maker for his heart problem. The insurer has rejected the claim, stating that they have found that he was suffering
from HTN and CAD since last 8-10 years. The complainant has urged that the claim of Rs. 45,000/- for the heart
problem was released to him for 4 days treatment in Jaswant Rai Hospital in September 2018.. After discharge from
Jaswant Rai Hospital the heart problem was aggravated and the pace maker was installed in Medanta Hospital to
resolve the heart problem .
The Policy has run for more than 6 years and exact period of inception of HTN and also treatment papers related to
HTN have not been adduced as proof that assured was having disease before purchasing the policy. On the other
hand the complainant has submitted the certificate of the Doctor treating the assured that the treatment of MI was
started in September 2016. Thus the insurer’s contention that the assured was suffering from CAD is not proved.
Moreover, the insurer was fully aware of the assured’s heart problem which is proved by the fact that they had paid
him claim of Rs. 45,000/- only in September 2019. Repudiation is set aside as being arbitrary.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the repudiation of the claim could not be
justified and is set aside, The Insurance company is directed to pay the claim amount Rs.
10,33,084/- to the complainant.
The complaint is treated as closed accordingly.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C. S. PRASAD
CASE OF RUCHI TAILONG V/S MAX BUPA HEALTH INSU. CO LTD.
COMPLAINT REF: NO: NOI-H-003-1920-0178
1.
Name & Address of the Complainant
RUCHI TELANG
H NO-1522 PARK VIEW APARTMENT
SECTOR -29 NOIDA U.P.- 201301
2.
Policy No:
Type of Policy
Duration of policy/Policy period
0198061380
HEALTH
14-03-2012
3.
Name of the insured
Name of the policyholder
Anurag Telang
Anurag Telang
4.
Name of the insurer
MAX BUPA HEALTH INSURANCE CO.
5.
Date of Rejection
21-03-2019
6.
Reason for rejection
Rejection for non disclosure of pre existing disease
7.
Date of receipt of the Complaint
23-09-2019
8.
Nature of complaint
rejection
9.
Amount of Claim
1,71,310.00
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
12.
Complaint registered under
IOB rules
Ys
13.
Date of hearing/place
18-12-2019/ NOIDA
14.
Representation at the hearing
q) For the Complainant
Ms. Ruchi Telang
r) For the insurer
Mr. Bhuwan Bhaskar
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17 . Brief Facts of the case : The complainant Mrs. Ruchi Telang’s husband Mr. Anurag Telang had purchased this policy
on 14-03-2012, with the cover of Rs. 5,00,000/- with Max Bupa Company. Mr.The Anurag Telang was admitted to

Bhardwaj Hospital with the problem of Cerebrovascular accident and shifted by taking LAMA to Max Hospital on 14-03-
2019. There it was diagnosed that assured was suffering from malignant left MCA infract. The insurer had approved the
cashless amount of 1.98 lacs but later the insurer had denied the payment of the same. The complainant shifted the patient
to Safadarjang by taking LAMA, because they could not afford high medical expenses. The insurer had rejected the claim
for non disclosure of material fact. Now, complainant has approached Ombudsman Office for solution.
18. Cause of the complaint:
A. Complainant’s argument :
The complainant has urged that the policy was purchased in year 2012. As per complainant’s statement, the policy
was taken with declaration of DM II and HTN . Her husband suffered with CVA on 14-03-2019 and was first
admitted in Bhardwaj Hospital, and later on the same day, shifted to Max Hospital. He was diagnosed with left
MCA infract. The insurer initially approved the cashless claim of Rs. 1,98,000/- but later withdrew the permission
and asked the complainant to file the reimbursement of claim, which also was denied. The complainant submitted
that the treating doctor had clarified that in their case, the disease could happen to any person not having Diabetes
or HTN, and as such no conclusive reason can be attributed to the cause of the disease. The rejection is not justified
and she wants the settlement of the claim.
B . Insurer’s argument
The insurer has stated in their SCN that the complainant was asked to submit the treatment record from Bhardwaj
Hospital. She was also asked to submit the photograph & ID of patient, case summary , exact duration of DM and
HTN and discharge summary of CABG, and also last 5 days treatment details of the patient. As per the insurer, the
required information were not provided by the complainant. After non receipt the required information, the insurer
scrutinized the case and repudiated, stating absence of treatment papers of Bhardwaj Hospital and cause of MCA
infract. The authenticity and accomplishment of document for claim procedure not established hence claim could
not be paid.
19. Reason for Registration of Complaint:
Rejection of claim for non disclosure of previous health problem.
20. Following documents were placed for perusal:
1. Complaint letter.
2. Medical treatment papers
3. SCN
21. Observation and conclusion :
Both the parties appeared for personal hearing and reiterated their submissions. The complainant stressed that her
husband is having a health insurance policy with the respondent insurer since 14-03-2012. Her husband suffered
with CVA on 14-03-2019, and was first admitted in Bhardwaj Hospital and later on the same day shifted to Max
Hospital. He was diagnosed with left MCA infract. The insurer initially approved the cashless claim of Rs.
1,98,000/- but later withdrew the permission and asked the complainant to file the reimbursement of claim, which
also was denied. She has complained only for the payment of claim pertaining to admission of her husband in Max
Hospital form 14-03-2019 to 21-03-2019.
The insurer submitted that the cashless permission was withdrawn for the want of treatment record from Bhardwaj
Hospital. Later the reimbursement of claim was denied due to the fact that as per the policy document diseases
related to DM-II and Hypertension were permanently excluded. The insurer maintained that MCA infract was
caused due to hypertension.
I have gone through the records and observe that the complainant’s husband, while taking insurance policy, had
declared DM-II & HTN as pre existing diseases. Consequently, treatment for diseases relating to DM-II & HTN
were permanently excluded from the scope of the policy. However, it is noticed that Dr. Ashish Jaiswal has certified
vide his letter dated 7-08-2019 that MCA infract can be caused by many risk factors including DM-II & HTN.
Another certificate dated 20-03-2019 by the treating doctor, Dr. Prakash Singh has also certified that the cause of
CVA in this patient is left internal carotid artery atherosclerotic disease which is not excluded. In view of specific
evidence provided by the complainant in the form of two certificates, the decision of the insurer to repudiate the
claim is not justified. The insurance company is directed to settle the claim as per other terms and conditions of the
policy.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the Insurance company is directed to pay the
claim amount to the complainant.
The complaint is treated as closed accordingly.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. YATINDER SINGH CHAUHAN V/S RELIANCE GENERAL INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-035-1920-0167
1.
Name & Address of the Complainant
Mr. Yatinder Singh Chauhan,
Flat No. 17-A/201, Vasundhara, Ghaziabad,
UP-201012.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
131691928451000018
BOI-Swasthya Bima Policy
13.03.2019 to 12.03.2020
3.
Name of the insured
Name of the policyholder
Yatinder Singh Chauhan
Yatinder Singh Chauhan
4.
Name of the insurer
Reliance General Insurance Co. Ltd.
5.
Date of Repudiation
30.07.2019
6.
Reason for repudiation
As per Policy Clause 5.1 – 2 : non disclosure of
PED.
7.
Date of receipt of the Complaint
03.09.2019
8.
Nature of complaint
Rejection of Claims
9.
Amount of Claim
Rs. 4,52,115/- (as per Annex. VI A)
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Rs. 4,52,115/-
12.
Complaint registered under IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019 at Noida
14.
Representation at the hearing
s) For the Complainant
Mr. Dharvendra Singh Chauhan, Brother
t) For the insurer
Ms. Priyanka Singh, Legal Manager,
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
Brief Facts of the Case: This complaint is filed by Mr. Yatender Singh Chauhan against M/s Reliance General
Insurance Co. Ltd. for rejection of his hospitalization claims.
17) Cause of Complaint:
a) Complainant’s argument: The complainant stated that he was covered under health insurance policy from
Reliance General Ins. Co. Ltd. under tie-up with Bank of India for the period from 13.03.2019 to 12.03.2020. This
policy was in continuation of National Insurance Co. Ltd. – BOI National Swasthya Bima from the year 2010. This
policy was discontinued by National Insurance Co. Ltd., and accordingly the policy was ported with Reliance
General Ins. Co. He was hospitalized on 09.06.2019 on complaints of uneasiness, sweating and anxiety, at
Vasundhara Hospital, Ghaziabad. He was discharged on 10.06.2019. The total bill amount was Rs. 15,323/- which
paid by him to the hospital. Dr. Dave of Vasundhara Hospital advised him spine surgery after examining the MRI
report. Later on, he submitted the claim bill for reimbursement but the insurance company rejected the claim for
non-disclosure of PED of HTN and DM. The complainant stated that he had not been diagnosed these diseases
before issuance of policy from them. Even, he was covered under medical policy with previous insurer for the last
nine years; all pre-existing diseases would have been automatically covered. The complainant then consulted Dr.
Kalra, Spine Surgeon, of Sir Ganga Ram Hospital, who also recommended spine surgery. He was admitted in
SGRH on 03.07.2019 and was discharged on 08.07.2019. His pre-authorization request was denied, so he submitted
claim form for reimbursement of hospitalization bill with all medical documents. The insurance company rejected
this claim also on the same ground of PED. He approached this Forum for settlement of claim bills for Rs.
4,52,115/-.
b.) Insurers’ argument: The insurance company in their SCN stated that the complainant was insured with them
from 13.3.2019 to 12.3.2020. He felt some uneasiness, sweating and anxiety and went to Vasundhara Hospital on
09.06.2019. He was admitted there and was diagnosed with HT/DM/Neuropathy/Lumber spondylosis/scoliosis with
radioculopathy/to rule out CAD/Accelerated Hypertension. On perusal of claim documents of Vasundhara Hospital
it was found that the complainant was a patient of Hypertension and Diabetes which was not disclosed by him at
the time of filling in the proposal form. The claim was rejected on the ground of non-disclosure of pre-existing
diseases. The complainant was again hospitalized at Sir Ganga Ram Hospital on 03.07.2019 for surgery. He was
discharged on 08.07.2019. He sent claim another for reimbursement of hospital expenses. The insurance company
appointed investigator. As per the questionaire filled by Dr. Girjesh Rustagi, the complainant was a known case of
hypertension and DM and was on medication from last 3 years. This fact was not disclosed by the complainant in
proposal form on 13.3.2019, at the time of taking policy, the insurance company repudiated the claim and cancelled
the policy as per Clause 5.1 clause 3 of general policy terms and conditions.
18) Reason for Registration of Complaint: Repudiation of claim.
20) The following documents were placed for perusal.
a) Complaint letter/Form VIA
b) Survey Report
c) Policy document
d) SCN
19) Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant’s brother stated that his brother, Mr. Yatinder Singh Chauhan, was covered
under BOI National Swasthya Bima for the past nine years. After the National Insurance had
withdrawn/terminated this policy, the Bank of India ported the policy with Reliance General Insurance

Company. His brother was hospitalized for spine surgery in Sr. Ganga Ram Hospital but the insurance company
not only denied the cashless facility but also repudiated the reimbursement claim, on the ground of non-
disclosure of HTN and DM as pre-existing disease. The insurance company reiterated that the current policy
was ported with their company, but the complainant did not disclose the material fact of pre-existing disease
that he was suffering from HTN and DM. The investigator appointed by their company, during the
hospitalization period, revealed the fact that the complainant was a known case of hypertension and DM and
was on medication from the last three years. He did not disclose the fact at the time of proposing for insurance
cover; hence they repudiated the claim as per terms and conditions of the policy.
On going through the documents exhibited and the oral submissions made by both the parties during the hearing,
it is noted that the complainant was covered under health insurance policy for the last 9 years from National
Insurance Company Ltd. This policy was withdrawn by National Insurance, so the Bank of India ported his
policy from National to Reliance General on 13.03.2019. The complainant was for the first time diagnosed with
HT and DM at Vasundhara Hospital on 09.06.2019 i.e. after the inception of policy. Secondly, the Discharge
Summary of SGRM dated 8.7.2019 does not show any past history of HT/DM, and his physical examination of
BP shows 120/80. In fact, the certificate of Dr. K.L. Kalra of SGRH also certifies that the complainant came with
c/o pain in back and neurogenic claudicatios since 1 year. He was taking self medication including painkillers
and did not consult any doctor. As per MRI Scan, he was found to have severe Stenois and was advised surgery.
Further, it is noted that the claim is for spine surgery which has nothing to do with hypertension and diabetes
which are life style diseases.
The complainant was covered in mediclaim policy for the last nine years. It has been mentioned in the Circular
issued by Health Cell, Head Office, National Insurance Co. Ltd. that: “We wish to assure policyholders that, on
migration, continuity benefits, as applicable will be extended. Similarly IRDAI portability norms shall apply in
case of change of insurer.” In this case, all his pre-existing diseases would automatically be covered under
portability clause as he was insured for the last 9 years. The insurance company has wrongly repudiated the
claim. The insurance company is directed to settle the claim as per the terms and conditions of the policy.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. AMIT SINHA V/S RELIGARE HEALTH INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-037-1920-0145
1.
Name & Address of the Complainant
Sh. Amit Sinha,
A-61, Sector-51, Opp. Parkview Apartment,
NOIDA-201301
2.
Policy No:
Type of Policy
Duration of policy/Policy period
10562856
Health
We.f. 03/05/2019 Till 02/05/2020
3.
Name of the insured
Name of the policyholder
Sh Amit Sinha
Sh. Amit Sinha
4.
Name of the insurer
Religare Health Insurance Company Limited
5.
Date of Repudiation
26/06/2019
6.
Reason for repudiation
Denial of Health Claim
7.
Date of receipt of the Complaint
29/07/2019
8.
Nature of complaint
Denial Of Health Claim
9.
Amount of Claim
124000/-
10.
Date of Partial Settlement
nil
11.
Amount of relief sought
124000/-
12.
Complaint registered under
IOB rules
YES
13.
Date of hearing/place
20.12.2019
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company is directed to pay the claim as per the terms and
conditions of the policy.
The complaint is closed accordingly.

14.
Representation at the hearing
u) For the Complainant
Sh. Amit Sinha
v) For the insurer
Sh Pratyush Prakash
15
Complaint how disposed
Dismissed
16
Date of Award/Order
31/12/2019
17) Brief Facts of the Case : This is a complaint filed by Sh Amit Sinha against Religare Health Insurance
Co.Ltd., relating to denial of health claim under policy no. 10562856.
18)Cause of Complaint:-Denial of health claim by the insurance company.
a) Complainants argument :- The complainant had taken health insurance policy No.10562856 from the above
company wherein insurance coverage was given for sum Assured of Rs.700000/- to the complainant , his
spouse and daughter w.e.f. 30/03/2016 Till 29/03/2018 and the policy was further renewed on yearly basis till
02/05/2020. The said policy was ported from Royal Sundram Alliance Gen. Ins. Co. Ltd. The insured was
admitted on 24/06/2019 for ailment of ACUTE CALCULUS CHOLECYSTITIS in Indraprastha Apollo
Hospital, Sarita Vihar, New Delhi. But, the insurance company rejected the request for cashless
hospitalization facility and stated that “NON DISCLOSURE OF MATERIAL FACTS/PRE-EXISTING
AILMENTS AT TIME OF PROPOSAL – H/O HTN BEFORE INCEPTION OF POLICY.
.
b) Insurers’ argument:- The insurance company vide their SCN dated 04/10/2019 submitted that the insured
had taken a Health insurance policy form the Insurance company. The said policy was ported from Royal
Sundram Alliance Gen Ins. Company and further, renewed till 02/05/2020. During the continuation of the
policy, the complainant approached to insurance company to avail the cashless facility for hospitalization at
Indraprastha Apollo Hospital, New Delhi on 24/06/2019 for 2 days with complaint of Gall Stone since 30 days.
The complainant was primarily diagnosed with Gall Stone and was admitted for surgical treatment i.e.
Laparoscopic/Open Cholecystectomy. As per the attending doctor`s assessment, the complainant was the
patient of Hypertension and was under medication . As per the clinical chart initial assessment sheet of
Hospital, the complainant was the patient of Hypertension since 4 years. Thus, in the light of the above noted
observation of doctor, it was concluded that insured did not disclose PED at the time of policy inception. The
cashless facility was rejected by the company vide letter dated 26/6/2019 as per terms and conditions in
accordance with clause 7.1 Non-disclosure of Material Facts/ Pre-existing decease at the time of proposal. The
complainant had the opportunity to disclose the pre-existing decease i.e. Hypertension prior to policy inception.
19)Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN
21) Observations and Conclusion: - Both the parties attended the hearing of 20.12.2019. The complainant, stated
that he had sent a request to insurance company for approval of cashless hospitalization facility on 24/6/2019 which
was denied by the insurance company on the grounds of non-disclosure of pre-existing disease – hypertension. The
complainant has submitted a copy of judgement of State Consumer Fourm,Delhi, in the case of New India
Insurance Company vs Shiv Kumar wherein, it was held by Justice J.D.Kapoor, President that malaise of
hypertension, diabetes, occasional pain, cold, headache, arthritis and like in the body are normal wear and tear of
modern day life which is full of tension at the place of work, in and out the house and are controllable on day to
day basis by standard medication and can not be used as concealment of pre-existing disease for repudiation of the
insurance claim unless the insured in the near proximity of taking of the policy is hospitalized or operated upon for
the treatment of these diseases or any other disease. The complainant clarified that he has since received its claim
from his corporate policy but insisted on compensation for mental agony caused to him by the insurer.
I have examined the document exhibited as evidence and written and oral submission made by both the parties and
observe that the deficiency in service is evident on the part of the insurer. But, since the complainant has been
indemnified by another insurer, it would be against the principles of insurance to order payment of another claim on
the same incident. However, insurer is advised to exercise more customer, sensitivity while settling the claim.
The complaint is dismissed.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties during the course of hearing, the complaint is dismissed.

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. SHYAM SUNDER PACHORI V/S THE ROYAL SUNDARAM GENERAL INSURANCE
COMPANY LTD.
COMPLAINT REF: NO: NOI-H-038-1920-0122
1.
Name & Address of the Complainant
Mr. Shyam Sunder Pachori
50B, Ganesh Nagar, Lawyers Colony, Agra,
UP-282005.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
PLB00048400000100
Lifeline Supreme Health Plan
25.07.2018 to 24.07.2019
3.
Name of the insured
Name of the policyholder
Mr. Anshu Pachori
Mr. Shyam Sunder Pachori
4.
Name of the insurer
Royal Sundaram General Insurance Co. Ltd.
5.
Date of Repudiation
Not repudiated
6.
Reason for repudiation
Not repudiated
7.
Date of receipt of the Complaint
05.07.2019
8.
Nature of complaint
Partial payment of claim
9.
Amount of Claim
Rs. 1,29,607/- as per complaint
10.
Date of Partial Settlement
Rs. 3,900/- on 30.04.2019
11.
Amount of relief sought
Rs.1,29,607/-
12.
Complaint registered under IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019
14.
Representation at the hearing
w) For the Complainant
Mr. Shyam Sunder Pachori, Self
x) For the insurer
Mr. Amit Upadhayay, Asstt. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. Shyam Sunder Pachori against Royal Sundaram
General Insurance for partial payment of accident claim of his son, Mr. Anshu Pachori.
18) Cause of Complaint:
a) Complainant’s argument: The complainant ported his family health insurance policy from New India
Assurance Co. to Royal Sundaram General Insurance Co. vide policy no. PLB00048400000100 which was
issued for the period from 25.07.2018 to 24.07.2019 – Lifeline Supreme Health Plan, for the sum insured of Rs.
5 lakhs. His son, Mr. Anshu Pachori met with the road accident on 19.09.2018 and sustained facial injury. He
was immediately admitted in People’s Heritage Hospital from 19.9.2018 and was discharged on LAMA on
21.09.2018, as no dentist was available in this hospital. He consulted Dr. Harpreet, Dental Specialist of Total
Dental Care & Implant Centre, Agra for dental treatment. After medical investigation/tests, it was found that
due to road accident, seven teeth and teeth bones were fractured and damaged. Dr. Harpreet recommended that
at this stage, he would straighten the fractured bones and after their development, may be after a period of five
months, teeth implant could be done. The complainant informed this status to the insurance company vide his
email dated 08.12.2018. After the development of teeth bones, Dr. Harpreet implanted teeth on 12
th
and 16
th
march, 2019. The complainant submitted claim bills to the insurance company for reimbursement but the
insurance company repudiated the claim on the ground of prescribed time limit of post-hospitalization treatment
upto 90 days from the date of discharge from the hospital. The complainant pleaded that the whole dental
treatment was carried on OPD basis with Dr. Harpreet as dental treatment of his son could not be done at
People’s Heritage Hospital due to non-availability of dental surgeon there. He requested for reimbursement of
Rs.1,29,607/- paid by him for the said treatment.
b) Insurers’ argument: The insurance company in their SCN dated 12.12.2019 stated that the complainant
preferred reimbursement claim for hospitalization of his son for treatment of facial injury due to Road Traffic
Accident for the period of hospitalization from 19.09.2018 to 21.09.2018 for Rs. 17,778/-. This claim was paid
to him for Rs. 16,908/- towards full and final settlement on 28.12.2018. Subsequently, the complainant
preferred second reimbursement claim on 05.04.2019 for Rs.1,33,507/- with regard to pre-post hospitalization
expenses. This claim was settled for Rs. 3,900/- after necessary deductions. The claim settlement voucher dated
05.05.2019 was sent to the complainant. The insurance company could not consider the claim amount of
Rs.1,29,607/- as they were incurred or fall beyond the period stipulated for considering as post hospitalization
expenses as per the policy term which was 90 days as per the plan variant (Supreme) opted by the complainant.
Further, the insurance company stated that the post hospitalization treatment was done on OPD basis which was
not covered under the policy as per policy exclusion E XXIII – OPD treatment is not covered. It was submitted
that as per the policy terms and conditions the company would be liable to pay only for expenses related to
surgical procedures with regards Dental/Oral treatments only when the treatment was undertaken on inpatient
basis whereas, in the current claim the post hospitalization claim for Rs. 1,26,000/- was for implants which was
not covered as per the definition of dental/oral treatment under the policy.

19) Reason for Registration of Complaint: - Repudiation of claim
20) The following documents were placed for perusal.
a) Complaint letter/Form VIA
b) Insurance Policy
c) SCN
d) Medical papers
21) Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant stated that his son, Mr. Anshu Pachori, met with road accident on 19.9.2018 and
admitted in People’s Heritage Hospital. In this accident, his teeth and teeth bones were fractured and damaged.
Since, no dentist was available in this hospital he took discharge under LAMA and consulted Dr. Harpreet, Dental
Surgeon who recommended teeth implant after a period of five months when the teeth bones would develop. As per
the recommendations of the dental surgeon, the complainant took teeth implant treatment of his son on OPD basis
on 12 and 16 March, 2019. The insurance company repudiated the claim of teeth implant on the grounds of post
hospitalization time limit and treatment was carried on OPD basis. The insurance company reiterated that the claim
was rightly repudiated by them. As per the terms and conditions of the policy, the post hospitalization limit is 90
days. The patient was discharged from hospital on 21.09.2019 and the claim was submitted for 12 and 16 March,
2019. Secondly, the treatment was done on OPD basis and as per the Exclusion E of the policy, OPD treatment is
not covered. They would oblige to pay the claim if the surgical procedure was done on inpatient basis.
On going through the documents exhibited and the oral submissions made by both the parties during the hearing, it
is evident from the People’s Heritage Hospital Discharge Summary dated 21.9.2019 that the insured was admitted in
hospital from 19.9.2018 to 21.09.2018 after he met with the road accident and suffered facial injuries. His dental
treatment could not be done in the hospital due to non-availability of dental surgeon. The complainant took LAMA
discharge from the hospital and consulted dental specialist, Dr. Harpreet Singh, who advised the patient to wait for
five months for dental implants. This fact was intimated by the complainant vide email dated 10.12.2018 to the
insurance company whereby he requested them not to close the claim file till the final treatment and implant of teeth
was done. This is corroborated by Dr. Harpeet Singh, Dental Surgeon, in his email dated 05.06.2019 that due to
injury to the bone they had to wait for another five months for bone healing which was a standard protocol for any
implant procedure. They opted for delayed implant placement in healed bone sites for the betterment of patient’s
health and intimated the insurance company. Hence, the first ground of the insurance company to reject the claim
that the limit of post hospitalization was 90 days have elapsed, does not stand to scrutiny and is unreasonable and
invalid. The treating doctor was the best judge to decide the line and protocol of the treatment. Dental Implants
were done on 12 and 16 March, 2019 and were in line of the accident, but got delayed on medical expert’s advice.
As regards the second ground of rejection, though the procedure was done on OPD basis, it was a surgical procedure
as is evident from the treating doctor’s email dated 05.06.2019. It is obvious that the cause of dental implant was
road accident. The treating doctor is the best judge to decide hospitalization and the line of treatment. In the case of
Bhanvarlal Purohit Vs. National Insurance Co. Ltd., the Vadodara District Consumer Dispute Redressal
Forum in August, 2018, ruled that “No insurance company can decide the line of treatment to be given to a
patient, only doctors can decide about the treatment”. The insurance company is directed to pay the claim as per
the terms and conditions of the policy.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MRS. NEETU SINGH V/S SBI GENERAL INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-040-1920-0149
1.
Name & Address of the Complainant
Mrs. Neetu Singh
W/o Pankaj Kumar (Advocate), H-60,
Yamunapuram, Bulandshahar, UP-203001.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
0000000003509587-03
Group Health (Family Floater) policy
03.11.2017 TO 02.11.2018
3.
Name of the insured
Name of the policyholder
Mr. Abhinav Teotia
Mrs. Neetu Singh
AWARD
Taking into account the facts and circumstances of the case and the submissions made by the
complainant during the course of hearing, the insurance company is directed to pay the claim as
per the terms and conditions of the policy.
The complaint is treated as closed accordingly.

4.
Name of the insurer
SBI General Insurance Co. Ltd.
5.
Date of Repudiation
18.06.2019
6.
Reason for repudiation
Pre-authorization was denied
7.
Date of receipt of the Complaint
07.08.2019
8.
Nature of complaint
Denial of Claim
9.
Amount of Claim
Rs.2,75,000/- apprx.
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Rs. 2,75,000/- apprx.
12.
Complaint registered under IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019 at Noida
14.
Representation at the hearing
y) For the Complainant
Mrs. Neetu Singh, Self
z) For the insurer
Ms. Chynikca Modie, Sr. Legal Executive
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
Brief Facts of the Case: This complaint is filed by Mrs. Neetu Singh against M/s SBI General Insurance against
rejection of hospitalization claim of her son, Mr. Abhinav Teotia.
17) Cause of Complaint:
Complainant’s argument: The complainant alongwith her family members were covered under group
mediclaim policy from SBI General Insurance Co. This policy was in continuation from the year 2015 bearing
policy no. 0000000003509587-03. She had never made any claim in previous year’s policies. Mr. Abhinav
Teotia, younger son of the complainant, suffered with medical problem on 08.06.2019. He was admitted in
Indogulf Hospital, Noida, on 11.06.2019. The claim for Rs. 16,224/- was approved and settled by the insurance
company on cashless basis. On 12.6.2019, Indiogulf Hospital referred the patient to Fortis Hospital for better
treatment. The treating doctors recommended brain surgery. The hospital sent cashless approval for the surgery
to the insurance company but they denied vide their letter dated 18.6.2019 on the ground that the disease was
congenital. The hospital again recommended that the present disease was not congenital and requested for
cashless approval to the insurance company. Again third time, the neurosurgeon sent certified copy of case
summary that the treatment was for accidental injury and not from congenital disease but they did not settle the
claim. The complainant further pleaded that the insurance company approved the claim for the first time and
second time, for the same disease, claim was not approved. She approached the grievance cell of the insurance
company but could not get any relief; hence, she approached this Forum for justice.
Insurers’ argument: The insurance company in their SCN dated 20.09.2019 stated that the complainant
submitted two claims for her son, Mr. Abhinav Teotia. The first claim was for hospitalization claim of the
insured at Indo Gulf Hospital for the treatment of Left Fronto-Partial Arachnoid Cyst with Subdural Effusion +
Nted With Focal Sezuuire with Postictal Hemiparesis. He was admitted from 11.6.2019 to 12.6.2019 and the
company settled the admissible amount of Rs.9,593/- in cashless manner to the hospital. The complainant again
sent cashless request for Mr. Abhinav Teotia for hospitalization claim in Fortis Hospital, Noida on 12.6.2019
for the treatment of Left Fronto Parietal Space Occupying Lesion With Left Fronto Parieto Occipital Sub Dural
Collection and underwent surgical management of the same. Based upon the medical documents, it was noticed
that the policy was in fourth year of operation. The imaging report showed possibility of the ailment being
congenital in nature, could not be ruled out at the time of cashless authorization, as the report showed presence
of arachnoid cyst which was congenital in nature. As per Clause 4 of the policy, congenital disease falls under
waiting period of 48 months. It was observed that the disease was pre-existing in nature hence the cashless
claim was not payable. Hence, they denied cashless authorization but it did not bar the complainant from
applying for reimbursement of the medical expenses by submitting relevant documents to the company.
18) Reason for Registration of Complaint: Denial of claim
20) The following documents were placed for perusal.
a) Complaint letter/Form VIA
b) Medical papers
c) Policy document
d) SCN
21)Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant stated that the insurance company rejected the hospitalization claim of her son
on the ground that the disease was congenital. She represented to the insurance company alongwith the
neurosurgeon’s recommendation that the treatment was for accidental injury and not for congenital disease. She
further stated that all the claim papers were sent to the Grievance Cell of the insurance company in the month of
June, 2019, and again she forwarded these documents vide e-mail dated 22.11.2019. The insurance company
reiterated that the claim was repudiated on the ground that there was possibility that the ailment was congenital in
nature. They have only denied cashless approval and the claim was not denied. They had not received the claim
documents for processing the claim.
On going through the documents exhibited and the oral submissions made by both the parties during the hearing, it
is noted that the insurance company rejected cashless approval of claim on the ground that the disease was suspected
to be congenital. To rule out this, the complainant had already submitted letter of Dr. Rahul Gupta of Fortis Hospital
who clarified on query letter dated 13.6.2019 that ‘that is not congenital that is incidental finding’ and a certificate
dated 14.6.2019 from the treating doctor who certified that the present ailment was not congenital in nature. She had
also submitted certificate dated17.06.2019 from Department of Neurosurgery, Fortis Hospital, Noida, that certified
in Case Summary that the Patient was admitted with sudden right side weakness andaphasia and apraxia. CT and
MRI showed Left side large fronto parietal subdural collection and midline shift, so working diagnosis is subdural
effusion and arachnoid cyst in which arachnoid cyst are incidental findings. Peroprative findings are chronic
subdural hematoma. This bleeding is subdural space is not realted to presence of arachnoid cyst. Bleeding is
because the patient had minor head injury one month back. Hence this case should be considered as a case of
sequel of head injury.”

During the discussion, the complainant was advised to submit claim documents to the insurance company before
the Forum. The complainant submitted all the required documents to the insurance company during the hearing. The
insurance company is directed to pay the claim, as per the terms and conditions of the policy, within a period of 3
weeks and confirm the same to this Forum.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF MR. RAJENDRA KUMAR TYAGI V/S STAR HEALTH & ALLIED INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-044-1920-0101
1.
Name & Address of the Complainant
Mr. Rajendra Kumar Tyagi
H.No.1144, Gali No.9/14,
Indra Lok Colony,Pannapuri,
HAPUR (UP)- -245101
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/161112/01/2018/005586
Family Health Optima Insurance Plan
We.f. 25/07/2017till 24/072018
3.
Name of the insured
Name of the policyholder
Mrs. Santosh Tyagi
Mr.Rajendra Kumar Tyagi
4.
Name of the insurer
Star Health & Allied Insurance Company
Limited
5.
Date of Repudiation
6/122017 & 22/2/2018
6.
Reason for repudiation
Repudiation of Health Claim
7.
Date of receipt of the Complaint
24/6/2019
8.
Nature of complaint
Denial Of Health Claim
9.
Amount of Claim
16434/-
10.
Date of Partial Settlement
nil
11.
Amount of relief sought
16434/-
12.
Complaint registered under
IOB rules
YES
13.
Date of hearing/place
22.11.2019/NOIDA
14.
Representation at the hearing
aa) For the Complainant
Sh. Rajendra Kumar Tyagi
bb) For the insurer
Dr. Madhukar & Sh. Mantosh Kumar
15
Complaint how disposed
AWARD
16
Date of Award/Order
13.12.2019
17) Brief Facts of the Case : This complaint is filed by Sh .Rajendra Kumar Tyagi regarding repudiation of
hospitalization claim of his wife Mrs. Santosh Tyagi against Star Health & Allied Insurance co. Ltd.
18) Cause of Complaint:- Repudiation of health claim by insurance company.
a) Complainants argument :- The complainant has taken a health insurance policy No.
P/161112/01/2018/005586 from the above company for his family members for the period w.e.f. 25/07/2017
till 24/07/2018. The said policy was ported from National Insurance Co. Ltd. for sum assured 500000/-. His
wife Mrs. Santosh Tyagi was admitted on 20/10/2017 in Arogya Medical and Diagnostic Center Hapur and
discharged on 23/10/2017. She was diagnosed as PYREXIA WITH TCP with Hepatitis by the attending doctor..
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company is directed to pay the claim as per the terms and conditions
of the policy within a period of 3 weeks from the receipt and confirm the same to this Forum.
The complaint is closed accordingly.

The company has rejected the claim of his wife Mrs. Santosh Tyagi on the ground that the patient`s name is
not found in the IP register and the hospital was not maintaining any register to confirm insured patient
hospitalization. The complainant has submitted all relevant documents for reimbursement of the claim.
b) Insurers’ argument:- The insurance company vide their SCN dated 30/7/2019 submitted that the insured has
purchased a above said Health Insurance policy form the company wherein the insurance overage to the
complainant`s wife w.e.f. 25/7/2017 to 24/7/2018 for a sum assured of Rs 500000/- to each insured subject to
the terms and conditions. The policy was ported form National Insurance Co.Ltd. subject to terms and
conditions. The insured was admitted on 20/10/2017 in the hospital and discharged on23/10/2017 and insured
was diagnosed as suffering from PYREXIA WITH TCP with Hepatitis. The complainant has submitted her
spouse claim for reimbursement of medical expenses and reconsideration of the claim. On scrutiny of the claim
documents, the patient`s name is not found in the IP register and the hospital was not maintaining any register to
confirm insured patient hospitalization. Hence, the claim was repudiated and communicated to the insured vide
letters dated 6/12/2017 and 22/2/2018 .
19) Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN
21) Observations and Conclusion : -
Both the parties appeared for hearing on 22.11.2019 and reiterated their submission. The complainant stated that the
cause of complaint arose as the respondent company has rejected the hospitalization claim in respect of her wife
despite submission of all papers. The Insurance Company explained that they suspected the veracity of In Patient
Register and therefore rejected the claim. They were asked to verify and submit report within 15 days.
The Insurance company submitted a report dated 4/12/2019 which could not throw any light on the veracity of the
submitted documents. The failure of the Insurance company to assail the claim with any credible evidence can not
be a ground for repudiating the claim As they failed prove, the documents to be wrong, the repudiation of claim can
not be upheld. Insurance company is directed to settle the hospitalization claim and pay the admissible amount to the
complainant.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 13.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S. PRADAD
CASE OF MRS. KULVINDER KAUR V/S STAR HEALTH AND ALLIED INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-44-1920-0133
1.
Name & Address of the Complainant
Mrs. Kulvinder Kaur,
D/O Sh. Balvinder Singh,
204/6, Dibdiba-5, Kaushalganj,
Rampur (UP) - 244921
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/161312/01/2019/012556
Family Health Optima Insurance policy
W.E.F. 8/2/2018 TILL 7/2/2019
3.
Name of the insured
Name of the policyholder
Mrs. Kulvinder Kaur,
Mrs. Kulvinder Kaur
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
24.6. 2019
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties during the course of hearing, the Insurance company is directed to settle the claim
and pay admissible amount to the complainant as per terms and conditions of the policy
Hence, the complaint is treated as closed accordingly.
..………………………………………………………………………….. is hereby awarded to be
paid by the Insurer to the Insured, towards full and final settlement of the claim.
Hence, the complaint is treated as ……

6.
Reason for repudiation
PED
7.
Date of receipt of the Complaint
15/7/2019
8.
Nature of complaint
Rejection of Hospitalization claim
9.
Amount of Claim
Rs.131803/-
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Rs.131803/-
12.
Complaint registered under
IOB rules
YES
13.
Date of hearing/place
20/12/2019/NOIDA
14.
Representation at the hearing
cc) For the Complainant
Mrs. Kulvinder Kaur
dd) For the insurer
Dr Madhukar Pandey/Mr. Mantosh Kumar
15
Complaint how disposed
AWARD
16
Date of Award/Order
31/12/2019
17) Brief Facts of the Case: This is a complaint filed by Mrs.Kulvinder Kaur against Star Health Insurance Co.
Ltd. regarding repudiation of hospitalization claim.
18) Cause of Complaint:- Rejection of claim due to Pre- existing decease.
a) Complainants argument :-. The complainant had taken the health policy from the above said insurer
w.e.f. 8/2/2017 to 7/2/2018 and further renewed w.e.f. 8/2/2018 till 7/2/2019. The insured was suffering
with abdomen pain and was admitted at Narayan Hospital & Trauma Center Rudrapur from 15.4.2019 to
20.4.2019 but she did not get any relief. Then she was referred to Sir Ganga Ram Hospital , New Delhi, and
was admitted on 3/5/2019 for treatment and discharged on 7/5/2019. The complainant submitted the claim
for reimbursement. Insurer rejected the claim due to PED.
b) Insurers’ argument:- The Insurance company vide their SCN dated 5/12//2019 submitted that Mrs.
Kulvinder Kaur was admitted on 3/5/2019 at Sir Ganga Ram Hospital New Delhi and was diagnosed with
Acute Enteritis Eosinophilic, Thrombocytopenia, Iron Deficiency Anaemia and discharged on 7/5/2019.
The insured sent pre-authorization request to avail cashless facility which was initially approved and then
withdrawn as the facts came to light that insured patient had ITP since 2009 and was taking Wysolone
which was prior to first policy and was not disclosed by the insured in the proposal form at the time of
commencement of the first policy. . The company has repudiated the claim vide letter dated 7/6/2019 on
the above grounds of pre-existing disease.
19) Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN
21)Observations and Conclusion:- Both parties appeared for personal hearing on 20.12.2019 and reiterated their
submissions. The complainant has taken health insurance policy from the above company. The insured was
suffering with abdomen pain and was admitted at Narayan Hospital & Trauma Center Rudrapur from 15.4.2019 to
20.4.2019 but she did not get any relief. Then she was referred to Sir Ganga Ram Hospital , New Delhi, and was
admitted on 3/5/2019 for treatment and discharged on 7/5/2019. The complainant submitted the claim for
reimbursement but insurance company rejected her claim on the ground that she suppressed her having ITP
(Idiopathic Thrombocytopenic Purpura) at the time of policy inception. The complainant vehemently denied of
having any knowledge of having ITP.
It is observed that the insurance company repudiated the claim only on the basis of OPD paper of AIIMS dated
17/4/2009, wherein there is a mention of ITP along with (?). The question mark indicate that the treating doctor
himself was not sure of the fact that the insured was having ITP. The administration of WYSOLONE has also been
prescribed in reducing manner which is also a proof that the doctor was not certain and wanted to mask the
symptoms of any unspecified disease No other evidence has been adduced by the insurer to buttress their
contention that the complainant deliberately did not disclose her illness at the time of taking policy. The rejection of
claim by the insurance company is not justified. Insurance company is directed to settle the hospitalization claim and
pay the admissible amount to the complainant.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties during the course of hearing, the Insurance company is directed to settle the claim
and pay admissible amount to the complainant as per terms and conditions of the policy.
Hence, the complaint is treated as closed accordingly.

22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH HARVINDER SINGH V/S STAR HEALTH & ALLIED INSURANCE CO. LTD.
COMPLAINT REF: NOI-L-044-1920-0137
AWARD NO:
1.
Name & Address of the Complainant
Sh. Harvinder Singh,
F-112, Sector-41, Noida(UP)-201301
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/161100/2018/027470
HEALTH
31/3/2018 TO 30/3/2019
3.
Name of the insured
Name of the policyholder
Sh Harvinder Singh
Sh Harvinder Singh
4.
Name of the insurer
Star Health & Allied Insurance Company
Limited
5.
Date of Repudiation
17/9/2018
6.
Reason for repudiation
Repudiation of Health Claim
7.
Date of receipt of the Complaint
8.
Nature of complaint
Denial Of Health Claim
9.
Amount of Claim
Rs. 58236/-& Rs 119988/-
10.
Date of Partial Settlement
nil
11.
Amount of relief sought
Rs. 58236/- & Rs.119988/-
12.
Complaint registered under
IOB rules
YES
13.
Date of hearing/place
20/12/2019, NOIDA
14.
Representation at the hearing
ee) For the Complainant
Sh. Bhupinder Pal Singh (Brother)
ff) For the insurer
Dr. Madhukar Pandey/ Sh.Mantosh Kumar
15
Complaint how disposed
AWARD
16
Date of Award/Order
31/12/2019
17) Brief Facts of the Case : This is a complaint filed by Sh. Harvinder Singh against decision of Star Health &
Allied Insurance Co. Ltd regarding repudiation of claim and for further renewal of above insurance policy.
18)Cause of Complaint:- Repudiation of health claim under the above policy by company & for further renewal
of policy also.
Complainants argument :- The complainant had taken the health policy from the above insurer w.e.f. 31/3/2018 to
31/3/2019. The complainant was admitted on 23/4/2018 at Kailash Hospital & Heart Institute, Noida with the
complaint of frequent urination since 2 week and urinary incontinence. He was discharged on 27/4/2018 after
treatment. Again, the complainant was admitted on 7/5/2018 at Kailash Hospital & Heart Institute, Noida with
complaint of retention of urine, weakness ,drowsiness. He was discharged on 17/5/2018. The complainant had
lodged both the claims for amount of Rs.58236/- on 11/5/2018 and Rs. 119988/- on 21.6.2018 respectively. But
the company did not update the complainant about status of both claims till date. The complainant sent demand
draft for renewal premium of the above policy but company returned the DD to the complainant.
Insurers’ argument:- The Insurance company stated vide their SCN dated 12/12/2019 submitted that the insured
has reported the following claims under the above policy.
1) The insured was admitted Kailash Hospital & Heart Institute, Noida on 23/4/2018 for treatment of
CKD(Chronic Kidney Disease) and submitted a claim for reimbursement of medical expense for Rs.58236/-
2) The insured was admitted on 7/5/2018 in the above hospital for treatment HTN/Vertigo with CKD with
Hyponatremia and submitted claim for reimbursement of Rs.98540/- and same was rejected due to non-
disclosure of Diabetes Mellitus .
3) The complainant was admitted on 3/8/2018 in the above hospital for the treatment of prostate surgery but he
has not submitted any claim documents. The company requested vide letter dated 18/8/2018 and 2/9/2018 to
submit the claim documents for reimbursement but insured has not submitted the required documents. Hence
the claim was treated as closed and rejected, the same was communicated to the insured vide letter dated
17/9/2018.
19) Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN

21) Observations and Conclusion:- Both the parties attended for personal hearing on 20/12/2019 and reiterated
their submissions. The complainant had lodged two claims but insurance company did not settle any claim and
discontinued the health policy, while the complainant sent Demand Draft of renewal premium for Health
policy. The insurance company stated the insured has not submitted required documents in spite of their
repeated queries. During the hearing, The insurance company offered to settle the health claims as per policy
condition and also continue the policy. I feel it just, fair, and equitable to make recommendations about the
settlement of the claim as full and final .
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S. PRADAD
CASE OF SH.MANOJ KUMAR PANDEY V/S STAR HEALTH AND ALLIED INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-44-1930-0152
1.
Name & Address of the Complainant
Sh.Manoj KumarPandey,
“Prayag Raj” Near Joshi Kunj
Grass Mandi, P.O. PAC, Nakatia,
Bareilly (UP)-243005
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/231116/01/2019/001309
HEALTH
W.E.F. 20/7/2018 TILL 19/7/2019
3.
Name of the insured
Name of the policyholder
Mrs. Mohini Devi
Sh. Manoj Kumar Pandey
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
30/7/2019
6.
Reason for repudiation
Request for review of claimed amount settled.
7.
Date of receipt of the Complaint
14/8/2019
8.
Nature of complaint
Partial payment of claim
9.
Amount of Claim
Rs.21639/-
10.
Date of Partial Settlement
29/7/2029
11.
Amount of relief sought
Rs.2158/- & Rs. 2752/-
12.
Complaint registered under
IOB rules
YES
13.
Date of hearing/place
20/12/2019/NOIDA
14.
Representation at the hearing
gg) For the Complainant
ABSENT
hh) For the insurer
Dr. Madhukar Pandey/Sh.Mantosh Kumar
15
Complaint how disposed
AWARD
16
Date of Award/Order
31/12/2019
17) Brief Facts of the Case: This is a complaint filed by Sh Manoj Kumar against Star Health Insurance Co. Ltd.
against partial payment of health claim in respect of the insured Mrs. Mohini Devi, mother of the complainant.
18) Cause of Complaint:- Partial payment of health claim.
a) Complainants argument :-. The complainant submitted two claims of Rs. 21639/- & Rs.8092/- of his
mother, Mrs. Mohini Devi insured in the above policy. The company settled the health claims of Rs. 19481/-
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by both the parties during the course of hearing, the insurance company is directed to
settle admissible amount of health claims and also continue the policy .
The complaint is thus treated as closed accordingly.
Hence, the complaint is treated as ……

& Rs. 5424/- to insured after deducting Rs.2158/- and Rs. 2752/- from claimed amounts. The complainant
stated that the above amount were deducted wrongly.
b) Insurers’ argument:-. Insurance company vide their SCN dated 5/12/2019 submitted that they had deducted
Rs.2158/- and Rs.2668/- from the two claims on account of post hospitalization expenses and non payable
items. The claim has been settled as per the terms and conditions of the policy.
19) Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN
21) Observations and Conclusion:- Personal hearing of the case was fixed on 20/12/2019. The complainant
could not attend the hearing, because his mother was in serious condition and sent e-mail on 19/12/2019 in this
regard. The insurer attended the hearing and reiterated their submissions. During the hearing, the insurance
company agreed to settle the balance claim amounts of Rs.2152/-- & Rs. 2292/- against claim No.
CLI/2020/231116/0149711 and claim No.CLI/2020231116/0236570 respectively, which were deducted against
post-hospitalization. The insurance company gave written consent dated 20/12/2019 for settlement of above
mentioned claim on humanitarian ground. I feel it just, fair, and equitable to make recommendation about the
settlement of the complaint as full and final.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTRAKHAND
UNDER INSURANCE OMBUDSMAN RULE 2017
OMBUDSMAN : SH. C.S. PRASAD
CASE OF SH. SAMIR KUMAR DAS V/S NATIONAL INSURANCE CO. LTD.
COMPLAINT REF. NO.: NOI-G-048-1920-0033
1.
Name & Address of the Complainant
Sh. Samir Kumar Das
T-6, Ground Floor,
Eldeco Residency Green, Sec. PI,
P.O. Greater Noida
Greater Noida, U.P.201315.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Sum Insured
366011501810000076
National Mediclaim Policy
01.06.2018 to 31.05.2019
Rs.2,00,000/- (Individual S.I.)
3.
Name of the insured
Name of the policyholder
Ms. Bharati Das, Spouse
Sh. Samir Kumar Das
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
N.A.
6.
Reason for repudiation/Partial Settlement
Insured was entitled for General Ward but
claimed for Private room.
7.
Date of receipt of the Complaint
04.04.2019
8.
Nature of complaint
Partial rejection of Medi-claim By Insurance
Company
9.
Amount of Claim
Rs.1,12,426/-
10.
Date of Partial Settlement
06.01.2019
11.
Amount of relief sought
Rs.29,094/-+ Rs.50,000/- for mental harassment
as per Annex. VI A
12.
Complaint registered under Insurance
Ombudsman Rule 2017
13 (2)
13.
Date of hearing/place
04.10.2019 and rehearing on 06.12.2019
AWARD
Taking into account the facts and circumstances of the case and the submissions made by the
insurer during the course of hearing, The insurance company is directed to settle the balance
claim amount Rs.2152/- & Rs 2292/- against post-hospitalization under the above mentioned
claim numbers.
The complaint is closed accordingly.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties during the course of hearing,
..………………………………………………………………………….. is hereby awarded to be
paid by the Insurer to the Insured, towards full and final settlement of the claim.
Hence, the complaint is treated as ……

at NOIDA
14.
Representation at the hearing
ii) For the Complainant
Sh. Samir Kumar Das
jj) For the insurer
Sh. Madhur Sood, Asstt. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
11.12.2019
17) Brief Facts of the Case:- Sh. Samir Kumar Das, the Complainant was covered alongwith his Ms. Bharati Das
under National Mediclaim No. 366011501810000076 for the period from 01.06.2018 to 31.05.2019 under
Individual S.I. Rs. 2,00,000/-. Mediclaim of treatment of his wife was rejected partially by the Insurance
Company stating that they have deducted the amount as per terms and conditions of the policy. Aggrieved, he
requested the TPA/insurer including its GRO to reconsider the claim but failed to get any relief. Thereafter, he
preferred a complaint to this office for resolution of his grievance.
18) Cause of Complaint:-
Complainant’s arguments: The Complainant stated that his wife Ms. Bharati Das was diagnosed with Gall Bladder
Stone and admitted on 04.01.2019. He opted for Single Bed Room facility package of Rs.89,400/- under
Cholocystectomy Lap GIPSA A17. The approval was received on 04.01.2019 for an amount of Rs.70,250/- against
the package of Rs.89,400/- opted.
Surgery was done on 05.01.2019 and the patient was discharged on 06.01.2019. Thereafter, the detailed Inpatient
Bill for Rs.95,322/- were forwarded by the Hospital to TPA on 06.01.2019. The Hospital received a mail from TPA
that the Cashless facility approved was rejected without assigning any reason. Subsequently, Hospital Authorities
received another mail with approval of Rs.60,000/-. The Complainant provided the claim detail as under:-
• Total Cost of Treatment : Rs.97,799.50
• Amount paid to the Hospital by TPA : Rs.60,000.00
• Amount transferred to his Bank Account on 26.03.2019 : Rs.8,705.00
• Amount transferred to his Bank Account on 28.08.2019 : Rs.5,000.00
• BALANCE AMOUNT TO BE REIMBURSED : Rs.24,094.50
Insurers’ argument: The Insurance Company in their SCN give point-wise reply of Complaint as under:-
1 to 6)- Self Statement of the Insured does not need any explanation.
7)- TPA had received pre authorization request from Sakra World Hospital, Bengaluru on 03/01/2019 only
requesting for an amount of Rs. 99650/-. It was found that this package amount claimed by the hospital was for a
Pvt. Room while the Insured’s entitlement is for a General Ward. TPA requested the hospital to revise the GIPSA
PPN package as per insured’s eligibility of General Ward. The Hospital replied stating that GIPSA Package for
General Ward is Rs. 70250/- . TPA initially approved Rs. 70250/- to avoid any delay.
8)- On receipt of Final Bill & Discharge Summary on 06/01/2019 at 13.40, it was noted that the agreed GIPSA PPN
package for General ward is Rs. 60000/- only. The Hospital had added two amounts of Rs.10,000/- & Rs. 250/-
towards OT consumables & dietician charges respectively. Both of these charges were a part of GIPSA Package.
Therefore, TPA gave a final approval of Rs. 60000/-.
9)- Self Statement does not need any explanation.
10)- The Insured had subsequently lodged reimbursement claim under file number 19RB01NAA4476 for
Rs.1,12,426/- which included hospital bill of Rs.95,322/- + pre/post expenses of Rs.17,104/- which was processed as
per policy terms & conditions. Since, the Insurer had already approved cashless for an amount of Rs.60,000/-
towards cashless facility, the claim was approved for Rs. 8705/- + Rs. 5000/- (approved on 26/07/2019 under a fresh
file number 20RB01NAA1381) = Rs.13705/- towards pre/post expenses, deducting therein an amount of Rs.
38721/-.
10.1 ,10.2, 102.1)- Under these points, the Insured had shown calculation under policy clause 2.1, 2.2 & 2.3
indicating an amount of Rs.81,295/- as admissible to him against Rs.73,705/- settled by the Insurer. It may please
be noted that policy clause no. 2.3 in the last para states that Sub limits (as mentioned in clause 2.1, 2.2, and 2.3)
will not apply in case of Hospitalization in a preferred provider network (PPN) hospital. Further pre hospitalization
expenses are payable with the limit of 30 days prior to hospitalization as specified under policy clause 3.24.
Therefore, limits / sublimits as mentioned in clause 2.1,2.2 & 2.3 were not applied while calculating the admissible
amount of claim for treatments at a PPN hospital under a PPN Package. The insured’s claim for Rs.21,295/- under
his point SUBMISSION (C) was not admissible.
11)- As explained in point no. 10, the Insured’s total claim was for Rs.1,12,426/-, out of which the Insurance
Company had paid an amount of Rs.73,705/-, deducting an amount of Rs.38,721/-.
12)- The Insured had prayed to the Hon’ble Ombudsman seeking an amount of Rs.29,094.50. The Insurance
Company had already shown the calculations above in point no.10. Therefore his claim for Rs.29,094.50 was not
tenable.
19) Reason for Registration of Complaint: - Partial payment of Mediclaim rejected.
20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN

21) Observations and Conclusion :-
Both the parties appeared for first hearing on 04.10.2019 and reiterated their submissions. The Complainant
stated that the Insurance Company had not paid his claim fully. He had submitted a bill of Rs. 97,799.50 in
which the Insurer paid Rs. 70250/- and he had to pay Rs.24,094.50 out of his pocket. The Insurance Company
reiterated that the TPA had received pre authorization request from Sakra World Hospital, Bengaluru on
03/01/2019 only requesting for an amount of Rs. 99,650/-. It was found that this package amount claimed by the
hospital was for a Pvt. Room while the Insured’s entitlement is for a General Ward. TPA requested the hospital
to revise the GIPSA PPN package as per insured’s eligibility of General Ward. The Hospital replied stating that
GIPSA Package for General Ward is Rs. 70250/- . TPA initially approved Rs. 70250/- to avoid any delay. On
receipt of Final Bill & Discharge Summary on 06/01/2019 at 13.40, it was noted that the agreed GIPSA PPN
package for General ward is Rs. 60000/- only. The Hospital had added two amounts of Rs.10,000/- & Rs. 250/-
towards OT consumables & dietician charges respectively. Both of these charges were a part of GIPSA
Package. Therefore, TPA gave a final approval of Rs. 60000/-. Total claim amount of Rs.73,705/ was approved
by the Insurer and Rs. 24,094.50 was deducted on the ground of GIPSA package for a General Ward according
to the entitlement of the complainant. The complainant stated that the insurance company never provided the
break-up of deducted amount of Rs.24,094/- to him. The Insurer was directed to provide the break up to the
complainant.
On 06.12.2019, second hearing was scheduled. During the course of hearing, the insurance company stated that
they visited the complainant’s home as well TPA’s office to clarify but they could not provide the breakup of
Rs.24,094/- to the insured because the claim was paid according to the GIPSA package. The Insurer said that
the Operative Clause of the terms and conditions of the policy is not applicable in case of PPN Hospital and the
breakup of cost heads under clause 2.1 Room Charges, 2.2 Medical Practitioner’s fees and 2.3 Others are not
applicable for settlement of bills because claim falls under GIPSA package in PPN Hospital.
The complainant argued that though, his case is related to PPN Hospital, his claim amount does not exceed the
Sum Insured i.e. Rs.2,73,750/-. According to the Operative Clause No.2 of the policy, Sub limit on clause
no.2.1,2.2 and 2.3 will not apply in case of Hospitalisation in a PPN Hospital. Therefore, he is entitled for the
Medical Practitioner’s fee and Other charges as full. Regarding the Room Charges, the complainant agreed as
per his entitlement on the basis of sum insured i.e. 1% of the sum insured per day subject to maximum of
Rs.5,000/-.
I have examined the documents exhibited and oral submissions made by both the parties. It was found that this
package amount claimed by the hospital was for a Pvt. Room while the Insured’s entitlement is for a General
Ward. Therefore, Room Charges is applicable as per the entitlement of the complainant. But, according to the
Operative Clause No.2 of the policy, Sub limit on clause no.2.1,2.2 and 2.3 will not apply in case of
Hospitalization in a PPN Hospital. Therefore, he is entitled for the Medical Practitioner’s fee and Other charges
as full. The complainant has also demanded the interest on the deducted amount which is not considered
because, there was no deficiency in service on the part of the Insurer. The Insurance Company is directed to
settle the entire claim without implementing any GIPSA package excluding deductions made as per policy’s
terms and conditions to the Complainant.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 11.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
AWARD
Taking into account the facts and circumstances of the case and the submissions
made by both the parties during the course of hearing, the Insurance Company is
directed to settle the entire claim without implementing any GIPSA package
excluding deductions made as per policy’s terms and conditions to the Complainant.
The complaint is treated as disposed off accordingly.

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P AND UTTARAKHAND
UNDER THE INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. ASHISH BHATNAGAR V/S NATIONAL INSURANCE CO. LTD.
COMPLAINT REF. NO. : NOI- H- 048- 1920 – 0119
1.
Name & Address of the Complainant
Sh. Ashish Bhatnagar
B-48, Ashok Nagar
Ghaziabad, U.P.201001.
Phone No.09711937849
2.
Policy No:
Type of Policy
Duration of policy/Policy period
S.I.
361201501810000155
BOI National Swasthya Bima Policy
03.05.2018 to 02.05.2019
Rs.5,00,000/-
3.
Name of the insured
Name of the policyholder
Ms. Mitika Bhatnagar (Spouse)
Sh. Ashish Bhatnagar
4.
Name of the insurer
National Insurance Co. Ltd.
5.
Date of Repudiation
N.A.
6.
Reason for repudiation
N.A.
7.
Date of receipt of the Complaint
23.07.2019
8.
Nature of complaint
Claim partially rejected
9.
Amount of Claim
NA
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs. 1,25,251- as per Annex VI A
12.
Complaint registered under
IOB Rules, 2017
13 (1) b
13.
Date of hearing/place
11.12.2019 / Noida
14.
Representation at the hearing
kk) For the Complainant
Sh. Yogesh Bhatnagar, Father of complainant
ll) For the insurer
Sh. Sanjay Kumar Asiwal, SBM
15
Complaint how disposed
Award
16
Date of Award/Order
12.12.2019
17) Brief Facts of the Case:- Sh. Ashish Bhatnagar, the Complainant stated in his complaint that his medi claim
for treatment of his wife Ms. Mitika Bhatnagar was partially settled by the Insurance Company. Aggrieved, he
requested the TPA/Insurer to reconsider the claim but failed to get any relief. Thereafter, he has preferred a
complaint to this office for resolution of his grievance.
18) Cause of Complaint:
a) Complainant’s argument:- The Complainant stated that he is a Non Life (Mediclaim) Policy holder No-
361201501810000155 from National Insurance Co.Ltd , 65, Hapur Road, Navyug Market, Ghaziabad,
Uttar Pradesh- 201001 and he had admitted his wife Ms. Mitika Bhatnagar due to GDM issue for which
Medical Treatment was given to her for four days but it did not came under control even after medical
treatment. Hence, in emergency circumstances the panel of Doctors Decided to operate a Pre-mature
Pregnancy to save the life of mother & Baby for which total Hospitalization cost was Rs.1,25,251/-, and
TPA has given a Gurantee Letter of 40,000/- and after that TPA settled an amount of Rs. 25,000 only
stating that it was a typing error and it was mentioned 40,000/- instead of 20,000/- against the Claim Filed
for Rs Rs. 1,25,251/-.
b) Insurers’ argument:- The insurer stated in their brief SCN that Sh. Ashish Bhatanagar applied for a BOI
National Swasthya Bima Policy on 25.04.2018 through BOI, Navyug market, Ghaziabad. The same
proposal was submitted by BOI on 03.05.2018 to National Insurance and office issued policy to Sh. Ashish
Bhatnagar, also covering his wife Ms. Mitika Bhatnagar (28 Years) in the policy. Ms. Mitika has been
hospitalized for pregnancy procedure on 18.01.2019 (and this policy was taken eight month before the
admission in the hospital for pregnancy) and has been discharged from the hospital on 24.01.2019 after
delivery of a baby. Sh. Ashish lodged a reimbursement claim with TPA M/s. East West. On 12.02.2019,
TPA sent a query letter to Sh. Ashish aksing for providing the policies copies before year 2018, if any,
because Sh. Ashish submitted bills of Rs.1,14,508/- but Sh. Ashish not provided the same since this is first
year running policy. Therefore, on 10.05.2019, TPA sent a letter to the insured stating that your claim has
been settled at an amount of Rs.25,000/- which was maximum payable as per the policy terms and
condition. As per policy terms & conditions (2.7), the claim related to maternity and baby care expenses is
subject to condition hereunder:
• Cover is available upto a limit of 5% of sum insured (5 lacs).
• A waiting period of 9 months is applicable for payment of any claim relating to normal delivery or
caesarean section.
Since this is a 1
st
year policy, therefore only 5% of S.I. i.e. Rs.25,000/- is payable under the policy, which
was already paid on 13.06.2019 to the complainant.
19) Reason for Registration of Complaint: - Partial settlement of mediclaim
20) The following documents were placed for perusal.
a) Policy copy
b) Complaint letter

c) Form VI A
d) SCN of the insurer
21) Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. The Complainant reiterated
that insured Ms. Mitika Bhatnagar was hospitalized in emergency, due to GDM issue. Doctors decided to
operate a Pre-Mature Pregnancy to save the life of mother & Baby for which total Hospitalization cost was
Rs.1,25,251/-. TPA had given a Guarantee Letter of 40,000/- and later settled an amount of Rs. 25,000/- only.
The Insurance Company reiterated that claim has been settled at an amount of Rs.25,000/- which was
maximum payable as per the policy terms and conditions no. (2.7) : the claim related to maternity and baby
care expenses is subject to condition i).Cover is available up to a limit of 5% of sum insured (5 lacs) and ii). A
waiting period of 9 months is applicable for payment of any claim relating to normal delivery or caesarean
section. Since this is a 1
st
year policy, therefore only 5% of S.I. i.e. Rs.25,000/- is payable under the policy,
which was already paid on 13.06.2019 to the complainant.
Ongoing through the documents exhibited and the oral submissions, it is observed that the claim has been paid
as per policy condition no.2.7 i and ii. Hence, I see no reason to interfere with the decision of the Insurance
Company. The complaint is thus dismissed.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 12.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTRAKHAND
UNDER INSURANCE OMBUDSMAN RULE 2017
OMBUDSMAN : SH. C.S. PRASAD
CASE OF SH. ASHOK SHARMA V/S NATIONAL INSURANCE CO. LTD.
COMPLAINT REF. NO. : NOI-H-048-1920-0120
1.
Name & Address of the Complainant
Sh. Ashok Sharma
B-105, Surya Nagar,
Ghaziabad, U.P.201011
Ph. No.9871399921
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Sum Insured
361700501810000602
National Mediclaim Policy
30.05.2018 to 29.05.2019
Rs.2,00,000/- +Rs.50,000/- C.Bonus
3.
Name of the insured
Name of the policyholder
Ms. Shanti Sharma
Ms. Shanti Sharma
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
N.A.
6.
Reason for repudiation/Partial Settlement
N.A.
7.
Date of receipt of the Complaint
22.07.2019
8.
Nature of complaint
Partial rejection of Medi-claim By Insurance
Company
9.
Amount of Claim
N.A.
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
Rs.1,50,000/-+ Harassment by Company as per
Annex VI A
12.
Complaint registered under Insurance
Ombudsman Rule 2017
13 (1)b
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, I see no reason to interfere with the decision of
the Insurance Company.
Hence, the complaint is thus dismissed.

13.
Date of hearing/place
11.12.2019 / NOIDA
14.
Representation at the hearing
mm) For the Complainant
Sh. Ashok Sharma
nn) For the insurer
Sh. Ramesh Kumar Taneja, Asstt. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
12.12.2019
17. Brief Facts of the Case:- Sh. Ashok Sharma, the Complainant son of the Insured Ms. Shanti Sharma had taken
Individual Health Insurance Policy No.361700501810000602 for the period from 30.05.2018 to 29.05.2019 for
the S.I. of Rs.2,00,000/- +Rs.50,000/- C.Bonus. The Insured was suffering from severe pain in abdomen with
recurred vomiting. The reimbursement of bills was partially rejected by the Insurance Company. Aggrieved, he
requested the insurer including its GRO to reconsider the claim but failed to get any relief. Thereafter, he has
preferred a complaint to this office for resolution of his grievance.
18. Cause of Complaint:-
a) Complainant’s argument:- Sh. Ashok Sharma, the Complainant stated that his mother was admitted in
Hospital with complaint of severe pain in abdomen with recurred vomiting. The Insurance Company did not
pay his claim in full against the sum insured of Rs.2,50,000/- , they only paid Rs.1,00,000/-.
b) Insurers’ argument:- The Insurer in their SCN stated that the current Policy No.361700501810000602 of Rs.2
lacs Sum Insured w.e.f. 30.05.2018 to 29.05.2019 is in the name of Ms. Shanti Sharma.
The insured renewed the policy with enhanced sum insured in the year of 2016 by Rs.1,00,000/- under Policy
No.361700/48/15/8500000725 and Policy No.36170048148500000762.
Ms. Shanti Sharma was hospitalized at Aarogya Hospital Ghaziabad from 16.02.2019 to 04.03.2019 as a case of
Acute billiary pancreatitis, modified CTSI score, septicaemia, SIRS+type II respiratory failure,
dyselectrolytemia, Hypoalbuminemia with DM II, Hypertension with AF with CVR MOD CTS-6 with
complaint of severe pain abdomen with vomiting According to the discharge summary, patient was known case
of hypertension on regular treatment, history of diabetes from last 4-5 years and OA from 7-8 years
As per policy condition 5.17, the cashless claim was approved on applicable sum insured Rs.1,00,000/- (year
2014-15 Policy No.36170048148500000762) by the TPA. The clause 4.1 and 5.17 of the policy are as under:-
4.1 Pre-existing diseases – All pre-existing diseases when the cover incepts for the first time until 48 months
of continuous coverage has elapsed. Any complication arising from pre-existing ailment/disease/injuries will
be considered as a part of the pre existing health condition or disease.
5.17 Enhancement of sum insured – Sum insured under the policy can be enhanced only at the time of
renewal. Sum insured can be enhanced up to Rs.5,00,000/-. The waiting period and conditions as
mentioned under exclusions 4.1, 4.2 and 4.3 will apply to incremental portion of the sum insured.
The cashless is extended up to the sum insured of Rs.1,00,000/-. The amount of Rs.50,000/- can be reimbursed
from balance cumulative bonus on submission of original receipts by the insured.
19) Reason for Registration of Complaint: - Partial Rejection of Mediclaim
20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN
22) Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. The Complainant stated that
The Insurance Company did not pay his claim in full against the sum insured of Rs.2,50,000/- ; they have only
paid Rs.1,00,000/-. The Insurance Company stated that the insured renewed the policy with enhanced sum
insured in May, 2016 from Rs.1,00,000/- to Rs.2,00,000/-. His mother was hospitalized in Feb 2019. The
patient was known case of hypertension and on regular treatment which is also mentioned in Final diagnosis in
the Discharge Summary. Hypertension and related complications are listed disease in two years waiting period
condition in case of enhancement of sum insured. Enhanced S.I. will be applicable after the waiting period of
24 months in case of the listed diseases. Therefore, the claim was settled on the ground of applicable sum
insured i.e. Rs.1,00,000/-. The insurer was ready to pay another Rs.50,000/- because the complainant is entitled
for reimbursement of another Rs.50,000/- as insured earned the cumulative bonus of Rs.50,000/- under the
policy.
I have examined the documents exhibited and oral submissions made by both the parties. It is observed that
the Insurer paid the claim amount on ground of restriction on enhanced sum insured as per the policy
conditions. Further, during hearing, Insurer agreed to pay another Rs.50,000/- as the cumulative bonus earned
by the insured as per policy terms and conditions. Hence, the Insurance Company is directed to pay the
additional Rs.50,000/- as agreed during the hearing to the complainant.

22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 12.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTRAKHAND
UNDER INSURANCE OMBUDSMAN RULE 2017
OMBUDSMAN : SH. C.S. PRASAD
CASE OF MS. MOUMITA ROY V/S NATIONAL INSURANCE CO. LTD.
COMPLAINT REF. NO. : NOI-H-048-1920-0113
AWARD NO:
1.
Name & Address of the Complainant
Ms. Moumita Roy
Deepali Tilak Colony,
Subhash Nagar, Badaun Road,
Bareilly, U.P.243001.
Ph. No.9634033204
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Sum Insured
104200501810004653
National Mediclaim Policy
15.07.2018 to 14.07.2019
Rs.1,00,000/- +Rs.25,000/- C.Bonus
3.
Name of the insured
Name of the policyholder
Ms. Moumita Roy
Ms. Moumita Roy
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
18.02.2019
6.
Reason for repudiation/Partial Settlement
Original documents not submitted
7.
Date of receipt of the Complaint
28.06.2019
8.
Nature of complaint
Rejection of Medi-claim By Insurance
Company
9.
Amount of Claim
N.A.
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
Rs.20,960/-as per Annex VI A
12.
Complaint registered under Insurance
Ombudsman Rule 2017
13 (1)b
13.
Date of hearing/place
11.12.2019 / NOIDA
14.
Representation at the hearing
oo) For the Complainant
Mr. Anindit Roy, Son of the complainant
pp) For the insurer
Sh. K.K. Tripathy, Manager
15
Complaint how disposed
Award
16
Date of Award/Order
13.12.2019
17. Brief Facts of the Case:- Ms. Moumita Roy, the Complainant had taken National Mediclaim Policy No.
104200501810004653 for the period from 15.07.2018 to 14.07.2019 for the S.I. of Rs.1,00,000/- +Rs.25,000/-
C.Bonus. The Complainant was diagnosed with severe vertigo and dehydration. The reimbursement of claim
was not done by the Insurance Company due to non submission of original claim documents. Aggrieved, she
requested the Insurer including its GRO to reconsider the claims but failed to get any relief. Thereafter, she has
preferred a complaint to this office for resolution of his grievance.
18. Cause of Complaint:-
a) Complainant’s argument:- Ms. Moumita Roy, the Complainant stated that she was hospitalized on 02.11.2018
and diagnosed with severe vertigo and dehydration. After the discharge on 04.11.2018, it took few days to
collate all relevant bills and documents in original and sent through DTDC courier services to her insurance
agent at Kolkata for filing her claim with TP Paramount Health Services.
The subject claim related original documents were misplaced in transit by DTDC courier. After a long follow
up process and undergoing their internal investigation process, finally a General Diary at the local police
station was registered on 17.12.2018 confirming misplacement of all original documents while in transit.
AWARD
Taking into account the facts & circumstances of the case and the submissions made
by both the parties during the course of hearing, the Insurance Company is directed to
pay the additional Rs.50,000/- as agreed during the hearing to the Complainant.
The complaint is treated as disposed off accordingly.

All the photocopy documents were certified by the doctor as True Copy and resubmitted to TPA on 01.01.2019
along with the copy of the General Diary registered with local police station.
It was intimated by the Insurer on 18.02.2019 that TPA has recommended for repudiation of the claim citing
reason for submission of photocopy of documents towards her claim.
b) Insurers’ argument:- The Insurer in their SCN stated that as per TPA, the claim is pending for following
reason : Original bills, payment receipts, medical history of the patient recorded, and discharge certificate, cash-
memo and original investigation test reports.
In view of the above, the claim is considered for rejection as per policy clause no.5.5.4.
19) Reason for Registration of Complaint: - Rejection of Mediclaim.
20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN
21) Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. The Insurance Company stated
that the claim was not settled because the required documents in original were misplaced in transit and the
Insured was unable to submit the same to the Insurance Company. The Complainant stated that she could not
submit the original documents as they got lost in transit by the DTDC Courier.
I have examined the documents exhibited and oral submissions made by both the parties. Original documents
were evidently misplaced by the courier service in transit. This is not the fault of the complainant. Hence, the
Complainant is directed to submit the Indemnity Bond to the Insurance Company that no claim payment was
received from any other forum and that she will not claim for the same claim from any other forum. The
Insurance Company is directed to pay admissible claim to the Complainant on submission of such a bond.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 13.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. PIYUSH KUMAR SINGHAL V/S NATIONAL INSURANCE CO. LTD.
COMPLAINT REF. NO: NOI-G-048-1920-0028
AWARD NO:
1.
Name & Address of the Complainant
Sh. Piyush Kumar Singhal,
R/O 602, Emperor-02,
Supertech Emerald Court,
Sector 93 A, NOIDA
Uttar Pradesh-201304.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
S.I.
460809501810000018
Baroda Health Policy
03.08.2018 to 02.08.2019
Rs.5,00,000/- (Floater)
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the Complainant is directed to submit the
Indemnity Bond to the Insurance Company that no claim payment was received from any
other forum and nor she would claim for the same claim from any other forum. The
Insurance Company is directed to pay admissible claim to the Complainant on submission
of such a bond.
The complaint is treated as disposed off accordingly.

3.
Name of the insured
Name of the policyholder
Ms. Shelley Singhal
Sh. Piyush Kumar Singhal
4.
Name of the insurer
National Ins. Co. Ltd.
5.
Date of Repudiation
Various
6.
Reason for repudiation
Treatment given to the patient does not support
the need for hospitalization
7.
Date of receipt of the Complaint
23.04.2019
8.
Nature of complaint
Claim repudiated
9.
Amount of Claim
N.A.
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
Rs.1,73,245/- Under various claims
12.
Complaint registered under
IOB rules, 2017
13 (2)
13.
Date of hearing/place
04.10.2019 / NOIDA
14.
Representation at the hearing
qq) For the Complainant
Sh. Piyush Kumar Singhal
rr) For the insurer
Sh. Ashutosh Solankey, Asstt. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
17.12.2019
17. Brief Facts of the Case:- Sh. Piyush Kumar Singhal, the Complainant and his wife Ms. Shelley Singhal and
two sons were insured under National Ins. Company’s Baroda Health Policy No. 460809501810000018 for the
period from 03.08.2018 to 02.08.2019 for the S.I. of Rs.5,00,000/- (Floater). Various claims of his wife for
Carcinoma Right Breast were rejected by the Insurance Company. Aggrieved, he requested the insurer including
its GRO to reconsider the claim but failed to get any relief. Thereafter, he preferred a complaint to this office for
resolution of his grievance.
18. Cause of Complaint:-
Complainant’s argument:- The Complainant stated that his wife Ms. Shelley Singhal was suffering from
Carcinoma Right Breast with Brain Metastasis and cervical nodes. Due to disease progression, she was
advised chemotherapy with Kadcyla by Dr. Manish Singhal, Sr. Medical Oncologist at Indraprastha Apollo
Hospital, Delhi. She received Chemotherapy with Kadcyla on 24.08.2018 at Indraprastha Apollo Hospital. A
bill of Rs.15,439/- was raised by the Hospital for said treatment and total expenses including pre
hospitalization tests and pharmacy came out to be Rs.49,104/-.
The above referred claim was filed with the TPA for Reimbursement of above amount on 04.09.2018. The
TPA has unjustifiably denied the claim on 27.11.2018 stating clause 4.13 of policy wording as basis of
repudiation.
The Complainant sought the relief for the claim amount of Rs. 1,73,245/- (Rs. 49,104/- + Rs.1,21,141/-)
alongwith interest at a rate of 2% above bank rate of April, 2019 as per clause 5.6.5 (iv) of the policy wordings
from respective due dates to the date of payment.
Insurers’ argument:- The Insurer in their SCN stated that Sh. Piyush Kumar Singhal along with his spouse
Ms. Shelley Singhal and two sons Mr. Aarush Singhal and Mr. Sparsh Singhal were covered for floater Sum
Insured of Rs.5,00,000/- under Baroda Health Policy numbered 460809501810000018 for policy period from
03.08.2018 to 02.08.2019.
Claim was filed with TPA for reimbursement of below mentioned claims total amount of Rs.1,21,141/- :
• MDI4523093 for claim amount of Rs.78,742/-
• MDI4578264 for claim amount of Rs.30,815/-
• MDI4620073 for claim amount Rs.14,584/-
Insured’s spouse Ms. Shelley Singhal had been under treatment for Carcinoma Breast since 2015 and presently
diagnosed to have Brain and Cervical Nodes Metastasis. Due to disease progression, she was advised
Chemotheraphy with Kadcyla by Dr. Manish Singhal, Sr. Oncologist at Indraprastha Apollo Hospital, New
Delhi and the same was repudiated / not admitted by the Insurer.
Reason for non-admissibility of the claim was as follows:
i. TPA after scrutiny of complete claim documents observed that the claim was not admissible in view
of “that as per claim documents received, it was observed that the treatment given to the patient did
not support the need for hospitalization hence claim was repudiated”. Claim was not admissible as
per policy clause no.4.13 which states “All expenses incurred at hospital primarily for diagnostic, X-
ray or laboratory examinations or other diagnostic studies not consistent with nor incidental to the
diagnosis and treatment of positive presence of any ailment, sickness or injury for which confinement
is required at a hospital”.
ii. Claimant received Hormonal therapy and immunotherapy and on the same point stand taken by
National Insurance Company’s Health Deptt., Head Office was as under:-
• Hormonal therapy/immunotherapy will be payable only if it forms a part of inpatient treatment in
case of hospitalization or part of discharge advice upto the limits for post hospitalization. Not
payable if hospitalization is done only for administration of medicine/drug”.
19) Reason for Registration of Complaint: - Repudiation of Mediclaim
20) The following documents were placed for perusal.

a) Customer complaint
b) Annexure VI and VI (a)
c) Reply of Insurance Company
d) SCN
22) Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. The Insurance Company stated
that that as per claim documents received, it was observed by them that the treatment given to the patient did
not support the need for hospitalization hence claim was repudiated. The complainant confirmed that the drug
Kadcyla could only be administered during hospitalization. During the hearing on 04.10.2019, the complainant
was asked to submit the certificate from the doctor that the drug Kadcyla could only be administered during
hospitalization. The complainant submitted the certificate of Dr. Manish K. Singhal dated 04.10.2019 to this
office. Documents submitted by the complainant on 10.10.2019 were forwarded to the Insurer on same day
wherein it was asked to the Insurer to submit their final position with regard to rejected claim. No clarification
has been received from the Insurer till date i.e. 17.12.2019. It is apparent that they have nothing to say further
in the matter. The deficiency in service by the insurer is self proved.
I have examined the documents exhibited and oral submissions made by both the parties. The treating doctor
is the best person to decide whether the procedure can be done on OPD basis, as an in-patient or in Day Care
Procedure. It is for the treating doctor to take the decision in the best interest of the patient. Hence, the
Insurance Company is directed to pay the admissible claim to the Complainant.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 17.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. KAILASH CHAND JOSHI V/S THE NEW INDIA ASSURANCE COMPANY LTD.
COMPLAINT REF: NO: NOI-H-049-1920-0131
1.
Name & Address of the Complainant
Mr. Kailash Chand Joshi
C/o LIC of India, Pithoragarh, Uttarakhand-
262501
2.
Policy No:
Type of Policy
Duration of policy/Policy period
12070034180400000004
Group Mediclaim Insurance Master Policy
01.04.2018 to 31.03.2019
3.
Name of the insured
Name of the policyholder
Mr. Kailash Chand Joshi
Mr. Kailash Chand Joshi
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
23.04.2019
6.
Reason for repudiation
Policy Clause F Exclusion VI : Use of Intoxicating
drugs/alcohal
7.
Date of receipt of the Complaint
08.07.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.1,00,525/- (as per Annex. VIA)
10.
Amount and date of Partial Settlement
Nil
11.
Amount of relief sought
Rs. 1,00,525/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019
14.
Representation at the hearing
ss) For the Complainant
The complainant was absent but he requested to
settle the matter on merits.
tt) For the insurer
Ms. Monika Goyat, AO Legal
15
Complaint how disposed
Award
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the Insurer is directed to pay the admissible
claim to the complainant.
The complaint is treated as disposed off accordingly.

16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. Kailash Chandra Joshi against New India Assurance
Co. for repudiation of his hospitalization claim.
18) Cause of Complaint:
a. Complainant’s argument: The complainant being an employee of LIC of India was covered under Group
Mediclaim Policy, taken by his employer, since 1988. He was hospitalised on 26.09.2018 to 29.9.2018 in Max
Hospital. He submitted claim for hospitalization bill to the insurance company but they rejected the claim.
b. Insurers’ argument: The insurance company submitted their SCN 27.11.2019 wherein they stated that Mr.
Kailash Chandra Joshi, an employee of LIC of India, was admitted in Max Super Speciality Hospital from 26.9.2018
to 29.9.2018. He was diagnosed with Liver Cirrhosis (Ethanol Related), PHTN Decompensated with Ascites, Small
Esophageal Varices with RCS (+), UGI Bleed ELV done, Alcohol Withdrawal, CPT-8. The claim was submitted for
Rs.2,34,763/-. The Discharge Summary dated 29.9.2018 clearly mentioned that the patient was admitted for Liver
Cirrhosis (Ethanol Related)/Alcohol Withdrawal. The admission was for Abdominal Distension and UGI Bleed
which were caused due to Ethanol Intake/Alcohol Withdrawal. He was advised to Stop Alcohol. The ailments i.e.
Ethanol related Liver Cirrhosis/Alcohol Withdrawal was also mentioned on the OPD Consultation paper dated
11.10.2018. During the hospitalisation, the complainant was treated for alcohol related ailment hence the claim was
not payable as per Policy Exclusion F Point no. vi which read as under:
“Convalescence, general disability, ‘Run-down’ conditions or rest cure, obesity treatment and its complications,
congenital external disease/defects or anomalies, treatment relating to all psychiatric and psychosomatic disorder,
infertility, sterility, use of intoxicating drugs/alcohol, use of tobacco leading to cancer”.
Hence, they rejected the claim on the above grounds.
19. Reason for Registration of Complaint: - Repudiation of claim.
20) The following documents were placed for perusal.
a) Complaint letter
b) Policy document
c) SCN
d) Discharge Summary/OPD Card
21) Observations and Conclusion:
The complainant was absent in personal hearing on 27.12.2019 but he sent his written request on 23.12.2019 to
settle the matter on merits. The insurance company appeared for personal hearing and reiterated that they had rightly
repudiated the claim as the hospitalization/treatment was for Cirrhosis Ethonal related/Alcohol withdrawal. As per
Exclusion F of the policy claim due to use of intoxicating drugs/alcohol is not payable.
On going through the documents exhibited and the oral submissions made by the insurance comapny during the
hearing, it is observed that the complainant lodged claim for Liver Cirrhosis (Ethanol Related/Alcohol Withdrawal.
It is evident from Discharge Summary dated 29.9.2019 that the complainant was admitted in hospital with the
complaints of Abdominal Distention and UGI Bleed. He was diagnosed with Liver Cirrhosis (Ethanol Related),
PHTN Decompensate with Ascites, Small Esophageal Varices with RCS (+) UGI Bleed, EVL Done, Alcohol
Withdrawal CPT-B. He was advised to stop Alcohol. Secondly, on the OPD Card dated 11.10.2018 – Clinical
Presentation – Liver Cirrhosis (Ethanol Related) and Alcohol Withdrawal are mentioned. Moreover, the complainant
did not raise any objection to the cause of rejection of claim due to alcohol but requested to pay claim on
sympathetical ground. The insurance company has rightly repudiated the claim as per the policy Exclusion No. F,
point no vi – treatment related to alcohol/use of intoxicating drugs was not payable.
I see no reason to interfere with the decision of the insurance company to repudiate the claim. The complaint is
dismissed.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company had rightly repudiated the claim as per the terms,
conditions and exclusions of the policy. I see no reason to interfere with the decision of
the insurance company.
The complaint is dismissed accordingly.

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. VIJENDRA KUMAR GARG V/S THE NEW INDIA ASSURANCE COMPANY LTD.
COMPLAINT REF: NO: NOI-H-049-1920-0131
1.
Name & Address of the Complainant
Mr. Vijendra Kumar Garg,
A-8, Sector-15, Noida, UP-201301.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
32310034179500000034
New India Mediclaim Policy
03.09.2017 to 02.09.2018
3.
Name of the insured
Name of the policyholder
Mr. Vijendra Kumar Garg
Mr. Vijendra Kumar Garg
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
23.04.2019
6.
Reason for repudiation
Section 2.16 po policy – Treatment could have
been taken in OPD, no requirement of
hospitalization.
7.
Date of receipt of the Complaint
29.07.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 79,853/-
10.
Amount and date of Partial Settlement
Nil
11.
Amount of relief sought
Rs. 79,853/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019
14.
Representation at the hearing
uu) For the Complainant
Mr. Vijendra Kumar Garg, Self
vv) For the insurer
Mr. Abhinandan Choudhary, A.O.
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. Vijendra Kumar Garg against New India Assurance
Co. for repudiation of his hospitalization claim.
18) Cause of Complaint:
a. Complainant’s argument: The complainant and his wife were covered under New India Mediclaim Policy vide
policy no. 32310034179500000034 for the period from 03.09.2017 to 02.09.2018. The complainant was admitted in
Delhi Pain Management Centre for a procedure to treat ‘L5-S1 PIVD with radiation and PIVD Neuropathy knees’.
He was hospitalized there on 31.08.2018 and was discharged on 01.09.2018, after more than 24 hours. The
hospitalization was done as suggested by the Consultant of the hospital. He submitted hospital bill along with
medical papers to the TPA of the insurance company on 11.09.2018 who repudiated the claim on 23.04.2019, after a
period of eight months; on their own convenient presumption that the treatment is usually done in outpatient
department and did not require hospitalization.
Further, he stated that initially a cashless pre-authorization request was approved by the insurance company for the
same treatment scheduled at SCI International Hospital but he decided to get treatment at DPMC considering it to be
more reputed and economical than SCI International Hospital. Since cashless facility was not available there, he
paid the claim and sent claim papers for reimbursement. The hospitalization was recommended by the specialist who
mentioned that there were multiple procedures involved and hospitalization was required for the same. He requested
this Forum for interest @24% p.a. and additional compensation of Rs.10,000/- for distress.
b. Insurers’ argument: The insurance company submitted their SCN dated 15.10.2019 wherein they stated that the
complainant was admitted in Delhi Pain Management Centre on 02.09.2018 (date wrongly mentioned) and
diagnosed with L5-S1 PVID with radiation and PVID neuropathy knees. As per international protocols and
standards the procedure was to be administered on OPD basis under local anaesthesia. (They submitted expert’s
opinion/medical references alongwith the SCN). As per Section 2.16 of the policy the claim was not payable that
that stated – “Hospitalization means admission in a hospital for a minimum period of 24 hours consecutive hours of
inpatient care except for special procedure/treatment as mentioned in Annexure I, where such admission could be
for a period of less than twenty four consecutive hours. Note: Procedures/Treatments usually done in outpatient
departments are not payable under the policy even if converted as in-patient in the hospital for more than twenty
four consecutive hours”.
The insurance company further submitted that the delay in settlement of claim was on the grounds that the
concerned TPA, M/s E-Meditek, was being investigated by IRDAI for financial irregularities. Later on, the custody
of files was given to the policy issuing office who settled the claims.
20. Reason for Registration of Complaint: - Repudiation of claim.
21. The following documents were placed for perusal.
a) Complaint letter
b) Policy document
c) SCN
d) Medical References
21. Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant stated that he was insured with the insurance company for the past 25 years. He
was planning for treatment for neuropathic knee pain from SCI International Hospital. The hospital sent an estimate

bill of Rs. 1,29,600/- to the TPA on 06.06.2018 and the TPA gave its approval on 09.06.2018. Later on, the
complainant planned the treatment to be done at a more reputed Delhi Pain Management Centre on 31.08.2018. He
submitted claim bill to the TPA on 11.09.2018. They did not reimburse the claim and after a period of 8 months of
sending claim documents, rejected the claim on the ground that the treatment could be done on OPD basis and the
hospitalization was not required. The insurance company reiterated that there was delay in settling claim as the TPA
was suspended by the IRDAI. The insurance company got their claim files back in April, 2019 and thereafter they
settled the claim. As per the international protocols and standards of procedure the treatment could be administered
on OPD basis, hence, they rejected the claim as per section 2.16.
On going through the documents exhibited and the oral submissions made by both the parties during the hearing, it
is noted that the TPA initially gave approval for the treatment in one hospital, but rejected the same treatment taken
in another hospital. The hospitalization was suggested by the treating doctor considering the line of treatment and
medical condition of the patient. The complainant submitted a certificate dated 25.08.2019 of Dr. G.P. Dureja,
Director, Delhi Pain Management Centre that certified that the treatment was done with mild anesthesia which
required observation. So patient needed one day admission and was discharged on the next day. In the case of
Bhanvarlal Purohit Vs. National Insurance Co. Ltd., the Vadodara District Consumer Dispute Redressal
Forum in August, 2018, ruled that “No insurance company can decide the line of treatment to be given to a
patient, only doctors can decide about the treatment”. The forum upheld the evidence and observed that the
TPA had given its opinion after examining the case papers only. “Opinion of the doctor who treated patient is
more truthful than the TPA's opinion which is based on examination of case papers,” the forum stated. The
ground on which the claim was rejected by the insurance company is unjustified and deserves to be set aside.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. S.N. ARORA V/S THE NEW INDIA ASSURANCE COMPANY LTD.
COMPLAINT REF: NO: NOI-H-049-1920-0173
1.
Name & Address of the Complainant
Mr. S.N. Arora,
C/o LIC of India, S.O. Quila, Bareilly, UP-243003.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
12070034160400000004
Group Mediclaim Insurance Master Policy
01.04.2016 to 31.03.2017
3.
Name of the insured
Name of the policyholder
Mr. Shubham Arora
Mr. S.N. Arora
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
19.06.2018
6.
Reason for repudiation
Policy Clause F Exclusion VI : Use of Intoxicating
drugs/alcohal
7.
Date of receipt of the Complaint
03.09.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.8,53,064/-
10.
Amount and date of Partial Settlement
Nil
11.
Amount of relief sought
Rs. 8,53,064/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019
14.
Representation at the hearing
ww) For the Complainant
Mr. S.N. Arora, Self
xx) For the insurer
Ms. Monika Goyat, AO Legal
15
Complaint how disposed
Award
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company is directed to pay the claim as per the terms and
conditions of the policy.
The complaint is closed accordingly.

16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. S.N. Arora against New India Assurance Co. for
repudiation of hospitalization claim of his son, Mr. Shubham Arora.
18) Cause of Complaint:
a. Complainant’s argument: The complainant, being an employee of LIC of India, was covered alongwith his
family members, under Group Mediclaim Policy taken by his employer. His son, Mr. Shubham Arora was
hospitalised in Indraprastha Apollo Hospital, New Delhi on 06.02.2017 due to problem of Diabetic Ketoacidosis and
Nose injury. He was discharged on 21.02.2017. He submitted claim papers to the insurance company, New India
Assurance Co., on 08.03.2017 through the TPA, Raksha. The insurance company rejected his claim on 28.06.2018,
after a period of one year and four months, on the grounds of Clause F-vi, use of intoxicating drugs/alcohol. The
complainant stated that his younger son was riding bike wearing helmet and the elder son, Mr. Shubham Arora, was
sitting behind. Due to applying high brake to save a dog, Shubham’s nose banged into the helmet and started
bleeding from nose. He further stated that his son had no past history of alcoholic disease and all problems arose
after nose injury. He was not habitual alcoholic. He disclosed honestly that the patient takes alcohol occasionally for
only last six months. The reason of hospitalization was nose injury and not alcoholic disease.
b. Insurers’ argument: The insurance company submitted their SCN dated 10.12.2019 wherein they stated that Mr.
Shubham Arora was admitted in Indraprastha Apollo Hospital from 06.02.2017 to 21.02.2017. He was diagnosed
with Type 1 diabetes presented in diabetic ketoacidosis, Aspiration Pneumonitis (Right lower zone opacity), acute
pancreatitis, Alcohol Liver Disease. The claim was lodged for Rs.853064/-. Two days before the admission in
Apollo Hospital, the patient was met with RTA (Road Traffic Accident) which led to bleeding from nose and was
admitted in hospital and was discharged after first aid. He started developing agitated behaviour (aggressive
behaviour) and lost his consciousness so he was rushed to Sri Ram Murti Swastika Hosptal where he was
mechanically ventilated and conservatively managed for one day. Then, he was shifted to Apollo Hospital fur
further management where various investigation and tests were conducted. As per the Discharge Summary the
patient was diagnosed with Alcoholic Liver Disease, and as per personal history, the patient was taking alcohol
occasionally for the past six months. He was referred to Dr. A. Bhagat, Sr. Consultant Psychiatry, for alcoholic
problem and he was prescribed medicines for the same. Hence, the claim was not payable as per Policy Exclusion F
Point no. vi which read as under:
“Convalescence, general disability, ‘Run-down’ conditions or rest cure, obesity treatment and its complications,
congenital external disease/defects or anomalies, treatment relating to all psychiatric and psychosomatic disorder,
infertility, sterility, use of intoxicating drugs/alcohol, use of tobacco leading to cancer”. The claim was rejected as
per the terms and conditions of the policy.
19)Reason for Registration of Complaint: - Repudiation of claim.
20) The following documents were placed for perusal.
a) Complaint letter
b) Policy document
c) SCN
d) Discharge Summary
21) Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant stated that his son met with an accident and sustained nose injuries. He
submitted claim documents to the insurance company through TPA on 08.03.2017 but after a period of 16 months
they rejected the claim as per exclusion F – use of intoxicating drugs/alcohol. He has further stated that his son is not
habitually alcoholic but takes alcohol occasionally for the past 6 months only. He disclosed this fact honestly and the
insurance company rejected the nose injury claim on this invalid ground. The insurance company on the other hand,
reiterated that as per the discharge summary, the patient was diagnosed with Alcoholic Liver Disease, and the
personal history also mentioned that the patient was taking alcohol occasionally for the past 6 months. Hence, the
claim was repudiated as per policy exclusion F vi – use of intoxicating drugs/alcohol.
On going through the documents exhibited and the oral submissions made by both the parties during the hearing, it
is evident that the hospitalization of the insured was basically due to road accident and nasal bleeding. The date of
accident of the insured was 04.02.2017 and after the accident, he was taken to Patel Hospital & SP Poly Clinic. The
OPD card clearly mentioned RTA & Nasal Bleeding. The patient was then admitted in Shri Ram Murti Smarak
Institute of Medical Sciences, Bareilly on 06.02.2017 and the discharge summary dated 06.02.2017 also mentioned
in Clinical Summary part - Head Injury 2 days back and traumatic nasal bleeding. The Discharge Summary of
Apollo Hospital stated that the patient was diagnosed with Type 1 diabetes presented in diabetic ketoacidosis,
Aspiration pneumonitis (Right lower Zone opacity), acute pancreatitis and Alcoholic liver disease. He was brought
to the hospital in unconscious state and was mechanically ventilated with the history of injury to nose while riding
bike 2 days back. The patient was a known case of Type 1 diabetes for past three years on insulin therapy.
Pertinently, the cause of hospitalization was nasal injury, and not any disease related to the alcohol. The insurance
company has failed to prove that the hospitalization was due to alcoholic disease or any disease related to alcohol.
Occasional drinking for the past 6 months does not make the insured alcoholic, to be denied the benefit of insurance
policy under Exclusion F vi. It is also noted that there is gross deficiency on the part of the insurance company as
they took more than 16 months to reject the claim on the ground of exclusion F – alcohol, which is not justified. The
insurance company is directed to pay the claim as per the terms and conditions of the policy.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company is directed to pay the claim as per the terms and conditions of
the policy.
The complaint is closed accordingly.

22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF DINESH KUMAR JAIN V/S THE ORIENTAL INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-050-1920-0112
1.
Name & Address of the Complainant
Mr. Dinesh Kumar Jain
F-2/195, Police Street, Meerut-25001, UP
2.
Policy No:
Type of Policy
Duration of policy/Policy period
252400/48/2019/1334
PNB-ORIENTAL Mediclaim Policy-2017
02.07.2018 to 01.07.2019
3.
Name of the insured
Name of the policyholder
Mr. Dinesh Kumar Jain
Mr. Dinesh Kumar Jain
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
Not repudiated
6.
Reason for repudiation
Not repudiated
7.
Date of receipt of the Complaint
01.07.2019
8.
Nature of complaint
Partial payment of claim
9.
Amount of Claim
Rs. 133920/-
10.
Amount of Partial Settlement
23.01.2019
11.
Amount of relief sought
Rs. 9826/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019 at Noida
14.
Representation at the hearing
a) For the Complainant
Mr. Dinesh Kumar Jain, Self
b) For the insurer
Ms. Praveena Choudhary, AM
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. Dinesh Kumar Jain against The Oriental Insurance
Company Ltd. for partial payment of his hospitalization claim.
18. Cause of Complaint:
a)Complainant’s argument: The complainant and his family members were covered under PNB-Oriental
Mediclaim Policy-2017 vide policy no. 252400/48/2019/1334, issued for the period from 02.07.2018 to 01.07.2019.
The complainant got admitted in Fortis Hospital on 14.11.2018 and was discharged on 15.11.2018. He submitted
claim documents to the TPA, M/s Raksha, for reimbursement of his claim bill. The TPA deducted Rs. 9826/-
towards hospital discount not payable as per the terms and conditions of the policy. He requested the TPA to
reimburse this amount to him but they denied his request on the ground of application of MOU on reimbursement
cases. Hence, he approached this Forum for reimbursement of balance claim amount of Rs. 9826/-.
b)Insurers’ argument: The Insurance Company in their SCN dated 06.09.2019 stated that the complainant and his
family members were covered under PNB-Oriental Mediclaim Policy-2017 vide policy no. 252400/48/2019/1334.
This policy was issued for the period from 02.07.2018 to 01.07.2019 for the sum insured of Rs. 5 lakhs. The
complainant submitted reimbursement bill whereas the hospital was a network hospital. The insurance company
clarified that as per their policy terms and conditions and circular of their Head Office, in reimbursement cases, the
rates applicable shall remain as per agreed rates. The TPA deducted Rs. 9776/- from the claim amount and paid
Rs.1,03,571/-. The complainant did not apply for cashless facility since the hospital was a network hospital, if he
would do so, he would automatically get the discounted rates from the hospital. The deductions were made as per
the terms and conditions of the policy.
19) Reason for Registration of Complaint: - Partial payment of Claim
20) The following documents were placed for perusal.
a) Complaint letter
b) Claim settlement Voucher
c) Policy document
d) SCN
21) Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant stated that the insurance company deducted Rs.9,826/- as 2.5% hospital
discounts, and he had to pay this amount by his own. The insurance company reiterated that the complainant was
admitted in Fortis Hospital which is a network hospital. The rates in network hospitals are discounted rates as per
the MOU signed between the hospitals and insurance company/TPAs. When an insured get admitted in network
hospitals he get the benefit of cashless facility under pre-agreed rates between the insurance company and hospital.

