
Regional Analysis of
Maternal and Infant Health
in Texas
PUBLIC HEALTH REGION 6/5S
Community Health Improvement Division
Maternal & Child Health Epidemiology
April 2018

TABLE OF CONTENTS
II
Table of Contents
Introduction ................................................................................................ 1
Data & Methods ........................................................................................... 2
Data Sources .............................................................................................. 2
Data Terms ................................................................................................ 4
List of Counties Included in each Public Health Region ..................................... 8
Overview of Texas ....................................................................................... 9
Geography ................................................................................................. 9
Population ................................................................................................ 10
Race/Ethnicity ....................................................................................... 10
Age and Gender ..................................................................................... 11
Foreign Born ......................................................................................... 11
Income and Poverty ............................................................................... 12
Birth Demographics ................................................................................... 13
Maternal Race/Ethnicity .......................................................................... 13
Maternal Age ......................................................................................... 14
Teen Births ........................................................................................... 15
Infant Mortality & Morbidity ........................................................................ 16
Infant Mortality ...................................................................................... 16
Leading Causes of Infant Death ............................................................... 17
Preterm Birth ........................................................................................ 18
Low Birth Weight ................................................................................... 19
17P Prescription ..................................................................................... 20
Health Care Coverage and Access ............................................................... 21
Health Insurance ................................................................................... 21
Health Professionals and Shortage Areas .................................................. 22
Prenatal Care in the First Trimester .......................................................... 23
Prenatal Care as Early as Wanted ............................................................. 24
Barriers to Prenatal Care ......................................................................... 25
Barriers to Maternal & Child Health Services .............................................. 26
Maternal Health ........................................................................................ 27
Pre-Pregnancy Obesity ........................................................................... 27

TABLE OF CONTENTS
III
Maternal Hypertension & Diabetes ............................................................ 28
Maternal Smoking .................................................................................. 30
Drinking During Pregnancy ...................................................................... 31
Physical Abuse Before/During Pregnancy ................................................... 32
Postpartum Depression ........................................................................... 33
Postpartum Checkup .............................................................................. 34
Maternal Mortality & Morbidity ................................................................. 35
Infant Health Practices............................................................................... 39
Breastfeeding ........................................................................................ 39
Safe Infant Sleep ................................................................................... 42
Well-baby Checkup ................................................................................ 42
Perinatal Periods of Risk ............................................................................. 43
Phase I Analysis ..................................................................................... 44
Phase II Analysis ................................................................................... 45
Recommendations .................................................................................. 47
Summary Table: Selected Health Indicators in Texas ..................................... 48
Public Health Region 6/5S: Key Findings .................................................. 49
Public Health Region 6/5S ........................................................................ 50
Birth Demographics ................................................................................... 51
Teen Births ........................................................................................... 51
Infant Mortality & Morbidity ........................................................................ 52
Preterm Birth ........................................................................................ 53
Low Birth Weight ................................................................................... 53
17P Prescription ..................................................................................... 54
Health Care Coverage and Access ............................................................... 54
Health Professionals ............................................................................... 55
Prenatal Care in the First Trimester .......................................................... 55
Prenatal Care as Early as Wanted and Barriers .......................................... 56
Barriers to Maternal & Child Health Services .............................................. 57
Maternal Health ........................................................................................ 57
Pre-pregnancy Obesity ........................................................................... 58
Maternal Hypertension & Diabetes ............................................................ 58
Smoking During Pregnancy ..................................................................... 59

TABLE OF CONTENTS
IV
Drinking During Pregnancy ...................................................................... 60
Physical Abuse Before/During Pregnancy ................................................... 60
Postpartum Depression ........................................................................... 61
Postpartum Checkup .............................................................................. 61
Infant Health Practices............................................................................... 62
Breastfeeding ........................................................................................ 62
Safe Infant Sleep ................................................................................... 63
Well-baby Checkup ................................................................................ 63
Perinatal Periods of Risk ............................................................................. 64
Phase I Analysis ..................................................................................... 64
Phase II Analysis ................................................................................... 65
Recommendations .................................................................................. 67
Summary Table: Selected Health Indicators in PHR 6/5S ............................... 68
References ................................................................................................ 69

INTRODUCTION
1
Introduction
This report provides a comprehensive analysis of key maternal and infant health
outcomes, as well as related risk and protective factors, in each of the eight Public
Health Regions in Texas. The findings are critical for informing evidence-based
practices, the Healthy Texas Mothers & Babies initiative, and strategies for building
and implementing regional coalitions, whose mission is to design and implement
public health interventions to meet the maternal and infant health needs identified.
Results from analysis of the latest population-level data are integrated with
available Title V Maternal and Child Health community outreach survey results and
focus group findings to address health concerns in each region. The report includes
an overview of geographic/socioeconomic characteristics, birth demographics,
infant mortality, access to health care and barriers, maternal health (obesity,
hypertension, diabetes, smoking, drinking, physical abuse, postpartum depression,
and postpartum checkup), infant health practices (breastfeeding, safe infant sleep,
and well-baby checkup), and comprehensive risk analyses for Texas as well as for
each Public Health Region. Statewide information regarding maternal mortality and
morbidity is also included.
When possible, geographic mapping at the county level was performed to gain a
better understanding of maternal and infant health indicators within a particular
region and the state as a whole. Data terms, sources, and methods are addressed.
For data monitoring purposes, a summary table showing trends for selected
maternal and infant health indicators is presented at the end of the Texas overview
and each region-specific section.

DATA & METHODS
2
Data & Methods
Major public health data sources and data terms used in this report are detailed
below, as well as a list of counties included in each of the eight Public Health
Regions in Texas.
Data Sources
For most of the infant and maternal health indicators in this report, vital records
data (information from Texas birth, death, fetal death, and linked birth/infant death
files), hospital discharge data, and results from the Texas Pregnancy Risk
Assessment Monitoring System (PRAMS) survey as well as the Texas Infant Feeding
Practice Survey (IFPS) among Women, Infants, and Children (WIC) participants
were used. Despite the few limitations described below, these data sources have
been used by the Texas Department of State Health Services (DSHS) and other
state agencies and stakeholders to inform, develop, and drive policies and
programs to improve the health of mothers and babies, and to understand their
emerging health needs. These invaluable sources of data provide a rich
understanding of both infant and maternal health, and serve as an important
resource for risk factor analysis and for identification of possible avenues for
prevention.
The DSHS Vital Statistics Section collects demographic data on all (or the vast
majority of) births and deaths in Texas, as well as information on fetal deaths
weighing 350 grams or more or, if weight is unknown, occurring at 20 weeks of
gestation or more. Vital records files are a rich and comprehensive source of data;
however, the quality of birth and death certificate data is dependent on how
accurately these records are completed by hospital staff, providers, or certifiers. It
is also thought that the birth file likely underreports the prevalence of several
maternal health indicators, such as diabetes and preeclampsia [1, 2]. All the years
of vital records data used in this report (2006-2015) are final. Data were
suppressed in county maps when there were fewer than 100 documented births in
a county and in regional reporting when there were fewer than 15 cases in the
numerator, to prevent identification of affected individuals that might be possible
with smaller numbers, thereby protecting the confidentiality and privacy of these
individuals and their families.
Texas Hospital Inpatient Discharge Public Use Data Files (PUDF) were used for
severe maternal morbidity (SMM) and Neonatal Abstinence Syndrome (NAS)
analyses in this report. The PUDF contains patient-level information for inpatient
hospital stays from all Texas licensed hospitals except those that are statutorily
exempt from the reporting requirement [3]. Data are available by quarter,
beginning with data for 1999. Texas county-level data from first quarter 2006

DATA & METHODS
3
through third quarter 2015 were analyzed to determine SMM rates and NAS rates.
Cases of NAS were identified by the International Classification of Diseases, Ninth
Revision, Clinical Modification (ICD-9-CM) diagnosis code for drug withdrawal
syndrome in newborns, and hospital births were identified using ICD-9 codes for
newborns born within the reporting hospital [4]. Cases of SMM were identified by
ICD-9 diagnosis and procedure codes included in the 2017 Federally Available
Resource Document provided by Health Resources and Services Administration
(HRSA) [5]. However, this report does not use the recalculation methods indicated
by HRSA to account for cases with unreasonably short hospital stays, and therefore
the SMM rates in this report are likely overestimated. Delivery hospitalizations for
SMM rates were identified by diagnosis codes for an outcome of delivery, diagnosis-
related group delivery codes, and procedure codes for selected delivery-related
procedures [6]. The estimates in these analyses do not include inpatient stays for
state residents that may have been treated in another state besides Texas.
Additionally, the estimates are not limited to only community hospitals, defined as
short-term, non-Federal hospitals, but also include long-term care facilities such as
rehabilitation, and alcoholism and chemical dependency hospitals. Data were
suppressed when there were fewer than 5 cases in the numerator.
In Texas, the PRAMS survey provides the most comprehensive population-based
data on maternal health before, during, and after pregnancy. Conducted in
partnership with the Centers for Disease Control and Prevention (CDC), DSHS has
been implementing PRAMS annually since 2002 [7]. The PRAMS survey asks
questions (via mail or telephone) of mothers who have recently given birth on
topics such as prenatal care, pregnancy intention, alcohol use, smoking, intimate
partner violence, postpartum depression, breastfeeding, infant sleep position, and
smoke exposure. Unlike vital records, which include information on almost all vital
events (births and deaths) in Texas, PRAMS data are obtained from a sample of
women who are residents of Texas and gave birth to a live infant. CDC provides
Texas with a survey data file that includes survey weights, and CDC ensures that
analyses are representative of women who have given birth to a live infant and are
residents of Texas. For example, the 1,322 women who completed the survey in
2015 were representative of all 396,093 Texas residents who had a live birth.
PRAMS data/results are generalizable to women who are Texas residents with at
least one live birth within a specific year, whereas the birth file represents all live
births in Texas. Because of this, along with potential sampling and reporting
differences, PRAMS findings may differ from results obtained from vital statistics
data. PRAMS results are reported along with 95 percent confidence intervals (CI),
and the width of the confidence interval – in other words, the distance between its
upper and lower limits – is an indicator of the variability, and thus the reliability, of
the results. Texas PRAMS data are presented as estimated percentages or
prevalence estimates to account for complex sampling and weighting. As with any

DATA & METHODS
4
self-reported survey, possibility of recall bias exists; that is, women may not
answer the question correctly or leave it blank because they may not remember the
event. However, the schedule of survey mailings begins 61 to 183 days after the
birth of the infant, so the recall risk is minimized. Based on CDC’s suppression
rules, PRAMS prevalence data were suppressed in this report when there were
fewer than 30 respondents (unweighted sample size) in the denominator.
Additionally, the 2016 Texas WIC IFPS survey data were used [8]. As part of efforts
to promote breastfeeding, DSHS periodically conducts a survey of breastfeeding
beliefs, attitudes, and practices among women receiving WIC services in Texas. The
purpose of this survey is to provide data to local WIC agencies to aid in planning
and activity development. These data may also provide valuable information to
coalitions, public health partners, policy makers, and those interested in supporting
breastfeeding. The 2016 IFPS surveys were assigned to clinics in all 66 local WIC
agencies operating at the time of the survey. WIC clinic supervisors were instructed
to offer the survey using the informed consent script to each eligible participant
presenting at the clinic for services during the survey administration period. Eligible
participants were women who were biological mothers, who were age 18 or older,
and who presented at the clinic for services and had a single baby who was aged 1
month through 30 months old at the time of the survey. A total of 10,325 surveys
were completed from March 1 through April 22, 2016. After eliminating ineligible
respondents, there were 8,561 eligible surveys for final analyses. The survey
results were not weighted or adjusted, and therefore may not be representative of
the general population presenting for WIC services in Texas. It’s also noted that
comparisons or conclusions cannot be reliably made when using analyses with small
sample sizes. Caution should be used when interpreting these responses. Results
for categories with fewer than 20 responses in IFPS were not reported.
Data Terms
Birth Weight
The weight of an infant at delivery, recorded in pounds and ounces or in grams.
Birth weights are classified into 3 groups: Normal, Low, and Very Low. Very Low
birth weight babies are also included in the Low birth weight group. A Normal birth
weight is defined as at least 5 pounds, 9 ounces (or 2,500 grams); Low birth weight
- less than 5 pounds, 9 ounces (or 2,500 grams); and Very Low birth weight - less
than 3 pounds, 5 ounces (or 1,500 grams).
Border and Non-Border Counties: Counties are designated as Border or Non-
Border according to Article 4 of the La Paz Agreement of 1983, which defines a
county as a Border county if that county is within 100 Kilometers of the U.S./Mexico
border. There are 32 counties in Texas designated as Border counties by this
definition.

DATA & METHODS
5
Body Mass Index: Body mass index (BMI) is a measure of weight-for-height that
is often used to classify adults as being underweight, of normal weight, overweight,
or obese [9]. In this report, maternal BMI is calculated using the mother’s pre-
pregnancy weight and height. BMI categories are defined using the standard cutoffs
for adults, even if the mother is younger than 22 years of age.
Causes of Infant Death: Cause of death categories from the National Center for
Health Statistics Instruction Manual are used to calculate information regarding the
leading causes of infant death in this report [10]. Not all infant deaths in Texas are
due to the leading causes shown in the report. Causes of infant death are reported
as the number of deaths per 10,000 live births.
Communities: In this report, the term ‘communities’ refers to combined statistical
areas (CSAs) and select large Metropolitan Statistical Areas (MSAs). CSAs and
MSAs are defined by the U.S. Office of Management and Budget (OMB). CSAs are
composed of adjacent metropolitan areas (containing an urban core of 50,000 or
more population) and micropolitan areas (containing an urban core of at least
10,000 but less than 50,000 population), and consist of the county containing the
urban core area, as well as adjacent counties with a high degree of social and
economic integration with the urban core. To be consistent with recent past Healthy
Texas Babies Data Books (from 2013-2017), this report uses the U.S. OMB CSA and
MSA definitions released in 2013, with two exceptions. First, the traditional CSA of
Dallas-Fort Worth was divided into three separate areas: Fort Worth-Arlington,
Dallas-Plano, and the remaining outlying counties of the metropolitan area. Second,
the county of Galveston was removed from the Houston-The Woodlands CSA so
that this county could be analyzed separately.
Gestational Age: Gestational age is used to calculate whether or not a birth is
preterm, as well as to calculate when in pregnancy the mother first received
prenatal care. However, exact gestational age is often unknown and must be
estimated. Beginning with final 2014 data, the National Center for Health Statistics
has changed the variable used to estimate gestation [11]. The current standard,
starting in 2014, uses the obstetric estimate of gestation on the birth certificate,
and not a combination of last menstrual period and the obstetric estimate, as had
been done in the past. This current standard for calculating gestational age is used
throughout the report.
High Parity for Age: Parity is defined as the number of live births or other
pregnancy outcomes that a woman has had including the birth being recorded. High
parity for age was calculated based on the mother’s age and total birth order.

DATA & METHODS
6
Age Total Birth Order*
<15 or 35+ 1
<20 or 40+ 2 or 3
<25 or 40+ 4
<30 or 35+ 5
All Ages 6 or more
*Sum of the live births or other pregnancy outcomes that a mother has had
including the birth being recorded.
Infant Mortality: Infant mortality rate (IMR) is defined as the number of infants
who died in a given year divided by the number of live births in that same year.
This number is then multiplied by 1,000 to calculate the IMR. All of the births that
comprise this rate are restricted to those women with Texas listed as their state of
residence.
Perinatal Periods of Risk: A comprehensive approach designed to help
communities use data to improve infant and maternal health outcomes. In addition
to infant deaths, fetal deaths are also included in the perinatal periods of risk
(PPOR) analysis to provide more information. The PPOR analysis divides fetal and
infant deaths into four risk periods (maternal health/prematurity, maternal care,
newborn care, and infant health), based on birth weight and age of death. An
excess feto-infant mortality rate (F-IMR) is then calculated for each of these
periods, both for the state as a whole (as well as for each Public Health Region) and
for specific demographic study populations. The reference group for each of these
calculations is a state-level reference population of mothers with near-optimal birth
outcomes [12, 13]. In this report, 2010-2014 fetal death and linked birth/infant
death files were used for the PPOR analysis.
Race/Ethnicity: For information obtained from birth records, fetal death records,
or from PRAMS, race/ethnicity information shown throughout this report refers to
the mother, not the infant. However, infant death data are classified according to
infant’s race/ethnicity. Women who identified themselves as only White or Black
and who did not indicate that they were Hispanic were classified as White or Black,
respectively. Women who identified themselves as Hispanic were classified as
Hispanic, regardless of their race designation. Women of all other races, including
multiracial women, were classified as ‘Other’, as long as the woman did not self-
identify as Hispanic. The ‘Other’ category is not homogeneous, and there have been
shifts in the demographics of women within this category. Since 2004, there has
been an increase in the number of women identifying themselves as multiracial.
Also, due to the limited number of women classified as ‘Other’ race/ethnicity in
PRAMS, women classified as ‘Other’ race/ethnicity and women classified as White

DATA & METHODS
7
were combined into one category called, White/Other women, for PRAMS
racial/ethnic analyses.
Urban and Rural Counties: Counties are designated as Metropolitan or Non-
Metropolitan by the U.S. Office of Budget and Management. Texas Health
Professions Resource Center (HPRC) currently uses the designations that took effect
in 2013. In Texas, 82 counties are designated as Metropolitan and 172 are
designated as Non-Metropolitan. HPRC uses the terms ‘Non-metropolitan and
Metropolitan’ interchangeably with ‘Rural and Urban’.

