
1
Centers for Medicare & Medicaid Services (CMS)
Center for Medicare and Medicaid Innovation (Innovation Center)
Kidney Care Choices (KCC) Model
PY2023 Request for Applications (RFA)
Table of Contents
I. The Kidney Care Choices (KCC) Model Overview ............................................................................. 3
A. Background and Introduction ............................................................................................. 3
B. The KCC Model .................................................................................................................. 4
C. Timeline .............................................................................................................................. 5
II. General Provisions ................................................................................................................................ 7
A. Monitoring and Oversight ................................................................................................... 7
B. Remedial Action and Termination ...................................................................................... 7
C. Screening ............................................................................................................................ 8
D. Evaluation ........................................................................................................................... 8
E. Learning and Diffusion Resources ...................................................................................... 9
F. CEHRT Requirements ...................................................................................................... 10
G. Waivers ............................................................................................................................. 10
H. Amendment ....................................................................................................................... 11
III. CMS Kidney Care First (KCF) Option ............................................................................................... 13
A. Legal Entity ....................................................................................................................... 13
B. Governance Structure Requirements ................................................................................ 13
C. Applicant Eligibility ......................................................................................................... 13
D. Beneficiary Alignment ...................................................................................................... 15
E. Finance and Payment ........................................................................................................ 20
F. Quality Strategy ................................................................................................................ 29
G. Benefit Enhancements ...................................................................................................... 29
H. Beneficiary Engagement Incentives ................................................................................. 32
I. Termination ....................................................................................................................... 34
J. Application for KCF Option ............................................................................................. 35
IV.
Comprehensive Kidney Care Contracting (CKCC) Options .............................................................. 40
A.
Legal Entity and Governance Requirements .................................................................... 40
B.
KCE Composition ............................................................................................................. 42
C.
Beneficiary Alignment ...................................................................................................... 44
D.
Finance and Payment ........................................................................................................ 50
Updated 03/06/2022 2
E.
Quality Measures and Scoring .......................................................................................... 65
F.
Benefit Enhancements ...................................................................................................... 66
G.
Beneficiary Engagement Incentives ................................................................................. 73
H.
Termination ....................................................................................................................... 75
I.
Application for CKCC Option .......................................................................................... 76
V.
Appendix A: Glossary of Key Definitions .......................................................................................... 83
VI.
Appendix B. Applicant Selection Criteria and Scoring ...................................................................... 87
Updated 03/06/2022 3
I. The Kidney Care Choices (KCC) Model Overview
A. Backg
round and Introduction
According to 2019 data from the Centers for Disease Control and Prevention (CDC), Chronic Kidney
Disease (CKD) impacts over 37 million or 15% of Americans, and most of them are unaware that their
kidneys have reduced function or are failing. While there are certain factors predisposing people to CKD,
most causes of CKD are acquired rather than inherited. Diabetes and hypertension accounted for up to
two-thirds of all cases, followed by diseases that damage the kidney’s filtration units.
According to the United States Renal Data System (USRDS), in 2017 Medicare beneficiaries with CKD
a
ccounted for $84 billion in Medicare spending, in addition to $35.9 billion for the End-Stage Renal
Disease (ESRD) population, for approximately $120 billion in total expenditures.
Once an individual has progressed to stage 4 CKD, when their glomerular filtration rate (GFR) has
d
ecreased to 15-30ml/min, kidney disease has become severe enough that the individual will likely
experience specific symptoms and need to consider planning for dialysis or kidney transplantation. Those
in stage 4 CKD are likely to develop more severe complications such as hypertension, anemia, bone
disease, heart disease, ischemic stroke, and other cardiovascular diseases. Once an individual’s GFR
drops below 15ml/min, they have progressed to stage 5 CKD. During this advanced stage, the kidneys
have lost nearly all function. Without intervention, the patient will progress to ESRD, at which point
dialysis or a kidney transplant is required for survival (National Kidney Foundation, 2018).
A major challenge in the study and treatment of CKD is the heterogeneity of the condition. For most
p
atients, CKD is asymptomatic and can only be detected with laboratory studies. The time of progression
to ESRD requiring renal replacement is variable depending on the patient and comorbidities. Early
intervention can sometimes slow the progression of CKD and ESRD.
The best renal replacement therapy for most patients with ESRD is a kidney transplant, which replaces
the failed kidneys with a more functional, healthy kidney from either a living or deceased donor. In 2018,
22,393 kidney transplants were performed in the United States, more than half of which were from
deceased donors. Patients who have received a kidney transplant still have kidney disease and still
require long term medications and medical care to ensure the health and function of their transplanted
kidney. However, kidney transplants are associated with improved quality of life, reduced cardiovascular
complications, improved morbidity and mortality, and reduced oxidative stress relative to dialysis. If the
transplanted kidney stops functioning, dialysis or another transplant is needed.
As patients with CKD are educated about their treatment options, some patients consider transplantation
b
efore, and others after, the initiation of dialysis. At the end of 2020, approximately 92,000 patients were
on the Organ Procurement and Transplantation Network (OPTN) deceased donor kidney transplant
waiting list. The demand for kidney transplant far exceeds the supply. Other barriers to transplantation
include: financial burdens, poor communication between provider and patient, poor patient education
regarding transplantation, lack of access to high quality health care services, and the absence of a
committed care taker.
The Comprehensive ESRD Care (CEC) Model began in October, 2015, and ended March 31, 2021. The
CE
C Model provided financial incentives for dialysis facilities, nephrologists, and other Medicare
providers and suppliers to work together to improve outcomes and reduce per capita expenditures for
aligned ESRD beneficiaries in an accountable care organization (ACO) framework. Key features of the
Updated 03/06/2022 4
CEC Model included: 1) total cost of care accountability; 2) comprehensive and coordinated care
d
elivery; and 3) improved access to care.
Evaluation of the first four Performance Years (PYs) of the CEC Model for the 37 ESRD Seamless Care
Or
ganizations (ESCOs) that participated in the CEC Model between October 1, 2015 through December
31, 2019) demonstrated promising findings, showing lower spending and improvements on some
utilization and quality measures. Reduced spending for ESCO beneficiaries was primarily attributed to a
reduction in hospitalizations and post-acute care. The CEC Model also showed improvement in quality of
care as demonstrated through a decline in catheter utilization among aligned beneficiaries relative to the
comparison (non-ESCO beneficiary) group.
While the CEC Model showed some positive results, the design had several limitations. Based on lessons
l
earned from the CEC Model, we have identified the following areas for potential improvement. We have
incorporated these areas in the design of the Kidney Care Choices (KCC) Model, which includes the
CMS Kidney Care First (KCF) and Comprehensive Kidney Care Contracting (CKCC) Options:
•
Including beneficiaries with CKD stage 4 and 5 before they progress to ESRD in the KCC Model
to promote later and better starts on dialysis, or to avoid dialysis entirely.
•
Including beneficiaries after they receive a transplant and incorporating financial incentives to
promote greater utilization of transplants.
•
Empowering nephrologists to take the lead in coordinating care for beneficiaries across the care
spectrum.
•
Including Benefit Enhancements to support improved utilization of skilled nursing facilities
(SNFs) and hospice care, telehealth services, and the Kidney Disease Education (KDE) benefit
•
Addressing nephrologist payment in order to better align payments with care.
The KCC Model seeks to address the limitations observed in the CEC Model in its test of whether a
m
odel of care in which a single set of health care providers with aligned incentives are responsible for a
patient’s care from the later stages of CKD to and through dialysis, transplantation, or end of life care will
improve overall quality of care and reduce the cost of care for beneficiaries with kidney disease. Statutory
Authority
Section 1115A of the Social Security Act (added by section 3021 of the Affordable Care Act) (42 U.S.C.
1315a
) authorizes the CMS Innovation Center to test innovative payment and service delivery models that
have the potential to lower Medicare, Medicaid, and CHIP spending while maintaining or improving the
quality of beneficiaries’ care. Under the law, preference is to be given to selecting models that also
improve coordination, efficiency and quality of health care services furnished to beneficiaries. Section
1899 of the Social Security Act establishes the Medicare Shared Savings Program, and authorizes CMS to
share Medicare savings with participating accountable care organizations under certain circumstances.
The KCC Model described in this Request for Applications (RFA) uses the CMS Innovation Center’s
au
thority to test a new model of care delivery and payment for Medicare beneficiaries with late stage
CKD and ESRD. CMS is testing whether the financial risk arrangements outlined in this RFA improve
quality of care for beneficiaries with CKD and ESRD and reduce Medicare costs.
B. The KCC Model
For the KCC Model (or the Model), the Innovation Center builds upon and improves the structure of the
financial and payment elements used in the CEC Model to address areas for potential improvement that
have been identified through testing the CEC Model. The KCC Model has four Model Options fitting in
Updated 03/06/2022 5
with the Innovation Center’s suite of total cost of care models. These Model Options will test whether
t
hese design elements reduce Medicare spending and improve the quality and coordination of care for
beneficiaries with late stage CKD, ESRD, and kidney transplants.
Under the CMS Kidney Care First (KCF) Option, CMS will make adjusted capitated payments to
pa
rticipating nephrology practices (KCF Practices) for managing beneficiaries with CKD Stages 4 and 5
and ESRD. CMS will additionally make performance-based payment adjustments to both participating
nephrology practices and, separately, to their nephrology professionals based on how well the practice
performs on specified quality measures. The KCF Option is designed to emulate the basic design of the
PCF Model, in which participating practices are accountable for managing the care of attributed
Medicare beneficiaries. The KCF Option further includes Benefit Enhancements and Beneficiary
Engagement Incentives that participating nephrology practices may choose to make available in order to
support high-value services and allow the practices to more effectively manage the care of their aligned
beneficiaries. The KCF Option is a Merit-based Incentive Payment System (MIPS) Alternative Payment
Model (APM) and an Advanced Alternative Payment Model (Advanced APM) beginning in 2022.
For the three Comprehensive Kidney Care Contracting (CKCC) Options, nephrology professionals must
pa
rtner with transplant providers, and may partner with dialysis facilities and other providers and
suppliers to become Kidney Contracting Entities (KCEs). KCEs will receive adjusted capitated payments
for managing beneficiaries with CKD Stages 4 and 5, ESRD, and kidney transplants. The KCE will
select a total cost of care accountability framework, and its payments under the Model will be adjusted
based on its performance on quality measures. KCEs participating in the CKCC Options select one of
following three options: the Graduated Option, the Professional Option, and the Global Option. The
CKCC Options are currently Advanced APMs for PY2022, with the exception of the one-sided Level 1 of
the Graduated Option. Guidance on Advanced APM status for PY2023 is forthcoming. KCEs affiliated
with Large Dialysis Organizations (LDOs) may not participate in the Graduated Option. For the purposes
of the KCC Model, CMS defines an LDO as an entity that as of the effective date of the applicable
Participation Agreement, owns in whole, or in part, more than 500 dialysis facilities. All of the CKCC
Options, including the one-sided Level 1 of the Graduated Option, are MIPS APMs beginning in 2022.
KCEs will also have access to Benefit Enhancements and Beneficiary Engagement Incentives to
strengthen care coordination for aligned beneficiaries and alternative payment mechanisms to manage
cash flow.
The terms of the KCF and CKCC Options of the Model will be set forth in separate participation
agreements
C. Timeline
The KCC Model performance period began on January 1, 2022, and will continue through December 31,
202
6. CMS solicited applications for the first cohort of KCC Model participants in October 2019. The
first cohort of KCC Model participants began their participation in the Model performance period on
January 1, 2022. CMS is now soliciting applications for a second cohort of KCC Model participants.
CMS invites interested applicants to submit their applications to CMS by March 25, 2022. If selected to
pa
rticipate in the Model, the second cohort of KCC Model participants would begin Model participation
on January 1, 2023, after executing performance period participation agreements that will set forth the
terms of the KCF Option or the CKCC Options of the KCC Model, as applicable. The performance period
participation agreements for these KCC Model participants will have a term of four Performance Years
(PYs) (2023, 2024, 2025, and 2026). CMS does not plan to conduct any further solicitations for KCC
Model participants.

