
Self-Care Social Prescribing
Kensington & Chelsea Social Council and
NHS West London Clinical Commissioning Group
January 2018
Social Return on Investment

This report was prepared by Envoy Partnership,
an advisor in evidence-based research and
strategic communications. We specialise in
measuring and demonstrating the value of social,
economic and environmental impacts. We are
dedicated to providing organisations, stakeholders,
investors and policy makers with the most holistic
and robust evaluation tools with which to enhance
their decision-making, performance management
and operating practices.
‘ All good GPs understand that healthcare and wellbeing
is made up of physical, psychological and social
problems. Providing holistic care involves all these
elements...however if somebody’s prime issue is
loneliness [or social isolation], it’s much better
that they’re NOT seeing a GP but getting support
from other parts of the community and other parts of
the system.
In the [consultation] room, all the time I’m
suggesting to [older] patients: charities, local
health groups, support groups; things they can join
and make them feel valued, worthwhile, and important
members of society.
I wasn’t trained to give social care advice, I was trained
to do medicine, but we care about our patients and want
to give holistic all-round care’
Dame Helen Stokes-Lampard
Chair of the Royal College of General Practitioners
12 October 2017, BBC News

1Social Return on Investment
Acknowledgements
Executive summary
Background
Services available through social prescribing
Impact evaluation objectives and method
Findings: Patients
Findings: Valuing the utility of patient health
and wellbeing outcomes
Findings: Health and Care system
Findings: Working with VCS providers
Programme fit in the local system
Recommendations
Appendices
Contents
1.
2.
3.
4.
5.
6.
7.
8.
9.
2
3
7
10
13
16
24
27
34
37
38
40
Self-Care
Social Prescribing
Kensington & Chelsea Social Council and
NHS West London Clinical Commissioning Group
Social Return on Investment

Self-Care Social Prescribing2
We would like to thank the voluntary and community service providers from the
pilot phase, frontline staff and volunteers who supported our research and helped
to arrange interviews, group observations, and surveys with their service users,
in particular: Action Disability Kensington & Chelsea (ADKC) in conjunction with
Life in Balance, Age UK, Citizens Advice Bureau (CAB) Westminster, Chinese
National Healthy Living Centre, Healthier Life 4 You (now Healthier Divas),
Metrosexual Health & Wellbeing Community Interest Company (MHW CIC),
Open Age, Resonate Arts (formerly Westminster Arts), and the Venture
Community Association.
We also wish to the thank the Case Managers, Health and Social Care Assistants,
and Dr Oisin Brannick (lead GP for West London Clinical Commissioning Group
(WLCCG) Social Prescribing) for the valuable information and insight provided for
our research.
We are very grateful to the members of the local Transformation Steering Group for
aiding our understanding of how the social prescribing model fits with local authority
objectives for the health and wellbeing of older people.
Our thanks also go to Dr Susan Procter at Buckinghamshire New University, who
was a valuable sounding board, and facilitated access to acute hospitalisation data.
Our research would not have been possible without the involvement of the
Kensington and Chelsea Social Council team, and input from Kalwant Sahota
and Henry Leak and colleagues at West London Clinical Commissioning Group,
to whom we are extremely grateful for their time and energy.
Finally, our greatest thanks go to the patients and service users. We feel privileged
to have been welcomed into their homes and lives, and for them to have shared
their experiences, feedback, and stories with us, often under very difficult
personal circumstances.
Acknowledgements

3Social Return on Investment
Health and social care services in North and
West London are building positive new models
of cross-sector working to make better use of
joined-up resources. Such cultural and operational
change is needed to improve choices available
for patients, and to support professionals to go
beyond the medical model alone. The status quo
is not sustainable, given our ageing population
and the growing prevalence of long-term life
limiting illnesses.
In West London, a frail older patient can take
up an average of 30 GP practice visits per year,
over 12 days in hospital per spell, and 8 visits to
outpatient clinics annually. Many older patients are
at risk of being increasingly isolated, housebound,
and are suffering from poor social and emotional
wellbeing. This further amplifies the problems with
their existing health conditions and can lead to
more rapid deterioration. However, treating such
non-medical drivers of poor health and wellbeing
are not the conventional domain of doctors, nurses,
and other clinical professionals.
The Self-Care social prescribing model enables
GP practice staff to refer patients with a non-
medical health and wellbeing need onto appropriate
specialist services from the voluntary and
community sector (VCS). Patients are provided
with a personal consultation with a Case Manager
or Heath and Social Care Assistant at their GP
practice, to identify their needs, interests, and
goals. One option available is for the patient to be
prescribed a service on the Self-Care directory.
Patients are contacted by the service provider
within a week to arrange their sessions and work on
their progression. The general aim of Self-Care is
to increase patient confidence in making informed
decisions about their health, and increase lifestyle
changes and new healthy habits, through accessing
more community-based support sessions. The
Self-Care social prescribing model has led to
reduced avoidable need for hospitalisations,
reduced need for GP practice hours, and
reduced levels of physical pain and depression
for patients.
This Self-Care social prescribing model and
directory of services is managed by Kensington
and Chelsea Social Council (KCSC) on behalf
of West London Clinical Commissioning Group
(WLCCG). The model forms part of WLCCG’s
integrated ‘My Care, My Way’ (MCMW)
programme, which places over-65s at the heart of
a personalised and holistic care and support plan.
Envoy Partnership were commissioned to conduct
research to evaluate the impact of this model and
include a Social Return on Investment (SROI)
analysis. This is detailed comprehensively in the
main report, which describes the total SROI value
created when compared with the annual contract
budget of £250,000. The results are as follows:
Executive
summary
£2.80 of social
value created
per
£1 invested
£

Self-Care Social Prescribing4
Executive summary
The Self Care model reached around 800 frail older
patients in the pilot year and is forecasted to reach
around 1300 patients in the year to March 2018.
Patient impacts observed from the research include:
• Reduced physical pain and discomfort
• Reduced depression and severe anxiety
• Reduced levels of loneliness and social isolation
• Improved self-confidence/self-worth
• Improved sense of health equality i.e. feeling
valued the same as other people by care services
• Maintained independence and dignity, especially
when enabled to access income support
• Reduced avoidable need for entering primary
and secondary care
Total attributable worth (or ‘utility’) to patients
of these impacts is valued at £278,400 for the
pilot year to March 2017. Patients receive six
sessions, with an option for re-referral for another
six sessions, sometimes with a different related
service. Through patient surveys (see Table A)
we observed an increase in the proportions of
patients who feel: i) No pain or little pain (+24%),
ii) No feelings of being down or depressed (+17%),
and iii) No feelings of anxiety (+14%).
Table A. Patient survey responses regarding
health status outcomes resulting from social
prescribing (based on the short EQ5-d and
PHQ9 surveys, N=134)
Resource value to health services
The social prescribing model has also led to
resource savings to GP practice staff - including
Health and Social Care Assistants (HSCAs) and
Case Managers – valued at £102,000 for the
pilot year (April ‘16-March ‘17) and forecasted at
£150,000 to March 2018. Resource savings for
hospitals are valued at £106,000 for the pilot
year and forecasted at £154,000 to March 2018
(see Table B). This is calculated for acute episodes,
by drawing on improved Patient Activation Measure
(PAM) scores. PAMs are recorded by GP staff with
patients, at different points in time.
YEAR END TO MARCH 2018 –
FORECASTED ‘SROI’
• c.£6.25 for every £1 invested, including
health service value (c.£1.22) and patient
health and well-being value (c.£5.03).
• After accounting for the attribution due to other
factors, the ‘attributable’ SROI is c. £2.80.
% of Patients
responding Before After Change
Little or No pain 15% 39% +24%
No feelings of
being depressed
30% 47% +17%
No feelings of anxiety 29% 43% +14%
PILOT YEAR TO MARCH 2017 – ‘SROI’
• c.£4.30 of value is created for every £1
invested, including health service resource
value (c.£0.85) and patient health and well-
being value (c.£3.45).
• After accounting for the contribution of
other factors that affect patients’ health and
wellbeing outcomes (the attribution), c.£1.90
of attributable value was created for
every £1 invested.

5Social Return on Investment
According to the PAM scoring system
1
used by
WLCCG, an improvement by one-point correlates
to 2% reduced hospitalisation likelihood. Around
62% showed an improvement from our sample.
The average improvement for those 62% was 5.8
points. Therefore, one of the areas of resource
savings indicated by the improvement in patient
activation would be an average 11.6% rate of
reduced hospitalisations, for the relevant proportion
of patients who improved.
Table B presents avoidable demand and resource
value to local health services, at GP practice level
and hospital level, with hospital estimates linked to
the PAM score for the proportion of patients who
showed improvement. Patient utility was valued
separately using a QALY approach.
Table B. Resource value to health services (from 24 GP practices, values rounded to
nearest 1000)
Areas of resource saving
Total
reduction
Pilot year
to Mar 2017
Equivalent
consult’ns
per practice
Pilot year
Total Value
Pilot year
to Mar
2017
Total Value
forecast
YE to Mar
2018
Average
incidence per
patient per
year, MCMW
GP Practice level total £102,000 £150,000
Diverted GP hours: initial
consultations (w/ re-referral)
340 hours 57 £18,000 £27,000
30 GP
practice visits
per patient
Diverted HSCA & CM
research/support hours: initial
consultations (w/ re-referral)
1025 hours 171 £21,000 £31,000
Avoided GP hours from patients
stopping need for consultations
(6-month period)
590 hours 98 £32,000 £46,000
Avoided HSCA & Case
Manager hours from patients
stopping need for consultations
(6-month period)
1480 hours 247 £31,000 £46,000
Hospital level total £106,000 £154,000
Reduced need for Hospital spells
51
incidences
n/a £68,000 £99,000
1.19 episodes
@12 bed days
Reduced need for A & E
54
incidences
n/a £6,000 £9,000 1.23 episodes
Reduced need for
Outpatient visits
579
incidences
n/a £32,000 £46,000 8 episodes
1
Licensed by NHS services from the US company, Insignia Health
c.11.5%
reduced
hospitalisations
1300 patients
reached in 2018

Self-Care Social Prescribing6
Key strengths of the model identified in our
research are that:
• The Self-Care offer enables agile and flexible
commissioning, whilst supporting some frontline
administrative functions.
• GP practices and patients are able to reach more
VCS services appropriate to their needs (and thus
work more effectively with their time).
• Management of the model by an accountable
VCS umbrella organisation. such as KCSC,
generates trust between providers, health
services, patients, and other statutory
stakeholders.
• It can foster cross-sector collaboration to better
join-up resources and access capacity.
• There are significant contributions to patient
wellbeing, motivation/activation, and confidence.
• Resource savings are created for care services,
especially reduced hospitalisations, and GP
time and Case Manager time spent on care co-
ordination, planning, and research.
Recommendations for the model are focused on:
• The need to improve feedback about patient
progression into Care Plans, through better
integration of information between two different
software systems used by WLCCG and KCSC.
• Expanding services to less frail patients therefore
supporting a preventive approach.
• Increasing initial number of sessions, whilst
reducing the need for re-referrals.
• Building the profile of the model and building
confidence more widely amongst professionals.
• Improving compliance and guidance, regarding
Quality standards and Information adequacy.
• Ensuring service providers and health
professionals meet their responsibility to
collectively improve learning and share
best practices.
Executive summary

7Social Return on Investment
Kensington and Chelsea Social Council (KCSC)
is operating a social prescribing model, known
as Self-Care, on behalf of West London Clinical
Commissioning Group (WLCCG). The Self-Care
model links patients in primary care with sources
of health and wellbeing support from specialist
voluntary and community services. The Self-Care
programme is targeted at patients aged 65+ with
long-term conditions. It provides GP practices in
Kensington and Chelsea and the Queens Park
and Paddington areas of Westminster with a
non-medical referral option.
The Self-Care social prescribing model is part of
the ‘Whole-Systems’ initiative, which is a cross-
sector network of commissioning authorities
across health care, social care, and other statutory
support. Self-Care currently operates within the
larger integrated ‘My Care, My Way’ (MCMW)
programme, which places over-65s at the heart of
a personalised and holistic care and support plan.
The aim of the Self-Care approach is to increase
patient confidence in making informed decisions
about their health. Simple lifestyle changes and
new healthy habits and goals are encouraged.
Consequently, Self-Care is expected to positively
contribute to patients’ confidence and motivation,
which in turn is expected to contribute towards a
long-term reduction in use of primary, secondary,
and some tertiary services.
It was originally planned that only patients in Tiers 2
and 3 (as described below) would receive Self-Care
services. This was later expanded to Tier 1 patients.
The Tiers of patients are defined as follows:
The key aspect of Self-Care social prescribing
is that it focuses on provision of services
and activities to patients by Voluntary and
Community Sector (VCS) organisations who
specialise in providing health and wellbeing
services to older residents.
Rationale for developing the
Self-Care model
Self-Care was created to offer a range of broader
benefits for anyone aged 65 or over, including:
1. Background
Tier 0: +65 years of age and are mostly healthy.
Tier 1: +65 years of age and have one well-
managed Long-Term Condition (LTC).
Tier 2: +65 years of age and have two LTCs,
mental health or social care needs.
Tier 3: +65 years of age and have three or
more LTCs, mental health or social
care needs.

Self-Care Social Prescribing8
• More time – patients have longer
appointments with their GP practice (as their
appointments can also be with non-GP staff).
This helps GPs to focus their time on medical
rather than non-medical factors affecting health
and wellbeing.
• More support – access to a broader range of
health and social care professionals to support
health and wellbeing.
• More help – through creating integrated care
centres that can offer a wide range of services
under one roof – including diabetes clinics,
pharmacists and social care services
(such as St Charles Integrated Care Centre).
• More choice – patients are offered local activities
to support them in looking after their own
physical, social, and emotional wellbeing.
(adapted from WLCCG service specification for Self-Care 2015)
Self-Care social prescribing model
The Self-Care referral process is conducted in
three main steps, as part of the My Care, My Way
offer to older patients:
After assessing and agreeing the patient’s needs
and choices, Case Managers or HSCAs refer
the patient via KCSC to one of the Self-Care
services or activities. KCSC receives the referral
and notifies the provider, who in turn contacts
the patient and arranges to deliver the activity or
service. KCSC have no direct contact with any
patients, and act as a bridge between the VCS
providers and practice-based staff who have
responsibility for patient contact. The graphic in
Figure 1 illustrates the pathway of how the six
sessions are prescribed within My Care, My Way.
With the innovative approach to working in
partnership, HSCA’s are employed by Age UK K&C
and Senior Case Managers and Case Managers are
employed by Central London Community Healthcare
NHS Trust (CLCH). HSCA’s are line managed by
SCM’s or CM’s, CM’s are line managed by the
SCM’s and the SCM’s are line managed by the
Clinical Business Unit manager in CLCH.
As part of a collaborative approach to managing
both clinical staff and non-clinical frontline staff,
HSCAs are line-managed by the local Age UK in
Kensington & Chelsea, whilst Case Managers are
line managed by WLCCG
1. Background
Step 1. Patient is allocated to a practice-based Health and Social Care Assistant (HSCA) or Case
Manager (CM)
Step 2. Patient assessment conducted by HSCA or Case Manager, which includes:
- Recording of a Patient Activation Measure (PAM) on ‘SystmOne’ software
- Recording of goals for the patient’s Care Plan
- Completion of referral form with patient’s requirements and notes on their situation
- Direct referral to an appropriate service from the Self-Care directory of services
Step 3. Referral completion, where KCSC informs the VCS provider of referral details. The Provider
must contact patients within 7 days to double-check suitability, and commence first of six
service sessions.