DATA & METHODS
8
List of Counties Included in each Public Health Region
Table 1.1

OVERVIEW OF TEXAS
9
Overview of Texas
Texas is a vast state, with regional differences in geography, population size,
demographic and socioeconomic characteristics, as well as various maternal and
infant health indicators. This section provides an overview of these variations and
relates them to the challenges that exist for health care availability and access.
Geography
Texas is the second largest state in the
United States (behind Alaska) in terms
of land. The Lone Star State
encompasses approximately 262,000
square miles, and accounts for 7.4
percent of the total U.S. land area [14].
Texas includes 254 counties that are
classified as either rural or urban (Figure
2.1) [15]. About 88.8 percent of Texas
population in 2015 resided in urban
counties. The five largest metropolitan
areas in Texas are located around the
cities of Houston, San Antonio, Dallas,
Austin, and Fort Worth, and these areas
encompass multiple counties.
Given the immense size of Texas, the distance that some individuals, especially
those living in rural counties, must travel to receive health care services can be a
significant challenge to accessing and receiving those services.
For administrative purposes, each of the
254 Texas counties is assigned to one of
8 public health regions (Figure 2.2).
Public Health Region 1 (PHR 1) is
administered from a regional office in
Lubbock. Public Health Region 2/3 (PHR
2/3) is administered from a regional
office in Arlington. Public Health Region
4/5 North (PHR 4/5N) is administered
from a regional office in Tyler and Public
Health Region 6/5 South (PHR 6/5S) is
administered from a regional office in
Houston. Public Health Region 7 (PHR 7)
is administered from a regional office in
Temple. Public Health Region 8 (PHR 8)
Figure 2.1
Figure 2.2

OVERVIEW OF TEXAS
10
is administered from an office in San Antonio, Public Health Region 9/10 (PHR 9/10)
is administered from an office in El Paso, and Public Health Region 11 (PHR 11) is
administered from an office in Harlingen. A list of counties in each PHR is also
presented in the Data & Methods section.
Population
Texas has the second largest population in the U.S. (behind California) [16], with
an estimated population of 27.5 million in 2015. Texas is one of the fastest-growing
states in the nation, with a population that has increased by 9.2 percent from 2010
to 2015. Public Health Regions 7 (11.6 percent), 6/5S (11.4 percent), and 8 (10.0
percent) experienced faster population growth rates than the state’s from 2010 to
2015. The Texas Demographic Center predicts that by 2050, the population in
Texas will exceed 31 million people using the zero migration scenario, will exceed
40 million people using the one-half 2000-2010 migration scenario, and will exceed
54 million people using the full 2000-2010 migration scenario [17, 18].
Race/Ethnicity
Hispanics (of all races) made up 40.0 percent of the state’s population in 2015.
Counties with the highest proportions of Hispanic populations were primarily located
in the southern and western regions of Texas, along the Texas-Mexico border
(Figure 2.3). Three major cities in Texas were located in counties where over 80
percent of the population were Hispanic: Brownsville, Laredo, and El Paso. The
region with the largest percentage of Hispanics was PHR 11 at 83.7 percent and the
lowest was PHR 4/5N at 15.6 percent. On the other hand, regional concentrations
of the Non-Hispanic Black population in Texas (Figure 2.4) were quite different from
that of the Hispanic population. Counties with the highest proportions of Black
Figure 2.3
Figure 2.4

OVERVIEW OF TEXAS
11
populations in 2015 were largely concentrated in the northeastern, eastern, and
north gulf-coast regions of the state. Blacks accounted for 11.5 percent of the total
population in Texas. In terms of regional differences, PHR 6/5S (17.0 percent) had
the highest Black proportion among its population and PHR 11 (1.1 percent) had
the lowest Black proportion.
Age and Gender
Texas has a larger proportion of youth among its population than most other U.S.
states [16]. In 2015, Texas was tied for the second largest proportion of the
population being children younger than 18 years old (26.4 percent) in the nation.
About 7.2 percent of the Texas population were younger than 5 years old, 14.6
percent were 5 to 14 years old, and 4.5 percent were 15 to 17 years old [19].
Border counties in South Texas had high percentages of individuals younger than 5
years old, as did several counties in west Texas and the Texas Panhandle.
Women comprised half of the total population in Texas in 2015. However, 5.7
million reproductive-aged women (ages 15-44) accounted for 20.9 percent of the
total population. For the most part, urban counties with large metropolitan areas
(including those containing the cities of Dallas-Fort Worth, Houston, San Antonio,
Austin, and El Paso) had high proportions of women in their childbearing years. By
region, PHR 7 had the highest proportion of women of reproductive age (22.1
percent) and PHR 4/5N had the lowest proportion of childbearing-aged women
(17.7 percent).
Foreign Born
According to 2011-2015 U.S. Census Bureau American Community Survey (ACS)
five-year estimates [20], Texas had a higher percentage of foreign-born residents
(16.6 percent) compared to the nationwide average (13.2 percent). Over 70
percent of foreign-born Texas residents were born in Latin American countries –
almost 19 percentage points more than the national average. About 29.5 percent of
Texans spoke Spanish at home, compared with 13.0 percent of U.S. residents.
Counties along the Texas-Mexico border had high concentrations of foreign-born
residents, as did several other counties in west and northwest Texas. Counties
containing the non-border cities of Houston, Dallas, and Austin also had high
concentrations of foreign-born residents. Within four metropolitan statistical areas
in PHR 9/10 and PHR 11 (Laredo, McAllen-Edinburg-Mission, Brownsville-Harlingen,
and El Paso), 72 to 92 percent of persons spoke a language other than English at
home, with the vast majority speaking Spanish.

OVERVIEW OF TEXAS
12
Income and Poverty
Income variations exist within different areas in Texas, and largely reflect gender
and race/ethnic differences [20, 21]. The 2011-2015 Census ACS data showed that
the median household income in 2015 inflation-adjusted dollars was $53,207 in
Texas, which was slightly lower than the national median household income of
$53,889. In Texas, non-Hispanic White households had a median income of
$65,714, Hispanic households of $41,248, and Black households of $39,345.
Poverty, lack of health care coverage, and limited access to providers are root
causes of many health disparities in Texas [22]. To determine who lives in poverty,
the U.S. Census Bureau uses a set of income thresholds that vary by family size
and composition. If a family’s total income is less than their determined income
threshold, then that family and every individual in it is considered to be in poverty.
These poverty thresholds are used throughout the U.S. and do not vary
geographically; however, they are updated each year to account for inflation. Based
on 2011-2015 Census ACS data, Texas had a higher proportion (38.0 percent) of
people living below 200 percent of the Federal Poverty Level (FPL) than the national
average of 34.3 percent.
Among the adult population aged 18 and older in Texas, counties with large
proportions of adults living below 200 percent FPL in 2011-2015 were concentrated
in the Texas-Mexico border area. Several counties in east Texas, north central
Texas, and the Texas Panhandle also had high rates of adults living below 200
percent FPL. It was also estimated that about 34.9 percent (3.6 million) of the adult
female population lived below 200 percent FPL in Texas in 2011-2015. Counties
along the Texas-Mexico border had high rates of poverty among women, as did
several counties in rural East Texas, west of Fort Worth, and between Lubbock and
Amarillo in the Panhandle (Figure 2.5). In terms of regional differences, PHR 11 had
the highest proportion of women living below 200 percent FPL (49.1 percent), and
PHR 2/3 had the lowest proportion (31.9 percent).
For children in poverty, Texas had a greater proportion of children under 5 years
old living in poverty (below 100 percent FPL) than the nation as a whole in 2011-
2015 (27.4 percent vs. 24.5 percent). About one-third of the counties in Texas had
more than 33.0 percent of their children under 5 years old living below 100 percent
FPL (Figure 2.6). By region, the poverty rate among children under 5 years old
ranged from 22.9 percent in PHR 7 to 45.6 percent in PHR 11.

OVERVIEW OF TEXAS
13
Birth Demographics
There were 403,439 live births to Texas residents in 2015, which was a 1.0 percent
increase from a decade ago. Male infants accounted for 51.1 percent of all births in
2015 and female infants accounted for 48.9 percent. While the number of births
increased by 8.0 percent in PHR 6/5S from 2006 to 2015, the number of births
decreased by 8.3 percent in PHR 11.
The birth rate was 14.7 births per 1,000
people in Texas in 2015. By region, the
birth rate ranged from 17.4 births per
1,000 in PHR 11 to 12.6 births per
1,000 in PHR 4/5N. The birth rate in
Texas as a whole has been fairly stable
since 2011, and has been consistently
higher than the national rate over the
past decade (Figure 2.7). However,
based on 2016 preliminary birth data,
the birth rate in Texas dropped slightly
to 14.2 births per 1,000 people [23].
Maternal Race/Ethnicity
Births to Hispanic mothers make up the largest percentage of all births in Texas,
followed by births to White mothers, Black mothers, and mothers classified as
‘Other’ race/ethnicity. The proportion of all births to Hispanic mothers decreased
Figure 2.7
Figure 2.5

OVERVIEW OF TEXAS
14
from 49.6 percent in 2006 to 47.4 percent in 2015. The proportion of all births to
White mothers also decreased from 34.7 percent in 2006 to 33.9 percent in 2015.
For Black mothers, the proportion of all births increased from 11.5 percent in 2006
to 11.8 percent in 2015.
Although births to mothers who are classified as ‘Other’ race/ethnicity make up a
small proportion of the total births in Texas, this race/ethnic group has had the
largest increase in the percent of total live births over the past decade, from 4.2
percent in 2006 to 7.0 percent in 2015. Over 28,000 births in 2015 were to
mothers who classified themselves as Asian, mixed race, or other race/ethnic
designations. However, it is important to know that this group is quite
heterogeneous (encompassing many different races/ethnicities), which often limits
the interpretability of results for this particular racial/ethnic category.
Maternal Age
In 2015, more than half (52.9 percent) of Texas live births were to mothers 20 to
29 years of age, 24.8 percent were to mothers 30 to 34 years of age, and 11.4
percent were to mothers 35 to 39 years of age. About 8.2 percent of live births
were to mothers younger than 20 years of age. While the percentage of births to
mothers aged 30-34 and to mothers aged 35-39 increased from 2014, the
percentage of births to mothers aged 20-29 and to mothers aged 19 or younger
decreased from 2014.
As in the United States as a whole, Texas has seen a shift in the maternal age of
women giving birth over time [24]. The average maternal age at birth in 2015 was
27.7 years of age, which was a
substantial increase from an average
age of 26.5 years in 2006. The average
age for women with a live birth in 2015
also differed by region in Texas (Figure
2.8). The oldest average maternal age
at birth occurred in PHR 7 (28.4 years of
age), and the youngest occurred in PHR
4/5N (26.3 years of age). Counties with
major urban centers, such as Dallas-Fort
Worth, Austin, and Houston areas,
tended to have an older average
maternal age.
Figure 2.8

OVERVIEW OF TEXAS
15
Teen Births
The increase in average maternal age observed over time is likely due in part to a
pronounced decrease in the teen birth rate. In 2015, a total of 32,683 babies
(about 8.1 percent of total births) were born to teenagers aged 15-19 in Texas,
which translates to a teen birth rate of 33.0 births per 1,000 females for this age
group. The teen birth rate in 2015 was a record low for Texas, but was still higher
than the corresponding teen birth rate in the nation (22.3 births per 1,000) [25]. In
Texas, the teen birth rate was much higher among adolescent females aged 18-19
(58.6 births per 1,000) than among adolescent females aged 15-17 (16.3 births per
1,000).
Texas, like the rest of the country, has reported dramatic decreases in teen birth
rates, especially since 2007 (Figure 2.9). In particular, the teen birth rate among
Hispanic youth aged 15-19 has declined by 51.3 percent from 2006 to 2015. The
teen birth rate also has decreased by
48.1 percent among Black youth and by
36.9 percent among White youth during
this timeframe. Although teen birth
rates among Hispanics and Blacks have
fallen faster than Whites, there is a wide
gap by race/ethnicity. In 2015, Hispanic
and Black teens had birth rates at least
twice as high as the rate among White
teens. Across all racial/ethnic groups,
both 15-year olds and 16-year olds had
a 56.0 percent decrease in their birth
rates from 2006 to 2015. This decrease
was the largest among each of the age
groups in the 15 to 19 years old range.
Teen birth rates vary widely across the
state. Teen birth rates are shown for
counties with 100 or more documented
births in 2015. Among these counties,
many counties along the Texas-Mexico
border, where there were large
concentrations of Hispanic women, had
high teen birth rates in 2015 (46.3
births per 1,000 or greater), as did
several counties in the Texas Panhandle
and East Texas (Figure 2.10). By region,
PHR 11 had the highest teen birth rate
Figure 2.9
Figure 2.10

OVERVIEW OF TEXAS
16
(50.9 births per 1,000), followed by PHR 9/10 (45.2 births per 1,000) and PHR 1
(43.5 births per 1,000). PHR 7 had the lowest teen birth rate in 2015 among all
Texas regions (25.5 births per 1,000).
From 2006 to 2015, all PHRs in Texas had sizeable declines in teen birth rates. PHR
7 had the largest decrease (a 51.3 percent decrease) in teen birth rates during the
past decade, and PHR 4/5N had the smallest decrease (a 36.8 percent decrease).
Infant Mortality & Morbidity
Infant mortality is the death of an infant before his or her first birthday. The
Healthy Texas Babies initiative in DSHS Title V Maternal and Child Health since
2011 has aimed to reduce infant mortality using evidence-based interventions [26].
Multiple factors and characteristics that affect infant mortality are addressed.
Infant Mortality
Infant mortality rate (IMR), the number of infant deaths per 1,000 live births,
continues to be one of the most widely used indicators of the overall health of a
community. The IMR for Texas as a whole has been at or below the national rate for
the past ten years, and since 2011, the state has consistently been below the
Healthy People 2020 (HP2020) target of 6.0 deaths per 1,000 live births [23]. The
state IMR reached a new low of 5.6 deaths per 1,000 in 2015, down from 6.2 per
1,000 in 2006. Additionally, based on 2016 preliminary death and birth files, the
state IMR remained at 5.6 deaths per 1,000 live births [23].
Racial/ethnic disparities in IMRs, however, have persisted in Texas. IMRs for Black
infants have been twice as high as IMRs for White and Hispanic infants over time
(Figure 2.11). Also, the overall decrease in IMR observed in Texas during the past
decade was not equally distributed across all racial/ethnic groups. The IMR among
Black infants decreased from 12.3 to
9.9 deaths per 1,000 live births from
2006 to 2008, then increased to 11.9
deaths per 1,000 in 2013 before
dropping to 10.9 deaths per 1,000 in
2015 – an 11.4 percent decline in the
past ten years. In comparison, the IMR
among infants classified as ‘Other’
race/ethnicity declined by 38.2 percent,
from 5.5 deaths per 1,000 in 2006 to
3.4 deaths per 1,000 in 2015.
Figure 2.11

OVERVIEW OF TEXAS
17
Regional differences in IMRs are
observed. Three regions (PHR 4/5N, PHR
8, and PHR 2/3) had IMRs higher than
the state rate in 2015, with PHR 4/5N
reporting the highest IMR of 7.2 deaths
per 1,000 live births (Figure 2.12). In
contrast, PHR 1 had the lowest IMR of
4.4 deaths per 1,000 among all Texas
regions. From 2006 to 2015, most of the
regions reported decreases in IMRs,
except for PHR 4/5N and PHR 8. The IMR
in PHR 4/5N continued to have an
upward trend in recent years, from 5.6 deaths per 1,000 in 2011 to 7.2 deaths per
1,000 in 2015. And, the IMR in PHR 8 had a recent spike from 5.1 deaths per 1,000
in 2014 to 6.3 deaths per 1,000 in 2015.
Additionally, eleven of Texas’ large communities met the HP2020 target of 6.0 or
fewer infant deaths per 1,000 live births in 2015. The Austin-Round Rock and El
Paso communities reported the lowest IMRs (3.8 deaths per 1,000 and 4.2 deaths
per 1,000, respectively). In contrast, four large Texas communities (Tyler-
Jacksonville, Victoria-Port Lavaca, Waco, and Longview-Marshall) had IMRs higher
than 7.3 deaths per 1,000 live births. Both Beaumont-Port Arthur and Fort Worth
communities had considerable declines in IMRs from 2014 to 2015.
Leading Causes of Infant Death
The top five leading causes of death among infants in Texas were congenital
malformation, short gestation and low birth weight, sudden infant death syndrome
(SIDS), maternal complications of pregnancy, and unintentional injuries. Leading
causes of infant death, however, differed by race/ethnicity [23]. The most common
cause of death among Black infants was short gestation and low birth weight, while
congenital malformation was the most common cause of death among White
infants, Hispanic infants, and infants classified as ‘Other’ race/ethnicity,
respectively. In 2015, the death rate due to short gestation and low birth weight
among Black infants (19.2 deaths per 10,000 live births) was three to five times
the rate among infants of all other racial/ethnic groups (3.5 to 7.3 deaths per
10,000 live births).
Based on 2011-2015 combined death files, congenital malformation topped the list
as the leading cause of infant death across all PHRs in Texas. PHR 7 was the only
region where SIDS did not make the top five leading causes of infant mortality.
Other causes of infant death listed as top five leading causes in all PHRs included
infections in the prenatal period, maternal complications of placenta, and neonatal
Figure 2.12

OVERVIEW OF TEXAS
18
hemorrhage. PHR 11 was the only region where neonatal hemorrhage made the top
five leading causes of infant death.
Preterm Birth
A preterm birth is one in which an infant is born before 37 weeks of gestation.
Using the obstetric estimate of gestational age, 10.2 percent of all live births in
Texas were delivered preterm in 2015, down from 11.3 percent in 2006. However,
the preterm birth rate in Texas has consistently been higher than the national
average over the past decade [23]. Based on 2016 preliminary birth data, the
preterm birth rate increased slightly to 10.4 percent in Texas.
Racial/ethnic disparities exist in preterm
birth rates. In 2015, Black infants (13.6
percent) had a higher preterm birth rate
than did infants of any other
racial/ethnic group (9.3 to 9.8 percent)
(Figure 2.13). However, over the past
decade, the preterm birth rate has
decreased most rapidly among infants
born to Black mothers, which has
slightly narrowed the racial/ethnic gap
in preterm birth rates.
Geographic differences in preterm birth
rates are observed. Among counties
with 100 or more documented live births
in 2015, many counties in the south and
south coastal area of Texas had higher
preterm birth rates than the state as a
whole (Figure 2.14). By region, PHR 11
had the highest rate of preterm births
(11.2 percent), while PHR 2/3 had the
lowest rate of preterm births (9.1
percent) in 2015. On the other hand,
from 2006 to 2015, PHR 1 had the
largest decrease of 22.5 percent in
preterm birth rates among all PHRs in
Texas.
Figure 2.13
Figure 2.14

OVERVIEW OF TEXAS
19
Low Birth Weight
Birth weight is another important factor associated with infants’ mortality. Infants
who have low birth weight (less than 2,500 grams) face infant mortality rates 25
times higher than that of their peers with birth weights of 2,500 grams or more
[27]. In 2015, there were 33,288 low birth weight infants in Texas, which
represented 8.3 percent of total live births. This rate was slightly higher than the
national rate (8.1 percent), and did not meet the HP2020 target of 7.8 percent or
fewer of all live births weighing less than 2,500 grams. The rate of low birth weight
infants has not changed much since 2006, either in Texas or in the nation [23].
Based on 2016 preliminary birth data, the low birth weight rate was 8.4 percent in
Texas.
As with IMRs and preterm births, Black mothers have a disproportionately high
percentage of low birth weight infants. In 2015, the rate of low birth weight infants
was 13.3 percent among Black mothers,
compared with 9.1 percent among
mothers of ‘Other’ race/ethnicity, 7.7
percent among Hispanic mothers, and
7.1 percent among White mothers
(Figure 2.15). Over the past decade, low
birth weight rates have decreased
among Black infants and White infants,
while rates have remained stable among
Hispanic infants and infants of ‘Other’
race/ethnicity.
Rates of low birth weight infants vary
across different areas of the state. In
2015, some counties met the HP2020
target of 7.8 percent or less for the
percentage of low birth weight infants,
but many counties did not (Figure 2.16).
Counties with high percentages (9.2
percent or greater) of low birth weight
infants were dispersed across the state.
There were no clear geographic patterns
for low birth weight rates across the
state. In 2015, PHR 7 had the lowest
rate of low birth weight infants among
all Texas regions (7.6 percent), while
PHR 8 had the highest rate (8.6
percent). Overall, the regional
Figure 2.15
Figure 2.16

OVERVIEW OF TEXAS
20
differences in low birth weight rates were somewhat less pronounced than the
regional differences in preterm birth rates. From 2006 to 2015, the low birth weight
rate declined by 17.6 percent in PHR 1, whereas the low birth weight rate did not
change much in other regions.
17P Prescription
Women who are at risk for a preterm birth are sometimes prescribed progesterone
supplementation by her health care provider. The Texas PRAMS survey asks
women, “During your most recent pregnancy, did a doctor, nurse, or other health
care worker try to keep your new baby from being born too early by giving you a
series of weekly shots of a medicine called Progesterone, Makena®, or 17P (17-
alpha-hydroxyprogesterone)?” Based on statewide PRAMS data, trends in the
prevalence of 17P use ranged from 4.8 percent (CI: 3.6-6.1) in 2009 to 5.6 percent
(CI: 4.1-7.2) in 2015.
The prevalence rate of 17P use for White/Other women and Hispanic women has
been similar to the statewide prevalence rate over time; however, the prevalence
rate for Black women has traditionally been higher. In 2015, Black women had the
highest prevalence rate of 17P use (6.2 percent, CI: 3.6-8.7), followed by Hispanic
women (5.8 percent, CI: 3.1-8.5) and White/Other women (5.3 percent, CI: 3.3-
7.3). The prevalence rate of 17P use among Black women has decreased from 10.3
percent (CI: 7.2-13.5) in 2014.
Among all PHRs in Texas, the pooled 2011-2015 PRAMS data revealed that PHR 1
had the highest rate of 17P use (8.1 percent, CI: 3.2-13.0) and PHR 7 had the
lowest rate of 17P use (4.4 percent, CI: 2.7-6.0). Using pooled 2011-2015 data,
the statewide prevalence rate of 17P use was 5.5 percent (CI: 4.8-6.2).