Updated 03/06/2022 6
Table 1 provides a high-level timeline of key milestones in the Model.
Table 1. Milestone Timeline
TARGET DATE MILESTONE
July 10, 2019 Advancing American Kidney Health initiative announced, including the
Kidney Care Choices Model
October 2019 Request for Applications for Cohort 1 of the KCC Model released
January 1, 2022 KCC Model PY2022 begins
February 28, 2022 Request for Applications for Cohort 2 of the KCC Model for PY2023
Released
March 25, 2022 Application responses to RFA due from potential KCF Practices and
KCEs
May 13, 2022 CMS releases decisions on Cohort 2 applications
June 1, 2022 Accepted applicants notify CMMI of intent to participate in the KCC
Model
June 29, 2022 Final deadline to add participants to KCF Nephrology Professional List
or KCE Participant or Preferred Provider Lists
No later than November 30,
2022
Selected applicants execute Performance Year Participation Agreements
2023 KCC Model PY2023 begins
2024 KCC Model PY2024 begins
2025 KCC Model PY2025 begins
2026 KCC Model PY2026 begins
December 31, 2026 End of KCC Model performance period
Updated 03/06/2022 7
II. General Provisions
A. Monitoring and Oversight
CMS will conduct monitoring and oversight activities to evaluate participants’ compliance with the terms
of
the participation agreement and to identify fraudulent behavior or program integrity risks, such as
inappropriate reductions in care, efforts to manipulate risk scores or aligned populations, overutilization,
and cost-shifting to other payers or populations. Each Model participant will be required to cooperate
with, and require its downstream providers and suppliers to cooperate with, CMS monitoring and
oversight activities.
CMS’s monitoring and oversight activities may include, but are not limited to, the following:
•
Analysis of specific financial and performance data reported by the KCF Practice or KCE;
•
Analysis of beneficiary and provider/supplier complaints including, but not limited to, those
submitted through 1-800-MEDICARE, surveys, and internal processes established and supported
by the KCF Practice or KCE for managing such complaints; and
•
Audits, including claims data mining, medical chart review, beneficiary survey data, coding
audits, and on-site compliance reviews.
•
Audit of samples of medical charts;
•
Monitoring of beneficiary complaints and surveys;
•
Interviews with beneficiaries, providers and suppliers
•
Analysis of claims and quality data;
•
Vetting of model participants and their providers/suppliers on the basis of program integrity
issues; and
•
Monitoring for appropriate use of Benefit Enhancements.
B. Re
medial Action and Termination
CMS may take remedial action against a participant for a variety of reasons, including but not limited to
the following:
• The participating entity (KCF Practice or KCE) or its participants’ noncompliance with any term
of the participation agreement;
•
Failure to submit or implement a corrective action plan;
•
Participating entity or its participants’ engage in actions that threaten the health or safety of a
patient or patient quality of care;
•
Submission of false data or other information in connection with the Model; and
•
Participating entity or participants’ past or present program integrity issues.
When grounds for remedial action exist, CMS may employ a variety of actions based on the nature and
severity of the issue identified, including, but not limited to:
•
Notify the participating entity of the grounds for remedial action;
•
Request additional information
•
Request a Corrective Action Plan (CAP);
•
Remove, or require the KCF Practice or KCE to remove, downstream provider or supplier;
•
Discontinue data sharing and reports;
Updated 03/06/2022 8
• Suspend or terminate the use of one or more Benefit Enhancements or Beneficiary Engagement
Incentives; and
• Recalculate payment amounts and recoup amounts owed.
In addition, nothing in the Participation Agreement would prevent CMS from exercising its authority to
make referrals to the Secretary for consideration under Section 1881(c)(3) of the Act or referrals to law
enforcement.
CMS may immediately or with advance notice terminate a participation agreement if grounds for
rem
edial action exist, if CMS determines that it no longer has the funds to support the Model, or as
otherwise specified in the relevant participation agreement. We also note that CMS is required to modify
or terminate the Model unless it is determined that the Model is expected to: (1) improve the quality of
care without increasing spending; (2) reduce spending without reducing the quality of care; or (3)
improve the quality of care and reduce spending.
CMS may add additional program integrity safeguards or other terms to the Model based on experience
during the Model performance period.
C. Screening
CMS may reject an application or terminate a Participation Agreement on the basis of the results of a
Pr
ogram Integrity (PI) screening regarding the applicant, its affiliates, and any other relevant individuals
or entities. The PI screening may include, without limitation, the following:
• Confirmation of current Medicare enrollment status and history of adverse enrollment actions;
• Identification of delinquent debt;
• Review of performance in, and compliance with the terms of, other CMS models, demonstrations,
pr
ograms, and initiatives;
• Review of compliance with Medicare program requirements;
• Review of billing history and any administrative audits, investigations, or other activities
conduc
ted regarding suspicious billing or other potential program fraud and abuse;
• Review of any civil or criminal actions related to participation in a federal health care program;
and
• Confirmation that the Applicant ACO has not engaged in anti-competitive practices.
D. Evaluation
In accordance with Section 1115A(b)(4) of the Act, an evaluation of the KCC Model will be conducted to
det
ermine whether the Model results in improved quality of care and reduced Medicare spending.
Pursuant to section 42 CFR 403.1110(b), participants must cooperate with CMS’s evaluation contractor
and provide data as requested. CMS’s model evaluation contractor will perform rigorous quantitative and
qualitative analysis to assess the impact of the KCC Model. A combination of administrative, claims, and
registry data, beneficiary surveys and focus groups, and interviews with providers and suppliers will
inform the research questions for the Model. The CMS Office of the Actuary (OACT) and the HHS
Secretary will take into account this evaluation in determining whether the criteria have been met to
expand the scope and duration of the Model through rulemaking in the future. Specifically, in accordance
with section 1115A(c) of the Act, the Secretary may expand the Model if: (1) the Secretary determines
that expansion is expected to either reduce Medicare expenditures without reducing care quality or
improve the quality of care without increasing spending; (2) the chief actuary of CMS certifies that such
expansion would reduce (or would not result in any increase in) net Medicare program expenditures; and