9Social Return on Investment
Figure 1. Social prescribing for Self-Care services, within My Care, My Way (source: WLCCG)
WHAT IS
SELF-CARE?
SELF-CARE
PATHWAY
MCMW
CM’s & HSCA’s
SELF-CARE
PROVIDERS
KCSC
Awareness
Activities
& Support
Referral
Follow up &
Sustaining
change
Complete care plan
Use PAM to understand
patient's current level of
engagement
Use the directory or People
First website to identify
suitable activities and
support
MCMW
Primary care staff are
aware of self-care and
know how to signpost
patients through the
directory or People First
website
MCMW
PATIENT
Check referral criteria and
ensure the referral includes
information on any additional
support needed and patient’s
goals
Send referral form in S1 to
selfcare nhs email address
(tiers 2 & 3) or contact
services directly (tiers 0 & 1)
Add accepted referrals to charity log
Keep referral
criteria updated
MCMW
KCSC
Ensure that there is up to
date information about the
services on offer
KCSC
Contact patient for assessment
Email CM/HSCA if they can’t
engage the patient
PROVIDER
Check charity log to get progress updates
Respond to any issues raised by provider
MCMW
Collate patient’s feedback
from across the different services
KCSC
Keep charity log up to date
Email CM/HSCA with any concerns
PROVIDER
Review PAM two weeks
after the last session and
feedback to MCMW
Gather patient feedback
If needed contact
HSCA/CM by e-mail or by
phone, to discuss next
steps
PROVIDER
Check with the provider if
there is no feedback two
weeks after the final
session
Follow up with patient - and
develop a plan to help
them sustain change
MCMW
Assessment
& Care planning
6 sessions
Exercise
Counselling De-cluttering Carer’s support
Befriending
+ Social Clubs
Supporting
daily living
Diet
& Nutrition
Dementia
Support
Information
+ Advice

Self-Care Social Prescribing10
Referred patients can have up to six sessions of
their chosen activity or service. Patients can also
be re-referred once, giving access to a total of
twelve sessions.
The services provide a range of personal one-to-
one interventions and group activities. This ‘roster’
of services is demand-led, and so can change
depending on which types of services prove popular.
The five highest funded services during the pilot
phase (between May 2016 and March 2017) were
also the most popular: ‘Dementia 1-2-1 support’ (c.80
referrals), ‘Link Up’ (c.180 referrals), ‘Information and
Advice’ (c.155 referrals), ‘Exercise at Home’ (c.135
referrals), and Massage therapy (c.85 referrals).
Services provided during the pilot phase are briefly
described and categorised below:
African Dance
Group sessions to encourage physical activity,
balance, and inter-cultural awareness through
learning traditional African Dances.
Arts and Culture In The
Community (for dementia)
Activities range from group sessions for those
in residential care to one-to-one interventions
for people living in their own homes and at risk
of isolation. Activities include supported visits to
galleries, heritage buildings, and theatres that
enhance and compliment individual care plans,
and help people to feel part of their wider
community. Creative and cultural befriending
is also offered on a one-to-one basis.
Befriending
Weekly one-to-one visits to those patients who live
alone in Kensington & Chelsea and are at risk of
becoming isolated. People are able to keep in touch
with the outside world through their befrienders who
help to combat isolation by making regular visits
to older people, providing companionship and a
listening ear.
Carers Support Network
Provides a tailored service to unpaid carers,
informing and supporting them to identify their
needs and empowering them to make informed
choices and pathways for themselves and the
person they care for.
De-cluttering at home
Using proven de-cluttering techniques, the
personalised service assists clients wanting to sort
their belongings at home. This can be because they
want to downsize, reduce clutter, or reduce anxiety
about growing volumes of paperwork e.g. bills,
2. Services available
through social
prescribing

11Social Return on Investment
notices, official letters. This can help with reducing
the risk of trip hazards or fire traps, and can also
help those clients who require support at end of life.
Dementia One-To-One Support
The service offers personalised support in coming
to terms with diagnosis, providing activities that can
promote cognitive ability, slow disease progression,
and future planning. Interactive activities are
tailored to the client’s interests and abilities,
depending on their level of progression.
Escorting
Clients are provided with personalised assistance
to attend GP, clinic, hospital or other healthcare
appointments, with a trained person who
can accompany and travel from home to the
appointment, support and advocate during any
consultations, and ensure clients return home safely.
Exercise at Home
One-to-one tailored service with a case worker
with a health and fitness background, to undertake
gentle home-based exercise. Exercise plans can
help improve core strength, balance and flexibility,
increase confidence, promote cardiovascular
fitness, reduce stress, assist with weight control,
and reduce falls risk.
Information and Advice
Provides impartial and independent advice on a
range of issues, including Attendance Allowance,
welfare benefits, health, disabilities, housing
advice, social care needs, fuel poverty and energy
efficiency, family issues, and form-filling assistance.
‘Link Up’
Link-Up is a hub-based service, available to help
older clients access physical, creative and mentally
stimulating activities, to help improve the health
and wellbeing. A large variety of support activities
are available, both at home and in the community,
on a one-to-one basis or in groups.
Massage Therapy
Massage therapy is specifically for patients who
are frail, often isolated, and suffer from limiting
long-term conditions and chronic pain, but are
unable to easily access services through disability
or lack of mobility.
Macular Degeneration Support
Group
Provision of advice and support for people with
macular conditions and related sight-loss problems,
including age-related macular degeneration.
Memory Cafe
Social support group for people with memory
problems, and their friends, family, and carers.
Can include memory exercises, mental stimulation
activities, and general learning and interaction.
Men’s Only Activities
Hub-based peer-based group for supporting
men’s health and well-being behaviours, health
knowledge, socialising, cooking and nutrition,
and interactive activities in the community.
Nutrition and Community Lunches
Enables older people to attend healthy community
lunches and nutrition groups, to improve diet,
nutrition intake, and reduce social isolation.
Safety at Home and Falls Prevention
Provides support to people who, due to health
reasons or their living conditions, are at risk of
falling within their homes. The service aims to
reduce the risk of falls in the home, reduce harm
from other hazards in the home, recommend
the equipment or repairs necessary to improve
safety, and provide information and advice on
‘de-cluttered’, healthier lifestyles.

Self-Care Social Prescribing12
Supported Gym Sessions
Group or one-to-one sessions for light exercise
with patients, to build strength, cardiovascular
health, and mobility.
Walking Support
One-to-one support to get clients out and about
within their local communities at their own pace,
promoting wellness, building confidence, improving
balance, and reducing social isolation. This
may involve taking immobile clients out in their
wheelchairs, or proving guided walking support
for those using mobility aids such as sticks or
walking frames.
New services are added when there is a need.
New services for 2018 include opportunities for
gardening, and more cultural activities for those
with mental health illnesses.
2. Services available through social prescribing
Barbara’s
case study
Barbara previously had cancer twice and had
recently suffered a broken hip due to brittle bones
(partly due to intensive radiotherapy treatment).
She also suffers from cellulitis, resulting in one
leg being almost twice the size of the other. This
is extremely painful, heavy-feeling, and impedes
her walking. Barbara currently can’t get dressed
by herself and has carers who come to help with
her personal care.
As part of WLCCG’s My Care My Way
programme, Barbara’s GP – with whom she has
a very good relationship – initially called to ask
if she wanted to be part of the Self-Care project.
She was provided with a consultation with her
Case Manager. They discussed various options
to help with her rehabilitation and get out and
about in the community to build her confidence.
She recorded a PAM score with her Case
Manager of 55.7 and was referred to the walking
support service.
The walking support provider got in touch to
arrange her weekly sessions, and also to check if
she had any additional mental wellbeing needs.
For the first session, they went to the end of the
road and back – ‘not very far’. She had to rest
at the end. For the second session, Barbara
needed some shopping, so they walked a little
further to the supermarket. During later sessions
she was able to walk to the park and was getting
further with each session. Barbara felt the service
was flexible, and that her walking support worker
was very nice and kind.
‘ I hadn’t realised how difficult I would find holding
on to a stick and checking both ways for traffic.
I wouldn’t have been confident going out alone.
The worker is very patient when I need to stop
and rest. I was worried she would be marching
me up and down the road, but in fact she is very
kind, and not over-protective.
I just want to say how nice everyone is. Not
patronising at all. I’m very impressed, the attitude
of all staff – they want to help so much. Everyone
who I have dealt with in this service and in the
special unit at St Charles has been so good’
(a local integrated care hub).
Barbara’s motivation and confidence for her own
Self-Care improved significantly; her follow-up PAM
score improved to 67.8, an increase of 12 points.
She feels there is less risk of her falling and of
being isolated at home. Barbara is keen to continue
getting out and about, and is looking into walking to
French language classes near her home.
Patient’s name changed for confidentiality purposes

13Social Return on Investment
In May 2017, KCSC commissioned Envoy
Partnership to produce an Impact Evaluation with
a Social Return on Investment (SROI) analysis of
the Self-Care social prescribing pilot. KCSC and
WLCCG felt this approach would provide the most
comprehensive and holistic form of evidence, as
it includes the identification and measurement
of outcomes for material stakeholders,
2
as well
as valuation of social (health and wellbeing) and
economic outcomes.
The key research themes in this evaluation are
as follows:
• Patients – Did the Self-Care pilot make a positive
contribution to patient confidence and motivation
to look after their own health?
• Carers and Families – Did the Self-Care pilot
make a positive contribution in supporting
patients’ carers and families?
• Cost Effectiveness – Did the Self-Care pilot
make a positive contribution to a reduction in
primary and secondary care use?
• Value for Money – What are the broader social
and economic impacts of the Self-Care pilot?
2
In SROI terms, material stakeholders are those who experience material outcomes, i.e. outcomes that are relevant and
significant enough to be measured, valued, and incorporated into the SROI model
3
A guide to Social Return on Investment, (2012), Cabinet Office. For more details, see socialvalueuk.org/resources/sroi-guide
• Voluntary and Community Sector (VCS) – Did the
Self-Care pilot enable the VCS providers to attract
or leverage in additional funding? Did the Self-Care
pilot facilitate wider strategic or organisational
change within provider organisations?
• KCSC – How effective is KCSC in harnessing
partnerships? As a result of KCSC as the
accountable body, are providers working together
in new, innovative ways?
A separate document containing a process
effectiveness report has also been produced as
part of our research remit, and this contains an
in-depth analysis of the efficacy of the Self-Care
model’s processes and structuring of activities.
The report is available from KCSC and WLCCG.
Social Return on
Investment methodology
Social Return on Investment is a type of cost-benefit
analysis that quantifies and values social as well as
economic benefits. The methodology followed in this
report directly draws on the UK Cabinet Office’s Guide
to Social Return on Investment .
3
SROI proceeds via
six distinct stages, as defined in the guide.
3. Impact evaluation
objectives and
method

Self-Care Social Prescribing14
SROI is a mixed methodology approach, relying
on both qualitative research (particularly in stage
2 below) and quantitative research (particularly in
stages 3 and 4 below):
4
Six SROI stages
1. Establishing scope and identifying
key stakeholders
2. Mapping of outcomes
3. Evidencing outcomes and giving them a value
4. Establishing impact
5. Calculating the SROI
6. Reporting, using and embedding
The Envoy research team conducted the SROI
research between May and November 2017.
The research was underpinned by the Seven
Principles of SROI as set out in the Cabinet Office
SROI Guide,
5
and shown in the box below.
Mapping a theory of change
SROI analysis involves the development of a
Theory of Change (under SROI stage 2 ‘Mapping
Outcomes’). This shows the stakeholders affected
by the Self-Care services, the inputs and activities
that occur, and the outcomes created by the Self-
Care pilot. The outcomes identified in the Theory
of Change are then measured. The measurement
focuses on the outcomes, i.e. the ultimate benefit
or change experienced by stakeholders, as well as
the outputs, i.e. the quantifications of activities e.g.
the number patients, or the number of episodes.
The Theory of Change is shown in section four.
Measuring outcomes for patients
To measure outcomes, we drew on validated
questions from existing clinical health
questionnaires, including EQ-5d, Warwick-
Edinburgh Mental Wellbeing Scale (WEMWBS),
PHQ-9 (Patient Health Questionnaire), ICECAP-A,
and SF-12 (see Appendices Part D for details).
There are a range of methods to: i) measure
subjective wellbeing outcomes, and ii) value
subjective wellbeing outcomes. Often, the challenge
is to ensure that the outcome is measured in a
way that allows it to then be valued appropriately.
Our recommendation is that binary measures (e.g.
Yes / No questions) should be avoided; instead,
measures that show the magnitude of change
experienced by patients should be used. The
validated questions above fit this criterion.
Establishing impact
In SROI terminology, ‘Impact’ is a measure of
the difference made by the project or organisation
being evaluated. It recognises that there is
likely to be a difference between the change
observed, and the change for which the project or
organisation can claim credit. Such considerations
are important to ensure that the analysis does not
over-estimate value created.
Four key areas are considered here:
• Deadweight (what outcomes are likely to have
happened anyway)
• Attribution (the extent to which outcomes arise
because of social prescribing, rather than
because of the contribution of other people
or organisations)
• Displacement (whether any value is
‘displaced’ elsewhere)
3. Impact evaluation objectives and method
The Seven Principles of SROI
1. Involve stakeholders
2. Understand what changes
3. Value the things that matter
4. Only include what is material
5. Do not over-claim
6. Be transparent
7. Verify the result
4
Ibid., pages 9 –10
5
A guide to Social Return on Investment, (2012), Cabinet Office. For more details, see socialvalueuk.org/resources/sroi-guide

