
Care Planning Guide
Achieving Best Life Experience
Sunn
ybrook
VETERANS
Restoring Abilities
After a Stroke

3
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Acknowledgments
This Care Planning Guide was written by:
Dr. Jocelyn Charles MD CCFP MScCH
Medical Director, Veterans Centre, Sunnybrook Health Sciences Centre
Associate Professor, Department of Family & Community Medicine, Faculty of Medicine, University of Toronto
Pearl Gryfe MSc BSc OT
Clinical & Managing Director Assistive Technology Clinic, Sunnybrook Health Sciences Centre
Adjunct Lecturer, Dept. of Occupational Science and Occupational Therapy,
Faculty of Medicine, University of Toronto
Selena Sun BSc PT
Physiotherapist, Veterans Centre, Sunnybrook Health Sciences Centre
Chris Watson MHSc SLP(C) Reg. CASLPO
Speech-Language Pathologist, Sunnybrook Health Sciences Centre
Kristen Paulseth MHSc SLP(C) Reg. CASLPO
Speech-Language Pathologist, Sunnybrook Health Sciences Centre
Cecilia Yeung RN MN GNC(C) IIWCC
Advanced Practice Nurse
Adjunct Lecturer, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto
With the input and assistance of the K1 Centre Care Team
We acknowledge the Heart & Stroke Foundation for sharing their educational resources referred to in this guide
Restoring Abilities After a Stroke:
Achieving Best Life Experience (ABLE)
Care Planning Guide
Veterans Centre
2012
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Responding to Behaviours Due to Dementia using Achieving Best Life Experience (ABLE) Care Planning Guide

4
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
GREETINGS FROM THE VETERANS CENTRE’S DIRECTORS
We are very pleased to launch this exciting series of Achieving Best Life Experience (ABLE) Care
Planning Guides to assist our interprofessional staff, our Veteran residents and their families in working
together for the best possible quality of life for our residents.
While traditional care focuses on achieving the best clinical outcomes using accepted scientic
evidence and traditional practice methods, our ABLE philosophy focuses on planning care with the
resident and family to achieve what the resident considers to be his or her best life experience in
the Veterans Centre. This involves integrating scientic evidence, the resident’s current abilities and
potential for improvement and the resident’s desired life experience. This collaborative care planning
welcomes and promotes creativity through understanding and sharing of perspectives and ideas.
The ABLE Care Planning Guides are intended for use beyond Sunnybrook’s Veterans Centre. It is
our hope that our ABLE guides will provide interprofessional staff working in complex continuing care
facilities and nursing homes with an easily accessible resource to use with residents and families in
planning and delivering care that is focused on what is important to each resident. We wish you a
successful implementation!
Dorothy Ferguson, RN, BScN, MBA Jocelyn Charles, MD, CCFP
Director of Operations Medical Director
Veterans Centre Veterans Centre

5
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
TABLE OF CONTENTS
INTRODUCTION 6
COMPONENT 1
ASSESS AND DOCUMENT ABILITIES 8
COMPONENT 2
IDENTIFY POTENTIAL FOR IMPROVED FUNCTION 15
COMPONENT 3
LISTEN TO THE VOICE OF THE RESIDENT 18
COMPONENT 4
CARE PLANNING TO ACHIEVE RESIDENT’S DESIRED LIFE EXPERIENCE 21
COMPONENT 5
INTERVENTIONS TO REDUCE ADVERSE OUTCOMES 34
COMPONENT 6
MONITORING THE RESIDENT’S RESPONSE TO INTERVENTIONS 47
DEFINITIONS 49
APPENDICES
APPENDIX 1
UNDERSTANDING STROKE 52
APPENDIX 2
SAFE TRANSFERS 55
APPENDIX 3
ENSURING HYDRATION AND NUTRITION 57
APPENDIX 4
SUGGESTED POST-STROKE EXERCISES 60
Appendix 5
REFERENCES 63

6
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
66
INTRODUCTION
At the Veterans Centre at Sunnybrook Health Sciences
Centre, our goal is to help each Veteran live according to
his or her preferences and to enjoy the best life experience
possible. While traditional best practice and clinical guidelines
focus on best clinical outcomes, in long term care (LTC) our
focus is on quality of life and helping residents perform his
or her desired activities. We encourage inter-professional
collaboration and teamwork focused on the resident’s goals.
Stroke is one of the most common causes of acquired
disability in the aged population and can be an overwhelming,
life-altering event. Approximately 20 per cent of residents
in LTC have a primary diagnosis of stroke. Many of these
residents have not had the opportunity to improve and
restore function. The goal of this guide is to help staff make
a difference in the lives of these residents by working with
them to restore the abilities that will allow them to achieve
their desired life experiences.
Traditional stroke rehabilitation involves evidence-based
assessment and treatment by a variety of health care providers
focused on achieving the highest possible independent
physical and psychological functioning. A signicant number of
long term care residents are not eligible for stroke rehabilitation
programs due to frailty, the severity of their decits, and/or
other physical and cognitive limitations. However, many can
benet from the approach outlined in this guide, even years
after a stroke.
This guide outlines a restorative care approach which respects
each resident’s individuality, and encourages listening to the
resident’s desired outcomes, attends to the resident’s physical
comfort and provides emotional support. Each resident has
his or her own unique values, preferences and needs. Care
should be consistent with the resident’s needs and how the
resident prefers to be assisted.
Written to help staff from any discipline nd information
quickly and easily, this guide is a resource to help caregivers
assist residents achieve their best possible quality of life and
life experience.

7
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
ABLE CARE GOAL-SETTING FRAMEWORK
ABLE CARE GOAL-SETTING FRAMEWORK
What is
preventing the
resident from
achieving these
goals?
Identify
interprofessional
strategies to
facilitate
achieving life
experience goals
Communicate &
implement
strategies
Establish realistic
goals to achieve
desired life
experience
How can we help
to enable the
resident to
achieve goals?
Share
assessments
with resident
/family
- Abilities
- Potentials
What would be
the ideal life
experience for
this resident in
the Veterans
Centre?
Identify current
abilities &
potential for
improved/
enhanced
abilities
Assess potential
for participation
in meaningful
leisure activities
Identify
limitations to
function
Assess verbal &
nonverbal
communication
skills
Assess cognition
Assess physical
abilities (motor,
sensory, pain,
cormorbid health
conditions)
Assess
psychological,
emotional & spiritu
al
needs
ASSESS
RESIDENT’S
ABILITIES &
NEEDS
ESTABLISH
LIFE
EXPERIENCE
GOALS
CREATE &
IMPLEMENT
STRATEGIES
TO ACHIEVE
GOALS
LISTEN TO
THE VOICE
OF THE
RESIDENT
IDENTIFY
POTENTIAL FOR
IMPROVED
FUNCTION &
QOL*
MONITOR
OUTCOMES
Observe
response to
interventions
Modify
interventios
based on
response
Periodic review
of abilities and
goals
*QOL = Quality of Life

8
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 1
ASSESS AND DOCUMENT ABILITIES
A stroke can affect a resident’s function in many ways. The brain controls all of our physical and mental functioning as
well as our emotions and social abilities. How a stroke impacts a resident depends on the part of the brain affected by
the stroke as well as the resident’s previous level of functioning, physical and mental health, personality, environment
and coping strategies. (See Appendix 1) Appropriate interventions through a restorative care approach
1
can lead to
signicant improvements in recovery and functioning even years after a stroke.
Describe Resident’s Current Function
The rst step is to understand a resident’s current limitations to physical, psychological and cognitive functioning.
Accurate recognition of functional impairments can allow for individualized restorative interventions which help reduce
permanent decits and improve a resident’s quality of life.
STEP 1: Describe General Appearance
Observe and document:
• Level of alertness
• Signs of discomfort or pain
• Ability to speak
• Ability to comprehend or understand
• Paralysis or paresis on one side
• Apathy or low motivation
• Frustration and/or irritability
• Specic verbal, non-verbal and/or physical behaviours. (Refer to ABLE Care Planning Guide: Responding to
Behaviours Due to Dementia.)
• Fluctuations in function or behaviours
• Possible barriers to functioning – communication, mobility, cognition

9
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
STEP 2: Describe Ability to Communicate
Difculties with communication may arise from a stroke affecting many different parts of the brain. In general, though, residents
who have had a stroke on the left side of the brain tend to have signicant difculties with communication. To plan appropriate
interventions to improve communication, start by to observing and documenting the resident’s current communication skills.
When documenting communication, only use the term “non-communicative” when the resident has no ability to communicate,
either verbally or non-verbally. Do not use nondescriptive or judgmental terms, such as “speaks funny,” “speaks nonsense”
or “incomprehensible.” Also, avoid labeling; for example, “demented.”
Components of Communication Assessment
Awareness of ability to
communicate
• Perceives communication difculties?
• Frustrated by communication difculties?
Ability to understand
(comprehend)
• Ability to respond reliably to simple yes/no questions (eg: name, season,
location)
• Ability to follow simple one-step commands, multi-step commands
• Ability to understand conversational speech
• Ability to understand more complex material (humor, information not related to
the immediate environment)
Ability to express
• Does spontaneous speech consist of full sentences, or single words?
• Is spoken message on-topic?
• Does spoken message contain non-existent or incorrect words?
• Ability to name objects, people
• Ability to repeat single words, sentences
Quality of speech
• Ability to produce voice
• Strength or volume of voice
• Quality of voice (hoarse, breathy, nasal, strained)
• Clarity of speech (clear, or slurred)
• Rate and rhythm of speech (fast and rushed, slow and laborious)
Written language skills
• Ability to write their name, letters, numbers, single words, sentences, and
paragraphs
• Ability to read single words, sentences, or paragraphs
Non-verbal language skills
• Level of engagement in the conversation: do they maintain eye contact, take
appropriate turns when speaking
• Responds to, or use facial expression to communicate?
• Responds to, or use gestures to communicate

10
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 1
STEP 3: Describe Motor Abilities
The ability to move after a stroke is affected by the resident’s pre-
stroke level of functioning, the type and extent of the stroke as
well as the degree of restorative care provided after the stroke.
Assessing the resident’s degree of limb and trunk mobility and
functional mobility provides the basics for understanding limitations
to enhanced function.
Describe abilities
Limb Mobility:
• Is the resident able to lift his or her affected limb up against gravity? Describe effort
required: minimal, moderate or maximal.
• Describe the degree of limb movement with and without assistance: passive and active
range of motion, full range or partial range for all the affected joints.
• Is there any pain with movement of the limbs, especially the shoulder?
Functional Mobility:
Ability to Roll:
• Is the resident able to roll from side to side independently? Describe assistance: use of
bed rail; one person assistance (minimal or moderate) or two person assistance.
• Is cueing needed for the affected limb?
Ability to sit up at
the edge of the bed:
• Is the resident able to get him/herself up to sit at the edge of the bed?
• Describe assistance needed cueing: minimal, moderate, maximal.
• Does he or she need to use a transfer pole or bed rail to move?
• Can he or she sit at the edge of the bed unsupported? With assistance?
• Does he or she lean to one side?
• How long can they sit at the edge of the bed?
Ability to sit in a
manual wheelchair:
• Can the resident sit comfortably in a manual wheelchair?
• Does he or she lean to one side or lean/fall forward?
• How long can he/she sit up in a wheelchair?
• Is support needed on the stroke limb when seated?
• Can the resident shift his/her weight or reposition him/herself independently in the
wheelchair?
• Is the resident able to move independently in the wheelchair?
• Is the resident able to use a power wheelchair safely?

11
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Describe abilities
Ability to stand up:
• Describe assistance needed: minimal, moderate, maximal.
• Need for gait aid to stand.
• Describe his/her posture: are the resident’s shoulders, hips and feet aligned and parallel?
Are they able to weight bear well on both legs?
• Can he/she stand unsupported? Describe the assistance needed for the resident to
remain standing (minimal/moderate/maximal)?
• Is a walker/pole needed for resident to stay standing?
• How long can he/she stand for?
Ability to walk:
• Can the resident weight bear well on the stroke leg or does that knee buckle?
• Can the resident take a normal step?
• How far can he/she walk?
• How much assistance is needed when walking: Supervision, Minimal, Moderate or
Maximum?
• Does the resident need a gait aid when walking? i.e. walker (with wheels), rollator?
Ability to Transfer:
• Is the resident able to follow directions safely for a safe transfer?
• Does the resident have good trunk control when sitting?
• Does the resident have good strength for weight bearing when standing?
• Is a transfer device needed i.e. transfer pole/walker?
Limitations to
Mobility:
• What is the resident’s energy level? Appears
fatigued? Are they too drowsy? Falling asleep
easily?
• Are there environmental obstacles to movement?
• Cognition: is resident able to follow directions
for safe mobility? Does the resident make
impulsive movements?
• Strength: does resident have enough strength
for safe mobility?
• Is there evidence of pain with movement:
grimacing, groaning, holding a specic body area,
limping, etc?
• Are aids/devices needed for safe transfers i.e.
transfer pole, sliding board, bed rails?
• Are aids/devices needed for mobility: walker, wheelchair, cane?