Updated 03/06/2022 9
(3) the Secretary determines that such expansion would not deny or limit the coverage or provision of
b
enefits for applicable individuals.
E. Learning and Diffusion Resources
The Innovation Center is working with national healthcare experts to develop resources and activities to
s
upport participants in the KCC Model. The Innovation Center will support KCEs and KCF Practices in
accelerating their progress towards improving care for CKD Stages 4 and 5, ESRD, and transplant
beneficiaries and achieving financial benchmarks by providing them with opportunities to learn how care
delivery organizations can achieve performance improvements quickly and effectively, and opportunities
to share their experiences with one another and with participants in other Innovation Center
initiatives. The Innovation Center will test various approaches to group learning and exchange, helping
Model participants effectively share their experiences, track their progress, and rapidly adopt new ways of
achieving improvements in quality, efficiency, and population health.
All selected KCF Practices and KCEs will be expected to participate in periodic conference calls and
m
eetings, and to actively share resources, tools, and ideas with each other.
The aim of the learning and diffusion strategy will be to establish an infrastructure to support shared
l
earning, improvement efforts, and innovations in care delivery among KCC participants by addressing
the following areas:
1. Assisting participants in applying improvement methods, with rigorous measurement that guides
r
apid cycle, iterative testing to achieve results.
2. Development of affinity groups among the participants for focused collaboration and sharing on
co
mmon strategies and topics, leveraging resources, and accelerating learning.
3. Disseminating good ideas and effective practices for both KCEs and KCF Practices as they
em
erge, thus allowing all participants to benefit from the work of their peers. These efforts will
result in structured case studies, useful and practical metrics, and prepared packages of change
concepts, and best practices.
Figure 1. Learning System
Participants will be expected to actively participate in and shape Learning System activities as part of
their participation in the KCC Model. The Learning System will facilitate peer learning and information
sharing around how best to achieve quick and effective performance improvement. The Learning System
will allow participants to glean promising practices from their peers and to further develop their own
Updated 03/06/2022 10
programs during their participation in the Model performance period. The Innovation Center will
unde
rtake various approaches to group learning and exchange, helping participants to effectively share
their experiences, track their progress, and rapidly adopt new ways of achieving improvements in care
quality, as well as reductions in Medicare FFS expenditures. Potential Learning System activities include
virtual learning sessions, topic-specific webinars, group-specific virtual collaboration, access to data
dashboards, a learning collaborative virtual platform, case studies/toolkits, and an annual face to face
collaborative.
As part of these Learning System activities, participants may also be expected to:
1. Participate in targeted learning on Driver Diagrams, develop and submit to CMS, or its
c
ontractors, an individualized participant Driver Diagram (after submission to CMS, the Driver
Diagram should be maintained and updated by the participant throughout the life of the Model as
a framework to guide and align the intervention design and implementation activities and shared
with CMS upon request).
2. Answer surveys, participate in interviews or engage in other activities to assist CMS and its
c
ontractors in identifying their learning needs.
3. Participate in the identification and dissemination of practices that are showing positive outcomes
by
sharing lessons learned with other Model participants (e.g. presenting on webinars).
4. Participate in at least one virtual KCF or CCKC Model learning activity every quarter during the
m
odel period.
5. Share with CMS, its contractors, and if relevant, other model participants, information on state
a
nd federal programs that complement the KCF and CCKC model interventions in the
communities they serve.
6. De
velop, track, and report to CMS on quality improvement efforts, activities, and program
measures, at regular intervals.
7. Par
ticipate in in-person events during some years of the model (TBD). These in-person events
will be held in the Baltimore/District of Columbia area and will be geared towards participant
learning, collaboration, and dissemination of promising practices for KCEs and KCF Practices,
and another participant needs.
F. CEHRT Requirements
KCF Practices and their KCF Nephrology Professionals and KCEs and their KCE Participants must use
C
ertified Electronic Health Record Technology (CEHRT), as such term is defined under 42 CFR §
414.1305, in a manner sufficient to meet the applicable requirements of 42 CFR § 414.1415(a)(1)(i),
including any amendments.
G. Waivers
The authority for the KCC Model is section 1115A of the Social Security Act (SSA). Under section
1
115A(d)(1) of the SSA, the Secretary of Health and Human Services may waive such requirements of
Titles XI and XVIII and of sections 1902(a)(1), 1902(a)(13), and 1903(m)(2)(A)(iii) as may be necessary
solely for purposes of carrying out section 1115A with respect to testing models described in section
1115A(b). CMS has waived certain Medicare payment requirements as necessary solely for purposes of
testing the KCF and CKCC Options. Certain payment rule waivers, referred to as “Benefit
Enhancements”, are detailed in Table 8 (KCF Option) and Table 18 (CKCC Option).
For the CKCC Option, and consistent with the authority under section 1115A(d)(1), the Secretary issued a
wai
ver of 1877(a) of the Act (relating to the Federal physician self-referral law) and sections 1128B(b)(1)
Updated 03/06/2022 11
and (2) of the Act (relating to the Federal anti-kickback statute) with respect to any startup arrangement
b
etween a KCE that has entered into an Implementation Period Participation Agreement and one or more
KCE Participants or Preferred Providers or both (as such terms were defined in the Participation
Agreements for the Implementation Period of the Model), provided that the conditions of the waiver are
satisfied. Because there is no Implementation Period for new applicants, this waiver is not available for
the second cohort of the CKCC Option.
For the CKCC Option, the anti-kickback statute safe harbor for CMS-sponsored model arrangements (42
C
FR § 1001.952(ii)(1)) is available to protect certain KCE financial arrangements between or among the
KCE, one or more KCE Participants, one or more Preferred Providers or a combination thereof, provided
that such arrangements comply with the applicable requirements set forth in the Performance Period
Participation Agreement for the CKCC Option. In addition, the anti-kickback statute safe harbor for
CMS-sponsored model patient incentives (42 CFR § 1001.952(ii)(2)) is available to protect the following
patient incentives in the CKCC Option, provided that they are furnished in a manner that complies with
the terms of the safe harbor and the relevant requirements set forth in the Performance Period
Participation Agreement: (i) certain in-kind incentives furnished by a KCE, KCE Participant, or Preferred
Provider; (ii) certain cost sharing support for Part B services provided to certain KCE Beneficiaries by a
KCE, KCE Participant, or Preferred Provider; and (iii) certain chronic disease management rewards
furnished by a KCE to certain KCE Beneficiaries.
For the KCF Option, the anti-kickback statute safe harbor for CMS-sponsored model patient incentives
(
42 CFR § 1001.952(ii)(2)) is available to protect the following patient incentives, provided that such
remuneration is furnished in a manner that complies with the terms of the safe harbor and the relevant
requirements set forth in the Performance Period Participation Agreement for the KCF Option: (i) certain
in-kind items and services furnished by a KCF Practice or a KCF Nephrology Professional to a KCF
Beneficiary; (ii) certain cost sharing support for face-to-face visits with KCF Beneficiaries; and (iii)
certain chronic disease management rewards furnished by the KCF Practice to certain KCF Beneficiaries.
Notwithstanding any other provision of this RFA, all individuals and entities must comply with all
ap
plicable laws and regulations, except as explicitly provided in any separately documented waiver issued
pursuant to Section 1115A(d)(1)specifically for the KCC Model. We note that the applicable law does not
include the anti-kickback statute safe harbor for CMS-sponsored models safe harbor, except to the extent
that CMS has made a determination that such safe harbor is applicable to the KCC Model.
Execution of a Participation Agreement to participate in the KCC Model is not intended and shall not be
construed as a waiver by the United States Department of Justice, the Internal Revenue Service, the
Federal Trade Commission, United States Department of Health and Human Services (HHS) Office of
Inspector General, or CMS of any right to institute any proceeding or action against a KCF Practice,
KCE, or any of its affiliated entities for violations of any statutes, rules or regulations administered by the
government, or to prevent or limit the rights of the government to obtain relief under any other federal
statutes or regulations, or on account of any violation of the respective Participation Agreement or any
other provision of law. The Participation Agreements for the KCC Model shall not be construed to bind
any government agency except CMS, and they bind CMS only to the extent provided therein.
H. Amendment
CMS may modify the terms of the KCC Model in response to stakeholder input, to reflect the agency’s
ex
perience with the Model, or as may be required under section 1115A of the Act or any other applicable
provision of law. The terms of the KCC Model as set forth in this Request for Applications may differ
from the terms of the Model as set forth in the Participation Agreement between CMS and the KCF
Updated 03/06/2022 12
Practice or between CMS and the KCE. Unless otherwise specified in the applicable Participation
Agreement, the terms of that Participation Agreement, as amended from time to time, shall constitute the
terms of the KCC Model’s performance period.
Updated 03/06/2022 13
III. CMS Kidney Care First (KCF) Option
Under the KCF Option, participating nephrology practices (referred to as KCF Practices) and their
pa
rticipating nephrologists and non-physician clinicians who specialize in nephrology (referred to
collectively as “nephrology professionals”) will receive capitated payments for managing beneficiaries
with CKD Stages 4 and 5 and ESRD who are aligned to the KCF Practice. KCF Practices will also
receive performance-based payment adjustments to those capitated payments, based on how well the KCF
Practice performs on quality and utilization measures.
A. Leg
al Entity
The applicant must be a Medicare-enrolled entity (i.e., physician practice or professional corporation) that
bills Medicare for physician services rendered by one or more nephrologists by the start of the
performance period. Each applicant must be recognized and authorized to conduct business under
applicable state law.
B. Governance Structure Requirements
A KCF Practice can be governed through the existing organizational structure of the practice, as long as
t
he existing structure is a single legal entity authorized to undertake the activities required under the
applicable KCF Participation Agreement and meets the requirements stated in this RFA. A separate
governing body or governance structure is not required for participation in the KCF Option.
C. Applicant Eligibility
Nephrology practices are the only entities eligible to apply for the KCF Option. Nephology practices that
p
articipated in a KCE as a KCE Participant in 2022 cannot apply to be a KCF Practice in 2023 unless
their KCE is terminating effective December 31, 2022 or earlier. KCF Practices include nephrology
professionals, which refers collectively to nephrologists and non-physician clinicians – such as Nurse
Practitioners and Physician Assistants – who specialize in nephrology or primarily provide nephrology
services. Dialysis facilities and other non-nephrologist supplier and provider types cannot to participate
in the KCF Option.
Nephrology professionals in KCF Practices must meet all of the following requirements for the duration
of their participation in the Model:
• Must be enrolled in Medicare.
•
Must have an NPI associated with a primary taxonomy/specialty in kidney health and the
treatment of kidney diseases or self-identify as nephrology professionals for the purposes of this
Model.
CMS will verify this information against PECOS, or through other means, including claims data.
The following is a list of Model policies and requirements that practices must meet in order to participate
i
n the KCF Option and for the duration of their participation:
• A practice is defined as all individual National Provider Identifiers (NPIs) billing under a single
TIN, which can include practices with a main billing address, but multiple physical locations;
•
The practices will need to demonstrate that at least 50% of the practice’s total Medicare payments
from the previous 12 months comes from nephrology services furnished by nephrologists to
Updated 03/06/2022 14
beneficiaries with CKD Stages 4 or 5, beneficiaries with ESRD, or beneficiaries with a
f
unctioning kidney transplant. CMS will calculate this threshold based on claims data.
•
CMS encourages participation by practices of all size, including multispecialty practices;
•
At least 80% of all nephrologists that have reassigned their rights to receive Medicare payment to
the practice and provide dialysis management services included in the Monthly Capitation
Payment (MCP) in an outpatient setting must participate in the Model;
•
The practice must maintain a minimum of 350 CKD Stages 4 and 5 and 200 ESRD aligned
Medicare beneficiaries over the course of the Model. There is no requirement that the KCF
Practice furnish services to a minimum number of transplant beneficiaries;
•
The practice and its nephrology professionals must use the CEHRT as such term is defined under
42 CFR § 414.1305;
•
The practice must demonstrate the ability to assume financial risk and make any required
repayments to the Medicare program; and
•
KCF Practices will not be restricted to a specific market area. However, in order to conduct
alignment, CMS will need to determine a KCF Practice’s Service Area. A KCF Practice’s
Service Area is defined as the Medicare Core Based Statistical Areas (CBSAs) and rural counties
in which the KCF Practice’s participating nephrologists and nephrology professionals provide
nephrology services to CKD and ESRD beneficiaries under the practice Tax Identification
Number (TIN).
Nephrology professionals participating in the KCF Option may not participate contemporaneously in a
KC
E or in more than one KCF Practice because CMS uses participating nephrology professionals to align
beneficiaries. A nephrology practice may apply to participate in both the KCF Option and one of the
CKCC Options for 2023. However, if selected for participation in both the KCF Option and one of the
CKCC Options, the practice will have to decide whether to participate in either the KCF Option or one of
the CKCC Options by June 1, 2022.
KCF Nephrology professionals and KCF Practices (collectively known as KCF Participants) and
beneficiaries aligned to a practice participating in the KCF Option, will be able to overlap with an ACO
participating in the Medicare Shared Savings Program. However, KCF Practices participating in both the
KCF Option and a Shared Savings Program ACO are required to have a written statement signed by a
representative of the leadership of the ACO acknowledging that the KCF Practice’s simultaneous
participation in the KCF Option may impact the ACO’s total expenditure calculations under the Shared
Savings Program. KCF Participants will not be allowed to simultaneously participate in other ACO
initiatives or models.
KCF Practices and their nephrology professionals are not permitted to simultaneously participate in the
I
ndependence at Home Demonstration (IAH), Primary Care First (PCF) Model, ACO Realizing Equity,
Access, and Community Health (ACO REACH) Model (formerly known as Global Direct and
Professional Contracting (GPDC) Model), or Vermont All-Payer ACO Model. For the Maryland Total
Cost of Care Model (MD TCOC), KCF Participants may simultaneously participate in the Maryland
Hospital Payment Program (HPP) and Care Redesign Program (CRP) options, but not the Maryland
Primary Care Program. CMS will use the KCF Practice’s TIN to check whether the KCF Practice is also
participating in the Shared Savings Program, while all other initiatives are checked using both the TIN
and NPIs of the KCF Practice’s nephrology professionals.
Updated 03/06/2022 15
D. Beneficiary Alignment
The patient population for the KCF Option is Medicare beneficiaries with CKD Stages 4 and 5, ESRD,
and kidney transplant recipients. It is important to note that the alignment of beneficiaries to KCF
Practices is for Model test purposes only. Beneficiary alignment is relevant for each KCF Practice’s
utilization calculations, quality performance measurement, and CMS monitoring of claims data.
Beneficiary alignment to a KCF Practice does not inhibit beneficiaries’ freedom to choose to receive care
from other Medicare providers and suppliers within Medicare Fee-For-Service (FFS). Similar to other
CMS programs and models, CMS will not allow beneficiaries that have been aligned to a KCF Practice to
opt out of alignment, but beneficiaries may opt out of CMS sharing certain information about them with
the KCF Practice. CMS will prospectively align eligible beneficiaries to KCF Practices through a claims-
based alignment process. Aligned beneficiaries may obtain nephrology services from nephrology
professionals not participating in a KCF Practice, as well as practices that are not participating in the KCF
Option, which could cause them to be de-aligned from a KCF Practice retroactively during alignment
reconciliation.
1. Beneficiary Eligibility
To be eligible for alignment and to remain aligned to a KCF Practice for a Performance Year,
ben
eficiaries must meet all of the following criteria, except where otherwise noted:
• Have either CKD Stage 4 or 5, or ESRD, or be a transplant recipient with a functioning kidney
who
was previously aligned to the KCF Practice while the beneficiary had CKD Stage 4 or 5 or
ESRD;
• Be enrolled in Medicare Parts A and B;
• Not be enrolled in a Medicare Advantage plan, cost plan, or other non-Medicare Advantage
Medicare managed care plan;
• Reside in the United States;
• Received greater than 50% of their nephrology services and MCP claims within the KCF
Pr
actice’s Service Area during the Alignment Lookback Period;
• Be 18 years of age or older;
• Be alive;
• Not have already been aligned to another participant in a Medicare program/demonstration/model
i
nvolving shared savings or another participant in a Medicare program/demonstration/model
where overlap is not allowed as of the date of alignment for the KCF Option.
• Not have Medicare as a secondary payer;
• Not had a kidney transplant in the last 13 months (initial alignment only);
• Not in an active election period of hospice care at the time CMS conducts alignment; and
• Not received hospice care at any time during the last three months of the 12-month period that
ends
3 months prior to the start of the quarter for which CMS is conducting alignment to the
Practice (“Alignment Lookback Period”) or during the period between the end of the Alignment
Lookback Period and the alignment run date (initial alignment only).
If a beneficiary meets the alignment eligibility criteria described above, the beneficiary will be initially
ali
gned to the KCF Practice if the beneficiary also meets the applicable criteria described in Table 2
below.
After each Performance Year, KCF Practices must have a minimum of 350 aligned Medicare
ben
eficiaries with CKD Stages 4 and 5 and 200 aligned Medicare ESRD beneficiaries or else they will

