GUIDE TO THRIVING AT THE DOC
2017-2018 Edition
Basic clinic information 3
Clinic contact info 3
Important phone numbers 3
Common Clinic Tasks 5
A checklist to complete during a patient visit 5
Filling out forms 5
Managing patients when not in the clinic 6
DOC after-hours telephone home call coverage 6
How to manage common calls 6
Prescribing Drugs 7
How to Make Prescription Drugs Affordable 7
Prescription Refills 9
Procedures 9
Scheduling (follow-up) Appointments 9
Sending letters to patients 10
Medical resources for patients at DOC 11
Group classes 11
Clinical pharmacy services 11
Physical therapy 11
DOC anticoagulation clinic 12
Behavioral health consultants 13
Psych consultation 13
DOC specialist Visits 14
Medications available in clinic 14
Ordering an outpatient blood transfusion 16
Diabetic patient resources 18
Medical resources outside of DOC 18
Outpatient referrals 19
Direct admissions, ED evaluations, and urgent care 19
Radiology 20
Home visit program 20
Dental care (free or low-cost) 20
Obstetrics 21
Smoking cessation options 21
Alzheimer disease support 21
Cancer-related support 21
Medical supplies 23
Diabetes Supplies 23
Durable Medical Equipment 23
CPAP/BIPAP 23
Home O2 24
Ensure 25
Care management and home health services 26
Care management 26
Page 2 Last revised: June 2017
Home health and personal care services 28
Home health services 28
Personal care services 28
Behavioral Health 28
Behavioral health access 28
Mental health crises 29
Domestic violence services 29
Social work and access to care 31
Clinical social work 31
Medical Transportation 31
How to make basic care affordable and accessible 32
Resources for essential daily needs 33
Controlled substances 34
Initiating narcotics 34
Pain contracts 34
Benzodiazepines 35
Urine drug screens Error! Bookmark not defined.
Controlled substances schedules 36
Clinical algorithms 38
Bridging (pausing) anticoagulation 38
Depression Management Algorithm 40
Table 1: Initiating Antidepressant Treatment with Sertraline* Error! Bookmark not defined.
Table 2: Switching to or augmenting with Venlafaxine XR Error! Bookmark not defined.
Table 3: Switching to or augmenting with Bupropion XL Error! Bookmark not defined.
Table 4: Augmenting with Mirtazapine Error! Bookmark not defined.
Potassium Management 44
Additional Treatment Considerations: 44
Vaccination Schedule (CDC) 45
Using Maestro Care (Epic) 46
Making your encounter more efficient 46
Epic inBasket 46
Visit types 47
Documentation outside a visit 47
Documentation of psychosocial needs 48
Smartphrases 48
Templates for clinic notes 48
HPI 48
Exam and procedures 49
Assessment and plan 49
Behavioral health 49
Patient instructions 49
Social work 50
How to help patient who cannot afford medication 51
CREDITS 52
Page 3 Last revised: June 2017
BASIC CLINIC INFORMATION
CLINIC CONTACT INFO
Duke Outpatient Clinic (DOC)
4220 N Roxboro Road
Durham, NC 27704
Main clinic number: 919-471-8344
Fax number: 919-477-3110
Fax number (refills): 919-477-5435
Door codes (all doors from waiting room to clinic area): 2-4-3-1
IMPORTANT PHONE NUMBERS
Faculty
Medical Director & Clinic Group A Leader, Lynn Bowlby, MD 919-970-4559 (p), 774-991-0041 (c)
Clinic Group B Leader, Dani Zipkin, MD 919-970-8947 (p)
Clinic Group C Leader, Larry Greenblatt, MD 919-660-9047 (o), 919-970-0496 (p)
Medical Director of Behavior Health, Greg Brown, MD 919-970-2532 (p), 847-927-0832 (c)
Ambulatory Chief Resident Dinushika Mohottige 919-970-6767 (p)
Teal Side Preceptor Room 919-660-9024
Lavender Side Preceptor Room 919-660-9023
Staff
Administrative Director Lisa Lowe-Hall 919-660-3064 (o), 919-970-0211 (p)
Amy Pollok, SAM 919-471-0459
Front Desk 919-660-9007 (or 9006 or 0919)
Financial Care Counselor 919-477-0829 (o); 919-471-9475 (o)
Social Worker, Jan Dillard 919-471-0084 (o), 919-970-4530 (p)
Clinical Pharmacist, Holly Causey 919-477-5904 (o), 919-970-3532 (p)
Clinical Pharmacy Assistant 919-660-9058
Nurse Manager Brenda Mutisya 919-660-9057 (o), 919-970-5178 (p)
Nurse Triage 919-660-9016
Nursing Pager 919-970-3624 (970-DOCHelp) (p)
HomeBASE Care Manager, Marigny Bratcher 919-309-6562
Medical Records, Carolyn Lawrence 919-660-9045
Laboratory, Angela Wilson 919-471-0546
Scheduling Hub, Rita Clark 919-479-2454
Scheduling Hub, Rita Maynor 919-479-2464
DHTS Help Desk: 919-684-2243
Hospital Transfer
DRH ER Triage: 919-470-4000 ext 1
Duke Transfer Center: 919-681-3440
Page 4 Last revised: June 2017
Hours and Parking
Clinic hours are 8am to 5pm.
The DOC is located on the second floor of the Durham Medical Center building on 4220 N Roxboro Rd. Enter
through the front door and exit through the side door. You must leave the building by 6:30pm, or alarms will go off
and the clinic will get charged a big fee! Please park at the side or back of the building so that patients can park in
the front.
Copy/Fax machines
- One located between the teal/lavender side nursing stations
- Another is located in medical records, no code needed
- Nursing can help you make copies
Late Policy for Patients
- Patient are considered late if they arrive >20 minutes after their scheduled appointment
- Patients arriving less than 20 minutes late will be seen
- Patients who are elderly, rely on others for transportation, are in the HomeBase program, or have an
issue that requires urgent medical attention will also be seen regardless of when they arrive
- If a patient is >20 minutes late:
o Nursing staff may ask you it you’re willing to see the patient, but the general goal is to see
everyone who walks in to clinic
o If you’re able, see the patient
o If you’re behind or have other people waiting, feel free to see others first, then see the late patient
o If you really don’t think you’ll have time, nursing staff may add the patient to someone else’s
schedule or schedule them for a later appointment in the day
Page 5 Last revised: June 2017
COMMON CLINIC TASKS
A CHECKLIST TO COMPLETE DURING A PATIENT VISIT
The majority of your patient care note can actually be completed prior to the end of the visit. The following
“checklist” highlights the different steps you should take during the visit in the “visit navigator” section of each
patient’s chart. Note that bolded items must be completed prior to discharging a patient from the visit. You may
use “.dazfu” or “.daznewtemplate” for a follow up or new visit respectively.
1. Document and/or review the “Chief Complaint”
2. Review documented “Allergies” (be sure to “mark as reviewed”)
3. Review and update the patient’s “Problem List” (be sure to “mark as reviewed”)
4. Review and revise patient history (PMH, PSH, family, social)
5. Review, reconcile, and refill patient medications under the “Medications” tab
6. Review and update the “Healthcare Maintenance” tab
7. Record a diagnosis (or multiple diagnoses) for the visit under “Visit Diagnoses” (note: you can
“push” problems from the “Problem List” section into “Visit Diagnoses” by clicking on the small arrow next
to each problem). Do NOT put ‘health maintenance’ as the first visit diagnosis, as we can’t bill visits that
way.
8. Document HPI
9. Order any additional tests or referrals under “Meds and Orders” (everything you order must be
“associated” with a visit diagnosis)
a. PEND orders until you know who you’re signing out with, so orders and referrals can link with
correct attending.
10. Document assessment and plan (note: use .DIAGMED to pull in each visit diagnosis with attached
orders)
11. Document a follow up in the “follow-up” section, specifically in the “For:” field (for example, “f/u in
2-4 months with PCP for HTN management”)
12. Route your note to the attending you signed out with (also in the “follow-up” section)
13. Write patient instructions in the “Patient Instructions” section (see Smart Phrases below)
Print the “After-Visit Summary (AVS)” and hand it directly to the patient
FILLING OUT FORMS
Partnership Folders
All paperwork needing attention is placed in partnership folders. You are responsible for addressing items in
folder each time you’re in clinic; please be conscientious of needs of patients when not in clinic, which can include
essentials such as diabetic supplies or home care orders. After completing, please place the form in the Medical
Records bin. Occasionally, if a partnership has no members in clinic for a few weeks, you’ll be asked to help with
forms for their patients. Dr. Bowlby can help with any paperwork—they are lots of different types and it is
complex! Dr. Zipkin will provide additional instruction on managing the folders during admin sessions during
ambulatory weeks.
Types of Forms
There are many types of forms that need to be completed; please ask your attending or more senior residents to
help you with forms that are new to you. All forms need to be copied and sent to medical records before returning
them to patients.
For questions about paperwork or obtaining records at the DOC, contact Carolyn Lawrence in Medical Records or
discuss with your attending.
Remember: Do not make copies of the patient’s information or discuss patient care with family members unless
you have permission, as HIPAA rules dictate. Document any verbal or written permission you have received.
Disability Forms
Page 6 Last revised: June 2017
Disability forms from insurance companies will be placed in your PP folder. These will be photocopied for the
patient’s chart. If it is a new disability form, it should be completed by the resident who most recently saw the
patient or the PCP, whoever knows the patient best. These forms and decisions are often complex, so please
speak with your attending or the Ambulatory Chief Resident. If it is a renewal form and continues to be
appropriate, old forms may be available for reference in the patient’s file kept in Medical Records.
FL-2 Forms
These are required for Medicaid patients transitioning from living at home to a skilled nursing facility (temporarily,
e.g., for low-intensity rehab) or rest home (i.e., more or less permanently, barring a dramatic change in home
circumstances); placement depends on there being an available bed at a facility accepting Medicaid. They are
also used to access funds to help a patient remain in their home in lieu of placement.
Health care power of attorney/advanced directive (HCPOA) forms
These forms may be completed by the patient and signed in front of any notary. Gloria Manley, financial
counselor, is the notary for DOC or the patient may use their own. Patient should provide a copy to DOC to be
scanned in to their record, and a Care Coordination Note and FYI flag entered, as well as the relevant additions to
the Problem List. Forms are available in each exam room in the manila folder. You may also refer patients to Jan
as needed to discuss HCPOA/Advance Directives, to ensure understanding of the process and the content.
Outside Medical Records
Outside medical records can be requested if patient completes a “Release of Medical Information” form, found in
the file drawers at the workstation. When the records arrive, they will be placed in your PP folder prior to filing in
the patient’s chart. If you need the medical record to be scanned, let Carolyn know.
Work excuses
Use pre-printed form in clinic located in the file drawers at the workstations, or available templates in Maestro
letters section (under “communication” tab. Do not use prescription pads.
Other miscellaneous folder Items
FYI items will come through from pharmacies and insurance companies and outside providers all the time. With
each item, your job is to determine the medical necessity of following up, or simply documenting in an encounter
that it was received to notify the care team, or signing it and returning to medical records to scan into the medical
record.
MANAGING PATIENTS WHEN NOT IN THE CLINIC
Away from Clinic
! Check your Maestro Care inbasket daily
! If you are going on vacation and will not be able to do so, ask a member of your provider practice to cover
for you
DOC AFTER-HOURS TELEPHONE HOME CALL COVERAGE
! Call is 5pm to 8am Monday-Friday and then all day/night Saturday and Sunday
! During regular work hours, calls are handled directly by clinic staff
! On the first Monday of your call week, call the Duke Operator to check in
! Carry your pager at all times including on the weekend
! The paging operator will page you first; if you cannot be reached, they will page the back-up attending
! Touch base with your attending in the middle of the week to discuss how the week is going
! Do not hesitate to call your attending. They get worried if they don’t hear from you every once in a while.
! Call / email / page Dr. Bowlby if you have questions or problems with your call experience
! Document all significant telephone encounters in Maestro
HOW TO MANAGE COMMON CALLS
Acute Complaints