12
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 1
STEP 4: Describe Perception of His or Her Environment
Understanding the perceptual challenges a resident is experiencing will enable you to identify strategies to overcome these
challenges and help the resident achieve his or her goals. Perception encompasses how one processes and interprets
information from one’s surroundings. In addition to referring to the ability to see, hear, feel and taste, perception includes an
awareness of time, an awareness of the location of objects in relation to each other (spatial relations), an awareness of his
or her body position in space (proprioception), and the ability to recognize familiar people, places and objects.
After a stroke, a person’s ability to feel, sense temperature and be aware of his or her body position can decrease or be
absent. Following a stroke on the right side of the brain, an individual may experience neglect of his or her affected side.
This individual can then unknowingly injure him or herself on the affected side. To identify neglect, you may nd it useful to
use the mnemonic “tune-in.”
A Mnemonic to Identify Neglect
T
Turning the head and/or eyes to one side and not spontaneously looking the other way
U
Unaware of where an arm and/or leg is in relation to the rest of the body
N
Neglecting one side of the body, as if it doesn’t exist
E
Evidence of repeated trauma to the affected limb, but individual is unaware of these injuries
I
Ignoring food on one side of the plate
N
Not able to distinguish temperature (hot/cold) on the affected side

13
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
STEP 5: Describe Mood and Behaviours
When a person has a stroke, the health care team initially focuses on the physical effects of the stroke. However, the
individual may also experience fear, anger, sadness, anxiety, frustration and a sense of grief over his or her physical and
mental losses. All of these emotions result in behaviour changes. Understanding some of the contributing factors to these
behaviour changes will help you plan appropriate care strategies.
The time following a stroke can be an emotional rollercoaster, with the individual experiencing a wide range of feelings – from
loss and despair, to hope, anger and resigned acceptance. In addition, a stroke can affect an individual’s ability to control
his or her emotions, resulting in emotional lability or marked uctuations in emotions.
Residents who have suffered a stroke are at high risk for depression, which may present as cognitive decline. On admission,
the clinical team should assess the resident’s prior history of depression and previous risk factors for depression. In addition,
the team should assess for depression every three months. Treating this mood disorder with medication may not only relieve
the depression, it may also improve mental functioning.
Describe Mood and Behaviours
Moods That May Indicate Depression:
• Apathetic or uninterested
• Withdrawn
• Sad
• Tearful
• Anxious
Emotions That May Indicate
Depression:
• Hopeless
• Helpless
• Sad
• Irritable
• Fearful
• Angry
• Suicidal thoughts
Behaviours That May Indicate
Depression:
• Withdrawn
• Emotional reactions that are inappropriate for the situation
• A raised voice
• Verbal outbursts to staff, family members and/or visitors
• Physically aggressive towards staff, family members and/or visitors

14
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 1
STEP 6: Describe Cognitive Function
The prevalence of cognitive loss in residents who
have had a stroke is affected by many factors,
including the resident’s personality and behaviour
patterns prior to the stroke, the degree of actual
and self-perceived loss resulting from the stroke,
the amount of social support, and the severity
and location of the stroke. If the stroke involved
parts of the brain responsible for memory,
learning and awareness, the residents may
lose his or her ability to remember, comprehend
meaning, learn new tasks, make plans and/or
engage in complex mental activities.
Determining Cognitive Losses
Orientation:
• Does the resident know where he or she is?
• Does the resident know what season it is?
• Does the resident know what year, month and day it is?
Attention:
• Does the resident have a reduced ability to attend to an activity (shortened attention span)?
Memory:
• Does the resident remember what he or she had for his or her last meal or snack?
• Can the resident tell you what activities he or she did today?
Comprehension:
• Can the resident follow simple instructions?
• Can the resident engage in a conversation?
• Can the resident understand written information, as in signs, pamphlets?
• Can the resident understand the humour in a joke?
Recognition:
• Does the resident recognize you?
• Does the resident recognize his or her surroundings?
Further cognition assessment can include the Mini-Mental State Examination (MMSE)
2
or the Montreal Cognitive
Assessment (MoCA).
3

15
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 2
IDENTIFY POTENTIAL FOR IMPROVED FUNCTION
After assessing the resident’s level of functioning, identify the resident’s potential for improving his or her functioning and
quality of life. This can be accomplished through careful observation and ongoing communication with the resident during
day-to-day activities. Look for opportunities to full unmet needs, enhance function and develop potential care goals.
Setting Potential Care Goals
A resident may have already achieved his or her maximum potential in some or all of the following areas of function. If this
is the case, the goal is to maintain current functioning.
Potential
for Improved
Function
Identify Opportunities for Improvement Potential Care Goals
Communicating • Appears frustrated in expressing self • Enhance expressive communication
• Has difculty nding words • Enhance non-verbal communication
to express self
• Has difculty understanding others
• Has difculty understanding humour and sarcasm
• Enhance comprehension
• Has difculty producing a voice
• Imprecise, unclear speech
• Enhance clarity of speech and/or
voice
• Consider input from caregiver(s) regarding
communication habits and/or strategies

16
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 2
Potential
for Improved
Function
Identify Opportunities for Improvement Potential Care Goals
Remembering,
making decisions
and following
instructions
• Requires frequent reminders
• Needs information to be repeated
• Frequently asks questions about where he or she is
• Enhance ability to understand the
information the resident desires
through cueing and other reminders
• Appears frustrated following task instructions • Reduce frustration and/or anxiety
related to poor memory
• Has difculty solving day-to-day problems • Enhance ability to use simple
strategies to solve day-to-day
problems
• Has difculty attending to a task – poor attention,
concentration, impulsive
• Improve ability to attend to a task
• Has difculty with planning and/or sequencing
activities for a particular function
• Enhance ability to perform desired
activities by helping with planning
and/or sequencing
Moving safely
and performing
desired tasks
• Able to partially perform an activity • Increase participation in activities
• Enhance satisfaction with task
performance
• Becomes frustrated trying to do an activity • Reduce frustration
• Weakness limits performance of an activity • Increase strength for activity
tolerance
• Impaired ne motor control • Improve ne motor control
• Has difculty with mobility/transfers • Enhance mobility using equipment,
if needed
• Enhance ability to move safely
• Decreased ability to judge a situation and recognize
the actions that are required
• Enhance judgement
• Has difculty with balance and/or posture

17
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Potential
for Improved
Function
Identify Opportunities for Improvement Potential Care Goals
Perceiving
one’s self and
surroundings
• Loss of awareness in the affected side (neglect)
• Decreased ability to feel part of his or her body
• Enhance recognition of self
• Unaware of his or her limitations • Enhance recognition of abilities
• Unable to see part or all of surroundings • Enhance appreciation of
surroundings
• Limited ability to hear • Optimize ability to hear
• Decreased recognition of people, objects and/or
the environment
• Has difculty appreciating the location of objects
around him or her
• Enhance awareness of
surroundings
• Decreased awareness of time • Enhance awareness of time
Feeling content • Appears withdrawn or socially isolated • Enhance mood
• Cries or laughs at the wrong time and cannot stop
(emotional ability)
• Changes in personality
• Enhance social engagement
• Increase contentment with daily
care activities
• Appears frustrated or anxious
• Expresses frustration and/or anxiety during daily
care activities
• Reduce frustration
• Appears angry • Decrease anger
• Displays aggressive behaviours (verbal and/or
physical)
• Reduce aggressive behaviour
• Lethargic (lack of interest) • Enhance energy level
Participating in
activities he or
she enjoys
• Doesn’t participate in desired leisure activities
• Short attention span
• Enhance participation in the
activities the resident enjoys
• Physical or cognitive limitations to participating in
activities
• Enhance ability/strength/endurance
required to participate in desired
activities.

18
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 3
LISTEN TO THE VOICE OF THE RESIDENT
A basic human need is to communicate our needs, emotions and thoughts. Everything we do involves sending messages
to others.
Communication decits are among the most frightening and frustrating results of a stroke for both the resident and the
caregiver. If a stroke damages the language centre in the brain, there will be language difculties. Some stroke residents are
unable to understand or speak at all. Others seem to know what to say, but the words that come out don’t make sense.
Some can no longer read or write. Many have difculty pronouncing words.
Speech, however, is only one way to communicate. We also communicate non-verbally through how we stand or move,
our facial expressions, as well as the tone of our voice. As we get to know another person, we learn to read each other’s
facial expressions and body language, and communication becomes easier and more successful.
Every conversation has at least two communication partners. Each partner has the responsibility to speak (to send a message)
and listen (to receive and understand the message the other has sent).
Strategies to Help Resident Communicate Successfully
Be aware that in addition to communication changes resulting from a stroke, many residents have decreased hearing and/
or vision. You will need to make adjustments to accommodate these challenges.
Create an Optimal Environment:
• Communicate in a quiet place – turn off the TV or radio, limit other distractions.
• Communicate face-to-face and at eye level.
• Ensure adequate lighting.
• Treat the resident with respect.
Enhance Communication:
• Don’t rush.
• Speak slowly and clearly, in a natural voice.
• Listen carefully and actively.
Monitor the Effect of Your Communication;
• Watch the resident’s facial expressions.
• Be aware of your non-verbal communication – facial expressions, tone of voice.

19
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
19
Do... Don’t...
Communication Do’s and Don’ts
9 Respect the person and his or her message.
9 Be supportive and offer encouragement.
9 Try to discern what the resident is really trying
to say.
9 Offer positive feedback by telling the resident that
he or she is managing well.
9 Gently offer information and assistance to the
resident to enable him or her to become more
independent.
9 Respond to the tone of the message if you are
unable to understand the words.
8 Dismiss the resident’s concerns.
8 Finish the resident’s sentences without rst
asking for his or her permission.
8 Ignore the emotion behind the message.
8 Give false assurances.
8 Offer unwanted advice or make assumptions.
8 Be judgmental.
Empathy and respect are essential to listening and understanding. Empathy is being able to put yourself in someone else’s
shoes and to be compassionate. Empathetic listening is an art that needs to be practised; it will allow you to look beyond
the words to discern what the person is really communicating.
One way to show the resident you are actively listening is to match his or her mood or affect. If the resident is happy and
cheerful, smile and be pleased for him or her. If the resident is sad or distressed, show concern and have a sympathetic
expression on your face.
How the Past Informs the Present
Understanding the resident’s past can help you to identify coping strategies and opportunities for improved life experiences.
Inquire About Resident’s Past:
• Family history, signicant relationships and involvement
• Military service and signicant past events
• Occupation
• Hobbies and interests, leisure activities
• Social history – desired engagement with others
• Specic care preferences
Social history

20
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 3
Inquire About Resident’s Current Realities:
• His or her life in the Veterans Centre
• His or her communication, cognitive and physical abilities
• Perception of family members
• Perception of staff
• Perception of the environment
• Desired activities
Questions to Guide a Discussion of Desired Life Experience
Establish the resident’s desired life experience in the Veterans Centre by asking:
• What is life like for you at the present time?
• Can you tell me about your concerns?
• What is most important to you?
• What information would you like?
• Given your current abilities and what your care team feels you are able to achieve, what activities would you like to be
able to do?
Communicating Your Assessment To Others
Share your cognitive, communicative and behavioural assessments with the resident’s substitute decision maker (SDM). If
the resident is capable, permission is required to share assessment information with the SDM.
Sharing the health care team’s assessment of the resident’s symptoms validates the team’s ndings and assists the resident
and/or SDM to understand the symptoms and the identied needs. This validation and understanding allows the resident
and/or SDM to fully participate in the development of an optimal care plan.
Many family members have a limited understanding of the physical and cognitive effects of a stroke. They may not know how
the stroke has affected the resident’s behaviour and his or her functional abilities. When sharing information, be sensitive to
the fact that in many families, lives are complex. People may be struggling with their own health problems, trying to balance
work and family responsibilities, as well as grieving the loss of their loved one’s abilities.
Effective communication among team members is essential when caring for a resident who has suffered a stroke. It is
important to have ongoing scheduled meetings, including rounds and family conferences, to discuss the resident’s progress
and develop a team approach to a care plan for treatment. Other ways of ensuring good communication include clear
consistent documentation, shift-to-shift reports, and staying up to date with the resident’s progress and care plans.
Staff members must respect the other team members’ values, opinions and expectations regarding treatment; individuals
often have different perceptions of and ideas for treatment approaches.
Resident’s perception

21
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
CARE PLANNING TO ACHIEVE RESIDENT’S DESIRED LIFE EXPERIENCE
Care planning and interventions for a resident who has had a stroke must be individualized. To guide care planning, use a
restorative care philosophy together with a goal-setting framework focused on achieving what the resident considers to be
his or her desired life experience.
Determining appropriate care strategies requires the inter-professional team to carefully assess the resident’s potential
for improvement (see Component 2). Rehabilitative care is most commonly associated with individual disciplines (e.g.,
occupational therapy, physical therapy, speech-language pathology, recreational therapy, neuropsychology), assessing
and treating an individual to achieve optimal functioning. The ABLE approach requires team members to work together to
assess the resident and recommend a restorative plan that specically addresses the resident’s individual needs to achieve
his or her desired life experiences.
Before initiating an intervention strategy, consider that each resident has unique cultural and cognitive perspectives that can
affect his or her motivation to participate. Before starting any treatment, speak with the resident and explain what is about
to happen. Move slowly and explain gently how the intervention will benet him or her. Encourage the resident to participate
as much as possible on his or her own volition.
COMPONENT 4