Updated 03/06/2022 16
have to aggregate their performance. CMS does not require the KCF Practice to have a minimum number
of
aligned transplant beneficiaries. Once an aligned beneficiary receives a kidney transplant, they do not
count towards a KCF Practice’s minimum required number of aligned CKD or ESRD beneficiaries.
However, if the beneficiary was aligned to a KCF Practice and had CKD Stages 4 or 5 or ESRD for a
period of time during the relevant Performance Year prior to receiving a kidney transplant, that period of
time may count towards the KCF Practice’s applicable alignment.
2. Alignment Process
Beneficiaries will be aligned to a KCF Practice based on services furnished by nephrology professionals
billing under the TIN of the KCF Practice. Aligned beneficiaries will be assigned a status, depending on
whether they have CKD Stages 4 and 5, ESRD, or are a transplant recipient who was previously aligned
to the KCF Practice while they had CKD Stages 4 and 5 or ESRD. This is different than the CEC Model,
where beneficiaries were aligned through the dialysis facility.
CMS believes that aligning beneficiaries to a KCF Practice through the nephrology professional has the
following advantages:
• Prioritizes the nephrologist relationship as the most important one for beneficiaries with CKD
Stages 4 or 5, ESRD, or a kidney transplant;
• Protects the continuity of care by aligning a beneficiary with the same nephrology professional(s)
who
furnished services to them in the past and may still be furnishing services to them at the time
of alignment; and
• Allows for beneficiaries who only dialyze at nursing facilities, instead of outpatient dialysis
fa
cilities, to be aligned to KCF Practices and included in the Model test, if they are seen by the
KCF Practice’s nephrology professionals.
Initial and Quarterly Alignment
CMS will initially align eligible beneficiaries to KCF Practices based on claims for nephrology or dialysis
services during a specified lookback period and the beneficiary’s kidney disease status (i.e. CKD Stages 4
or 5, ESRD, or kidney transplant recipient) at the time of alignment, as summarized in Table 2 below.
CMS will also retrospectively finalize beneficiary alignment as part of a reconciliation process after each
Performance Year, allowing for a minimum of three months claims run-out. CMS will identify the final
aligned beneficiary population for the KCF Practice. Beneficiaries will be de-aligned from a KCF
Practice’s list of aligned beneficiaries if they do not receive certain health services from a KCF Practice
nephrology professional during the Performance Year, or receive the majority of certain health services
outside of the KCF Practice’s Service Area.
KCF Practices will receive a list of initially aligned beneficiaries before the start of the performance
per
iod. KCF Practices will be accountable for the quality of care furnished to these beneficiaries during
the performance period. New beneficiaries who satisfy the alignment eligibility criteria will be added to
each KCF Practice’s alignment list on a quarterly basis. Once aligned, beneficiaries remain aligned to the
KCF Practice until they meet one of the criteria for de-alignment.

Updated 03/06/2022 17
Table 2. Some Alignment Criteria by Beneficiary Type
Beneficiaries with CKD Beneficiaries with ESRD Beneficiaries who
Receive Kidney
Transplants
Aligning
Participant
Nephrology professional Nephrology professional N/A – Must have been
previously aligned by
virtue of CKD or ESRD
Criteria for
Alignment
Diagnosis of CKD Stages
4 or 5; 2 or more
Nephrology Services
(Professional/Carrier
claims) within a 12-month
period with a KCF
Nephrology Professional;
50% or more of
Nephrology Services
within the KCF Practice
Service Area; no MCP
claims
Kidney disease status of
ESRD; 2 or more MCP
claims with a KCF
Nephrology Professional
within a 3-month period;
50% or more MCP claims
within the KCF Practice’s
Service Area;
Being previously aligned
to the KCF Practice as a
CKD or ESRD beneficiary
and receiving a kidney
transplant
Criteria for
De-alignment
Beneficiaries received the
majority of Nephrology
Services outside the KCF
Practice Service Area; or
did not receive any
Nephrology Services from
a KCF Nephrology
Professional during the
months of the performance
year in which they were an
eligible beneficiary.
Beneficiaries received the
majority of MCP claims
outside the KCF Practice
Service Area or did not
receive any MCP claims
with a KCF Nephrology
Professional during the
months of the Performance
Year in which they were
an eligible beneficiary, or
did not receive any
maintenance dialysis
treatments during the
Performance Year.
Kidney transplant failure
(the beneficiary may be
aligned as a CKD or
ESRD beneficiary post-
transplant failure if the
applicable requirements
for alignment are met); 3
years past their transplant
The alignment lookback period is the 12-month period that ends 3 months prior to the start of the quarter
for which CMS is conducting beneficiary alignment within which claims must occur in order to be
considered for the quarterly alignment process. For example, for PY2023 Quarter 1 (PY2023 Q1), the
lookback period is October 2021 to September 2022. CMS will run beneficiary alignment for PY2023 Q1
in October 2022. CMS will then send beneficiary alignment lists to KCF Practices in advance of the start
of the performance period (January 1, 2023).
Ineligibility and Dealignment
If an aligned beneficiary no longer meets certain eligibility criteria, they will remain aligned to the KCF
Pract
ice for the remainder of the Performance Year, but CMS will assign to them an eligibility status of
“ineligible.” Beneficiaries aligned to a KCF Practice during one Performance Year will remain aligned to
the KCF Practice in the next Performance Year, unless they are de-aligned during the annual alignment
reconciliation that occurs after the end of the Performance Year. Ineligible beneficiaries' expenditures are
not counted toward utilization performance calculations for months in which they are ineligible.
Ineligible beneficiaries may become eligible again in the future if CMS determines that they meet
alignment criteria.