15Social Return on Investment
• Drop Off (the extent to which outcomes are
sustained over time)
The details for these considerations are further
explained in Appendices part B.
Primary data
The primary research conducted for this evaluation
is summarised in Table 1 below.
Table 1. Primary research
The secondary data analysed for the evaluation is
as follows:
• WLCCG data regarding the average number of
GP appointments per year for all My Care, My
Way patients, in the period April 2016 – July 2017
• WLCCG aggregate data for MCMW acute
hospital episodes from 29 practices, in the period
April 2016 – March 2017
• WLCCG social prescribing PAM scores data for
the period April 2016-July 2017
• Insignia Health research into the impact of PAM
scores on patients
• WLCCG GP practice staff cost data
Data limitations
• De-identified acute hospitalisation data and
GP appointment data was shared by WLCCG
but was not made available by episode type
(e.g. specialist surgery, diabetes, cancer). We
therefore were only able to use unit costs for
average incidence costs.
• PAMs survey wording is seen by many patients
and practice staff as inappropriate for some
conditions, e.g. dementia. In these cases, PAMs
data was not collected; a simpler alternative
version would have been needed if data was to
be collected. Nonetheless, a reasonable amount
of data was collected; we received 247 baseline
and follow-up PAM scores to analyse.
• For certain outcomes, e.g. preventive effects
of interventions, our analysis is reliant on
subjective indicators through primary survey
data from HSCAs and Case Managers. This
data shows their perceptions on the extent to
which preventive effects are being achieved.
However, we remain confident with the results;
we achieved a sample of over half of the HSCA/
Case Manager population who were actively
referring. Improvements observed in PAM scores
for our sample also provide confidence that a
significant proportion of patients benefit from
reduced need.
• We did not receive patient postal survey returns
for all services, particularly for those with a low
number of referrals. There were no returns from
T’ai Chi, African Dance, or community lunch,
for example.
Stakeholder groups Sample Methodology
Qualitative
Patients
(Tiers 2 and 3)
33 Face-to-face
interviews,
often in the
patient’s home
Case Managers
& HSCAs
31 Telephone
interviews
VCS providers 9 Face-to-face
interviews
Statutory authorities
(public health,
adult care)
3 Face-to-face
interviews
GP lead for
Self-Care
1 Telephone
interview
WLCCG managers
for Self-Care
2 Face-to-face
interviews
Quantitative
Patients
(Tiers 1,2,3)
134 Paper survey
delivered by post
Case Mangers
and HSCAs
(75 actively referring)
42 Online survey

Self-Care Social Prescribing16
Service themes and patient outcomes
In our research, we identified different categories of services that led to slightly different groups of
outcomes, as shown below in Table 2:
Table 2: Patient benefits from Self-Care services
Service theme Patient outcomes
Physical & Exercise activities
• African Dance
• Escorting
• Exercise at Home
• Massage Therapy
• Supported Gym Sessions
• Walking support
Physical wellbeing
Reduced isolation
Mental and Emotional wellbeing
Reduced anxiety
Maintain independence
Respite for patients’ carers (during patient sessions)
Mental wellbeing and reduced isolation
(non-dementia specific)
• Befriending
• ‘Link Up’ activities
• Memory Café
• Men’s Only Club Activities
• Carers Support Group
Reduced isolation
Mental and Emotional wellbeing
Reduced depression
Reduced anxiety
Maintain independence
Memory retention
Respite for patients’ carers (during patient sessions)
Dementia-specific support
• Arts and Culture in The Community (for dementia)
• Creative and Cultural befriending
• Dementia One-To-One Support
N.B. Exercise at Home and Walking Support are also
provided to dementia referrals with a tailored approach
Mental stimulation and concentration
Reduced isolation
Reduced depression
Mental and Emotional wellbeing
Improved Self-Worth
Reduced anxiety
Maintain independence
Respite for patients’ carers (during patient sessions)
Safety & Welfare Information and Advice
• De-cluttering at home (can also be considered as
part of mental wellbeing services)
• Safety and falls prevention at home
• Information and Welfare support advice
New source of income support
Reduced anxiety
Maintain independence
Physical wellbeing
Improved living conditions
Respite for patients’ carers (during patient sessions)
Health Education & Nutrition
• Healthy Lungs
• Macular Degeneration Group
• Nutrition and community lunches
Physical wellbeing
Reduced isolation
Maintain independence
Improve health knowledge
4. Findings:
Patients

17Social Return on Investment
Chart 1 shows the proportion of referrals by service
theme for the pilot period (Apr ‘16 – Mar ’17).
The largest categories of referrals were physical
activity, mental/emotional wellbeing and isolation,
and information/advice and safety at home.
Chart 2 illustrates that the majority of referrals for
the pilot period were comprised of Tier 2 patients
(almost 53%) with just over a third from Tier 3. A
much lower proportion of 7.6% were Tier 1 patients.
Chart 1. Referrals by service theme,
Apr 16 – Mar 17
Chart 2. Referrals by Tier,
Apr 16 – Mar 17
Patient referral proportions by service type
(n=807)
31.1%
Physical activity
& exercise
29.6%
Mental/Emotional
Wellbeing &
Isolation
4.8%
Health Education
& Nutrition
0.9%
Carers
Support
34.6%
Tier 3
7.6%
Tier 1
5.1%
Unknown
52.8%
Tier 2
22.6%
Info & Advice +
Safety at Home
11%
Dementia
specific support
Patient tier proportions (n=807)

Self-Care Social Prescribing18
Outcomes for patients
Much of the benefits to patients come through
re-building their balance and self-confidence in
their mobility (e.g. when being able to walk around
outside or at home), and through reducing pain
and discomfort, improving their support networks
and social networks, and reducing levels of
depression or anxiety. Across most of the service
themes, patients feel they have benefited from
reduced levels of anxiety about their condition(s)
or health situation, and have also felt more valued
by others – especially by the health care system.
Reduced social isolation, and improved re-
connection to their community, are also particularly
important for patients. Some patients felt that
maintaining their ability to live as independently
as possible was important, although for many
others who are extremely frail and housebound,
this may not be a realistic outcome. Maintaining
independence at the same level is a good outcome
for many.
Outcomes for Carers and Families
Evidence collected from interviews and surveys
suggests that informal carers of patients gain
some relief of around one hour during each of the
patient’s sessions. In most cases, carers will either
use the time to continue with other tasks regarding
the patient’s care needs or day-to-day tasks
around the patient’s home. Some will use the
time for respite.
15 from 134 patient survey responses fed back on
respite for carers. Around half of these responses
indicated that the Self-Care service was moderately
to extremely helpful for creating respite time for
carers. However, this is a small sub-sample, and
the research indicates that the more significant
outcomes actually relate to the carer feeling
happier for the patient, if the patient feels better in
themselves or if their health condition improves.
When information and advice support (from CAB
Westminster and Age UK), leads to successful
claims for welfare payments, there is a longer-term
impact on carers, both in terms of relief, and their
wellbeing. This appears to be a stronger outcome
for carers who are the spouse or partner of the
patient, and sometimes have their own health
conditions to manage.
For the small number of cases where referrals
were made for the carer to access specific support
through the Carer’s Support Network, the most
important outcomes were:
• Reduced feelings of being isolated and alone
• An improved awareness about other
available support
• Better able to navigate a plethora of health
agency/service material and contact details,
that they would otherwise feel overloaded with
There was some less positive feedback from
carers. In some cases, carers express frustration
and disappointment with health professionals and
statutory support, claiming inadequate information
about Self-Care from their GP and a disjointed
approach between housing support, GP practices,
and social care.
4. Findings: Patients
‘ The professionals from housing, health, social
care, all look at our case one-sided, from
only their viewpoint and how it affects them,
rather than communicating and helping each
other to avoid conflicting decisions for my frail
parents…I’m upset my GP didn’t mention these
services [social prescribing] in the first place.’
T.B., son and carer of frail parents

19Social Return on Investment
‘ From the experience of family members’ illness, a map/picture of introduction information might help
people to understand A) how to get help from whom in a ‘direction’ guide. B) how NHS care system
works in the relation with hospital, local council, nurses, and GP, and C) Basic knowledge of ‘NHS
uniform’ meaning.’
Carer and relative of patient receiving Exercise at Home and Walking Support
Tej and his parents
case study
Tej is a full-time carer for his elderly parents, who
are extremely frail and housebound (‘Tier 3’ frailty).
His parents also suffer from poor mental health.
His father’s condition means he is unable to speak
at all, and his mother is unable to speak English.
Tej had to go through a lengthy process to
obtain a Power of Attorney to represent his
parents at their local health services and GP
surgery. At one consultation, front-desk staff also
recommended he attend a further consultation
with a HSCA, to explore if there were other
community-based services appropriate for his
parents. After identifying the condition and needs
of his parents and recording a PAM score on
their behalf (c.70), the HSCA suggested either
exercise at home or massage therapy, to help
support his parents’ overall wellbeing, mobility,
and strength in their joints and muscles.
Tej was referred and contacted within a week
by the provider for exercise at home, to arrange
the session plans for his parents. This required
Tej to be available during the sessions to
translate some of the instructions, session
planning, and to help ensure his parents were
comfortable with a stranger in the home. The
exercise instructor guided them through gentle
exercises, which mostly focused on limbs, arm,
hand, and neck exercises. It was important that
the provider enabled each of his parents to feel
they were making progress at their own pace
and within their respective capabilities, whilst
the intensity increased a little for each session.
After completing the sessions, Tej felt his parents
were a little stronger and benefitted from better
sleep. However, they still felt some pain, anxiety,
and blood circulation problems; and so Tej also
requested massage therapy at home, on his next
HSCA appointment.
The massage therapy provider contacted Tej
within a few days, and had sessions scheduled
for both parents, one after the other at home.
Tej described is parents as ‘uncertain aft first,
especially have a different female [the therapist]
in the home…but she [the therapist] was very
sensitive and understanding…they [parents]
loved and enjoyed the massage service, I can
see them much happier and responsive mentally,
even after just the second session…the pain
reduced for them and they are more relaxed than
before…and now [it’s] a little less difficult to move
them [around the home, or from sofa to bed],
and they are more peaceful’.
Tej felt that it was important for all frail, older
people to have access to more services like
those made available to his parents, especially if
it gives a boost to carers to see their service user
or relative benefitting so tangibly. Tej is following
up with his HSCA about receiving more carer
support, and exploring how to arrange more
ad hoc sessions at home for his mother.
Patient’s name changed for confidentiality purposes

Self-Care Social Prescribing20
Theory of Change
In an (SROI) analysis, qualitative research from
stakeholder engagement should inform the
creation of a Theory of Change. The Theory of
Change is the foundation for identifying which
stakeholder outcomes should be measured and
valued. It presents stakeholders, activities, and
outcomes that arise from the social prescribing
model. It can be useful for helping understand the
different pre-conditions that exist, and for helping
understand where potential barriers to change
might occur. It aligns with HM Treasury Magenta
Book guidance on logic mapping.
6
Figure 2 shows the Theory of Change for the
Self-Care pilot. It summarises the outcomes
for material stakeholders arising from core
activities of the Self-Care model. It shows
how the activities lead to outcomes, and how
short-term outcomes lead to long-term outcomes
which should be valued.
We have presented a theory of change for the
whole Self-Care pilot, across all the services
provided. Not all of the patient outcomes will be
applicable for all of the patients. The left-hand side
of the Theory of Change maps the main activities
that preceded referrals into the social prescribing
services. These then build from left to right into
the short to medium term outcomes, and to the
long-termer outcomes, which we define below:
• Short-term to Medium outcomes are those
that can happen during the sessions or in the
first month after all sessions are completed
(including re-referral).
• Long-term outcomes are those that are
expected to arise around six months after
the sessions are completed.
As services are paid for from the contract budget
to VCS providers, they are treated as part of the
overall inputs to the activities. It should be noted
that outcomes for carers discussed in the previous
section of this report were not monetised in our
analysis, due to relatively low referral numbers
for inclusion in our postal survey.
Changes to Patient Activation
Measures (PAM)
One objective of Self-Care is to improve patients’
activation and motivation about managing their
own health and wellbeing. Patient Activation
Measures (PAMs) are designed to help medical
services to understand whether patients’ activation
and motivation has changed. PAMS are recorded
by practice-based staff with patients, to track
their levels of activation and motivation. This is
important as part of My Care My Way’s drive to
educate and empower older patients to self-
manage their conditions as much as possible.
We received WLCCG data for over 2,000 social
prescribing PAM records across 2016 – 2017.
However only 247 patients had both baseline
and follow-up scores in this period. Of those
patients who had follow-up PAM scores, around
62% showed an improvement. The average
improvement for those 62% was 5.8 points.
According to the PAM scoring system,
7
an
improvement by one-point correlates to 2%
reduced hospitalisation likelihood. Therefore,
one of the areas of resource savings indicated by
the improvement in patient activation would be an
average 11.6% rate of reduced hospitalisations,
for patients who showed an improvement.
PAM scores are presented by Tier level in Table 3.
There are only marginal differences between Tier 2
and Tier 3.
4. Findings: Patients
6
The Magenta Book: Guidance for Evaluation, HM Treasury (2011) see logic model in Chapter 5
7
Licensed from the US company Insignia Health

21Social Return on Investment
Figure 2. Theory of Change for the Self-Care social prescribing model
Patient arranges visit to GP practice
re: non-medical health/wellbeing issue
Consultation with HSCA or
Case Manager instead of GP
to discuss needs
Provider contacts
patient to arrange
and manage sessions
Provider logs case
notes and updates to
Charity Log software
Provider may arrange appropriate
forward referral to other services
or sources of support
Patient referral logged with
KCSC; patient needs,
background, goals shared
Select service from Directory
- Provider 1 - Provider 3
- Provider 2 - Provider 4 etc
- Carer relief in short-term
- Less alone/isolated in short-term
- Improved knowledge to better
navigate care services
- Sustained tenancies for housing
providers of patients
- Avoid patient need for entering
long term care home
- Provider provides 6 sessions to
patient (1-2-1 basis or Group activity)
- Provide health guidance & coaching
- Develop service directory
- Select and recruit services
- Manage contracts and payments
- Manage overall capacity
- Co-ordinate referrals
- Record data and track activities
-Learning and knowledge-sharing
- Connect local VCS networks
- Reduced pain and discomfort
- Reduced depression
- Reduced levels of loneliness and social isolation
- Improved self-confidence/self-worth
- Improved independence
- Feeling equally valued by health services
- Avoided GP consultations
- Avoided HSCA & CM research
and consultation hours
- Reduced hospital spells
- Reduced outpatient clinic visits
- Avoided A & E incedence
Care plan update with
involvement of patient
KCSC co-ordinates referral
and notifies selected Provider
- Diverted GP hours
- Diverted HSCA & CM research hours
Patient may choose to
discontinue sessions
Some patients health
may deteriorate anyway
Self-activation
(self care)
Feedback
Loop
Provider resourcing,
staff times and training
Short to Medium Term Long Term
Legend:
Health service activities
KCSC activities
VCSS Provider activities
Outcomes – patients
Outcomes – health services
Outcomes – carers & relatives
Outcomes – statutory services
Outcomes – other