OVERVIEW OF TEXAS
21
Health Care Coverage and Access
Health care coverage and access to health care are fundamental to the health of
Texans. A major finding that emerged from the Title V stakeholder meetings was
that limited access to health care was a widespread concern [22].
Health Insurance
Based on 2011-2015 Census ACS data, more than 5.36 million Texans did not have
health insurance. Texas led the nation in the proportion of the total population
without health insurance coverage in 2011-2015 (20.6 percent). The national
uninsured rate was 13.0 percent. In terms of race/ethnicity, higher rates of
uninsured were observed among Hispanics (31.9 percent), Blacks (18.3 percent),
and Whites (11.8 percent) in Texas, compared with national rates (Hispanics, 25.8
percent; Blacks, 15.3 percent; Whites, 9.0 percent).
Texas also had higher proportions of uninsured women of reproductive age (ages
18-44) and uninsured children compared to the nation. About 30.4 percent of
women aged 18-44 in Texas were uninsured in 2011-2015, compared to 18.7
percent nationwide. About 8.5 percent of children younger than 6 years old in
Texas were uninsured, compared to 5.2 percent nationwide.
Counties along the Texas-Mexico border
as well as several counties outside
Lubbock and Waco had high proportions
(36.6 percent or more) of women aged
18-44 without health insurance (Figure
2.17). A few large counties (Houston,
Dallas, Hidalgo, and El Paso counties)
had higher rates of uninsured women of
reproductive age than did the state as a
whole. In terms of regional differences,
the uninsured rate among women aged
18-44 ranged from 22.3 percent in PHR
7 to 47.4 percent in PHR 11.
Figure 2.17

OVERVIEW OF TEXAS
22
On the other hand, counties with high
proportions (10.3 percent or more) of
uninsured children younger than 6 years
old were concentrated in west Texas
between Odessa and San Antonio, as
well as in the Panhandle area (Figure
2.18). A few large counties (Harris,
Dallas, and Hidalgo counties) had higher
rates of uninsured children for this age
group than did the state as a whole. In
terms of regional differences, the
uninsured rate among children younger
than 6 years of age ranged from 6.8
percent in PHR 7 to 9.6 percent in PHR
9/10.
Health Professionals and Shortage Areas
Given the size of the state and the vast distances between facilities for health
services in rural areas, access to care in Texas can be a challenge. According to the
most recent health professions data, there were 20,578 primary care physicians
(PCPs) in Texas in 2016, with a density of 72.9 PCPs per 100,000 population [28].
Twenty-nine counties in Texas had no PCP in 2016. Overall, urban counties in the
state (75.9 PCPs per 100,000 population) had better access to PCPs than the rural
counties (49.4 PCPs per 100,000 population). By region, PHR 9/10 had the lowest
density of 54.4 PCPs per 100,000 population and PHR 2/3 had the highest density
of 78.0 PCPs per 100,000 population. Counties in the Panhandle, West Texas, and
the Texas-Mexico border area typically had lower PCPs per 100,000 population.
There were 2,594 obstetrics and/or gynecology specialists (OB/GYNs) in Texas,
with a density of 18.3 OB/GYNs per 100,000 females in the population. A little over
58 percent of the counties in Texas (148 counties) had no OB/GYN in 2016. Overall,
the OB/GYN density in urban counties (19.4 OB/GYNs per 100,000 females) was
two times as high as that in rural counties (9.1 OB/GYNs per 100,000 females). In
terms of regional differences, PHR 11 had the lowest density of 13.5 OB/GYNs per
100,000 females, and PHR 6/5S had the highest density of 20.8 OB/GYNs per
100,000 females.
Health Professional Shortage Areas (HPSAs) are designated by employing a ratio of
population to PCPs to determine whether or not an area has a shortage of
physicians. The ratio threshold is 3,500:1 and is reduced to 3,000:1 in areas with
high needs, such as at least 20 percent of population below poverty level or more
than 20 infant deaths per 1,000 live births [29]. Areas that exceed these ratios may
Figure 2.18

OVERVIEW OF TEXAS
23
qualify for designation as HPSAs. Other factors, such as time/distance to nearest
source of care and population composition, are also included in the federal HPSA
criteria. As of September 2017, over 34 percent of Texans had unmet primary care
needs based on the primary care HPSA ratios [30].
Recruiting and retaining health
professionals is an ongoing challenge not
only in rural areas, but in some urban
areas as well. In rural areas, retention of
health professionals is mostly due to
population size, but in some urban
areas, access is limited because many
providers do not accept Medicaid or
patients are not enrolled in Medicaid and
unable to pay out-of-pocket. Most
counties in Texas are designated as
either a whole-county or a partial-county
HPSA (Figure 2.19). A little over 25
percent of Texas counties (65 counties)
were not designated as a geographic or
population HPSA as of June 2017.
Prenatal Care in the First Trimester
The HP2020 target is to increase the proportion of pregnant women who receive
prenatal care beginning in the first trimester of pregnancy to 77.9 percent. Texas,
as a whole, is not meeting this target percentage. In 2015, about 65.9 percent of
mothers in the state entered prenatal care within the first trimester (Figure 2.20).
The 2016 preliminary birth data showed a small decrease in timely access to
prenatal care to 65.1 percent in Texas [23].
Disparities in timely prenatal care
access exist among different
racial/ethnic groups. A larger proportion
of White women begin receiving
prenatal care in the first trimester of
pregnancy, compared with all other
racial/ethnic groups. In 2015, 75.2
percent of White mothers reported
receiving prenatal care in the first
trimester of pregnancy, compared with
56.6 percent of Black mothers, 61.1
percent of Hispanic mothers, and 67.0
Figure 2.19
Figure 2.20

OVERVIEW OF TEXAS
24
percent of mothers classified as ‘Other’ race/ethnicity. Timely access to prenatal
care increased in Texas from 2009 to 2011 (mostly driven by a sharp increase in
the percentage of Hispanic mothers receiving prenatal care in the first trimester
during this timeframe), but has decreased slightly since 2011. Unlike other
racial/ethnic groups, mothers of ‘Other’ race/ethnicity showed a continuous
decrease in timely access to prenatal care from 2006 to 2015.
Late entry into prenatal care is a
statewide problem. Among counties with
100 or more documented live births in
2015, only one urban county
(Williamson County, in central Texas)
met the HP2020 target percentage of
women entering prenatal care in the
first trimester (Figure 2.21). High
proportions (37.6 percent or greater) of
women not receiving prenatal care in
the first trimester were concentrated
mostly in East Texas, South Texas, and
west of Lubbock and Amarillo in the
Panhandle. In 2015, PHR 7 had the
lowest proportion of mothers who did
not receive prenatal care within the first
trimester of pregnancy (25.9 percent), whereas PHR 11 had the highest proportion
(37.1 percent). From 2006 to 2015, decreases in late entry into prenatal care were
observed in most regions, except for PHR 6/5S and PHR 8.
Prenatal Care as Early as Wanted
Early prenatal care allows for early and timely treatment that can help manage or
prevent health problems. The PRAMS survey asks women, “Did you get prenatal
care as early in your pregnancy as you wanted?” Based on statewide PRAMS data,
trends in the prevalence of prenatal care as early as the mother wanted increased
only slightly, from 77.2 percent (CI: 74.5-79.8) in 2009 to 78.4 percent (CI: 75.5-
81.4) in 2015.
The prevalence rate among White/Other women in Texas has been consistently
higher than the statewide prevalence rate over time, compared with the prevalence
rates among Black and Hispanic women which have been lower (Figure 2.22). In
2015, White/Other women had the highest rate of obtaining prenatal care as early
Figure 2.21

OVERVIEW OF TEXAS
25
as they wanted (82.1 percent, CI: 78.4-85.8), compared with Black women (76.7
percent, CI: 72.4-81.1) and Hispanic women (75.7 percent, CI: 70.6-80.9).
Based on pooled 2011-2015 PRAMS data, PHR 7 and PHR 8 had the highest rate of
obtaining prenatal care as early as they wanted (81.4 percent, CI: 77.8-85.1 and
80.9 percent, CI: 76.5-85.4, respectively) (Figure 2.23). On the other hand, PHR 1
had the lowest rate (73.2 percent, CI: 64.9-81.4) among all PHRs in Texas. Using
pooled 2011-2015 data, the statewide prevalence rate of receiving prenatal care as
early as they wanted was 79.1 percent (CI: 77.8-80.5).
Barriers to Prenatal Care
Understanding the barriers women experience related to prenatal care is also
important because women who experience late or no prenatal care are at higher
risk for pregnancy complications and health problems. Women who indicated they
did not get prenatal care as early as they wanted in the PRAMS survey were then
asked a series of questions about barriers and obstacles, “Did any of these things
keep you from getting prenatal care when you wanted it?”
The survey questions included the following: a) I couldn’t get an appointment when
I wanted one; b) I didn’t have enough money or insurance to pay for my visits; c) I
didn’t have any transportation to get to the clinic or doctor’s office; d) The doctor or
my health plan would not start care as early as I wanted; e) I had too many other
things going on; f) I couldn’t take time off from work or school; g) I didn’t have my
Medicaid or Texas Health Steps card; h) I didn’t have anyone to take care of my
children; i) I didn’t know that I was pregnant; and j) I didn’t want anyone else to
know I was pregnant.
Based on pooled 2011-2015 PRAMS data, 20.9 percent (CI: 19.5-22.2) of women in
Texas did not receive prenatal care as early as they wanted, and the five most
frequently noted barriers were:
1) I didn’t have my Medicaid or Texas Health Steps card;

OVERVIEW OF TEXAS
26
2) I didn’t have enough money or insurance to pay for my visits;
3) I didn’t know that I was pregnant;
4) I couldn’t get an appointment when I wanted one; and
5) The doctor or my health plan would not start care as early as I wanted.
Barriers to Maternal & Child Health Services
Many Texans face significant barriers to accessing health care. Stakeholder
feedback and identification of the needs and challenges, however, can lead to policy
improvements and strategic planning initiatives for improving access across the
state.
As part of the DSHS 2015 Title V Needs Assessment, a report that is submitted
every five years under the Maternal and Child Health (MCH) Block Grant program,
qualitative information on community needs was gathered through focus groups
and stakeholder meetings [22]. In the summer of 2014, SUMA Social Marketing,
Inc. (SUMA) conducted 16 focus groups statewide to gather qualitative data on the
health needs of mothers, men, children, and youth in various communities. Twelve
of the focus groups were held with women between the ages of 19 and 30 who had
at least one child three years of age or younger. An additional four focus groups (in
San Antonio and San Angelo) were held with men between the ages of 19 and 30
who worked in the oil and gas field or in an industrial environment. SUMA also
facilitated eight meetings across the state with providers and other stakeholders to
gather their perceptions of the needs of the clients and patients they served.
A central theme that emerged from the stakeholder meetings and focus groups was
the need to improve access to a variety of health care services; this was a priority
need in most regions in the state. Stakeholders enumerated many different types of
factors that they believed limited access to health care. The main barriers were the
inability to pay, undocumented status, a shortage of primary care providers and
specialists, and a limited number of Medicaid providers. Other causes of limited
access included lack of awareness of available services, lack of transportation, lack
of culturally-sensitive providers, and difficulty of navigating affordable
insurance/Medicaid system. For pregnant women, the delays in establishing
eligibility for Medicaid prevented them from accessing prenatal care services earlier.
In addition to limited access to health care, obesity and diabetes were also
identified as top health care concerns statewide.
A number of the focus groups identified areas that, if better funded, could
potentially improve access to health care services: health education for parents and
children, case management and other forms of support in navigating the system,
improved coordination and collaboration among providers, better continuity of care,
and a shift to a focus on the whole person across the life course.

OVERVIEW OF TEXAS
27
Maternal Health
To reduce infant mortality and improve infant health outcomes, it’s very important
to understand and assess the maternal health before, during, and after pregnancy.
Selected maternal indicators are discussed, including obesity, hypertension &
diabetes, smoking, drinking, physical abuse, postpartum depression, and
postpartum checkup. Statewide information regarding maternal mortality and
morbidity are also included in the section.
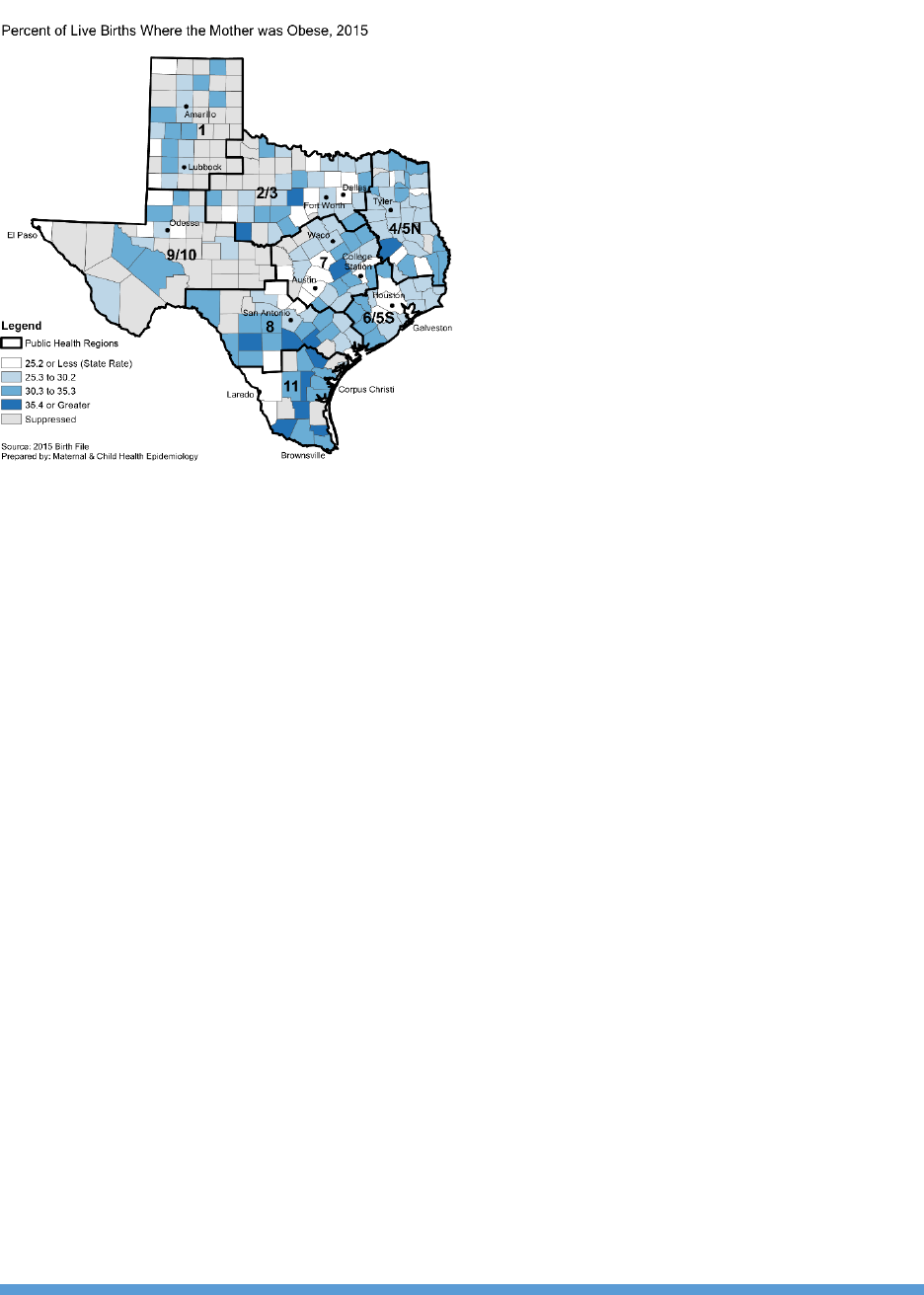
Pre-Pregnancy Obesity
Obesity among women of reproductive age is of great concern, becase of its
association with multiple adverse maternal and infant health outcomes. A recent
study has found that pre-pregnancy obesity is strongly related to infant mortality,
and deaths from congenital anomalies and SIDS are much higher among babies
born to obese mothers than to mothers with normal pre-pregnancy weights [31].
Obesity is also a well-established risk factor for a variety of pregnancy and birth
complications, including gestational diabetes, preeclampsia, miscarriage, and
cesarean delivery [32, 33].
A rise in pre-pregnancy obesity has been observed over time, both in Texas and in
other states [34]. The statewide proportion of mothers with a pre-pregnancy body
mass index (BMI) in the obese range increased from 20.1 precent in 2006 to 25.2
percent in 2015. Based on 2016 preliminary birth data, the pre-pregnancy obsesity
rates continued to increase to 25.9 percent in Texas [23].
Black and Hispanic mothers had higher
percentages of obesity before pregnancy
than did White mothers and mothers of
‘Other’ race/ethnicity (Figure 2.24). In
2015, pre-pregnancy obesity was almost
three times more prevalent among Black
mothers (31.0 percent) than among
mothers of ‘Other’ race/ethnicity (11.8
percent). However, since 2006, the pre-
pregnancy obesity rate in Texas has
increased most sharply among mothers
of ‘Other’ race/ethncity (a 55.3 percent increase). Hispanic mothers have also seen
a relatively large increase in pre-pregnancy obesity between 2006 and 2015 (a 33.2
percent increase among Hispanic mothers, compared with increases of 19.7 percent
and 19.2 percent among White and Black mothers, respectively).
Figure 2.24
OVERVIEW OF TEXAS
28
Many rural and suburban counties in
Texas have higher pre-pregnancy
obesity rates than the state as a whole.
In 2015, a few counties in the southern
area had high rates of pre-pregnancy
obesity (35.4 percent or greater), when
compared to the rest of the state
(Figure 2.25). Overall, mothers in rural
counties in the state (30.3 percent)
experienced a higher rate of pre-
pregnancy obesity than their urban
counterparts (24.6 percent). In 2015,
PHR 2/3 had the lowest rate of pre-
pregancy obesity (22.1 percent), while
PHR 11 had the highest rate of pre-
pregnancy obesity (30.4 percent). From
2006 to 2015, increases in pre-pregnancy obesity rates were observed among all
regions in Texas. Of particular note, the pre-pregancy obesity rate has increased
substantially in PHR 2/3 by almost one-third over the past decade.
Maternal Hypertension & Diabetes
Hypertension (high blood pressure) and diabetes are two common medical
problems encountered during pregnancy. Babies born to women with diabetes are
at an increased risk for a variety of complications, including preterm birth, low
blood sugar, respiratory distress syndrome, and birth injury [35]. Hypertensive
related pregnancy complications can lead to fetal growth retardation, fetal death,
and maternal mortality and morbidity [36]. Hypertension/eclampsia is a diagnosis
closely related to severe maternal morbidity, and a leading cause of maternal death
for Black women in Texas [37].
According to 2015 birth certificate data, 7.4 percent of all live births in Texas were
to mothers with some form of hypertension, and 5.5 percent of all live births were
to mothers who had diabetes (these mothers either had hypertension or diabetes
pre-pregnancy, or developed the condition over the course of the pregnancy). Rates
of both maternal hypertension and maternal diabetes have increased since 2006
(Figure 2.26 & Figure 2.27). Based on 2016 preliminary birth data, the maternal
hypertension rate was 7.5 percent and the maternal diabetes rate was 5.7 percent
in Texas [23].
Both maternal hypertension and diabetes rates vary by race/ethnicity. Of all
racial/ethnic groups, Black mothers followed by White mothers have the highest
Figure 2.25

OVERVIEW OF TEXAS
29
percentages of maternal hypertension over time, while mothers of ‘Other’
race/ethnicity followed by Hispanic mothers have the highest percentages of
maternal diabetes. From 2006 to 2015, the maternal hypertension rate among
Black mothers was 1.9 to 2.2 times that of mothers of ‘Other’ race/ethnicity, who
were least likely to have diagnosed hypertension before and/or during pregnancy
(Figure 2.26). In 2015, the maternal diabetes rate was 8.2 percent among mothers
of ‘Other’ race/ethnicity, 6.1 percent among Hispanic mothers, 4.6 percent among
Black mothers, and 4.4 percent among White mothers (Figure 2.27).
Among all PHRs in Texas, both PHR 4/5N and PHR 8 had the highest rates of
maternal hypertension in 2015 (8.7 percent), while PHR 11 had the lowest rate of
maternal hypertension (6.0 percent) (Figure 2.28). On the other hand, PHR 1 had
the highest percentage of live births to mothers with diabetes (7.4 percent), while
PHR 9/10 had the lowest percentage (3.8 percent) (Figure 2.29). Overall, mothers
in rural counties (8.1 percent) experienced a higher prevalence of maternal
hypertension than their urban counterparts (7.3 percent). Statewide, small
urban/rural differences were observed in the prevalence of maternal diabetes.
Figure 2.26
Figure 2.27
Figure 2.28
Figure 2.29