Updated 03/06/2022 18
When an aligned CKD or ESRD beneficiary receives a kidney transplant, they will remain aligned to their
KCF Pr
actice for three years from the month of transplant. While the KCF Practice will be eligible to
receive Kidney Transplant Bonus payments, the beneficiary will no longer be included in the KCF
Practice’s quality and utilization performance calculations. If the transplant fails within three years, the
beneficiary will be de-aligned from the KCF Practice. It is possible for a beneficiary whose transplant has
failed to be realigned as a CKD or ESRD beneficiary to the original KCF Practice or to a different KCF
Practice if they meet eligibility requirements. It is also possible that an aligned beneficiary progresses
from CKD to ESRD during the Performance Year. CMS reviews and updates each aligned beneficiary’s
kidney disease status (e.g., CKD, ESRD, or transplant recipient) on a quarterly basis. CMS will also
determine each aligned beneficiary’s final kidney disease status for each month that the beneficiary was
aligned to the practice during a Performance Year after the end of the Performance Year.
De-alignment criteria, including de-alignment based on a beneficiary not receiving care from a KCF
Prac
tice nephrology professional during the Performance Year or receiving the majority of claims for
Nephrology Services or MCP claims outside the KCF Practice’s Service Area, are designed to ensure an
accurate measure of the cost and quality of the beneficiary care in the model test. The de-alignment
criteria are based on the care relationship between the KCF Practice and the aligned beneficiaries. While
there may be some incentive for a KCF Practice to refer aligned beneficiaries outside of the Service Area
in order to de-align them from the KCF Practice (and in doing so, take advantage of the de-alignment
criteria), experience in the CEC Model has shown that the market areas, as defined above, tend to be large
enough that seeking care outside of the market area truly represents a change in beneficiary residence
rather than strategic referrals. This approach balances predictability in beneficiary populations, accuracy
in alignment, and the unique way CKD and ESRD beneficiaries interact with the health care system.
Finalizing Alignment
Alignment will be retrospectively finalized as part of a reconciliation process after each Performance
Year. CMS will identify the final aligned population for the KCF Practice after the Performance Year
allowing for a minimum of three months claims run-out. In certain cases, a beneficiary may become de-
aligned from the KCF Practice alignment list for the entire Performance Year at reconciliation if they:
• Received the majority of their Nephrology Services or MCP claims outside of the KCF Practice’s
Service Area.
• Did not receive any Nephrology Services or MCP claims from a KCF Practice Nephrology
Prof
essional during the months of the Performance Year in which their eligibility status was
“eligible.”
As a result of the quarterly alignment review and/or the reconciliation process, an aligned beneficiary may
be rem
oved from a KCF Practice’s list of aligned beneficiaries for certain months (e.g., months following
a beneficiary’s death).
3. Beneficiary Minimums and Aggregation
During each Performance Year, KCF Practices must have a minimum of 350 aligned Medicare
benefi
ciaries with CKD Stages 4 or 5 and 200 aligned ESRD beneficiaries. If at any point a KCF Practice
drops below the minimum aligned beneficiary threshold, the KCF Practice may be required to submit a
Corrective Action Plan (CAP) explaining the steps it will take to meet the minimum threshold for CMS
review and approval. If, after the end of the Performance Year CMS determines that a KCF Practice did
not maintain these beneficiary minimums during the Performance Year, the KCF Practice will be
required to aggregate its performance with other KCF Practices for purposes of calculating performance

Updated 03/06/2022 19
on quality and utilization measures. If the minimum threshold remains unmet prior to the start of the next
Performance Year , CMS may pursue additional remedial actions including, but not limited to,
termination of the KCF Practice’s Participation Agreement. CMS does not require the KCF Practice to
have a minimum number of aligned transplant beneficiaries.
KCF Practices will have the opportunity to choose an aggregation partner for the purposes of meeting the
minimum number of aligned beneficiaries, subject to CMS approval. The aggregation partner or partners
must be chosen before the deadline specified in the Participation Agreement for the given Performance
Year. If an aggregation partner is not chosen, then CMS will assign an aggregation partner or partners.
A KCF Practice cannot aggregate with a KCE. If at the end of the Performance Year one aggregation
partner meets the minimum aligned beneficiary threshold and others does not, then the performance for
the practices in the aggregation group will still be aggregated. If all aggregation partners meet the
minimum aligned beneficiary threshold at the end of the Performance Year, then the KCF Practices in the
aggregation group will no longer be required to aggregate. There can be up to 5 aggregation partners in a
group in order to meet the minimum aligned beneficiary threshold.
4. Beneficiary Notifications and Marketing Materials
All KCF Practices will be required to share with aligned beneficiaries certain details about their alignment
to the KCF Practice and the practice’s participation in the Model. For KCF Practices’ ease, CMS will
provide templates that participants may use for aligned beneficiary notification purposes. If CMS
provides a template to be used for these notification requirements, such template will include all of the
required information described below and will indicate the required content that the KCF Practices may
not change as well as the places where KCF Practices can insert their own content. The KCF Practice and
its nephrology professionals must also comply with all applicable federal laws regarding interaction with
Medicare FFS beneficiaries.
Specifically, KCF Practices will be required to display materials in their office or facility locations
notifying beneficiaries that they are participating in the Model. KCF Practices are also required to
distribute a paper copy of the informational materials to each aligned beneficiary at the beneficiary’s first
office visit with KCF Practice nephrology professional after the nephrology professional receives notice
that the beneficiary is aligned to the KCF Practice.
The notification must include the following elements:
• A short description of the KCF Option and what that means for their care.
• An explanation that the beneficiary retains full Medicare FFS benefits and the freedom to choose
his or her providers and suppliers, including his or her nephrology professionals.
1
• Information on how to opt out of CMS sharing certain information about them with the KCF
Practice (described in more detail in the Data Sharing section, below).
• Contact information for the KCF Practice and 1-800-MEDICARE for questions and/or concerns
about beneficiary protections and the KCF Practice’s participation in the KCC Model.
KCF Practices and their nephrology professionals must provide any KCF marketing materials and
activities to CMS upon request. If CMS requests such materials and activities, CMS will review them to
ensure that the materials comply with the terms of the KCF Participation Agreement, including that they
1
The beneficiary maintains the right to see any Medicare participating healthcare provider at any time under the traditional
Medicare FFS benefit structure. Example language may read “You still have the right to visit any dialysis facility, doctor,
hospital, or healthcare provider that accepts Medicare” and/or “This is not a Medicare Advantage Plan or any kind of managed
care plan.”
Updated 03/06/2022 20
are not inaccurate or misleading, are not discriminatory or used in a manner that is discriminatory, and
make
clear that alignment to a KCF Practice does not remove or otherwise affect a beneficiary’s freedom
to choose a provider or supplier. Additional requirements concerning this review process will be
provided in the KCF Participation Agreement.
To ensure beneficiary freedom of choice, the KCF Practice shall not, and shall require its KCF
Nephr
ology professionals to not, commit any act or omission, nor adopt any policy that inhibits Medicare
beneficiaries from exercising their freedom to obtain health services from providers or suppliers who are
not KCF Participants.
5. Data Sharing
CMS will make historical and monthly claims data available to KCF Practices upon request, consistent
with
data sharing practices in shared savings models and programs, and consistent with all applicable
laws and regulations, including the Health Insurance Portability and Accountability Act (HIPAA) and the
Part 2 regulations governing the disclosure and use of certain substance use disorder patient records.
Upon a KCF Practice’s request, CMS will make available several types of Medicare data for the sole
pur
poses of developing and implementing activities related to care coordination and quality assessment
and improvement for beneficiaries aligned to the KCF Practice under the KCF Option. Such data may
include: (1) individually identifiable demographic and Medicare eligibility status information about
aligned beneficiaries and various summary reports with data relevant to the KCF Practice’s operations
and performance in the Model (such as data related to quality, expenditures, etc.); and (2) detailed claims
data files that will include individually identifiable claim and claim line data for services furnished by
Medicare-enrolled providers and suppliers to aligned beneficiaries. Historical data files for aligned
beneficiaries will be limited to three years of historical data, consistent with the approach under the CPC+
Model and shared savings models and programs.
The claims data provided to the KCF Practice will not include individually identifiable data for aligned
benef
iciaries who have opted out of data sharing. KCF Practices are required to provide aligned
beneficiaries who inquire about or wish to modify their preferences regarding claims data sharing with
information regarding how to modify their data sharing by calling 1-800-MEDICARE. The
communications that the KCF Practices share with such beneficiaries must note that, even if a beneficiary
has elected to decline claims data sharing, CMS may still engage in certain limited data sharing for care
coordination, quality improvement activities for aligned beneficiaries, and population-based activities
relating to improving health or reducing health care costs, as well as claims data sharing regarding claims
subject to the CKD QCP Fee Reduction.
E. Finance and Payment
CMS will make
the following payments to KCF Practices for aligned beneficiaries with CKD Stages 4
and 5, ESRD, and kidney transplants: :
• CKD Quarterly Capitation Payment (CKD QCP)
• Adjusted Monthly Capitation Payment (A
MCP)
• Kidney Transplant Bonus (KTB)