The complainant did not apply for cashless facility, otherwise he would have get the treatment at discounted rates.
The insurance company cannot pay claim beyond the prescribed limit. During the discussion, the complainant was
asked whether he applied for cashless facility and if so, he was asked to show the proof. The complainant denied the
same.
On going through the documents exhibited and the oral submissions made by both the parties during the hearing, it
is observed that the Policy Condition 5.2 states that : Conditions applicable subsequent to claims : iii : Procedure for
availing cashless access services in Network Hospital/Nursing Home : (d) “Liability under the policy in respect of
all expenses incurred in a Network Provider shall be subject to the pre-agreed rates between the Company/TPA and
the Network Provider. This is irrespective of the claim being under cashless or re-imbursement.” In this case, the
complaint did not opt for cashless facility but sent bill for reimbursement of his claim. The TPA/insurance company,
deducted an amount of Rs. 9826/- being 2.5% Hospital Discount deducted on consumable charges, 2.5% Hospital
Discount deducted on medication charges and 10% Hospital Discount deducted on bill. The insurance company had
rightly deducted an amount of Rs.9826/- as per the MOU signed between the insurance company and network
hospital. I see no reason to interfere with the decision of the insurance company.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF LAL CHAND BINDAL V/S THE ORIENTAL INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-050-1920-0159
1.
Name & Address of the Complainant
Mr. Lal Chand Bindal,
Vishnudham, New Madho Nagar, Saharanpur, UP-
247001.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
254101/48/2019/1024
PNB-ORIENTAL Mediclaim Policy 2017 – Group
Health Insurance for bank account holders
23.08.2018 to 22.08.2019
3.
Name of the insured
Name of the policyholder
Mrs. Nirmala Bindal
Mr. Lal Chand Bindal
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
Not repudiated
6.
Reason for repudiation
Not repudiated
7.
Date of receipt of the Complaint
17.09.2019
8.
Nature of complaint
Partial payment of claim
9.
Amount of Claim
Rs. 83380/-
10.
Date of Partial Settlement
Rs. 40,224/-
11.
Amount of relief sought
Rs. 83380/- as per Annex VI A
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019 at Noida
14.
Representation at the hearing
a) For the Complainant
Mr. Amit Kumar Bindal, Son
b) For the insurer
Mr. Rakesh Kumar, A.M.
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. Lal Chand Bindal against The Oriental Insurance
Company Ltd. for partial payment of hospitalization claims of his wife, Mrs. Nirmala Bindal.
18. Cause of Complaint:
Complainant’s argument: The complainant and his wife Mrs. Nirmala Bindal, were covered under under PNB-
Oriental Mediclaim policy vide policy no. 254101/48/2019/1024 for the period from 23.08.2018 to 22.08.2019 for a
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company had rightly deducted an amount of Rs.9826/- as per the
MOU signed between the insurance company and network hospital. I see no reason to
interfere with the decision of the insurance company.
The complaint is closed accordingly.

sum insured of Rs. 5 lakhs. His wife was admitted in Saksham Hospital, Saharanpur, in September, 2018 and later
on, she was admitted in Medanta Hospital, Gurgaon. The total bill was Rs. 47,321. The hospital provided him
receipt for Rs. 10,000/- at the time of admission but they did not provide receipt of balance amount of Rs. 37321/-
paid by him. He submitted all claim documents to Raksha TPA. The TPA asked for the receipt for Rs. 37321/- and
the same was submitted to them vide registered post on 13.12.2018 that was received in their office on 19.12.2018.
The file was reviewed by the TPA and they further asked for ID proof and Receipt of Saksham Hospital for Rs.
8.950/-. He submitted these documents on 24.1.2019. His claim was recommended by the Divisional Manager but
they again asked for the receipt of Rs.37321/- that he had already submitted. He received one claim for Rs. 7,773/-
via neft ON 31.07.2019. The complainant was aggrieved by the delay in settlement of claim and negligence on the
part of TPA and the insurance company.
Insurers’ argument: The Insurance Company in their SCN wherein they stated that the claim for the medical
expenses incurred for treatment of acute acalculous choleystitis at Medanta Hospital had been paid for Rs. 40,224/-
on 19.09.2019. They further clarified that the claim amount was Rs.83,380/-, deductions was Rs. 43,156/- and the
claim amount was Rs. 40,224/-. These deductions were made for room rent entitled and subsequent expenses, non
payable items, admission charges, ambulance charges and claim file separated. They submitted Claim Settlement
Voucher to show the deductions. They have settled the claim as per the entitlement, terms and conditions of the
policy.
19) Reason for Registration of Complaint: - Repudiation of Claim.
20) The following documents were placed for perusal.
a) Complaint letter
b) Claim settlement Voucher
c) Policy document
d) SCN
21) Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant’s son stated that his father, Mr. Lal Chand Bindal, paid Rs. 83,380/- towards
hospitalization bills of Medanta Hospital and Saksham Hospital, but the insurance company reimbursed him only
Rs. 40,224/- and deducted Rs. 43,156/-. He referred his case to the insurance company many times but they never
replied. The insurance company reiterated that the deductions were made as per the recommendations of TPA as per
the terms and conditions of the policy.
On going through the documents exhibited and the oral submissions made by both the parties during the hearing, it
is noted that the complainant paid hospital bill of Medanta for Rs. 83,380/-, out of which the insurance company has
paid only Rs.40,224/-. The deductions of Rs.43,156/- were made by the TPA/insurance company. The deductions
have been made as under:
Total hospitalization bill of Saksham
Hospital and Medanta Hospital
83,380/-
paid by the insurance company
40,224/-
Disputed amount
43,156/-
Disputed amount
43,156/-
pre-post hospitalization amount
16,243/-
Settlement under this head was done for Rs.
7773/- Balance of Rs. 8,400/- was deducted for
the reason acommodation charges not payable
as the admission was for investigation purpose
and Rs. 20/- for Infusion Set. Deductions made
as per the policy conditions.
balance of disputed amount
26,913/-
Deductions towards Ambulance charges
17,500/-
Appropriate deducted as per the policy
conditions.
balance of disputed amount
9,413/-
Deductions in room rent
3,000/-
As per room capping in policy
6,413/-
Doctor's fees
765/-
As per room capping in policy
5,648/-
Investigation Charges
525/-
X-ray film not attached
5,123/-
Investigation Charges
51/-
As per room capping in policy
5,072/-
Lab charges
1,819/-
As per room capping in policy
3,253/-

Medication charges
2,903/-
non payable items as per the policy
350/-
Admission charges
350/-
not payable as per the policy conditions.
Balance
0
Hence, the insurance company had settled the claim as per the terms and conditions of the policy. I see no reason to
interfere with the decision of the insurance company.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF RENESH JAIN V/S THE ORIENTAL INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-050-1920-0176
1.
Name & Address of the Complainant
Mr. Renesh Jain,
H-39, Sita Ram Colony, Balkeshwar, Agra,
UP-282005.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
272800/48/2018/7212
PNB-ORIENTAL Royal Mediclaim Policy :
16.03.2018 to 15.03.2019
3.
Name of the insured
Name of the policyholder
Mr. Rajendra Kumar Jain
Mr. Rajendra Kumar Jain
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
15.10.2019
6.
Reason for repudiation
Clause 2.5 – Day Care Treatment is not payable
7.
Date of receipt of the Complaint
17.09.2019
8.
Nature of complaint
Repudiation of claims
9.
Amount of Claim
Rs. 17,000/- and Rs.30,040/-
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Rs. 47,040/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019 at Noida
14.
Representation at the hearing
a) For the Complainant
Mr. Renesh Jain, Self
b) For the insurer
Mr. Shubham Raj, A.O.
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. Renesh Jain against The Oriental Insurance Company
Ltd. for repudiation of hospitalization claims of his father, Mr. Rajendra Kumar Jain.
18) Cause of Complaint:
Complainant’s argument: The complainant’s father, Mr. Rajendra Kumar Jain, was covered under under PNB-
Oriental Mediclaim policy. His father was suffering from NHL (Cancer) and was taking treatment under the
supervision of Dr. Ajay Bapna, HOD Oncology, at Bhagwan Mahaveer Cancer Hospital & Research Centre
(BMHRC), Jaipur. The doctor recommended Inj. MABTAS (Rituximab) to be given as 6-8 hours infusion under
medical supervision which required admission for one day for each cycle of Rituximab. His father was admitted in
Day Care on 01.06.2018 for Inj. MABTAS (RITUXIMAB). The cashless request was denied by the TPA. Hence,
he submitted claim for reimbursement of bills on 22.06.2018 and post-hospitalization bills on 23.08.2018 to the TPA
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, I see no reason to interfere with the decision of the insurance company.
The complaint is closed accordingly.

of the insurance company. The TPA repudiated both the claims on 27.9.2018 giving the reason “claimant admitted
for Inj. Mabtas (non-conventional chemotherapy drug), this treatment does not require hospitalization, it can be
treated under OPD and not listed day care procedure. Hence the claim denied under clause 2.5”. The complainant
preferred his claim with the concerned officer of the insurance company and they also rejected the claim giving the
reason “Hospitalization was only for Injection MABTAS (Rituximab), which was not allowed without supporting
other medicine”.
The complainant further quoted two similar cases where Award was given in favour of complainant, namely,
Ombudsman Case of Nikhil Garg Vs. Oriental Insurance Co. Ltd. (Case No. CHD-G-1516-0340) and Case of R.R.
Iyer Vs. Teh New India Assurance Co. Ltd. dated 3.01.2017. The complainant also pleaded that the insurance
company had settled four claims bearing claim nos. 16709452, 17803740, 18131002 and 18490888 where Inj.
MATBAS was given under Day Care Treatment.
Insurers’ argument: The Insurance Company in their SCN dated 13.11.2019 submitted that the insured, Mr.
Rajendra Kumar Jain, was admitted at Bhagwan Mahaveer Cancer Hospital & Research Centre, Jaipur, on
01.06.2018 with NHL. Chemotherapy was given and he was discharged on the same day i.e. 01.06.2018. As per the
discharge summary and other medical documents, he was admitted for Inj. MABTAS (non-conventional
chemotherapy drug) and this treatment did not require hospitalization. It could be treated on OP basis and also not
listed in day-care procedure list. Hence, they denied the claim under Clause 2.5 which stated : DAY CARE
TREATMENT Day Care treatment refers to medical treatment, and/or surgical procedure which is : i. Undertaken
under General or Local Anaesthesia in a hospital/day care centre in less than 24 hrs because of technological
advancement, and, ii. which would have otherwise required a hospitalization of more than 24 hours. Treatment
normally taken on an out-patient-basis is not included in the scope of this definition”.
19) Reason for Registration of Complaint: - Repudiation of Claim
20) The following documents were placed for perusal.
a) Complaint letter
b) Rejection letters
c) Policy document
d) SCN
e) Case references
21) Observations and Conclusion: Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submission. It is evident from the Discharge card dated 01.06.2018 that the complainant’s father Sh. Rajendra
Kumar Jain is a known case of NHL (low grade cancer) and was under the treatment of Dr. Ajay Bapna, HOD
Oncology at Bhagwan Mahavir Cancer Hospital and Research Centre, Jaipur. The patient was given injection
Rituximab as a part of Chemotherapy. This injection is given as 6-8 hours infusion under medical supervision and
the patient is required to be hospitalised for one day for each cycle of Rituximab therapy. The insurer has repudiated
the claim under clause 2.5 of the policy as the treatment did not require hospitalisation and could have been given on
OPD basis.
During the hearing, the complainant has submitted that the insurance company had earlier approved the cashless
claims of his father for Rituximab injection on 02.04.2018, and 20.07.2017 and had also paid the claim on
06.08.2018 and 10.10.2018. Therefore, he is at a loss to understand as to why his claims bearing no-17253925 and
17687398 for the same treatment of his father have been rejected by the insurance company under clause 2.5 of the
policy.
It is observed that Dr. Ajay Bapna has also clarified to the TPA Medi Assist that the injection Rituximab (Anti-
cancer monoclonal anti bodies drug) is an essential part of the cancer treatment …. and can be given only under
doctor’s supervision for which hospitalisation is recommended. It is further noticed that as per insurance policy
clause 2.3, the treatment given to the complainant’s father in the hospital is covered under the terms and conditions
of the policy.
In view of above, the insurance company is directed to pay the two aforesaid claims which are under dispute before
me.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties, the insurance company is directed to pay two claim bearing claim nos.
17253925 and 17687398.
The complaint is closed accordingly.

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF AASHIMA VINAYAK V/S THE ORIENTAL INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-050-1920-0146
1.
Name & Address of the Complainant
Ms. Aashima Vinayak
Defence Estate, Gwalior Road, Agra, UP-282001.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
272800/48/2018/7038
Happy Family Floater 2015
13.02.2018 to 12.02.2019
3.
Name of the insured
Name of the policyholder
Mr. Nirwan Datt
Mrs. Geeta Datt
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
Not repudiated
6.
Reason for repudiation
Not repudiated
7.
Date of receipt of the Complaint
29.07.2019
8.
Nature of complaint
Partial payment of claim
9.
Amount of Claim
Rs. 1,01,000/-
10.
Amount of Partial Settlement
Rs. 47160/-
11.
Amount of relief sought
Rs. 60,770/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019 at Noida
14.
Representation at the hearing
yy) For the Complainant
Mr. Ankit Dutt, Spouse
zz) For the insurer
Absent
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Ms. Aashima Vinayak against The Oriental Insurance
Company Ltd. for partial payment of hospitalization claim of her father, Shri Nirwan Datt.
18. Cause of Complaint:
Complainant’s argument: The complainant’s parents were covered under Happy Family Floater-2015 Policy
bearing Policy No. 272800/48/2018/7038, issued for the period from 13.02.2018 to 12.02.2019. The policy plan
was SILVER and the sum insured was Rs. 2 lakhs. This policy was in continuation from the year 2009-2010. Her
father, Mr. Nirwan Datt, was operated for RT Upper Calyx Calculus at Shanti Vaid Hospital, Agra. The
hospitalization bill was for Rs.1,07,930/- but the TPA of insurance company reimbursed only Rs. 47,160/- and
deducted Rs. 60,770/-. They deducted Rs.50,000/- for Holmium laser, IITV charges and Flexible Uterorenoscop
charges, being non-payable as per guidelines. Further, they deducted Rs. 5,000/- as breakup was not attached
against OT medicines and Rs. 5,240/- as 10% co-payment.
Insurers’ argument: The Insurance Company in their SCN dated 23.09.2019 wherein they stated that the claim for
reimbursement of hospitalization for Rs. 1,07,400/- was settled by their TPA, Raksha Health Insurance, as per the
policy’s guidelines. As per the recommendation of the TPA, the following amount were not admissible in the claim
amount:
i. Holmium Laser Charges Rs.24,000/-
ii. Flexible Uterorenoscop Rs. 24,000/-
iii. IITV Rs. 2,000/-
iv. OT Medicines (breakup not attached) Rs. 5,000/-
v. 10% Co-payment (mandatory) Rs. 5,240/-
vi.
The insurance company further stated that they requested the insured to provide breakup of OT medicines for
releasing the balance admissible amount. They paid Rs. 47,160/- being the admissible claim amount on 07.03.2019.
The insurance company clarified that the insured had taken the lowest cover plan i.e. Silver Plan which provide only
reasonable charges for medically and necessary treatment only for illness/diseases contracted/suffered or injury
sustained by the insured during the policy period upto the limit of sum insured.
19) Reason for Registration of Complaint: - Partial payment of Claim
20) The following documents were placed for perusal.
a) Complaint letter
b) Claim settlement Voucher
c) Policy document
d) SCN
21) Observations and Conclusion: - The complainant’s spouse was present and the insurance company was absent
for personal hearing on 27.12.2019. The complainant’s spouse stated that the policy was in continuation from the
year 2009 and not a single claim was lodged. The insurance company deducted Rs. 60,770/- from the hospital bill
for Rs.1,07,930/-
On going through the documents exhibited and the oral submissions made by the complainant’s representative
during the hearing, it is noted that the insured was hospitalized for the treatment for RT Upper Calyx Calculus. The
treating doctor adopted the method of Holmium Laser treatment as a more effective and potentially less costly
surgery for urinary obstruction. In this case the line of treatment was decided by the treating doctor, keeping in view
the medical conditions of the insured. The deduction made towards advanced technological treatment like Holmium
Laser Charges, Flexible Uterorenoscop and IITV do not fall under the exclusions of the policy. In the case of

Bhanvarlal Purohit Vs. National Insurance Co. Ltd., the Vadodara District Consumer Dispute Redressal
Forum in August, 2018, ruled that “No insurance company can decide the line of treatment to be given to a
patient, only doctors can decide about the treatment”. The forum upheld the evidence and observed that the
TPA had given its opinion after examining the case papers only. “Opinion of the doctor who treated patient is
more truthful than the TPA's opinion which is based on examination of case papers,” the forum stated. The
ground on which the claim was rejected by the insurance company is unjustified and deserves to be set aside. The
insurance company in their SCN was also ready to pay Rs. 5000/- which was deducted towards breakup of
medication charges not given, if the same would be provided by the complainant. The insurance company is directed
to settle the disputed amount after receiving required documents from the complainant within a month under
intimation to this office.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. SUBHASH SINGHAL V/S UNITED INDIA INSURANCE COMPANY LTD.
COMPLAIN REF. NO.: NOI-H-051-1920-0095
1.
Name & Address of the Complainant
Sh. Subhash Singhal
C-38, Sector-12, Noida
Uttar Pradesh-201301.
Phone No.9873280207, 0120-4204491
2.
Policy No:
Type of Policy
Duration of policy/Policy period
190801/48/05/24/00002474
and 190801/48/06/24/00001128
Bhavishya Arogya Policy
25.02.2007 to 24.02.2008
3.
Name of the Insured
Name of the policyholder
Sh. Subhash Singhal
Sh. Subhash Singhal
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of Repudiation
--
6.
Reason for repudiation
--
7.
Date of receipt of the Complaint
15.07.2019
8.
Nature of complaint
Partial payment of maturity amount
9.
Amount of Claim
--
10.
Date of Partial Settlement
19.06.2019
11.
Amount of relief sought
Payment of balance amount plus interest and
compensation of Rs.50,000/- for mental agony
as per Annex VI A
12.
Complaint registered under
IOB rules, 2017
13 (1)(d)
13.
Date of hearing/place
11.12.2019 / NOIDA
14.
Representation at the hearing
aaa) For the Complainant
Sh. Subhash Singhal
bbb) For the insurer
Ms. Rajni Ahuja, Dy. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
26.12.2019
17. Brief Facts of the Case:- Sh. Subhash Singhal, the Complainant had taken Bhavishya Arogya Policy No.
190801/48/05/24/00002474 dated 25.02.2006 and 190801/48/06/24/00001128 for the period from 24.02.2007
to 23.02.2008. At the time of surrender the policy, less premium refunded by the Insurance Company to the
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by both the parties, the insurance company is directed to settle the disputed amount
after receiving required documents from the complainant within a month under
intimation to this office.
The complaint is closed accordingly.

complainant. Aggrieved, he requested the insurer including its GRO to reconsider the fact but failed to get any
relief. Thereafter, he has preferred a complaint to this office for resolution of his grievance.
18. Cause of Complaint:-
A) Complainant’s argument:- Sh. Subhash Singhal, the Complainant stated that premiums of Rs.5,172/-
were paid against both policies (i.e. Total Rs.10,344/-) against which an amount of Rs.10,540/- was paid on
28.03.2019 by UIIC. Almost the same amount of premium was refunded after a period of 12 or 13 years.
The details in the matter are as under :-
i. The complainant submitted copies of policies on 19.04.2018 to the Insurer, so that advance action can be
taken by them for updation of their records.
ii. The complainant surrendered policies on 10.09.2018.
iii. To expedite payment of maturity proceeds, matter was followed up through telephone as well as through
personal visits to Guna Branch office. Since there was no progress, matter was referred to Customer Care
Bhopal vide email dated 11.04.2019.
iv. Subsequently, on 27.12.2018, a grievance was registered at www.pgportal.gov.in and reminder was
registered on 23.03.2019. Once the reminder was registered, officials of UIIC in haste and in arbitrary
manner made on line payment of Rs.10,540/- on 28.03.2019 against these policies.
v. It appears that in order to close the grievance, United India have made the payment in arbitrary manner
which is nothing but harassment of customer.
vi. Vide mail dated 11.04.2019 and 03.05.2019, the matter was referred to Grievance Redressal Officr, United
India but till now there is no response.
vii. Vide e-mail dated 14.05.2019, basis for payment of Rs.10,540/- was sought from Branch Office Guna.
Copy of clarification dated 15.06.2018 obtained by me in a similar case from the Oriental Insurance Co.
viii. Insurer vide e-mail dated 17.05.2019 informed that “With reference to your mail, we clarify that we have
received your letter regarding surrender of Bhavishya Aarogya policies dated 10.04.2018 on 19.04.2018 in
our Branch. As per your policies, you have selected the age of retirement at 60 years, i.e. 11.09.2018.” But
as per your letter, it was clearly written that –“The above policies shall be due for surrender on 11.09.2018.
The copies are being submitted so that advance action may be taken at your end for updation of records
etc.” Based on this, it is clearly understood that you want to surrender the policies after the date of
retirement i.e. after the risk commencement.”
ix. The complainant stated that he has never mentioned in his letter dated 10.04.2019 from which any
inference like I want to surrender the policies after the date of retirement, i.e. after the risk commencement
can be drawn
x. The complainant stated that other companies inform the customer 4-6 months in advance about the maturity
of the Policy, but United India did not inform their customers.
B) Insurers’ argument:- The Insurer in their SCN stated that regarding the complaint, their para wise reply is
as follows:-
i. Complaint Point No.1 is accepted
ii. Complaint Point No.2 is accepted
iii. Regarding Complaint Point No.3 the insurer stated that after receiving intimation from the insured, they
have started working on her refund. Since, the policies were made on their old software “Genisys” it
requires some time to migrate them into their present software “GC”. The same had been intimated to
Insured.
iv. Regarding Complaint Point No.4 the insurer stated that after receiving the grievance in December 2018,
their Regional Office has also taken up the matter and the pending issue for policy migration into GC Core
has been expedited by them and when the same is being done by Regional Office, they had refunded the
amount on insured’s request and as per Bhavishya Arogya Policy Manual after getting payment approval
from their Divisional Office Gwalior on 27.03.2019 amounting Rs.10,540/-
v. Regarding Complaint Point No.5 the insurer stated that they have made the refund only as per the request
from the insured and according to the terms and conditions of the policy but not in any haste or arbitrary
manner.
vi. Regarding Complaint Point No.6, the insurer stated that the fresh grievance raised by complainant via mail
dated 11.04.2019 and 03.05.2019 was not reported to their branch till the time of writing this note.
vii. Complaint Point No.7 is accepted
viii. Complaint Point No.8 is accepted
ix. Regarding Complaint Point No.9, the insurer stated that in the insured’s 1
st
letter to them dated 10.04.2018,
he has nowhere written that he is surrendering the policies on the same date. It was written by him that this
is advance intimation only for updation of records regarding his policies which are due for surrender on
11.09.2018. Since, insured has selected retirement age 60 years, i.e. 11.09.2018. The refund is made as per
our table – “No Claim refund after commencement of risk”.
x. Regarding Complaint Point No.10 the insurer stated that although all the peculiarities of the policies were
explained to the insured before the starting of their contract. They admitted that they have not send any
reminders regarding policy maturity to the insured because the policy was of their old software “Genisys”,
such facilities back then were not incorporated in their systems. Presently through their new software “GC
Core”, this facility has been enabled by them.
The insured has nowhere written about his willingness to surrender the policy before maturity i.e. risk
commencement and has clearly written that he is giving advance intimation for updation of records regarding his
policies which are due for surrender on 11.09.2018. Based on this, it is clearly understood that he wants to surrender
the policies after the selected expiry date i.e.11.09.2018. Accordingly, refund has been made to him as per the
insured request and terms & conditions of their policy.
It is understood that the insured might have gotten some different refund from the Oriental Insurance policy which
he has referred in Point 7, but this could be because of his request for surrender of policy before the risk
commencement. In this case also, if he placed the request for surrendering the policy before the risk commencement
he will be entitled for a higher refund.

19) Reason for Registration of Complaint: - Less payment at the time of maturity of Bhavishya Arogya Policy
20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN
21) Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. Sh. Subhash Singhal, the
Complainant reiterated that he had taken two policies bearing nos.190801/48/05/24/00002474 and
190801/48/06/24/00001128 for Sum Insured of Rs.1,00,000/- each and premium being Rs.5,700/- and Rs.5,805/- on
25.02.2006 and 24.02.2007 respectively. On maturity, Rs.10,540/- were refunded by the respondent company on
28.03.2019 which is almost the same amount which was deposited 11-12 years back. The Respondent Company
contended that the payment has been made as per the rules.
I have gone through the documents submitted by both the parties and observe from the circular of the Bhavishya
Arogya Policy submitted by the Insurer that at point no.1.7, it is mentioned that the basic policy is of Rs.50,000/-
and benefits can be increased in the unit of Rs.10,000/- by paying additional premium. It is noticed that the
complainant had purchased both the policies for sum insured of Rs. I lac each and had paid the additional premium.
However the maturity payment has been erroneously calculated as per basic policy having sum insured of Rs.
50000/- and benefits have not been proportionately increased to the applicable sum insured for which enhanced
premium had been charged. This is grossly unjustified on part of the insurer.
Apropos the issue of maturity amount it is observed that the complainant chose the date of maturity to be the date of
attainment of 60 years of age i.e. 11.09.2018. The application for updation of records was sent on 10.04.2018
wherein the complainant clearly mentioned that “the policy shall be due for surrender on 11.09.2018” i.e. the
attainment of age of 60 years. This means that the complainant wanted the maturity amount. It is observed that the
maturity payment has been correctly made treating the request made after the date of maturity as intended by the
complainant.
The Insurance Company is directed to pay the difference amount by revising the calculation of maturity amount as
discussed above.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 26.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF MS. ANITA SINGHAL V/S UNITED INDIA INSURANCE COMPANY LTD.
COMPLAIN REF. NO.: NOI-H-051-1920-0118
1.
Name & Address of the Complainant
Ms. Anita Singhal
C-38, Sector-12, Noida
Uttar Pradesh-201301.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
190801/48/05/24/00002473
and 190801/48/06/24/00001129
Bhavishya Arogya Policy
25.02.2007 to 24.02.2008
3.
Name of the Insured
Name of the policyholder
Ms. Anita Singhal
Ms. Anita Singhal
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of Repudiation
--
6.
Reason for repudiation
--
7.
Date of receipt of the Complaint
15.07.2019
8.
Nature of complaint
Partial payment of maturity amount
9.
Amount of Claim
--
10.
Date of Partial Settlement
27.03.2019
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by both the parties during the course of hearing, the Insurance Company is directed
to pay the difference amount by revising the calculation for maturity amount.
The complaint is treated as disposed off accordingly.

11.
Amount of relief sought
Payment of balance amount plus interest and
compensation of Rs.50,000/- for mental agony
as per Annex VI A
12.
Complaint registered under
IOB rules, 2017
13 (1)(d)
13.
Date of hearing/place
11.12.2019 / NOIDA
14.
Representation at the hearing
ccc) For the Complainant
Sh. Subhash Singhal
ddd) For the insurer
Ms. Rajni Ahuja, Dy. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
26.12.2019
17. Brief Facts of the Case:- Ms. Anita Singhal, the Complainant had taken Bhavishya Arogya Policy No.
190801/48/05/24/00002473 dated 25.02.2016 and 190801/48/06/24/00001129 for the period from 25.02.2007
to 24.02.2008. At the time of surrender the policy, less premium refunded by the Insurance Company to the
complainant. Aggrieved, she requested the insurer including its GRO to reconsider the fact but failed to get any
relief. Thereafter, she has preferred a complaint to this office for resolution of her grievance.
18. Cause of Complaint:-
a) Complainant’s argument:- Ms. Anita Singhal, the Complainant stated that premiums of Rs.5,166/- each (i.e.
Rs.10,332/-) plus service tax were paid for subject policies. The retirement age selected was 58 years i.e.
24.07.2017. Maturity proceeds of Rs.10,300/- was paid on 28.03.2019 by UIIC against her policies. Less than
amount of premium was refunded after a period of 12 or 13 years. The details in the matter are as under :-
xi. The complainant surrendered policies on 19.04.2018.
xii. To expedite payment of maturity proceeds, matter was followed up through telephone as well as through
personal visits to Guna Branch office. Since there was no progress, matter was referred to Customer Care
Bhopal vide email dated 05.11.2018.
xiii. Subsequently, on 27.12.2018, a grievance was registered at www.pgportal.gov.in and reminder was
registered on 23.03.2019. Once the reminder was registered, officials of UIIC in haste and in arbitrary
manner made on line payment of Rs.10,300/- on 28.03.2019 against these policies.
xiv. It appears that in order to close the grievance, United India have made the payment in arbitrary manner
which is nothing but harassment of customer.
xv. Vide mail dated 07.04.2019 and 22.04.2019, the matter was referred to Grievance Redressal Officr, United
India but till now there is no response.
xvi. The complainant stated that other companies inform the customer 4-6 months in advance about the maturity
of the Policy, but United India did not inform their customers.
The complainant further stated that the Oriental Insurance Company has provided payment details to her husband
and paid maturity value of Rs.17,430/- in year 2018 against premium of Rs.10,000/- in year 2005.
b) Insurers’ argument:- The Insurer in their SCN stated that regarding the complaint, their para wise reply is as
follows:-
xi. Complaint Point No.1 is accepted
xii. Regarding Complaint Point No.2 the insurer stated that after receiving intimation from the insured, they have started
working on her refund. Since, the policies were made on their old software “Genisys” it requires some time to migrate
them into their present software “GC”. The same had been intimated to Insured.
xiii. Regarding Complaint Point No.3 the insurer stated that after receiving the grievance in December 2018, their Regional
Office has also taken up the matter and the pending issue for policy migration into GC Core has been expedited by
them and when the same is being done by Regional Office, they had refunded the amount on insured’s request and as
per Bhavishya Arogya Policy Manual after getting payment approval from their Divisional Office Gwalior on
27.03.2019 amounting Rs.10,300/-
xiv. Regarding Complaint Point No.4 the insurer stated that they have made the refund only as per the request from the
insured and according to the terms and conditions of the policy but not in any haste or arbitrary manner.
xv. Regarding Complaint Point No.5 the insurer stated that the fresh grievance raised by complainant via mail dated
07.04.2019 and 22.04.2019 was not reported to their branch till the time of writing this note.
xvi. Regarding Complaint Point No.6 the insurer stated that although all the peculiarities of the policies were explained to
the insured before the starting of their contract. They admitted that they have not send any reminders regarding policy
maturity to the insured because the policy was of their old software “Genisys”, such facilities back then were not
incorporated in their systems. Presently through their new software “GC Core”, this facility has been enabled by them.
At the time of commencement of both policies, insured had chosen the date of surrender of both these policies as
11.09.2017, i.e. 58 years of her age. The Insurer had received her Policy surrender letter dated 10.04.2018 on
19.04.2018 which is after the selected surrender date and since the refund request has come after commencement of
risk accordingly refund has been made to her as per her request and terms and conditions of the policy and as per
their table – “No Claim refund after commencement of risk”.
The Insurer understood that the insured spouse might have got some different refund from the Oriental Insurance
Policy which he has referred, but this could be because of his request for surrender of policy before the risk
commencement. In the case of United India, if she placed the request for surrendering the policy before the risk
commencement (in that case before 11.09.2017) she will be entitled for a higher refund.
19) Reason for Registration of Complaint: - Less payment at the time of maturity of Bhavishya Arogya Policy
20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN

21)Observations and Conclusion :-
Both the parties appeared for personal hearing and reiterated their submissions. Sh. Subhash Singhal, husband of
the insured Ms. Anita Singhal, reiterated that he had taken two policies bearing nos. 190801/48/05/24/00002473 and
190801/48/06/24/00001129 for Sum Insured of Rs.90,000/- each and premium being Rs.5,693/- and Rs.5,798/- on
25.02.2006 and 24.02.2007 respectively. On maturity, Rs.10,300/- were refunded by the respondent company on
28.03.2019 which is almost the same amount which was deposited 11-12 years back. The Respondent Company
contended that the payment has been made as per the rules.
I have gone through the documents submitted by both the parties and observe from the circular of the Bhavishya
Arogya Policy submitted by the Insurer that at point no.1.7, it is mentioned that the basic policy is of Rs.50,000/-
and benefits can be increased in the unit of Rs.10,000/- by paying additional premium. It is noticed that the
complainant has purchased both the policies for sum insured of Rs. 90,000/- each and had paid the additional
premium. However the maturity payment has been erroneously calculated as per the basic policies having sum
insured of Rs.50,000/-, and benefits have not been proportionately increased to the applicable sum insured for which
enhanced premium had been charged. This is grossly unfair on the part of the insurer.
Apropos the issue of maturity amount it is observed that the complainant chose the date of maturity to be the date of
attainment of 58 years of age i.e. 24.07.2017. The application for surrender was sent on 10.04.2018 i.e. after the
date of maturity. It is observed that the maturity payment has been correctly made as intended by the complainant.
The Insurance Company is directed to pay the difference amount by revising the calculation of maturity amount as
discussed above.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 26.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. AKHIL KUMAR BANSAL V/S UNITED INDIA INSURANCE COMPANY LTD.
COMPLAIN REF. NO.: NOI-H-051-1920-0144
1.
Name & Address of the Complainant
Sh. Akhil Kumar Bansal
S/O Ms. Sudha Gupta, A-390,
Sector – 19, Noida,
Uttar Pradesh-201301.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Sum Insured
0426002818P115339722
Super Top Up Medicare Policy
28.02.2019 to 27.02.2020
Rs.3,00,000/-
3.
Name of the Insured
Name of the policyholder
Ms. Sudha Gupta, Mother of complainant
Sh. Akhil Kumar Bansal
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of Repudiation
--
6.
Reason for repudiation
--
7.
Date of receipt of the Complaint
19.08.2019
8.
Nature of complaint
Partial repudiation of claimed amount
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.72,263/- as per Annex VI A
12.
Complaint registered under
IOB rules, 2017
13 (1)(b)
13.
Date of hearing/place
11.12.2019 / NOIDA
14.
Representation at the hearing
c) For the Complainant
Sh. Akhil Kumar Bansal
d) For the insurer
Ms. Rajni Ahuja, Dy. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
26.12.2019
17. Brief Facts of the Case:- Sh. Akhil Kumar Bansal, the Complainant had taken Super Top Up Medicare Policy
No.0426002818P115339722 for the period from 28.02.2019 to 27.02.2020 for the S.I. of Rs.3,00,000/-
alongwith Individual Health Policy bearing No.0426002818P115338881 for the period from 28.02.2019 to
27.02.2020 for the S.I. of Rs.3,00,000/- . The Complainant’s mother was admitted in the hospital with complaint
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both the parties
during the course of hearing, the Insurance Company is directed to pay the difference amount by revising
the calculation for maturity amount.
The complaint is treated as disposed off accordingly.

of choking in trachea. The reimbursement of bills was partially rejected by the Insurance Company. Aggrieved,
he requested the insurer including its GRO to reconsider the claim but failed to get any relief. Thereafter, he has
preferred a complaint to this office for resolution of his grievance.
18. Cause of Complaint:-
a) Complainant’s argument:- Sh. Akhil Kumar Bansal, the Complainant stated that he has lodged claim with the
Insurer. The Insurance Company has partially settled his claim and deducted the amount of Rs.74,227/- due to
the sum insured in basic policy was exhausted. Despite the fact that he had taken Super Top Up Medicare
Policy for the last 6+ years bearing No. 0426002818P115339722 for the same period and the S.I. was of
Rs.3,00,000/-, the amount of Rs.74,227/- was deducted by the Insurer.
b) Insurers’ argument:- The Insurer in their SCN stated that the complainant’s mother Ms. Sudha Gupta, Age 85
years, covered under Policy No.0426002818P115338881 applied for cashless request from Kailash Hospital,
Noida on 15.04.2019.
Insured was admitted on 14.04.2019 in emergency with complaint of choking in trachea and was unconscious.
Patient was incubated and kept on ventilator.
Patient was diagnosed as a case of DM with HTN and Aspiration Pneumonitis.
Patient was discharged on 23.04.2019 and final bill of Rs.3,74,227/- was sent to TPA and TPA approved whole
sum insured of the policy of Rs.3 Lakhs and balance Rs.74,227/- could not be approved as sum insured in basic
the policy was exhausted.
Insured Party submitted a claim of Rs.1,14,984/- for reimbursement in Super top up policy no.
0426002818P115339722.
This claim amount includes Rs.74,227/- amount not paid in basic policy as S.I. exhausted and Rs.26,854/- a
hospitalization bill of DOA 23.04.2019 and 24.04.2019.
Rs.42,721/- was only paid to the claimant and deducted 72,263/-, details are here under :
Rs.26,854/-, the hospitalization bill of 2
nd
hospitalization was deducted as insured was hospitalized for
less than 24 hours in this hospitalization.
Rs.8,000/- was deducted Ambulance Charges.
Rs.31,556/- was deducted as non-payable items as per policy clause 4.13, 4.14 and 4.15.
19) Reason for Registration of Complaint: - Partial Rejection of Mediclaim
20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN
22) Observations and Conclusion :-
Both the parties attended the hearing and reiterated their written submissions. The complainant further added that
the complaint has arisen on account of deductions made towards reimbursements of the medical claim in respect of
hospitalization of his mother from 14.04.2019 to 24.04.2019. The Insurer has rejected the second hospitalization bill
amounting to Rs.26,854/- by treating it as hospitalization for less than 24 hours. The complainant stated that on 23
rd
April 2019, the hospital conveyed to discharge the patient on the same day but it took long hours to get the actual
discharge. As a result, it was too late in the night to shift the patient who was under critical condition in ICU to
Modi Nagar which is around 50 KM from NOIDA. Even the doctors advised against it, and so the patient continued
in the ICU and the actual discharge was done on 24
th
April 2019 in the early hours. Thus, the hospitalization was in
continuation, but due to some clerical convenience, the hospital has treated it as second hospitalization. Regarding
other deductions, the complainant said that the list of other deductions also have not been provided to him.
On the basis of the documents and the submissions made during the hearing by both the parties, it is absolutely clear
that the insured was continuously under hospitalization from 14.04.2019 to 24.04.2019 and the deductions made by
treating hospitalization from 23
rd
to 24
th
April 2019 as second hospitalization are absolutely unnecessary, unilateral
and unjustified. The Insurance Company is directed to review the claim assessment by treating hospitalization from
14.04.2019 to 24.04.2019 as a single hospitalization and pay the difference. Also, the Insurer is directed to provide
the list of deductions to the complainant after reassessment of the claim.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by both the parties during the course of hearing, the Insurance Company is directed to
review the claim assessment by treating hospitalization from 14.04.2019 to 24.04.2019 as a single
hospitalization and pay the difference. Also, the Insurer is directed to provide the list of
deductions to the complainant after reassessment of the claim.
The complaint is treated as disposed off accordingly.

a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 26.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MRS. MUDITA DAYAL V/S UNIVERSAL SOMPO GENERAL INS. CO. LTD.
COMPLAINT REF: NO: NOI-G-052-1920-0094
AWARD NO:
1.
Name & Address of the Complainant
Mrs. Mudita Dayal
CI-18, Suryodaya Vihar, Ansal Colony, Shastri
Nagar, Meerut, UP-250094
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2827/58288885/00/000
Allahabad Bank Health Care Plus Insurance
26.03.2019 to 25.03.2020
3.
Name of the insured
Name of the policyholder
Late Shri Rajeshwar Dayal
Mrs. Mudita Dayal
4.
Name of the insurer
Universal Sompo General Insurance Co. Ltd.
5.
Date of Repudiation
30.01.2019
6.
Reason for repudiation
Mis-representation, non disclosure of material fact
– Diabetes as PED
7.
Date of receipt of the Complaint
12.06.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.7,05,563/-
10.
Date of Partial Settlement
Nil
11.
Amount of relief sought
Rs.7,05,563/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
28.11.2019 at Noida
14.
Representation at the hearing
a) For the Complainant
Mrs. Mudita Dayal, Self
b) For the insurer
Mr. Shailendra Kumar, Assistant Manager
15
Complaint how disposed
Award
16
Date of Award/Order
11.12.2019
17) Brief Facts of the Case: This complaint is filed by Mrs. Mudita Dayal against Universal Sompo General
Insurance Company Ltd. for repudiation of hospitalization claim of his husband, Late Shri Rajeshwar Dayal.
18. Cause of Complaint:
a) Complainant’s argument: The complainant had ported mediclaim policy, covering herself and family members,
from New India Assurance Co. to Universal Sompo, after a continuous coverage from 26.3.2005 to 25.03.2018
(without break for 13 years). The policy was issued by Universal Sompo for the period from 26.03.2018 to
25.03.2019 for a sum insured of Rs. 5 lacs. She intimated an accidental claim of his husband but the TPA of
insurance company denied cashless facility. She submitted claim form for reimbursement but the insurance company
rejected the claim on the ground of first year exclusion of disease, as the same was not covered. Her husband could
not survive and she was suffering due to financial problems. She requested this Forum for reimbursing an amount of
Rs. 7,05,563/- towards medical expenses paid in hospital.
b) Insurers’ argument : The insurance company submitted their SCN on 11.09.2019 wherein they stated that the
complainant had taken Allahabad Bank Health Care Plus Insurance policy for herself, her spouse and two children.
She renewed this policy through portability. She filed a claim for medical expenses amounting to Rs.7,05,563/-. The
claim papers were scrutinized and it was found that her husband, Late Shri Rajeshwar Dayal, was a known case of
diabetes mellitus, hypertension and chronic kidney disease. They took medical opinion of Dr. Ahmad Ansari,
Consultant Family Physician and Insurance Claims Consultant, who opined that hypertension was a strong predictor
of cerebral stroke. The claim was repudiated vide letter dated 30.01.2019 mentioning that the patient was admitted
in BLK Hospital with diagnose of Acute Stroke and was diagnosed with Diabetes mellitus for 20 years,
hypertension for 10 years. The same were not disclosed by the complainant at the time of policy inception, hence the
claim was repudiated. The claim was closed due to mis-representation, mis-description or non-disclosure of any
material facts. Non-disclosure shall include non-intimation of any circumstances which may affect the insurance
cover granted.
19) Reason for Registration of Complaint: - Repudiation of Claim
20) The following documents were placed for perusal.
a) Complaint letter
b) Discharge Summary
c) Policy document
d) SCN

21) Observations and Conclusion: - Both the parties appeared for personal hearing on 28.11.2019 and reiterated
their submissions. The complainant stated that the insurance policy covering her husband and her was in
continuation since the year 2005 from New India. She ported this policy with Universal Sompo in 2018 through an
agent. Her husband was admitted in BLK Super Speciality Hospital for brain surgery but he could not survive. The
insurance company first rejected the cashless facility and then also rejected the reimbursement claim on the ground
of non disclosure of PED. The insurance company reiterated that the said policy was ported with their company with
enhanced sum insured, but the complainant did not disclose the PED at the time of porting the policy. They
repudiated the claim on the grounds of non disclosure of material facts. The insurance company produced proposal
form signed by the complainant where no PED was mentioned. The complainant stated that an agent from the
insurance company did the procedure of porting and she did not sign the form shown by the insurance company and
these signatures were not hers. Hence, the allegation of non disclosure of PED was not valid. During the hearing, the
insurance company was asked to obtain the signatures of complainant from the bank and submit the same to this
Office within a week.
The insurance company sent an email dated 7
th
December, 2019 stating that the bank authority denied sharing the
details of customers but they submitted some additional documents viz. copy of cancelled cheque of Late Shri
Rajeshwar Dayal, copy of Pan Card of Mrs. Mudita Dayal (having actual signature of her), copy of claim form
(which did not have signature of proposer Mrs.Mudita Dayal) and Copy of proposal form (Signature done by Late
Shri. Rajeshwar Dayal).
It is observed the insurance company repudiated the claim on the ground of non declaration of PED at the time of
porting the policy. The question is whether the complainant wilfully not disclosed the material fact at the time of
filling in the proposal form. From the documents, it is prime facie clear that the proposal form was not signed by the
complainant and the same was submitted by an agent by forging of the signature of the complainant. The insurance
company has failed to prove that the proposal form was signed by the complainant and she deliberately not disclosed
the PED of her husband, as her signature on the proposal form and on the claim form as well as on PAN card are
different. Obviously, the proposal form and portability forms were not signed by the complainant, hence, the charge
of non-disclosure of material fact cannot be attributed to her. From the available documents, it is also evident that
the policy was in continuation since the year 2005 i.e. 13 years, hence waiting period of 48 months for PED does not
apply in case of portability.
As per The Insurance Regulatory and Development Authority of India (Health Insurance) Regulations, 2016,
Chapter IV: Administration of Health Insurance Policies, Schedule-I : Portability of Health Insurance Policies
offered by General Insurers and Health Insurers, it has been clearly mentioned in Clause 12 that “On receipt of the
data from the existing insurance company, the new insurance company may underwrite the proposal and convey
its decision to the policyholder in accordance with the Regulation 4 (6) of the IRDA (Protection of Policyholders’
interest) Regulations, 2002.” While fetching the data of the complainant from his previous insurer, the insurance
company must have gone through the details of policy holder and only after satisfaction; they would have issued the
policy. The insurance company’s failure to obtain online data from the previous insurer is their own failure, and for
that the insured cannot be penalised.
The insurance company is directed to pay the claim as per the terms and conditions of the policy.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 11.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. RANJEET SINGH V/S UNIVERSAL SOMPO GENERAL INS. CO. LTD.
COMPLAINT REF: NO: NOI-G-052-1920-0111
1.
Name & Address of the Complainant
Mr. Ranjeet Singh
H.No. 73, VPO – DEHPA, Sambhal, Moradabad,
UP-244242.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2825/57129938/02/000
Complete Healthcare Policy
21.04.2019 to 20.04.2020
3.
Name of the insured
Name of the policyholder
Mr. Ranjeet Singh
Mr. Ranjeet Singh
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company is directed to pay the claim as per the terms and conditions
of the policy.
The complaint is closed.

4.
Name of the insurer
Universal Sompo General Insurance Co. Ltd.
5.
Date of Repudiation
23.05.2019
6.
Reason for repudiation
23.05.2019
7.
Date of receipt of the Complaint
28.06.2019
8.
Nature of complaint
Repudiation of Claim
9.
Amount of Claim
Rs.2,40,000/- (as per Annex VIA)
10.
Amount of Partial Settlement
n.a.
11.
Amount of relief sought
Rs.2,40,000/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27.12.2019 at Noida
14.
Representation at the hearing
a) For the Complainant
Mr. Ranjeet Singh, Self
b) For the insurer
Mr. Shailendra Kumar, AM
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of the Case: This complaint is filed by Mr. Ranjeet Singh against Universal Sompo General
Insurance Company Ltd. repudiation of cashless request for treatment.
18. Cause of Complaint:
a) Complainant’s argument: The complainant purchased health insurance policy in April, 2017 and later on
renewed it. The claim occurred under Policy No. 2825/57129938/02/000 for the period from 21.04.2019 to
20.04.2020. The complainant fell down from the roof of his house in the month of August, 2017, and internally
injured his lower back and hips. He took treatment from village doctor. Later on, as he was suffering from pain and
swelling at right hip, he was admitted in Apollo Hospital from 27.5.2019 to 31.5.2019 for total hip replacement. The
insurance company rejected his cashless approval on account of PED. He stated that he had any problem before
August, 2017.
b) Insurers’ argument: The insurance company submitted their SCN dated 20.08.2019 wherein they stated that the
complainant was hospitalized from 27.5.2019 to 31.05.2019 for Pain Swelling right hip. It was observed that he was
having PED AVN for which they issued endorsement in policy based upon the documents submitted by the
complainant. As per mentioned observation it was confirmed that the complainant was symptomatic at the time of
inception of policy which was not disclosed in the proposal form, hence, they rejected the claim as per policy’s Mis-
description clause.
19) Reason for Registration of Complaint: - Denial of cashless claim request.
20) The following documents were placed for perusal.
a) Complaint letter
b) Endorsement
c) Policy document
d) SCN
21) Observations and Conclusion: - Both the parties appeared for personal hearing on 27.12.2019 and reiterated
their submissions. The complainant stated that he took the policy for the first time in April, 2017. He fell down from
the roof of his house in August, 2017 and he took treatment from doctor of his village. He was suffering from pain
in hips so he consulted Dr. Niraj Garg on 22.9.2017 who suggested MRI. The MRI report suggested osteo-necrosis
(AVN) of both femoral heads (R>L). The complainant informed his medical status to the insurance company on
19.3.2018, at the time of renewal of policy. The insurance company renewed the policy for the period from 2018-
2019 without any endorsement. Again, when the policy was renewed for the year 2019-2020 they added condition
that expenses related to Osteonecrosis AVN, its related causes and complications, were not covered for a continuous
period of 36 months without any break in policy renewal w.e.f. March, 2018 (as per request received by us from
Insured for PED endorsement). The complainant stated that he informed his medical status in March, 2018 but when
he applied for cashless approval of his treatment for total hip replacement, it was denied by the insurance company
on 23.5.2019 giving reason for PED not covered for 36 months of continuous cover. But later on, they permanently
excluded this treatment from the scope of policy.
The insurance company stated that they received the information about the medical condition of the complainant in
March, 2019 and they added the condition of PED at the time of renewal of policy for the year 2019-20. Since, the
complainant was having PED of AVN, they excluded the treatment from the scope of policy. So the critical question
to determine is whether the insured informed about his condition in March, 2018 or in March, 2019 as contended by
the insurance company. It is clearly evident from complainant’s email dated 19.3.2018 to the insurance company
that he intimated his condition, and also submitted related medical papers to them, seeking advice as to whether it
would be covered by his policy. In fact, the insurance company advised vide their email dated 20.03.2018 to go
ahead with his treatment.
It is noted that the insured fell down from the height after inception of policy in the year August, 2017. He honestly
disclosed his disease to the insurance company in March, 2018, at the time of renewal of the policy. It is evident
from the insurance policy for the period 2018-19 that they did not endorse any special condition related to the PED
of the complainant and issued the policy. It is also evident from the policy issued for the period from 21-4-2019 to
20-04-2020 that the insurance company subsequently added special condition that Ranjeet Singh:All expenses
related to Osteonecrosis AVN its related causes and complications are not covered for a continuous period of 36
months without any break in policy renewal w.e.f. March, 2018 (as per request received to us from Insured for PED
endorsement). Then on 23.04.2019, the insurance company further issued an endorsement that stated that all
expenses related to Osteo-necrosis (AVN) of both femoral heads/Osteoporosis and its related causes and
complications are permanently excluded from policy coverage since policy inception.
The complainant was planning to go for treatment on 27.5.2019 in Apollo Hospital. The hospital submitted cashless
request on 23.5.2019 to the insurance company. The insurance company vide their letter dated 23.5.2019 rejected
cashless approval of the treatment on the ground of waiting period of 36 months. The complainant could not and has

not taken treatment due to his financial conditions till date. The changing position of the insurance company despite
being intimated by the insured shows their malafide intention. When the complainant planned for the treatment, they
first issued special condition for waiting period, and again they permanently excluded the treatment. The
complainant has not yet taken the treatment. The insurance company is directed to stick to their condition for the
waiting period of 36 months from the inception of policy and delete the endorsement for permanently exclusion of
Osteo-necrosis (AVN) of both femoral heads/Osteoporosis and its related causes and complications.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S.PRASAD
CASE OF BHARAT BHUSHAN KAPOOR V/S LIFE INSURANCE CORPORATION OF INDIA
COMPLAINT REF: NO: NOI-L-029-1920-0315
AWARD NO:
1.
Name & Address of the Complainant
Sh. Bharat Bhushan Goel
105, Gandhi nagar, Gali no.3,Sardhana,
Meerut , Uttarpradesh-250342
2.
Policy No:
Type of Policy
Duration of policy/Policy period
256757939 257671860
Health Plan Health Plan
Plan903 Plan 904
3.
Name of the insured
Name of the policyholder
Sh. B.B.Goel Sh. B.B. Goel
Sh. B.B. Goel Mrs. Priyanka Gupta
4.
Name of the insurer
Life Insurance corporation of India
5.
Date of Repudiation
9.11.2018 9.11.2018
6.
Reason for repudiation
Pre –Existing Disease
7.
Date of receipt of the Complaint
2.8.2019
8.
Nature of complaint
Rejection of Medi Claim under Jeevan Arogya
Policy
9.
Amount of Claim
Rs.
10.
Date of Partial Settlement
NIL
11.
Amount of relief sought
Rs.
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
13.12.2019 at Noida
14.
Representation at the hearing
eee) For the Complainant
Sh. Bharat Bhushan Goel, Self
fff) For the insurer
Sh. Naresh Piplani, AAO
15
Complaint how disposed
Award
16
Date of Award/Order
17.12.2019
17)Brief Facts of case;-This complaint is filed by Sh. Bharat Bhushan Goel against the decision of LIC of India
relating to rejection of health claim under policy no’s 256757939 and 25671860 issued on his life.
18)Cause of Complaint:- Rejection of Health Claim under policy.
Complainants argument :- The complainant stated that he had taken a Jeevan Arogya plan-903 from LIC of
India on 10.9.2012. The complainant is the insured member in the other policy no. 257671860 issued on the
life of his daughter inlaw , Priyanka Gupta under Plan-904 with date of commencement of policy on
28.10.2014.The complainant was admitted to Max Hospital , Saket , New Delhi on 9.7.2018 for Supraumblical
Hernia. On 10.7.2018 the complainant was operated for Laproscopic Intraperitoneal Onlay Mesh Repair. And
was discharged from hospital on 11.7.2018. The complainant had submitted all the required claim form s to the
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties, the insurance company is directed to stay on their condition for the waiting
period of 36 months from the inception and delete the endorsement for permanently
exclusion of Osteo-necrosis (AVN) of both femoral heads/Osteoporosis and its related
causes and complications.
The complaint is closed accordingly.

insurer for settlement of death claim. The insurer had rejected payment on the ground of pre-existing disease
vide letter dated 9.11.2018
Insurers’ argument:- The insurer stated that The policy no. 256757939 was issued on the life of complainant
on 10.9.2012 under Jeevan Arogya Plan-903. The other policy no. 257671860 was issued on 28.10.2014 under
Jeevan Arogya Plan 904. The complainant was admitted to Max Super Specialty Hospital on 9.7.2018 and was
discharged on 11.7.2018. During hospitalization, Epigastric Hernia Surgery was done. The insurer had
repudiated the claim payment on the basis of Pre-Existing disease as shown in Discharge Summary of Max
Hospital as per Exclusion 7 (i) of policy terms and conditions.
19) Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN
21)Observations and Conclusion:- Personal hearing in the case was held on 13.12.2019. Both the complainant and
insurer attended the hearing and reiterated their submissions. The insurer stated that the discharge summary of Max
Hospital shows history of open Epigastric Hernia repair in 1988, which the complainant did not disclose at the time
of inception of policy. I see that the complainant had Hernia repair 30 years before inception of policy and perhaps
forgot to mention it since it did not give any trouble. Moreover the policy was taken on the life of complainant on
10.9.2012 and as per policy terms and conditions ‘Specific Waiting Period of 2 years have also been completed
under the policy. Hence insurer’s decision of repudiation of health claim payment on the basis of pre-existing
disease in not justified and set aside.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 17.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S.PRASAD
CASE OF V/S LIFE INSURANCE CORPORATION OF INDIA
COMPLAINT REF: NO: NOI-L-029-1920-0190
1.
Name & Address of the Complainant
Sh. Vinod Kumar Agarwal
552, Civil Lines North, Saket Road
Muzaffarnagar, Uttar Pradesh
Pin- 251001
2.
Policy No:
Type of Policy
Duration of policy/Policy period
273391372 273595419
Health plan Health plan
3.
Name of the insured
Name of the policyholder
Vinod Kumar Vinod Kumar
Vinod kumar Vinod kumar
4.
Name of the insurer
Life Insurance Corporation of India
5.
Date of Repudiation
15.06.2019
6.
Reason for repudiation
Exclusion as per policy conditions
7.
Date of receipt of the Complaint
12.6.2019
8.
Nature of complaint
Rejection of Medi claim
9.
Amount of Claim
Rs.
10.
Date of Partial Settlement
None
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by both the parties during the course of hearing, the insurer is directed to make
payment of health claim under the policy.
The complaint is disposed off accordingly.

11.
Amount of relief sought
Rs.
12.
Complaint registered under
IOB rules
13 (1) ( b )
13.
Date of hearing/place
On 14.11.2019 and 13.12.2019 at Noida
14.
Representation at the hearing
a) For the Complainant
Absent on both days
b) For the insurer
Sh. I.S. dugtal, Manager (HI)
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17)Brief Facts of case:- This complaint is filed by Sh. Vinod Kumar Agarwal against Life Insurance Corporation of
India relating to rejection of medi claim under policy issued on his own life.
18)Cause of Complaint:- Rejection of Health Claim of policy
a) Complainants argument :- The complainant stated that he had taken 2 health policies bearing no’s 273391372
and 273595419 from Life Insurance Corporation of India on 25.7.2011 and 28.7.2013 respectively. The
complainant was admitted to Heart Clinic & Emergency Care Centre, Multispeciality Hospital Muzaffarnagar, in
ICU due to Acute Respiratory Syndrome on 7.7.2018 and was discharged from Hospital on 13.07.2018 . The
complainant was again admitted to Sir Ganga Ram Hospital, Rajender Nagar, Delhi on 13.7.2018 and was
diagnosed of Large Ostium Secundum ASD, Severe Pulmonary Arterial Hypertension, Chronic Obstructive
pulmonary Disease, Obstructive Sleep Aponea, Obesity and was discharged from the hospital on 23.07.2018.The
complainant had submitted all the relevant claim forms to the insurer for payment of claim . The insurer rejected
claim payment vide their letter dated 14.1.2019.
b)Insurers’ argument:- The insurer stated that 2 policies named Jeevan Arogya bearing no. 273391372 and
273595419 were issued on the life of Sh. Vinod kumar Agarwal on 25.7.2011 and 28.7.2013 respectively. The
complainant was admitted to Heart Clinic & Emergency Care Centre, Multispeciality Hospital Muzaffarnagar, in
ICU due to Acute Respiratory Syndrome on 7.7.2018 and was discharged from Hospital on 13.07.2018 . The
complainant was again admitted to Sir Ganga Ram Hospital, Rajender Nagar, Delhi on 13.7.2018 and was
diagnosed of Large Ostium Secundum ASD, Severe Pulmonary Arterial Hypertension, Chronic Obstructive
pulmonary Disease, Obstructive Sleep Aponea, Obesity and was discharged from the hospital on 23.07.2018. The
complainant had submitted claim form on 26.9.2018.The claim payment had been rejected as per policy conditions
7 (x) exclusions which states that the treatment taken by the insured is under the category of convalescence, general
debility, nervous or other breakdown , rest cure, congenital diseases or defect or anomaly, sterilization or infertility (
diagnosis and treatment), any sanatorium, spa or rest cure or long term care or hospitalization under taken as a
preventive or recuperative measure. Hence claim payment rejected vide letter dated 14.1.2019.
19) Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN
21)Observations and Conclusion;- ):- Personal hearing of the case was held on14.11.2019 and on 13.12.2019. The
complainant was absent on both days . The insurer attended the hearing on both days. The complainant has sent a
letter dated 03.12.2019, stating his inability to attend the hearing and stated that he had paid premium for 5 years
under both policies. During this period of 5 years, he was not suffering from any disease. He had nothing to add
apart from his written complaint. The insurer submitted that the treatment taken by the complainant is for congenital
diseases/defect/anomaly i.e Large Ostium Secundan Atrial Septal defect , which is a type of congenital heart
defect. Hence, claim is not payable as per policy exclusions 7 (x) of policy terms and conditions. In view of above ,I
see no reason to interfere with the decision of insurance company.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by the insurer during the hearing, the complaint is dismissed.
The complaint is disposed off accordingly.

PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SH. C.S.PRASAD
CASE OF SH.VIMAL KISHORE V/S LIFE INSURANCE CORPORATION OF iNDIA
COMPLAINT REF: NO: NOI-L-029-1920-0277
1.
Name & Address of the Complainant
Sh. Vimal Kishor
S/O Darshan Lal,
Shyam Lal Bagicha
Padampur Sukhro, Pauri Garhwal
Kotdwara, Uttarakhand-246149
2.
Policy No:
Type of Policy
Duration of policy/Policy period
274421902
Health Plan
41 years
3.
Name of the insured
Name of the policyholder
Sh. Vimal Kishore
Sh. Vimal Kishore
4.
Name of the insurer
LIC of India
5.
Date of Repudiation
17.1.2019
6.
Reason for repudiation
Pre-Existing Disease
7.
Date of receipt of the Complaint
15.7.2019
8.
Nature of complaint
Rejection of health claim payment
9.
Amount of Claim
10.
Date of Partial Settlement
NIL
11.
Amount of relief sought
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
13.12.2019 at Noida
14.
Representation at the hearing
a) For the Complainant
Absent
b) For the insurer
Sh. I.S. Dugtal, Manager( HI)
15
Complaint how disposed
Award
16
Date of Award/Order
31.12.2019
17) Brief Facts of case;- This complaint is filed by Sh. Vimal Kishore relating to Non-Settlement of Health Claim
under policy issued on his life.
18) Cause of Complaint:- Non-Settlement of Health Claim of the Policy.
a) Complainants argument :- The complainant stated that he had taken a Jeevan Arogya policy from LIC of India
on 28.10.2016. The complainant was admitted to Medanta Hospital, Gurgaon on 25.8.2017 for surgery related to
Coronary Artery Disease. He was discharged from hospital on 28.8.2017.The complainant had submitted claim
forms to the insurer on 1.11.2018 for payment of claim. The insurer rejected the claim vide their letter dated
17.1.2019 on the ground of Pre-existing disease.
b)Insurers’ argument:- The insurer stated that a policy named “Jeevan Arogya bearing no. 274421902 was issued
on the life of Sh. Vimal Kishore on 28.10.2016. As per discharge summary of Medanta hospital , the complainant
was suffering from Coronary Artery Disease for last 1 year. The complainant was admitted to Medanta Hospital,
Gurgaon on 25.8.2017 and surgery was performed for Coronary Angioplasty with stent implantation. The
complainant was discharged from hospital on 28.8.2017. The claim forms were submitted by the complainant on
1.11.2018. It was found from the proposal form that the Principal Insured had replied in negative to all questions
related to his health at the time of proposal and had suppressed the details pertaining to the pre-existing disease.
The principal Insured was suffering from DYSPNEA on exertion for 1 year. Thus as per terms and policy
conditions at point 7(i)Exclusion, No Benefits are available and no payment will be made by the insurer to any claim
on account of surgery arising out of “Any pre-existing disease/ condition, ailment or injury or related conditions for
which you had signs or symptoms, and were diagnosed or received medical advice/ treatment with in 48 months
prior to the date of commencement of policy”. Hence the above said claim was repudiated and same was
communicated to the complainant vide letter dated 17.1.2019.
19) Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint Letter
b) Repudiation Letter
c) Policy Document
d) SCN
21) Observations and Conclusion):- Personal hearing of the case was held on13.12.2019. The complainant was
absent on the date of hearing. The insurer attended the hearing. The insurer submitted that the assured was suffering
from Dyspnea for last 1 year i.e. prior to the inception of policy. The complainant had suppressed the details
pertaining to the pre-existing disease. The insurer has not submitted any other proof to support their allegation of
pre-existing disease except discharge summary.
It is observed that the complainant was diagnosed with CAD/ DVD after Angiography on 22.8.2017, he was
admitted in the hospital on 25.8.2017.This has nothing to do with Dyspnea. Further, there is no evidence of any
mensrea on the part of the insured. Therefore, it is unfair to say that he deliberately concealed the information about
his having Dyspnea. Hence, the insurer is directed to make payment of claim under the policy.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by the
insurer during the course of hearing, the insurer is directed to make payment of health claim
under the policy.
The complaint is disposed off accordingly.

22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award within
thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 31.12.2019 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Rajesh Pathak ………………..……....………………. Complainant
V/S
L.I.C.OF INDIA …………………………………….………...Respondent
COMPLAINT NO: LCK-L-029-1718-0862 Order No. IO/LCK/A/LI/ 0142/2019-20
1.
Name & Address of the Complainant
Mr. Rajesh Pathak
E-20, Shiv Nagar Colony
Chandpur
Dist-VARANASI
Uttar Pradesh-221106
2.
Policy No:
Type of Policy
DOC/ DOR
Duration
287393025
Health Insurance Plan
24.06.2011/ 08.08.2012
3.
Name of the insured
Name of the policyholder
Mrs. Reeta Pathak
Mrs. Reeta Pathak
4.
Name of the insurer
L.I.C.OF INDIA
5.
Date of Repudiation/Rejection
31.08.2017
6.
Reason for repudiation/Rejection
N/A
7.
Date of receipt of the Complaint
13.03.2017
8.
Nature of complaint
Pre-existing illness
9.
Amount of Claim
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Full Claim Amount
12.
Complaint registered under Rule
Rule No.13(1)(b)of Insurance Ombudsman
Rule 2017
13.
Date of hearing/place
06.12.2019 at 10.15A.M.
14.
Representation at the hearing
a) For the Complainant
Mr. Rajesh Pathak
b) For the insurer
Mr. Rajendra Prasad
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
06.12.2019
17. Mr. Rajesh Pathak (Complainant) has filed a complaint against L.I.C.OF INDIA.
(Respondent) alleging that claim under Health Insurance policy has been rejected.
Brief Facts of the Case: -
18. As per complaint, the complainant has stated that policy no.287393025 was issued under
Health Insurance Policy on the life of his wife Smt. Reeta Pathak on 24.06.2011 for sum
assured Rs. 100000/- .Policy became lapse due to non-payment of premium in time. Policy was
revived on 08.08.2012. His wife became ill and hospitalized on03.02.2017 at 1.00PM and
discharged on 05.02.2017 at 6.30PM. The date of Surgery was 04.02.2017.The disease
diagnosed was Cholecystis with Right Ovarian Cyst with Type 2 Diabetes Mellitus since 7
months Hypothyroidism since 2 years. Hence her claim was rejected on the ground Pre-existing
illness irrespective of prior medical treatment or advice.
19. According to claimant, Pre-existing disease clause exist for 48 months and LIC was made
known about the disease on 08.08.2012 i.e. day of revival and accepted it and now claim is

being rejected for hospitalization for a period of 03.02.2017 to 05.02.2017.Hence it is total
injustice.
20. Being aggrieved, the complainant approached this forum for the redressal of his grievance.
Written reply/SCN:-
21. In SCN/reply dated 30.11.2019, respondent has submitted that the policy no.287393025
was issued under Health Insurance plan. Claim for hospitalization period from 06.12.2014 to
23.12.2014 and 01.01.2015 to 06.01.2015 was submitted by the policyholder and was rejected
on the basis of PED (Pre-Existing Disease) and recommendation of TPA.
22. It is also stated that repudiation action through module could not be taken timely,
consequent upon which status of the policy could not be changed and further due premium up
to 06/2018 could be deposited by the policyholder under aforesaid policy. In between one more
claim for hospitalization period 03.02.2017 to 05.02.2017 was submitted by the policyholder on
18.08.2017 and was also repudiated on the basis of previous repudiation.
23. It is further stated that policyholder had deposited the premium knowingly with a motive to
receive the claim amount.
24. The complainant has filed a complaint letter annexure VI A, and correspondence with
respondent while respondent has filed SCN with enclosures.
25. I have heard both the parties at length and perused paper filed on behalf of the
complainant as well as the Insurance Company. Mr. Yogesh Kumar Srivastava was also present
during hearing.
Findings:-
26. Complainant filed the claim for the treatment for his wife which under took from 03-02.2017
from 05.02.2017. Admittedly the policy was issued from 24.06.2011 but the next premium was
made on 08.08.2012. Hence policy was lapsed and revival was done on 08.08.2012. Claim was
made by the claimant for hospitalization from his wife from 06.12.2014 to 23.12.2014 and
01.01.2015 to 06.01.2015 which were repudiated on the ground of pre existing disease in the
discharge summary. Present claim is also repudiated on the ground of previous repudiation. At
the very outset it would be relevant to mention that neither revival proposal nor DGH is filed by
the respondent. It is also pertinent to note that the complainant is still making the payment of
premium. It means that policy has yet not been cancelled. Repudiation order is passed on the
basis of previous repudiation but the present hospitalization relates to the period from
03.02.2017 to 05.02.2017. DGH is not filed hence it could be accepted that it has been
repudiated merely on the basis of previous repudiation. Hence the repudiation order suffers
from material irregularities and liable to be quashed.
Order:-
27. Complaint is allowed. Repudiation order is quashed. Respondent are directed to reopen the
claim of the claimant and decide the same within a period of 30 days after affording opportunity
of hearing to the claimant. If after the claim is decided by the respondent claimant has any
grievance he would be at liberty to took legal remedy in accordance with rules.
28. Let the copies of this award be sent to both the parties.
Date: 06.12.2019 (Justice Anil Kumar Srivastava)
Place: Lucknow Insurance Ombudsman

PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Lallan Ram Maurya…………..……....………………. Complainant
V/S
Max Bupa Health Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-031-1718-0148 Order No. IO/LCK/A/GI/0080/2019-20
1.
Name & Address of the Complainant
Mr. Lallan Ram Maurya,
S-20/51, 1A, Varuna Bridge,
The Mall Road, Cantt,
Varanasi - 221002
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
30395162201601 , 30391364201702
Health Companion Health Insurance Plan
31.01.16 to 30.01.17 & 31.01.17 to 30.01.18
3.
Name of the life insured
Name of the policyholder
Mr. Lallan Ram Maurya
Mr. Lallan Ram Maurya
4.
Name of the insurer
Max Bupa Health Insurance Company Limited
5.
Date of Repudiation/Rejection
07.06.2017 and 04.10.2017
6.
Reason for repudiation/Rejection
Repudiation as per Policy Clause Nos: 4E(xi) and non
disclosure of previous medical history
7.
Date of receipt of the Complaint
25.09.2017
8.
Nature of complaint
Repudiation of claims
9.
Amount of Claim
Rs.342058.00
10.
Date of Partial Settlement
---
11.
Amount of relief sought
---
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 02.12.2019 at 11.00 am at Lucknow
14.
Representation at the hearing
ggg) For the Complainant
Absent
hhh) For the insurer
Mr. Digvijay Singh
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
02.12.2019
17. Mr. Lallan Ram Maurya (Complainant) has filed a complaint against Max Bupa Health Insurance
Company Limited (Respondent) alleging repudiation of his two health claims.
18. Brief Facts Of the Case:- The complainant has stated that he had taken the policy from RIC and it
is running from 31.01.2015. During the policy period, he had taken treatment for eyes and stomach
and two bills of approx Rs. 35,000/- were submitted for settlement. But the claims were rejected on
the ground of non disclosure of previous medical history of CAD. He further stated that he already
disclosed his previous history and even respondent had conducted medical examination by their
empanelled doctors and policy was issued after he was found to be in sound health. Aggrieved with the
decision of the RIC, he had made a grievance to this forum.
In their SCN/reply, RIC has stated that on the basis of information given by the insured in the proposal
form, RIC has issued the said policy to the insured effective from 31.01.2015 to 30.01.2016 and the
said policy was renewed from time to time. The complainant has submitted two claims asking for
reimbursement of medical expenses and the same was denied by the RIC. It is submitted that the first
claim for treatment of Eye Sight Correction was denied on the grounds of 4e(xi) of the policy terms
and conditions which clearly states that eye sight correction procedures are specifically excluded from
the policy. 2
nd
claim of the insured for the treatment of Acute Gastroenteritis WI, it was observed by
the RIC that the claim fell outside the purview of the policy as the patient/insured had history of CAD
since 1993 and the same was not disclosed to the RIC at the time of proposal. Hence, RIC has
repudiated the claim due to non disclosure of material fact. The respondent has communicated the
decision of both the claims to the insured on 07.06.2017 and 04.10.2017 respectively.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures.
20. During hearing complainant remained absent. I have heard the representative of respondent at
length and perused paper filed on behalf of the complainant as well as the Insurance Company.
21. This is a third hearing in this matter. Notices for hearing were sent to the complainant through
speed post which were duly delivered on 21.10.2019.
There are two claims of the complainant. One for Rs.9000/- for treatment of Eye Sight Correction. This
claim was made on 28.01.2017 which is within two years of waiting period as per Condition No:4e(xi)

of the policy bond. The policy was taken on 31.01.2016 to 30.01.2017. Operation was done on
28.01.2017. The claim was rightly repudiated on the ground that it is made within two years of waiting
period which is against the Clause No: 4e(xi) of the policy bond.
2
nd
claim for Rs.32058/- is for Acutue Gastroentitis. Ground of repudiation is non disclosure of CAD in
the proposal form and this fact is admitted by the complainant himself that he was an old patient of
CAD. Although according to the complainant he disclosed this fact to the concerned agent but in the
proposal form, this fact has been concealed. Accordingly the claim is rightly repudiated by the
respondent insurance company.
Accordingly complaint lacks merit and liable to be dismissed.
22. Complaint filed by Mr. Lallan Ram Maurya stands dismissed
23. Let copy of award be given to both the parties.
Dated : December 2, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Vidhu Chauhan…………..……....………………. Complainant
V/S
Max Bupa Health Insurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-031-1819-0008 ORDER NO. IO/LCK/A/GI/0090/2019-20
1.
Name & Address of the Complainant
Mr.Vidhu Chauhan,
199, Phool Bagh, Opp. Gayatri Jewellers,
Lucknow-226001
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
30651079201700
Health Policy
27.03.2017 to 26.03.2018
3.
Name of the life insured
Name of the policyholder
Mr. Rajendra Bahadur Singh & Mrs.Radha Singh
Mr. Vidhu Chauhan
4.
Name of the insurer
Max Bupa Health Insurance Co. Ltd.
5.
Date of Repudiation/Rejection
-
6.
Reason for repudiation/Rejection
-
7.
Date of receipt of the Complaint
12.04.2018
8.
Nature of complaint
Non settlement of claim
9.
Amount of Claim
Rs.210473/-
10.
Date of Partial Settlement
-
11.
Amount of relief sought
Rs. 210473/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 04.12.2019 at Lucknow
14.
Representation at the hearing
iii) For the Complainant
Absent
jjj) For the insurer
Absent
15.
Complaint how disposed
Dismissed as settled
16.
Date of Award/Order
04.12.2019
17. Mr. Vidhu Chauhan (Complainant) has filed a complaint against Max Bupa Health Insuance
Company Limited (Respondent) alleging repudiation of medi claim of his father Mr. Rajendra Bahadur
Singh.
18. Brief Facts Of the Case:- The complainant has stated that his father was hospitalized in Sahara Hospital,
Lucknow. He has submitted all relevant claim documents to RIC/TPA for settlement of medi-claim of his father
amounting to Rs.210473/- but his claim was not settled by the respondent company. He also lodged his grievance
with the respondent but no reply was received by him. Later on, his claim was repudiated by the RIC citing reason
as violation of policy conditions. Aggrieved with decision of the RIC, he has approached this forum.
In their SCN/Reply, RIC stated that the said policy was issued for Rs.5 lacs covering the complainant’s father and
mother. On perusal of the claim document, it was observed that his father was admitted in Charak hospital,
Lucknow from 21.10.2017 to 26.10.2017 for treatment of dorso- lumber spondylosis and insured submitted the bill
amounting to Rs.42912/-. The loss took place within seven months from the date of inception of the policy. The
reimbursement of claim was denied by the RIC on the ground that the event falls under two years specific waiting
period. (refer page 4 of SCN dt.28.06.2018).
Another claim was lodged by the complainant with the RIC for reimbursement of Rs. 1,67,561/- incurred for the
treatment of his father at Sahara Hospital, Lucknow during the period 26.10.2017 to 01.11.2017. The MRI report
dated 23.10.2017, which was received from the hospital at pre-auth stage mentioned that it is case of dorso-lumber

spondylosis. They had repudiated the claim under Exclusion No:3(c)[5] expenses related to spondylosis are not
admissible during the first 2 years from the date of policy in force and the same was conveyed to the complainant.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and copy of
policy document while respondent filed SCN with enclosures.
20. None appeared on behalf of the complainant and respondent. I perused paper filed on behalf of the
complainant as well as the insurance company.
21. Complainant as well as respondent insurance company are not present. I have gone through the mail dated
21.11.2019 of the respondent in which the respondent has reviewed the claim and offered Rs.42627/- and
Rs.162927/- to the complainant. The complainant vide his mail dated 01.12.2019 has accepted the offer of the
respondent.
In view of the above facts and circumstances, the complaint is amicably settled between the parties. Respondent is
hereby directed to make the payment within 15 days.
Accordingly, complaint is disposed off as settled.
22. Let copy of award be given to both the parties.
Dated : December 4, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Akhilesh Kumar Singh…………..……....………………. Complainant
V/S
Religare Health Insurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-037-1819-0128 ORDER NO. IO/LCK/A/GI/0113/2019-20
1.
Name & Address of the Complainant
Sri. Akhilesh Kumar Singh,
Khewali, Hathi Bazar,
Varanasi.
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
12144161
Religare Health Insurance
22.02.2018 to 21.02.2019
3.
Name of the life insured
Name of the policyholder
Sri. Akhilesh Kumar Singh,
Sri. Akhilesh Kunar Singh,
4.
Name of the insurer
Religare Health Insurance Co. Ltd.
5.
Date of Repudiation/Rejection
28.12.2018
6.
Reason for repudiation/Rejection
Non-receipt of necessary documents in accordance
with Policy terms & conditions.
7.
Date of receipt of the Complaint
20.11.2018
8.
Nature of complaint
Delay in settlement of claim
9.
Amount of Claim
Rs.67,055/-
10.
Date of Partial Settlement
---
11.
Amount of relief sought
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 27.12.2019 at Lucknow
14.
Representation at the hearing
kkk) For the Complainant
Absent
lll) For the insurer
Mr. Pratyush Prakash
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
27.12.2019
17. The Complainant, Sri Akhilesh Kr. Singh has filed a complaint against Religare Health Insurance
Company Limited (Respondent) alleging delay in settlement of his health claim.
18. Brief Facts Of the Case:- The complainant vide his trailing mail dated 09.10.2018 has stated that his
hospitalization claim has not been settled by the respondent. Even though, when he enquired with
respondent’s customer service team he was apprised that his claim was under process. On perusal of
trail mails it is revealed that the complainant was supplied with a QTD (query to Doctor) letter by the
respondents & was asked to co-ordinate with the treating Doctor to satisfy queries raised by them & to
submit a few documents necessary for processing the claims. However, the complainant replied that as

per hospital, all treatment related documents have already been provided to the respondents. Vide our
e-mail dated 05.11.2018 the complainant was asked to write his complete grievance & also the relief to
be sought by him from this forum but, the complainant did not submit his grievance in writing though
he had submitted form VIA on 01.07.2018 seeking reimbursement of his hospital claim.
In their SCN/Reply, RIC has stated that the documents submitted by the complainant were assessed in
the light of terms & conditions of the policy particularly 6.1 i.e. prerequisites for admissibility of a claim
& 6.3 i.e. duties of claimant / insured person in the event of claim. As they found certain discrepancies /
necessary medical omissions in the line of treatment of the complainant they sent a QTD dated
12.07.2018 seeking justification from the treating doctor which was followed by their subsequent
reminder dated 21.07.2018. But, the complainant failed to provide any reply hence, In absence of details
& specified information they could not ascertain & assess their liability and finally repudiated the claim
vide their letter dated 28.12.2018.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent
through e-mail and copy of policy document while respondent filed SCN with enclosures.
20. Despite notice to the complainant he is not present. Mr. Pratyush Prakash, Manager Legal
respondent is present. I heard the respondent representative and perused the record.
21. The complaint was initially registered as delay in claim settlement which was based on an e-mail
message from the complainant dated 03.11.2018 to the effect that his claim is pending for a long time
but the Insurance Company was not responding. It appears that the respondent asked for certain
information from treating doctor of the complainant as well as complainant. The query to doctor was
also sent by the respondent but the same was not replied. Consequently the claim of complainant was
repudiated vide letter date 28.12.2018 on following grounds:-
1. Query reply not received. Hence rejected.
2. Deficiencies not reply.
In the form VI A which was also received in this office on 01.07.2019, no details of the claim was made.
No grounds are mentioned on which claim is been preferred.
Initially the complaint was regarding delay in the settlement of claim. Claim was repudiated by the
respondents on 28.12.2018. Complainant has not sent any complaint separately or in-continuation of
the earlier complaint challenging the repudiation letter. Hence the complaint itself becomes
infructuous. Accordingly complaint is liable to be dismissed.
Order:-
22. Complaint is dismissed as infructuous. However, the complaint would be at liberty to challenge the
repudiation letter, if he so wishes, in accordance with rules.
23. Let copy of award be given to both the parties.
Dated : December 27, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman

PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr Nausad Ahmad…………..……....………………. Complainant
V/S
National Insurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-048-1718-0217 ORDER NO. IO/LCK/A/GI/0084/2019-20
1.
Name & Address of the Complainant
Mr. Naushad Ahmad,
130/80, L-1, Bagahi,
Post TP Nagar, Kanpur-208023
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
450401/48/16/8500000317
National Mediclaim Policy
13.12.2016 to 12.12.2017
3.
Name of the life insured
Name of the policyholder
Self and his wife
Mr. Naushad Ahmad
4.
Name of the insurer
National Insurance Co. Ltd.
5.
Date of Repudiation/Rejection
09.10.2017
6.
Reason for repudiation/Rejection
-
7.
Date of receipt of the Complaint
05.01.2018
8.
Nature of complaint
Repudiation of Claim
9.
Amount of Claim
Rs.14966/-
10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs. 14966/-
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 02.12.2019 at Lucknow
14.
Representation at the hearing
mmm) For the Complainant
Absent
nnn) For the insurer
Mr. Ram Kumar Gupta,
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
02.12.2019
17. Mr. Naushad Ahmad (Complainant) has filed a complaint against National Insurance Company
Limited (Respondent) against repudiation of his medi claim.
18. Brief Facts Of the Case:- Complainant has stated that he was insured with the respondent. He was admitted at
New Leelamani Hospital, Kanpur on 02.08.2017 with diagnosis of T2DM with vertigo and discharged on 05.08.2017.
After discharge from the hospital, he has submitted a claim of Rs.14966/- to the RIC for its reimbursement but his
claim was rejected by the RIC on 24.08.2017. TPA vide its letter dated 09.10.2017 maintained its decision of
repudiation of my claim under policy clause 4.18. The complainant further stated that he lodged his grievance with
the IRDA on 12.11.2017 which remained un-replied. Aggrieved with the unjustified repudiation of the claim, the
complainant approached this forum.
In their SCN/Reply, RIC has stated that the said complaint lodged by the complainant for repudiation of his claim
under the mediclaim policy issued by the respondent. Health claims are processed by TPA’s on behalf of the
respondent company. The Health India Ins. TPA Services Pvt.Ltd is the TPA assigned for the servicing of our
mediclaim. As per information received from the concerned TPA regarding the said claim, the claim has been
repudiated as per the Clause NO:4.18 (exclusion) as the treatment taken by the insured can also be taken as OPD.
Hence Claim is not admissible.
19. The complainant has filed a complaint, correspondence with the respondent. Annexure-VIA duly filled/signed
submitted by the complainant while respondent not filed SCN along with enclosures.
20. Complainant remained absent. I have heard the representative of the respondent at length and perused paper
filed on behalf of the complainant as well as the insurance company.
21. Complaint was filed by the claimant as the claim for his hospitalization for treatment of T2D with vertigo were
not made by the respondent insurance company.
At the very outset, it is to be observed that the respondent insurance company has not passed any order either
sanctioning or repudiating the claim of the complainant. Merely TPA had recommended for repudiation of the claim
but no order was passed by the insurance company. Policy bond was issued by the respondent insurance company
who was under legal obligation to pass the order on the claim of the complainant.
In such circumstances, it would be appropriate that the insurance company should pass specific order on the claim
of the complainant within 30 days. If the complainant is not satisfied with the order, he has full liberty to move as
per rules.
Accordingly, complaint is disposed off.
22. Let copy of award be given to both the parties.

Dated : December 2, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Vijay Tandon…………..……....………………. Complainant
V/S
National Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-048-1819-0023 Order No. IO/LCK/A/GI/0100/2019-20
1.
Name & Address of the Complainant
Mr. Vijay Tandon,
16/78, Civil Lines,
Kanpur
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
450402/48/16/8500001096
National Mediclaim
31.12.2016 to 30.12.2017
3.
Name of the life insured
Name of the policyholder
Mrs Leenika Tandon,
Mr. Vijay Tandon
4.
Name of the insurer
National Insurance Company Limited
5.
Date of Repudiation/Rejection
---
6.
Reason for repudiation/Rejection
---
7.
Date of receipt of the Complaint
03.05.2018
8.
Nature of complaint
Delay in settlement of claim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
--
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 02.12.2019 at 10.15 am at Lucknow
14.
Representation at the hearing
ooo) For the Complainant
Mr.Vijay Tandon
ppp) For the insurer
Mr. Rajendra Kumar, Sr. Branch Manager
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
16.12.2019
17. Mr. Vijay Tandon (Complainant) has filed a complaint against National Insurance Company Limited
(Respondent) alleging delay in settlement of health claim of his wife.
18. Brief Facts Of the Case:- The complainant has stated that his wife was admitted in SGPGI, Lucknow
for the treatment of abdominal ;pain and distension since two months. The patient was having
abdominal pain more in the upper abdomen, increases with food intake. The patient was known
diabetic since last eight year. The patient was hospitalized during the period from 09.03.2017 to
08.04.2017. The claim was submitted for reimbursement to the concerned TPA/RIC. A query was raised
by the TPA which was replied by the complainant on 15.11.2017 and 09.02.2018. But no reply was given
by the TPA. Aggrieved with the delay settlement of his wife’s claim, the complainant had approached
this forum.
In their SCN/reply, RIC has stated that they have issued the said mediclaim policy to the complainant
for a sum insured of Rs.2 lacs. The claim was lodged on 09.03.2017 for the hospitalization of his wife at
SGPGI, Lucknow due to acute pain in abdominal. The TPA has reviewed the file and send the query
letters for settlement of the claim which was not provided by the complainant till date. RIC has further
submitted the mail, copy of the TPA letter dated 22.11.2019, for processing of the claim. Reply of
queries are required is still pending from the complainant.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures on the date of hearing.
20. I have heard the complainant and representative of the respondent at length and perused paper
filed on behalf of the complainant as well as the insurance company.

21. Claimant Sh. Vijay Tandon and respondent representative Sh. Rajendra Kumar, Sr. Branch Manager,
National Insurance Company Limited, Branch Office, Govindnagar, Kanpur are present.
This matter was taken up on 2
nd
December 2019. On the basis of submission of the respondent
representative, complainant was required to submit certain papers.
Today, complainant submits that he has already submitted all the papers which are in his possession. It
is further submitted that now apart from the all the papers already submitted, there is no other
document which can be provided.
List of documents required by the respondent shows that all these documents relates to the treatment
undertaken at SGPGI, Lucknow. Even if any document is required, respondent or his agent i.e. TPA can
obtain the same from SGPGI, Lucknow. Some of the queries appears to be unwarranted. At Point No:5,
respondent requires to know the reasons for prolong stay in the hospital from the treating doctor.
Only Bed Head Ticket can show the reasons for stay in the hospital. How and why complainant would
be asked to provide any document on this count. It all shows the harassment being made by the
respondent in settling the claim.
Likewise in Point No:3, summary of treatment done in SGPGI during course of hospitalization is
required. Again the same has already been submitted by the complainant. Further complainant has
already submitted point wise reply of all the queries vide his letter dated 05.05.2017. Complainant has
already submitted the reply of queries made by the respondent or TPA. All the documents of treatment
are available at SGPGI, Lucknow. Respondent is under an obligation to settle the claim expeditiously but
for oblique motive, claim is not being settled,
It appears that the respondent is intentionally withholding the disposal of the claim.
Having considered the submissions, it is directed that the respondent shall settle the claim within a
period of 30 days from today. If they need any document apart from those already submitted by the
complainant, respondent has full liberty to collect the same from SGPGI, Lucknow.
Accordingly complaint is disposed off.
22. Let copy of award be given to both the parties.
Dated : December 16, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr Jai Prakash Bharati…………..……....………………. Complainant
V/S
New India Assurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-049-1718-0209 ORDER NO. IO/LCK/A/GI/0083/2019-20
1.
Name & Address of the Complainant
Mr. Jai Prakash Bharati, SR No : 228484
Life Insurance Corporation of India,
Branch Office, Unnao-209801
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
120700/34/16/04/00000004
Group Mediclaim Policy
01.04.2016 to 31.03.2017
3.
Name of the life insured
Name of the policyholder
All employee and his/her spouse.
M/s Life Insurance Corporation of India
4.
Name of the insurer
New India Assurance Company Limited
5.
Date of Repudiation/Rejection
20.02.2017
6.
Reason for repudiation/Rejection
Repudiation as per Policy Exclusion Clause F Point No:vi
7.
Date of receipt of the Complaint
27.12.2017
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.112546/-
10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs.112546/-
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 02.12.2019 at Lucknow
14.
Representation at the hearing

qqq) For the Complainant
Mr. Jai Prakash Bharti
rrr) For the insurer
Mr. Ashwini Kumar
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
02.12.2019
17. Mr. Jai Prakash Bharati (Complainant) has filed a complaint against United India Insurance
Company Limited (Respondent) alleging repudiation of his health claim.
18. Brief Facts Of the Case:- Complainant has stated that he was hospitalized on 02.10.2016 and
discharged on 10.10.2016 with complaints of acute pancreatitis. Complainant had further stated that he
had submitted all the claim related documents to RIC for settlement of his mediclaim but claim was not
settled. Later on respondent company rejected the claim as per Policy Exclusion Clause F Point No: vi.
Aggrieved with the unjustified repudiation of the claim, the complainant had approached this forum.
In their SCN/Reply, RIC has stated that the complainant was admitted in SKD hospital from 02.10.2016
to 10.10.2016 for acute pancreatitis. As per history and clinical findings patient was suffering from pain
in abdomen. The most common cause of acute pancreatitis is alcohol intake. In case of the complainant,
as per history and examination of hospital, it is clearly mentioned that before complaint the patient has
taken alcohol. It is also mentioned as Alcohol+. Hence this claim is not payable as per Clause F Exclusion
– Point No:vi which reads as under :
“Convalescence, general debility, ‘Run Down’ condition or rest cure, obesity treatment and its
complications, congenital external disease/defects or anomalies, treatment relating to all
psychiatric and psychosomatic disorders, infertility, sterility, use of intoxicating drugs/alcohol,
use of tobacco leading to cancer”
19. The complainant has filed a complaint, correspondence with the respondent. Annexure-VIA duly
filled/signed submitted by the complainant while respondent not filed SCN along with enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as well
as insurance company.
21. There is no dispute that the complainant was insured with the respondent. Claim for Rs.112546/-
made by him as he was suffering from acute Pancreatitis. Claim was repudiated on the ground that the
complainant is habit of taking alcohol. As per Clause No : F Exclusion – Point No: vi, claim could not be
granted.
Complainant submits that he is not alcoholic and he has never taken the alcohol. Further in the discharge
card also, there is no diagnosis of Acute Pancreatitis due to habit of alcohol. Respondent representative
tried to place reliance upon a sheet,which is a scanned copy and is not legible. He has further placed
reliance upon the letter of TPA wherein it is mentioned that as per hospital record, complainant had habit
of alcohol intake.
In order to bring the case under the exclusion clause, burden lies upon the insurer to prove it. TPA had
informed that the hospital record shows that the complainant is a habit of taking alcohol but there is no
material on record to show that there was a diagnosis by the doctor that the ailment of Acute
Pancreatitis is the outcome of alcoholism by the complainant.
Any claim can not be repudiated merely on surmises and conjectures. There must be some material
available on record to show that the complainant case is covered in the Exclusion Clause. But respondent
failed to prove it.
In such circumstances, I am of the view that the complainant would be entitled for his claim as well as
interest @6% per annum from the date of claim till the date of actual payment.
Complaint is allowed. Respondent are directed to make the payment of the claim to the complainant with
interest @ 6% per annum from the date of claim till the date of actual payment.
22. Let copy of award be given to both the parties.
Dated : December 2, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Rajesh Dubey …………..……....………………. Complainant
V/S
The New India Assurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-049-1819-0064 Order No. IO/LCK/A/GI/0096/2019-20
1.
Name & Address of the Complainant
Mr. Rajesh Dubey
Surya Vishal Flat No. – 405
Kothuwa Vinayak Varanasi- 221010

2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
1207003417040000004
Group Mediclaim Policy
01.04.2017 to 31.03.2018
3.
Name of the life insured
Name of the policyholder
Mr. Rajesh Dubey
LIC of India
4.
Name of the insurer
The New India Assurance Company Limited
5.
Date of Repudiation/Rejection
28.11.2017
6.
Reason for repudiation/Rejection
Policy Exclusion clause F – Point No. v “Dental
treatments except arising out of an accident”
7.
Date of receipt of the Complaint
02.07.2018
8.
Nature of complaint
Repudiation the claim
9.
Amount of Claim
Rs. 16,103/-
10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs. 16,103/- + Interest
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 10.12.2019 at 11.00 am at Lucknow
14.
Representation at the hearing
For the Complainant
Mr. Rajesh Dubey
For the insurer
Mr.Ashwini Kumar,Asstt.Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
10.12.2019
17. Mr. Rajesh Dubey (Complainant) has filed a complaint against New India Assurance
Company Limited (Respondent) alleging repudiation of his health claim.
18. Brief Facts Of the Case:- The complainant has stated that he had lodged a claim with the
TPA/RIC for amount Rs. 16,103/- on 21.08.2017. He did not get any reply till 10.11.2017 so he
talked to the customer care of TPA for status of his claim. further he received repudiation letter
dated 30.11.2017 on his mail. After he mailed clarification to the RIC and also called several
times at customer care of the TPA/RIC but no action was taken for my complaint. Aggrieved
with the decision of the RIC, complainant has approached this forum.
In their SCN/reply, the respondent has stated that RIC has processed the patient consulted in
OPD on 03.08.2017 as a case of Periapical Abscess. Doctor advised him oral medication, Root
Canal Therapy and Apicoectomy ( Root – end filling). Therefore this claim is not payable as per
terms and conditions of the policy. As per clause F Exclusions – Point No. v which reads as
under:
“All types of dental treatments except arising out of an accident” and
Annexure – II – Point No: 61 which reads as under :
“Dental treatment expenses that do not require hospitalization – Not payable”
19. The complainant has filed a complaint letter, annexure VI A, correspondence with
respondent and while respondent has filed SCN with enclosures.
20. I have heard the parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
21. Admittedly the complainant is a member of Group Medical Policy. Claim for treatment of
the insured for dental problem was repudiated on the basis of Exclusion Clause No:F Point
No: v of the policy bond which reads as under :
“All types of dental treatments except arising out of an accident”
Annexure II – Point No:61 which reads as under :
“Dental treatment expenses that do not require hospitalization – Not Payable”
Exclusion No: F Point No:v did not allow the claim for dental treatment, I do not find any
infirmity in the impugned order of the repudiation of the claim.
Hence complaint is liable to be dismissed.
22. Complaint filed by Mr. Rajesh Dubey stands dismissed.
23. Let copy of award be given to both the parties.
Dated : December 10, 2019 (Justice Anil Kumar Srivastava)
Place: Lucknow Insurance Ombudsman

PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Madhukar Bajpai …………..……....………………. Complainant
V/S
New India Assurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-049-1819-0132 Order No. IO/LCK/A/GI/0110/2019-20
1.
Name & Address of the Complainant
Mr. Madhukar Bajpai,
Life Insurance Corporation of India,
BO-Lalbaugh, Lucknow-226001.
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
12070034170400000004
Group Mediclaim Policy.
17.02.2016 to 16.02.2017
3.
Name of the life insured
Name of the policyholder
Sri. Madhukar Bajpai.
Sri. Madhukar Bajpai.
4.
Name of the insurer
New India Assurance Company Limited
5.
Date of Repudiation/Rejection
---
6.
Reason for repudiation/Rejection
---
7.
Date of receipt of the Complaint
22.11.2018
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 45,652/-
10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs. 45,652/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 27.12.2019 at 11.00 am at Lucknow
14.
Representation at the hearing
sss) For the Complainant
Mr. Madhukar Bajpai
ttt) For the insurer
Mr. Ashwini Kumar
15.
Complaint how disposed
Recommendation
16.
Date of Award/Order
27.12.2019
17. The complainant Sri Madukar Bajpai has filed a complaint against New India Assurance Company
Limited (Respondent) challenging repudiation of health claim of his daughter Ms. Nancy Bajpai.
18. Brief Facts Of the Case: The complainant has stated that he & his family was insured under the aforesaid
policy issued by the respondent. He has further stated that his daughter Ms. Naincy Bajpai underwent eye
treatment (Lasik both eyes) at Garg Opthalmic Centre on 20.01.2018 & discharged on thesame date. He
submitted a claim on 27.01.2018 for Rs.45,652/- with the respondent through proper channel which was
repudiated by the respondent vide their letter dated 30.03.2018. The complainant has stated that he had
submitted a revised prescription (along with Doctor’s undated clarification) on 19.06.2018 under cr no.18367
dated 15.01.2018 wherein the chief complaint has been mentioned as “Recurrent-Redness-BE-Not
comfortable with own Glasses-BE.” From the available records / documents it has been observed that the
complainant has neither approached grievance department of respondent’s regional office nor the grievance
department of their Head office.
In their SCN/reply, RIC has stated that the patient admitted for the customized Lasik of both eyes on dated
20.01.2018 at hospital and discharged on 20.01.2018. As per discharge summary patient chief complaints
was “She wants to do away with glasses”. Since the treatment was taken just to get rid of Spectacles hence
this claim was not payable under exclusions section (ii) and (xxiv) which states
F(ii) – Circumcision, cosmetic or aesthetic treatment, plastic surgery unless required to treat injury or illness
F(xxiv)- Lasik Laser treatment performed to get rid of spectacles or contact lenses unless ”the treatment is
for Keratotomy of insured having more than (-4) refractive error, therapeutic reasons like recurrent corneal
erosions, nebular opacities and non healing ulcers”
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
repudiation letter while respondent filed SCN with enclosures.
20. Sincere efforts were made for mediation to resolve the subject matter of complaint. The complainant
and the representative of the respondent company were heard. During course of the mediation, both the
parties filed joint application (Mediation Agreement) duly signed by the complainant and the representative
of the respondent mentioning therein about settlement of the matter willingly and mutually and agreed to
settle the subject matter of the complaint as follows

The respondent New India Assurance Co. Ltd. has agreed to admit and pay the claim as per terms
and conditions of the policy. The Complainant also agreed for the same.
22. As matter within parties has resolved mutually, hence the complaint is decided in terms of
mediation/mutual agreement between both the parties.
23. Let copies of this award be given to both the parties.
Dated: December 27, 2019 (Justice Anil Kumar Srivastava)
Place: Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Satish Chandra Agarwal…………..……....………………. Complainant
V/S
Oriental Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-050-1718-0283 ORDER NO. IO/LCK/A/GI/0102/2019-20
1.
Name & Address of the Complainant
Mr. Satish Chandra Agarwal
33, KP Kakkar Road,
Allahabad-211003.
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
224302/48/2017/1851
PNB-Oriental Royal Mediclaim Policy
20.02.2017 to 19.02.2018
3.
Name of the life insured
Name of the policyholder
Mr. Satish Chandra Agarwal
Mr. Satish Chandra Agarwal
4.
Name of the insurer
Oriental Insurance Co. Ltd.
5.
Date of Repudiation/Rejection
10.05.2018
6.
Reason for repudiation/Rejection
Claim falls under Exclusion Clause No:4.2
7.
Date of receipt of the Complaint
15.03.2018
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
---
10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs. 2,02,000/-
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 31.10.2019 at Lucknow
14.
Representation at the hearing
uuu) For the Complainant
Mr. Satish Chandra Agarwal
vvv) For the insurer
Mr. Jeet Lal Yadav, Branch.Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
18.12.2019
17. Mr. Satish Chandra Agarwal (Complainant) has filed a complaint against Oriental Insurance Company Limited
(Respondent) alleging delay in settlement of his health claim.
18. Brief Facts Of the Case:- According to the complainant, he was admitted at Vatsalya Hospital, Allahabad on
20.09.2017 with complaint of chest pain, palpitation, breathlessness etc and discharged on 27.09.2017. As per
discharge card the complainant was diagnosed, chest pain, ACA and CVA and underwent Coronary Angioplasty.
He also requested for cash-less facility which was denied by M/s Raksha TPA vide their letter 22.09.2017. After
discharge from the hospital the claimant submitted a claim bill for Rs. 2,14,529- with the RIC for reimbursement.
But, even after receipt of all the original medical papers, the claim was not settled by the TPA. He further stated
that he had written many letters to the respondent but no reply was given by them. After making complaints in
this forum, his claim was rejected by the respondent company. Aggrieved with the decision of RIC, the
complainant has approached this forum for redressal of his complaint.
In their SCN/Reply, RIC has admitted that the said policy was issued by the respondent to the insured for the first
time at the age of 69 years. On receipt of claim papers submitted by the insured to M/s Raksha TPA, it was found
that the patient had previous history of Acute Coronary Syndrome as well as he was a known case of CVA, and also
suffering from hypertension and diabetes Mellitus which is cause of ACS and CVA which falls under two years
waiting period. Hence, the TPA recommended this claim for repudiation due to violation of Policy Clause 4.2. In
view of the above mentioned grounds, the RIC repudiated the claim under Exclusion No:4.2 vide their letter dated
10.05.2018.
Supplementary self contained note is submitted on 18.12.2019 wherein it is stated that at the time of admission,
patient was hypertensive. Treating Dr. Neeraj Agarwal confirmed that patient was known case of Multiple Lacunar
Infract In Left Basal Ganglion. It is further submitted that allegedly two stents were implanted but neither sticker
nor details were provided except for the detail of one stent. It is further submitted that two cheques given by the
complainant to the hospital were not en-cashed rather bounced. As per policy condition patient can only claim the
reimbursement of treatment cost and hospital bill once they are paid. But in the present case, payment was not
paid and complainant is not entitled for reimbursement.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and copy of
policy document while respondent have filed SCN with enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as well as the
Insurance Company.
21.Basically complaints relates to a medical claim submitted by the complainant with the respondent for his
treatment at Vatsalya Hospital, Prayagraj which was repudiated vide letter dated 24.04.2018 on the following
grounds :
“Chest pain, ACS, CVA patient was admitted with C/o chest pain, palpitation, breathleeness on
dated 20.09.2017 treated surgically with CAG/PTCA and discharged on 27.09.2017, as policy
coverage is only in first year hence this case is non-payable as per Policy Clause 4.2”.
Complainant submits that he is neither hypertensive nor diabetic. He gave two cheques to the hospital but his
claim is wrongly repudiated.
Respondent representative submits that the complainant is known case of CVA. Both the cheques given by the
complainant to the hospital were bounced hence he has not paid any amount to the hospital, so there is no
reason for making the reimbursement. It is further submitted that doctor himself has opined that the patient had
previous history of Acute Coronary Syndrome. Although it is fairly admitted by the respondent representative
that claimant is not known case of Diabetes Mellitus.
Whole controversy revolves upon the interpretation of Clause No:4.2 of the policy bond coupled with the fact that
complainant has not paid any payment to the hospital. His request for Cash Less Treatment was also refused.
Dr. Agarwal has mentioned that the patient is known case of CVA and ACS in the patient case sheet of Vatsalya
Maternity and Surgical Centre Pvt.Ltd, Allahabad. It is specifically mentioned that the complainant is having
history of Acute Coronary Syndrome and is under treatment for the same. The blood pressure of the complainant
also measured at 160/90 mg/dl at the time of admission.
Dr. Neeraj Agarwal has given a certificate to this effect that finding of Multiple Lacunar Infract In Left Basal
Ganglion was also mentioned as per information given by the patient. Even on the discharge card, it was
mentioned that it is a known case of CVA.
In such circumstances, claim is rightly repudiated by the respondent.
The conduct of the complainant itself shows that he has not bonafidely making the claim. Cheques were bounced
as per return memo issued by Bank of India but the complainant has given a false information and certificate that
he has made the payment to the hospital through cheques which have been encashed. It shows that complainant
wants to get the claim cleared on the basis of false information which itself would be a ground for dismissal of
the claim. There may be some reasons that hospital discharged the complainant without depositing of hospital
charges. It is a matter between the complainant and the hospital. But at the same time, claim from the
respondent can only be justified when complainant makes the payment to the hospital then reimbursement of
the amount can be made. Since no amount has been made by the complainant to the hospital only on this
ground also, complaint is liable to be dismissed.
Having considered the submissions of the parties, I am of the view that the complaint lacks merit and liable to be
dismissed.
22. Complaint filed by Mr. Satish Chandra Agarwal stands dismissed.
23. Let copy of award be given to both the parties.
Dated : December 18, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman

PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Santosh Kumar…………..……....………………. Complainant
V/S
United India Insurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-051-1718-0169 ORDER NO. IO/LCK/A/GI/0091/2019-20
1.
Name & Address of the Complainant
Mr. Santosh Kumar,
18/532, Sector-18,
Indiranagar,Lucknow-226016
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
411500/48/2018/482 [Emp.No:22769]
Staff GMC Policy
01.04.2017 to 31.03.2018
3.
Name of the life insured
Name of the policyholder
Smt. Madhu Chaudhary,
United India Insurance Company Limited
4.
Name of the insurer
United India Insurance Co. Ltd.
5.
Date of Repudiation/Rejection
06.07.2017
6.
Reason for repudiation/Rejection
Not covered under Maternity benefit 1.2 (6)
7.
Date of receipt of the Complaint
01.11.2017
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.1,00,000/-
10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs. 1,00,000/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 10.12.2019 at Lucknow
14.
Representation at the hearing
www) For the Complainant
Mr. Santosh Kumar
xxx) For the insurer
Mr. Prateek Raj, Asstt.Manager
15.
Complaint how disposed
Dismissed.
16.
Date of Award/Order
10.12.2019
17. Mr. Santosh Kumar (Complainant) has filed a complaint against United India Insurance Company
Limited (Respondent) alleging repudiation of maternity claim of his daughter in law.
18. Brief Facts Of the Case:- The complainant has stated that he is an employee of United India. He and
his family were covered under staff medical policy and premium was being deducted from his salary. His
Daughter-in-law Smt. Madhu Chaudhary was admitted in Goel Nursing Home, Lucknow from 19.06.2017
to 23.06.2017 for full term pregnancy and underwent LSCS. He has submitted the claim bills to the
concerned TPA for settlement. Concerned TPA vide their letter dated 06.07.2017 informed that this claim
is not payable. He has further stated that against the recommendation of TPA, a grievance was submitted
to the respondent. But no response has been received by him from the respondent. Now the
complainant has approached this forum for redressal of his complaint.
In their SCN/Reply, RIC has stated that his daughter in law Smt. Madhu Chaudhary had included from in
SGMC policy on 02.03.2015 and date of hospitalization was 19.06.2017. As per policy condition No : 1.2
sub section (6) Maternity benefits reads as “maternity claim is extended to the independent child or a
family member of the dependent/independent child provided such child or family member has been
covered in policy at least for the last three years as on the date of hospitalization under maternity cover.”
Therefore this claim was repudiated for not being covered under the policy.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures.
20. I have heard the complainant and respondent representative at length and perused paper filed on
behalf of the complainant as well as the Insurance Company.
21. Complainant and respondent representative are present.