Page 7 Last revised: June 2017
! Your role is to triage, not necessarily to solve or treat problems. Decide whether the issue is urgent or
not.
! Urgent: Active suicidal ideation, cardiac chest pain, mental status change, vomiting/diarrhea with no PO
intake for > 24 hrs.
o Call your attending to review the case and decide whether patient needs to go to ED vs urgent
care (Duke Urgent Care is open 8A-8P 7 days/week).
o If patient is having active suicidal ideation or needs substance abuse detox, consider directing
them to Durham Center Access at 309 Crutchfield St (919-560-7305).
o It is patient’s responsibility to call 911 or arrange their own transportation
o If patient is going to ED, call the hospital and explain the reason for ED visit
! Not urgent
o Suggest possible home treatment options or refer for an acute care visit in the upcoming days.
o If an urgent appointment is needed, send an inbasket message to the front desk supervisor to
make the appointment for the next day.
Medication needs
! Routine medication refills: Tell patient to call their pharmacy and have the pharmacy fax a request to
DOC. Do not order the refill yourself.
! Urgent medication refill: If you determine that you can safely refill on review of records and discussion
with patient, either call the pharmacy directly or generate a medication refill encounter thru Maestro
(preferred).
! Urgent refill but patient has not been seen in past 6 months: Provide a one month supply and set up a
follow-up appointment as above
PRESCRIBING DRUGS
HOW TO MAKE PRESCRIPTION DRUGS AFFORDABLE
! Use generics whenever possible
! GoodRx smartphone app provides coupons for many medications; useful for uninsured patients
! Large chains (Walmart, Costco, Kmart, Target, Harris Teeter, Kroger) have $4-5 generic prescription
drugs; some require a small annual fee
! Harris Teeter dispenses free generic antibiotics and oral DM meds for $4.95/year
! Coupons: http://www.needymeds.org/coupons.taf?_function=list&letter=A
! Mail order: https://www.rxassist.org/docs/rxoutreachfrm.pdf or https://xubex.com/BMLIntro.aspx
! For some plans (including Medicaid), Maestro Care alerts you when you order a non-formulary
medication
! Ask the pharmacist to walk you through pre-authorizations
! Ask social worker for additional recommendations
Patient Assistance Programs (PAP)
! Certain brand-name prescription drugs can be obtained directly from pharmaceutical companies
! Check rxassist.org to see if a medication is covered under a PAP
! Determine whether need for medication assistance is long-term or not
! Type ‘.docfreemedspap’ in patient instructions and/or ask a nurse to explain to patient what to do.
o Patient calls 684-9563 to speak with a pharmacy tech at the Duke Specialty pharmacy, to initiate
the screening process.
o Patient brings prescription for 90 day supply with 3 refills to the PAP staff at Duke Specialty
Pharmacy (Duke Cancer Center)
! Email Pharmacy-[email protected]uke.edu with patient name, MRN and medication. CC the attending.
Pharm Tech will email you the application to complete and have the attending sign. Then send back to
tech.
! Call physician line (684-9276) with questions
! PAP delivers 3 months of medications to patient home or Duke Specialty Pharmacy

Page 8 Last revised: June 2017
Senior PharmAssist-Patients with Medicare
! Phone number: 919-688-4772
! Website: http://www.ncdoi.com/SHIIP/SHIIP_County_Sites.aspx
! Counseling service and prescription assistance program
! Reviews medications, fills pillboxes, covers premiums and copays
! Available to patients >60 years old
!
Patient Has Medicaid Only
! Send prescriptions to Gurley’s Pharmacy (919-688-8978, 114 West Main St) or Josef’s Pharmacy (919-
680-1540, 3421 N Roxboro Rd)
! No copay if unable to pay
! Pharmacy delivers medications and can fill pill box (blister packs) for patient
NC MedAssist:-Uninsured Patientslong-term solution
! Refer patient to SW
! E-prescribe to NC MedAssist prescription for 90-day supply with 3 refills
! Set medication formulary for low-income uninsured NC residents
! Ships medications to patient for free
! Website: http://medassist.org/available-medications/
Duke Hospital Sponsorship: short-term solution for patients without insurance
! Refer patient to SW
! One-time support for medications
! Not available for insured patients who just need copay assistance
Medicare and Medicaid Difficulty with Drug Coverage
In some cases, Medicare and Medicaid may not cover a drug you think should be covered, or the cost of the drug
is higher than it usually is for the patient.
Medicare
1. Check if there are generic, over-the-counter or less expensive brand name drugs that are equally as
effective
2. Call 1-800-MEDICARE (1-800-633-4227) or visit
www.cms.gov/MedPrescriptDrugApplGriev/13_Forms.asp to find out what the barrier is, eg prior
authorization, step therapy requirements, quantity/dosage limits
3. Request a “coverage determination” if the pharmacist or plan tells you one of the following:
a. A drug you believe should be covered isn’t covered
b. A drug is covered at a higher cost than you think it should be
c. The patient has to meet a plan coverage rule (such as prior authorization) before they can get the
drug
d. The plan believes the patient does not need the drug.
4. Request a coverage determination with an “exception” if:
a. You think the plan should cover a drug that is not on the formulary because the other treatment
options on the formulary will not work
b. You believe the patient cannot meet one of the plan’s coverage rules, such as prior authorization,
step therapy, or quantity or dosage limits
c. You think the plan should charge a lower amount for a drug on the plan’s non-preferred drug tier
because the other treatment options in the plan’s preferred drug tier will not work for your patient
5. Wait 72 hours for a determination
6. If the patient cannot wait 72 hours, call or write to the plan to request a decision within 24 hours, letting
the know that the patient’s life or health may be at risk
7. Refer patient to Senior PharmAssist (919-688-4772) for financial assistance and assessment of
alternative prescription plans

Page 9 Last revised: June 2017
Medicaid
- Visit http://www.ncdhhs.gov/dma/pharmacy/PDL.pdf or call 866-246-8505 to find out what the barrier is,
eg prior authorization, step therapy requirements, quantity/dosage limits
- Complete prior authorization form OR submit required information via email OR call for prior authorization
- Submit prior authorization requests to 866-246-8507 (fax), nc.providerrelations@acs-inc.com, or ACS
State Healthcare, P.O. Box 967, Henderson, NC 27537-0967
- PA requests are typically answered within 24 hours, if not immediately.
- Pharmacy can issue a 72 hour supply while waiting for PA determination.
- For more information, go to http://www.ncmedicaidpbm.com/
PRESCRIPTION REFILLS
! For routine refill requests, patients should ask their pharmacist to fax requests to (919) 477-3110
! Your partnership’s RN will refill many prescriptions by protocol
! If patient has not been seen in >1 year, they may receive a 30 day refill but must be seen in clinic for
future refills
! Narcotic (schedule II) prescriptions require a written monthly prescription by a medical provider
PROCEDURES
For some procedures, you must obtain written informed consent from the patient on the pre-printed consent forms
available at the nursing work stations. Procedures that need BOTH a consent form AND a “time out” include skin
biopsies, joint aspirations and injections, and I&Ds. Include a brief description of the procedure in your clinic note.
1. Pelvic exams:
a. Let your nurse or CMA/CNA know in advance so he/she can get the patient ready
b. Order the tests you want before performing the exam
c. Commonly ordered tests: Pap with reflex HPV testing, gonorrhea, chlamydia, gram stain,
trichomonas
2. EKGs: place the order in Maestro, but be sure to let your nurse or CNA know because it doesn’t
automatically pop up in their system
3. Spirometry: simple spirometry can be ordered same-day or as a future nursing visit, and is done by the
CMA/CNA (note: you can also order formal PFTs by placing an order for “Ambulatory Referral for
Pulmonary Function Testing” in Maestro)
4. Nebulizer treatments
5. IV fluids: for short duration only
6. Cryotherapy for skin lesions
7. Skin biopsies
8. Joint aspirations and injections
9. Incision and drainage
10. Suture/staple removal
11. PPD placement
12. Injections: includes vitamin B12, Depo-Provera, vaccinations, ketorolac, ceftriaxone, insulin, and others—
see appendix for full list of medications
SCHEDULING (FOLLOW-UP) APPOINTMENTS
- During a clinic visit:
o Scheduling a follow up MD appointment: go to the “Wrap-Up” tab -> “Follow-up” section ->
“For: “ text box where you can type a return appointment time (e.g., “2-4 months with Dr. Smith”).
Always specific a time range to give schedulers leeway.
o Scheduling a pharmacist, DOC PT, or group visit (DM, HTN, Pain): go to the “Wrap-Up” tab -
> “Follow-up” section -> “Check Out Note: ” box and type your request. Examples “Follow-up with
Pharmacist 1:1 for insulin titration in 2-3 weeks,” “Follow-up with DOC PT,” “Schedule with HTN
group”
Page 10 Last revised: June 2017
- At any time: send an InBasket message to the “P DUKE OUTPATIENT SCHEDULING [10372].” This
option should start popping up after typing “P DUKE OUT” in the “To:” field. Use the “Patient Lookup”
button to add the relevant patient.
- Patients can schedule by calling the scheduling hub at (919) 471-8344 (extension 1) during business
hours to request an appointment (they should be encouraged to ask for you by name)
SENDING LETTERS TO PATIENTS
- If you are asked to write a letter to a patient, please review it with an Attending (if possible the one who
you precepted the patient with or who has seen them recently).
- You may notify patients of lab results by using letters.
- Select the “letters” tab (it may be hidden if you don’t use it frequently). Select recipient at the top.
Compose the letter (right click to make selected text editable to get rid of extraneous stuff in lab results)
à (1) ROUTE or (2) SEND the letter
o Click “route” to send the letter to your medical records pool or designated person (route to
Lawrence, Carolyn) who will mail the letter to the patient (preferred) and the attending who
reviewed the letter with you.
o Click “send” to print letters and then have someone send them. To print later, go to Letters tab in
Chart Review.
Page 11 Last revised: June 2017
MEDICAL RESOURCES FOR PATIENTS AT DOC
GROUP CLASSES
• DM2 class:
- Day/Time: two Fridays each month from 1:30-3:00 pm
- Brief description: multidisciplinary education and support group run by a clinical social worker and a
clinical pharmacist/diabetes educator. Also includes 1:1 MD visit for med titration.
- How to refer your patients: Type “DM Group” in the “Check-out note” box if in a clinic visit.
• HTN class:
- Day/Time: every 4th Monday from 10:00-11:30am
- Brief description: provides education on BP goals, diet, monitoring, stress reduction. Also includes 1:1
pharmacist visit for med titration.
- How to refer your patients: Type “HTN Group” in the “Check-out note” box if in a clinic visit.
• PAIN class (Prevent And Intervene NOW):
- Day/Time: every other Thursday of each month from 1-2 pm
- Brief description: chronic pain education and support. Explains origin of pain, strategies for coping
and adapting, and provides support.
- How to refer your patients: Type DOC PAIN Group in the “Check-out note” box if in a clinic visit or
message Jan Dillard if not in a visit.
For all group visits: Be sure to discuss with your patient and let them know of the referral.
CLINICAL PHARMACY SERVICES
What is a Clinical Pharmacist Practitioner (CPP)? A CPP is a pharmacist with specialized training who can independently
provide drug therapy management and implement pre-determined drug therapy through a collaborative practice agreement
under the supervision of a licensed physician. Holly’s supervising physicians are: Dr. Lawrence Greenblatt, Dr. Patrick
Hemming, Dr. Daniella Zipkin and Dr. Lynn Bowlby.
One-on-one pharmacy visits for DM2, HTN, anticoagulation, smoking cessation, and difficult med rec/education.
A clinical pharmacist practitioner will meet with patients and can titrate hypertension and diabetes medications.
This is a great way to add an additional visit between MD visits with the PCP for patients who need frequent visits
/ close monitoring. They can also do difficult med recs and educate patients (ensure patient knows to bring all
their home medications with them). Finally, they do pain management (see pain section).
Specify in your clinic note what you are expecting from the pharmacist. In the “Check Out Note” box ask for a 1:1
with pharmacist in x amount of time (e.g., 1-2 weeks). In patient instructions, type “.docpharmreferral”
Staff
! Clinical pharmacist practitioner Holly Causey (PharmD, BCACP, CPP, CDE) is the head CPP
! Dinah Harris, CPhT is present every day and assists Holly
! Ben Smith (PharmD, BCACP is present once a week (Monday AM)
! Lisa Bendz (PharmD) is present twice per month (Tues AM)
! Rotating pharmacy residents and students
PHYSICAL THERAPY
A variety of physical therapy services are available throughout the health system, including outpatient PT/OT,
speech, gait and balance training, mobility evaluations for motorized wheelchairs and other assistive devices,
cardiac and pulmonary rehab, vestibular rehab (for vertigo), and aquatic therapy.
Services Provided
The DOC has on-site physical therapy on Mon PM, Tues/ Thurs AM, for both scheduled appointments and
informal consultation. Conditions treated on site include:
- Neck pain
- Back pain
- Knee injuries

Page 12 Last revised: June 2017
- Shoulder injuries
- Pre-surgical management
- Post-surgical management
- Sports rehabilitation
- Arthritis conditions
- Traumatic injuries
- Overuse/repetitive injuries
For questions, email or InBasket Melissa Carvalho, or Dr. Bowlby (a former practicing PT herself!). For referrals to
PT, just write DOC PT in the follow-up section of the visit navigator in Maestro. Erik can see patients regardless of
insurance status.
DOC ANTICOAGULATION CLINIC
Joint nurse-pharmacist anticoagulation service for patients on warfarin
Referral Process
! Resident and attending identify patient to be enrolled in the anticoagulation clinic.
! Patients who are new to warfarin have an initial 30-45min appointment with pharmacy
! Subsequent visits with pharmacy are 15mn
! Once a patient reaches therapeutic level at 2-3 consecutive visits, s/he is assigned to follow up with RN
! Patients who are new to DOC but are already on warfarin follow up with RN
During the Anticoagulation Appointment
! POC INR test (POCT6003)
! Collect patient-reported dose of warfarin, missed doses, dietary changes, EtOH, other drug changes,
signs of bleeding or unusual bruising, other acute issues.
! If INR >5, the patient is sent to the lab for INR by phlebotomy (LAB320)
o Patients may leave if no clinically significant bleeding AND no s/s concerning for bleeding (eg
headache) AND can provide a reliable phone number
o If no s/s concerning for bleed but no reliable phone number, patient must stay for INR results or
return in 3-4 hours for results
o If s/s concerning for bleed, pharmacist or RN notifies a physician to evaluate need for acute
appointment or ED transfer
INR Checks at Home
! Home health agency checks INR
! Results are faxed, called in, or emailed to the clinic (attn. Holly Causey)
! Charge nurse notifies pharmacist if not therapeutic or RN if therapeutic
INR Checks During Physician Appointment
! MD may want to check an INR outside of the designated anticoagulation clinic time due to clinical
changes, transportation difficulties, etc.
! RN or LPN checks POC INR
! MD is responsible for adjusting warfarin and ensuring follow-up with the anticoagulation service
Follow-up
! All patients should have INR checked at least monthly
! If INR is at goal and has been at goal for >2 visits, follow up in 4 weeks
! If INR is not at goal, adjust dose and recheck in 1-2 weeks
! If INR is at goal x1, recheck in 1-2 weeks.
! Poor follow-up:
o If patient has 3 no-shows, they are referred back to their PCP for further management
o TAGTEAM (Team Approach Geared Towards Effective Anticoagulation Management):
Challenging patients are discussed once a month at the DOC leadership meeting. Providers
review the cases and make recommendations for further management.