Updated 03/06/2022 21
2
The use of this code was discontinued in the CY 2020 PFS final rule. As this code is no longer used, it will not generate
claims. However, we are retaining the code for documentation purposes, as it was used in analyses supporting the development
of the CKD QCP methodology.
1. Payment Types
CKD Quarterly Capitated Payment
CMS will pay KCF Practices through an innovative per beneficiary CKD Quarterly Capitated Payment
(CKD QCP), which combines payment for several different outpatient Evaluation and Management
(E/M) services and other care management services listed below, referred to as Nephrology Services, into
a single capitated payment. The CKD QCP is intended to provide an upfront payment to facilitate
delivery of care for aligned beneficiaries with CKD Stages 4 or 5. The CKD QCP will replace Medicare
FFS payments for Nephrology Services furnished to aligned beneficiaries by nephrology professionals in
the KCF Practice.
KCF Practices will be required to have financial arrangements with their nephrology professionals to
reimburse these practitioners for services provided. These arrangements must be negotiated in good faith
and be consistent with fair market value. Nephrology professionals will still be required to submit
Medicare FFS claims as they would otherwise for services for which CMS pays the CKD QCP . CMS
will only pay the CKD QCP to the KCF Practice for Nephrology Services furnished to aligned
beneficiaries with CKD Stages 4 or 5. The CKD QCP is designed to allow flexibility in care delivery and
provide a more stable payment stream to deliver advanced care for aligned beneficiaries with CKD Stages
4 or 5. The prospective increase in cash-flow may result in increased beneficiary access to nephrologist
care for their CKD, improved efficiency and coordination in addressing health issues, and improved
patient experience. The Model will test whether upfront, predictable revenue will help nephrology
professionals or the KCF Practice to coordinate care for aligned beneficiaries with other specialists to
better address their renal needs.
Table 3. Nephrology Services Included in the CKD QCP
Service Type Codes
Office/Outpatient Visit E/M 99201-99205,
99211-99215,
Complex Chronic Care Coordination Services 99487
Home Care / Domiciliary Care E/M 99348-99349
Prolonged E/M 99354-99355
Transitional Care Management Services 99495-99496
Advance Care Planning 99497-99498
Welcome to Medicare and Annual Wellness Visits G0402, G0438,
G0439
Chronic Care Management Services 99490
Prolonged non-face-to-face E/M Services 99358
2
Assessment/care planning for patients requiring CCM services G0506
Online digital E/M for an est. patient, for up to 7 days 99421 – 99423
Phone E/M phys/qhp 99441 – 99443
Updated 03/06/2022 22
Nephrology professionals in KCF Practices will continue to receive normal fee-for-service payments for
services furnished to aligned beneficiaries that are not included in the CKD QCP, such as inpatient visits,
and services for beneficiaries with CKD Stages 4 and 5 who have received transplants. Nephrology
professionals in KCF Practices will also continue to receive normal fee-for-service payments, rather than
the CKD QCP, for services furnished to beneficiaries who are not aligned to the KCF Practice. Aligned
beneficiary cost sharing for the services included in the CKD QCP will be set at the cost-sharing amount
which a beneficiary would have paid for the particular Nephrology Service furnished to the beneficiary
during a particular encounter, rather than the amount the beneficiary would have had to pay based on the
CKD QCP amount. The CKD QCP amount will be approximately one third the KCF Practice’s
anticipated two- or three-monthly recent visit MCP rate from the most recent Physician Fee Schedule.
The CKD QCP payment amount will be the same amount for a CKD Stage 4 or CKD Stage 5 beneficiary.
These payments will not be risk adjusted, given very similar risk profiles in the CKD Stages 4 and 5
populations.
Because the CKD QCP is paid prospectively, KCF Practices may receive CKD QCPs for beneficiaries
who
are deemed eligible at the time of alignment but are subsequently found ineligible for some period of
time during the quarter. As a result, CMS will withhold a percentage of the CKD QCP amount paid each
quarter to account for these changes in alignment status and will calculate alignment-based adjustments
after the Performance Year to ensure CMS did not overestimate the withhold. The withhold and
adjustments ensure that the CKD QCP (and corresponding FFS claims for services included in the CKD
QCP) is paid accurately for services provided. For PY2023 CMS will withhold 20 percent of CKD QCP
amounts that would otherwise be paid to participants during the Performance Year. This percentage is
unlikely to change and CMS currently plans a 20% withhold for PY2023, but CMS may increase or
decrease the withhold percentage for entities participating in PY2023 and subsequent Performance Years
if indicated by the KCC’s Model’s prior financial data. We refer to this withhold as the CKD QCP
Alignment Withhold (note that this withhold is different from the CKD QCP reduction applied above for
cost-sharing). After the end of each Performance Year, CMS will reconcile the CKD QCP Alignment
Withhold against the value of the KCF Practice’s alignment adjustments. Based on this analysis of
changes in beneficiary alignment, CMS will pay to the KCF Practice any amount owed to the Practice,
but the KCF Practice will not be liable for payments to CMS even if the KCF Practice is deemed to owe
CMS.
CMS will adjust the CKD QCP to account for “leakage,” or the dollar value of FFS claims for
Ne
phrology Services furnished to aligned beneficiaries by nephrology professionals that are not in the
KCF Practice that receives the CKD QCP during a Performance Year. CMS will do so through a
prospective CKD QCP leakage withhold, which is 10% of the CKD QCP paid to a KCF Practice. This
adjustment incentivizes a sustained doctor-patient relationship; increases in services delivered by
nephrology professionals outside of the KCF Practice to aligned beneficiaries will lead to a reduction in
the CKD QCP paid to the KCF Practice. CMS will determine leakage for each KCF Practice, and after the
Performance Year, CMS will reconcile the 10% CKD QCP leakage withhold to the actual amount of the
leakage. Based on this analysis, CMS will either pay the KCF Practice any amount of the leakage
withheld in excess of actual leakage during the Performance Year, or recoup from the KCF Practice any
amount that the KCF Practice owes to CMS because the actual leakage exceeded the CKD QCP leakage
withhold. Consistent with PCF, to support continuous care, CMS may also share data with participants on
Nephrology Services delivered outside of the KCF Practice to the KCF Practice’s aligned beneficiaries.

Updated 03/06/2022 23
Adjusted Monthly Capitation Payment (AMCP)
Currently, Medicare pays physicians and other practitioners who manage dialysis care for beneficiaries
receiving dialysis through the MCP. The per-patient-per-month MCP is for all outpatient visit services
related to the dialysis patient’s ESRD. The amount of the MCP varies based on several criteria:
• The location where the beneficiary dialyzes (at home or in center).
• The number of face-to-face visits with the beneficiary for beneficiaries who dialyze in center (one
monthly visit, two- or three-monthly visits, or four or more monthly visits).
• The age of the beneficiary.
Under the KCF Option, CMS will modify payments made to KCF Practices under the current MCP
structure. KCF Practice nephrologists and nephrology professionals will continue to bill the MCP as they
ordinarily would and will receive the MCP FFS amount from CMS that they would have received had
they not been in the Model.
However, the current payment structure of the MCP can create a bias towards in-center hemodialysis
because the highest MCPs are available for beneficiaries who dialyze in-center and receive four in-person
visits a month. According to a 2015 Government Accountability Office (GAO) report, equalizing
nephrologist payments for home and in-center dialysis removes the financial disincentive for prescribing
home dialysis and supports beneficiaries dialyzing at home.
The AMCP addresses this disincentive for prescribing home dialysis through the Home Dialysis True-Up,
which will standardize MCP reimbursement amounts for nephrology services regardless of where a
beneficiary dialyzes. The national average MCP for a nephrologist who visits a patient in-center 4 or
more times per month is $221 PBPM. The majority of MCP claims (over 70%) are billed at this 4+
monthly visit level. The national average MCP for a nephrologist who delivers care to a patient who
dialyzes at home is approximately $185 PBPM. The AMCP standardizes the MCP for home dialysis and
in-center dialysis patients by paying KCF Practices an additional $35 per MCP home dialysis claim for
services delivered to aligned ESRD beneficiaries. CMS will make this payment to KCF Practices at the
end of the Performance Year.
Therefore, the AMCP consists of the MCP, which is paid to each nephrology professional at current FFS
rates, plus the Home Dialysis True-Up, which is paid to the KCF Practice after financial reconciliation
after the end a given Performance Year. As a result, the AMCP reduces the variance in reimbursement
for ESRD dialysis services delivered to aligned beneficiaries who dialyze in center compared to at home.
Unlike the CKD QCP, which is paid to the KCF Practice on a prospective basis, CMS will pay the KCF
Practice the Home Dialysis True-Up component of the AMCP in a lump sum after the end of the
Performance Year.
Kidney Transplant Bonus (KTB)
KCF Practices are eligible for a Kidney Transplant Bonus (KTB) payment for every kidney transplant
received by an aligned beneficiary with CKD or ESRD during the Model performance period, regardless
of whether it is a living or deceased donor transplant.
3
The KTB will create a direct incentive for model
participants to support beneficiaries through the transplant process, including continued care management
of patients to support graft success.
CMS recognizes the lack of supply of available kidneys and that nephrologists do not control access to
the transplant wait list. However, CMS believes that this payment could better incentivize providers and
3
KCEs and KCF Practices would also receive the KTB payment when an aligned beneficiary receives any future FDA-approved
products that replace physiological kidney function.