This is a claim regarding full term pregnancy occurred to the complainant daughter-in-law Mrs. Madhu
Chaudhary. There is no dispute on the point that she was covered in the policy of Group Mediclaim policy
of the complainant who is an employee of M/s United India Insurance Company Limited.
As per complaint of the complainant, his daughter-in-law was covered in the Group Medilaim Policy and
the incident relates to Year 2017. The claim was repudiated on the ground that Mrs.Madhu Chaudhary
was not covered in the policy in view of the Condition No: 1.2 which provides that “Hospitalization
benefits point No:6 Maternity benefits reads as “Maternity/independent child provided such child or
family member has been covered in the policy at least for the last three years as on the date of
hospitalization under maternity cover.”
Claim was repudiated mainly on the ground that as per Policy Condition No : 1.2 sub section (6)
Maternity benefits which reads as under “
“Maternity claim is extended to the independent child or a family member of the
dependent/independent child provided such child or family member has been covered
in policy at least for the last three years as on the date of hospitalization under
maternity cover.”
In my opinion, I do not find any infirmity in the impugned order of repudiation. Accordingly complaint is
devoid of merit and is liable to be dismissed.
22. Complaint filed by Mr. Santosh Kumar stands dismissed.
24. Let copy of award be given to both the parties.
Dated : Decemebr 10, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Naman Kumar Srivastava…………..……....………………. Complainant
V/S
United India Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-051-1718-0182 Order No. IO/LCK/A/GI/0086/2019-20
1.
Name & Address of the Complainant
Mr. Naman Kumar Srivastava,
SBI General Ins. Co. Ltd.
BK Square , Ist floor,10—Park Road
Civil Lines , Gorakhpur- 273001
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
Tailormade Group Health Policy
28.08.2016 to27.08.2017
3.
Name of the life insured
Name of the policyholder
Retired employees of SBI and family members
SBI General Insurance Co.Ltd
4.
Name of the insurer
United India Company Limited
5.
Date of Repudiation/Rejection
---
6.
Reason for repudiation/Rejection
---
7.
Date of receipt of the Complaint
07.11.2017
8.
Nature of complaint
Non settlement of claim
9.
Amount of Claim
Rs.32520/-+ interest
10.
Date of Partial Settlement
---
11.
Amount of relief sought
---
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 04.12.2019 at 10.15 am at Lucknow
14.
Representation at the hearing
yyy) For the Complainant
Mr. Naman Kumar Srivastava
zzz) For the insurer
Mrs. Shashi Bala, Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
04.12.2019
17. Mr. Naman Kuamr Srivastava (Complainant) has filed a complaint against United India Insurance
Company Limited (Respondent) alleging non settlement of health claim of his father.

18. Brief Facts Of the Case:- The complainant has stated his father was hospitalized in Rachit Hospital,
Gorakhpur on 07.04.2017 and discharged on 10.04.2017 due to traumatic Head Injury. Complainant has
submitted all claim related documents to RIC/TPA for settlement of his claim but his claim was not settled by the
insurance company. Aggrieved with the non-settlement of mediclaim, he approached this forum for redressal of
his grievance.
In their SCN/reply, RIC has stated that complainant’s father was admitted at Rachit Hospital, Gorakhpur on
07.04.2017 for Head Injury and discharged on 10.04.2017. He incurred a total hospitalization expenses of
Rs.32520/- towards medical expenses incurred by the insured. He submitted an undated emergency treatment
certificate from Dr RN Rain. But even after continuous reminders dated 12.09.2017, 24.09.2017 and 03.10.2017,
the client has not submitted the following documents :
1. A letter from treating doctor stating the exact incident history [ not mentioned in undated certificate].
2. MLC/FIR copy.
3. Original investigation reports confirming diagnosis of left parietal bone with film plate.
4. Original investigation reports for Rs.1800/- dated 07.04.2017 and Rs.200/- dated 07.04.2017, Rs.1700/- dated
07.04.2017.
5. Original bill for Rs.600/- dated 07.04.2017 and Rs.1800/- dated 07.04.2017.
6.
In consequence of the above, due to non receipt of query documents, the claim is closed as NO CLAIM.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and copy of
policy document while respondent filed SCN with enclosures.
20.. I have heard both the parties at length and perused paper filed on behalf of the complainant as well as the
insurance company.
21. I have gone through the record, complaint is made for payment of the claimant for Rs.32520/-. As per the
mail communication of the respondent dated 03.12.2019, claim for Rs.30542/- has already been paid to the
complainant on 27.11.2019 through NEFT. This fact is undisputed and admitted by the complainant.
Accordingly complaint is disposed off as full satisfaction.
22. Complaint filed by Mr. Naman Kumar Srivastava stands dismissed as full satisfaction.
23. Let copy of award be given to both the parties.
Dated : November 4, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Satyanand Bhattacharya…………..……....………………. Complainant
V/S
United India Insurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-051-1718-0203 ORDER NO. IO/LCK/A/GI/0081/2019-20
1.
Name & Address of the Complainant
Mr Satyanand Bhattacharya,
Sahara Shahar,Vipul Khand,
Gomtinagar,Lucknow-226010..
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
0802002817P108839696
Individual Health Policy
29.09.2017 to 28.09.2018
3.
Name of the life insured
Name of the policyholder
Mr. Satyanand Bhattacharya
4.
Name of the insurer
United India Insurance Co. Ltd.
5.
Date of Repudiation/Rejection
-
6.
Reason for repudiation/Rejection
Partial repudiation of claim
7.
Date of receipt of the Complaint
18.12.2017
8.
Nature of complaint
Partial Repudiation of claim
9.
Amount of Claim
Rs.32731/- with interest
10.
Date of Partial Settlement
01.07.2017
11.
Amount of relief sought
Rs. 32731/- plus interest.
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 02.12.2019 at Lucknow
14.
Representation at the hearing

For the Complainant
Mr. Satyanand Bhattacharya
For the insurer
Mr. Vijay P.Singh
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
02.12.2019
17. Mr. Satyanand Bhattacharya (Complainant) has filed a complaint against United India Insurance
Company Limited (Respondent) alleging partial repudiation of his medi claim.
18. Brief Facts Of the Case:- The complainant, Sri Satyanand Bhattacharya has stated that he was
covered under policy no.0802002817P108839696 for a period of one year incepting from 29.09.2017
which is a continuous renewal of previous policy no.0802002816P108433755 expired on 28.09.2017.
He suffered a serious attack of Hematuria with large blood clots blocking urination. He further stated
that he got himself admitted in Microlap Nursing Home, Kolkata on 07.10.2017 & discharged on
14.10.2017 where Dr. Amlan Chakraborty examined him & decided to operate on the same evening
with surgery by LASER to achieve lesser blood loss & post operative trauma. The complainant has
stated that his family members as well as The Microlap Nursing Home tried to contact Raksha TPA for
seeking pre-Authorization for cashless treatment but in vain. However, after frantic call to Divisional
office –II, Lucknow of RIC & also to TPA, the Raksha TPA initially sanctioned Rs.69281/- on 12.10.2017
but later, lowered the sanctioned amount to 66281/-vide their undated letter & also asked about the
justification of Laser based surgery. Dr. Amlan Chakraborty, vide his letter dated 13.102017 explained
to the TPA the reason for laser based surgery however, the TPA approved only a sum of Rs.10520/-
towards Doctor’s fee in place of Rs.40000/-. An amount of Rs.3251/- were deducted from medication
charges & processing charges. As Such, a total sum of Rs.32731/- were deducted from a total hospital
bill of Rs.99012/-
In their revised SCN/reply submitted with this office on 29.11.2019, the RIC has referred to point no. 6
of their Head Office’s circular no. HO: HEALTH:043:16-17 dated May 05, 2016 & have stated that “In
case of Laser assisted Haemorrhoidectomy / Prostatectomy liability to be restricted to the cost of
conventional Haemorrhoidectomy / Prostatectomy. The RIC has further mentioned that Rs.500/-were
deducted on account of processing charges & Rs.2751/- were deducted on several consumable items
which are not payable under their health policy.
The RIC has further stated that Rs.2751/- & Rs. 500/- were deducted towards Medication charges and
processing charges respectively which is not payable.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as well
as the Insurance company.
21. There is no dispute that the complainant insured was operated upon for Hematuria Prostatomhgaly
with median Lobe Hypertrophy at Microlap, Kolkatta. Although prior to that he was under treatment at
Sahar Hospital, Lucknow. Operation was done by laser to achieve lessor blood loss and post operative
trauma. Claim was submitted for Rs.99012/- out of which an amount of Rs.66281/- was sanctioned as
cash less settlement. Payment of Rs.2751/- towards consumables charges, Rs.500/- towards processing
charges and Rs.29480/- for laser charges were deducted.
So far as the deduction for consumables and registration charges are concerned, they are deducted in
accordance with the terms and conditions of the policy. Complainant also agrees for the deductions.
So far as the deduction of Rs.29480/- is concerned, it was deducted as per United India Insurance
Co.Ltd, Head Office, Chennai circular No:HO:Health:043:16-17 dated May 5, 2016. At the very outset, it
would not be out of place to observe that any directions issued by the Head Office of United India
Insurance Company are binding upon the insurance company only. The same could have binding effect
upon the insured, provided such directions find place in the policy bond.
There is no standardization in the policy that only conventional method should be used for surgery. It is
for the surgeon to decide the mode of surgery. If the insurance company wants that laser method should
not be used in the surgery, charges for the same will not be payable by the insurer. The condition to this
effect should find place in the policy bond. In the policy bond, there is no such condition.
There is no dispute that the claim has incurred expenses on a specialized surgery, I am of the view that
the insured is entitled for an amount of Rs.29480/- from the insurer.
Complaint is partially allowed to the extent that the respondent shall pay Rs.29480/- alongwith interest
@ 6% per annum from the date of the claim till the date of actual payment to the claimant.

22. Let copy of award be given to both the parties.
Dated : December 2, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr Bharath Prasad…………..……....………………. Complainant
V/S
United India Insurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-051-1718-0205 ORDER NO. IO/LCK/A/GI/0082/2019-20
1.
Name & Address of the Complainant
Mr. Bharat Prasad Dwivedi,
House NO:15, Viramkhand-4,
Gomtinagar,Lucknow-226010
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
070300281P113047823
Group Mediclaim Policy
01.02.2016 to31.01.2017
3.
Name of the life insured
Name of the policyholder
Retired employee and his/her spouse.
M/s Hindustan Aeronautics Limited
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of Repudiation/Rejection
18.09.2017
6.
Reason for repudiation/Rejection
Repudiation as per Policy Clause No:1.5 (Note-2)
7.
Date of receipt of the Complaint
22.05.2018
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.14039/-
10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs.14039/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 02.12.2019 at Lucknow
14.
Representation at the hearing
aaaa) For the Complainant
Mr.Bharat Prasad Dwivedi
bbbb) For the insurer
Mrs Nishi Srivastava, AM
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
02.12.2019
17. Mr. Bharath Prasad (Complainant) has filed a complaint against United India Insurance Company
Limited (Respondent) against repudiation of his wife Mrs. Pramila Dwivedi’s health claim.
18. Brief Facts Of the Case:- Complainant has stated that his wife was hospitalized on 04.06.2016 and
discharged on 06.06.2016 with complaints of acute vertigo. Complainant had further stated that he had
submitted all the claim related documents to RIC for settlement of mediclaim of his wife but claim was
not settled. Later on respondent company rejected the claim as per Policy Condition NO:1.5 Note(2).
Aggrieved with the unjustified repudiation of the claim, the complainant had approached this forum.
In their SCN/Reply, RIC has stated that the complainant Mr. Bharat Prasad Dwivedi along with his wife is
covered under policy issued to HAL for the sum insured of Rs.400000/- since 01.02.2014. Beneficiary
Mrs. Pramila Dwivedi (spouse) was admitted to St.Josephs Hospital, Lucknow on 04.06.2016 with
complaints of Acute Vertigo treated conservatively and discharged on 06.06.2016. Insured submitted a
claim for reimbursement for the expenses of Rs.14124/- incurred during hospitalization. Documents were
received by RIC on 24.09.2016 and claim was processed. While processing the claim, it was noted that
discharge summary was not available. Hence, request was raised for short fall document, complainant
did not submit the requirement document, hence, a closure notice was sent on 26.10.2016. Claim was
closed on 03.11.2016 and closure letter too was sent on 03.11.2016.
Insured submitted the discharge summary after closure of the claim hence, claim was reopened. As per
discharge summary, claimant is a known case of hypertension with giddiness. Underwent investigations
and diagnosed to have acute vertigo due to cervical spondylitis. Medical management done upon the
patient and she was discharged on 06.06.2016. It was noted that there was no active line of treatment
during hospitalization, treated with oral medicines which does not warrant hospitalization. Treatment
could have been done on OPD basis. As per the policy conditions expenses on the treatment/procedure
usually done on OPD converted into inpatient are not admissible under the policy hence claim stands
denied under Condition 1.5 Note(2) of the policy.

19. The complainant has filed a complaint, correspondence with the respondent. Annexure-VIA duly
filled/signed submitted by the complainant while respondent forwarded the SCN received by them from
their Bangalore offce along with enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as well
as the insurance company.
21. Admittedly Smt. Pramila Dwivedi wife of Sh. Bharat Parsad was admitted in St. Joseph Hospital,
Lucknow on 04.06.2019 with complaint of acute vertigo alongwith High Blood Pressure and was
discharged on 06.06.2016. Age of Smt. Pramila Dwivedi is about 75 years.
Claim was made for Rs.14124/- which was repudiated under Condition No:1.5 (Note-2) of the policy
which reads as under :
“Charge incurred at Hospital or nursing home primarily for diagnosis, x-ray or laboratory
examinations or other diagnostic studies not consistent with or incidental to the diagnosis and
treatment of positive existence of presence of any ailment, sickness or injury for which
confinement is required at a hospital/nursing home.
Complainant submits that his wife is aged about 75 years. She got complaint of blood pressure and
vertigo, concerned doctor after check up, advised her for admission in the hospital. It is submitted that
he acted upon the advice of the doctor. Respondent representative submits that the hospitalization was
not at all necessary as only oral medicines were given.
Age of the patient was about 75 years. She was having actue problem of vertigo and high blood pressure
wherein doctor advised her for hospitalization. Respondent has not filed any counter information of any
doctor which says that in such a case, there was no need of hospitalization.
Today complainant has submitted photo copy of the Bed Head Ticket which further shows, the
genuineness of the claim of the complainant. There is nothing on record submitted by the insurer that
there was no necessity of need for hospitalization.
In such circumstances, I am of the view that Smt. Pramila Dwivedi was admitted in the hospital under
the advice of doctor, complainant is entitled for the claim in accordance with rules, terms and conditions
of the policy. Complainant is also entitled for interest @ 6% from the date of the claim is made till the
date of actual payment.
Accordingly, complaint is allowed. Respondent are hereby directed to process the claim and make the
payment in accordance with the policy bond alongwith interest @ 6% within a period of 30 days.
22. Let a copy of award be given to both the parties.
Dated : December 2, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr Abhishek Kumar Chopra…………..……....………………. Complainant
V/S
United India Insurance Co. Limited…………..………..…………Respondent
COMPLAINT NO. LCK-G-051-1819-0033 ORDER NO. IO/LCK/A/GI/0085 /2019-20
1.
Name & Address of the Complainant
Mr. Abhishek Kumar Chopra,
11/M/9, Dabouli, Kanpur Urban, Kanpur (U.P.)
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
0808022817P103122407
Family Medicare Policy
10.06.2017 to 09.06.2018
3.
Name of the life insured
Name of the policyholder
Mr. Abhishek Kumar Chopra.
Mr. Abhishek Kumar Chopra.
4.
Name of the insurer
United India Insurance Co. Ltd.
5.
Date of Repudiation/Rejection
-
6.
Reason for repudiation/Rejection
-
7.
Date of receipt of the Complaint
04.05.2018
8.
Nature of complaint
Partial repudiation of claim
9.
Amount of Claim
---

10.
Date of Partial Settlement
---
11.
Amount of relief sought
Rs. 41,492/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 02.12.2019 at Lucknow
14.
Representation at the hearing
For the Complainant
Mr. Abhishek Kumar Chopra
For the insurer
Mrs. Beena, Sr. Branch Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
02.12.2019
17. Complainant Sri Abhishek Kumar Chopra has filed a complaint against United India Insurance
Company Limited (Respondent) against partial settlement of his Medi-claim.
18. Brief Facts Of the Case:- The complainant, vide Annexure VI A has stated that he consulted
Dr. Neeraj Kumar of LPS Institute of Cardiology & cardiac Surgery on 17.09.2017 as outdoor patient.
He was having Varicose Vein of left lower limb for last two & a half years. As per Annex-VI A the
surgery was planned in September-2017 itself but the same was postponed as he developed
Cellulites & Venous Ulcer and as such, he was kept on medical management. He was then admitted
to the hospital on 08.12.2017 & discharged on 10.12.2017. The surgery for Laser Ablation was
performed during this period. However, during the intervening period the complainant purchased
medicine worth Rs.1,172/- & a medical device known as Elves Radial Kit worth Rs.40,320/- totaling a
sum of Rs.41,492/- Since, these items were purchased 30 days prior to the date of hospitalization
these items were not approved by RIC out of the total amount claimed i.e. Rs.59,699/-. Aggrieved
with the decision of Respondent the complainant approached this Forum.
In their SCN/Reply, Lucknow Regional Office of RIC has stated that Rs. 40,320/- bill dated
18.09.2017 and Rs. 1,172/- bill dated 17.09.2017 for medicine charges pertain prior to the 30 days
from the date of admission(08.12.2017),hence, not payable. As per policy clause 3.30 Pre-
hospitalization medical expenses incurred immediately 30 days before the insured person is
hospitalized provided that:
a. Such medical expenses are incurred for the same condition for which the insured person’s
hospitalization was required.
b. The inpatient hospitalization claim for such hospitalization is admissible by the insurance
company.
19. The complainant has filed a complaint, correspondence with the respondent. Annexure-VIA duly
filled/signed submitted by the complainant while respondent has filed an incomplete SCN along with
enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as
well as the insurance company.
21. There is no dispute that the complainant Mr. Abhishek Kumar Chopra was operated upon for
Vericosity Bilateral Lower Limb on 08.12.2017 at LPS Institute of Cardiology & Cardiac Surgery,
Kanpur. One “LC01 Elves Radial Kit A” was purchased on 18.09.2017. Claim was filed for Rs.59699/-.
Claim of Rs.18207/- was allowed while Rs.41492/- was disallowed as per Condition No: 3.30 of the
policy bond which reads as under :
“Pre-hospitalization medical expenses, relevant medical expenses incurred immediately 30
days before the insured person’s hospitalized provided that :
a.such medical expenses are incurred for incurred for the same conditions for which the
insured person’s hospitalization was required and.
b.the in-patient hospitalization claim for such hospitalization is admissible by the insurance
company.”
Complainant submits that with all bonafides, he had purchased laser fibre but the operation was
postponed for 08.12.2017. A certificate to this effect was also issued by the concerned doctor.
Prescription shown to me by the complainant shows that medicine for seven days were prescribed on
17.09.2017 thereafter the complainant approached the concerned doctor on 08.12.2017.
In such circumstances, when even the operation was not scheduled why the instrument was
purchased on 18.09.2017. However, even it was purchased, the claim can not be granted and
allowed in view of Condition No: 3.30 of the policy bond.
Certificate of the doctor did not find support from the prescription. Further no document showing the
scheduled date of operation within a month from 18.09.2017 could not be produced by the
complainant.
Accordingly complaint lacks merit and liable to be dismissed.

22. Complaint filed by Mr. Abhishek Kumar Chopra stands dismissed.
23. Let copy of award be given to both the parties.
Dated : December 02, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Rakesh Agarwal…………..……....………………. Complainant
V/S
United India Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-051-1819-0063 Order No. IO/LCK/A/GI/0095/2019-20
1.
Name & Address of the Complainant
Mr. Rakesh Agarwal,
House No:293, Sector-18,
Indira Nagar, Lucknow-226016
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
5001002816P110321838
Tailormade Group Mediclaim Policy
01.10.2016 to 30.09.2017
3.
Name of the life insured
Name of the policyholder
Indian Overseas Bank employees, spouse etc.
IBA M/s Indian Banks Association
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of Repudiation/Rejection
---
6.
Reason for repudiation/Rejection
---
7.
Date of receipt of the Complaint
31.07.2018
8.
Nature of complaint
Delay in settlement of claim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
--
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 10.12.2019 at 10.15 am at Lucknow
14.
Representation at the hearing
For the Complainant
Mr. Rakesh Agarwal
For the insurer
Mrs Monika Nishal
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
10.12.2019
17. Mr. Rakesh Agarwal (Complainant) has filed a complaint against United India Insurance Company
Limited (Respondent) alleging delay in settlement of health claim of his wife.
18. Brief Facts Of the Case:- The complainant has stated that his wife was admitted in Shekhar Hospital
Pvt. Ltd., Lucknow for the treatment of DM with HTN. The patient was hospitalized during the period from
10.06.2017 to 12.06.2017. The claim was submitted for reimbursement to the concerned TPA/RIC
amounting to Rs.14850. Since the claim was not settled for a long time, the complainant approached
the grievance cell of the respondent but no resolution was provided by the RIC. Aggrieved with such
unjustified delay, the complainant approached this forum.
In their SCN/reply dated 06.12.2019, RIC has stated that they have settled the claim for Rs.11,750/-
(Net) after deducting an amount of Rs.3,100/- from the total claimed amount of Rs.14,850/-. The
amount of Rs.11,750/- was paid to the insured account in time which bounced back. Once again the
amount was disbursed but in vain. The respondent has further stated that they are ready to pay the
amount in bank’s corporate account after taking confirmation from the insured.

19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures on the date of hearing.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
21. There is no dispute that the insured’s wife was admitted for treatment of [Surgical] Dm with Htn in
Shekhar Hospital, Lucknow. Total hospitalization charges were Rs,14850/-. Claim was processed and
settled for Rs.11750/- but could not be paid due to in correct bank details Respondent representative
submits that the company is still prepared to make the payment.
Complaint is disposed off with a direction to the complainant to send his correct complete bank details
to the insurance company. On receipt of the bank details company shall make the payment of
Rs.11750/- within 15 days.
22. Let copy of the award be given to both the parties.
Dated : December 10, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mrs. Moni Bahen Patel…………..……....………………. Complainant
V/S
United India Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-051-1819-0067 Order No. IO/LCK/A/GI/0097/2019-20
1.
Name & Address of the Complainant
Mrs. Mony Bahan Patel
Shiv-11/14 , A-9 Patel Nagar Colony
Shivpur Varanasi -221003
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
500100/48/15/41/00000481
Group Mediclaim Policy
01/11/2015 to 30.09.2016
3.
Name of the life insured
Name of the policyholder
Smt. Moni Bahan Patel
IBA A/c Union Bank of India
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of Repudiation/Rejection
20.06.2018
6.
Reason for repudiation/Rejection
claim was submitted after 30 days from discharge
7.
Date of receipt of the Complaint
30.07.2018
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
---
10.
Date of Partial Settlement
---
11.
Amount of relief sought
---
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 10.12.2019 at 10.15 am at Lucknow
14.
Representation at the hearing
For the Complainant
Mr.Ajeet Kumar Singh
For the insurer
Mrs. Monika Nishal
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
10.12.2019
17. Mrs. Moni Bahan Patel (Complainant) has filed a complaint against United India Insurance Company
Limited (Respondent) alleging repudiation of her claim.
18. Brief Facts Of the Case:- The complainant has stated that she had submitted all her bill and necessary
documents for the reimbursement. She also stated that she could not submit the bill within the stipulated
time provided because her medical condition was not good. But her claim was repudiated by the
TPA/RIC under clause 5.5 of their policy. Aggrieved with the decision of the RIC, the complainant
approached this forum for her grievance.
In their SCN/reply RIC has stated that the above policy was issued as a group mediclaim policy to
Union Bank of India Employees and their dependents. The complainant was admitted for Primi Gravida
Term pregnancy and submitted documents indicate LSCS was administrated. The claim documents
were submitted after 347 days after discharge. As per terms and conditions of the policy all the
supporting documents related to the claim must be filed with the RIC within 30 days from the date of
discharge from the hospital. In the above complaint the claim documents were not submitted as per
prescribed limit and not even in time extension also provided to the bank employees.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures on the date of hearing.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
21. Complainant Smt. Mony Bahan Patel, is Asstt. Manager in Union Bank of India who submitted a
claim for reimbursement of her bill which were paid by him for Primigravida Term Pregnancy.
According to the documents, LSCS was administered to her. She was admitted in the hospital on
13.04.2016 and discharged on 18.04.2016. Thereafter she submitted her claim for the first time on
18.07.2017. Claim was repudiated under Clause No:5.5 of the policy bond which provides that the
claim should be submitted to either bank or TPA within 30 days from the discharge from the hospital.
Complainant representative submits that the complainant was on maternity leave for one year when
she joined then she came to know, claim is to be dealt by the Insurance company.
Respondent representative submits that bank has a limited role in the claim. Bank only forward the
claim papers to the respondent wherein it is scrutinized. However Condition No:5.5 of the policy bond
is very specific. Although delay may be condoned but that period too had expired. Condition No: 5.5 of
the policy bond is as under :
“All supporting documents relating to the claim must be filed with the office of the bank
dealing with the claims or Third Party Administrator within 30 days from the date of
discharge from the hospital. In case of post-hospitalization, treatment (limited to 90 days),
(as mentioned in para 2.32) all claims documents should be submitted within 30 days after
completion of such treatment.”
Claim papers were not submitted within the stipulated period hence the claim was rightly repudiated by
the respondent which did not require any interference.
Accordingly complaint lacks merit and liable to be dismissed.
22. Complaint filed by Mrs.Moni Bahan Patel stands dismissed.
23. Let copy of the award be given to both the parties.
Dated : December 10, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman

PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Ashok Kumar Pal…………..……....………………. Complainant
V/S
United India Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-051-1819-0073 Order No. IO/LCK/A/GI/0099/2019-20
1.
Name & Address of the Complainant
Mr. Ashok Kumar Pal
394, Nai Basti
Barra-II , Kanpur-208012
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
08080228117P113867660
Family Medicare Policy
29.12.2017 to 28.12.2018
3.
Name of the life insured
Name of the policyholder
Mr. Ashok Kumar Pal & Smt. Laxmi Devi
Mr. Ashok Kumar Pal
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of Repudiation/Rejection
---
6.
Reason for repudiation/Rejection
---
7.
Date of receipt of the Complaint
16.08.2018
8.
Nature of complaint
Delay in settlement of claim
9.
Amount of Claim
---
10.
Date of Partial Settlement
---
11.
Amount of relief sought
---
12.
Complaint registered under Rule
Rule No. 13(1)(a) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 10.12.2019 at 10.15 am at Lucknow
14.
Representation at the hearing
For the Complainant
Mr.Ashok Kumar Pal
For the insurer
Mrs Beena Tripathi, Branch Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
10.12.2019
17. Mr. Ashok Kumar Pal (Complainant) has filed a complaint against United India Insurance Company
Limited (Respondent) alleging delay in settlement of health claim of his wife.
18. Brief Facts Of the Case:- The complainant has stated that he had lodged a claim with the TPA on the
above policy on 02.02.2018 for treatment of his wife. He had sent the intimation to the RIC regarding the
above claim but he had not received any reply for the TPA/RIC. Since the claim was not settled, the
complainant approached this forum for his grievance.
In their SCN/reply RIC has stated that the above policy was issued to the complainant and his wife for the total
sum insured of Rs. 1,50,000/-. The complainant had lodged a claim for the treatment related to Osteoarthritis
both knees of his wife. His wife was hospitalized at Satya Trauma & Maternity Centre, Kanpur from 02.01.2018 to
04.01.2018 and underwent injection Hyaluronic acid in both knees. The total reimbursement claim was lodged for
Rs. 43,305/- . Based on the above bills & submitted documents (IPD papers) it was observed that this
management does not require confinement in the hospital and could be managed in OPD also. It was further
observed that OPD management being converted into IPD. Here the patient not admitted in hospital only for
Intra articular injection, which is neither covered in day care procedure list nor does it require 24 hours
hospitalization.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and copy of
policy document while respondent filed SCN with enclosures on the date of hearing.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as well as the
Insurance Company.
21. Smt. Laxmi Devi wife of the complainant was admitted in Satya Trauma and Maternity Centre, Kanpur on
02.01.2018 and discharged on 04.01.2018. It was alleged, she was having some pain in both the knees due to
arthritis. As per diagnosis, it was a case of Osteoarthritis. After admission, only injection was administered to her.

Claim was repudiated on the ground that the hospitalization was not required. It was a case of OPD which was
converted into indoor patient. Bed Head Ticket and prescription subsequently shows that no treatment was
given which needs hospitalization. Even during the hospitalization, no regular monitoring was done by the
medical team of the nursing home.
In such circumstances, claim of the claimant has rightly been repudiated by the respondent which did not require
any interference. Accordingly complaint is devoid of merit and is liable to be dismissed.
22. Complaint filed by Mr. Ashok Kumar Pal stands dismissed.
23. Let copy of award be given to both the parties.
Dated : December 10, 2019 ( Justice Anil Kumar Srivastava )
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Narendra Kumar Shukla…………..……....………………. Complainant
V/S
Star Health & Allied Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-044-1819-0102 ORDER NO. IO/LCK/A/GI/0105/2019-20
1.
Name & Address of the Complainant
Mr. Narendra Kumar Shukla
Village – Kachvachiya Kalan Post – Asan
Distt- Ballia-277302
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
P/161111/01/2018/01213
Family Health Optima Insurance Plan
14.11.2017 to 13.11.2018
3.
Name of the life insured
Name of the policyholder
Mr. Narendra Kumar Shukla
4.
Name of the insurer
Star Health & allied Insurance Company Limited
5.
Date of Repudiation/Rejection
04.09.2018
6.
Reason for repudiation/Rejection
Treatment taken under OPD
7.
Date of receipt of the Complaint
09.10.2018
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
---
10.
Date of Partial Settlement
---
11.
Amount of relief sought
---
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 18.12.2019 at 11.00 am at Lucknow
14.
Representation at the hearing
For the Complainant
Mr. Narendra Kumar Shukla
For the insurer
Mr. C.S.Tandon
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
18.12.2019
17. Mr. Narendra Kumar Shukla (Complainant) has filed a complaint against Star Health & Allied Insurance
Company Limited (Respondent) alleging repudiation of his daughter’s health claim.
18. Brief Facts Of the Case:- Complainant has stated that his daughter wad admitted in Panacea Hospital,
Varanasi on 11.08.2018 with a complaint of abdominal pain, back pain, lower limb and treated for
constitutional delay of growth and puberty and discharged on 11.08.2018. He submitted a claim bill of
Rs.8290/- to RIC for its reimbursement but my claim was rejected by the RIC on the ground of false and

fabricated grounds. He approached GRO of RIC on 10.09.2018. Aggrieved with the decision of RIC,
complainant had approached this forum.
In their SCN/reply, RIC has submitted that insured has submitted the claim records for reimbursement of medical
expenses. On scrutiny of the submitted medical records, it is observed that insured patient has taken treatment as
on outpatient and not as an in-patient in the hospital. As per the terms and conditions of the policy, the expenses
towards inpatient is only payable. Thus the claim was repudiated and the same was informed to the insured vide
letter dated 03.09.2018.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and copy of
policy document while respondent filed SCN with enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as well as the
Insurance Company.
21. Admitted, insured’s daughter was not admitted in the hospital rather she was conventionally treated by the
doctor. As per policy condition, such type of treatment is not covered under the policy.
Hence the claim beyond the scope of the policy, claim has rightly been repudiated by the respondent company.
Accordingly complaint lacks merit and liable to be dismissed.
22. Complaint filed by Mr. Narendra Kumar Shukla stands dismissed.
23. Let copy of award be given to both the parties.
Dated : December 18, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Narendra Kumar Shukla…………..……....………………. Complainant
V/S
Star Health & Allied Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-044-1819-0169 ORDER NO. IO/LCK/A/GI/0109/2019-20
1.
Name & Address of the Complainant
Mr. Narendra Kumar Shukla
Village – Kachvachiya Kalan Post – Asan
Distt- Ballia-277302
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
P/161111/01/2018/01213
Family Health Optima Insurance Plan
14.11.2017 to 13.11.2018
3.
Name of the life insured
Name of the policyholder
Mr. Narendra Kumar Shukla
Mr. Narendra Kumar Shukla
4.
Name of the insurer
Star Health & allied Insurance Company Limited
5.
Date of Repudiation/Rejection
04.12.2018
6.
Reason for repudiation/Rejection
Due to pre-existing disease
7.
Date of receipt of the Complaint
24.01.2018
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
---
10.
Date of Partial Settlement
---
11.
Amount of relief sought
---
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 18.12.2019 at 11.00 am at Lucknow
14.
Representation at the hearing
For the Complainant
Mr. Narendra Kumar Shukla
For the insurer
Mr. C. S. Tandon
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
18.12.2019

17. Mr. Narendra Kumar Shukla (Complainant) has filed a complaint against Star Health & Allied Insurance
Company Limited (Respondent) alleging repudiation of his health claim.
18. Brief Facts Of the Case:- Complainant has stated that he was insured with health insurance from
respondent from 13.11.2017 to 12.11.2018. He had taken eye treatment in Indira Gandhi Eye Hospital from
and submitted all the claim documents for medical reimbursement for Rs. 49,975/- with the respondent.
After one month the claim was rejected on 05.12.2018 on baseless ground. He further stated that he is
aggrieved due to rejection of his claim. Aggrieved with the decision of RIC, complainant had approached
this forum.
In their SCN/reply, RIC has submitted that insured was diagnosed as a case of retinal detachment. The
complainant has submitted the claim records for reimbursement of medical expenses on . On scrutiny
some queries were raised and some more documents were also asked to submit. The complainant had
replied their query on 24.11.2018. On scrutiny of the claim documents , it is observed that the
consultation report dated 23.12.2017 reveals that the insured patient was a known case of Type-II Diabetes
Mellitus for the past four years and Hypertension for past three months which is prior to the inception of
the policy. The present admission and treatment of the insured patient was for the complications of pre-
existing Diabetes Mellitus. Hence, the claim was repudiated under waiting period no. 3(iii) of the policy
vide letter dated 04.12.2018.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as well as
the Insurance Company.
21. Claim was repudiated on the ground that the insured is known case of Diabetic Mellitus prior to inception of the
policy. Further claim has been put within 4 years of the policy which is not payable as per Exclusion No.1 of the
policy bond.
Complainant has not submitted any documents related to the admission in Indira Gandhi Eye Hospital. No inpatient
summary or discharge card is filed. Those documents were also called by the respondent on 12.11.2018 but were
not submitted by the complainant.
As per prescription dated 23.12.2017 submitted vide earlier claim 542497/2018, the insured patient was a known
case of Type II diabetes mellitus for past four years and hypertension for past three months which is prior to the
first date of inception of the policy. Therefore it was noted that the insured had pre-existing Diabetes mellitus. and
the present admission and treatment of the insured patient for the complications of pre-existing Dibetes Mellitus.
Thus as per waiting period 3(iii) of policy, Pre-Existing Disease was not covered until 48 months of continuous
coverage.
Having submission of the parties, I am of the view that the insurer has rightly repudiated the claim of the
complainant.
Accordingly complaint lacks merit and is dismissed.
22. Let copy of award be given to both the parties.
Dated : December 18, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman

PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, LUCKNOW
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr. Ram Sumer Gupta…………..……....………………. Complainant
V/S
Oriental Insurance Company Limited…………..………..…………Respondent
COMPLAINT NO:LCK-G-050-1819-0131 Order No. IO/LCK/A/GI/0106/2019-20
1.
Name & Address of the Complainant
Mr. Ram Sumer Gupta
537 B 5/91 , Faizullaganj
Sitapur Road Lucknow
2.
Policy No:
Type of Policy
Duration of policy/DOC/Revival
221301/48/2018/1748
PNB Oriental Royal Mediclaim policy
24.09.2017
3.
Name of the life insured
Name of the policyholder
Mr. Ram Sumer Gupta & his family members
Mr. Ram Sumer Gupta
4.
Name of the insurer
Oriental Insurance Company Limited
5.
Date of Repudiation/Rejection
12.10.2018
6.
Reason for repudiation/Rejection
Under exclusion clause 4.7
7.
Date of receipt of the Complaint
30.10.2018
8.
Nature of complaint
Repudiation of health claim
9.
Amount of Claim
---
10.
Date of Partial Settlement
---
11.
Amount of relief sought
---
12.
Complaint registered under Rule
Rule No. 13(1)(b) of Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 18.10.2019 at 11.00 am at Lucknow
14.
Representation at the hearing
For the Complainant
Mr. Ram Sumer Gupta
For the insurer
Mrs.Shalini Pawah, Branch Manager
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
18.12.2019
17. Mr. Ramsumer Gupta (Complainant) has filed a complaint against Oriental Insurance Company
Limited (Respondent) challenging the repudiation of health claim of his wife.
18. Brief Facts Of the Case:- Complainant has stated that he had taken a mediclaim policy from the
respondent and he along with his family were covered since 2015. His wife was admitted on
25.07.2018 in hospital. After discharge from the hospital all the claim documents were also submitted
to the respondent for reimbursement. On checking the status of claim on TPA site, he came to know
about rejection of claim. He further stated that in rejection letter, the diagnosis was written as Anxiety
Disorder Unspecified. In this regard he had also sent the Doctor’s certificate to the TPA/RIC. His claim
was opened & reviewed but he had received the no claim letter from the TPA/RIC. Aggrieved with the
decision of the respondent, complainant approached this forum for his grievance.
In their SCN/reply, RIC has submitted the copy of the proposal form, policy schedule with conditions,
copy of repudiation letter with copy of claim documents along with self contained note. It is stated that
on reviewing the claim documents it was noted that the patient was admitted as a case Genralised
Anxiety Disorder (GAD) with post Hysterectomy pain and was managed conservatively and discharged.
As per terms and conditions of the policy the claim was repudiated as per clause no 4.7 as treatment
was related with Psychiatric & Psychosomatic disorder. These ailments are excluded from the scope of
the policy. On the submission of the certificate of the doctor the claim was again reviewed and it was
noted that now the diagnosis was changed and the patient had not visited the same doctor/surgeon
who had operated her for Hysterectomy. So the claim was again recommended for repudiation by the
TPA.
19. The complainant has filed a complaint letter, annexure VI A, correspondence with respondent and
copy of policy document while respondent filed SCN with enclosures.
20. I have heard both the parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.

21. Initially claim for surgery of hysterectomy of the insured was paid by the insurer. When she
developed some problem, she was again admitted in Harsha Hospital on 25.07.2018 and was
discharged on 01.08.2018. Doctor has specifically mentioned in the discharge card that the diagnosis is
“GAD with Post Hysterectomy Pain”. Due to one or other reasons when TPA has disallowed the claim.
Insured obtained two certificates from the hospital which were issued by the hospital as well as Head
of the Hospital specifically mentioning that the insured was suffering from Generalised Anxiety Disorder
with Post Hysterectomy pain. No doubt, psychiatric and psychosomatic disorder are covered under
Exclusion Clause but in the present case, the proximate cause of the ailment is post hysterectomy pain.
Due to this reason, insured remained admitted in the hospital for about 8 days. Claim has wrongly
been repudiated considering the fact that it is a case of psychiatric and psychosomatic disorder which
did not find support from the medical record of the insured.
Having considered the submissions, I am of the view that claim has been wrongly repudiated by the
insurer. Complaint is liable to be allowed.
Order :
Complaint is allowed. Respondent is directed to make the payment of the claim to the complainant
alongwith interest @ 8% per annum from the date of claim till the date of actual payment within a
period of 30 days.
22. Let copy of award be given to both the parties.
Dated : December 18, 2019 (Justice Anil Kumar Srivastava)
Place : Lucknow Insurance Ombudsman
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF RAJASTHAN
UNDER THE INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – MS. SANDHYA BALIGA
CASE OF MR. NITESH M CHOPRA V/S HDFC ERGO GENERAL INSURANCE CO. LTD.
COMPLAINT REF: NO JPR-G-018-1920-0220
AWARD NO: IO/JPR/G/A/1920/00
1.
Name & Address of the Complainant
Mr. Nitesh M Chopra, Jaipur
2.
Policy No:
Type of Policy
Duration of policy/Policy period
SUM INSURED
282510044968600000
Health Suraksha Policy
09.05.2019 to 08.05.2020
Sum Insured Rs. 4 lakh
3.
Name of the insured
Name of the policy holder
Mr. Nitesh M Chopra
Mr. Nitesh M Chopra
4.
Name of the insurer
HDFC Ergo General Insurance Co. Ltd.
5.
Date of Repudiation
02.09.2019
6.
Reason for repudiation
Falls under exclusion-PED Sec 9 a (iii)
7.
Date of receipt of the Complaint
21.10.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.225000/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs 225000/-
12.
Complaint registered under
Rule no: of IOB rules
13 i (b)
13.
Date of hearing/place
10.12.2019/ Jaipur
14.
Representation at the hearing
For the Complainant
Mr. Nitesh Chopra
For the insurer
Mr. Digvijay Singh, Manager, Consumer
15
Complaint how disposed
Award
16
Date of Award/Order
10.12.2019
17) Mrs. Nitesh Chopra (herein after referred to as the complainant) had filed a complaint
against the decision of HDFC Ergo General Insurance Co. Ltd.(Jaipur) (herein after referred to as
the respondent Insurance Company) alleging repudiation of hospitalisation claim.
18) Cause of Complaint:
Complainant’s argument: :- The complainant Sh Nitesh Chopra had taken a Health Suraksha
Policy(Silver Plan) 282510044968600000 wef 09.05.2019 to 08.05.2020 for the Sum Insured of
Rs.4 Lakh covering the complainant his spouse and dependant child, from the respondent company
HDFC Ergo General Insurance Co. Ltd. The complainant Sh Nitesh M Chopra was admitted to

Advance Knee and Shoulder Hospital, Ahmedabad on 25.07.20019 and discharged on 26.07.2019
and was diagnosed ACL tear R knee with chondral injury with lateral meniscal injury. The
Complainant stated that he filed a claim towards hospitalization expenses for Rs. 2,25,000 /-, the
same was repudiated by the Insurance Company. The submitted that discharge summary bear h/o fall
from bike on 19.06.2019 and no h/o alcohol abuse, no MLC/FIR. The case was registered with Police
authorities and the DDR was lodged. Aggrieved, he requested the insurer, including its GRO to
reconsider the claim but failed to get any relief. Thereafter, he preferred a complaint to this office for
resolution of his grievance.
Insurers’ argument:- The insurer stated in their SCN dated 30.10.2019 received on 29.11.2019
that the insured patient Mr. Nitesh M Chopra was admitted and treated for ACL tear with meniscal
Tear Right Knee. The claim was investigated and on perusal of treatment record and investigation
report the claim was repudiated as per policy terms and conditions. On verification of MRI report
dated 29.06.2017, the patient was diagnosed with ACL tear with a meniscal tear Right Knee, the
ailment was preexisting in nature and the insured had not disclosed the said ailment while purchasing
the policy on 09.05.2019, there was non disclosure of material fact and thus the claim was repudiated
under Section 9 a (iii )of policy terms and conditions.
19) Reason for Registration of Complaint: - Case of Non settlement of claim
20) The following documents were placed for perusal.
a) Complaint letter
b) Policy copy, repudiation letter,
c) Discharge Summary
d) Form VI A duly signed by the complainant.
e) SCN and a form VIIA duly signed by the Insurance Company
21) Results of hearing with both parties (Observations and Conclusion):- Both the parties
appeared in the personal hearing and reiterated their submissions. The complainant submitted that
he met with an accident on 19.07.2019 and had ACL tear and was operated on 25.07.2019 at
Ahmedabad. He submitted that he also lodged a DDR is detailing the facts of the incident. The
Insurance Company stated that the insured as per MRI report dated 29.06.2017 the patient
already had ACL tear and the ailment was preexisted at the time of proposal from. The policy
incepted from 09.05.2019 and the date of accident as per discharge summary was 19.06.2019.
The claim was repudiated on account of non disclosure of the medical condition at the time of the
issuance of the policy.
I have perused the documents placed on record and submissions during the hearing. I find that as
per discharge summary the patient had the history of fall from bike on 19.06.2019. The
complainant submitted a certificate from the treating doctor that the date of the accident was
19.07.2019 and he had Right knee injury and the injury was with the slip from bike. The
complainant admitted that in the yar 2017 he had a ACL sprain while playing football and MRI
was done. I find that as per MRI dated 29.06.2017, there was Mildly lox ACL with low grade
sprain of ACL close to femoral attachment. He also submitted that he was a regular player and
had played a tournament before the injury sustained in the accident. I find that it was not a case
of pre existing ailment to the insured at the time of the issuance of the policy. In view of the facts
and circumstances, I direct the Insurance Company to settle the claim as admissible.
Accordingly, an Award is passed with the direction to settle the claim as admissible.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties during the course of hearing, the Insurance Company is directed to settle the claim as
admissible.
The complaint is treated as disposed off accordingly.

22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. According to Rule 17(5) of Insurance Ombudsman Rules, 2017, A copy of the award
shall be sent to the complainant and the insurer named in the complaint.
b. As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30
days of the receipt of the award and shall intimate the compliance to the Ombudsman.
Place: Jaipur SANDHYA BALIGA
Dated: 10.12.2019 INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF RAJASTHAN
UNDER THE INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – MS. SANDHYA BALIGA
CASE OF RAJESH MAHESHWARI V/S THE NEW INDIA ASSURANCE CO. LTD.
COMPLAINT REF: NO JPR-H-049-1920-0218
AWARD NO: IO/JPR/HI/A/1920/00
1.
Name & Address of the Complainant
Rajesh Maheshwari, Jaipur
2.
Policy No:
Type of Policy
Duration of policy/Policy period
IDV
33170034182800001117
New India Floater Insurance
04.09.2018 to 03.09.2019
Rs. 5 lakh
3.
Name of the insured
Name of the policyholder
Ms. Seema maheshwari (Wife)
Rajesh Maheshwari
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
02.09.2019
6.
Reason for repudiation
Maternity expenses not covered
7.
Date of receipt of the Complaint
05.11.2019
8.
Nature of complaint
non Settlement of health claim
9.
Amount of Claim
Rs.30544/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs 30544/-
12.
Complaint registered under
Rule no: of IOB rules
13 i (b)
13.
Date of hearing/place
10.12 .2019/Jaipur
14.
Representation at the hearing
For the Complainant
Mr. Rajesh Maheshwari and Mrs. Seema
Maheshwari
For the insurer
Sh. Vijay Prakash Sharma SDM Dr. Deepak Vyas
AO, Medical
15
Complaint how disposed
Dismiss
16
Date of Award/Order
10.12.2019
17) Mrs. Rajesh Maheshwari (herein after referred to as the complainant) had filed a
complaint against the decision of The New India Assurance Co. Ltd.(Jaipur) (herein after
referred to as the respondent Insurance Company) alleging non settlement of medical expenses
reimbursement claim.
19) Cause of Complaint:
Complainant’s argument: Mr. Rajesh Maheshwari, had New India Floater Mediclaim policy
no 33170034182800001117 for the period from 04.09.2018 to 03.09.2019 for the Sum Insured
of Rs.5 lakh covering self and his family(spouse and one child) from The New India Assurance
Co. Ltd.. The Complainant stated in his complaint letter that his wife Mrs. Seema Maheshwari
was hospitalized at the KMS Hospital, Jaipur for the period from 15.06.2019 to 16.06.2019
with diagnosis c/o Amen 11/2/12 wants a termination. The patient was h/o RA on MTX and
undergone MTP. A claim bill for Rs.30000/- towards treatment was raised, but the Insurance
Company repudiated the claim. The complainant submitted that his wife, Mrs. Seema was
chronic patient of Rheumatoid Arthritis from last more than 15 years and her haemoglobin level
remains below normal as per Doctor’s advice it was risky to give a birth to a child in this
condition. As per Gynaecologist’s advice they decided for MTP. Aggrieved, he requested the
insurer, including its GRO to reconsider the claim but failed to get any relief. Thereafter, he
preferred a complaint to this office for resolution of his grievance.

Insurers’ argument:- The insurer stated in their SCN dated 22.11.2019 that Mrs. Seema
Maheshwari the spouse of Mr. Rajesh Maheshwari was admitted in K M S Hospital , Jaipur
from 15.06.2019 to 16.06.2019 and had undergone MTP for eugenic reason. The termination of
pregnancy was done at the desire of the patient and the patient was discharged on 16.06.2019. As
per policy terms and conditions and as per policy exclusion clause 4.4.13, the claim was not
tenable. The clause 4.4.13 reads maternity expenses, treatment arising out of pregnancy,
miscarriage, abortion or complication…. Except life threatening one if left untreated.
19. Reason for Registration of Complaint: - Case of non settlement of claim
20) The following documents were placed for perusal.
f) Complaint letter,
g) Policy copy schedules and conditions,
h) Discharge Summary KMS Hospital,
i) Form VI A duly signed by the complainant.
j) SCN and a form VIIA duly signed by the Insurance Company
22) Result of hearing with both parties (Observations and Conclusion):- Both the parties
appeared in the personal hearing and reiterated their submissions. The complainant submitted
that his wife had history of Rheumatic arthertitis and at the advise of the doctor (eugenic
reason)on dated 14.06.2019 she had MTP at KMS hospital Jaipur. The complainant
submitted that as per condition of his wife he resorted MTP. The Insurance Company
submitted that hospitalization was done primarily for MTP and as per discharge summary the
patient wants MTP. There as no medical emergency and no life threatening pregnancy. As
per policy condition maternity expenses, except abdominal operation …. except life
threatening one if left untreated, as per exclusion clause 4.4.13 of the policy.
I have considered the documents placed on the record and submissions made during the
personal hearing. As per the doctor’s certificate dated 14.06.2019, patient on MTX , MTP
for Eugenic reason. As per Discharge summary dated 15.06.2019 the patient wants
termination. I find that as per policy exclusion clause 4.4.13, No claim will be payable under
the policy for the maternity expenses, treatment arising from or traceable to pregnancy,
miscarriage, abortion or complications: except abdominal operation for extra uterine
pregnancy (ectopic pregnancy) which is proved by submission of Ultra Sonographic report
and certification by Gynaecologist that it was life threatening one if left untreated. The
instant case does not fall under the said category.
In view of the facts and circumstances, I find no reason to interfere with the impugned
order. The complaint is dismissed.
Accordingly, the complaint is hereby dismissed.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the complaint is hereby dismissed.

22. The attention of the Complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rules, 2017:
According to Rule 17(5) of Insurance Ombudsman Rules, 2017, A copy of the award shall
be sent to the complainant and the insurer named in the complaint.
Place: Jaipur. SANDHYA BALIGA
Dated: 10.12.2019 INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, GUWAHATI
(UNDER RULE NO: 16(1)/17 of INSURANCE OMBUDSMAN RULES 2017)
OMBUDSMAN – K.B. SAHA
CASE OF: : Complainant DR.HARI CHARAN MEDHI VS THE UNITED INDIA INSURANCE CO.LTD.
COMPLAINT REF NO: GUW-H-051-1920-0102 : Award No
1.
Name & Address of the Complainant
DR HARI CHARAN MEDHI
C/O GREENLAND NURSING HOME,VIP ROAD,
GUWAHATI-781015, ASSAM.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
1301062818P114703080 ; SI Rs 3,00,000/-
INDIVIDUAL HEALTH POLICY.
12months/12.02.2019 to12.02.2020
3.
Name of the insured
Name of the policyholder
MRS GIRIZA MEDHI
DR HARI CHARAN MEDHI
4.
Name of the insurer
THE UNITED INDIA INSURANCE CO.LTD.
5.
Date OF OCCURANCE OF LOSS/CLAIM
24.02.2018
6.
DETAILS OF LOSS
The Insured Mrs Giriza Medhi, age about 68 years old
had fallen sick and was admitted at Hayat
Hospital,Guwahati on 24.02.2019.The patient was
diagnosed with sick sinus syndrome, HTN,
Hypothyroidism. The consultant cardiologist advised
her for emergency PPI(PERMANENT PACEMAKER
IMPLANT).Her PPI was done on 25.02.2019 and she
was discharged on 01.03.2019.Insured had incurred
medical expenses for Rs 2,24,253/-.
7.
REASON FOR GRIEVANCES
It is alleged that in spite of submission of all
documents, the company has repudiated the claim
under clause 4.1 of the policy conditions and hence,
the aggrieved party has escalated this grievance.
8.a
8.b
Nature of complaint
Date of receipt of the complain
Dissatisfaction for repudiation of claim and hence the
Insured has complained for natural justice.
9.
Amount of Claim
Rs 2,24,253/-
10.
Date & Amount of Partial Settlement
N/A.
11
Amount of relief sought
Rs 2,24,253/-
12.
Complaint registered under
Rules of Insurance Ombudsman 2017
13(1)(b)
13.
Date of hearing/place
On 23.12.2019 at O/O the Insurance OMBUDSMAN
Guwahati.
14.
Representation at the hearing
• For the Complainant
Dr Hari Charan Medhi.
• For the insurer
Mr Atual Chandra Barman
15
Complaint how disposed
Through personal hearing.
16
Date of Award/Order
23.12.2019
17) Brief Facts of the Case : The insured had the Individual Health policy ( sub type policy is senior citizen) with United India
Insurance co. Ltd ,Adabari Branch,Guwahati vide Policy no.1301062818P114703089 for period 12.02.2019 to 11.02.2020.It
was an old policy ,the 1st policy was incepted on 22.03.2007 and renewed up to 11.02.2020.The above policy was accepted
a with a gap of 9 months approx after expiry of immediate previous. Policy was taken for self and his wife Mrs Girija Medhi
was admitted at HAYAT Hospital,Guwahati on 24.02.2019 and done PPI on25.022019 and discharged on 01.03.2019. The
insured incurred medical bills for Rs 2,24,253/-. The bills with supporting documents were submitted at Insurance office but
the Insurer had repudiated claim under clause 4.1 of the policy condition i.e. for pre- existing disease.
18 ) Complainant’s argument: The Insured stated that he had submitted all the documents to claim settlement
authority TPA but the TPA/Insurer had repudiated the claim under clause 4.1 of policy condition. The Insured
has also stated that he is a regular health insurance policy holder and his first policy was incepted on 22.03.2007
and the last policy was issued on 12.02.2019. But due to some gaps of current policy with the previous policy,the
claim for his wife due to sick SINUS syndrome and with pre existing symptom HTN since 6 months prior to PPI
on 25.02.2019 was repudiated by the company under clause 4.1 condition of the policy. Insured has also stated
that in spite of submission of all the documents in time and ground for delay in renewal policy(company had not
sent renewal notice in time as alleged), the company has not considered his claim which is an unjustified, willful
and malicious act on the part of the INSURANCE COMPANY and hence prayed for proper justice .
18 b) Insurers’ argument: - The policy is required to be renewed within 30 days of expiry to have continuation
benefit under the policy but the policy was renewed after a gap of 9 months of last policy (which expired on
27.05.2018 but renewed on 12.02.2019).Exclusion clause no. 4.1 under the policy specifies that Pre- Existing

disease are excluded. In the instant case, Policy was renewed after a gap of approximately 9 months, the nature
of policy becomes as a fresh policy. The patient was diagnosed with Hyper-Tension six months before
hospitalization for treatment of sick sinus syndrome and hence, as per Exclusion condition no.4.1, the disease is
considered as Pre –existing disease. Therefore, the claim was repudiated the company.
19) Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules 2017 (Rule after proper
approval from honorable ombudsman13 (1) (b).
20) The following documents were placed for perusal.
a) Complaint letter
b) Annexure – VI A
c) Copy o the policy
d) Annexure VII A
e) S C N
Result of hearing with both parties (Observations & Conclusion):- Both the parties were called for hearing
on 23.12.2019. The complainant Dr Hari Charan Medhi was present and the insurer was represented by Mr. Atul
Chandra Barman.
DECISION
We have taken in to consideration the facts and circumstances of the case from the documentary as
well as verbal submission made by the claimant and discussion had with the Insurance Company’s
representative present in the hearing.
The policy was issued with the gap of 9 months approx with the immediate previous policy. As a result,
it has lost the continuity benefit of the policy. Hence, the disease suffered was treated as pre –existing
disease under clause 4.1 of the policy condition and not payable. The Insurer’s decision is fair as per terms
and conditions of the policy.
Hence, the complaint is treated as closed without any relief to the claimant.
Dated at- Guwahati 23rd Day of Dec. 2019.
K.B.Saha
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, GUWAHATI
(UNDER RULE NO: 16(1)/17 of INSURANCE OMBUDSMAN RULES 2017)
OMBUDSMAN – K.B. SAHA
CASE OF: : Complainant MS. PRANATI KAR VS SBI GENERAL INSURANCE CO. LTD.
COMPLAINT REF NO: GUW-H-040-1920-0103 : Award No
1.
Name & Address of the Complainant
MS PRANATI KAR
2.
Policy No:
Type of Policy
Duration of policy/Policy period
0000000006213672-02
SBI MEDICLAIM POLICY.
12 MONTHS / 09.04.2019 TO 07.09.2020.
3.
Name of the insured
Name of the policyholder
MS PRANATI KAR
MS PRANATI KAR
4.
Name of the insurer
SBI GENERAL INSURANCE CO. LTD.
5.
Date OF OCCURANCE OF LOSS/CLAIM
15.05.2019
6.
DETAILS OF LOSS
The Insured was suffering from age related Cataract
problem for both eyes and during first week of May
2018 she had visited Sri Sankardeva Nethralaya,
Guwahati for checkup and as per physician’s advise
her right eye cataract operation was done on
14.5.2018.Initially, the claim was not paid by Insurance
company as per exclusion clause no.1 but as per clause
no.7, the Hon’ble Ombudsman, Guwahati vide award
no.10/GUW/A/GI/0080/2018-2019 directed the
company to pay her claim and the same paid
accordingly. Again, the Insured got admitted at Sri
Sankardeva Nethralaya on 15.05.2019 and cataract
operation of her left Eye was done on the same day.
But this time also the Insurance company has rejected
her claim for Rs 33,153/- as per exclusion clause no.1
and hence, the Insured has prayed us vide letter dt.
12.12.2019 for natural justice.
7.
REASON FOR GRIEVANCES
Claim bill for her Right Eye cataract operation was paid
by the company as per clause no.7 of the policy( as per
award of Hon’ble Ombudsman) but next time when
the Insured had submitted claim bill for her cataract
operation of Left Eye dt.15.05.2019, the claim was
rejected by company. Therefore, the Insured has made

grievance for his claim.
8.a
8.b
Nature of complaint
Date of receipt of the complain
Complaint for rejection of her claim by the Insurance
company.
16.12.2019
9.
Amount of Claim
Rs 33,153/-
10.
Date & Amount of Partial Settlement
N/A.
11
Amount of relief sought
Rs33,153/-
12.
Complaint registered under
Rules of Insurance Ombudsman 2017
3( i)(b).
13.
Date of hearing/place
23.12.2019
14.
Representation at the hearing
• For the Complainant
Mr Sankar Lal Kar
• For the insurer
Mr Sanjibv Tripathi
15
Complaint how disposed
Through personal hearing.
16
Date of Award/Order
23.12.2019
17) Brief Facts of the Case- SBl Claim no.98453754 under group Health lnsurance
policy was registered towards reimbursement of expenses for medical treatment of
insured Mrs Pranati Kar,for age related Cataract with she had history of resistant pupil,
diabetes mellitus, hypertension, hypothyroidism, coronary artery bypass grafting etc.
Her left eye phacoemulsification with intraocular lens implantation was done at SRI
SANKARDEVA NETHRALAYA on 15.05.2019.She incurred expenses of Rs33,153/-.
On submission of the claim,lnsurance Co repudiated the claim on the ground of pre-
existing. But clause no 7 of the policy states as "it is hereby declared and agreed that
the exclusion clause no 1 of the exclusion stands deleted and insurer will pay the
expenses up to the limit and sub limit as mentioned in the schedule against the insured
persons.All other terms and conditions under the policy remain unaltered".
Complainant's argument: As per the advise of Dr. Harsha Bhattacharjee she was
admitted in Hospital on 15.05.2019 for PHACO +FIOL TECINS + VISCOT+ HOOK
Surgery of her left eye and was discharged on same day. She spent Rs33,153/- and
submitted the claim in time but insurance company vide letter dt 03.07.2019 informed
her regarding the repudiation of the claim for Pre Existence of disease. But as per policy
condition no.7 "it is hereby declared and agreed that the exclusion clause no 1 of the
exclusion stands deleted and insurer will pay the expenses up to the limit and sub limit
as mentioned in the scheduled against the insured persons all other terms and
conditions under the policy remain unaltered" so it is payable.
18) lnsurers' argument: - The Company has stated that the Insured had been admitted
in Hospital on 15.05.2019 for cataract operation but the first policy inception date is
27.03.2017.As per certificate of hospital dt.10.06.2019,the insured has age related
cataract since 3 years and diabetes mellitus since 20 years, which is pre-existing in
nature and current ailment is the complication of the same. As per terms of the policy
the expenses arising out of above ailment is not payable as pre-existing illness is not
covered under the policy exclusion clause 1 which states as benefits will not be
available for any condition, ailment or injury or related condition(s) for which insured has
been diagnosed, received medical treatment, had signs and/or symptoms, prior to
inception of the insured’s first policy, until 48 consecutive months have elapsed, after
the date of inception of the first policy with the insurer. This claim for hospitalization falls
beyond purview of policy coverage and hence not payable.
19) Reason for Registration of Complaint: -
from honorable ombudsman13 (1) (b). Scope of the lnsurance Ombudsman Rules 2017
(Rule after proper approval
20) The following documents were placed for perusal.
a) Complaint letter
b) Annexure Vll A
c) SCN
d)copy of the policy
e)Annexure Vll A
Result of hearing with the both parties (observation and conclusion):- Both the parties
were called for hearing on 23.12.2019.The complainant Mr Sankar Lal Kar (on behalf of
his wife) and Insurer was represented by Mr Sanjeev Tripathi.

DECISION
We have taken into account facts & circumstances of the case aside from Documentary as
well as Verbal submission made by both the parties during the course of hearing. As per the
hospital certificate diminision of vision for distance and near, duration is 2 years and gradually
worsening. Age -related cataracts duration is 3 years. Past medical history – Diabetes mellitus
duration is 20 years and open heart S/P done 2 years ago. However, simple mention of
duration as three years in certificate dt.10.06.2019 does not establish Pre Existence of disease
conclusively because,
(a) threre is no mention in the discharge summery nor is there any diagnosis to the effect
done earlier. At best it can be treated as logical assumption by the certifying doctor.
(b) The complainant persistently refuted having had any knowledge of cataract earlier to
consulting Shankardeva Netralaya.
(c) Since the patient is aged above 60 years ,DM AND Hypertension can not be treated as
directly responsible for causing cataract.It is more likely to be age related.
Hence in order to meet the end of Natural Justice, we have relied upon logical,
interpretation of the policy terms and conditions and hereby direct the insurance co. to
pay Rs.33,153/- (less mandatory deduction for non-payable items if any).
The complaint is thus treated as CLOSED.
The attention of the complaint and the insurer is hereby invited to the following
provisions of insurance ombudsman Rues,2017.
According to the Rules 17(6)of the said rules,2017 the insurer shall comply with the
Award within 30 days of the receipt of the award and shall intimate the compliance to
the same to the ombudsman.
K.B.Saha
INSURANCE OMBUDSMAN
Dated at Guwahati on the 23th day of Dec………2019.
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Narender Singh versus Religare Health Insurance Company Limited
Complaint Ref: No: DEL-H-037-1920-0223
Case No: HI/Religare/153/19
1.
Name & Address of the complainant
Shri Narender Singh
WZ-1146, Palam Village, New Delhi -110045
2.
Policy No.
Type of Policy
Policy term/Policy Period
10483263
Health Insurance
22.12.2018 to 21.12.2021
3.
Name of the insured
Name of the policy holder
Shri Narender Singh
Shri Narender Singh
4.
Name of Insurer
Religare Health Insurance Company Limited
5.
Date of Repudiation
27.02.2019
6.
Reason for Grievance
Rejection of claim
7.
Date of receipt of the Complaint
18.07.2019
8.
Nature of Complaint
Rejection of mediclaim
9.
Amount of Claim
Rs.4,45,836/-
10.
Date of Partial Settlement
-----
11.
Amount of Partial Settlement
-----
12.
Amount of relief sought
Rs.4,45,836/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing
17.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Shri Narender Singh – Self.
b) For the Insurer
Dr. Nisha Sharma Manager Claims & Mr. Ravi Mgr. Legal
16.
Date of Award/Order
17.12.2019.

17. Brief Facts of the Case
Shri Narender Singh (hereinafter referred to as the complainant) had filed the complaint
against the decision of Religare Health Insurance Company Limited (hereinafter referred
to as the Respondent Insurance Company) alleging wrong rejection of mediclaim bill.
18. Cause of Complaint:
a) Complainant's Argument: The complainant, vide his complaint letter dated 15.07.2019
stated that he was admitted to Akash Health care hospital from 16.02.2019 to 20.02.2019
due to health problem and applied for cashless treatment. Requirements, called for vide
their deficiency letter dated 16.02.2019 were submitted to company along with other
required documents. After 3 days treatment, the complainant was shifted to
Venkateshwar Hospital for further treatment, for the period 22.02.2019 to 05.03.2019. In
the meanwhile, the Insurer issues a Denial Letter for pre-Authorisation dated
27.2.2019.He thensubmitted claims for Rs.8,45,837/-, which were rejected by the Insurer
on the ground of pre- existing nature of ailment and that their deficiency was not replies.
The complainant has sent representation letter to GRO on 18.04.2019 through speed post,
and the same was returned with a remark ‘Not Delivered, refused’.He has now
approached this forum for relief.
b) Insurer's Argument: The Insurer vide their Self-contained Note (SCN) dated
09.09.2019 have stated that they issued a policy for Rs.5,00,000/- SI for the period
22.12.2018 to 21.12.2021 to the complainant. The complainant approached them on
16.02.2019 for cashless treatment. The form duly filled & signed by hospital hadnoted
therein that it was a known case of diabetes mellitus type 2. The query letters were sent to
complainant for submission of previous history for diabetes mellitus vide letters dated
16.02.2019, 17.02.2019 and 18.02.2019, which was not responded by the complainant.
Owing to non-receipt of documents, the Insurer refused cashless treatment and requested
the complainant to apply for reimbursement of claim with required documents. A bill for
Rs.44,125/- was submitted for reimbursement without the required documents. Insurer
sent query letters dated 24.06.2019, 04.07.2019, 14.07.2019 and 31.07.2019 to settle the
claim but got no reply from the complainant. Another cashless treatment request was
made on 22.02.2019 byVenkateshwar Hospital, Dwarka for the complainant with
complaint of Diabetes Mellitus type 2, and the same was rejected on the same ground of
pre- existing nature of ailment. The insurer also denied the allegation of complainant in
letter dated 18.04.2019, addressed to GRO, and marked as “not delivered, refusal”.
Accordingly, the claims was rejectedunder clauses 6.1(iv), 6.2(a)(vi), 6.2 (b), 6.3, 6.4 (iii)
and clause 6.5 of the policy.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal.
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) SCN
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present. Complainant states that he had submitted the documents required by
the Insurer by speed post which were returned undelivered.
Insurer states that they are still open to receiving the required documents and would process the same
further.
It is necessary for the Complainant to submit the required documents to the Insurer by personally
visiting the office within 7 days and thereafter the Insurer should decide about the claim within 3 weeks.
Award
The complaint is disposed off in the following framework: Complainant should submit the required
documents to the Insurer by personally visiting the office within 7 days and thereafter the Insurer
should decide about the claim within 3 weeks thereafter.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Nikhil Goel versus The New India Assurance Company Ltd.
Complaint Ref. No: DEL-H-049-1920-0224
Case No.: GI/NIA/154/19
1.
Name & Address of the Complainant
Shri Nikhil Goel. H. No. 106, Kapil Vihar,
Pitampura, New Delhi- 110034.
2.
Policy No.
Type of Policy
Policy term/Policy Period
32320034172800002036
Mediclaim Policy
29.12.2017 to 28.12.2018.
3.
Name of the insured
Name of the policy holder
Smt. Neha Goel
Shri Nikhil Goel
4.
Name of insurer
The New India Assurance Company Ltd.
5.
Date of Repudiation
NA
6.
Reason for Grievance
Inadequate Settlement of claim.
7.
Date of receipt of the Complaint
22.07.2019.
8.
Nature of Complaint
Inadequate Settlement of claim.
9.
Amount of Claim
Rs.151135 /-
10.
Date of Partial Settlement
16.04.2019.
11.
Amount of Partial Settlement
Rs.322000/-
12.
Amount of relief sought
Rs. 151135/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules 2017
Rule 13(1)(b)– any partial or total
repudiation of claims by an insurer
14.
Date of hearing
17.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Shri Nikhil Goel- Self.
b) For the Insurer
Shri Yogesh Chand Gupta- AO
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri Nikhil Goel(hereinafter referred to as the complainant) had filed the complaint
against the decision of The New India Assurance Company Ltd. (hereinafter referred to
as the Respondent Insurance Company) alleging inadequate settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant, vide his letter dated 22.07.2019, has stated
that his wife Neha Goel was hospitalized at Maharaja Agrasen Hospital for the period
from 14.10.2018 to 17.10.2018 for treatment of pain in right lower limb, diagnosed as
DVT and Thormbocytopenia. He submitted his claim for Rs.473135/- out of which the
Insurance Company paid Rs.322000/- only and deducted Rs.151135/-. He represented his
case before the Insurance Company vide his letter dated 08.05.2019 for the remaining
amount of claim, but got no relief. He has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company vide their Self Contained Note dated
21.08.2019, stated that they had already paid Rs. 322000/- only to the complainant vide
their voucher dated 16.04.2019 as per terms and conditions of the policy after getting
Insured’s consent dated 25.03.2019 for 25% deduction due to over usage of oral
contraceptives in recent past before hospitalization, which is mentioned in the case
history of Discharge Summary.
19. Reason for registration of Complaint:- Inadequate Settlement of claim.
20. The following documents were placed for perusal.
a) Copy of policy
b) Copy of Discharge Summary, Bill, Receipt, Report etc.
c) Copy of consent letter from the insured and claim Settlement voucher from the
Company.
d) Self Contained Note.
21. Result of hearing with both parties (Observations and Conclusion) :
Case called. Parties are present. Complainant had made an agreement with the Insurer by way of giving
a letter dated 25.3.2019 agreeing to accept the settlement of the claim at 75% of the claimed amount.

Prior to that, there was no letter of settlement, full or partial, from the Insurer. Complainant states that
he was in need of money and therefore he involuntarily signed the letter. Complainant being well
educated and well placed in the society and even the claim was not excessively prolonged for
settlement. Moreover, Complainant’s father, who attended the hearing today, is a practicing physician.
Therefore, the agreement offered by the Complainant to the Insurer on 25.3.2019 cannot be called as
under duress or misguidance. Consequently, the Complainant having agreed to settle the claim for 75%
cannot now be justified to seek the balance 25%.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Rajesh Chander Katyal versus The New India Assurance Company Ltd.
Complaint Ref. No.: DEL-H-049-1920-0227
Case No.: GI/NIA/157/19
1.
Name & Address of the Complainant
Shri Rajesh Chander Katyal.
Flat No. C- 57, Green Valley, Sector- 41- 42,
Faridabad, 121003.
2.
Policy No.
Type of Policy
Policy term/Policy Period
32350434172800000211
Medi claim Policy
18.09.2017 to 17.09.2018
3.
Name of the insured
Name of the policy holder
Shri Rajesh Chander Katyal
Smt. Sangeeta Katyal
4.
Name of insurer
The New India Assurance Company Ltd.
5.
Date of Repudiation
05.03.2019
6.
Reason for Grievance
Repudiation
7.
Date of receipt of the Complaint
18.07.2019.
8.
Nature of Complaint
Repudiation
9.
Amount of Claim
Rs.35940/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs.35940/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing
17.12.2019
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Shri Rajesh Chander Katyal- Self.
b) For the Insurer
Ms. Monika Goyal- AO.
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri Rajesh Chander Katyal(hereinafter referred to as the Complainant) had filed the complaint
against the decision of The New India Assurance Company Ltd.(hereinafter referred to as the
Respondent Insurance Company) alleging wrong repudiation of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated vide his letter dated 17.07.2019
that he was hospitalized at Max hospital for the period from 03.07.2018 to 05.07.2018 for
the treatment of severe Acute Low Backache, for which he had submitted all the claim
documents to the Insurance Company. The said claim was repudiated by the Insurance
Company on the basis of line of treatment. He represented his case before the Insurance
Company vide his e-mail dated 06.06.2019, but got no relief. Hence, he has now
approached this forum for relief.
b) Insurer's Argument: The Insurance Company, vide its letter dated 05.03.2019, stated
that the charges incurred at hospital were primarily done for diagnosis, x- ray, laboratory

examination or other diagnostic studies, not consistent with or incidental to the treatment
of positive existence or presence of any illness or injury, for which confinement is
required at hospital. Need for hospitalization was not established. Accordingly they had
rejected the said claim under Clause 4.4.11 of the policy. They have not submitted their
Self Contained Note till date.
19. Reason for registration of Complaint:- Repudiation of claim and cancellation of policy.
20. The following documents were placed for perusal.
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection and Policy Cancellation letter.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present.
Complainant states that he was admitted in a trauma situation, as he could not even move as his both
legs were cramped. Insurer rejected the claim on the ground that the illness did not require
hospitalisation.
As per the MRI Report noted in the discharge summary dated 5.7.2018, certain issues found mention
with the disc and nerves. However, the treatment given is reported as conservative management with
suitable medicines, administered and prescribed for treatment of palpitation, pain-killer, analgesic,
gastric and vitamin D3.
Therefore, the illness justifies hospitalization and accordingly, the Insurer was not justified in repudiating
the claim.
Award
The complaint is allowed and the Insurer is directed to settle the claim within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri PrashantRai V/s Religare Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-037-1920-0226
Case No.: GI/Religare/156/19
1.
Name & Address of the Complainant
Shri Prashant Rai,
Flat No. 7575, First Floor, Ram Nagar, Pahar Ganj,
New Delhi-110055.
2.
Policy No.
Type of Policy
Policy term/Policy Period
12772266
Health Care Policy
29.07.2018 to 28.07.2019.
3.
Name of the insured
Name of the policy holder
Smt. Sumitra
Shri Prashant Rai.
4.
Name of insurer
Religare Health Insurance Company Ltd.
5.
Date of Repudiation
11.10.2019
6.
Reason for Grievance
Repudiation
7.
Date of receipt of the Complaint
08.07.2019.
8.
Nature of Complaint
Repudiation
9.
Amount of Claim
Rs.48000/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs.48000/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of
claims by an insurer
14.
Date of hearing
17.12.2019
Place of hearing
Delhi
15.
Representation at the hearing
For the Complainant
Shri Mohan Rai- Father
For the Insurer
Dr. Nisha Sharma Manager Claims & Mr. Ravi
Manager Legal
16.
Date of Award/Order
17.12.2019.

17. Brief Facts of the Case
Shri Prashant Rai(hereinafter referred to as the complainant) had filed the complaint against the
decision of Religare Health Insurance Company Ltd. (hereinafter referred to as the Respondent
Insurance Company) alleging wrong repudiation of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated vide his e-mail dated 08.07.2019
that his wife was hospitalized at Jeewan Mala hospital for the period from 13.09.2018 to
15.09.2018 for the treatment of Arboviralfever with UTI, for which he had submitted all
the claim documents to the Insurance Company. The said claim was repudiated by the
Insurance Company on ground of main claim not covered under the policy. He
represented his case before the Insurance Company vide his e-mail dated 22.01.2019, but
got no relief. Hence, he has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company, vide its letter dated 11.10.2018, stated
that they had rejected the said claim on ground of main claim not covered under the
policy.They have not submitted their Self Contained Note till date.
19. Reason for registration of Complaint:- Repudiation of claim .
20. The following documents were placed for perusal.
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and inform that they have agreed to settle the claim for Rs. 30,370
and sign a conciliation agreement, which I find fair and reasonable.
Award
The complaint is allowed in terms of the conciliation agreement signed by the parties today.
Accordingly, Insurer should settle the claim for Rs. 30,370 within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Rakesh Kumar Srivastava V/sReligare Health Insurance Company Ltd.
Complaint Ref. No: DEL-H-037-1920-0228
Case No.: GI/Religare/158/19
1.
Name & Address of the Complainant
Shri Rakesh Kumar Srivastava,
Flat No. L-1/ 31 B, First Floor, DDA Flats,
Kalkaji, New Delhi-110019
2.
Policy No.
Type of Policy
Policy term/Policy Period
12325318
Health Care Policy
01.04.2019 to 31.03.2020.
3.
Name of the insured
Name of the policy holder
Smt. Nirmala Srivastava
Shri Rakesh Kumar Srivastava
4.
Name of insurer
Religare Health Insurance Company Ltd.
5.
Date of Repudiation
29.04.2019
6.
Reason for Grievance
Rejection
7.
Date of receipt of the Complaint
18.07.2019
8.
Nature of Complaint
Rejection
9.
Amount of Claim
Rs.424231/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs.424231/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing
17.12.2019

Place of hearing
Delhi
15.
Representation at the hearing
For the Complainant
Shri Rakesh Kumar Srivastava- Self.
For the Insurer
Dr. Nisha Sharma Manager Claims & Mr.
Ravi Manager Legal.
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri Rakesh Kumar Srivastava (hereinafter referred to as the complainant) had filed the complaint
against the decision of Religare Health Insurance Company Ltd. (hereinafter referred to as the
Respondent Insurance Company) alleging wrong rejection of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated vide his letter dated 17.07.2019
that his mother was hospitalized at Fortis hospital for the period from 21.04.2019 to
29.04.2019 for the treatment of pain and swelling over right hip/ thigh due to injury, for
which he had submitted all the hospitalization and post hospitalization claim documents
to the Insurance Company for Rs.4,24,231/-. The said claim was repudiated by the
Insurance Company on the ground of non-disclosure of pre-existing disease at the time of
proposal. He represented his case before the Insurance Company vide his e-mail dated
29.04.2019, but got no relief. Hence, he has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company, vide its letter dated 29.04.2019, stated
that they had rejected the said claim on ground of non disclosure of pre- existing disease
of depression disorder at the time of proposal. In their Self Contained Note, dated
10.10.2019, the Insurance Company stated that the patient, as per the Prescription dated
18.06.2016, was taking Tab. Serlift 50 and Revotril 0.5 mg, which are antipsychotic
medicines, which suggests that the patient had been suffering from depression disorder
prior to the inception of policy. The same was not disclosed at the time of proposal;
hence they rejected the said claim.
19. Reason for registration of Complaint:- Rejection of claim.
20. The following documents were placed for perusal.
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present. Insurer had repudiated the claim by noting from the Emergency
Record of 21.4.2019 which had noted past history as ‘Depression’ and medication as Tab. Serlift and
Revotril as OD (one per day). Insurer has also produced copy of a Neuro Clinic prescription of the
insured which recommends these two tablets on OD basis for a month. Accordingly, Insurer has
concluded that the insured was suffering from depression disorder, which was a PED that was not
disclosed while taking the policy on 1.4.2018 renewed in 2019.
Insurer states that the repudiation was not on account of medication history but for non-disclosure
of PED of depression disorder as stated in Clause 4.2.13. However, 4.2.13 in respect of Permanent
exclusions reads as follows: “Treatment of mental illness, stress or psychological disorder or
Parkinson’s disease or alzheimer’s disease even if caused or aggravated by or related to an accident
or illness/”.
Clause 4.2.13 is not relevant in this case.
Complainant has submitted a certificate from the treating physician stating that this fall was not
related to any medication for depression.
The inference of Insurer is not adequately supported by the various documents produced by them
and accordingly the repudiation of the claim was not justified.
Award
The complaint is allowed and the Insurer is directed to admit and settle the claim within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Rajesh Kumar Gupta V/S Religare Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-037-1920-0261
Case No.: GI/Religare/183/19
1.
Name & Address of the Complainant
Shri Rajesh Kumar Gupta.
Flat No. B-1/101, 2
nd
. Floor, Janakpuri, New
Delhi-110058.
2.
Policy No.
Type of Policy
Policy term/Policy Period
11206038
Health Care Policy
17.04. 2019 to 16.04.2020.
3.
Name of the insured
Name of the policy holder
Shri Rajesh Kumar Gupta.
Shri Rajesh Kumar Gupta.
4.
Name of insurer
Religare Health Insurance Company Ltd.
5.
Date of Repudiation
31.05.2019
6.
Reason for Grievance
Rejection
7.
Date of receipt of the Complaint
22.07.2019.
8.
Nature of Complaint
Rejection
9.
Amount of Claim
Rs.298300/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs.298300/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing
17.12.2019
Place of hearing
Delhi
15.
Representation at the hearing
For the Complainant
Absent
For the Insurer
Dr. Nisha Sharma Manager Claims & Mr.
Ravi Manager Legal.
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri Rajesh Kumar Gupta (hereinafter referred to as the complainant) had filed the complaint
against the decision of Religare Health Insurance Company Ltd. (hereinafter referred to as the
Respondent Insurance Company) alleging wrong rejection of mediclaim.
18. Cause of Complaint:
a. Complainant's Argument: The complainant has stated vide his letter dated
19.07.2019 that he was hospitalized at BLK hospital for the period from 06.05.2019
to 08.05.2019 for the treatment of Chest pain and SOB, for which he had submitted
all the claim documents to the Insurance Company. The said claim was rejected by
the Insurance Company on ground that his main claim was not covered under the
policy due to non disclosure of pre- existing disease. He represented his case before
the Insurance Company vide his e-mail dated 09.05.2019, but got no relief. Hence, he
has now approached this forum for relief.
b. Insurer's Argument: The Insurance Company, vide its letter dated 31.05.2019, had
stated that they had rejected the said claim on the ground that his main claim was not
covered under the policy due to non disclosure of pre-existing disease. Hence the said
claim was also not payable under the policy on the same ground. They have
submitted the supporting documents and reiterated the above facts in their Self
Contained Note (SCN) dated 4.12.2019.
19. Reason for registration of Complaint:-Rejection of claim.
20. The following documents were placed for perusal.
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.

d) SCN
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent. Insurer is present.
Insure has submitted the in-patient record dated 6.5.2019 wherein the Complainant is specified to
have idiopathic thrombocytic disorder (ITP) since 2006 and ulcerative colitis since 2008, which both
existed before the policy inception but were not disclosed while taking the policy. Hence the Insurer
was justified in repudiating the claim on the grounds of non-disclosure of PED.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri. Ashok Kumar Narang versus Apollo Munich Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-003-1920-0256
Case No.: GI/Apollo/179/19
1.
Name & Address of the Complainant
Shri. Ashok Kumar Narang
24/18, Double Storey, Moti Nagar,
New Delhi-110015.
2.
Policy No.
Type of Policy
Policy term/Policy Period
120100/12001/AO12708/684
Mediclaim Policy
18.12.2018 to 17.12.2019.
3.
Name of the insured
Name of the policy holder
Shri. Ashok Kumar Narang
Shri. Ashok Kumar Narang
4.
Name of insurer
Apollo Munich Health Insurance Company Ltd.
5.
Date of Repudiation
16.01.2019.
6.
Reason for Grievance
Rejection of claim and Cancellation of Policy
7.
Date of receipt of the Complaint
25.07.2019.
8.
Nature of Complaint
Rejection of claim and Cancellation of Policy
9.
Amount of Claim
Rs.71356/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs. 71356/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules 2017
Rule 13(1)(b) – any partial or total repudiation of
claims by an insurer
14.
Date of hearing
17.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Absent
b) For the Insurer
Shri Vivek Yadav- Manager
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri. Ashok Kumar Narang (hereinafter referred to as the complainant) had filed the complaint
against the decision of Apollo Munich Health Insurance Company Ltd. (hereinafter referred to as
the Respondent Insurance Company) alleging wrong rejection of mediclaim and cancellation of
Policy.
18. Cause of Complaint:
a) Complainant's Argument: The complainant, vide his letter dated 25.07.2019, has stated that
he was hospitalized at Maharaja Agrasen Hospital for the period from 14.02.2019 to 17.02.2019
and was diagnosed as Large Stricture Urethra with obstruction of flow. He submitted the claim
forRs. 71,356/- which was rejected by the company on the ground of pre-existing disease and
surgery of Urethral Stricture in 2010. Herepresented his case before the Insurance Company vide
his letter dated 21.02.2019 for payment of his claim, but he got no relief. He has now approached
this forum for relief.
b) Insurer's Argument: The Insurance Company had stated vide their rejection letter dated
16.01.2019 and 28.03.2019, that based on verification conducted, it was noted that there is history
of surgery of the claimant for Urethral Stricture in 2010, i.e. prior to the inception of policy, hence

the Insurance Company rejected the said claim due to incorrect health declaration under Section 3t
of the policy. Further, the Insurance Company sent Policy Cancellation Notice dated 23.03.2019 to
the policy holder. The Insurance Company quoted various Supreme Court decisions in theirSelf
Contained Note dated 04.12.2019, and reiterated that that there is history of surgery of the claimant
for Urethral Stricture in 2010, i.e. prior to the inception of policy, which was not disclosed at the
inception of policy. Accordingly they rejected the said claim under Section 3t of the policy.
19. Reason for registration of Complaint:-Rejection of claim and Cancellation of Policy.
20. The following documents were placed for perusal.
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection and Policy Cancellation letter.
d) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent and has sought adjournment. Insurer is present and states
that the Complainant had earlier sought for pre-authorisation for cashless treatment for an
earlier hospitalisaion in December 2018. However, the Insurer had denied the same on
7.10.2018 as the hospital had mentioned a past illness, for which the Complainant had not given
details while applying for the policy. This led to set of letters exchanged between the
Complainant and the Insurer, and Insurer had informed the Complainant vide email dated
16.1.2019 that while cashless was not approved, he could seek reimbursement with the
required document. However, Complainant did not submit the claim for reimbursement for that
instance.
Subsequently, the Complainant fell ill again and was hospitalized during 14-17 Feb. 2019, but
this time he did not seek cashless and opted for reimbursement, which was rejected by the
Insurer vide letter dated 28.3.2019 on the grounds of incorrect good health declaration
submitted by the Complainant while applying for the policy. This rejection has been questioned
by the Complainant in the present case.
A careful reading of the letter dated 28.3.2019 of the Insurer indicates that the Insurer had
rejected the claim citing the ground of non-declaration of the history of surgery for urethral
stricture in 2010. However, in the same letter, the Insurer had also advised the Complainant that
he should revert to the Insurer in case he felt that the Insurer had overlooked any material fact
or circumstance. The Complainant has chosen to approach this forum instead of responding to
the Insurer. This approach of the Complainant is not correct and his complaint is not justified
before this forum at this stage. Complainant should reply to the Insurer with the required
documents and thereafter approach the GRO of the Insurer and only thereafter approach this
forum, as required.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Ajit KumarAgarwalversus United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-1920-0257
Case No.: GI/UII/180/19
1.
Name & Address of the Complainant
Shri Ajit Kumar Agarwal
C-21, DGS CGHS Plot No. 6, Sector- 22, Dwarka,
New Delhi-110077.
2.
Policy No.
Type of Policy
Policy term/Policy Period
500100/28/17/ P111/247136
Mediclaim Policy
01.11.2018 to 31.10.2019.
3.
Name of the insured
Name of the policy holder
Smt. Neena Agarwal
Shri Ajit Kumar Agarwal
4.
Name of insurer
The United India Insurance Company Ltd.
5.
Date of Repudiation
NA
6.
Reason for Grievance
Inadequate Settlement
7.
Date of receipt of the Complaint
30.07.2019.

8.
Nature of Complaint
Inadequate Settlement
9.
Amount of Claim
Rs.127347/-
10.
Date of Partial Settlement
20.08.2018.
11.
Amount of Partial Settlement
114117/-
12.
Amount of relief sought
Rs.127347/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules 2017
Rule 13(1)(b) – any partial or total repudiation
of claims by an insurer
14.
Date of hearing
17.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Shri Ajit Kumar Agarwal- Self.
b) For the Insurer
Shri Sanjay Ahuja- AO.
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri Ajit Kumar Agarwal(hereinafter referred to as the complainant) had filed the
complaint against the decision of United India Insurance Company Ltd. (hereinafter
referred to as the Respondent Insurance Company) alleging inadequate settlement of
mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated vide his complaint dated
14.06.2019 that his wife Neena Agarwal was hospitalized at Manipal Hospital, Delhi for
the period from 13.12.2018 to 02.01.2019 for the treatment of Respiratory failure Type-
II and Urosepsis. He lodged claim for Rs.241464/-, out of which the Insurance Company
paid Rs.114117/- only and deducted Rs.127347/-. He approached the Grievance cell of
the company online for the remaining amount of his claim, but got no relief. Hence he
has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company has stated, vide their letter dated
21.06.2019, that they had already paid the claim as per terms and conditions of the policy
for Rs. 114117/- only, and informed the complainant about the deductions. The Company
has not submitted their Self Contained Notetill date.
19. Reason for registration of Complaint: Inadequate Settlement of claim.
20. The following documents were placed for perusal:
a) Copy of policy
b) Copy of Discharge Summary, Bill, Receipt, Report etc.
c) Copy of claim Settlement Advice.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present. Complainant states that his claim before this Insurer was for
two items, namely, diagnosis and medicines and the Insurer paid him for diagnosis, but in
respect of his claim of Rs. 1.27 lakh towards medicines, the Insurer had settled it for Rs. 24,137
only, which is his grievance. The remaining parts of the claim towards bed charges etc., were
settled by another Insurer (Royal Sundaram).
Insurer states that the total hospital bill was Rs. 6,68,055, against which the hospital provided a
discount of Rs. 1,05,688, leaving the net claim as Rs. 5,62,367. Against this amount, an amount
of Rs. 1,40,827 was considered as non-payable, and included EEG claim not supported by
original report= Rs. 13,480, Excess room rent= Rs. 1,21,800, Towel charges= Rs. 3,267, and Extra
bed charges= Rs. 2,280. The net admissible claim was accordingly determined as Rs. 4,21,540.
Out of this amount, the other Insurer (Royal Sundaram) had reimbursed (through cashless, to
the hospital) Rs. 3,07,423, leaving a balance of Rs. 1,14,117, which this Insurer has already paid.
Complainant states that this Insurer should focus only on two items of the total bill, namely,
diagnosis and medicines, as the other components were handled by the other Insurer (Royal
Sundaram).
As per the prevalent principle and practice in medical insurance sector, a person can take
parallel policies from two insurers and submit the claim to the two insurers separately.
However, in such a case, each insurer would examine the claim in totality and settle the same
according to the respective policy conditions. The insurer who settles the claim later, would
deduct the amount paid by the first insurer. In this process, the policy holder would not have
the choice to submit part bills to the two insurers.

Therefore, the Insurer had settled the claim correctly.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Nitish Jain versus United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-1920-0258
Case No: GI/UII/181/19
1.
Name & Address of the Complainant
Shri Nitish Jain C-21, DGS CGHS Plot No. 6,
Sector- 22, Dwarka, New Delhi-110077.
2.
Policy No.
Type of Policy
Policy term/Policy Period
500100/28/17/ P111/247136
Mediclaim Policy
01.11.2018 to 31.10.2019.
3.
Name of the insured
Name of the policy holder
Shri Pawan Jain
Shri Pawan Jain
4.
Name of insurer
The United India Insurance Company Ltd.
5.
Date of Repudiation
NA
6.
Reason For Grievance
Inadequate Settlement
7.
Date of receipt of the Complaint
30.07.2019.
8.
Nature of Complaint
Inadequate Settlement
9.
Amount of Claim
Rs.73350/-
10.
Date of Partial Settlement
27.06.2018.
11.
Amount of Partial Settlement
46941/-
12.
Amount of relief sought
Rs. 73350/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules 2017
Rule 13(1)(b) – any partial or total repudiation
of claims by an insurer
14.
Date of hearing
17.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a. For the Complainant
Shri Nitish Jain s/o. Shri Pawan Jain
b. For the Insurer
Shri Deepak Ahuja- Dy. Manager
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri Nitish Jain (hereinafter referred to as the complainant) had filed the complaint against the
decision of United India Insurance Company Ltd. (hereinafter referred to as the Respondent
Insurance Company) alleging Inadequate Settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated vide his complaint dated
04.06.2019 that his fatherSh. Pawan Jain was hospitalized at Balaji Action Medical
Institute, Delhi for the period from 07.05.2018 to 10.05.2018 for the treatment of
Ureteric Calculi with CKD. A claim was lodged claim for Rs.120291/-, out of which
the Insurance Company paid Rs.46941/- only and deducted Rs.73350/-. He
approached the Grievance cell of the company vide his e-mail dated 13.05.2019 for
the remaining amount of his claim, but got no relief. Hence he has now approached
this forum for relief.
b) Insurer's Argument: The Insurance Company has stated, vide their letter dated
11.07.2019, that they had already paid the claim as per terms and conditions of the
policy for Rs. 46941/- only, and informed the complainant vide their mail dated
20.07.2018 about the deductions. The Company has not submitted their Self
Contained Note till date.

19. Reason for registration of Complaint:- Inadequate Settlement of claim.
20. The following documents were placed for perusal.
a) Copy of policy
b) Copy of Discharge Summary, Bill, Receipt, Report etc.
c) Copy of claim Settlement Advice.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present. Complainant (Policyholder Sh. Pawan Jain) had gone in for
hospitalisation in a PPN hospital. The treatment was to be in cashless mode. The Policy Clause
3.25 mandates the reimbursement shall be subject to rates applicable to PPN package pricing.
Insurer has settled the claim accordingly. Therefore, there is no case of inadequate settlement.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Binod Kumar Gupta versus United India Insurance Company Ltd.
Complaint Ref. No: DEL-H-051-1920-0264
Case No.: GI/UII/186/19
1.
Name & Address of the Complainant
Shri Binod Kumar Gupta Allahabad Bank,
RMPC Large,1
st
. Floor, 17, Parliament
Street, New Delhi-110001
2.
Policy No.
Type of Policy
Policy term/Policy Period
5001002817P109940139
Mediclaim Policy
01.10.2018 to 30.09.2019.
3.
Name of the insured
Name of the policy holder
Shri Adyansh Gupta
Shri Binod Kumar Gupta
4.
Name of insurer
The United India Insurance Company LTd.
5.
Date of Repudiation
04.06.2019
6.
Reason for Grievance
Rejection
7.
Date of receipt of the Complaint
030.07.2019.
8.
Nature of Complaint
Rejection
9.
Amount of Claim
Rs.70300/-
10.
Date of Partial Settlement
-
11.
Amount of Partial Settlement
-
12.
Amount of relief sought
Rs.70300/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules 2017
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing
17.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Absent
b) For the Insurer
Shri Sanjay Ahuja- AO.
16.
Date of Award/Order
17.12.2019.
17. Brief Facts of the Case
Shri Binod Kumar Gupta (herein after referred to as the complainant) had filed the
complaint against the decision of United India Insurance Company Ltd. (hereinafter
referred to as the Respondent Insurance Company) alleging wrong rejection of
mediclaim.
18. Cause of Complaint: Rejection of claim.
a) Complainant's Argument: The complainant, vide her letter dated 09.07.2019, stated
that his son was treated. He submitted two claims for Rs.70300/- which were denied on

the ground that Sum Insured exhausted under his policy cover. He represented his case to
Insurance Company vide his bank e-mail dated 10.06.2019for the payment of his claims.
But he got no relief. He has now approached this forum for relief. Now, we have received
a mail dated 26.11.2019 from the complainant, informing us that his claim had been paid
by the Company, and his grievance has been resolved. Hence, he has withdrawn his
grievance.
b) Insurer's Argument: The Insurance Company, vide their e-mail dated 04.06.2019, stated
that they rejected the said claims, as the OPD limit of Sum Insured exhausted under the
policy. The Insurance Company have not submitted any further Self Contained Note.
19. Reason for registration of Complaint:- Rejection of claim.
20. The following documents were placed for perusal.
a) Copy of policy
b) Copy of Domiciliary Claim, Bill, Receipt, Report etc
c) Copy of claim Settlement Advice.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Insurer is present. Complainant is absent, but has sent an email on 29.11.2019 stating
that the complaint has since been resolved as the insurer had paid the claimed amount. Insurer
confirms this statement.
Award
The complaint is allowed, as the insurer has paid the claimed amount already.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
17
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Pradeep Kumar Sethi versus Religare Health Insurance Company Limited
Complaint Ref. No.: DEL-H-037-1920-0308
Case No.: HI/Religare/215/19
1.
Name & Address of the Complainant
Shri Pradeep Kumar Sethi
232, First Floor, Chand Nagar, New Delhi -110018
2.
Policy No.
Type of Policy
Policy term/Policy Period
11173811
Health Insurance
02.04.2017 to 01.04.2020.
3.
Name of the insured
Name of the policy holder
Shri Pradeep Kumar Sethi
Shri Pradeep Kumar Sethi
4.
Name of Insurer
Religare Health Insurance Company Limited
5.
Date of Repudiation
31.10.2018.
6.
Reason for Grievance
Rejection of mediclaim
7.
Date of receipt of the Complaint
20.08.2019
8.
Nature of Complaint
Rejection of mediclaim
9.
Amount of Claim
Rs.148656/-
10.
Date of Partial Settlement
-
11.
Amount of Partial Settlement
-
12.
Amount of relief sought
Rs.148656/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims
by an insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
c) For the Complainant
Shri Pradeep Kumar Sethi – Self.
d) For the Insurer
Dr. Nisha Sharma Manager (Claims) & Mr. Pratyush
Prakash- Manager (Legal)
16.
Date of Award/Order
30.12.2019.