Page 13 Last revised: June 2017
Contacting patients who are overdue for INR check
! Anticoagulation provider (pharmacist or RN) sends a notification to DOC front desk via inbasket message
to let them know the patient should be contacted 3 times on different days and at different times
! DOC staff documents each telephone call attempt as a telephone encounter
! After the third attempt, the encounter is forwarded to anticoagulation provider
! Provider sends a letter to the patient
! If no response is received within 1 week, a second letter is sent requesting that the patient contact the
clinic to make an appointment
! If no response within 2 weeks of the second letter, provider is notified
! Provider documents that the patient is no longer active in anticoagulation clinic and sends a message to
PCP and medical director
BEHAVIORAL HEALTH CONSULTANTS
! Who: Ashley Cyr and Joy Long (as well as Jan Dillard). All are LCSW.
! What they do:
o Provide consultation to PCP for patients whose problems are related to behavior (for both
physical health and mental health)
o Targeted Counseling
o Brief visits (20-30 minutes)
o Develop treatment plans
o Teach self-improvement techniques (wellness/self-management)
o Schedule follow up if needed
o Refer to specialty mental health as needed
o Document in Maestro
! Common reasons for referral:
o Chronic disease management (e.g., hypertension, diabetes, headaches, chronic pain)
o Wellness (e.g., sleep, healthy eating, smoking cessation)
o Adjustment to new diagnosis (e.g., STIs, cancer)
o Dementia, cognitive impairments, I/DD (Intellectual/Developmental Disabilities)
o Fatigue without medical etiology
o Socio-emotional problems (e.g., bereavement, marital problems)
o Parenting and behavioral problems in kids of patients
o Typical psych complaints (e.g., mood disorders, ADHD, substance abuse, psychosis)
! How to make the behavioral health consult as effective as possible:
o Identify patient behavior issue
o Ensure willingness for patient to see BHC
o Warm handoff – face to face introduction
o Monitor and support patient progress with tx plan
o Continue to refer to Jan as usual for broader social work needs, comprehensive assessment and
long term counseling
o If you are not sure whether to refer to BHC, do it anyway and they will sort it out
PSYCH CONSULTATION
The DOC has two Med-Psych attendings who specialize in medically complex psychiatric patients, and are
available to see patients with several types of conditions.
- Patients MUST be referred by their PCPs (no self-referrals)
- The following patients can be referred directly for clinical assessment:
o Patients with Schizophrenia or Bipolar disorder without a current psychiatrist
o Patients with depression or an anxiety disorder without psychiatrist AND have been hospitalized
or seen in the ER psychiatrically within the past 3 months
- The following patients should be scheduled during Med/Psych preceptor time (Mon PM, Tues PM, Wed
AM and Fri AM):
Page 14 Last revised: June 2017
o Patients with Schizophrenia or Bipolar disorder who have a psychiatrist BUT their psychiatric
illness is interfering with their ability to manage their medical illnesses
o Patients with depression or an anxiety disorder who have a psychiatrist AND have been
hospitalized or seen in the ER for a psychiatric diagnosis within the past 12 months
o Patients with depression or an anxiety disorder who have not responded to or not tolerated
medication trials per the DOC Depression Management Algorithm
o Patients with substance abuse, personality disorders or other psychiatric issues whose
psychiatric illness is interfering with their ability to manage their medical illness
o Patients with suspected psychiatric illness but unclear psychiatric diagnosis
- Once patients are psychiatrically stable, their care will be transferred back to their PCP
- Please do not utilize Med-Psych consultation for patients with routine depression without first attempting
treatment through the depression treatment algorithm
- If there are ever any questions about the appropriateness of referrals, please feel free to page or call Dr.
Brown in real time
DOC SPECIALIST VISITS
• Several specialists see patients at the DOC. This may be an easier location for patients, and these
clinicians are familiar with the DOC patient population. Request a specialist clinic visit by asking for the
relevant specialist clinic in the “Check-out note” box after a patient visit.
• The following specialists see patients at the DOC on certain days:
o Endocrinology clinic (Wednesday afternoons)
o Hepatology clinic (with Dr. Muir)
o Cardiology clinic
o Physical Therapy (Thursdays)
o Weight loss (with Dr. Westman). For motivated patients, his comprehensive clinic (next door to
the DOC) teaches the low-carb (i.e., ketogenic / Atkins) diet and has successfully had many
patients control their diabetes and even reduce / eliminate their insulin requirement.
o Pulmonary clinic
MEDICATIONS AVAILABLE IN CLINIC
Allergy
Diphenhydramine 25mg capsule
Epinephrine (Epi-Pen) 0.3mg syringe
Antibiotics
Azithromycin 250 mg tablet
Ceftriaxone 250mg and 500mg vial (IM)
Metronidazole 500 mg tablet
Neomycin/Polymyxin/Bacitracin ointment
Penicillin G 2.4 million units/4mL
Cardiology
Aspirin 81mg chewable tablets
Aspirin 325mg tablets
Atropine sulfate 1mg/mL vial
Clonidine 0.1mg and 0.2mg tablets
Furosemide 20mg tablet
Hydralazine 50mg tablet
Metoprolol 25mg tablet
Nitroglycerin 0.4mg tablet
Endocrinology
Cosyntropin 0.25mg vial
Dexamethasone 4 mg/mL vial
Dextrose 50%, 50mL vials
Glucagon 1mg kit vial
Glucose 40% gel 31g tube
Insulin lispro (Humalog) 100 units/mL
Insulin regular (Humulin R) 100 units/mL

Page 15 Last revised: June 2017
Methylprednisolone sodium succinate (solu-medrol) 40 mg/mL and
125 mg/mL
Methylprednisolone acetate (depo-medrol) 40 mg/mL
Prednisone 20mg tablet
Gastroenterology/Nausea
Docusate Sodium (Colace) syrup 100mg/10mL
Magnesium, aluminum, simethicone (Mag-Al Plus XS)
Ondansetron ODT 4mg tablet
Promethazine 25mg tablet and 25mg/mL1 mL vial
Hematology
Epoetin Alfa (Procrit) 10,000 units/mL
Phytonadione (vitamin K) 5mg tablet
Pain or anti-inflammatory
Acetaminophen 325mg and 500mg tablets
Colchicine 0.6 mg tablet
Ibuprofen 200mg tablets
Ketorolac 15 mg/mL and 30mg/mL
Sumatriptan 25 mg tablet
Psychiatric/Substance Abuse
Aripiprazole (Abilify Maintena) 300 mg syringe and 400 mg syringe
Naloxone 2 mg/2mL vial
Naltrexone (Vivitrol) 380 mg vial
Pulmonary/Respiratory
Albuterol 2.5mg/3mL inhalation ampule
Reproductive
Etonogestrel (Nexplanon) 68mg implant
Medroxyprogesterone acetate (Depo-Provera)150 mg
Testosterone cypionate (Depo-testosterone)
Vaccines
Hepatitis A vaccine
Hepatitis B vaccine
Human Papillomavirus 9-valent(Gardasil)
Influenza virus vaccine
Pneumococcal 13-valent conjugate (Prevnar)
Pneumococcal 23-valent conjugate (Pneumovax)
Tetanus, Diphtheria- Td (Decavac) vaccine
Tetanus, Diphtheria, Pertussis (Boostrix)
Miscellaneous
Ammonia aromatic inhalant 2% ampule
Carbamide Peroxide Otic Soln 6.5%
Cyanocobalamin (vitamin B12) 1000mcg/mL
Hylan G-F 20 (Synvisc-One) 8mg/mL
Lidocaine 1% and 2% injections
Lidocaine with epinephrine 1%
Silver nitrate applicator stick
Silver sulfadiazine cream 25mg tube
Thiamine 100mg/mL
Triamcinolone acetonide (Kenalog) 40mg/mL
Tuberculin PPD skin test

Page 16 Last revised: June 2017
ORDERING AN OUTPATIENT BLOOD TRANSFUSION

Page 17 Last revised: June 2017
Infusion Center Orders: Brenda, nurse manager will assist you!
- Call first to set up appointment: 919-681-0645
- Location: 2A in Duke South
- Make sure to draw a type and screen the day BEFORE the infusion visit (if you are ordering PRBCs)
- Be sure to be on your pager in case you get called for clarification
- Steps on Maestro:
o Select: Patient Station and locate your patient
o Select: More activites (bottom left of your screen)
o Select: Encounters (first option on the pop-up menu option)
o Select: New (on the bottom left)
o Select: Orders Only encounter
o Then in your new encounter select: Orders
o Then you must select: orders for later on the top menu option (last on the right)
o It will then ask you to designate a location: Select DUH
o You will be directed to another screen and select: order sets and open Adult Blood
administration (or designated medication e.g. IV iron) and enter desired orders
o Sign orders

Page 18 Last revised: June 2017
DIABETIC PATIENT RESOURCES
"#$%&'$()#*(
+,&!-%#.&$&*
/01(≥ 23
45,)#6(
785'$9("5.:%;(
<&#:$)
78'$#;$(<&%-%(=;)8&++'&,>(0=>(?4>(
@4A(B(CDC!EFG!HIHF(8,(
)*;)8&++'&,B-;8';JK8L
/01(M(23
4N7(40(
O,85+(P%*%$
"#$%&'$(,&Q5*&*(
K,85+*
4N7(/&)#L%8,#:(
<&#:$)(
78'*5:$#'$
"#$%&'$()#*(
-%#.&$&*
"#$%&'$(%*(
)86&.85'-
?&Q&,($8(<86&(<&#:$)(A5,*%'K
RS6.(,&Q&,,#:($8()86&()&#:$)T
"#$%&'$((%*(
'&U:9(
-%#K'8*&-(8,(
&V+,&**&*('&&-(
Q8,(&-5;#$%8'(8,(
*5++8,$
DOC%DM%Group%Visit
(2%consecutive,%
ideally%all%7%in%
series)
Include%in%the%
follow-up%in%
Maestro
"#$%&'$('&&-*(
'5$,%$%8'(
&-5;#$%8'
O,8;&,9(=$8,&(W85,
X6#%:Y(
:*U%::%#6*B-;8';JK8L
45,)#6(
785'$9("5.:%;(
<&#:$)
?&Q&,,#:(Q8,6(Q85'-(8'(
)$$+YZZUUUJ-;8';JK8LZ%'-&VJ#*+V[+#K&\D]2G
4?<(4%#.&$&*(
^(A5$,%$%8'(
X-5;#$%8'
J4?<41S/XWX=?X_X??S@
8,(#6.5:#$8,9(,&Q&,,#:($8('5$,%$%8'(
788+&,#$%L&(
&V$&'*%8'(
#K&';9
A7(XV+#'-&-(_88-(^(A5$,%$%8'(
X-5;#$%8'(",8K,#6(
RUUUJ;&*J';*5J&-5ZX_AX"ZT
0&-%;#%-(
4%&$%;%#'
`';8'$,8::&-
A8(%-&'$%Q%#.:&(
,%*a(Q#;$8,*(N?(
+*9;)8*8;%#:
?&Q&,($8(*8;%#:(U8,a(Q8,(+*9;)8*8;%#:(
#**&**6&'$Z*5++8,$
J=b4N7=b?X_X??S@
SD;(c(Cd(e(
5';8'$,8::&-( /"
OR%SD;(c(D2d
OR
XV$&'*%L&(
-5,#$%8'
4N7(/&)#L%8,#:(<&#:$)(78'*5:$#'$(#$(
'&V$(#++8%'$6&'$
<8::9(7#5*&9(R")#,64>(/7S7">(7"">(74XT(
DYD
1';:5-&(%'($)&(Q8::8U!5+(*&;$%8'(%'(0#&*$,8