22
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 4
Encouraging Communication
After a stroke, some people have specic communication impairments that result from injury to specic areas of the brain.
It is important to know the kind and extent of communication problems to develop appropriate strategies. Improving a
resident’s ability to express and understand will reduce frustration and enhance his or her quality of life.
Communicating with Residents with Aphasia
Goal Approach
Reduce the
person’s
frustration with
communication
• Give the resident your undivided attention
• Provide adequate time for the resident to speak and respond to questions
• Ensure you have facilitative materials to aid in the interaction (pen and paper, alphabet board,
communication board/book, hearing aids)
• Conrm that you have understood the resident by summarizing what they have said, and
verifying their responses to questions (by asking the same question in a different way)
• If the resident appears frustrated and unable to access a specic word, ask them if you can
try and supply it
• If the actual message is not understood, respond to the emotional content
• Reassure the resident that you understand that they know what they want to say, and that it is
the language difculty that is causing problems.
Enhancing
the person’s
understanding
• Ensure a quiet environment
• Face the resident when speaking; ensure you have their attention before speaking
• Speak slowly and clearly, in your natural voice
• Give information in short, simple sentences
• Print key words on paper
• Use pictures, gestures, or refer to objects in the room, to increase clarity of your message
• Refer to clocks and calendars when speaking about date and time
• Discuss one topic at a time. Make changes in topic explicit.
Enhancing
the person’s
expression
• Allow time for responses
• Ignore grammatical mistakes and articulation errors; the goal is to communicate a message,
not perfect speech
• If the resident is stuck on a specic word, either ask them if they can provide a different word,
provide a description instead, or ask if you can try and supply it
• If the resident is not able to verbally express themselves, encourage them to try using gesture,
point to an object, draw, write, or use an alphabet or communication board/book

23
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Goal Approach
Enhancing
the person’s
speech
intelligibility
• Encourage the resident to speak slowly and clearly as able
• If part of a message is not understood, ask the resident to repeat only the part of the
message that was missed
• Repeat the message back to the resident to conrm that you have understood
Communicating with Residents with Cognitive Impairment
• Frequently introduce yourself to the
resident using your name and role.
• Smile and make eye contact.
• Always remain pleasant and calm.
• Listen carefully.
• Watch the resident’s facial expressions
and body language to understand what
he or she is trying to communicate.
• Check with the resident to ensure you
have understood what he or she is
trying to communicate.
Approaches to communicating with
individuals who have cognitive impairment
due to stroke are similar to communicating with residents with dementia. (Refer to Component 3 in Responding to Behaviours
Due to Dementia: ABLE Care Planning Guide.)
Enhancing Movement
Positioning is essential for comfort and to promote optimal functioning. Proper positioning can help a resident function, increase
his or her awareness, and reduce complications such as pain, skin breakdown, contractures and respiratory problems.
24
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 4
Positioning the Upper Limbs
Goal Approach
Reduce discomfort due to a
dropped shoulder (reduced
muscle tone)
• When the resident is sitting, support the affected arm using a lap tray or arm
trough.
• When moving the resident, always ensure the arm is supported.
• When assisting with walking and transfers, avoid pulling the affected arm.
• When lying in bed, place small pillow under the shoulder / arm
• May need to consider a sling during tranfers/ambulation
Reduce discomfort due to an
elevated shoulder
(increased muscle tone)
• Ensure the arm is aligned.
• Support the arm:
· Use a pillow or folded towel in bed.
· Use a lap tray when seated.
• Assist with appropriate exercises
• Monitor for pain.
• When lying in bed, place small pillow under the shoulder/arm.

25
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Goal Approach
Reduce discomfort and/or
limitations due to a weak hand
with decreased muscle tone
• When the resident is sitting, support the hand using a lap tray or trough.
• To reduce swelling, elevate and support the wrist and hand using a foam
wedge or arm support.
• Place the affected hand in front of the resident with his or her ngers in an open
position. Then, encourage the resident to use his or her other hand to gently
open the affected hand and extend the ngers.
Reduce discomfort and/or
limitations due to a weak hand
with increased muscle tone
(spasticity)
• Position the arm slightly forward from the shoulder.
• Observe for any signs of pain or swelling.
• Elevate the hand on a foam wedge or arm support. Gently open the ngers.
• Encourage the resident to use his or her unaffected hand to gently open the
hand and ngers on the affected side.
• Encourage nger/wrist extension as possible.

26
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 4
Positioning the Lower Limbs
Goal Approach
Reduce limitations due to a
weak leg
• To decrease stiffness and deformity of the foot, encourage the resident to
stand, if possible.
• When the resident is lying down, elevate his or her feet and/or lower legs. Avoid
pillows under the knees if there is increased tone.
• Try to keep ankles at 90° - may need braces/positioning devices to prevent
plantar exion contractures (Requires OT/PT consult).
• Encourage leg extension
Ensure an appropriate sitting
position to reduce discomfort
and enhance function
• Ensure that the feet are supported and the ankles are at 90° angles.
• Ensure that the hips and knees are at 90° angles.
• Be sure the resident sits with his or her hips at the back of the chair.
• Ensure that the resident’s chair or wheelchair supports proper positioning.
• Make certain that the resident is comfortable.
• Reposition and assess skin every two hours – look for redness, possible
pressure areas.
• If resident is sitting on a chair cushion, ensure it is properly inated.

27
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Promoting a Sense of Surroundings
Goal Approach
Enhance
awareness of
time
• Explain when things will happen in relation to known events – e.g., The music will begin after
dinner.
• Each day, explain the daily schedule and provide reminders.
• To limit confusion, keep the schedule consistent.
• If the resident appears anxious about being late for or missing an appointment or meeting, be
reassuring.
• Gently reinforce the passage of real time – e.g., Your daughter left an hour ago.
• Use a digital or talking clock.
Enhance
awareness
of physical
environment
• Ensure the environment is safe and free of clutter.
• Arrange the environment so there is some stimulation on the side affected by the stroke.
• Place objects of interest on the resident’s affected side to increase awareness of the space.
• To avoid startling the resident, approach from the unaffected side.
• Use visual cues to assist the resident – e.g., place a line of red tape at the edge of a table on
the affected side.
• Encourage the resident to scan the environment. With the Lighthouse Strategy
4
, you ask
the resident to imagine his or her eyes as beams of light sweeping from side to side.
Reduce neglect
of affected side
of body
• Use the affected arm or leg in daily care, if the resident can tolerate it.
• Position the affected arm so the resident can see it.
• Gently rub the affected arm to stimulate sensation and awareness.
• Encourage the resident to help position the affected arm and/or leg for function and visibility.
• Use cues to draw attention to the affected side.
Enhancing Mood and Behaviour
A stroke can decrease a resident’s ability to control his or her emotions. It can also change the way the resident behaves
and interacts with others.

28
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 4
Approaches to Mood and Behaviour Modications
Goal Approach in Responding
Express
emotions
• Ask the resident how he or she is feeling.
• If the resident loses control of his or her emotions, gently reassure the resident that controlling
emotions can be difcult after a stroke. Consider distracting the resident with an activity he or
she enjoys.
Enhance social
engagement
• Help the resident to engage in his or her favourite activities.
• Speak with the resident when in his or her room.
• Encourage the resident to attend activities that relate to his or her interests and are within his
or her abilities.
• Give the resident opportunities to verbalize life experiences and share his or her memories.
• Support the resident in contacting and participating in spiritual and/or cultural events.
Maximize
function
and reduce
frustration
• Learn the resident’s preferences for daily routines. Follow his or her preferences whenever
possible. Explain when routines need to be broken.
• Explain what you are planning to do so the resident is prepared.
• Help the resident be successful with tasks by alternating between easy and difcult tasks.
• Observe for signs of frustration and offer support or assistance.
• Give resident adequate rest breaks.
• If a situation or activity causes signicant frustration and/or anger, offer to help the resident to
go to another location. Then, redirect the resident’s attention to something he or she enjoys.
Enhance
interest in
activities
• Make it as easy as possible for the resident to participate in activities.
• Reinforce and support any interest the resident shows.
• Use praise to encourage the resident.
• If the resident is initially unsuccessful at a task or activity, gently encourage him or her to try
again.
• If the resident declines participating in an activity he or she will likely enjoy, try asking him or
her to participate again later.
Enhance
judgment
• Avoid situations that require the resident to make decisions beyond his or her capabilities.
• Inform the resident of inappropriate or unsafe behaviours in a simple, direct way.
• Offer appropriate alternatives.
• Avoid criticizing the resident.
• Use praise to reinforce appropriate behaviour.

29
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Improving Memory and Cognition
After someone has had a stroke, his or her memory and other aspects of cognitive function may be affected. Over time and
with appropriate interventions, a resident can improve some of these skills. Use individualized strategies to reduce frustration
and help the resident perform activities of daily living as independently as possible.
Strategies to Improve Memory and Cognition
Goal
Strategies
Improve attention • Reduce distractions – TV, radio, other conversations.
• Give short, simple, step-by-step instructions.
• Ensure the resident understands the instructions you have given before you continue.
• Face the resident and make eye contact to help the resident focus on what you are
saying.
• Give the resident enough time to think and respond.
• Speak and move slowly so the resident doesn’t feel pressured to respond before he or
she is able.
Enhance orientation • Give gentle reminders about time and place – e.g., What a nice spring day!
• Post a calendar to help the resident keep track of the month and day.
• Use a bulletin board to post personal information and family pictures.
• To avoid confusion, try to keep the resident’s schedule consistent and limit changes.
Enhance memory • Encourage memory aids – e.g., calendar, white board, daily planner if the resident is able
to read, recorded voice reminder if the resident is unable to read.
• Patiently repeat information to help the resident remember it.
• Provide simple, clear information that focuses on the information the resident needs.
• Store items in the same places.
• Ensure drawers and cupboards are clearly labelled with their contents.
Enhance insight • Gently remind the resident about his or her limitations, as required.
• Discuss concerns about the resident’s safety with the resident and care team.
• Develop strategies to optimize safety and functioning with the care team.
• Avoid situations in which the resident needs to make decisions beyond his or her abilities.
• If the resident uses a cane or walker, keep it within reach.
• Use signs to remind the resident about safety.
30
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 4
Goal
Strategies
Enhance ability to
sequence actions
to complete a task
• Encourage the resident to slow down and plan his or her actions.
• Help the resident think about and plan a task.
• Give clear, specic instructions.
• Divide a task into small steps to help the resident focus on one step at a time.
• Give the resident time to practise the task.
• Follow the same sequence each time the task is repeated.
Enhance ability to
solve problems
• Encourage the resident to think about different ways to solve a problem.
• Listen to the resident’s ideas for solving a problem.
• Discuss the benets and risks of possible approaches with the resident.
Encouraging Participation in Activities of Daily Living
After a stroke, a resident may feel previous activities of daily living and/or leisure pursuits are now too difcult. To engage in
desired activities, the resident may need attention to the environment and encouragement with appropriate cueing, assistive
devices and the proper pacing of activities.
General Guidelines:
• Ensure hearing aids and/or glasses are used appropriately.
• Ensure the resident can hear and/or see you.
• Identify how the resident would like to participate in his or her activities of daily living. Ask about:
· timing
· order of care
· how assistance is best provided.
• Assess and manage pain or discomfort.
• Recognize fatigue and respond with a exible approach.
• Remain optimistic.
• Expect uctuations in cognitive and physical abilities from day to day.
Create an Optimal Environment:
• Ensure an appropriate room temperature and privacy.
• Reduce distractions – noise from TV, radio, room, hallway.
• Minimize barriers to movement.
• Ensure adequate lighting.
• Ensure that appropriate equipment and/or assistive devices are available and within reach.

31
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Reminding Through Cueing
Visual Cueing Verbal Cueing
Tactile Cueing
• Position the resident’s impaired limb within
his or her view.
• Help the resident turn his or her head to the
affected side to see objects.
• Move objects to the resident’s visual eld on
the affected side.
• Consider moving the bed so the main action
of the room is on the resident’s affected
side.
• Remind the resident of the
stroke-affected side of his or
her body.
• Encourage the resident to
touch and view the affected
side.
• Touch the affected limb with
various textures.
• Encourage and help the
resident to participate in
activities that require the use
of both hands. (This is an
effective way to develop an
awareness of an affected
limb.)
Caregiving Strategies:
• Encourage adequate rest periods.
• Provide care when the resident is motivated and agreeable to participating.
• Always monitor for pain and discomfort during care.