17. Brief Facts of the Case
Shri Pradeep Kumar Sethi (hereinafter referred to as the complainant) had filed the
complaint against the decision of Religare Health Insurance Company Limited
(hereinafter referred to as the Respondent Insurance Company) alleging wrong rejection
of mediclaim.
18. Cause of Complaint
c) Complainant's Argument: The complainant vide his complaint letter dated 19.08.2019,
has stated that he was admitted to Kalra hospital from 30.09.2018 to 04.10.2018 due to
pain in abdomen, vomiting and breathlessness problem and was diagnosed to be suffering
from Acute Intestitial Edemetous Pancreatitis, for which he submitted the claim for
Rs.148656/-, which was rejected by the Insurer on the ground of being a chronic
alcoholic. Complainant sent representation letter to GRO on 11.02.2019 through
registered post, stating that he was not a chronic alcoholic and admitted that he used to
drink alcohol occasionally, but got no relief. He has now approached this forum for relief.
d) Insurer's Argument: The Insurer vide their letter dated 31.10.2018 has stated that as per
submitted documents, the patient was admitted with A/H/Ochronic alcoholic for the
treatment of Acute Intestitial Edemetous Pancreatitis. As per policy condition, disease
due to intoxication is not payable. Hence claim is not admissible and rejected under the
policy. In their Self Contained Note dated 04.11.2019, the Company stated that as per an
article of American Pancreartic Association, ‘alcohol abuse is a well recognized
association of both pancreatic necro- inflammation, leading to chronic disease. The risk
of developing Pancreatitis increases with increased consumption of alcohol.’In the
proposal, the complainant did not disclose pre-existing Hypertension and the habit of
drinking alcohol, hence they rejected the said claim accordingly under Clause 4.2 of the
policy.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal.
e) Copy of policy.
f) Copy of Discharge Summary, Bill, Receipt, Reports etc.
g) Copy of Rejection letter.
h) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present.
Complainant admits to be consuming alcohol for 2-3 days in a week since past 30 years.
Insurer states that the claim was repudiated on the grounds of the Policy Exclusion Clause 4.2.23,
that is, illness attributable to consumption or use of alcohol.
It is quite apparent that the ailment of Pancreatitis would have definitely arisen out of regular
consumption of alcohol by the insured claimant.
In the circumstances explained by the parties, the Insurer appears justified in repudiating the claim.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
30
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ashlok Malik versus Religare Health Insurance Company Limited
Complaint Ref. No.: DEL-H-037-1920-0302
Case No: HI/Religare/209/19
1.
Name & Address of the Complainant
Shri Ashlok Malik s/o. Late Shri Gopal Krishan Malik - 65,
Kadambari Apartment, Sector- 9, Rohini, Delhi -110045

2.
Policy No.
Type of Policy
Policy term/Policy Period
10978132 (Complaint filed by Nominee Shri Ashlok Malik)
Health Insurance
24.01.2017 to 23.01.2019.
3.
Name of the insured
Name of the policy holder
Late Shri Gopal Krishan Malik
Late Shri Gopal Krishan Malik
4.
Name of Insurer
Religare Health Insurance Company Limited
5.
Date of Repudiation
19.01.2019
6.
Reason For Grievance
Rejection of claim
7.
Date of receipt of the Complaint
27.08.2019
8.
Nature of Complaint
Rejection of mediclaim
9.
Amount of Claim
Rs.272841/-
10.
Date of Partial Settlement
-
11.
Amount of Partial Settlement
-
12.
Amount of relief sought
Rs. 272841/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims
by an insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a. For the Complainant
Shri Ashlok Malik – Self.
b. For the Insurer
Dr. Nisha Sharma Manager (Claims) & Mr. Pratyush
Prakash- Manager (Legal)
16.
Date of Award/Order
30.12.2019.
17. Brief Facts of the Case
Shri Ashlok Malik (hereinafter referred to as the complainant) had filed the complaint
against the decision of Religare Health Insurance Company Limited (hereinafter referred
to as the Respondent Insurance Company) alleging wrong rejection of mediclaim bill.
18. Cause of Complaint:
a) Complainant's Argument: The complainant vide his complaint letter dated
17.06.2019, has stated that his father was admitted to Fortis hospital on 19.01.2019
for treatment, where he was declared dead the same day. He submitted claim bill for
Rs.272841/-, which was rejected by the Company on the ground of 4 years Waiting
period for the pre- existing disease (PED). However his deceased father had declared
PED of Diabetes, but that was not the cause of death. Accordingly, the complainant
has sent representation letter to GRO on 17.06.2019 through registered post, but the
Company did not provide any relief. He has now approached this forum for relief.
Insurer's Argument: The Insurer vide their letter dated 19.01.2019, has stated that Diabetes was
mentioned on the face of policy subject to 4 Years Waiting period, and the claim occurred
during the second year of policy. Hence they rejected the said claim under Clause 4.1 of the
policy. In their Self Contained Note dated 15.10.2019, the Company reiterated that the said
claim occurred during the second year of policy which was issued subject to 4 Years Waiting
period. Hence they rejected the said claim under clause 4.1 of the policy due to 4 Years Waiting
Period Clause.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion)
Case called. Parties are present.
The insured policyholder Gopal Krishan Malik was hospitalized on 19.1.2019 following illness and
expired the same day in the hospital. The treating hospital had applied for cashless settlement,
which was rejected by the Insurer on the same day, that is, 19.1.2019, on the grounds of 4-year
waiting period for a pre-existing disease (PED). Subsequently, his son Ashlok Malik, who is the
Complainant in this case, applied for reimbursement of the hospitalization expenses on 15.2.2019,
which was rejected by the Insurer vide letter dated 22.2.2019 citing the same ground of 4-year

waiting period for a PED. The PED in question is diabetes. The Policyholder had declared in the policy
proposal form on 15.12.2016 that he was having diabetes since August 2016. The treating doctor
had given a certificate dated 12.12.2019, that the insured died due to a heart attack, which was a
known complication of extensive micro cordial infraction and diabetes itself was not the cause.
In the rejection letters dated 19.1.2019 and 22.2.2019, Insurer did not quote the relevant Policy
Clause Number or its text. However, in the SCN and in today’s hearing, Insurer clarified that it was
Clause 4.1.(iii). A careful reading of this clause indicates that it excludes claims only in respect of
diagnosis or treatment of a PED for the first 48 months of the policy. Therefore, I conclude that the
death of the insured person, who had declared his affliction of diabetes since August 2016, was not
due to diabetes. Accordingly, the repudiation on the ground of Clause 4.1 (iii ) was not justified.
Award
The complaint is allowed and the Insurer is directed to settle the claim No. 90856424 of the
Complainant within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
2
nd
January, 2020
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Nitin Mittal versus Religare Health Insurance Company Limited
Complaint Ref. No.: DEL-H-037-1920-0324
Case No: HI/Religare/231/19
1.
Name & Address of The Complainant
Shri Nitin Mittal
D- 14/125, Sector- 8, Rohini, Delhi -110088.
2.
Policy No.
Type of Policy
Policy term/Policy Period
10480946
Health Insurance
30.12.2018 to 29.12.2019.
3.
Name of the insured
Name of the policy holder
Shri Nitin Mittal
Shri Nitin Mittal
4.
Name of Insurer
Religare Health Insurance Company Limited
5.
Date of Repudiation
31.10.2018.
6.
Reason For Grievance
Non Settlement of mediclaim
7.
Date of receipt of the Complaint
20.08.2019
8.
Nature of Complaint
Non Settlement of mediclaim
9.
Amount of Claim
Rs. 47361/-
10.
Date of Partial Settlement
-
11.
Amount of Partial Settlement
-
12.
Amount of relief sought
Rs. 47361/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(a) – any delay in Settlement of claim by an
insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a. For the Complainant
Absent.
b. For the Insurer
Dr. Nisha Sharma Manager (Claims) & Mr. Pratyush
Prakash- Manager (Legal)
16.
Date of Award/Order
30.12.2019.
17. Brief Facts of the Case
Shri Nitin Mittal (hereinafter referred to as the complainant) had filed the complaint
against the decision of Religare Health Insurance Company Limited (hereinafter referred
to as the Respondent Insurance Company) alleging non-settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant vide his complaint letter dated
03.09.2019 has stated that he submitted his hospitalization claim, which was settled
by the company, but his post hospitalization claim for Rs.47361/- was not settled. The
complainant has sent representation letter to GRO on 28.06.2019, for payment of his
post hospitalization claim, but got no relief. He has now approached this forum for
relief.

b) Insurer's Argument: The Insurer paid the main hospitalization claim but did not
settle the said post hospitalization claim to the complainant. In their Self Contained
Note dated 23.12.2019, the company reiterated that they have not paid non medical
items like Volini Gel/ Analgesic gel, excluded under Annexure- II of the policy.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent. Insurer explains that they had paid about Rs. 2 lakh to the
Complainant for various items of claim related to his hospitalization during April 2019 and July
2019. Complainant is now seeking payment two disallowed items amounting to Rs. 4736. Insurer
had given details of this disallowed item to the Complainant vide settlement letter dated 30.6.2019,
explaining that these related to inadmissible items. Insurer had also advised the Complainant to
revert to them for any further assistance.
In the facts and circumstances apparent from the documents, the settlement made by the Insurer
appears justified.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
30
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shivani Sundriyal V/s The New India Assurance Company Ltd.
Complaint Ref. No.: DEL-H-049-1920-0306
Case No.: GI/NIA/213/19
1.
Name & Address of the Complainant
Ms Shivani Sundriyal. H. No. C- 1760, Palam
Vihar, Gurugram-122017.
2.
Policy No.
Type of Policy
Policy term/Policy Period
31060034189500000859
Mediclaim Policy
18.09.2018 to 17.09.2019.
3.
Name of the insured
Name of the policy holder
Ms. Shivani Sundriyal
Ms. Shivani Sundriyal
4.
Name of insurer
The New India Assurance Company Ltd.
5.
Date of Repudiation
NA
6.
Reason For Grievance
Inadequate Settlement of claim.
7.
Date of receipt of the Complaint
08.08.2019.
8.
Nature of Complaint
Inadequate Settlement of claim.
9.
Amount of Claim
Rs.86030 /-
10.
Date of Partial Settlement
09.07.2019.
11.
Amount of Partial Settlement
Rs.51837/-
12.
Amount of relief sought
Rs. 86030/-
13.
Complaint registered under Rule no:
Insurance Ombudsman rules
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
For the Complainant
Absent
For the Insurer
Shri Anuj Nagar- AO and Dr. P. Sharma- Dy.
Manager.
16.
Date of Award/Order
30.12.2019.
22. Brief Facts of the Case:

Ms. Shivani Sundriyal (hereinafter referred to as the complainant) had filed the complaint
against the decision of The New India Assurance Company Ltd. (hereinafter referred to
as the Respondent Insurance Company) alleging inadequate settlement of mediclaim.
23. Cause of Complaint:
c) Complainant's Argument: The complainant vide her letter dated 07.08.2019, has stated
that she was hospitalized at MMFR Memorial Hospital for the period from 15.06.2019 to
17.06.2019 for treatment of Left Pyleon nephritis with Urethral Stricture. She submitted
her claim for Rs.137867/- out of which the Insurance Company paid Rs.51837/- only and
deducted Rs.86030/- She represented her case before the Insurance Company vide her
e-mail dated 11.07.2019 for the remaining amount of claim, but got no relief. She has
now approached this forum for relief.
d) Insurer's Argument: The Insurance Company vide their Settlement cum Discharge
Voucher dated 09.07.2019, stated that they had already paid Rs. 51837/- only to the
complainant as per terms and conditions of the policy. They have not submitted their
SCN till date.
24. Reason for registration of Complaint: Inadequate Settlement of claim.
25. The following documents were placed for perusal:
e) Copy of policy
f) Copy of Discharge Summary, Bill, Receipt, Report etc.
g) Copy of claim Settlement letter cum Discharge voucher.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent. Insurer is present. Insurer states that the claim was settled as
per GIPSA rates. As per Policy Condition No. 5.5, the Complainant was required to intimate the TPA
in writing before any hospitalization. The Complainant did not follow the required procedure and
chose to get treatment in a hospital of her choice, which charged her more than the GIPSA rates.
In these circumstances, the Insurer was justified in limiting the claim to GIPSA rates.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
30
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Parminder Singh Arora V/s The New India Assurance Company Ltd.
Complaint Ref. No.: DEL-H-049-1920-0320
Case No.: GI/NIA/227/19
1.
Name & Address of the Complainant
Shri Parminder Singh Arora.
Flat No. E- 143, 2
nd
. Floor, GK- III, New
Delhi- 110048.
2.
Policy No.
Type of Policy
Policy term/Policy Period
31190034180400000021
Medi claim Policy
12.12.2018 to 11.12.2019.
3.
Name of the insured
Name of the policy holder
Smt. Meera Arora
Shri Parminder Singh Arora
4.
Name of insurer
The New India Assurance Company Ltd.
5.
Date of Repudiation
29.06.2019
6.
Reason for Grievance
Repudiation
7.
Date of receipt of the Complaint
22.08.2019.
8.
Nature of Complaint
Repudiation
9.
Amount of Claim
Rs.93,029.00 (Rs. 58230/-& Rs. 34799/-)
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs.93,029.00

13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing
24.12.2019
Place of hearing
Delhi
15.
Representation at the hearing
For the Complainant
Absent
For the Insurer
Mrs. Madhu Batra- Dy. Manager
16.
Date of Award/Order
30.12.2019.
22. Brief Facts of the Case
Shri Parminder Singh Arora (hereinafter referred to as the complainant) had filed the complaint
against the decision of the New India Assurance Company Ltd. (hereinafter referred to as the
Respondent Insurance Company) alleging wrong repudiation of his mediclaim.
23. Cause of Complaint
c) Complainant's Argument: The complainant has stated vide his letter dated 22.08.2019
that his wife was hospitalized at Shalby Hospital, Mohali for the period from 22.01.2019
to 24.01.2019 for the treatment of old Post Traumatic Fracture D-12 with Osteoporosis
and pain, for which he had submitted all the claim documents to the Insurance Company
for Rs.58230/- + Rs. 34799/-. The said claim was repudiated by the Insurance Company
on the basis of line of treatment. He represented his case before the Insurance Company
vide his e-mail dated 03.07.2019 and requested for payment of the said claim, but got no
relief. Hence, he has now approached this forum for relief.
d) Insurer's Argument: The Insurance Company, vide its e-mail dated 29.06.2019, has
stated that the said claim was repudiated under Clause 4.4.11 of the policy, which clearly
states that ‘Diagnosis, X- Ray, or Lab Examination, not consistent with or incidental to
the diagnosis of positive existence and treatment of any ailment, sickness or injury, for
which confinement to the hospital is not required’ are not payable under the policy. In
their Self Contained Note dated 23.12.2019, the company reiterated the same that
admission for investigation and evaluation purpose is excluded under Clause 4.4.11 of the
policy.
24. Reason for registration of Complaint: Repudiation of claim.
25. The following documents were placed for perusal:
d) Copy of policy.
e) Copy of Discharge Summary, Bill, Receipt, Reports etc.
f) Copy of Rejection letter.
g) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent. Insurer is present and has also vide letter dated 19.12.2019
informed this forum that they have already settled the claim for Rs. 83,245 and released the same
on 6.11.2019, which appears reasonable.
Award
The complaint is allowed in terms of the settlement, already made by the Insurer by way
of payment of an amount Rs. 83,245 to the Complainant on 6.11.2019.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
30
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Anindita Chakravorty V/s The New India Assurance Company Ltd.
Complaint Ref. No.: DEL-H-049-1920-0320
Case No.: GI/NIA/227/19
1.
Name & Address of the Complainant
Smt. Anindita Chakravorty.
No. B- 807, Kenwood Tower, Charmwood,
Surajkund, Faridabad-121009

2.
Policy No.
Type of Policy
Policy term/Policy Period
31250034172500000066
Medi claim Policy
23.04.2017 to 22.04.2018.
3.
Name of the insured
Name of the policy holder
Smt. Anindita Chakravorty
Shri Arun Kumar Chakravorty
4.
Name of insurer
The New India Assurance Company Ltd.
5.
Date of Repudiation
27.05.2019
6.
Reason for Grievance
Repudiation
7.
Date of receipt of the Complaint
22.08.2019.
8.
Nature of Complaint
Repudiation
9.
Amount of Claim
Rs.40000/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs.40000/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing
24.12.2019
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Shri Arun Kumar Chakravorty- Husband
b) For the Insurer
Shri Sunil Saraf- AO.
16.
Date of Award/Order
30.12.2019.
17. Brief Facts of the Case
Smt. Anindita Chakravorty (hereinafter referred to as the complainant) had filed the complaint
against the decision of The New India Assurance Company Ltd. (hereinafter referred to as the
Respondent Insurance Company) alleging wrong repudiation of her mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated vide her letter dated
16.08.2019 that she was hospitalized at Visitech Eye Centre, Delhi for the period
from 13.01.2018 to 13.01.2018 for the treatment of her Right Eye by I/V Ozurdex
Injection, for which she had submitted all the claim documents to the Insurance
Company for Rs.40000/-. The said claim was repudiated by the Insurance Company
on the basis of treatment by Injection Ozurdex is not payable under the policy. She
represented her case before the Insurance Company vide her letter dated 08.04.2019
and requested for payment of the said claim, but got no relief. Hence, she has now
approached this forum for relief.
b) Insurer's Argument: The Insurance Company, vide its letter dated 27.05.2019, has
stated that treatment by Injection Ozurdex is not payable under the policy. In their
Self Contained Note dated 15.10.2019, the Company reiterated that treatment of eye
by Injection Ozurdex is not payable under the policy, because the same are not
included in Day Care Procedure list in the policy.
19. Reason for registration of Complaint: Repudiation of claim
20. The following documents were placed for perusal.
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present. Complainant states that Injection Ozurdex was the only remedy
available for the ailment of his wife, but this injection was to be administered only as a Daycare
procedure. Insurer states that as per clause 2.16 of the policy, read with Annexure- I, this injection
is not listed in the list of procedures admissible for reimbursement in Daycare mode of treatment.
Complainant states that he was not provided with the policy terms & conditions. Insurer states that
the policy was renewed by the Complainant online and while doing so, he could have as well
downloaded the policy terms & conditions too.
Complainant states that his complaint about repudiation of a similar claim was allowed by this
forum in Case No. GI/NIA/307/18 vide Award dated 11.10.2019. Insurer admits that during the
hearing for that case, he could not cite relevant clause/ provision of the policy, which excludes
payment of claim for treatment by Injection Ozurdex, and the complaint was allowed accordingly.

In the present case, it is concluded that this treatment was not admissible under ‘Daycare’ category
and hence the repudiation of claim was justified.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
30
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Pawan Chuphal versus Apollo Munich Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-003-1920-0305
Case No.: GI/Apollo/212/19
1.
Name & Address of the Complainant
Shri Pawan Chuphal
8233, 2
nd
. Floor, L.R. Builders, Rani Jhansi Road, New
Delhi-110006.
2.
Policy No.
Type Of Policy
Policy term/Policy Period
110106/11119/AA00679259-01
Mediclaim Policy
07.10.2018 to 06.10.2019.
3.
Name of the insured
Name of the policy holder
Shri Pawan Chuphal
Shri Pawan Chuphal
4.
Name of insurer
Apollo Munich Health Insurance Company Ltd.
5.
Date of Repudiation
20.07.2019.
6.
Reason For Grievance
Rejection of claim
7.
Date of receipt of the Complaint
16.08.2019.
8.
Nature of Complaint
Rejection of claim
9.
Amount of Claim
Rs.172500/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs. 172500/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims
by an insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
For the Complainant
Absent
For the Insurer
Dr. Mohammad Danish- AM.
16.
Date of Award/Order
31.12.2019.
17. Brief Facts of the Case
Shri Pawan Chuphal (herein after referred to as the complainant) had filed the complaint against the
decision of Apollo Munich Health Insurance Co. Ltd. (hereinafter referred to as the Respondent
Insurance Company) alleging wrong rejection of mediclaim.
18. Cause of Complaint:
c) Complainant's Argument: The complainant, vide his letter dated 16.08.2019, has stated that a
biker hit him and he fell down and got injury. He was hospitalized at Sir Gangaram Hospital for the
period from 24.07.2019 to 25.07.2019 and was diagnosed as ACL Tear with Medial and Lateral
Maniscus Tear Left Knee. He submitted the claim for Rs.172500/-, which was rejected by the
company on the ground of 2 Years Waiting Period. He represented his case before the Insurance
Company vide his e-mail dated 23.07.2019 for payment of his claim, but he got no relief. He has
now approached this forum for relief.
d) Insurer's Argument: The Insurance Company had stated vide their rejection letter dated
20.07.2019 that treatment of ACL Tear (diagnosis/ ailment/ procedure) has a specific two year
waiting period as per policy condition. They have not submitted their Self Contained Note till date.
19. Reason for registration of Complaint: Rejection of claim.

20. The following documents were placed for perusal.
e) Copy of policy.
f) Copy of Discharge Summary, Bill, Receipt, Reports etc.
g) Copy of Rejection letter.
h) Billing Sheet dated 19.12.2019 for Rs. 1,70,976/- of the Insurer.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent. His claim is for Rs. 1,70,976/-.
Insurer is present and states that they have decided to settle the claim for Rs. 93,635/- and are also willing
to examine the claim in respect of the remaining amount also, subject to submission of the documents by
the Complainant soon.
I find the offer of the Insurer reasonable, though an agreement to this effect could not be signed by the
parties today owing to the absence of the Complainant.
Award
The complaint is allowed in terms of the offer of the Insurer to settle the claim for Rs. 93,635/- and also
to examine the claim in respect of the remaining amount, subject to submission of the documents by the
Complainant within 15 days.
.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
31
st
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Pawan Kumar versus Apollo Munich Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-003-1920-0312
Case No.: GI/Apollo/219/19
1.
Name & Address of the Complainant
Shri Pawan Kumar
272- B, Munrika Village, New Delhi-110067
2.
Policy No.
Type Of Policy
Policy term/Policy Period
110101/11121/AA00531939-02
Mediclaim Policy
09.01.2019 to 08.01.2020.
3.
Name of the insured
Name of the policy holder
Shri Pawan Kumar
Shri Pawan Kumar
4.
Name of insurer
Apollo Munich Health Insurance Company Ltd.
5.
Date of Repudiation
14.07.2018.
6.
Reason For Grievance
Rejection of claim due to 2 Years Waiting Period
7.
Date of receipt of the Complaint
02.09.2019.
8.
Nature of Complaint
Rejection of claim
9.
Amount of Claim
Rs.559544/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs. 559544/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a) For the Complainant
Shri Pawan Kumar – Self.
b) For the Insurer
Dr. Mohammad Danish- AM.
16.
Date of Award/Order
02.01.2020.
17. Brief Facts of the Case
Shri. Pawan Kumar (herein after referred to as the complainant) had filed the complaint
against the decision of Apollo Munich Health Insurance Company Ltd. (hereinafter referred to
as the Respondent Insurance Company) alleging wrong rejection of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant, vide his letter dated 28.08.2019, has
stated that he was hospitalized at Medanta Hospital for the period from 15.07.2018 to
20.07.2018. He submitted the claim for Rs. 559544/- which was rejected by the
company on the ground of 2 Years Waiting Period. He represented his case before the

Insurance Company vide his e-mail dated 24.11.2018 for payment of his claim, but he
got no relief. He has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company had stated vide their rejection letter
dated 14.07.2018 that treatment of Bronchial Carcinoid is excluded from the policy, if
admitted in 2 years of policy inception date. In their Self Contained Note
dated19.12.2019, they have stated that they had closed the claim for non submission of
documents, investigation reports and detailed Discharge Summary.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) Self Contained Note.
e) Conciliatory Settlement Agreement
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present.
Insurer states that the Complainant had provided all documents relating to his illness. However, while
scrutinizing the documents, Insurer discovered that the child of the Complainant was suffering from a
congenital disease, which the Complainant had not disclosed while taking the policy. Complainant states
that he has studied only upto Class-IX and was advised by the agent not to disclose the ailment of his child
while applying for the policy. Complainant states that he became aware of the matter only when the
Insurer started their inquiry for this claim. Complainant agrees to remove his child from the policy
coverage.
Parties sign an agreement to the effect that the congenital heart afflictions of the minor son (Sh. Ansh)
of the Complainant shall be excluded from the coverage of the policy from its commencement and the
pending claim No. 863772 of the Complainant shall be settled within 30 days.
I find this agreement fair and reasonable.
Award
The complaint is allowed in terms of the conciliatory settlement agreement signed by the
parties today. Accordingly, the congenital heart afflictions of the minor son (Sh. Ansh) of
the Complainant shall be excluded from the coverage of the policy from its commencement
and the pending claim No. 863772 of the Complainant shall be settled within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
2
nd
January, 2020.
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Rahul Saini versus Apollo Munich Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-003-1920-0307
Case No.: GI/Apollo/214/19
1.
Name & Address of the Complainant
Shri Rahul Saini
6032, Soloman Heights, Sector- 19 B, Dwarka, New Delhi-
110075.
2.
Policy No.
Type Of Policy
Policy term/Policy Period
160100/11229/AX00003379-02
Mediclaim Policy
15.06.2018 to 14.06.2019.
3.
Name of the insured
Name of the policy holder
Smt. Monika Saini
Shri Rahul Saini
4.
Name of insurer
Apollo Munich Health Insurance Company Ltd.
5.
Date of Repudiation
18.02.2019.
6.
Reason For Grievance
Rejection of claim due to 2 Years Waiting Period
7.
Date of receipt of the Complaint
08.08.2019.
8.
Nature of Complaint
Rejection of claim
9.
Amount of Claim
Rs.155392/-

10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs. 155392/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017.
Rule 13(1)(b) – any partial or total repudiation of claims
by an insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a. For the Complainant
Absent
b. For the Insurer
Dr. Mohd. Danish, Asst. Manager
16.
Date of Award/Order
02.01.2020.
17. Brief Facts of the Case
Shri. Rahul Saini (hereinafter referred to as the complainant) had filed the complaint against the
decision of Apollo Munich Health Insurance Company Ltd. (hereinafter referred to as the
Respondent Insurance Company) alleging wrong rejection of his wife’s mediclaim.
18. Cause of Complaint:
a. Complainant's Argument: The complainant, vide his letter dated 02.08.2019, has stated that his
wife was hospitalized at Venkateshwar Hospital for the period from 22.12.2018 to 25.12.2018
for the treatment of constipation, urinary retention, breathlessness etc. He submitted the claim for
Rs. 155392/-, which was rejected by the company on the ground of maternity related disorders,
which are subject to 2 Years Waiting Period. He represented his case before the Insurance
Company vide his letter dated 10.06.2019for payment of his claim, but got no relief. He has now
approached this forum for relief.
b. Insurer's Argument: The Insurance Company had stated vide their rejection letter dated
18.02.2019 that the patient was admitted for management of a condition, which is related to
maternity and its related disorders, which is not covered under Section 5 C VIII o of the policy.
In their Self Contained Note dated 20.12.2019, they have reiterated the same.
19) Reason for registration of Complaint: Rejection of claim.
20) The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) Self Contained Note.
21) Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent. Insurer is present and reiterates the averments as noted in
Para 18b above.
The diagnosis of the insured during the hospitalization as per the discharge summary dated
25.12.2019 reports her ailments as, inter alia, post partum cardiomyopathy, global hypokinesis
LVEF etc., which are related to maternity, birth (caesarian) which is specifically excluded under
Medical Exclusion Clause viii(o) of the policy. Therefore, repudiation of this claim was justified.
Complainant has mentioned about three other claims also, which were repudiated by the
Insurer. However, Complainant has not submitted the discharge summary in respect of those
claims. The Insurer states that out of these three claims, two relate to the same cause and
deserve to be treated on the same footing, whereas the last claim relates to an OPD based
treatment, which is not covered in this policy at all.
Keeping the facts narrated above in view, the complaint deserves to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
2
nd
January, 2020.

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Anil Jain versus Manipal Cigna Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-053-1920-0304
Case No.: GI/Cigna/211/19
1.
Name & Address of the Complainant
Shri Anil Jain
J- 1/ 51, Budh Vihar, Phase- 1, Delhi-110086.
2.
Policy No.
Type Of Policy
Policy term/Policy Period
PROCSH980427087
Health Policy
31.01.2019 to 30.01.2020.
3.
Name of the insured
Name of the policy holder
Shri Anil Jain
Shri Anil Jain
4.
Name of insurer
Manipal Cigna Health Insurance Company Ltd.
5.
Date of Repudiation
04.06.2019.
6.
Reason For Grievance
Rejection of claim
7.
Date of receipt of the Complaint
20.08.2019.
8.
Nature of Complaint
Rejection of claim
9.
Amount of Claim
Rs.74982/-
10.
Date of Partial Settlement
NA
11.
Amount of Partial Settlement
NA
12.
Amount of relief sought
Rs. 74982/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation
of claims by an insurer
14.
Date of hearing
24.12.2019.
Place of hearing
Delhi
15.
Representation at the hearing
a. For the Complainant
Shri Anil Jain, Complainant
b. For the Insurer
Shri Darpan Gupta, Agency Manager
16.
Date of Award/Order
02.01.2020.
17. Brief Facts of the Case
Shri Anil Jain (herein after referred to as the complainant) had filed the complaint against the
decision of Manipal Cigna Health Insurance Company Ltd. (hereinafter referred to as the
Respondent Insurance Company) alleging wrong rejection of his mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant, vide his letter dated 16.08.2019, has stated that
he was hospitalized at Cygnus Sonia Hospital for the period from 20.04.2019 to 28.04.2019
for the treatment of RTA Head Injury and Chest Pain. He submitted the claim for Rs. 74982/-,
which was rejected by the company on the ground of incorrect statements, misrepresentation
or non-disclosure of material particulars in the proposal form. He represented his case before
the Insurance Company vide his e-mail dated 04.06.2019 for payment of his claim, but he got
no relief. He has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company had stated vide their rejection letter dated
04.06.2019 that they rejected the said claim on the ground of incorrect statements,
misrepresentation or non disclosure of material particulars in the proposal form. In their Self
Contained Note dated 20.12.2019, they have reiterated the same.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Receipt, Reports etc.
c) Copy of Rejection letter.
d) Self Contained Note.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant states that he holds two policies from this Insurer. One is Policy No.
PROHLN000099248, which is for cashless mediclaim, while the other is Policy No.
PROCSH980427087, which is for cash benefit during hospitalisation. He was hospitalized during 20-
28 April 2019, for which the Insurer settled the cashless claim under Policy No. PROHLN000099248.
However, the Insurer did not provide cash benefit under Policy No. PROCSH980427087.

Insurer states that the claim was repudiated on the grounds of serious discrepancies and
manipulation found in the documents submitted for the claim. The cashless mediclaim was settled
by the Insurer based on the documents received from the hospital, in good faith. However, while
scrutinizing the claim for the cash benefits, the company found many discrepancies. For instance,
the discharge summary notes head injury as the cause of admission whereas the MRI report is for
shoulder and back and not for head. Also, the Complainant on admission had complained of chest
pain but no report of radiology etc. was submitted for the chest. The vital charts seem fudged, for
which Insurer has given details.
The discrepancies in the documents submitted by the Complainant for the claim are serious
enough to justify repudiation of the claim.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
2
nd
January, 2020.
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Shanti Lal Bothra versus National Insurance Company Ltd.
Complaint Ref: DEL: H-048-1920-0315
Case No: HI/NIC/222/19
17. Brief Facts of the Case:
Shri Shanti Lal Bothra (herein after referred to as Complainant) had filed a complaint against the decision of
National Insurance Company Ltd (herein after referred to as respondent Insurance Company) alleging wrong
repudiation of claim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that he had taken a mediclaim policy from the
National Insurance Company Ltd. He was admitted in Sant Parmanand Hospital, Delhi from 22.04.2019 to
23.04.2019. The Insurance Company had repudiated his claim, on the ground that hospitalization was not
required. The complainant wrote a letter to grievance redress department of Insurance Company, and
has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company has stated in their Self Contained Note that as per
discharged summary, the complainant was found quite normal, in all respect. The complainant was
1.
Name & Address of the Complainant
Shri Shanti Lal Bothra, 1619, 2
nd
Floor, Outram Line,
G.T.B. Nagar, Kingsway Camp, New Delhi 110009
2.
Policy No:
Type of Policy
Duration of policy/Policy period
360700501810002279
Mediclaim
21.07.2018 to 20.07.2019
3.
Name of the insured
Name of the Policy holder
Shri Shanti Lal Bothra
Shri Shanti Lal Bothra
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
13.08.2019
6.
Reason for repudiation
Admission for Investigations Purpose only.
7.
Date of receipt of the Complaint
04.09.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 29991/-
10.
Date of Partial Settlement
N.A.
11.
Amount of Partial Settlement
N.A.
12.
Amount of relief sought
Rs. 29991/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.
14.
Date of hearing/place
12.12.2019 / Delhi
15.
Representation at the hearing
For the Complainant
Shri Anil Kumar
For the insurer
Shri P. K. Bakshi, Dy. Manager.
16.
Complaint how disposed/ date of
Award/Order
Award /16.12.2019

admitted only for investigation purpose and hospitalization was not medically necessary, hence claim
has been repudiated as per policy clause no 4.22.
19. Reason for registration of Complaint: Admission for Investigations Purpose only.
20. The following documents were placed for perusal:
a) Self Contained Note
b) Discharged summary
c) Policy Documents
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
The discharge summary has noted that the Complainant was a known case of suffering from diabetes,
hypertension CKD, anemia and peripheral neuropathy. However, the purpose for which he was
hospitalized is stated as general body ache and tingling sensation in hand and feet for 10-12 days. The
discharge summary also states that during the hospitalization, he was treated conservatively. All this had
led the Insurer to conclude that hospitalization was not necessary.
The inference of the Insurer appears reasonable and accordingly, the complaint deserves to be rejected.
Award
, The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Rohit Bansal versus Max Bupa Insurance Co. Ltd.
Complaint Ref: DEL-H-031-1920-0280
Case No: HI/MAX/194/19
17. Brief Facts of the Case:
Shri Rohit Bansal (hereinafter referred to as the Complainant) has filed a complaint against the decision of
Max Bupa Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company) alleging wrong
repudiation of claim
18. Cause of Complaint:
1.
Name & Address of the Complainant
Shri Rohit Bansal, D-159, 2
nd
Floor, Kamla Nagar,
New Delhi 110007
2.
Policy No:
Type of Policy
Duration of policy/Policy period
30362122201804
Mediclaim
23.09.2018 To 22.09.2019
3.
Name of the insured
Name of the Policy holder
Smt Swati Bansal
Shri Rohit Bansal
4.
Name of the insurer
Max Bupa Insurance Co. Ltd.
5.
Date of Repudiation
31.01.2019
6.
Reason for repudiation
Non-disclosure of material fact of P.E.D.
7.
Date of receipt of the Complaint
30.07.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
Rs. 551767
10.
Date of Partial Settlement
N.A.
11.
Amount of Partial Settlement
N.A.
12.
Amount of relief sought
Rs. 551767
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract
14.
Date of hearing/place
12.12.2019 / Delhi
15.
Representation at the hearing
For the Complainant
Shri Rohit Bansal
For the insurer
Ms Chandrika Bhattacharyya- Chief Manager (Legal)
16.
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019

a) Complainant’s Argument: The complainant has stated that he had taken a mediclaim insurance policy
for himself and his family from Max Bupa Insurance Company, and the Insurance Company had done all the
pre medical tests before issuing the Insurance policy and the complainant had declared the previous illness
(Surgery of stomach) of his wife to the Insurance Company. The complainant has also stated that the
Insurance Company had already passed the claim of his wife for the Chronic Pancreatitis in the month of
May 2017.
His wife was again admitted to the Apollo Hospital for breast cancer in the month of November 2019 and
the Insurance Company initially sent an approval of Rs. 99245 but later on declined their claim, citing non-
disclosure of material facts as reason. The complainant wrote a letter to G.R.O. of Insurance Company. He
has now approached this forum for relief.
b) Insurer’s Argument: The Insurance Company has stated that they are willing to settle this claim, and
accordingly have sent a mail to the complainant on 04.12.2019, but till date no revert has been received.
19. Reason for registration of Complaint: Repudiation of claim
20. The following documents were placed for perusal:
a) Self Contained Note by Insurer
b) Policy document
c) Discharged summary
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
Insurer offers to settle the Claim No. 384530 for Rs. 5,49,513 and Claim No. 391226 for Rs. 1,08,060 and
also to reinstate the policy subject to payment of renewal premium dues. Insurer shall also examine and
settle the other pending claims of the Complainant after renewal of the policy. Complainant accepts this
offer and parties sign a conciliation agreement to this effect, which I find fair and reasonable to both.
Award
The complaint is allowed in terms of the conciliation agreement signed by the parties today.
Accordingly, the Insurer should settle the claim No. 384530 for Rs. 5,49,513 and claim No. 391226 for Rs.
1,08,060 and also to reinstate the policy within 30 days subject to payment of renewal premium dues.
Insurer should also examine and settle the other pending claims of the Complainant after renewal of the
policy.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Ram Kumar Tanwar versus Star Health and Allied Insurance Co. Ltd.
Complaint Ref: DEL-H-044-1920-0314
Case No: HI/STAR/221/19
1.
Name & Address of the Complainant
Shri Ram Kumar Tanwar,
WZ-509, Basai Darapur, Delhi
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P 161121/01/2019/017599
Mediclaim
04.03.2019 To 03.03.2020
3.
Name of the insured
Name of the Policy holder
Shri Nand Kishore
Shri Ram Kumar Tanwar
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
26.03.2019
6.
Reason for repudiation
Non-disclosure of material fact
7.
Date of receipt of the Complaint
02.09.2019
8.
Nature of complaint
Repudiation of Mediclaim & Cancelation of policy.
9.
Amount of Claim
Rs. 22066
10.
Date of Partial Settlement
N.A.
11.
Amount of Partial Settlement
N.A.
12.
Amount of relief sought
Rs. 22066
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.

17. Brief Facts of the Case:
Shri Ram Kumar Tanwar (herein after referred to as Complainant) had filed a complaint against the
decision of Star Health and Allied Insurance Company Ltd. (hereinafter referred to as the Respondent
Insurance Company) alleging wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The complainant has stated that he had taken a star health medi- classic
policy for his brother from Star Health and Allied Insurance Company. The Insurance Company had done
all requisite medical tests of insured person at the inception of policy. His brother had some breathing
problem in the month of January 2019 and was admitted in Vallabh Bhai Patel Chest Institute,
Department of Respiratory Medicine, Delhi, and discharged from the hospital in the month of February
2019. The complainant had received a mail on 26.03.2019 from the Insurance Company regarding
repudiation of claim citing non-disclosure of pre-existing diseases, as reason for repudiation. The
complainant wrote a letter to the Grievance. Redressal Officer of the Insurance Company and got a mail
from that department, in which they had suggested to change the comprehensive policy to Medi Classic
(Rs. 2 lakh) policy. The complainant has now approached this forum for relief.
b) Insurer's Argument: The Insurance Company have telephonic informed us on 03.12.2019., that they
are settling this claim. Now we have received a mail from the complainant, originally addressed to the
Insurance Company in which complainant agree to withdraw his case from this office.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Policy document.
b) Claim rejection letter from Insurance Company.
c) Letter to the Grievance Redressal Officer of the Insurance Company.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
Insurer informs that they have reviewed the matter and decided to accept the claim and also restore the
policy. Complainant accepts this offer but still expresses grievance about the delay in settlement of his
claim, which I consider to be a reasonable grievance.
Award
The complaint is allowed in terms of the offer of the Insurer to accept and settle the claim and also
restore the policy. In addition, Insurance Company should also pay to the Complainant interest for
delayed payment for the period commencing from the date the Complainant submitted the required
documents till the date the payment of claim is actually made, as prescribed under the Insurance
Regulatory and Development Authority of India (Protection of Policyholders’ Interests) Regulations,
2017.
Insurance Company should implement this award within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Praveen Garg versus Max Bupa Health Insurance Co. Ltd.
Complaint Ref: DEL-H-031-1920-0289
Case No: HI/MAX/200/19
14.
Date of hearing/place
12.12.2019, Delhi
15.
Representation at the hearing
For the Complainant
Shri Ram Kumar Tanwar
For the insurer
Shri Mantosh Kumar-Manager
16.
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019
1.
Name & Address of the Complainant
Shri Praveen Garg, 1601, Tower 12, Valley View Estate,
Gwal Pahari, Gurugram, Haryana-122003
2.
Policy No:
Type of Policy
Duration of policy/Policy period
30181907201906
Mediclaim
13.02.2019 to 12.02.2020
3.
Name of the insured
Name of the Policy holder
Shri Rahul Garg
Smt. Chhaya Garg
4.
Name of the insurer
Max Bupa Health Insurance Company Ltd.
5.
Date of Repudiation
30.06.2019
6.
Reason for repudiation
Non-disclosure of P.E.D.

17. Brief Facts of the Case:
Shri Praveen Garg (hereinafter referred to as Complainant) has filed a complaint against the decision of
Max Bupa Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company)
alleging wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The complainant has stated that he had submitted a claim on 25
th
May
2019 for his son to the Max Bupa Insurance Company. On 19
th
June 2019, he got a letter from the
Insurance Company, stating that the claim and policy stands cancelled as per policy condition No. 3, for
non-disclosure of pre-existing disease. The complainant stated that he had informed Paras Hospital at
the time of admission of his son (who attended head injury case of his son) that his son was on
psychiatric medication for the last 10-12 years, but at the time of injury he was conscious and
cooperative. The complainant also stated that the Insurance Company denied his genuine claim on
account of mis-interpretation of policy terms. He wrote a letter to grievance cell of the Insurance
Company. The complainant has now approached this forum for relief.
b) Insurer’s Argument: The Insurance Company have stated in Self Contained Note that as per
documents submitted by the complainant and as per Investigation report, it was found that his son had
a history of taking psychiatric medication for the last 10 to 12 years and, therefore, it was non-
disclosure of material facts. Hence the claim had been rejected and policy stands cancelled as per
policy terms and condition No 10.21.
19. Reason for registration of Complaint: Rejection of claim and cancellation of policy.
20. The following documents were placed for perusal:
a) Self Contained Note
b) Policy Documents
c) Claim rejection letter.
21. Result of hearing of both parties (Observations and Conclusion):
Case called. Parties are present.
Insurer had rejected the claim and canceled the policy on the grounds of non-disclosure of pre-existing
ailment. Insurer had come to this conclusion based on the OPD card of Paras Hospital which notes, inter
alia, that the patient had a history of taking psychiatric medication for 10-12 years. Complainant states
that the patient has been taking such medication as and when required and not on regular basis.
Insurer states that the incidence which has led to claim was made this was materially related to the
issuance of the policy inasmuch as the Insurer would not have issued the policy itself.
Complainant has also argued about the apparent defects in the policy terms & conditions. However, the
case has been examined by this forum in terms of the existing policy documents.
It is apparent from the facts, evidence and circumstances submitted by the parties that the insured patient
was suffering from psychiatric ailment and was on medication for past 10-12 years, which was material
information for issuance of the policy but was not disclosed by the policy holder while applying for the
policy in 2013. Hence the Insurer was justified in cancelling the policy and repudiating the claim.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman Delhi
16
th
December, 2019
7.
Date of receipt of the Complaint
16.07.2019
8.
Nature of complaint
Repudiation of claim and cancellation of policy
9.
Amount of Claim
Rs. 15546
10.
Date of Partial Settlement
N.A.
11.
Amount of Partial Settlement
N.A.
12.
Amount of relief sought
Rs. 15546
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.
14.
Date of hearing/place
12.12.2019 / Delhi
15.
Representation at the hearing
For the Complainant
Shri Praveen Garg
For the insurer
Ms Chandrika Bhattacharyya- Chief Manager (Legal)
16.
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Mohan Namdeo versus Star Health and Allied Insurance Co. Ltd.
Complaint Ref: DEL-H-044-1920-0283
Case No: HI/STAR/197/19
17. Brief Facts of the Case:
Shri Mohan Namdeo (hereinafter referred to as the Complainant) has filed a complaint against
Star Health and Allied Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance
Company) alleging non-settlement of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The complainant has stated that he had taken a family floater
mediclaim policy of Star Health and Allied Insurance Co. He had lodged an O.P.D. benefit claim
on Insurance Company, but despite various reminders, complainant has not received any
response from Insurance Company. He has now approached this forum for relief.
b) Insurer’s Argument: The Insurance Company has stated in Self Contained Note that the
complainant is seeking O.P.D. benefits/expenses. As per internal verification made by the
Insurance Company, it was observed that the complainant had not given any claim intimation
about the hospitalization to the Insurance Company. The Insurance Company has further stated
that “the terms and conditions of policy were explained to the complainant at the time of
proposing policy and same was served to the complainant along with Policy Schedule”, hence
O.P.D. benefit could not be processed.
19. Reason for registration of Complaint: Non settlement of claim.
20. The following documents were placed for perusal:
a) Self Contained Note from the Insurer
b) Policy Document
c) Claim Rejection Letter
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
Insurer has not settled the claim so far on the grounds that the Complainant had not given prior
intimation before taking the consultation. The policy document states that ‘admission intimation
to be given within 24 hours’. However, there was no admission involved here, being mere OPD
1.
Star Health and Allied Insurance
Company Ltd
Shri Mohan Namdeo, B-456, Rockview Officer’s
Enclave, Air Force Station Palam, New Delhi 110010
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P 231114/01/2016/000340
Mediclaim
18.05.2015 to 17.05.2016
3.
Name of the insured
Name of the Policy holder
Shri Mohan Namdeo,
Shri Mohan Namdeo,
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
N.A.
6.
Reason for repudiation
N.A.
7.
Date of receipt of the Complaint
01.08.2019
8.
Nature of complaint
Non settlement of claim
9.
Amount of Claim
N.M.
10
Date of Partial Settlement
N.A.
11
Amount of Partial Settlement
N.A.
12
Amount of relief sought
N.M.
13
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.
14
Date of hearing/place
12.12.2019 / Delhi
15
Representation at the hearing
For the Complainant
Shri Mohan Namdeo
For the insurer
Shri Mantosh Kumar- Manager.
16
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019

consultation. The policy document does not require the policy holder to give prior intimation to
the Insurer for OPD treatment. Therefore, Insurer should settle the claim forthwith.
Award
The complaint is allowed and the Insurer is directed to settle the claim and also pay to the Complainant
interest for delayed payment for the period commencing from the date the complainant submitted the
required documents till the date the payment of claim is actually made, as prescribed under the
Insurance Regulatory and Development Authority of India (Protection of Policyholders’ Interests)
Regulations, 2017.
Insurance Company should implement this award within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Deepak Mani versus The Max Bupa Health Insurance Co. Ltd.
Complaint Ref: DEL-H-031-1920-0317
No: HI/Max/224/19
17. Brief Facts of the Case:
Shri Deepak Mani (herein after referred to as Complainant) had filed a complaint against the decision
of Max Bupa Health Insurance Company Ltd. (herein after referred to as respondent Insurance
Company) alleging inadequate settlement of mediclaim.
18. Cause of Complaint:
Complainant's Argument:
a) The complainant stated that he had taken a mediclaim policy of Max Bupa Health Insurance Company Ltd.
He was admitted in Shri Moolchand Kharaiti Ram Hospital & Ayurvedic Research Institute from 21.11.2018 to
22.11.2018. He got initial approval for Rs 69000 from the Insurance Company, while the total bill was for Rs.
77337, but the final amount paid by the Insurance Company to the complainant was Rs. 52762. Complainant
wrote a letter to grievance cell of Insurance Company. He has now approached this forum for relief.
b) Insurer’s Argument:
The Insurance Company have stated in their Self Contained Note that the complainant’s claim was
repudiated on the ground that the Insurance Company had approved and paid the approved amount to the
1.
Name & Address of the Complainant
Shri Deepak Mani, H.No. 2D, Mansarovar Apartment,
Sector 61, Gautam Bodh Nagar, Uttar Pradesh- 201307
2.
Policy No:
Type of Policy
Duration of policy/Policy period
30476989201803
Mediclaim
24.11.2018 To 23.11.2019
3.
Name of the insured
Name of the Policy holder
Shri Deepak Mani
Shri Deepak Mani
4.
Name of the insurer
Max Bupa Health Insurance Co. Ltd.
5.
Date of Repudiation
21.08.2019
6.
Reason for repudiation
N.A.
7.
Date of receipt of the Complaint
27.08.2019
8.
Nature of complaint
Inadequate settlement of mediclaim
9.
Amount of Claim
Rs. 24575/-
10
Date of Partial Settlement
19.11.2018
11
Amount of Partial Settlement
Rs. 52762/-
12
Amount of relief sought
Rs. 24575/-
13.
Complaint registered under Rule no:
Insurance Ombudsman rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.
14
Date of hearing/place
12.12.2019 / Delhi
15
Representation at the hearing
For the Complainant
Shri Deepak Mani
For the insurer
Ms Candrika Bhattacharyya.- Chief Manager (Legal)
16.
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019

complainant in main claim. The complainant had filed the subsequent claim for disallowed amount which was
deducted as per the terms and condition of the policy, as proportionate deduction has been applied.
19. Reason for registration of Complaint: Inadequate settlement of mediclaim
20. The following documents were placed for perusal:
a) Policy Documents
b) Rejection letter by Insurance Company
c) Self Contained Note
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
Complainant had submitted claim for Rs. 77,337, against which Insurer settled the same for Rs. 52,762,
disallowing the balance claim of Rs. 24,575. Complainant is seeking payment of some part at least, stating that
on certain items like higher room rent (Rs.4,350), he has no grievance.
At this stage, Insurer offers to settle the remaining claim for Rs.10,000. Complainant accepts this offer and
parties sign a conciliation agreement to this effect, which I find fair and reasonable.
Award
The complaint is allowed in terms of the conciliation agreement signed by the parties today.
Accordingly, Insurer should pay a further sum of Rs. 10,000 towards full and final settlement of Claim
No. 387996 in respect of Policy No. 30476989201803, within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Dev Mohan Gupta versus Max Bupa Health Insurance Co. Ltd.
Complaint Ref: DEL-H-031-1920-0326
Case No: HI/MAX/232/19
17. Brief Facts of the Case:
Shri Dev Mohan Gupta (hereinafter referred to as the Complainant) has filed a complaint against the decision
of Max Bupa Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company)
alleging wrong repudiation of claim.
18) Cause of Complaint:
1.
Name & Address of the Complainant
Shri Dev Mohan Gupta, 1, Under Hill Lane, S.O., Civil
Lines, New Delhi 110010
2.
Policy No:
Type of Policy
Duration of policy/Policy period
36810/04201800
Mediclaim
27.09.2018 To 26.09.2019
3.
Name of the insured
Name of the Policy holder
Shri Dev Mohan Gupta
Shri Dev Mohan Gupta
4.
Name of the insurer
Max Bupa Health Insurance Co. Ltd.
5.
Date of Repudiation
20.08.2019
6.
Reason for repudiation
P.E.D. Exclusion
7.
Date of receipt of the Complaint
06.09.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 194113/-
10
Date of Partial Settlement
N.A.
11
Amount of Partial Settlement
N.A.
12
Amount of relief sought
Rs. 194113
13
.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.
14
Date of hearing/place
12.12.2019 / Delhi
15
Representation at the hearing
For the Complainant
Shri Dev Mohan Gupta
For the insurer
Ms Chandrika Bhattacharyya- Chief Manager (Legal)
16
.
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019.

a) Complainant’s Argument: The complainant has stated that he had taken a mediclaim policy, without any
exclusion from Max Bupa Health Insurance Company Ltd. The complainant was admitted in Fortis Escort
Hospital from 14.04.2019 to 13.04.2019, and lodged a claim on Insurance Company. The Insurance
Company had denied the claim & cancelled the policy due to non-disclosure of pre-existing disease viz
Hypertension, CAD Balloon Angioplasty, COPD. The complainant has stated that Ballooning Angioplasty
was not available in India in the year 1980. The complainant wrote a letter to grievance redress
department of Insurance Company. He has now approached this forum for relief.
b) Insurer’s Argument: The Insurance Company has stated in their Self Contained Note that as per
Investigation report and documents shared by complainant, the complainant had suppressed the material
facts about his health condition; he was suffering from coronary artery disease, which falls prior to policy
inception date, and therefore PED exclusion applies. Hence claim was repudiated under policy clause no 7.1,
and policy stands canceled as per policy clause no. 12.20.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Self Contained Note of Insurance Company
b) Policy document
c) Discharge summary
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
Complainant has submitted certificate dated 14.5.2019 from Dr. Ashok Seth of Fortis Hospital stating that the
Outpatient Record of the hospital has wrongly mentioned that he is a patient of CABG (Bypass surgery).
However, Insurer states that the same doctor had noted in the Pre-authorisation form on 15.4.2019 that the
Complainant was having past history of heart disease since 1996 and this was also signed by the Complainant
in the same form.
Insurer has produced copy of the prescription dated 18.5.2017 from Dr. Ashwani Gupta of Sir Gangaram
Hospital, which states that the Complainant has a history of hypertension since 50 years and that CAD-heart
ballooning was done by Dr. A Seth in 1984. Complainant submits a certificate form Dr. Ashwani Chopra which
states that the technology of ballooning did not exist in 1980.
The conflicting certificates given by the doctors make the same unreliable.
It is apparent from the facts, evidence and circumstances submitted by the parties that the Complainant was
suffering from ailments of Hypertension for 50 years and had got ballooning done in 1984. These were
material information for issuance of the policy but the Complainant had not disclosed all these facts while
applying for this policy in September 2018. Hence the Insurer was justified in cancelling the policy and
repudiating the claim.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Charan Singh versus The National Insurance Co. Ltd.
Complaint Ref: DEL-H-048-1920-0322
Case No: HI/NIC/229/19
1.
Name & Address of the Complainant
Shri Charan Singh, WZ-564/A, Naraina Village,
New Delhi 110015
2.
Policy No:
Type of Policy
Duration of policy/Policy period
360300501810000944
Mediclaim
25.05.2018 to 24.05.2019
3.
Name of the insured
Name of the Policy holder
Smt Kamlesh
Shri Charan Singh
4.
Name of the insurer
The National Insurance Co. Ltd.
5.
Date of Repudiation
15.11.2018
6.
Reason for repudiation
Use of Drug/alcohol abuse

17. Brief Facts of the Case:
Shri Charan Singh (hereinafter referred to as Complainant) has filed a complaint against the decision of
National Insurance Company Ltd (hereinafter referred to as the Respondent Insurance Company) alleging
wrong repudiation of claim relating to hospitalization of his wife Smt. Kamlesh.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that he had been having a mediclaim policy of
the National Insurance Company Ltd. since last 10 years. His wife was admitted in B.L.K. Hospital
from 05.09.2018 to 13.09.2018 for infection in kidney. The Insurance Company had repudiated the
claim. The complainant wrote a letter to grievance cell of Insurance Company, and has now
approached this forum for relief.
b) Insurer's Argument: The Insurance Company has stated in their Self Contained Note that as per the
discharge summary, the complainant’s wife was suffering from AKI with sepsis, as a result of over
dosage of NSAIDS, which is excluded under policy clause no 4.21.-Drug/Alcohol abuse.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Policy documents
b) Discharge summary
c) Self Contained Note
21. Result of hearing the parties (Observations and Conclusion):
Case called. Parties are present.
Insurer had repudiated the claim under exclusion clause 4.21: Drug/alcohol abuse. However, alcohol is not
an issue in this case and therefore the repudiation was only on the basis of the noting in the discharge
summary dated 13.9.2018 that the patient had a history of ‘b/l knee osteoarthritis and nsaids++’. The TPA
had recommended rejecting the claim stating it to be a case of mis-use/self-use of drugs.
The term ‘nsaid’ is acronym for non-steroidal anti-inflammatory drugs. The discharge summary does not
indicate that the patient was a case of mis-use/self-use of nsaid or any drugs, nor has it recommended to
stop nsaid or any other such drug.
Therefore, the inference of the Insurer that the patient has misused any harmful drugs was not correct.
Accordingly, the repudiation was not justified.
Award
The complaint is allowed and the Insurer is directed to settle the claim and also pay to the Complainant
interest for delayed payment for the period commencing from the date the complainant submitted the
required documents till the date the payment of claim is actually made, as prescribed under the
Insurance Regulatory and Development Authority of India (Protection of Policyholders’ Interests)
Regulations, 2017.
Insurance Company should implement this award within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi,
16
th
December 2019
7.
Date of receipt of the Complaint
13.09.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 256406/-
10.
Date of Partial Settlement
N.A.
11.
Amount of Partial Settlement
N.A.
12.
Amount of relief sought
Rs. 256406/-
13.
Complaint registered under Rule no:
Insurance Ombudsman rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.
14.
Date of hearing/place
12.12.2019 / Delhi
15.
Representation at the hearing
For the Complainant
Shri Jeetender Tanwar.
For the insurer
Shri Mani Mahto, Admn. Officer
16.
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Akhileshwar Kumar Chaudhary versus Star Health and Allied Insurance Co. Ltd.
Complaint Ref: DEL-H-044-1920-0318
Case No: HI/STAR/225/19
Brief Facts of the Case:
Shri Akhileshwar Kumar Chaudhary (hereinafter referred to as the Complainant) has filed a complaint
against the decision of Star Health and Allied Insurance Company Ltd. (hereinafter referred to as the
Respondent Insurance Company) alleging wrong repudiation of claim.
Cause of Complaint:
Complainant's Argument: The complainant has stated that his son had taken a mediclaim policy from
Star Health and Allied Insurance Company Ltd on 22.04.2019. The complainant felt shortness of breath
on 23.04.2019 and had consulted the doctor, who advised him to take medicines for 10 days, but on
03.05.2019, the complainant again felt chest pain. On the advice of doctor, he underwent some tests,
which confirmed that complainant had the blockage of all three arteries and suffering from
Hypothyroidism. The complainant was admitted in hospital on 06.06.2019 and on 07.06.2019, he
received a mail from the Insurance Company, stating that his claim had been rejected and policy
cancelled. He wrote a letter to their grievance cell, and has now approached this forum for relief.
Insurer's Argument: The Insurance Company have stated in their Self Contained Note dated 18.11.2019
that as per the documents received from the Hospital, the complainant has been suffering from the
coronary artery disease and hypothyroidism, with the complaint of shortness of breath for the past 3-4
months. The complainant was admitted for CAD and TVD, which was prior to inception of his first policy.
So it was a pre-existing disease, which was not disclosed, and this amounted to concealment of material
facts. Therefore the claim was not admissible in accordance with the policy condition no 6.
Reason for registration of Complaint: Repudiation of claim and cancellation of policy.
The following documents were placed for perusal:
d) Discharge summary
e) Rejection letter and Self Contained Note of Insurance Company.
f) Policy document.
Result of hearing of the parties (Observations and Conclusion):
1.
Name & Address of the Complainant
Shri Akhileshwar Kumar Chaudhary, B-4/128D,
Keshavpura, Lawrence road, New Delhi 110015
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P 700001/01/2020/002629
Mediclaim
23.04.2019 To 22.04.2020
3.
Name of the insured
Name of the Policy holder
Shri Akhileshwar Kumar Chaudhary.
Shri Anupam Kumar Chaudhary
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
07.06.2019
6.
Reason for repudiation
Pre-Existing disease not covered.
7.
Date of receipt of the Complaint
06.09.2019
8.
Nature of complaint
Repudiation of claim & Cancelation of policy
9.
Amount of Claim
Rs. 841515/-
10
Date of Partial Settlement
N.A.
11
Amount of Partial Settlement
N.A.
12
Amount of relief sought
Rs. 841515/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(d)- Misrepresentation of policy terms and
conditions any time in the policy bond or policy contract.
14
Date of hearing/place
12.12.2019/ Delhi
15
Representation at the hearing
For the Complainant
Shri Akhileshwar Kumar Choudhary
For the insurer
Shri Mantosh Kumar, Manager
16.
Complaint how disposed/ date of
Award/Order
Award / 16.12.2019

Case called. Parties are present.
Policy was taken for the first time for one year, from 23.4.2019. Policy holder is Anupam Kumar Chaudhary
and the complaint relates to his father Akhileshwar Kumar Chaudhary. This claim relates to hospitalization
of the latter (Complainant) during 11-24 June 2019 for a variety of ailments including coronary artery
disease, triple vessel disease, hypertension, hypothyroidism etc. The discharge summary records the
patient to be known case of hypertension and hypothyroidism. Complainant had, through the Medanta
Hospital, sought for pre-authorisation for cashless treatment on 5.6.2019, which was before
hospitalization. Insurer made inquiries and informed on 7.6.2019, that as per the documents received by
them, it was observed that the patient was suffering from this condition for past 3-4 months, which is
prior to inception of the policy. Hence the Insurer took it as a case of non-disclosure of pre-existing disease
and thus concealment of material facts while applying for the policy. Insurer also proceeded to cancel the
policy on the same grounds, per clause 12 of the policy.
Insurer states that the in response to the query for pre-authorisation, the Medanta Hospital had informed
that the patient was admitted for the first time on 4.5.2019 and had no past history of cardiac ailment.
However, as per the papers filed by the parties, the same hospital had treated this patient on 24.4.2019
for chest pain and breathlessness on exertion for past 5-6 months. This makes the response of the hospital
unreliable.
Parties have also submitted the discharge summary of an earlier hospitalization of the Complainant in the
same hospital during 4 to 15 May 2019, wherein it was noted that he was a known case of coronary artery
disease and hypothyroidism and the angiography had revealed severe triple vessel disease.
The discharge summary of the hospitalization for 11 to 24 June 2019, signed by Dr. Anil Bhan of Medanta,
notes that the Complainant was a k/c/o hypothyroidism, presented with complaints of angina and
dysphonia on exertion. Complainant submits two certificates dated 11.6.2019 and 26.8.2019 from a
different doctor of Medanta, which state that he had no past ailments of the kinds cited above. It is
important to note that the certificate indicating no prior illness was issued on 11.6.2019, while the
discharge summary 24.6.2019 notes many past ailments.
The conflicting certificates issued by the doctors make the same unreliable and the repudiation and
cancellation of the policy based on the grounds stated by them was justified.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ms Bhawana Bansal versus Manipal Cigna Health Insurance Company Ltd.
Complaint Ref: DEL-H-053-1920-0293
Case No: HI/MANIPAL CIGNA/201/19
1.
Name & Address of the Complainant
Ms Bhawana Bansal, 1/186 Kamna, Vaishali, sector-1
Vaishali, Ghazizbad-201010.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
PROCSH 980366501
Health policy
05.01.2019 To 04.01.2020
3.
Name of the insured
Name of the policy holder
Ms Bhawana Bansal
Ms Bhawana Bansal
4.
Name of the insurer
Manipal Cigna Health Insurance Company Ltd.
5.
Date of repudiation
26.06.2019
6.
Reason for repudiation
Untrue or incorrect statements and misrepresentation.
7.
Date of receipt of the complaint
20.08.2019
8.
Nature of complaint
Rejection of claim
9.
Amount of claim
Rs.52922/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 52922/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Ms Bhawana Bansal

17. Brief Facts of the Case:
Ms Bhawana Bansal (hereinafter referred to as the complainant) had filed the complaint against the decision
of Manipal Cigna Health Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance
Company) alleging wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The complainant has stated that she was admitted in Sonia Hospital from
21.05.2019 to 26.05.2019 for loose motion, vomiting, pain in abdomen, decreased oral intake and was
diagnosed as Acute Gastro Enteritis with dehydration with acute febrile illness with Polyarthralgia and
managed conservatively. The complainant had stated that she got a claim from HDFE ERGO Insurance
Company for the same problem. The Insurance Company had denied her Claim due to non disclosure of
material fact and claim non genuine as per policy clause no VI.1. The complainant has now approached this
forum for relief.
b) Insurer's Argument: The Insurance Company has stated, in their claim rejection letter that the
complainant was admitted at Sonia Hospital New Delhi with acute Gastroenteritis with dehydration. As
per investigation reports, multiple discrepancy and manipulation found in claim documents, hence
claim was rejected as per policy terms and condition no VI.1. which were states that “The policy shall
be null and void and no benefit shall be payable in the event of untrue or incorrect statement,
misrepresentation, mis-description or non-disclosure of any material particulars in proposal form and
Insurance Company have sole discretion to cancel the policy and the premium paid shall be forfeited”.
19. Reason for registration of Complaint: Repudiation of claim
20. The following documents were placed for perusal:
a) Policy Documents.
b) Claim rejection letter from Insurance Company.
c) Discharge summary.
d) Self Contained Note of the Insurance Company.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Complainant is present. Insurer is absent. The claim was repudiated on the ground of violation
of Policy Clause VI.1 (Duty of Disclosure), which states that the policy shall be null and void and no benefits
shall be payable in the event of untrue or incorrect statements, misrepresentation, non-disclosure etc.
However, Insurer has not explained the reasons for arriving at the conclusion in their repudiation letter
dated 31.05.2019. In fact, this clause includes many eventualities that could lead to repudiation of a claim.
Merely citing the whole clause for repudiation without citing any specific part of the clause and relevant
evidence makes the repudiation wholly unjustified.
Award
The repudiation of Claim No. 19718427 by the Insurer Manipal Cigna Health Insurance Company is set
aside and the insurer is directed to settle the claim within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
27
rth
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Ram Mehar Yadav versus United India Insurance Company Ltd.
Complaint Ref: DEL-H-051-1920-0254
Case No: HI/UII/178/19
For the insurer
Absent
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019.
1.
Name & Address of the Complainant
Shri Ram Mehar Yadav,
C-39A, Radhey Shyam Park Extn,
Krishna Nagar, Delhi-110051

17. Brief Facts of the Case:
Shri Ram Mehar Yadav (hereinafter referred to as the complainant) has filed the complaint against the decision
of United India Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance Company)
alleging wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The Complainant has stated that his wife is taking treatment for breast cancer by
AIIMS, New Delhi. She is getting free treatment from AIIMS, New Delhi, but he has to pay for a medicine
(Trastuzumab), which is not available at AIIMS, New Delhi and he has to bring from the market at the time
of chemotherapy. Every time the complainant gets reimbursement from the Insurance Company for this
medicine, but this time the Insurance Company refused to give it. The complainant has now approached
this forum for relief.
b) Insurer’s Argument: The Insurance Company have not submitted their self-contained note. However, they
have stated in their claim rejection letter that duration of admission for current illness, Carcinoma Breast
was for 1 day and as per the policy terms and condition no 1.21, the expenses on hospitalization for
minimum period of 24 hours are admissible. Trastuzumab, being human epidermal growth factor receptor
2-positive, which is not a parental chemotherapy drug, is not covered as a day-care procedure.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Policy Documents
b) Claim rejection letter from Insurance Company.
c) Discharge summary.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
The Insured was getting treatment for cancer and had four rounds of chemotherapy followed by surgery on 19-
21.4.2019 at AIIMS, Delhi. The expenditure for the surgery was largely free, except for Rs. 3200, which was
reimbursed by this Insurer. Complainant states that Insurer had also paid for the same Inj. Trastuzumab for Day
care administration prior to this surgery. However, Insurer now denied for the same Inj. Trastuzumab for Day
care administration post this surgery for 14.5.2019, 13.6.2019, on the grounds of being only for
immunotherapy.
Insurer accepts that the Inj. Trastuzumab during Day care administration post this surgery would have been
admissible for reimbursement if it were administered along with chemotherapy. The prescriptions of AIIMS for
all these five days of repudiated claims indicate that this injection was administered along with chemotherapy,
but the chemotherapy itself was administered free of cost by AIIMS and therefore the claim was only for Inj.
Trastuzumab.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
040781/28/19/P101996204
Health policy
01.06.2019 to 31.05.2020
3.
Name of the insured
Name of the policy holder
Ms Leelawati Yadav.
Shri Ram Mehar Yadav
4.
Name of the insurer
United India Insurance Company Ltd.
5.
Date of repudiation
12.07.2019
6.
Reason for repudiation
Day care is not covered.
7.
Date of receipt of the complaint
25.07.2019
8.
Nature of complaint
Rejection of claim.
9.
Amount of claim
Rs.46170/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs.46170/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Shri Ram Mehar Yadav.
For the insurer
Shri Rajeev Kumar Gupta. A.M.
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019

In these circumstances, the claim deserves to be accepted.
Award
The repudiation of the MediClaim of the Complainant Shri Ram Mehar Yadav by the Insurer United India
Insurance Company for administration of Inj. Trastuzumab post surgery on 14.5.2019, 13.6.2019, is set
aside and the Insurer is directed to settle the claim within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
23
rd
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Sunil Bhat versus Apollo Munich Health Insurance Co. Ltd.
Ref: DEL-H-003-1920-0262
Case No: HI/ Apollo /184/19
17. Brief Facts of the Case:
Shri Sunil Bhat (hereinafter referred to as the complainant) had filed the complaint against the Apollo Munich
Health Insurance Co.Ltd. (hereinafter referred to as the Respondent Insurance Company) alleging wrong
repudiation of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The complainant has stated that his wife was admitted to B.L.K. Hospital and
during the hospitalization; she was diagnosed for the neurocysticerosis. The Insurance Company had
rejected his claim and stated that policy was not in force at the time of claim. The complainant has now
approached this forum for relief.
b) Insurer’s Argument: The Insurance Company telephonically informed us that they have settled his claim.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Policy Documents
b) Claim rejection letter from Insurance Company.
1.
Name & Address of the Complainant
Shri Sunil Bhat,
34/17, 1
st
floor, West Patel Nagar, New Delhi-110008
2.
Policy No:
Type of Policy
Duration of policy/Policy period
110100/11121/6000093826-05-09
Health policy
30.03.2018 to 29.03.2019
3.
Name of the insured
Name of the policy holder
Smt. Semi Bhat.
Shri Sunil Bhat
4.
Name of the insurer
Apollo Munich Health Insurance
5.
Date of repudiation
17.06.2019
6.
Reason for repudiation
Policy expired.
7.
Date of receipt of the complaint
24.07.2019
8.
Nature of complaint
Rejection of claim.
9.
Amount of claim
Rs. 48023/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 48023/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Absent
For the insurer
Dr. Danish Asst. Manager.
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019.

c) Discharge summary.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Insurer is present and inform that they have settled the claim of Rs. 48,022 for Rs. 23,556 and
have also advised the Complainant the reasons for not admitting the remaining amount.
Complainant is absent but has sent a letter dated 20.12.2019 stating that he has received settlement for his
claim from the Insurer and that his case before this forum may be closed.
I find this communication from the parties as a conciliatory settlement, even though a formal agreement
could not be signed today owing to the absence of the Complainant.
Award
The complaint is allowed in terms of the offer of the Insurer to settle the claim for Rs. 23,556, which the
complainant has also accepted.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
23
rd
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Amit Luthra versus Apollo Munich Health Insurance Co. Ltd.
Complaint Ref: DEL-H-003-1920-0297
Case No: HI/ Apollo /204/19
17. Brief Facts of the Case:
Shri Amit Luthra (hereinafter referred to as the complainant) had filed the complaint against the Apollo
Munich Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company) alleging
wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The complainant has stated that his daughter was admitted in Max Hospital
Saket New Delhi from 31.10.2018 to 02.11.2018. She was diagnosed chronic malabsorption with failure
to thrive under evaluation. As per discharge summary and medical reports, the treatment being given
for Liver disease and as per D.N.A. test “No pathogenic or likely pathogenic variants causative of the
reported phenotype were indentified” but the Insurance Company had rejected her claim on the ground
that the claim for treatment of Mednik Syndrome which fall under genetic disorder is excluded in the
policy. The complainant has now approached this forum for relief.
b) Insurer’s Argument: The Insurance Company have stated that in their Self Contained Note (S.C.N.) that, as
per claim papers submitted by the complainant treatment were given for mednik syndrome, which falls
1.
Name & Address of the Complainant
Shri. Amit Luthra,
D-211, D-Block Jilmil Colony, Shahdara, Delhi-110095.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
110105/11051/1000185745-08
Health policy
29.03.2019 to 28.03.2020
3.
Name of the insured
Name of the policy holder
Baby Kriti Luthra
Shri Amit Luthra
4.
Name of the insurer
Apollo Munich Health Insurance Co. Ltd.
5.
Date of repudiation
07.12.2019
6.
Reason for repudiation
Genetic disorder not covered.
7.
Date of receipt of the complaint
05.08.2019
8.
Nature of complaint
Rejection of claim.
9.
Amount of claim
Rs. 78928/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs.78928/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Shri Amit Luthra and Shri Deep Kumar Luthra.
For the insurer
Dr. Danish. Asst. Manager.
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019.

under genetic disorder. Treatment related to a condition, which is due to Genetic disorder has been
excluded in the policy. Hence claim had been rejected.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Self Contained Note.
b) Discharge Summary
c) Policy Document
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and reiterate their arguments.
Insurer states that liver ailment of the insured was primarily arising from the mednik syndrome, as was
stated in the Discharge Summary of Max Hospital dated 2.11.2018. Complainant has produced a letter
dated 17.1.2019 from the same treating physician which states, inter alia, that the insured child did not
meet the diagnostic criteria of mednik syndrome. Thus the treating doctor has given conflicting inferences,
which make it difficult to accept.
The relevant policy clause reads as follows:
C. General exclusion.
We will not pay for any claim, which is caused by, arising from or in any way attributable to:
Medical Exclusions.
xi) Types of treatment, defined illnesses/conditions/supplies:
n. Congenital external diseases, defects or anomalies, genetic disorder.
The liver biopsy report dated 1.11.2019 records the following clinical impression: “CLD with genetically
mednik syndrome with very low ceruloplasmin’. Insurer states that low ceruloplasmin leads to hepatic
dysfuntion and CLD. The earlier DNA test report 7.8.2018 had also identified the disease of the insured as
mednik syndrome though the classification is noted as of uncertain significance.
After going through the evidence adduced by both parties I come to the conclusion that the ailment of the
insured arose from mednik syndrome, which is a genetic disorder. Accordingly, Insurer was justified in
repudiating the claim.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
23
rd
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Smt Ila Jain versus Apollo Munich Health Insurance Co. Ltd.
Complaint Ref: DEL-H-003-1920-0303
Case No: HI/ Apollo /210/19
1.
Name & Address of the Complainant
Smt Ila Jain, 49, Bhiku Ram Jain Marg, Rajpura Road,
Civil Lines, NewDelhi-110008.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
110100/11051/1000097450-09-05-09
Health policy
26.09.2018 to 25.09.2019
3.
Name of the insured
Name of the policy holder
Shri Naren Bhikuram Jain
Smt Ila Jain
4.
Name of the insurer
Apollo Munich Health Insurance Co. Ltd.
5.
Date of repudiation
20.07.2019
6.
Reason for repudiation
Claim for Investigation and Evaluation of aliment.
7.
Date of receipt of the complaint
24.07.2019
8.
Nature of complaint
Rejection of claim.
9.
Amount of claim
Rs. 44061/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.

17. Brief Facts of the Case:
Smt. Ila Jain (hereinafter referred to as the complainant) had filed the complaint against the Apollo
Munich Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company)
alleging wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant’s Argument: The Complainant has stated that she had taken a health floater policy
from Apollo Munich Health Insurance Company Ltd. for her husband. Her husband was admitted in
ILBS Hospital, New Delhi from 02.08.2018 to 04.08.2018, with an aliment of Hepatitis C. The
Insurance Company had already paid earlier two claims of same disease to the Complainant earlier,
whereas the Insurance Company had rejected his third claim with the remark that “admission is for
investigation and evaluation of aliment only”. The complainant has now approached this forum for
relief.
c) Insurer’s Argument: The Insurance Company telephonically informed us that they are going to settle
his claim within week time.
19. Reason for registration of Complaint: Admission for Investigation only.
20. The following documents were placed for perusal:
a) Policy Documents
b) Claim rejection letter from Insurance Company.
c) Discharge summary.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Insurer is present and informs that they have settled the claim of Rs. 82,144 for Rs. 80,879 and
have also advised the Complainant the reasons for not admitting the remaining amount.
Complainant is absent.
I find this communication from the Insurer as a conciliatory settlement, even though a formal agreement
could not be signed today owing to the absence of the Complainant.
Award
The complaint is allowed in terms of the offer of the Insurer to settle the claim for Rs. 80,879.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
23
rd
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Shri Shyam Sunder versus Religare Health Insurance Co. Ltd.
Complaint Ref: DEL-H-037-1920-0295
Case No: HI/Religare/203/19
12.
Amount of relief sought
Rs. 44061/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
For the insurer
16.
Complaint how disposed/ date of
Award/Order
1.
Name & Address of the Complainant
Shri Shyam Sunder,
F-100 A, Rajdhani Park, Nangloi, New
Delhi-110041
2.
Policy No:
Type of Policy
Duration of policy/Policy period
11932225
Mediclaim
12.01.2018. to 11.01.2019
3.
Name of the insured
Name of the policy holder
Shri Shyam Sunder
Shri Shyam Sunder

17. Brief Facts of the Case:
Shri Shyam Sunder (hereinafter referred to as the complainant) had filed the complaint against the decision
of Religare Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company) alleging
wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that, the Insurance Company had rejected his claim
due to some discrepancy in medical documents. He was admitted in Ashirwad Nursing Home with fever
and vomiting and all the papers prepared by Hospital have been submitted to the Insurance Company. The
complainant wrote a letter to the grievance cell of the Insurance Company but his complaint was not
resolved. The complainant has now approached this forum for relief.
b) Insurer’s Argument: The Insurance Company has stated in their Self Contained Note that as per
Investigation reports, it was found that Delhi Medical Council (D.M.C.) number of treating doctor of
complainant was not correct. The complainant stated to the Insurance Investigator that, he was suffering
from fever, however on Indoor Care Papers (ICP), verified by the Investigator in the Hospital record, the
complainant had multiple Complaints, and copy of ICP’s was not provided by the hospital to the Insurance
Investigator. As per discharged summary the complainant was diagnosed for chest infection but no X’Ray
was done. The final bill of hospital was for Rs. 37106/- but the complainant stated to Investigator that he
paid Rs. 10000/- only and there was no TIN number and GST number on final bill. Hence the Insurance
Company had rejected claim.
19. Reason for registration of Complaint: Repudiation of claim
20. The following documents were placed for perusal:
a) Self Contained Note.
b) Policy Documents.
c) Discharged Summary.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present.
Insurer states that the Complainant had reported his ailment as fever. However, the Indoor Care Papers (ICP)
had noted the ailments as headache, vomiting and pain in abdomen. Moreover, the Discharge Summary for
10-13 December had noted the diagnosis as chest infection with sepsis. Also, the blood test report dated
10.12.2018 had recorded TLC as 30000, which was far higher than the tolerable limit of 11000, yet it has not
been reported in the Discharge Summary at all. All this made the claim suspicious and, accordingly, the claim
was rejected under the non-disclosure clause 7.1.
Complainant has no response to these arguments except stating that he would like the Insurance Company to
check out the facts with the hospital.
After going through the evidence presented by both parties, I come to the conclusion that the Insurer was
justified in repudiating the claim.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
26th December, 2019
4.
Name of the insurer
Religare Health Insurance Co. Ltd.
5.
Date of repudiation
12.02.2019
6.
Reason for repudiation
Discrepancy in documents
7.
Date of receipt of the complaint
05.08.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of claim
Rs. 37106/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 37106/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total
repudiation of claims by an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Shri Shyam Sunder
For the insurer
Dr. Nisha Sharma Manager Claims.
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ms Pravesh Lata versus Religare Health Insurance Co. Ltd.
Complaint Ref: DEL-H-037-1920-0298
Case No: HI/Religare/205/19
17. Brief Facts of the Case:
Ms Pravesh Lata (hereinafter referred to as the complainant) had filed the complaint against the decision of
Religare Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company) alleging
wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that, the Insurance Company had rejected her
claim on 24.06.2019 on the ground of discrepancy found in medical documents. The complainant wrote a
letter to grievance cell of Insurance Company on 29.09.2019, but till now no revert had been received. The
complainant has now approached this forum for relief.
b) Insurer’s Argument: The Insurance Company has stated in their Self Contained Note that the complainant
was hospitalized from 18.05.2019 to 23.05.2019 in Parth Hospital New Delhi with complaint of high grade
fever since 3-4 days, vomiting, nausea, pain in abdomen and loss of appetite. As per Investigation report
of the Insurance Company, the Delhi Medical Council (DMC) number of treating Doctor and pathologist
are not correct. The complainant’s spouse stated that complainant had complained of vomiting, nausea
and fever on 10.05.2019, whereas as per O.P.D. sheet dated 10.05.2019 of Acharya Shree Bikshu
Government Hospital, Delhi, and the complainant had complained of burning micturition. In the final bill
dated 23.05.2019 of Parth Hospital New Delhi, the room rent was charged for six days whereas
complainant was hospitalized for 5 days, and there was neither TIN number nor GST number on the bill. In
the light of these facts, the Insurance Company denied claim as per policy clause no 7.1.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Self Contained Note.
b) Policy Documents.
c) Discharged Summary.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present. Complainant states that he had produced the documents as were
provided by the hospital.
Insurer states that the documents submitted for the claim had many discrepancies as have been
described in Para 18(b) above.
The discrepancies in the documents submitted by the Complainant for the claim are serious enough to
justify repudiation of the claim.
1.
Name & Address of the Complainant
Ms Pravesh Lata,
134 Mitraon Village, Najafgarh, New Delhi 110043.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
13741133
Mediclaim
13.02.2019. to 12.02.2020.
3.
Name of the insured
Name of the policy holder
Ms Pravesh Lata
Ms Pravesh Lata
4.
Name of the insurer
Religare Health Insurance Co. Ltd.
5.
Date of repudiation
29.06.2019
6.
Reason for repudiation
Discrepancy in documents
7.
Date of receipt of the complaint
05.08.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of claim
Rs. 40839/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 40839/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Shri Bal Singh.
For the insurer
Dr. Nisha Sharma. Manager Claims.
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019.
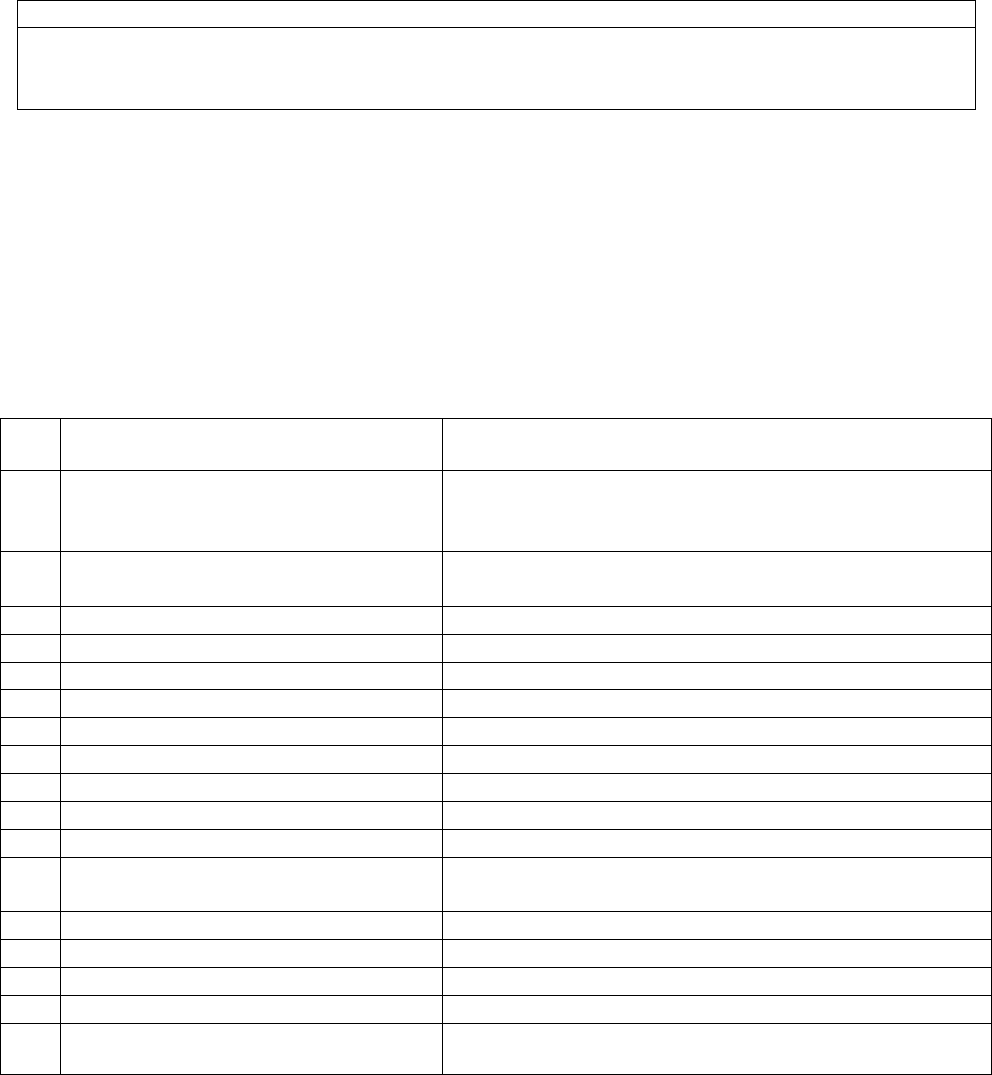
Insurer also states that they have placed a notice on their website, listing hospitals from where claims,
whether cashless or reimbursement, will not be payable. This list includes the Parth Hospital, New Delhi.
I have seen the website of the insurer and find that this is indeed so. However, in addition to placing
such caution notice on their website, the insurer should also inform all their policy holders about this
caution by way of email and registered post.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
23
rd
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ms Sunita Gupta versus Religare Health Insurance Co. Ltd.
Complaint Ref: DEL-H-037-1920-0300
Case No: HI/Religare/207/19
17. Brief Facts of the Case:
Ms Sunita Gupta (hereinafter referred to as the complainant) had filed the complaint against the decision of
Religare Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company) alleging
wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that she underwent a major surgery of removing
uterus and ovaries. Due to oversight, the treating doctor had mentioned in the documents that the
Complainant was suffering from Depression and Hypothyroidism diseases since 25 years instead of 25
months. The Insurance Company has rejected her claim. The complainant has now approached this forum
for relief.
b) Insurer’s Argument: The Insurance Company has stated in their Self Contained Note (SCN) that on receipt
of the claim documents from the Complainant, the Insurance Company came to the conclusion that the
Complainant had a history of depression before the date of policy inception and same was not disclosed to
Insurance Company at the time of the policy proposal. Even though the treating doctor had clarified that
the Complainant had a history of depression since 25 months and not 25 years, the Insurance Company
denies the same as such a grave mistake cannot happen by any doctor without any intention to write the
same. The Insurance Company denied claim on the ground of non-disclosure of depression at the time of
policy inception in accordance with clause no 7.1 of the policy terms and conditions.
19. Reason for registration of Complaint: Repudiation of claim.
1.
Name & Address of the Complainant
Ms Sunita Gupta 5252, First Floor, Kohlapur House,
Above Apollo Pharmacy, Malka Ganj, Dehli-110007
2.
Policy No:
Type of Policy
Duration of policy/Policy period
10214762
Mediclaim
20.03.2019 to 19.03.2021
3.
Name of the insured
Name of the policy holder
Ms Sunita Gupta
Ms Sunita Gupta
4.
Name of the insurer
Religare Health Insurance Co. Ltd.
5.
Date of repudiation
12.05.2019
6.
Reason for repudiation
Pre-existing disease of depression.
7.
Date of receipt of the complaint
05.08.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of claim
Rs. 172153/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 172153/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Ms. Sunita Gupta and Shri Gaurav Garg.
For the insurer
Dr. Nisha Sharma. Manager Claims.
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019.

20. The following documents were placed for perusal:
a) Self Contained Note.
b) Policy Documents.
c) Discharged Summary.
21. Result of hearing of both parties (Observations and Conclusion):
Case called. Parties are present.
Claim was rejected on grounds of non-disclosure of pre-existing disease (PED) at the time of taking the
policy on 20.3.2015. Insurer states that in the policy proposal form, Complainant had stated ‘No’ for the
question asking for history of thyroid, any kind of medication, any condition of nervous system (migraine
etc.), which were all proved to be false as per the various medical records. Insurer also states that had the
Complainant disclosed the ailment of depression, they would not have issued the policy at all. Moreover,
non-disclosure of PED would lead to repudiation of the claim under Clause 7.1 of the policy.
Complainant states that she was suffering from Depression for 25 months and not 25 years and has not
been taking any medication for depression and that she had received reimbursement from this Insurer for
an illness of March 2019 but has denied the subsequent claim for the illness of April 2019. She also says
that she is quite healthy and does not know the meaning of the ailment of depression. She has also give a
letter from the treating doctor stating that the ailment of April 2019 had no relation with depression.
Insurer states that the treating doctor had in the Consultation Paper dated 8.4.2019 noted that the
Complainant was k/c/o depression and hypothyroidism for 25 years. Complainant submits copy of a letter
dated 20.5.2019 from the treating doctor of the same hospital which states that the history of depression
was 25 months and the word ‘years’ was written by mistake and also that the patient’s history of
depression and thyroid disorder were no ground to decline her insurance claim.
The conflicting certificates of the treating physician in regard to the pre-existing ailment of the insured
make the same unreliable therefore the Insurer was right in holding that the Complainant had not
disclosed the PED while going in for the policy and, accordingly, the repudiation of the mediclaim was
justified.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
December, 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 16 (1)/17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Mr. Shri Pal versus Religare Health Insurance Co. Ltd.
Complaint Ref: DEL-H-037-1920-0299
Case No: HI/Religare/206/19
1.
Name & Address of the Complainant
Mr. Shri Pal, B-16, J.J. Colony, Sector15. Bharat Vihar,
Kakrola, New Delhi -110078
2.
Policy No:
Type of Policy
Duration of policy/Policy period
11513153
Mediclaim
13.08.2018. To 12.08.2019
3.
Name of the insured
Name of the policy holder
Ms Himanshi
Mr. Shri Pal
4.
Name of the insurer
Religare Health Insurance Co. Ltd.
5.
Date of repudiation
28.06.2019
6.
Reason for repudiation
Discrepancy in documents
7.
Date of receipt of the complaint
05.08.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of claim
Rs. 36085/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 36085/-

17. Brief Facts of the Case:
Mr. Shri Pal (hereinafter referred to as the complainant) had filed the complaint against the decision of
Religare Health Insurance Co. Ltd. (hereinafter referred to as the Respondent Insurance Company) alleging
wrong repudiation of claim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant had stated that his daughter had taken medical treatment in
the Parth Hospital. The Insurance Company had rejected his claim on 28.06.2019 on the ground of
“discrepancy in medical documents”, he wrote a letter to grievance rederssal officer of the Insurance
Company on 28.06.2019 but till date Insurance Company has not given any reply. The complainant has now
approached this forum for relief.
b) Insurer’s Argument: The Insurance Company has stated in their Self Contained Note that they had received
a request for reimbursement of hospitalization expenses of the Insured. The Insured was hospitalized at
the Parth Hospital, New Delhi from 01.06.2019 to 05.06.2019. As per the patient’s statement, she was
having only high fever and not chills but, as per Indoor Care Papers (ICP) and discharge summary, she was
having high grade fever with chills and rigor. The bill book of hospital shows that receipt no. 1015 dated
29.05.2019 was issued for Sh. Gulab Singh and receipt no. 829 dated 01.06.2019 was issued to Ms Himanshi
(insured). Medicine charts were written by single handwriting; it is not possible for a person to be on duty
for five continuous days. Inj. Tazowin 4.5 gm was started at the time of admission (TOA) without seeing
total leucocyte count (TLC) and, her TLC was normal. The Insured stated that her fever had continued for 5
days in hospital, but as per vital chart, she did not have fever after 03.06.2019. On the basis of afore
mentioned facts, the Insurance Company denied the claim.
19. Reason for registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Self Contained Note.
b) Policy Documents.
c) Discharged Summary.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present. Complainant states that he had produced the documents as were
provided by the hospital.
The discrepancies in the documents submitted by the Complainant for the claim, as described by the
Insurer, are serious enough to justify repudiation of the claim.
Insurer also states that they have placed a notice on their website, listing hospitals from where claims,
whether cashless or reimbursement, will not be payable. This list includes the Parth Hospital, New Delhi.
I have seen the website of the insurer and find that this is indeed so. However, in addition to placing
such caution notice on their website, the insurer should also inform all their policy holders about this
caution by way of email and registered post.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
23
rd
December, 2019
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
23.12.2019
15.
Representation at the hearing
For the Complainant
Mr. Shri Pal
For the insurer
Dr. Nisha Sharma. Manager Claims.
16.
Complaint how disposed/ date of
Award/Order
Award / 23.12.2019.

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule No: 16 (1)/17 Of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Sh. Gaurav Jain VERSUS The Oriental Insurance Company Ltd.
Complaint Ref: No: DEL-H-050-1920-0350
Case No: HI/OIC/240/19
1.
Name &Address of the Complainant
Sh. Gaurav Jain
160, Arihant Nagar, Punjabi Bagh,
New Delhi-110026
2.
Policy No.
Type of Policy
Policy term/Policy Period
211200/48/2019/1218
Mediclaim Policy
01.06.2018 to 31.05.2019
3.
Name of the insured
Name of the policy holder
M/s Times Publishing House Ltd.
(patient Smt.Rama Jain)
Sh. Gaurav Jain
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
NA
6.
Reason for Grievance
Inadequate settlement of mediclaim
7.
Date of receipt of the Complaint
27.09.2019
8.
Nature of Complaint
Inadequate settlement of mediclaim
9.
Amount of Claim
Rs.3,27,729/-
10.
Date of Partial Settlement
10.03.2019
11.
Amount of Partial Settlement
Rs.1,00,000/-
12.
Amount of relief sought
Rs.2,27,729/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claim
14.
Date of hearing/ Place of hearing
11.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. Gaurav Jain
b) For the Insurer
Sh. GopalKrishan, Dy. Manager
16.
Date of Award/Order
Award/11.12.2019
17. Brief Facts of the Case:
Sh. Gaurav Jain (hereinafter referred to as the complainant) has filed the complaint against the decision
of the Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance Company)
alleging inadequate settlement of mediclaim.
18.Cause of Complaint:
a) Complainant's Argument: The complainant had stated that his mother Mrs. Rama Jain was
admitted in the Rajiv Gandhi Cancer Institute and Research Centre, New Delhi from
07.03.2019 to 10.03.2019 and was diagnosed for Cancer of Endometrium (Malignant
Neoplasm: Corpus Uteri, Unspecified) Hysteroscopy and D&C conducted were suggestive of
Invasive Endometrial Adenocarcinoma and Cervix Biopsy suggestive of Chronic Cervicitis
and High Grade Adenocarcinoma suggestive of seous carcinoma. The total bill for the said
surgery and hospitalization was Rs.3,27,729/- whereas the TPA has approved
onlyRs.1,00,000/- on the ground that there was a capping of Rs.1,00,000/- for the disease of
Hysterectomy and Robotic charges were not payable. As per complaint, this was not a case of
Hysterectomy but of cancer which is a Critical Illness and the patient was under the Radical
Hysterectomy surgery which is done for the Cancer patients; hence the said capping was not
applicable in this case.
b) Insurer's Argument: The Insurance Company, vide its settlement letter dated 10.03.2019,
informed the complainant that the claim had been settled as per policy conditions. The Policy
has ailment capping of Rs.1 lakh for hysterectomy. Robotic surgery is not covered under the
policy, however, the claim has been processed for hysterectomy for Rs.1 lakh towards full and
final settlement of the claim. In their self-contained note (SCN) dated 09.12.2019, the
Insurance Company has stated that the patient Mrs. Rama Jain was operated for robotic
radical hysterectomy. The policy has ailment capping of Rs. 1 lakh for hysterectomy and
robotic surgery was not covered under the policy. Hence the claim was settled as per the
policy terms & condition in full and final for Rs. 1 lakh.
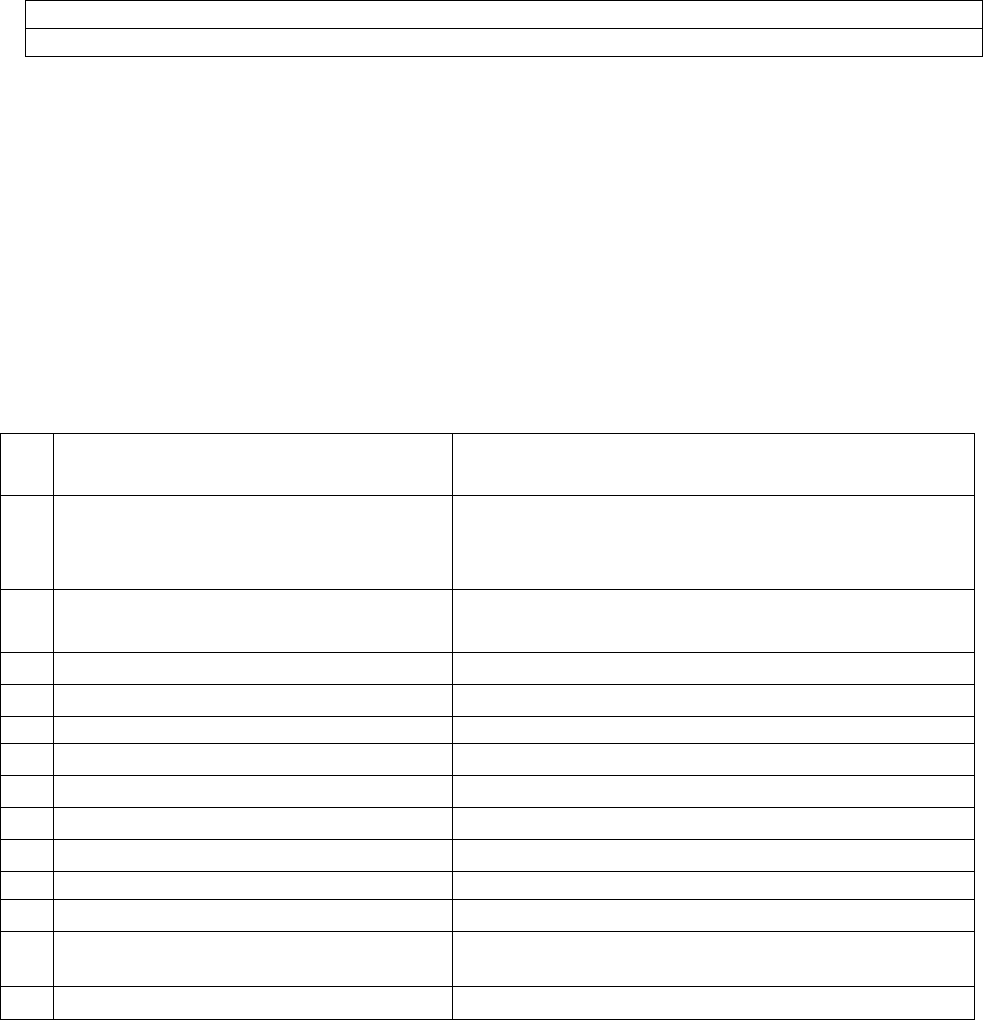
19. Reason for registration of Complaint: Repudiation of claim as stated in Para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bills, OPD Card, Receipt.
c) Copy of Settlement letter.
21. Result of hearing with the parties (Observations and Conclusion):
a) Case called. Parties are present and explain their respective position, which is the
same as has been summarised in Para 18 above.
b) Insurer has relied on the clause of the policy which prescribes monetary limits for
reimbursement of seven specific common ailments, namely, cataract operation
(Rs.40000/-), hysterectomy (Rs.100000/-), gall bladder, unilateral hernia, bilateral
hernia, kidney stone and prostate. Complainant states that this clause is inaccurately
worded, as some of these terms relate to ailment (e.g. hernia), whereas some are
merely procedures (e.g. hysterectomy). Insurer has quoted this clause to limit the
claim in respect of hysterectomy to Rs.100000/-.
c) However, the same policy document also states that for 11 specified illnesses, which
include cancer, an additional limit of Rs.3 lakh per person would be available.
Complainant is seeking reimbursement under this clause.
d) I conclude that the specific provision for hysterectomy should prevail for the specific
procedure of hysterectomy. Accordingly, the Insurer was justified in limiting the
claim to Rs.100000/-.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
11
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule No: 16 (1)/17 Of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Sh. Ram Bhawan Upadhyay VERSUS The Oriental Insurance Company Ltd.
Complaint Ref: No: DEL-H-050-1920-0359
Case No: HI/OIC/248/19
1.
Name &Address of the Complainant
Sh. Ram Bhawan Upadhyay
2330, D/2, Vasant Kunj, New Delhi- 110070
2.
Policy No.
Type of Policy
Policy term/Policy Period
272900/48/2019/10393
Mediclaim Policy
23.08.2018 to 22.08.2019
3.
Name of the insured
Name of the policy holder
Sh. Ram Bhawan Upadhyay
Sh. Ram Bhawan Upadhyay
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
NA
6.
Reason for Grievance
Inadequate settlement of mediclaim
7.
Date of receipt of the Complaint
30.09.2019
8.
Nature of Complaint
Inadequate settlement of mediclaim
9.
Amount of Claim
Rs.28595/-
10.
Date of Partial Settlement
17.06.2019
11.
Amount of Partial Settlement
Rs.24000/-
12.
Amount of relief sought
Rs.4595/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claim.
14.
Date of hearing/ Place of hearing
11.12.2019/Delhi

15.
Representation at the hearing
c) For the Complainant
Sh. Ram BhawanUpadhyay
d) For the Insurer
Ms. UpdeshKaur, Admn. Officer
16.
Date of Award/Order
Award/16.12.2019
17. Brief Facts of the Case:
Sh. Ram Bhawan Upadhyay (hereinafter referred to as the Complainant) has filed the complaint against the
decision of the Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance Company)
alleging inadequate settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant had stated that he had filed a claim with the Insurance
Company for the cataract surgery of his left eye on 02.05.2019, at Centre for Sight Hospital,
Safdarjung Enclave and submitted the bills to TPA including pre and post hospitalization expenses but
the Insurance Company had approved only Rs.24000/- for the main surgery whereas pre and post
expenses were not paid to him. Hence, he wants relief from this forum.
b) Insurer's Argument: The Insurance Company, vide its Self Contained Note (SCN) had stated that the TPA had
received request for reimbursement of claim amount for Rs.68603/- from the complainant, for the expenses
incurred by him for Cataract Surgery of his left eye which was held on 02.05.2019 at Centre for Sight Hospital,
Safdarjung Enclave. As Sum Insured under the Policy is Rs.500000/-, TPA had settled the claim for Rs.24000/-
which is maximum amount payable in case of Cataract procedure, as per Policy terms & Condition 2(F)(1).
There is specific disease wisecapping under the policy which is applicable for all the admissible expenses
incurred by the insured person for specific procedure. Capping limit is inclusive of hospitalization expenses
and all pre and post hospitalization expenses for the particular admissible claim of specific disease/illness. As
there is capping in the said case, the maximum amount payable under the Cataract procedure had been paid
to the insured and nothing is left in the said case.
19. Reason for registration of Complaint: Repudiation of claim as stated in Para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bill, Copy of settlement mail.
c) SCN of the Insurer.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present.
Insurer had not allowed the claim on the grounds that the Cataract Treatment cost is limited to Rs. 24,000 as per
Policy Clause 2F1, and as the hospital has charged Rs.24,000/- for the surgery itself, any further claim for pre &
post hospitalization would not be admissible.
Insurer states that had the charge for the surgery been less than Rs.24,000/-, they would have admitted the claim
for the remaining amount towards pre & post hospitalization expenses.
Clause 2F1 of the Policy states that a limit of Rs.24,000/- shall apply for the procedure of cataract. Insurer is
unable to explain as to whether the word ‘procedure’ relates to only the surgery or to the pre & post
hospitalization in the agreement that they have made with the Network Hospitals.
Therefore, I conclude that the word ‘procedure’ relates to only the surgery and the pre & post hospitalization
expenses are to reimbursed additionally under the same policy.
Award
The complaint is allowed and the Insurer is directed to admit and settle the claim for the pre & post
hospitalization expenses separately, within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December 2019

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule No: 16 (1)/17 Of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Sh. Arun Sarawagi VERSUS The Oriental Insurance Company Ltd.
Complaint Ref: No: DEL-H-050-1920-0367
Case No: HI/OIC/256/19
1.
Name &Address of the Complainant
Sh. Arun Sarawagi
Block-MV 57, 3
rd
floor, Pitam Pura, New Delhi-110034
2.
Policy No.
Type of Policy
Policy term/Policy Period
272601/48/2018/3338
Mediclaim Policy
04.02.2018 to 03.02.2019
3.
Name of the insured
Name of the policy holder
Sh. Arun Sarawagi
Sh. Arun Sarawagi
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
NA
6.
Reason for Grievance
Inadequate settlement of mediclaim
7.
Date of receipt of the Complaint
13.09.2019
8.
Nature of Complaint
Inadequate settlement of mediclaim
9.
Amount of Claim
Rs.2,30,750/-
10.
Date of Partial Settlement
-----------
11.
Amount of Partial Settlement
Rs.1,50,914/-
12.
Amount of relief sought
Rs.79,616/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claim
14.
Date of hearing/ Place of hearing
11.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. ArunSarawagi
b) For the Insurer
Sh. D. C. Gupta, Sr. Branch Manager
16.
Date of Award/Order
17. Brief Facts of the Case:
Sh. Arun Sarawagi (hereinafter referred to as the Complainant) has filed the complaint against the
decision of the Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance
Company) alleging inadequate settlement of mediclaim.
18. Cause of Complaint:
19. a) Complainant's Argument: The Complainant had stated that due to deteriorating health condition
on 5
th
December, 2018, he was admitted in Sir Ganga Ram Hospital and on the advice of the doctor,
PTCA with stent operation was performed and he was discharged on 07.12.2018. Out of the total
bills, TPA disallowed an amount of Rs.55000/- towards OCT Cardiology charges. Afterwards, he
applied for pre and post hospitalization alongwith charges of Rs.55000/- but disallowed Rs.60495/-
from the pre and post hospitalization expenses also.
b) Insurer's Argument: No SCN received from the Insurance Company till date.The
Insurance Company, vide its mail dated 23.05.2019, informed the complainant that the claim
was rightly settled as per policy terms and conditions. The package agreed upon with the
hospital was that the company shall pay to the hospital or reimburse the insured, the amount
of such reasonable, customary and medically necessary expenses. The concerned procedure
of OCT Cardiology, an advancement in technology, had not been covered in the PPN
package. Further in the pre and post hospitalization expenses, disallowed amount was on a/c
of 10% copayment and other consumable items.
19. Reason for registration of Complaint: Repudiation of claim as stated in Para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary,Bills, GRO mail.
c) Copy of Settlement letter.

21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present.
Complainant had made a total claim of Rs.2,56,189/- of which 10% was to be borne by him and he
does not dispute the same. Against the balance amount of Rs.2,30,570/- Insurer has approved the
claim for Rs.1,50,616/-, leaving a balance of Rs.79,616/-. Of this, the major part is for OCT-
Cardiology charges, which has been disallowed as perPolicy Clause 3.41, which refers to reasonable
and customary charges. Insurer has capped the reimbursement to the PPN Network Hospital
charges. The Policy Bond on Page No. 2 has specifically advised the policyholder to contact his TPA
or any of the Insurer’s offices for information about the preferred hospitals before going for a
treatment. Therefore, Insurer was justified in capping the reimbursement to the PPN Network
Hospital charges.
Insurer has also given details of other disallowed items, such as non-submission of Doctor’s
prescription, policy exclusion clauses, cost of medicines for period beyond 60 days of discharge
from hospital etc. and had conveyed these in a letter to the Complainant.
Therefore, the settlement extended by the Insurer was justified.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule No: 16 (1)/17 Of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Mrs. Sangeeta Bhardwaj VERSUS The Oriental Insurance Company Ltd.
Complaint Ref: No: DEL-H-050-1920-0354
Case No: HI/OIC/243/19
1.
Name &Address of the Complainant
Mrs. Sangeeta Bhardwaj
G-52, Ashok Vihar, Phase-I, New Delhi- 110052
2.
Policy No.
Type of Policy
Policy term/Policy Period
271500/48/2019/5085
Mediclaim Policy
25.02.2019 to 24.02.2020
3.
Name of the insured
Name of the policy holder
Mrs. Sangeeta Bhardwaj
Mrs. Sangeeta Bhardwaj
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
16.07.2019
6.
Reason for Grievance
Non settlement of mediclaim
7.
Date of receipt of the Complaint
25.09.2019
8.
Nature of Complaint
Non settlement of mediclaim
9.
Amount of Claim
Rs.127452/-
10.
Date of Partial Settlement
-----------
11.
Amount of Partial Settlement
-----------
12.
Amount of relief sought
Rs.127452/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claim
14.
Date of hearing/ Place of hearing
11.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Mrs. SangeetaBhardwaj
b) For the Insurer
Absent
16.
Date of Award/Order
Award/16.12.2019
17. Brief Facts of the Case:

Mrs. Sangeeta Bhardwaj (hereinafter referred to as the Complainant) has filed the complaint against the
decision of the Oriental Insurance Company Ltd.(hereinafter referred to as the Respondent Insurance
Company) alleging non-settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument:The Complainant had stated that she was admitted in Fortis
Hospital, Shalimar Bagh from 26.02.2019 to 02.03.2019 and was diagnosed with
ADPKD, Hypertension, CKD, Ascites and Hemorrhagic Cyst right lobe of liver. She
filed her claim with the Insurance Company for Rs.127452/- but her claim was repudiated
on the ground that it falls under clause 4.15. She filed a complaint with the Grievance
Cell of the Insurance Company but nothing has been received till date. Hence, she wants
relief from this forum.
b) Insurer's Argument: The Insurance Company, vide its Self Contained Note (SCN)
dated 17.10.2019, had stated that the Complainant Mrs. Sangeeta Bhardwaj was covered
under Happy Family floater Policy and submitted reimbursement claim for Rs.127452/- .
The patient was admitted in the hospital from 26.02.2019 to 02.30.2019 and was
diagnosed with ADPKD (Autosomal Dominant Polycystic Kidney Disease),
Hypertension, CKD, Ascites and Hemorrhagic Cyst right lobe of liver. Since the patient
was a known case of ADPKD (Autosomal Dominant Polycystic Kidney Disease) which
is an genetic condition that causes small, fluid-filled sacs called cysts to develop in
kidneys. As genetic disorders are excluded from the scope of coverage under policy, the
claim was repudiated under clause 4.15 (Genetic disorders and stem cell
implantation/surgery).
18. Reason for registration of Complaint: Repudiation of claim as stated in Para 18 (a) above.
19. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bills, Receipt, GRO letter, Rejection letter.
c) SCN of the Insurer along with enclosures.
20. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is present. Respondent Insurer is absent.
Insurer had repudiated the claim on the grounds that the Complainant was treated for ADPKD, which
is a genetic disorder and thus excluded vide Policy Clause 4.15.
The discharge summary does record a series of ailments for the Complainant, which include ADPKD.
However, Complainant states that the treatment undertaken in the hospital was not for any kidney
ailment but for liver related problems. The Complainant seems correct as per the discharge
summary.
Accordingly, the Insurer was not justified in repudiating the claim.
Award
The complaint is allowed and the repudiation of the claimby the Insurer is held as unreasonable.
Accordingly, Insurer is directed to admit and settle the claim within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule No: 16 (1)/17 Of The Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ms.RajniVersus ICICI Lombard General Insurance Company Ltd.
Complaint Ref: No: DEL-H-020-1920-0278
Case No: HI/ICICI/192/19
1.
Name &Address of the Complainant
Ms. Rajni
RZ-65, Nand Vihar, Kakrola, South West,
Delhi- 110078

2.
Policy No.
Type of Policy
Policy term/Policy Period
4128i/iH/167638617/00/000
Mediclaim Policy
25.03.2019 to 24.03.2020
3.
Name of the insured
Name of the policy holder
Ms. Rajni
Ms. Rajni
4.
Name of insurer
ICICI Lombard General Insurance Company Ltd.
5.
Date of Repudiation
02.07.2019
6.
Reason for Grievance
Non-settlement of mediclaim
7.
Date of receipt of the Complaint
03.09.2019
8.
Nature of Complaint
Non-settlement of mediclaim
9.
Amount of Claim
Rs.42535/-
10.
Date of Partial Settlement
---------------
11.
Amount of Partial Settlement
--------------
12.
Amount of relief sought
Rs.42535/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claim
14.
Date of hearing/ Place of hearing
11.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Absent
b) For the Insurer
Sh. Krashanu Pundir, Legal Manager
16.
Date of Award/Order
Award/16.12.2019
17. Brief Facts of the Case:
Ms. Rajni (hereinafter referred to as the Complainant) had filed the complaint against the decision of the
ICICI Lombard General Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance
Company) alleging non-settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant had stated that her claim for Rs.42535/-
was rejected by the Insurance Company without any reason. The Insurance Company
should tell her about any requirement so that she can ask from the hospital for the same
and submit the same to them.
b) Insurer's Argument: The Insurance Company, vide its Self Contained Note (SCN)
dated 02.07.2019, stated that the patient was admitted in the Parth Hospital from
09.05.2019 to 13.05.2019, for treatment of fever, vomiting and pain in abdomen,whereas
in the Discharge Summary, nothing is mentioned about degree of fever for which he was
admitted. The patient was admitted for high fever but after going through the vital sign
record of the hospital, the fever temperature was normal i.e. 92 to 97.8 from May 10,
2019 which clearly indicate that the hospitalization was not required, the treatment could
have been managed through OPD. Further, the Insurance Company would like to
highlight that the hospital had generated the payment receipt No. 811 on May 9, 2019 and
receipt no.500 was generated on May 13, 2019. There was no co-relation between the
serial numbers of the receipts and the date on which the same were generated. After
verifying all the Invoice copies and hospital documents, the said claim was rejected and
the policy was cancelled on the basis of fraudulent claimsas per part III of the scheduleof
the Policy terms and conditions which states that “If any claim is in any respect
fraudulent, or if any false statement, or declaration is made or used in support thereof, or
any fraudulent means or devices are used by the insured or any one acting on his means
or devices are used by the insured any one acting on his behalf to obtain any benefit
under this not payable.”
19. Reason for registration of Complaint: Repudiation of claim as stated in Para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge Summary, Bills, GRO letter.
c) Copy of Rejection letter.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Complainant is absent. Insurer is present.