Page 19 Last revised: June 2017
MEDICAL RESOURCES OUTSIDE OF DOC
OUTPATIENT REFERRALS
These are generally ordered by typing “ambulatory referral [blank specialty].” A few specific referrals
• Driving Evaluation
o Laura Juel, OT
• Incontinence
o Males -> Urology
o Females UroGyn
o PT for stress incontinence: “Amb Ref PT” and indicate UroGyn PT
• Ophthalmology for low income/Medicaid
For screenings: http://www.dukehealth.org/events/lions_club_eye_screenings/20120418 There
are regular free vision and glaucoma screenings offered. These are usually posted on the
bulletin board in the lobby.
For uninsured patients with eye disease: Duke Eye Triage nursing suggests patient make an
early morning appointment with the Comprehensive Service at Duke Eye/Erwin Road; # is 681-
0896. Patient will be asked to sign a financial agreement but can say they cannot afford to pay. If
the MD thinks they need a Consult, a fellow will see the pt. that same day.
For patients whose insurance does not cover glasses (e.g. Medicaid, the uninsured), refer
to social work for help filling out the following applications:
! http://www.onesight.org/na/ Network of providers (including Sears Optical and Target that will
provide free glasses)
! www.neweyesfortheneedy.org/us/us.html Will provide a voucher; must apply through SW if
unable to get glasses through OneSight.
! http://www.firmoo.com/free-glasses.html (just pay shipping)
• Wheelchair evaluation
o Laura Juel, OT
DIRECT ADMISSIONS, ED EVALUATIONS, AND URGENT CARE
Duke Regional Hospital
3643 North Roxboro Street, Durham, NC 27704
Preferred for patients with routine exacerbations of chronic conditions who probably will not require a procedure
or surgical intervention not available at DRH.
Direct admissions: Reserved for patients who require admission for management of a known diagnosis and are
stable for admission to the floor. Page hospitalist managing admissions at 970-9050 or call the Assistant Chief
Resident (919) 470-5150 and give patient’s name, MRN and reason for admission. The patient should proceed to
Admissions via car or ambulance as appropriate. Call the admitting team and give brief history, reason for
admission and plan; also complete a note in Maestro. The clinic nurses should be made aware of the plan.
ED evaluation: Ask the clinic charge nurse or nurse you are assigned for assistance with calling 911. Call (919)
470-5345 and ask to speak with the ED attending/resident/charge nurse about the incoming patient, giving a brief
history and reason for ED evaluation. Complete a note in Maestro. If you have to leave clinic before the
ambulance arrives, make sure you sign out to a resident/attending who will assume responsibility for the patient.
Duke University Hospital
2301 Erwin Road, Durham, NC 27710
Direct admissions: Call the Assistant Chief Resident at DUH (970-1010); otherwise as above.

Page 20 Last revised: June 2017
ED evaluation: Call 684-8111 (Duke); otherwise as above.
Urgent Care
1. Duke Urgent Care South
5716 Fayeteville Road, Durham, NC 27713
919-525-3967
2. Duke Urgent Care Croasdaile
1821 Hillendale Road #24-A, Durham, NC 27705
919-338-4355
3. Duke Urgent Care Brier Creek
10211 Alm Street #1200, Raleigh, NC, 27617
RADIOLOGY
All radiology services are offsite, many next door at the Medicine-Pediatrics clinic located in the Duke Health
Center on Roxboro Rd. Front desk staff schedules all imaging studies. Imaging should be ordered during the
patient’s visit (if possible) and should be ordered in Maestro Care – remember to link the order to a diagnosis in
Maestro Care.
HOME VISIT PROGRAM
One time: The DOC offers a one-time in-home consultation service for our patients by a team: usually a resident,
the Ambulatory CR, pharmacist and SW. These visits generally take place once monthly. Indications for referral
include: difficulty completing thorough med rec in clinic, follow-up of acute illness, caregiver stress assessment,
frequent falls, non-adherence, suspected abuse/neglect, or needs assessment. If you have a patient who you
feel is appropriate, send a staff message to Jan Dillard in Maestro using .SWDOCHOMEVISITREFERRAL in the
message to provide more information as to what your specific concerns are. You can walk down to Jan’s office
and give her a heads-up as well, particularly if you feel the need is urgent.
Ongoing in-home medical care: Just For Us, a home-based primary care program offers in-home medical
services to Durham's seniors and adults with disabilities who have barriers to routine primary care services in the
traditional office setting. Medical team includes a physician, an advanced practice provider, SW, OT,
phlebotomist. Patients are expected to continue care relationship with their primary care provider, and to see that
provider at least once per year for chronic care and for acute needs that cannot be addressed in the home. For
more information or to refer a patient, contact the Just for Us office at (919) 956-5386 or talk to Jan Dillard.
DENTAL CARE (FREE OR LOW-COST)
Check Jan’s door for copies of lists.
For patients with Medicaid
May receive dental treatment from any dentist enrolled in NC Medicaid Program and willing to provide dental care
to Medicaid recipients. Providers who have a "Y" indicated in the "Accepting New Patients" column may be more
likely to accept new Medicaid recipients, but patients should confirm this by contacting the provider:
http://www.ncdhhs.gov/dma/dental/dentalprovlist.pdf
For those with Medicare or no insurance (Sliding Fee Scale)
! Lincoln Community Health Center Dental Clinic: Eligibility for sliding fee scale discounts based on the
number of people in family and total family income, but patients are served regardless of ability to pay.
! Needy Meds Free Clinic List: Lists Free and Low Cost Clinics offering health care at no cost, for a small
fee, or on a sliding scale.
For those with Medicare or no insurance
! SNDA (Student National Dental Association) CAARE Clinic: Includes cleanings, non-surgical periodontal
treatment, simple restorative work, and simple extractions for patients without dental insurance.

Page 21 Last revised: June 2017
! Donated Dental Care: Donated dental care to people who are disabled, medically compromised, or
elderly and who have no financial resources with which to pay for their extensive dental care needs. Does
not provide emergency care or routine cleanings.
! Samaritan Health Center : Comprehensive medical and dental care to the homeless and underserved of
Durham, regardless of their ability to pay. Must apply.
! Baptist Men’s Medical/Dental Bus: Patients targeted through this ministry include people without
insurance, the impoverished, Hispanic and other ethnic groups, migrant workers, fair workers, the
homeless, elderly, and more.
! North Carolina Missions of Mercy: Services provided to adults with income less than 200% of the Federal
Poverty Level Guidelines.
! Dental SHAC (Student Health Action Coalition): Free, student run for those in Orange County who cannot
afford care elsewhere—services include screenings, cleanings, restorative procedures, extractions and
emergency care.
For those with Medicare who require medically necessary dental treatment
! Drs. Patterson, Kendell, Frost, Bechtold, and Sacco, PA
! UNC-Chapel Hill, Maxillofacial Surgeon
OBSTETRICS
ALL newly pregnant patients:
Scan current medications for possible teratogens, prescribe prenatal vitamins, assess and counsel as needed re:
cessation of smoking/alcohol and/or other drugs, and assess for safety/support at home.
If your newly pregnant patient is high-risk:
Enter referral to Duke Obstetrics/Maternal Fetal Medicine (type in ‘high-risk’)
If your newly pregnant patient is not high-risk and has Medicaid or is uninsured:
Can direct them to the Durham County Health Department (located at 414 E. Main St; (919) 560-7882), which is
also where the area Women, Infants and Children (WIC) nutrition program is based. Consider asking Marigny
Bratcher for one-time follow-up to ensure patient has connected with that clinic.
SMOKING CESSATION OPTIONS
NC Quit Line: (Packets are available in the black folders in the exam rooms or can insert smartphrase into
discharge papers)
Breath of Life: Free stop smoking program offered to individuals, community and worksite groups and
organizations in Durham County. Series features five classes that assess readiness to quit smoking, preparation,
quitting methods and tips to successfully remain a non-smoker. Additional resources and educational materials
are provided for each participant. Contact, (919) 560-7765
DOC Quit At Duke Smoking Cessation Program
Comprehensive evaluation to determine which treatments will be most effective
Evidence-based medications — often combination medications or adaptive treatment
The option of several evidence-based behavioral treatments
Long-term phone-based “check-ups”
Access to research studies
919-613-QUIT
ALZHEIMER DISEASE SUPPORT (AND OTHER CHRONIC CONDITIONS OF LATER LIFE)
The Duke Family Support Program: In addition to resources for families, as providers you can email, call or
schedule an in-person consultation with a social workers for help with your questions about elder care.
http://www.geri.duke.edu/service/dfsp/index.htm
CANCER-RELATED SUPPORT

Page 22 Last revised: June 2017
Information packet is available in the Green Folder in the exam rooms
Duke Cancer Patient Support Program (DCPSP): free services/resources to help support patients and their
loved ones throughout their experience with cancer. Services—individual, couple, and family therapy; Support
groups; Self-image resources; Volunteer companionship and peer
support. http://www.dukehealth.org/cancer/support-services/cancer-patient-support/about
Cornucopia: free support services to patients with cancer and their loved ones—peer support and support
groups, education, connection to resources, massage, yoga and acupuncture! http://www.cancersupport4u.org/

Page 23 Last revised: June 2017
MEDICAL SUPPLIES
All requests for medical supplies for patients with Medicare require an attending signature.
DIABETES SUPPLIES
Medicaid: formulary is limited; order generic glucometer and testing strips, and print out so patient can obtain
from local medical supply store
Medicare: Patients have option of ordering from diabetic supply companies; patients would need to call company
of their choosing; form is faxed to the DOC and placed in your PP folder for you to complete and an attending to
sign. Can ask Carolyn Lawrence in Medical Records for help as well.
Uninsured: Walmart Relion brand has 50 strips for $9.
DURABLE MEDICAL EQUIPMENT
Simple equipment
Enter it as an order, but select ‘Print’ to produce a hard copy that the patient can take to a medical supply store.
Motorized chair
Generally, no scooters or Hoveround; only electric chairs
Steps to order:
1. Appointment with MD (AKA Face to Face) Face to Face- Resident uses smart phrase and/or documents
trouble/inability to walk in the home or frequent falls, attending signs that note, and that is the attending who signs
all further documentation (7 element form)—45-day window to complete the medical provider face 2 face and
signing/concurrence of the therapy wheelchair evaluation.
2. Refer to PT/OT Wheelchair Evaluation (can be before or after Face to Face); if evaluation agrees with need for
power device, same attending signs her note. There is no time limit on the OT evaluation, it can be far ahead of
the face to face visit.
3. Paper work packet- signed by same attending then fax back to the vendor.
CPAP/BIPAP
Diagnosing OSA
The order is called “Ambulatory Referral to Sleep Studies.” Within the order, you can choose routine
polysomnography (will be your choice most of the time), CPAP titration (if the patient already has a diagnosis of
OSA in the past 10 years and needs their device setting adjusted), or Home Sleep Test (only choose this if you
are fairly certain the patient has OSA and they have a reliable home and social situation to be able to complete
the test at home). As part of the order, you can also automatically request a referral to pulmonary or neurology
clinic if the test is positive.
Treating OSA
Once the diagnostic sleep study and subsequent titration study have been done, with recommendations for
treatment and settings, enter an order for ‘CPAP Machine’ in Maestro, click the ‘Qty-1, External’ link and then the
‘Click to add text’ behind it, and then use the dot-phrase .DOCCPAPORDER. Write in recommended pressure
(from titration study), and print out copy of order AND sleep study results (which must be attached). We have
forms for some agencies in the orange ‘Respiratory Services’ folder in the Forms drawers in each work area.
Leave in the medical records bin with a note indicating which agency patient has selected, for it to be faxed to
and/or the form for that agency. If the patient has Medicare, get an attending to co-sign the order and the
form; Medicare requires an attending signature (and NPI) for durable medical equipment.
Two agencies that Dr. Ambrose Chiang in the Pulmonary Clinic recommends are: Sheepless Nights (in Garner,
NC; fax: (919) 662-2739) and Advanced HomeCare (ph: (919) 852-0052). Two others that Carolyn Lawrence in
Medical Records suggested are: Kight's Medical (in Morrisville, NC; fax: (919) 878-4411) and Apria Healthcare
(also in Morrisville, NC; fax: (919) 380-1185).
Troubleshooting OSA
If a patient has had a prior sleep study confirming a diagnosis of OSA, it remains “good” for 10 years; all they
would need, if they are attempting to re-start CPAP use, is to have a recent titration study. Dr. Chiang and his PA