OVERVIEW OF TEXAS
30
As mentioned earlier, pre-pregnancy obesity is associated with both hypertension
and diabetes during pregnancy [32, 33]. In 2015, 20.7 percent of all mothers in
Texas with pre-pregnancy obesity also had hypertension, diabetes, or both
conditions. In contrast, 7.2 percent of mothers with normal pre-pregnancy BMI
were hypertensive, diabetic, or had both conditions.
Maternal Smoking
Women and their offspring face additional health risks if women smoke cigarettes
during pregnancy, as smoking increases the risk of low birthweight, prematurity,
placenta previa, placental abruption, and SIDS [38]. Texas is one of the better
performing states when it comes to maternal smoking before and during pregnancy
[39].
In Texas, the reported rate of smoking
three months before pregnancy has
decreased from 8.2 percent in 2006 to
5.4 percent in 2015 (Figure 2.30). This
rate is better than the HP2020 target of
14.6 percent. All racial/ethnic groups in
the state have met the HP2020 target
rate since 2010. Part of the reason for
the low maternal smoking rate in the
state is because of a large number of
births to Hispanic women – about 47.4
percent of all births in Texas were to
Hispanic women in 2015. Overall, Hispanic women have a lower prevalence of
smoking before pregnancy than women of all other races/ethnicities in Texas. In
2015, only 2.1 percent of Hispanic women and 2.7 percent of women of ‘Other’
race/ethnicity smoked three months prior to becoming pregnant, compared with
5.3 percent of Black women and 10.6 percent of White women.
Hispanic women and women of ‘Other’
race/ethnicity also have the lowest
prevalence of smoking during pregnancy
over time (Figure 2.31). In 2015, only
Hispanic women (1.0 percent) were
meeting the HP2020 target of at least
98.6 percent abstinence from smoking
during pregnancy in Texas. Based on
2016 preliminary birth data, both
Hispanic women (1.0 percent) and
women of ‘Other’ race/ethnicity (1.3
Figure 2.30
Figure 2.31

OVERVIEW OF TEXAS
31
percent) were meeting the HP2020 target rate [23]. While the overall proportion of
women who smoke during pregnancy has decreased by two-fifths in Texas from
2006 (6.0 percent) to 2015 (3.6 percent), there is still room for improvement,
especially among White women.
In 2007, 29.2 percent of women who smoked three months prior to pregnancy
abstained from smoking (did not smoke at all) once becoming pregnant. In 2015,
this rate of total abstinence from smoking during pregnancy among previous
smokers increased to 35.2 percent [23].
Geographic differences in rates of
smoking during pregnancy exist across
the state. In 2015, counties near the
Texas-Mexico border generally had
lower rates of smoking during
pregnancy, while higher rates of
smoking during pregnancy were seen in
many counties in East and North Texas
(Figure 2.32). By region, PHR 4/5N had
the highest rate of smoking during
pregnancy in 2015 (12.1 percent),
followed by PHR 1 (7.5 percent) and
PHR 7 (4.3 percent). PHR 11 had the
lowest rate (1.1 percent) and was the
only region meeting the HP2020 target
of at least 98.6 percent abstinence from smoking during pregnancy. From 2006 to
2015, all regions in Texas had dramatic declines in the prevalence of smoking
during pregnancy.
Drinking During Pregnancy
Alcohol use during pregnancy has been associated with several adverse outcomes
for the baby, including Fetal Alcohol Syndrome (FAS) and other Fetal Alcohol
Spectrum Disorders (FASD), birth defects, and low birth weight [40]. The PRAMS
survey asks women, “During the last 3 months of your pregnancy, how many
alcoholic drinks did you have in an average week?” According to CDC, the definition
of “drinking” is someone who has any amount of alcohol during an average week.
Based on statewide PRAMS data, trends in the prevalence of drinking in the last
three months of pregnancy ranged from 5.7 percent (CI: 4.4-7.0) in 2009 to 7.7
percent (CI: 6.0-9.4) in 2015.
The prevalence rate of drinking in the last three months of pregnancy among
Hispanic women and Black women in Texas has been generally below the statewide
Figure 2.32

OVERVIEW OF TEXAS
32
prevalence rate over time, with White/Other women demonstrating the highest
prevalence rate (Figure 2.33). In 2015, White/Other women had the highest rate of
drinking in the last three months of pregnancy (10.0 percent, CI: 7.2-12.8),
followed by Black women (9.3 percent, CI: 6.3-12.3) and Hispanic women (5.3
percent, CI: 2.7-7.8). For Black women, the 2015 prevalence rate of drinking in the
last three months of pregnancy surpassed the statewide prevalence rate for the
first time since 2010.
There are regional differences in the prevalence of drinking during pregnancy.
Based on pooled 2011-2015 PRAMS data, both PHR 2/3 (9.1 percent, CI: 7.4-10.8)
and PHR 7 (8.9 percent, CI: 6.6-11.3) had the highest rate of drinking in the last
three months of pregnancy, while PHR 4/5N (4.4 percent, CI: 2.1-6.8) had the
lowest rate of drinking in the last three months of pregnancy (Figure 2.34). Using
pooled 2011-2015 data, the statewide prevalence rate was 7.8 percent (CI: 7.0-
8.7).
Physical Abuse Before/During Pregnancy
Physical abuse before and/or during pregnancy has been associated with adverse
outcomes for the mother and the infant. The PRAMS survey asks women: “During
the 12 months before you got pregnant with your new baby, did your husband or
partner push, hit, slap, kick, choke, or physically hurt you in any other way?” and
“During your most recent pregnancy, did your husband or partner push, hit, slap,
kick, choke, or physically hurt you in any other way?”
Women who answered “yes” to one or both of the questions above were considered
as having experienced physical abuse by a husband or partner before and/or during
pregnancy. Women under the age of 18 were not asked questions on abuse. Based
on statewide PRAMS data, trends in the prevalence of physical abuse before and/or
during pregnancy ranged from 6.9 percent (CI: 5.2-8.5) in 2009 to 2.5 percent (CI:
1.4-3.6) in 2015.
Figure 2.33
Figure 2.34

OVERVIEW OF TEXAS
33
The prevalence rate of physical abuse before and/or during pregnancy among Black
women and Hispanic women in Texas has been generally higher than the statewide
prevalence rate over time, with White/Other women demonstrating the lowest
prevalence rate (Figure 2.35). In 2015, Black women reported the highest rate of
physical abuse before and/or during pregnancy (5.2 percent, CI: 2.9-7.5), followed
by Hispanic women (3.5 percent, CI: 1.4-5.5) and White/Other women (0.6
percent, CI: 0.0-1.4).
Based on pooled 2011-2015 PRAMS data, PHR 11 had the highest rate of physical
abuse before and/or during pregnancy (6.9 percent, CI: 4.0-9.8), while PHR 2/3
had the lowest rate of abuse before and/or during pregnancy (2.8 percent, CI: 1.8-
3.7) (Figure 2.36). Using pooled 2011-2015 data, the statewide prevalence rate
was 4.0 percent (CI: 3.4-4.6).
Postpartum Depression
Postpartum depression (PPD) is a type of clinical depression that is thought to
affect 10-15 percent of women after childbirth [41]. CDC provides the participating
PRAMS states an indicator of PPD symptoms based on these two questions: “Since
your new baby was born, how often have you felt down, depressed, or hopeless?”
and “Since your new baby was born, how often have you had little interest or little
pleasure in doing things?” These two questions asking about PPD symptoms were
included on the 2012-2015 Texas PRAMS survey. Based on statewide PRAMS data,
trends in the prevalence of PPD symptoms ranged from 12.4 percent (CI: 9.8-15.0)
in 2012 to 14.7 percent (CI: 12.3-17.2) in 2015.
The prevalence rate for PPD symptoms among White/Other women and Hispanic
women in Texas has been generally below the statewide prevalence rate over time,
with Black women demonstrating the highest prevalence rate (Figure 2.37). In
2015, Black women had the highest rate of PPD symptoms (18.5 percent, CI: 14.4-
Figure 2.35
Figure 2.36

OVERVIEW OF TEXAS
34
22.5), followed by Hispanic women (15.4 percent, CI: 11.2-19.6) and White/Other
women (12.9 percent, CI: 9.6-16.1).
Regional differences in the prevalence of PPD symptoms are observed in Texas.
Based on pooled 2012-2015 PRAMS data, both PHR 6/5S and PHR 11 had the
highest rate of PPD symptoms (15.7 percent, CI: 13.3-18.2 and 15.6 percent, CI:
10.7-20.5, respectively), while PHR 7 had the lowest rate of PPD symptoms (10.7
percent, CI: 7.6-13.8) (Figure 2.38). Using pooled 2012-2015 data, the statewide
prevalence rate was 13.8 percent (CI: 12.6-15.1).
Postpartum Checkup
Postpartum visits are important for screening and assessing the health of the
mother. The PRAMS survey asks women, “Since your new baby was born, have you
had a postpartum checkup for yourself? A postpartum checkup is the regular
checkup a woman has about 4-6 weeks after she gives birth.” Based on Texas
PRAMS data, trends in the statewide prevalence of a postpartum checkup ranged
from 83.9 percent (CI: 81.5-86.3) in 2009 to 86.1 percent (CI: 83.6-88.5) in 2015.
The prevalence rate of postpartum checkup among Hispanic women and Black
women in Texas has been generally below the statewide prevalence rate over time,
with White/Other women demonstrating the highest prevalence rate (Figure 2.39).
Figure 2.37
Figure 2.39
Figure 2.40

OVERVIEW OF TEXAS
35
In 2015, White/Other women had the highest postpartum visit rate (90.8 percent,
CI: 88.0-93.5), followed by Black women (89.9 percent, CI: 86.7-93.1) and
Hispanic women (81.1 percent, CI: 76.6-85.7).
Regional differences also exist in the prevalence rate of postpartum visits. Based on
pooled 2011-2015 PRAMS data, PHR 1 had the highest postpartum visit rate (92.4
percent, CI: 87.7-97.1), whereas PHR 11 had the lowest postpartum visit rate
(73.7 percent, CI: 68.4-78.9) (Figure 2.40). Using pooled 2011-2015 data, the
statewide prevalence rate of postpartum visits was 86.0 percent (CI: 84.9-87.2).
Maternal Mortality & Morbidity
Maternal mortality and morbidity are important indicators of the quality of health
and healthcare in a population. Recent trends in maternal mortality and severe
maternal morbidity are discussed in this section.
Maternal Mortality
The death of a mother is an immeasurable loss for her children and family. In this
report, maternal death is defined as the death of a woman while pregnant or within
365 days of the end of a pregnancy from causes associated with or aggravated by
the pregnancy [42].
The maternal mortality rate (MMR) is the number of maternal deaths while
pregnant or within 42 days of the end of pregnancy for every 100,000 live births.
Compared to the other 49 states and District of Columbia, Texas ranked 44
th
in the
nation for overall MMR for the combined years 2005-2014 [43]. Maternal mortality
rates have been increasing in Texas and in the United States over the past decade.
This increase could be partly attributed to rising rates of chronic health conditions,
such as hypertension, diabetes, and chronic heart disease [44]. However, some
research suggests that recent observed increases in MMR may be due to changes in
medical coding, changes in surveillance, and data error on death certificates [45,
46].
Because the majority of maternal deaths occur after 42 days postpartum, the rest
of the maternal death statistics shown focus on numbers and corresponding rates of
maternal death while pregnant or within 365 days of the end of pregnancy. Also,
because of potential data issues associated with identifying maternal deaths using
death certificate data alone [46], only confirmed maternal deaths were used to
calculate these maternal death rates. Maternal deaths were confirmed by matching
each woman's death record with a birth or fetal death event within 365 days. In
Texas, there were 382 confirmed maternal deaths in the four-year period between
2012 and 2015.

OVERVIEW OF TEXAS
36
For the combined years 2012-2015, the
rate of maternal death among Black
mothers (42.6 per 100,000 live births)
was 1.5 times higher than the rate
among White mothers (27.6 per 100,000
live births) and 2.2 times higher than
the rate among Hispanic mothers (19.2
per 100,000 live births) (Figure 2.41).
Mothers aged 40 years and older had
the highest maternal death rate of all age groups, at 55.0 maternal deaths per
100,000 live births. Higher rates of maternal death were also observed among
women with diabetes (39.9 per 100,000 live births), hypertension (56.3 per
100,000 live births), and pre-pregnancy obesity (29.2 per 100,000 live births), as
well as among women who smoked during pregnancy (86.0 per 100,000 live
births).
Between 2012 and 2015, the most common specific causes of death for mothers
during pregnancy or within 365 days postpartum were drug overdose (16.8
percent), cardiac event (14.4 percent), homicide (11.0 percent), suicide (8.6
percent), and infection/sepsis (8.4 percent). The top causes of maternal death
during pregnancy or within 7 days postpartum were hemorrhage (19.0 percent),
cardiac event (17.7 percent), and amniotic embolism (12.7 percent).
The relatively large proportion of maternal deaths in Texas due to drug overdose is
particularly concerning in light of the current opioid epidemic and recent increases
in maternal opioid use during pregnancy [47]. The risk of maternal death due to
drug overdose was higher for White mothers and for mothers aged 40 years or
older. Opioids were involved in 58 percent of maternal deaths from drug overdose,
and almost 80 percent of drug overdose deaths occurred after 60 days postpartum.
Among all PHRs in Texas, PHR 1 had the
highest maternal death rate (34.0 per
100,000 live births) and PHR 11 had the
lowest maternal death rate (17.8 per
100,000 live births) for the combined
years 2012-2015 (Figure 2.42). PHR
2/3 had the highest drug overdose
maternal death rate, at 6.4 maternal
deaths from drug overdose per 100,000
live births, followed by PHR 1 (6.0 per
Figure 2.41
Figure 2.42

OVERVIEW OF TEXAS
37
100,000 live births) and PHR 9/10 (5.2 per 100,000 live births). PHR 4/5N had the
lowest drug overdose maternal death rate (1.3 per 100,000 live births).
Severe Maternal Morbidity
Severe maternal morbidity (SMM) is a term used to describe any unintended
outcomes of labor and delivery that result in significant consequences for a
mother’s health [48]. A hospital delivery was considered a SMM case if the mother
had one or more of the conditions or procedures indicated on a list of SMM-related
medical codes, including conditions such as acute renal failure, cardiac arrest,
eclampsia, and sepsis, and including procedures such as blood transfusion and
hysterectomy.
SMM is closely related to maternal mortality because it involves conditions that, if
left untreated, could result in maternal death. Like maternal mortality, SMM rates in
the United States have been rising in the past decade. According to data from
Texas Hospital Inpatient Discharge Public Use Data Files, the SMM rate in Texas
increased by 19.3 percent between 2006 and 2011, from 174.1 cases per 10,000
delivery hospitalizations to 207.7 cases per 10,000 delivery hospitalizations.
However, Texas has seen a slight decrease in SMM between 2011 and 2014. There
was also a substantial decrease in SMM observed between 2014 and 2015, from
205.6 cases per 10,000 delivery hospitalizations to 172.4 cases per 10,000 delivery
hospitalizations, but SMM rates for 2015 are based only on 3 quarters of data (due
to a coding change) and therefore may not be as reliable as previous years’ rates.
Blood transfusions during delivery hospitalizations were used to estimate obstetric
hemorrhage, the top contributor of SMM. Trends in obstetric hemorrhage rates
were similar to those seen in overall SMM. Other common causes of SMM included
cardiac event, disseminated intravascular coagulation (DIC), hysterectomy, and
eclampsia.
Mirroring the trends observed for
maternal deaths, there are substantial
racial/ethnic disparities in the rates of
mothers with serious pregnancy
complications. Black mothers in Texas
had an SMM rate at least 1.2 times
higher than SMM rates observed among
mothers of other racial/ethnic groups,
with 235.6 SMM cases per 10,000
delivery hospitalizations in 2015
compared with 180.6 cases per 10,000
delivery hospitalizations for Hispanic
Figure 2.43

OVERVIEW OF TEXAS
38
mothers and 142.3 cases per 10,000 delivery hospitalizations for White mothers
(Figure 2.43). Although White mothers had higher maternal death rates than did
Hispanic mothers, the opposite was true for SMM – higher SMM rates were
observed among Hispanic mothers than among White mothers. Similarly, rates of
obstetric hemorrhage were highest among Black mothers, followed by Hispanic
mothers and then White mothers.
Four public health regions had SMM
rates above the Texas rate in 2015: PHR
6/5S (201.2 cases per 10,000 delivery
hospitalizations), PHR 8 (185.5 cases
per 10,000 delivery hospitalizations),
PHR 1 (175.2 cases per 10,000 delivery
hospitalizations) and PHR 9/10 (173.4
cases per 10,000 delivery
hospitalizations) (Figure 2.44). The
lowest regional SMM rates were seen in
PHR 7 (128.4 cases per 10,000 delivery
hospitalizations) and PHR 4/5N (147.8 cases per 10,000 delivery hospitalizations).
Maternal Drug Use and Neonatal Abstinence Syndrome
The use of opioids or certain other drugs during pregnancy can result in a drug
withdrawal syndrome in newborns called neonatal abstinence syndrome (NAS).
Newborns with NAS are more likely than other infants to have low birthweight,
respiratory and feeding problems, and other complications [47]. Similarly, mothers
who use drugs such as opioids during pregnancy are more likely to have
complications, such as prolonged hospital stay and death before hospital discharge
[49]. Since drug overdose is a frequent cause of maternal death in Texas, it is
important to monitor the rate of maternal drug use during pregnancy. NAS data can
be used as an indicator of trends of drug use in pregnant mothers, but because not
all newborns whose mothers use drugs will develop NAS, the true incidence of drug
use during pregnancy can be expected to be higher than the observed rate of NAS
[47].
Data from the Texas Hospital Inpatient Discharge Public Use Data File indicate that
the rate of infants born each year experiencing NAS has more than doubled since
2006, from 1.2 cases per 1,000 hospital births in 2006 to 2.6 cases per 1,000
hospital births in 2015 (Figure 2.45). This was less than the increase observed in
the rest of the United States, in which NAS rates increased 5-fold from 2000 to
2012, and Texas had lower rates of NAS than the national average in 2012 (2.2
cases compared to 5.8 cases per 1,000 hospital births) [46].
Figure 2.44

OVERVIEW OF TEXAS
39
Among all PHRs in Texas, PHR 8 had the highest NAS rate in 2015 (9.0 cases per
1,000 hospital births), and PHR 6/5S had the lowest NAS rate (1.2 cases per 1,000
hospital births) (Figure 2.46). For each year from 2006 to 2015, PHR 8 consistently
had a rate of NAS that was over three times the statewide NAS rate, yet it had one
of the lowest average percent changes from 2006 to 2015. Using data available for
all reported years, the lowest average yearly percent increases were seen in PHR
6/5S (5.2 percent), PHR 11 (7.6 percent), and PHR 8 (10.5 percent). The highest
average yearly increases were observed in PHR 1 (25.5 percent), PHR 4/5N (21.5
percent), and PHR 7 (17.8 percent). NAS rates in Texas overall increased at an
average of 9.6 percent per year from 2006 to 2015.
Based on the most recent four-quarter data records in 2014, the counties with the
highest percentages of reported NAS cases in the state were Bexar County (29.0
percent of the state total), Dallas County (9.7 percent), Harris County (8.6
percent), Tarrant County (6.5 percent), and Travis County (4.8 percent). In
particular, Bexar County in PHR 8 has reported the highest annual number of NAS
cases since 2006, accounting for almost one-third of Texas’ total NAS cases every
year.
Infant Health Practices
Protecting and improving the well-being of infants is an important task. Known
protective infant health practices are addressed in this section, such as
breastfeeding, safe infant sleep, and well-baby checkup [50].
Breastfeeding
Studies have shown that breastfeeding or giving expressed breast milk to infants is
protective against SIDS, and this effect is stronger when breastfeeding is exclusive
[51]. Mothers are encouraged to feed the infant breast milk as much as possible
and for as long as possible. According to the National Immunization Survey, 83.1
percent (CI: 79.9-86.3) of infants born in Texas in 2014 were breastfed at least
Figure 2.45
Figure 2.46