32
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 4
• Offer choices about order and pace of care.
• Use visual, verbal and tactile cues.
• Enable the resident to perform activities and/or tasks he or she can
perform.
• Ensure clothing design, t and fasteners are appropriate for the
resident.
• Dress the affected side rst.
• Undress from the non-affected side rst.
• Encourage family members and other visitors to verbally reinforce the
resident’s efforts to participate in his or her daily care.
Enhancing Dressing and Grooming
What To Use What To Avoid
9 A mirror
9 Clothes that fasten at the front
9 Velcro fasteners
9 A long-handled shoe horn
8 Tight-tting sleeves, armholes, pant legs and waistlines
8 Clothes that need to be put on over the head.
8 Small buttons, ne zippers and other fasteners that require dexterity
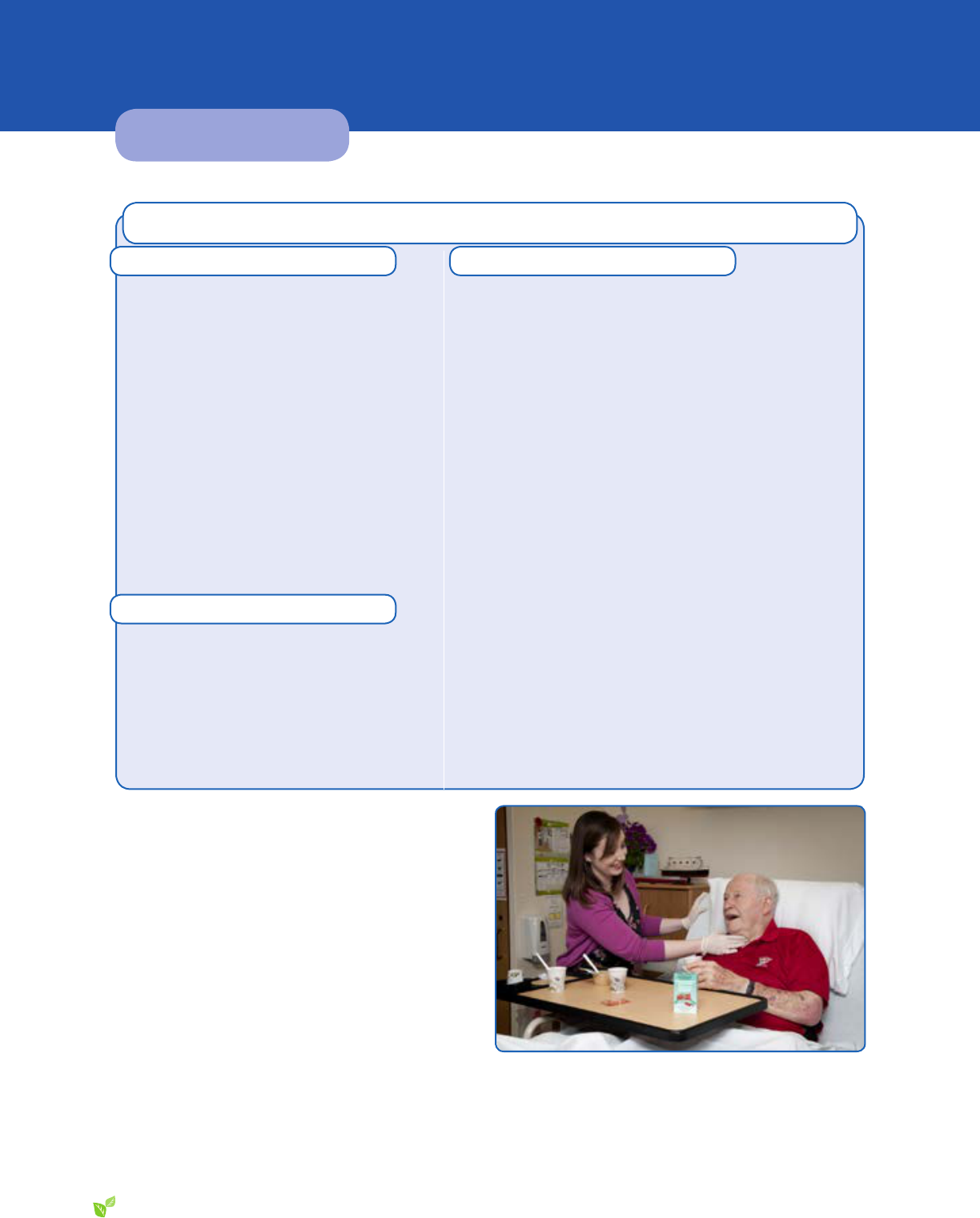
Dining
Create a pleasurable dining experience by paying attention to the resident’s abilities and his or her preferences.
• Ensure the level of auditory, social and visual stimulation is appropriate for the resident. To decrease distractions,
consider providing one food item at a time.
• Conrm that food choices are consistent with the resident’s preferences and recommended diet.
• Ensure the food texture is appropriate for resident’s ability to chew and swallow. (A dentist and/or speech-language
pathologist can provide this assessment.)
• Consider more frequent smaller meals if the resident appears to become tired before nishing a meal.
• Use assistive feeding devices to allow for independence.
Consider:
· Plates with rims
· Plate guards
· Non-slip placemats
· Modied cups
· Large handled spoons
· One-handed rocker knives

33
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Recreation and Leisure Activities
To enhance the resident’s participation in leisure activities, discover ways
to engage him or her in recreational, and religious or spiritual activities. By
participating in social gatherings, exercise and/or music groups, creative
arts and pet visits, the resident can enhance his or her quality of life.
Ensure adequate rest prior to the activity. Then, make sure the resident
is dressed and positioned appropriately for the activity. Before, during
and after the activity, monitor for pain.
Enhancing Participation in Leisure Activities
What to Use What to Avoid
Games
9 A card holder
9 Large playing cards
9 A battery-operated shufer
9 Puzzles with large pieces
Games
8 Small cards
8 Games beyond the resident’s cognitive skill set
Reading
9 A book holder
9 Books on tape
9 Large-print crosswords
9 Magazines
Reading
8 Books with small print
8 Paperback books that are to small to t into a book holder
8 Newspapers
Computer
9 A large monitor
9 A large font size
9 A modied keyboard
Computer
8 Frustration from an inability to use the computer or see
the screen
Crafts
9 A needle threader
9 A one-handed embroidery hoop
9 A one-handed knitting and crochet clamp
9 A C-clamp to stabilize projects
9 Enlarged grips for pens, pencils, paintbrushes
Crafts
8 Activities requiring ne nger movements beyond the
resident’s abilities
8 Crafts with complex instructions or sequencing
8 Activities requiring a co-ordination of movements beyond
the resident’s abilities

34
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
INTERVENTIONS TO REDUCE ADVERSE OUTCOMES
After a stroke, a resident is at risk for a number of health issues. With careful attention and monitoring, you can identify these
risks early and plan interventions to prevent a decline in health and function.
Ensuring Adequate Hydration and Nutrition
After a stroke, a resident may not eat and drink enough to maintain his or her hydration and nutritional needs. This can be
due to a reduced appetite, difculty swallowing, a reduced ability to feed him or herself and decreased cognition.
Ways to Enhance Oral Intake:
• Ensure the resident’s diet includes his or her preferred foods.
• Offer food and uids more frequently than the scheduled times.
• Provide rest periods, as needed.
• Set up the resident’s meal so he or she can see it and be as independent as possible.
• Offer assistance if a resident is having difculty self-feeding.
COMPONENT 5

35
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Hydration
Dehydration occurs when a resident’s uid intake is less than the uid required to meet the body’s needs. There may be
a sudden decrease in uid intake or a gradual decline over days to weeks. Careful monitoring of uid intake can detect
insufcient uid consumption prior to adverse outcomes.
Consider Dehydration if There Is:
• Decreased urinary output
• Dark or strong-smelling urine
• Frequent urinary infections
• Thick saliva
• Constipation
• Dry mouth (causing difcult speaking)
• Dizziness when changing positions
• Increased confusion
• Weight loss
• Decreased skin turgor
• Sunken eyes
For strategies to encourage uid intake, see Appendix 3.
Nutrition
Malnutrition occurs when a resident’s food intake does not meet his or her calorie, protein and other nutrient requirements.
To identify a resident at risk of malnutrition, monitor his or her food intake on a daily and weekly basis, and weigh the resident
every month (or more frequently, if needed)
Consider Malnutrition if There Is:
• Weight loss
• Fatigue and reduced motivation
• Impaired wound healing
• Skin breakdown
• An increased number of infections
Swallowing
A stroke may cause muscle weakness, paralysis and decreased co-ordination in the mouth and throat. This can lead to
slow and/or ineffectual swallowing (dysphagia) and an increased risk of aspiration.
36
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 5
Warning Signs Associated with Dysphagia and Aspiration Risk
5
General Observations:
• Decreased level of alertness
• New delirium or heavy sedation
• Facial weakness or drooping
• Drooling
• Dysarthria
• Weak or absent voice
• Weak or absent cough
• Unexplained weight loss
• Inability to handle oral secretions
• Medical history of recurrent chest infection/
pneumonia
Changes in approach to food:
• Avoidance of eating
• Spitting food out
• Special preparation of food or avoidance
of specic items
• Prolonged meal time, intermittent cessation
of intake
Observations or complaints of:
• Excessive, lengthy chewing
• Holding food in the mouth
• Pocketing or pooling of food and drink in the mouth
(in the cheek, on the tongue, or on the roof of the mouth)
• Delay or absence of the swallow (elevation of the Adam’s
apple or thyroid cartilage)
• Multiple swallows used with each sip/bite
• Wet, or hoarse voice
• Shortness of breath
• Coughing
• Frequent throat-clearing
• Regurgitation
• Sensation of obstruction in throat or chest
• Use of compensatory measures (using drinks to “wash
down” each bite, excessive head movements while
swallowing)
Aspiration refers to the inhalation of food or liquid into the
airway. It can cause an airway obstruction (choking), upper
respiratory infections or pneumonia. Individuals may cough
or silently aspirate their food and/or beverage. If there are
concerns about risk for aspiration, consult a physician and/
or speech-language pathologist. To remember ways to
promote safe eating and feeding, you may nd it useful to
use the mnemonic “pâté.”

37
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Positioning
• Sit upright (90 degree angle if possible).
• Position and maintain the head with the chin tilted slightly down towards their chest. use pillows, blanket rolls, or
head rests behind the head (not the neck) to position the head and maintain the chin tilted downward. It is critical
to maintain the chin tilt position throughout the meal to prevent foods or uids from falling into the throat.
• To maintain downward chin positioning and prevent tilting the head back, remember to:
1. Be at eye level with the person, do not stand over them
2. Use wide rim cups or “nosey“ cups for drinks
3. Position the person so that they can see you and the food
• To prevent reux, avoid lying down for 2 hours after a meal (if the resident is in bed, elevate the head of the bed
to 45 degree angle)
Amount
• Encourage 1 (teaspoon - tablespoon) of food or 1 small sip uid per swallow. Watch the neck for the swallow action
before giving more. Postpone feeding if swallow action is not present.
• Give rest breaks when feeding
Textures
• Check that the person is receiving the recommended food texture and uid texture (see Appendix 3)
• Avoid mixing foods together
• Avoid washing down solids with thin liquids
Enablements
• Check the Care Plan for specic feeding recommendations.
• Ensure that glasses, hearing aids and feeding aids are used if required.
• Check the temperature of the food / uid before feeding
• Acknowledge the resident’s likes / dislikes / preferences / abilities.
*© Sunnybrook Health Sciences Centre (Chris Watson SLP) 2001
SAFE UNSAFE
P.A.T.E.* - Safe Eating and Feeding Guidelines

38
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 5
Preventing Contractures
A contracture is a permanent shortening of a muscle. The result is deformity of a joint with or without pain. It can be
caused by increased tone in a muscle after a stroke, improper positioning or decreased movement of a joint. Prevention
of contractures is important in maintaining abilities and achieving comfortable and functional positioning. Follow these tips:
• Encourage the resident to actively move his or her muscles and joints through daily routines identied by the inter-
professional team.
• Provide activities that encourage the resident to move his or her muscles and joints.
• If the resident has muscle weakness, carry out assisted but gentle range-of-motion exercises during bathing, dressing
and/or other daily activities. If the resident resists, ask for an assessment from an occupational or physical therapist.
• Use splints and/or braces to help prevent contractures, if needed. They can ensure optimal positioning during sleep.
(refer to OT/PT)
• Support the affected limb(s) when the resident is in bed or a wheelchair. When possible, the resident’s arms and legs
should be placed in their longest positions.
• Ensure the knees are as straight as possible when in bed.
• Encourage frequent changes of position.
Do’s and Don’ts for Preventing Contractures
Do Don’t
• Place small towels, rolls or pillows under the scapula
and pelvis.
• Try to keep the affected arm/leg straight as extended
as possible.
• Place small towels or rolls under the pelvis.
• Ensure the body is aligned in a neutral position.
• Encourage resident to actively move/stretch his/her
limbs as often as possible.
• Let the wrist or ngers stay in a exed position.
• Put pillows under the knees.
• Let the resident lean or bend to one side when lying in
bed.
• Allow the resident to lean or bend to one side when
sitting.