Page 24 Last revised: June 2017
Steve Taxman in the Pulmonary Clinic are skilled at helping patients who are having difficulty using CPAP/BiPAP.
This can be an indication for referral.
HOME O2
1. If patient had assessment (documented O2 saturation <88% while walking/sleep study w/titration, print a copy
of the note where this was documented. Enter an order for ‘Oxygen’ in Maestro, click the ‘Qty-1, External’ link and
then the ‘Click to add text’ behind it, and then use the dot-phrase .DOCHOMEOXYGEN. Write in the qualifying
readings, relevant diagnoses, and required statements (see Documentation above); sign, and print. Copy all of
this text from the order into the assessment and plan of a Progress Note that lists hypoxia as a problem, which
must also be attached.
2. Does patient have a provider preference? If no preference, can provide them with a list of choices or just
choose—Lincare, Adult and Pediatric Specialists, Apria and Active Healthcare are frequently used. If they have
private insurance, specific providers may be preferred.
3. Complete the form (orange respiratory services folder in the drawers at each nurse’s station) for the provider
chosen.
4. Fax (or place in Medical Records basket) the form and assessment, along with demographic/insurance
information, to the provider.
We have forms for some agencies in the ORANGE ‘Respiratory Services’ folder in the Forms drawers in each
work area. Leave in Partnership Folder or medical records basket with a note indicating which agency patient has
selected, for it to be faxed to and/or the form for that agency.
If the patient has Medicare, get an attending to co-sign the order and the form; Medicare requires an attending
signature (and NPI) for durable medical equipment including home oxygen. Medicare also requires
documentation in the medical record; the easiest way to do this is copy the text from the order into a note in
Maestro, either in a Progress Note for an existing encounter or a separate Documentation or Orders Only
encounter.
Medicare Requirements for Home Oxygen
Testing must be performed with the patient in a chronic stable state (i.e., values from ED cannot be used): 1) As
an outpatient: within 30 days prior to initial certification, 2) For patient transitioning from hospital stay to home:
within two (2) days prior to discharge from an inpatient hospital stay to home, 3) For a patient in a skilled nursing
facility or hospice: within 30 days prior to initial certification
Patient’s chart notes must document the following:
! Documentation of patient’s hypoxia-related condition and his/her condition should improve with oxygen
therapy
! Documentation that other treatments have been tried and deemed insufficient (e.g., medications, inhalers,
etc.)
Qualifying Saturation Test Results:
#1 At Rest
#2 During Exercise
#3 Overnight
(e.g., during sleep study)
Context
Patient tested on room air at
rest
Patient tested while walking
Patient tested while
sleeping
Threshold
for
medical
necessity
SpO2 ≤ 88%
All three must be documented:
a) SpO2 on room air at
rest
b) SpO2 on room air
during exercise – must
be ≤ 88%
Oxygen must be measured
for at least two hours;
desaturation to ≤ 88% for at
least 5 minutes.

Page 25 Last revised: June 2017
c) SpO2 on oxygen
during exercise – must
show improvement
Notes
If > 88% and you think patient
would benefit from O2, go to
#2
Will not qualify patient for
portable O2.
Note: For #2, all three readings must be from the same testing session.
ENSURE
It is a two-step (two form) process to get Medicaid to cover Ensure. In the Medicaid system, it is DME. One is
specific to oral nutritional supplements, the other is a general Prior Approval form. The medical justification must
be documented in the medical record as well.
Policy with key points highlighted: “Examples of conditions that may indicate a need for oral nutrition products
include, inborn errors of metabolism, such as phenylketonuria (PKU) or galactosemia; history of prematurity, very
low birth weight (VLBW), or low birth weight (LBW); cystic fibrosis; human immunodeficiency virus (HIV);
necrotizing enterocolitis (NEC); short bowel syndrome; cleft lip or cleft palate; central nervous system disorders
resulting in dysphagia; and Crohn’s disease. Oral nutrition products are considered medically necessary when all
of the following conditions are met: a) There is a documented diagnosis in which caloric or dietary nutrients
cannot be safely or adequately consumed, absorbed, or metabolized; and b) oral nutrition product is an integral
component of a documented medical treatment plan and is ordered in writing by the treating physician. Medical
necessity of the oral nutrition product is substantiated by documented physical findings, and laboratory data if
available, that demonstrate malnutrition or risk of nutritional depletion. If a nutritional assessment is ordered, it
must be conducted by a licensed dietitian/nutritionist (LDN) or registered dietitian (RD). The prescriber may also
order a feeding or swallowing evaluation by a licensed therapist (SLP-CCC or OTR/L) which must be maintained
within the health record as supporting documentation to substantiate medical necessity. Must submit a new Oral
Nutrition Product Request Form and CMN/PA every six months with documentation supporting the effectiveness
of the oral nutrition supplementation.
Note: Oral nutrition products are not covered when medical necessity is not established, or when they are used as
convenient food substitutes.”

Page 26 Last revised: June 2017
CARE MANAGEMENT AND HOME HEALTH SERVICES
CARE MANAGEMENT
HomeBASE care Our first major Redesign work, one year of planning, program began 2014
! HomeBASE is a program whose goal is to reduce ED utilization via better connection to coordinated
primary and specialty care, with a focus on better health coping in our patients.
! Marigny Bratcher (Manson in Duke system) is the RN Care Manager for the DOC HomeBASE program.
! Criteria: patient should have 6 or more Emergency Department visits in a 3 month period, with some
ongoing use of the ED.
! Referral: send the patient’s name and MRN to Marigny via email, inbasket or by stopping by her office (in
the lobby behind copier).
Marigny is also available for one-time case management interventions for non-HomeBASE patients. Examples
include: referral to outside medical case management agencies, follow up phone calls requiring clinical skill,
complex history gathering from outside Duke system. To request, contact Marigny with the intervention you would
like. If you don’t exactly what the situation needs that’s ok too! We can figure it out together.
HiDOC Second major Redesign project, program began Jan 2017.
! Hi intensity Primary Care
! Provides more on site medical care for acute illnesses
Duke Connected Care and DukeWELL
Duke Connected Care (DCC) is an Accountable Care Organization (ACO) that manages population health for
patients with traditional Medicare or Cigna insurance in the general Duke service area. DukeWELL is a free care
management program that assists in providing DCC’s care management services. DukeWELL also manages
other populations, including qualifying patients with Duke Basic/Select insurance, specific Medicare Advantage
insurance plans, and others.
To identify if a patient qualifies for DCC or DukeWELL services: Look for the “DukeWELL: Y” notation in the
patient’s chart. This is located in the top banner beneath their MRN and CSN.
DukeWELL or DCC may identify a patient and contact you for input on potential opportunities to improve
care. You may also refer directly via an ambulatory referral to DukeWELL. Include the reason for referral in the
comments section.
Services include:
! Free RN home visits (limited to DCC Medicare patients)
! Care coordination
! Patient outreach and engagement
! Appointment reminders and coordination
! Transportation assistance
! Medication access assistance
! Skilled nursing facility transition coordination
! Coordination with Duke Home Health and Hospice
! Quality measure gap closure (may include outreach to patient and/or provider)
! Telephonic RN disease management education and coaching
! Virtual specialist and clinical pharmacist rounds (geriatrics, CKD, and DM)
NPCC – Kenya Gomez is the DOC Care Manager
Northern Piedmont Community Care (NPCC) is the umbrella for two networks: Durham Community Health
Network (for Durham county) and Community Care Partners (for Vance, Warren, Person, Franklin and
Page 27 Last revised: June 2017
Granville counties). NPCC promotes wellness to strengthen the self-care capacity of its Medicaid members
and their families.
With an interdisciplinary staff of professional and paraprofessional providers, NPCC has focused its efforts
and energies on the development of community-based care/disease management that supports the integration
and collaboration of the various patient delivery systems within the community. The staff of NPCC deliver
at-risk social work services, service coordination, access support, education and nutrition counseling.

Page 28 Last revised: June 2017
HOME HEALTH AND PERSONAL CARE SERVICES
HOME HEALTH SERVICES
What: Skilled and unskilled services provided in patients’ homes: RN, PT, OT and speech therapy (skilled) and
medical social work, in-home aide, and short term OT (unskilled).
Who: Patients with Medicaid for whom you can certify that it would be in the best interests of the patient to have
the service at home; patients with Medicare who are homebound (requires considerable and taxing effort
to leave home AND only leaves home for things such as medical visits, family visits, religious services,
haircuts); some patients with private insurance; uninsured patients enrolled in Duke Charity Care (Duke
Home Health only)
How: 1) Discuss referral with the patient. Does patient have a provider preference? If patient wants a referral
list, SW can provide that. Must document that they were given the chance to choose and have a referral
list to consider. Extensive list of agencies: http://www.homeandhospicecare.org/directory/index.html.
Frequently used agencies are:
! Duke Home Care & Hospice (must inform patient of financial relationship, i.e., that Duke owns
and operates DHCH, and document that this information was provided)
! Others: Liberty Home Care, Intrepid, WellCare, Amedisys
2) Complete Amb Referral to Home Health. Be sure to document patient’s preferred provider.
3. Complete Order and Certification for Home Health Services (“face to face”) using the dot phrase given
in the referral.
4. If the patient already has home health in place and you want to add a service, you can call the
providing agency to give a verbal order and have your note with the written order sent to the agency.
PERSONAL CARE SERVICES
! What: Hands-on assistance by a paraprofessional aide with Activities of Daily Living (ADLs). NC
recognizes 5 ADLs: (1) Bathing, (2) Dressing, (3) Mobility, (4) Toileting, (5) Eating (NOT
cooking/cleaning). Patient must need at least partial assistance with 3 of 5 ADLS or total
assistance with 1 or 2 of them.
! Who: Patients with Medicaid; patients with Medicare who are also receiving a home health skilled
service; some patients with private insurance. Also available for out-of-pocket cost.
! Patients with Medicaid:
o To determine whether your patient qualifies, use the Personal Care Services (PCS)
screening tool, which can be found in the attending room folders. This tool uses
information on 1) why the patient thinks they need an aide, 2) their ability to perform
ADLs, and 3) whether they are ambulatory.
o If you can legally attest that patient qualifies, complete Personal Care Services (PCS)
Request for Services form (MUST include diagnoses AND ICD-10 codes) and fax to
Liberty. Form is available at http://info.dhhs.state.nc.us/olm/forms/dma/dma-3051-ia.pdf
(instructions at http://info.dhhs.state.nc.us/olm/forms/dma/dma-3051-tips.pdf.) In
downtime, form is available in the BLUE folder in the exam rooms
o If patient has services, but needs additional hours: complete above form including pg 2
“Change in status” and fax to Liberty.
! Patients with Medicare/private insurance: When ordering Home Health skilled service, also
order In-Home Aide as needed. Otherwise, must pay out of pocket.
! Patients who plan to pay out of pocket: Patient contacts provider; directory of available
providers: http://www.homeandhospicecare.org/directory/index.html
Incomplete forms will be rejected, causing delay in starting services. Reference instructions as needed, or ask
Jan for help in completing forms correctly.
BEHAVIORAL HEALTH
BEHAVIORAL HEALTH ACCESS