OVERVIEW OF TEXAS
40
once, exceeding the HP2020 target of 81.9 percent for proportion of infants having
ever breastfed [52]. The same survey also found that 24.6 percent (CI: 21.5-27.7)
of Texas-born infants were exclusively breastfed for the first six months after birth,
which was slightly lower than the HP2020 target of 25.5 percent [52].
Ever Breastfeeding
A question about ever breastfeeding is included in the Texas PRAMS survey that
asks women, “Did you ever breastfeed or pump breast milk to feed your new baby,
even for a short period of time?” Based on statewide PRAMS data, trends in the
prevalence of ever breastfeeding ranged from 83.0 percent (CI: 80.7-85.3) in 2009
to 88.3 percent (CI: 85.8-90.7) in 2015.
The prevalence rate of ever breastfeeding among Black women in Texas has been
below the statewide prevalence rate over time, with White/Other women and
Hispanic women generally above the statewide prevalence rate (Figure 2.47). In
2015, White/Other women (91.3 percent, CI: 88.5-94) reported the highest rate of
ever breastfeeding, followed by Hispanic women (86.8 percent, CI: 82.4-91.2) and
Black women (83.8 percent, CI: 79.8-87.8).
Based on pooled 2011-2015 PRAMS data, PHR 1 had the highest rate of ever
breastfeeding (90.1 percent, CI: 84.7-95.5), while PHR 8 (81.9 percent, CI: 77.5-
86.4) and PHR 9/10 (81.6 percent, CI: 75.9-87.4) had the lowest rates of ever
breastfeeding (Figure 2.48). Using pooled 2011-2015 data, the statewide
prevalence rate of ever breastfeeding was 87.4 percent (CI: 86.3-88.5).
For women who reported they breastfed their infant, they were also asked a series
of questions about experiences in the hospital: “This question asks about things
that may have happened at the hospital where your new baby was born. For each
item, check No if it did not happen or Yes if it did happen.” The survey questions
include the following: a) Hospital staff gave me information about breastfeeding; b)
Figure 2.48
Figure 2.47

OVERVIEW OF TEXAS
41
My baby stayed in the same room with me at the hospital; c) Hospital staff helped
me learn how to breastfeed; d) I breastfed in the first hour after my baby was
born; e) I breastfed my baby in the hospital; f) My baby was fed only breast milk at
the hospital; g) Hospital staff told me to breastfeed whenever my baby wanted; h)
The hospital gave me a breast pump to use; i) The hospital gave me a gift pack
with formula; j) The hospital gave me a telephone number to call for help with
breastfeeding; and k) Hospital staff gave my baby a pacifier.
Based on pooled 2011-2015 PRAMS data for Texas, the five most frequently noted
hospital experiences that women had about breastfeeding were:
1) Hospital staff gave me information about breastfeeding;
2) I breastfed my baby in the hospital;
3) My baby stayed in the same room with me at the hospital;
4) The hospital gave me a telephone number to call for help with breastfeeding;
and
5) Hospital staff helped me learn how to breastfeed.
Exclusive Breastfeeding
While a relatively large proportion of Texas mothers report having ever breastfed,
rates of exclusive breastfeeding are much lower. The Texas PRAMS survey does not
collect data on exclusive breastfeeding. However, the 2016 Texas WIC IFPS survey
asked mothers using WIC clinic services when their child first ate or drank anything
other than breastmilk, indicating the amount of time after birth during which the
child was exclusively breastfed. In 2016, about 18.4 percent (CI: 17.2-19.6) of
Texas WIC participants reported exclusively breastfeeding their child for the first
three months after delivery, and 6.0 percent (CI: 5.1-6.8) reported exclusively
breastfeeding their child for the first six months after delivery. This was
substantially lower than the 2014 National Immunization Survey rate (24.6
percent) among all mothers in Texas who breastfed exclusively for the first six
months.
The highest rates of exclusive breastfeeding for the first three months among WIC
participants were reported by PHR 1 (30.7 percent, CI: 23.6-37.8) and PHR 9/10
(23.2 percent, CI: 18.3-28.2), while the lowest rates were reported by PHR 6/5S
(15.4 percent, CI: 13.0-17.9) and PHR 11 (16.3 percent, CI: 13.5-19.0). Due to
low responses in PHR 1, PHR 4/5N, and PHR 8 for the WIC IFPS survey, the rates of
exclusive breastfeeding for the first six months were not reported in those regions.
The rates of WIC participants who breastfed exclusively for the first six months
among the remaining five regions ranged from 4.4 percent (CI: 2.7-6.1) in PHR 11
to 10.4 percent (CI: 6.5-14.3) in PHR 9/10.

OVERVIEW OF TEXAS
42
Safe Infant Sleep
For decades, public health research has shown that infants placed on their backs to
sleep are less likely to die from SIDS [53]. The PRAMS survey asks women, “In
which one position do you most often lay your baby down to sleep now?” Based on
Texas PRAMS data, trends in the statewide prevalence of placing infants to sleep on
their backs ranged from 60.7 percent (CI: 57.6-63.8) in 2009 to 71.2 percent (CI:
68.1-74.4) in 2015. The HP2020 objective is to increase the proportion of infants
placed on their backs to sleep to 75.8 percent [52].
The prevalence rate of infant back sleeping among Hispanic women in Texas has
been similar to the statewide prevalence rate over time, with White/Other women
demonstrating the highest prevalence rate. The prevalence rate among Black
women has consistently fallen below the statewide prevalence rate, however, there
has been a measurable increase statewide and for each race/ethnic group since
2009 (Figure 2.49). In 2015, White/Other women had the highest rate of placing
their infants to sleep on their backs (77.8 percent, CI: 73.9-81.8), followed by
Hispanic women (70.6 percent, CI: 65.1-76.0) and Black women (50.2 percent, CI:
44.9-55.5). Only White/Other women in Texas are currently meeting the HP2020
target of 75.8 percent of infant back sleeping.
Based on pooled 2011-2015 PRAMS data, women in PHR 9/10 reported the highest
rate of placing their infants to sleep on their backs (76.9 percent, CI: 70.8-82.9),
and women in PHR 11 reported the lowest rate of placing their infants to sleep on
their backs (65.1 percent, CI: CI: 59.6-70.6) (Figure 2.50). Using pooled 2011-
2015 data, the statewide prevalence rate was 70.8 percent (CI: 69.3-72.2).
Well-baby Checkup
Well-baby visits are important for screening and assessing the health of an infant.
The PRAMS survey asks women, “Has your new baby had a well-baby checkup? A
well-baby checkup is a regular health visit for your baby usually at 1, 2, 4, and 6
Figure 2.50
Figure 2.49

OVERVIEW OF TEXAS
43
months of age.” Based on Texas PRAMS data, trends in the statewide prevalence of
a well-baby checkup remained stable from 98.2 percent (CI: 97.4-99.1) in 2009 to
98.4 percent (CI: 97.5-99.3) in 2015.
The prevalence rate of a well-baby checkup among Hispanic and Black women in
Texas has been generally below the statewide prevalence rate over time, with
White/Other women demonstrating a higher prevalence rate (Figure 2.51). In 2015,
White/Other women reported a higher well-baby checkup rate (99.0 percent, CI:
98.0-100.0) than Hispanic women (98.0 percent, CI: 96.5-99.6) and Black women
(97.8 percent, CI: 96.3-99.3).
Well-baby checkups are consistently high across the state. Based on pooled 2011-
2015 PRAMS data, the percentage of women reporting a well-baby checkup ranged
from 96.9 percent (CI: 95.8-97.9) in PHR 2/3 to 98.8 percent (CI: 97.8-99.8) in
PHR 1 (Figure 2.52). Using pooled 2011-2015 data, the statewide prevalence rate
of a well-baby checkup was 97.6 percent (CI: 97.1-98.1).
Perinatal Periods of Risk
In order to provide communities and stakeholders more in-depth information to
help reduce infant mortality, a comprehensive Perinatal Periods of Risk (PPOR)
approach for the state as a whole and for each region was undertaken. PPOR gives
analytic steps to investigate and address the specific causes of high fetal and infant
mortality rates and disparities among study populations (such as Whites, Blacks,
Hispanics, and Teens). Both Phase I and Phase II analyses were conducted. PPOR
analysis results are provided in the report, along with practicable recommendations.
PPOR examines the risk of feto-infant mortality during different perinatal periods.
Based on birth weight and age at death, fetal and infant deaths are partitioned into
four corresponding risk periods: maternal health/prematurity, maternal care,
newborn care, and infant health (Figure 2.53).
Figure 2.51
Figure 2.52

OVERVIEW OF TEXAS
44
Each of these periods has different risk factors and causes of death, and
subsequently, different opportunities for prevention. Therefore, the four risk periods
represent distinct points of intervention in the health care continuum (Figure 2.54).
In this report, 2010-2014 fetal death and linked birth/infant death files were used
for the PPOR analysis. The five most recent years of vital records data were
combined to reach sufficient numbers of deaths for all regions.
Phase I Analysis
Texas and specific study populations (i.e., Black, White, Hispanic, or teens) were
compared to a state-level reference group generally known to have better feto-
infant mortality outcomes (i.e., non-Hispanic White women who are at least 20
years of age and have 13+ years of education). In the following analysis, these
study populations are not mutually exclusive. The feto-infant mortality rate (F-IMR)
is calculated as the number of fetal and infant deaths per 1,000 live births and fetal
deaths. The excess F-IMR is the difference in F-IMR between the study population
and the reference group.
The 2010-2014 F-IMRs in Texas were
6.5 per 1,000 for White mothers, 11.8
per 1,000 for Black mothers, 6.7 per
1,000 for Hispanic mothers, and 8.3 per
1,000 for teen mothers. In 2010-2014,
Black mothers experienced a total of 6.6
excess fetal and infant deaths per 1,000
live births and fetal deaths (Figure
2.55). Total excess F-IMRs for White
Figure 2.53
Figure 2.54
Figure 2.55

OVERVIEW OF TEXAS
45
mothers, Hispanic mothers, and teen mothers were 1.3 per 1,000, 1.5 per 1,000,
and 3.1 per 1,000, respectively.
Black women had the highest excess F-IMR for all four risk periods, with 56 percent
of all Black fetal and infant deaths being potentially preventable deaths (i.e. excess
fetal and infant deaths). Moreover, 47 percent of the overall excess Black fetal and
infant deaths occurred in the Maternal Health/Prematurity risk period. For teen
mothers, 85 percent of excess feto-infant deaths occurred in the Maternal
Health/Prematurity and Infant Health risk periods.
Phase II Analysis
For fetal and infant deaths occurring in the Maternal Health/Prematurity risk period,
a Kitagawa analysis was conducted for each study population, to examine whether
excess feto-infant mortality was primarily due to a greater number of very low birth
weight (VLBW) births in the study population compared to the reference population
(a difference in birth weight distribution), or to a higher mortality rate among VLBW
infants than seen in the reference population (a difference in birth weight specific
mortality). The percentage of excess deaths attributable to a difference in birth
weight distribution compared with the percentage attributable to a difference in
birth weight specific mortality rates in Texas are shown in Figure 2.56 for each
study population.
For all subpopulations examined, the
majority of excess Maternal
Health/Prematurity risk period deaths
were attributable to a greater number of
VLBW births in these groups when
compared to the reference population.
Notably, Black infants (0 percent) had
lower mortality rates among VLBW births
than the reference population; for this
subgroup, all excess deaths (100
percent) were potentially attributable to
a greater number of VLBW births (Figure
2.56). For all of these study populations, and especially for infants born to Black
mothers, interventions aimed at reducing the number of VLBW births are likely to
be most effective at closing the gap in feto-infant mortality. For White mothers,
Hispanic mothers, and teen mothers, some proportion of excess feto-infant death
was also attributable to a higher mortality rate among VLBW births than the
reference population.
Figure 2.56

OVERVIEW OF TEXAS
46
To examine differences in birth weight distribution during the Maternal
Health/Prematurity risk period, a multivariable logistic regression analysis was
conducted to identify factors associated with risk of delivering a VLBW baby.
Factors examined included maternal demographic factors (race/ethnicity, age, and
education), multiple gestations, smoking during pregnancy, high parity for age,
previous preterm birth, maternal weight gain during pregnancy, adequacy of
prenatal care, trimester prenatal care began, and payment source for the delivery.
Factors that contributed the most to risk of a VLBW birth in Texas included weight
gain less than 15 pounds and inadequate prenatal care. Approximately 19 percent
of all VLBW births were attributable to weight gain less than 15 pounds. Five
percent of all VLBW births could be attributed to inadequate prenatal care. Black
mothers and teen mothers in the state were more likely to gain less than 15 pounds
or receive inadequate prenatal care compared to the reference population.
To identify factors related to birth weight specific mortality in the Maternal
Health/Prematurity risk period, an analysis was also performed to assess risk of
infant death among VLBW births. Factors examined in this analysis included
maternal demographics, congenital anomalies, inadequate prenatal care, maternal
diabetes, maternal hypertension, infant transfer, maternal transfer, respiratory
care, ruptured membranes, and prenatal steroids.
Inadequate prenatal care and congenital anomalies contributed the most to infant
mortality among VLBW births in Texas. Specifically, 3 percent of infant deaths to
this group were attributable to inadequate prenatal care, and an additional 3
percent were attributable to congenital anomalies. Among VLBW births, infants
whose mothers received prenatal steroids had a 22 percent reduced risk of infant
death. Compared to the reference population, White mothers and teen mothers
were more likely to deliver an infant with congenital anomalies or receive
inadequate prenatal care. Hispanic mothers and Teen mothers were also less likely
to receive prenatal steroids compared to the reference population.
Among all infant deaths in the Infant
Health risk period, perinatal conditions
were the primary cause of death,
accounting for 51 percent of excess
infant deaths in Texas (Figure 2.57). Of
the subgroups examined, Black infants
and infants born to teen mothers had
the greatest excess infant mortality in
this risk period, with perinatal conditions
accounting for a large proportion of
Figure 2.57

OVERVIEW OF TEXAS
47
excess infant deaths. Birth defects contributed to 18 percent of excess infant deaths
to teen mothers and to 21 percent of excess deaths among White infants. SIDS
accounted for 28 percent of excess deaths among White infants and for 10 percent
of excess deaths among Black infants.
To further examine excess mortality in the Infant Health risk period, an analysis
was conducted to determine risk factors associated with infant death among infants
28 days and older. Maternal demographic factors, smoking during pregnancy,
adequacy of prenatal care, breastfeeding status at hospital discharge, and trimester
prenatal care began were all examined. No first trimester prenatal care,
breastfeeding at hospital discharge, and smoking had the greatest impact on overall
risk of infant death during this time period in Texas. Among all infants 28 days and
older, infants who were breastfed at hospital discharge had a 9 percent reduced
risk of infant death. About 2 percent of infant deaths were attributable to not
receiving prenatal care in the first trimester, and 1 percent of infant deaths were
attributable to maternal smoking during pregnancy.
Recommendations
Phase I analyses identified the populations and periods of risk with the largest
excess feto-infant mortality compared to the reference population. In Texas, the
period of risk and study population with the highest excess feto-infant mortality
rate, and thus the greatest opportunity for potential impact, was the Maternal
Health/Prematurity risk period among the Black population. Interventions should
also be targeted to Black populations for Maternal Care and Infant Health-related
deaths. Among teen mothers, interventions should focus on Maternal
Health/Prematurity and Infant Health-related deaths. Maternal Health/Prematurity-
related deaths should also be targeted among the Hispanic population, while Infant
Health-related deaths should be the focus among the White population.
Phase II analyses identified modifiable risk factors that contributed the most to
excess feto-infant mortality. To reduce excess feto-infant mortality in the Maternal
Health/Prematurity period of risk, interventions in Texas should focus on improving
access to and use of prenatal care among Black, Hispanic, and teen mothers;
reducing the number of women gaining less than 15 pounds during pregnancy;
reducing rates of teen pregnancy; and reducing rates of premature rupture of the
membranes. Interventions likely to be most effective in reducing Infant Health-
related excess feto-infant mortality include reducing prematurity among all race
groups; reducing birth defects among White infants and infants born to teen
mothers; increasing rates of breastfeeding; reducing SIDS among White infants and
Black infants; improving access to and use of prenatal care; and reducing parental
smoking.

OVERVIEW OF TEXAS
48
For your convenience, a companion PPOR fact sheet for Texas, 2010-2014 can be
found at this website: https://www.dshs.texas.gov/healthytexasbabies/data.aspx
Summary Table: Selected Health Indicators in Texas
Lastly, a summary table for selected health indicators from 2006 to 2015 is
presented below, to help easily monitor/depict statewide trends.
Indicators
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 10-Year Trend
Birth Rate
a
17.0 17.0 16.7 16.2 15.3 14.7 14.7 14.6 14.8 14.7
Maternal Age (in Years) 26.5 26.5 26.6 26.7 26.9 27.1 27.2 27.4 27.6 27.7
Teen Birth Rate
b
60.2 60.6 59.7 57.4 52.2 45.9 42.3 39.7 36.3 33.0
Infant Mortality Rate
c
6.2 6.2 6.1 6.0 6.1 5.7 5.8 5.8 5.8 5.6
Preterm Birth
d
11.3 11.3 11.2 11.1 10.9 10.7 10.5 10.4 10.3 10.2
Low Birth Weight
d
8.5 8.4 8.4 8.5 8.4 8.5 8.3 8.3 8.2 8.3
Prenatal Care in the 1st
Trimester of Pregnancy
d
64.0 61.8 61.5 61.4 63.9 66.3 66.2 66.1 65.2 65.9
Pre-Pregnancy Obesity
d
20.1 20.7 21.4 21.9 22.5 22.9 23.5 24.0 24.4 25.2
Maternal Hypertension
d
5.7 5.4 5.5 5.7 6.3 6.3 6.4 6.4 6.9 7.4
Maternal Diabetes
d
4.3 4.6 4.6 4.4 4.5 4.9 5.0 4.9 5.5 5.5
Smoking During Pregnancy
d
6.0 5.6 5.4 5.1 4.9 4.6 4.4 4.3 3.9 3.6
Severe Maternal Morbidity
(SMM)
e, g
174.1 175.8 178.2 196.3 200.0 207.7 207.0 203.3 205.6 172.4
Neonatal Abstinence
Syndrome (NAS)
f, g
1.2 1.3 1.4 1.6 1.7 2.1 2.2 2.4 2.8 2.6
a
Live births per 1,000 population
b
Live births per 1,000 teen females (aged 15-19)
c
Deaths per 1,000 live births
d
Percent of live births
e
Cases per 10,000 delivery hospitalizations
f
Cases per 1,000 hospital births
g
Year 2015 data only includes the first three quarters.
Sources: 2006-2015 Texas Birth and Death files, Center for Health Statistics, DSHS; 2006-2015 Texas Population Estimates,
Texas Demographic Center; 2006-2015 Texas Hospital Inpatient Discharge Public Use Data File, Texas Department
of State Health Services.
Texas