Self-Care Social Prescribing22
4. Findings: Patients
Table 3: Change in PAM scores of the
62% of Self-Care patients showing
an improvement.
n=247 for Self-Care patients with baseline and
follow-up scores, n=151 for those who see
an improvement.
PAM results also indicate that approximately 38%
of referred patients either experienced no change
in activation, or a reduction in activation. The SROI
model assumes that this reduction in activation
would have occurred anyway; the age and frailty of
many patients means that a reduction in activation
over time might be expected. The qualitative
research gave no indication that the services
significantly reduced activation, and the survey
responses from Case Managers and HCSAs
indicate that the proportion of patients whose
health got worse as a result of the Self-Care
intervention is negligible.
8
Furthermore, the SROI model may under-estimate
the positive impact of the Self-Care pilot. For
those patients who experience an increase in
PAM score, it might be that their PAM score would
have fallen without Self-Care, meaning that Self-
Care’s impact would be greater than stated here.
Likewise, for those patients who experience a
decrease in PAM score, it might be that their PAM
score would have fallen even more without Self-
Care. Without data from a control group, getting
a credible estimate of such change is difficult.
8
See section 5
PAM scoring is not necessarily an indicator of
health. Improvements in patient activation and
motivation do not necessarily result in improved
health outcomes in all cases – but receiving a
Self-Care service may have helped those patients
manage their condition better and maintain
important aspects of their quality of life, even
if there has been no increase in PAM score.
Measures of change for patients
In addition to evidence collected through
qualitative interviews, we also collected 134 patient
surveys across different Self-Care service themes
(Table 2). The aim was to quantify the outcomes
identified in the qualitative research. The measures
are presented below in Chart 3 and Table 4.
Tier 3 Tier 2 Tier 1
+ 5.9
(51.1 to 57.0)
+ 6.4
(50.2 to 56.6)
+ 3.2
(56.8 to 60.0)
‘ Very good and I have no suggestions to
make. My main adversary is laziness – hardly
your fault!’
‘ I think Men’s Only activities do a wonderful job,
it is just what I need to motivate myself into a
better and healthier way of life’
‘ A wonderful idea to keep the elderly [like me]
active and motivated.’’
Self-Care patients’ feedback
‘ Linking patients in with activities, or the
increased level of interaction provided by
services such as walking support etc – very
clearly improves outcomes in terms of
emotional wellbeing and isolation.’
HSCA feedback, Kensington & Chelsea

23Social Return on Investment
9
As corroborated by PAM improvements: see Table 3
Table 4 Shows patients’ responses on pain,
depression and anxiety. We can see increases in
the proportions of patients who feel: i) No pain or
little pain (+24%), ii) No feelings of being down or
depressed (+17%), and iii) No feelings of anxiety
(+14%). Survey questions in Table 4 were based
on the short EQ5-d and PHQ9 surveys.
Table 4. Patient survey responses regarding
health status outcomes
Chart 3 shows patients’ level of agreement with
statements regarding their well-being, both before
and after the Self-Care service. The largest change
(67% to 78%) was in patients’ sense of self-worth
and motivation to take care of their own health and
medication,
9
and feeling more valued by the health
care system. Before their Self-Care referral, 63%
felt as valued by health services as other people.
This increased to 69% after their referral.
There is also a small reduction in isolation, with
slightly more patients reporting they had enough
people they personally felt close to in their lives
after the service (69%) compared to before (65%).
Chart 3 also indicates that there are small changes
for independence and dignity. For many of the
patients, there appears to be a lower starting
point for the ‘Before’ referral score for living
independently, relative to other indicators. It was
clear from our interviews that maintaining the
independence that they have is a good outcome
for many patients.
Chart 3. Patient’s self-reported change in well-being
I feel motivated to
take care of my health
and medication needs
I can live as
independently as I want
My living conditions
help me to live in dignity
There are enough people
I personally feel close to
When accessing health
and care support I feel
I’m valued just as much
as other people like me
Before
Strongly Agree
3
%
1
%
Neither Agree nor Disagree Strongly DisagreeDisagreeAgree
Before
Before
Before
Before
After
After
After
After
After
Q. “Please put a cross (X) in the box that best describes how much you agree or disagree with each statement below:”
All self-care patients responding to survey, Nov/Dec 2017. n=89, 98, 87, 95, 68, 78, 77, 85, 85, 94.
9%52%
29%
4%5%
7%54%31% 5%4%
7%22%45%22% 4%
13%54%24% 5%
17%15%46%19% 2%
12%18%40%29%
9%
9%
5%
4%
17%
21%
7%
5%
20%
12%
24%
22%
38%
41%
48%
50%
17%
17%
15%
19%
% of Patients
responding Before
After Change
Little or No pain 15% 39% +24%
No feelings of
being depressed
30% 47% +17%
No feelings
of anxiety
29% 43% +14%
Self-Care Social Prescribing24
SROI requires the monetisation of social,
environmental and economic outcomes.
10
Patient
wellbeing outcomes valued in our analysis are
as follows:
• Reduced pain and discomfort
• Reduced depression
• Reduced levels of loneliness and social isolation
• Improved self-confidence/self-worth
• Improved sense of health equality i.e. feeling
equally valued by health services
• Improved independence
Approach to valuation
Our approach to valuing patient outcomes are
based on Quality Adjusted Life Year (QALY)
approaches to valuing health. These align with
similar approaches used by both WLCCG, and
the NHS and the National Institute for Health
and Care Excellence (NICE) more broadly. In
terms of QALY value, we have used the British
Medical Association’s guidance from their recent
paper about preventive intervention, Exploring
the cost effectiveness of early intervention and
prevention (2017). This states that NICE considers
interventions costing up to £20,000 per QALY
gained as cost effective. The BMA also refers to
a NICE analysis on 200 interventions between
2006 and 2010, where 70.5% (i.e. a clear majority)
costed less than £20,000 per QALY gained’.
We drew on a range of sources for valuations.
These value ranges are described in the Appendix
Part C. These included Devlin, Shah et al, from
the Office for Health Economics and University
of Sheffield, published in the Journal of Health
Economics (JHE) in 2016,
11
and Jia and Lubetkin,
in the journal, Health and Quality of Life Outcomes
(2017).
12
We also drew on guidance from other
research (New Economy Manchester; and Bield
Housing, Hanover Scotland and Trust Housing),
13
in
order to attach value ranges to the overall measures
of patient wellbeing. The value or worth of subjective
wellbeing is termed ‘utility’ in the JHE research.
5. Findings: Valuing the utility
of patient health
and wellbeing
outcomes
10
However, environmental outcomes are out of scope of our research as they were deemed immaterial
11
Valuing health-related quality of life: An EQ-5D-5L value set for England (March 2016)
12
Incremental decreases in quality-adjusted life years (QALY) associated with higher levels of depressive symptoms for U.S.
Adults aged 65 years and older (2017)
13
New Economy Manchester (2012) Understanding the Wider Value of Public Policy Interventions, and Bield, Hanover and Trust
Housing (2012) SROI of Stage Three Adaptations, and SROI of Very Sheltered Housing

25Social Return on Investment
Through applying these value ranges to the
amount of change experienced by patients, we
calculated the values of the outcomes experienced
by patients. The values are presented by service
category total, and on a per patient average basis,
in Table 5. The results account for attribution
adjustment, to reflect that patients recorded c.23%
attribution to the services for the overall impact
experienced (see Appendices Part B, and also
section three).
Our results indicate that services supporting
physical activity and exercise, and mental
wellbeing and isolation tend to generate higher
values, both per patient and overall. However,
Table 5 also indicates that dementia-specific
support has a relatively high ‘per patient’ value,
even though there were fewer referrals.
Table 5. Attributable values for patients’
health and wellbeing outcomes, pilot year
to March 2017 (rounded)
*Excludes new welfare payments to patients of c.£112,000 in total
According to our patient survey, around one in
four patients who received Information and Advice
support went on to receive welfare payments. The
average amount received by patients was c.£2,732
per year. Most payments were Attendance
Allowance payments (e.g. payments to attend
health appointments when it is physically difficult to
do so without support), and smaller allowances for
energy support.
Service category
Overall Health
and Wellbeing
value per patient
pre-attribution
Health and
Wellbeing value
per patient after
attribution
Number of
patients
Attributable
Health and Well-
being Value –
All patients
Physical & Exercise £1,330 £290
251
£73,500
Mental wellbeing
& Isolation
£1,000 £230
239
£54,500
Safety at home
& Welfare
Information/Advice*
£330 £70
182
£13,000*
Health Education
& Nutrition
£50 £10 39 £400
Dementia-specic
support
£1,280 £280 89 £25,000

Self-Care Social Prescribing26
Moira’s
case study
Moira has dementia, lives alone, and needs her
walking stick to walk for long periods. Her HSCA
at the local GP clinic identified Moira’s strong
interest in arts and culture and that she was
comfortable interacting with other people. As
part of her consultation and Care Plan, to avoid
the negative effects of loneliness and isolation
on her dementia, Moira’s HSCA referred her to
attend arts and culture activities for people with
dementia. The service contacted Moira and
clearly explained how the activities would work;
what support would be available for her during
the activity; they provided clear instructions
and directions to attend; and followed up with
a reminder through her support worker. This
encouraged Moira and put her at ease.
The service enabled Moira to attend dementia-
friendly group activities at various culture and
arts venues. This included visits to art galleries,
Kensington Palace, and an opera production in
Holland Park – with a backstage tour with the
opera singers. At the activities, the provider’s
session workers are posted at different locations
at the venue and near the entrance, to welcome
participants, help with wayfinding, and help find
resting points.
There are often many interactive components
of the activity, which requires input and sharing
of ideas and stories between participants, as
well as learning from speakers or learning from
people working at the venue e.g. a costume
and set designer, an opera conductor, or a
heritage specialist.
This really suited Moira, who has a sharp sense
of humour and has a fun-loving personality, and
is keen to get involved and learn the value of
objects and artefacts. The activities are designed
in a way which enables her to be engaged with
by friendly staff and group participants, and
to participate in creative activities, including
art work, walking tours, music, and singing.
She stated that some of the experiences with
Resonate were ‘just wonderful’ and that she felt
‘very lucky to join in…it’s so nice to be with such
special people [including the volunteers]’. Moira
continues to access the service ‘on her own
steam’ as this is one of her only opportunities for
combining social interaction, enrichment, and
mental stimulation. It gives her ‘quite a boost
to feeling good…and builds confidence’ when
managing her condition.
5. Findings: Valuing the utility of patient health and
wellbeing outcomes
Patient’s name changed for confidentiality purposes

27Social Return on Investment
Major priorities for GP practices taking part in
the Self-Care pilot include tackling diabetes
(for example, through improvements in active
lifestyle, diet, and medical compliance), managing
dementia, and reducing the effect of social and
emotional isolation on older patients’ overall
wellbeing. The service themes within the social
prescribing directory therefore seem appropriate
as they contribute towards supporting patients
with these health problems.
HSCAs and Case Managers reported back on the
health status of patients now, compared to before
their referral. Table 6 shows the average proportion
of patients who have improved. Improvement was
higher for Mental Wellbeing than Physical health.
Within Physical health the proportions for ‘Much
better’ health were highest for Tier 2 and Tier 1.
Proportions of patients who had got worse after
the service were negligible.
Table 6. HSCA and Case Manager survey
responses on physical health and wellbeing
status (n=42)
The ‘Much better’ responses corroborate well with
proportions indicated by patient survey results.
Conversely, a lower proportion of HSCA and
Care Managers (38%) agreed that their GPs
recognised the VCS providers as partners in their
work. Even fewer (36%) agreed that GPs had a
clear appreciation of the outcomes from social
prescribing referrals. This suggests that some
knowledge barriers may exist around the benefits
of cross-sector collaboration and recognition about
the Self-Care social prescribing model.
To compound this challenge, in our analysis of
process effectiveness, we also observed that
there is a need for effective feedback to be more
regularly recorded, and accessed by practices. This
is especially important as GPs are accountable
for their patient Care Plans. Currently there are
two software systems where a lot of information
is recorded but needs to be better integrated:
‘SystmOne’ (used by health services) and ‘Charity
Log’ (used by VCS case partners).
6. Findings:
Health and
Care system
Health status summary
Physical health NOW
vs before referral
Mental wellbeing NOW
vs before referral
Tier 3 Tier 2 Tier 1 Tier 3 Tier 2 Tier 1
% of referrals ‘Much better’ 3% 10% 27% 20% 33% 34%
Total % of referrals ‘Much better’
and ‘Somewhat better’
58% 70% 66% 83% 91% 90%

Self-Care Social Prescribing28
Preventive impacts
The research highlighted a number of preventative
impacts of the Self-Care pilot. Case Manager
and HCSAs gave estimates of the proportion of
patients who stopped the need for frequent GP
visits; this is presented in Table 7 below. Case
Managers and HCSAs indicate a lower proportion
for Tier 3 than Tiers 1 or 2. We have used this
lower proportion (23%) to avoid over-claiming
in our calculations. Our calculations therefore
estimate this to be the equivalent of 185 patients
stopping the need for GP appointments during the
pilot period.
Table 7. Case Manager and HSCA
perceptions of proportion of patients stopping
the need for frequent GP visits (n=42)
According to WLCCG data for older patients
across all of My Care, My Way, the average
number of GP appointments per year is 30 per
patient (excluding no-shows).
In addition, we collected HSCA and Case Manager
perspectives on the preventive effect of the Self-
Care model. By preventative effect, we mean
reduction in health deterioration and the need for
other services in the future. The results are shown
in Table 8.
Table 8. Case Manager and HSCA survey
perceptions of preventive effect of services
(n=42)
Outcomes for health and
care services
In order to quantify the preventive impacts in more
detail, we have analysed data from WLCCG for
GP appointments and acute hospital incidences
across My Care, My Way, and triangulated this with
PAM score data and our survey findings. There are
also number of key considerations arising from our
research, which underpin our overall measurement.
These are all explored in the following sections.
Deadweight considerations
‘Deadweight’ in our analysis is a similar concept
to counterfactual – meaning the likelihood that
some outcomes would happen anyway without the
services. This acknowledges that observing and
measuring change does not in itself tell us that the
change only happened because of the intervention.
Response summary Tier 3 Tier 2 Tier 1
% referrals stopped need
for frequent GP visits
23% 31% 40%
Response summary Tier 3 Tier 2 Tier 1
% staff reporting High to
Very High preventive effect
32% 57% 67%
‘ I had a patient who was calling the surgery and
requesting call outs from the G.P. mainly due
to health anxiety. When the services began
working with him his call-outs dramatically
reduced and he engaged better [with therapy].’’
Case Manager feedback,
Knightsbridge practice
‘ We had a 91-year-old gentleman who had a
stroke. Prior to being referred, his living carer
was constantly calling the GP Practice and…
even called the London ambulance service
(LAS). Once he was referred to our service,
we had the opportunity to undertake a holistic
assessment... He is now able to walk with his
walking aid and goes out for walk daily with
his carer... he gets physio input [plus] in terms
of Self-Care, he receives massage [therapy]
which he enjoys. The phone calls to the surgery
have been stopped, including those to the LAS.’
Case Manager feedback,
Pembridge Villas practice
6. Findings: Health and Care system

29Social Return on Investment
Within our analysis, we focus on how the issue
of deadweight affects healthcare resources in
the following ways:
• Without the ‘in-practice’ role of HSCAs and Case
Managers, GPs would have to use more hours
dealing with non-medical consultations that could
otherwise be referred through social prescribing.
• Without the ‘in-practice’ role of HSCAs and Case
Managers, GPs would have to use more hours
researching appropriate support services in the
community, in addition to consultation hours.
• A proportion of MCMW patients would have been
referred to other services by HSCAs and Case
Managers that are not on the social prescribing
directory, and so those patients may have
experienced similar outcomes.
• Without the social prescribing model and directory,
HSCAs and Case Managers would have fewer
options available for patients, and would have
to use more hours on research and applications
support for those referred patients, in addition to
the consultation hours they also provide.
• Currently hospitals don’t refer their patients to
social prescribing services, but may refer to other
services to help with recovery, e.g. British Red
Cross wheelchair loan.
We assume in our modelling that whilst some
patient needs become more familiar to staff, who
are then able to deal with them more efficiently,
over the long-term this is balanced out by: i) new
patients with new needs accessing Self-Care, and
ii) staff churn and the resulting loss of expertise.
We have taken these deadweight considerations
into account when quantifying the preventative
impacts, before giving them a valuation.
Quantifying the preventative impacts
We have quantified these preventative impacts
on an annualised basis for the pilot phase, April
2016–March 2017, and also forecasted pro-rata
for the current year’s activity, where there has
been an increase from 800 to 1300 patients
(see Table 9). We did not receive WLCCG data
regarding prescription scripts for this patient group;
this is therefore excluded from our analysis.
The preventative impacts are as follows:
Hospital level resource savings
• Reduced frequency of acute hospital spells,
as indicated by PAM score average improvement
for the relevant proportion of patients.
• Reduced frequency of A & E emergency
admissions, as per PAM score.
• Reduced frequency of outpatient clinic visits,
as per PAM score.
GP practice level resource savings
• Diverted GP hours from initial social prescribing
consultations as these are conducted with
Case Managers or HSCAs instead (10–20
mins per consultation, as set out in the MCMW
business case).
• Diverted HSCA and Case Manager research/
support time. For example, researching local
services, helping with welfare applications, as
this is streamlined by the KCSC directory and
co-ordination (0.75 hours per consultation).
• Avoided GP hours from patients stopping the
need for frequent consultations (proportion
reported by HSCAs and Case Managers).
• Avoided HSCA and Case Manager research/
support hours from patients stopping the need
for frequent consultations (proportion reported
by HSCAs and Case Managers).