Page 29 Last revised: June 2017
If any patient needs help connecting to mental health resources, refer to social work (Jan Dillard) for assistance.
HomeBASE Care Manager (Marigny Manson) is an RN who follows the clinic’s high-utilizing patients; she is also
available for short-term care coordination. See HomeBase section. Financial Counselors & Referral Coordinators
(Gloria Manley and Diane Bullock) can also help with referrals.
Patients with Private Insurance
Contact behavioral health customer service for the patient’s insurance (on insurance card) for pre-certification and
to locate an in-network provider.
Patients with Medicare
Directory of available providers: http://www.medicare.gov/physiciancompare/search.html
Patients with Medicaid or no insurance
! Contact local management entity (LME): http://www.ncdhhs.gov/mhddsas/lmeonblue.htm.
o 24-hour access for regular and crisis referrals
o LME refers patient to an appropriate community provider
o Services include therapy, group therapy, medication management, case management
! If a patient with Medicaid knows a provider that accepts Medicaid, they can self-refer
! Durham, Wake, Johnston and Cumberland counties
o Patient or provider + patient calls Alliance Behavioral Health at 800-510-9132 (line is open 24/7)
o Screening over the phone (~15-20 minutes) for insurance information, contact information,
primary concern, a safety screening, drug/alcohol use
o Patients can use the same number during mental health crises
o Use .ALLIANCEREFERRAL in patient instructions
! Other counties
! Orange, Person and Chatham counties: call Cardinal Innovations (800-939-5911).
! Franklin, Granville, Halifax, Warren and Vance counties: call Five County Area Program (877-619-
3761).
! Bladen, Columbus, Duplin, Edgecombe, Greene, Lenoir, Nash, Robeson, Sampson, Scotland,
Wayne, and Wilson Counties: call Eastpointe (800-913-6109).
MENTAL HEALTH CRISES
! If a patient has a mental health, substance abuse, or developmental disabilities service provider, they
should contact that provider first.
! If a patient does not already have a mental health provider, consider sending them to the Durham
Recovery Response Center (formerly Durham Center Access/DCA). DRRC is a place for emotional crisis
or substance abuse detox. It is run by Recovery Innovations and located at 309 Crutchfield St (919-560-
7305). It is open 24/7/365.
! If you don’t think the patient is safe to get to DRRC by themselves, you can call 919-428-0819 for the
Mobile Crisis Team. The mobile crisis team can meet the patient in a safe location (eg home, school,
workplace, doctor’s office, etc.) and/or take them to DRRC.
Contact information for other county teams:
https://www.ncdhhs.gov/assistance/mental-health-substance-abuse/crisis-services
DOMESTIC VIOLENCE SERVICES
! Refer to SW
! If patient declines SW referral, give info for Durham Crisis Response Center 24 hour crisis line (919-403-
6562 (English), 919-519-3735 (Spanish)) and document refusal.
! Services:
o Free legal clinic
o Safety Planning
o Support groups
o Information and case management
o Sexual assault services
Page 30 Last revised: June 2017
o Specialized safety programs
o Emergency shelter
o Counseling
o Hospital response
o Community outreach, education and training
o Rape prevention education
Page 31 Last revised: June 2017
SOCIAL WORK AND ACCESS TO CARE
CLINICAL SOCIAL WORK
- Jan Dillard, social worker
- HomeBASE Care Manager (Marigny Bratcher): RN who follows the clinic’s high-utilizing patients; she is
also available for short-term care coordination. See HomeBase section above.
- Financial Counselors & Referral Coordinators (Gloria Manley and Sophia Navarro)
o Assist patients with insurance-related questions and financial arrangements
o Manage patient referrals
o Meet with patients without insurance who might be eligible for Duke charity care.
Social Work Services
! Safety assessments and referrals/reports: SI, HI, domestic violence, abuse/neglect.
! Brief behavioral interventions at the time of appointment with the medical provider
! Assess patient using tools such as PHQ-9 and MoCA
! Comprehensive psychosocial assessments and chart review: obtain detailed work history, substance
use history, mental health history, funding, emotional support, coping strategies and personal
strengths/resources, ability to access medications and medical services.
! Individual and Group Counseling/Psychotherapy in may areas, including: depression, anxiety,
adjustment to illness, expression of suicidal/homicidal ideation, altered cognitive status, trauma,
substance abuse, patient and family education, grief, medication adherence, caregiver stress, crisis
pregnancy
! Home visits (1-2 per month)
! Brief crisis intervention and psychosocial support.
! Assistance with legal issues: guardianship, power of attorney, impending release from prison, criminal
issues, divorce and custody issues, undocumented immigrants, children in foster care system.
! Increase access to medications: NC MedAssist, Pharmacy Assistance Program at DUHS, community
resources.
! Refer to local community resources for help with housing, food, mental health, substance abuse,
developmental disabilities resources, legal aid, case management, job finding, etc..
! Help patients identify and locate programs for which they may be eligible: Medicaid, Medicare, SSI, SSDI,
food stamps
! Answer questions about provider-ordered home health and personal care service referrals and assist
patient with selecting a provider.
! Monthly Home visits with the DOC home visit team
! Discussion of healthcare power of attorney and advanced directives
! Provide%support%to%the%team>(#'-(,&Q& , ,# :* (# *('&&-& - >(+ # , $%; 5 :# , :9 (U%$)(,&K # ,- ($ 8 (6#'#K %'K($)&(
,&*+8'*&($8($) &(;) #::&' K&* (8Q()& #:$); #,& J
How to Refer to Social Work
- Best way is tostop by Jan’s office
- or send her an InBasket message, email, phone message or page
- In the body of in-basket message, use .SWDOCSWREFERRAL and complete template
- If you have time and Jan is available, stop by her office to give her a heads-up
MEDICAL TRANSPORTATION
A flyer containing all of the information below is in the SW door.
Medicaid
Patient can call any of the following for free Medicaid Access transportation 8a-5p
- Durham County Department of Social Services, 919-560-8607
- Orange County Public Transportation, 919-245-2871
- Person County Area Transport, (do not dial 1) 336-503-1178
Page 32 Last revised: June 2017
- Vance, Granville, Franklin, Warren Counties KARTS (Kerr Area Rural Transportation System), 800-682-
4329
- Franklin County, 919-496-5721
- Wake County Human Services 919-212-7000 option 2, then option 1
No Medicaid
Small fee per trip
- American Red Cross in Durham County: 919-489-6541; 8:30am-4pm; starts at $10/round trip
- Orange Public Transportation: 919-245-2008; 8am-4pm; cost varies depending on circumstance
- Person Area Transport: 336-597-1771; 8:30am-5pm; $10 to Duke, $2 local
- Vance, Granville, Franklin, Warren Counties KARTS (Kerr Area Rural Transportation System): 800-682-
4329; weekdays 5am-7:30pm, Saturdays 8am-5pm; $4-8 depending on length of trip
- Wake County TRACS: 919-212-7005; Monday-Friday 7am-12pm and 1-6pm; cost varies depending on
destination, starting at $2
Transportation for cancer treatment
American Cancer Society Road to Recovery: 800-227-2345
HOW TO MAKE BASIC CARE AFFORDABLE AND ACCESSIBLE
If your patient has barriers to care (eg vision, hearing, literacy, cultural and religious beliefs/practices, emotional
barriers, desire and motivation to learn, physical and cognitive limitations, language, lack of resources, history of
prior trauma, competing priorities), document them and get help addressing them from the SW staff, including Jan
Dillard and the financial counselors & referral coordinators (Gloria Manley and Diane Bullock).
Subsidized health insurance via the affordable care act
Uninsured patients who have an income can be referred to a navigator working with Project Access of Durham
County (PADC) to help them apply for subsidized coverage during open enrollment for the federal health
insurance exchange.
North Piedmont Community Care (NPCC) / Durham Community Health Network (DCHN)
- NPCC serves Durham and five rural counties north of the Triangle. The unit serving Durham is called the
Durham Community Health Network (DCHN).
- Patient population: patients who have been hospitalized or are using healthcare resources inefficiently,
patients with heart failure or diabetes, patients with Medicaid (automatically enrolled)
- Services:
o Health education
o Coordination of community resources
o Opioid safety
o Palliative care
o Transitions of care for hospitalized Medicare recipients
o In-home assessments with information relayed back to the referring provider
o Referral to mental health services
- Contact NPCC (919-620-8034) for more information
NC breast and cervical cancer control program (for the uninsured)
! Covers breast cancer screening for women 50-64yo
! Covers cervical cancer screening for women 18-64yo
! Covers cancer treatment and full Medicaid if diagnosed
Duke Charity Care
! Application process:

Page 33 Last revised: June 2017
o Patients must first apply for NC Medicaid and be denied. The only patients who do qualify for
Medicaid in NC are low income AND >65yo, visually impaired, disabled with inability to work for
>12 months, OR parenting a child <19yo.
o Patient must bring letter of denial
! Services that qualify for financial assistance or financial hardship are limited to:
o Emergent Services without which the patient’s health (or unborn child’s health if patient is
pregnant) could reasonably be expected be placed in serious jeopardy. These services are
limited to those provided in the ED.
o DUHS Physician Approved Services are services that are non-emergent but necessary and
appropriate to prevent serious deterioration in the health of the patient from injury or disease.
Often follow up services for care originating in the Emergency Department is included. DUHS
Physician approval is required prior to the service being provided.
! Application for coverage of prescription medications is separate.
! Some specialty services (eg elective ortho) may not be available.
! Refer patient to a financial care counselor for help applying.
The DOC Fund
Provides resources (medications, medical supplies, transportation, etc.) to patients on a case-by-case basis.
Used for short-term needs. Refer to Jan Dillard, LCSW to request.
Durham Medical Respite Program
! What: medical respite for homeless patients with acute medical needs
! Who: homeless patients who need home-like environment to recover from acute illness or prep for a
procedure
! How: If at DOC, send an inbasket message to Julia Gamble, who will review the case. If on inpatient
rotation, ask your PRM to refer the patient to Chrissie Moody, the complex care PRM at DUH.
RESOURCES FOR ESSENTIAL DAILY NEEDS
Below are lists of resources for food, shelter, clothing, etc.
- Durham County: http://www.blessdurham.org/wp-content/uploads/2011/07/DURHAM-RESOURCES-
MASTER-LIST.pdf
- Wake County: http://www.mentalhealthadvocacyinc.org/raleigh-resource-guide
- Orange County: http://www.needhelppayingbills.com/html/orange_county_assistance_progr3.html
- Vance, Granville, Henderson, Warren and Halifax counties:
http://issuu.com/hendersondispatch/docs/mhrd__11_mini-
tab__in_seq_?viewMode=presentation&mode=embed
Non-Medical Transportation
- Durham County
o DATA Fares and Schedules: 919-485-RIDE (7433)
o DATA ACCESS for people with disabilities: 919-560-1551, press 1; requires completion of an
application, medical provider’s signature
o Durham Center for Senior Life: 919-688-8247 ext.103; transportation to congregate meal at
Senior Center; free
- Orange Public Transportation: 919-245-2008; 8am-5pm; cost varies depending on circumstance
- Person Area Transport: 336-597-1771; 8:30am-5pm; $10 to Duke, $2 local
- Vance, Granville, Franklin, Warren Counties KARTS (Kerr Area Rural Transportation System): 800-682-
4329; weekdays 5am-7:30pm, Saturdays 8am-5pm; $4-8 depending on length of trip
- Wake County TRACS: 919-212-7005; Monday-Friday 7am-12pm and 1-6pm; cost varies depending on
destination, starting at $2

Page 34 Last revised: June 2017
CONTROLLED SUBSTANCES
DOC Pain group provides education and support to patients with pain. The clinical pharmacist administers pain
contracts with patients and meets monthly with them.
INITIATING NARCOTICS
What patients
! Failed to respond to 2-3 OTC analgesics and/or NSAIDS within a reasonable time period.
! Failed other pharmacologic therapies, eg steroid injections, nerve block
! Failed non-pharmacologic therapies, eg PT, rehab, TENS units
Contraindications
! Active substance abuse
! History of substance abuse (relative)
! Uncontrolled psychiatric disorder
! Chaotic home environment with difficult medication management (consult SW)
! Full body pain, fibromyalgia, chronic headaches, vague pain, or no diagnosis
! Positive screen for any illicit drugs in the past 3-6 months.
What to do before initiating narcotics
! Specify the cause of the pain
! Document intensity of the pain, current and past treatments, coexisting diseases, effect of pain on
physical and psychological function, history of substance abuse, negative urine drug screen
! Discuss and document risks and benefits of controlled substances
! Consider referring to social work for a psychosocial assessment to identify risk factors
! Refer patient to DOC PAIN Group for education and support
Medication choice & dosing
! Scheduled doses (vs PRN) if patient has continuous or frequently recurring pain
! Short-acting narcotics: tramadol, oxycodone
! Long-acting narcotics: if patient requires frequent short-acting narcotics, replace with long-acting
narcotics
o MS Contin
o Methadone (max dose at DOC is 40mg QD)
o Do NOT use oxycontin because it is expensive and can be abused more easily
! Breakthrough short-acting narcotics:
o No need for patients on methadone
o 30 pills per month for patients on MS Contin
Follow-up visits
! MD should see patient every 1-4 weeks initially; every 3 months once pain control is stable
! Document intensity, location, duration, aggravating and alleviating factors, effect of pain on function
! Document opioid-related side effects, aberrant drug-related behaviors
! No refills for early, lost or stolen meds.
! Additional short-acting pain medication can be prescribed when deemed appropriate by an attending
when there is an acute need.
PAIN CONTRACTS
When to start
! Patient has been on the same stable dose of a particular narcotic for >3 months
! Patient has been seen at DOC at least once before
! Nothing sketchy on the NC Controlled Substances Reporting System (aka the NC database)
! Nothing sketchy in North Carolina Department of Correction Public Access Information System
(http://webapps6.doc.state.nc.us/apps/offender/search1).
Page 35 Last revised: June 2017
! Patient passes Mayo drug screen x1
First narcotic prescription
! Get a blank agreement from Holly’s office or one of the preceptor rooms
! Review agreement with patient
! Explain to the patient that s/he will need to follow up every 3 months and provide urine samples upon
request
! Educate patient about side effects; differences between physical dependence, tolerance and addiction;
risk of developing physical dependence, tolerance and/or addiction; and potential for cognitive
impairment. MD, PharmD, LPN or RN can do this.
! Both provider and patient sign the agreement
! Duke UDS
! Give patient first prescription at this visit.
! In the ‘Follow-up’ section of Visit Navigator, under ‘Check-out instructions,’ type “Pharm CII on or before
[30 days from date of Rx].”
! Return signed agreement to Holly’s office along with 3 future 30d prescriptions for the prescribed opioid
Follow-up visits
! All visits: pharmacist evaluates pain, functioning, adverse effects, and potential for misuse
! Visit #2: review the Controlled Substances Agreement in detail.
! Visit #3: after the initial 3 prescriptions have been used, a request for refills will be placed in your
partnership folder. Print out 3 new 30d prescriptions, place them in the file, and return to Holly’s office.
! Yearly: pharmacist or PCP must review the pain contract with the patient
! No refills for chronic pain medications during acute care visits
! If a prescription is lost or stolen, do NOT supply a new prescription. Police report will not change this.
! Drug screening
o UDS q3-4 months for compliance (Mayo) and illicit substances (Duke); Mayo should be sent at
least 1-2x per year
o Serum drug levels is used in rare cases, usually anuria.
Violations
! Terminate contract if pt exhibits aberrant behavior on multiple occasions (document each in chart):
o Multiple missed appointments
o Prescriptions from another provider
o Taking medications inappropriately
o Repeatedly contacting PCP or clinic for refills
! Terminate contract immediately if:
o Forged prescriptions
o UDS screen for illicit substance (including THC) or non-prescribed controlled substance (including
benzodiazepine)
o Mayo UDS results negative for prescribed narcotic
o Mayo UDS results inconsistent with dosing
! If narcotics are discontinued, this should be clearly documented in the problem list
Reinstatement of pain contract
! This is a decision that is made on an individual basis after at least 6 months
! Patient must attend PAIN group or substance abuse treatment
! No reinstatement if patient has been violent
! Must be approved by attending
BENZODIAZEPINES
! Use of non-addicting medication such as SSRI’s is preferred for anxiety.
! Referral to psychiatry for use of benzodiazepines is preferred.
! Prescribe short-acting benzodiazepines (eg lorazepam) for 3 months maximum; for continued use,
psychiatry needs to prescribe