As per the discharge summary and vital signs records, the ailment was not serious enough to call
for hospitalization. Also, the documents submitted for claim, such as the vouchers for payment, are
also haphazard, giving credence to treatment of the claim as a fraud. Accordingly, the repudiation
by the Insurer was justified.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
16
th
December 2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule NO: 17 ofThe Insurance Ombudsman Rules, 2017)
OMBUDSMAN: SHRI SUDHIR KRISHNA
Case of Sh. AmitBhambri V/s Oriental Insurance Company Ltd.
Complaint Ref: DEL-H-050-1920-0357
Case No: HI/OIC/246/19
1.
Name & Address of the
Complainant
Sh. AmitBhambri
3 Park View, Karol Bagh, New Delhi-110005
2.
Policy No.
Type of Policy
Policy term/Policy Period
272203/48/2019/983
Mediclaim Policy
26.08.2018 to 25.08.2019
3.
Name of the insured
Name of the policy holder
Smt. ShaliniBhambri
Sh. AmitBhambri
4.
Name of insurer
Oriental Insurance Company Ltd.
5.
Date of Repudiation
05.05.2019,16.05.2019,17.06.2019, 26.06.2019,
23.08.2019 and 19.09.2019
6.
Reason for Grievance
------
7.
Date of receipt of the Complaint
13.09.2019
8.
Nature of Complaint
Non settlement of mediclaim
9.
Amount of Claim
Rs.719662/-
10.
Date of Partial Settlement
------
11.
Amount of Partial Settlement
------
12.
Amount of relief sought
Rs.719662/-
13.
Complaint registered under Rule
no:Insurance Ombudsman Rules
2017
Rule 13(1)(b) – any partial or total Repudiation of
claim.
14.
Date of hearing
03.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. AmitBhambri
b) For the Insurer
Sh. Anil Bhatia, Branch Manager
16.
Date of Award/Order
Award/04.12.2019
17. Brief Facts of the Case:
Sh. AmitBhambri (hereinafter referred to as the complainant) has filed the complaint against the
decision of Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance
Company) alleging non- settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that he had filed various claims in respect
to medical treatment of his wife who has been diagnosed as Stage IV Metastatic Carcinoma
Bilateral Brest Cancer with Skeletal Metastatic Invasive Ductal Carcinoma having ER/PR
Positive and her negative and is under treatment at Max Hospital Delhi, wherein she has been
prescribed Tab. Palbocilib 125mg along with Tab Letrozole and Inj. Zoledronic. All these drugs
are essential and is life saving. Injection Zoledronic is given as an inpatient under Oncologist
supervision and no OPD and no visitation day care analogy but treatment of Skeletal Metastisis
that has indisputable mortality and triggering hopeless prognosis. Most of the claims have been
rejected, one fully paid and one partially paid, giving reason that Inj. Zolderonic is not required as
in patient and does not fall into day care treatment. Though, it was held by TPA VipulMedicorp

vide their letter dated 02.05.2019 to Max Hospital that the administration of the Zoledronic Inj.
required medical supervision, however the Insurance Company has not approved this drug under
day care list. The complainant submitted the judgment of High Court as well as the order of State
Consumer Dispute Redressal Commission.
b) Insurer's Argument: The Insurance Company, vide its SCN dated 29.11.2019 has stated that the
patient was a known case of CA Breast, admitted for administration of Injection Zoledronate
which is a class of medications called bisphosphonate. As such the treatments through
bisphosphonates are not admissible under day care treatment. Neither administration of this drug
requires24 hour of hospitalization nor is it covered in day care procedure list given under
Appendix 1. Hence claim was not payable and recommended for rejection under clause 3.11.
19. Reason for registration of Complaint: Non settlement of mediclaim, as stated in Para 18 (a)
above.
20. The following documents were placed for perusal:
a) Copy of policy
b) Copy of discharge Summary, GRO letter, reports, Bills, Rejection letters.
c) Rejection letters, SCN of the Insurer along with enclosures.
21. Result of hearing with both parties (Observations and Conclusion):
I heard both the parties, the complainant as well as the Insurer.
Complainant was treated under hospitalisation in December 2018 for vacuum assisted excision of right
breast under local anaesthesia for which a claim under this policy was settled for Rs.2,52,238 including
pre-& post treatments.
Subsequently, the Complainant was administered a monthly dose of Inj. Zoledronate starting from
5.2.2019 for seven months, up to August 2019. Insurer has repudiated the seven claims for these
injections on the ground of Clause 3.11, which provides for reimbursement of only such day-care
procedures that are listed in Appendix-I.
Insurer states that Inj. Zoledronate is bisphosphonate, which is an antibody for enhanced immunity but
is not a chemotherapy to classify for reimbursement under Item 116 of Appendix-I. This appears to be
correct.
In the circumstances and evidences adduced by the parties, I come to the conclusion that the Insurer
was justified in repudiating the claim on the grounds stated above.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
04.12.2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
((Under Rule NO: 17 ofThe Insurance Ombudsman Rules, 2017))
OMBUDSMAN: SHRISUDHIR KRISHNA
Case of Ms. SurinderKaur V/S Oriental Insurance Company Ltd.
Complaint Ref: DEL-H-050-1920-0310
Case No: HI/OIC/217/19
1.
Name & Address of the Complainant
Ms. SurinderKaur
A-3/24, Sector-8, Rohini, New Delhi-110085
2.
Policy No.
Type of Policy
Policy term/Policy Period
272300/48/19/1656
Mediclaim Policy
30.09.2018 to 29.09.2019
3.
Name of the insured
Name of the policy holder
Ms. SurinderKaur
Ms. SurinderKaur
4.
Name of insurer
The Oriental Insurance Company Ltd.

5.
Date of Repudiation
04.06.2019
6.
Reason for Grievance
------
7.
Date of receipt of the Complaint
13.09.2019
8.
Nature of Complaint
Non settlement of mediclaim
9.
Amount of Claim
Rs.39328/-
10.
Date of Partial Settlement
------
11.
Amount of Partial Settlement
------
12.
Amount of relief sought
Rs.39328/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules 2017
Rule 13(1) (b) – any partial or total Repudiation of
claim.
14.
Date of hearing
03.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Ms. SurinderKaur
b) For the Insurer
Ms. Sushila Devi, Dy. Manager
16.
Date of Award/Order
Award/04.12.2019
17. Brief Facts of the Case
Ms. SurinderKaur (hereinafter referred to as the complainant) had filed the complaint against the
decision of Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent
Insurance Company) alleging non- settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that she was admitted in Dr. RP Centre,
AIIMS, NewDelhi with diagnosed Diabetic Retinopathy & Diabetic Macular Edema and
underwent administration of Intravitreal InjectionLucentis in her right eye on 04.02.2019. She
lodged claim for the same with the Insurance Company and the Insurance Company passed her
claim. She was again admitted in the same hospital and underwent the same procedure of
administration of Intravitreal Injection Lucentis in her right eye on 11.03.2019 and 15.04.2019.
She again lodged both the claim but this time Insurance Company repudiated both the claim
stating that Injection Lucentis is not included in the list of Daycare Procedures/Surgeries, hence
not payable.
c) Insurer's Argument: The Insurance Company, vide its SCN letters dated 13.11.2019 has stated
that the complainant was hospitalized twice at All India Institute of Medical Sciences, New Delhi
from 11.03.2019 to 12.03.2019 and from 15.04.2019 to 16.04.2019with diagnosis Moderate Non-
Proliferative Diabetic Retinopathy Right eye with Proliferative Diabetic Retinopathy Left Eye and
underwent administration of Intravitreal InjectionLucentis in Right eye. The claim is not
admissible since:
• administration of Intravitreal InjectionLucentis falls under OPD Protocol (out Patient treatment
vide definition 3.34 and Outpatient diagnostic, Medical/Surgical Procedure or treatment vide
exclusion clause 4.24)
• The policy covers the expenses incurred for hospitalization for a minimum period of 24 inpatient
care consecutive hours vides definition 3.17.
• The name of the procedure Administration of Intravitreal InjectionLucentis is not included in the
list of Daycare Procedure/Surgeries annexed at Appendix 1 of the Policy.
Further, the Insurance Company informed that inadvertently a claim of Rs.17644/- was paid to the
complainant. To rectify the mistake, a letter dated 27.04.2019 and reminder letter dated 20.06.2019 was
written by TPA to the complainant requesting her to return the amount to the Park Mediclaim as the mistake
was due to the human error, which was not replied by the complainant.
19. Reason for registration of Complaint: Non settlement of mediclaim as stated in para 18 (a)
above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of discharge summary, claim form, bills, Rejection.
c) SCN of Insurer along with enclosures.
21. Result of hearing with both parties (Observations and Conclusion):
I heard both the parties, the complainant as well as the Insurer.

Complainant was reimbursed an amount of Rs.17,644/- on 08.04.2019 by TPA for treatment of non-
proliferative diabetic retinopathy of right eye for which she was administered Inj. Lucentis on 4 February
2019. Subsequently she was administered the same injection in March 2019 and again in April 2019. For
these two treatments she had submitted the claim to the Insurer on 11.03.2019 and 15.04.2019,
respectively.
Insurer informed the Complainant on 04.06.2019 that the treatment undertaken was only an OPD
Protocol and was not covered in the list of Day-care procedures eligible for reimbursement vide
Appendix-I of the Policy.
Insurer states that in their internal audit, they realised that the payment made by TPA for the first claim
was a mistake and recovered the amount from the TPA on 19.06.2019, who in turn wrote to the
Complainant on 20.06.2019 to pay back the amount.
In the circumstances and evidences adduced by the parties, I come to the conclusion that the treatment
for which the claim was repudiated was not covered in the list of Day-care procedures eligible for
reimbursement vide Appendix-I of the Policy. Accordingly, Insurer was justified in repudiating the claim.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
3.12.2019
PROCEEDINGS OFTHE INSURANCE OMBUDSMAN, DELHI
((Under Rule NO: 16(1)/17 ofThe Insurance Ombudsman Rules, 2017))
OMBUDSMAN: SHRI SUDHIR KRISHNA
Case of Sh. AmarnathNarang V/S Oriental Insurance Company Ltd.
COMPLAINT REF: DEL-H-050-1920-0273
CASE No: HI/OIC/187/19
1.
Name & Address of the Complainant
Sh. AmarnathNarang
3, Neelgiri Apartments, Sector-9, Rohini, Delhi-
110085
2.
Policy No.
Type of Policy
Policy term/Policy Period
272900/48/2019/6661
Mediclaim Policy
16.07.2018 to 15.07.2019
3.
Name of the insured
Name of the policy holder
Sh. AmarnathNarang
Smt. Anpurna
4.
Name of insurer
Oriental Insurance Company Ltd.
5.
Date of Repudiation
29.08.2019
6.
Reason for Grievance
------
7.
Date of receipt of the Complaint
20.09.2019
8.
Nature of Complaint
Inadequate settlement of mediclaim
9.
Amount of Claim
Rs.14365/-
10.
Date of Partial Settlement
------
11.
Amount of Partial Settlement
------
12.
Amount of relief sought
Rs.14365/-
13.
Complaint registered under Rule
no:Insurance Ombudsman Rules
2017
Rule 13(1) (b) – any partial or total Repudiation
of claim.
14.
Date/Place of hearing
03.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. AmarnathNarang
b) For the Insurer
Ms. UpdeshKaur, Admn. Officer
16.
Date of Award/Order
Award/04.12.2019
17. Brief Facts of the Case
Sh. AmarnathNarang (hereinafter referred to as the complainant) has filed the complaint against
the decision of Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent
Insurance Company) alleging non- settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that he had undergone Bilateral Knee Surgery
in Saroj Hospital from 06.04.2019 to 10.04.2019 by cashless system in GIPSA PPN Hospital. As per
Discharge Card, surgeon had recommended for certain treatments/advice to be taken/followed after

Discharge. Accordingly, he had Physiotherapy and medication at his residence under the care of
physiotherapist with medicines as per discharge reports. The claim was lodged for Rs.14365/- to
TPAMedi Assist. His claim of Rs.14365/-was repudiated as per clause 2F (Sub-Limit 2F) of the
Policy.
b) Insurer's Argument: The Insurance Company, vide its SCN dated 13.11.2019 has stated that the
complainant is covered under PNB-Oriental Royal Mediclaim Policy for a Sum Insured of Rs.5 lakh with risk
commencement date from 16.07.2018 to 15.07.2019. The patient was admitted in Saroj Hospital & Heart
Institute for his treatment of bilateral primary osteoarthritis of knee on 06.04.2019 and was discharged on
10.04.2019. The amount claimed by the hospital under cashless was Rs.301444/- which was settled for
Rs.294444/- as full and final settlement by TPA as per policy terms & conditions. It is admitted that there is a
GIPSA/PPN rate agreement between Hospital, TPA and Insurance Company but these rates are applicable not
only for specific policy but also for other mediclaimproducts of the Company i.e. Happy Family Floater Policy,
Individual Mediclaim Policy etc. and the subject claim is for hospitalization for a procedure for which there is
specific capping of admissible expenses which are clearly mentioned in condition 2F(2) of the Policy. As per
Policy condition 2F(2), if Sum Insured opted is between Rs.200000/- to Rs.500000/-, maximum amount
payable for Bilateral Knee replacement is Rs.165000/- (Rs.110000/- + additional 40% for bilateral procedures)
plus cost of implant and medicines during hospitalization i.e. Rs.129444/-. Thus the liability of the Insurance
Company for that specific illness/injury/surgery during the entire policy period of one year is limited to the
capped amount.It is further submitted that insured applied for reimbursement of post hospitalization expense
of Rs.14365/- to TPA which was denied. It is pertinent to mention here that pre and post hospital expense
become admissible only for the specific disease for which there was hospitalisation. The cappingis for a
specific disease or procedure.
19. Reason for registration of Complaint: Inadequate settlement of mediclaim as stated in para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of discharge summary, claim form, GRO letter, settlement letter.
c) SCN of the Insurer along with enclosures.
21. Result of hearing with both parties (Observations and Conclusion):
I heard both the parties, the complainant as well as the Insurer.
Complainant was treated under hospitalisation on 6-10 April 2019 for treatment of knee pain. He made a
mediclaim No. 19334450 of Rs.3,01,444, which was settled in full except for Rs.7000/-through cashless
settlement. Complainants at first contested the non-settlement of this amount of Rs.7000/-, but vide his
letter dated 18.9.2019 to this office, withdrew the claim for the same.
Subsequently, Complainant filed another claim No. 19960081, which was changed to 20312385, on 29.6.2019
for post-hospitalisation treatment of physiotherapy and some medication, which were prescribed in the
Discharge Summary. This claim was repudiated by the Insurer vide Letter dated 29.8.2019 citing clause 2F(2)
of the Policy, which puts a sub-limit of Rs.1.10 lakh for the procedure of Total Knee Replacement excluding
implant, with 50% extra coverage for bilateral procedure. Insurer states that they have accordingly settled
the claim at 150% of Rs. 1.10 lakh, which is Rs.1.65 lakh. In addition, Insurer also paid Rs.1,29,444/- towards
the implant, which is indicated separately in the note below the same clause of the policy.
Complainant states that his claim for post-hospitalisation treatment should be settled separately under
Clause 2A (viii).
However, Insurer states that specified treatments are reimbursed as per package rates, which in this case is
the clause 2F (2) and additional claim under Clause 2A (viii) would not be applicable.
In my view, Insurer’s stand is correct. Accordingly, Insurer was justified in repudiating the claim
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
04.12.2019
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, DELHI
(UNDER RULE NO: 16 (1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN: SHRI SUDHIR KRISHNA
Case of M/s Space Travels V/S TheOreintal Insurance Company Ltd.
COMPLAINT REF: NO: DEL-G-050-1920-0126
CASE NO: HI/OIC/64/19
1.
Name & Address of The Complainant
M/s Space Travels
D-40/796,2
nd
Floor, 100 Feet Road SSN Marg,

ChattarpurPahari, New Delhi -110074
2.
Policy No.
Type of Policy
Policy term/Policy Period
212707/31/2019/3185
Motorclaim
12.09.2018 to 11.09.2019
3.
Name of the insured
Name of the policy holder
M/s Space Travels
M/s Space Travels
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
21.05.2019
6.
Reason for Grievance
Non-settlement of motor claim
7.
Date of receipt of the Complaint
26.11.2019
8.
Nature of Complaint
Non-settlement of motorclaim
9.
Amount of Claim
Rs.11,63,446/-
10.
Date of Partial Settlement
-----------
11.
Amount of Partial Settlement
-------------
12.
Amount of relief sought
Rs.11,63,446/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims
by an insurer
14.
Date of hearing/ Place of hearing
03.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. RakeshChanderKatyal, Proprietor
b) For the Insurer
Sh. ManoharLal, Asstt.
16.
Date of Award/Order
Award/05.12.2019
17. Brief Facts of the Case:
M/s Space Travels (hereinafter referred to as the complainant) had filed the complaint against the
decision of the Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance
Company) alleging non- settlement of motorclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that the vehicle met with an accident on
10.12.2018. He immediately lodged claim with the Insurance Company. The vehicle was
damaged beyond repair/total loss as per the repair estimate taken. Also, the driver died
subsequently during treatment at Safdarjung Hospital. All the information was duly recorded in
the FIR and informed to the Insurance Company along with the claim application. The Insurance
Company rejected the claim on the ground that class of vehicle under consideration can only be
driven by drivers with suitable endorsement on their private vehicle driving license. The
Complainant has quoted Supreme Court ruling and Transport Department notification in support
of the claim.
d) Insurer's Argument: The Insurance Company, vide its Self Contained Note (SCN) dated
14.10.2019 have stated that the Driving License No. BR45 20170043035 issued to Mr. Manoj Pal
was valid for LMV (Non-transport) and not for Passenger Carrying Vehicles. As such at the time
of accident, Mr. Manoj Pal (driver of the vehicle) was not authorized to drive passenger carrying
vehicle, which is violation of ‘Driver Clause’ of Motor Tariff which states that: “Any person
including insured: provided that a person driving holds an effective and valid driving license at
the time of the accident and is not disqualified from holding or obtaining such license”.
19. Reason for registration of Complaint: Repudiation of claim as stated in Para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of RC, DL.
c) Copy of information sought by the complainant under RTI from Ministry of Road Transport
and Highways.
d) Copy of the Circular No. RT-11016/01/2019-MVL dated 20.02.2019 ofMinistry of Road
Transport and Highways in compliance of judgment of Hon’ble Supreme Court in Civil
Appeal No. 5826 dated 03.07.2017.
e) Copy of Rejection & SCN of the Insurer along with enclosures.
21. Result of hearing with both parties (Observations and Conclusion):
Insurer had repudiated the claim on the grounds that the Driver had the driving licence (DL) only for
driving personal vehicle and not for commercial vehicle, which in this case was a six-seater Toyota
Innova. The Policy Bond states that a driver should have an effective driving licence but does not specify
any further, except in respect of Learner’s Licence, which in any case is not relevant here.

As the Ministry of Road Transport and Highways have clarified in their Circular dated 20.02.2019 in
compliance of the judgment of Hon’ble Supreme Court in Civil Appeal No. 5826 dated 03.07.2017 that
the LMV private driving license holder can ply the commercial LMV vehicle also and there is no need for
in DL endorsement to drive LMV commercial vehicle.
Complainant states that the LMV Licence, which his driver was holding, permits him to drive commercial
vehicle as well.
In the light of the judgment of the Supreme Court and the follow up notification by the Ministry of Road
Transport and Highways as cited above, the Complainant is right and, accordingly, repudiation by the
Insurer was not justified.
Award
The complaint is allowed and the Insurer is directed to to admit and settle the claim within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
05.12.2019
(UNDER RULE NO: 16 (1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN: SHRI SUDHIR KRISHNA
Case of Mrs. SumitraAggarwal V/S The Oriental Insurance Company Ltd.
Complaint Ref: No: DEL-H-050-1920-0294
Case No: HI/OIC/202/19
1.
Name & Address of The Complainant
Mrs. SumitraAggarwal
H.No. C-562, Block C, New Friends Colony, New Delhi-
110065
2.
Policy No.
Type of Policy
Policy term/Policy Period
272900/48/2019/4130
Mediclaim Policy
21.06.2018 to 20.06.2019
3.
Name of the insured
Name of the policy holder
Mrs. SumitraAggarwal
Mrs. SumitraAggarwal
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
20.11.2018
6.
Reason for Grievance
----------
7.
Date of receipt of the Complaint
12.09.2019
8.
Nature of Complaint
Non-settlement of mediclaim
9.
Amount of Claim
Rs.4,43,299/-
10.
Date of Partial Settlement
-------------
11.
Amount of Partial Settlement
------------
12.
Amount of relief sought
Rs.4,43,299/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claim
14.
Date of hearing/ Place of hearing
03.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. Jai PrakashAggarwal, Husband
b) For the Insurer
Ms. UpdeshKaur, Admn. Officer
16.
Date of Award/Order
Award/04.12.2019
17. Brief Facts of the Case:
Ms. SumitraAggarwal (hereinafter referred to as the complainant) had filed the complaint against the
decision of the Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance
Company) alleging non-settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant has stated that she was diagnosed with carcinoma
of the left breast pursuant to which she underwent a surgery in October, 2017 and was advised
eighteen cycles of chemotherapy on a 3 week basis. Thereafter the complainant received 6
maintenance chemotherapy sessions from June, 2018 to October, 2018 at Indraprastha Apollo
Hospital and submitted the claims forms simultaneously. Subsequently, the Insurance Company
wrongly repudiated all the claims stating therein that the drug used in the chemotherapy is non-
conventional and therefore the same is not payable under the policy terms and conditions. The
complainant also submitted the copy of the award of the Insurance Ombudsman, Pune in which
the claim was allowed for the same injection.

b) Insurer's Argument: The Insurance Company, vide its SCN dated 02.12.2019 has stated that
they have received the request for reimbursement of expenses for six claims incurred by Insured
on different dates for injection Hertraz 440mg at Indraprastha Apollo Hospital, New Delhi. It is
pertinent to mention that as per the medical opinion and other hospital documents, claimant was
treated with Chemo drug Trastuzumab, an antineoplastic which is adjuvant/targeted/maintenance
Chemotherapy. The claim pertains to targeted/maintenance Chemotherapy for administration of
injection Herteraz, hence the claims for administration of injection are not admissible under
policy exclusion clause 4.21. Further, the treatment does not required hospitalization and it can
be treated under OPD and it is not listed under day care procedure mentioned in terms and
conditions of the Policy. Hence claim was denied under the clause 3.14 of Day Care treatment
and 4.21 which states that: “Treatment in respect sleep apnoea and immune modulator drugs for
cancer treatment” are not covered under the policy.
19. Reason for registration of Complaint: Repudiation of claim as stated in Para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of, Bill, Receipt, etc.
c) Copy of Rejection Letter, SCN of the Insurer along with enclosures.
21. Result of hearing with both parties (Observations and Conclusion):
Complainant was treated under hospitalisation in October 2017 for surgical management of breast
cancer, which was settled by the Insurer for Rs. 5 lakh, which was the sum assured for 2017-18.
Subsequently, the policy was renewed for 2018-19 and Complainant was administered a series of
maintenance chemotherapy through Inj. Hertraz 44mg, which is same as Trastuzumab. She submitted
six claims for these treatments.
Complainant states that the procedure under claim/repudiation was the same as cancer chemotherapy,
which is an admissible item in the Appendix-1 at Sl. No. 116.
Insurer repudiated all these claims on the following two grounds:
a. Insurer treated these treatments as Day-care and repudiated all these claims by invoking
the Clause 3.14 read with Appendix-1, which lists such Day-care procedures that are
admissible for reimbursement.
b. Insurer treated these treatments as immune-modulator drugs for cancer treatment, which
are excluded from reimbursement under Clause 4.21.
In the circumstances and evidences adduced by the parties, I come to the conclusion that the Insurer
was justified in repudiating the claim on the grounds stated above.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
04.12.2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(UNDER RULE NO: 16 (1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN: SHRI SUDHIR KRISHNA
Case of Sh. Om Dutt SharmaV/S The Oriental Insurance Company Ltd.
Complaint Ref: No: DEL-H-050-1920-0353
Case No: HI/OIC/242/19
1.
Name & Address of the Complainant
Sh. Om Dutt Sharma
49/A, AbhayKhand 1, Inderapuram, Ghaziabad
Uttar Pradesh- 201010
2.
Policy No.
Type of Policy
Policy term/Policy Period
271700/48/2019/2298
Mediclaim Policy
10.02.2019 to 09.02.2020
3.
Name of the insured
Name of the policy holder
Sh. Om Dutt Sharma
Sh. Om Dutt Sharma
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
23.08.2019
6.
Reason for Grievance
-----------
7.
Date of receipt of the Complaint
23.10.2019
8.
Nature of Complaint
Non-settlement of mediclaim

9.
Amount of Claim
Rs.1,56,406/-
10.
Date of Partial Settlement
--------------
11.
Amount of Partial Settlement
-------------
12.
Amount of relief sought
Rs.1,56,406/-
13.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claim
14.
Date of hearing/ Place of hearing
03.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. Om Dutt Sharma
b) For the Insurer
Sh. Kushal Kumar, Admn. Officer
16.
Date of Award/Order
Award/04.12.2019
17. Brief Facts of the Case:
Sh. Om Dutt Sharma (hereinafter referred to as the complainant) has filed the complaint against the decision
of the Oriental Insurance Company Ltd. (hereinafter referred to as the Respondent Insurance Company)
alleging non-settlement of mediclaim.
18. Cause of Complaint:
a) Complainant's Argument: The complainant had stated that he had taken the Health Insurance
Policy from the Oriental Insurance Company. He preferred a health claim to the Insurance
Company for hospitalisation at Saaol Heart Centre, Delhi from 14.04.2019 to 17.06.2019 for
treatment of EECP (natural by pass) BCA/EDTA therapy. The Insurance Company repudiated
his claim under Clause 4.19 which states that treatment for age related macular degeneration
(ARMD) external counter pulsation (ECP), Enhanced External Counter Pulsation (EECP),
Hyperbaric Oxygen Therapy is not covered under the Policy. He was suffering from coronary
Artery disease (CAD) and taken treatment EECP (natural bypass) and BCA for CAD under the
supervision of Dr. BimalChhajer, MBBS, MD trained doctor from AIIMS. Hence, the claim
should be paid to him.
b) Insurer's Argument: The Insurance Company, vide its SCN dated 31.10.2019 had stated that the
complainant had taken treatment at SAAOL HEART CENTRE, PreetVihar which does not fall
under the category of Hospital, as per the definition of Hospital/nursing Home, defined in the
terms and conditions of the policy. The hospital is neither Regd. nor it fulfills the required criteria
of inpatient beds, fully equipped OT, surgical, diagnostic & Pathological facilities of its own. The
patient had gone through a process of various sittings which were not a part of hospitalization, but
a kind of OPD treatment like that of Physiotherapy,which is not covered under clause3.11 of the
policy terms and conditions. The complainant had submitted Discharge Summary, prepared by
the treating doctor on his prescription and was not a discharge summary of the hospital, which
itself was a proof that the treatment was not under hospitalization and that too in a hospital
defined under the scheme. Hence, the claim was repudiated.
19. Reason for registration of Complaint: - Repudiation of claim as stated in Para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of Discharge summary, Copy of Insurance Ombudsman Award Copy, Bill, Receipt.
c) Copy of Rejection letter, SCN of the Insurer along with enclosures.
21. Result of hearing with both parties (Observations and Conclusion):
I heard both the parties, the complainant as well as the Insurer.
Complainant states that the treatment undertaken by him for the coronary artery disease (CAD) was
cheaper and safer alternative to the conventional angioplasty/bypass surgery.
Insurer states that the treatment undertaken by the Complainant is yet an unproven procedure. He also
states that the hospitalisation was on 14.04.2019, whereas the Discharge Summary is dated 17.06.2019,
and includes subsequent day-to-day treatments, which do not qualify as approved procedures for
reimbursement.
In the circumstances and evidences adduced by the parties, I come to the conclusion that the Insurer
was justified in repudiating the claim on the grounds stated above.

Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
04.12.2019
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(UNDER RULE NO: 16 (1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN: SHRI SUDHIR KRISHNA
Case of Sh. SohanDobriyal V/S The Oriental Insurance Company Ltd.
Complaint Ref: No: DEL-H-050-1920-0332
Case No: HI/OIC/238/19
1.
Name & Address Of The Complainant
Sh. SohanDobriyal
N-46, Sectpr-12, Noida, Uttar Pradesh- 201301
2.
Policy No.
Type Of Policy
Policy term/Policy Period
215400/48/2017/5281
Mediclaim Policy
14.03.2017 to 13.03.2018
3.
Name of the insured
Name of the policy holder
Sh. SohanDobriyal
Sh. SohanDobriyal
4.
Name of insurer
The Oriental Insurance Company Ltd.
5.
Date of Repudiation
28.05.2018
6.
Reason For Grievance
-------------
7.
Date of receipt of the Complaint
23.09.2019
8.
Nature of Complaint
Non-settlement of mediclaim
9.
Amount of Claim
Rs.2,27,833/-
10.
Date of Partial Settlement
----------
11.
Amount of Partial Settlement
-------------
12.
Amount of relief sought
Rs.2,27,833/-
13.
Complaint registered under Rule no:
Insurance Ombudsman rules
Rule 13(1)(b) – any partial or total repudiation of claim
14.
Date of hearing/ Place of hearing
03.12.2019/Delhi
15.
Representation at the hearing
a) For the Complainant
Sh. SohanDobriyal
b) For the Insurer
Sh. VedPrakash, Sr. Divisional Manager
16.
Date of Award/Order
Award/04.12.2019
17. Brief Facts of the Case:
Sh. SohanDobriyal (hereinafter referred to as the complainant) had filed the complaint against the
decision of the Oriental Insurance Company Ltd. (hereinafterreferred to as the Respondent Insurance
Company) alleging non-settlement of mediclaim.
18.Cause of Complaint:
a) Complainant's Argument: The complainant has stated that he was admitted in Metro Hospital,
Noida from 13.01.2018 to 17.01.2018 with diagnosis of Coronary Artery Disease (Triple Vessel
Disease), Acute Lateral Wall MI, Adequate LV Function, Accelerated Hypertension, DM Type II.
The Insurance Company had denied his claim under Exclusion 4.3 whereas Coronary Artery
Disease and Acute lateral wall MI are not listed in the exclusion list. As per the policy wordings
Diabetes and Hypertension has a waiting period of 2 years, so the Insurance Company can
deduct the charges related to these diseases along with copayment as applicable and reimburse
the balance to him.
b) Insurer's Argument: The Insurance Company, vide its SCN dated 16.10.2019 has stated that the
complainant wad admitted in the Metro Hospital from 13.01.2018 to 17.01.2018 with
complaints of retrosternal chest pain on exertion. He has been diagnosis with Coronary Artery
Disease (CAD), Acute Lateral Wall MI, Adequate LV Function, Accelerated Hypertension &
Diabetes Mellitus (DM Type-II). The claim was lodged during the first year of Policy for
Hypertension and Diabetes Mellitus which is under the exclusion of 2 years in the policy terms
and conditions. Hence, the claim was repudiated under clause 4.1 relating to all pre-existing
disease which is covered after 4 year from the inception of the policy.
19. Reason for registration of Complaint: - Repudiation of claim as stated in Para 18 (a) above.

20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of, Bill, Receipt, etc.
c) Copy of Rejection, SCN of the Insurer along with enclosures.
21. Result of hearing with both parties (Observations and Conclusion):
I heard both the parties, the complainant as well as the Insurer.
Complainant was treated under hospitalisation during 13-17 Jan. 2018 for Coronary Artery Disease and
was administered stent. Insurer states that as per Policy Clause No. 4.1, this ailment is excluded for
reimbursement for 48 months from the inception of the Policy.
Complainant states that he had received an email from the TPA informing that his claim was partially
settled for Rs.15,407/- then why has the Insurer not admitted the remaining claim.
Insurer states that they have made inquiries and found out that the said amount of Rs.15,407 pertained
to another Insurer and has no relation with this Insurer.
In the circumstances and evidences adduced by the parties, I come to the conclusion that the Insurer
was justified in repudiating the claim on the grounds stated in the rejection letter.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
04.12.2019
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Brigadier Arjun Ravi Kant & Others V/S The Oriental Insurance Co. Ltd.
COMPLAINT REF. NO: CHD-G-050-1819-0807
1.
Name & Address of the Complainant
Mr. Brigadier Arjun Ravi Kant & Others
HIC-054, Block, Wested Heights, Paras Hospital
Road, DLF Phase- V, Gurugram, Haryana-
122009
2.
Policy No:
Type of Policy
Duration of policy/Policy period
121600/48/2011/24, 121600/48/2011/23,
121600/48/2011/26, 121600/48/2012/525,
121600/48/2012/526
3.
Name of the insured
Name of the policyholder
Mr. Mukul Dutt, Mr. Brigadier Arjun Ravi Kant
& Others
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the Complaint
17-01-2019
8.
Nature of complaint
Misselling / fraud in policy issuance
9.
Amount of Claim
NA
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
NA
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(g) –issuance of policies which is not
in conformity with the proposal form
submitted by proposer
13.
Date of hearing/place
23-09-2019, 07-11-2019 and 03/12/2019 /
Chandigarh
14.
Representation at the hearing
For the Complainant
03/12/2019 Brig. Arun Kumar Ravi Kant
For the insurer
23/09/2019 Sh. Balwinder Kumar
07/11/2019 Ms. Indu Khurana
03/12/2019 Ms. Indu Khurana
15
Complaint how disposed
Award

16
Date of Award/Order
03/12/2019
17) Brief Facts of the Case:
On 17-01-2019, Mr. Brigadier Arjun Ravi Kant & Others had filed a complaint regarding
fraudulent issuance of seven deferred bhavishya Arogya health care policies applied by his
family members and close friends under the express assurance by broker of oriental insurance
for deferred comprehensive health insurance for life time from the deferment age of 58 for a
total life time fixed sum of Rs.20,00,000/-till exhausted by Medicare as and when needed. But
they frequently issued for concurrent cover ending in 10 years..
1. Arjun Ravi Kant , Pol. No 121600/48/2011/24 dated 06/04/2010,Paid Rs. 36337/-
2. Sarat Chopra, Pol. No 121600/48/2011/23 dated 06/04/2010,Paid Rs. 78261/-
3. Shivani Chopra, Pol. No 121600/48/2011/26 dated 06/04/2010,Paid Rs. 64517/-
4. Mohit Thukral, ,Paid Rs. 86172/-
5. Latika Thukral,
6. Mukul Datt, Pol. No 121600/48/2012/525 dated 20/09/11,Paid Rs. 48600/-
7. Vandana Datt, Pol. No 121600/48/2012/526 dated 06/04/2010,Paid Rs. 36442/-
Policies were issued by Oriental Insurance, Mumbai although were applied at Delhi.
The risk on this policy shall commence on attaining the age of 58 yrs and would continue for lifetime.
They observe that there is a seemingly deliberate faint date stamp, mysteriously almost masked by a
superimposed rubber stamp, uniformly on all policies, as if on purpose with deliberate intent to mask
the policy period since it violates the requirement of deferred validity mandated in the Bhavishya
Arogya Schedule. Further policy documents are titled ‘Special Contingency insurance policy Schedule’
and not ‘Bhavishya Arogya Policy, for which proposal forms were filled and money tendered.
Complainants requested for directions to the insurance company to ensure that the providing lifetime
cover for Rs. 20 lakhs after age 58, as stated in Clause (2) period of risk, on page 6 of schedule of
Bhavishya Arogya policy for Reliance.
On 28-02-2019, the complaint was forwarded to The Oriental Insurance Co. Ltd. Regional Office,
Chandigarh, for Para-wise comments and submission of a self-contained note about facts of the case,
which was made available to this office on 19.09.19.
As per SCN submitted by insurance company, their Mumbai office has issued following five Special
Contingency Policies (Bhavishya Arogya cover) & they confirm these policies are not fraud policies:
1. 121600/48/2011/23
2. 121600/48/2011/24
3. 121600/48/2011/26
4. 121600/48/2012/525
5. 121600/48/2012/526
As policy numbers were not provided in respect of Mohit Thukral and Ms. Latika Thukral, they can’t
comment on same.
Another SCN dt. 29/11/2019 has been received and it is submitted by the insurer that a good number of
Bhavishya Arogya Policies were issued through a Broker Reliance Insurance Broking Limited. Later, this
policy was discontinued but the risks which were already incepted were required to be booked in INLIAS
so that the claim if any can be processed and settled in future. It was,therefore, booked under “ Special
Contingency Policy since Bhavishya Arogya Policy “ which no longer existed. The period of insurance also
could not be appropriately reflected because in INLIAS Policy period fields does not allow period more
than 10 years. Under these circumstances, from the face of policy, the complainant appears to have
become suspicious about the policy documents issued to him. The matter was initially discussed at R.O
and as per the line of action suggested, the broker vide their mail dated 19/11/2018 had confirmed that
the policies were placed through them i.e. Reliance Insurance Broking Limited. However we could not
write to the insured clarifying above position. As such no correspondence exchanged with the Insured.
The risk covered under Bhavishya Arogya Policy is for life time from the retiring date opted under the
policy. As such the coverage is for life time.i.e till exhaustion of the Sum Insured or death of the insured
which ever is earlier. But since our U/W software INLIAS ask for input in its field of data while
underwriting, we cannot put an indefinite period in the policy. Therefore the policy was punched by
giving some date for period i.e 5 years/ 10 years. As regards, certified copy of all the policies mentioned
in the complaint regarding endorsement rectifying the coverage of the insurance, we have already taken
up the matter with our regional office.As the product, Bhavishya Arogya Policy was discontinued, in its
place Special Contingency Policy was issued.
The complainant was sent Annexure VI-A for compliance, which reached this office on 26-03-2019.
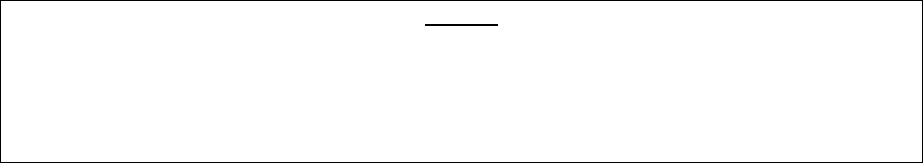
20) Cause of Complaint:
c) Complainant’s argument: The deferred Bhavishya Argogya policies issued to the complainant
family members and close friends appears to be fraudulent because the cover does not
commence at the age 58 years for life time and ends just after a short period of 10 years.
d) Insurers’ argument: Insurance Company stated that all the details of the policies are genuine
and underwriting office has confirmed that policies number given by the complainant are
checked in system and found correct.
19) Reason for Registration of Complaint:- within the scope of the Insurance Ombudsman Rules,
2017.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
22) Result of Personal hearing with both parties (Observations & Conclusion).
On careful examination of various documents including the copy of the complaint, SCN
submitted by insurance company and submissions made by the parties during personal hearing,
it is observed that the complainants had raised the issue that why the policy documents issued
to them are titled “Special Contingency Insurance Policy schedule” and not Bhavishya Arogaya
Policy for which proposal forms were filled and money tendered. The cover for fixed Sum
Insured of Rs. 20,00,000/- was to commence on attaining the age of 58 years and would
continue for life time or till the sum insured is exhausted by way of claims . But the documents
received are titled Special Contingency insurance policies having a faint date and stamp with
deliberate intent to mask the policy period. Hence they became suspicious about the policy
documents issued to them and took up the matter with the insurer as it does not commence for
lifetime but ends after a short period of just 10 years. Insurance company confirmed that
Bhavishya Arogya Policies were issued through a Broker Reliance Insurance Broking Limited.
Later on this type of policy was discontinued but the risks which were already incepted were
required to be booked in INLIAS. It was, therefore, booked under “Special Contingency Policy
since Bhavishya Arogya Policy “which no longer existed. The period of insurance also could not
be appropriately reflected because in INLIAS Policy period fields does not allow period more
than 10 years. Under these circumstances, from the face of policy, the complainant appears to
have become suspicious about the policy documents issued to him. However they have
admitted about not writing to the insured clarifying above position. In the light of explanation
given by the insurance company, it can be concluded that policies issued in the names of Sh.
Arjun Ravi Kant, Sh. Sarat Chopra, Ms Shivani Chopra, Sh. Mukul Dutt & Ms. Vandana Dutt are
genuine. The complainants have raised the issue of genuineness and defects in their policies at
this belated stage after eight years of issuance. The policies issued by the insurance company
have been found to be defective with regard to period of insurance and not using the proper
policy bonds. The insurance company’s representative offered to issue proper endorsement for
coverage and removal of defects pointed out in the policies to which the complainant’s
representative agreed. Therefore the insurance company is directed to issue the necessary
endorsement rectifying all the defects in the policies issued in the names of Sh. Arjun Ravi Kant,
Sh. Sarat Chopra, Ms Shivani Chopra, Sh. Mukul Dutt & Ms. Vandana Dutt within a period of 30
days from the receipt of award copy. No order is passed with regard to the complaint of Mutika
Thukral and Mohit Thukral as they did not provide any policy particulars.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of personal hearing, the insurer is hereby directed to issue proper
endorsements rectifying the defects in the policies.
Hence, the complaint is hereby treated as closed.
Dated at Chandigarh on 3
rd
day of December, 2019.
D.K. VERMA
INSURANCE OMBUDSMAN

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Major Harpal Singh Virk V/S The New India Assurance Co. Ltd.
COMPLAINT REF. NO: CHD-H-049-1920-0031
1.
Name & Address of the Complainant
Mr. Major Harpal Singh Virk
Apt. 1008 A, The Magnolias DLF Phase-5,
Golf Course Road, Gurugram, Haryana- 122009
Mobile No.- 9313116799
2.
Policy No:
Type of Policy
Duration of policy/Policy period
31280134179500000619,31280134177800000393,
31280134189500000730, 31280134187800000308
Mediclaim Policy
01-03-2018 to 28-02-2019, 01-03-2018 To 29-02-
2020
3.
Name of the insured
Name of the policyholder
Mr. Major Harpal Singh Virk
Ms. Sudeep Virk
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
Various
6.
Reason for repudiation
Sum Insured exhausted and Procedure not payable
7.
Date of receipt of the Complaint
16-04-2019
8.
Nature of complaint
Non payment of claim
9.
Amount of Claim
Rs. 1131851/-
10.
Date of Partial Settlement
Feb. 2019
11.
Amount of relief sought
Rs. 8,07,789/-
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation of
claim by an insurer
13.
Date of hearing/place
07-11-2019 / Chandigarh
14.
Representation at the hearing
For the Complainant
Major Harpal Singh, Complainant
For the insurer
Ms. Deep Shikha, Deputy Manager
15
Complaint how disposed
Award + Interest
16
Date of Award/Order
25-11-2019
17) Brief Facts of the Case:
On 16-04-2019, Mr. Major Harpal Singh Virk had filed a complaint vide which he informed that he and
his wife has mediclaim base policy of 12 lakhs each and Top up policy of 22 lakh each for years 2018-19
and then for the year 2019-20. In Aug.2018, his wife Mrs. Sudeep Virk was diagnosed with Cancer Ovary
Stage 111 c. The course of treatment recommended by Doctor of Max Cancer Care, New Delhi was 3
cycles of 36 weekly Neo-Adjuvant Chemotherapy followed by surgery and another 3 weekly 3 cycles of
Adjuvant Chemotherapy. This to be followed by a maintenance dos of Avastin (Bevacizumab)
(Bevacizumab). As advised and on pre-authorization approval by TPA, they started treatment on
28.08.18 initially from Max Cancer Care, New Delhi and then from Manipal Hospital, Banglore. The
expenses of the hospitalization came to Rs. 13,21827/- out of which TPA passed only Rs. 11,04,606/-
with the remark – ‘SI Exhausted’, when the patient has 12 lakhs plus 22 lakhs policies. Due to continuous
vomiting, she was admitted in the hospital from 16
th
to 19
th
Nov.18. The hospital bill of Rs. 90368/- was
declined by E-Meditek. With remarks ‘Threshold limit not (?) exhausted.’ They have total insurance of
Rs. 12 lakhs plus Rs. 22 lakhs, i.e. 34 lakhs, but TPA declined the claim of just Rs. 13 lakhs with the
remark, ‘SI Exhausted’. Further, they returned to Gurgaon from Bangalore resumed the Adjuvant
Chemotherapy. As E-Mediteck has been black listed by IRDAI, they have to pay from their pocked and
subsequently claim reimbursement. Various reimbursement claims have been put in for the Adjuvant
Chemotherapy, various investigations and anti cancer prevention maintenance treatment of Avastin
(Bevacizumab) (Bevacizumab) besides the two balance amounts mentioned above of the hospital
admissions, i.e. Rs. 2,17,211 and Rs. 90,368/- lying pending since Mid November 2018. After claim of 3
rd
dose of Anti Cancer Prevention Maintenance, mediclaim policy was renewed for the year 2019-20 for
the same sum of Rs. 12 lakh (base) and Rs. 22 lakh(top up) with TPA was now Health Insurance TPA of
India Ltd. But when for fourth doze, cash less was applied, the same was denied by TPA with the remark
that ‘Admission for Inj. Bevacizumab is not payable’. The total claims lying outstanding with till date
amount to Rs. 10,81,979/- out of this, company has paid Rs. 3,24,062/- in the mid of Feb. 2019, leaving a
balance of Rs. 7,57,917/-.
On 30-04-2019, the complaint was forwarded to The New India Assurance Co. Ltd. Regional Office, New
Delhi, for Para-wise comments and submission of a self-contained note about facts of the case, which
was made available to this office on 05.11.19.
As per SCN received from insurance company, they have issued pol.no. 31280134179500000619 & top
up 31280134177800000393 for the period 01.03.18 to 28.02.19 & also issued pol.no.
31280134189500000730 & top pol.no. 31280134187800000308. Mrs. Sudeep Virk is a diagnosed case of
CA-OVARY and the expenses of hospitalization for same came to Rs. 13,21,827/-. TPA has passed Rs.
11,04,606/-. Amount of claim of Rs. 217,211/- was paid in top-up policy which was claimed by insured
with Rs. 90,368/-(being hospitalization paid by insured) + Rs. 37,794.12 (being post hospitalization
expenses) totaling to Rs. 3,45,373/-. Out of this, total claim amount of Rs. 2,63,462/- was paid to
Mr.Harpal Singh Virk on 06.03.2019, and the balance of Rs. 81,911/- was deducting being non payable
items.
In Aug.2018, Rs. 79091/- for tests conducted for detection and confirmation of cancer. As per insurance
company they have not received claim file from TPA in which the same amount was claimed by insured.
Claim of 4
th
Adjuvant chemotherapy dt. 01.12.18 paid on 06.03.19. Rs. 100/- deducted being a non-
payable item. Claim of 5
th
Adjuvant chemotherapy dt. 22.04.18, Rs. 33351/- paid on 03.03.19. Rs. 5287/-
was deducted being non payable. Claim of 21.01.19, for Rs. 1,47,529/- was paid against claimed amount
of Rs. 1,56,433/- on 24.03.19. An amount of Rs. 8904/- was deducted in absence of doctors prescription
against bill dt. 15.01.19 of Rs.8904/-. Insurance company has no information of status from TPA
regarding claim of Rs. 153749/- of dt. 14.02.19 related with PET CT Scan test on 30.01.19 plus
maintenance dose of Avastin (Bevacizumab) Admission on 02.02.19 & also information regarding claim
of Rs. 1,29,056/-, 3
rd
dose of Avastin (Bevacizumab) , dt. 27.02.19.
Complaint is also made regarding16.03.19,4
th
dose of Avastin (Bevacizumab) , claim of Rs. 1,22,652/-
and no cashless approved for claim of Rs. 41,872/-. Two claims has been repudiated vide letter dt.
08.07.19 & 07.08.19 as per clause 2.16, bevacizumab monoclonal antibody is given, which is not listed
day care procedure and hospitalization is not justified.
The complainant was sent Annexure VI-A for compliance, which reached this office on 07-05-2019.
18) Cause of Complaint:
a) Complainant’s argument: Complainant stated that his genuine claim is repudiated on the flimsy
ground by the insurance company. He pleaded that his claim is not paid by the insurance
company on the ground that sum insured is exhausted whereas he had adequate sum insured
under the policies.
b) Insurers’ argument: Insurance Company stated that all the deductions are made as per policy
terms and condition and nothing is due to payment. Insurance Company stated that as per
policy terms and conditions the dose of Avastin (Bevacizumab) is not a listed day care procedure
and also the hospitalization not justified.
19) Reason for Registration of Complaint:- within the scope of the Insurance Ombudsman Rules, 2017.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21) Result of Personal hearing with both parties(Observations & Conclusion)
I have gone through the contents of the complaint and supporting documents, SCN given by the
insurance company, additional documents submitted by the complainant during personal hearing and
submission made by both the parties during personal hearing. It is seen that there is no dispute with
regard to diagnosis of complainant’s wife with CA ovary stage 111c in August 2018. Complainant is
continuously renewing the policy on time for last 20 years. There is also no dispute with regard to
mediclaim policies which complainant and his wife had where a normal policy with sum insured of Rs 12
lakhs and top up policy of Rs 22 lakh is issued by Insurance Company. It is seen that course of treatment
recommended by senior oncologists of Max cancer care New Delhi was 3 cycles of 3 weekly neo-
adjuvant chemotherapy followed by surgery and another 3 weekly 3 cycles of adjuvant chemotherapy
which was followed by a maintenance dose of Avastin (Bevacizumab) . Complainant took his wife to
Manipal Hospital, Bangalore for surgery by famous Oncologist on 08-10-2018 and accordingly Insurance
Company was informed in advance after obtaining pre-authorization for surgery which was planned for
31-10-2018. His wife was discharged on 14-11-2018 and the expenses of hospitalization came to Rs
1321827/- but TPA has passed only Rs 1104606/- with the remark that sum insured exhausted and
asked the complainant to pay Rs to 217211/- from his pocket. Complainant inspite of having a top up
policy with sum insured of Rs 22,00,000/- was not given the approval by the concern TPA/Insurance
company and they kept on lingering the payment and ultimately complainant have to make a payment
to get his wife discharge from the hospital. Complainant wife was re-admitted in hospital from 16-11-
2018 to 19-11-2018 due to severe dehydration and the hospital bill of Rs 90368/- was again declined by
insurance company with a remark threshold limit not exhausted. Complainant wife underwent PET CT
scan test on 30-01-2019 plus maintenance dose of Avastin (Bevacizumab) and bill amounting to Rs
153749/- is still pending. Complainant’s wife underwent third dose of Avastin (Bevacizumab) on 27-02-
2019 and he incurred an expense of Rs 129056/-. Fourth dose of Avastin (Bevacizumab) was given to

complainant’s wife on 16-04-2019 and he incurred an expense of Rs 122652/-. Fifth dose of Avastin
(Bevacizumab) was given to complainant’s wife on 06-04- 2019 wherein he incurred an expense of Rs
41872/-. Complainant stated that all these are reimbursement claim which he paid from his pocket and
as per policy which was supposed to be cashless payment and it has resulted in breaking off his life’s
saving fixed fund and undergone great mental stress. He requested for payment of his pending claims
which is being denied on flimsy ground of sum insured exhausted in spite of having the proper and
adequate coverage. Complainant also informed that claims of February 2019 is still pending and vide
letter 18-10-2019 he came to know that files are still oscillating between the offices and TPA for
processing. Insurance company denies having any knowledge of claim lodged by complainant of
February 2019 with them.
On going through the documents, it is seen that complainant has informed that four claims filed by
complainant for his treatment on various dates for has been denied by insurance company by various
repudiation letters due to reasons that the complainant has been treated with injection Avastin
(Bevacizumab) and still are pending. According to insurance company the treatment with the said
injection being not a listed day care procedure and also that hospitalization is not justified the said
claims have been denied. As per documents complainant has been discharged on same day it is also a
fact that the complainant is a case of CA ovary stage 111c that has been prescribed and on regular
treatment by chemotherapy. I have gone through the terms and conditions of policy Cancer
chemotherapy is specifically covered under the list of day care procedure at Annexure- I under 139. The
treatment by injection Avastin (Bevacizumab) which is nothing but chemotherapy being specifically
covered. Further, there is also no term and conditions in the policy which states denial of claim for the
above said reason. It is very erroneous on the part of insurance company to repudiated claim on shaky
and flimsy grounds. It is not only non-settlement of genuine claim by insurance company but also is a
direct harassment of genuine policyholder who has been holding policy since long. As such there is
deficiency of service noted on the part of insurance company where by insurance company have simply
taken into account the TPA action and without reviewing the same claim has been made non- payable. It
is also like adding insult to injury, wherein insurance company denies of complainant lodged claim of
February 2019 in personal hearing and on other hand complainant produces the letter of insurance
company written to TPA on 18
th
October 2019 wherein TPA is directed to process these claim files of
February 2019 claim. This itself reflects about the service parameters of insurance company and need of
customer for insurance benefit. There is inordinate delay noted on the part of insurance company by
denying the legitimate claim on fragile and feeble ground of exhausting of sum insured to harass
policyholder. As such the insurance company is directed to pay admissible claim amount subject to
terms and condition of policy in all pending claim along-with 6% simple interest from the date of
submission of claim form to TPA for two cases i.e 28.02.2019 for claim no NIA-111 and NIA110 and in
other pending cases from the date of submission of claim form to TPA till realization towards full and
final settlement of the claim within 30 days after the receipt of copy of award.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by
both the parties during the course of personal hearing, insurance company is directed to
pay admissible claim amount subject to terms and condition of policy in all pending claim
along-with 6% simple interest from the date of submission of claim form to TPA for two
cases i.e 28.02.2019 for claim no NIA-111 and NIA110 and in other pending cases from the
date of submission of claim form to TPA till realization is hereby awarded to be paid by the
Insurer to the Insured, towards full and final settlement of the claim.
Hence, the complaint is treated as closed.
Dated at Chandigarh on 25
th
day of November 2019.
D.K. VERMA
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Varun Bedi V/S The National Insurance Co. Ltd.
COMPLAINT REF. NO: CHD-H-048-1920-0067
1.
Name & Address of the Complainant
Mr. Varun Bedi
SCO- 17, Sector- 34C, Chandigarh,
Mobile No.- 9855666666
2.
Policy No:
Type of Policy
Duration of policy/Policy period
420201/48/16/8500000029
Mediclaim Policy
23-06-2016 To 22-06-2017
3.
Name of the insured
Name of the policyholder
Mr. Varun Bedi, Mrs. Meena Bedi
Mr. Varun Bedi

4.
Name of the insurer
The National Insurance Co. Ltd.
5.
Date of Repudiation
13.02.19
6.
Reason for repudiation
Peritoneal dialysis not payable.
7.
Date of receipt of the Complaint
03-05-2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 11,12,741.40 P
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs. 11,12,741.40 P
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claim by an insurer
13.
Date of hearing/place
07-11-2019 / Chandigarh
14.
Representation at the hearing
For the Complainant
Mr. Varun Bedi
For the insurer
Mr. Subash Munshi
15
Complaint how disposed
Dismissed
16
Date of Award/Order
24.12.2019
17) Brief Facts of the Case:
On 03-05-2019, Mr. Varun Bedi had filed a complaint that he has policy since 2004. In 2016, his wife was
diagnosed with chronic Kidney disease and dialysis was the only option for her. Doctors of PGIMER put
her on Peritoneal Dialysis which is an advanced form of Dialysis for the kidney patients. They
approached the insurer for the reimbursement of the claim, and after lot of persuasion, they accepted
their claims in 2018 but their TPA Vipul Medicorp kept on delaying the claims on one pretext or the
other. Further as per report of IRDA working group committee, insurers should not deny coverage for
claims of peritoneal dialysis, where dialysis is allowed. As in this case, dialysis is allowed by the insurer,
claim of peritoneal dialysis should be paid by the insurer.
SCN not received till 05.11.19. As per repudiation letter dt. 13.02.19, claim for peritoneal dialysis as per
NIC circular, is not payable and as per clause 4.24 claims for equipments external/durable medical/non
medical equipments/ instruments of any kind used for diagnosis / treatment including CPAP,CAPD,
Infusion Pump, Ambulatory device like Walker, Crutches, belts, collars, caps, splints, slings, braces,
stockings, diabetic foot wear, glucometer, thermometer, similar related items and any medical
equipment which could be used at home subsequently are not payable. Hence this claim is not payable.
The complainant was sent Annexure VI-A for compliance, which reached this office on 04-06-2019.
18) Cause of Complaint:
a) Complainant’s argument: Complainant stated that the claim has been repudiated by insurance
company and he requested for settlement of his wife’s claim.
b) Insurers’ argument: Insurance Company stated that the claim has been repudiated as per terms
and conditions of policy.
19) Reason for Registration of Complaint: - within the scope of the Insurance Ombudsman Rules,
2017.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21) Result of Personal hearing with both parties (Observations & Conclusion):
I have gone through the various documents available in file including the copy of complaint, copy of
relevant policy, repudiation letter, discharge summary of PGI, Chandigarh and also considered the
submissions made by both complainant and insurance company during the personal hearing. It is seen
from documents that the complainant filed a complaint for denial of claim for treatment taken by his
wife for chronic kidney disease at PGI by way of peritoneal dialysis. The claim has been repudiated by
insurance company vide repudiation letter dated 13.02.2019 on ground that the ambulatory peritoneal
device is not payable as per (serial no. 30) clause 4.24 of policy terms and conditions which stated as
under. On perusal of treatment chart of patient for treatment taken at PGI, Chandigarh it is observed
that she was treated by peritoneal dialysis for her chronic kidney disease during January to March, 2017.
The complainant on another hand referred to working group for standardization of exclusions in health
insurance contracts of October, 2018 wherein certain recommendations have been made for
standardization of exclusion in health insurance policy. It does make a reference to the inclusion of
peritoneal dialysis and these recommendations based on current health scenario and technology
advancement in health sector are at initial stage and have to be finally accepted/ approved by IRDAI and
Insurance Company. As such these cannot be basis for approval/ denial of the claim. Moreover, the
recommendations for inclusion of peritoneal dialysis clearly suggest that same was excluded in existing
policies. As such the repudiation of claim as per clause 4.24 of terms and conditions of policy is in order
and the same doesn’t call for any interference. In view of above the complaint is dismissed.

AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of personal hearing, the case is dismissed.
Hence, the complaint is treated as closed.
Dated at Chandigarh on 24
th
day of December, 2019.
D.K. VERMA
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Satish Kumar Saluja V/S Max Bupa Health Insurance Co. Ltd.
COMPLAINT REF. NO: CHD-H-031-1920-0089
1. On 10.05.2019, Mr. Satish Kumar Saluja had filed a complaint in this office against
Max Bupa Health Insurance Co. Ltd. for not settling the health claim. The required
documents were submitted to the insurance company but the insurance
company did not settle the health claim under policy no. 30679638201801.
2. This office pursued the case with the insurance company to re-examine the complaint and
they agreed to reconsider the claim.
3. Mr. Satish Kumar Saluja confirmed vide letter dated 06-12-2019 that his complaint has been
resolved by insurance company and he has received payment of his claim and wants to
withdraw his complaint from this forum.
4. In view of the above, no further action is required to be taken by this office and the complaint
is disposed off accordingly.
Dated : 06.12.2019 (Dr. D.K. VERMA)
PLACE: CHANDIGARH INSURANCE OMBUDSMAN
PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Suresh Mehta V/S The United India Insurance Co. Ltd.
COMPLAINT REF. NO: CHD-H-051-1920-0070
1.
Name & Address of the Complainant
Mr. Suresh Mehta
578, Sector- 21- B, Faridabad,
Haryana- 121001
Mobile No.- 9810672415
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2210002818P103230645
Individual Health Policy
28-06-2018 to 27-06-2019
3.
Name of the insured
Name of the policyholder
Mr. Suresh Mehta
Mr. Suresh Mehta
4.
Name of the insurer
The United India Insurance Co. Ltd.
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the Complaint
03-05-2019
8.
Nature of complaint
Deductions in claim.
9.
Amount of Claim
Approx. Rs. 50,000/-

10.
Date of Partial Settlement
Not provided
11.
Amount of relief sought
Rs. 50,000/-
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claim by an insurer
13.
Date of hearing/place
26-11-2019 / Chandigarh
14.
Representation at the hearing
For the Complainant
Requested for Decision on Merits.
For the insurer
Ms. Shweta Dhiman, Administrative Officer
Dr. Pearly Sharma , TPA
15
Complaint how disposed
Dismissed
16
Date of Award/Order
18-12-2019
17) Brief Facts of the Case:
On 03-05-2019, Mr. Suresh Mehta had filed a complaint that insurance company has refused to pay the
total amount of claim taking refuge of totally unjustified 10/20 % co payment clause. According to
complainant when his wife was advised a knee replacement surgery for one of her knees, they
approached HITPA for a cashless facility but they sanctioned the same with a rider to deduct 10% as co
payment in the initial approval which strangely got enhanced to 20% co-payment when the final
approval was sent. Thus against the total bill of the hospital of Rs. 2,01,000/- the insurance company
paid only Rs. 1,51,000/- . On the one hand insurance company increase premiums every 5 years for
persons over 60 years of age and on the other hand they deduct from the pay outs exactly for the same
reason i.e. you are over 60 years of age. Initially letter from the TPA said for co-payment of 10%, but in
final approval asked for 20% without giving any reason or justification for the same. Further his daughter
Archana Dutta is employed with Hyatt consultancy Pvt. Ltd. After the refusal by UIIC to pay the full
amount of hospitalization, he had submitted the bills for balance payment to this insurer, who refused it
on the grounds that since full amount of UIIC insurance has not been used, their liability does not start
till the same gets exhausted. If he might have submitted his claim to them, they would have paid the full
amount of Rs.2 lakhs (without any co payment, as it is a corporate policy) but would not pay Rs. 50,000/-
. Thus, having a total insurance cover of Rs. 8 lakhs from the two companies, he still ends up paying a
substantial sum from his savings.
On 16-05-2019, the complaint was forwarded to The United India Insurance Co. Ltd. Regional Office,
New Delhi, for Para-wise comments and submission of a self-contained note about facts of the case,
which was made available to this office on 05-07-2019.
As per SCN submitted by insurance company, the claim is for replacement of right knee of Mrs. Pramila
Mehta, who claim Rs. 2,00,017/-, out of which after 20% co-payment balance Rs. 158017/- paid to
insured. In policy clause 1.3, mainly two conditions are there. First is, pre and post hospitalization
expenses payable in respect of each hospitalization shall be the actual expenses incurred subject to a
maximum of 10% of the sum insured, whichever is less. Second is, expenses on major illnesses charged
as a total to be settled with co-pay on 80:20 basis. The co-pay of package 20% will be applicable on the
admissible claim amount. Under policy exclusion clause 4.4 for any joint replacement last four years
continuous coverage is required. Considering this clause, HITPA has taken sum insured Rs. 3,00,000/- i.e.
of 2014-15 policy. Insured has claimed Rs 2,00,017/- and after deducting 20% co-pay insurance company
has paid Rs. 158017/- to insured. Further, HITPA has deducted Rs. 2439/- for walker and Rs. 525/- for
hand rub plus Rs. 26273/- deducted against consumables which are not payable at the time of cashless.
Insured has claimed this deducted amount for Rs. 29,237/-+Rs. 22,103/- under the head of pre-post
reimbursement claim. HITPA has paid Rs. 22103/- against this claim. Hence, HITPA has paid total Rs.
1,58017/- +22103/- = Rs. 180120/- against Rs. 222103/-, after deducting 20% co-payment.
The complainant was sent Annexure VI-A for compliance, which reached this office on 03-06-2019.
18) Cause of Complaint:
a) Complainant’s argument: Complainant submitted his undated written reply received in this
office on 21st November 2019 and requested for decision on the basis of documents submitted
by him. He stated that the crux of his argument is a deduction of 20% payment on account of co-
payment. He has taken this policy at the age of nearly 30 years thus more than 37 years ago.
Insurance Company on one hand says that not more than 70% of policy amount can be paid
towards the knee replacement surgery and on another hand they are adding another rider of
co-payment of 20% this according to him is a double whammy. He says that it when the
insurance company had approved the final payment of Rs 168000/- then why I was made to pay
a sum of Rs 46273/- out of a bill of Rs 1,99,273/- and not Rs 31273/-. He requested that amount
spent by him on the surgery may be reimbursed to him in full and the clause of copayment

should be deleted in all insurance policies forthwith. Complainant requested for balance
payment of deduction from his claim.
b) Insurers’ argument: Insurance Company stated that all the deductions are made as per policy
terms and condition and nothing is due to payment.
19) Reason for Registration of Complaint:- within the scope of the Insurance Ombudsman Rules, 2017.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21) Result of Personal hearing with both parties(Observations & Conclusion)
On perusal of complaint, SCN, written brief of complainant and submission made by insurance company
during personal hearing it is observed that complainant has given complaint for deduction of amount
and urged for payment of balance payment. Out of claim amount of Rs. 222103/- as per policy terms
and condition Rs. 180120/- have been paid. As per IRDAI regulation certain deduction were made in
pharmacy which are not payable in standard health policy. In the present case, Rs. 2439/- for walker and
Rs. 525/- for hand rub plus Rs. 26273/- deducted against consumables were deducted from claim
amount. Further, complainant plea for changing policy terms and condition of co-payment clause as well
as inbuilt capping on surgery cannot be entertained since same are being approved by Insurance
regulatory and Development authority of India (IRDAI) after due consideration. Hence, the decision of
the insurance company is in order. Keeping in view of the above facts, the said complaint is hereby
dismissed and no relief is granted.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of personal hearing, the said complaint is hereby dismissed on merits.
Hence, the complaint is treated as closed.
Dated at Chandigarh on 18
th
day of December 2019.
D.K. VERMA
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Manjit Singh Tuli V/S The Oriental Insurance Co. Ltd.
COMPLAINT REF. NO: CHD-H-050-1920-0177
1.
Name & Address of the Complainant
Mr. Manjit Singh Tuli
High Flat No.- 1426, Phase- 9,
S.A.S. Nagar(Mohali), Punjab- 160062
Mobile No.- 8437016503
2.
Policy No:
Type of Policy
Duration of policy/Policy period
233500/48/2018/1778, 233500/48/2018/831
PNB ORIENTAL Mediclaim Policy
06-08-2017 To 05-08-2018, 22-05-2017 To 21-
05-2018
3.
Name of the insured
Name of the policyholder
Mr. Manjit Singh Tuli, Mr. Anoop Siddak Singh
Tuli
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
26/07/2018
6.
Reason for repudiation
Pre existing disease
7.
Date of receipt of the Complaint
19-06-2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 5,00,000/-
10.
Date of Partial Settlement
N.A
11.
Amount of relief sought
Rs.5 ,00,000/-
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claim by an insurer
13.
Date of hearing/place
03-12-2019 / Chandigarh

14.
Representation at the hearing
For the Complainant
Sh. Manjit Singh Tuli
For the insurer
Ms. Maninder Kaur A.M
15
Complaint how disposed
Award
16
Date of Award/Order
16.12.2019
17) Brief Facts of the Case:
On 19-06-2019, Mr. Manjit Singh Tuli had filed a complaint about the rejection of claim vide
letter dt. 26/07/2018 by the oriental insurance Co. Ltd. under mediclaim policy No
233500/48/2018/000831 & 233500/48/2016/1464 for the kidney transplant of his son Sh.
Annop Sidak Singh Tuli (Recipient) and wife Mrs Maninderjit Kaur (Donor) . He informed that
they are having PNB-ORIENTAL ROYAL MEDICLAIM POLICY No 233500/48/2018/1778 effective
from 06/08/2017 to 05/08/2018 for sum insured of Rs. 5,00,000/- covering Sh. Manjit Singh Tuli
, Maninderjit Kaur and Annop Siddak Singh Tuli which is a continuous renewal of policy No
233500/48/2016/1464 since 06/08/2015.On getting employment by his son Sh. Anoop Siddak
Singh Tuli ,separate insurance policy bearing No 233500/48/2018/831 effective from
22/05/2017 to 21/05/2018 was taken in his name which renewed under policy No
233500/48/2019/412 from 22/05/2018 to 21/05/2019.In the month of April2018, Anoop siddak
Singh Tuli ‘s creatinine went above normal limit and was advised for kidney transplant which
was done on 25/05/2018.Claim for Rs. 605294/- for recipient and Rs. 21850/- for the donor
was submitted . The oriental insurance company vide letter dt. 26/07/2018 rejected the claim
with the reason that this is a case of CKD & HTN. Renal Transplant done. As patient is a K/C/O
HTN since 2014. HTN is a pre disporting factor in CKD and HTN diagnosed before policy in
caption is pre- existing. Pre existing disease are payable after 3 years. Policy is in 3
rd
year. So the
claim is not payable as per clause 4.1. It is submitted that he has never availed medical leave/
hospitalized and cause of HTN& CKD was known only after Renal Biopsy in April 2017. Case was
resubmitted to the insurance company on 28/09/2018 for review & it was repudiated by TPA on
17/1/2018.It was informed by the dealing officer/ In charge at OIC, that they have sought expert
opinion of Specialist Doctor, but returned papers without opinion of specialist doctor. Insurance
Company be directed to pay the claim as the request is genuine.Further complainant vide his
letter dt. 27/07/2019 has further submitted that claim has been wrongly repudiated on the plea
of Pre Existing disease. According to complainant his son had never taken leave during his study
at school/ Engineering Colledge – PEC Chandigarh & /IIM – Ahmadabad. The cause of
Hypertension and need for renal transplant was confirmed only after BIOPSY in April 2017.
Kidney was donated by his wife / Mother of recipient who was also covered under the policies.
He further requested that it is a case of giving life to a person, who has no remedy except
transplant & technical issues may please be ignored. He also mentioned that the condition of 3
years in case of pre existing disease, the applicant to wait of 3-4 months and to be on dialysis for
becoming eligible and his condition might deteriorate further.
On 12-07-2019, the complaint was forwarded to The Oriental Insurance Co. Ltd. Regional Office,
Chandigarh, for Para-wise comments and submission of a self-contained note about facts of the
case, which was made available to this office on 29-11-2019…
As per SCN received, the insured Mr. Manjit Singh Tuli Purchased PNB Purchased PNB-Oriental
mediclaim policy on 06/05/2015 covering himself, spouse Maninderjit Kaur and Son Anoop
Siddak Singh Tuli with policy No 233500/48/2016/1464. The policy was renewed for the period
from 06/08/2016 to 05/08/2017 with policy no 233500/48/2017/1641 and from 06/08/2017 to
05/08/2018 with policy no 233500/48/2018/1778. Mr. Anoop Siddak Singh Singh Tuli bought a
separate policy thereafter vide policy no 233500/48/2018/831 ( from 22/05/2017 to
21/05/2018 ) and policy no 233500/48/2019/412 ( from 22/05/2018 to 21/05/2019. The
complaint has been filed by Mr. M.S. Tuli under two different policies covering the different
Principal Insureds. On receipt of the complaint from office of the Insurance Ombudsman, the
claim file was reviewed and it was observed that due to an oversight and some
miscommunication with TPA ,The claim was repudiated earlier as the policy in the name of Mr.
Anoop Tuli was in second year of inception at the time of claim. After observing the above, the
claim was referred to TPA again for reconsideration on the basis of insurance coverage.. After
reconsideration of the claim, vide their mail dated 26/11/2019 and 27/11/2019 has submitted
that Rs. 5,00,000/-is payable as claim mount under
The policy 233500/48/2019/412 A/c Anoop Siddak Singh Tuli . The competent authority of the
oriental insurance company has agreed and approved to pay Rs. 5,00,000/-as claim amount to
the insured.
The complainant was sent Annexure VI-A for compliance, which reached this office on 30-07-
2019.

18) Cause of Complaint:
a) Complainant’s argument: Claim of kidney transplant of his son has been wrongly repudiated
on the plea of Pre Existing disease. The cause of Hypertension and need for renal transplant was
confirmed only after BIOPSY in April 2017.The insured person is covered under med claim
policy taken by complainant since 06/08/2015. And also under separate individual policy
233500/48/2019/0412 effective from 22/05/2018 to 21/05/2019 which is continuous renewal
since 22/05/2017.
b) Insurers’ argument: The insurer rejected the claim with the reason that this is a case of CKD &
HTN. As patient is a K/C/O HTN since 2014. HTN is a pre disposing factor in CKD and HTN
diagnosed before policy in inception is pre-existing. Pre existing disease are payable after 3
years. Policy is in 3
rd
year. So the claim is not payable as per clause 4.1.
19) Reason for Registration of Complaint:- within the scope of the Insurance Ombudsman Rules,
2017.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21) Result of Personal hearing with both parties(Observations & Conclusion) :
After hearing both the parties and examining the documents placed on record, it has been
observed that complainant reiterated that the claim has been wrongly repudiated on the
ground of pre existing disease. On the other hand, the insurance company in their SCN has
stated that after receipt of the complaint from the office of the insurance Ombudsman, the
claim file was reviewed and it is observed that due to oversight and some miscommunication
with the TPA ,the claim was repudiated and now after reconsideration Rs. 5,00,000/- is payable
as claim amount under policy no 233500/48/2019/412. The complainant during the personal
hearing also agreed to accept Rs. 5,00,000/- subject to terms and conditions of policy as final
amount. .Since the insurance company is ready to pay the admissible amount of Rs. 5,00,000/-
as per terms and conditions of the policy, the insurance company is directed to settle the claim
within 30 days from the receipt of copy of award.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of personal hearing, Rs.5,00,000/- is hereby awarded to be paid by the
Insurer to the Insured, towards full and final settlement of the claim. Hence, the complaint is
treated as closed.
Dated at Chandigarh on 16
th
day of December, 2019
D.K. VERMA
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Ashish Gupta V/S The Oriental Insurance Co. Ltd.
COMPLAINT REF. NO: CHD-H-050-1920-0197
1.
Name & Address of the Complainant
Mr. Ashish Gupta
S/o Sh. Vinod Bala Gupta, House No.- 3, Sector-
14, Faridabad, Haryana- 121007
Mobile No.- 9311114800
2.
Policy No:
Type of Policy
Duration of policy/Policy period
272401/48/2019/730
Mediclaim Individual Policy
02-12-2018 To 01-12-2019
3.
Name of the insured
Name of the policyholder
Smt. Vinod Bala Gupta
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
28/03/2019
6.
Reason for repudiation
Repudiation under clause 4.23 (OPD)
7.
Date of receipt of the Complaint
24-06-2019
8.
Nature of complaint
Claim Denied ( Two Claims )

9.
Amount of Claim
Rs. 54000/-
10.
Date of Partial Settlement
N.A
11.
Amount of relief sought
Rs. 54000/-
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claim by an insurer
13.
Date of hearing/place
03-12-2019 / Chandigarh
14.
Representation at the hearing
For the Complainant
Sh. Ashish Gupta
For the insurer
Ms. Indu Khurana
15
Complaint how disposed
Award
16
Date of Award/Order
17.12.2019
17) Brief Facts of the Case:
On 24-06-2019, Mr. Ashish Gupta had filed a complaint that the insurer have denied eye surgery
treatment claim of his mother Smt. Vinod Bala Gupta .She is insured with the oriental insurance
company for almost 20 years. She suffered sudden loss of vision of one eye almost 2-1/2 Years
back for which she was treated at Nayanjyoti Eye & Laser Centre ,by Dr. Avnendra Gupta, Her
Diagnosis was Right Eye occult CNVM. My Mother is a diabetic & hypertensive for several years.
She was kept under hospitalization for 24 hours under advice of treating doctor. Though the
insurance company denied the reimbursement but the claim was finally settled in her favour by
the consumer court & payment was made to the insured by the oriental insurance company Ltd.
She suffered from the same problem again for the same eye & was treated by same doctor at
same hospital for the same illness & same treatment was given. But insurance company has
again declined the Reimbursement for claim no 181400206984 & 191400034582.The mother of
complainant is a senior citizen, continuously insured for 20 Years. She is suffering from partial
loss vision in her very precious Right Eye(Left eye total loss of vision) and sincerely takes the
advice of their Ophthalmologist, who advises a stay of at least 24 hours due to her medical
condition of being Diabetic and hypertensive.
On 18-07-2019, the complaint was forwarded to The Oriental Insurance Co. Ltd. Regional Office,
New Delhi, for Para-wise comments and submission of a self-contained note about facts of the
case, which was made available to this office on 27/11/2019
As per the SCN, The insured Smt. Vinod Bala Gupta 71 Years old female covered under
mediclaim policy diagnosed case of OCCULT. ANVM(Choroidal Neovascular Membrance ) and
administered with inj. Accentrix on 22/12/2018.Patient Got admitted on 22/12/2018 and
discharged on 23/12/2018 . As the procedure underwent is out patient procedure, one day
admission not justified and as per policy terms and conditions out patient procedure are not
covered. Hence the claim is not admissible and the claim falls under exclusion no 4.23 (Out
patient diagonistic,Medical or surgical procedures or treatments, No prescribed drugs and
medical supplies, hormone replacement therapy, sex change or treatment which results from or
is in any way related to sex change )The hospitalization is for more than 24 hours but in the bill,
“Day care charges mentioned for room rent. Further administration of intravitreal injection is
not listed in Appendix 1- List of day care procedures/surgeries .As per policy also 24 hours
hospitalization is not required in the procedure. For the day care procedures/treatment, ENT
coverage under policy both the conditions are taken into account as stated below in the
definition clause 2.11 day care treatment : Refers to medical treatment, and / or surgical
procedure which is :
i) Undertaken under the general or local anesthesia in Hospital/day care centre in less than 24
hours because of the technological advancement and
ii) Which would have otherwise required a hospitalization of more than 24 hours. Intra Vitreal
injection is itself and advanced treatment, which does not require 24 hours hospitalization.
The claim has been repudiated by Bo Palwal vide their letter dated 28/05/2019
18) Cause of Complaint:
a) Complainants argument: The complainant submitted that insurer denied the eye surgery claim
of his mother for the diagnosed case of Occult CNVM. She was kept under hospitalization for 24
hours under the advice of treating doctor being diabetic and hypertensive for several years.
b) Insurers’ argument: Insurance Company stated that patient got admitted and administered
with Inj. Accentrix .The procedure underwent is outpatient procedure one day admission is not
justified and such procedures are not covered as per policy terms and conditions of the policy.

21) Reason for Registration of Complaint:- within the scope of the Insurance Ombudsman Rules,
2017.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21) Result of Personal hearing with both parties(Observations & Conclusion)
On going through the complaint document in the file and submission made by both the parties
during personal hearing, it is observed that the claim is on account of admission to hospital for
more than 24 hours. The insured Smt. Vinod Bala Gupta 71 years is covered under mediclaim
insurance, diagnosed case of Occult CNVM and administered with Inj. Accentrix. As per
complainant, the insurance company has denied two claims bearing claim No’s 181400206984 &
191400034582 of his mother for the eye treatment for which she was admitted for more than
24 hours under the advice of treating doctor being diabetic and hypertensive for several years.
The insurance company rejected the claims on the ground that the procedure underwent is
outpatient procedure, one day admission is not justified and such procedures are not covered
under clause: 4.23 of policy terms and conditions. In the instant case the patient is a diagnosed
case of Occult CNVM and is administered with injection Accentrix . The said injection is
administered in an operation theatre under strict sterile conditions and requires post procedure
observations of the patient since the same is not free from complications. On going through the
various day care procedures in relation to eye surgery it is observed that due to rapid
technological advancement in the medical field most of the surgical procedures on eye do not
require hospitalization as it used too few years back and even the smallest excision/incision on
eyes are covered under day care procedures. Since the administration of injection Accentrix
requires highly sophisticated procedures done under the supervision of a consultant eye
specialist in an operation theater, in my view the case is covered under eye surgery and hence
payable. The decision of the insurance company to reject the claim of the insured in respect of
the said treatment taken by her at Nayanjyoti Eye & Laser Centre, Faridabad is not proper and
devoid of merits. The insurance company is directed to settle the claims within 30 days after the
receipt of the copy of award.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of personal hearing, admissible claim amount as per terms and condition
of the policy is hereby awarded to be paid by the Insurer to the Insured, towards full and final
settlement of the claim.
Hence, the complaint is treated as closed.
Dated at Chandigarh on 17
th
day of December, 2019.
D.K. VERMA
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN- Dr. D.K. VERMA
Case of Mr. Rakesh Kumar V/S The New India Assurance Co. Ltd.
COMPLAINT REF. NO: CHD-H-049-1920-0115
1.
Name & Address of the Complainant
Mr. Rakesh Kumar
S/o Late Sh. Surjit Kumar,
House No.- 870 FF, Sector- 12 A, Panchkula,
Haryana- 134112
Mobile No.- 9318969000
2.
Policy No:
Type of Policy
Duration of policy/Policy period
35010134179500000063
Mediclaim Policy
29-03-2018 to 28-03-2019
3.
Name of the insured
Name of the policyholder
Mr. Rakesh Kumar
Mrs. Sangeeta Dhiman
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
Not applicable
6.
Reason for repudiation
Not applicable

7.
Date of receipt of the Complaint
24-05-2019
8.
Nature of complaint
Deduction of claim amount
9.
Amount of Claim
Rs 503300/-
10.
Date of Partial Settlement
Rs 125500/- (25% of claim amount paid)
11.
Amount of relief sought
Rs 377475 + bank interest
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation
of claim by an insurer
13.
Date of hearing/place
10-12-2019 / Chandigarh
14.
Representation at the hearing
For the Complainant
Mr. Rakesh Kumar, Complainant
For the insurer
Ms. Deep Shikha, Deputy Manager
15
Complaint how disposed
Award
16
Date of Award/Order
11-12-2019
17) Brief Facts of the Case:
On 24-05-2019, Mr. Rakesh Kumar had filed a complaint regarding partial payment of his mediclaim by
the insurance company. He stated that his wife Mrs. Sangeeta Dhiman was admitted at Kirloskar
Hospital, Hyderabad for treatment where n the surgery was carried out by the doctors for hernia and
other ailments. Accordingly he lodged hospitalization claim with Raksha TPA for reimbursement of claim
amounting to Rs 503300/-. When he checked the status of his claim from the TPA website online, it was
observed that TPA has settled the claim for Rs 125500/- arbitrarily deducting the balance amount from
the claim lodged. Complainant submitted that he is continuously renewing his policies since 2006
without any break and no claim has ever been reported till date except for the above mentioned claim.
As per TPA reply to concerned branch, the treatment relates to obesity and that is not admissible.
Complainant stated that he had already submitted all the required documents alongwith the certificate
of concerned doctor from Kirloskar Hospital, Hyderabad confirming that the treatment given to Mrs
Sangeeta dhiman doesn’t relate to obesity and the surgery is a life saving surgery, despite that, they
have deducted his rightful claim. He requested for intervention and to resolve the issue so that his
rightful claim may be settled without any further mental agony.
On 12-06-2019, the complaint was forwarded to The New India Assurance Co. Ltd. Regional Office,
Chandigarh, for Para-wise comments and submission of a self-contained note about facts of the case,
which was made available to this office on 26-06-2019.
Insurance Company submitted in the SCN, that complainant has lodged claim of his wife Mrs. Sangeeta
Dhiman for Rs 503300/- and the TPA have approved the claim for Rs 125500/- and the remaining
amount deducted. Deduction in the claim has been made due to permanent exclusion clause 4.4.6
which reads that “convalescence, general debility, rundown condition or rest cure, any treatment
related to obesity or complication of obesity, treatment relating to all psychiatric and psychosomatic
disorder, infertility, sterility, venereal disease, intentional self injury and illness or injury caused by the
use of intoxicating drug/ alcohol.” The claim was paid for treatment of hernia and the expenses related
to treatment of obesity in the form for gastric bypass surgery were deducted as per the discharge
summary. It is observed that treatment was got for bariatric surgery obesity along with umbilical hernia
surgery as such their deduction is logical since claim for treatment related to treatment of obesity which
is an exclusion under the policy.
The complainant was sent Annexure VI-A for compliance, which reached this office on 13-09-2019.
18) Cause of Complaint:
a) Complainant’s argument: Complainant stated that insurance company has arbitrarily deducted
claim amount. He requested for the payment of balance amount from the claim lodged.
Complainant also pointed that insurance company plea of cosmetic surgery is illogical as the
surgery was life saving treatment
b) Insurers’ argument: Insurance Company reiterated their stand of SCN and requested that they
have paid the 25% amount in respect of umbilical hernia surgery as such their deduction is
logical since claim for treatment related to obesity and same is exclusion as per policy terms and
conditions.
19) Reason for Registration of Complaint: - within the scope of the Insurance Ombudsman Rules,
2017.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21) Result of Personal hearing with both parties(Observations & Conclusion)
On perusal of various documents available in the file including the copy of complaint dated 24.05.2019,
company reply dated 26.06.2019 about the rejection of the health claim in respect of the treatment
taken by complainant, treatment record of Kirloskar Hospital, Hyderabad and also after consideration of

submission made by both parties during the course of personal hearing, it is seen that complainant was
diagnosed as a case of Metabolic Syndrome with systematic involvement [Hypertension, Breathlessness,
Obstructive Sleep apnoea, Morbid obesity] + umbilical hernia + Epigastric hernia. There is no dispute
with regard to admission and diagnosis of the complainant by insurance company. The issue to be
decided is whether payment of 25% of claim amount by insurance company is justified or not? It is seen
that during the course in hospital complainant’s wife was advised the laparoscopoic Metabolism surgery
of Duodeno- Ileal bypass with sleeve gastrectomy with repair of umbilical and epigastric hernias, to
control her blood pressure with urinary infection and remained hospitalized at Kirloskar Hospital,
Hyderabad from 17.02.2019 to 27.02.2019. The claim for reimbursement of the expenses incurred on
the treatment filed for Rs 503300/- under the policy no. 35010134179500000063 was paid 25% by the
insurance company for umbilical hernia surgery and rest of amount was deducted by insurance
company under exclusion 4.4.6 of policy terms and conditions which provides treatment of obesity or
condition arising there from (including morbid obesity) and any other weight control Programme and
similar services or supply. The patient in the instant case was admitted for breathlessness on walking
and any routine activity. She was treated at Kirloskar Hospital, Hyderabad during the above period for
complications of the umbilical Hernia + Epigastric hernia. On going through the various documents
available in the file, it is evident that the patient has been treated for umbilical Hernia + Epigastric
hernia. Further, doctor certificate dated 18-02-2019 also stated that this is not a cosmetic surgery for
her, but a life-saving procedure to bring her back to good health, preventing future ailments and
increased medical expenditure. The patient i.e. Sangeeta Dhiman w/o complainant was treated under
general anesthesia wherein metabolic surgery, sleeve gastrectomy and repair of umbilical and epigastric
hernias was done by surgical intervention and all the three procedures were done simultaneously during
the patient hospitalization. The repudiation of claim in the instant case is not based on reasonable
grounds and the insurance company has made an attempt to stretch the exclusion clause in respect of
obesity to the complications of the treatment taken for umbilical Hernia + Epigastric hernia. Further, the
insurance company has paid 25 % of amount claim by complainant on the proportionate basis for
treatment of umbilical & epigastric hernia. It is, however, neither clear nor evident from any of
documents or SCN as to the basis on which the insurance company has arrived at such conclusion &
such amount. Surprisingly the company has chosen to reject this claim despite the fact that the
complainant has not filed any claim for treatment taken for obesity. It is highly improper on the part of
insurance company to reject the claim on arbitrary basis by stretching the policy wordings to their
advantage. Hence the insurance company is directed to settle the claim as per terms and conditions of
the policy within 30 days after receipt of award copy.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of personal hearing, the insurance company is directed to settle the
claim as per terms and conditions of the policy within 30 days after receipt of award copy.
Hence, the complaint is treated as closed.
Dated at Chandigarh on 11
th
day of December 2019.
D.K. VERMA
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, CHANDIGARH
(UNDER INSURANCE OMBUDSMAN RULES, 2017)
INSURANCE OMBUDSMAN-Dr. D.K. VERMA
Case of Mr. Anil Gupta Vs Star Union Dai-ichi- Life Insurance Co. Ltd.
CASE NO-CHD-H-045-1920-0311
1.
Name & Address of the
Complainant
Mr. Anil Gupta
H. No.- 1735, Nirvana Society, Opp. Ryan School,
Chandigarh-0
Mobile No.- 9814915700
2.
Policy No: DOC
Type of Policy
Duration of policy/Policy period
00975387
SUD Life Aarogyam
10 Years
3.
Name of the insured
Name of the policyholder
Mr. Anil Gupta
Mr. Anil Gupta
4.
Name of the insurer
Star Union Dai-ichi- Life Insurance Co. Ltd.
5.
Date of Repudiation
05.04.2019
6.
Reason for repudiation
Concealment of material facts
7.
Date of receipt of the Complaint
01-08-2019
8.
Nature of complaint
Rejection of Health Insurance claim
9.
Amount of Claim
10.
Date of Partial Settlement
Rs. 105858/-

11.
Amount of relief sought
Payment of balance amount
12.
Complaint registered under
Rule no: Insurance Ombudsman
Rules, 2017
13 1 (b)
13.
Date of hearing/place
04-12-2019 / Chandigarh
14.
Representation at the hearing
For the Complainant
Mr. Anil Gupta
For the insurer
Ms. Priyanka Mishra Roy
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
24.12.2019
17. Brief Facts of the case:
On 01-08-2019, Mr. Anil Gupta had filed a complaint against Star Union Dai-ichi- Life Insurance Co. Ltd.
in respect of policy bearing no. 00975387. He has stated that he had taken the said policy from the
above company and when lodged the health claim to the company he was paid Rs. 105858/- only and
the company has not paid full claim, Hence, feeling aggrieved, he approached this office to seek justice.
18) Cause of Complaint:
a) Complainant’s argument: The complainant stated that the insurance company has not paid his full
claim and he requested for the payment of balance amount.
b) Insurers’ argument: The insurance company representative stated that the company vide its letter
dated 15.03.2019 called for additional documents from the complainant and during evaluation of the
claim it was found that the complainant was suffering from hypertension since 2015 and Type-II
Diabetes Mellitus since past 07 years and was taking treatment for the same. In this regard reliance
may be placed on the consultation paper dated 02.09.2015 by Dr. Gurpreet S Bhatia. Further in the
discharge summary report dated 18.02.2019 of Fortis hospital Mohali it is clearly mentioned that the
complainant was suffering from hypertension and Type-II Diabetes Mellitus. The company vide its
letter dated 05.04.2019 has rejected the claim of the complainant and further cancelled the policy in
accordance with section 45 of the Insurance Act as there was past history of hypertension since 2015
with type II diabetes since 7 years which was not disclosed in the proposal form at the time of taking
policy. They further stated that the company has refunded the premium amount of Rs. 105858/- under
the said policy.
19) The following documents were placed for perusal:-
a) Copies of the proposal forms b) Complaint to the insurer. c) Reply of the company
20) Result of personal hearing with both parties (Observations & Conclusion):
On perusal of various documents available in file including the copy of complaint, repudiation letter and
SCN submitted by insurance company and the hospital record of Fortis hospital where complainant Mr.
Anil Gupta was admitted on 16.02.2019 and discharged on 18.02.2019. The claim filed by complainant
for the treatment taken by him as per the claim form dated 28.02.2019 for critical illness has been
repudiated by insurance company vide repudiation letter dated 05.04.2019 on the basis of non-
declaration of past illness of hypertension before inception of policy and type II diabetes mellitus since 7
years. The complainant was admitted in Fortis hospital on 16.12.2019 with presenting symptoms of
recurrent syncope, bifascicular block, CAD-SVD, PTCA, diabetes mellitus type II and systemic
hypertension and left against medical advice on 18.02.2019 after under going treatment in the form of
PTCA and stent in RCA on 17.02.2019. I have also gone through the proposal form submitted by
complainant at the time of taking policy. It is evident that complainant has not declared the existing
hypertension and diabetes mellitus type II in his personal details. Moreover the fact that he was
suffering from hypertension and diabetes mellitus before inception of policy in supported by the report
card of Dr. Gurpreet Singh Bhatia dated 09.05.2015 which clearly mentions that the patient is a case of

diabetes mellitus for last 7 years and he was on regular medication both for hypertension and diabetes
mellitus. The concealment of material facts relating to above in proposal form dated 02.09.2015 is
evident on perusal of proposal form. In view of what has been stated and discussed above the
repudiation of claim by insurance company being in order doesn’t call for any interference. As such the
complaint is dismissed.
ORDER
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of hearing, there is no need to interfere with the decision of the insurer
and the complaint is dismissed.
Hence, the complaint is treated as closed
Dated at Chandigarh on 24
th
day of December, 2019.
D.K.VERMA
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Pradip Mohanty Vrs. M/S The New India Assurance Co Ltd
COMPLAINT REF: NO: BHU-G-049-1920-0025
AWARD NO: IO/BHU/A/GI/ /2019-20
1.
Name & Address of the
Complainant
Mr. Pradip Mohanty
Patrapada, Sundergarh, Odisha. 770001
9437083310, 7008400466
2.
Policy No:
Type of Policy
Duration of policy/Policy
period
55050234172800000010
Floater Mediclaim Policy- SIV Rs.8,00,000/-
(Self+spouse+Child)
02.03.2018 to 01.03.2019 (DoA-05.12.2018)
Wife’s treatment period: 05.12.2018 to 08.01.2019
3.
Name of the insured
Name of the policyholder
Mrs Pratiti Mohanty
Mr. Pradip Mohanty
4.
Name of the insurer
M/S The New India Assurance Co Ltd (Sundergarh Branch)
5.
Date of Repudiation
Claim is settled for Rs.3,00,000/- against Rs.6,26,857/-
The complainant wants settlement balance amount of the
claim
6.
Reason for repudiation
7.
Date of receipt of the
Complaint
24.06.2019
8.
Nature of complaint
Partial settlement
9.
Amount of Claim
Rs.6,26,857/-
10.
Date of Partial Settlement
11.
Amount of relief sought
Rs.3,26,857/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
06.12.2019, Balangir
14.
Representation at the
hearing
cccc) For the
Complainant
Self
dddd) For the
insurer
Shri Pitamber Marandi, Sr. BM, Sundergarh
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017

16
Date of Award/Order
06.12.2019
17. a. Brief Facts of the Case/ Cause of Complaint: - The Complainant had covered himself,
his spouse and daughter under New India Floater Mediclaim Policy for the floating sum insured
of Rs.8,00,000/- for the period from 02.03.2018 to 01.03.2019. Unfortunately, the
complainant’s wife Mrs. Pratiti Mohanty was admitted in NISC on 05.12.2018 for treatment of
Atrial Septal Defect Closure and underwent Open Heart Surgery. She was discharged on
08.01.2019. She was denied cash-less facility by the TPA, therefore, the complainant submitted
the hospitalization bills amounting to Rs.6,26,857/- towards the settlement of the medi-claim
under the policy. But the insurer settled the claim at Rs.3,00,000/- against the bill of Rs.
Rs.6,26,857/-. Being aggrieved on partial settlement of the claim, the complainant preferred an
appeal before this forum for redressal.
b. The insurer states that the policy has been renewed with them since 29.12.2012. The
policy sum insured was Rs. 3 lac for 2012-13, 2013-14, 2014-15, 2015-16 and 2016-17. The
policy was renewed with enhanced SIV of Rs. 8 lac on time without any delay in 2017-18. But in
2018-19 policy was renewed after 59 days of gap with SI of Rs. 8 lac. The previous policy (2017-
18) has expired on 02.01.2018 but the present policy (2018-19) was renewed only on
02.03.2018. The insurer states during claim process, it has come to the knowledge of their TPA
that the acquired Atrial Septal Defect not specified as current complication following
Myocardial infraction which is internal congenital disease, which has two years waiting period
of policy, where enhancement of sum insured is Rs.3 lac to 7 lac. Hence the claim amount is
restricted to sum insured of Rs.3,00,000/- and the said claim is settled by the TPA on the basis
of policy for 2015-16.
18. a) Complainant’s Argument: - The complainant states that he has lodged the claim for
Rs.6,26,857/-, but surprised to receive Rs.3,00,000/- and therefore made this appeal for
payment of balance amount.
b) Insurer’s Argument: - The Insurer has given a statement showing the renewal of the policies
over the years and has mentioned that the policy of 2018-19 under which the claim has arisen,
is not insured within 30 days of expiry of the previous policy. The insurer further states that
during claim process, it has come to the knowledge of their TPA that the acquired Atrial Septal
Defect not specified as current complication following Myocardial infraction which is internal
congenital disease, which has two years waiting period of policy, where enhancement of sum
insured is Rs.3 lac to 7 lac. Hence the claim amount is restricted to sum insured of Rs.3,00,000/-
and the said claim is settled by the TPA on the basis of policy for 2015-16.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Photocopies of Policy,
b. Photocopies of Medical documents
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents submitted relating the complaint and heard both the
parties. The conditions of the policy were examined, which states that Congenital Internal
Disease or Defects or anomalies shall be covered after twenty-four months of Continuous
Coverage, if it was unknown to the policyholder or the Insured Person at the commencement of
such Continuous Coverage. The insured was treated for Atrial Septal Defect, which is congenital
in nature. It is found that the insured has enhanced the sum insured from Rs.3.00 lac to Rs.7.00
lac (enhanced by Rs.4.00 lac) from 03.01.2017 to 02.01.2018 and then continued from
02.03.2018 to 01.03.2019. The treatment was taken on 05.12.2018, which was before
completion of 24 months of the enhanced sum insured of Rs.4.00 lac.