Self-Care Social Prescribing30
MCMW patients take up an average of 30 GP
appointments per year, excluding ‘no-shows’.
When calculating avoided GP and HSCA
consultations, we estimate that the relevant
patients stop needing to visit the GP only during
the six months after completing their sessions.
This is reflective of HSCAs and Case Managers
feedback: they reported the benefit period of 0.55
years for Tier 3 and 0.75 years for Tier 2. The
benefit period is longer at 1.3 years for Tier 1
patients, but we have under-claimed this to ensure
we are not overclaiming the impact in our analysis.
In addition, project data from the patient survey
sample indicates double-counting adjustment of
1% i.e. to account for the proportion of referrals
across different service themes. We have
increased the double-count adjustment to 10% to
be conservative, and further ensure avoidance of
over-claim.
Comparisons with outcomes
from external projects
In addition, data from other external projects,
such as Bradford Community Health Advice
Team (CHAT) suggests that the majority of their
clients visited a health care professional on fewer
occasions in the six months following CHAT
intervention, than in the six months prior (Age UK,
The Social Prescribing Pilot Project, Age Concern
Support Services – Yorkshire and Humber 2012).
Alternatively, Refresh Social Prescribing service
in Salford found that two-thirds of its clients had
fewer visits to their GP in the twelve months after
assessment with Refresh. About a third of clients
had reduced their number of GP visits by three or
more. Also, 46% of clients had a reduced number
of prescription scripts in the twelve months after
Refresh assessment.
The Department of Health’s findings in north east
England indicate that meeting older people’s
needs with a preventative approach can create
efficiencies, such as through the Partnership for
Older People project. This produced an average
of around £1.20 saving in emergency bed days
for every extra £1 spent on prevention. (A range
of between £0.80 and £1.60 is given). These
efficiency gains were on top of the £1 of additional
service utility to older people (Improving Care and
Saving Money, 2010).
14
Higher efficiency gains
were available from more intensive, targeted
interventions, which involved very close joint
working between health and social care.
This included:
• Hospital overnight stays reduced by 47%
• Accident and emergency attendances reduced
by 29%
• Clinic or outpatient appointments reduced by 11%
• Physiotherapy/occupational therapy
appointments reduced by 8%
However, this did not include an attribution
adjustment to account for other contributing factors.
There is also relevant data for the social prescribing
model in Rotherham, delivered by Voluntary Action
Rotherham and VCS providers, and contracted
by NHS Rotherham. A report by Sheffield Hallam
indicates that A&E attendances reduced by 21%,
hospital admissions reduced by 9%, and outpatient
appointments reduced by 29%. This was for a
patient cohort comprised of two thirds aged over-75
years, and with just 11% under the age of 60 years.
Attribution adjustment for other contributing factors
was also not obtained. It is clear that positive
benefits were achieved with this model for both
health and care resources and patient wellbeing.
14
Department of Health, Improving Care and Saving Money: Learning the lessons on prevention and early intervention for older
people (2010)
6. Findings: Health and Care system

31Social Return on Investment
Resource savings to
health care
Table 9 illustrates the resource value for GP
practices and hospitals, both for the pilot period, and
for the current period to Year End March 2018. We
define resource savings as the value of resources
freed up for health care services. These are not
necessarily the same as cashable cost savings.
Table 9. Resource value to health services
(values rounded to nearest ,000)
In our analysis, the social prescribing model
leads to resource savings to GP practice staff –
including HSCAs and Case Managers – valued at
£102,000 for the pilot phase, and forecasted at
£150,000 to March 2018.
This is specifically for: i) diverted consultation hours
and related work hours from an average of two
social prescribing consultations per referred patients,
and ii) avoided consultation hours for patients who
stopped needing to visit their GP practice in the six
months after completing their sessions.
Areas of resource saving
Total
reduction
Pilot year
to Mar 2017
Equivalent
consult’ns
per practice
Pilot year
Total Value
Pilot year
to Mar
2017
Total Value
forecast
YE to Mar
2018
Average
incidence per
patient per
year, MCMW
GP Practice level total £102,000 £150,000
Diverted GP hours: initial
consultations (w/ re-referral)
340 hours 57 £18,000 £27,000
30 GP
practice visits
per patient
Diverted HSCA & CM
research/support hours: initial
consultations (w/ re-referral)
1025 hours 171 £21,000 £31,000
Avoided GP hours from patients
stopping need for consultations
(6-month period)
590 hours 98 £32,000 £46,000
Avoided HSCA & Case
Manager hours from patients
stopping need for consultations
(6-month period)
1480 hours 247 £31,000 £46,000
Hospital level total £106,000 £154,000
Reduced need for Hospital spells
51
incidences
n/a £68,000 £99,000
1.19 episodes
@12 bed days
Reduced need for A & E
54
incidences
n/a £6,000 £9,000 1.23 episodes
Reduced need for
Outpatient visits
579
incidences
n/a £32,000 £46,000 8 episodes

Self-Care Social Prescribing32
Resource savings for hospitals are valued at
£106,000 for the pilot phase, and forecasted at
£154,000 to March 2018. These relate to reduced
need for hospital spells, emergency admissions
(A&E) and outpatient visits, calculated through
improvement in PAM scores for the relevant
Self-Care services.
Table 10 presents the estimate of resource saving
for health service outcomes described above, split
by service theme for the pilot phase only. This
provides an indication of the relative value of the
different service themes, which may be useful if
comparing against the average unit costs for those
service themes. This indicates that Physical &
Exercise services, and Dementia-specific support,
have a relatively high ‘per patient’ value.
Table 10. Resource Value and Utility Value
per patient per service category pilot phase
Apr 2016–Mar 2017, adjusted for deadweight
and double-count of cross-referrals between
service themes (rounded)
When the total value created is compared with the
annual contract budget of £250,000, the results of
the SROI are as follows:
Service category
(Pilot phase
Apr ’16–Mar ‘17)
Total Health
Service
resource value
Resource
value per
patient
Attributable Health
and Wellbeing Value
– All patients
Health and Wellbeing
value per patient after
attribution
Physical & Exercise £95,000 £380 £73,500 £290
Mental wellbeing &
Isolation
£42,000 £175 £54,500 £230
Safety & Welfare
Information/Advice
£29,000 £155 £13,000* £70
Health Education &
Nutrition
£7,000 £175 £400 £10
Dementia-specic
support
£34,000 £380 £25,000 £280
* Excludes new welfare support payments
YEAR END TO MARCH 2018 –
FORECASTED ‘SROI’
• c.£6.25 for every £1 invested, including
health service value (c.£1.22) and patient
health and well-being value (c.£5.03).
• After accounting for the attribution due to other
factors, the ‘attributable’ SROI is c. £2.80.
6. Findings: Health and Care system
PILOT YEAR ‘SROI’
• c.£4.30 of value is created for every £1
invested, including health service resource
value (c.£0.85) and patient health and well-
being value (c.£3.45).
• After accounting for the contribution of
other factors that affect patients’ health and
wellbeing outcomes (the attribution), c.£1.90
of attributable value is created for every
£1 invested

33Social Return on Investment
Patient health and wellbeing outcomes were
valued using a lower QALY value of £20,000 (see
section 5) as per NICE and BMA guidance. The
attributable SROI would increase if NICE’s higher
£30,000 QALY threshold is used: c.£2.25 in the
pilot year, and c.£3.30 in forecast to year end
March 2018.
Broader material outcomes:
long-term social care
Broader statutory outcomes were identified
with local authority stakeholders. These related to
reducing the need for patients to enter long-term
care, i.e. nursing homes and care homes. Royal
Borough of Kensington & Chelsea (RBKC) Adult
Social Care (ASC) offers around 88 care home
placements in the borough, and 309 placements
out of the borough. The average weekly rates
(defined through the West London Alliance) for
local authority placements include:
• Residential £555 – £689 per week (minimum
£28,860 per year)
• Residential for Dementia £675 – £783 per week
(minimum £35,100 per year)
• Nursing home: Frail £814.25 – £895 per week
(minimum £42,340 per year)
• Nursing home: for Dementia £819.25 – £895 per
week (minimum £42,600 per year)
There are 79 placements for dementia, and 152
placements for the physically limited.
Reducing the need for entering long-term care
is only likely to be a result for the patients who
maintain behaviour change and activation for
their own self-care, i.e. they choose to continue
actively accessing services after they complete
their sessions.
We have identified the proportion of referrals
with improved activation and motivation scores
(62%), which correlates to a c.12% reduction in
hospitalisations (see section four). If we use the
12% as a proxy for reduction in long-term care
needs, an estimate can be made of reduction in
long-term care need.
It was not possible to ascertain the probability
of a patient choosing to enter long-term care, as
a result of their long-term condition. However,
we can ascertain RBKC’s total number of care
placements for dementia and limiting long-term
illnesses (LLTI) as a proportion of the RBKC
population with those conditions. This provided an
indication of the proportion of patients with those
conditions entering care homes.
In summary, around 1 in 20 (5%) of over-65s with
dementia in RBKC are in a care home, and around
1 in 59 (1.7%) of over-65’s with a LLTI in RBKC are
also in a care home. Using this data, an estimate
of resource savings can be made: £33,000 in the
pilot phase, and forecasted as £48,000 for the year
ending March 2018 – equivalent to approximately
one placement.
However, we have not currently included this
provisional estimate within the SROI calculations
above, as we feel more primary research data
would be required. In addition, we would require
more data from Adult Social Care services, to
better understand the relationship between Self-
Care social prescribing and effects on home-based
social care needs.

Self-Care Social Prescribing34
7. Findings:
Working with
VCS providers
The Self-Care model has increased capacity for the
health care system to offer support services that
address non-medical health and wellbeing needs.
VCS providers in the social prescribing directory
have generally offered the right skills, experience,
and capabilities to provide the key services they
are contracted for.
However, capacity for some popular services can
at times be outstripped by sharp increases in
demand. This has also led to a reduction in the
availability of re-referrals for some patients who
may need that choice. HSCAs and Case Managers
are updated by WLCCG and KCSC co-ordinators
when this is the case.
For some other services, there has been lower
demand than first hoped, e.g. T’ai Chi, and
community lunches. These components of the
contract were re-negotiated and no longer offered
through Self-Care (Providers are always free to
continue provision outside of the model).
Making the most of available capacity depends on
two key characteristics of the model:
• Local VCS providers already deliver services as
part of their ongoing activities in the community
– (Self-Care supports only a small component of
providers’ existing service).
• Good contract administration by KCSC of the
network of VCS providers, in conjunction with
good HSCA line management by Age UK.
Self-Care co-ordinators at WLCCG and at KCSC
have fostered a strong partnership working
approach. Without this, the contract administrator
(KCSC) would have reduced credibility to
negotiate, drive, and where needed empower
the VCS network in the local system. Whilst
there are some elements of overlap and potential
competition between providers, we observed that
they recognised the strategic value of the model
in terms of sharing best practices, organisational
learning, and being more empowered as a ‘bloc’
to work with statutory services. In some cases, for
smaller providers, building a track record with a
prominent CCG has helped to build credibility with
other funders. However, it was difficult to ascertain
the long-term value of this across all providers, as
these were exploratory considerations during the
pilot phase.
Capacity
Effective use of capacity has partly relied on
good communication between practices and
providers, to avoid inappropriate referrals.
However, some communication about services has
been inconsistent from one practice to another.
This must be better driven, and to clear agreed
standards, by KCSC, WLCCG, and Line managers
of HSCAs (through Age UK).

35Social Return on Investment
Whilst the services may have been identified with
input from patient panels, the nature of demand-
led service selection – and therefore the capacity
that is brought in by provider – is reactive, rather
than predictive. Services do not necessarily need
to be pre-tested beforehand (e.g. by clinical trial),
though it is difficult to test a new service for how it
will cope with fluctuations in demand if it becomes
more popular than first anticipated. In turn, this
more acutely focuses the need for KCSC to
ensure personnel across the network of VCS
providers are deployed to join up capacity and
resourcing. Compared to the outset of the project,
KCSC has now more consistently tracked these
to better match the needs of referred patients as
quickly as possible.
Provider strengths
The core strength of the model is that VCS
providers are already geared-up to deliver the
services as part of their expertise and existing
programmes of activity. In addition, the VCS
organisations already work in partnerships with
other organisations or programmes in the area,
where resource-sharing can be seen as part of the
norm. For example, being able to share physical
space, materials, or equipment, has been a key
strength and source of flexibility when working
with VCS groups. At a local level this was brought
to the fore in the aftermath of the Grenfell Tower
tragedy in June 2017.
Furthermore, in comparison to other potential
models, it is also a strength that the contractor
organisation (KCSC) is from the voluntary and
community sector, as they can be held accountable
to VCS groups, as much as to WLCCG. This
forms an effective bridging organisation that can
be trusted by both sides, and empowers both
sides within the contract structure. It also gives
some license to KCSC to encourage learning and
knowledge-sharing even though there may be
elements of both competition and co-production
between the provider organisations.
Overall provision
Based on observation of one-to-one and group
activities, and personal feedback from patients,
we believe that the VCS provision is generally
person-centric, sensitive, and focused on the
individual’s situation, personality, and emotions.
Service providers are patient and discreet, and
patients have reported they feel enabled to
progress at a pace that is appropriate for their
condition. Adapting the pacing and flexibility of
the service is an important part of provision,
to help ensure patients are comfortable and feel
positive about the experience of the service.
Having the services available on a directory
and having exposure to the session workers’
expertise also helped to increase patient
awareness of health support options available
through community-based services. In some
cases, this resulted in forward referrals to other
services after the sessions were completed,
for example to occupational therapy.
Provision for highly frail and housebound patients
has been enhanced through traditionally ‘centre-
based’ services being able to provide some home
visits. For example, CAB Westminster and Age
UK advice and information service is so well-
used because they are spending more time than
anticipated meeting patients at their home.
We also recorded Net Promoter scores as part of
the research, to indicate how likely patients are to
recommend them to other people. On a scale of
0 to 10, where 0 is “Very Unlikely” to recommend,
and 10 is “Extremely Likely” to recommend,
patients give an average rating of 8 out of 10
(from a sample of 134 responses). This provides
an indication as to most patients’ perception of the
quality and appropriateness of service(s) provision.
Furthermore, around three-quarters of HSCAs
and Case Managers responding to surveys either
‘strongly agreed’ (50%) or ‘somewhat agreed’
(25%) that referrals were seen to in a timely
and efficient manner during the past six months.