Updated 03/06/2022 24
suppliers to move beneficiaries onto the waitlist, assist beneficiaries with understanding and progressing
through the living donation process, and support beneficiaries after they receive a transplant in
maintaining the health of the transplanted organ.
As stated, the purpose of the KTB is to incentivize KCF Practices to support beneficiaries during and after
the transplant process through care coordination and other services – including patient engagement and
support – that are necessary to maximize the likelihood of long-term success for an organ transplant.
CMS does not intend that the KTB be used for, or imply that model participants are permitted to, exert
inappropriate influence over the transplant process, or that model participants can acquire, receive, or
otherwise transfer organs in exchange for valuable consideration. The exchange or transfer of valuable
consideration for a human organ for transplantation is in violation of section 301 of the National Organ
Transplant Act of 1984 (NOTA), as amended. Certain payments, including “reasonable payments
associated with the removal, transportation, implantation, processing, preservation, quality control, and
storage of a human organ,” are not valuable consideration for purposes of this criminal prohibition.
Inappropriate or illegal use of the KTB, in violation of NOTA or any other laws or regulations, would
result in removal from the Model and referral to the appropriate law enforcement organization.
The KTB is up to $15,000 per successful transplant, paid in installments to the KCF Practice at set
intervals following the transplant. In particular, the KTB will be disbursed to the KCF Practice in three
installments as follows: $2,500 one year after transplant, $5,000 two years after the transplant, and $7,500
three years after the transplant. In order to receive KTB installment payments, three criteria must be met
at the time of disbursement, as follows:
• The beneficiary must remain alive.
• The beneficiary’s kidney transplant has not failed (e.g., the beneficiary must not have returned to
maintenance dialysis).
• The KCF Practice must be participating in the Model.
The KTB installment schedule and amounts differ depending on when the beneficiary receives their
transplant. To ensure that CMS makes all KTB payments before the final settlement for the final
Performance Year is completed, CMS will alter both the amount and schedule of KTB installments for
transplants made in PY2025 and PY2026. CMS will increase the proportion of the KTB paid to
participants in CY2027 to ensure that no KTB payments are made to KCF Practices after CY 2027.
Table 4. Schedule of KTB Installments
Installment
Transplants
PY2022 – PY2024
Transplants PY2025 Transplants PY2026
Amount per
Transplant
Date of
Payment*
Amount per
Transplant
Date of
Payment*
Amount per
Transplant
Date of
Payment*
1
st
Installment $2,500 1 year after
transplant
$2,500 1 year after
transplant
$2,500 1 year after
transplant
2
nd
Installment
$5,000 2 years after
transplant
$5,000 2 years after
transplant
$2,500 1 year after
transplant
3
rd
Installment
$7,500 3 years after
transplant
$3,750 2 years after
transplant
$3,750 1 year after
transplant
Maximum
Total KTB
$15,000 $11,250 $8,750
*Provided transplant remains successful
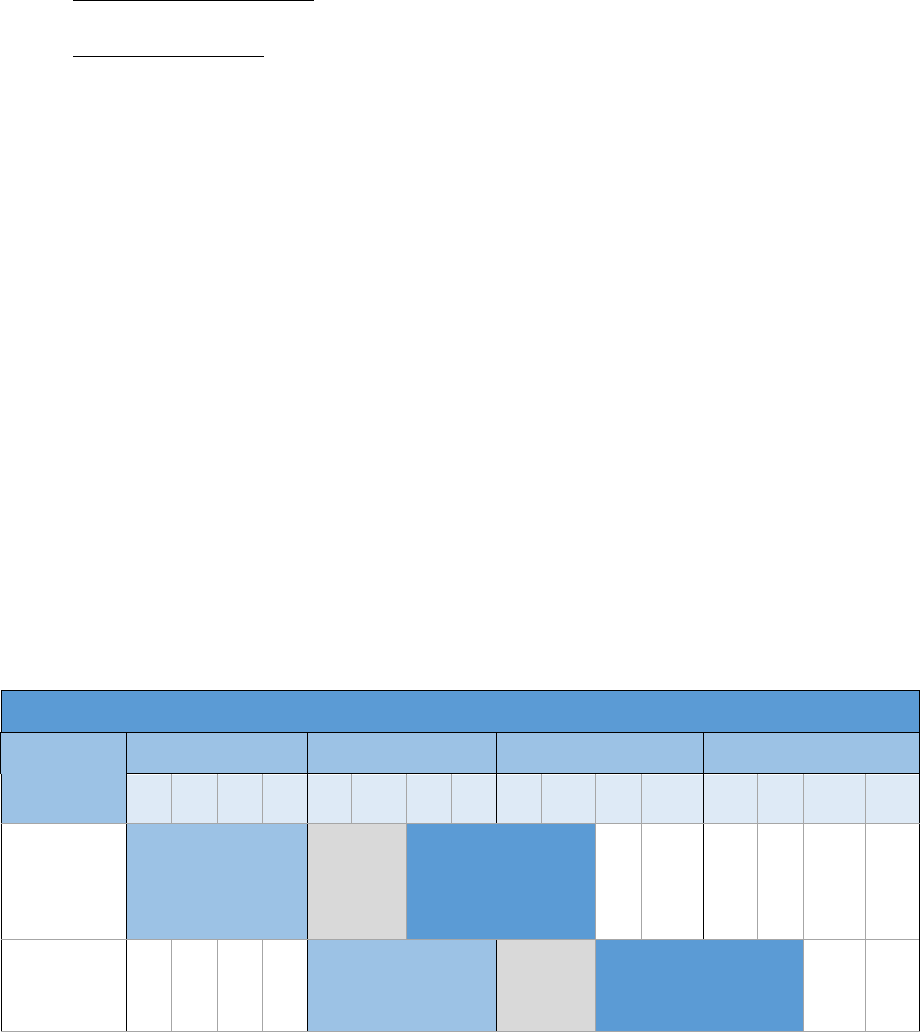
Updated 03/06/2022 25
2. Performance-Based Adjustment (PBA)
In addition to the CKD QCP and AMCP, the KCF Option will include a Performance-Based Adjustment
(P
BA), which could increase the amount of the CKD QCP and the MCP component of the AMCP for a
KCF Practice by up to 20 percent, or reduce that amount by as much as 20 percent.
Two distinct sets of performance measures will be used in calculating the PBA, which are described in
d
etail under Quality Strategy:
•
Quality Gateway Measures – a set of quality measures, with performance thresholds, designated
to reflect appropriate clinical care and patient experience for the affected population.
•
Utilization Measures - aimed at incentivizing efficient and appropriate provision of
health care services for the patient population.
There are two components of the PBA, each of which factors in the Quality Gateway and Utilization
m
easures:
•
Relative Performance (RP) Component – Each KCF Practice’s performance is assessed using a
set of the Quality Gateway measures. If the KCF Practice passes the Quality Gateway then CMS
will assess its performance on the Utilization measures relative to other KCF Practices.
Depending on this relative performance, the KCF Practice’s performance on the Utilization
measures may also be compared to that of all nephrology practices nationwide. As a distinct
component of the PBA, this financial adjustment based on relative performance could be either
positive or negative.
•
Continuous Improvement (CI) Component – For each KCF Practice that passes the Quality
Gateway threshold and achieves sufficient improvement on Utilization measures as compared to a
prior performance period, the PBA will include the CI component.
The PBA is the sum of the RP Component and the CI Component, which are assessed based on the KCF
Pr
actice’s performance during 12-month performance periods. After the end of the performance period,
CMS calculates the RP and CI Components, to determine the KCF Practice’s PBA. The PBA is applied to
the CKD QCP and the MCP component of the AMCP beginning in the third quarter that follows the end
of the performance period. Table 5, below, illustrates the relationship between PBA performance periods
and PBA payment adjustment periods.
Table 5. Timeline for Applying PBA to Model Payments
PBA Performance, Calculation, and Payment Adjustment Period
PBA
Payment
Applied
PY2023 PY2024 PY2025 PY2026
Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4
PY2024Q3 -
PY2025Q2
(for RP
only)
Measurement
Period
Calculate Adjustment Period
PY2025Q3 -
PY2026Q2
(RP and CI)
Measurement Period Calculate Adjustment Period

Updated 03/06/2022 26
PBA Performance, Calculation, and Payment Adjustment Period
PBA
Payment
Applied
PY2023 PY2024 PY2025 PY2026
Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4
PY2026Q3-
PY2026Q4
(RP and CI)
Measurement Period Calculate
Adjustment
Period
Measurement
Period
Data collection on measure performance concludes at end of PBA performance period
Calculation
Period
PBA amount calculated during PBA calculation period based on performance during PBA performance
period
Adjustment
Period
Performance-based adjustment applied to CKD QCP and AMCP during the PBA payment adjustment
period
For each KCF Practice, determination of the PBA will proceed according to a sequence of steps.
Relative Performance (RP) Component Calculation
Each KCF Practice will be placed into one of five performance levels (RP Level(s)), based on the
following determinations:
For each 12-month performance period, CMS will calculate the KCF Practice’s performance on the
Q
uality Gateway measures to determine if the KCF Practice achieved the Quality Gateway threshold, and
will calculate the KCF Practice’s performance on the Utilization measures.
• If the KCF Practice passes the Quality Gateway threshold, then it will be placed in RP Levels 1
through 5;
•
If the KCF Practice does not pass the Quality Gateway threshold, it will automatically be placed
in RP Level 5.
For KCF Practices that pass the Qu
ality Gateway threshold, the RP Level (1 through 5) and the
corresponding RP Component of the PBA will be determined by performance on the Utilization
measures:
• First, the KCF Practice’s performance on the Utilization measures will be compared to all other
KCF Practices.
•
If the KCF Practice’s performance on the Utilization measures is in the top 50 percent of all KCF
Practices, then it is placed within RP Levels 1 or 2, with the specific level depending on the KCF
Practice’s performance. The RP Component for these RP Levels will be positive, with the
magnitude of adjustment increasing with relative performance.
•
If the KCF Practice’s performance on the Utilization measures is in the bottom 50 percent of all
KCF Practices, then the RP Level will be determined by its performance in comparison to all
nephrology practices nationwide. If the KCF Practice’s performance on the Utilization measures
falls:
o
Within the top 50 percent of nephrology practices nationwide, then the KCF Practice will
be placed in RP Level 3, which results in a 0% RP Component of the PBA.

Updated 03/06/2022 27
o Between the 50
th
and 25
th
percentile of nephrology practices nationwide, then the KCF
Practice will be placed in RP Level 4, which results in a negative RP Component of the
PBA.
o In the bottom 25
percent, or below the 25
th
percentile, of nephrology practices
nationwide, then the KCF Practice will be placed in RP Level 5, which results in the
largest negative RP Component of the PBA.
Table 6 summarizes the RP Levels, along with the resulting either positive or negative RP adjustments.
Table 6. Magnitude of the RP Component by RP Level
RP Level Criteria for RP Level RP Component
Level 1 Top 25% of KCF Practices +10%
Level 2 26% – 50% of KCF Practices +2%
Level 3 Bottom 50% of KCF Practices and the top 50% of nephrology
practices nationally
0%
Level 4 Bottom 50% of KCF Practices and 51% – 75% (25
th
to 50
th
percentile) of nephrology practices nationally
-6%
Level 5 Bottom 50% of KCF Practices and bottom 25 percent (below
the 25
th
percentile) of nephrology practices nationally or did
not pass Quality Gateway
-20%
Continuous Improvement (CI) Component Calculation
For each 12-month period, starting in PY2024, the KCF Practice’s PBA may include a CI Component.
• If the KCF Practice passes the Quality Gateway threshold, then it will be eligible for the CI
Component. The extent of improvement needed on the Utilization measures to receive the CI
Component of the PBA, as well as the magnitude of the CI Component, will depend on the RP
Level for the KCF Practice.
• If the KCF Practice does not pass the Quality Gateway threshold, then it will not be eligible for
the CI Component.
CMS will assess KCF Practice improvement based on comparing the KCF Practice’s performance on the
Utilization measures to a previous performance period. For KCF Practices that begin participation in
PY2023, the first CI Component will be determined by comparing a KCF Practice’s performance on
utilization between the 12-month performance period for PY2023 and the 12-month period for? PY2024.
The CI Component and RP Component are added to calculate the PBA, and the PBA is then applied to
the CKD QCP and MCP component of the AMCP for a KCF Practice beginning in PY2025 Q3. The
target improvement on Utilization measures from one performance period to another will range from 3.5
to 5 percent.
The CI Component will range between 4 percent and 10 percent. Table 7 details the percent improvement
in Utilization measures needed for each RP Level, and the amount of the CI Component, as a percentage
of the CKD QCP and MCP component of the AMCP.