39
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Recognizing and Responding to Pain
After a stroke, many residents experience pain. Pain can be a direct result of the stroke (e.g., central post-stroke pain) or
from a disability resulting from the stroke (e.g., shoulder-hand syndrome). In addition, a resident may have pain or discomfort
from other conditions, such as arthritis, previous injuries and/or poor circulation.
The rst step in minimizing pain is to recognize that the resident is having pain. Since the resident may not be able to
communicate that he or she has pain, be alert for signs of discomfort.
Cues to Consider Pain
Verbal and Oral Cues:
• Words such as “itching,” “burning,” “throbbing”
• Moaning or groaning
• Crying or sighing
• Gasping
• Yelling or swearing
Non-Verbal Behaviours:
• Rubbing or massaging a part of the body
• Bracing, holding or guarding a part of the body, especially when moving
• Shifting or rocking (an inability to sit or be still)
• Incontinence due to pain
Facial Expressions:
• Frowning
• Grimacing
• Wincing
• Turning face away
• An angry expression
• A furrowed brow
Behavioural Changes:
• Increased restlessness
• Being quieter than usual
• Decreased appetite
• Decreased interest in usual activities
• Less social interaction

40
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 5
Stroke-Related Pain Syndrome
(6-8)
Type of
Pain
Cause Characteristics Management
1. Central
post-stroke
pain (<10%
of residents)
• Direct result of an
injury to the brain and/
or spinal cord
• Pain can be constant or
intermittent
• Pain can be burning,
tingling or stabbing
• Pain is worse with
activity, a light touch, cold
temperatures or weather
change
• No visible sign of injury or
tissue damage
• Pain often more than
expected from touch and/
or contact
• Ensure optimal positioning
• Minimize touch and/or contact with
objects that increase pain
• Medications:
· Analgesics
· Antidepressants
· Anticonvulsants
• Consider:
· Nerve blocks
· Local anesthetics
2. Shoulder
subluxation
• Stiff, spastic muscles
and/or contractures
• Overstretched or limp
muscles
• Shoulder pain on side
affected by stroke
• Carefully support and position the
shoulder
• Gently move the arm and shoulder,
avoiding aggressive range-of-motion
movements or exercises
• Support the arm and shoulder during
activities of daily living
• Ensure the arm and shoulder are
supported when the resident is
walking, standing or sitting
• Slings, arm boards and lap trays
maybe benecial in some patients
howewer need to be monitored to
prevent over-correction
3. Spasticity
• High muscle tone
resulting from the
stroke shortening
muscles around a joint
• Stiff muscles
• Reduced joint
movements, usually in
the shoulder, elbow, wrist
and/or hand
• Position properly
• Offer gentle range-of-motion exercises.
(Consider a physiotherapy consult.)
• Avoid forcing the limb to move
• Apply custom-made or t splints
as directed by an occupational or
physical therapist
• Consider anti-spasticity medications
and/or a referral to a physiatrist

41
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Type of
Pain
Cause Characteristics Management
4. Shoulder-
Hand
Syndrome
• Reex dystrophy of
the upper extremity
• Intense, burning pain
• Continuous pain
• Increased pain over time
• Limited movement of
hands and/or ngers
• Diffuse tenderness and
decreased shoulder
movement
• Avoid touch and contact that causes
pain
• Follow the recommended positioning
to protect the affected arm or hand
• Physiotherapy
• Analgesic medications
• Be sympathetic
• Consider a ganglion block if the pain
persists
5. Adhesive
capsulitis
• Tightening of the
capsule of the
shoulder due to
inammation or a lack
of movement
• Stiffness with a decreased
range of motion in the
shoulder
• Pain with range of motion
• Offer gentle mobilization exercises, as
directed by a physiotherapist
• Position properly
• Physiotherapy
6. Bursitis
• Inammation of the
subacromial bursa
• Pain on the outside
of shoulder that with
movement may travel
down the arm
• Physiotherapy
• Position properly
• Offer gentle range-of-motion
exercises
• Consider a subacromial steroid
injection
7. Brachial
plexus
fraction
neuropathy
• Flaccid arm that has
been unsupported
• Pulling on resident’s
arm during transfers
• Loss of sensation or
neglect can increase
the risk of fraction
neuropathy
• Continuous pain
• Pain often has burning
quality
• May have reduced
movement and/or
sensation in the hands
and/or ngers
• Forearm
• Use proper transfer techniques, as
recommended by a physiotherapist
• Position properly
8. Trauma
due to
neglect or
decreased
sensation
• Inadvertent injury to
arm, hand, leg or foot
• Failure to appreciate
environment because
of decreased
sensation in the
affected side
• Variable, depending on
the location and type of
injury
• Treat the injury
• Educate the resident, family members
and staff about protecting the
affected limb during activities and/or
movement
9. Rotator
cuff
tendonitis
and/or tear
• Inammation of the
rotator cuff tendons
of the shoulder due to
overuse or injury
• Tears can result from
movement beyond
• Pain only with certain
shoulder movements
• Less pain when shoulder
moved passively
• Physiotherapy
• Range-of-motion exercises
• Corticosteroid injections, if
appropriate
42
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 5
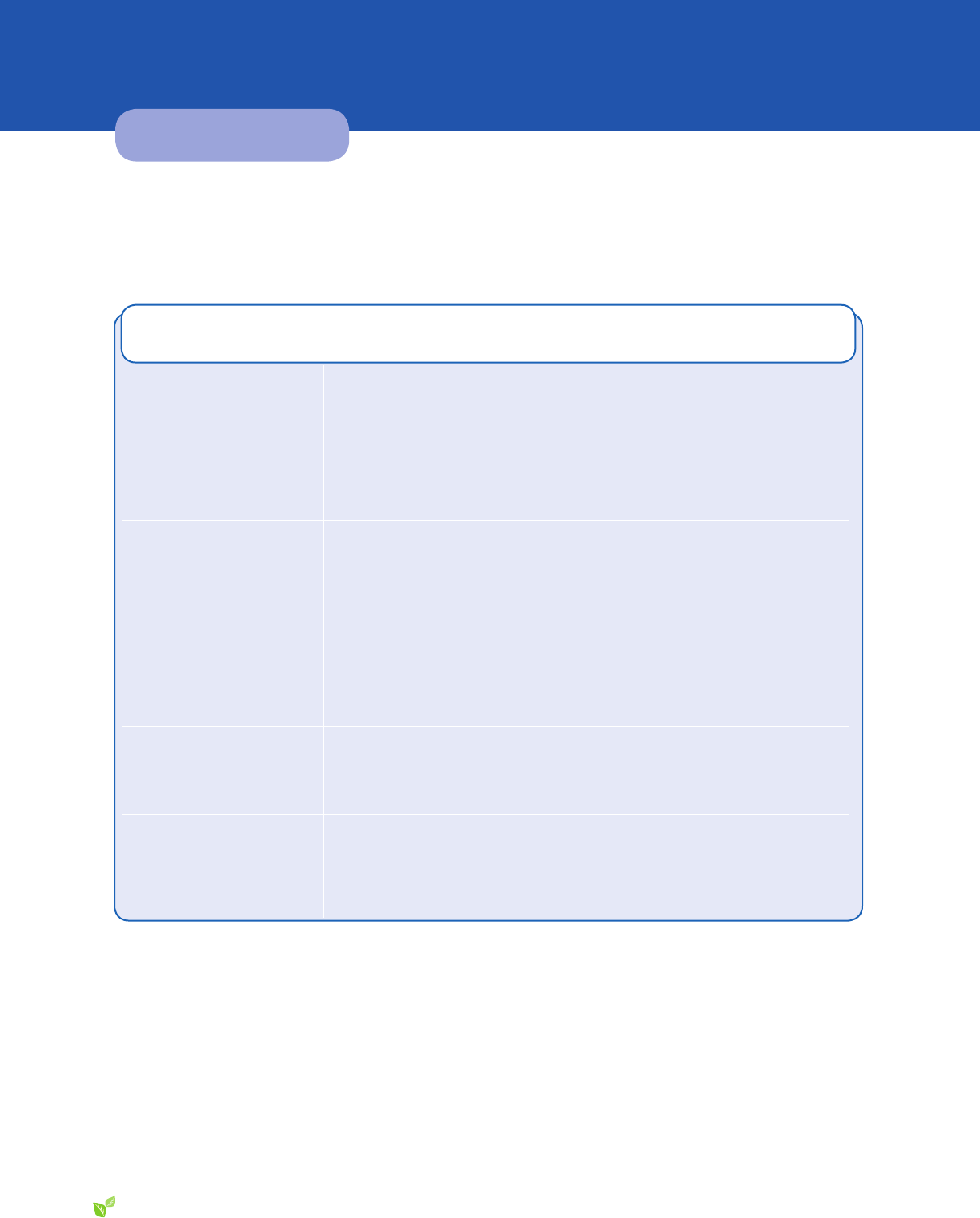
Promoting Continence
Bladder control
Stroke can affect a person’s ability to recognize the need to urinate and respond in a timely manner. It can also affect the
intensity and frequency of bladder contractions, and the ability of the urethral sphincter (valve) to contract and relax.
Mechanism Affected
by the Stroke
Result Strategy
Increased bladder
contractions
9,10
• Urge incontinence
• Frequency
• Urgency
• Incontinence
• Nocturia
• Schedule voiding with gradually longer
intervals between voiding
• To decrease urges, use distraction and
relaxation strategies
11
Decreased bladder
contractions/coordination
with sphincter
10
• Overow incontinence
• Prolonged bladder emptying and/or
failure to empty)
• Over-distended bladder
• Retention of urine
• Ask the resident to attempt to void
twice (double voiding) each time
• Recognize decreased output
• Consider a post-void bladder scan
to identify physiological issues.
If > 300mL, immediately notify the
physician because catheterization is
required
frequent coughing from
dysphagia
13
• Stress incontinence • Kegel exercises
• Consult a physician about whether a
pessary would help a female resident
Decreased mobility,
cognition and/or
coordination
9
• Functional incontinence – not able
to get to the bathroom when the
urge to void occurs because of
physical and/or cognitive limitations
• Regularly assist with toileting
Bowel Function
Ensuring adequate bowel function is an important aspect of post-stroke care. Constipation is common due to neurological
changes that affect bowel motility, the sensory awareness of stool in the rectum, the mobility to respond to the urge to
defecate, the ability to communicate the need to defecate and the cognitive function required for self-toileting
14
.
Fecal incontinence can develop at any time after a stroke. It can be due to a temporary problem, such as constipation
with overow of liquid stool. Or, it can be due to physical and/or cognitive disabilities that impair self-toileting. A medical
assessment may be required to determine the cause of constipation or fecal incontinence.

43
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Managing Constipation
Prevention Recognition Management
• Regular toileting
• Ensure adequate intake of uid (at least
1,500 mL/day, unless contraindicated)
• Ensure an adequate intake of bre (more
than 30 g/day)
• Encourage optimal activity
• Offer to and/or assist with regular
toileting
• Review regular bowel routine with
physician
• Decreased frequency of
movements (2 or fewer per week if
baseline frequency unknown)
• Straining to pass stool
• Hard stools
• Prolonged time to complete a
bowel movement
• A feeling of incomplete emptying
• Use appropriate laxatives.
(Stool softeners are often
insufcient to manage
constipation.)
• Review medications for
cause of constipation.
Preventing Avoidable Cognitive Decline
Residents who have cognitive impairment after a stroke are at risk of a
further decline in their ability to think and remember. Follow these strategies
to prevent an unnecessary cognitive decline:
• Ensure a regular review of medications as some can impair cognitive
functioning.
• Ensure the level of sound and visual stimulation is appropriate for the
resident’s ability to hear, see, and comprehend his or her environment.
• Provide needed environmental cues and reminders to maximize
orientation and function.
• Provide an appropriate level of social interaction, based on the resident’s
abilities and preferences.
• To promote and maintain independence, balance the assistance
you offer with the resident’s demonstrated needs. Excess disability
can result from performing tasks for a resident who can do them
independently or with less assistance.
• Provide simple one-step directions, if necessary.
• If the resident has a sudden onset of confusion, ensure an appropriate medical assessment to determine the underlying
cause of the delirium.