Self-Care Social Prescribing36
Challenges of service delivery
The nature of older patients with higher levels
of frailty and complexity can sometimes add
complications to provision arrangements. For
example, some patients suffer from memory loss,
have emergency hospital admissions, or they
don’t hear when a provider arrives at their home
because they suffer from poor hearing or they are
asleep. It has been important that VCS providers
have some existing track-record with this group
and are sensitive to these issues and how to
manage them.
Providers have generally taken care to ‘get things
right first time’ with the patients. It has often fallen
on providers to spend time chasing up patients.
Providers also spend time chasing-up when more
detailed or more accurate case information is
required from Case Managers and HSCAs.
There have sometimes been misconceptions
or misunderstandings amongst some HSCAs
and Case Managers, about the practicalities or
exact purpose of a service. This has created
inappropriate or avoidable demand in some cases.
In these instances, it has fallen mostly on VCS
providers to identify a better alternative service or
pathway during or before the patient’s first session:
for example, in one case, recommending de-
cluttering and walking support instead of exercise
at home.
Around one in ten patients gave a net promoter
score of below 5 out of 10. Partly this has been
due to some patients having misconceptions about
service providers, and this is best addressed
during practice consultations. Feedback we
received also indicates that some patients
can be put off if: i) they have not understood
that their VCS provider is from a particular
ethnic background that they may have some
subconscious negative preconception about,
or ii) they feel the service is beneath their socio-
economic status/wealthier standing e.g. “that kind
of group isn’t for people like me”.
Many patients are also not used to attending
provision outside of the medical model and their
knowledge of what is available outside the medical
model can be limited. Many patients have an
expectation, built up over many years, that their
problems will be dealt with by the care system and
clinical professionals. This can be hard to break
down, and is reflected by many patients being of
an age and level of need where they feel more
comfortable in one-to-one services, than group
activities. Patients can also be very anxious or
embarrassed about being in a group with their
condition in ‘full view’.
Importantly, KCSC and WLCCG shifted the way
in which the Self-Care directory information was
communicated and structured, to be specifically
about the services, rather than about the providers.
This has been crucial in enabling HSCAs and
Case Managers to recommend appropriate
activities, rather than inadvertently bias choice
towards selecting providers. This also helps KCSC
to spread demand between different providers,
and manage capacity.
7. Findings: Working with VCS providers

37Social Return on Investment
Partner commissioners in local authorities who
are on the local ‘Transformation Steering Group’
are also interested in the potential of the Self-Care
social prescribing model. For example, delivering
home visits effectively, whilst helping residents feel
more included.
The Transformation Steering Group praised the
flexibility of KCSC and the providers, stating that
if Council services did what was set out in the
contract they wouldn’t have been able to achieve
as much – indicating that KCSC and the Provider
network are able to “go over and above.”
Transformation Steering Group members stated
that before Self-Care, the equivalent Case
Managers and HCSAs at that time were taking two
hours to get to know one patient, but didn’t have
the time to follow-up with in-depth work. Now, they
know they have six weeks to test different provision
and support through Self-Care with the input of
VCS providers rooted in the area.
The Transformation Steering Group stated key
outcomes that are most important for their work.
Firstly, whether the patient group feel safe and
supported to stay independent in their home,
and secondly, whether they feel supported to
increase their social inclusion. This was seen to be
important in terms of specific behaviours linked to
future health outcomes: for example, have they left
the house more; have they walked for ten minutes;
have they talked to more people?
The Group stated that their interest in Self-Care
is whether the testing approach helps patients to
develop secondary behaviours that may impact on
existing provision, e.g. day-centre visits, exercise to
maintain mobility, which in turn helps them sustain
independence and avoid the need for long-term
care or nursing homes.
In conjunction with this, a number of patients
in the target Tier groups might have personal
budgets for their care from the local authority.
These patients could be supported by Self-Care
to purchase some of these interventions through
their personal budgets, including paying for
transport to access services.
There may also be a wider role for other
stakeholders in the system, in particular, social
housing providers, but this requires careful
consideration. Some social housing landlords
already work in partnership with VCS providers
listed on Self-Care. Therefore, a balanced and
targeted approach is needed: on one hand there
may be a degree of duplication if social housing
providers are promoting and offering similar
services to tenants (but don’t require a referral). On
the other hand, housing providers may be offering
their own activities that may sit well within the
Self-Care directory. For example, Genesis (soon
to merge with Notting Hill housing), and Peabody
offer opportunities for older residents to share skills
and experiences with other older residents (the
V50 Project, co-funded by NESTA).
8. Programme
fit in the
local system

Self-Care Social Prescribing38
We feel the Self-Care model overall is an
increasingly effective way of working towards the
‘six core elements of the Whole Systems Model
of care’ (see Appendices part A).
Self-Care has helped to begin the transformation of
provision and cross-sector collaboration between
aspects of health and social care, and the VCS
sector. However, this will take time to be more
fully embedded in practice and mindsets of health
and social care professionals, and much work
still needs to be done, especially as the target
patient groups will grow in number and have
changing needs. This implies the model needs to
be prepared for higher demand and ever-changing
needs in the foreseeable future. Therefore, it
should be managed as a live, dynamic model.
We recommend that future planning and
considerations for the Self-Care model are
underpinned by Envoy’s separate analysis of
process effectiveness. Part E of the Appendices can
also provide a helpful reference point in this case
(Strengths, Limitation, Opportunities, Challenges)
derived from our process effectiveness analysis.
We recommend a number of immediate actions,
and medium to long-term actions, as follows:
Immediate actions
For KCSC
• Build information adequacy guidance and
compliance, for both referral information
(SystmOne) and Charity Log.
• Develop appropriate minimum service quality
and information/feedback standards, using input
of practice staff, clinicians, providers and patient
feedback e.g. from Envoy surveys, Charity Log.
• Tighten full cost recovery with VCS providers
and new services, through: i) slight adjustments
between up front block components and later
spot payments, ii) a simple, fair approach for unit
costs to include resource required for ongoing
learning network costs, and iii) a simple and fair
approach for discontinued services who have had
to resource setting-up and administrative costs,
but who have not been provided with a minimum
number of referrals within a set period e.g. first
four months.
• Plan for expanding services more formally to
Tier 1, where there is a greater potential for
preventative effects on poor health.
• Better record the rate at which GP consultations
are avoided. This could be achieved by linking
patient ID number to self-care feedback at GP level.
• Improve reach and build capacity to deliver more
services to more patients, but without sacrificing
quality of patient experience and impact on
quality of life. For example, group activities are
not necessarily the ideal solution, compared to
slightly extending the initial number of one-to-one
sessions whilst reducing re-referrals.
9. Recommendations

39Social Return on Investment
For WLCCG
• Consider options for increasing from six initial
sessions to eight sessions, but reducing
re-referral options, e.g. 2–3 re-referral sessions
only. Or introduce flexibility, e.g. offer 6 to 10
sessions only.
• Expand services more formally to reach
‘high-risk’ Tier 1, and consider targeting priority
BAME patients.
• Ensure better integration and synthesis of
information between ‘SystmOne’ and ‘Charity
Log’ for input back to patient Care Plans.
• Build feedback loops by sharing relevant
findings with wider WLCCG internal and external
partners, other CCGs, and professional bodies,
e.g. Royal College of General Practitioners.
• Increase marketing internally at practices and
within MCMW, and market more broadly to local
tenants through other new partners, e.g. social
housing landlords who want to sustain tenancies.
For frontline staff
• HSCA and Case Manager to build their
confidence and compliance with using Charity
Log at practice-level as much as possible.
HSCAs and Case Managers to remain
responsible for attending refresher sessions,
feedback meetings, and provide learning and
information updates.
Medium to long term actions
For KCSC
• Ask new VCS providers to demonstrate evidence
of the health and wellbeing impact of their service
before being selected for the directory.
• Patients could be offered a bundle of
complimentary activities from the directory within
their sessions quota, and a ‘Patient Exchange’
function could be introduced, where unused
sessions from patients who drop out are offered to
other existing service-users where most needed.
• Explore how ‘Personal Budgets’ can be
best allocated, with support and input from
Transformation Steering Group.
• Proactively balance the contract structures for
certain services, for example by having a small
up-front component in block structure, and
thereafter spot contracts.
For WLCCG
• Roll-out communications for awareness-raising
amongst the rest of the clinical and reception
staff about the success and impact of Self-Care
services in supporting patient goals.
• PAMs survey wording can be inappropriate for
various conditions – this may need a simpler
alternative version to be in place, rather than
having no follow-up measures at all.
For frontline staff
• Patient perceptions and concerns about the
socio-economic background of other service
users, and ethnic background of providers need
to be addressed at initial consultation by Case
Manager or HSCA, as this will help to flag risk of
patient drop-out.
• Consider implications if affordable transport
provision increases in the local area, the potential
impact on demand should be planned for carefully.

Self-Care Social Prescribing40
Part A
Six core elements of the Whole Systems
model of care
Part B
SROI: Accounting for Impact
Part C
SROI calculation sources
Part A
Six core elements of the Whole Systems model
of care
The Whole Systems model of care specifies six core
elements for care planning and provision. The six
elements are integrated into My Care, My Way, and
therefore also apply to Self-Care social prescribing.
The six elements specify that all models of health care
provision should:
1. Be centred around the holistic needs of the service
users and their Carers, involving them in all decisions
while providing with simpler access and a shared
care plan.
2. Be personalised and tailored to changing health as
well as social needs, covering planned as well as
reactive needs and one that empowers self-care.
3. Have a clear point of accountability (both for clinical
and non-clinical outcomes) with a core team that
reflects user’s needs.
4. Be supported by a number of local operational
whole-systems bases, where joint teams work
on a day-to-day basis coordinating the care and
tracking outcomes.
5. Help co-ordinate the services (via the base) as
needed from different organisations, on behalf of the
service users and their Carers.
6. Be brought together by an accountable partnership of
organisations commissioned to deliver a single set of
outcomes with shared systems and incentives.
( summarised from WLCCG Business Plan and service specifications
for Whole Systems, 2015)
Part B
SROI: Accounting for Impact
To avoid over-claiming of value, the SROI analysis
measured impact with a range of adjustments. This
was also informed by triangulating different primary
data (patient surveys and interviews) with secondary
research elements to help establish impact credibly.
We identified ‘attribution’, which is a measure of the
proportion of outcomes that is directly attributable to
Self-Care, i.e. the Self-Care service model can take
credit for. It acknowledges that, although the calculations
already consider the outcomes that would have occurred
without Self-Care (through deadweight estimations –
see below), the remaining outcomes are nonetheless
due to the work of a number of different people and
organisations, and are not solely due to Self-Care. In
this SROI, attribution was determined through surveys of
patients, cross-referenced with interview feedback.
We also assessed ‘displacement’, which is a measure
of whether some of the outcomes observed have not
actually been created, but have been moved elsewhere.
One example is where a fall in crime is recorded, but
some or all of the reduced crime has actually relocated
to another area. For the outcomes in this SROI,
displacement is not deemed to be an issue; one client’s
improvement in health and well-being does not come at
the expense of another individual.
SROI also requires assessment of impact ‘drop off’,
if claiming future longer-term outcomes beyond a year.
This is because some outcomes may last longer for
individuals over multiple years, but not necessarily to the
same magnitude, i.e. the strength of impact drops off in
year two and year three, after an intervention. However,
as the impacts on patients are short-term i.e. less than
one year, the drop off in our calculation is effectively 0%.
Part D
Survey design
Part E
Strengths, Limitations, Opportunities, Challenges
Part F
Key references
Appendices

41Social Return on Investment
The specific adjustments are summarised
as follows:
• Attribution: Is calculated from self-reported patient
survey responses. In terms of scaling,
a 5-point scale for level of attribution agreement was
used (‘None of it’, ‘A little of it’, ‘Some of it’, ‘Most of
it’, ‘All of it’) for different outcome categories, and
stakeholder responses were converted to 0–1 scale
(0–100%).The average results provided attribution
score of c.23% for subjective patient outcomes.
• Displacement: we deemed this to be 0%,
because improving the activation and health of
the patients should not negatively impact other
material stakeholders.
• Drop-off of impact and discount rates: The benefit
period for patients does not exceed one year in
our model, and therefore a drop-off rate and a
discount rate for future impact is not required for
our calculations.
Deadweight considerations
‘Deadweight’ is a measure of what would have
happened in the absence of the intervention being
evaluated. It is a similar concept to counterfactual, and
acknowledges that observing and measuring change
does not in itself tell us that the change only happened
because of the intervention.
Within our analysis, we focus on how the issue
of deadweight affects healthcare resources in the
following ways:
• Without the ‘in-practice’ role of HSCAs and Case
Managers, GPs would have to use more hours dealing
with non-medical consultations that could otherwise be
referred through social prescribing.
• Without the ‘in-practice’ role of HSCAs and Case
Managers, GPs would have to use more hours
researching appropriate support services in the
community, in addition to consultation hours.
• A proportion of MCMW patients would have been
referred to other services by HSCAs and Case
Managers that are not on the social prescribing
directory, and so those patients may have experienced
similar outcomes.
• Without the social prescribing model and directory,
HSCAs and Case Managers would have fewer options
available for patients, and would have to use more
hours on research and applications support for those
referred patients, in addition to the consultation hours
they also provide.
• Currently hospitals don’t refer their patients to
social prescribing services, but may refer to other
services to help with recovery, e.g. British Red Cross
wheelchair loan.
We assume in our modelling that whilst some patient
needs become more familiar to staff, who are then able
to deal with them more efficiently, over the long-term
this is balanced out by: i) new patients with new needs
accessing Self-Care, and ii) staff churn and the resulting
loss of expertise.
Our model also assumes that the proportion of patients
who may have improved without any support from
GPs or social prescribing or any additional services,
is cancelled out by the proportion of patients whose
health would have deteriorated without their social
prescribing referral.
We have used a 16% deadweight / counter-factual
measure to further reduce the amount of impact
claimed, based on interview feedback about the
likelihood that outcomes would have happened anyway,
and cross-referenced with patient survey feedback for
those who felt the service did not add to the wellbeing
outcomes they had experienced anyway. This is
effectively a proportion of 1 in 5 patients who may
have experienced the same outcomes anyway, minus
an assumed proportion (20%) to account for patients
who are housebound and bedbound. Housebound
and bedbound patients are unlikely to access similar
services or support offered outside of Self-Care.