Dated at Balangir on 06
th
day of December, 2019
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Kirty Bikram Das Vrs. M/S Star Health and Allied Insurance Co Ltd
COMPLAINT REF: NO: BHU-H-044-1920-0009
AWARD NO: IO/BHU/A/GI/ /2019-20
1.
Name & Address of the
Complainant
Mr. Kirty Bikram Das
Suniti Niwas, Plot No 353/21, Jayadev Vihar. BHUBANESWAR
751013 (Contact No- 94371 77888)
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/191212/01/2018/007191 (Family Health Optima Policy)
Covering Self+spouse + 2 dependent Children for SIV Rs. 505000/-
28.03.2018-27.03.2019 (Hospitalizatiom 21.09.2018- 27.09.2018)
Policy inception date28.03.2016
3.
Name of the insured
Name of the policyholder
Mr. Kirty Bikram Das
Mr. Kirty Bikram Das
4.
Name of the insurer
Star Health and Allied Insurance Co Ltd
5.
Date of Repudiation
Claim is settled at Rs.75906/- as aginst Rs.95551/-
Non-consideration of balance amount of Rs.19645/-
6.
Reason for repudiation
7.
Date of receipt of the Complaint
21.02.2019
8.
Nature of complaint
Partial settlement
9.
Amount of Claim
Rs.95551/-
10.
Date of Partial Settlement
11.10.2018
11.
Amount of relief sought
19645/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
11.12.2019, Bhubaneswar
14.
Representation at the hearing
eeee) For the
Complainant
Self
ffff) For the insurer
Shri Amarendra Nanda, Executive (Claims)
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
11.12.2019
17. a. Brief Facts of the Case/ Cause of Complaint: - The Complainant had taken a family floater
(Family Health Optima Policy) health insurance policy covering self, spouse and dependent children for
SIV of Rs.505000/- (Basic SIV Rs.4,00,000/- plus bonus Rs.1,05,000/-). The complainant was admitted in
Apollo Hospital on 21.09.2018 for treatment of Dengue fever with Thrombocytopenia, AKI and got
discharged on 27.09.2018. The insurer allowed cash-less settlement and paid Rs.75906/- against the
hospital bills of Rs. 95551/-. The complainant paid the balance amount of Rs.19645/- to the hospital and
requested the insurer for reimbursement of Rs.19645/-. The insurer informed the complainant that they
have settled the claim to the maximum after deduction of non-payable/non-medical items as final
AWARD
Taking into account the facts and circumstances of the case and the submissions made
by both the parties during the course of hearing, it is found that the treatment in
question is internal congenital in nature, which is covered after 24 months of continuous
coverage. The Policy has the sum insured of Rs.7.00 lac as on the date of hospitalization,
which was enhanced from Rs.3.00 lac to Rs.7.00 lac from 03.01.2017 that means as on
date of hospitalization, SI of Rs.3.00 lac has completed 24 months whereas increased SI
of Rs.4.00 lac has not completed 24 months of continuous coverage. Therefore, the
complainant is not entitled for more than Rs.3.00 lac. It is found that the insurer has
already settled the claim at Rs.300 lac.
The insured has pointed out that the complainant did not renew the policy within the
grace period of 30 days, to which the complainant informed that the insurer did not
send the renewal notice, which caused the break in insurance. Though the insurer is not
obliged, they are advised to send renewal notice for mutual benefits of both the parties.
Considering the above, the complaint stands dismissed.

settlement. The complainant, on not getting the full amount as claimed, has got aggrieved and preferred
an appeal before this forum for redressal.
b. The insurer in the Self-Contained Note (SCN) states that the difference between the amount
paid by them to the hospital and the hospital bill is due to non-payable/non-medical items under the
policy terms and conditions.
18. a) Complainant’s Argument: - The complainant states that the insurer did not settle the full
claim amount though the policy promises for the same and hence he requested for payment of balance
amount of Rs. 19645/-.
b) Insurer’s Argument: - The insurer in the Self-Contained Note (SCN) states that the difference
between the amount paid by them to the hospital and the hospital bill is due to non-payable/non-
medical items under the policy terms and conditions. The insurer also states that the amount already
paid is the maximum under the policy.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Photocopies of Policy,
b. Photocopies of Bills
c. Photocopy of Insurer’s claim calculation sheet
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has carefully gone
through all the documents submitted relating the complaint and heard both the parties. During hearing,
the insurer informed their decision to pay the balance amount of the claim.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall comply with
the award within 30 days of the receipt of the award and shall intimate the compliance of
the same to the Ombudsman.
As per the Rule 17(7) the complainant shall be entitled to such interest at a rate per annum
as specified in the regulations framed under the Insurance Regulatory and Development
Authority of India Act 1999, from the date of the claim ought to have been settled under
the regulations, till the date of payment of amount awarded by the Ombudsman.
As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be binding
on the Insurers.
Dated at Bhubaneswar on the 11
th
day of December, 2019 INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Tushar Kanta Muduli Vrs. M/S The New India Assurance Co Ltd
COMPLAINT REF: NO: BHU-H-049-1920-0034
AWARD NO: IO/BHU/A/GI/ /2019-20
1.
Name & Address of the
Complainant
Mr. Tushar Kanta Muduli
Plot No- 183/561, Gajapati Nagar, PO- Sainik School,
Bhubaneswar, Odisha.
2.
Policy No:
Type of Policy
Duration of policy/Policy
period
55030134179500000003
New India Mediclaim Policy with SIV Rs.5,00,000/-
05.09.2017 to 04.09.2018 (DoL: 10.05.2018)
Inception of policy date: 05.09.2017
AWARD
The Forum has gone though the documents submitted and heard both the parties. During
the course of hearing, the insurer informed that they have decided to pay the balance
amount of the claim. Therefore, the insurer is directed to pay the balance amount of
Rs.19645/- (Rupees Nineteen thousand six hundred forty-five only) to the complainant
towards full and final settlement of the claim.
Hence, the complaint is admitted accordingly.

3.
Name of the insured
Name of the policyholder
Mr. Akash Muduli
Mr. Akash Muduli
4.
Name of the insurer
M/S The New India Assurance Co Ltd
5.
Date of Repudiation
06.07.2018
Claim is not admissible under the policy
6.
Reason for repudiation
7.
Date of receipt of the
Complaint
23.08.2019
8.
Nature of complaint
Repudiation of Reimbursement of Health Insurance Claim
9.
Amount of Claim
Rs.62,979/-
10.
Date of Partial Settlement
Not applicable as the claim is repudiated
11.
Amount of relief sought
Rs.62,979/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
11.12.2019, Bhubaneswar
14.
Representation at the hearing
gggg) For the
Complainant
Self
hhhh) For the insurer
Shri Braja Kishore Sahoo, Dy. Manager
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
11.12.2019
17. a. Brief Facts of the Case/ Cause of Complaint: - The Complainant is the father of the insured
Mr. Akash Muduli (hereinafter is called as Insured). The Insured had taken a Mediclaim policy from M/S
the New India Assurance Co Ltd for the period from 05.09.2017 to 04.09.2018 with a sum insured of
Rs.5,00, 000/-. Unfortunately, the insured was admitted in AMRI Hospital on 10.05.2018 for treatment
of Right maxillary sinusitis with DNS and got discharged on 11.05.2018. The Hospital intimated the TPA
on 09.05.2018 and the TPA of the insurer, on 10.05.2018, denied the cashless facility to the hospital
stating the treatment is not covered under the policy during the first 24 months from inception of the
policy date. The insured, after treatment, submitted concerned medical documents and the bills for
reimbursement of the claim. But as advised by the insurer, the TPA has denied the claim stating there is
no scope under the policy for consideration as the treatment of maxillary sinusitis within 24 months of
inception of the first policy is not payable. Being aggrieved on closure of the claim case, the complainant
preferred an appeal before this forum for redressal.
b. The insurer states that the patient intimated the TPA on 09.05.2018 and the TPA informed the
hospital about denial of cash-less authorization on 10.05. 2018 as any decision regarding admissibility,
depends on examination report of the hospital, which was known to TPA only on 10.05.2018.The claim
was submitted on 24.05.2018 and the TPA informed the claimant on 06.07.2018 about non-admissibility
of the claim as the disease Maxilary Sinusitis with DNS is not payable for the first 24 months from the
inception of the policy i.e. 05.09.2017. Therefore, repudiation of the claim is in order and there is no
delay or deficiency on the part of the TPA or insurer.
18. a) Complainant’s Argument: - The complainant states that the pre-authorization request for
cash-less facility was not responded in time but the claim was rejected on some false grounds citing
clause 4-3-1, which was not informed to him while accepting premium by the insurer. He states that the
claim shuld be honoured.
b) Insurer’s Argument: - The Insurer argues that the concerned disease falls under clause 4.3.1
of the policy and hence, the claim qualifies for denial and there is no delay or deficiency on the part of
the TPA or insurer.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Photocopies of Policy,
b. Photocopies of Medical documents
22. Result of hearing with both parties (Observations & Conclusion): - This Forum has carefully gone
through all the documents submitted relating the complaint and heard both the parties. During
hearing the complainant informed that the insurer has not provided the policy terms and conditions
except the policy schedule. The insurer said that they have given the policy terms and conditions
also. But the insurer could not provide any document substantiating their claim. The Complainant
says that the Hospital, on 09.05.2018 at 12.43 hours, had informed the TPA about this case of
admission and then accordingly the insured was admitted on 10.05.2018 at 07.31 hours, but the TPA
sent the cash-less denial information at about 14.00 hours on 10.05.2018, after the operation. The
complainant paid the expenses to the hospital and preferred for reimbursement as per the TPA’s
cash-less denial letter. Finally, the claim was denied by the TPA for reimbursement under 24 moths
exclusion clause. The complainant says that the Cash-less denial letter clearly mentions as “It also
does not prevent the patient to submit for reimbursement” and in spite of such assurance for

reimbursement, the claim was denied. The insurer argued that they have given the terms and
conditions and the treatment falls under exclusion clause (1
st
24 months exclusion) and therefore,
the claim is not payable under the policy terms.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall comply with
the award within 30 days of the receipt of the award and shall intimate the compliance of
the same to the Ombudsman.
As per the Rule 17(7) the complainant shall be entitled to such interest at a rate per annum
as specified in the regulations framed under the Insurance Regulatory and Development
Authority of India Act 1999, from the date of the claim ought to have been settled under
the regulations, till the date of payment of amount awarded by the Ombudsman.
As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be binding
on the Insurers.
Dated at Bhubaneswar on 11
th
day of December, 2019 INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – SHRI SURESH CHANDRA PANDA
CASE OF Mr. Rabindra Ku Dash Vrs. Iffco Tokio General Insurance Co Ltd.
COMPLAINT REF: NO: BHU-H-023-1920-0010
AWARD NO: IO/BHU/A/GI/ /2019-20
1.
Name & Address of the Complainant
Mr. Rabindra Ku Dash,
Plot No- 18, GGP enclave
Pandra Road, PO_ GGP,
Bhubaneswar. 94370 21429, 7008201219
2.
Policy No:
Type of Policy
Duration of policy/Policy period
52517692 (SIV Rs.3 lac + Bonus Rs.15000/-)
Swasthya Kavach (Family Health Policy)
(1
st
inception 28.08.2014)
27.08.2015 to 26.08.2016 (DoH 12.07.2016)
3.
Name of the insured
Name of the policyholder
Lelina P samant (Wife)
Mr. Rabindra Ku Dash,
4.
Name of the insurer
Iffco Tokio General Insurance Co Ltd.
5.
Date of Repudiation
09.09.2016
6.
Reason for repudiation
Non-disclosure of material facts
7.
Date of receipt of the Complaint
23.05.2018
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.33188/-
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs.33188/-
12.
Complaint registered under
13(1)b
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both the
parties during the course of hearing, the Forum did not find any conclusive proof in support of
delivery of policy terms and conditions by the insurer to the complainant. Non-delivery of the
policy terms and conditions with the policy schedule surely deprived the complainant to know the
coverage/exclusion details. Further, the TPA failed to inform the hospital/complainant before the
operation and took more than 24 hours to communicate the denial of cash-less. Had the TPA
informed about the applicable exclusion, on time at least before the patient’s admission, the
situation could have been different. More so, the tone and tenor of TPA’s cash-less denial letter
with wordings “It also does not prevent the patient to submit for reimbursement” gives a positive
assurance to the complainant for reimbursement. Under the above circumstances, the Forum is of
the view that the insured has all justified rights for his claim and therefore, the insurer is directed
to settle and pay Rs.62,979/- to the claimant towards full and final settlement of the claim.
Hence the complaint stands admitted.

Rule no: of IO rules
13.
Date of hearing/place
13.12.2019, Bhubaneswar
14.
Representation at the hearing
a) For the Complainant
Self
b) For the insurer
Shri Amit Maharana, Asst. Manager
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
13.12.2019
17. a. Brief Facts of the Case/ Cause of Complaint: - The Complainant has taken a health
insurance policy covering his wife and child from Iffco Tokio General insurance Co Ltd for a
family floater SIV of Rs.3,00,000/- for the period from 27.08.2015 to 26.08.2016. The wife of the
complainant was admitted in Health Village Hospital for treatment of severe headache on
12.07.2016 and got discharged on 15.07.2016. Previously she was treated in SUM Hospital on
05.07.2016, which records history of patient as Episodic Headache for 5 years and then by Dr.
Bikash Kumar Mishra, which says that the patient had 14 years hypertension history. The
complainant submitted bills of the hospitalization expenses and claimed Rs.33188/-. The Bills
submitted in the complaint pertains to Health village Hospital amounting to Rs.23942/- only.
The Insurer repudiated the claim considering the disease to be pre-existing before the inception
of the 1
st
policy- 28.08.2014, which was not declared in the proposal form and the same is
misrepresentation of facts. The complainant submitted a rectified OP Registration Slip of the
treating hospital by correcting 5 years as 5 moths and also has given a certificate of the doctor
to this effect. But the insurer did not consider the changes. Being aggrieved on repudiation of
the claim, the complainant filed an appeal before this Forum for redressal.
The insurer pleads that the petition with the Ombudsman is time barred as the claim was
repudiated on 09.09.2016. And the complainant failed to submit the documents in relation with
past treatments as the patient had episodic headache for 5 years and 14 years hypertension.
18. a) Complainant’s Argument: - The complainant states that he had submitted
consultation papers dated 29.12.2015 and 17.09.2015. He has also submitted the certificates
from the treating hospital as well as the doctor who treated the patient on 05.07.2016. The
Hospital does not say any past history of the ailment. Similarly, the Doctor, who had mentioned
the history of head-ache as 5 years has now issued a certificate mentioning the history to be 5
months old. In this situation, this cannot be considered as a pre-existing disease and therefore,
the claim should be settled.
b) Insurer’s Argument: -The insurer argues that as per the Medical documents of Sum
Hospital dated 05.07.2016, the patient had episodic head-ache for last 5 years, but the insured
did not declare the same in the proposal, which amounts to non-disclosure of pre-existing
disease. Secondly, the insurer also states that the complainant did not approach any court
within 12 months from 09.09.2016 (date of repudiation) and hence the case stands to be time-
barred and should not be entertained by the Hon’ble Ombudsman now. Thirdly, the insurer
also cited some judgements deciding in favor of insurers on non-disclosure of pre-existing
disease cases. Therefore, denial of claim is correct.
19. Reason for Registration of Complaint: - Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Photocopy of insurance
b. Photocopies of medical documents and certificates
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the submitted documents relating to the complaint and heard both
the parties. The insurer, in the SCN among other points, has pleaded to dismiss the case as it is
time barred in filing the case. It is observed that the insurer repudiated the claim on 12.07.2016
and the petition of the complainant was received in this office on 09.07.2017, which is well
within 12 months of repudiation and as per IO Rules, 2017 it cannot be considered as time
barred. Coming to the complaint, it is observed that the Medical documents have recorded the
medical history of the disease as Episodic Head-ache since last 5 years. The complainant, who is
also an agent of the said insurer, had submitted a doctor’s certificate dated 05.07.2016
subsequently rectifying the duration as five months instead of 5 years. The complainant argued
that it was a mistake on the part of the doctor, which was corrected later on. The complainant

stated that he had gone to many other doctors for treatment but was not satisfied. The medical
history also records about hypertension for last 14 years to which the complainant further
disputed as a mistake.
Dated at Bhubaneswar on 13
th
day of December, 2019 INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA
(UNDER RULE NO: 16(1)/17 of
THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Sri Suresh Chandra Panda
CASE OF (Mrs. Kuntala Naik Vs. SBI Life Ins. Co.ltd)
COMPLAINT REF: NO: BHU-L-041-1819-0449
AWARD NO: IO/BHU/A/LI/ 124/2017-2018
1.
Name & Address of the Complainant
Mr. Kuntala Naik, At- Baijapali,
Po- Bagdehi, Dist- Jharsuguda
2.
Policy No:
Type of Policy
Duration of policy/Policy period
46005685403
Life
28.10.2013
3.
Name of the insured
Name of the policyholder
Mr. Kuntala Naik
----do-----
4.
Name of the insurer
SBI Life Insurance Co. ltd
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of admission of the Complaint
07.03.2019
8.
Nature of complaint
Non-payment of Health claim
9.
Amount of Claim
Rs.250000/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs.250000/-
12.
Complaint registered under Rule no:
of Insurance Ombudsman Rules
13(1)(b)
13.
Date of hearing/place
05.12.2019 / Bhubaneswar
14.
Representation at the hearing
iiii) For the Complainant
Sundarmani Naik
jjjj) For the insurer
Sushanta Kumar Rout
15
Complaint how disposed
Under Insurance Ombudsman Rule 17.
16
Date of Award/Order
05.12.2019
17) Brief Facts of the Case:- The above mentioned Health Insurance policy was purchased by the complainant on
28.10.2013 from the present insurer. As per the policy schedule this policy provides health insurance on his own and his
wife’s life. The base plan covered Daily Hospital Benefit, Intensive care unit benefit and family care benefit. As per the
policy conditions any hospitalization should be intimated to the insurer before hospitalization in case of pre-planned
hospitalization or within 24 hours of hospitalization in case of emergency. The complainant mentioned 5 instances of
hospitalization on different dates and in different hospitals and claimed the insurance benefits which were rejected by the
insurer on different grounds. Hence, being aggrieved he approached this forum for redressal.
The insurer on the other hand submitted SCN stating that as per the terms and conditions of the policy, LA should
intimate the insurer regarding hospitalization prior to the occurrence. Only in case of emergency, the LA has the right for
delay in information up to 24 hours. In this case, there seems to be no emergency and all the time LA failed to intimate the
insurer prior to hospitalization. Even, it was delayed by more than 24 hours after hospitalization. In addition to it, the
complainant also failed to submit all the necessary documents before the insurer for admission of claim. Hence, the
complaint should be dismissed.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, it is observed that though the case is related
to Head-ache and is not related to hypertension, the complainant failed to provide any
convincing answer to the point that the disease (Head-ache) was not pre-existing. Given
the circumstances, the Forum accepts the disease to be pre-existing disease, which is
excluded until 48 months of continuous insurance coverage under the policy. Therefore,
the complainant is not entitled for the claim under the policy terms and conditions.
Hence, the complaint stands dismissed.

18) Cause of Complaint:
a) Complainant’s argument:- The complainant argued that she had purchased the above Health Insurance
policy from the present insurer on 28.10.2013. As per the policy schedule this policy provides health insurance on her
life. The base plan covered Daily Hospital Benefit, Intensive care unit benefit and family care benefit. As per the policy
conditions any hospitalization should be intimated to the insurer before hospitalization in case of pre-planned
hospitalization or within 24 hours of hospitalization in case of emergency. The complainant mentioned 3 instances of
hospitalization on different dates and in different hospitals and claimed the insurance benefits which were rejected by the
insurer on the ground of delayed intimation. But as per the complainant, in all the cases, he had intimated to the TPA
immediately after the admission just like the previous claim made by her and also settled by the insurer. During that time
the insurer had never objected for delayed intimation. Hence, the repudiation of claim by the insurer is arbitrary and not
justified.
b) Insurers’ argument:- The insurer on the other hand stated that as per the terms and conditions of the policy, LA
should intimate the insurer regarding hospitalization prior to the occurrence. Only in case of emergency, the LA has the
right for delay in information up to 24 hours. In this case, there seems to be no emergency and all the time LA failed to
intimate the insurer prior to hospitalization. Even, it was delayed by more than 24 hours after hospitalization.
19) Reason for Registration of Complaint: - scope of the Insurance Ombudsman Rules 2017.
This is a complaint against non-settlement of claim by Insurer.
20) The following documents were placed for perusal.
21)
a) Photo copies of proposal/policy document.
b) Photo copy of complaint letter and rejection letter by Insurer.
21) Result of hearing with both parties (Observations & Conclusion):- After going through the arguments
and submissions of both the parties it was observed that, in this case, the claims are repudiated because of
delayed intimation. But it was observed that in some instances, the claim in respect of the said policy was also
settled earlier by the insurer inspite of delayed intimation. Insurer have already settled claim in respect of the
same policy previously vide claim no. 100061512049 & 100031502056. The same procedure was adopted by
the claimant in these two cases for intimating to the insurer regarding admission for treatment. However, the
claimant stated that in all the occasions, he had intimated to the TPA immediately after the admission in
Hospital for treatment. Hence, this forum is of the opinion that all the claims applied by the complainant is to
be admitted and amount to be paid by the insurer as per rules.
22) The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. According to Rule 17(6) of the Insurance Ombudsman Rule 2017, the Insurer shall comply with
the Award within 30 days of the receipt of the award and shall intimate the compliance to the
Ombudsman.
b. As per rule 17(7) the complainant shall be entitled to such interest at a rate per annum as specified in the
regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date the claim ought to have been settled under the regulations, till the date of payment of the amount
awarded by the Ombudsman.
c. As per the rule 17(8), of the said rules the award of the Insurance Ombudsman shall be binding
on the Insurers.
Dated at Bhubaneswar on 05
th
Dec. 2019
(SURESH CHANDRA PANDA)
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA
(UNDER RULE NO: 16(1)/17 of
THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Sri Suresh Chandra Panda
CASE OF (Mr. Sundarmani Naik Vs. SBI Life Ins. Co.ltd)
COMPLAINT REF: NO: BHU-L-041-1819-0594
AWARD NO: IO/BHU/A/LI/122 /2017-2018
1.
Name & Address of the Complainant
Mr. Sundarmani Naik, At- Baijapali,
Po- Bagdehi, Dist- Jharsuguda
AWARD
Taking into account the facts & circumstances of the case and the submissions
made by both the parties during the course of hearing, it is awarded that the
health insurance claim in respect of the above complaint is to be admitted and paid
to the complainant as per rules.
The complaint is treated as allowed accordingly.

2.
Policy No:
Type of Policy
Duration of policy/Policy period
46005685403
Life
28.10.2013
3.
Name of the insured
Name of the policyholder
Mr. Sundarmani Naik
----do-----
4.
Name of the insurer
SBI Life Insurance Co. ltd
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of admission of the Complaint
07.03.2019
8.
Nature of complaint
Non-payment of Health claim
9.
Amount of Claim
Rs.250000/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs.250000/-
12.
Complaint registered under Rule no:
of Insurance Ombudsman Rules
13(1)(b)
13.
Date of hearing/place
05.12.2019 / Bhubaneswar
14.
Representation at the hearing
kkkk) For the Complainant
Sundarmani Naik
llll) For the insurer
Susanta Kumar Rout
15
Complaint how disposed
Under Insurance Ombudsman Rule 17.
16
Date of Award/Order
05.12.2019
17) Brief Facts of the Case:- The above mentioned Health Insurance policy was purchased by the complainant on
28.10.2013 from the present insurer. As per the policy schedule this policy provides health insurance on his own and his
wife’s life. The base plan covered Daily Hospital Benefit, Intensive care unit benefit and family care benefit. As per the
policy conditions any hospitalization should be intimated to the insurer before hospitalization in case of pre-planned
hospitalization or within 24 hours of hospitalization in case of emergency. The complainant mentioned 5 instances of
hospitalization on different dates and in different hospitals and claimed the insurance benefits which were rejected by the
insurer on different grounds. Hence, being aggrieved he approached this forum for redressal.
The insurer on the other hand submitted SCN stating that as per the terms and conditions of the policy, LA should
intimate the insurer regarding hospitalization prior to the occurrence. Only in case of emergency, the LA has the right for
delay in information up to 24 hours. In this case, there seems to be no emergency and all the time LA failed to intimate the
insurer prior to hospitalization. Even, it was delayed by more than 24 hours after hospitalization. In addition to it, the
complainant also failed to submit all the necessary documents before the insurer for admission of claim. Hence, the
complaint should be dismissed.
18) Cause of Complaint:
a) Complainant’s argument:- The complainant argued that the above mentioned Health Insurance policy was
purchased by him on 28.10.2013 from the present insurer. As per the policy schedule this policy provides health insurance
on his own and his wife’s life. The base plan covered Daily Hospital Benefit, Intensive care unit benefit and family care
benefit. As per the policy conditions any hospitalization should be intimated to the insurer before hospitalization in case
of pre-planned hospitalization or within 24 hours of hospitalization in case of emergency. The complainant mentioned 5
instances of hospitalization on different dates and in different hospitals and claimed the insurance benefits which were
rejected by the insurer on the ground of late intimation. The complainant also argued that he has purchased insurance on
the life of all members of his family and the insurer has also settled the claim on previous occasions. Even the insurer has
settled one claim amount of Rs.20000/- on 21.01.2015 against the same policy of the claimant. At that time also intimation
was sent to the insurer after the completion of treatment. Hence, repudiating claim on the ground of delayed intimation is
arbitrary on the part of the insurer.
b) Insurers’ argument:- The insurer on the other hand stated that as per the terms and conditions of the policy, LA
should intimate the insurer regarding hospitalization prior to the occurrence. Only in case of emergency, the LA has the
right for delay in information up to 24 hours. In this case, there seems to be no emergency and all the time LA failed to
intimate the insurer prior to hospitalization. Even, it was delayed by more than 24 hours after hospitalization. In addition
to it, the complainant also failed to submit all the necessary documents before the insurer for admission of claim. Hence,
the complaint should be dismissed.
19) Reason for Registration of Complaint: - scope of the Insurance Ombudsman Rules 2017.
This is a complaint against non-settlement of claim by Insurer.
20) The following documents were placed for perusal.
a) Photo copies of proposal/policy document.
b) Photo copy of complaint letter and rejection letter by Insurer.
21) Result of hearing with both parties (Observations & Conclusion):- After going through the arguments
and submissions of both the parties it was observed that, in this case, most of the claims are repudiated
because of delayed intimation. But it was observed that in some instances, the claim in respect of the said
policy was also settled by the insurer inspite of delayed intimation. However, the claimant stated that in all
the occasions, he had intimated to the TPA immediately after the admission in Hospital for treatment. In
addition to it in one case the insurer mentioned that “Hospitalization due to any condition where no active
management of the condition is involved or rest cures” which seems to be ridiculous. In case of the claim
no.100121509134, the insurer has called for some documents from the claimant which is genuine. The
claimant, during the course of hearing, stated that he has submitted all the documents as required by the
insurer from time to time. Now, the insurer is advised to check at it’s end and if the documents are still not
available, has to intimate the claimant to provide it once again. But, in regard to other cases, the insurer is
directed to settle the claim immediately without any further delay.

22) The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. According to Rule 17(6) of the Insurance Ombudsman Rule 2017, the Insurer shall comply with
the Award within 30 days of the receipt of the award and shall intimate the compliance to the
Ombudsman.
b. As per rule 17(7) the complainant shall be entitled to such interest at a rate per annum as specified in the
regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date the claim ought to have been settled under the regulations, till the date of payment of the amount
awarded by the Ombudsman.
c. As per the rule 17(8), of the said rules the award of the Insurance Ombudsman shall be binding
on the Insurers.
Dated at Bhubaneswar on 05
th
Dec. 2019
(SURESH CHANDRA PANDA)
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA
(UNDER RULE NO: 16(1)/17 of
THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Sri Suresh Chandra Panda
CASE OF (Mrs. Kanaka Kumari Nayak Vs. SBI Life Ins. Co.ltd)
COMPLAINT REF: NO: BHU-L-041-1819-0593
AWARD NO: IO/BHU/A/LI/123/2017-2018
1.
Name & Address of the Complainant
Mrs. Kanaka Kumari Nayak, At- Baijapali, PS_
LaikeraPo- Bagdehi, Dist- Jharsuguda
2.
Policy No:
Type of Policy
Duration of policy/Policy period
46005685403
Life
28.10.2013
3.
Name of the insured
Name of the policyholder
Mrs. Kanaka Kumari Naik
----do-----
4.
Name of the insurer
SBI Life Insurance Co. ltd
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of admission of the Complaint
07.03.2019
8.
Nature of complaint
Non-payment of Health claim
9.
Amount of Claim
Rs.165000/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs.165000/-
12.
Complaint registered under Rule no:
of Insurance Ombudsman Rules
13(1)(b)
13.
Date of hearing/place
05.12.2019 / Bhubaneswar
14.
Representation at the hearing
mmmm) For the Complainant
Sundarmani Nayak
nnnn) For the insurer
Susanta ku Rout
15
Complaint how disposed
Under Insurance Ombudsman Rule 17.
16
Date of Award/Order
05.12.2019
17) Brief Facts of the Case:- The above mentioned Health Insurance policy was purchased by the complainant on
28.10.2013 from the present insurer. As per the policy schedule this policy provides health insurance on her own and her
spouse’s life. The base plan covered Daily Hospital Benefit, Intensive care unit benefit and family care benefit. As per the
policy conditions any hospitalization should be intimated to the insurer before hospitalization in case of pre-planned
hospitalization or within 24 hours of hospitalization in case of emergency. The complainant mentioned 2 instances of
hospitalization on different dates and in different hospitals and claimed the insurance benefits which were rejected by the
insurer on different grounds. Hence, being aggrieved she approached this forum for redressal.
The insurer on the other hand submitted SCN stating that as per the terms and conditions of the policy, LA should
intimate the insurer regarding hospitalization prior to the occurrence. Only in case of emergency, the LA has the right for
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both
the parties during the course of hearing, it is awarded that the insurer has to call for all the
required documents( in case of claim ID no 100121509134) and settle the claim immediately.
But in regard to other cases, the claim is to be admitted and paid to the complainant without
any further delay.
Hence, the complaint is treated as allowed accordingly.

delay in information up to 24 hours. In this case, there seems to be no emergency and all the time LA failed to intimate the
insurer prior to hospitalization. Even, it was delayed by more than 24 hours after hospitalization. In addition to it, the
complainant also failed to submit all the necessary documents before the insurer for admission of claim. Hence, the
complaint should be dismissed.
18) Cause of Complaint:
a) Complainant’s argument:-The complainant argued that he purchased the above mentioned Health
Insurance policy from the present insurer on 28.10.2013. As per the policy schedule this policy provides health
insurance on her own and her spouse’s life. The base plan covered Daily Hospital Benefit, Intensive care unit benefit and
family care benefit. As per the policy conditions any hospitalization should be intimated to the insurer before
hospitalization in case of pre-planned hospitalization or within 24 hours of hospitalization in case of emergency. The
complainant mentioned 2 instances of hospitalization on different dates and in different hospitals and claimed the
insurance benefits which were rejected by the insurer on the ground of i) delayed intimation and ii) Hositalization due to
any condition where no active management is involved or rest cures.
b) Insurers’ argument:- The insurer on the other hand stated that as per the terms and conditions of the policy, LA
should intimate the insurer regarding hospitalization prior to the occurrence. Only in case of emergency, the LA has the
right for delay in information up to 24 hours. In this case, there seems to be no emergency and all the time LA failed to
intimate the insurer prior to hospitalization. Even, it was delayed by more than 24 hours after hospitalization. In addition
to it, the complainant also failed to submit all the necessary documents before the insurer for admission of claim. Hence,
the complaint should be dismissed.
19) Reason for Registration of Complaint: - scope of the Insurance Ombudsman Rules 2017.
This is a complaint against non-settlement of claim by Insurer.
20) The following documents were placed for perusal.
a) Photo copies of proposal/policy document.
b) Photo copy of complaint letter and rejection letter by Insurer.
21) Result of hearing with both parties (Observations & Conclusion):- After going through the arguments
and submissions of both the parties it was observed that, in this case, the claims are repudiated because of
delayed intimation. But it was observed that in some instances, the claim in respect of the said policy was also
settled earlier by the insurer inspite of delayed intimation. Insurer have already settled claim in respect of the
same policy previously vide claim no. 100071525615 & 100041512978. The same procedure was adopted by
the claimant in these two cases for intimating to the insurer regarding admission for treatment. However, the
claimant stated that in all the occasions, he had intimated to the TPA immediately after the admission in
Hospital for treatment. In addition to it in one case the insurer mentioned that “Hospitalization due to any
condition where no active management of the condition is involved or rest cures” which seems to be
ridiculous. Whether the patient requires admission in the Hospital or not, will be decided by the treating
Doctor, not the insurer. Hence, this forum is of the opinion that both the claims applied by the complainant is
to be admitted and amount to be paid by the insurer as per rules.
22) The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. According to Rule 17(6) of the Insurance Ombudsman Rule 2017, the Insurer shall comply with
the Award within 30 days of the receipt of the award and shall intimate the compliance to the
Ombudsman.
b. As per rule 17(7) the complainant shall be entitled to such interest at a rate per annum as specified in the
regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date the claim ought to have been settled under the regulations, till the date of payment of the amount
awarded by the Ombudsman.
c. As per the rule 17(8), of the said rules the award of the Insurance Ombudsman shall be binding
on the Insurers.
Dated at Bhubaneswar on 5
th
Dec. 2019
(SURESH CHANDRA PANDA)
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both
the parties during the course of hearing, it is awarded that the health insurance claim in
respect of the above complaint is to be admitted and paid to the complainant as per rules.
The complaint is treated as allowed accordingly

PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, STATE OF M.P. & C.G.
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
Mr.Rameshwar Nath….……………………………….…………..….. Complainant
V/S
National Insurance Co. Ltd ……………………………..…………..…..Respondent
COMPLAINT NO: BHP-G-048-1819-0284 ORDER NO: IO/BHP/A/GI/0165/2019-2020
• Mr. Rameshwar Nath (Complainant) has filed a complaint against National Insurance Co.
Ltd. (Respondent) alleging Repudiation of mediclaim.
• Brief facts of the Case - The complainant has stated that his wife was covered under
above policy issued by the respondent. She was admitted to Choithram Hospital &
Research Centre, Indore for treatment of low back ache with failed back surgery syndrome
on 10.07.2018 for which cashless request was raised to TPA. Pending disposal of request
the patient was admitted to the hospital on 10.07.2018 and was discharged on 12.07.2018.
Claim in question was wrongly rejected on the ground that particular line of treatment as
per TPA has not been followed namely epidural steroid procedure. Further clause 4.19 is
not applicable as patient was required to be admitted as inpatient for treatment. The
complainant has approached this forum for redressal of his grievance.
•
The respondent in their SCN have stated that complainant is covered in the above
policy along with his spouse for a floater sum insured of Rs.2 lacs. The claim pertains to
complainant’s wife. As per discharge summary the patient was admitted with complaints of
low back ache with failed back surgery syndrome, LBA since 15 days radiating to right
lower limb. As per patient, she was o/c of Spine surgery in the year 1979 and was having
pain since then for which TF was done in the year 2016 and was relieved. In June 2018 she
had jerky car travel since then she is c/o low back pain radiating to right lower limb. As per
discharge summary, patient was given treatment of radio frequency (RF) ablation of L3,
1.
Name & Address of the
Complainant
Mr. Rameshwar Nath,
G-1, Astha Residency Shiv City Nagar,
IPS academy AB Road, Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
604400/50/18/10000065
Hospitalisation Benefit Policy
01.04.2018 to 31.03.2019
3.
Name of the insured
Name of the policyholder
Dr.(Mrs.)Dinesh Nandini,
Mr. Rameshwar Nath
4.
Name of the insurer
National Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
Hospitalization not required
7.
Date of receipt of the Complaint
30.01.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
Rs.62,978/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.62,978/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
02.12.2019 at Bhopal
14.
Representation at the hearing
oooo) For the Complainant
Mr Rameshwar Nath
pppp) For the insurer
Mr S N Dale, Sr D M
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
02.12.2019

L4,L5,
Medical BRANC under MAC under II TV Guidance done on 12.07.2018 and for this
treatment, hospitalization is not warranted and does not fall under approved day care list.
Therefore patient got admitted only for diagnostic and evaluation purposes which could
have been done as outpatient and claim was repudiated as per Clause 4.19 of the policy
conditions.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• A claim under above policy was filed by the complainant for the reimbursement of
expenses incurred in the treatment of complainant’s wife from 10.07.2018 to 12.07.2018
taken at Choithram Hospital & Research Centre, Indore where she was diagnosed with low
back ache with failed back surgery syndrome. Claim was repudiated stating that during
hospitalisation insured’s MRI was done, treated with Radio frequency ablation and
hospitalisation for these were not warranted under clause 4.19 of policy terms and
conditions. Discharge summary reveals that insured was diagnosed with low back ache with
failed back surgery syndrome and during hospitalisation her MRI was done on 10.07.2018
and she was treated with radio frequency ablation on 12.07.2018. Clause 4.19 of policy
terms and conditions states that the insurer is not liable to pay for expenses incurred in
respect of diagnostic and evaluation purposes where such diagnosis and evaluation can be
carried out as outpatient procedure and the condition of the patient does not require
hospitalisation. In this case, insured had undergone MRI on 10.07.2018 and radio frequency
ablation on 12.07.2018 only during hospitalisation from 10.07.2018 to 12.07.2018 which
reveals that insured got admitted for diagnostic and evaluation purposes and such diagnosis,
evaluation and radio frequency ablation could have been carried out as outpatient
procedure. The representative of the respondent has argued that the procedure / treatment
which insured underwent does not fall under approved day care list also. Above facts and
circumstances shows that repudiation of claim is in accordance with the terms and
conditions of the policy and needs no interference. In the result, complaint is liable to be
dismissed.
• The complaint filed by Mr Rameshwar Nath stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated : Dec 2, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. Chacko Abraham….……………………………….………….. Complainant
V/S
National Insurance Co. Ltd ………………………………….………..Respondent
COMPLAINT NO: BHP-G-048-1819-0287 ORDER NO: IO/BHP/R/GI/ 0164 /2019-2020
1.
Name & Address of the
Complainant
Mr. Chacko Abraham,
Kanchan Medicare & Research Centre,

• Mr.Chacko Abraham (Complainant) has filed a complaint against National Insurance Co.
Ltd.(Respondent) alleging non settlement of mediclaim.
• Brief facts of the Case - The complainant has stated that he and his family members were
covered under above policy issued by the respondent. His wife was treated and operated
for Carcinoma of Left Breast in Amrita Institute of Medical Sciences, Kochi and he
incurred Rs.73,037/- till surgery. He preferred his claim for Rs.73,037/- to respondent
company on 16.05.2018 along with all relevant information and documents. Insured was
advised by team of doctors to go for four cycles of chemotherapy from 15.06.2018 to
16.07.2018. Thereafter he submitted additional claim for Rs.47,831/- on 12.09.2018 for
reimbursement. These claims have not been settled till this date. The complainant has
approached this forum for redressal of his grievance.
The respondent in their SCN have stated that Insured has taken the above Mediclaim
Policy and carried out Two hospitalizations in Amrita Institute, Kochi. 1st Hospitalization
was from 23.04.2018 to 26.04.2018 for the treatment diagnosed for Carcinoma of Left
Breast which was first detected on 10.04.2018 and respondent had paid the claim for
Rs.55,572/- on 20.05.2019. 2
nd
Hospitalization was from 04.06.2018 to 05.06.2018 which
was considered as No claim due to Non-compliance / submission of DOA & Discharge
Card, Investigation Reports, Dr’s Consultation / Prescription, Medicine purchased Bills
etc. As the insured has not submitted the above requirements even after continuous
reminders given by TPA vide mail dated 04.10.2018, 18.10.2018 & 02.11.2018 respondent
has repudiated the claim as per recommendation of TPA. Respondent had sent an email
dated 29.11.2019 stating that while matching with claimed amount it is found that an
amount of Rs.7,000/- as discount added by the insured during his hospitalisation and
amount of Rs.3,370/- & Rs.245.03 were left due to oversight which they are ready to pay
Rs.3,615.03.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
Opp.Gurudwara, Guna, Gwalior, MP
2.
Policy No:
Type of Policy
Duration of policy/Policy period
320604501710000101
National Mediclaim Policy
31.03.2018 to 30.03.2019
3.
Name of the insured
Name of the policyholder
Mrs.Suja Chacko
Mr.Chacko Abraham
4.
Name of the insurer
National Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
--
7.
Date of receipt of the Complaint
31.01.2019
8.
Nature of complaint
Non settlement of mediclaim
9.
Amount of Claim
Rs.1,20,868/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.1,20,868/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
02.12.2019 at Bhopal
14.
Representation at the hearing
for the Complainant
Absent
For the insurer
Mr Hemant Singh Rawat, Admn.Officer
15.
Complaint how disposed
Partially allowed
16.
Date of Award/Order
02.12.2019

• During hearing complainant remained absent. I have heard the representative of the
respondent company and perused papers filed on behalf of the complainant as well as the
Insurance Company.
• As per complaint two claims were lodged by the complainant 1) for amount of Rs,73,037/-
and 2) for Rs.47,831/-.
1
st
claim : As per SCN for first claim, date of first hospitalisation was 23.04.2018 with
discharge date 26.04.2018 and for this hospitalisation claim for Rs.55,572/- was paid on
20.05.2018 through NEFT. Respondent has filed a copy of calculation in which billed
amount has been shown as Rs.62,421.97, out of which approved amount is Rs.55,526.24
after deduction of Rs.6,895.73. Respondent later on filed re-calculation chart in which
billed amount has been shown as Rs.73,037/- and after deduction of Rs.13,895.73 approved
amount is shown as Rs.59,141.27. During hearing representative of the respondent has
informed that due to oversight amount of Rs.3,370/- and Rs.245.03 was left for payment
and they are ready to pay amount of Rs.3,615.03 (Rs.3,3,70 + Rs.245.03). He further
informed that amount of Rs.7,000/- was of hospital bill discount which was added by the
insured hence this amount is not payable to the insured. During hearing complainant
remained absent. Calculation sheet of respondent shows that out of claimed amount of
Rs.73,037/-, amount approved was Rs.59,141.27 by deducting amount of Rs.13,895.73.
Amount of Rs.7,000/- which was given to the insured as discount is not payable. Hence
under this claim respondent is liable to pay Rs.3,615.03 to the complainant.
2
nd
claim : As per SCN, for this claim hospitalisation was for 10.04.2018 and 04.06.2018
for the treatment taken at Amrita Institute of Medical Science and Research Center, Kochi.
As per complaint amount claimed by the complainant is Rs.47,831/-. Respondent with
respect to this claim has stated that as the insured had not submitted required documents
even after continuous reminders given by their TPA vide mail dated 04.10.2018,
18.10.2018, 02.11.2018 and 17.11.2018, claim was closed as No Claim on the ground of
non-compliance of their queries. As the requirements raised by the respondent were not
complied by the complainant, hence order of No Claim passed by the respondent is justified
and is in accordance with terms and conditions of the policy. Besides this none appeared on
behalf of the complainant to press the complaint with respect to this claim.
• In view of above discussed facts and circumstances, in first claim (for Rs.73,037),
complainant is entitled to get amount of Rs.3,615.03 more from respondent and in second
claim respondent has acted rightly in accordance with the terms and conditions of the
policy. Hence complaint is partially allowed with above observations and respondent is
ordered to make payment of Rs.3,615.03 to the complainant within 15 days from the date of
receipt of this award.
• Let copies of the order be given to both the parties.
Dated : Dec 2, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman

Mr. Kawaldeep Singh Tulli ….….…..……………….……….. Complainant
V/S
Star Health and Allied Insurance Co.Ltd ………..………..….Respondent
COMPLAINT NO: BHP-G-044-1819-0286 ORDER NO: IO/BHP/R/GI/ 0167/2019-2020
• Mr.Kuldeep Singh Tulli (Complainant) has filed a complaint against Star Health and
AlliedInsurance Co. Ltd.(Respondent) alleging rejection of mediclaim. Mr Preetpal Singh
Tulli policyholder / insured adopted the complaint filed by the brother of insured / wife of
Policyholder.
• Brief facts of the Case -The complainant has stated that insured / wife of policyholder was
covered under above mediclaim policy issued by the respondent company. She was
initially diagnosed with Ca.colon in January 2017 and was operated in January 2017.
Subsequently she was given chemotherapy of duration 6 months for 12 cycles, after some
times when the disease reoccurred she was advised 12 more cycles of chemotherapy over a
period of 6 months. Finally in VIMS hospital where the patient was admitted on
01.11.2018 she was diagnosed with Dengue as it is clearly mentioned in the DAMA
summary given by VIMS hospital. It is very clear that colon cancer was the first disease
and Dengue was the second. Claim was wrongfully denied by the respondent while patient
is eligible to get the claim under the salient feature of the policy terms as “Automatic
Restoration of Sum Insured”. The complainant has approached this forum for payment of
claim.
Respondent has filed three SCNs dated 08.05.2019, 02.12.2019(through email) and
03.12.2019(through email). The respondent in their SCN dated 02.12.2019 have stated that
their Claims Review Committee has considered the claim for settlement as per terms and
conditions of the policy for Rs.3,02,116/- against claimed amount of Rs.6,59,946/- after
deducting Rs.3,57,830/- (towards treatment received for cancer and non payable items). In
1.
Name & Address of the
Complainant
Mr. Kuldeep Singh Tulli,
Mr. Preetpal Singh Tulli,
Main Road PO Chikhlakasa, Balod,
Dallirajhara, C.G.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/201124/01/2019/000015
Family Health Optima Ins.2017
24.04.2018 to 23.04.2019
3.
Name of the insured
Name of the policyholder
Mr. Sarabjeet Kaur Tulli
Mr. Preetpal Singh Tulli
4.
Name of the insurer
Star Health and Allied Insurance Co.Ltd.
5.
Date of Repudiation/ Rejection
17.12.2018
6.
Reason for Repudiation/ Rejection
Sum assured already exhausted
7.
Date of receipt of the Complaint
27.01.2019
8.
Nature of complaint
Rejection of mediclaim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs. 4 lakhs
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
03/12/2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Preetpal Singh Tulli & Mr Kawaldeep
Singh Wahi, Brother of the deceased
For the insurer
Mr Ravi Tiwari, AGM Claims
15.
Complaint how disposed
Recommendation
16.
Date of Award/Order
03.12.2019

SCN dated 03.12.2019 sent through email by the respondent it is stated that their Claims
Review Committee has considered the claim for settlement as per terms and conditions of
the policy for Rs.3,57,830/- against claimed amount of Rs,7,43,475/- after deducting
Rs.3,57,830/- (towards treatment received for cancer and non payable items).
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• During course of hearing, both the parties has filed joint application (Mediation
Agreement) duly signed by the representative of complainant and respondent mentioning
therein about settlement of the matter willingly and mutually and agreed to settle the
subject matter of the complaint as follows–
The respondent has agreed to make the payment of amount of Rs.3,85,915/- to the
complainant towards full and final settlement of his claim No.CLI/2019/201124/0443150
under above policy / complaint within 30 days from the date of receipt of this award . The
complainant has also agreed for the same.
• As matter within parties has resolved mutually, hence the complaint is decided in terms of
mediation/mutual agreement between both the parties. Compliance of above shall be
intimated to this forum.
• Let copies of this order be given to both parties.
Dated: Dec 03, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance
Ombudsman
Mr. Ravi Mehta ………………………………………….……….. Complainant
V/S
United India Insurance Co.Ltd ………………………..……….…..Respondent
COMPLAINT NO: BHP-G-051-1819-0298 ORDER NO: IO/BHP/A/GI/ 0168 /2019-2020
1.
Name & Address of the
Complainant
Mr. Ravi Mehta,
BG 11 Scheme No. 74 C, Indore.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
1903002817P113528745
Individual Health Policy
09.01.2018 to 08.01.2019
3.
Name of the insured
Name of the policyholder
Mrs. Suchitra Mehta (wife)
Mr. Ravi Mehta
4.
Name of the insurer
United India Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
21.12.2018
6.
Reason for Repudiation/ Rejection
Policy covers only parental chemotherapy
(clause 2.1) and hospitalisation was less than
24 hours
7.
Date of receipt of the Complaint
21.02.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
Rs.1,22,000/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.1,22,000/-
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
03.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Absent
For the insurer
Mr Badal Jain, Admn Officer

• Mr. Ravi Mehta (Complainant) has filed a complaint against United India Insurance Co.
Ltd. (Respondent) alleging repudiation of mediclaim.
• Brief facts of the Case -The complainant has stated that his wife was covered under above
mediclaim policy issued by the respondent. His wife was diagnosed with cancer after tests
conducted on 23
rd
& 24
th
May 2017. She was hospitalized on 30
th
May 2017 at Apollo
Hospital, Indore. She was discharged on 05.06.2017. Following her surgery we went to
Tata Memorial in Mumbai on 15.06.2017 for a second opinion on her chemotherapy and
radiation therapy. This included 6 chemotherapy sessions to be done every 21 days and 12
sessions every week and was followed by 35 days of radiation therapy. After radiation,
doctor recommended to complete Tata Memorial’s treatment and do further chemotherapy
sessions to be done every 21 days. Respondent reimbursed all the chemotherapy session in
the year 2017 and when she reached the maximum payment of coverage in December, they
paid in January 2018 when claim was renewed. In 2018, when she reached the final
chemotherapy session, respondent reimbursed her first few claims for treatment with
Vivitra for the months of March, April and May. For her claim made on 16.06.2018 for
Rs.30,864/- they denied reimbursement. After this they even refused to accept our claims
for 07.07.2018(Rs.31,170/-), 28.07.2018 (Rs.30,864/-) and 18.08.2018 (Rs.29,564/-). The
complainant has approached this forum for redressal of his grievance.
The respondent in their SCN have stated that the above policy was issued for the
period 09.01.2018 to 08.01.2019 for a SI of Rs.3,00,000/- in the name of the complainant
and his wife. This policy is a continuous renewal of their own previous policy. Claim was
lodged by complainant for hospitalization of his wife on 16.06.2018 which was rejected as
per the recommendations of TPA MD India as injection Vivitra was administered which is
a monoclonal antibody specifically designed to target HER2 Receptors on breast cancer. It
flags the cancer cells for destruction by body’s immune system. Parental Chemotherapy is
not given in this case. Only supportive treatment is given and policy covered only parental
chemotherapy as per clause 2.1 of policy terms & condition. Moreover, as per Discharge
Card, the admission for hospitalization was for less than 24 hours. Clarification for why it
was reimbursed till May 2018 is that Audit team has initiated recovery proceedings against
the TPA M/s MD India for wrong reimbursement of claim for supportive treatments in
June 2018 and thereafter as per terms and conditions of policy, they have started
repudiating claims for supportive treatments.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• During hearing complainant remained absent. I have heard the representative of the
respondent company and perused papers filed on behalf of the complainant as well as the
Insurance Company.
• A claim for Rs.30,864/- under above policy was filed by the complainant on 16.06.2018
which was repudiated on 21.12.2018 stating that only supportive treatment was given,
parenteral chemotherapy was not given hence not payable under Clause 2.1 of policy. The
representative of the respondent has argued that insured was given injection Vivitra 440 mg
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
03.12.2019

(supportive treatment) which is a monoclonal antibody specifically designed to target
HER2 and flags the cancer cell for destruction by body immune system. As per medical
opinion Vivitra is a monoclonal antibody which is supportive treatment and not parenteral
chemotherapy. Clause 2.1 of policy terms and conditions states that expenses on
hospitalisation for minimum period of 24 hours are admissible and this time limit is not
applied to specific treatment of parenteral chemotherapy. Complainant has mentioned in his
complaint that the respondent had reimbursed for their first few claims for treatment with
Vivitra and now denied for claim of 16.06.2018. The representative of the respondent has
clarified that their TPA had wrongly reimbursed such claims for supportive treatments and
recovery has been initiated at the instance of Audit team. As the treatment given is a
supportive treatment and not parenteral chemotherapy hence respondent has rightly
repudiated the claim as per terms and conditions of the policy. None appeared on behalf of
the complainant to press the complaint. In the result, the complaint is liable to be
dismissed.
• The complaint filed by Mr Ravi Mehta stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 03, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance
Ombudsman
Mrs. Vibha Nema …………….….…..……………….……..…….. Complainant
V/S
Star Health and Allied Insurance Co.Ltd ………..……………..….Respondent
COMPLAINT NO: BHP-G-044-1819-0317 ORDER NO: IO/BHP/A/GI/0171/2019-2020
• Mrs.Vibha Nema (Complainant) has filed a complaint against Star Health and Allied
Insurance Co. Ltd.(Respondent) alleging rejection of mediclaim and cancellation of
policy.
1.
Name & Address of the
Complainant
Mrs. Vibha Nema
M/s Ganesh Traders, Main Road Kareli,
Narsinghpur, Jabalpur
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/201116/01/2018/003191
Mediclasic Insurance Policy (Individual)
30.09.2017 to 29.09.2018
3.
Name of the insured
Name of the policyholder
Mrs. VibhaNema
-same-
4.
Name of the insurer
Star Health and Allied Insurance Co.Ltd.
5.
Date of Repudiation/ Rejection
21.09.2018
6.
Reason for Repudiation/ Rejection
Non disclosure of material facts
7.
Date of receipt of the Complaint
26.02.2019
8.
Nature of complaint
Rejection of mediclaim
9.
Amount of Claim
Rs.44,177/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.44,177/-
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
04.12.2019 at Bhopal
14.
Representation at the hearing
qqqq) For the Complainant
Sh. Rahul Nema
rrrr) For the insurer
Mr Ravi Tiwari, AGM (Claims)
15.
Complaint how disposed
Recommendation
16.
Date of Award/Order
04.12.2019

• Brief facts of the Case -The complainant has stated that she was covered under above
mediclaim policy issued by the respondent company. In June 2018 her health deteriorated
and she had back pain. So she was admitted in Arneja Insitute, Nagpur and was given
treatment. Thereafter she had lodged her claim along with all documents which was
rejected stating that this is a pre-existing disease which was not disclosed at the time of
inception of policy. Prior to the incidence of pain in June 2018, she had shown to doctor
for back pain in June 2017 and doctor had told that she has Hemivertebra L2 problem.
But she has not experienced this type of pain before. The complainant has approached
this forum for payment of her claim and reinstatement of policy.
The respondent in their SCN dated 03.04.2019 have stated that the above policy was
issued in the name of complainant for the period 30.09.2017 to 29.09.2018 for SI of Rs.5
lacs and insured has reported claim in the 4
th
year and for an amount of Rs.44,177/-.
Insured was admitted to Arneja Institute of Cardiology Pvt Ltd, Nagpur on 25.05.2018.
As per Discharge summary the insured was diagnosed as Sensorimotor Polyneuropathy
Bilatern Ul and LL – Hemivertebra L2 Conversion disorder. Insured had submitted pre-
authorisation for cashless treatment on 26.05.2018 and a query was raised to submit
necessary documents and the same was not replied by the insured. Insured submitted a
claim for reimbursement of medical expenses for Rs.44,177/- on 21.06.2018. On scrutiny
it was found that MRI spine report dated 10.03.2017 submitted in response to query
raised shows Hemivertebra at L2/3 vertebral level which is congenital in nature and the
same was not disclosed at the time of proposing the policy. As per letter dated 10.03.2017
of the treating doctor, insured patient is suffering from SCOLIOSIS and as per letter
dated 22.08.2018, the insured patient is a k/c/o Hemivertebra prior to the inception of
policy. Hence it is evident that the insured patient is suffering from above mentioned
disease prior to the date of commencement of first year policy and the present admission
is for the treatment of pre-existing disease, hence claim was repudiated as per clause No.7
and 13. 30 days notice dated 21.09.2018 as per condition No. 13 for cancellation of
policy was sent to the proposer and the same was blocked from renewal. The respondent
had sent an email dated 03.12.2019 in which it is mentioned by them that their Claims
Review Committee has considered the claim for settlement as per terms and conditions of
the policy for Rs.42,489/- after deducting Rs.975/- as non-payables.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the
complainant as well as the Insurance Company.
• During course of hearing, both the parties has filed joint application (Mediation
Agreement) duly signed by the representative of complainant and respondent mentioning
therein about settlement of the matter willingly and mutually and agreed to settle the
subject matter of the complaint as follows–
The respondent has agreed to make the payment of amount of Rs.42489/- to the complainant
towards full and final settlement of his claim No.CLI/2019/201116/0096063 under above policy /
complaint within 30 days from the date of receipt of this award. The respondent is also agreed to
reinstate the policy from the date of receipt of award subject to completion of other formalities by
the complainant. The complainant has also agreed for the same.

• As matter within parties has resolved mutually, hence the complaint is decided in terms of
mediation/mutual agreement between both the parties. Compliance of above shall be
intimated to this forum.
• Let copies of this order be given to both parties.
Dated : Dec 4, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. Neeraj Kasliwal...…………………………………………….…….. Complainant
V/S
Oriental Insurance Co. Ltd ……………………………..……………..…...Respondent
COMPLAINT NO: BHP-G-050-1819-0295 ORDER NO: IO/BHP/A/GI/ 0172/2019-2020
• Mr. Neeraj Kasliwal (Complainant) has filed a complaint against Oriental Insurance Co.
Ltd. (Respondent) alleging non settlement of 5 mediclaims for an amount of Rs,4,30,553/-.
• Brief facts of the Case - The complainant has stated that he and his family members
including dependant parents were covered under above mediclaim policy issued by the
respondent for the period 11.04.2018 to 10.04.2019. After inception on 11.04.2011 he has
been regularly renewing the policy. His mother was suffering from cancer and so she was
admitted in Suyesh Hospital Pvt Ltd, Indore and he had preferred his claim to TPA
Medicorp Pvt Ltd, Indore. According to IRDA Regulations, 2016 an insurer shall settle or
reject a claim, as the case may be, within thirty days of receipt of the last necessary
documents. But Claim No.1, 3, 7, 9, 11 have not been settled by the respondent even after
220 days. In this connection he had written to respondent company on 13.12.2018 and their
Head office at Delhi but has not got any response from them. The complainant has
approached this forum for redressal of his grievance.
1.
Name & Address of the
Complainant
Mr. Neeraj Kasliwal,
17/3 Parsi Mohalla, Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
151300/48/2019/213
Happy Family Floater 2015
11.04.2018 to 10.04.2019
3.
Name of the insured
Name of the policyholder
Mrs.Usha Kasliwal
Mr.Neeraj Kasliwal
4.
Name of the insurer
Oriental Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
As per SCN injections administered to the
insured pertains to adjuvant / neo adjuvant
therapy, no basic anti cancer drug given and
therefore not payable on stand alone basis
7.
Date of receipt of the Complaint
14.02.2019
8.
Nature of complaint
Non settlement of mediclaim
9.
Amount of Claim
Rs. 4,30,553/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs. 4,30,553/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
09.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Nirmal Kasliwal, Father
For the insurer
Mr Girish Magre, Asstt Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
09.12.2019
The respondent in their SCN have stated that insured was diagnosed with carcinoma
breast for which she was admitted on different dates. She was given injection VIVITRA
440 and Injection ZOLASTA 4 MG in all these claims on stand alone basis. Both these
drugs are adjuvant neo adjuvant therapy and no basic anti cancer drug were given,
therefore any claim for adjuvant or neo adjuvant therapy is not payable on standalone
basis. Also all these claims are not forming part of pre and post hospitalization of any main
hospitalisation claim. Injection Vivitra is a monoclonal antibody and is a type of antibody
therapy that can be used alone or with chemotherapy. This drug works in different ways to
find and attack the cells where cancer starts and it is not a basic anti cancer drug. It is a
supportive adjuvant therapy and if given on standalone basis is not payable. Administration
of monoclonal antibody – Injection Vivitra is not listed in the day care list of the policy.
The insured was also given injection Zolendric acid (Injection Zolasta). It is also an
adjuvant therapy, this medication is used to treat high blood calcium levels that may occur
with cancer. Injection Zolendric acid is not a basic anti cancer drug but adjuvant therapy
and if given on standalone basis, is not payable.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• As per complaint, Claim No.19RB09OIH0830 for hospitalisation from 27.06.2018 to
28.06.2018 amounting to Rs.83,932/-, Claim No.19RB09OIH1047 for hospitalisation from
18.07.2018 to 19.07.2018 for Rs.70,916/-, Claim No.19RB09OIH1368 for hospitalisation
from 29.08.2018 to 30.08.2018 for Rs.1,34,669/-, Claim No.19RB09OIH1523 for
hospitalisation from 19.09.2018 to 20.09.2018 for Rs.69,013/-, Claim No.19RB09OIH1731
for hospitalisation from 10.10.2018 to 11.10.2018 for Rs.72,023/- for the total amount of
Rs..4,30,553/- were filed by the complainant towards the treatment of his mother on above
given dates for the treatment of Carcinoma of Breast at Suyesh Hospital Pvt Ltd, Indore and
all the above claims were not settled. A letter dated 16.10.2018 written by TPA addressed
to the respondent has been filed by the respondent which is with reference to the
representation of the claim in which TPA had noted that as the Injection Vivitra and
Zolendric acid are not basic anti cancer drug hence not payable. As per SCN, Injection
Vivtra 440 and Injection Zolasta 4 mg are not basic anti cancer drug and pertains to
adjuvant neo adjuvant therapy which is not payable on stand alone basis. The representative
of the respondent has argued that insured was given injection Vivitra 440 which is a
monoclonal antibody that can be used alone or with chemotherapy but not a basic anti
cancer drug and if these injections were given on stand alone basis are not payable. The
representative of the complainant has opposed the above argument of respondent and
argued that Dr Alok Modi has given a certificate that Vivitra 440 and Zolasta are standard
treatment for breast cancer and as the condition of the patient was very low, so she needed
hospitalisation. The representative of the complainant has filed original certificate of Dr
Modi while a photocopy of certificate of Dr Alok Modi has been filed by the respondents
representative also disclosing that above injections are only drugs for breast cancer. Both
the certificates are undated but in original certificate filed by the complainant only numeric
13 near the place earmarked for date has been written and from these certificates it cannot

be inferred when the certificates - one typed and the other handwritten were issued. As per
medical opinion, Vivitra 440 injection is a monoclonal antibody specifically designed to
target HER2 receptors and zolendric acid (Injection Zolasta) lowers high blood calcium
levels and these drugs are not basic anti cancer drugs but are only a supportive treatment.
Clause 3.17 of the policy terms and conditions states that hospitalisation means admission
in a Hospital for a minimum period of 24 consecutive hours inpatient care except for
specified procedure / treatments where such admission could be for a period of less than 24
hours. In Appendix I Day care procedures are listed in which cancer chemotherapy is
allowed as Day Care treatment. In Appendix I no procedure / surgery with respect to
administration of Vivitra 400 and Zolasta has been mentioned, hence in this case under day
care procedure also treatment administered to the insured is not allowed. Respondent has
filed Short Admission Discharge summary C5 Day Care – Unit I, Department of Pediatrics,
All India Institute of Medical Science in which also for RituxiMab therapy patient was
admitted as a day care procedure. As treatment / procedures could have been done on day
care basis, hence hospitalisation was also not warranted. As the treatment given is a
supportive treatment and not chemotherapy hence claims are not payable as per terms and
conditions of the policy. In the result, complaint is liable to be dismissed.
• The complaint filed by Mr Neeraj Kasliwal stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated : Dec 9, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. Pramod Kumar…...….………………………………………….. Complainant
V/S
Oriental Insurance Co.Ltd …………………………….……………....Respondent
COMPLAINT NO: BHP-G-050-1819-0294 ORDER NO: IO/BHP/A/GI/0173/2019-2020
1.
Name & Address of the
Complainant
Mr. Pramod Kumar, C/o Mittal Appliances
Ltd, 303, Apollo Trade Centre,
Geeta Bhawan Square, A.B.Road, Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
151191/48/2018/1846
Happy family floater-2015
20.12.2017 to 19.12.2018
3.
Name of the insured
Name of the policyholder
Mrs.Rashmi Kumar
Mr. Pramod Kumar
4.
Name of the insurer
Oriental Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
05.12.2018
6.
Reason for Repudiation/ Rejection
Admitted for diagnostic purpose only and no
active line of treatment given
7.
Date of receipt of the Complaint
13.02.2019
8.
Nature of complaint
Non settlement of Mediclaim
9.
Amount of Claim
Rs.21,174/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.21,174/-
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
09.12.2019 at Bhopal
14.
Representation at the hearing
ssss) For the Complainant
Mr Pramod Kumar
tttt) For the insurer
Mr A K Kotwani, Sr Branch Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
09.12.2019

• Mr. Pramod Kumar(Complainant) has filed a complaint against Oriental Insurance Co.
Ltd.(Respondent) alleging non settlement of mediclaim.
• Brief facts of the Case -The complainant has stated that he and his wife were covered
under above policy issued by the respondent company. He had preferred a claim for
Rs.21,174/- towards reimbursement of hospitalization expenses of his wife. Claim
documents were submitted to TPA on 30.07.2018 and further documents required by them
were submitted on 21.08.2018. Many reminders were sent to both TPA and respondent for
settlement of claim. Finally he received a letter dated 05.12.2018 stating that the claim is
not payable as per clause No.4.10. Thereafter he submitted a certificate of treating doctor
in response to respondent’s query on 11.01.2019 regarding hospitalization of the insured.
The complainant has approached this forum for redressal of his grievance.
The respondent in their SCN have stated that they have repudiated the liability due to
breach of policy clause No.4.10. As per claim documents, patient was admitted for gastro
esophageal reflux disease with irritable bowel syndrome and managed conservatively. But
as per received documents patient was on oral medication and admission was only for
diagnostic purpose, followed by No active line of treatment.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• Discharge summary of Amol Gastroentrology Hospital, Indore shows that the insured was
admitted to above Hospital on 18.07.2018 and discharged on 19.07.2018. Insured was
diagnosed with Gastro Esophageal Reflux Disease with irritable bowel syndrome. As per
Discharge Summary, during hospitalisation insured was treated conservatively and
hematology investigation, whole abdomen sonography and UGI Pan endoscopy were done.
On 18.07.2018 and 19.07.2018 insured was treated with capsules and tablets. In Discharge
Card medicines administered during hospitalisation are not mentioned. At the time of
discharge insured was also advised to take capsules and tablets. Bill of above Hospital are
also under Head registration charges, room rent, nursing charges, doctor visit charges,
gastroscopy and colonoscopy. Clause 4.10 of policy terms and conditions states that the
company shall not be liable to make payment of expenses incurred at Hospital or Nursing
Home primarily for evaluation / diagnostic purpose which is not followed by active
treatment for the ailment during the Hospitalization period. In this case also only
investigations through hematology, gastroscopy/colonoscopy and sonography were done
and there was no active line of treatment given to the insured. Hence as per above clause
respondent is not liable to pay such expenses as claimed. In the result complaint is liable to
be dismissed.
• The complaint filed by Mr Pramod Kumar stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated : Dec 9, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman

Dr.Abhay Kumar Jain ….... ..….……………………………….……….. Complainant
V/S
New India Assurance Co. Ltd ………………………………………..………..Respondent
COMPLAINT NO: BHP-G-049-1819-0297 ORDER NO: IO/BHP/A/GI/0174/2019-2020
• Dr.Abhay Kumar Jain(Complainant) has filed a complaint against New India Assurance Co. Ltd.
(Respondent) alleging repudiation of mediclaim. Complainant’s son has sent a letter dated
24.11.2019 for consideration of the complaint stating that complainant had expired on 10.03.2019
• Brief facts of the Case -The complainant has stated that he was covered under above mediclaim
policy issued by the respondent. He was admitted in Dr. Hinduja National Hospital and Medical
Research Centre, Mumbai from 15.11.2018 to 17.11.2018 for the treatment of Inflammatory
arthritis. Complainant incurred Rs.84,719/- towards medical expenses. Respondent denied the
claim stating that patient was admitted for Osteoporosis and treated by Injection Zoledronic acid
and no other active treatment was given. The complainant has approached this forum for redressal
of his grievance.
The respondent in their SCN have stated that complainant was hospitalized for Osteoporosis,
and during hospitalization patient was administered with injection Zoledronic acid and no other line
of treatment given to patient which requires hospitalisation. Patient was managed with oral
medication. Hence need for hospitalization is not justified & patient could be treated on OPD Basis.
Hence claim is not payable as per condition no. 2.16 of policy.
• The complainant has filed complaint letter, Annex. VI A and correspondence with respondent,
while respondent have filed SCN with enclosures.
• During hearing none appeared on behalf of complainant and a letter for absence was sent by his son.
I have heard the representative of the respondent company and perused papers filed on behalf of the
complainant as well as the Insurance Company.
• A Claim under above policy was filed by the complainant for the reimbursement of expenses
incurred in the treatment from 15.11.2018 to 17.11.2018 at P D Hinduja National Hospital &
Medical Research Centre, Mumbai which was repudiated by the respondent stating that insured was
administered with injection Zoledronic Acid 5mg and no other active line of treatment was given
which could have been done on OPD Basis and hospitalisation is not justified. The representative of
1.
Name & Address of the Complainant
Dr.Abhay Kumar Jain
City Hospital, Guard Lane,
Damoh
2.
Policy No:
Type of Policy
Duration of policy/Policy period
451002/34/17/95/00000010
New India Mediclaim Policy
27.03.2018 to 26.03.2019
3.
Name of the insured
Name of the policyholder
Dr. Abhay Kumar Jain
-same-
4.
Name of the insurer
New India Assurance Co. Ltd
5.
Date of Repudiation/ Rejection
17.01.2019
6.
Reason for Repudiation/ Rejection
Hospitalisation not justified
7.
Date of receipt of the Complaint
20.02.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
Rs.84,719/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.84,719/-
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
10.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Absent
For the insurer
Mr Ratnesh Tripathi, Dy Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
10.12.2019

the respondent has argued that the claim is also not payable as per policy condition No.2.16 and the
treatment is also not covered under Day care procedure listed in Annexure I. Discharge summary of
above Hospital shows that the complainant was admitted on 15.11.2018 and discharged on
17.11.2018. Insured was admitted with complaints of bilateral knee pain associated with swelling,
mid and low back pain and his Xray PBH, DEXA Scan was done and was given injection of
Zoledronic acid 5mg over 30 minutes. As per Discharge summary insured was diagnosed with
Inflammatory arthritis and was managed on the line of inflammatory arthritis. Besides above
injection, Injection Depo-Medrol and tablets of other medicines were also administered during
hospitalisation. Treatment given to the insured can also be done on OPD / Day Care Basis for which
hospitalisation is not justified. Condition 2.16 of the policy states that Hospitalisation means
admission in a hospital for a minimum period of 24 consecutive hours of inpatient care except for
specified procedures / treatments as mentioned in Annexure I, where such admission could be for a
period of less than 24 consecutive hours. In this condition it is also mentioned that procedures /
treatments usually done in OPD are not payable under the policy even if converted as an inpatient in
the Hospital for more than 24 consecutive hours. Treatment undergone by insured is not listed in
Annexure I. Hence as per above clause claim is not payable. In the result complaint is liable to be
dismissed.
• The complaint filed by Mr Abhay Kumar Jain stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated : Dec 10, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. Anil Rathi…...….………………………………………….. Complainant
V/S
Iffco-Tokio General Insurance Co. Ltd ……………….………..Respondent
COMPLAINT NO: BHP-G-023-1819-0316 ORDER NO: IO/BHP/A/GI/ 0180/2019-2020
1.
Name & Address of the
Complainant
Mr.Anil Rathi,
254 Dhar Road, Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
52893137
Individual Medishield policy
19.01.2018 to 18.01.2019
3.
Name of the insured
Name of the policyholder
Mrs. Sudha Rathi (wife)
Mr. Anil Rathi
4.
Name of the insurer
Iffco-Tokio General Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
27.11.2018
6.
Reason for Repudiation/ Rejection
Treatment taken is diagnostic and evaluatory
in nature and no active line of treatment was
given and hospitalisation not warranted
7.
Date of receipt of the Complaint
27.02.2019
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of Claim
Rs.2,27,024/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.1,90,000/- approx
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
11.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Dr Shashank Anant Vaidya, Personal
Physician
For the insurer
Dr Aditya Gulati, Asstt Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
11.12.2019

• Mr. Anil Rathi (Complainant) has filed a complaint against Iffco-Tokio General Insurance
Co. Ltd. (Respondent) alleging repudiation of mediclaim.
• Brief facts of the Case -The complainant has stated that his wife was covered under above
policy issued by the respondent company. His wife was admitted in Asian Heart Hospital,
Mumbai on 29.10.2018 and for this claim was settled by the company. As per advise of
doctor on 30.10.2018, before discharging from Asian heart Hospital she was advised to go
for Stress Thulium Test. As per doctor’s advise, she was admitted on 30.10.2018 for stress
thulium test in Jaslok Hospital, Mumbai because such test is only available in this hospital.
It was the continues treatment of M/s Asian Heart Hospital, Mumbai. He made claim
before the respondent for treatment at Jaslok Hospital, Mumbai form 01.11.2018 to
02.11.2018 but they rejected his claim. The complainant has approached this forum for
payment of his claim.
The respondent in their SCN have stated that the complainant has submitted three
claims before the respondent out of which two claims were already settled. The third claim
No.2018110100017.R1 for Rs. 2,17,430/- was submitted by complainant for admission of
patient in Jaslok Hospital, Mumbai from 01.11.2018 to 02.11.2018 under diagnosis
Fractional Flow Reserve to LAD. On going through the claim documents submitted by the
insured, it was found that the treatment given as per discharge summary which indicates
that patient was admitted only FFR not for stress thallium, which was prescribed by
Dr.Prafull Kerkar on 30.10.2018. As FFR was not prescribed and it is a diagnostic &
evaluator in nature, no active line of treatment was followed during hospitalization which
warrants the need of hospitalization and patient was primarily admitted for investigation
purpose only. This hospitalization is also not fall under day care list, hence claim was
repudiated under Clause 9 and definition 28 of policy.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• Claim No.2018110100017.R1 for Rs.2,17,430/- was filed for the treatment of insured taken
at Jaslok Hospital, Mumbai from 01.11.2018 to 02.11.2018 which was repudiated by the
respondent stating that the admission was only for diagnostic and evaluatory purpose, no
active line of treatment was given and hospitalisation was not warranted. Discharge
Summary of Jaslok Hospital, Mumbai states that the insured was admitted on 01.11.2018,
discharged on 02.11.2018 and diagnosed with FFR to LAD. Discharge Summary also
reveals that the insured was admitted and posted for FFR to LAD and procedure was done
by Dr A B Mehta on 01.11.2018. Her CAG was also done. Bill of above Hospital also
shows that Fractional Flow Reserve Measurement and Angiography was done. The bill for
Rs.2,17,430/- issued by the Hospital is for FFR and Angiography only. Hence, insured’s
FFR and Angiography was done at Jaslok Hospital, Mumbai while as per complainant
insured was advised for Stress Thallium test. Treatment undergone i.e. FFR and
Angiography is a diagnostic and evaluatory test. The representative of the complainant,
who is a personal Physician of the complainant, during hearing has accepted that FFR,
Angiography and Stress Thallium Test are diagnostic and evaluatory. Discharge summary

also reveals that no active line of treatment was given during hospitalisation. As no active
line of treatment was given to the insured hospitalisation was not warranted. Condition No.
9 of coverage clause of the policy states that the respondent will not pay for Expenses on
diagnostic, X-ray or Laboratory examinations unless related to the active treatment of
Disease or injury falling within ambit of Hospitalization or Domiciliary Hospitalisation
claim. Hence as per above clause, claim is not payable and respondent has acted in
accordance with the terms and conditions of the policy. In the result, complaint is liable to
be dismissed.
• The complaint filed by Mr Anil Rathi stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 11, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance
Ombudsman
Mr. Alok Singhai ………………….…………………………..….... Complainant
V/S
United India Insurance Co.Ltd ………………………..…………..Respondent
COMPLAINT NO: BHP-G-051-1819-0330 ORDER NO: IO/BHP/A/GI/0183/2019-2020
• Mr. Alok Singhai (Complainant) has filed a complaint against United India Insurance Co.
Ltd. (Respondent) alleging rejection of mediclaim.
• Brief facts of the Case -The complainant has stated that he is having the Mediclaim Policy
since last 8 years. He was hospitalized from 23.09.17 to 26.09.17 in Bombay Hospital,
Indore for Complex Partial Seizure and submitted the claim papers / bills etc. along with
clarification note from treating Doctor but claim was declined with the reason stating that
claim is not admissible as the expenses incurred for diagnostic purpose not consistent with
or incidental to the diagnosis or presence of any ailment is an exclusion under the policy
terms and conditions. Whereas the condition of disease was established in the diagnostic
1.
Name & Address of the
Complainant
Mr. Alok Singhai,
429, Royal Krishna Bunglows, Rau, Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
1918002817P105751636
Family Medicare policy 2014
28.07.2017 to 27.07.2018
3.
Name of the insured
Name of the policyholder
Mr. Alok Singhai
-same-
4.
Name of the insurer
United India Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
29.03.2018
6.
Reason for Repudiation/ Rejection
Expenses incurred for diagnostic purpose
7.
Date of receipt of the Complaint
22.03.2019
8.
Nature of complaint
Non settlement of mediclaim
9.
Amount of Claim
Rs.85,754/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.85,754/-
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
12.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Alok Singhai
For the insurer
Mr G S Chhabra, Divisional Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
12.12.2019

test Video EEG was overlooked by the respondent and treatment is continuing even after
discharge from Hospital. On denial of claim, the complainant has approached this forum
for redressal of his grievance.
The respondent in their SCN have stated that the insured has lodged a claim under
the policy for hospitalization as referred above. On scrutiny & as per TPA’s Doctor it was
observed that insured was treated conservatively with few diagnostic tests and no
therapeutic treatment was done during hospitalisation. It is further noticed (from the
admission Note of hospital) that the patient had come for Video EEG. His vitals were
stable. The Hospital’s Discharge Summary also mentions that the patient was admitted for
Video EEG. The subsequent Doctor’s certificate is false which states that he requires the
admission on emergency basis due to complex partial seizure and that he was unresponsive
in casualty. Even that certificate also mentions that for further management, he requires
Video EEG for 24 hours. Admission at hospital was mainly for diagnostic tests which falls
under exclusion clause No.4.11 of policy.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• Claim for Rs.85,754/- was filed for the reimbursement of expenses incurred in the
treatment of insured taken at Bombay Hospital, Indore from 23.09.2017 to 26.09.2017
which was repudiated by the respondent stating that the admission was only for diagnostic
purpose. Discharge Summary of Bombay Hospital, Indore states that the insured was
admitted on 23.09.2017, discharged on 26.09.2017 and diagnosed with Complex Partial
Seziser (right temporal low origin), Rem sleep behaviour disorder. Discharge Summary
and Initial assessment form reveals that the insured was admitted for Video EEG. Insured’s
USG and MRI were also done. Bill of above Hospital is under Head Room charges,
miscellaneous, surcharge, medicine (PSD), Doctors fees, clinical pathology, bio-chemistry,
EEG, MRI and ultrasound. The representative of the respondent has argued that insured
was admitted for video EEG, MRI, USG, managed conservatively and no therapeutic
treatment was given during hospitalisation. He further argued that at the time of admission,
as per Discharge Summary insured’s vitals were stable and hospitalisation was not
warranted as no active line of treatment was given to the insured. Clause 4.11 of the policy
states that the company shall not be liable to make payment in respect of any expenses /
charges incurred at Hospital or Nursing Home primarily for diagnosis, X ray, or laboratory
examination or other diagnostic studies not consistent with or incidental to the diagnosis
and treatment of positive existence or presence of any ailment, sickness or injury, for
which confinement is required at a Hospital / Nursing Home. Hence as per above clause,
claim is not payable and respondent has acted in accordance with the terms and conditions
of the policy. In the result, complaint is liable to be dismissed.
• The complaint filed by Mr Alok Singhai stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 12, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman

Mr. Virendra Suri…..….……………………………….……….. Complainant
V/S
National Insurance Co. Ltd ……………………………..………..Respondent
COMPLAINT NO: BHP-G-048-1819-0333 ORDER NO: IO/BHP/A/GI/ 0185 /2019-2020
• Mr. Virendra Suri (Complainant) has filed a complaint against National Insurance Co. Ltd.
(Respondent) alleging partial settlement of mediclaim.
• Brief facts of the Case - The complainant has stated that he was covered under above
Insurance policy issued by the respondent. He was admitted in Kokilaben Hospital,
Mumbai from 25.10.2018 to 29.10.2018 for surgery of Gangrenous Cholecystitis.
Thereafter he lodged the claim before the respondent company for reimbursement of
medical expenses, but respondent had deducted Rs.26,398/- in the name of ‘Reasonable
and Customary Charges’. The complainant has approached this forum for payment of
balance amount.
The respondent in their SCN have stated that TPA assessed and settled the claim for
Rs.1,45,000/- deducting Rs.26,380/- on account of Reasonable and customary clause
guidelines on standardization in health insurance of IRDAI in chapter I. This claim is
related to Laparoscopic cholecystectomy. Claim has not been repudiated by TPA but only
deducted amount of Rs.26,380/- on account of Reasonable and customary charges. They
further stated that TPA GIPSA charges in Hospital in Mumbai/Delhi/Kolkata etc. the
surgeon charges for the same surgery were much less than what was charged by the
hospital, hence GIPSA charges were considered as Reasonable & customary for a
comparable geographical location and the deduction were done accordingly.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
1.
Name & Address of the
Complainant
Mr. Virendra Suri,
A72, Central Avenue Road, Smriti Nagar,
Bhilai, Chattisgarh
2.
Policy No:
Type of Policy
Duration of policy/Policy period
295203501810000128
Baroda Health Policy
03.07.2018 to 02.07.2019
3.
Name of the insured
Name of the policyholder
Mr. Virendra Suri
-same-
4.
Name of the insurer
National Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
--
7.
Date of receipt of the Complaint
31.01.2019
8.
Nature of complaint
Partial settlement of mediclaim
9.
Amount of Claim
Rs.26,398/-
10.
Date of Partial Settlement
03.04.2019
11.
Amount of relief sought
Rs.26,398/-+Rs.5,000/- interest+Rs.25,000/-
harassment
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
12.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Anil Vohra, Friend
For the insurer
Mr Shibu John, A.M.
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
12.12.2019

• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• Out of claimed amount of Rs.1,79,335/- amount of Rs.1,45,000/- was paid by the
respondent deducting Rs.26,398/- (Rs.6,000/- anesthetist fee, Rs.10,000/- surgeon charges
and Rs.10,398/- major OT charges). As per respondent, deductions were made in
accordance with Reasonable and Customary clause of the policy. Representative of the
respondent has argued that charges for above has been paid considering GIPSA PPN rates
for similar geographical area i.e. Mumbai. Representative of the respondent has filed
Mumbai GIPSA PPN rates for Mumbai Hospital, S L Raheja and Jaslok Hospital &
Research Centre at Mumbai. Total package for cholecystectomy (laproscopy) at Mumbai
Hospital, Mumbai is Rs.1,42,700/-, S L Raheja, Mumbai is Rs.1,32,560/- and Jaslok
Hospital & Research Centre Mumbai is Rs.1,32,000/- (B1 Class). Clause 3.23 of policy
states that Reasonable and Customary charges means the charges for services or supplies,
which are standard charges for the specific provider and consistent with the prevailing
charges in the geographical area for identical and similar services taking into account the
nature of the illness / injury involved. As in this case, amount of Rs.1,45,000/- has been
paid by deducting Rs.26,398/- to the complainant for above treatment hence settlement of
claim is in accordance with the terms and conditions of the policy.
• In view of above facts and discussions, I come to the conclusion that the respondent has not
erred in settling the claim as per terms and conditions of the policy. In the result, the
complaint is liable to be dismissed.
• The complaint filed by Mr Virendra Suri stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 12, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. Sanjeev Raj Nimoria……….…………………..…..………………….. Complainant
V/S
Star Health & Allied Insurance Co.Ltd………………..………..………...…Respondent
COMPLAINT NO: BHP-H-044-1920-0009 ORDER NO: IO/BHP/A/HI/ 0001/2019-2020
1.
Name & Address of the
Complainant
Mr Sanjeev Raj Nimoria
24, Piyush Nagar, Awadhpuri Kalan BHEL
Bhopal
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/201113/01/2019/005996
Family Health Optima Insurance Plan
09.01.2019 to 08.01.2020
3.
Name of the insured
Name of the policyholder
Mr.Sanjeev Raj Nimoria & 3 others
Mr. Sanjeev Raj Nimoria
4.
Name of the insurer
Star Health & Allied Insurance Co.Ltd
5.
Date of Repudiation/ Rejection
02.03.2019, 18.05.2019, 21.05.2019
6.
Reason for Repudiation/ Rejection
Chronic Kidney disease not disclosed
7.
Date of receipt of the Complaint
28.03.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
Rs.2,700/- per dialysis
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.2,700/- per dialysis
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
13.12.2019 at Bhopal
14.
Representation at the hearing

• Mr. Sanjeev Raj Nimoria (Complainant) has filed a complaint against Star Health & Allied
Insurance Co.Ltd (Respondent) alleging repudiation of claims.
• Brief facts of the Case -The complainant has stated that he has filed claim Nos.
CLI/2019/201113/0586428, 0592647, 0599057, 0611210, 0604211, 0617991 and 0625256
with the respondent company. These claims were repudiated by the respondent company.
He took the policy on 09.01.2015 and had disclosed diabetes in the policy. The
complainant has approached this forum for payment of his claims.
The respondent in their SCN have stated that the complainant was covered under
above Family Health Optima Insurance Plan with PED-Diabetes Mellitus and its
complications, his wife and two dependent children for a floater sum insured of Rs.5 lacs
vide policy No. Policy No.P/20113/01/2015/002710 for the period 09.01.2015 to
08.01.2016, No.P/20113/01/2016/003071 for the period 09.01.2016 to 08.01.2017,
No.P/20113/01/2017/003646 for the period 09.01.2017 to 08.01.2018,
No.P/20113/01/2018/004634 for the period 09.01.2018 to 08.01.2019, No.P/2
0113/01/2019/005996 for the period 09.01.2019 to 08.01.2020 and the insured has reported
claims in the 5
th
year of the medical insurance policy. Insured was admitted in Nav Jeevan
Hospital, Kodi on 11.01.2019 and as per Discharge Summary insured was diagnosed with
CKD. Insured submitted a claim for reimbursement of medical expenses on 11.02.2019 for
a sum of Rs.2,645/-. Thereafter insured was hospitalized in the same hospital on
15.01.2019, 18.01.2019, 24.01.2019, 21.01.2019, 28.01.2019, and 31.01.2019 for the same
treatment i.e. Dialysis and submitted 6 bills on 05.02.2019 for Rs.2,645/- each. On scrutiny
it is observed that as per Discharge Summary of Noble Multispeciality Hospital for
admission on 15.09.2015, the insured patient is a known case of Chronic Kidney Disease
and is on treatment for the same since then. Based on above documents it is observed that
the insured has longstanding kidney disease. Thus called for previous treatment records
and the same were closed due to non submission of documents. In reply the insured
submitted a representation to reconsider the claim along with the previous treatment
records. On scrutiny of the same it is observed that as per prescription dated 07.03.2017 by
Doctor Rubina Vohra, from CHL Hospital, patient is a known case of CKD since 3 years.
From the above it is observed that insured patient is suffering from above mentioned
disease prior to the commencement of first year policy and the present admission and
treatment of insured patient is for the related complications. The failure to disclose the pre-
existing disease amounts to non-disclosure of material facts. From the above it is clear that
the proposer / complainant who signed the proposal form has deliberately not disclosed the
past medical history and this amounts to misrepresentation / non-disclosure of material
facts. Claim was repudiated as per condition No.6 of the policy. They further stated that
respondent has issued notice dated 20.05.2019 informing that policy will be cancelled on
account of misrepresentation and non disclosure of material facts as per terms and
conditions of the policy No.12.
For the Complainant
Mr Sanjeev Raj Nimoria
For the insurer
Mr Ravi Tiwari, AGM Claims
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
13.12.2019

• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
• Seven Claims - Nos.CLI/2019/201113/0586428, 0592647, 0599057, 0611210, 0604211,
0617991 and 0625256 were filed for the reimbursement of expenses incurred in the
treatment of complainant at Nav Jeevan Hospital on different dates which were repudiated
as per conditions No.6 by the respondent stating that insured is a k/c/o Chronic Kidney
Disease since March 2014 which is prior to the date of commencement of first policy year
and this ailment was not disclosed at the time of taking the policy. The representative of
the respondent has argued that Discharge Summary of Noble Multispeciality Hospital for
admission on 15.09.2015 states that the patient is a k/c/o Chronic Kidney Disease. As per
prescription dated 07.03.2017 of Doctor Rubina Vohra of CHL Hospital, patient was
having a CKD since 3 years i.e. since March 2014 which is prior to the inception of first
policy. He further argued that above ailment was not disclosed at the time of taking first
policy with them. Above mentioned discharge summary and prescription clearly reveals
that the patient is k/c/o CKD and as per prescription of Doctor Rubina Vohra insured was
having this ailment since 3 years i.e. from March 2014. First policy commenced on
09.01.2015. In proposal form above ailment was not shown. Hence complainant had not
disclosed his ailment of CKD while taking the first policy. Claims for dialysis were filed
and dialysis is directly related to CKD. Condition No.5.6 of the policy terms and condition
states that the company shall not be liable to make any payment under the policy in respect
of any claim if information furnished at the time of proposal is found to be incorrect or
false. As the complainant had not disclosed the ailment of CKD at the time of inception of
first policy, as per above clause claims are not payable. Hence repudiations of respondent
are justified and are in accordance with the policy terms and conditions. In the result,
complaint is liable to be dismissed.
• The complaint filed by Mr Sanjeev Raj Nimoria stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 13, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. V P Srivastava ..………….…………………..…..…………….. Complainant
V/S
Star Health & Allied Insurance Co.Ltd………………..………..…..…Respondent
COMPLAINT NO: BHP-H-044-1920-0015 ORDER NO: IO/BHP/A/HI/0003 /2019-2020
1.
Name & Address of the
Complainant
Mr. V P Srivastava
Flat No. G-3 Yamuna Block Ultimate
Campus, Mandakini Colony,
Kolar Road, BHOPAL
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/201113/03/2018/000019
Star Travel Protect Insurance
23.05.2017 to 20.08.2017
3.
Name of the insured
Name of the policyholder
Mr. V P Srivastava
Mr. V P Srivastava
4.
Name of the insurer
Star Health & Allied Insurance Co.Ltd

• Mr. V P Srivastava (Complainant) has filed a complaint against Star Health & Allied
Insurance Co.Ltd (Respondent) alleging rejection of claim.
• Brief facts of the Case -The complainant has stated that he is insured under Mediclassic
Insurance Policy (individual) since 06.01.2014 and the same has been continuously
renewed. In this policy DM and its complications are mentioned as PED. This policy
having run for four claim free years, exclusion clause is not applicable under this policy.
Complainant has stated that there are over-writing on the medical history sent by
respondent to him as he had replied as NO to question enquiring whether he is suffering
or have suffered from any illness / disease upto the time of making this proposal. But the
same has been written and someone has mentioned BP last 6 years. He has stated that he
suffered with Hyponatremia which is a condition directly caused by Urinary NA
(Sodium) and potassium losses and therefore no way related with ‘Hypertension” and its
complications. He had submitted an application dated 27.03.2019 for reconsideration of
his claim. Failing to receive any communication from the respondent office he has
approached this forum for payment of his claim.
The respondent in their SCN have stated that the above policy was issued to the
complainant for his travel abroad for the period 23.05.2017 to 20.08.2017 for a SI of
USD 2,50,000. At the time of inception of policy insured disclosed Blood Pressure in the
proposal form and the same was incorporated as PED in the policy schedule. The insured
submitted claim documents on 20.12.2017 for reimbursement of medical expenses for
USD 10,261 for the treatment of Hyponatremia on 15.06.2017 (i.e. 23
rd
day). As Per
Discharge Referral date 15.06.2017 the insured was administered with Clinidipine,
Telmisartan, Hydrochlorathiazide and Clopidgrol. As per pre-authorisation form
submitted by the Hospital to TPA Pvt Ltd, it is observed that the insured patient had past
history of T2DM, HTN, IHD and Anxiety. From the above findings it is observed that the
insured patient had pre-existing disease and the same was not disclosed at the time of
inception of policy. Further it is stated that BP was incorporated as PED in the policy
schedule based on the declaration in the proposal form. Now the insured was treated with
Hyponatremia which is the condition of pre-existing systemic hypertension. The insured
concealed material facts at the time of availing policy, further the claim of the
complainant is towards the treatment of complication of pre-existing disease.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
5.
Date of Repudiation/ Rejection
07.02.2019
6.
Reason for Repudiation/ Rejection
PED Excluded under the policy
7.
Date of receipt of the Complaint
25.04.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Australian Dollar 10,019.60
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
17.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Absent
For the insurer
Mr Ravi Tiwari, AGM Claims
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
17.12.2019

• During hearing complainant remained absent and had sent a written statement and
information regarding his absence dated 05.08.2019. I have heard the representative of
the respondent at length and perused papers filed on behalf of the complainant as well as
the Insurance Company.
• A Claim under above policy was filed by the complainant for the reimbursement of
expenses incurred by the insured / complainant in the treatment taken at Cantebury
Hospital, Cantebury Road, Sydney from 15.06.2017 to 20.06.2017. Claim was repudiated
by the respondent as pre-existing diseases are not payable as per point No.3 of special
exclusion under section 1 of policy terms and conditions stating that insured was having
history of hypertension and diagnosed disease of hyponatremia is a complication of
hypertension. Discharge Referral of Cantebury Hospital, Sydney reveals that the insured
was admitted on 15.06.2017, discharged on 20.06.2017 and was diagnosed with
Hyponatremia. In the cashless pre-authorisation form submitted to TPA through Hospital,
in the column of past medical surgical history it is mentioned that insured is having past
history of Type 2 DM, HTN, IHD and anxiety. As per Discharge summary and above
pre-authorisation form it is clear that the insured was suffering from HTN prior to the
inception of the policy. Opinion of Dr S Guru Mageswaran of Chennai dated 05.02.2019
is on record in which Doctor has opined that Hyponatremia is the complication of pre-
existing systemic hypertension. As per medical opinion, disease Hyponatremia is the
complication of Hypertension.
As per Part IV Special exclusions No.3 of policy terms and conditions, company shall not
be liable to make any payment in respect of medical condition prior to commencement of
this insurance. As per this exclusion, respondent is not liable to make payment of claim
with respect to disease Hyponatremia. Hence respondent has rightly repudiated the claim,
as per terms and conditions of the policy. In the result, complaint is liable to be
dismissed.
• The complaint filed by Mr V P Srivastava stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 17, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. Pankaj Meliwal ………….…………………..…..………………….. Complainant
V/S
Star Health & Allied Insurance Co.Ltd………………..………..………...…Respondent
COMPLAINT NO: BHP-H-044-1920-0010 ORDER NO: IO/BHP/A/HI/0002/2019-2020
1.
Name & Address of the
Complainant
Mr.Pankaj Meliwal
40 B Kailash park colony
Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/201114/01/2018/010196
Family Health Optima Insurance
13.01.2018 to 12.01.2019
3.
Name of the insured
Name of the policyholder
Mr.Pankaj Meliwal
Mr. Pankaj Meliwal
4.
Name of the insurer
Star Health & Allied Insurance Co.Ltd
5.
Date of Repudiation/ Rejection
07.03.2019, 17.05.2018 and 16.05.2018

• Mr. Pankaj Meliwal (Complainant) has filed a complaint against Star Health & Allied
Insurance Co.Ltd (Respondent) alleging repudiation of two claims. Claim
No.CLI/2019/201114/0020520 for Rs.1,22,044/- has also been mentioned in Annexure VI
as rejected by the respondent and filed three rejection orders dated 07.03.2019, 17.05.2018,
16.05.2018 with original complaint.
• Brief facts of the Case -The complainant has stated that he has filed claims bearing
No.CLI/2019/201114/0382025, CLI/2018/201114/640685 and CLI/2019/201114/0020520
for Rs.98,300/-, Rs.3,78,836/-, and Rs.1,22,044/- respectively with the respondent
company. Respondent company has denied the claims stating that there is over writing in
Doctor’s prescription. His Doctor Atul Shinde gave a personal letter / consent about the
over writing on prescription, but still respondent company is not ready to accept the claim.
Complainant has approached this forum for payment of his claims.
The respondent in their SCN dated 12.12.2019 have stated that the complainant had
filed 2 claims i.e. Claim No.CLI/2019/201114/0382025, CLI/2018/201114/0640685 and
under the above policy. Under claim No.CLI/2019/201114/ 0382025 an amount of
Rs.86,754/- was paid to the complainant on 05.07.2019 as full and final settlement vide
DD No.303935 on 01.07.2019. Under claim No. CLI/2018/201114/0640685 an amount of
Rs.3,37,377/- was paid to the complainant on 05.07.2019 as full and final settlement vide
DD No.480095 on 03.07.2019. They further stated that above claims were reviewed and
considered for settlement and based on the consent for withdrawal of complaint they have
settled. The insured has also furnished Discharge voucher on 05.07.2019. Another Claim
No.20520 was reviewed and Claims Review Committee has considered the claim for
settlement as per terms and conditions of the policy for Rs.87,525/- against the claimed
amount of Rs.1,21,901/- after deducting Rs.34,376/-. Respondent vide email dated
06.12.2019 have further informed that the complainant has agreed for settlement of claim
No.20520 for Rs.87,525/- and has agreed to withdraw the case after receipt of Bank DD for
Rs.87,525/-. The respondent has also mentioned in their SCN that the above amount of
Rs.87,525/- will be paid within 30 days.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• During hearing complainant remained absent. I have heard the representative of the
respondent company and perused paper filed on behalf of the complainant as well as the
Insurance Company.
6.
Reason for Repudiation/ Rejection
Consultation report date is tampered /
Misrepresentation – Clause No. 6
7.
Date of receipt of the Complaint
15.04.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
Rs.5,99,180/- (for three claims)
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.5,99,180/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
16.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Absent
For the insurer
Mr Ravi Tiwari, AGM Claims
15.
Complaint how disposed
Partially allowed
16.
Date of Award/Order
16.12.2019

• As per respondent Claim No.CLI/2019/201114/0382025, CLI/2018/201114/640685 has
been settled and amount of Rs.86,654/- and Rs.3,37,377/- were paid to the complainant on
05.07.2017. Discharge voucher of these claims dated 03.07.2019 and 04.07.2019 have
been filed by the respondent in which it is mentioned by the complainant that the amounts
are for full and final settlement of these claims. Hence these claims have been settled and
paid to the complainant to the satisfaction of the complainant.
With respect to third Claim No. CLI/2019/201114/0020520 respondent in their SCN have
stated that they have reviewed the claim filed for Rs.1,21,901/- and have considered
payment of Rs.87,525/- after deduction of Rs.34,376/- as full and final settlement and
amount will be paid within 30 days of receipt of this order to the complainant.
Complainant vide email dated 06.12.2019 addressed to the respondent has given his
consent and mentioned that he is agree to settle the claim for amount of Rs.87,525/- offered
by the respondent and will withdraw the complaint after receiving the DD. Hence it is
clear that third claim is also settled for amount of Rs.87,525/- for which complainant has
also agreed. Today on the date of hearing complainant remained absent. The
representative of the respondent has mentioned in SCN that they will pay the above
amount within 30 days of receipt of this order. Hence amount of Rs.87,525/- is payable to
the complainant under this claim.
• In view of above facts and discussions, complaint with respect to Claim No.
CLI/2019/201114/0020520 is allowed and respondent is directed to make the payment
within 30 days from the date of receipt of this order. Complaint with respect to claim
Nos.CLI/2019/201114/0382025, CLI/2018/201114/640685 stands dismissed as settled and
paid .
• The complaint filed by Mr Pankaj Meliwal stands partially allowed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 16, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr.Bhadar Singh ……………...……….………………………….. Complainant
V/S
Apollo Munich Health Insurance Co.Ltd ………………………..………..Respondent
COMPLAINT NO: BHP-H-003-1920-0021 ORDER NO: IO/BHP/A/HI/0006/2019-2020
1.
Name & Address of the
Complainant
Mr.Bhadar Singh,
703, Gali No-3, Meerpur Alipur Ashtha
Distt- Sehore M.P
2.
Policy No:
Type of Policy
Duration of policy/Policy period
170500/11001/AA0065943
Easy Health Individual Standard policy
01.09.2016 to 31.08.2017
3.
Name of the insured
Name of the policyholder
Mr.Bhadar Singh
-same-
4.
Name of the insurer
Apollo Munich Health Insurance Co.Ltd
5.
Date of Repudiation/ Rejection
07.09.2017
6.
Reason for Repudiation/ Rejection
Claim filed with fraudulent intention
7.
Date of receipt of the Complaint
12.04.2019
8.
Nature of complaint
Non settlement of Claim
9.
Amount of Claim
Rs.68,984/-
10.
Date of Partial Settlement
--

• Mr.Bhadar Singh (Complainant) has filed a complaint against Apollo Munich Health
Insurance Co.Ltd (Respondent) alleging non settlement of Claim.
• Brief facts of the Case -The complainant has stated that he had taken the above policy.
Suddenly he fell ill and took treatment at Mehcko Hospital, Bhopal from 15.04.2017 to
21.04.2017. Thereafter he lodged the claim for the reimbursement of expense incurred in
the treatment but respondent have not paid the claim amount. The complainant has
therefore approached this forum for redressal of his grievance.
The respondent in their SCN have stated that the above policy was issued to the
complainant based on the proposal form submitted by him for the period 01.09.2016 to
31.08.2017. Complaint has lodged claim for Rs.68,984/- for his treatment taken at Mehcko
Hospital, Bhopal. Thereafter respondent sought query demanding additional information /
documents i,e In-patient record, lab reports etc. Respondent initiated detailed verification
in which it was found that the hospital did not provide In-patient record for verification as
the concerned person was unavailable. No lab reports or pharmacy bills were provided for
verification. Complainant was also not available when the investigator tried to contact him
on his mobile (not reachable). They further stated that during investigation Dr R K Tiwari
the pathologists verification was conducted and as per statement of Dr R K Tiwari neither
had he visited the lab nor the reports were made or signed by him. Pathologists name and
registration certificate was used without his knowledge by the Hospital. Complainant had
lodged the claim fraudulently. Hence the claim was repudiated on the grounds of fraud as
per policy section VII k.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• A claim for Rs.68,9894/- was lodged under above policy by the complainant for the
reimbursement of expenses incurred in the treatment of insured taken at Mehcko Hospital,
Bhopal from 15.04.2017 to 21.04.2017 which was repudiated and policy was cancelled as
per policy Section VII k by respondent stating fraud claim was filed. Representative of the
respondent has argued that after intimation of claim they investigated the matter through
their investigator and found that lab Pathologist Dr R K Tiwari who had given investigation
reports has denied the visits to the concerned lab and also denied his signatures on
pathology reports. He further argued that the reports submitted were fake and fabricated in
order to gain from insurance. Blood report, RFT, LFT, Urine report, Blood glucose report,
Widal has been filed by the respondent which have been issued on the letter head of
Mehcko Hospital, Bhopal with seal and signature of Dr R K Tiwari, Pathologist.
Investigation report has been filed by the respondent in which it is mentioned that
11.
Amount of relief sought
Rs.68,984/-
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
19.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Bhadar Singh
For the insurer
Mr Manoj Gupta, Executive Field Ops.
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
19.12.2019

investigator visited the Pathologist at his residence and showed him the reports for his
credentials, then he provided written statement that neither he visited this lab nor the reports
were signed by him. Along with investigation report statement of Dr R K Tiwari which
was given on the report of Urine, has been filed by the respondent on which it is mentioned
that “I state solemnly that I do not visit above lab nor these reports signed by me”. Hence
statement of Dr R K Tiwari given to the investigator clearly reveals that the pathological
reports submitted by the complainant with his claim are fake and not signed by the
Pathologist, Dr R K Tiwari. This creates doubt about the genuineness of pathological
reports. Section VII k of policy terms and conditions states that if any claim is in any
manner dishonest or fraudulent, or is supported by any dishonest or fraudulent means or
devices then all benefits payable under the policy shall be forfeited and policy shall be
cancelled. In this case as the pathological reports are doubtful hence the claim has been
lodged on the basis of created / fake pathological reports. As per this clause respondent
company has rightly repudiated the claim and cancelled the policy.
Representative of the respondent has argued that when their investigator visited the
Hospital for verification of ICP of patient, but Hospital’s record was not provided by the
Hospital stating that the concerned person is out of station for 10 days. Verification of
Hospital record is a right of respondent and by non-cooperation of Hospital, rights of
respondent got affected.
• In view of above facts and circumstances, I come to the conclusion that the respondent
company has rightly rejected the claim and cancelled the policy and has acted in accordance
with the terms and conditions of the policy. In the result, complaint is liable to be
dismissed.
• The complaint filed by Mr Bhadar Singh stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 19, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. D S Upadhyay..…………………..…..………………….. Complainant
V/S
New India Assurance Co.Ltd………………..………..………...…Respondent
COMPLAINT NO: BHP-H-049-1920-0005 ORDER NO: IO/BHP/A/HI/0004 /2019-2020
1.
Name & Address of the
Complainant
Mr. D S Upadhyay
AG 182 Scheme No.54
Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
450800/34/18//95/00000596
New India Mediclaim policy
08.11.2018 to 07.11.2019
3.
Name of the insured
Name of the policyholder
Mrs. Pratibha Upadhyay
Mr. D S Upadhyay
4.
Name of the insurer
New India Assurance Co. Ltd
5.
Date of Repudiation/ Rejection
19.02.2019
6.
Reason for Repudiation/ Rejection
Under Policy Condition No.2.16 and 2.10
7.
Date of receipt of the Complaint
08.04.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.1,06,467/-

• Mr. D S Upadhyay (Complainant) has filed a complaint against New India Assurance
Co.Ltd (Respondent) alleging repudiation of claim.
• Brief facts of the Case -The complainant has stated that he was receiving claim from
respondent company since last two years. His wife was suffering with Multiple Myeloma
and required hospitalization for chemotherapy as advised by doctor. Suddenly respondent
has refused the claim for the treatment of his wife taken on 20.12.2018. His claims for the
same disease and for the same treatment were settled earlier by the respondent company.
Now they have declined the claim. The complainant has approached this forum for
redressal of his grievance.
The respondent in their SCN have stated that above policy was issued to complainant
for the period 08.11.2018 to 07.11.2019. Complainant lodged a claim for treatment of his
wife taken at Greater Kailash Hospital, Indore on 20.12.2018. Discharge summary of
insured shows that insured was diagnosed with Multiple Myeloma and was hospitalized for
administration of injections BORETEZOMIB and ZOLENDRIC ACID on 201.12.2018.
These injections are a monoclonal antibody drugs and is a supportive therapy. Since it is
not an anti cancer drug, it is not chemotherapy. These were given on stand alone basis and
no anti cancer drug had been given along with these. These are not forming part of pre and
post hospitalisation. As the treatment was taken on day care basis which is not listed in
Annexure I of the policy hence claim was rejected under clause No.2.16 and 2.10 of policy
terms and conditions.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
• A Claim for Rs.1,06,467/- was filed by the complainant for the treatment of his wife taken
at Greater Kailash Hospital, Indore on 20.12.2018 which was repudiated by the respondent
under Policy clause No.2.16 and 2.10 stating that the administered injections Boretizomib
and Zoledronic acid is a monoclonal antibody drug and not an anti cancer drug and these
injections are supportive therapy which were given on stand alone basis. In repudiation it is
also mentioned that treatment given is not included in Annexure I of the Day Care list.
Discharge summary of Greater Kailash Hospital, Indore shows that on 20.12.2018 Injection
Boretizomib 2mg and Injection Zoledronic 4 mg were administered to insured. The
respondent could not show any evidence showing that injection Boretizomib is a
monoclonal antibody drug. Medical information at Google shows that Boretizomib is a anti
cancer drug and is a type of chemotherapy. Hence administration of Injection Boretizomib
is a chemotherapy treatment. List of day care procedures which are allowed as per clause
2.16 of policy terms and conditions is given in Annexure I of policy and cancer
chemotherapy is included at Sl No.139 in the list. As the treatment administered to the
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 18.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr K P Maheshwari, Friend
For the insurer
Mr Ratnesh Tripathi, Dy Manager
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
18.12.2019

insured is a type of chemotherapy, claim is payable to the complainant. Hence, repudiation
of respondent is not justified. In the result, claim is liable to be allowed.
• The complaint filed by Mr D S Upadhyay is allowed and respondent is directed to allow the
claim as per terms and conditions of the policy within 30 days from the date of receipt of
this order.
• Let copies of the order be given to both the parties.
Dated: Dec 18, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr.Vijay Yadav………………....……….………………………….. Complainant
V/S
Max Bupa Health Insurance Co.Ltd …………………….…………..………....Respondent
COMPLAINT NO: BHP-H-031-1920-0027 ORDER NO: IO/BHP/A/HI/ 0007 /2019-
2020
• Mr.Vijay Yadav (Complainant) has filed a complaint against Max Bupa Health Insurance
Co.Ltd (Respondent) alleging partial settlement of Claim.
• Brief facts of the Case -The complainant has stated that he had taken the above policy and
lodged a claim for hospitalization expenses from 19.02.2019 to 23.02.2019 but respondent
has settled the claim for an amount of Rs.13,365/- and remaining claimed for Rs.11,779/-
was not paid. A complaint was made to grievance Cell of the respondent but he did not get
settlement for remaining claim. Hence the complainant has approached this forum for
redressal of his grievance.
The respondent in their SCN have stated that they have processed the claim papers of
insured Mr.Kavyansh Yadav and paid the claim for Rs.13,665/- admissible as per policy
through NEFT. The deduction for Rs.11,779/- was made due to following reasons;
Rs.6000/- excess room charges, Rs.3750/- excess visit charges deducted as per tariff,
Rs.187/- excess lab charges deducted as per tariff; provider discount is applied in the
1.
Name & Address of the
Complainant
Mr.Vijay Yadav S/O Raghyanath Makan
H.No-239, Gram Ninas
Distt- Dewas M.P
2.
Policy No:
Type of Policy
Duration of policy/Policy period
30752236201800
Health Companion Variant 2
16.03.2018 to 15.03.2019
3.
Name of the insured
Name of the policyholder
Mr.Kavyansh Yadav
Mr.Vijay Yadav
4.
Name of the insurer
Max Bupa Health Insurance Co.Ltd
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
--
7.
Date of receipt of the Complaint
16.05.2019
8.
Nature of complaint
Partial settlement of claim
9.
Amount of Claim
Rs.25,444/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.11,779/-
12.
Complaint registered under Rule
Rule No. 13(1)(b)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
19.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Vijay Yadav
For the insurer
Mr Sudhanshu Shekhar, Branch Manager
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
19.12.2019

referred deductions. Present complaint is filed for dispute with respect to deductions made
by the company for Rs.11,779/-. They further stated that without getting into merits of the
matter they have decided to initiate settlement in the manner that amount of Rs.10,434/- is
payable is to the complainant after deducting non-payables amount of registration and
service charges as Rs.1,345/-.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• In this claim, out of claimed amount of Rs.25,444/-, amount of Rs.13,685/- was paid to the
complainant, deducting Rs.11,779/-. As per SCN and email of respondent dated 04.12.2019
respondent is agree to make further payment of Rs.10,434/- after deducting registration and
service charges of Rs.1,345/- which are non-payables as per policy. Deduction of
Rs.1,345/- with respect to registration charges and service charges is in accordance with
policy conditions. As the respondent is agreed to make payment of Rs.10,434/- to the
complainant, hence complaint is liable to be allowed. In the result complaint is allowed and
respondent is directed to make payment of balance amount of Rs.10,434/- to the
complainant within 30 days from the date of receipt of this order.
• Let copies of the order be given to both the parties.
Dated: Dec 19, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mr. Mukesh Wadhwani ..………….…………………..…..………………….. Complainant
V/S
Star Health & Allied Insurance Co.Ltd………………..………..………...…Respondent
COMPLAINT NO: BHP-H-044-1920-0038 ORDER NO: IO/BHP/A/HI/0012/2019-2020
1.
Name & Address of the
Complainant
Mr. Mukesh Wadhwani
62/2,Berathi Colony, Khatiwala Tank Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/201114/01/2018/008955
Family Health Optima Insurance Plan
12.12.2017 to 11.12.2018
3.
Name of the insured
Name of the policyholder
Mr. Piyush Wadwani
Mr. Mukesh Wadhwani
4.
Name of the insurer
Star Health & Allied Insurance Co.Ltd
5.
Date of Repudiation/ Rejection
-
6.
Reason for Repudiation/ Rejection
-
7.
Date of receipt of the Complaint
21.05.2019
8.
Nature of complaint
Less payment of mediclaim
9.
Amount of Claim
Rs.33,448/-
10.
Date of Partial Settlement
27.09.2018, 14.01.2019
11.
Amount of relief sought
Rs.33,448/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 24.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Piyush Wadhwani, Son
For the insurer
Mr Ravi Tiwari, AGM Claims
15.
Complaint how disposed
Partially allowed
16.
Date of Award/Order
24.12.2019

• Mr. Mukesh Wadhwani (Complainant) has filed a complaint against Star Health & Allied
Insurance Co. Ltd (Respondent) alleging less payment of mediclaim.
• Brief facts of the Case -The Complainant has stated that he has taken above policy in
which his son was also insured. His son Mr.Piyush Wadhwani was admitted in Kokilaben
Dhirubhai Ambani Hospital, Mumbai for the period 31.07.2018 to 03.08.2018 and then
from 08.10.2018 to 16.10.2018. He filed a claim of Rs. 4,73,818/-. out of which
Rs.3,89,071/- was paid and unpaid amount was Rs.84,748/-. Then the Company again paid
an amount of Rs.49,300/ and Rs.2,000/-. The Complainant has requested that an order be
passed for payment of Rs.33,448/- which remained unpaid by the respondent.
The respondent in their SCN have stated that the complainant and his family
members were covered under above policy for the period 12.12.2017 to 11.12.2018.
Insured submitted 2 claims in the 8
th
year of Insurance policy bearing
Nos.CLI/2019/201114/0218563 and CLI/2019/20114/0377700. The insured patient was
hospitalized from 31.07.2018 to 03.08.2018 and was diagnosed with Refractory seizures.
Out of the total claim of Rs.93,590/ an amount of Rs.92,763/ was paid to the insured. The
excluded expenses towards easy bath, alcohol swabs etc. are not payable hence Rs.827/-
was deducted. Again the insured person was admitted in Kokilaben Dhirubhai Ambani
Hospital, Mumbai on 08.10.2018 and discharged on 16.10.2018. An amount of
Rs.2,91,537/- was authorized and settled as cashless to the insured. The insured further
submitted claim for reimbursement towards the balance deducted amount. Rs.54,071/ was
considered and settled. On further representation a further amount of Rs.2,000/- was also
paid. Thus out of total claimed amount of Rs.3,60,671/- an amount of Rs.3,47,608/
(Rs.2,91,537/- + Rs.54,071/- + Rs.2,000/) was settled to the insured. As per exclusion
No.26 nutritional charges are not payable hence Rs. 650/- was deducted. An amount of
Rs.7,992/- was deducted on account of excluded expenses like gluco test, blood group,
bacto scrub etc. As per exclusionNo.5 the charges towards rehabilitation are not payable
hence an amount Rs.4,421/- was deducted. Thus out of total claimed amount of
Rs.4,54,261/- (Rs.3,60,671/ + Rs.93,590/-) the total amount of Rs.4,40,371/-
(Rs.3,47,608/- + Rs.92,763/-) settled towards the both the claims. Respondent vide SCN
dated 24.12.2019 have stated that in Claim No.0218563 amount claimed was Rs.1,02,590/-
and they have received bills for Rs.93,590/- . Against these bills, they have settled amount
of Rs.92,763/- after deducting nonpayables items of Rs.827/-. Insured had claimed amount
of Rs.9,000/- towards Hospital cash benefit which is not payable since patient was
admitted in Non preferred hospital as per coverage ‘M’ and not occupied I sharing room
as per coverage ‘N’. In Claim No.0377700 patient remained for 2 days in ICU and 6 days
in sharing room. He claimed amount of Rs.2,91,537/- cashless which was approved in full.
Insured submitted reimbursement claim of Rs.79,691/- out of which bills for Rs.67,570/-
were received by them.They had settled amount of Rs.54,507/- after deducting non-
payable items of Rs.13,063/-. Insured also claimed Rs.9,800/- towards hospital cash benefit
which is not payable since patient was admitted in their non preferred hospital as per
coverage ‘M’. They further stated that patient occupied sharing room for 6 days hence as
per coverage ‘N’ Rs.4,800/- (6 x Rs.800/- ) can be considered more and they are ready to
pay this amount to the insured.

• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
• Two claims were filed by the complainant for different hospitalisation which were partially
settled by the respondent.
Claim No. CLI/2019/201114/0218563 – In this claim, claimed amount was Rs.1,02,590/-.
Bills submitted were for Rs.93,590/- against which respondent had settled amount of
Rs.92,763/- after deducting non payable items of Rs.827/- ( Rs.667/- for easy bath,
alcohol, swabs, bisleri, IV kit charges and other charges). As per SCN, bill of Rs.9,000/-
was not submitted but claimed towards hospital cash benefit. Hospital cash benefit is not
payable since patient was admitted in non preferred hospital as per coverage ‘M’ and not
occupied in sharing room as per coverage ‘N’. Hence settled and deducted amount is in
accordance with the policy.
CLI/2019/20114/0377700 - In this claim amount of Rs.3,71,228/- (Rs.2,91,537/- cashless
and Rs.79,691/- as reimbursement) was claimed. Cashless amount was approved fully. In
reimbursement claim respondent have received bills of Rs.67,570/- out of which they have
settled amount of Rs.54,507/- deducting non-payable items of Rs.13,063/- (Rs.650/-
nutritional charges; Rs.7,992/- glucotest, blood group others, gloves, bactoscrub, bactorub,
electrode, mask, alcohol swab, plain sheet, apron, sharp edge knife, betadine, bandage, Neb
mask, grilinctus, easy bath wipes, becosules, triptometer and Rs.4,421/- for EEG others
and rehabilitation). As per SCN, insured has claimed Rs.9,800/- towards hospital cash
benefit which is not payable as patient was admitted in respondent’s non preferred hospital
as per coverage ‘M’. In SCN respondent has specifically mentioned that the insured
occupied sharing room for 06 days hence as per coverage ‘N’, amount of Rs.4,800/- (6 x
Rs.800/-) can be considered more and they are ready to pay this amount to the insured.
Above deductions are as per policy terms and conditions. As respondent is ready to pay an
amount of Rs.4,800/- more to the insured for sharing room, hence complaint with respect
to this claim is liable to be partially allowed directing the respondent to pay amount of
Rs.4,800/-.
Complainant in his complaint has not disclosed why he should get amounts deducted by
respondent. During hearing, the representative of the complainant / insured was unable to
explain why deductions made by the respondent are not in accordance with the policy.
22. In view of above facts and circumstances, I come to the conclusion that the settlement of
claims and payable amount calculated by the respondent are in accordance with the terms
and conditions of the policy except amount of Rs.4,800/- in claim No.0377700 for which
respondent had agreed to pay. Respondent is directed to make payment of Rs.4,800/- under
Claim No.0377700 to the complainant within 30 days from the date of receipt of this
award.
23. The complaint filed by Mr Mukesh Wadhwani stands partially allowed as above.
24. Let copies of the order be given to both the parties.
Dated : Dec 24, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman

Mr. Dharam Das Israni….……………………………….…………..….. Complainant
V/S
The Oriental Insurance Co. Ltd
……………………………..…………..…..Respondent
COMPLAINT NO: BHP-H- 050-1920-0037 ORDER NO: IO/BHP/A/HI/0011/2019-2020
• Mr. Dharam Das Israni (Complainant) has filed a complaint against Oriental Insurance Co.
(Respondent) alleging less settlement and payment of claim.
• Brief facts of the Case - The complainant has stated that he had taken the above
Mediclaim policy No.151209/48/2019/311. A claim was lodged with the respondent/TPA
vide CCN371901973 in which amount of Rs.1,00,585/- was deducted. Then a Notice was
given vide dated 17.02.2019 but respondent had refused to pay the remaining amount. The
complainant has approached this forum for redressal of his grievance.
The respondent in their SCN dated 03.06.2019 have stated that complainant has
taken the above policy, lodged the claim for hospitalization at Bansal Hospital, Bhopal
from 20.12.2018 to 27.12.2018. The TPA settled the claim for Rs.33,008/- less Rs.3,301/- (
TDS Deduction ) = Rs.29,707/-. As per Medical Officer Review sheet Net Bill amount was
Rs. 1,45,367/- out of which Rs.1,00,585/- was deducted thereby Net Payable amount was
Rs.44,782/-. TPA Discount of Rs.11,774/- was deducted from net payable amount of
Rs.33,008/-. After deduction of TDS @ 10% amounting to Rs.3,301/- final amount comes
to Rs.29,707/-. Thus claim is settled as per medical Policy clause 1.2 Coverage of the
Policy. In SCN dated 20.12.2019 it is stated by the respondent that the insured /
complainant was admitted in Bansal Hospital from 20.12.2018 to 26.12.2018 and was
treated for Coronary Artery Disease with Acute Myocardial Infarction and insured is a
patient of Diabetes Melitus and Hypertension since 2003. Insured had taken his mediclaim
policy in 2015 for Rs.1 lac only which was subsequently renewed in the year 2016 for Rs.2
1.
Name & Address of the
Complainant
Mr. Dharam Das Israni,
Rajshree Saree Centre, Main Road,
Hirderam Nagar Market, Bhopal M.P-
2.
Policy No:
Type of Policy
Duration of policy/Policy period
152109/48/2019/311
Mediclaim Insurance Policy
09.07.18 to 08.07.19
3.
Name of the insured
Name of the policyholder
Mr. Dharam Das Israni
Mr. Dharam Das Israni
4.
Name of the insurer
The Oriental Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
--
7.
Date of receipt of the Complaint
10.05.2019
8.
Nature of complaint
Settlement of claim with partial amount
9.
Amount of Claim
Rs.1,00,585/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.1,00,585/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
24.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Deepak Janbandhu, Friend
For the insurer
Mr D N Dharade, Branch Manager
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
24.12.2019
lacs. Sum Assured in 2017 and in 2018 were Rs.2 lacs. Insureds disease is caused by
Diabetes Melitus and Hypertension which comes under pre existing disease which is
covered only after completion of 4 years without interruption. In this case, the disease
occurred in the fourth year and they have taken original sum assured as Rs.1 lac as per
policy condition 4 & 4.1. Insured has taken room as well as ICU in excess of his entitled
category i.e. room rent for Rs.1,000/- per day and ICU charges Rs.2,000/- per day. All
other expenses except pharmacy bill and body implants are reduced in the same proportion.
They further stated that in this claim they have allowed expenses as per insureds
entitlement and deducted amount in excess of his entitlement.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• A claim for Rs.1,45,367/- was lodged by the complainant, out of which amount of
Rs.44,782/- was allowed after deductions of Rs.1,00,585/-. As per SCN, TPA Discount of
Rs.11,774/- and TDS Rs.3,301/- @ 10% were deducted from amount of Rs.44,782/-. The
representative of the respondent has argued that the policy commenced from 09.07.2015 to
08.07.2016 for a SI of Rs.1 lac and in 2016-17 the SI was enhanced to Rs.2 lacs and in
subsequent years also the SI were Rs.2 lacs. He further argued that as the claim pertains to
treatment taken from 20.12.2018 to 26.12.2018 hence as per clause No.4.1 which is with
respect to pre-existing diseases, SI shall be taken into consideration as Rs.1 lac only
because 48 months has not elapsed on the date of treatment since year of enhancement of SI
under the policy. He further argued that the room category @ 1% and ICU charges @ 2%
were taken treating SI as Rs.1 lac and as the room category and ICU charges taken by the
insured were on the higher side, hence eligible room rent @ 1% and ICU charges @ 2%
were allowed. The representative of the complainant has opposed the above argument and
argued that calculation of charges of room category and ICU shall be taken treating Sum
assured as Rs.2 lacs i.e. complainant is entitled for room charges of Rs.2,000/- per day and
ICU charges @ Rs.4,000/- per day. In the policy effective from 09.07.2015 to 08.06.2016
SI was Rs.1 lac and SI was enhanced to Rs.2 lacs from 09.07.2016 to 08.06.2017 and
onwards. As per Clause 4.1 of policy, pre existing diseases shall be covered only after the
policy has been continuously in force for 48 months. As the SI was enhanced in 2016-17
hence SI for purpose of claim settlement shall be taken 48 months prior to the date of
treatment which was Rs.1 lac. In this case claim shall be settled treating SI as Rs.1 lac and
accordingly room rent and ICU charges shall be Rs.1,000/- per day and Rs.2,000/- per day
respectively. Above argument on behalf of complainant is not acceptable. Deductions made
in calculation sheet with respect to room rent and ICU charges are in accordance with
above charges which is in order. As per clause No.1.2 (A)(c&d) of policy terms and
conditions, Professional charges, OT, blood, O2, investigation and procedures shall be as
per limits of SI. Hence as per this clause amounts deducted under Professional charges, OT,
blood, O2, investigation and procedures are in order. Out of medical bill of Rs.27,622/-
amount of Rs.6,389/- was deducted on account of wipes, masks, gloves, tegaderm, strip,
electrode, cotton, adult diaper, micro tough gloves, jelly, oxyset, plastic apron and draw
sheet which are not payable as per policy, hence deductions under this head is also in order.

• In view of above facts and discussions, I come to the conclusion that the calculation of
deducted amount and paid amount is in accordance with the terms and conditions of the
policy. In the result, the complaint is liable to be dismissed.
• The complaint filed by Mr Dharam Das Israni stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 24, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance
Ombudsman
Mrs. Sheerin Alvi ..………….………………..………………….. …………Complainant
V/S
Liberty Videocon General Insurance. Ltd. ………….…..………..………......…Respondent
COMPLAINT NO: BHP-H-028-1920-0018 ORDER NO: IO/BHP/A/HI/ 0013 /2019-2020
• Mrs. Sheerin Alvi (Complainant) has filed a complaint against Liberty General Insurance
(Respondent) alleging cancellation of policy and refund of premium.
• Brief facts of the Case -The Complainant has stated that she had taken the above policy
on 10.07.2018. Due to financial problems she wrote a letter dated 22.01.2019 to the
Company to close the policy. She received a phone call from the Company but after that no
action was taken by the Company. She has approached this forum with request for closure
of the policy and refund of the amount by the Company.
The respondent in their SCN have stated that the above policy was issued on the
basis of proposal form filled in and submitted by the complainant for the period 10.07.2018
to 09.07.2019. On 24.01.2019 the respondent received a letter dated 22.01.2019 from the
complainant requesting for cancellation of the policy on the ground that in the month of
October she was admitted in hospital where upon she tried to contact the Company but
couldn’t contact and as such she wanted to cancel the policy. The respondent has stated
that in the policy all contact details are mentioned by the Company. On 24.01.2019 the
1.
Name & Address of the
Complainant
Mrs.Sheerin Alvi
Flat No. F-4, Apex Avenue Near Sulemani
School Rethgath Bhopal -462001
2.
Policy No:
Type of Policy
Duration of policy/Policy period
4216-200101-18-7003121-00-000
Health Connect Supra Policy
10.07.2018 to 09.07.2019
3.
Name of the insured
Name of the policyholder
Mrs. Sheerin Alvi
Mrs. Sheerin Alvi
4.
Name of the insurer
Liberty General Insurance
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
--
7.
Date of receipt of the Complaint
27.03.2019
8.
Nature of complaint
Cancellation of policy and & refund of
premium amount
9.
Amount of Claim
Rs.30,000/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.30,000/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 26.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mrs Sheerin Alvi
For the insurer
Mr Ritesh Singh, BM
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
26.12.2019

Company wrote email to the complainant stating that the Company tried to contact on
phone but was unable to establish contact. The Company wrote to the complainant to
provide the consent to cancel the policy vide ref no. 42162001011870031210000
informing that the policy will be cancelled with zero refund as per the policy terms and
conditions. Till date Company has not received the consent from the insured to proceed
with cancellation of the policy and also the original policy document submission. Policy
was effective from 10.07.2018 and complainant had requested for its cancellation on
22.01.2019 i.e. after expiry of 6 months from policy risk date. In view of the condition
No.14 governing the cancellation there is nil and or zero refund payable to the insured. As
such in absence of consent and non return of original policy documents company was
unable to cancel the policy.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
• Above Health Connect Supra Policy was issued from 10.07.2018 to 09.07.2019 to the
complainant and as per complainant she had requested the respondent on 22.01.2019 to
cancel the policy due to financial problems. Hence after taking of policy on 10.07.2018
complainant approached the respondent for cancellation of policy on 22.01.2019 i.e. after
six months. As per respondent they had sent a letter to the complainant referring clause
No.14 of policy which is with respect to cancellation and termination of policy, to
provide consent for cancellation of policy which was not sent by the complainant till date
and not complied with the requirements sought by the respondent. It is evident that the
complainant had not applied for free look cancellation within time and had not complied
with the requirements sought by the respondent for cancellation/termination of policy.
Hence respondent has acted in accordance with the terms and conditions of the policy. In
the result complaint is liable to be dismissed.
• The complaint filed by Mrs Sheerin Alvi stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 26, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance
Ombudsman
Mr.Vimal Garg .…………………..…..…………………..…………Complainant
V/S
The Oriental Insurance Co. Ltd…………..……………….………...………….Respondent
COMPLAINT NO: BHP-H-050-1920-0041 ORDER NO: IO/BHP/A/HI/ 0014 /2019-2020
1.
Name & Address of the
Complainant
Mr. Vimal Garg
D -1996 Sudama Garg,
Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
151200/48/2018/10061
PNB – ORIENTAL ROYAL MEDICALIM
20.10.2017 to 19.10.2018
3.
Name of the insured
Name of the policyholder
Mr. Vimal Garg
Mr. Vimal Garg
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation/ Rejection
--
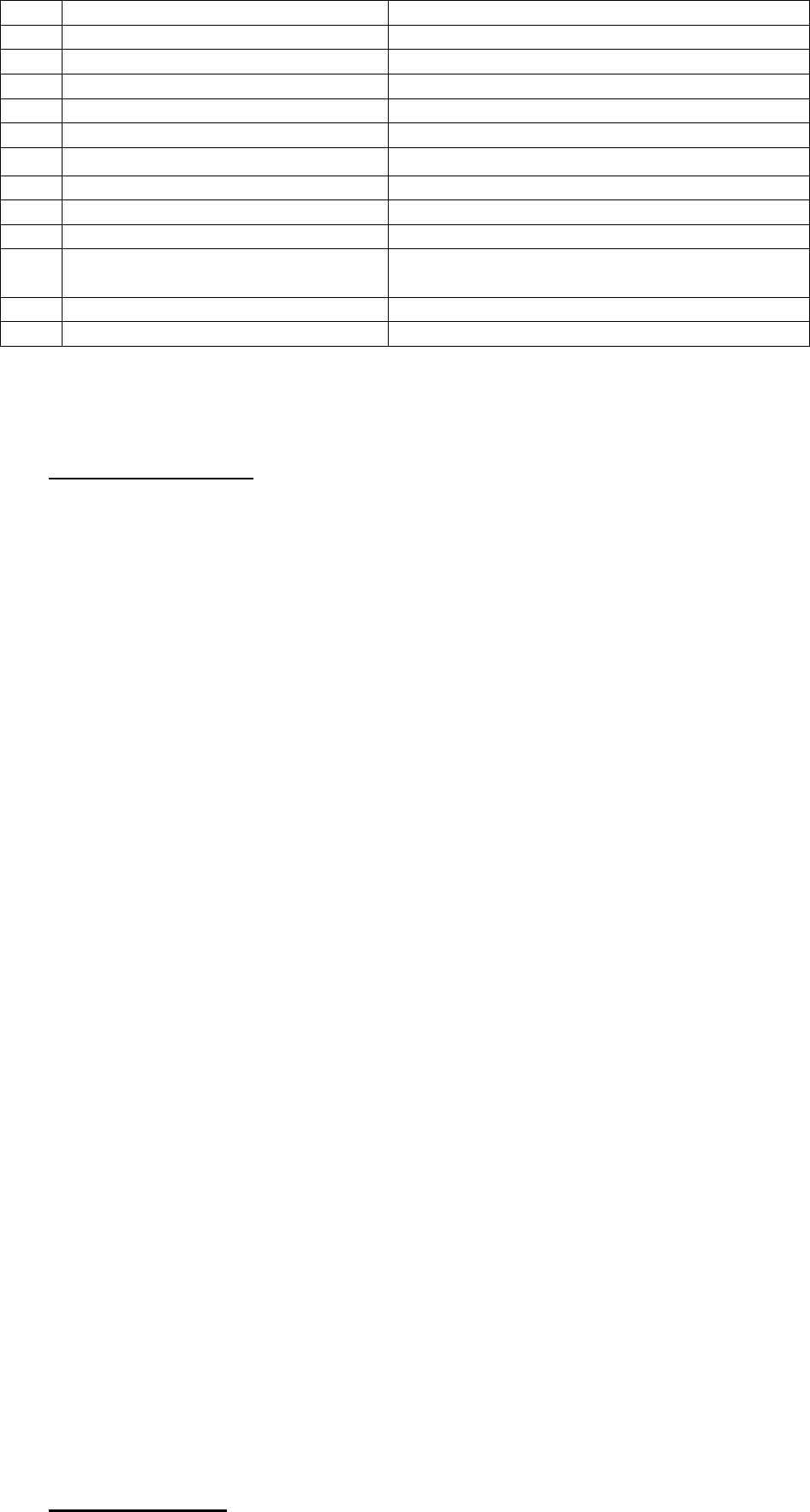
• Mr. Vimal Garg (Complainant) has filed a complaint against The Oriental Insurance Co.
Ltd. (Respondent) alleging less payment in two claims and rejecting one claim.
• Brief facts of the Case -The Complainant has stated that he had filed 3 claims in respect to
the treatment of his wife but respondent Company had not paid full claimed amount of
these claims. Number of claim numbers are 18465098, 17583235 and 18611098. Though
the complainant has written 3 letters dated 08.02.2019, 26.02.2019, 25.02.2019 but no
action has been taken by the Insurance Company
The respondent in their SCN have stated that the insured has filed claim number
18465098, 17583235 and 18611098. In claim no. 18465098, amount of claim is
Rs.1,26,101/- Company has repudiated the claim as the claim papers were submitted after
a period of 309 days, patient was discharged on 27.01.2018 and the documents were
submitted on 06.12.2018. As per policy condition 5.2 (v) claim documents in original
have to be submitted within 15 days from date of discharge. In claim no.17583235 for
claim amount of Rs.95,416/- an amount of Rs.60,730/- was paid after making the
deductions which are not admissible. Sum Insured under the policy is Rs.2,00,000/- hence
eligible to take room @ Rs.2,000/- per day and in ICU eligibility is Rs.4,000/- per day.
Since insured stayed in room higher than her entitlement accordingly the claim was settled.
Rs.15,103/- was deducted as excess of room rent eligibility, Rs.2,090/- as no reports,
Rs.250/- admission charges and Rs.17,243/- as the amount included in final bill claimed
twice including other non-payables. In claim No.18611098 as against claimed amount of
Rs.60,000/- an amount of Rs.20,792/- was paid after making deductions as per policy terms
and conditions. The claim is paid as per rates agreed with the hospital for treatment. Patient
was treated with chemo drugs and oral drugs and they have processed the claim for
radiation only rest of the treatment is not admissible under the policy and hence deducted
an amount of Rs.39,208/-.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
• Complainant had filed 3 claims, out of which claim No.18465098 was repudiated and other
two claims were partially settled.
Claim No.18465098 – Claim was filed for an amount of Rs.1,26,101/- which was
repudiated as per policy condition 5.2(v) on the ground that the complainant has submitted
6.
Reason for Repudiation/ Rejection
--
7.
Date of receipt of the Complaint
28.03.2019
8.
Nature of complaint
Less payment of mediclaims
9.
Amount of Claim
Rs.1,77,381/--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.1,77,381/--
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 24.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Vimal Garg
For the insurer
Mr Vimal Verma, Divisional Manager & Mr
A K Kotwani, Sr Branch Manager
15.
Complaint how disposed
Partially Allowed
16.
Date of Award/Order
26.12.2019

the claim documents on 06.12.2018 after a period of 309 days from the date of discharge
i.e. on 27.01.2018. Policy condition 5.8 states that final claim along with documents stated
in the policy should be submitted to the company / TPA within 15 days of discharge from
Hospital / Nursing Home. Respondent has argued that in this case insured was discharged
on 27.01.2018 and documents were submitted after a period of 309 days i.e. on 06.12.2018
which is a violation of above policy condition. No.5.8. During hearing complainant also
accepted that he had filed claim documents after a long period. As per policy condition
No.5.8 repudiation of claim is justified and is in accordance with the policy.
Claim No.17583235 – Under this claim, claimed amount was Rs.95,416/-, out of which
claim was settled for Rs.60,730/- deducting amount of Rs.34,686/- as non-payables. As per
SCN under hospital charges head bill was of Rs.35,963/-, out of which amount deducted
was Rs.15,103/-. Cause has been shown that room rent and ICU excess charges were
deducted. Sum Insured under this policy is Rs.2 lacs hence insured is eligible to take room
@ Rs.2,000/- per day and in ICU eligibility is of Rs.4,000/- per day. As per Sum Insured
and policy terms and conditions deductions under hospital charges are in consonance with
the policy. Under investigation and lab charges Rs.2,090/- was deducted because of no
reports of RBS, Xray chest and AVG. This deduction is also in order. Rs.250/- for
admission charges was not paid which is also in order. Amount of Rs.17,243/- under head
pharmacy and medicine charges were deducted out of which amount of Rs.15,173/- of
medicine bill was included in final bill and claimed twice. Amount with respect handrub
mouth wash, bath wipes, sheet, thermometer, gauge, Dettol, Urometer, tegaderm, gloves,
cotton, gamzeeroll, ECG electrodes were deducted as non payables. Deducted amount of
Rs.34,686/- (15,106+2090+250+17243)is as per policy terms and conditions. Hence,
settled and deducted amount shown in calculation is in accordance with policy terms and
conditions and in order.
Claim No.18611098 – Under this claim, claimed amount was Rs.60,000/-, out of which
amount of Rs.20,792/- was settled & paid after deducting Rs.39,208/-. In their SCN
respondent has mentioned that the claim is paid as per rates agreed with the hospital and
patient was treated with chemo and oral drugs for which they processed the claim for
radiation only. They have further mentioned that as rest of the treatment is not admissible
under the policy hence under head investigation and lab charges Rs.39,208/- was deducted.
Respondent in their letter dated 24.12.2019 has mentioned that the deductions were made
as insured had undergone 3 DCRT which is an advanced form of radio therapy and charges
were taken by the Hospital for this surgery and they allowed normal/prevailing charges for
this procedure. In this letter it is also mentioned that deductions were made as per Section 2
of policy conditions - coverage which states that the policy covers reasonable and
customary charges in respect of hospitalisation and/or domiciliary/hospitalisation for
medically necessary treatment only for illness/diseases. In SCN, respondent had nowhere
mentioned the bifurcation details under head investigation and lab charges. Cause of
deduction has been shown in SCN that they have processed the claim for radiation only
and rest of treatment is not admissible. No details of radiation and rest treatment charges
has been provided by the respondent. He could not show the policy condition under which
they have deducted rest treatment charges. During hearing representative of the respondent
has argued that as per Section 2 of policy condition they allowed normal prevailing charges

as the insured had undergone DCRT which is an advanced form of radiotherapy. During
hearing when representative was asked to show what are the normal/prevailing charges and
what are the charges for advanced radio therapy, he could not provide details of these. He
also could not explain whether the advanced radio therapy is covered or not under the
policy. Hence no justifiable reason could be given by the respondent for the deductions
made by them and which can be attributed to any of the policy condition.
• In view of above facts and circumstances, I come to the conclusion that the respondent
company could not show justifiable grounds for deduction of amount of Rs.39,208/- and
has erred in not allowing the full claimed amount under claim No.18611098. Therefore the
complaint with respect to Claim No.18611098 is liable to be allowed. Complaints with
respect to Claim Nos.18465095 and 17583235 stands dismissed.
• The complaint filed by Mr Vimal Garg is partially allowed and respondent is directed to
make payment of Rs.39,208/- under Claim No.18611098 to the complainant within 30
days from the date of receipt of this award.
• Let copies of the order be given to both the parties.
Dated : Dec 26, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
Mrs Rama Bhadoriya ..………….…………………..…..………………….. Complainant
V/S
Star Health & Allied Insurance Co.Ltd………………..………..………...…Respondent
COMPLAINT NO: BHP-H-044-1920-0017 ORDER NO: IO/BHP/A/HI/0015/2019-2020
• Mrs Rama Bhadoriya (Complainant) has filed a complaint against Star Health & Allied
Insurance Co.Ltd (Respondent) alleging rejection of claim.
• Brief facts of the Case -The complainant has stated she had taken the above policy and
was hospitalized for treatment of cold, cough and fever at Apple Hospital, Indore. She has
1.
Name & Address of the
Complainant
Mrs Rama Bhadoriya
1, Kaveri Nagar, Near Pandey Parisar
Sangam Nagar, INDORE
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/201114/01/2018/014117
Family Health Optima Insurance Plan
22.03.2018 to 21.03.2019
3.
Name of the insured
Name of the policyholder
Mrs Rama Bhadoriya
Mrs Rama Bhadoriya
4.
Name of the insurer
Star Health & Allied Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
08.12.2018
6.
Reason for Repudiation/ Rejection
Waiting period of 48 months for PED
7.
Date of receipt of the Complaint
25.04.2019
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.25,000/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 26.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mrs Rama Bhadoriya & Ms Divya
Bhadoriya, Daughter
For the insurer
Mr Ravi Tiwari, AGM Claims
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
26.12.2019

further stated that in the list of hospitals covered by respondent company under the policy,
the name of Apple Hospital was also included in the list but when she got admitted she
came to know that cashless facility was not available in the Hospital Thereafter she lodged
the bill for reimbursement of claim which was rejected for the reason that treatment is
related to Migraine. Then she represented to the Co. with Dr.’s certificate But respondent
did not settle the claim. So she has approached this forum for payment of her claim.
The respondent in their SCN have stated that the insured has taken the above policy
for self, spouse and children. The patient was hospitalized from 16.09.2018 to 19.09.2018,
diagnosed with Status Migranicus with 1st detected DMT2. She submitted the claim for
Rs.44,554/- in the sixth month of the policy. On scrutiny of the claim papers and as per
Field verification report, it is observed that insured patient is a known case of migraine for
last 1 year which is prior to inception of the policy and the present admission is also for
PED and therefore the claim was repudiated under waiting period clause 3(iii) of the
policy.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
• A claim for Rs.44,554/- was lodged by the complainant for the reimbursement of expenses
incurred in the treatment of insured / complainant taken at Apple Hospital, Indore from
16.09.2018 to 19.09.2018 which was repudiated by the respondent stating that the disease
of insured is pre existing and pre existing disease are not covered until 48 months of
continuous coverage. The representative of the respondent has argued that the insured is a
k/c/o of migraine since one year i.e. prior to the inception of policy. Discharge Summary of
Apple Hospital, Indore reveals that insured was admitted on 16.09.2018, discharged on
19.09.2018 and diagnosed with Status Migranicus with 1
st
time detected DM type II.
Admission history and physical assessment of Apple Hospital dated 16.09.2018 reveals
that insured is having a past history of hypertension since 5 years, migraine since one year
and piles since 5-6 years. Respondent’s PVR (PAN INDIA) is on record which is signed
by the Ms Divya Bhadoriya, daughter of the insured also shows that insured was having
migraine since one year back. Hence it is established that insured was suffering from
migraine prior to the inception of policy i.e. 22.03.2018. In proposal form also insured has
mentioned of having no chronic headache. As per policy condition 3(iii), waiting period for
pre-existing disease shall be 48 months since inception of the policy and pre-existing
disease shall be covered after 48 consecutive months of continuous coverage has elapsed
since inception of the policy. Hence as per above clause, respondent has rightly repudiated
the claim and acted in accordance with the terms and conditions of the policy. In the result
complaint is liable to be dismissed.
• The complaint filed by Mrs Rama Bhadoriya stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 26, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman

Mr. Prakash Agarwal ………….…………………..…..………………….. Complainant
V/S
National Insurance Company Limited ………………..………..………...…Respondent
COMPLAINT NO: BHP-H-048-1920-0016 ORDER NO: IO/BHP/A/HI/ 0016 /2019-2020
• Mr. Prakash Agarwal (Complainant) has filed a complaint against National Insurance
Company Limited (Respondent) alleging wrong repudiation of mediclaim.
• Brief facts of the Case -The complainant has stated that he was having diabetes problem
since last two years for which he was taking treatment from Dr.Prakhar Agarwal, M.D.
on regular basis. In July 2018 he noticed pain in both legs and thereafter acute pain in
August first week for which he consulted Dr.Agarwal who advised Sonography. It was
diagnosed that there is flow occluded in interior and posterior tibial artery and
dorsalispedis artery. On the advice of Dr.Agarwal, he consulted Dr.Tarun Gandhi of CHL
Hospital advised Angioplasty of veins of both legs. So he got admitted in Lilavati
Hospital, Mumbai where Angioplasty of both veins were done on 01.09.2018. Thereafter
he lodged claim for Rs.3,42,748/- with the respondent company. But the same was
repudiated by respondent company stating that disease is due to smoking and intoxicating
substance is not payable under policy exclusion No.4.11. He then submitted his point
wise representation to respondent company and has not got any reply so far. The
complainant has approached this forum for redressal of his grievance.
The respondent in their SCN have stated that the above policy was issued to the
complainant for the period 18.03.2018 to 17.03.2019. Complainant was diagnosed to
have peripheral vascular disease and was admitted in Lilavati Hospital, Mumbai from
31.08.2018 to 03.09.2018. CT Angiography was done which showed occlusion of Rt
SFA and Lt lilac and SFA Stenosis peripheral angioplasty was done. As insured is a
chronic smoker, claim was repudiated under clause 4.11. Opinion of Dr K G Agarwal
was also obtained in the matter and in his report also it is mentioned that tobacco contains
1.
Name & Address of the
Complainant
Mr. Prakash Agarwal
121,Ambedkar Nagar,MHOW
2.
Policy No:
Type of Policy
Duration of policy/Policy period
321104501710000268
BOI National Swasthya Bima Policy
18.03.2018 to 17.03.2019
3.
Name of the insured
Name of the policyholder
Mr.Prakash Agarwal
Mr. Prakash Agarwal
4.
Name of the insurer
National Insurance Company Limited
5.
Date of Repudiation/ Rejection
13.11.2018
6.
Reason for Repudiation/ Rejection
Not payable under Exclusion Clause No.4.11
7.
Date of receipt of the Complaint
25.04.2019
8.
Nature of complaint
Wrong repudiation of mediclaim
9.
Amount of Claim
Rs.3,42,748/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.3,42,748/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
On 26.12.2019 at Bhopal
14.
Representation at the hearing
For the Complainant
Mr Prakash Agarwal
For the insurer
Mr Shailendra Joshi, Sr DM
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
26.12.2019

nicotine which is intoxicating substance and causes narrowing of peripheral blood
vessels.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant
as well as the Insurance Company.
• A claim for Rs.3,42,748/- under above policy was lodged by the complainant for the
reimbursement of expenses incurred in the treatment taken at Lilavati Hospital, Mumbai
from 31.08.2018 to 03.09.2018 which was repudiated by the respondent on 13.11.2018
stating that peripheral vascular disease is due to smoking only and as per policy terms
and conditions 4.11 disease originating due to intoxicating substance is not payable.
Discharge Summary of Lilavati Hospital, Mumbai reveals that the complainant was
admitted on 31.08.2018, discharged on 03.09.2018 and diagnosed with Peripheral
vascular disease. The representative of the respondent has argued that the disease of
insured was due to smoking and by smoking nicotine is inhaled which leads to
development of peripheral vascular disease. The representative of respondent has referred
to prescriptions of Medanta Super Specialty Hospital, Indore and Dr Tarun D Gandhi
dated 25.08.2018 and 28.08.2018. In prescription dated 25.08.2018 of Medanta Hospital,
Indore and 28.08.2018 of Dr Tarun Gandhi, it is mentioned that the insured is taking one
bundle beedi daily and is a smoker. Complainant has opposed the argument of the
respondent and argued that he never smokes. Above prescriptions clearly reveals that
insured is a smoker. As per medical information available at Google, Nicotine is found in
tobacco plants and one of the causes of peripheral vascular disease is smoking. As per
medical information, peripheral vascular disease is a blood circulation disorder and
typically causes pain and fatigue, often in legs in which blood vessels become narrowed
and blood flow decreases. As per complainant, flow occluded in interior and posterior
tibial artery and dorsalispedis artery. Report of Dr K G Agarwal is on file in which
Doctor has opined that tobacco contains Nicotine which is intoxicating substance and
causes narrowing of peripheral blood vessels. Clause 4.11 of policy terms and conditions
states that the company shall not be liable to make any payment in respect of treatment
arising out of illness / disease / injury due to misuse or abuse of drugs / alcohol or use of
intoxicating substances. It is established by prescriptions that insured is a smoker and
smokes one bundle beedi daily in which tobacco is filled up and tobacco contains
nicotine which is an intoxicating substance. Hence as per above clause respondent has
rightly repudiated the claim and acted in accordance with the terms and conditions of the
policy. In the result complaint is liable to be dismissed.
• The complaint filed by Mr Prakash Agarwal stands dismissed herewith.
• Let copies of the order be given to both the parties.
Dated: Dec 26, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman

Mr. Jitendra Silwadiya..…………………..…..………………….. Complainant
V/S
Royal Sundaram General Insurance Co.Ltd………………..………..………...…Respondent
COMPLAINT NO: BHP-H-038-1920-0007 ORDER NO: IO/BHP/A/HI/0009/2019-2020
• Mr. Jitendra Silwadiya (Complainant) has filed a complaint against Royal Sundaram
General Insurance Co.Ltd (Respondent) alleging repudiation of claim.
• Brief facts of the Case -The complainant has stated that he and his family members were
covered under above mediclaim policy issued by the respondent. His wife was admitted in
Gaurav Hospital, Indore from 07.12.2018 to 12.12.2018 for UTI with viral fever.
Complainant preferred claim before respondent company on 19.12.2018. The case was
investigated on 21.01.2019 and respondent vide letter dated 31.01.2019 rejected the claim
stating mis-description / fraud / non-disclosure of facts / mis-representation. The
complainant has approached this forum for payment of his claim.
The respondent in their SCN have stated that above Family Health Floater policy was
issued to complainant for the period 15.08.2018 to 14.08.2019. Complainant preferred
claim for reimbursement of expenses incurred in the treatment of his wife at Gaurav
Hospital for Urinary Tract Infection for the period 07.12.2018 to 12.12.2018. Scrutiny of
the claim documents revealed gross discrepancies. Hospitalisation appears to be prolonged
as indoor records indicate only a conservative line of treatment. Further investigation
revealed that TPR chart of the insured was stable and yet the patient was admitted for 6
days and there was no record of any notes maintained by visiting doctor, Dr Aparna Jain.
Insured had undergone CBC and urine test which showed WBC-13500 and 9-10 pus cells
in urine but no repeat test / investigation had been done for comparison. It was also found
that ICP seemed to be written in a single stretch and the treating doctor failed to cooperate
with our investigator. It is therefore evident that hospitalization appears to be managed for
1.
Name & Address of the
Complainant
Mr. Jitendra Silwadiya
361, Village Datoda
District Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
HSAA1554223000100
Family Health Floater policy
15.08.2018 to 14.08.2019
3.
Name of the insured
Name of the policyholder
Mrs. Aarti Silwadiya & 2 others
Mr. Jitendra Silwadiya
4.
Name of the insurer
Royal Sundaram General Insurance Co. Ltd
5.
Date of Repudiation/ Rejection
31.01.2019
6.
Reason for Repudiation/ Rejection
Gross discrepancies and exaggerated costs in
bill to make unlawful gain
7.
Date of receipt of the Complaint
05.04.2019
8.
Nature of complaint
Repudiation of mediclaim
9.
Amount of Claim
Rs.57,000/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.93,940/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
13.12.2019 at Bhopal
14.
Representation at the hearing
uuuu) For the Complainant
Mr Jitendra Silwadiya
vvvv) For the insurer
Mr Amit Upadhyay, Asstt Manager
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
20.12.2019
the purpose of claiming benefit and for making unlawful gains from the policy which
tantamounts to mis-description.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant as
well as the Insurance Company.
• A claim under above policy was filed for the reimbursement of expenses incurred in the
treatment of insured / wife of complainant taken at Gaurav Hospital, Indore from
07.12.2018 to 12.12.2018 which was repudiated by the respondent on the ground of gross
discrepancies, stay unduly prolonged and charges grossly exaggerated to derive undue
benefit. Discharge summary of Gaurav Hospital, Indore shows that insured was admitted
on 07.12.2018, discharged on 12.12.2018 and diagnosed with UTI along with viral fever.
The representative of the respondent has argued that hospitalisation appears to be
prolonged as the indoor records indicate only a conservative line of treatment. He further
argued that temperature, pulse and respiration chart of insured was stable and yet the
patient / insured was admitted for 6 days. In Discharge Summary it is mentioned that the
insured was treated with IV fluids and intravenous injections. Doctors Order Sheets dated
07.12.2018 to 11.12.2018 reveals that the insured was administered with IV NS, DNS,
Oframax Fort, Pentocid, HV Mol, Zofer, Loxof during these period. Doctors sheet dated
12.12.2018 also shows that insured was advised for follow up after 5 days. Hence medical
record reveals that the insured during hospitalisation was not treated conservatively but
administered IV fluids and injections, etc. Remaining stable in pulse, temperature and
respiration does not mean that insured did not require to remain in hospital. It is for the
Doctor to decide the discharge from hospital. Representative of the respondent has also
argued that no repeat tests/ investigation or WBC and urine pus cells were conducted. This
also can be decided only by the Treating Doctor and in absence of repeated investigations
it cannot be inferred that the hospitalisation was not required. Hence repudiation on the
ground that the hospitalisation was prolonged is not acceptable. It is argued on behalf of
respondent that no record of visiting Doctor (Dr Aparna Jain) were maintained. This
cannot be a ground for the repudiation of the whole of the claim. It is also argued that
indoor case papers seems to be written in a single stretch. No evidence in respect of this
argument has been filed by the respondent. Besides this, this can also not be ground of
rejection of claim. In repudiation it is mentioned by the respondent that the charges are also
exaggerated to derive undue benefit. In their SCN respondent has not pleaded with respect
to exaggeration of charges. Respondent has also not specified which charges are
exaggerated and for the sake of argument if some charges are exaggerated according to
them, then it could be seen while processing of the claim instead of rejection of whole
claim. Hence, grounds of repudiation are not such that the whole claim is repudiated.
• In view of above facts and circumstances, I come to the conclusion that the respondent has
erred by rejecting the claim. In the result, complaint is liable to be allowed.
• The complaint filed by Mr Jitendra Silwadiya is allowed and respondent is directed to
allow the claim as per terms and conditions of the policy within 30 days of receipt of this
award.

• Let copies of the order be given to both the parties.
Dated: Dec 20, 2019 (G.S.Shrivastava)
Place : Bhopal Insurance Ombudsman
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- NEERJA SHAH
In the matter of: SMT. SUSHMA D.R V/s RELIGARE HEALTH INSURANCE COMPANY LIMITED
Complaint No: BNG-H-037-1920-0322
Award No: IO/BNG/A/HI/229/2019-20
• The Complaint emanated from the rejection of claim under policy number 14112228 CARE
Individual Plan valid for the period 27.04.2019 to 26.04.2020
• The Complainant’s submitted that the RI had rejected the claim amounts of ₹.49313/- towards
hospitalization, Pre &Post hospitalization for the period 06.08.2019 to 06.08.2019 diagnosed as
Metastatic Carcinoma Lung under evaluation admitted for Biopsy. The claim was registered with
Claim ID No.91073645. Representation with RI could not be resolved
• Aggrieved with the rejection of settlement of the claims, the Complainant approached this
Forum and the complaint was posted for personal hearing on 12.12.2019.
• RI did not submit SCN. Before the hearing date vide mail dt.11.12.2019 RI submitted that they
reopened the Case and initiated process of payment of Rs.48,188/- after deducting non medical
charges to the tune of Rs.1125/- . It was informed to Forum that they tried to contact
complainant but were unable to reach. Forum forwarded mail communication to the
complainant for their consent to RI & Forum.
• Complainant gave consent as agreed with the full and final settlement and requested the Forum
to close the complaint. After the consent from the complainant , RI made the payment of
Rs.40,585/- on 11.12.2019 with respect to claim No.91073645 and communicated vide mail
dt.12.12.2019 that remaining payment of Rs.7603/- towards pre & post hospitalization under
claim No. 91073645-01 & 02 for Rs.900/- and Rs.6703/- respectively are under process.
• RI settled the amount of Rs.7603/- through NEFT on 12.12.2019.
• The complainant confirmed receipts of the claim amount vide mail dt.13.12.2019 and has
requested for Closure of the Complaint.
• The complaint was resolved on compromise basis wherein both have agreed for the same and
hence, the Complaint is treated as Closed and Disposed off accordingly.
Dated at Bengaluru on the 16th day of December 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of MR. S SANDEEP Vs STAR HEALTH & ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-289
Award No.: IO/(BNG)/A/HI/0215/2019-20
1
Name & Address of the
Complainant
Mr. S Sandeep
No.152, 1
st
floor, 9
th
main, 4
th
Block,
Opp. Satya Shaneshwara Temple Arc,
Nandini Layout, Bangalore 560096
Ph. 8105109103
2
Policy Number
Type of Policy
Duration of Policy/ Policy
Period
P/141137/01/2019/006071
Family Health Optima Insurance Plan
21.12.2018 to 20.12.2019
3
Name of the Insured/
Mr. Sandeep S

Proposer
Name of the policyholder
4
Name of the Respondent
Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
15.07.2019
6
Reason for repudiation
Rejection of claim for non-disclosure of
PED
7
Date of receipt of Annexure
VI-A
08.11.2019
8
Nature of complaint
Repudiation of claim
9
Amount of claim
₹. 2,00,000/-
10
Date of Partial Settlement
Not Applicable
11
Amount of relief sought
₹. 2,00,000/-
12
Complaint registered under
Rule no:
13 (1) (d) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
05.12.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
1. Mr. Mahadevan, Sr.Consultant
2. Dr.Umadevi, Sr. Manager
15
Complaint how disposed
Disallowed
16
Date of Award/Order
09.12.2019
17. Brief Facts of the Case:
The complaint emanated from the rejection of the claim and cancellation of coverage for his father Mr.
Shankar Narayana on the grounds of non-disclosure of pre-existing disease.
18. Cause of Complaint:
a) Complainant’s arguments:
complainant submitted that they took policy during 2016 and have been continuously renewing without
break paying premium without claiming any amount. The condition mentioned by the Star Health in
their repudiation letter is not as pre existing disease as evident from Doctor’s Certificate dated
11.07.2019. The disease for which the insured person is diagnosed is not related to pre existing disease.
Besides he was not undergoing any treatment or taking any kind of medication. This proves that insured
person was not suffering from any pre existing disease at the inception of the first policy and they have
never hidden material facts for the queries raised by Star Health. He requested for settlement of claim
and continuance of the policy for upcoming years.
b) Respondent Insurer’s Arguments:
The Respondent Insurer in their Self Contained Note (SCN) dated 24/11/2019 submitted that the insured
person had undergone treatment for AVM prior to policy inception which is evident through
Dr.Raghuram’s certificate dated 11/07/2019, discharge summary dated 11/07/2019 and ICP dated
03/07/2019 and also evident from the progress note that the insured had post traumatic
intraventricular bleed since 2015.
It is the duty of the insured to disclose all the material facts to the insurer to enable them to evaluate
the proposal . Insurance contract is based on utmost good faith. However the above medical condition
was not disclosed in the proposal form submitted which amounted to non-disclosure of material fact
making the contract of insurance voidable as confirmed by Supreme Court in Swatwant Kaur Sandhu vs.
New India Assurance Co. Ltd., (2009) 8 SEC 316 (citation).
Hence, the claim was repudiated invoking condition no. 6 of the policy, ‘the company shall not be liable
to make any payment under the policy in respect of any claim if information furnished at the time of
proposal is found to be incorrect or false or such claim is in any manner fraudulent or supported by any
fraudlent means or device, misrepresentation whether by the insured person or by any other person
acting on his behalf.
They cancelled the Policy on 24.08.2019 by sending 30 days time notice on 15.07.2019 by invoking
condition no. 12 of the policy, ‘’the company may cancel this policy on grounds of misrepresentation,
fraud, moral hazard, non-disclosure of material fact as declared in the proposal form/at the time of claim
or non-co-operation of the insured person’’. Hence the policy was cancelled due to non disclosure of PED
Non Traumatic Intracerebral Hemorrhage.
Respondent Insurer requested to absolve them from the complaint made.

19. Reason for Registration of complaint:-
The complaint was registered as it falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A.
21. Result of personal hearing with both the parties (Observations & Conclusions):
The issues which require consideration is whether the action of the R I to repudiate the claim and cancel
the policy on the grounds of non disclosure of pre existing disease in the proposal form is in order.
21.1. During the personal hearing, both the parties reiterated their earlier submissions.
21.2. The insured has reported the claim in the 3
rd
year of the Medical insurance Policy.
21.3 Forum finds that the insured person was admitted to Colombia Asia on 03.07.2019 and discharged
on 11.07.2019. His admission diagnosis and discharge diagnosis was “Nontraumatic intracerebral
Hemorrhage”. Significant post medical and surgical history in the discharge summary reveals that he
was diagnosed to have AVM in 2015 and completely cured – not on any medication.
21.4 Certificate dated 11.07.2019 produced by the complainant in his support from consultant
neurosurgeon states interalia that the insured person was diagnosed with AVM in April 2015. He was
treated for the same and was cured completely without any signs and symptoms in the last four
years….He has not been taking any medications related to his previous ailment…….
21.5 Perusal of the proposal form dated 07.12.2016 reveals that to the query “Have you
consulted/taken treatment/been admitted for any illness/disease/injury/surgery. If yes, details”, the
complainant stated “NO”. Since the insured person was diagnosed with AVM in April 2015, the
complainant was required to mention the same in the Proposal Form. Non disclosure of pre existing
disease result in breach of insurance principle of utmost good faith.
21.6 On the basis of the above facts the Forum does not find any reason to interfere with the decision of
R I.
21.7. Reliance is placed on the Supreme Court’s decisions in the case of Satwant Kaur Sandhu vs The
New India Assurance Company Limited dated 10.07.2009 and LIC of India vs. Manish Gupta dated
15.04.2019 to arrive at this decision.
Hence the rejection of claim by RI is in order.
A W A R D
Taking into account of the facts and circumstances of the case and the submissions made
by both the parties and documents submitted during the course of the Personal Hearing,
the rejection of the claim by the Respondent Insurer is in order and in consonance with
the terms and conditions of the policy which does not require any interference at the
hands of the Ombudsman.
The Complaint is Disallowed.
Dated at Bangalore on the 9
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of Shri S.V.Phaneesha V/s RELIGARE HEALTH INSURANCE COMPANY LIMITED
Complaint No: BNG-H-037-1920-0242
Award No. : IO/(BNG)/A/HI/0198/2019-20
1
Name & Address of the
Complainant
Shri S.V.Phaneesha
201, Arya Heights Apartments,
Opp. Thalaghattapura Police Station,
Kanakapura Main Road,
BENGALURU – 560 109
Mob.No. 9940069408
E Mail ID : svphan[email protected]om
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
11581988
Religare Health Insurance - Care Floater
Individual
12.09.2018 to 11.09.2019
3
Name of the Insured/
Proposer
Name of the policyholder
Smt.M.G.Vijaya
Shri S.V.Phaneesha
4
Name of the Respondent
Insurer
Religare Health Insurance Company
limited
5
Date of repudiation/rejection
1
st
Claim -19.04.2019
2
nd
claim – 06.07.2019
3
rd
claim- 08.07.2019
6
Reason for repudiation
1
st
claim- Does not warrant
Hospitalization . Admission not justified.
2
nd
claim- Admission for evaluation
/diagnostic purpose is permanent
exclusion.
3
rd
claim- Ailment falls under specific
waiting period of 24 months.
7
Date of receipt of the
Annexure VI-A
09.09.2019
8
Nature of complaint
Denial of Claim
9
Amount of claim
₹.2,20,728/-
10
Date of Partial Settlement
N.A.
11
Amount of relief sought
₹.2,20,728/-
12
Complaint registered under
Rule no:
13 (1)(b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
21.11.2019 / Bengaluru
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
Dr .Channakeshava Prasad (Zonal
Manager)
Dr.Bharateesh Patwari (FCU Manager )
15
Complaint how disposed
Partially allowed
16
Date of Award/Order
03.12.2019
17. Brief Facts of the Case:
The Complaint emanated from the rejection of 3 No. of claims for hospitalisation :
1. 1
st
claim –for the period from 04.04.2019 to 07.04.2019.
2. 2
nd
claim – for the period from 05.07.2019 to 06.07.2019.
3. 3
rd
claim- for the period from 09.07.2019 to 13.07.2019.
Inspite of taking up the complaint with the GRO of the Respondent Insurer (RI), the same was
not resolved and hence, the Complainant has approached this Forum.
18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant along with his wife and 2 sons were insured with the RI from 12.09.2017 to 11.09.18
and renewed for the period 12.09.2018 to 11.09.2019 under Health Insurance policy No. 11581988. He
submitted 3 No. of claims during the policy period.
Claim No.1 : Complainant’s wife was suffering from continuous vomiting and persistent nausea,
decrease oral intake, generalized weakness and low back ache with increased frequency of
micturition since 28.01.2019 . She has been given OPD treatment by Dr.Chidanand of Ananya

Hospital. Since there was no improvement she was admitted to Ananya Hospital, Bengaluru for
the period from 04.04.2019 to 07.04.2019. As the hospital has no tie up with Religare Health
Insurance he submitted bill for reimbursement of Rs.29,880/-
Claim was rejected on 19.04.2019 by R.I on the grounds that treatment can be managed on
OPD basis without hospitalization and admission was not justified. He took up the matter with
customer care and was told to submit justification for hospitalization from the hospital . He
submitted letter dt. 20.04.2019 issued form Ananya Hospital justifying her hospitalization. As
there was no response he escalated matter to Grievance help desk. He was asked to submit
indoor case papers from the hospital. He submitted the same on 12.07.2019. Still his claim was
not reconsidered.
Claim No.2: Complainants wife was hospitalized in Vasavi Hospital for the period from
05.07.2019 to 06.07.2019 . Cashless claim was repudiated on 06.07.2019 on the ground,
admission for evaluation /diagnostic purpose is not covered .There is no indication for
hospitalization.
Claim No.3: His wife was admitted to Vasavi Hospital for the period from 09.07.2019 to
13.07.2019 to undergo Laproscopic surgery due to further deterioration in her health. Cashless
claim was repudiated on 08.07.2019 on the ground , treatment falls under specific waiting
period of 24 months.
In spite of representation to RI, the above were not considered. Hence, he has approached this Forum.
b) Respondent Insurer’s Arguments:
The Respondent Insurer submitted their Self Contained Note dated 20.09.2019 admitting insurance
coverage, preferring 3 No. of claims during the policy period.
Claim No.1: RI reiterate that on perusal of the documents received for reimbursement it came to
forefront that IP was admitted for investigation and evaluation. IP underwent various investigations and
evaluations . She was treated with IV Fluids and Antibiotic Injections which can be managed on OPD
basis.
Her claim is rejected as per policy terms & conditions clause 4.2 (1) read with Annexure-II(71) which is
reproduced herein:
4.2 Permanent Exclusions:
The following list of permanent exclusions is applicable to all the benefits and optional covers. Any claim
in respect of any of the insured person for, arising out of or directly due to any of the following shall not
be admissible unless expressly stated to the contrary elsewhere in the policy terms and conditions.
(1) Any item or condition or treatment specified in List of Non-medical items(Annexure-II) to the
Policy terms and conditions.
(71)-Hospitalization for evaluation/diagnostic purpose.
Claim No.2: RI resubmit that complainant approached for cashless facility request for the planned
hospitalization of IP at Vasavi Hospital on 05.07.2019 . It was found from the medical records that IP
was admitted and was diagnosed with Lower Back pain & UTI. She was admitted for further evaluation
and Investigation. RI reiterate that as per Doctor’s Assessment on admission report dt.05.07.19 it is
found that IP was admitted for evaluation from Orthopaedic and Gynaecologist. She was administered
with only IV injections and oral medicines. No active line of treatment was given .
Her claim cannot be considered as per policy terms & condition clause 4.2(1) read with Annexure –
II(71).
Claim No.3 : R.I submits that complainant approached for cashless facility request for the planned
hospitalization of IP at Vasavi Hospital on 09.07.2019. She was provisionally diagnosed with
Cholelithiasis, right adnexal cyst excision. Her admission was for Laparoscopic Cholecystectomy and
Right Adnexal mass Excision.
R.I reiterate that claim related to kidney stone/ureteric stone/Lithotripsy/Gall Blader stone are covered
only after 24 months of continuous policy coverage. IP’s claim falls under this category. Her policy
inception period was 12.09.2017 to 11.09.2018 . Claim is under 2
nd
year policy period i.e. 12.09.18 to
11.09.19.
In view of which her claim is rejected as per policy terms and conditions relevant clause which is
reproduced hereunder :
4.1 Waiting Periods:
(ii) Specific Waiting period: Any claim for or arising out of any of the following illness orSurgical
procedures shall not be admissible during the first 24(Twenty Four) consecutive month of coverage of the
insured person by the company from the first policy period start date:
11. Kidney stone/ureteric stone/Lithotripsy/Gall Blader stone.
19. Reason for Registration of complaint:
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017 and so it was registered.

20. The following documents were placed for perusal:
d. Complaint along with enclosures,
e. Respondent Insurer’s SCN along with enclosures and
f. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is as to whether treatment is payable as per policy terms and conditions .
The Forum has perused the documentary evidence available on record and the submissions made by
both the parties during the personal hearing.
Claim No. 1 : The Complainant reiterated his contentions IP was suffering with the complaint since
January 2019 . She was treated in OPD . As there was no improvement it was medically necessitated to
admit her to the hospital.
The RI reiterated their contentions in SCN and stated IP underwent various investigations and
evaluations . She was treated with IV Fluids and Antibiotic Injections which can be managed on OPD
basis.
The Forum found from the hospital records that she was treated for three days . Investigations are
medically necessary and relevant to her treatment as certified by the treating doctor of Ananya Hospital.
Forum does not concur with the decision of the Respondent Insurer in rejecting the claim.
Forum directs the RI to settle the same as per the terms and conditions of policy with interest.
Claim No.1 is allowed.
Claim No.2: The Complainant reiterated his contentions, IP continued to suffer even after her discharge
from first hospitalization. As per Dr.’s advice she was admitted for treatment & investigations.
The RI reiterated their contentions in SCN and stated IP she was administered with only IV injections and
oral medicines. She was admitted for further evaluation and Investigation. No active line of treatment
was given.
The Forum found from the hospital records that she was admitted for one day . Under the column
Courses in the hospital it is mentioned ‘out patient USG shows ‘Right Adnexal Complex cyst, Fatty liver,
Cholelithiasis. Advised for Laparoscopic ovarian cystectomy.
It shows admission is done only for evaluation & investigation.
Forum concurs with the decision of the Respondent Insurer in rejecting the claim.
Accordingly, Claim No.2 is dismissed.
Claim No.3 : The Complainant reiterated his contentions as per Dr’s advice which is stated in the earlier
discharge summary it was planned to undergo Laparoscopic Cholecystectomy and Right Ovarian
Cystectomy for IP .Hence cashless request was submitted. RI rejected the claim.
The RI reiterated their contentions in SCN that IP is covered since 12.09.2017 to 11.09.2018 . Renewed
for 2
nd
year policy period i.e. 12.09.18 to 11.09.19. Her admission was for Laparoscopic
Cholecystectomy and Right Adnexal mass Excision. Though the admission falls under current policy
period , as per Clause 4.1 Waiting Periods of policy condition, the said treatment falls under waiting
period of 24 months. Hence, IP is not entitled for claim.
The Forum found as per the hospital records IP’s Diagnosis is Cholelithaisis, Right ovarian. Procedure
done shows as Laparpscopic Cholecystectomy and Right Ovarian Cystectomy under General Anaesthesia
on 10.07.2019.
The said treatment falls under Waiting period of 24 months as per policy terms & condition.
Forum concur with the decision of the Respondent Insurer in rejecting the claim.
Accordingly, Claim No.3 is Dismissed
The Complaint is Partially Allowed
A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral
submissions made by the RI, this Forum is of the opinion that the decision of the Respondent
Insurer in respect of:
Claim No.1: is not in accordance with the terms and conditions of policy and not found to be in
order.
Claim No.2 and 3: Forum does not find any flaw with the decision of Respondent Insurer in
rejecting the claim amount .

This Forum directs the Respondent Insurer to settle the Claim No.1 as per the terms and
conditions of policy along with interest @ 6.25% + 2% from the date of receipt of last necessary
documents to the date of payment of claim, as per regulation 16 (1) (ii) of Protection of Policy
holders’ Interests Regulations, 2017 issued by IRDAI vide notification dated 22.06.2017 and to
extend the continuity benefits under the policy.
Hence, the complaint is PARTIALLY ALLOWED.
22. Compliance of Award: The attention of the Complainant and the Respondent Insurer is hereby
invited to Rule 17(6) of the Insurance Ombudsman Rules, 2017, where under the Respondent Insurer
shall comply with the Award within 30 days of the receipt of the Award and shall intimate compliance of
the same to the Ombudsman.
Dated at Bengaluru on the 3
rd
day of December 2019.
( NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
Case of: MR. DINYAR R PATELL V/s STAR HEALTH AND ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-309
Award No.: IO/(BNG)/A/HI/217/2019-20
1
Name & Address of the
Complainant
Mr. Dinyar R Patell
Cytadel, 853, 4
th
Main
12
th
Cross, 1
st
Stage,
Indira nagar,
Bangalore – 560038
Ph.9986659952
Email: dinyarpat[email protected]
2
Policy Number
Type of Policy
Duration of Policy/ Policy
Period
P/141125/01/2019/018872
Senior Citizen Red Carpet Health Insurance
16.02.2019 to 05.02.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Mr. Dinyar R Patell
4
Name of the Respondent
Insurer
Star Health and Allied Insurance co. Ltd.
5
Date of repudiation
NA
6
Reason for repudiation
NA
7
Date of receipt of Annexure
VI-A
06.11.2019
8
Nature of complaint
Short settlement of claim amount
9
Amount of claim
Rs.1,05,851/-
10
Date of Partial Settlement
12.06.2019
11
Amount of relief sought
Rs.1,05,851/-
12
Complaint registered under
Rule no:
13 (1) (d) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
05.12.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
1. Mr. Mahadevan, Sr.Consultant
2. Dr.Umadevi, Sr. Manager
15
Complaint how disposed
Partially Allowed

16
Date of Award/Order
09.12.2019
17. Brief Facts of the Case:
The complaint emanated from the short settlement on the ground of short payment of claimed amount.
Despite taking up the matter with the GRO of Respondent Insurer (RI) against the short settlement of
claim, the same was not considered and hence, he has approached this Forum.
18. Cause of Complaint:
a) Complainant’s Arguments:
1) He has obtained Senior Citizen Red Carpet Health Insurance Policy covering himself and his wife
from 16/02/2019 to 15/02/2020 by paying a renewal premium of Rs.53,100/-. His policy incepted
from 05/03/2012. and renewed continuously without any break. He was admitted to St.
Philomena’s Hospital, Bangalore on 03.06.2019 and was discharged on 11.06.2019 for the treatment
of Pituitary Macrodenoma. Out of the total bill of Rs.2,44,506/- R I has reimbursed only an amount
of Rs.1,48,504/-. He was required to bear only 30% of Co-Pay but has incurred more than required
30%. He has not been reimbursed for certain surgical investigations, attender’s diet charges,
surgical disposables and Pre Hospitalisation Expenses totalling to an amount of Rs.105821/- and
requested for reimbursement.
b) Respondent Insurer’s Arguments:
The insured patient was admitted in St.Philomenas Hospital on 03.06.2019 for the treatment of Pituitary
Macrodenma and Hypertension for which an amount of Rs.1,48,504/- was approved vide letter dated
dated 12.06.2019.
Thereafter insured person submitted the pre hospitalisation claim for reimbursement of Rs.55,230/-. It
was observed that all the bills/receipts were prior to the date of admission ie 03.06.2019 which are not
payable as per policy.
On receipt of notice from Ombudsman, the claim was reviewed once again by their medical panel and
have considered to pay an amount of Rs.10,201/- as per terms and conditions of the policy and have
given the worksheet as under:
Bill
No
Bill
Date
Classification
Bill
Amt
Deduction
Payable
Amout
Reason for Deduction
Room Rent
40500
0
40500
Room Rent
4700
0
4700
A
SUB TOTAL
45200
0
45200
B
PROFESSIONAL
FEES
73200
0
73200
OT
28080
0
28080
MEDICINE OUT
SIDE HOSPITAL
36793
0
36793
MEDICINE
16333
1760
14573
GLOVES, MICROSCOPE COVER GAUZE,
MOAP PER ONE, CAUTERY PLATE,
GOWN, PLAIN SHEET, GLOVES NOT
PAYABLE.
INVESTIGATION
12690
300
12390
CROSS MATCHING NOT PAYABLE
ANH PACKAGE
22485
6000
16485
C ARM, EQUIPMENT, PROCEDURE,
OXYGEN ALLOWED MICROSCOPE
DISALLOWED.
OTHERS
9505
9505
0
ATTENDERS, DIET, PULSE OXIMETER,
DISCHARGE, REGISTRATION CHARGES,
DRESSING NOT PAYABLE.
C
SUB TOTAL
125886
17565
108321
A+B+C
SUB TOTAL
244286
17565
226721
LESS
-68016
30% - COPAY
SUB TOTAL
244286
158705
LESS
-148504
ALREADY PAID TO HOSPITAL
TOTAL PAYABLE
AMOUNT
244286
10201

19. Reason for Registration of complaint:-
The complaint was registered as it falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal.
g. Complaint along with enclosures,
h. Respondent Insurer’s SCN along with enclosures and
i. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A.
21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is for short settlement of the claim amount. Forum has perused the documentary evidence
available on record and the submissions made by both the parties during the personal hearing.
21.1 The insured is covered under Senior Citizen Red Carpet Health Insurance Policy wherein the insured
has to bear 30% co pay of the total expenses claimed by him.
21.2 Pre-Hospitalisation expenses of Rs.55,230/- which are incurred by the insured before the admission
date ie 03.06.2019 and are not covered under the terms and conditions of the policy.
21.3 On mediation with the Forum, the R I have once again reviewed the claim by their medical Panel
and have considered for settlement for an amount of Rs.10201/- towards Hospitalisation Expenses as
per terms and conditions of the policy which is in order.
21.4 Other deductions made by the R I towards the expenses for excluded items as explained above are
in line with the policy terms and conditions and hence the complainant is not entitled for the same.
21.5 The claim is partially allowed.
AWARD
Taking into account of the facts and circumstances of the case and upon scrutiny of the
documents submissions made by both the parties, the Respondent Insurer is advised to
settle the balance claim of ₹. 10201/- along with interest @ 8.25% (Bank rate of 6.25% + 2%)
from the date of filing of the last relevant document by the Insured till the date of payment
of the claim as per Regulation 16.1.(ii) of IRDAI (Protection of Policyholders’ Interests)
Regulations, 2017.
The attention of the Complainant and the Respondent Insurer is hereby invited to Rule 17 (6) of the
Insurance Ombudsman Rules, 2017, where under the Respondent Insurer shall comply with the
Award within 30 days of the receipt of the Award and shall intimate compliance of the same to the
Ombudsman.
Dated at Bangalore on the 9
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN - NEERJA SHAH
In the matter of Shri MOHAN KUMAR SAPRE V/s UNITED INDIA INSURANCE COMPANY LIMITED
Complaint No: BNG-H-051-1920-0291
Award No. : IO/(BNG)/A/HI/211/2019-20
1
Name & Address of the
Complainant
Shri MOHAN KUMAR SAPRE
H No.1291, BasavanGalli,
Shahapur, Belagavi,
Karnataka -590 003
2
Policy No.
Type of Policy
Duration of Policy/ Policy
500100/28/17/P112448453
Tailormade Group
MediclaimPolicy(Retirees)

Period
01.11.2017 To 31.10.2018
3
Name of the Insured/
Proposer
Name of the policyholder
Shri MOHAN KUMAR SAPRE
Self
4
Name of the Insurer
United India Insurance Company Limited
5
Date of repudiation
Partial settlement
6
Reason for repudiation
NA
7
Date of receipt of Annexure
VI-A
04.11.2019
8
Nature of complaint
Short settlement of claim
9
Amount of claim
Rs.60,000/-
10
Date of Partial Settlement
Cash less
11
Amount of relief sought
Rs. 60,000/-
12
Complaint registered under
Rule no:
13 (1)(b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
26.11.2019/ Bengaluru
14
Representation at the
hearing
a) For the Complainant
Absent- submitted letter dt.09.11.2019
expressing inability to attend due to heart
surgery and requested .
b) For the Respondent
Insurer
Smt.H.A.Pannaga,Dy.Manager
15
Complaint how disposed
Allowed
16
Date of Award/Order
06.12.2019
17. Brief Facts of the case : Complaint emanated from the partial settlement of claim on the ground
that FFR (Fractional Flow Reserve)charges were not paid as the same were included in the package.
18. Cause of Complaint :
a. Complainant’s argument: The Complainant’s submission was that he is insured with United India
Insurance Company under the Group Mediclaim policy . During the month of June 2018 he developed
chest pain. After the medical examination he was diagnosed with IHD and doctor advised him to
undergo PTCA with two No of stent implant which would cost him Rs. 3,10,082.00
He sought second opinion from Dr. Dixit , who suggested him to undergo FFR for Angioplasty. After the
test Dr.Dixit advised for one stent implant only. He incurred Rs. 59050.00 towards the test and
underwent PTCA on 31.07.2018 at Lakeview Hospital. Total Hospitalization expenses were
Rs.2,85,577.00 including FFR test. RI deducted cost of FFR stating that the said cost is included in the
package.
He represented RI vide letter dt. 20.07.2019 and by mail dt.19.07.2019 but issues were not resolved and
hence has approached this Forum.
b. Insurers argument: The Respondent Insurer (RI) submitted their Self-Contained Note dated
22.11.2019 admitting their coverage and settlement of claim. They submitted that total cashless
approval was for Rs.2,26,727.00 as per hospital tariff. Deductions of Rs.71486.00 was made as it was
beyond package charges under reasonable and customary charges.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of the personal hearing with both the parties (Observations & Conclusions):
Complainant vide his letter dt.09.11.2019 expressed his inability to attend personal hearing. Forum has
perused the documentary evidence available on record and the submissions made by RI during the
personal hearing.
RI reiterated their contentions and stated that Reports of FFR and Receipts are not produced by the
complainant. The settlement is done by TPA as per the terms and conditions of the policy and the cost
of FFR test is included in the package Tariff.
The Forum noted form the Inpatient final Bill of Lakeview Hospital that Complex PTCA and FFR Test are
shown separately . Cost of FFR is shown as Rs. 57,500.00 out of total bill of Rs.2,85,777.00

Cashless approval shows details of cost as , FFR Rs.57,500/-+ Non Medical expenses Rs.190/- + Lab
charge Rs.1360/- which works out to Rs.59050/- Further, it is mentioned that Lab charge is included in
tariff.
In view of the above, the Forum does not agree with the decision of the RI in reducing the claim amount
of Rs.59050/- and allows the expenses of FFR test only.
Complaint is Allowed.
A W A R D
Taking into account facts & circumstances of the case and the documents oral submissions
made by RI during the course of hearing , Complainant is hereby awarded to be paid by the
Insurer, towards cost of FFR test subject to production of proof of receipt and test report,
as final settlement of the claim.
Forum directs the Respondent Insurer to settle the claim as above as per the terms and
conditions of policy along with interest @ 6.25% + 2% from the date of receipt of last
necessary documents to the date of payment of claim, as per regulation 16 (1) (ii) of
Protection of Policy holders’ Interests of IRDA Regulations, 2017 issued vide notification
dated 22.06.2017.
The complaint is Allowed.
22. Compliance of Award:
The attention of the Complainant and the Respondent Insurer is hereby invited to Rule 17(6) of the
Insurance Ombudsman Rules, 2017, where under the Respondent Insurer shall comply with the Award
within 30 days of the receipt of the Award and shall intimate compliance of the same to the
Ombudsman.
Dated at Bengaluru on the 6th day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of Shri Amarnath M V/s NATIONAL INSURANCE COMPANY LIMITED
Complaint No: BNG-H-048-1920-0265
Award No. : IO (BNG)/A/HI/222/2019-20
1
Name & Address of the
Complainant
Shri Amarnath M
No.27, Akshaya , 19trh Cross,
Krishnaiah Layout,
Ittamodu, BSK 3
rd
State,
7
th
Phase, J P Nagar
BENGALURU – 560 85
Mob.No. 9448093074
E-mail : amarnathv[email protected]m
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
604500501810003172
Critical Illness of Varistha Mediclaim
Individual policy
28.03.2019 to 27.03.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Shri Amarnath M
Shri Nagaraj T.(Father)
4
Name of the Respondent
Insurer
National Insurance Company Limited
5
Date of repudiation
03.07.2019

6
Reason for repudiation
No permanent neurological deficit
7
Date of receipt of Annexure
VI-A
26.09.2019
8
Nature of complaint
Rejection of claim
9
Amount of claim
₹.2,00,000/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹.2,00,000/-
12
Complaint registered under
Rule no:
13 (1)(b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
04.11.2019/Bengaluru
14
Representation at the
hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
Smt.Kalavathy Deputy Manager
15
Complaint how disposed
Dismissed
16
Date of Award/Order
13.12.2019
17. Brief Facts of the Case:
The complaint emanated from the rejection of one time payment under Critical Illness mediclaim policy
on the ground that it is not covered under the policy conditions. Despite taking up the matter with the
Respondent Insurer (RI), the same was not settled and hence, the Complainant has approached this
Forum to uphold justice.
18. Cause of Complaint:
a) Complainant’s arguments: The Complainant submitted that his father was insured with the RI and
was admitted into Apollo Hospital for CVA/stroke(Cerebrovascular accident infarct) for the period from
15.03.2019 to 12.04.2019. Later he was admitted to NIMHANS from 12.04.2019 to 28.04.2019 for
further treatment. Due to poor oral intake and recurrent UTI Pneumonia/aspiration he was again
admitted to Apollo Hospitals from 28.04.2019 to 29.05.2019. He was unable to walk independently and
taking feeds through PEG and was being given Oxygen through O2 concentrator and was on indwelling
urinary catheter. The claim for critical care policy was rejected by the RI. The Complainant Represented
to RI along with opinion of Doctor to reconsider the claim and their reply was not satisfactory. Hence,
he approached this Forum to arrange to release pending payment.
b) Respondent Insurer’s Arguments:
The Respondent Insurer (RI) in their Self-Contained Note dated 30.09.2019, admitted the issuance
coverage, preferring of claim and rejection of claim.
They submit that Insured person (IP) was admitted to Apollo Hospital from 15.03.2019 for the treatment
of great toe Cellulitis and difficulty in walking . MRI report indicates Small acute ischemic involving para
median left hemipons. Discharge summary CNS examination indicates -“conscious and oriented”. No
focal neurological defects . Hence No Permanent symptoms.
IP was admitted to NIMHANS from 12.04.2019 to 28.04.19 . As per discharge summary neurological
examination of cranial nerves, motor system, muscle tone, range of motion, coordination movement,
range of movements and reflexes were within normal limit which indicates he has no neurological
defects.
In the referral letter of NIMHANS dt.28.04.2019 ,it is mentioned that “able to move all 4 limbs” which
clearly shows that he has no neurological defects.
The admission to Apollo Hospital for the period from 28.04.19 to 29.05.2019 is for the treatment of
recurrent UTI, Aspiration Pneumonia ,PEG insertion, DM & HTN and medical management for acute
infarct PONS.
Hence claim was rejected as per terms and conditions of policy under Critical Illness Section –II 1.1.1.
Stroke resulting in permanent symptoms. After rejection, complainant resubmitted claim on 05.08.2019
along with Dr.’s certificates issued from Apollo Hospital and NIMHANS which are issued later to claim
rejection . None of the certificates confirm Stroke resulting in Permanent symptoms to comply with
policy conditions and it appears resubmission of revised version of the doctors just to favour the
patient.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
d. Complaint along with enclosures,
e. Respondent Insurer’s SCN along with enclosures and
f. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A

21. Result of personal hearing with both the parties (Observations & Conclusions):
The case before the Forum is whether the complainant is eligible for Critical Illness claim as per policy
condition.
The personal hearing was scheduled on 21.11.2019. At the request of the complainant, it was
adjourned to 04.12.2019. During the personal hearing on 04.12.2019 the R.I and the Complainant
reiterated their stand.
This Forum has perused both the documentary evidence available on record and as well as the
submissions made by the parties during the personal hearing.
The Complainant informed that after discharge from the hospital IP needed full support for his day-
today necessity and unfortunately he died on 09.11.2019. He produced Death certificate issued from
Apollo Hospital in this regard.
Critical Illness is defined in the policy is :-
1.1 -means stroke resulting in permanent symptoms, cancer of specified severity, kidney failure
requiring regular dialysis, major organ/bone marrow transplant, multiple sclerosis with persisting
symptoms and open chest CABG(Coronary Artery Bypass Graft) as mentioned in the policy.
Critical illness also includes permanent paralysis of limbs and blindness if mentioned in the schedule.
Stroke resulting in permanent symptoms is defined in Section 1.1.1 :-
Any Cerebrovascular incident producing permanent neurological sequelae. This includes infarction of
brain tissue, thrombosis in an intracranial vessel, haemorrhage and embolisation from an extracranial
source. Diagnosis has to be confirmed by a specialist medical practitioner and evidenced by typical
clinical symptoms as well as typical findings in CT scan or MRI of the brain. Evidence of permanent
neurological deficit lasting for at least 3 (three) months has to be produce.
Forum notes from the medical records that IP was initially admitted to hospital from 15.03.19 to
12.04.2019 with the complaint of left great toe insidious in onset, progressive ,non radiating , moderate
to severe aggravated on walking exertion and increased in intensity since 2 days associated with
difficulty in walking . Second admission was with NIMHANS for the period from 12.04.2019to
28.04.2019. Chief complains shows ‘Difficulty in walking since 15.03.2019’. Handwritten certificate
dt.28.04.2019 issued by NIMHANS at the time of discharge shows that IP is able to move all 4 limbs ,
responding to commands. Third hospitalization with Apollo Hospital is 28.04.2019 to 29.05.2019 which
is in continuation of second hospitalization Diagnosed with UTI,DM ILD-NSIP CVA-acute infract(Pons)
Hypo-natremia (resolved) Aspiration Pneumoinia S/p PEG insertion on 18.05.2019. Cause of Death
shows Aspiration pneumonia/ILD-NSIP.
Further, medical certificates do not show the evidence of permanent neurological deficit lasting for at
least 3 (three)months which is the condition for eligibility of claim under clause 1.1.1.of the policy.
Therefore, Forum does not find any flaw with the decision of the RI in rejecting the claims which is as
per the terms and conditions of policy and hence, the Complaint is Dismissed
A W A R D
Taking into account of the facts and circumstances of the case and the submissions made
by both the parties and documents submitted during the course of the Personal Hearing,
the decision of the Respondent Insurer in repudiating the claim is in consonance with the
terms and conditions of the policy and does not warrant any interference at the hands of
the Ombudsman.
Hence, the complaint is Dismissed.
Dated at Bangalore on the 13
th
day of December , 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of Shri B.P.SRINIVAS V/s RELIGARE HEALTH INSURANCE COMPANY LIMITED
Complaint No: BNG-H-037-1920-0294
Award No. : IO/(BNG)/A/HI/234/2019-20
1
Name & Address of the
Complainant
Shri B.P.SRINIVAS
A-203, Mantri Paradise, Next to HSBC.
Arekere Gate, Bannerghata Road,
BENGALURU
KARNATAKA – 560 076
Mob.No. 9341292491
E Mail ID : bpsrinu@gmail.com
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
12144567
Care Freedom Plan –I Individual
22.02.2018 to 21.02.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Smt.Bhagavathi Anjanamma (mother )
Shri B P Srinivas
4
Name of the Respondent
Insurer
Religare Health Insurance Company
5
Date of repudiation/rejection
17.08.2019
6
Reason for repudiation
Non-disclosure of IHD/CABG
Non –disclosure of material facts/pre-
existing ailment at the time of proposal
7
Date of receipt of the
Annexure VI-A
31.10.2019
8
Nature of complaint
Rejection of claim settlement
9
Amount of claim
Rs.2,69,717.00
10
Date of Partial Settlement
N.A.
11
Amount of relief sought
Rs.2,69,717.00
12
Complaint registered under
Rule no:
13 (1)(b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
05.12.2019/ Bengaluru
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
Dr.Chennakeshava Prasad S.L ,Zonal
Manager
Dr.Bharateesh Patwari, Manager
15
Complaint how disposed
Disallowed
16
Date of Award/Order
20.12.2019
17. Brief Facts of the Case:
The Complaint emanated from the rejection of claim for hospitalisation on the ground of Non-disclosure
of IHD/CABG prior to inception of policy.
18. Cause of Complaint:
a) Complainant’s arguments: The Complainant submitted that he had a policy with Max Bupa Health
Insurance Co., from 22.02.2013 which is ported to Religare Health Insurance Co. (herein after referred as
R.I) in Feb 2018. His mother Insured Person (IP) was admitted to Apollo Hospital, Bengaluru and
underwent operation for CRIF Proximal Femur Nailing on 14.08.2019. The R.I pre approved cashless for
Rs.1,70,000/- on 13.08.19, but on the day of discharge i.e. on 17.08.2019 he was denied cashless claim
approval. This put him under enormous stress and mental agony & he paid an amount of Rs.2,59,417/-.
Subsequently when he filed the claim for reimbursement the same was denied on the ground that IP
had a history of IHD/CABG.
Complainant submitted that IP underwent CABG operation in Apollo Hospital on 25.06.2014 which was
rejected by Max Bupa Health Insurance Co., due to 48 months lock-in-period which he did not contest.
She underwent another operation on 03.07.2017 for Left sided Uncemented Bipolar Anthroplasty which
was settled by them. Further, under policy exclusion clause it is stated that benefits will not be available
for any pre-existing conditions for 48 months, whereas policy was taken from Max Bhupa on 22.02.2013
which is 6 years 5 months before. The present operation is an Ortho operation, no way connected to
IHD/CABG. Therefore, denial of non disclosure is not applicable. In spite of representation to RI, the
same was not considered. Hence, he has approached this Forum.
b) Respondent Insurer’s Arguments:

The Respondent Insurer submitted their Self Contained Note dated 18.11.2019 and requested that, the
complaint should be dismissed as the same is not maintainable under the provisions Rule 14 sub-rule 3
of Insurance Ombudsman Rules, 2017.
They further submitted that the said policy was ported from Max Bupa Health Insurance having policy
period from 06.01.2018 to 05.01.2019. They took confirmation from the previous insurer regarding the
claims and disclosure details of the IP. As per the confirmation received from the previous insurer over
the IRDA IIB portal no details on any claims pertaining to the current non-disclosure are reflected.
During current policy period insured person (IP) preferred cashless request with complaint of pain in the
right hip since slip and fall at home and underwent CRIF PROXIMAL NAILING –RIGHT and their initial
approval was for ₹.1,70,000/-. On perusal of cashless form and documents, cashless facility was denied
for non-disclosure. On receipt of claim for reimbursement, the RI found that the IP was a known case of
IHD-Unstable Angina and CABG since 19.8.2014. Echocardiography and Doppler report under the head
of Echo Diagnosis post CABG was detected. This was not disclosed at the time of porting the policy. R.I
repudiated the claim on 17.08.2019 in accordance to clause 7.1 of the policy terms and condition i.e.
non-disclosure prior to the inception of policy.
RI further submitted that in the proposal form under the head “Medical and life style related
information” complainant wrongly mentioned that IP has not been detected with any heart disease or
disorder, chest pain or discomfort, irregular beats, palpitation or heart murmur. But IP had IHD which is
reflected is discharge summary and Echocardiography Report by the Apollo Hospital. Complainant
straightaway denied in the proposal form that IP has been hospitalized/recommended to take
investigation or has been under prolonged treatment/undergone surgery for any illness other than
childbirth or minor injuries . Finally complainant signed declaration stating that what is stated in the
proposal form is true to the best of his knowledge.
RI specifically stated that if pre-existing ailment/surgery of IHD and CABG were disclosed at the time of
proposal form then they would not have issued policy or would have issued the policy on different terms
& conditions.
RI strongly relayed on clause 19(4) of IRDA (Protection of Policy Holder’s Interest) Regulation, 2017
enumerating the “General Principal” .
Finally requested to dismiss the complaint.
19. Reason for Registration of complaint:
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017 and so it was registered.
20. The following documents were placed for perusal:
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
R.I has contended that Ombudsman has no jurisdiction to mediate as no representation has been made
by the complainant under Rule 14(3) of Ombudsman Rule 2017.
Forum observed from the record that R.I has reviewed the claim and rejected vide their letter
dt.10.09.2019. Hence the complaint is maintainable under 14 (3)(a)(iii) of the said Rules.
The dispute is as to whether there was Non –disclosure of material facts/pre-existing ailment at the time
of proposal. This Forum has perused the documentary evidence available on record and the submissions
made by both the parties during the personal hearing.
During the course of personal hearing the Complainant reiterated his contentions and submitted that IP
underwent treatment for fracture of femur during 2017 and the same has been settled by Max Bupa
Health Insurance. He admitted that he has not disclosed the said treatment during porting.
The RI reiterated their contentions in SCN and stated that their decision was based on facts, documents
and terms and conditions of policy. Representatives of RI contended that in the proposal form under the
column Details of Existing Insurance Policy/Insured Date of First enrolment is stated as 22.02.2016.
When the complainant disclosed information of Hypertension since Jan2015 and DM since Jan 2016
nothing prevented him to reveal information on IHD/CABG done during 2014 when IP was having policy
from 2013. If the same were disclosed they would not have accepted proposal and issued policy or
would have accepted the proposal with different terms and conditions.
RI placed reliance on Supreme Court’s decision in the case law in the Export Credit Guarantee Corp of
India Ltd. V/s Garg Sons International to strengthen their argument.
After careful examination of the medical records available, documents furnished and the submissions
made, this Forum notes from the proposal form dt. 12.02.2018 submitted by the complainant, to the

query regarding I.P(insured person) whether any heart disease or disorder, chest pain or discomfort,
irregular beats, palpitation or heart murmur, he has tick marked NO. He has tick marked Yes for
HTN/High Blood Pressure (BP)/High Cholestrol and DM/High Blood sugar/Diabetes on insulin or
medication. To the query No.15:-Has any of the Proposed to be insured been hospitalized/recommended
to take investigation or has been under any prolonged treatment/undergone surgery for any
illness/injury other than for childbirth/minor injuries, he has ticked NO. More importantly, to the query:-
have any of the person(s) to be insured ever filed a claim with their current/previous insurer? If Yes,
provide details on a separate sheet again he has replied on the negative.
Clause 7.1 of the policy Terms and condition is reproduced as follows:
“if any untrue or incorrect statement are made or there has been a misrepresentation, misdescription,or
non-disclosure of any material particulars or any material information having been withheld or if the
claim is fraudulently made or any fraudulent means or devices are used by the policy the holder or the
insured person or any one acting on his/her behalf, the company
shall have no liability to make payment or any claims and the premium paid be forfeited ab initio to the
company”
Clause 19(4) of IRDA (Protection of Policy Holder’s Interest) Regulation, 2017 enumerating the “General
Principal” are reproduced as follows:
“The policy holder shall furnish all the information that is sought from him by the insurer, either directly
or through the distribution channels which the insurer consider as having a bearing on the risk to enable
the insurer to assess properly the risk covered under a proposal for insurance”
In view of the above clear provisions Forum concludes that this is a case of non-disclosure of material
facts/pre-existing diseases/ailments at the time of proposal.
This Forum relies on the Hon’ble Supreme Court of India’s decision in the case of Satwant Kaur Sandhu
v/s. The New India Assurance Company Limited IV (2009) CPJ 8 (S.C), wherein the hon’ble court held:
“The upshot of the entire discussion is that in a Contract of Insurance, any fact which would influence
the mind of a prudent insurer in deciding whether to accept or not to accept the risk is a "material fact".
If the proposer has knowledge of such fact, he is obliged to disclose it particularly while answering
questions in the proposal form. Needless to emphasise that any inaccurate answer will entitle the
insurer to repudiate his liability because there is clear presumption that any information sought for in
the proposal form is material for the purpose of entering into a Contract of Insurance”.
Forum concur with the decision of the Respondent Insurer in rejecting the claim as per terms and
conditions of the policy.
In view of the above, the Complaint is Disallowed
A W A R D
Taking into account of the facts and circumstances of the case and the submissions
made by both the parties and documents submitted during the course of the
Personal Hearing, the decision of the Respondent Insurer in repudiating the claim in
consonance with the terms and conditions of the policy and does not warrant any
interference at the hands of the Ombudsman.
Hence, the Complaint is Dismissed.
Dated at Bengaluru on the 20
th
day of December , 2019.
( NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of Shri N SAMBASHIVAN V/s STAR HEALTH & ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-0257
Award No.: IO/(BNG)/A/HI/0201/2019-20
1
Name & Address of the
Complainant
Shri N SAMBASIVAM
T- 2, Sri Mahalakshmi Apartment
30, 31, 5
th
Main Road
8
th
Cross, Malleswaram
BENGALURU – 560 003
Mob.No. 82773 99485
Mail ID : nsambasi[email protected]m
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
P/141113/01/2019/009885
Senior Citizens Red Carper Health
Insurance Policy 01.01.2019 to 31.12.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Shri N Sambasivam
Self
4
Name of the Respondent
Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
29.07.2019
6
Reason for repudiation
Failure to submit required documents
7
Date of receipt of Annexure
VI-A
15.10.2019
8
Nature of complaint
Non settlement of Claim
9
Amount of claim
₹.26,000/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹.26,000/- with compensation
12
Complaint registered under
Rule no:
13 (1) (a) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
20.11.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
Dr. Umadevi M B, Sr. Manager
15
Complaint how disposed
DISMISSED
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case:
It is a case of rejection of claim policy on the ground of non submission of required documents. The
Complainant took up the matter with the Grievance Cell of the Respondent Insurer (RI) and the same
was not considered favourably.
18. Cause of Complaint:
a) Complainant’s arguments: The Complainant submitted that he is insured with the RI from 01.01.2016
and is valid upto 31.12.2019. He was admitted to Manipal North Side Hospital on 25.05.2019 with
complaints of increased thirst, polyuria and fatigue. He was kept in observation for 3 days and switched
over from tablets to insulin. The past history as per discharge summary is DM, hypothyroid, IHD, S/p
PTCA 10 years back and CKD. He was diagnosed as type II DM, hypertension and hypothyroid. His
request for cashless was rejected. Subsequently, he submitted the papers for reimbursement and RI is
insisting for 2016 records on serum and other investigations. He submitted routine blood test conducted
during 2016 for lipid profile and inspite of it, RI is insisting for investigation results, which he has not
undergone and have rejected the claim.
The approach to Grievance cell of RI also did not yield any result and hence, the Complainant had
approached this Forum.
b) Respondent Insurer’s Arguments:
The RI sent their Self Contained Note dated 09.11.2019 admitting insurance coverage from 01.01.2016
to 31.12.2019, preferring of claim and their rejection as per condition No. 4. It is submitted that patient
has a past history of DM, Hypothyroid, CKD and IHD-SP PTCA 02.08.2006. Also, the treating doctor letter

dated 26.05.2019 states patient’s creatine level in 2016 is 1.31. Hence, RI has raised a query to submit
the earlier reports and consultations papers. Hence, the claim was repudiated invoking condition no. 4
of the policy.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is for rejection of claim on the ground of non submission of previous consultations and
treatment records taken during the year 2009 and 2016.
During the personal hearing, both the parties reiterated their earlier submissions.
It is noted from the denial of pre authorization request for cashless treatment letter dated 27.05.2019
that the denial was for non submission of previous consultations and treatment records of 2016 and
PTCA of 2009.
However, as per repudiation letter dated 29.07.2019 the denial of claim was for non-submission of
required documents of 2016 invoking condition no. 4 of the policy, “The insured person/s shall obtain
and furnish the company with all original bills, receipts and other documents upon which a claim is based
and shall also give the company such additional information and assistance as the company may require
in dealing with the claim.”
As the repudiation of claim is for non-submission of required documents of 2016, the Forum cannot take
cognizance of arguments of representative of RI that there is non-disclosure of Pre existing disease of
CAD and PTCA of 2009 which has been maintained by the RI in their SCN dated 09.11.2019.
The Forum noted from the medical report of Shri Jugraj Lodha Medical Centre dated 01.11.2016 that
creatine value was 1.31 mg/dl which is slightly higher than the reference range (0.5 – 1.2) or normal
values whereas policy was effective from 01.01.2016. Hence, RI cannot repudiate the claims for the
diagnosis/treatment taken after the issuance of the policy.
The RI has submitted the copy of proposal form along with schedule with terms and conditions.. The
perusal of the proposal form shows that the insured person has replied in the negative to the Health
history query Sr. No. 2 “Have you consulted / taken treatment/been admitted for any
illness/injury/disease/surgery, if yes, details”. Also, in Sr. No. 3.c. “Have you ever suffered or suffering
from any of the following - Heart disease, if yes since when.” In contract of insurance it is the bounden
duty of the insured person to give the detail about his medical condition as required in the proposal
form.
As the insured was aware of his PTCA of 2009 at the time of submitting the proposal form, it was his
duty to disclose the same at the time of taking the policy and having not disclosed, it amounted to non
disclosure of material facts. Accepting the case laws quoted by RI, this Forum relies on the Hon’ble
Supreme Court of India’s decision in the case of Satwant Kaur Sandhu v/s. The New India Assurance
Company Limited IV (2009) CPJ 8 (S.C), wherein the Hon’ble court held:
“The upshot of the entire discussion is that in a Contract of Insurance, any fact
which would influence the mind of a prudent insurer in deciding whether to accept
or not to accept the risk is a "material fact". If the proposer has knowledge of such
fact, he is obliged to disclose it particularly while answering questions in the
proposal form. Needless to emphasise that any inaccurate answer will entitle the
insurer to repudiate his liability because there is clear presumption that any
information sought for in the proposal form is material for the purpose of entering
into a Contract of Insurance.”
Considering the above, this Forum is of the opinion that the complainant having not disclosed the
material facts to the RI in proposal form has breached uberrima fides i.e. utmost good faith of insurance
contract. Hence, the Complaint is dismissed.
Since the complainant is having medical insurance from 2016, Forum advises the RI to revive the
cancelled policy, if cancelled as procuring fresh insurance at this age (69 years) would be difficult.

A W A R D
Taking into account of the facts and circumstances of the case and the submissions made
by both the parties and documents submitted during the course of the Personal Hearing,
the decision of the Respondent Insurer in repudiating the claims are in consonance with
the terms and conditions of the policy and does not warrant any interference at the hands
of the Ombudsman.
The RI is directed to re-instate the policy, if cancelled.
Hence, the Complaint is Dismissed.
Dated at Bengaluru on the 6
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of MR. THANIGAVELU S V/s STAR HEALTH & ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-0284
Award No.: IO(BNG)/A/HI/0202/2019-20
1
Name & Address of the
Complainant
Mr. Thanigavelu S
#1492, 1
st
Cross,
1
st
Main Road, Mariyappanapalya,
Bangalore - 560021
Mobile No.: 9448211743
Email ID: acchu0[email protected]m
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
P/141123/01/2019/014888
Family Health Optima Insurance Plan
28.03.2019 to 27.03.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Mr. Thanigavelu S
Miss Pavithra T (Daughter)
4
Name of the Respondent
Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
06.10.2019
6
Reason for repudiation
Onset of disease during break in period
7
Date of receipt of Annexure
VI-A
24.10.2019
8
Nature of complaint
Repudiation of claim
9
Amount of claim
₹. 8,68,486/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹. 8,68,486/- with interest
12
Complaint registered under
Rule no:
13 (1) (b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
26.11.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
Dr. Umadevi, Manager
15
Complaint how disposed
Allowed
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case:
The Complaint emanated from the rejection of claim for hospitalisation. The Complainant took up the
matter with the Grievance Cell of the Respondent Insurer (RI) and the same was not considered
favourably.