44
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 5
Preserving Skin Integrity
Residents who have had a stroke are at an increased risk of skin breakdown. The reduced ability to feel discomfort and
pain from pressure and/or a reduced ability to move to relieve pressure can contribute to skin breakdown. Interventions to
preserve skin integrity include:
Positioning
• Ensure good posture
• Avoid pressure on bony prominences
• Reposition regularly to relieve pressure areas
• Avoid friction, and shear during repositioning
Moisture
• Minimise incontinence with regular toileting
• Use protective barriers
• Moisturize dry skin with non-alcohol creams
Nutrition/Hydration
• Ensure adequate nutrition and hydration
Preventing Injuries
Injuries are common after a stroke because of the reduced ability to feel pain or discomfort, muscle weakness, neglect of
part of the body and impaired judgment due to cognitive decline.
• When transferring or repositioning in bed, always support the resident’s weak arm in an unweighted position.
• Avoid pulling the resident’s affected arm or leg during a transfer or when providing care.
• When the resident is sitting, ensure his or her weak arm has appropriate support.
• If a resident’s arm appears to be poorly supported when he or she is standing, consider a physical or occupational
therapy consult. A sling may be helpful for maintaining appropriate positioning.
• If a resident expresses pain or discomfort with the passive range of motion of a joint or if resistance is encountered,
stop the activity.
Preventing Falls
Residents able to move independently after a stroke may be at higher risk for falls and fall- related injuries. Many falls and
injuries due to falls can be prevented by recognizing risks for falls and putting strategies in place to reduce these risks. Refer
to the ABLE Care Planning Guide: Maintaining Mobility. (pending)
Managing Behavioural Symptoms
Behavioural symptoms are often a resident’s attempt to communicate unmet physical, social, psychological or medical
needs. Identifying a resident’s needs and understanding why a behaviour is occurring leads to appropriate management
and may prevent the need for medication. Refer to Responding to Behaviours Due to Dementia: ABLE Care Planning Guide.
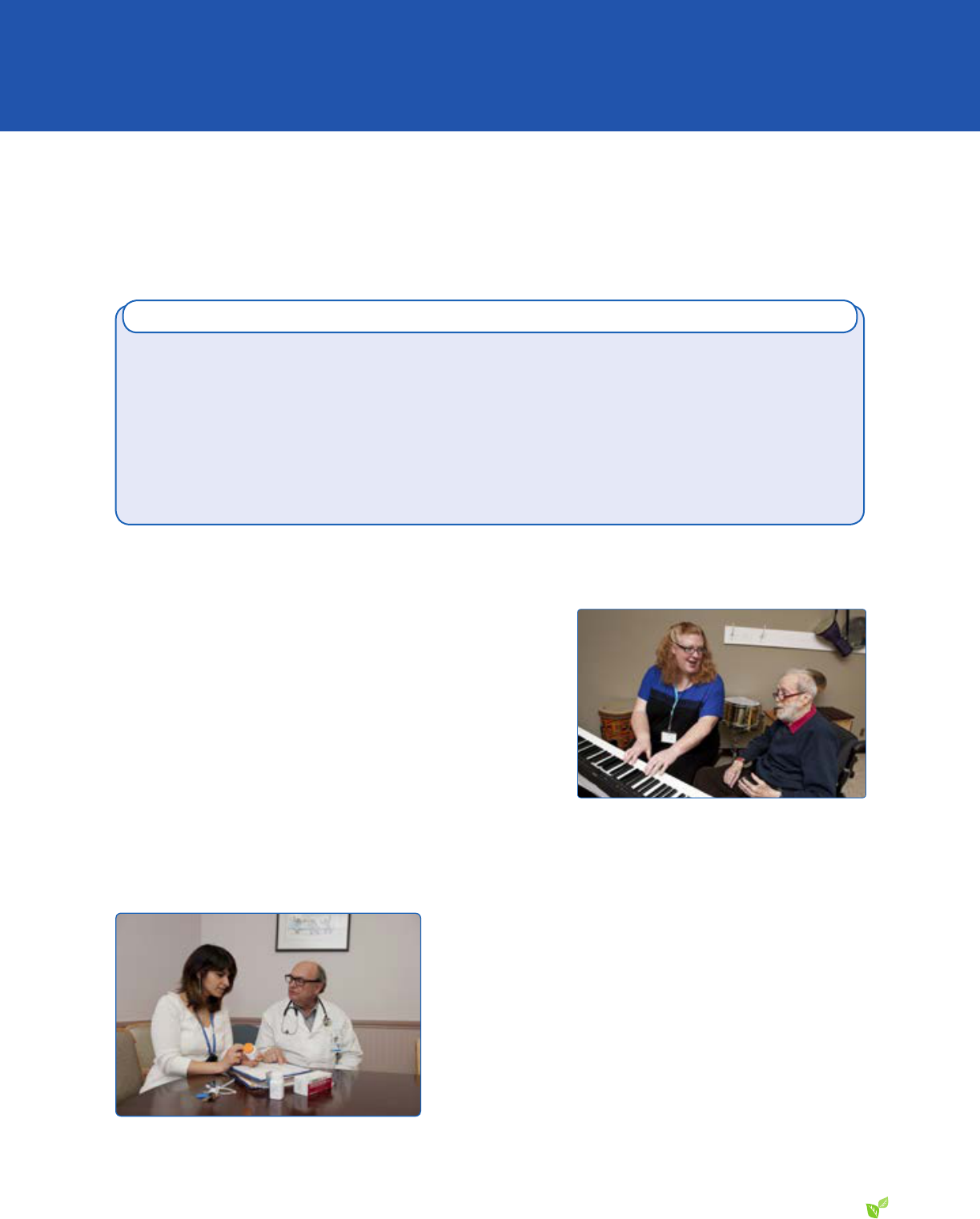
45
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Managing Depression and Social Isolation
Depression affects about a third of people who have had a stroke. Depression reduces energy, interest, motivation and
concentration and limits the individual’s ability to function and participate in desired activities. Recognize the signs of
depression early and offer appropriate treatment.
Symptoms of Depression:
• Reduced or increased sleep
• Decreased interest in usual activities
• Feeling guilty
• Less energy
• Reduced ability to concentrate
• Reduced appetite
• Moving more slowly than usual
• Showing signs of agitation
• Suicidal ideation
· Passive – not wanting to live anymore
· Active – wanting to harm self (seek immediate medical attention)
(The Cornell Scale for Depression can be used to screen for depression.
15
Interventions for Depression and Social Isolation:
• Encourage the resident to express his or her feelings and experiences.
• Ensure frequent contact with staff, volunteers and visitors, if possible.
• Encourage the resident to maintain as much control as possible over
his or her environment, activities and social interactions.
• Identify the resident’s present and past coping strategies, and then
encourage him or her to try them, if they’re effective and possible.
• Assist the resident in identifying new coping strategies.
• Assess, monitor, document and report to the physician any risk for self-harm. Include statements, behaviours, observed
helplessness, and concerns regarding the resident’s judgment and awareness of safety concerns.
Reducing the Risk of Recurrent Stroke
Once a person has a stroke, he or she is at risk of a recurrent stroke.
Drug therapies – including anti-platelet, anticoagulants and anti-
hypertensive medications – are often prescribed to prevent clotting and
treat underlying vascular risk factors. Other agents may be prescribed
to treat additional risk factors for stroke, such as high cholesterol, heart
disease and diabetes. In addition, exercise, diet and stroke education
can lower the risk of and/or prevent a stroke recurrence.
Look for the warning signs for stroke and respond immediately to
improve the resident’s survival and function
16
.

46
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 5
The Five Signs of Stroke
16
1. Weakness – Sudden loss of strength or sudden numbness in the face, arm or leg, even if temporary.
2. Trouble speaking – Sudden difculty speaking or understanding, or sudden confusion, even if temporary.
3. Vision problems – Sudden trouble with vision, even if temporary.
4. Headache – Sudden severe and unusual headache.
5. Dizziness – Sudden loss of balance, especially with any of the above signs.

47
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
MONITORING THE RESIDENT’S RESPONSE TO INTERVENTIONS
To ensure the desired life experience can be maintained, the inter-professional team needs to monitor all aspects of a
resident’s function on an ongoing basis.
Observational Measures to Evaluate Abilities and Function
Ability Regularly Assess
Communication
• The resident’s ability to communicate effectively with staff
• The staff’s ability to communicate effectively with the resident
• The resident’s ability to express his or her needs and wishes
Mobility
• The resident’s ability to achieve the mobility required for his or her desired life experiences
• The resident’s access to appropriate assistive technology and appropriate therapy
Activities of
Daily Living
• The resident’s ability to contribute to his or her basic ADL with minimal frustration
• The resident’s feelings about whether he or she has been able to achieve desired life
experiences
Meals
• The resident’s nutrition and hydration to ensure it’s adequate
• The resident’s ability to enjoy meals
Leisure
Activities
• The resident’s ability to engage in desired leisure activities
Psychosocial/
Spiritual
• The resident’s participation in social activities – such as outings, music therapy and lunch
groups – as tolerated and if willing
• The resident’s opinion of whether he or she is receiving adequate emotional and spiritual
support
COMPONENT 6

48
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
COMPONENT 6
Table 10: Tools for Monitoring Cognitive Abilities and Behaviours
Tool Purpose of Tool
Frequency of
Documentation
Duration
Recommended
Use
Canadian
Neurological Scale
17
To assess residents’
neurological status
Initial and as
appropriate
30 min • On admission
• When a new stroke
is suspected and
a more detailed
assessment is
desired
Mini-Mental State
Examination
(MMSE)
2
To assess and
monitor cognitive
function in residents
with moderate
cognitive loss
When changes in
memory and other
areas of cognitive
function are
suspected
10 min • On admission
• When moderate
cognitive impairment
is suspected
Montreal Cognitive
Assessment Battery
(MoCA)
3
To assess and
monitor cognitive
function in residents
with mild cognitive
loss
When changes in
memory and other
areas of cognitive
function are
suspected
10 to 15 min • On admission
• As necessary for mild
cognitive impairment
Resident Behaviour
Observation Record
Refer to Responding to Behaviours Due to Dementia: ABLE Care Planning Guide
Behaviour
Assessment Form
*Requires adequate vision and an ability to write to complete this test.

49
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
DEFINITIONS
ADL function:
Tasks that involve basic activities of daily living (ADL), including bathing, dressing, grooming,
toileting, transferring, eating, walking.
Affect:
Observable expressions of emotional feeling, tone and mood.
Aphagia (or dysphagia):
Difculty swallowing.
Aphasia:
A language disorder affecting a person’s ability to talk, read, write, understand.
Apraxia:
Inability to plan or execute movements.
Assistive devices:
Specialized equipment that can be used to assist with leisure pursuits, feeding, dressing,
grooming, other activities, and mobility.
Ataxia:
Inability to co-ordinate movements.
Cerebral infarction:
An area of necrosis (tissue death) in the brain due to the obstruction of a blood vessel
by a thrombus or embolus.
Cortical blindness:
Inability to see due to damage to the occipital lobe in the brain but with no damage to
visual structures.
Diplopia:
Double vision.
Dysarthria:
An impairment of the ability to make the sounds of speech clearly because of weakness
or lack of co-ordination. Words may be slurred or the voice may be weak.
Dysphagia (or aphagia):
Difculty swallowing.
Embolus:
A piece of clot originating outside the brain that breaks loose and travels through the
arteries to the brain. The clot may plug a small vessel, cutting off the blood supply.
Expressive aphasia:
Loss of the ability to produce language (spoken or written), usually due to a lesion in
the left temporal lobe. Ability to understand language is better than production. Most
common type of expressive aphasia is Broca’s.
Global aphasia:
Severe communication decit, resulting in an extremely limited ability to speak or
comprehend language. May result in being non-verbal and relying only on facial
expressions and gestures to communicate.
Hemiparesis:
Weakness / partial muscle loss one side of the body
Hemiplegia:
Complete paralysis of the arm, leg and trunk on one side of the body from damage to
the parts of the brain that control muscle movements.
Hemorrhagic stroke:
Occurs when a blood vessel in the brain leaks or ruptures.

50
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
DEFINITIONS
Ischemic stroke:
Occurs when a blood vessel (artery) supplying blood to the brain becomes blocked by
afatty deposit (plaque), or when blood clots develop within blood vessels in the brain,
An embolic stroke (a form of ischemic stroke) occurs when blood clots develop in the
heart or other part of the body, and then travel to the brain causing a stroke.
Neglect:
Inability to recognize or attend to the existence of the affected side of the body.
Paralysis:
Loss of voluntary movement as a result of damage to the nervous system.
Paresis:
Partial inability to move a body part or muscle weakness because of a disease of the
nervous system.
Perception:
How information is interpreted from the senses – sight, hearing, taste, touch, smell.
Proprioception:
Ability to know the position of the body in space.
Receptive aphasia:
A language disorder in which the individual is able to speak with normal grammar, syntax,
rate, intonation and stress, but language content is incorrect. May use the wrong words,
insert nonexistent words or randomly string together words. Ability to understand spoken
language and written material is also impaired. Most common type of receptive aphasia
is Wernicke’s.
Stimuli:
An agent or factor that causes an activity or a process to begin, increase or develop.
Stroke:
A sudden injury to the brain due to a blocked blood vessel (as in ischemic stroke) or a
bleed into the brain due to a ruptured blood vessel (as in hemorrhagic stroke).
Thrombus:
A blood clot that forms inside an artery in the brain or in the neck arteries, blocking
blood ow to the brain.
Tissue plasminogen
activator (t-PA):
A clot-busting drug used to reverse the detrimental effects of an ischemic stroke if
administered within 4.5 hours of symptom onset.
Transient ischemic
attack (TIA):
A small stroke, usually only lasting a few seconds.

51
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
APPENDICES
APPENDIX 1
UNDERSTANDING STROKE 52
APPENDIX 2
SAFE TRANSFERS 55
APPENDIX 3
ENSURING HYDRATION AND NUTRITION 57
APPENDIX 4
SUGGESTED POST-STROKE EXERCISES 60
Appendix 5
REFERENCES 63
APPENDICES

52
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
UNDERSTANDING STROKE
How the Location of a Stroke Affects Function
As in real estate, location, location, location is of utmost importance with stroke. The brain “real estate” affected by a stroke
determines the individual’s functional outcomes. However, a stroke never affects two people in exactly the same way.
The brain is divided into two sides: the left hemisphere and the right hemisphere. Each hemisphere is divided into four
regions, or lobes. Each lobe controls different functions. Despite the general division of functions between the sides and
lobes, there is variability from person to person. In addition, some functions are controlled by both sides of the brain. See
gure 3 to refer to the function controlled by each hemisphere.
APPENDIX 1
Tips and Tools for Everyday Living: A guide for stroke caregivers
Heart and Stroke Foundation
The brain is divided into two parts. These are called the left and right hemispheres. Each hemisphere
is divided into regions, which control different functions. The right side of the brain controls some
functions, the left others. Some functions are controlled by both sides of the brain.
The left hemisphere of the brain controls:
motor functions) and feeling
(sensory functions) of the right side of
the body
4 x(18)
y+2x
Left Hemisphere
Right Hand Left Hand
Music
Spacial
Orientation
Artistic
Functions
Art Awareness
Insight
Creativity
Reasoning
Written
Language
Scientific
Functions
Number
Skills
Spoken
Language
Right Hemisphere
1.2
The right hemisphere of the brain controls:
left
side of the body
and insight
sense of the surrounding environment
Figure 3: Hemispheres and Function
• Movement and feeling on the right side of the body
• Understanding written and spoken language
• Movement and feeling on the left side of the body
• Perception: being aware of, and making sense of
the surrounding environment
Adapted from Tips and Tools for Everyday Living: A Guide for Stroke Caregivers, Heart and Stroke Foundation of Ontario
8
.