Self-Care Social Prescribing42
Part C
SROI calculation sources
Outcome
Proxy
value
Source of
proxy value
Average
amount of
change in
outcome or
incidence Evidence of change
Literature reference for
change indicator
GP practice level
GP hours diverted:
social prescribing
consultations
£60.39
per hour
WLCCG
average
annual cost,
including
London
weighting, NI
and pension:
2017/2018
0.25 hours x 2
consultations
Actual number of social
prescribing consultations
not requiring GP time
Consultation time length
based on MCMW
business case
GP hours avoided
from reduced need
0.25
hours x 15
consultations
Case Managers and
HSCA survey response,
combined with WLCCG
data for average half year
number of GP visits per
My Care, My Way patient
Consultation time length
based on MCMW
business case
Case Manager &
HSCA research
and support
hours diverted:
social prescribing
consultations
£23.40
per hour
Mean of
WLCCG
HSCA and
Case Manager
annual cost,
including
London
weighting, NI
and pension:
2017/2018
0.75 hours x 2
consultations
Case Managers and
HSCA survey response,
combined with Actual
number of social
prescribing consultations
Research time length
based on Case Manager
and HSCA survey
response and qualitative
interviews
Case Manager &
HSCA research
and support hours
avoided from
reduced need
0.75
hours x 15
consultations
Case Managers and
HSCA survey response,
combined with WLCCG
data for average half-year
number of GP visits per
My Care, My Way patient
Research time length
based on Case Manager
and HSCA survey
response and qualitative
interviews
Hospitals level
Reduced A&E
incidence
£142
WLCCG
acute hospital
incidence
and costs
per MCMW
patient, Apr
2016–March
2017
0.116
reduction
PAM score correlation,
for patients using relevant
service category
Insignia Health (PAM
scoring system)
Reduced hospital
spells
£1,734
WLCCG
acute hospital
incidence
and costs
per MCMW
patient, Apr
2016–March
2017
0.116
reduction
PAM score correlation,
for patients using relevant
service category
Insignia Health (PAM
scoring system)
Appendices

43Social Return on Investment
Outcome
Proxy
value
Source of proxy
value
Average
amount of
change in
outcome or
incidence Evidence of change
Literature reference for
change indicator
(Hospitals level
continued…)
Reduced
outpatient visits
£72.34
WLCCG acute
hospital incidence
and costs per MCMW
patient, Apr 2016–
March 2017
0.116
reduction
PAM score correlation,
for patients using
relevant service
category
Insignia Health (PAM
scoring system)
Other statutory agency level
Avoided need
for entering
long term care
placement with
local authority
£42,341
Annual care
placement cost
for Royal Borough
of Kensington &
Chelsea, Nursing
home for Frail
0.017
reduction
Number of placements
in local authority care
for dementia and long
term limiting illness
as proportion of local
population with those
conditions
Adult Social Care (ASC)
and Health Scrutiny
Committee – Report of
Interim Executive Director
for ASC May 2017,
combined with ONS
data/RBKC factsheet
extrapolated to 2017/18
Housing re-let
cost avoided
£2,909
Average cost for
social housing
tenancy failure (The
Ferry Project, Octavia
View SROI, reference
to Ofce for Deputy
Prime Minister
estimate 2005), linked
to 2% ination
0.017
reduction
Number of placements
in local authority care
for dementia and long
term limiting illness
as proportion of local
population with those
conditions
Adult Social Care (ASC)
and Health Scrutiny
Committee – Report of
Interim Executive Director
for ASC May 2017,
combined with ONS
data/RBKC factsheet
extrapolated to 2017/18
Patient level
Reduced
physical pain/
discomfort
(improved
mobility)
£20,000
Full QALY from
National Institute of
Health and Clinical
Excellent, and British
Medical Association,
Exploring the cost
effectiveness of early
intervention and
prevention (2017)
0.028
reduction
Patient survey indicator
based on EQ-5d
questionnaire and linked
to corresponding QALY
average improvement
scores
Devlin, Shah et al,
Valuing health-related
quality of life: An EQ-5D-
5L value set for England,
in Health Economics
journal (2016)
Avoided
depression
£20,000
Full QALY National
Institute of Health and
Clinical Excellent,
and British Medical
Association, Exploring
the cost effectiveness
of early intervention
and prevention (2017)
0.056
improvement
QALY linked to Patient
survey indicator
based on PHQ9
questionnaire and linked
to corresponding QALY
average improvement
scores, with EQ-5d
equivalent thresholds
Jia & Lubetkin,
Incremental decreases
in quality-adjusted life
years (QALY) associated
with higher levels of
depressive symptoms for
US Adults aged 65 years
and older, in Health and
Quality of Life Outcomes
(2017)

Self-Care Social Prescribing44
Appendices
Outcome
Proxy
value
Source of proxy
value
Average
amount of
change in
outcome or
incidence Evidence of change
Literature reference for
change indicator
(Patient level
continued…)
Improved self-
efcacy/self-
worth*
£704
Sub-proportion of
Mental Wellbeing
QALY; Mental
wellbeing comprising
0.352 of a Full QALY
(Centre for Mental
Health, The economic
and social costs of
mental illness, 2003)
0.03*
improvement
PAM score change
New Economy
Manchester (2012)
Social Value:
Understanding the wider
value of public policy
interventions (2012)
Retaining
independence*
£352
Sub-proportion of
Mental Wellbeing
QALY; Mental
wellbeing comprising
0.352 of a Full QALY
(Centre for Mental
Health, The economic
and social costs of
mental illness, 2003)
0.11*
improvement
Patient survey indicator
based on ASCOT
questionnaire and linked
to corresponding QALY
average improvement
scores
Based on ranking of
older service user
outcomes from Bield,
Hanover, and Trust
housing, SROI on Stage
3 housing adaptations
and Very Sheltered
Housing (2012)
Reduced
social isolation/
loneliness*
£1,173
Sub-proportion of
Mental Wellbeing
QALY; Mental
wellbeing comprising
0.352 of a Full QALY
(Centre for Mental
Health, The economic
and social costs of
mental illness, 2003)
0.02*
reduction
Patient survey indicator
based on ‘Warwick-
Edinburgh Mental
Wellbeing Scale’
questionnaire and linked
to corresponding QALY
average improvement
scores
New Economy
Manchester, Social
Value: Understanding
the wider value of public
policy interventions
(2012)
Feeling more
valued by
others*
£235
Sub-proportion of
Mental Wellbeing
QALY; Mental
wellbeing comprising
0.352 of a Full QALY
(Centre for Mental
Health, The economic
and social costs of
mental illness, 2003)
0.044*
improvement
Patients reporting
outcome in survey and
linked to corresponding
QALY average
improvement scores
Assumed sub-proportion
based on New Economy
Manchester, Social
Value: Understanding
the wider value of public
policy interventions
(2012)
Carer level
Not
included
Not included, low
referrals
Not
included, low
referrals
Not included, low
referrals
Not included, low
referrals
* Average amount of change pro-rated by proportion of population in each service category to whom change applies

45Social Return on Investment
Part D
Surveys
There is a significant methodological difference
between i) survey questions asked at the beginning
and end of the programme, with respective results
between the two compared; and ii) survey questions
where respondents are asked how they feel now, and
also asked to recall how they felt previously (this can
be termed as a Retrospective Post-then-Pre approach).
Both approaches have their advantages. The first
approach is more common, particularly among social
science research, and it does not rely on participants
recalling how they felt some time in the past. The
second approach can avoid Response Shift bias, which
occurs when a participant uses a different frame of
reference for understanding a question. For example,
it might be that an individual thinks they are good at
‘Dealing with Problems’. They then learn more effective
ways of dealing with problems, and realise that they are
actually not as ‘good’ as they thought they were. They
might end up scoring themselves the same before and
after the programme, even though they have improved,
because their understanding of how to ‘Deal with
Problems’ effectively has changed.
15
As a general rule,
the Pre/Post method may understate any change, while
the Retrospective Post-then-Pre method may overstate
it. When it is possible to take the different approaches
together (e.g. PAM scores and additional Retrospective
survey), they can give a better indication of change.
Patient survey
Survey versions can be made available on request.
The full list of patient survey questions are summarised
below. Some questions were not relevant or appropriate
for specific services; other questions were specific to
only one or two services. The pro forma was adapted
to the outcomes relevant to the specific service themes
(see section two of the report).
Certain questions are drawn directly from validated
health questionnaires, in particular EQ-5d, regarding
physical pain (using the scoring system designed by
EuroQol Research Foundation), PHQ9 indicator relating
to depression (developed by Columbia University and
widely used in primary care settings), the Warwick-
Edinburgh Mental Wellbeing Scale regarding isolation
and loneliness, and ASCOT quality of life measures,
regarding independence (developed by the University
of Kent).
Patients were asked to provide responses to the
questions for their situation now, and then to provide
their responses for their situation before receiving
the service. Each pro forma was pre-filled with a
generic anonymised ID number linked to the service(s)
accessed by that patient.
Response options about frequency were accompanied
by colour-coded visual aids as follows:
Not at all A little Moderately
Quite a lot Extremely
Response options about (dis)Agreement were
accompanied by colour-coded visual aids as follows:
(Question statement…)
Strongly agree Agree
Neither agree nor disagree
Disagree Strongly disagree
The wording of the questions and response scales
remained consistent for all pro forma as follows below,
except for surveys with dementia patients, which did not
require reflective recall questions, and were simplified
in question design to align with i) the objectives set out
in the National Dementia Declaration from Dementia
Action Alliance, and ii) British Medical Journal Open
research by Spencer, K. et al (2017):
1. Please indicate if the survey is being completed
either:
About myself / On behalf of someone else
(please write your relationship)
2. How likely would you be to recommend _______
service(s) to a friend/someone you know?
0–10 scale where 0 is ‘Not at all likely’ and 10 is
‘Extremely Likely’
3. In general how would you rate your health?
Excellent / Very good / Good / Fair / Poor
4. Please think about any change in your health
over the past year. To what extent do you
think this change is because of the service(s)
mentioned?
All of it / Most of it / Some of it / A little of it / None of it
15
For more information on the two approaches, see Program Development and Evaluation. Using the Retrospective Post-then-
Pre Design, Quick Tips #27. University of Wisconsin-Extension, Madison, WI. © 2005
uwex.edu/ces/pdande/resources/pdf/Tipsheet27.pdf

Self-Care Social Prescribing46
5. I feel motivated to take care of my own health and
medication needs
Strongly agree / Agree / Neither Agree nor disagree /
Disagree / Strongly disagree
6. I can live as independently as I want
[based on ASCOT]
Strongly agree / Agree / Neither Agree nor disagree /
Disagree / Strongly disagree
7. My living conditions help me to live in dignity
Strongly agree / Agree / Neither Agree nor disagree /
Disagree / Strongly disagree
8. There are enough people I personally feel close to
[based on De Jong Gierveld/SWEMWBS]
Strongly agree / Agree / Neither Agree nor disagree /
Disagree / Strongly disagree
9. When accessing health care support I feel I’m
valued just as much as other people like me
Strongly agree / Agree / Neither Agree nor disagree /
Disagree / Strongly disagree
10. I use techniques I have learned to help me
remember things more easily
Strongly agree / Agree / Neither Agree nor disagree
/ Disagree / Strongly disagree
11. How much do you feel in pain or discomfort
[based on EQ-5d]
Not at all / A little / Moderately / Quite a lot /
Extremely
12. How much do you feel limited in what you can
do [based on SF 12]
Not at all / A little / Moderately / Quite a lot /
Extremely
13. How often have you been bothered by the
following problem: Feel down, depressed
or hopeless
[based on PHQ9]
Not at all / Several days / More than half the days /
Nearly every day
14. How often have you been bothered by the
following problem: Feeling anxious
[based on ICECAP-A & PHQ9]
Not at all / Several days / More than half the days /
Nearly every day
15. In the past 3 months, indicate roughly how often
you tended to visit your local GP clinic:
Once a week or more / Once a fortnight / Once a
month / Less than once a month / Did not use
16. In the past 3 months, indicate roughly how often
you needed emergency admission /A&E:
Once a week or more / Once a fortnight / Once a
month / Less than once a month / Did not use
17. In the past 3 months, indicate roughly how
often you needed other treatment e.g. specialist
surgery, mental health unit:
Once a week or more / Once a fortnight / Once a
month / Less than once a month / Did not use
Please describe any further reasons for this
[open text]
[Welfare payments and Carer relief]
18. If relevant to you, did the service help you to
access any extra financial welfare support e.g.
benefit payments or allowance to support your
situation?
If yes*, please indicate payment support received £
[Pound numerical value ] per year income
Please describe any further reasons for this
[open text]
19. If you have a carer or relative caring for you, to
what extent was the service helpful in freeing
up your carer/relative’s time to arrange other
things, or take a break?
Extremely helpful / Moderately / A little / No change
20. If you have further comments about the
service(s) you received, please write here
[open text]
Appendices
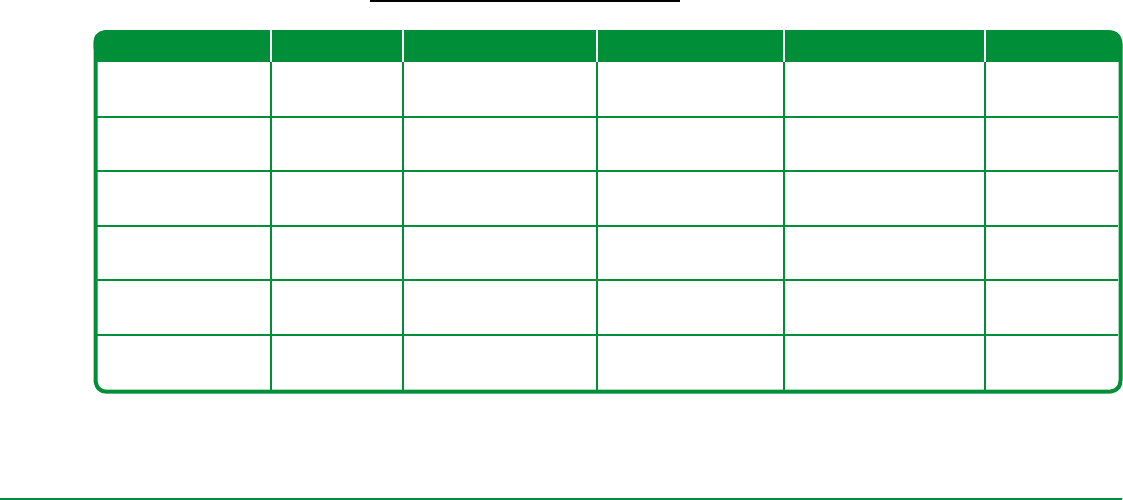
47Social Return on Investment
Case Manager and HSCA survey
The following questions regarding referred patients
were configured onto online survey software and
completed online by Case Managers and HSCAs.
Q1. Are you a HSCA or Case Manager?
I am a HSCA / I am a Case Manager
Q2. Which is the main practice or clinic at which
you are based?
[open text]
Q3. In your opinion, approximately what proportion
of patients referred onto Self-Care services go
on to improve self-activation about taking care
of their own health?
Tier 1 patients [0–100% scale]
Tier 2 patients [0–100% scale]
Tier 3 patients [0–100% scale]
Q4. In your opinion, roughly how long do you think
this improvement – if any – generally lasts for
patients referred onto Self-Care services?
Tier 1 patients
[Up to 1 month/Up to 3 months/Up to 6 months/Up
to 1 year/1–2 years/Rest of their lives]
Tier 2 patients
[Up to 1 month/Up to 3 months/Up to 6 months/Up
to 1 year/1–2 years/Rest of their lives]
Tier 3 patients
[Up to 1 month/Up to 3 months/Up to 6 months/Up
to 1 year/1–2 years/Rest of their lives]
Q6. If the Self-Care directory information and
referral model were not in place, how many
more hours per week do you estimate your
practice GP(s) would have to work on the
non-medical needs of these related patients’?
Number of hours per week per GP [Number]
Number of GPs at practice [Number]
Q7. If the Self-Care directory information and referral
model were not in place, how many more hours
per week would You have to work on researching
similar local voluntary and community services
to refer patients to?
Hours per week [Number]
Much better Somewhat better About the same Somewhat worse Much worse
Tier 1
Physical health
Tier 1
Mental wellbeing
Tier 2
Physical health
Tier 2
Mental wellbeing
Tier 3
Physical health
Tier 3
Mental wellbeing
Q5. In your opinion, how would you rate the recent physical health and mental wellbeing of patients referred
onto Self-Care activities, compared to before their referral: [Select a box]