49
Public Health Region
6/5S: Key Findings
Key Findings:
Overall, the region’s infant mortality rate
(5.6 deaths per 1,000 live births in
2015) was similar to the state. Houston-
The Woodlands and Galveston
communities met the HP2020 target of
6.0 or fewer infant deaths per 1,000.
The Beaumont-Port Arthur community
had the highest percentage of low birth
weight infants among all large
communities in Texas.
A low rate of smoking during pregnancy
was observed (2.5 percent in 2015),
compared to the state’s 3.6 percent.
Late entry into prenatal care was a
serious concern in several counties,
including Harris County and Galveston
County.
Three-tenths of childbearing-aged
women had no health insurance. Many
families struggled with the high cost of
health care and had difficulty navigating
the system to get the best care.
PHR 6/5S had a higher rate of severe
maternal morbidity than all other Texas
regions.
Interventions to reduce fetal/infant
mortality should focus on healthy weight
gain during pregnancy; reducing
prematurity and birth defects; reducing
SIDS among Black and White infants;
and increasing breastfeeding rates and
access to prenatal care.
PUBLIC HEALTH
REGION 6/5S
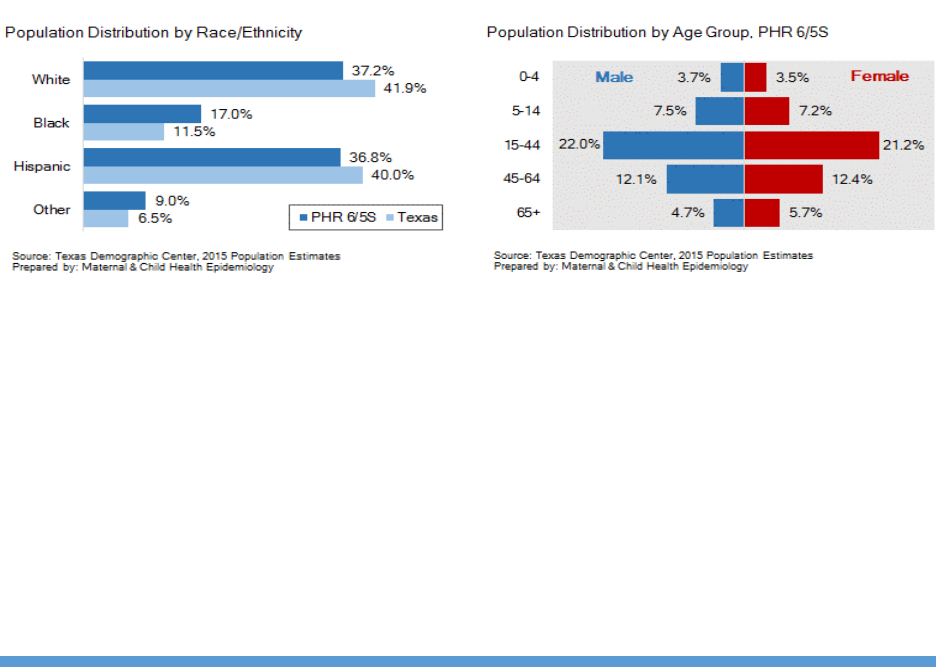
PUBLIC HELATH REGION 6/5S
50
Public Health Region 6/5S
Public Health Region 6/5S (PHR 6/5S) consists of 16 counties of Southeast Texas.
This region includes the metropolitan area of Houston–The Woodlands–Sugar Land,
the second largest metropolitan area in Texas (after Dallas–Fort Worth-Arlington)
and the fifth largest one in the United States. PHR 6/5S had a total population of
7,213,320 in 2015, making it the second most populous region in Texas. The
region’s population growth rate was 11.4 percent from 2010 to 2015, which was
faster than the state’s growth rate (9.2 percent) and was the second highest
growth rate (after PHR 7) among all PHRs in Texas. The population of the Houston-
The Woodlands-Sugar Land metro area is centered in the city of Houston, the
largest economic and cultural center of the American South, with a population of
about 2.3 million.
Blacks accounted for 17.0 percent of the population in PHR 6/5S in 2015, and
persons of ‘Other’ race/ethnicity accounted for 9.0 percent (Figure 3.1). Both
proportions were higher than the state’s average, and were higher than among all
other regions in Texas. PHR 6/5S had the same proportion of young people under
15 years of age as the state (21.9 percent) (Figure 3.2). The proportion of women
of reproductive age (ages 15-44; 21.2 percent) in PHR 6/5S was similar to the
state’s proportion (20.9 percent).
Based on 2011-2015 Census ACS data, PHR 6/5S had a higher percentage of
foreign-born residents (21.5 percent) compared to the state (16.6 percent).
Especially, within the counties containing and nearby the city of Houston, more
than a quarter of the residents were foreign-born. Spanish is the most spoken non-
English language in Texas homes. About 27.8 percent of Texans in PHR 6/5S spoke
Spanish at home, compared with 29.5 percent of Texans in the state as a whole.
Socioeconomic characteristics such as income level and poverty are added
challenges for meeting the health needs of mothers, children, and families within a
community. According to 2011-2015 Census ACS data, seven counties in PHR 6/5S
had a median household income that was higher than the state’s median household
Figure 3.1
Figure 3.2

PUBLIC HELATH REGION 6/5S
51
income of $53,207. The county-level median household income in this region
ranged from $37,666 to $89,152. PHR 6/5S had a lower proportion of adult females
living below 200 percent FPL (32.3 percent) compared to the state (34.9 percent).
Similarly, PHR 6/5S had a lower rate of children younger than 5 years old living
below 100 percent FPL (25.5 percent) compared to the state (27.4 percent). Seven
counties in this region had child poverty rates higher than the state’s rate.
Birth Demographics
A total of 110,148 births were registered in PHR 6/5S in 2015, which was an 8.0
percent increase from 2006. This percent increase in the total number of births was
the largest among all PHRs in Texas. In comparison, the total number of births in
Texas has increased by 1.0 percent since 2006. The birth rate for PHR 6/5S was
15.3 births per 1,000 people in 2015, which has declined from 17.0 births per
1,000 in 2006. The region’s birth rate over the past decade has declined slower
than the birth rate for the state as a whole (The Texas birth rate decreased from
17.0 births per 1,000 in 2006 to 14.7 births per 1,000 in 2015).
Male infants accounted for 50.9 percent of all births in 2015 in PHR 6/5S, and
female infants accounted for 49.1 percent of births. Births to Hispanic mothers
made up the largest percentage of all births in this region (42.5 percent), followed
by births to White mothers (30.6 percent), Black mothers (17.6 percent) and
mothers classified as ‘Other’ race/ethnicity (9.4 percent). Among all PHRs in Texas,
PHR 6/5S had the largest proportion of births to Black mothers and mothers of
‘Other’ race/ethnicity, respectively. While the proportions of births to White, Black,
and Hispanic mothers have decreased over the past decade in PHR 6/5S, the
proportion of births to mothers of ‘Other’ race/ethnicity has increased.
The average age for women with a live birth in 2015 in PHR 6/5S was 28.3 years of
age, older than the state’s average maternal age at birth (27.7 years of age).
Among all PHRs in Texas, PHR 6/5S had the second oldest average maternal age.
As in the state as a whole, this region has seen an increase from an average
maternal age of 26.9 years a decade ago. Counties with major urban centers, such
as Houston and Galveston areas, had an older average maternal age than other
counties in the region.
Teen Births
The increase in average maternal age observed over time is likely due in part to a
prominent decrease in the teen birth rate. In 2015, a total of 7,639 babies (about
6.9 percent of total births) were born to teenagers aged 15-19 in PHR 6/5S, for a
teen birth rate of 30.0 births per 1,000 teen females. The region’s teen birth rate in
2015 was lower than the corresponding teen birth rate in Texas as a whole (33.0

PUBLIC HELATH REGION 6/5S
52
births per 1,000). PHR 6/5S, like the rest of the state, has experienced a
substantial decrease in teen birth rates since 2006 (53.6 births per 1,000). The
teen birth rate in PHR 6/5S has declined by 44.0 percent over the past decade,
compared to an overall decrease of 45.2 percent in the state’s teen birth rate.
Teen birth rates vary widely across the
region. Four counties had high teen birth
rates in 2015 (46.3 births per 1,000 or
greater), when compared to the rest of
the region (Figure 3.3). Teen birth rates
are shown for all PHR 6/5S counties with
100 or more documented births in 2015.
Among these counties, teen birth rates
ranged from 9.6 births per 1,000 teen
females to 49.7 births per 1,000 teen
females.
Infant Mortality & Morbidity
In 2015, a total of 615 infants in PHR
6/5S died before reaching their first
birthday; this comprised about 27.1 percent of the total infant deaths in Texas. PHR
6/5S had an IMR of 5.6 deaths per 1,000 live births in 2015, which was the same
as the state IMR. The region’s IMR has decreased by 8.0 percent since 2006,
compared to a 9.3 percent decrease for Texas as a whole during this timeframe.
Two large communities (Houston-The Woodlands and Galveston) in the region met
the HP2020 target of 6.0 or fewer infant deaths per 1,000 live births in 2015.
Although the Beaumont-Port Arthur community did not meet the HP2020 target,
the community had a prominent decrease in IMR, from 9.9 deaths per 1,000 in
2014 to 6.9 deaths per 1,000 in 2015.
Based on 2011-2015 combined death files, congenital malformation was the most
common cause of death among infants in PHR 6/5S; this was similar to all other
PHRs. Other causes of infant death listed as top five leading causes in this region
included short gestation and low birth weight, maternal complications of pregnancy,
SIDS, and infections in the perinatal period. Compared to previous 2006-2010 data,
the region saw a decrease in infant deaths caused by SIDS and infections in the
perinatal period, and an increase in infant deaths caused by congenital
malformation and maternal complications of pregnancy.
Figure 3.3

PUBLIC HELATH REGION 6/5S
53
Preterm Birth
Preterm births are those that occur prior to 37 weeks of gestation. Using the
obstetric estimate of gestational age, about 10.7 percent of live births in PHR 6/5S
were delivered preterm in 2015, compared to the state’s preterm birth rate of 10.2
percent. The region’s preterm birth rate has decreased from 11.3 percent in 2006.
Preterm birth rates vary by race/ethnicity in PHR 6/5S. Black infants (14.0 percent)
had a higher rate of preterm birth in 2015 than did infants of any other
racial/ethnic group (9.8 to 10.1 percent). Over the past decade, preterm birth rates
have declined among Black and White infants, while rates have remained stable
among Hispanic infants and infants of
‘Other’ race/ethnicity in the region.
Geographic differences in preterm birth
rates exist in PHR 6/5S. A few counties
in the southern area of the region had
high rates of preterm birth (12.3
percent or greater), when compared to
the rest of the region (Figure 3.4).
Preterm birth rates are shown for all
PHR 6/5S counties with 100 or more
documented births in 2015. Among
these counties, preterm birth rates
ranged from 7.9 percent to 11.8
percent.
Low Birth Weight
Low birth weight (less than 2,500 grams) is another important factor related to
infant mortality. In 2015, about 8.5 percent of all newborns in PHR 6/5S had low
birth weight, similar to the state’s rate of 8.3 percent. The region’s low birth weight
rate has remained stable since 2006.
In 2015, Black infants (12.9 percent) had the highest rate of low birth weight,
followed by infants classified as ‘Other’ race/ethnicity (9.8 percent) and White and
Hispanic infants (7.2 percent). From 2006 to 2015, decreases in low birth weight
rates were observed among Black and White infants, while increases in low birth
weight rates were seen among infants of ‘Other’ race/ethnicity in the region.
Figure 3.4
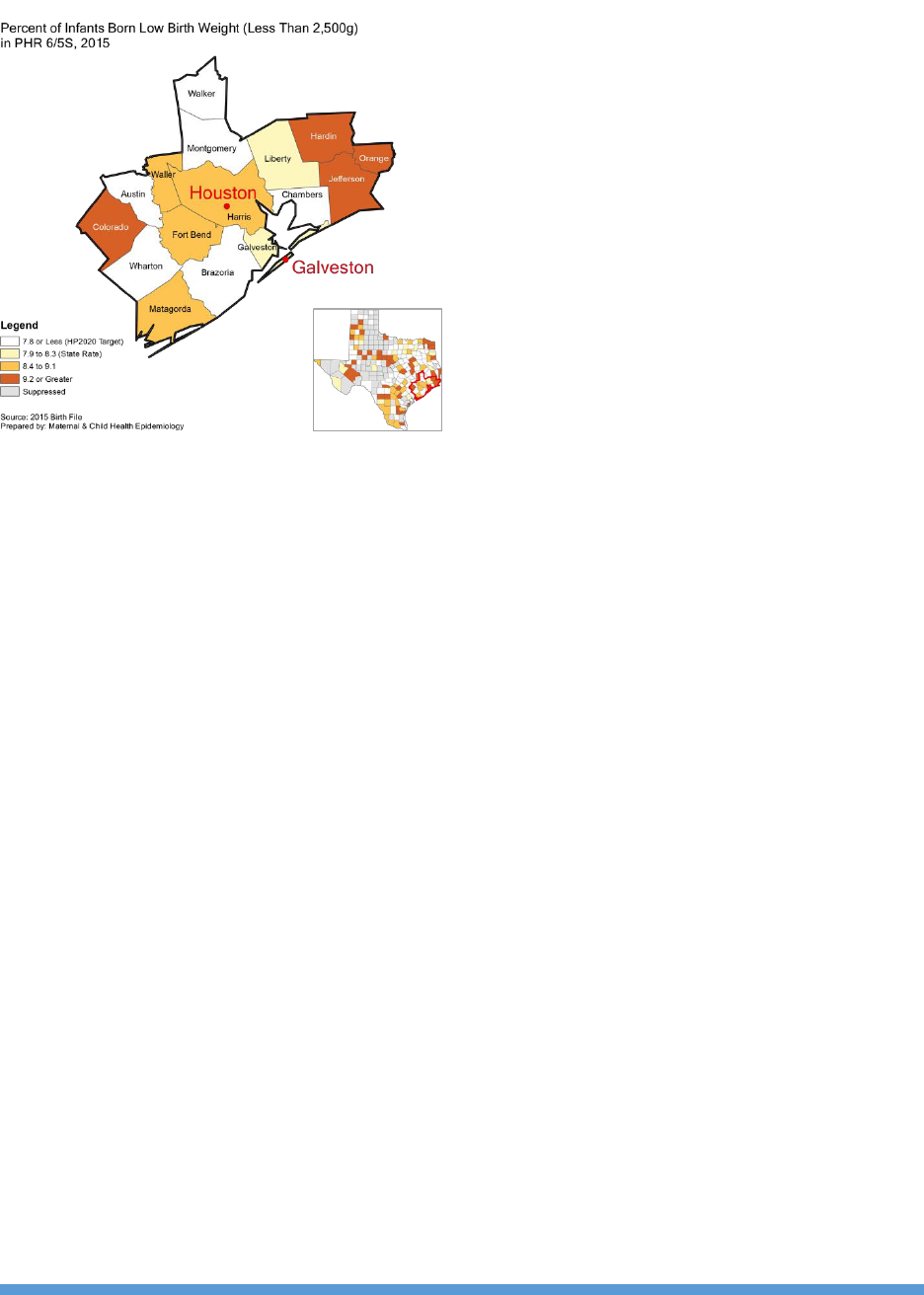
PUBLIC HELATH REGION 6/5S
54
Low birth weight rates vary by county in
PHR 6/5S. Six counties in the region
met the HP2020 target of 7.8 percent or
fewer of all live births weighing less than
2,500 grams, while four counties
(mainly in the Beaumont-Port Arthur
community) had high percentages (9.2
percent or greater) of low birth weight
infants (Figure 3.5). Low birth weight
rates are shown for all PHR 6/5S
counties with 100 or more documented
births in 2015. Among these counties,
low birth weight rates ranged from 5.5
percent to 11.7 percent.
17P Prescription
Women who are at risk of preterm birth may benefit from taking 17P (17-alpha-
hydroxyprogesterone). Based on pooled 2011-2015 PRAMS data, about 5.7 percent
(CI: 4.4-7.1) of women in PHR 6/5S said 17P was prescribed by their doctors or
health care workers during their most recent pregnancy to help keep their new
babies from being born too early. The prevalence rate for this region was about the
same as the statewide prevalence rate (5.5 percent, CI: 4.8-6.2).
Based on pooled 2011-2015 PRAMS data for PHR 6/5S, Black women had a higher
rate of 17P use than White/Other and Hispanic women. Black women in PHR 6/5S
had about the same prevalence rate of 17P use (8.4 percent, CI: 6.3-10.5) as Black
women in the state as a whole (8.7 percent, CI: 7.4-10.1). However, the
prevalence rate of 17P use among White/Other women in the region (5.7 percent,
CI: 3.7-7.8) was higher than the rate of White/Other women in Texas (4.6 percent,
CI: 3.7-5.5). Hispanic women in the region also had about the same prevalence
rate of 17P use (4.7 percent, CI: 2.3-7.0) as Hispanic women in Texas (5.5 percent,
CI: 4.4-6.7).
Health Care Coverage and Access
Health insurance and access to health care are crucial to the health of Texans.
Based on 2011-2015 Census ACS data, more than 1.4 million individuals in PHR
6/5S had no health insurance coverage. The region’s uninsured rate among the
total population was 21.2 percent, compared to the state’s rate of 20.6 percent.
About 30.7 percent of women of reproductive age (ages 18-44) in PHR 6/5S did not
have health insurance; this was similar to the state’s uninsured rate for this age
Figure 3.5

PUBLIC HELATH REGION 6/5S
55
group (30.4 percent). Only two counties in the region had high proportions (36.6
percent or greater) of women aged 18-44 years without insurance. Also, the
proportion of uninsured children younger than 6 years was 8.9 percent in PHR 6/5S,
compared to 8.5 percent of the state as a whole. Five counties in the northern area
of the region had high proportions (10.3 percent or greater) of uninsured children
under 6 years of age.
Health Professionals
According to the most recent health professions data, there were 5,675 primary
care physicians (PCPs) in PHR 6/5S in 2016, with a density of 77.2 PCPs per
100,000 residents [28]. The PCP density in the region was higher than that in the
state as a whole (72.9 PCPs per 100,000). Urban-rural disparities in access to PCPs
exist in the region. Urban counties in PHR 6/5S had a PCP density of 77.7 PCPs per
100,000 residents, compared with 57.5 PCPs per 100,000 residents in rural
counties.
There were 765 obstetrics and/or gynecology specialists (OB/GYNs) in PHR 6/5S,
with a density of 20.8 OB/GYNs per 100,000 female residents. The OB/GYN density
in the region was higher than that in the state as whole (18.3 OB/GYNs per
100,000 females), and in fact, was the highest among all Texas regions. Four
counties in PHR 6/5S had no OB/GYN in 2016. Overall, urban counties in the region
(20.9 OB/GYNs per 100,000 females) had better access to these specialists than
rural counties (17.3 OB/GYNs per 100,000 females).
Prenatal Care in the First Trimester
Receiving prenatal care in the first trimester is recommended for all pregnant
women to enhance a healthy pregnancy. In 2015, only 63.4 percent of women
delivering a live birth in PHR 6/5S entered prenatal care within the first trimester.
This rate was lower than the state’s rate of 65.9 percent, and did not meet the
HP2020 target of 77.9 percent of pregnant women receiving prenatal care
beginning in the first trimester of pregnancy. The proportion of mothers who began
receiving prenatal care in the first trimester in the region has not changed much
since 2006.
In 2015, about 73.1 percent of White mothers in PHR 6/5S received prenatal care
beginning in the first trimester of pregnancy, compared with 55.1 percent of Black
mothers, 59.3 percent of Hispanic mothers, and 65.2 percent of mothers classified
as ‘Other’ race/ethnicity. Over the past decade, the proportion of women receiving
prenatal care in the first trimester has increased among Hispanic mothers, but not
among the other racial/ethnic groups.