53
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Canadian Stroke Network – Heart and Stroke Foundation of Canada (used with permission)
Functions of the Brain and Their Relation to Stroke
Structure/Circulation Key Functions Associated Dysfunction
Frontal Lobe
(emotions, motor, cognition, expressive
language)
Anterior Cerebral Artery (ACA)
Middle Cerebral Artery (MCA)
Voluntary motor function
Memory for habits and motor activities
Controls expressive language, articulating speech
(Broca’s Area)
Assigns meaning to words we choose
Behavioural spontaneity
Controls emotional responses
Executive Functions: task initiation, motivation, planning
and self-monitoring
Concentration/reasoning
Judgment/problem solving
Bladder control (micturation center)
Paralysis/paresis: of the face, arm and leg (MCA) or leg and foot (ACA)
Inability to express language (Broca’s Aphasia)
Emotional lability, mood changes
Impulsivity of thought, affect and action
Lack of spontaneity in interacting with others
Inability to attend to task
Inability to plan a sequence of complex tasks, i.e. making cof fee
Impaired judgment, problem-solving
Change in personality, sexual and social behaviour
Incontinence
Parietal Lobe
(Sensation and Perception,
Integration of Sensory Input)
Anterior Cerebral Artery
Middle Cerebral Artery
Posterior Cerebral Artery
Visual attention
Touch perception
Goal directed voluntary movements
Manipulation of objects
Integration of different sensory input
The ability to sense the position, location, orientation
and movement of the body and its parts
(Proprioception)
Difficulty focusing visual attention or attending to more than one object at a time
Loss of sensation
Difficulty with hand/eye coordination; distinguishing left and right
Inability to perceive objects normally (Agnosia)
Neglecting part of the body or space (contralateral neglect/dif ficulties with ADLs)
Difficulty reading, writing (Agraphia), drawing, constructing, naming objects,
calculating
Denial of deficits (Anosagnosia)
Provided as an educational service by Hoffmann-La Roche Limited
Registered Trade-Mark of Hoffmann-La Roche Limited
0420E05

54
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
APPENDIX 1
Functions of the Brain and Their Relation to Strok e (Continued)
Structure/Circulation Key Functions Associated Dysfunction
Temporal Lobe
(Auditory Sensation and Perception,
Memory, Language Comprehension, Affect)
Middle Cerebral Artery
Posterior Cerebral Artery
Hearing ability
Receptive language (Wernicke’s Area)
Integration of visual, auditory, somatic
information
Memory (storage, retrieval of words,
experiences)
Emotions
Impaired auditory sensation and perception
Difficulty recognizing faces
Difficulty selectively attending to auditory and visual input
Disturbed language comprehension, word recognition (Wernicke’s Aphasia)
Difficulty organizing verbal information
Short-term memory loss
Disturbance of long-term memory
Altered personality, emotional behaviour, sexual behaviour
Impulsiveness, aggressiveness, indifference, depression
Persistant talking
Occipital Lobe (Vision)
Posterior Cerebral Artery
Middle Cerebral Artery
Vision
Spatial organization and interpretation of
visual information
Visual reflexes
Defects in vision: visual field cuts, diplopia. (Hemianopia)
Inability to recognize familiar objects, words, colours, or movement of an object
(Agnosias)
Difficulty with reading and writing
Brainstem
(Body Functions and Movements)
(Midbrain, Pons, Medulla)
Basilar Artery
Vertebral Artery
Houses Cranial Nerves III-XII
1) Receives information from cranial
structures and controls muscles of the head
(Cranial Nerves)
2) Contains neural circuits that transmit information
from the spinal cord up to brain structures and
from brain down to spinal cord
3) Brainstem structures work together to regulate
arousal (reticular activating system)
4) Individually they subserve specific sensory
and motor functions
Midbrain (Visual/auditory reflexes)
Unable to move eye up, down or in
Inappropriate responses to visual or auditory stimuli
Pons (Blood pressure and respiratory regulation)
Altered respiratory function
Impaired chewing and facial sensation
Unable to move the eye out
Altered taste
Abnormal facial expression
Problems with equilibrium and hearing
Medulla (Blood pressure and respiratory regulation)
Altered respiratory, cardiac and blood pressure function
Altered sensation and limb weakness
Difficulty maintaining posture control
Swallowing problems
Unable to move head and shoulder, tongue
Altered salivation
Diencephalon
(Thalamus, Hypothalamus)
Posterior Cerebral Artery
Thalamus
Transmits information to cerebral hemispheres
for sensation and movement
Hypothalamus
Integrates the function of the autonomic nervous
system (maintains blood pressure, heart rate,
respiratory rate, temperature, fluid balance,
hormone synthesis, sleep-wakefulness)
Contralateral weakness
Contralateral sensory loss
Vertical and lateral gaze deficits
Hypersensitivity response to stimulus
Alteration in temperature regulation
Diabetes insipidus
Abnormal heart and respiratory patterns
Impaired blood sugar levels
Cerebellum (Motor Control)
Posterior Cerebral Artery
Basilar Artery
Vertebral Artery
Regulates movements of eyes and limbs;
helps maintain posture and balance
Coordinates voluntary movement, muscle
tone, balance and equilibrium
Control of fine motor movements
Limb and gait ataxia; impaired ability to walk
Difficulty judging distance, when to stop
Difficulty performing rapid alternating movements
Vertigo
Tremors
Loss of balance and coordination
Poor coordination of fine motor movements, weak muscles
Basal Ganglia
Middle Cerebral Artery
Production of dopamine and coordination of
muscle movement and posture
Loss of postural control
Tremor, rigidity, involuntary movements
References:
Hickey, JV. The clinical practice of neurological and neurosurgical nursing (4th ed.) Philidelphia: Lippincott, 1997.
Lehr, RP. Brain functions and map. Retrieved September 27, 2005, from www .neuroskills.com
Martin, JH. Neuroanatomy: Text and atlas. 2nd ed. Connecticut: Appleton and Lange, 1996.
Testani-Dufour, L.& Marano Morrison, CA. Brain attack: Correlative anatomy . J Neurosc Nurs 1997; 29:213-225.
This is a quick reference card for your use. The key functions of each area of the brain are highlighted.
Developed in 2005 by Rhonda McNicoll, Jana Lee Breton, Lisa Colizza, Hamilton Health Sciences and Linda Kelloway, Trillium Health Centre.
Canadian Stroke Network – Heart and Stroke Foundation of Canada (used with permission)

55
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
SAFE TRANSFERS
When assisting a resident to transfer, ensure the resident’s
safety and comfort, and promote the resident’s highest level of
independence. If you are unsure of how to transfer or experience
difculty in assisting, seek the advice and assistance of your
physiotherapist.
Before you start the transfer, speak with the resident to ensure
he or she understands what you are about to do and how you
are going to assist him / her. Move slowly and gently, never pull
on the resident’s affected arm or under the shoulders, and do not
lift the resident. Instead, encourage the resident to participate as
much as possible. Employ a problem-solving approach to transfers. If the transfer requires two staff members, communicate
clearly with each other as well as with the resident to ensure a co-ordinated effort.
General Principles of a Safe Transfer:
To assess if a person is able to transfer without the mechanical lift, the resident must be able to:
• Lift and hold limb up in the air against gravity.
• Mobilize in bed with minimal to moderate assistance
• Go from a supine to a sitting position with minimal to moderate assistance
• Demonstrate good trunk control when they are sitting at the edge of the bed (can sit with supervision or minimal assistance)
If a person cannot do any of these movements well, a mechanical lift is suggested until they become much stronger. Be
exible with the resident’s method of transfer as resident’s abilities may uctuate depending on fatigue. See STABLE Algorithm
below to reduce your risk of injury.
Cognition is also an important factor. The resident must be able to follow simple directions to ensure a safe transfer.
STABLE Algorithm for Safe Transfers and Ensuring Good Body Mechanics
18
S
Maintain in the natural curves of your spine
T
Avoid Trunk twisting
A
Keep your Arms close to your body
B
Maintain a wide Base of support
L
Use your Legs, weight shift
E
Evaluate the Environment (load, abilities, limitations)
APPENDIX 2
56
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
APPENDIX 2
Using a Mechanical Lifting Device
Lifting devices such as the Hoyer, ceiling lift do not promote functional recovery and are discouraged for residents who
have had a stroke. However, if the resident is unable to roll or otherwise get to the edge of the bed or cannot assist with
the transfer, it may be necessary to use a lifting device. When using the device, ensure that the affected arm is positioned
inside the sling. Never let the affected arm hang outside the sling. Also, once resident is sitting in the chair, try to remove
the sling from under them to avoid skin breakdown.
DO’s DON’Ts
• Review chart/care plan regarding transfer abilities
• Assess resident’s:
· Cognition: co-operative and following instructions
· Strength, Endurance & Balance: ability to lift limbs
against gravity, sit on edge of bed, lean forward, stand
and take step
• Do not pull on the resident’s affected limb
• Do not let the affected limb hang provide support
to the limb or assess the need for a sling
• Avoid holding/pulling on resident’s clothing
• Do not block resident’s direction of movement
• Transfer resident towards their strong (unaffected) side.
Rearrange furniture as needed.
• Set up equipment appropriately prior to transfer:
· Position wheelchair at a slight angle to the bed
· Remove foot plates/armrests of the side closest to
the bed
· Lock brakes of wheelchair
· Set up equipment if needed i.e. sliding board, walker,
etc.
· Adjust the height of the bed so that the resident is
transferring from a high position to a lower position
• Communicate with your partner/resident throughout the
transfer process
• Use good body mechanics when transferring
• Liaise with physiotherapy if there are any concerns
• Do not lift the resident the resident should be
assisting with all movements
• Do not transfer resident if he/she is not able to
follow your directions
• Do not transfer resident if you need maximum
assistance for any mobility use mechanical lift
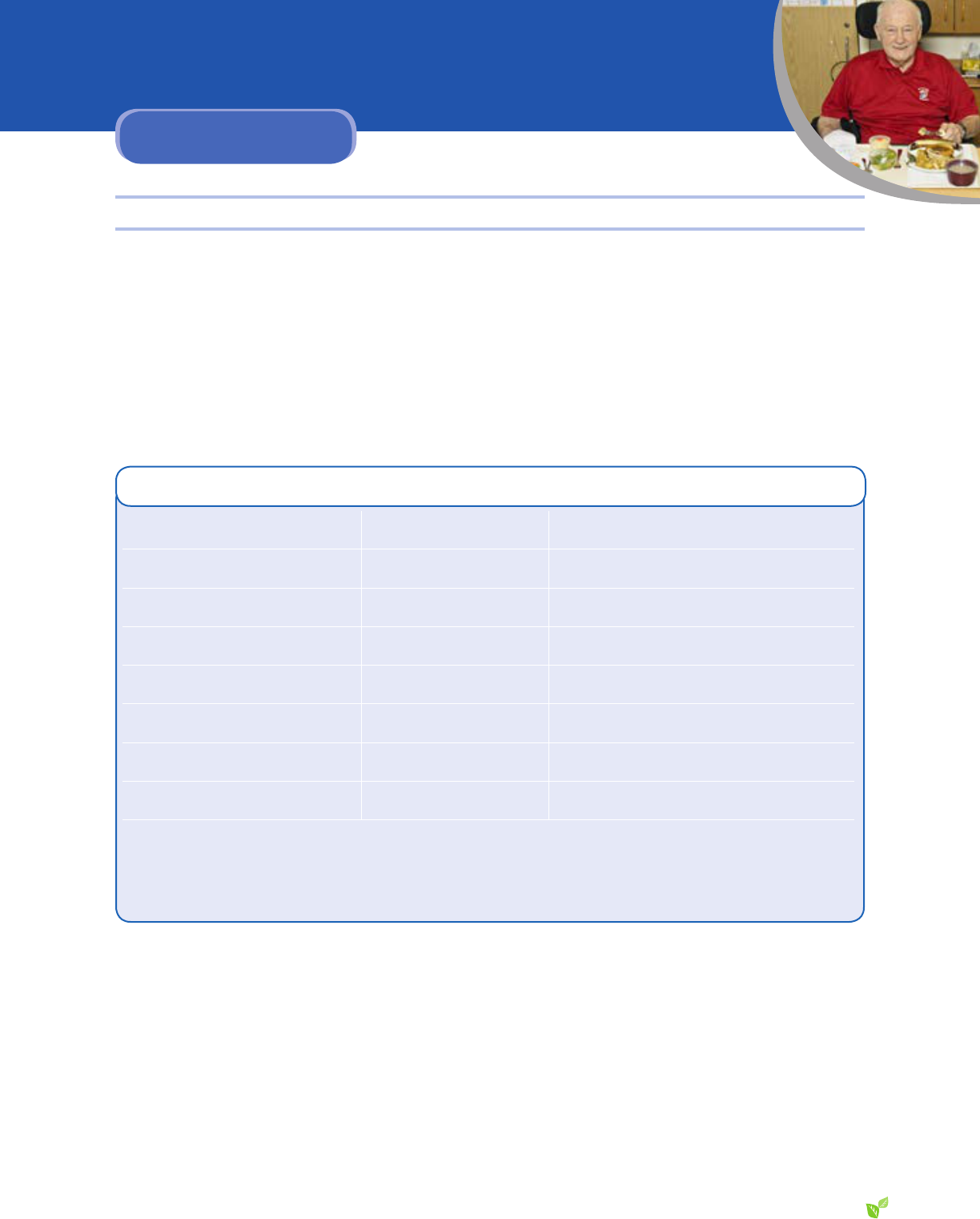
57
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
ENSURING HYDRATION AND NUTRITION
Fluid Requirements
Most people need about 1-½ to 2 litres (6 to 8 cups) of uid per day. Take the time to nd out what types of juice, milk and
other drinks the resident prefers. Frozen juice bars, Popsicles, Jell-O, pudding, ice cream, soup, meal supplements (such
as Ensure and Boost) and puréed fruit contain liquid to contribute to the resident’s uid intake.
Before offering any of these foods, though, ensure the resident can have them. If the resident has a swallowing problem,
contact the speech-language pathologist to determine the appropriate liquid consistency and best-tolerated food items.
Estimated Fluid Content of Common Foods
Food Serving Size
Fluid Provided
Jell-O ½ cup or 125 mL 105 mL
Pudding (vanilla, chocolate) 85 g 56 mL
Ice cream 100 mL 34 mL
Sherbet 100 ml 50 mil
Yogurt 100 g 75 mL
Puréed fruit 125 mL 108 mL
Cream soup 120 mL 107 mL
Juice or milk 125 mL 109 mL
½ cup = 125 mL
1 cup = 250 mL
1 litre = 4 cups = 1,000 mL
2 litres = 8 cups = 2,000 mL
APPENDIX 3