Self-Care Social Prescribing48
Q9. In your opinion, how would you rate the
possible preventive effects of Self-Care
services on longer-term health conditions
of referred patients?
Tier 3 patients
[No effect / Slight effect / Moderate effect / High
effect / Very high effect]
Tier 2 patients
[No effect / Slight effect / Moderate effect / High
effect / Very high effect]
Tier 1 patients
[No effect / Slight effect / Moderate effect / High
effect / Very high effect]
Q10. What are the main types long term conditions
being dealt with at your practice for +65 year
olds? Please describe:
[open text]
Q11. In your opinion, approximately what
percentage of referred patients do you feel
have gone on to experience the following
outcomes, after completing their Self-Care
sessions? Please rate for each statement,
and each Tier of patient.
Note you may leave blank or ‘0%’ responses
where appropriate: [Select a box]
If you have an example, please describe below:
[Open text]
Q12. If you have any other important comments,
please write them below:
[Open text]
Appendices
Strongly
Agree
Somewhat
Agree
Neither Agree
nor Disagree
Somewhat
Disagree
Strongly
Disagree
Referrals have been seen to in a timely and
efcient manner during the past 6 months
Appropriate feedback about patient
progression is accessible for me
Clear minimum standards are in place for
services to ensure appropriate quality of
patient experience
Self-Care service providers often call me to
request further information about referrals
Clinical staff at the practice(s) where I work
have a clear appreciation of the outcomes
achieved by Self-Care services
Clinical staff at the practice(s) where I
work view Self-Care service providers as
partners in their work
Q8. Thinking about Self-Care services in general, please select one response that best describes how much
you agree or disagree with each statement below: [Select a box]
Tier 1
patients
%
Tier 2
patients
%
Tier 3
patients
%
Stopped all need for
visit or call to GP
Stopped all need for
emergency admission
Stopped all need for
tertiary care
Slightly reduced need
for visit or call to GP
Slightly reduced
need for emergency
admission
Slightly reduced need
for tertiary care

49Social Return on Investment
Part E
Strengths, Limitations, Opportunities, Challenges
This section summarises key strengths, limitations,
opportunities, and challenges of the Self-Care model in
generating patient activation and bringing knowledge
to patients about VCS services in the community. The
summary tables are based on i) analysis of feedback
from service providers, patients, and practice-based GP,
Case Managers, and HSCAs, as well as ii) our research
observations from several service sessions – including
one-to-one befriending, and also group activities (Men’s
club, and cultural group activities for dementia patients).
Strengths of the model
• Contracting a well-positioned co-ordinating VCS
organisation that is accountable to both VCS
organisations as well as to the CCG has been key, to:
i) enable agile and flexible commissioning, whilst
supporting some frontline administrative functions
ii) enable GP practices and patients to reach more VCS
services appropriate to their needs (and thus work
more effectively with their time)
iii) generate trust between providers, health services,
patients, and stakeholders, and
iv) foster cross-sector collaboration to better join
up resources.
• The role of the HSCA and being based at a clinic/
surgery practice, is crucial in assisting broader
patient choice; HSCAs are equipped with richer
information and knowledge about options across
the local system that can more appropriately meet
patients’ non-medical health and wellbeing needs.
Line management by an external specialist VCS
organisation such as Age UK has supported frontline
administration. This might potentially reduce human
resource tensions if clinical managers were previously
having to line managing them.
• New partnership working and cross-sector
collaboration between health, VCS, and statutory
services, has improved capacity across the
health and social care system to meet patient
needs more appropriately.
• There have been some significant resource savings to
care services, especially GP time and Case Manager
time spent on care co-ordination, planning, and research.
• It has enabled broader reach to patients in need, for
VCS services that support frontline health care.
• It enables patients, especially those who are
housebound or bedbound, to live as independently
as they wish for longer; and better support patients to
decide to move to long term care on their own terms,
or in some cases to die in the place they wish.
Limitations of the model
• Tier 3 are often ‘too far progressed’ with their conditions
to transform their health, even though activation or
motivation might improve in the short-term.
• Tier 1 are not always offered services, creating a
gap in a preventive approach; there may be more
sustained resource savings from targeting longer-term
outcomes for this group, as indicated by HSCAs and
Case Manager survey, before their condition escalates
to Tier 2.
• Six sessions are not enough in many cases to
encourage sustained change in habits – although it is
difficult to balance the ‘introductory taster’ rationale to
the service vs becoming perceived as a frontline service.
Evidence suggests Eight consecutive sessions to
be more effective to embed behaviour change for the
majority of patients (Handbook of Psychotherapy and
Behaviour Change, M. Lambert, 2013).
• Clear minimum standards are not in place for:
- Quality of service provision/care
- Information adequacy provided on referral forms,
or Charity Log (and subsequent usage of this for
patient Care Plans)
• Patients could be offered a bundle of different
complimentary activities within their sessions, and a
‘Patient Exchange’ function could be introduced, where
unused sessions from patients who drop out are offered
to other existing service-users where appropriate.
• Contract and payment structure (e.g. block payment
in advance, or ‘pay-per-play’ spot contract) with each
VCS provider can influence their up-front resource and
capacity risks.
• It is a demand-led model rather than clinically tested
services, and so there is some churn when low service
demand leads to discontinuation; in which instance, a
clear criteria or policy for discontinuation needs to be
fully understood and agreed by all partners.
• Charity Log is inconsistently utilised by HSCAs and
Case Managers; there does not appear to be strong
line management of this at practices, or compliance
in place, about regular use/practice-setting. Some of
this is down to churn of staff, and some wider lack of
confidence across all staff about its use.

Self-Care Social Prescribing50
• There is significant variation in effective
communication and feedback between certain
practices and providers about patient situation, and
patient progression.
• There can be information overload for both patients
and HSCAs and Case Managers, when they are
getting to grips with all the services and how they really
work, and given the plethora of other care pathway
information and service contact details they receive.
However, HSCAs and Case Managers still hold a
responsibility to attend to refresher meetings, feedback
meetings, and learning and information updates.
• The range of services and how they are delivered
may need to be refined with regards to reaching older
patients from broader BAME and LGBT backgrounds.
Opportunities for the model
• Self-Care is clearly a new innovative delivery model
that works in many instances, and potentially reduces
duplication between health and social care, and
VCS providers
• It can support reduction in wellbeing inequality, and
especially improve patients’ sense of being valued by
the care system.
• Can help explore new co-investment models with
other statutory services e.g. Transformation Steering
Group, or making use of Personal Budgets.
• Increases awareness and education amongst clinical
staff about cross-sector collaboration, and the effect
of VCS services on supporting patient outcomes;
Self-Care is helping to slowly build culture change
amongst clinical and health professionals about this
collaboration and also about non-medical and social
variables affecting health and wellbeing.
• In terms of some forms of medication (e.g. anti-
depressants, pain management medication), Self-
Care can help to identify alternative options to avoid
inappropriate medical interventions.
• Self-Care can help diversify client groups (e.g. more
men, BAME patients, LGBT patients), and also
supports the socialising and destigmatising of certain
conditions such as dementia or mental health.
• Correct and appropriate quality of information could
potentially be shared between referrers and providers
(two-way), to reduce waste and optimise activities
that best meet Care Plan goals; this would also be
enhanced by sharing parts of the patient Care Plan
where appropriate and consented to.
• Improve ongoing feedback and communication
between providers and practices; this requires
appropriate use of Charity Log (and better integration
with System One).
• Improved word-of-mouth and awareness-raising about
services to target clients.
• Continuous improvement practices for CCG, KCSC
and VCS providers, especially through shared
learning, action-setting, and target-setting, which they
remain responsible for.
Challenges for the model
• There will likely be ongoing changes to criteria for
provider selection as the model grows, and both
demand levels and needs change.
• Having to balance demand-led vs evidence-led services;
both have their advantages and disadvantages.
• Transport / Mobility barriers and under-funding are
prevalent in the local system.
• Patient perceptions about socio-economic class (their
own vs service target group) and ethnic background
can sometimes become a barrier, or lead to reluctance
to engage.
• The need to reduce patient drop-out.
• Awareness vs misconceptions amongst rest of clinical
and reception staff about the success and impact of
Self-Care services in supporting patient goals, which
is linked to required improvements to feedback-
sharing between SystmOne and Charity Log.
• PAMs survey wording can be inappropriate for various
conditions – this may need a simpler alternative
version to be in place, rather than having no follow-up
measures at all.
• Effective compliance regarding line management of
HSCAs by Age UK, to reduce potential for conflict of
interest with Age UK services.
Appendices

51Social Return on Investment
Part F
Key references
Age UK (2012) The Social Prescribing Pilot Project, Age
Concern Support Services – Yorkshire and Humber,
London UK
Bield Housing, Hanover Scotland Housing Association,
Trust Housing & Envoy Partnership (2012) SROI of
Stage Three Adaptations and Very Sheltered Housing,
Edinburgh UK
British Medical Association, (2017) Exploring the cost
effectiveness of early intervention and prevention,
London UK
Centre for Mental Health (2003) The economic and
social costs of mental illness, London UK
City and Hackney CCG and the Health Foundation
(2014) Shine 2014 final report – Social Prescribing:
integrating GP and Community Assets for Health,
London UK
Dementia Action Alliance (2011) National Dementia
Declaration for England, UK
Department of Health (2010) Improving Care and
Saving Money: Learning the lessons on prevention and
early intervention for older people, London UK
Devlin, N. J., Shah, K.K. et al (2016) Valuing health-
related quality of life: An EQ-5D-5L value set for
England, Office for Health Economics with the University
of Sheffield, in Journal of Health Economics, UK
English Partnerships (2008) Additionality Guide –
Method Statement Third Edition, UK
EuroQol Foundation (2012) EQ-5d 5 domain
questionnaire, Rotterdam, the Netherlands
HM Treasury (2011) The Magenta Book: Guidance for
Evaluation, London UK
Insignia Health (2015) Application of the Patient
Activation Measure to Improve Health Outcomes,
Portland Oregon, USA
Jia, H. & Lubetkin, E.I. (2017) Incremental decreases
in quality-adjusted life years (QALY) associated with
higher levels of depressive symptoms for U.S. Adults
aged 65 years and older, in Health and Quality of Life
Outcomes, USA
Lambert, M. (2013) Handbook of Psychotherapy and
Behaviour Change, Wiley, New York USA
Mid Essex Hospital Trust (2013) Dementia Carers
Questionnaire, Cathy Geddes Chief Nurse, Essex, UK
Ogden, J. (2017) QALYs and their role in the NICE
decision-making process, in Prescriber, UK
National Institute of Health and Care Excellence
(2017) The NICE menu of general practice and clinical
commissioning group indicators, London UK
New Economy Manchester (2012) Understanding
the Wider Value of Public Policy Interventions,
Manchester, UK
NHS Improvement (2017) The incidence and costs
of inpatient falls in hospitals, London UK
NHS Newcastle Gateshead CCG (2017) Ways to
Wellness Social Prescribing Scheme, The Learning
Environment, Newcastle UK
North West London CCG, LSE PSSRU and Nuffield Trust
(2015) Putting Integrated care into Practice: The North
West London experience, London UK
Pfizer (1999) PHQ-9 Overview
Sheffield Hallam University & Centre for Regional
Economic and Social Research (2013) From
dependence to independence: emerging lessons from
the Rotherham Social Prescribing Pilot, Rotherham UK
Royal Borough of Kensington and Chelsea (2017)
Adult Social Care and Health Scrutiny Committee –
Report of Interim Executive Director for Adult Social
Care and Public Health, London UK
Royal Borough of Kensington and Chelsea (2016)
Report by the Director for Housing: KCTMO Board,
Tenants Consultative Committee, Housing and Property
Scrutiny Committee January 2016, London UK
Royal Borough of Kensington & Chelsea, Baker, D.
(2011) Census 2011 RBKC, Policy and Partnerships
Unit, London UK
Royal Borough of Kensington & Chelsea (2008) Impact
of Population Change on Limiting Long Term Illness:
Aged 65+ 2008–2028, London UK
Royal Borough of Kensington & Chelsea (2008)
Diseases Known to GPs: Dementia, London UK

Self-Care Social Prescribing52
Spencer, K. et al (2017) Delivering dementia care
differently – evaluating the differences and similarities
between a specialist medical and mental health unit and
standard acute care wards: a qualitative study of family
Carers’ perceptions of quality of care, in BMJ Open, UK
The Ferry Project (2008), Octavia View SROI,
Wisbech UK
UK Cabinet Office (2012) A Guide to Social Return on
Investment, London UK
University College London and Canterbury Christ
Church University (2015) A Review of Community
Referral Schemes, London UK
University of Kent (2011) ASCOT Adult Social Care
Outcomes Toolkit: Additional Guidance Scoring,
Kent UK
NHS Scotland, University of Edinburgh and University
of Warwick (2005) The Warwick-Edinburgh Mental
Wellbeing Scale, UK
West London CCG & RBKC (2017) Quality of Care in
Residential Nursing Homes, London UK
West London CCG (2015) Whole Systems Integrated
Care (Older People) Business Case and Implementation
Plan – Governing Body report, London UK
Appendices

1. T’ai Chi 2. Link Up service & Men’s activities group 3. Creative group 4. Massage therapy 5. Chair-based
exercise 6. Information & Advice 7. Dancing & exercise 8. Local VCS groups
1. 2.
4.
8.
3.
5. 6.
7.

@KCSocialCouncil
/KCSocialCouncil
Kensington & Chelsea Social Council
1st Floor
111-117 Lancaster Road
London
W11 1QT
020 7243 9800
www.kcsc.org.uk