18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant along with Wife and 2 daughters was insured under Family Health Optima Insurance
for a Basic Floater Sum Insured of ₹. 3,00,000/-, Bonus ₹. 1,65,000/- with limit of coverage ₹. 4,65,000/-
and Recharge benefit ₹. 75,000/- for the period from 28.03.2019 to 27.03.2020. The Insured Person,
Miss Pavithra T, underwent Exploratory Laparotomy + Massive Resection of small bowel + Subtotal
colectomy + Loop Ileostomy under GA on 24.08.2019 at Fortis Hospital, Bangalore and unfortunately
declared dead on 03.09.2019 at 10:55 PM. The complainant applied for cashless treatment but RI
repudiated the said claim stating the onset of the disease was during break in period of the policy. He
then applied for reimbursement of claim, however his request is not considered favourably. In spite of
approaching the Grievance cell of RI, the same was not resolved and he has approached this Forum.
b) Respondent Insurer’s Arguments:
The RI has not submitted their Self Contained Note. But forwarded an e-mail dated 25.11.2019 stating
they are ready to settle the claim ₹. 4,81,606/-.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is for repudiation of claim as per the terms and condition of the policy.
During the course of personal hearing, the representative of RI submitted that their Claims Review
Committee approved the claim for ₹. 4,81,606/- and forwarded an email to the complainant for his
consent vide their email dated 25.11.2019. The details are given as (amounts in ₹. only):
Sr.
N
o
.
Nature of
expenditure
Claimed
Amount
Amount
Disallowed
Approved
Amount
Remark
1
Room rent &
nursing charges
6120
0
6120
2
ICU charges
86400
0
86400
3
Professional Fees
43120
1930
41190
Dietician consultation, RMO
charges not payable
4
Investigatin &
diagnostics
121090
15130
105960
Some charges are not
payable as per terms and
conditions of the policy
5
Medicines
262095
34128
227967
Some charges are not
payable as per terms and
conditions of the policy
6
Package charges
209180
41836
167344
No breakup for package
charges. Hence 20%
deduction
7
Miscellaneous
Charges
143340
143340
Deductions as per policy
terms & conditions
8
Others
60142
2030
58112
Some charges are not
payable as per terms and

conditions of the policy
TOTAL
931487
238394
630093
(Less Hospital Discounts
63000)
Amount Claimed
931487
Net amount (Approved amount after deductions and discounts)
630093
Amount settled by other Insurer (The New India Assurance Co. Ltd.)
148487
Balance payable to the Complainant
481606
The Complainant confirmed during the hearing that he received an email from RI but he disagrees over
Sr. No. 6 (Package charges) and some reports charges which were denied by RI for non submissions of
the reports and over the TDS deduction. It is also submitted that he had applied with other insurer (The
New India Assurance Co. Ltd.) from where he received ₹. 1,48,487/-.
The Forum notes that Fortis Hospital is a network hospital and hence deduction of 20% amount (Sr. No.
6) towards breakup of package charges is unjustified. Also, it advises the complainant to submit all the
reports and related bills to RI which were disallowed by the RI but payable as per terms & conditions of
the policy.
The Forum noted that as per IT act, Tax Deducted at Source (TDS) is a system introduced by Income Tax
Department, where person responsible for making specified payments such as salary, commission,
professional fees, interest, rent, etc. is liable to deduct a certain percentage of tax before making
payment in full to the receiver of the payment. Hence, it would either be adjusted against his tax liability
or refunded on filing IT returns.
In the view of forgoing, the Forum directs the RI to settle the claim as per the terms and condition of the
policy as soon as they receive the medical reports and related bills. Hence, the complaint is Allowed.
A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral
submissions made by both the parties, this Forum is of the opinion that the decision of the
Respondent Insurer is not in accordance with the terms and conditions of policy and not found
to be in order.
This Forum directs the Respondent Insurer to settle the claim as above as per the terms and
conditions of policy along with interest @ 6.25% + 2% from the date of receipt of last necessary
documents to the date of payment of claim, as per regulation 16 (1) (ii) of Protection of Policy
holders’ Interests of IRDA Regulations, 2017 issued vide notification dated 22.06.2017.
Hence, the complaint is ALLOWED.
22. Compliance of Award:
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. The Complainant shall submit all requirements/Documents required for settlement of award
within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall comply
with the award within thirty days of the receipt of the award and intimate compliance of the
same to the Ombudsman.
Dated at Bengaluru on the 6
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of MRS. K R LALITHA V/s APOLLO MUNICH HEALTH INSURANCE COMPANY LIMITED
Complaint No: BNG-H-003-1920-0283
Award No.: IO/(BNG)/A/HI/0203/2019-20
1
Name & Address of the
Complainant
Mrs. K R Lalitha
Door No. 1645/148,
2
nd
Cross, Behind Anjaneya Temple,
Vidyanagar,
Devnagere-577005
Karnataka
Mob: 9448533956
2
Policy /Cert. No.
Type of Policy
Duration of Policy/ Policy
Period
120100/12001/2018/A012706/894
Easy Health Group Insurance
13.04.2019 to 12.04.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Mrs. K R Lalitha
Self
4
Name of the Respondent
Insurer
Apollo Munich Health Insurance Company
Limited
5
Date of
repudiation/rejection
28.08.2019
6
Reason for repudiation
Incorrect good health declaration
7
Date of receipt of Annexure
VI-A
16.10.2019
8
Nature of complaint
Rejection of medi-claim
9
Amount of claim
₹. 40,250.62/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹. 40,250.62/-
12
Complaint registered under
Rule no:
13 (1) (b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
27.11.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Mr. K B Ramalingappa (Spouse)
b) For the Insurer
Dr. Yeshwant Kumar, Manager
15
Complaint how disposed
Allowed
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case:
The complaint emanates from the repudiation of claim for the hospitalisation and cancellation of policy
on the ground of incorrect good health declaration in the proposal. The Complainant approached the
Grievance Cell of the Respondent Insurer (RI), but the complaint was not resolved. Therefore, the
Complainant has approached this Forum.
18. Cause of Complaint:
a. Complainant’s arguments:
The Complainant’s submission was that she was insured with the above RI from 13.04.2016 and valid till
12.04.2020. She was admitted to SNR Hospital, Bengaluru on 18.07.2019 and discharged on 19.07.2019
and her claim was rejected by the RI and policy was cancelled. The reason given for rejection was that as
per medical history details of coronary artery disease since 14 years is not revealed while taking the
policy in the proposal form.
b. Respondent Insurer’s Arguments:
The Respondent Insurer has not submitted Self Contained Note. However, RI has sent an email dated
19.11.2019 that they are willing to settle the claim for ₹. 17,753/- but they denied to reinstate the
policy.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A

21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is with regard to the repudiation of the claim for incorrect good health declaration in
proposal form and thereby cancellation of the policy.
During the personal hearing, representative of RI submitted that they are willing to settle the claim for
₹. 17,753/- as per following table but denied to reinstate the policy. (Amount in ₹.)
Sr. No.
Hospital Expenses
Claimed
amount
Disallowed
amount
Approved
amount
Remarks
1
Room rent &
Nursing charges
1200
0
1200
2
Professional
Charges
5900
1000
4900
Not Payable other
charges
3
Pharmacy
4973
0
4973
4
Others
200
200
0
Admission charges
not payable
5
Investigations
15480
8800
6680
Disallowed amount
not within pre
hospitalisation
period
TOTAL
27753
10000
17753
Complainant’s husband agreed for the above settlement but contended that he should get interest
amount for delay in payment and the policy should be reinstated.
The Forum on perusal of rejection letter and termination notice dated 28.08.2019 observed that the
reason for termination of the policy is incorrect good health declaration in proposal form. RI has failed
to provide proposal form duly signed by the complainant and hence they have failed to establish the
veracity of their statement. In the absence of proposal form, RI’s decision to cancel the policy is
unjustified.
Considering the above, this Forum is not in agreement with the decision of the RI that there was
incorrect good health declaration and directs the RI to settle the claims as per the terms and conditions
of policy and to reinstate the cancelled policy. The Complaint is allowed.
A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral
submissions made by both the parties, this Forum is of the opinion that the decision of the
Respondent Insurer is not in accordance with the terms and conditions of policy and not found
to be in order.
This Forum directs the Respondent Insurer to settle the claim for ₹. 17,753/- along with
interest @ 6.25% + 2% from the date of receipt of last necessary documents to the date of
payment of claim, as per regulation 16 (1) (ii) of Protection of Policy holders’ Interests of
Regulations, 2017 issued by IRDAI vide notification dated 22.06.2017 and also directed to
reinstate the cancelled policy.
Hence, the complaint is ALLOWED.
22. Compliance of Award: The attention of the Complainant and the Respondent Insurer is hereby
invited to Rule 17(6) of the Insurance Ombudsman Rules, 2017, where under the Respondent Insurer
shall comply with the Award within 30 days of the receipt of the Award and shall intimate compliance of
the same to the Ombudsman.
Dated at Bangalore on the 6
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN - NEERJA SHAH
In the matter of MR. SANDIP KUMAR V/s UNITED INDIA INSURANCE COMPANY LIMITED
Complaint No: BNG-H-051-1920-0261
Award No.: IO/(BNG)/A/HI/0204/2019-20
1
Name & Address of the
Complainant
Mr. Sandip Kumar
219, 7
th
Main,
Sadanand Nagar NGEF East,
Bangalore – 560 038
Mob. No.- 9686271127
Email- sandipkumar11@yahoo.com
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
0725002818P107679907
Super top up Medicare policy
12.09.2018 to 11.09.2019
3
Name of the Insured/
Proposer
Name of the policyholder
Mr. Sandip Kumar
Self
4
Name of the Insurer
United India Insurance Company Limited
5
Date of repudiation
22.05.2019
6
Reason for repudiation
Non-medical and not-payable amount
7
Date of receipt of Annexure
VI-A
12.11.2019
8
Nature of complaint
Repudiation of claim
9
Amount of claim
₹.7,17,686/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹. 1,80,382/-
12
Complaint registered under
Rule no:
13 (1)(b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
04.12.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Absent
b) For the Respondent
Insurer
1. Mrs H A Pannaga, Dy. Manager
2. Mrs. R Sumathi, AO
15
Complaint how disposed
ALLOWED
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case:
The complaint emanated from rejection of claim on the ground that basic sum insured got exhausted
and Non-medical and not-payable amount as per the policy. Despite taking up the matter with the
Grievance cell of Respondent Insurer (RI) against rejection of his claim, the same was not considered and
hence, he has approached this Forum.
18. Cause of Complaint:
a) Complainant’s arguments: The Complainant submitted that he is a retired employee of Bosch India
Ltd. In January 2019, he underwent surgery for prostate cancer at Manipal Hospital, Bangalore and the
total bill amounts to ₹. 7,17,686/-. He was covered for a sum insured of ₹. 5,00,000/- with other insurer
Bajaj Allianz Ins. Co. Ltd which was taken by his employer. He also took super top insurance cover from
RI for ₹. 5,00,000. Bajaj Allianz paid ₹. 5,00,000 and for balance claim, he applied to the RI on 09.03.2019
but his claim was repudiated by the RI stating non-medical and non-payable amount. In spite of
approaching the Grievance cell of RI, the same was not resolved.
b) Respondent Insurer’s Arguments: RI submitted their Self-Contained Note dated 03.12.2019 admitting
coverage preferring of claim and repudiation of claim. It is submitted that Robotic surgeries liability has
to be restricted to the cost of customary procedure and as per PPN GIPSA package rates prostrate
removal Holmium/Diode for special ward is ₹. 1,23,266/- and Mediassist TPA has already settled the
charges beyond the cost PPN.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017

20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
It is noted from the available documents that the complainant preferred a claim with Bajaj Allianz (other
Insurer) which they have settled for ₹. 5,00,000/- and for the balance claim amount of ₹. 2,17,686/-, he
applied to the RI under the super top policy which has been repudiated by them. The dispute is whether
the repudiation of claim by RI is in order or not.
During the personal hearing, the representatives of RI and TPA were present but the complainant
expressed his inability to attend the hearing as per letter dated 01.12.2019 and requested the forum to
consider the case on the basis of available papers.
The representatives of RI vehemently submitted that the complainant underwent Robotic assisted
radical prostectomy but as per the policy terms and conditions, liability on Robotic surgeries has to be
restricted to the cost of customary procedure and as per PPN GIPSA package rates. The prostrate
removal Holmium/Diode for special ward in other similar hospitals amounts to average ₹. 1,23,266/-
and previous TPA Mediassist has already settled the charges beyond the cost PPN.
The relevant policy terms and conditions quoted by the RI are reproduced as below:
2. Covered Expenses:
2.1 In the event of any claim(s) becoming admissible under the policy, the Company will
pay expenses as are reasonable and medically necessary through TPA to the
hospital/Nursing or the insured person.
3.29 Reasonable and customary charges:
Reasonable and customary charges means the charges for services or supplies, which are
the standard charges for the specific provider and consistent with the prevailing charges
in the geographical area for identical or similar services, taking into account the nature of
the illness/injury involved.
3.33 Surgery or Surgical Procedure:
Surgery or Surgical Procedure means manual and/or operative procedure(s) required for
treatment of an illness or injury, correction or deformities and defects, diagnosis and cure
of diseases, relief of suffering or prolongation of life, performed in a hospital or day care
centre by a medical practitioner.
It is noted from worksheet provided by the present TPA i.e. Genesis India TPA Ltd. /RI that the
Sr. No.
Services/Charges
Type
Amount
Claimed
Deduction/Discount
Payable
amount
Remarks
1
File admission
charges
1500
1500
0
Not Payable
2
Room rent, nursing
charges
117600
0
117600
3
Consultation visit
charges
30500
0
30500
4
Instrument charges
14280
0
14280
5
Investigations
25708
3648
22060
HIV & Hbsag
reports not
payable
6
OT Charges
113300
0
113300
7
Surgeon fees,
Anaethesist
128750
0
128750

charges
8
Miscellaneous
950
0
950
9
Drugs
55492
24919
30573
Non payable
items
10
Disposables
229501
190472
39029
Not payable
F & B
105
105
0
Diet charges not
payable
Hospital discount
18652
TOTAL
717686
239296
497042
On perusal of the above terms and conditions, it is nowhere mentioned that the robotic surgery is
excluded or comes under Reasonable and customary charges. Hence, the stand taken by the RI in
restricting the claim is unjustified.
However, the RI shall not be liable to make any payment under the policy in respect of any expenses
whatsoever incurred in connection with or in respect of exclusion no. 4. That means, Admission Charges
– ₹. 1,500/-, HIV & Hbsag- ₹. 3,648/-, Documentation charges – ₹. 950/- and Diet Charges – ₹. 105/- are
not payable. In addition to this, Hospital discount – ₹. 18,652/- availed by him is also not payable.
Since the RI has not given any annexure related to the non payable items, the Forum finds that the
following items are admittedly used in the robotic surgery for one time only and thus clearly payable.
1. Bladeless excel trocar- ₹. 10,672/-
2. Drape arm- ₹. 25,043/-
3. Fenestrated bipolar forceps- ₹. 32,614/-
4. Large needle driver – ₹. 53,289/-
5. Monopolar curved scissor- ₹. 38,729/-
6. Bladeless obturator- ₹. 1,006/-
7. Prograsp forceps- ₹. 26,644/-
8. Tip cover accessory – ₹. 2,475/-
Total- ₹. 1,90,472/-
Hence the complaint is allowed.
A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral
submissions made by the RI, this Forum is of the opinion that the decision of the Respondent
Insurer is not in accordance with the terms and conditions of policy and not found to be in
order.
This Forum directs the Respondent Insurer to settle ₹. 1,90,472/- as per the terms and
conditions of policy along with interest @ 6.25% + 2% from the date of receipt of last necessary
documents to the date of payment of claim, as per regulation 16 (1) (ii) of Protection of Policy
holders’ Interests of Regulations, 2017 issued by IRDAI vide notification dated 22.06.2017.
Hence, the complaint is ALLOWED.
22. Compliance of Award: The attention of the Complainant and the Respondent Insurer is hereby
invited to Rule 17(6) of the Insurance Ombudsman Rules, 2017, where under the Respondent Insurer
shall comply with the Award within 30 days of the receipt of the Award and shall intimate compliance of
the same to the Ombudsman.
Dated at Bengaluru on the 6
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of: MR. ARUN KUMAR B R v/s THE ORIENTAL INSURANCE COMPANY LIMITED
Complaint No: BNG-H-050-1920-0298
Award No: IO/(BNG)/A/HI/0209/2019-20
1
Name & Address of the Complainant
Dr. Arun Kumar B R
#28, 2
nd
Floor, 2
nd
Cross,
New Kempegowda Layout Kathriguppe,
BSK III stage,
Bangalore-560085
Mobile No.: 9448519183
E-mail: drarunkumarbr@yahoo.co.in
2
Policy No.
Type of Policy
Duration of Policy/ Policy Period
423101/48/2019/931
PNB-Oriental Royal Mediclaim Policy
25.06.2018 to 24.06.2019
3
Name of the Insured/Proposer
Name of the Insured Person
Dr. Arun Kumar B R
Self
4
Name of the Respondent Insurer
The Oriental Insurance Company Limited
5
Date of Repudiation
03.05.2019
6
Reason for repudiation
Investigations alone were carryout without active line
of treatment
7
Date of receipt of Annexure VI-A
30.10.2019
8
Nature of complaint
Rejection of claim
9
Amount of claim
₹. 1,03,006/-
10
Date of Partial Settlement
Not Applicable
11
Amount of relief sought
₹. 1,03,006/-
12
Complaint registered under Rule no.
13 (1) (b) of Insurance Ombudsman Rules, 2017
13
10.01.2019
05.12.2019 /Bengaluru
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent Insurer
1. Dr. Rachana, TPA
2. Mr. D G Gowda Raja Swamy, AM
15
Complaint how disposed
Allowed
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case: -
The complaint emanated from the rejection of the claim on the ground that the investigations and
diagnostic tests were alone carried out without active line of treatment and the same could have been
managed on OPD basis. Despite representing to Grievance cell of Respondent Insurer (RI), the claim was
not settled. Hence, the Complainant approached this Forum for settlement of his claim.
8. Cause of Complaint: -
a) Complainants argument:
The Complainant obtained the cited policy covering himself, his wife, and son for a floater Sum Insured
of ₹. 5,00,000/-. The Complainant was admitted to Apollo Hospital, Bangalore on 20.06.2019. As per
the Discharge Summary (DS) he was admitted with complaints of swelling in supraclavicular region and
was diagnosed as Right supraclavicular Lymphodenopathy and discharged on 22.06.2019. The
reimbursement claim was rejected vide RI’s letter dated 03.05.2019 stating that only investigations were
carried out without any active line of treatment. Hence the Complainant approached this Forum for
settlement of his claim.
b) Respondent Insurer’s Arguments:
The Respondent Insurer, in their Self Contained Note (SCN) dated 28.10.2019, whilst admitting the
insurance coverage, submitted that as per records the patient was admitted with swelling in right
supraclavicular region, managed conservately and discharged with the diagnosis Right Supraclavicular
Lymphadenopathy. During the hospitalization period, there was right supraclavicular Lymph node biopsy
& underwent various investigations which does not require hospitalization and can be done on OPD
basis. Hence, the claim was repudiated as per exclusion clause 4.9 which reads as ‘Expenses incurred at

Hospital or Nursing Home primarily for evaluation/diagnostic purposes which is not followed by active
treatment for the ailment during the hospitalised period.
Hence their decision was in order.
19. Reason for Registration of Complaint: -
The complaint was registered as it falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal: -
g. Complaint along with enclosures,
h. SCN of the Respondent Insurer along with enclosures along with the enclosures and
i. Consent of the Complainant in Annexure VI A & Respondent Insurer in Annexure VII A.
21. Result of personal hearing with both the parties (Observations & Conclusions): -
The issue which requires consideration is whether there was active line of treatment or treatment
required hospitalisation.
During the personal hearing, the Complainant reiterated that the claim does not attract exclusion clause
4.9 of the policy as it was necessary to follow the standard operating procedure required for the ailment
to avoid any risk to his health and life.
It is noted from certificate issued by treating surgeon Dr. Ravishankar Bhat B dated 07.08.2019 that the
patient had right Supraclavicular Lymphonode, which was deep and large and close to major vessels and
nerves. Performing lymphonode biopsy under Local anaesthesia would have been risky, therefore the
patient was admitted and lymphonode biopsy was done on 21.06.2018 under general anaesthesia.
It is also noted that after histo-pathology report, the complainant is under medication for TB under
DOTS. Hence, repudiation on the ground of exclusion clause 4.9 of the policy is not established.
During the personal hearing, the representatives of RI submitted that they are ready to consider the
claim as per terms and conditions of the policy.
Hence, the complaint is allowed.
AWARD
Taking into account of the facts and circumstances of the case and upon scrutiny of the documents
submitted by both the parties, the Respondent Insurer is advised to settle the claim along with
interest @ 8.25% (Bank rate of 6.25% + 2%) from the date of filing of the last relevant document by
the Insured till the date of payment of the claim as per Regulation 16.1.(ii) of IRDAI (Protection of
Policyholders’ Interests) Regulations, 2017.
The Complaint is Allowed.
22) Compliance of Award:
The attention of the Complainant and the Respondent Insurer is hereby invited to Rule 17 (6) of the
Insurance Ombudsman Rules, 2017, whereunder the Respondent Insurer shall comply with the Award
within 30 days of the receipt of the Award and shall intimate compliance of the same to the
Ombudsman.
Dated at Bengaluru on the 6
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of MR. AJIT S KADUR V/s STAR HEALTH & ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-0302
Award No.: IO/(BNG)/A/HI/0213/2019-20
1
Name & Address of the
Complainant
Mr. Ajit S Kadur
Shree Gokula, 80-3/4 A,
Next to Rishi Sandipani School,
Nagadevanahalli,
Bangalore – 560056
Mobile No.: 9538532229
Email: ajit.s.kadu[email protected]
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
P/141135/01/2019/004931
Family Health Optima Insurance Plan
31.12.2018 to 30.12.2019
3
Name of the Insured/
Proposer
Name of the policyholder
Mr. Sathyanarayana Kadur
Mr. Sathyanarayana Kadur
4
Name of the Respondent
Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
20.05.2019
6
Reason for repudiation
Misrepresentation/Non-disclosure of material
facts
7
Date of receipt of Annexure
VI-A
22.10.2019
8
Nature of complaint
Rejection of Claim and cancellation of
policy
9
Amount of claim
₹.9,56,372/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹.5,00,000/- + interest
12
Complaint registered under
Rule no:
13 (1) (b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
05.12.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
Dr. Umadevi M B, Sr. Manager
Mr. Mahadevan G, Sr. Consultant
15
Complaint how disposed
DISMISSED
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case:
It is a case of rejection of claim policy on the ground of non disclosure of material facts before the
inception of policy. The Complainant took up the matter with the Grievance Cell of the Respondent
Insurer (RI) and the same was not considered favourably.
18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant’s submission was that he along with his parents was insured continuously with the RI
since 31.12.2018. His father was admitted to BGS Hospital on 06.02.2019 and discharged on 25.02.2019.
He was diagnosed as CVD – acute infarcts in bilateral ACA-MCA and right MCA-PCA watershed regions
and medulla region. The complainant applied for cashless claim but it got rejected.
Again his claim for reimbursement was rejected and the approach to Grievance cell also did not yield
any result and hence, the Complainant had approached this Forum.
b) Respondent Insurer’s Arguments:
The RI vide their Self Contained Note dated 05.11.2019 admitting insurance coverage from 31.12.2018
to 30.12.2019, preferring of claim and their rejection as per condition No. 6. It is contended that as per
the prescription dated 13.08.2016 of the hospital that patient has many episodes for the past 4-5 years.
Also, MRI brain dated 13.02.2019 shows “compared to prior MRI done on 06.02.2018, there are few
infarcts in the right thalamus, posterior medulla and inferior vermis. These facts were not disclosed and
hence claim was rejected for misrepresentation/non-disclosure of material facts and policy was
cancelled as per the terms and conditions of policy.

19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is for rejection of claim and cancellation of policy on the ground of non disclosure of
material facts.
The complainant reiterated his contentions that he had given full information of medical history of his
father that he has Diabetes mellitus and hence on the basis of that RI had issued the policy with PED –
Diabetes mellitus and its complication.
Representative of RI submitted that prescription dated 13.08.2016 of the hospital reveals that patient
has many episodes for the past 4-5 years. Also, MRI brain dated 13.02.2019 shows “compared to prior
MRI done on 06.02.2018, there are few infarcts in the right thalamus, posterior medulla and inferior
vermis” which means he had undergone MRI in 06.02.2018 and these facts were not disclosed by the
insured person in the proposal form and hence claim was rejected.
Forum notes that RI submitted OPD statement of the hospital where the insured person went to regular
visits since 02.04.2014. Prescription letter dated 13.08.2016 reveals that patient was treated with
Neurologists with history of episodic neurological disturbance since 4-5 years. Also, H/o urinary
disturbance, occasional drowsiness, gait imbalance and walking with support from past 4-5 yrs,
Impression- Dementia under evaluation. MRI brain report dated 13.02.2019 shows that there was prior
MRI done on 06.02.2018 which is found to be prior to the date of inception of the policy.
The RI has submitted the copy of proposal form along with schedule with terms and conditions. The
perusal of the proposal form shows that the insured person has replied in the affirmative to the Health
history query Sr. No. 2 “Has the person proposed for insurance consulted / diagnosed/taken
treatment/been admitted for any illness/injury. If Yes, give details. For insured person 1 the answer was
yes, Diabetes. Also, in Sr. No. 5.A. “Has the person proposed for insurance undergone any medical test?”
the answer was negative for the insured person. But the facts of MRI done on 06.02.2018 and various
consultations done prior to inception of policy were not revealed in the proposal form. In a contract of
insurance it is the bounden duty of the insured person to give the detail about his medical condition as
required in the proposal form.
As the insured was aware of his ailments at the time of submitting the proposal form, it was his duty to
disclose the same at the time of taking the policy and having not disclosed, it amounted to non
disclosure of material facts. Accepting the case laws quoted by RI, this Forum relies on the Hon’ble
Supreme Court of India’s decision in the case of Satwant Kaur Sandhu v/s. The New India Assurance
Company Limited IV (2009) CPJ 8 (S.C), wherein the Hon’ble court held:
“The upshot of the entire discussion is that in a Contract of Insurance, any fact
which would influence the mind of a prudent insurer in deciding whether to accept
or not to accept the risk is a "material fact". If the proposer has knowledge of such
fact, he is obliged to disclose it particularly while answering questions in the
proposal form. Needless to emphasise that any inaccurate answer will entitle the
insurer to repudiate his liability because there is clear presumption that any
information sought for in the proposal form is material for the purpose of entering
into a Contract of Insurance.”
Considering the above, this Forum is of the opinion that the complainant has breached uberrima fides
i.e. utmost good faith of insurance contract. Hence, the Complaint is dismissed
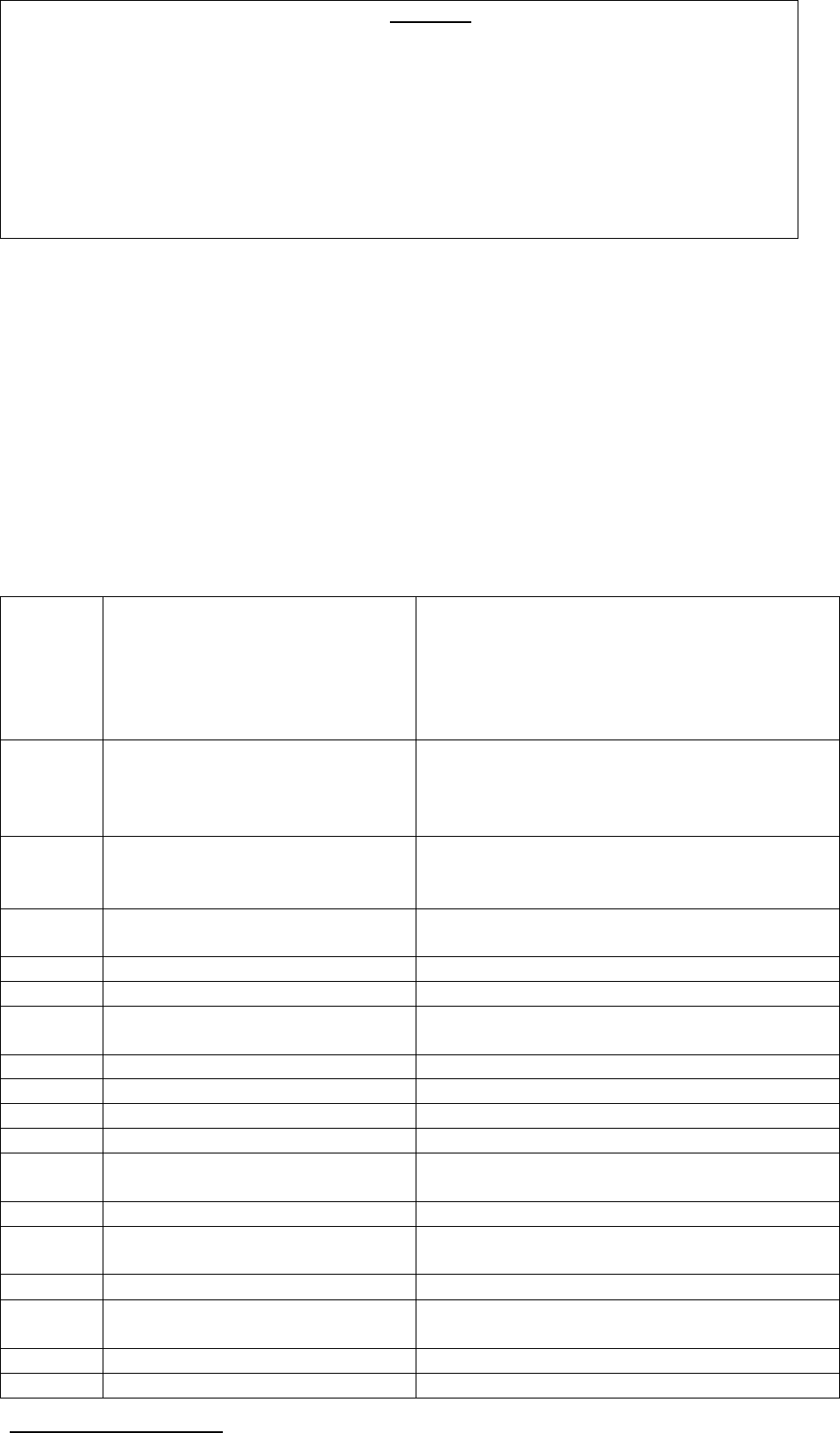
.
A W A R D
Taking into account of the facts and circumstances of the case and the submissions made
by both the parties and documents submitted during the course of the Personal Hearing,
the decision of the Respondent Insurer in repudiating the claims are in consonance with
the terms and conditions of the policy and does not warrant any interference at the hands
of the Ombudsman.
Hence, the Complaint is Dismissed.
Dated at Bangalore on the 6
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN –NEERJA SHAH
In the matter of: MR. S SUBBARAMA SHARMA V/s STAR HEALTH & ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-0316
Award No.: IO(BNG)/A/HI/0225/2019-20
1
Name & Address of the
Complainant
Mr. S Subbarama Sharma
#36, BBMP, #106, 2
nd
Main,
Muneshwara Nagar,
Subramanyapura Main Road,
Bangalore-560061
Mobile No.: 8088541151
2
Policy Number
Type of Policy
Duration of Policy/ Policy
Period
P/141111/01/2019/012953
Family Health Optima Insurance Plan
28.02.2019 to 27.02.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Mr. S Subbarama Sharma
Mrs. Radha C R
4
Name of the Respondent
Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
17.08.2018
6
Reason for repudiation
Non disclosure of Pre existing Diseases
7
Date of receipt of Annexure
VI-A
05.09.2019
8
Nature of complaint
Rejection of hospitalisation claim
9
Amount of claim
₹. 55,262/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹. 50,000/-
12
Complaint registered under
Rule no:
13 (1) (b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
12.12.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
Ms. Umadevi M B, Sr. Manager
Mr. Mahadevan G, Sr. Consultant
15
Complaint how disposed
Allowed
16
Date of Award/Order
13.12.2019
17. Brief Facts of the Case:
The complaint emanated from the rejection of claims on the ground that the treatment existed prior to
inception of the policy. The Complainant represented to Grievance Redressal Officer (GRO) of the
Respondent Insurer for reconsideration of his claim. However the claim was not settled. Aggrieved with
the decision of RI, he approached this forum for settlement of the claim.

18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant along with his wife was insured with RI for a floater sum insured of ₹. 4,00,000/- with
recharge benefit ₹. 1,00,000/- since 28.02.2019. It is submitted that policy was issued to the
complainant with declared PED “Diabetes Melitus and its complications” and to his wife with declared
PED “Hypertension and its complication”. His wife was admitted on 09.08.2019 in Sagar Hospitals,
Bangalore and discharged on 12.08.2019. She was diagnosed with infiltrating duodenal lesion with
ulceration/malignancy/Tuberculosis/HTN/hypothyroid disease and underwent upper GI endoscopy on
09.08.2019 and 10.08.2019. He applied for cashless preauthorization but it was denied. Subsequently,
he applied for reimbursement of medical expenses, but RI rejected the claim stating the insured person
was symptomatic since 6 months which was prior to inception of the policy. He represented to GRO to
consider his claim; however his claim was not settled. Hence the complainant approached this Forum
for settlement of his claims.
b) Respondent Insurer’s Arguments:
The Respondent Insurer in their Self Contained Note dated 24.11.2019 whilst admitting the insurance
coverage submitted that insured person underwent treatment for infiltrating duodenal lesion with
ulceration and the patient was symptomatic since 6 months which was prior to policy commencement.
Hence, the diagnosis is pre-existing disease and hence the claim was repudiated as per waiting period
exclusion 3 (iii) of the policy, the RI is not liable to make any payment in respect of expenses for
treatment of the pre-existing disease/condition, until 48 months of continuous coverage has elapsed,
since the date of commencement of the policy is 28.02.2019. The Respondent Insurer sought to absolve
them from the complaint made. It is also submitted that the maximum liability under the terms of the
policy shall be ₹. 57,303/-.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017 and so it was registered.
20. The following documents were placed for perusal.
Complaint along with enclosures,
Respondent Insurer’s SCN along with enclosures and
Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The issue which requires consideration is whether the complainant was suffering from the said illness
prior to the commencement of the policy.
During the personal hearing, both the parties reiterated their earlier submissions.
The forum notes from the Discharge Summary of Sagar Hospitals that the patient was having history of
dull pain abdomen on and off since 6 months and pain abdomen increased since 1 week. Also,
complaints of passing black stools, anorexia/nausea since 1 week.
It is also noted that all the diagnostic tests and investigations were carried out during her stay in hospital
or after that and it is only then she was diagnosed with the ailments.
The forum observed that there is no documentary evidence of the complainant having or was a known
case of infiltrating duodenal lesion with ulceration prior to the inception of the policy.
The forum relies on the Supreme Court Judgment in the case of Satwant Kaur Sandhu vs. The New India
Assurance Co. Ltd., wherein it is stated that disclosure of material facts extends only to facts which are
known to the applicant and not to what he ought to have known. The obligation to disclose necessarily
depends upon the knowledge one possesses. His opinion of the materiality of that knowledge is of no
moment.
During the course of hearing, representative of RI submitted that the claim falls under exclusion Pre-
existing disease. But, the RI has not established with documentary evidence that the complainant had
the knowledge of the existing ailments prior to inception of policy.
Considering the above, the decision of the RI is not in accordance with the terms and conditions of the
policy. Hence, the Complaint is hereby allowed with interest.

A W A R D
Taking into account the facts & circumstances of the case and the personal submissions
made by both the parties and the information/documents placed on record, the
respondent insurer is advised to settle the claim as per terms and conditions of the policy
along with interest @ 8.25% (Bank rate of 6.25% + 2%) from the date of filing of the last
relevant document by the Insured till the date of payment of the claim as per Regulation
16.1.(ii) of IRDAI (Protection of Policyholders’ Interests) Regulations, 2017.
Hence, the Complaint is Allowed.
23) Compliance of Award:
The attention of the Complainant and the Respondent Insurer is hereby invited to Rule 17 (6) of the
Insurance Ombudsman Rules, 2017, where under the Respondent Insurer shall comply with the Award
within 30 days of the receipt of the Award and shall intimate compliance of the same to the
Ombudsman.
Dated at Bengaluru on the 13
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of: MR. N S VASUDEVA M V/s STAR HEALTH AND ALLIED INSURANCE COMPANY
LIMITED
Complaint No: BNG-H-044-1920-0312
Award No: IO(BNG)/A/HI/0231/2019-20
1
Name & Address of the Complainant
Mr. N S Vasudeva
#863, 14
th
Cross,
Behind RJ Garden Apartment,
Indiranagar, 2
nd
Stage,
BENGALURU – 560 038
Mobile No.- 9731397815
2
Policy No.
Type of Policy
Duration of Policy/ Policy Period
P/141113/01/2019/011205
Family Health Optima Insurance Plan
12.01.2019 to 11.01.2020
3
Name of the Insured/ Proposer
Name of the policyholder
Mr. N S Vasudeva
Self
4
Name of the Respondent Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
NA
6
Reason for repudiation
NA
7
Date of receipt of Annexure VI-A
19.11.2019
8
Nature of complaint
Short settlement of claim
9
Amount of claim
₹. 30,590/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹. 3,453/- + compensation towards mental
agony
12
Complaint registered under Rule no:
13 (1) (b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
12.12.2019 / Bengaluru
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent Insurer
Dr. Umadevi, Sr. Manager
Mr. Mahadevan G, Sr. Consultant
15
Complaint how disposed
Dismissed

16
Date of Award/Order
16.12.2019
17. Brief Facts of the Case:
It is a case of short settlement of mediclaim on the ground of non-payable expenses as per
terms and conditions of the policy. The Complainant took up the matter with the Grievance Cell
of the Respondent Insurer (RI) and the same was not considered favourably.
18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant along with his wife was insured from 12.01.2019 to 11.01.2020 for sum
insured of ₹. 5,00,000/-. He was admitted to A V Hospital, Bangalore on 06.06.2019 with case of
severe onset of neck pain, chest pain, radiating to left shoulder and numbness in left hand. He
diagnosed as left upper limb cervical reticulopathy and discharged on 08.06.2019. He applied
for pre authorization of cashless treatment and Respondent Insurer (RI) approved ₹.27,137/-
out of total hospitalization bill of ₹.30,590/- towards settlement of claim. He applied to RI for
reconsideration of the balance claim; however his balance claim was not settled. Hence the
Complainant approached the Forum for settlement of his claim.
b) Respondent Insurer’s Arguments:
The Respondent Insurer not submitted their Self Contained Note, however vide their email
dated 24.10.2019, the Respondent Insurer RI considered the claim for balance amount for ₹.
1,575/-. Also it is submitted that the Complainant has confirmed the receipt of payment vide his
email dated 13.11.2019.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is for short settlement of claim due to non-payable expenses as per terms and
conditions of the policy.
During the course of personal hearing, the complainant reiterated that he has received Rs.
27,137/- towards cashless settlement and Rs. 1,575/- out of balance claim amount of Rs.
3,453/-. However RI has not given Vitamin D lab charges.
The representatives of RI submitted that as per exclusion 4.5 of the policy, vitamin D lab
charges are not payable.
The relevant policy term and condition quoted by the RI is reproduced as below:
Exclusion 4.5- “the Company shall not be liable to make any payments under this policy in
respect of any expenses what so ever incurred by the insured person in connection with or in
respect of nutritional deficiency states.”
The complainant reiterated that without analysing the deficiency in the body, how can doctor
treat the patient and hence the charges towards vitamin D test should be paid.
The forum notes from the exclusion 4.5 that nutritional deficiency states are excluded in the
policy. Hence, the decision of RI in denying charges towards such test is in order with the terms
and conditions of the policy.
Hence, the complaint is hereby dismissed.

A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral
submissions made by both the parties, this Forum is of the opinion that the decision of the
Respondent Insurer is in accordance with the terms and conditions of policy.
Hence, the complaint is Dismissed.
Dated at Bengaluru on the 16
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of: MR. ACHALCHAND P. JAIN V/s THE NATIONAL INSURANCE COMPANY LIMITED
Complaint No: BNG-H-048-1920-0317
Award No.: IO(BNG)/A/HI/0232/2019-20
1
Name & Address of the Complainant
Mr. Achalchand P Jain
M/s Mahaveer Creations,
#F-121, D K Line,
Chickper Cross,
Bangalore-560 053
Mobile No.: 9448347817
E-mail ID : mahaveercr[email protected]
2
Policy Number
Type of Policy
Duration of Policy/ Policy Period
604100501810000414
Parivar Mediclaim
10.06.2018 to 09.06.2019
3
Name of the Insured/ Proposer
Name of the policyholder
Mr. Achalchand P Jain
Self
4
Name of the Respondent Insurer
The National Insurance Company Limited
5
Date of repudiation
NA
6
Reason for repudiation
NA
7
Date of receipt of Annexure VI-A
21.11.2019
8
Nature of complaint
Short settlement of claim
9
Amount of claim
₹. 2,25,613/-
10
Date of Partial Settlement
Not Applicable
11
Amount of relief sought
₹. 2,25,613/-
12
Complaint registered under Rule no:
13 (1) (b) of Insurance Ombudsman Rules, 2017
13
Date of hearing/place
12.12.2019 / Bengaluru
14
Representation at the hearing
a) For the Complainant
Son ( Gautham Kumar Jain)
b) For the Respondent Insurer
Mr. S. Murali, Divisional Manager
Mr. Amarnadh Sadasivuni, Asst Manager
15
Complaint how disposed
Allowed
16
Date of Award/Order
16.12.2019
17. Brief Facts of the Case:
The Complaint emanated from short settlement of claim for hospitalization. The Complainant took up
the matter with the Grievance Cell of the Respondent Insurer (RI) and the same was not considered
favourably.
18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant along with Wife was insured with RI since 04.06.2007 and for the policy period
10.06.2018 to 09.06.2019 the sum insured was ₹.5,00,000/-. In May 2019, he was admitted to Shelchar
Hospital and the total hospital bill was ₹. 2,89,363/-. But the claim was settled for ₹. 50,000/-. Later
when he approached Grivance cell of RI, they have increased the claim amount by ₹. 13,750/- and

denied the balance claim quoting exclusion 4.3 of the policy and considering SI of ₹. 1,00,000/- & bonus
₹. 50,000/-. In spite of approaching the Grievance cell of RI, the balance claim was not settled and he has
approached this Forum.
b) Respondent Insurer’s Arguments:
The Respondent Insurer in their Self Contained Note dated 22.11.2019 whilst admitting the insurance
coverage submitted that insured person underwent treatment for calculus disease in May 2019 which
has 2 years waiting period as per clause 4.3 (xii) of the policy. Hence, they have considered SI for the
year 2016-17 i.e. ₹.1,00,000/- along with bonus ₹.50,000/- for calculation of claim amount. As per the
terms and conditions of the policy, total claim payout per illness is 50% of sum insured, hence, they have
settled the claim for ₹.63,750/-.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
Complaint along with enclosures,
Respondent Insurer’s SCN along with enclosures and
Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The dispute is for short settlement of claim as per the terms and condition of the policy.
During the course of personal hearing, complainant’s son submitted that his father was insured with RI
since 04.06.2007 and for present complaint, the total hospital bill was ₹.2,89,363/-. Although SI for the
policy period is ₹.5,00,000/-, RI settled only ₹. 63,750/- and refused to pay balance claim.
The representative of RI submitted that insured person underwent treatment for calculus disease in
May 2019 which has 2 years waiting period as per clause 4.3 (xii) of the policy. Hence, they have
considered SI for the year 2016-17 i.e. ₹.1,00,000/- along with bonus ₹.27,500/- for calculation of claim
amount. As per the terms and conditions of the policy, total claim payout per illness is 50% of sum
insured, hence, they have settled the claim for ₹.63,750/-.
The relevant policy terms and conditions quoted by the RI are reproduced as below:
3.33 Sum insured means the floater sum insured as mentioned in the schedule. The sum insured
represents maximum liability for the family, for any and all benefits claimed during the policy period.
3.37 Waiting Period means a period from the inception of the first policy during which specified
disease/treatment is not covered. On completion of the period, disease/treatment will be covered
provided the policy has been continuously renewed without any break.
4.3 Exclusion – Two years waiting period : The company shall not be liable to make any payment under
the policy in respect of any expenses whatsoever incurred by any insured person in connection with or in
respect of following disease/treatment subject to a waiting period of two years
Xii Calculus disease
Sublimit (a): total expenses incurred for any one illness is limited to 50% of sum insured.
On perusal of the available documents, the Forum notes that the complainant was insured with RI since
04.06.2007 and renewed his policies without any break as below:
Sr.
No.
Policy Number
Type of policy
Period of
insurance
Sum
insured
Remarks
1
604100/48/07/8500000272
Individual
mediclaim
04.06.2007 to
03.06.2008
₹.50,000/
2
604100/48/08/8500000253
Individual
mediclaim
04.06.2008 to
03.06.2009
₹.50,000/
3
604100/48/09/8500000293
Individual
mediclaim
04.06.2009 to
03.06.2010
₹.50,000/
4
604100/48/10/8500000322
Individual
mediclaim
04.06.2010 to
03.06.2011
₹.50,000/
5
604100/48/11/8500000375
Individual
mediclaim
04.06.2011 to
03.06.2012
₹.50,000/
6
604100/48/12/8500000355
Individual
04.06.2012 to
₹.50,000/

mediclaim
03.06.2013
7
604100/48/13/8500000380
Individual
mediclaim
04.06.2013 to
03.06.2014
₹.50,000/
8
604100/48/14/8500000416
Individual
mediclaim
04.06.2014 to
03.06.2015
₹.50,000/-
9
604100/50/15/10000410
Individual
mediclaim
10.06.2015to
09.06.2016
₹.1,00,000/-
SI enhanced to
₹.1,00,000/-
10
604100/50/16/10000440
Individual
mediclaim
10.06.2016 to
09.06.2017
₹.1,00,000/-
11
604100/50/17/10000475
Individual
mediclaim
10.06.2017 to
09.06.2018
₹.1,50,000/-
SI enhanced to
₹.1,50,000/-
12
604100/50/18/10000414
Floater policy
– Parivar
Mediclaim
10.06.2018 to
09.06.2019
₹.5,00,000/-
Type of policy
changed and SI
enhanced to
₹.1,00,000/-
The representative of RI argued that the condition of enhanced sum insured is mentioned in Individual
Mediclaim Policy which has a waiting period 2 years for the enhanced sum inured.
The Forum notes that the hospitalization of the complainant for calculus disease is under Parivar
Mediclaim Policy and not under Individual mediclaim policy. On perusal of the Parivar mediclaim policy
it observes that condition of increased or enhanced sum insured requiring a waiting period of 2 years is
not mentioned anywhere in the policy. Representatives of RI concurred with this observation during the
personal hearing.
In the absence of any condition restricting the SI or waiting period in the policy document, the decision
of RI in limiting SI to ₹.1,00,000/- is not in order. Hence, the Forum directs the RI to settle the claim
considering SI for the policy period 2018-19 i.e. ₹.5,00,000/-, considering Sublimit (a) to 50% of sum
insured as mentioned above.
Hence, the complaint is Allowed.
A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral submissions
made by both the parties, this Forum is of the opinion that the decision of the Respondent Insurer is
not in accordance with the terms and conditions of policy and not found to be in order.
This Forum directs the Respondent Insurer to settle the balance claim as above as per the terms and
conditions of policy along with interest @ 6.25% + 2% from the date of receipt of last necessary
documents to the date of payment of claim, as per regulation 16 (1) (ii) of Protection of Policy holders’
Interests of IRDA Regulations, 2017 issued vide notification dated 22.06.2017.
Hence, the complaint is ALLOWED.
24) Compliance of Award:
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. The Complainant shall submit all requirements/Documents required for settlement of award within
15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall comply with the
award within thirty days of the receipt of the award and intimate compliance of the same to the
Ombudsman.
Dated at Bangalore on the 16
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
Case of: Mr.PRAVEEN P V/s RELIGARE HEALTH INSURANCE COMPANY LIMITED
Complaint No: BNG-H-037-1920-0295
Award No: IO/BNG/H/037/200
1
Name & Address of the
Complainant
Mr. Praveen P
No.37, Sree veerabhadreshwara Nelya,
1
st
Main, 9
th
Cross, Kalyan Nagar,
T Dasarahalli, Bangalore 560057
Ph.9164524401
Email: [email protected]
2
Policy No.
Type of Policy
Duration of Policy/Policy Period
Date of Admission/Discharge
13504345
Religare Health Insurance
06.01.2019 to 05.01.2020
15.09.2019/18.09.2019
3
Name of the Insured/ Proposer
Name of the policyholder
Mr. Praveen P
4
Name of the Insurer
Religare Health Insurance
5
Date of Repudiation/Rejection
26.09.2019
6
Reason for Repudiation/Rejection
Non disclosure of PED
7
Date of receipt of Annexure VI A
06.11.2019
8
Nature of complaint
Rejection of claim
9
Amount of claim
Rs.57,000/-
10
Date of Partial Settlement
N.A.
11
Amount of relief sought
Rs.57,000/-
12
Complaint registered under Rule
no
13 (1) (d) of Insurance Ombudsman Rules, 2017
13
Date of hearing/place
05.12.2019
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent
Insurer
1) Dr. Channakeshava Prasad, zonal
Manager
2) Dr.Bhaveesh Patwari, Manager
15
Complaint how disposed
Disallowed
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case: -
The complaint is for non-settlement of claim under non-disclosure of Pre-existing Diseases. Though the
Complainant contended that the said PEDs had no nexus with the subject claims, the insurer stuck to
their earlier decision of rejection of claim. Being aggrieved with non-consideration of his request, the
Complainant approached this Forum.
18. Cause of Complaint: -
a)Complainants argument:
The Complainant had taken the Health Insurance policy from National insurance Company Limited from
2013 through agent Ratna Associates and ported the same to Religare Health Insurance in 2019. The
Complainant’s father Mr. Parameshwarappa R K was admitted to Ramaiah Memorial Hospital,
Bengaluru from 15/09/2019 to 18/09/2019 for complaints of fever since 3 days cough with
expectoration since 2 days and alleged h/o giddiness and fall in bathroom and was finally diagnosed
with viral fever with thrombocytopenia. His present complaint of fever and head wound is not related to
pre existing ailment craniotomy which happened 10 years back.
However, the Respondent Insurer did not consider his request. Hence, the Complainant approached
this Forum for settlement of his claims.
b) Respondent Insurer’s Arguments:
The Respondent Insurer in their Self Contained Note dated 08.11.2019 that the complainant has not
made any representation to the Respondent Insurer (R I). During the currency of the policy while the

cashless claim request got triggered the R I found from the documents/records submitted by the
hospital that the patient was having a history of head surgery Craniotomy which the insured failed to
disclose in the proposal form a nd medical examination form.
The Complainant did not disclose the said illnesses, which amounted to wilful non-disclosure of material
facts and pre-existing diseases and thus, caused the breach of basic insurance principle of utmost good
faith and invoked condition no. 7.1. Therefore, the Insurance Policy stands void abinitio. It was further
submitted that, had the Complainant disclosed the above medical condition, the policy would not have
been issued/underwritten.
The respondent insurer accordingly denied the reimbursement claim request vide their letter dated
26.09.2019.
The Respondent Insurer also relied on the Supreme Court decision in case of Satwant Kaur Vs. New India
Assurance Co Ltd., and National Consumer Disputes Redressal Forum’s decision in the case of LIC Vs.
Smt. Neelam Sharma. They sought for absolving them from this complaint.
19. Reason for Registration of Complaint: -
The Complaint falls within the scope of the Insurance Ombudsman Rules, 2017 and so, it was registered.
20. The following documents were placed for perusal: -
j. Complaint along with enclosures,
k. SCN of the Respondent Insurer along with enclosures along with the enclosures and
l. Consent of the Complainant in Annexure VI A & Respondent Insurer in Annexure VII A
21. Result of personal hearing with both the parties (Observations & Conclusions): -
Based on the documents on record and the submissions made during the personal hearing, the issue for
consideration is whether the Insured had wilfully non disclosed the Craniotomy at the time of porting
the policy. .
21.1. The Respondent Insurer’s representative reiterated their earlier submissions.
21.2.The Forum observes from the Proposal form submitted at the time of portability that the insured
has filled the column in negative which reads as “ Has any of the proposed insured been
hospitalised/recommended to take investigations/medication or has been under any prolonged
treatment /undergone any surgery for any illness/injury other than for childbirth/minor injuries.
21.3. Whilst the Complainant is agitating for the denial of claim on the pretext that the said PEDs had no
nexus with the present treatment, he does not deny the pre-existence of the same at the inception of
the Policy. Thus, the Forum has no hesitation to infer that the Complainant was suffering from the said
illness, prior to taking the policy and failed to disclose the same in the Proposal Form as well as in the
medical examination form, which amounts to non-disclosure of pre-existing medical condition.
21.4. In the light of the Respondent Insurer’s assertion that, had the pre-existing position been declared
whilst taking the first policy, the proposal would not have underwritten/accepted on the same terms
and conditions, the Forum upholds their decision of repudiation of the claim.
21.5. The Forum relies on the Supreme Court decision in the case of Satwant Kaur Sandhu vs The New
India Assurance Company Limited dated 10.07.2009 to arrive at the decision.
AWARD
Taking into account of the facts and circumstances of the case and upon scrutiny of the documents
submitted by both the parties, the decision of the Respondent Insurer is found to be in order and
does not requirement any interference at the hands of the Ombudsman.
The Complaint is Disallowed.
Dated at Bengaluru on the 6
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
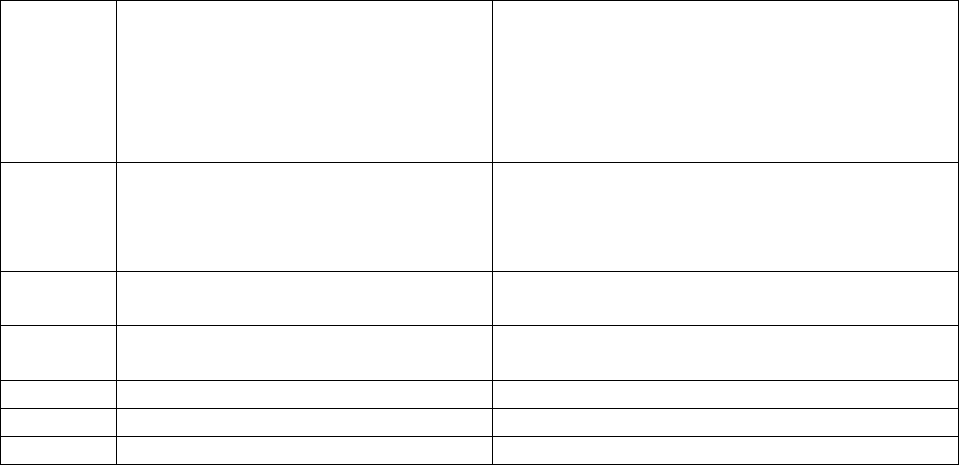
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of: MR. SUGUMAR D v/s MAX BUPA HEALTH INSURANCE COMPANY LTD
Complaint No: BNG-H-031-1920-0290
Award No: IO(BNG)/A/HI/0206/2019-20
.
• The Complaint emanated from cancellation of insurance policy by Respondent Insurer (RI) for
non disclosure of Pre-Existing disease.
• Complainant submitted that he is a known case of CKD since 2007 and was on dialysis since
then. RI issued Heart Beat Family First policy to the complainant in 2012 based upon the
declaration made in proposal form.
• When complainant approached RI for claim under the policy in 2014, RI repudiated claim on the
ground that complainant had not disclosed his condition regarding CKD in proposal form at time
of taking the first policy in 2012. Proposal form has been produced by RI to this forum.
• Complainant contested that RI’s employee had promised that he would be covered after 48
months from taking the policy in 2012. RI allowed policy to be continued after declaration of
past medical condition to RI in December 2014. Copy of letter communication addressed to
Branch Manager of RI as well as e-mail communication to Grievance Redressal Officer (GRO) has
been produced by the complainant. Furthermore, RI had admitted claims under the policy in
2017 for diagnosis of CKD.
• Complainant was hospitalised again in 2019. On scrutiny of medical documents RI rejected the
claim for non-disclosure of Pre-existing Disease of CKD and Chronic IGA Nephropathy (BX 2007)
and cancelled the policy.
• Complainant once again approached GRO of RI for reinstatement of policy for future benefits.
However the same was not considered favourably. Aggrieved he approached this forum for
revival of the policy. The complaint was posted for personal hearing on 05.12.2019.
• After registering the complaint with this office, RI has agreed to reinstate the policy vide mail dt
29.11.2019 and complainant has given consent for the same to RI vide mail dt 02.12.2019.
• The complaint was resolved on compromise basis and hence, the Complaint is treated as Closed
and Disposed off accordingly.
Dated at Bengaluru on the 6
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN - NEERJA SHAH
In the matter of: Karkala Maruthi Prasad Vs MAX BUPA HEALTH INSURANCE COMPANY LIMITED
Complaint No: BNG-H-031-1920-0269
Award No: IO/(BNG)/A/HI/210/2019-20
1
Name & Address of the
Complainant
Mr. Karkala Maruthi Prasad
No.2355, Second Floor,
24
th
Main, Sector 1, HSR Layout,
Bangalore – 560102
Ph.9886043774
maruthiprasadk@yahoo.com
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
30122043201806
Max Bupa Health Insurance
(Hearbeat Silver 3L 2A1C)
09.08.2019 to 08.08.2019
3
Name of the Insured/ Proposer
Name of the policyholder
Mr. Karkala Maruthi Prasad
4
Name of the Respondent
Insurer
Max Bupa Health Insurance Company
Limited
5
Date of repudiation/rejection
16.08.2019
6
Reason for repudiation
Cancellation of policy
7
Date of receipt of the Consent
25.09.2019

(Ann VI A)
8
Nature of complaint
Cancellation of policy
9
Amount of claim
NA
10
Date of Partial Settlement
N.A.
11
Amount of relief sought
NA
12
Complaint registered under
Rule no:
13(1) (b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
21.11.2019 / Bengaluru
14
Representation at the hearing
a) For the Complainant
Requested for postponment
b) For the Respondent
Insurer
Ms. Shital Patwa, Manager, Legal
15
Complaint how disposed
Closed
16
Date of Award/Order
06.12.2019
17. Brief Facts of the Case:
The Complainant arose out of the cancellation of policy on the basis of non disclosure of facts. He
received a mail dated 16/08/2019 from the respondent insurer stating that they would not be able to
continue the policy as they found non disclosure of kidney seizure disorder by him. Hence the
Complainant approached this Forum for reinstatement of the cancelled policy.
18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant obtained Max Bupa Health Insurance covering himself and his wife and son for the
period from 09.08.2018 to 08.08.2019 for a base Sum Insured of ₹. 3,90,000/- with a loyalty addition
amount accrued of Rs. 90,000. He has insurance since 2012. He has been paying premium regularly
since 2012 except in 2019 wherein the dispute arose. While filling the proposal form, he had informed
the sale representative about complex partial seizure suffered by the insured person. He sent email to
Max Bupa in 2017 about correction of PED in the policy. Max Bupa communicated that after 4 years and
as per inception policy document PED void for him and his wife.
He received a mail dated 16/08/2019 from the respondent insurer stating that they would not be able
to continue the policy informing discontinuance of the policy on the grounds of non disclosure of kidney
seizure disorder.
Complainant feels aggrieved by the of cancellation of policy since he has never made a claim even once
during these years and requested for getting back the policy or return of all premiums paid by him.
b) Respondent Insurer’s Arguments:
The Respondent Insurer contended during the hearing that insured person’s complaint is being solved
and policy will be reinstated.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017 and so it was registered.
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A.
21. Result of personal hearing with both the parties (Observations & Conclusions):
21.1. Complainant sought postponement of hearing whereas R I attended the hearing wherein they
offered settlement of the issue.
21.2 This Forum has perused the documents available on record and find that Complainant received a
mail dated 07/11/2019 from the respondent insurer offering one time settlement further stating that
the company shall reinstate the captioned policy with all the continuity benefits subject to receipt of
conditional consent and renewal premium from the complainant and simultaneous withdrawal of
present complaint.
21.3 R I have sent a mail dated 14.11.2019 confirming reinstatement of Heart beat silver health
Insurance policy with all the continuity benefits and coverage of pre existing disease policy in future.

21.4 The policy was reinstated vide policy number30122403201907 for the period from 09.08.2019 to
09.08.2020 with a continuity benefits of the policy and the softcopy of the policy was sent to the
complainant by Respondent Insurer.
21.5 As the policy is reinstated with continuity benefits, the complaint may be disposed off and Closed.
A W A R D
Taking into account of the facts and circumstances of the case and the submissions made and
documents submitted during the course of the Personal Hearing/mail, the decision of the Respondent
Insurer in renewing of the policy with continuity benefits are in consonance with the terms and
conditions of the policy and does not warrant any interference at the hands of the Ombudsman.
Hence the complaint is disposed off and closed.
Dated at Bangalore on the 06
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of: MR. VINOD KUMAR AGARWALA v/s THE ORIENTAL INSURANCE COMPANY LTD
Complaint No: BNG-H-050-1920-0293
Award No: IO/(BNG)/A/HI/0218/2019-20
1
Name & Address of the Complainant
Mr. VINOD KUMAR AGGARWALA
A-1103, Summer Block
Shilpitha Sunflower Borewell Road,
Whitefield, BENGALURU – 560 066
Mobile # 9971094467
E-mail: vkagarwala1[email protected]om
2
Policy No.
Type of Policy
Duration of Policy/ Policy Period
215100/48/2019/76
Individual Mediclaim Insurance Policy
20.04.218 to 19.04.2019
3
Name of the Insured/Proposer
Name of the Insured Person
Mr. Vinod Kumar Aggarwala
Self
4
Name of the Respondent Insurer
The Oriental Insurance Company Limited
5
Date of Repudiation
NA
6
Reason for repudiation
NA
7
Date of receipt of Annexure VI-A
30.10.2019
8
Nature of complaint
Delay in settlement of claim
9
Amount of claim
₹. 1,84,543/-
10
Date of Partial Settlement
23.09.2019
11
Amount of relief sought
₹. 1,84,543/-
12
Complaint registered under Rule no.
13(1)(a) of Insurance Ombudsman Rules, 2017
13
10.01.2019
05.12.2019 /Bengaluru
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent Insurer
1) Dr Raghvendra, Dy Manager
2) Mr. Sivakumar, Asst. Manager
2) Mr. Dilip Kumar, AO
15
Complaint how disposed
Allowed
16
Date of Award/Order
09.12.2019
17. Brief Facts of the Case: -
The complaint emanated from the delay in settlement of the reimbursement of hospitalisation claim.
Despite representing to Grievance Redressal Officer (GRO) of Respondent Insurer (RI), the claim was not
settled. Hence, the Complainant approached this Forum for settlement of his claim.
18. Cause of Complaint: -
a) Complainants argument:

The Complainant obtained the cited policy covering himself and his wife for a floater Sum Insured of ₹.
4,00,000/-. He had continuous insurance since 20.04.2007. The Complainant was admitted in Columbia
Asia Hospital, Bengaluru in semi-conscious state in Emergency Section from 27.02.2019 till 04.03.2019
for diagnosis of Acute on Chronic SDH (Right side). Neurosurgery was performed by Dr Tejus M Rao on
27.02.2019. Complainant availed cashless authorisation request and was sanctioned payment of ₹.
1,88,995/- on discharge. Out of total bill of ₹. 3,68,238/-, balance ₹. 1,79,243/- was paid by him.
Expenses towards post-hospitalisation expenses were ₹. 7,012/-. He preferred a reimbursement claim to
RI for the balance amount towards hospitalisation and post-hospitalisation expenses on 04.05.2019. A
meagre amount of ₹. 1,712/- was paid to him on 23.09.2019 without any intimation regarding status of
balance amount claimed. Despite representing to the RI, the claim was not settled. Hence the
Complainant approached this Forum for settlement of his claim.
b) Respondent Insurer’s Arguments:
The Respondent Insurer, in their Self Contained Note (SCN) dated 29.11.2019 submitted that SI (Sum
Insured) under the policy was increased from ₹. 3 lacs to ₹. 4 lacs from 2016-17. At the time of pre-
authorisation, erroneously ₹. 3 lacs was considered. However now upon revisiting the claim, they have
allowed further payment of ₹. 77,409/- (₹. 76,409/- towards hospitalisation and ₹. 1,000/- towards post
hospitalisation expenses) as per the following calculation:
HEAD
ENTITLED
AMT (RS)
CLAIMED
AMT (RS)
APPROVED
AMT (RS)
DEDUCTED
AMT (RS)
REASON
ICU Charges
+ Nursing
charges
2% of SI
22500
16000 (8000x2)
6500
ICU difference
deducted
Room Rent
+ Nursing
charges +
RMO
1% of the SI
29100
12000 (4000x3)
17100
Room rent
difference
deducted
Investigation
Charges
63290
34344
28946
Room rent &
ICU linked
proportionate
deduction
Consultation
Charges
14599
7922
6677
Room rent &
ICU linked
proportionate
deduction
Medicines &
consumables
64469
64469
0
Surgery
charges
147412
79992
67420
Room rent &
ICU linked
proportionate
deduction
Other
charges
26869
16348
10521
Room rent & ICU
linked
proportionate
deduction + Food
charges- 715/-
+Admission
charges-1250/- +
Registration
charges-313/-
+Ambulance
charges- 940/- +
admin charges-
646/-
Co-pay
NA
NA
0
0
Total
Amount
368238
231075
137164
Final Bill Amount
368238
Admissible amount
231075
Amount already settled
154666
Difference amount payable further
76409
Out of Post hospitalization expenses for Rs.7012/-; RI already settled Rs.1712/- and Rs.5300/- was
deducted. Further Rs.1000/- (Consultation Bills dtd. 07.03.19 for Rs.250/- and dtd. 09.04.19 for Rs.750/-)

was received on 23.07.19, hence it is payable. Rs. 4300/- Report of CT Brain dtd. 09.04.19 was not
available, hence was not payable.
19. Reason for Registration of Complaint: -
The complaint was registered as it falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal: -
Complaint along with enclosures,
SCN of the Respondent Insurer along with enclosures along with the enclosures and
Consent of the Complainant in Annexure VI A & Respondent Insurer in Annexure VII A.
21. Result of personal hearing with both the parties (Observations & Conclusions): -
The forum has perused the available documents on records and submissions made by both the parties
during the personal hearing.
During the personal hearing, both the parties reiterated their earlier submissions.
The hospitalisation claim is not disputed by RI. Furthermore, RI has agreed to settle the claim for
additional ₹. 77,409/- as per revised calculation.
Perusal of policy terms and conditions do not lay down that coverage under the policy will be restricted
proportionately to room rent/ICU charges. Furthermore the hospital is a PPN network Hospital. Hence RI
is not correct in deducting claim amount in proportion to room rent charges on the ground that it is
required as per terms and conditions of the policy.
Further, as per Coverage Clause 1.2 (f), complainant is eligible for Daily Hospital Cash Allowance for 0.1%
of SI for max of 6 days, subject to deductible of 02 days for a claim admissible under the policy under
continuous hospitalisation.
Furthermore, as per Coverage Clause 1.2 (e) Ambulance service charges are payable upto ₹. 2,000/- or
1% of SI, whichever is less per hospitalisation subject to aggregate expenses not exceeding ₹. 4,000/-
under the policy.
In view of above, RI is directed to re-examine the claim and settle the claim in full (i.e. without any
proportionate deduction) as per eligibility subject to terms and conditions of the policy
Hence, the complaint is hereby allowed.
A W A R D
Taking into account of the facts and circumstances of the case and the submissions made by both
the parties and documents submitted during the course of the Personal Hearing, the Respondent
Insurer is advised to re-examine the claim in full without applying proportionate deduction clause,
subject to eligibility as per terms and conditions of the policy, along with interest @ 8.25% (Bank
rate of 6.25% + 2%) from the date of filing of the last relevant document till the date of payment
of the claim as per regulation 16 (1) (ii) of Protection of Policy holders’ Interests Regulations, 2017
issued by IRDAI vide notification dated 22.06.2017.
The Complaint is ALLOWED.
22. Compliance of Award:
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. The Complainant shall submit all requirements/Documents required for settlement of award within
15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall comply with the
award within thirty days of the receipt of the award and intimate compliance of the same to the
Ombudsman.
Dated at Bengaluru on the 9
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of MRS. YASHODAMMA V/s APOLLO MUNICH HEALTH INSURANCE COMPANY LIMITED
Complaint No: BNG-H-003-1920-0328
Award No.: IO(BNG)/A/HI/0223/2019-20
1
Name & Address of the
Complainant
Mrs. Yashodamma
W/o HG Ananda
JC Extension Holalkere (post)
Chitradurga Distt,
KARNATAKA - 577 526
Mob No: 9243253699
2
Policy /Cert. No.
Type of Policy
Duration of Policy/ Policy
Period
120100/12001/2018/A012706/800
Easy Health Group Insurance
16.03.2019 to 15.03.2020
3
Name of the Insured/
Proposer
Name of the policy holder
Mrs. Yashodamma
Self
4
Name of the Respondent
Insurer
Apollo Munich Health Insurance Company
Limited
5
Date of repudiation/rejection
18.10.2019
6
Reason for repudiation
Non-disclosure of PED
7
Date of receipt of Annexure
VI-A
19.11.2019
8
Nature of complaint
Reinstatement of Policy with coverage of
PED after completion of 48 months
9
Amount of claim
NA
10
Date of Partial Settlement
NA
11
Amount of relief sought
Reinstatement of Policy with coverage of
PED after completion of 48 months
12
Complaint registered under
Rule no:
13 (1) (f) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
12.12.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Absent
b) For the Insurer
Dr. Yashwant, Sr. manager
15
Complaint how disposed
Allowed
16
Date of Award/Order
13.12.2019
17. Brief Facts of the Case:
The complaint emanated from the cancellation of Insurance policy on the ground of non disclosure of
PED (Pre-Existing Diseases). The Complainant approached the GRO of the Respondent Insurer (RI), but
the same was not resolved. Hence, the Complainant has approached this Forum.
18. Cause of Complaint:
a. Complainant’s arguments:
Complainant submitted that she is an illiterate person, a senior citizen and holder of Canara Bank
Savings A/c No 0453101021677. On basis of recommendation of Branch Manager, Canara Bank,
Holalkere she enrolled for Group health policy (Easy Health Group Insurance) with RI on 16.03.2017 for
Sum Insured of ₹. 5,00,000/- and renewed continuously till 16.03.2019 without any break. Since Canara
Bank was an intermediary of RI, Branch Manager told her that being a Group policy, no medical tests
were required at time of taking the policy and it would cover all illness/PED. Subsequently she was
admitted to Columbia Asia Hospital on 26.03.2018 for diagnosis of OSA with Co2 Narcosis, DM and HTN.
She submitted a cashless pre-authorisation request, which was denied on 31.03.2018 for non-disclosure
of past history of COPD, OSA, IHD since 2016, which was prior to inception of first policy coverage with
RI. On 28.08.2018 she submitted letter to Branch Manager, Canara Bank not to renew health insurance
policy by debiting her Savings A/c with bank branch. Nonetheless the policy was renewed. She again
gave a reminder notice on 29.06.2019 to Branch Manager, Canara Bank. The Branch Manager thereafter
informed her that PED will be covered and claims will be settled soon and asked her to resubmit the
claim. Accordingly she filed reimbursement claim on 09.10.2019 vide claim no 1157566. Meanwhile she
was again admitted to Columbia Asia Hospital on 17.10.2019 and obtained cashless pre-authorisation
approval for ₹. 30,000/- on 18.10.2019 vide claim no 672202/2. On same day, she was given 30 days
notice for cancellation of policy for previous claim (Claim No: 1157566). On 26.10.2018, the cashless

facility was denied as scrutiny of DS (Discharge Summary) which revealed that she had past history of
Severe OSA. She approached this forum against cancellation of policy and contested that RI was aware
of her medical condition in 2018 and still policy was renewed in 2019.
b. Respondent Insurer’s Arguments:
The Respondent Insurer vide their mail dt 09.12.2019 has agreed to settle the claim for ₹. 2,25,987/-
without revival of policy.
19. Reason for Registration of complaint:
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal:
m. Complaint along with enclosures,
n. Respondent Insurer’s SCN along with enclosures and
o. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
Complainant vide his mail dt 11.12.2019 submitted that she has agreed to payment of ₹. 2,25,987/-
from RI and will not be attending the personal hearing.
The forum has perused the documentary evidence available on record and submissions made by RI
during the personal hearing. The dispute is with regard to
(a) Acts of omission or commission of Intermediary in contract of insurance policy
(b) Renewal of insurance medical records when claim was denied by RI on basis of non-disclosure of
previous medical history in the past.
As per Regulation 26 (to be read with Schedule III) of Registration Of Corporate Agents Regulations,
2015 issued by IRDAI, certain guidelines for code and conduct of Corporate Agents are specified. While
reiterating these regulations, IRDAI issued circular IRDA/CAGTS/ClR/MSL/1 5210812016 dt 01.08.2016
noting therein that lnsurance policies were issued by Banks under Corporate Agency of Insurers without
obtaining consent of their customers, without obtaining their signatures and/or the policy documents
issued with incorrect contact details
In present case, clearly the Intermediary has violated the regulations as laid down by regulator as per
Schedule III, General Code of Conduct which states that: Every corporate agent shall follow recognised
standards of professional conduct and discharge their duties in the interest of the policyholders. Inspite
of complainant having submitted written letter to Bank for not renewing the policy, the renewal
premium was deducted from her account without consent. This is violation of the regulations and
circular issued by the Insurance regulator.
‘
Sub regulation 5 of Regulation 8 of Insurance Regulatory and Development Authority of India
(Registration Of Corporate Agents) Regulations, 2015 lays down that “The insurer shall be responsible for
all acts and omissions of its agents including violation of code of conduct specified under these
Regulations, and shall be liable to a penalty which may extend to one crore rupees.” In view of above, RI
is advised to apprise their Corporate Agent of the violations committed by them and not to repeat them
in future.
As regards dispute for policy cancellation subsequent to claim denial, RI vide its mail dt 09.12.2019 has
confirmed that as a customer centric approach, they are willing to settle claim for ₹. 2,25,987/- without
revival of said policy. Since RI has agreed to settle the claim amount as per terms and conditions of the
policy, this forum does not wish to interfere with decision of RI with regards to claim liability.
Forum notes that Regulation 27 of Insurance Regulatory And Development Authority Of India (Health
Insurance) Regulations, 2016 (amended on 19.11.2019) states that “The information that the insurer has
captured in the proposal form at the time of accepting the proposal, the terms & conditions offered
under the policy, the medical history as revealed by earlier claims, if any, and the prior claims experience
shall all be maintained by the insurer as an electronic record and shall not be called for again from the
policyholder/insured at the time of subsequent claim settlements.” RI was aware of the fact that
Complainant had past medical history of OSA when it repudiated claim no 1157566 on 31.03.2018.
Despite this, the policy was not cancelled by RI and subsequently renewed on 16.03.2019. Even for its
repudiation mentioning that complainant was suffering from OSA, COPD and IHD since 2016, RI has not
produced any documentary record to prove the fact that there was a non-disclosure at time of inception
of policy in 2017. Hence RI has not acted in a fair and transparent manner with regard to policy servicing
guidelines as mentioned above. Hence the forum extends the benefit to complainant and directs RI to
revive the cancelled policy.
The Complaint is Allowed.

A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral
submissions made by both the parties, this Forum does not interfere with the decision of RI to
settle claim for ₹. 2,25,987/-. The forum extends the benefit to the complainant and directs RI
to revive the cancelled policy.
Hence, the complaint is ALLOWED.
23. Compliance of Award:
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. The Complainant shall submit all requirements/Documents required for settlement of award within
15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall comply with the
award within thirty days of the receipt of the award and intimate compliance of the same to the
Ombudsman.
Dated at Bengaluru on the 13
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of MR. K R DATTATREYA Vs STAR HEALTH & ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-0315
Award No.: IO/(BNG)/A/HI/0227/2019-20
1
Name & Address of the
Complainant
Mr. K R Dattatreya
106, 1st Main, M S Ramaiah City,
J P Nagar,
Bangalore – 560077
Ph. 9886254629
Email: tigervishwa[email protected]
2
Policy Number
Type of Policy
Duration of Policy/ Policy
Period
P/141128/01/2019/003575
Senior Citizen Red Carpet Health Insurance
10.10.2018 to 09.10.2019
3
Name of the Insured/
Proposer
Name of the policyholder
Ms. A V Vanajakshi
4
Name of the Respondent
Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
02.08.2019
6
Reason for repudiation
Rejection of claim for non-disclosure of
PED
7
Date of receipt of Annexure
VI-A
08.11.2019
8
Nature of complaint
Repudiation of claim
9
Amount of claim
₹. 5,00,000/-
10
Date of Partial Settlement
Not Applicable
11
Amount of relief sought
₹. 30,00,000/-
12
Complaint registered under
Rule no:
13 (1) (d) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
12.12.2019 / Bengaluru
14
Representation at the
hearing

a) For the Complainant
Self
b) For the Respondent
Insurer
1. Mr. Mahadevan, Sr.Consultant
2. Dr.Umadevi, Sr. Manager
15
Complaint how disposed
Disallowed
16
Date of Award/Order
13.12.2019
17. Brief Facts of the Case:
The complaint emanated from the rejection of the claim and cancellation of coverage for his wife Mrs. A
V Vanajakshi on the grounds of non-disclosure of pre-existing disease.
18. Cause of Complaint:
a) Complainant’s arguments:
Insured person took the policy with effect from 10.10.2017 and had declared her diabetic condition
before the inception of policy. Prior to Oct 2017 she went to Manipal Hospital for checkup as she was
experiencing pain in her shoulder and underwent Angiography on the advice of doctor. However the
report was negative showing no blockages and surgery ruled out for Angioplasty.
Out of precaution she once again went to Apollo Hospital for second opinion wherein she was once
again subjected to angiogram procedure. Here also report did not show any blockages and Angioplasty
was ruled out. The claim for compensation was rejected by the Respondent Insurer (R I) on the grounds
that she did not disclose her Heart Condition at the time of taking the policy which amounted to non
disclosure of facts.
Once again in July 2019 she developed shoulder pain and was admitted to Apollo Hospital from
27/07/2019 to 09/08/2019 where she was subjected to various tests and treatments and was kept as
inpatient for 14 days and saddled with the bill of around Rs.5,00,000/-.
RI sent a letter dt.03.08.2019 rejecting the claim on the ground that insured failed to disclose the pre
existing Heart disease in the proposal form at the time of inception of the policy and sent a letter dated
05/08/2019 giving notice for cancellation of the policy wef 14/09/2019.
RI sent a letter dt.09.08.2019 seeking certain documents creating hope in the mind of the complainant
and reiterates that the complainant neither at the time of inception of the policy nor later had any heart
disease and question of non disclosure/pre existing disease does not arise. . Insured claimed Rs.5 Lacs
towards amount spent and Rs.25 Lacs towards mental agony and financial hardship.
b) Respondent Insurer’s Arguments:
The Respondent Insurer in their Self Contained Note (SCN) dated 09/12/2019 submitted that the insured
person has made 2 claims during the 2
nd
year of Policy.
1
st
Claim : Insured person (IP) was admitted on 27.05.2019 at Apollo Hospital and was discharged on the
same day. As per dishcharge summary (DS) the insured was diagnosed as Effort Angina, sinus rhythm,
adequate LV systolic function, CAG insignificant Coronary Artery Disease, DM Type II, Hypertension and
undergone CAG- standard procedure. Query was raised to the complaiant to submit DCM’s consultation
paper, DS treatment records with CAG 2016 and consultation investigation reports of AWMI, and all
other investigation reports. Subsequently Insured submitted few documents only. Inspite of reminder
the insured did not submit all the required documents mandatory to process the claim. Hence the claim
was rejected vide letter dated 08.09.2019.
2
nd
Claim : IP was again admitted from 27.07.2019 to 09.08.2019 in the same Apollo Hospital. As per DS
the IP was diagnosed as Pyrexia of unknow origin generalised lymphadenopathy, Atropic Gastritis,
sjogrens Syndrome DM Type 2, IHD and undergone Iliac Lymph Node Biopsy. Patient history from Apollo
hospital records showed past history of hernia and varicose vein surgery. Query was raised wrt exact
duration of IHD and sjogrens syndrome and records of Hernia and Vericose vein surgery done
previously. The mandatory required documents were not submitted by the insured. Hence claim was
rejected vide their letter 11.10.2019.
They submitted that It is the duty of the insured to disclose all the material facts to the insurer to enable
them to evaluate the proposal . Insurance contract is based on utmost good faith. However the above
medical condition was not disclosed in the proposal form submitted which amounted to non-disclosure
of material fact making the contract of insurance voidable as confirmed by Supreme Court in Satwant
Kaur Sandhu vs. New India Assurance Co. Ltd., (2009) 8 SEC 316.
The claims were repudiated as per condition no. 9 of the policy, ‘if there is any misrepresentation/non
disclosure of material facts whether by the insured person or any other person acting on his behalf, the
Company is not liable to make any payment in respect of any claim”.
The policy was cancelled wef 14.09.2019 by sending 30 days time notice on 05.08.2019 by invoking
condition no. 13 of the policy, ‘’the company may cancel this policy on grounds of misrepresentation,

fraud, moral hazard, non-disclosure of material fact as declared in the proposal form/at the time of claim
or non-co-operation of the insured person’’.
Respondent Insurer requested to absolve them from the complaint made.
19. Reason for Registration of complaint:-
The complaint was registered as it falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A.
21. Result of personal hearing with both the parties (Observations & Conclusions):
The issues which require consideration is whether the action of the R I to repudiate the claim and cancel
the policy on the grounds of non disclosure of pre existing disease in the proposal form is in order.
21.1. During the personal hearing, both the parties reiterated their earlier submissions.
21.2. Forum find that the Insured person’s policy incepted from 10.10.2017. The insured has reported
the claim in the 2nd year of the Medical insurance Policy.
21.3 R I has cancelled the Health policy wef 14.09.2019 for the year 2018-19 in respect of IP and the
proportionate premium has been returned.
21.4 From the documents produced, the forum notes that the insured person was admitted from
17.09.2014 to 20.09.2014 in Cardiology Department in Manipal Hospital wherein she was diagnosed
with “Congestive Cardiac Failure, Normal Coronaries (18.09.2014) Moderate LV Dysfunction ” She
underwent coronary angiogram which revealed normal coronaries and LV Angio showed global
hypoinesia of LV with moderate LV function and was advised medical management.
21.5 Perusal of the proposal form reveals that to the query “Have you consulted/taken treatment/been
admitted for any illness/disease/injury/surgery. If yes, details”, the complainant stated “NO”. Since the
insured person was diagnosed with Heart disease in September 2014, the complainant was required to
mention the same in the Proposal Form. Non disclosure of pre existing disease result in breach of
insurance principle of utmost good faith.
21.6 During the personal hearing the complainant informed that he had not filled in the proposal form
and left this to be filled by the agent of the R I and had put his signature in the form . the forum holds
the complainant cannot be absolved from the consequences of appending his signature in the proposal
form even though he had assigned the agent to fill the same.
The Forum relies on Supreme Court’s decision in case of Reliance Life Insurance Company Limited &
another vs Ms. Rekaben Nareshbhai Rathod dated 24.04.2019 wherein the Court inter-alia held that -
‘’Now it is clear that a person who affixes his signature to a proposal which contains a statement which
is not true, cannot ordinarily escape from the consequence arising there from by pleading that he chose
to sign the proposal containing such statement without either reading or understanding it. That is
because, in filling up the proposal form, the agent normally, ceases to act as agent of the insurer but
becomes the agent of the insured and no agent can be assumed to have authority from the insurer to
write the answers in the proposal form. If an agent nevertheless does that, he becomes merely the
amanuensis of the insured, and his knowledge of the untruth or inaccuracy of any statement contained
in for of proposal does not become the knowledge of the insurer’’
21.7 Reliance is placed on the Supreme Court’s decisions in the case of Satwant Kaur Sandhu vs The
New India Assurance Company Limited dated 10.07.2009 and LIC of India vs. Manish Gupta dated
15.04.2019 to arrive at this decision.
21.8. On the basis of the above facts the Forum does not find any reason to interfere with the decision
of R I.
Hence the rejection of claim by RI is in order.

A W A R D
Taking into account of the facts and circumstances of the case and the submissions made
by both the parties and documents submitted during the course of the Personal Hearing,
the rejection of the claim by the Respondent Insurer is in order and in consonance with
the terms and conditions of the policy which does not require any interference at the
hands of the Ombudsman.
The Complaint is Disallowed.
Dated at Bangalore on the 13
th
day of December, 2019
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN - NEERJA SHAH
In the matter of Shri Manivel Madhan V/s MANIPAL CIGNA HEALTH INSURANCE COMPANY
LIMITED
Complaint No: BNG-H-053-1920-285
Award No.: IO (BNG)/A/HI/230/2019-20
1
Name & Address of the Complainant
Mr. Manivel Madhan
4, Jangamappa Road, 21
st
Main,
4
th
Cross, Ejipura,
Viveknagar, Behind Srirama Temple,
Bangalore – 560047
Mob. 9036836462
Email: mmvel[email protected]m
2
Policy No.
Type of Policy
Duration of Policy/ Policy Period
Date of Admission/discharge
PROHLR205422424
Cigna TTK ProHealth Insurance
11/08/2018 TO 10/08/2019
14.06.2019 TO 22.06.2019
3
Name of the Insured/ Proposer
Name of the Complainant
Mr.Manivel Madhan
4
Name of the Insurer
Manipal Cigna Health Insurance Company Ltd
5
Date of repudiation
14.08.2019
6
Reason for repudiation
Non-disclosure of PED
7
Date of receipt of the Annexure VI-A
30.10.2019
8
Nature of complaint
Rejection of claim
9
Amount of claim
₹.1,77,869/-
10
Date of Partial Settlement
N.A.
11
Amount of relief sought
₹.1,77,869/-
12
Complaint registered under Rule no:
13 (1) (b) of Insurance Ombudsman Rules, 2017
13
Date of hearing/place
05.12.2019/ Bengaluru
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent Insurer
Requested for absence since claim takenup for
payment
15
Complaint how disposed
Closed
16
Date of Award/Order
16.12.2019
17. Brief Facts of the Case:
The Complaint emanated from the rejection of hospitalisation claim on the ground of non-disclosure of
material facts by the Respondent Insurer (RI). The Complainant had taken up with the Grievance
department of RI, who had also maintained earlier stand of rejection. Hence, the Complainant has
approached this Forum.

18. Cause of Complaint:
a) Complainant’s arguments:
The Complainant’s submitted that he has taken the policy from Respondent Insurer (R I) from
11.08.2017 till date, it was issued after thorough medical examination. He was admitted to Majumdar
Shaw Medical Centre for treatment of left lower limp cellulites, Hepatic encephalopathy for the period
from 14.06.2019 to 22.06.2019. He submitted the bills for reimbursement of claim. He received a mail
dated 16.08.2019 from R I denying the claim since he had not declared his Asthma condition in the
proposal form at the time of taking the policy.
Complainant averred that he had not made any incorrect statement intentionally and is having only
minor wheezing problem for which he has never been hospitalised nor taken any regular medicine . He
has submitted the Doctor’s certificate dated 24.08.2019 from Mazumdar Shaw Medical Centre which
states that patient is clinically suspected over the long term to have reactive airway disease probably
Asthma which is not in any way related to his probable underlying disease. He has also submitted a copy
of certificate from the Doctor from St.John’s Medical college Hospital which states that patient’s CVA is
unrelated to his Bronchial Asthma.
He submitted that his present ailment is not related to Asthma and he has not intentionally hidden any
material facts.
The Grievance department also maintained the company’s earlier decision and hence, he has
approached this Forum to help him in getting the reimbursement and continuation of policy.
b) Respondent Insurer’s Arguments:
The Respondent Insurer did not submit their Self Contained Note. They have sent the mail dated
04/12/2019 Stating that the company in bonafide interest has declared to accept the claim of the
complainant and settle the claim as per policy terms and conditions. It is submitted that they have
acted as per the terms and conditions of policy and hence, requested this Forum to close the Complaint.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal.
p. Complaint along with enclosures,
q. Respondent Insurer’s SCN along with enclosures and
r. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
21.1. The complainant attended the hearing and reiterated the same.
21.2 The R I forwarded the consent for withdrawal of complaint by the complainant offering to settle
the claim amount of Rs.170441/- which was consented by the complainant provided the due claim
amount of Rs.170441/- is paid to him before 11.00 am on 05/12/2019 ie the date of hearing in this case.
21.3 R I have credited an amount of Rs.1,64,411/- to the complainant on 04.12.2019 and have submitted
the worksheet to the insured person towards short payment of Rs. 13458/- from the total claimed
amount. The following deductions are made by the R I as per mail dated 10.12.2019 sent by them.
Expense Head Amount Reason for deduction
Medicines/drugs
5121/-
Alchohol swabs 2/-, underpads 72/-(2), 24/-(2), 23/-, Glucometer
16/- , lancet 9/-, clohex mouthwash 139/-, diaper 159/-, gauze
swab 122/-, 82/-, 62/-,107/- (2), gloves 210/-, 76/-, 4/-, 201/-, 17/-
(2), 16/-, 13/- nebuliser mask 42/-, ounce glass 7/-, oxygen mask
32/-, apron 45/-, tegaderm 228/-, 1404/-, 152/-, thermometer
66/-, urinal 32/- , wet wipes 120/-(2), lancet 2/-, cast paddling 51/-
(2), 152/- crepe bandage 108/-(2), 14/- gauze 4/-, 61/-, bandage
10/-, dressing apd 31/-, gloves 33/-, 13/-, bandage 15/-, gauze
41/-, bandage 14/-, 72/- , cast pad 130/-, 390/-, gauze swab 139/-,
72/-.

Medicines/drugs
156/-
Cast pad 130/-, gauze 26/-
Medicines/drugs
501/-
Cast Pad 260/-, Gauze 36/-, 106/-
Consultation/visit
2520/-
Procedure charges
Other Misc.
charges
240/-
Casnnulation
Other Misc.
charges
1410/-
Admission 1000/-, medical records 350/-, im iv injection 60/-
Radiology/MRI/CT
/xray
3510/-
CRP Blood gas analysis, xray
The deduction of Rs.3510/- under the head Radiology is for the following reasons.
1. CRP – deducted as there is repeat of CRP
2. Blood gas - related to bronchial asthma-oxygen saturation often affected in asthmatic patient
(asthma endorsed as PED)
3. 3. X-ray – Asthma related
The deductions made by R I are in order and are as per terms and conditions of the policy.
21.4 R I is advised to ascertain and process the final claim amount before communicating to the
complainant in future.
21.5 Since the claim is already settled by the Respondent Insurer, the complaint is disposed off and
closed.
AWARD
Taking into account of the facts and circumstances of the case and upon scrutiny of the documents
submitted by both the parties, the settlement of the claim by the Respondent Insurer is found to be
in order and does not require any interference at the hands of the Ombudsman.
Hence the complaint may be disposed off and closed.
Dated at Bengaluru on the 16
th
day of December, 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – NEERJA SHAH
In the matter of Miss Namitha B.S V/s THE ORIENTAL INSURACE COMPANY LIMITED
Complaint No: BNG-H-050-1920-0282
Award No. : IO (BNG)/A/HI/219/2019-20
1
Name & Address of the
Complainant
Miss Namitha B.S
No.285, RamaIyengar Road,
V.V.Puram,
Bangalore
Karnataka 560 004
Mob.No.9448171606
Mail ID : hsadananda@gmail.com
2
Policy No.
Type of Policy
Duration of policy/Policy
period/ PPT
421902/48/2019/2903
Happy Family Floater -2015
01.12.2018 to 30.11.2019
3
Name of the Insured
Miss Namitha B.S

Name of the Policyholder
Smt.M.Umadevi
4
Name of the Respondent
Insurer
The Oriental Insurance Company
Limited.
5
Date of repudiation/rejection
NA
6
Reason for repudiation
NA
7
Date of receipt of Annexure VI-
A
15.10.2019
8
Nature of complaint
Partial settlement of claim
9
Amount of claim
₹.47,626/-
10
Date of partial settlement
Cashless
11
Amount of relief sought
₹.47,626/-
12
Complaint registered under
Rule no:
13 (1) (b) of Insurance Ombudsman
Rules, 2017
13
Date of hearing/place
27.11.2019 / Bengaluru.
14
Representation at the hearing
wwww) For the Complainant
Self
xxxx) For the Respondent
Insurer
Smt.Kalavathy Dy.Manager
15
Complaint how disposed
Partially allowed
16
Date of Award/Order:
09.12.2019
17. Brief Facts of the Case: The complaint emanated from the short settlement of claim for the
hospitalization on the ground that the ailment was pre-existing and enhanced sum insured at the time
of renewal is covered after four continuous renewals. Insured occupied room rent above eligible sum
insured. Hence proportionate deductions are made . In spite of representation with Respondent
Insurer (RI), her request was not considered. Hence, the Complainant has approached this Forum.
18. Cause of Complaint:
a. Complainant’s arguments: The Complainant’s submission was that she has taken Mediclaim
Insurance Policy for self and her mother from RI . Mother was admitted to Rangadore Memorial
Hospital for the period from 16.02.2019 to 23.02.2019 with the history of breathlessness since 2 days,
fever with chills, cough with expectoration since 5 days. R.I rejected part of the claim , 34% of
Hospitalization claim has been disallowed & for want of documents which she has submitted . In spite
of representation with RI, her request was not considered.
b. Respondent Insurer’s Arguments: The RI submitted their Self Contained Note dated 30.10.2019
admitting the insurance coverage, preferring of claim and their partial settlement. They submitted that
Insured is covered under Mediclaim Insurance policy (Individual) for Rs 1.5 lakhs for the period from
2015 to 2017. On renewal insured changed coverage to Happly Family Floater - 2015 policy and opted
increased Sum Insured of Rs. 3 Lakhs for the policy period 01.12.2018 to 30.11.2019. Claim falls under
current policy period.
It is submitted that the IP was admitted to Rangadore Memorial hospital form 16.02.2019 to 23.02.2019
and diagnosed as a case of Carcinoma of Breast-Stage IV, Radiation induced pulmonary fibrosis treated
conservatively. Insured availed cashless facility and expenses approved for Rs.81909/- based on eligible
room rent as per policy terms and conditions.
Subsequently insured submitted claim of Rs.13246/- towards pre-post hospitalization. Claim was settled
for Rs.9308/- by deducting non-medical expenses and for some bills insured did not produce
prescriptions. All the claims are settled within 15 days.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
Complaint along with enclosures
s. Complaint along with enclosures,
t. Respondent Insurer’s SCN along with enclosures and
u. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
Forum notes that the dispute is for partial settlement of claim on the ground that enhanced sum
insured at the time of renewal is covered after four continuous renewals.
This Forum has perused the documentary evidence available on record and the submissions made by
both the parties during the personal hearing.

The Complainant admitted the fact that IP was suffering from Breast Cancer and treated since 1995.
But the present hospitalization is for breathlessness, fever and cough with expectoration. And requested
for settlement as she was insured for Rs.3 lakhs.
The Respondent Insurer reiterated their contentions and submitted that in the discharge summary
under the column COURSE IN THE HOSPITAL it is clearly stated that on 18.02.19 IP was readmitted to
ICU following an episode of bronchospasm with tachycardia. HRCT chest suggestive of right and left
basal segment consolidation mediastinal, fibrosis post RT related. Hence ,their decision was based on
medical records and policy terms and conditions.
RI submitted and relied on clause 4.3 NOTE and 9(iv), the same is reproduced:
Clause 4. General Exclusions: The Company shall not be liable to make any payment under this policy in
respect of any expenses whatsoever incurred by any Insured Person in connection with or in respect of:
Clause 4.3 Note: If the continuity of the Renewal is not maintained then subsequent cover will be
treated as fresh policy and clause 4.1,4.2,4.3 shall apply afresh unless agreed by the Company and
suitable endorsement passed on the Policy, the duly authorized official of the Company. Similarly, if the
Sum Insured is enhanced subsequent to the inception of the first Policy, Clause 4.1,4.2,4.3 shall apply
afresh on the enhanced portion of the Sum Insured.
Clause 9 : States about terms on Renewal of Policy
Sub clause (iv) : If the Policy is renewed for enhanced Sum Insured then the clause (4.1, 4.2 & 4.3) as
applicable to a fresh shall apply to additional Sum Insured as if a separate Policy has been issued for the
difference. In respect of Pre-existing Disease or for a disease/ailment/injury for which treatment has
been taken in the earlier policy period , the enhanced Sum Insured will be available only after four
continuous renewals with the increased sum insured.
Copies of policy proof produced by RI shows that IP was covered for Sum Insured of Rs. 1.25 Lakhs
during 2014-15 under Individual Mediclaim policy . S I is enhanced to Rs. 1.5 lakhs during 2015-16,
2016-17 & 2017-18 . Further, during 2017-18 Complainant has taken Happy Family floater -2015
policy and opted for higher sum insured of Rs.3 lakhs . Existing enhanced sum insured has not run for
four continuous renewal period.
From the copies of mail correspondence submitted by complainant it is found that RI has already
explained the reason for proportionate deductions in claim amount.
Forum does not find any flaw with the decision of Respondent Insurer in partial settlement of
hospitalization claim.
Forum noted from the Claim Settlement Voucher that RI disallowed following expenses due to non
submission of prescriptions/Bills/reports .
1. Echo Report in the main Bill for Rs.1000/-
2. Ward consumables break up not enclosed in main bill for Rs. 2,900/- Rs.200/- Rs.200/-, Rs.150/-
3. Original consultation paper no enclosed for Rs.300/-
4. Prescription not enclosed dt. 29.03.19 for Rs. 189/-
5. Lab requisition not enclosed dt. 02.02.2019 Rs. 54/-
6. Medicine prescription not enclosed dt. 26.02.19 an dt. 24.02.19 for Rs. 114/- and Rs. 370/-
respectively.
Considering the above facts, the Forum is not in a position to consider the request of the Complainant
and does not find any flaw with the decision of RI in reducing the claim settlement . RI is directed to
relook the claim subject to production of required documents as above as per terms and conditions of
policy.
The Complaint is Partially Allowed.
A W A R D
Taking into account of the facts and circumstances of the case, the documents the oral
submissions made by the RI, this Forum is of the opinion that the decision of the Respondent
Insurer in partial settlement of the claim for hospitalization is in accordance with the terms
and conditions of policy .
This Forum directs the Respondent Insurer to relook and settle the claim by collecting
necessary documents as per the terms and conditions of policy along with interest @ 6.25% +
2% from the date of receipt of last necessary documents to the date of payment of claim, as
per regulation 16 (1) (ii) of Protection of Policy holders’ Interests of IRDA Regulations, 2017

issued vide notification dated 22.06.2017.
Hence, the complaint is PARTIALLY ALLOWED.
22. Compliance of Award:
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a. The Complainant shall submit all requirements/Documents required for settlement of award
within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rule,2017, the insurer shall comply with
the award within thirty days of the receipt of the award and intimate compliance of the same
to Ombudsman.
Dated at Bangalore on the 9th day of December , 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Mrs NEERJA SHAH
In the matter of Shri NAVEENCHANDRA D KAMATH V/s STAR HEALTH & ALLIED INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-1920-0244
Award No.: IO/(BNG)/A/HI/0197/2019-20
1
Name & Address of the
Complainant
Shri NAVEENCHANDRA D KAMATH
S/o Shri S R Devdas Kamath
52
nd
Heroor Village, Brahmavar
Udupi, Karnataka - 576 213
Mob.No. 99020 00427
Mail ID : krevathyprabhu@licindia.com
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
P/141120/01/2019/007395
Senior Citizen Red Carpet Health Insurance
Policy.
19.01.2019 to 18.01.2020
3
Name of the Insured/
Proposer
Name of the policyholder
Shri M Devdas Kamath
Self – Complaint by son
4
Name of the Respondent
Insurer
Star Health and Allied Insurance Company
Limited
5
Date of repudiation
19.07.2019
6
Reason for repudiation
Claim not payable during fist 2 years.
7
Date of receipt of Annexure
VI-A
03.09.2019
8
Nature of complaint
Repudiation of claim
9
Amount of claim
₹.90,000/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
₹.90,000/-
12
Complaint registered under
Rule no:
13 (1) (b) of Insurance Ombudsman Rules,
2017
13
Date of hearing/place
27.11.2019 / Bengaluru
14
Representation at the
hearing
a) For the Complainant
Absent–requested vide letter
dt.05.11.2019 inability to attend hearing
and to proceed the case in absentia.
b) For the Respondent
Insurer
Dr.Umadevi, Sr.Manager
15
Complaint how disposed
Dismissed
16
Date of Award/Order
03.12.2019
17. Brief Facts of the Case: It is a case of repudiation of mediclaim for hospitalisation for liver cirrhosis
on the ground that the claim is not payable during first 2 years of insurance. The Complainant took up
the matter with the Grievance Cell of the Respondent Insurer (RI) and the same was not considered
favourably.
18. Cause of Complaint:
a) Complainant’s arguments: The Complainant’s submission was that his father was insured with the RI
from 19.01.2018 and was renewed on 19.01.2019. His father was admitted to Pranav Hospital,

Handady,Udupi Dist., on 24.05.2019 as he found him disoriented and speech was not clear. After
investigation, he was diagnosed as Liver Cirrhosis and after suffering for 12 days, he expired on
05.06.2019. The request for cashless was rejected and claim for reimbursement was also rejected under
exclusion 3(b) of the policy. He submits that the said exclusion applies to gall bladder and pancreatic
diseases but not to liver. The approach to GRO also did not yield any result and hence, the Complainant
approached this Forum.
b) Respondent Insurer’s Arguments:
RI submitted their Self Contained Note dated 15.11.2019 admitting coverage under Senior Citizen Carpet
Health Insurance, preferring of claim in the 2
nd
year of policy and their rejection. It is stated that the
insured person was admitted to Pranav Hospital 24.05.19 and discharged on 05.06.2019 with complaints
of Irrelevant speech/disoriented and was diagnosed as Hepatic encephalopathy, cirrhosis of liver and
Ascitis. As the claim falls under exclusion 3(b) of the policy, the same was rejected.
Hence, RI has requested to absolve them from the complaint made.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
a. Complaint along with enclosures,
b. Respondent Insurer’s SCN along with enclosures and
c. Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
The present dispute is for rejection of claim on the ground that the ailment is within the waiting period
of 2 years. The complainant vide his letter dt. 5.11.2019 expressed his inability to attend hearing and to
proceed the case without his presence. This Forum has perused the documentary evidence available on
record and the submissions made by RI during the personal hearing.
The complainant reiterated his contentions in the complaint and submitted that liver cirrhosis does not
fall under the said exclusion.
The RI reiterated their contentions stated in SCN and submitted that their decision was based on the
medical records and as per the terms and conditions of policy.
As the rejection is based on exclusion 3 (b), the same is reproduced:
3 - Exclusions
3 - During the first two years of continuous operation of this Senior Citizen Carpet Health Insurance policy
any expenses on
b) Gall bladder and Pancreatic diseases and all treatment (conservative, interventional, laparoscopic and
open) related to Hepato-pancreato-bilary disease including and Pancreatic calculi. All types of
management for Kidney and Genito-urinary tract calculi.
As per the discharge summary, the patient was diagnosed as Hepatic encephalopathy and as per
information available on public domain, the said ailment is defined as a spectrum of neuropsychiatric
abnormalities in patients with liver disfunction, after exclusion of brain disease.
The exclusions apply to all treatments related to Hepato-pancreato-bilary disease and this disease refers
to any condition that affects the liver, pancreas, gall bladder and the bile ducts.
Considering the facts on record and the submissions made and analysing the information available in
public domain, the Forum does not wish to interfere with the decision of the RI in rejecting the Claim, as
the same is as per the terms and conditions of the policy.
The complaint is Dismissed.
A W A R D
Taking into account of the facts and circumstances of the case and the submissions made by
both the parties and documents submitted during the course of the Personal Hearing, the
decision of the Respondent Insurer in repudiating the claim is in consonance with the terms
and conditions of the policy and does not warrant any interference at the hands of the
Ombudsman.
Hence, the complaint is Dismissed.
Dated at Bangalore on the 3rd day of December , 2019.
(NEERJA SHAH)
INSURANCE OMBUDSMAN
FOR THE STATE OF KARNATAKA