58
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
APPENDIX 3
Food Textures
All residents need a recommended selection from the food texture list and a recommended selection from the liquid texture list.
Name of the
Modied Texture
Diet
Standard used
to assess
Examples from
the SHSC menu
Examples
of items not
included
Regular
• no restriction • roast beef
• raw vegetables & hard fruits
• chewy bread (e.g. bagels, crusty
buns)
• pineapple, grapes, wieners,
sausages
• all salads
Mechanical Soft
(“soft solids”)
• all foods are soft
and easily cut with
a metal fork in the
middle and the
edges
• food texture
combinations
allowed (e.g.
fruit salad plate,
casseroles)
• Salisbury steak, chicken ngers
• Mixed consistencies in foods:
stews, casseroles, pastas, pies,
etc
• Breads, soft sandwiches
• Canned fruit, orange sections
• All sh, tuna, egg, salmon salad
llings
• All eggs and cheese
• Most cakes and pies (no nuts or
seeds)
• No toast, hard
buns
• No green salads
• no encased meats
(e.g. sausage,
wieners)
• no hard cookies
• no foods with
skins (corn, peas)
• no nuts or seeds
Minced
(This food is ground up into
very small bits, and is moist
and soft, requiring very
little chewing before it is
swallowed)
• must be moist, soft-
textured and easily
formed into a bolus
• minimal variation in
texture
• meats are ground or minced into
small pieces and moistened
• soft, minced vegetables and fruit
• salad llings (e.g. tuna salad), not
containing hard bits
• oatmeal, cottage cheese
• scrambled eggs
• no bread
• no mixed
consistencies (e.g.
vegetable soup)
• no dry foods
Puréed
(All food is a uniform smooth
texture with no lumps or
hard bits, which does not
need to be chewed before it
is swallowed)
• uniform smooth
texture
• no lumps, hard bits
• drops off a spoon
• yogurt, custards, puddings
• puréed meat and vegetables
• cream of wheat
• no oatmeal
• no heavy or sticky
purees
• no seeds or fruit in
yogurt

59
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Liquid Consistencies
Diet Standard Description of Texture Avoid
Regular
• no restrictions • any thin liquid tolerated
Thin, no mixed
consistencies
• avoid foods mixed with
liquids or served in a
liquid
• water, tea, coffee, juice
• broth, bouillon, cream soups
• milk, creamer, milkshakes
• powders mixed into drinks (e.g.:
instant hot chocolate or instant
breakfast)
• strained canned fruit
• ice cream & sorbet
• popsicles, ice, Resource or
other liquid supplements
• fruit served in juice
• soups with small bits of solid
food (e.g. chicken noodle,
vegetable soup, lentil soup)
• soupy stews
• dry cereal (served with milk)
• juicy fruits (e.g. orange
sections)
Nectar-thick
(green box)
• Must open the box
and pour it into a
cup or use with a
straw
• may drink with a wide
straw
• Resource Nectar-thick products
(milk, water, juices)
• strained cream soups
• ice cream & sorbet (melts to a
nectar-thick consistency)
• cold tomato juice or V8
• Resource mixed equally with
honey-thick milk to form a
nectar-thick drink
• all liquids from ‘no mixed
consistency’ category
• Resource liquid supplements
Honey-thick
(purple box)
• Must be sipped from a
cup (no straws)
• Resource Honey-thick products
(milk, water, juices)
• All fruit purées
• Extra-thick cream soups
• all liquids from the ‘no mixed’
and ‘nectar-thick’ categories
• most cream soups
• Jell-O, ice cream & sorbet
• Milk in hot cereal requires
individual assessment by SLP
Pudding-thick • Must open the
container and use a
spoon
• Thickened to a solid
level – eaten with a
spoon
• extra-thick juices
• fruit purées
• all liquids from the ‘no
mixed’, ‘nectar’, and ‘honey’
categories
• thin purées
• milk mixed in hot cereals
• Jell-O requires individual
assessment by SLP
Fruit purée
• Must open the
container and use a
spoon
• fruit purées (apple, pear, peach,
etc)
• all thickened uids
• all of the above

60
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
SUGGESTED POST-STROKE EXERCISES
Exercises can be done either in a seated or lying position.
Choose at least 2 exercises from each group. To perform these exercises, the resident should be able to sit independently
in a chair or locked wheelchair. If possible, the resident’s feet should be at on the oor.
Exercises
1
Instructions
Head Turns
• Look over the right shoulder, count to 5.
• Look over the left shoulder, count to 5.
• Repeat the sequence 5 times.
Head Tilts
• While looking forward, tilt the head to the right shoulder, count to 5.
• While looking forward, tilt the head to the left shoulder, count to 5.
• Repeat the sequence 5 times.
I Don’t Know
• Look forward and shrug the shoulders up to the ears, count to 5.
• Lower the shoulders to the starting position, count to 5.
• Repeat the sequence 5 times.
Shoulder Rolls
• Look forward, roll both shoulders forward; repeat 5 times.
• Look forward, roll both shoulders backward; repeat 5 times.
Airplanes
• Hold onto a stable surface with the right hand.
• Lift the left arm straight out to the front.
• Circle the left arm 5 times to the right and 5 times to the left.
• Return the arm to the side.
• Repeat the sequence using the right arm.
Modication: If the resident is able, he or she can do this exercise with both arms at the
same time.
Check Those Toes
• Lift the toes up while keeping heels touching the oor, count to 5.
• Lower the toes to the oor.
• Repeat up to 10 times.
APPENDIX 4

61
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
Exercises
1
Instructions
Show Those Toes
• While keeping the left foot on the oor, lift the right foot until the right knee is as
straight as possible.
• Point the toes forward, and then ex the toes back.
• Repeat 10 times.
• Lower the foot to the oor.
• Repeat the sequence using the left foot.
or
• Circle the right foot clockwise 5 times.
• Circle the right foot counterclockwise 5 times.
• Lower the foot to the oor.
• Repeat the sequence using the left foot.
Caution: This exercise may not be suitable for residents who have had a hip
replacement or who have severe degeneration of the hip joint.
Popeye Exercise
• Hold the right arm straight down at the side.
• Keep the elbow glued to the waist.
• Face the palm forward.
• Bend the elbow.
• Lift the palm up to the shoulder.
• Return to the starting position.
• Repeat up to 10 times.
• Switch to the left arm and repeat up to 10 times.
Advanced level: Hold a weight in each hand or use an elastic exercise band.
Hugs
• Hold slightly bent arms horizontally out to the side.
• Face the palms towards each other.
• Bring the arms in towards the centre and give yourself a hug, count to 5.
• Open the arms out to the side, keeping them slightly bent.
• Repeat the sequence up to 10 times.
Advanced level: Hold a weight in each hand.

62
continued
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
APPENDIX 4
Exercises
1
Instructions
Fly Away Wings
• Hold both arms straight down at the sides with palms facing the thighs.
• Raise both arms out to the sides.
• Stop at shoulder height, count to 5.
• Lower to the starting position.
• Repeat the sequence up to 10 times.
Advanced level: Hold a weight in each hand.
Scrub the Countertop
• Hold the arms as straight as possible out front with the palms facing down.
• Keep the elbows at shoulder height as you pull the hands towards the chest.
• Straighten the arms as you return to the starting position.
• Repeat up to 10 times.
Advanced level: Hold a weight in each hand or use an elastic exercise band anchored
behind the chair.
Bring in the Band
• Lift the knees one after the other (right, left, right, left) as if marching.
• Work up to 60 without stopping. (Each knee lift counts as 1.)
Dance Away the Night
• Begin with the knees and feet as close together as possible.
• Lift the left knee about ½ inch.
• Move the left leg 5 to 6 inches out to the left side.
• Return to the starting position.
• Repeat up to 10 times.
• Repeat the sequence using the right leg.
Advanced level: Attach a weight to each ankle.
Sitting Ballet
• Lift both heels 1 to 3 inches off the oor, count to 5.
• Lower both heels to the oor.
• Repeat up to 10 times.

63
© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
APPENDIX 5
REFERENCES
1. Resnick B. Restorative care nursing for older adults: A guide for all care settings. (2004) New York: Springer Publishing.
2. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients
for the clinician. (1975) J Psychiatr Res. Nov 12(3): 189-98.
3. Nasreddine Z. The Montreal Cognitive Assessment. (2003) www.mocatest.org.
4. Niemeier JP, Cifu DX, Kishore R. The Lighthouse Strategy: Improving the Functional Status of Patients with Unilateral
Neglect After Stroke and Brain Injury Using a Visual Imagery Intervention. (2001 )Topics in Stroke Rehabilitation. Summer;
8(2): 10-8.
5. Perlman, AL, Schulze-Delrieu, K. (Eds.) Deglutition and its Disorders; Anatomy, Physiology, Clinical Diagnosis, and
Management. (2003) NY: Thomson Delmar Learning.
6. Teasell R, Foley N, Bhogal SK, Salter K. Management of Post-Stroke Pain. EBRSR: Evidence-based review of stroke
rehabilitation. (2011) www.ebrsr.com/~ebrsr/uploads/Appendix-Pain.pd
7. Teasell R, Foley N, Bhogal SK, Salter K. The painful hemiplegic shoulder. EBRSR: Evidence-based review of stroke
rehabilitation. (2011) www.ebrsr.com/uploads/Module-11 hemiplegic-shoulder001.pdf
8. Heart & Stroke Foundation of Canada. Tips & Tools for Everyday Living: a Guide for Stroke Caregivers. (2010)
9. Gray ML. Urinary & Fecal Incontinence: Current Management Concepts. In DB Doughty (Ed.): Physiology of voiding,
3rd edition. (2006) St Louis MI: Mosby Elsevier.
10. Sakakibara R, Hatton T, Yasuda K, Yamanishi T. Micturitional disturbance after acute hemispheric stroke: analysis of
the lesion site by CT and MRI. (1996) J Neurol Sci. 137(1): 47-56. 1996.
11. Burgio KL. Current perspectives on management of urgency using bladder and behavioral training. (2004) J Am Acad
Nurse Pract. 16(10 Suppl.): 4-7.
12. Chen YC, Liao YM, Kuo HC. Lower urinary tract dysfunction in stroke patients. (2007) JTUA. 18(3):147-150.
13. Dumoulin C, Korner-Bitensky N, Tannenbaum C. Urinary incontinence after stroke: Does rehabilitation make a difference?
A systematic review of the effectiveness of behavioral therapy. (2005) Topics in Stroke Rehabilitation. 12(3):66-76.
14. RNAO Best Practice Guideline. Prevention of constipation in the older adult population. (2011)
15. Alexopoulos GA, Abrams RC, Young RC, Shamoian CA: Cornell scale for depression in dementia. (1988) Biol Psych.
23:27-284.
16. Heart & Stroke Foundation of Canada. www.heartandstroke.on.ca
17. Cote R, Hachinski V, Shurvell B, Norris J,Wolfson C. The Canadian Neurological Scale: A Preliminary Study in Acute
Stroke. (1986) Stroke 17:731-737.
18. Work Readiness Program, Gorge Road Hospital, Victoria, BC. The STABLE Body Mechanics Approach. (1996).
http://www.worksafebc.com/about_us/history/historical_reports/nding_solutions/assets/pdf/96FS-05manual.pdf

© 2012, Sunnybrook Health Sciences Centre | Veterans Centre. All rights reserved.
Restoring Abilities After a Stroke using Achieving Best Life Experience (ABLE) Care Planning Guide
2012
Sunn
ybrook
VETERANS
PR 13030 (Dec. 2012)