PUBLIC HELATH REGION 6/5S
56
Late entry into prenatal care is a
problem in PHR 6/5S. Five counties,
including Harris County and Galveston
County, had high proportions (37.6
percent or greater) of mothers not
receiving prenatal care in the first
trimester, when compared to the rest of
the region (Figure 3.6). Among all PHR
6/5S counties with 100 or more
documented live births in 2015, the
percentage of live births where the
mother had late entry into prenatal care
ranged from 27.3 percent to 42.3
percent.
Prenatal Care as Early as Wanted and Barriers
Early and adequate prenatal care is extremely important for the health of both the
mother and baby. Based on pooled 2011-2015 PRAMS data, about 79.8 percent
(CI: 77.3-82.3) of women in PHR 6/5S indicated they received prenatal care as
early as they wanted. The prevalence rate for this region was about the same as
the statewide prevalence rate (79.1 percent, CI: 77.8-80.5).
Based on pooled 2011-2015 PRAMS data for PHR 6/5S, White/Other women
reported a higher rate of receiving prenatal care as early as they wanted than
Hispanic and Black women. White/Other women in PHR 6/5S reported about the
same prevalence of receiving prenatal care as early as they wanted (84.4 percent,
CI: 81.1-87.6) as White/Other women in Texas (83.9 percent, CI: 82.3-85.6).
However, Hispanic women in the region reported a higher prevalence of receiving
prenatal care as early as they wanted (77.5 percent, CI: 72.8-82.2) compared to
Hispanic women in the state as a whole (76.1 percent, CI: 73.7-78.4). Black
women in the region also reported about the same prevalence of receiving prenatal
care as early as they wanted (75.2 percent, CI: 71.8-78.6) as Black women in
Texas (75.0 percent, CI: 72.9-77.1).
Understanding barriers to prenatal care for women who did not get prenatal care as
early as they wanted is also important. Based on pooled 2011-2015 PRAMS data,
about 20.2 percent (CI: 17.7-22.7) of women in PHR 6/5S did not receive prenatal
care as early as they wanted, and the five most frequently noted barriers were:
1) I didn’t have enough money or insurance to pay for my visits;
2) I didn’t have my Medicaid or Texas Health Steps card;
3) I didn’t know that I was pregnant;
Figure 3.6

PUBLIC HELATH REGION 6/5S
57
4) I couldn’t get an appointment when I wanted one; and
5) I had too many other things going on.
Barriers to Maternal & Child Health Services
Many Texans face substantial barriers to accessing health care. Stakeholder
feedback and identification of the needs and challenges, however, can lead to policy
improvements and strategic planning initiatives for improving access.
A common theme that emerged from the 2014 Title V stakeholder meetings and
focus groups with mothers in Houston was the high cost of health care and the
difficulty to navigate the system to get the best care [22]. Many women seeking
prenatal care during their first trimester often faced delays because of the long
Medicaid approval process or the time it took to get other insurance coverage in
place. Stakeholders also identified a lack of access to mental health services for
women and children as a priority problem. Many behavioral health providers in PHR
6/5S did not participate in Medicaid or Children’s Health Insurance Program due to
reimbursement issues; and, the racial and cultural diversity in the area further
complicated the access to services. Another barrier was the limited access to dental
care for many children and women at multiple stages in their life and for uninsured
individuals without the means to pay.
Most participants in the meetings agreed that coordination and continuity of care
were regional priorities, as providers rarely coordinated among themselves and
referrals often were made in an untimely manner or not at all. Many providers and
families were unaware of available services and programs. It was a priority need to
educate parents about child safety, parenting, and how to help their teenagers
develop life skills as well as to inform pregnant women the importance of access to
prenatal care. In addition, Houston women identified obesity as a top health
concern. Some mothers addressed time constraints and the obligation to care for
small children made physical activity challenging, some described losing weight
they gained during their pregnancies was challenging, and others said the high cost
of eating healthily made it challenging for them to follow a healthy diet.
Maternal Health
Maternal well-being is important to the health of children and families. Selected
health indicators for women before and during pregnancy are discussed, including
obesity, hypertension & diabetes, smoking, drinking, physical abuse, postpartum
depression, and postpartum checkup.

PUBLIC HELATH REGION 6/5S
58
Pre-pregnancy Obesity
Obesity among women of reproductive age is of major concern, because of its
association with multiple adverse maternal and infant health outcomes. In 2015,
about 24.7 percent of women in PHR 6/5S were obese before becoming pregnant,
slightly lower than the state’s rate of 25.2 percent. The region’s pre-pregnancy
obesity rate has increased from 19.4 percent in 2006.
Black mothers in PHR 6/5S had the highest rate of pre-pregnancy obesity in 2015
(31.7 percent), followed by Hispanic mothers (27.4 percent), White mothers (21.3
percent), and mothers of ‘Other’ race/ethnicity (10.4 percent). The region’s pre-
pregnancy obesity rate was lower than the corresponding state rate among all
racial/ethnic groups, except for Black mothers. However, since 2006, the pre-
pregnancy obesity rate in PHR 6/5S has risen most sharply among mothers of
‘Other’ race/ethnicity (an 82.5 percent increase). In comparison, the pre-pregnancy
obesity rate has increased by two-fifths among Hispanic mothers and by one-fifth
among Black and White mothers over the past decade.
Pre-pregnancy obesity rates vary by
county in PHR 6/5S. Three counties in
the region had pre-pregnancy obesity
rates lower than the state’s rate (Figure
3.7). Among all PHR 6/5S counties with
100 or more documented births in 2015,
pre-pregnancy obesity rates ranged from
20.0 percent to 34.7 percent. Overall,
mothers in rural counties in the region
(32.6 percent) experienced a much
higher rate of pre-pregnancy obesity
than their urban counterparts (24.6
percent).
Maternal Hypertension & Diabetes
Hypertension (high blood pressure) and diabetes are two common maternal health
problems a woman may experience during pregnancy. The 2015 birth certificate
data showed that in PHR 6/5S, about 7.7 percent of all live births were to mothers
with some form of hypertension, and 6.1 percent of all live births were to mothers
who had diabetes (these mothers either had hypertension or diabetes pre-
pregnancy, or developed the condition over the course of the pregnancy). Both
rates in the region were slightly higher than the state’s rate of maternal
hypertension (7.4 percent) and maternal diabetes (5.5 percent), respectively. Over
the past decade, the maternal hypertension rate has increased by more than one-
third in the region, while the maternal diabetes rate has remained stable.
Figure 3.7

PUBLIC HELATH REGION 6/5S
59
Rates of maternal hypertension and diabetes vary by race/ethnicity. In 2015, Black
mothers in PHR 6/5S had the highest rate of maternal hypertension (10.9 percent),
followed by White mothers (8.2 percent), Hispanics mothers (6.6 percent), and
mothers of ‘Other’ race/ethnicity (4.7 percent). From 2006 to 2015, increases in
maternal hypertension rates were observed among all racial/ethnic groups. In
contrast, mothers of ‘Other’ race/ethnicity in PHR 6/5S had the highest rate of
maternal diabetes (8.3 percent), followed by Hispanic mothers (7.2 percent) and
Black and White mothers (4.5-5.0 percent). Over the past decade, the maternal
diabetes rate has increased among Hispanic mothers, but not among the other
racial/ethnic groups in the region.
Both large communities in PHR 6/5S, Beaumont-Port Arthur (8.7 percent) and
Galveston (8.3 percent), had high percentages of babies where the mother had
some form of hypertension in 2015. Overall, mothers in rural counties in PHR 6/5S
(9.4 percent) experienced a higher prevalence of maternal hypertension than their
urban counterparts (7.6 percent). While the Houston-The Woodlands community
(6.2 percent) reported a higher rate of maternal diabetes than the state as a whole,
the Galveston community (4.8 percent) had a lower maternal diabetes rate than
the state. Small urban/rural differences in the prevalence of maternal diabetes were
observed in the region.
Smoking During Pregnancy
Smoking while pregnant has also been linked with many health problems, including
premature birth, low birth weight, birth defects, and infant death. In PHR 6/5S,
only 2.5 percent of women who gave birth in 2015 smoked during pregnancy. This
region’s rate was lower than the statewide rate of 3.6 percent. The percentage of
live births where mothers smoked during pregnancy in the region has decreased
from 5.0 percent in 2006.
Of all racial/ethnic groups in PHR 6/5S, White women have the highest percentage
of maternal smoking. In 2015, White women (5.8 percent) had a rate of smoking
during pregnancy that was three times that of Black women (2.2 percent). Both
Hispanic women (0.6 percent) and women of ‘Other’ race/ethnicity (0.7 percent) in
the region are currently meeting the HP2020 target of at least 98.6 percent
abstinence from smoking during pregnancy. From 2006 to 2015, sizable decreases
in rates of smoking during pregnancy were observed among all racial/ethnic groups
in the region.

PUBLIC HELATH REGION 6/5S
60
Geographic variation exists in rates of
smoking during pregnancy. In 2015, two
counties in PHR 6/5S had low rates of
smoking during pregnancy (1.4 percent
or less) that met the HP2020 target,
while three counties in the northern part
of the region had high rates of smoking
during pregnancy (10.9 percent or
greater) (Figure 3.8). Among all PHR
6/5S counties with 100 or more
documented births in 2015, smoking
rates during pregnancy ranged from 0.8
percent to 14.9 percent. Overall, women
in rural counties in the region (5.6
percent) had a higher prevalence of
smoking during pregnancy than their counterparts in urban counties (2.4 percent).
Drinking During Pregnancy
Alcohol use during pregnancy has been associated with several adverse birth
outcomes. Based on pooled 2011-2015 PRAMS data, 7.6 percent (CI: 6.1-9.1) of
women in PHR 6/5S reported drinking in the last three months of pregnancy. The
prevalence rate for this region was about the same as the statewide prevalence
rate (7.8 percent, CI: 7.0-8.7).
Based on pooled 2011-2015 PRAMS data for PHR 6/5S, White/Other women
reported a higher rate of drinking in the last three months of pregnancy than Black
and Hispanic women. White/Other women in PHR 6/5S reported about the same
rate of drinking in the last three months of pregnancy (10.0 percent, CI: 7.4-12.6)
as White/Other women in Texas (10.2 percent, CI: 8.8-11.5). However, Black
women in the region reported a higher rate of drinking in the last three months of
pregnancy (8.4 percent, CI: 6.2-10.6) compared to Black women in Texas (7.4
percent, CI: 6.1-8.6). Hispanic women in the region reported about the same rate
of drinking in the last three months of pregnancy (5.1 percent, CI: 2.8-7.4) as
Hispanic women in the state as a whole (6.0 percent, CI: 4.7-7.2).
Physical Abuse Before/During Pregnancy
Physical abuse before and/or during pregnancy has been associated with adverse
outcomes for the mother and the infant. Based on pooled 2011-2015 PRAMS data,
3.8 percent (CI: 2.7-4.9) of women in PHR 6/5S reported experiencing physical
Figure 3.8

PUBLIC HELATH REGION 6/5S
61
abuse before and/or during pregnancy. The prevalence rate for this region was
about the same as the statewide prevalence rate (4.0 percent, CI: 3.4-4.6).
Based on pooled 2011-2015 PRAMS data for PHR 6/5S, Black women reported a
higher rate of physical abuse before and/or during pregnancy than White/Other and
Hispanic women. Black women in PHR 6/5S reported about the same rate of
physical abuse before and/or during pregnancy (5.1 percent, CI: 3.3-6.8) as Black
women in Texas (5.4 percent, CI: 4.3-6.5). However, White/Other women in the
region reported a higher rate of physical abuse before and/or during pregnancy (4.1
percent, CI: 2.4-5.8) compared to White/Other women in Texas (2.9 percent, CI:
2.2-3.7). On the other hand, Hispanic women in the region reported a lower rate of
physical abuse before and/or during pregnancy (3.0 percent, CI: 1.3-4.8) compared
to Hispanic women in Texas (4.6 percent, CI: 3.5-5.7).
Postpartum Depression
Postpartum depression (PPD) has been associated with adverse health outcomes for
mothers and infants. Based on pooled 2012-2015 PRAMS data, 15.7 percent (CI:
13.3-18.2) of women in PHR 6/5S reported PPD symptoms. The prevalence rate for
this region was higher than the statewide prevalence rate (13.8 percent, CI: 12.6-
15.1). PHR 6/5S, along with PHR 11, had the highest prevalence of PPD symptoms
among all PHRs in Texas.
Based on pooled 2012-2015 PRAMS data for PHR 6/5S, Black women reported a
higher rate of PPD symptoms than White/Other and Hispanic women. Black women
in PHR 6/5S reported a higher rate of PPD symptoms (21.9 percent, CI: 18.2-25.6)
compared to Black women in Texas (19.4 percent, CI: 17.2-21.5). White/Other
women in the region also reported a higher rate of PPD symptoms (15.0 percent,
CI: 11.5-18.6) compared to White/Other women in Texas (12.4 percent, CI: 10.7-
14.1). However, Hispanic women in the region reported about the same rate of PPD
symptoms (14.0 percent, CI: 9.5-18.4) as Hispanic women in Texas (13.7 percent,
CI: 11.6-15.8).
Postpartum Checkup
Postpartum visits are important for screening and assessing the health of the
mother. Based on pooled 2011-2015 PRAMS data, 86.0 percent (CI: 83.8-88.2) of
women in PHR 6/5S reported a postpartum checkup. The prevalence rate for this
region was the same as the statewide prevalence rate (86.0 percent, CI: 84.9-
87.2).
Based on pooled 2011-2015 PRAMS data for PHR 6/5S, White/Other women
reported a higher postpartum visit rate than Black and Hispanic women.

PUBLIC HELATH REGION 6/5S
62
White/Other women in PHR 6/5S reported about the same postpartum visit rate
(91.4 percent, CI: 89.0-93.9) as White/Other women in Texas (91.3 percent, CI:
90.0-92.6). However, Black women in the region reported a lower postpartum visit
rate (83.8 percent, CI: 80.9-86.8) compared to Black women in Texas (84.8
percent, CI: 83.0-86.6). Hispanic women in the region also reported about the
same postpartum visit rate (81.9 percent, CI: 77.6-86.2) as Hispanic women in the
state as a whole (81.8 percent, CI: 79.7-83.9).
Infant Health Practices
Protecting and improving the well-being of infants is an important task. Known
protective infant health practices are addressed in this section, such as
breastfeeding, safe infant sleep, and well-baby checkup.
Breastfeeding
Breastfeeding protects babies from infections and illnesses, reduces the risk of
sudden infant death syndrome, and also has many health benefits for mothers.
Based on pooled 2011-2015 PRAMS data, 88.0 percent (CI: 86.1-89.9) of women in
PHR 6/5S reported ever breastfeeding. The prevalence rate for this region was
about the same as the statewide prevalence rate (87.4 percent, CI: 86.3-88.5).
Based on pooled 2011-2015 PRAMS data for PHR 6/5S, Hispanic women and
White/Other women reported higher rates of ever breastfeeding than Black women.
Hispanic women in PHR 6/5S (91.3 percent, CI: 88.2-94.5) reported a higher rate
of ever breastfeeding compared to Hispanic women in Texas (88.2 percent, CI:
86.4-90.0). White/Other women in the region (89.4 percent, CI: 86.5-92.3),
however, reported the same rate of ever breastfeeding compared to White/Other
women in Texas (89.4 percent, CI: 88.0-90.9). On the other hand, Black women in
the region (75.5 percent, CI: 72.0-79.0) reported a lower rate of ever
breastfeeding compared to Black women in the state as a whole (76.6 percent, CI:
74.5-78.8).
In addition, based on pooled 2011-2015 PRAMS data for PHR 6/5S, the five most
frequently noted hospital experiences that women had about breastfeeding were:
1) Hospital staff gave me information about breastfeeding;
2) I breastfed my baby in the hospital;
3) My baby stayed in the same room with me at the hospital;
4) Hospital staff helped me learn how to breastfeed; and
5) The hospital gave me a telephone number to call for help with breastfeeding.
PRAMS does not collect data on exclusive breastfeeding, but according to the 2016
WIC IFPS survey for Texas, 15.4 percent (CI: 13.0-17.9) of WIC participants in PHR

PUBLIC HELATH REGION 6/5S
63
6/5S exclusively breastfed their child for the first three months. This rate was lower
than the state’s rate of exclusive breastfeeding for the first three months among
WIC participants (18.4 percent, CI: 17.2-19.6), and was the lowest rate among all
PHRs in Texas. Also, about 4.5 percent (CI: 2.9-6.1) of WIC participants in PHR
6/5S exclusively breastfed their child for the first six months; this was lower than
the state’s rate of 6.0 percent (CI: 5.1-6.8).
Safe Infant Sleep
To reduce the risk of SIDS and other sleep-related deaths, infants should be placed
on their backs to sleep. Based on pooled 2011-2015 PRAMS data, 68.8 percent (CI:
66.1-71.6) of women in PHR 6/5S reported placing their infants to sleep on their
backs. The prevalence rate for this region was lower than the statewide prevalence
rate (70.8 percent, CI: 69.3-72.2).
Racial/ethnic disparities exist in infant safe sleep practices. Based on pooled 2011-
2015 PRAMS data for PHR 6/5S, White/Other women reported a higher rate of
placing their infants to sleep on their backs than Hispanic and Black women.
White/Other women in PHR 6/5S reported the same rate of placing infants to sleep
on their backs (77.0 percent, CI: 73.3-80.7) as White/Other women in Texas (77.0
percent, CI: 75.1-78.9). Hispanic women in the region also reported about the
same rate of placing infants to sleep on their backs (70.8 percent, CI: 65.7-75.9)
as Hispanic women in Texas (70.6 percent, CI: 68.1-73.1). However, Black women
in the region reported a lower rate of placing infants to sleep on their backs (43.4
percent, CI: 39.3-47.4) compared to Black women in the state as a whole (48.2
percent, CI: 45.7-50.7).
Well-baby Checkup
Well-baby visits are important for screening and assessing the health of an infant.
Based on pooled 2011-2015 PRAMS data, 97.7 percent (CI: 96.7-98.8) of women in
PHR 6/5S reported a well-baby checkup. The prevalence rate for this region was
about the same as the statewide prevalence rate (97.6 percent, CI: 97.1-98.1).
Based on pooled 2011-2015 PRAMS data for PHR 6/5S, White/Other women and
Black women reported higher well-baby checkup rates than Hispanic women.
White/Other women in PHR 6/5S reported about the same well-baby checkup rate
(98.7 percent, CI: 97.8-99.7) as White/Other women in Texas (98.1 percent, CI:
97.4-98.7). However, Black women in the region reported a higher well-baby
checkup rate (98.5 percent, CI: 97.5-99.5) compared to Black women in Texas
(97.4 percent, CI: 96.6-98.2). Hispanic women in the region also reported about
the same well-baby checkup rate (96.6 percent, CI: 94.5-98.7) as Hispanic women
in Texas (97.3 percent, CI: 96.4-98.2).