Page 36 Last revised: June 2017
! NO alprazolam (Xanax)
! Consider long-acting benzodiazepines after discussion with patient and signing a pain contract
Drug Screens commonly used & available at Duke Outpatient Clinic
In-House
1. Toxicology (Drug) Screen, Urine
a. Order in Maestro: LAB6266
b. Results same day
c. Tests for: amphetamines, barbiturates, benzodiazepines, Cocaine, opiates, THC
2. Toxicology (Drug) Screen, Serum
a. Order in Maestro: Lab678
b. Results same day
c. Tests for acetaminophen, salicylate, ethanol
d. Do not recommend using
3. Methadone (dolophine), serum confirmation – can use if methadone not detected in either of the Mayo
drug screens
a. Order in Maestro: Lab6655
b. Not detected unless 25 ng/mL à if negative, consider calling LabCorp for verification (their limit of
detection is a total daily dose of 25 mg)
c. Results back within 48 business hours
d. This is run through LabCorp in Burlington, NC
4. 10 Panel Drug Screen
a. Order in Maestro: Lab7797
b. Tests for: methadone, propoxyphene, amphetamine, barbiturates, benzodiazepines, cocaine,
opiates, THC, methamphetamines, PCP,
c. Would recommend this for a patient that you want a broader illicit substances screen than the
typical UDS
d. Of note, methadone confirmation is 250 ng/mL
Send -Out
1. Mayo Drug Screen, urine
a. Order in Maestro: Pain Clinic Survey, Urine Lab (Lab9486)
b. Results back in approximately one week since this is a send out
2. Mayo Serum Drug Screen
a. Order in Maestro: Gen Code Commercial Lab – Blood; in the comments: insert Mayo
serum/plasma panel 9 drug screen FDS9R
b. Results back in approximately one week since this is a send out
Cannot do the RAPIDDRUG Screens since these require special equipment that we do not have.
CONTROLLED SUBSTANCES SCHEDULES
Schedule
1
2
3
4
5
6 (NC)
Substance
Heroi
n
Cocaine
(illicit)
Codeine
Fentanyl
Hydrocodone
Buprenorphi
ne
Butalbital ±
aspirin
(Fiorinal)
Benzodiazepin
es (i.e.
diazepam,
lorazepam,
etc)
Cough
syrups
with
codeine
10-12
Marijuana,
Tetrahydrocannbin
ols, Synthetic
Cannabinoids

Page 37 Last revised: June 2017
Hydromorpho
ne
Meperidine
Methadone
Methylphenid
ate
Morphine
Oxycodone
Pentobarbital
Codeine
+APAP
(tablet form)
Dronabinol
Ketamine
Oxandrolone
Testosteron
e
Butorphanol
Carisoprodol
Lorcaserin
Midazolam
Phenobarbital
Phentermine
Tramadol
Zaleplon
Zolpidem
mg/5mL
Lacosami
de
Pregabali
n
Potential
for Abuse
++++
++++
+++
++
+
Accepted
Medical
Use
No
Yes
Yes
Yes
Yes
----
Prescripti
on
Required
----
Yes
Yes
Yes
Yes/No
----
Quantity
Limit
----
None
180 days
180 days
None
----
Telephone
Prescribin
g
----
No
Yes
Yes
Yes
----
Electronic
Prescribin
g
----
No
No
No
No
----
Refills
Allowed
----
No
5 refills within 6 months
No
restriction
----
Notes:
APAP+Butalbital+Caffeine (Fioricet) is a non-scheduled substance.
Prepared by Holly Causey, PharmD, BCACP, CPP, CDE; version 2/15/17
Reviewed by Mackenzie Dolan, PharmD Candidate; version 2/15/17

Page 38 Last revised: June 2017
CLINICAL ALGORITHMS
BRIDGING (PAUSING) ANTICOAGULATION
Source: Duke Medicine Clinical Practice Guideline for the Management of Anticoagulation Therapy in
the Ambulatory Setting. January 2009.

Page 39 Last revised: June 2017

Page 40 Last revised: June 2017
DEPRESSION MANAGEMENT ALGORITHM
Always offer counseling to your patients who suffer from depression. Talk to the Med-Psych attending for help
determining whether they should be seen by a Med-Psych resident at DOC or by a psychologist or psychiatrist
outside of DOC.

Page 41 Last revised: June 2017

Page 42 Last revised: June 2017
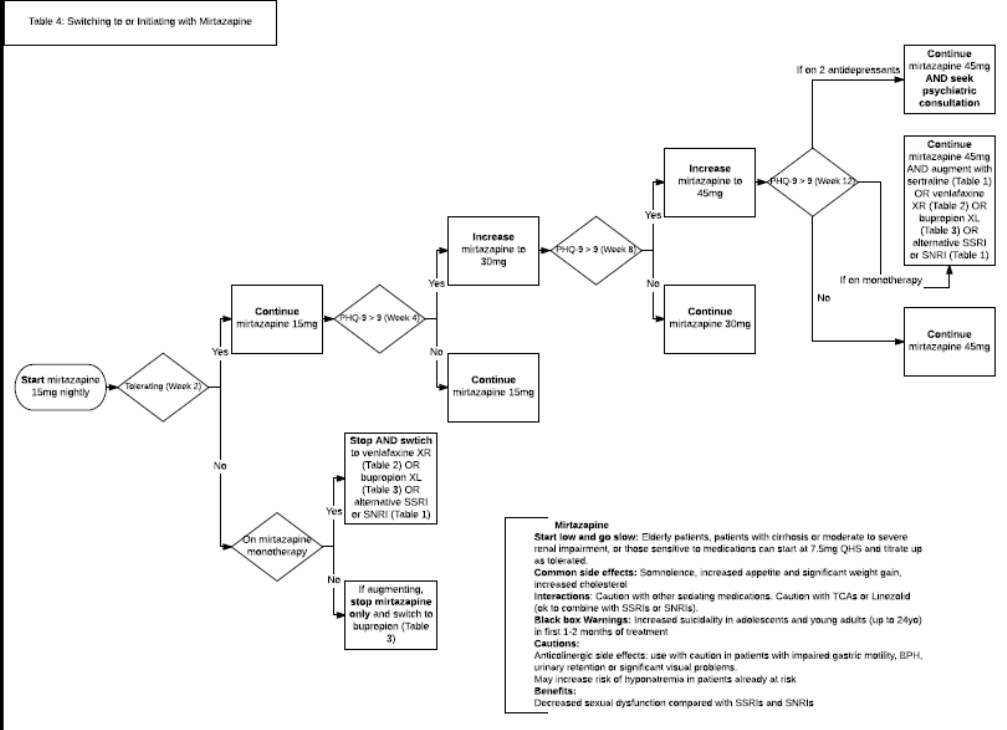
Page 43 Last revised: June 2017

Page 44 Last revised: June 2017
POTASSIUM MANAGEMENT
Under the Clinical Pharmacist Practitioner agreement at the DOC, our clinical pharmacist Holly Causey can
manage potassium in patients with clinical conditions receiving diuretic or other anti-HTN meds.
Table 1: Potassium replacement
Notify Attending MD for K+ < 2.7 or > 5.9. For K+ > 6.5, recommend emergency treatment, including an
EKG.
ADDITIONAL TREATMENT CONSIDERATIONS:
- Dietary counseling. Review foods high in potassium that patient should consume or avoid.
- Hyperkalemia symptoms: listlessness, mental confusion, weakness, paresthesias
- Hypokalemia symptoms: fatigue, myalgia, weakness, and cramping
- Patients with any cardiac history and/or taking digoxin are considered high risk.
- If patient taking K+ salts such as LiteSalt or NuSalt, or NSAIDs, recommend discontinuation.
- If patient is prescribed spironolactone or an ACEi/ARB with hyperkalemia (K+ ≥ 5.6) on no potassium
supplementation, instruct patient to hold the medication for 2 days then resume at half dose. If patient is
taking a potassium supplement as well as spironolactone or an ACEi/ARB, instruct patient to hold
medication for one day and follow above recommendations for holding potassium supplement.
References:
Asheville Cardiology Associates. Potassium Protocol
UK Renal Association. Clinical Practice Guidelines: Treatment of Acute Hyperkalemia in Adults. July 2012.
Creatinine
Potassium
2.7-2.9
Potassium
3 – 3.2
Potassium
3.3-3.4
Potassium 3.5-
3.9
Potassium
5.6-5.9
< 1.5
40 meq bid x 2
days, in addition
to current dose.
Then long term
dose increase of
30 meq’s daily
40 meq bid x 1
day, in addition
to current dose.
Then long term
dose increase of
20 meq’s daily
Consider long term
dose increase of 20
meq’s daily
Re-check in 1
week if increasing
diuretic
Hold x 2 days
then decrease
dose by 50%
1.5-2
40 meq bid x 2
days, in addition
to current dose.
Then long term
dose increase of
20 meq’s daily
40 meq bid x 1
day, in addition
to current dose.
Then long term
dose increase of
10 meq’s daily
Long term dose
increase of 10 meq’s
daily
Re-check in 1
week if increasing
diuretic
Hold x 2 days
then decrease
by 50%
2-2.9
40 meq daily x 2
days, in addition
to current dose.
No long term
dose increase
40 meq daily x 1
day, in addition
to current dose.
No long term
dose increase
20meq x 1 day, in
addition to current
dose. No long term
dose increase.
Re-check in 1
week if increasing
diuretic
Hold x 2 days
then decrease
by 75%
>3
Notify Attending
Notify Attending
20 meq
x 1 day, no increase
in chronic dose
Re-check in 1
week if increasing
diuretic
Notify
Attending
Labs
should
include
BMP
Follow up labs
4 days
Follow up labs
7 days
Follow up labs 7-10
days
Follow routine
monitoring if no
med changes
48 hours

Page 45 Last revised: June 2017
VACCINATION SCHEDULE (CDC)
https://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf

Page 46 Last revised: June 2017
USING MAESTRO CARE (EPIC)
Troubleshooting
Helpdesk: (919) 684-2243, choose option #5
Maestro “Super Users” at DOC: Dr. Bowlby & Dr. Zipkin
MAKING YOUR ENCOUNTER MORE EFFICIENT
• Order items on the left hand column for better function during all encounters
• Move diagnoses between History, Problem List, and Visit
• Review Flowsheets (vitals, diabetes detail)
• Common Diagnosis buttons: populate these for easy use for routine healthcare maintenance orders
• Orders favorites: Go to Epic menu à preference list composer à Patient Care Tools
• Medication prescribing: delete END DATE, make sure quantity is correct, refills for 30 or 90 day supply.
• Be aware that we CANNOT discontinue meds in the system, must add that on as a note to the pharmacy
when you do a new Rx.
• Uploading images: Take a photo using the Epic Haiku app (ask a resident or attending to show you how).
It will automatically upload to the “Media” tab of the patient’s chart. Copy and paste the image into your
note
o To get Haiku on your phone, go to
https://intranet.dm.duke.edu/sites/MaestroCare/Mobile/SitePages/Home.aspx
• Speed buttons for check out in the ‘follow up’ section
See Dr. Zipkin for extra tips!
EPIC INBASKET
You are responsible for your patient panel and following up on all tests ordered on your patients. When you are
on a busy service, new patient questions will be routed to other people in your partnership group. However, tests
you ordered from clinic will still result to you. No one is necessarily double checking how you handle your test
results, so make sure you act in timely manner, and if you need help be sure to ask!
When you need help with something and want to route an encounter to your nurse, please refer to the partnership
map to know who your team nurse is (Group A is Amber Walters, Group B is Diana (Glenda) Wamsley, Group C
is Johna Weilacher) and put that nurse in the routing field.
• Move folders up and down per your preferences (use the wrench)
• Involve the nursing team where appropriate. They can contact patients on your behalf if needed.
• Patient Calls: click “QuickNote” to bounce back to nurse, or “Enc” to document your portion of the call.
Do not use “comment”, as this doesn’t go anywhere.
• Patient advice request: click “Reply to pt,” or “MyChtEnc”. Route if needed. Clicking on “tel call” creates
a new encounter.
• Results: click “Rslt Release” to release the results in MyChart (if patient has MyChart). Click “Letter” to
populate a letter with the results, and then route the letter to the medical records pool so they can send
the letter to the patient. Click “result note” to comment and route to nurse for help
o Please note that abnormal results for HIV, GC, Chlamydia, and Syphilis are to be sent to Molly
Jarvis. She collects them and reports to the health department for us. This is in addition to you
notifying the patient and treating them.
• Rx request: click “EditRx,” or “Approve All.” If you want to enlist nursing help, click “Enc,” or “QuickNote.”
• Referral message: Right click, reply to all or reply to sender
• CC’d charts: Specialists route their notes to you, as the patient’s PCP. These are mostly FYI.
• Staff Messages: This is like email, except harder to figure out who is sending and who is copied. These
messages are not recorded in the patient’s chart.
• Patient station (icon on topmost banner of Epic): Click on this to start any new encounter or go into an
existing open encounter, whether routed to you or not.
Page 47 Last revised: June 2017
• Orders only encounters: For times when a patient needs to return for blood work outside an encounter;
make all orders “future”, even if being done that same day.
VISIT TYPES
Although from a scheduling/administrative perspective there are officially only two basic visit types (new patient
visits defined by Medicare as not having been seen at the DOC for 3 years; and returns), there are actually
many different visit “flavors,” which we encourage you to use explicitly (e.g., bringing patients with uncontrolled
chronic illness back for prepared chronic disease-focused visits at regular intervals, outside of acute visits). Doing
so can help you avoid becoming overwhelmed by having to address every issue at every visit, or being purely
reactive. Of course, the realities of patients’ lives force us to be opportunistic as well, taking care of what we can
when patients present to clinic, regardless of reason (e.g., refills, health maintenance, interrupted workups for
potentially concerning complaints, etc.)
Visit “flavor”
Brief description (including objectives for visit)
New
Complete review of past medical history, social history, family history, plus
thorough review of 10+ systems
Return
Second official visit type; but actually fall into many subtypes. Can be to follow up
on acute complaints not able to be addressed in a single visit; or in follow-up of
prepared chronic illness visit, at whatever interval/frequency is required.
Acute
Patient-made appointment to address a particular problem
Annual
Although the evidence for the benefit of these is mixed, can provide a set-aside
opportunity to catch up specifically on health maintenance, update history, and
address patient self-management goals and goals of care. It can also be a good
time for completing PHQ-9 (depression) and AUDIT (EtOH) screening. Of note,
Medicare has a very specific Annual Wellness Visit format, reimbursed separately.
Chronic illness
PREPARED visits focused on one or more chronic conditions that a patient may be
struggling to get under control. Verbally contract w/ patients before setting these
up that these visits will be to address their chronic condition(s). In reality, care
cannot easily be compartmentalized, but it can provide both you and the patient
some time/space/clarity to establish a plan for the next 12 months, to-dos, etc.
Group
In conjunction with weekly PAIN, diabetes or hypertension group visits
Home
A multidisciplinary team (resident, Ambulatory Chief Resident, pharmacist, social
worker) can visit a patient’s home to identify/address potential barriers to health
Hospital follow-up
Use the .DAZHOSPFU template within your note. Main purposes are to: a)
assess condition s/p hospitalization, and patients’ understanding of why they were
hospitalized and what they can do to avoid re-hospitalization; b) complete to-dos
from discharge summary; c) ensure any medication changes made on discharge
have in fact been implemented w/o adverse events; d) address any urgent issues;
and e) schedule them soon (< 6 weeks) to return to their assigned PCP.
Paperwork
To enable completion of a particularly time-consuming form (e.g., FMLA), or one
that requires a provider assessment (e.g., FL-2)
Procedure
New this year, staffed by Larry Greenblatt and intended to be where patients can
be “referred” for joint/bursa injections, cryotherapy, even punch biopsies, etc. in
clinic
DOCUMENTATION OUTSIDE A VISIT
Maestro Care has specific documentation pathways that vary based on whether you are documenting information
during a patient visit versus outside of a patient visit. The following table highlights the workflow for a few
different types of documentation outside of a patient visit in Maestro Care.
Documentation Purpose (when
completed outside of patient visit)
Encounter Type
Medication refill
Medication Refill Encounter
Page 48 Last revised: June 2017
Documenting a phone
conversation
Telephone Encounter
Ordering a referral
Orders Only Encounter OR
In Basket message to the Referral
Pool
DOCUMENTATION OF PSYCHOSOCIAL NEEDS
A third, emerging priority will be to better understand the impact of social determinants of health on the needs of
our patients – which requires better documentation. The following list was compiled after extensive discussion:
Code
Notes
Lack of Housing Z59.0
also refers to unstable housing
Financial Difficulties Z59.8 and Dependent
for Transport Z74.8
e.g., transportation, clothing
Problems with Literacy Z55.0
1-question screen: “How confident are you filling out
medical forms by yourself?” Screening for health literacy is
also a PCMH (primary care medical home)
REQUIREMENT.
Lack of Adequate Food Z59.4
Adult Maltreatment T74.91XA
includes ONGOING adult physical, sexual, psychological
abuse, and neglect (i.e., domestic violence, elder abuse)
Cognitive Impairment 294.9
including memory problems, not rising to level of dementia
Ineffective Self Health Management
V49.89
Underdosing of medications due to
financial hardship Z91.120
History of Childhood Maltreatment Z62.819
Lives in a Group Home Z59.3
SMARTPHRASES
Note: To insert the smartphrases below into your note or patient instructions, each phrase must be preceded by a
period (“.”). For example, to insert a template for a follow-up visit, start typing “.dazfu” and choose the
smartphrase you’re looking for from the drop-down menu that pops up.
TEMPLATES FOR CLINIC NOTES
Name of template
Description
DAZANNUAL
Template for an annual visit
DAZFU
Template for a follow-up visit
DAZNEWTEMPLATE
Template for a patient who is new to the DOC
DAZHOSPITALFU
Insert this template into the “HPI” section of your new or follow-up
note if the visit is a hospital follow-up appointment
DOCGROUPDM
Template for DM group visit
DOCGROUPHTN
Template for HTN group visit
DOCSARHANDOFF
Template for SAR handing patient off to intern
DOCNEWFEMALEUNDER50
Template for new female patient under age 50
DOCNEWMALEUNDER50
Template for new male patient under age 50
HPI
Name of template
Description
DAZHPIDM
HPI info for a routine diabetes visit
DOCASTHMASEVERITY
HPI info for routine asthma visit
DOCCOPDSEVERITY
HPI info for routine COPD visit

Page 49 Last revised: June 2017
DOCDNRDISCUSSION
To document DNR discussion in HPI
WEIGHTLOSSSURGERY
For patients who present for f/u of weight loss attempt in preparation
for bariatric surgery
EXAM AND PROCEDURES
Name of template
Description
LASTWT(3)
Quick trend of weights
LASTTEMP(3)
Quick trend of temperatures
LASTBP(3)
Quick trend of BPs
LASTPULSE(3)
Quick trend of pulses
LASTDM(3)
Quick trend of diabetes data
DOCDIABFOOTEXAM
To document a diabetic foot exam (including monofilament)
LGKNEEINJECTION
Template for knee injection procedure
LGSHOULDERINJ
Template for shoulder injection procedure
ASSESSMENT AND PLAN
Name of template
Description
DIAGMED
Pulls in all orders as linked to diagnoses, with nicely formatted area
for writing your thoughts
DOCDMGOOD
Include in the a/p for a patient who has DM and all parameters are in
order
DOCDMUNCONTROLLED
Include in the a/p for a patient with uncontrolled DM
DOCLBPUNCOMPLICATED
Text for the a/p about management of uncomplicated lower back pain
DOCACCLIPIDS
Text for the a/p about using the new ACC lipid guidelines
LGDRYSKIN
Text for the a/p about management of xerosis
DOCHOMEHEALTHFACETOFA
CEDOCUMENTATION
Order and certification for home care services (include in your
progress note)
HOMEHEALTHSETUP
Info for YOU (not the patient) on how to order home health
BEHAVIORAL HEALTH
Name of template
Description
FFGAD7
Validated, widely-used 7-item anxiety screening tool
FFPTSDSCREEN
2-item validated PTSD screening tool (from the VA)
DOCPHQ2
Brief depression screen
PHQ9
Full PHQ-9 in compact format
DAZPHQ9FLOW
Pulls PHQ-9 flowsheet into note
DOCETOHCAGEQUESTIONS
CAGE questionnaire for alcohol abuse
DOCAUDITC
3-item standard alcohol abuse screening
DOCAUDIT
10-item standard alcohol abuse screening (more accurate)
DOCDAST10
10-item drug abuse (prescription or otherwise) screening
DOCACESCORE
Calculator for adverse childhood events
NC41CRISISLINE
Phone number for Durham Center Access Crisis Line and Suicide
Prevention Line
SUICIDERISK
Suicide risk assessment
DOCCRISISSERVICES
List of crisis resources
DOCSLEEPHYGIENE
Sleep hygiene instructions
PATIENT INSTRUCTIONS
Name of template
Description
DAZLOWCARBREC
Dr. Zipkin’s brief recommendations for low carb diet
DOCDIETADVISOR
Includes “my plate” and table of glycemic index of

Page 50 Last revised: June 2017
common foods
DOCLOWGLYCEMIC
Table of glycemic index of common foods
DOCEXERCISEOPTIONS
Options for daily exercise
DOCQUITSMOKINGHOTLINE
Smoking cessation hotline
DOCMEDLINEPLUS
Instructions for patient on how to get information
from Medline Plus
DOCASTHMAACTIONPLAN
Asthma action plan
DOCDEPRESSIONSELFCAREPLAN
Behavioral interventions for depression
DOCDIABHYPOGLYLCEMIAINSTRUCTIONS
Instructions re: hypoglycemia for patients on insulin
DOCDIABINSULININSTRUCTIONS
Instructions re: diabetes care if taking insulin
DOCDIABORALINSTRUCTIONS
Instructions re: diabetes care if taking oral meds
DOCDIABSLIDINGSCALEINSTRUCTIONS
Instructions re: insulin sliding scale
DOCEMERGENCYPSYCHMEDS
For patients who have a psychiatrist and are
requesting meds
NARCOTICEDUCATIONBASIC
Low literacy information about narcotics
NARCOTICEDUCATIONFULL
Information about narcotics
DOCOPIOIDVIDEOPATIENTEDUCATION
12 patient education videos regarding opioids
DOCGROUPSERVICES
Explains the group visits (DM,HTN and pain)
DOCMYCHART
Explains MyChart and how to install
DOCPACEREFERRAL
Information for YOU (not patient) about PACE
(program of all-inclusive care for the elderly) and
referral instructions
DOCBRIEFMENTALHEALTHREFERRALTO-
ALLIANCE
For patients with Medicaid or without insurance
who need to connect with substance abuse, mental
health, or developmental disability services
DOCHEALTHINSURANCEEXACHANGE
Information about signing up for the exchanges
DOCMEDICAIDTRANSPORTATION
How to get free transportation if you have Medicaid
DOCPHARMREFERRAL
Information regarding what a clinical pharmacist will
do and what to bring to an appointment with
pharmacy
DOCADVANCEDDIRECTIVES
Instructions re: what AD are and where to find the
appropriate forms
SOCIAL WORK
Name of template
Description
FFHOUSINGSCREEN
Standard screening tool looking for risk factors for unstable
housing and homelessness (from the VA)
DOCSWREFERRAL
Use when referring a patient to DOC social worker (use in the
text of an InBasket message to Jan Dillard)
SWFREEMEDSAP
Info for patient on how to apply for patient assistance program
to get medications sponsored
DOCCANIMANAGEMONEY
Info for patient about how to become his or her own payee if
he/she currently has a representative payee
DOCAIRCONDITIONERLETTER
Letter documenting a patient’s need for electricity, heating, or
air conditioning
DOCHOMEVISITREFERRAL
Use when referring patient for a home visit by the DOC team

Page 51 Last revised: June 2017
HOW TO HELP PATEINT WHO CANNOT AFFORD MEDICATIONS

Page 52 Last revised: June 2017
CREDITS
Please email questions/comments/suggestions to Lynn Bowlby or Ben Ranard
2017-2018 Revision
Lynn Bowlby
Larry Greenblatt
Joseph Plaksin
Benjamin Ranard
Dani Zipkin
Holly Causey
Jan Dillard
Greg Brown
Previous editions
Armando Bedoya
Adrienne Belasco
Stephen Bergin
Lynn Bowlby
Holly Causey
Alex Cho
Natasha Cunningham
Jan Dillard
Denise Duan-Porter
Megan Gillum
Gina Green
Larry Greenblatt
Ivan Harnden
Kathleen Kiernan Harnden
Brandie Johnson
Marigny Manson
Jay Mast
Laura Musselwhite
Sarah Nouri
Venu Reddy
Marcus Ruopp
Kevin Shah
Jessica Simo
Caroline Sloan
Ben Smith
Dani Zipkin