PUBLIC HELATH REGION 6/5S
64
Perinatal Periods of Risk
In order to provide communities and stakeholders more in-depth information to
help reduce infant mortality, a comprehensive Perinatal Periods of Risk (PPOR)
approach for PHR 6/5S was undertaken. PPOR gives analytic steps to investigate
and address the specific causes of high fetal and infant mortality rates and
disparities among study populations (such as Whites, Blacks, Hispanics, and
Teens). Both Phase I and Phase II analyses were conducted. PPOR analysis results
are provided in this report, along with practicable recommendations.
PPOR examines the risk of feto-infant mortality during different perinatal periods.
Based on birth weight and age at death, fetal and infant deaths are partitioned into
four corresponding risk periods: maternal health/prematurity, maternal care,
newborn care, and infant health. Each of these periods has different risk factors and
causes of death, and subsequently, different opportunities for prevention.
Therefore, the four risk periods represent distinct points of intervention in the
health care continuum (see PPOR Section in Overview of Texas).
Phase I Analysis
PHR 6/5S and specific study populations (i.e., Black, White, Hispanic, or teens)
were compared to a state-level reference group generally known to have better
feto-infant mortality outcomes (i.e., non-Hispanic White women who are at least 20
years of age and have 13+ years of education). These study populations are not
mutually exclusive. The feto-infant mortality rate (F-IMR) is calculated as the
number of fetal and infant deaths per 1,000 live births and fetal deaths. The excess
F-IMR is the difference in F-IMR between the study population and the reference
group.
In PHR 6/5S, 2010-2014 F-IMRs were
6.1 per 1,000 for White mothers, 11.5
per 1,000 for Black mothers, 6.5 per
1,000 for Hispanic mothers, and 8.5 per
1,000 for teen mothers. Black mothers
experienced a total of 6.3 excess fetal
and infant deaths per 1,000 live births
and fetal deaths in 2010-2014 (Figure
3.9). Total excess F-IMRs for White
mothers, Hispanic mothers, and teen
mothers were 0.9 per 1,000, 1.3 per
1,000, and 3.3 per 1,000, respectively.
Figure 3.9

PUBLIC HELATH REGION 6/5S
65
Black women had the highest excess F-IMRs for three of the four perinatal risk
periods, with 55 percent of all Black fetal and infant deaths being potentially
preventable (i.e. excess fetal and infant deaths). Moreover, 50 percent of the
overall excess Black fetal and infant deaths occurred in the Maternal
Health/Prematurity risk period. For teen mothers, 83 percent of excess feto-infant
deaths occurred in the Maternal Health/Prematurity and Infant Health risk periods.
Phase II Analysis
For fetal and infant deaths occurring in the Maternal Health/Prematurity risk period,
a Kitagawa analysis was conducted for each study population, to examine whether
excess feto-infant mortality was primarily due to a greater number of very low birth
weight (VLBW) births in the study population compared to the reference population
(a difference in birth weight distribution), or to a higher mortality rate among VLBW
infants than seen in the reference population (a difference in birth weight specific
mortality). The percentage of excess deaths attributable to a difference in birth
weight distribution compared with the percentage attributable to a difference in
birth weight specific mortality rates in PHR 6/5S are shown in Figure 3.10 for each
study population.
Overall, as well as for all study
populations, the majority of excess
Maternal Health/Prematurity risk period
deaths in PHR 6/5S were attributable to
a greater number of VLBW births in
these groups when compared to the
reference population. Notably, Black
infants (0 percent) had lower mortality
rates among VLBW births than the
reference population; for this subgroup,
all excess deaths (100 percent) were
potentially attributable to a greater
number of VLBW births (Figure 3.10). Especially for infants born to Black mothers,
interventions aimed at reducing the number of VLBW births are likely to be most
effective at closing the gap in feto-infant mortality. For infants born to White
mothers, Hispanic mothers, and teen mothers, some proportion of excess feto-
infant death was also attributable to a higher mortality rate among VLBW births
than the reference population.
To examine differences in birth weight distribution during the Maternal
Health/Prematurity risk period, a multivariable logistic regression analysis was
conducted to identify factors associated with risk of delivering a VLBW baby.
Factors examined included maternal demographic factors (race/ethnicity, age, and
Figure 3.10

PUBLIC HELATH REGION 6/5S
66
education), multiple gestations, smoking during pregnancy, high parity for age,
previous preterm birth, maternal weight gain during pregnancy, adequacy of
prenatal care, trimester prenatal care began, and payment source for the delivery.
Factors that contributed the most to risk of a VLBW birth in PHR 6/5S included
weight gain less than 15 pounds and inadequate prenatal care. Approximately 19
percent of all VLBW births were attributable to weight gain less than 15 pounds.
Four percent of all VLBW births could be attributed to inadequate prenatal care. All
study populations were more likely to gain less than 15 pounds or receive
inadequate prenatal care compared to the reference population.
To identify factors related to birth weight specific mortality in the Maternal
Health/Prematurity risk period, an analysis was also performed to assess risk of
infant death among VLBW births. Factors examined in this analysis included
maternal demographics, congenital anomalies, inadequate prenatal care, maternal
diabetes, maternal hypertension, infant transfer, maternal transfer, respiratory
care, ruptured membranes, and prenatal steroids. Inadequate prenatal care and
congenital anomalies contributed the most to infant mortality among VLBW births in
PHR 6/5S. Specifically, 4 percent of infant deaths to this group were attributable to
inadequate prenatal care, and 2 percent of deaths were attributable to congenital
anomalies. Compared to the reference population, all study populations were less
likely to receive adequate prenatal care compared to the reference population.
Among all infant deaths in the Infant Health risk period, perinatal conditions were
the primary cause of death, accounting for 35 percent of excess infant deaths in
PHR 6/5S (Figure 3.11). Of the subgroups examined, Black infants and infants born
to teen mothers had the greatest excess
infant mortality in this risk period, with
perinatal conditions accounting for a large
proportion of excess infant deaths in the
region. SIDS contributed to 10 percent of
excess deaths among Black infants and to
7 percent of excess deaths among White
infants. Birth defects accounted for 30
percent of excess deaths among White
infants and for 14 percent of excess
infant deaths to teen mothers.
To further examine excess mortality in the Infant Health risk period, an analysis
was conducted to determine risk factors associated with infant death among infants
28 days and older. Maternal demographic factors, smoking during pregnancy,
adequacy of prenatal care, breastfeeding status at hospital discharge, and trimester
Figure 3.11

PUBLIC HELATH REGION 6/5S
67
prenatal care began were all examined. Not receiving prenatal care in the first
trimester and breastfeeding had the greatest impact on overall risk of infant death
during this time period. Among PHR 6/5S infants 28 days and older, infants who
were breastfed at hospital discharge had an 11 percent reduced risk of infant death,
and about 4 percent of infant deaths were attributable to not receiving prenatal
care during the first trimester.
Recommendations
Phase I analyses identified the populations and periods of risk with the largest
excess feto-infant mortality compared to the reference population. In PHR 6/5S, the
period of risk and study population with the highest excess feto-infant mortality
rate, and thus the greatest opportunity for potential impact, was the Maternal
Health/Prematurity risk period among the Black population. Interventions should
also be targeted to Black populations for Maternal Care and Infant Health-related
deaths. Among teen mothers, interventions should focus on Maternal
Health/Prematurity and Infant Health-related deaths. Maternal Health/Prematurity-
related deaths should be targeted among the Hispanic population, while Infant
Health-related deaths should be the focus among the White population.
Phase II analyses identified modifiable risk factors that contributed the most to
excess feto-infant mortality. To reduce excess feto-infant mortality in the Maternal
Health/Prematurity period of risk, interventions in PHR 6/5S should focus on
improving access to and use of prenatal care; reducing the number of women
gaining less than 15 pounds during pregnancy; and reducing rates of congenital
anomalies. Interventions likely to be most effective in reducing Infant Health-
related excess feto-infant mortality include reducing prematurity among all race
groups; reducing birth defects among White infants and infants born to teen
mothers; increasing rates of breastfeeding; reducing SIDS among Black infants and
White infants; and increasing access to prenatal care.
For your convenience, a companion PPOR fact sheet for PHR 6/5S, 2010-2014 can
be found at this website:
https://www.dshs.texas.gov/healthytexasbabies/data.aspx

PUBLIC HELATH REGION 6/5S
68
Summary Table: Selected Health Indicators in PHR 6/5S
Lastly, a summary table for selected health indicators from 2006 to 2015 is
presented below, to help easily monitor/depict regional trends.
Texas
Indicators
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 10-Year Trend 2015
Birth Rate
a
17.0 17.0 16.9 16.7 15.6 14.8 14.9 14.8 15.1 15.3 14.7
Maternal Age (in Years) 26.9 27.0 27.1 27.2 27.4 27.6 27.8 27.9 28.1 28.3 27.7
Teen Birth Rate
b
53.6 54.2 54.2 51.7 47.8 42.0 38.2 35.8 32.4 30.0 33.0
Infant Mortality Rate
c
6.1 5.9 6.0 6.1 6.0 5.5 5.7 6.2 5.8 5.6 5.6
Preterm Birth
d
11.3 11.5 11.6 11.6 11.4 11.1 11.0 10.9 10.8 10.7 10.2
Low Birth Weight
d
8.7 8.7 8.7 8.9 8.7 8.8 8.6 8.6 8.5 8.5 8.3
Prenatal Care in the 1st
Trimester of Pregnancy
d
63.8 61.0 60.0 59.2 61.0 63.5 63.3 63.7 62.4 63.4 65.9
Pre-Pregnancy Obesity
d
19.4 20.6 21.5 22.0 23.0 23.1 23.3 24.2 24.1 24.7 25.2
Maternal Hypertension
d
5.7 5.3 5.7 5.9 6.5 6.7 6.5 6.7 6.9 7.7 7.4
Maternal Diabetes
d
5.7 5.5 5.4 5.0 5.1 5.6 5.4 5.5 6.1 6.1 5.5
Smoking During Pregnancy
d
5.0 4.6 4.4 4.1 3.8 3.3 3.3 3.0 2.6 2.5 3.6
a
Live births per 1,000 population
b
Live births per 1,000 teen females (aged 15-19)
c
Deaths per 1,000 live births
d
Percent of live births
Sources: 2006-2015 Texas Birth and Death files, Center for Health Statistics, DSHS; 2006-2015 Texas Population Estimates,
Texas Demographic Center.
Public Health Region 6/5S

REFERENCES
69
References
[1]
N. Haghighat, M. Hu, O. Laurent, J. Chung, P. Nguyen and J. Wu,
"Comparison of Birth Certificates and Hospital-Based Birth Data on
Pregnancy Complications in Los Angeles and Orange County, California,"
BMC Pregnancy Childbirth, vol. 16, no. 93, 2016.
[2]
L. Vinikoor, L. Messer, B. Laraia and J. Kaufman, "Reliability of Variables on
the North Carolina Birth Certificate: A Comparison with Directly Queried
Values from a Cohort Study," Paediatric and Perinatal Epidemiology, vol.
24, no. 1, pp. 102-112, 2010.
[3]
Texas Department of State Health Services, "Texas Inpatient Public Use
Data File (PUDF)," [Online]. Available:
https://www.dshs.texas.gov/thcic/hospitals/Inpatientpudf.shtm. [Accessed
December 2017].
[4]
J. Y. Ko, S. W. Patrick, V. T. Tong, R. Patel, J. N. Lind and W. D. Barfield,
"Incidence of neonatal abstinence syndrome- 28 states, 1999-2013," CDC
MMWR, vol. 65, no. 31, pp. 799-802, 2016.
[5]
Health Resources and Services Administration (HRSA), "Federally Available
Data (FAD) Resource Document," [Online]. Available:
https://mchb.tvisdata.hrsa.gov/uploadedfiles/Documents/FADResourceDoc
ument.pdf. [Accessed March 2018].
[6]
E. Kuklina, M. Whiteman, S. Hillis, D. Jamieson, S. Meikle, S. Posner and P.
Marchbanks, "An Enhanced Method for Identifying Obstetric Deliveries:
Implicatoins for Estimating Maternal Morbidity," Maternal & Child Health
Journal , vol. 12, pp. 469-477, 2008.
[7]
Texas Department of State Health Services, "PRAMS," [Online]. Available:
http://dshs.texas.gov/mch/PRAMS.aspx. [Accessed September 2017].
[8]
Texas Department of State Health Services, "Women, Infants, and Children
Program: Surveys and Reports," 2016. [Online]. Available:
https://www.dshs.texas.gov/wichd/bf/surveysreports.aspx. [Accessed
August 2017].
[9]
World Health Organization, "BMI Classification," 2016. [Online]. Available:
http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. [Accessed
October 2016].
[10]
National Center for Health Statistics, "ICD–10 cause-of-death lists for
tabulating mortality statistics (updated March 2011 to include WHO updates

REFERENCES
70
to ICD–10 for data year 2011)," 2011. [Online]. Available:
https://www.cdc.gov/nchs/data/dvs/Part9InstructionManual2011.pdf.
[Accessed August 2017].
[11]
J. Martin, M. Osterman, S. Kirmeyer and E. Gregory, "Measuring
Gestational Age in Vital Statistics Data: Transitioning to the Obstetric
Estimate," National Vital Statistics Reports, vol. 64, no. 5, 2015.
[12]
M. Peck, W. Sappenfield and J. Skala, "Perinatal Periods of Risk: A
Community Approach for Using Data to Improve Women and Infants'
Health," Matern Child Health J., vol. 14, no. 6, pp. 864-874, 2010.
[13]
CityMatCH: The National Organization of Urban MCH Leaders, "What is
PPOR?," 2016. [Online]. Available: http://www.citymatch.org/perinatal-
periods-risk-ppor-home/what-ppor. [Accessed October 2016].
[14]
United States Census Bureau, "Geography - State Area Measurements and
Internal Point Coordinates," January 2010. [Online]. Available:
https://www.census.gov/geo/reference/state-area.html. [Accessed
February 2018].
[15]
Texas Department of State Health Services, "Definitions of County
Designations," 3 June 2015. [Online]. Available:
https://www.dshs.state.tx.us/chs/hprc/counties.shtm. [Accessed July
2017].
[16]
Kids Count Data Center, "Total Population by Child and Adult Populations,"
August 2017. [Online]. Available:
http://datacenter.kidscount.org/data/tables/99-total-population-by-child-
and-adult#detailed/2/2-52/false/573/39/417. [Accessed September 2017].
[17]
Texas State Data Center, Office of the State Demographer, "Projections of
the Population of Texas and Counties in Texas by Age, Sex and
Race/Ethnicity for 2010-2050," November 2014. [Online]. Available:
http://www.txsdc.utsa.edu/Data/TPEPP/Projections/Methodology.pdf.
[Accessed September 2017].
[18]
L. Potter and N. Hoque, "Texas Population Projections, 2010 to 2050,"
November 2014 . [Online]. Available:
http://demographics.texas.gov/Resources/Publications/2014/2014-
11_ProjectionBrief.pdf. [Accessed February 2018].
[19]
Texas Demographic Center, "Texas Population Estimates Data Tool
Results," [Online]. Available:
http://txsdc.utsa.edu/Data/TPEPP/Estimates/Report?id=56ab122865a44f5e
89dee55c442c46fd. [Accessed September 2017].

REFERENCES
71
[20]
United States Census Bureau, American FactFinder, "2011-2015 American
Community Survey 5-Year Estimates," 8 December 2016. [Online].
Available:
https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refre
sh=t. [Accessed September 2017].
[21]
Deloitte, MIT Macro Connections Group & Datawheel, "Data USA: Texas,"
April 2016. [Online]. Available: https://datausa.io/profile/geo/texas/.
[Accessed October 2017].
[22]
Texas Department of State Health Services, Division for Family and
Community Health Services, Office of Program Decision Support, "Scientific
Analysis of the Current State and Needs of Maternal and Child Health
Population in Texas," Austin, TX, February 2015.
[23]
M. Kormondy and N. Archer, "2017 Healthy Texas Babies Data Book,"
Division for Community Health Improvement, Texas Department of State
Health Services, Austin, TX, 2017.
[24]
T. Mathews and B. Hamilton, "Mean Age of Mothers is on the Rise: United
States, 2000–2014," NCHS Data Brief, vol. 232, January 2016.
[25]
J. Martin, B. Hamilton, M. Osterman and A. Driscoll, "Births: Final Data for
2015," National Vital Statistics Reports, vol. 66, no. 1, January 2017.
[26]
Texas Department of State Health Services, "Healthy Texas Babies,"
[Online]. Available:
https://www.dshs.texas.gov/healthytexasbabies/data.aspx. [Accessed
September 2017].
[27]
T. Mathews, M. MacDorman and M. Thoma, "Infant Mortality Statistics From
the 2013 Period Lined Birth/Infant Death Data Set," National Vital Statistics
Reports, vol. 64, no. 9, August 2015.
[28]
Texas Department of State Health Services, "Health Professions," 11
January 2017. [Online]. Available:
https://www.dshs.texas.gov/chs/hprc/health.shtm. [Accessed November
2017].
[29]
M. Ryan, "Health Professional Shortage Areas and Scoring," Bureau of
Health Workforce, Health Resources and Services Administration, March
2017.
[30]
Health Resources and Services Administration, Bureau of Health Workforce,
"Fourth Quarter of Fiscal Year 2017 Designated HPSA Quarterly Summary,"
Rockville, MD, September 2017.

REFERENCES
72
[31]
E. Declercq, M. MacDorman, H. Cabral and N. Stotland, "Prepregnancy Body
Mass Index and Infant Mortality in 38 U.S. States, 2012-2013," Obstetrics
& Gynecology, vol. 127, no. 2, pp. 279-287, February 2016.
[32]
S. Ahmed, M. Ellah, O. Mohamed and H. Eid, "Prepregnancy Obesity and
Pregnancy Outcome," International Journal of Health Sciences, vol. 3(2),
pp. 203-208, July 2009.
[33]
R. Gaillard, B. Durmus, A. Hofman, J. Mackenbach, E. Steegers and V.
Jaddoe, "Risk Factors and Outcomes of Maternal Obesity and Excessive
Weight Gain During Pregnancy," Obesity, vol. 21, no. 5, pp. 1046-1055,
May 2013.
[34]
A. Branum, S. Kirmeyer and E. Gregory, "Prepregnancy Body Mass Index by
Maternal Characteristics and State: Data From the Birth Certificate, 2014,"
5 August 2016. [Online]. Available:
https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_06.pdf. [Accessed
November 2017].
[35]
MedlinePlus, "Infant of Diabetic Mother," U.S. National Library of Medicine,
[Online]. Available: https://medlineplus.gov/ency/article/001597.htm.
[Accessed December 2017].
[36]
A. Lapidus, "Effects of Preeclampsia on the Mother, Fetus, and Child,"
OBGYN.net, 10 October 2010. [Online]. Available:
http://www.obgyn.net/pregnancy-and-birth/effects-preeclampsia-mother-
fetus-and-child. [Accessed December 2017].
[37]
Texas Department of State Health Services, "Maternal Mortality and
Morbidity Task Force and Department of State Health Services Joint Biennial
Report," Texas Department of State Health Services, Austin, TX, July 2016.
[38]
Centers for Disease Control and Prevention, "The Health Consequences of
Smoking: a Report of the Surgeon General," U.S. Department of Health and
Human Services, Atlanta, GA, 2004.
[39]
S. Curtin and T. Mathews, "Smoking Prevalence and Cessation Before and
During Pregnancy: Data From the Birth Certificate, 2014," National Vital
Statistics Reports, 10 February 2016. [Online]. Available:
https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_01.pdf. [Accessed
December 2017].
[40]
Centers for Disease Control and Prevention, "Facts about FASDs," June
2017. [Online]. Available: https://www.cdc.gov/ncbddd/fasd/facts.html.
[Accessed November 2017].

REFERENCES
73
[41]
S. Thurgood, D. Avery and L. Williamson, "Postpartum Depression (PPD),"
American Journal of Clinical Medicine, vol. 6, no. 2, Spring 2009.
[42]
World Health Organization (WHO), "Maternal Mortality Ratio (per 100,000
live births)," 2017. [Online]. Available:
http://www.who.int/healthinfo/statistics/indmaternalmortality/en/.
[Accessed December 2017].
[43]
A. Moaddab, G. Dildy, H. Brown, Z. Bateni, M. Belfort, H. Sangi-Haghpeykar
and S. Clark, "Health care disparity and state-specific pregnancy-related
mortality in the United States, 2005-2014," Obstetrics & Gynecology, vol.
128, no. 4, pp. 869-875, 2016.
[44]
Centers for Disease Control and Prevention (CDC), "Pregnancy Mortality
Surveillance System," November 2017. [Online]. Available:
https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html.
[Accessed December 2017].
[45]
K. Joseph, S. Lisonkova, G. Muraca, N. Razaz, Y. Sabr, A. Mehrabadi and E.
Schisterman, "Factors Underlying the Temporal Increase in Maternal
Mortality in the United States," Obstetrics & Gynecology, vol. 129, no. 1,
pp. 91-100, 2017.
[46]
N. Davis, D. Hoyert, D. Goodman, A. Hirai and W. Callaghan, "Contribution
of maternal age and pregnancy checkbox on maternal mortality ratios in
the United States, 1978-2012," American Journal of Ostetrics &
Gynecology, vol. 217, pp. 352.e1-7, 2017.
[47]
National Insitute on Drug Abuse, "Dramatic Increases in Maternal Opioid
Use and Neonatal Abstinence Syndrome," [Online]. Available:
https://www.drugabuse.gov/related-topics/trends-
statistics/infographics/dramatic-increases-in-maternal-opioid-use-neonatal-
abstinence-syndrome. [Accessed November 2017].
[48]
Centers for Disease Control and Prevention (CDC), "Severe Maternal
Morbidity in the United States," November 2017. [Online]. Available:
https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severemater
nalmorbidity.html. [Accessed December 2017].
[49]
V. Whiteman, J. Salemi, M. Mogos, M. Cain, M. Aliyu and H. Salihu,
"Maternal opioid drug use during pregnancy and its impact on perinatal
morbidity, mortality, and costs of medical care in the United States,"
Journal of Pregnancy, 2014.

REFERENCES
74
[50]
R. Carlin and R. Moon, "Risk Factors, Protective Factors, and Current
Recommendations to Reduce Sudden Infant Death Syndrome: A Review,"
JAMA Pediatrics, vol. 171, no. 2, February 2017.
[51]
F. Hauck, J. Thompson, K. Tanabe, R. Moon and M. Vennemann,
"Breastfeeding and Reduced Risk of Sudden Infant Death Syndrome: A
Meta-Analysis," Pediatrics, vol. 128, no. 1, July 2011.
[52]
U.S. Department of Health and Human Services, "Maternal, Infant, and
Child Health," Office of Disease Prevention and Health Promotion, 2017.
[Online]. Available: https://www.healthypeople.gov/2020/topics-
objectives/topic/maternal-infant-and-child-health/objectives. [Accessed
December 2017].
[53]
National Institutes of Health, "Safe to Sleep campaign," [Online]. Available:
https://www1.nichd.nih.gov/sts/about/Pages/default.aspx. [Accessed
December 2017].