Updated 03/06/2022 28
Table 7. Magnitude of CI Component and percent improvement on Utilization measures needed by PBA
performance level
RP Level Target: Required Percent
Improvement on Utilization
Measures to receive CI
Component
CI Component
Level 1 +3.5% +10%
Level 2 +4.0% +5%
Level 3 +4.5% +4%
Level 4 +4.5% +4%
Level 5 +5.0% +10%
Magnitude of the PBA
For KCF Practices entering the Model in PY2023, the PBA will be based solely on the RP Component.
Therefore, for PBAs applied from July of PY2024 through June of PY2025, the PBA will range from +20
percent (maximum upside potential) to -20 percent (downside risk) adjustment to the CKD QCP and the
MCP component of the AMCP for the measurement period. We believe that this risk structure, along
with the frequency of assessment, will provide an incentive for continuously improving health outcomes
for aligned beneficiaries and reducing unnecessary utilization.
Table 8. PBA Magnitude by PBA Level –Starting in PY2024
PBA RP Level PBA Components (Percent
Adjustment to CKD QCP & MCP
component of the AMCP)
Total PBA Impact (% Adjustment
to CKD QCP and MCP component
of the AMCP)
Relative
Performance RP
Component
Continuous
Improvement CI
Component
(Available
starting PY2025)
RP + CI
(Maximum
Upward PBA
Adjustment)
(Available
Starting PY2025)
RP Only
(Does not qualify
for CI)
Level 1
+10% +10% +20% +10%
Level 2 +2% +5% +7% +2%
Level 3
+0% +4% +4% 0%
Level 4
-6% +4% -2% -6%
Level 5
Passed Quality
Gateway
-20% +10% -10% -20%
Failed to Pass
Quality Gateway
-20% 0% -20% -20%

Updated 03/06/2022 29
F. Quality Strategy
Th
ere are two sets of measures that CMS will use to evaluate the performance of KCF Practices: Quality
Gateway measures and Utilization measures. The Quality Gateway measure set includes measures that
indicate appropriate clinical care and engagement for the patient population. These measures are directly
and indirectly related to the beneficiary’s kidney disease, and applicable to both patients with CKD Stages
4 or 5 and patients with ESRD. The Utilization measure set includes measures of health care utilization
that are direct outcomes of quality clinical care, care management, and care coordination. These will be
adapted for the Model context from existing measures with demonstrated reliability and validity, if
adaptions are necessary.
As described above, both the Quality Gateway and Utilization measures will be used to determine the RP
a
nd CI components of the PBA.
The Quality Gateway measures are:
•
Gains in Patient Activation (PAM®) Scores at 12 Months; NQF ID #2483
•
Depression Remission at Twelve Months – Progress Towards Remission; NQF ID #1885
The Utilization measures are:
•
Optimal End Stage Renal Disease (ESRD) Starts; NQF ID #2594 – This measures the percentage
of new ESRD patients during the measurement period who experience a planned start of renal
replacement therapy by receiving a preemptive kidney transplant, by initiating home dialysis, or
by initiating outpatient in-center hemodialysis via arteriovenous fistula or arteriovenous graft.
•
Per Capita Costs Measures – The Innovation Center has worked with CMS Center for Clinical
Standards and Quality (CCSQ) to develop two total cost of care measures that are similar to the
Total Per Capita Costs (TPCC) measure that CMS currently uses in MIPS, but are appropriate for
the KCC Model's patient and participant population. There are two cost measures: one for CKD
Stages 4 or 5 and one for ESRD. These measures are payment standardized, annualized, risk
adjusted, and specialty adjusted to evaluate the overall efficiency of care provided to KCF
Beneficiaries.
Measures to be developed
CMS will develop new performance measures for the specific patient population that incentivize optimal
care management that delays progression to ESRD or dialysis and lowers mortality. The measures under
development – i.e., Standardized Mortality Ratio for Late Stage CKD and ESRD, and Measure of Delay
or Reduction of Progression to ESRD (or dialysis) – will be incorporated into the KCF quality strategy as
they become available.
G. Benefit Enhancements
Under section 1115A(d)(1) of the Act, the Secretary of Health and Human Services may waive such
requirements of Titles XI and XVIII and of sections 1902(a)(1), 1902(a)(13), 1903(m)(2)(A)(iii), and
certain provisions of section 1934 of the Act as may be necessary solely for purposes of carrying out
section 1115A with respect to testing models described in section 1115A(b). CMS has found that it is
necessary for purposes of testing the KCF Option to waive certain provisions of the Medicare statute and
regulations. As a result of these waivers, participating KCF Practices can choose to make certain
additional benefits available to their aligned beneficiaries during the performance period of the Model.

Updated 03/06/2022 30
These additional benefits are referred to as benefit enhancements. CMS anticipates that the following
ben
efit enhancements will be available for PY2023:
Table 9. Benefit Enhancements
Name Description
Kidney Disease
Education (KDE)
Benefit Enhancement
Medicare currently covers up to six 1-hour sessions of KDE services for
beneficiaries that have CKD Stage 4. While the KDE benefit is intended to
ensure beneficiaries are informed about the effects and treatment of kidney
disease, diet and nutrition, transplantation, dialysis modalities, and vascular
access, the uptake of this service has been exceptionally low at less than two
percent of eligible patients. In the KCC Model, beneficiary education is a
crucial component of increasing rates of transplants and home dialysis and
delaying the onset of ESRD. Therefore, CMS will make available to KCF
Practices a conditional waiver of certain KDE requirements as necessary to
test ways to increase the provision of the KDE benefit under the KCC Model.
The programmatic waivers would:
• Waive the requirement that the KDE be performed by a physician,
physician assistant, nurse practitioner, or clinical nurse specialist to allow
certain additional types of clinical staff to furnish KDE services incident to
the services of a participating KCF Nephrology Professional.
• Waive the requirement that a beneficiary have Stage 4 CKD in order to
test furnishing the KDE benefit to beneficiaries with CKD Stage 5 and
those in the first 6 months of starting dialysis, who can also benefit from
KDE.
• Waive the requirement that the content of KDE services include the
management of comorbidities, including for the purpose of delaying
initiation of dialysis, to allow participating nephrologists to cover this
topic only where relevant to a beneficiary, as delaying dialysis would not
be relevant to beneficiaries with ESRD who have already begun dialysis.
• Waive the requirement that an outcomes assessment designed to measure
beneficiary knowledge of chronic kidney disease and its treatment be
conducted during one of the KDE sessions, provided that such an
assessment is administered by a qualified person (as that term is defined
under 42 CFR 410.48(a)) within one month of a beneficiary’s final KDE
session.

Updated 03/06/2022 31
Name Description
Post-Discharge Home
Visits Benefit
Enhancement
CMS will make available to KCF Participants a conditional waiver of certain
supervision requirements in order to allow payment for certain home visits to
eligible, non-homebound aligned beneficiaries when such home visits are
furnished “incident to” a physician’s (or other practitioner’s) professional
services by “auxiliary personnel” as defined in 42 CFR §410.26(a)(1), under
general supervision (instead of direct supervision) of a physician or other
practitioner who is a KCF Participant.
Payment for these visits will only be allowed when visits are furnished
following the beneficiary’s discharge from an acute inpatient hospital,
inpatient psychiatric facility, inpatient rehabilitation facility, long-term care
hospital, or skilled nursing facility. The beneficiary must not qualify for
Medicare coverage of home health services (or qualifies for Medicare
coverage of home health services on the sole basis of living in a medically
underserved area). Further, a beneficiary would not be eligible to receive
covered home visits under this Benefit Enhancement if they are receiving
services under the Home Health Homebound Waiver Benefit Enhancement.
Also, under this benefit enhancement, a beneficiary is eligible to receive up to
nine post-discharge home visits within 90 days following discharge. The nine
home visits do not accumulate across multiple discharges; if the beneficiary is
admitted within 90 days of the initial discharge and before receiving nine
home visits, the beneficiary may receive only nine home visits in connection
with the subsequent discharge.
Telehealth Benefit
Enhancement
CMS will make available to qualified KCF practices a conditional waiver of
the following requirements with respect to otherwise covered telehealth
services furnished by an Eligible Telehealth Provider to a KCF Beneficiary
when furnished in accordance with the CKCC PA :
1. Waiver of Originating Site Requirements. CMS waives the
requirements in Section 1834(m)(4)(C) of the Act and 42 CFR §
410.78(b)(3)–(4) with respect to telehealth services furnished in
accordance with the CKCC PA.
2. Waiver of Originating Site Requirement in the Eligible Telehealth
Individual Provision. CMS waives the requirement in Section
1834(m)(4)(B) of the Act that telehealth services be “furnished at an
originating site” when the services are furnished in accordance with
the CKCC PA.
3. Waiver of Originating Site Facility Fee Provision. CMS waives the
requirement in Section 1834(m)(2)(B)(ii) of the Act and 42 CFR §
414.65(b)(3) with respect to telehealth services furnished to a
Beneficiary at his/her home or place of residence when furnished in
accordance with the CKCC PA.
Updated 03/06/2022 32
H. Beneficiary Engagement Incentives
General
Except as permitted by applicable law and the KCF Participation Agreement, KCF Practices are
p
rohibited and shall ensure that its and KCF Nephrology Professionals, and other individuals or entities
performing functions and services related to KCF activities shall not provide gifts or other remuneration
to beneficiaries to induce them to receive items or services from the KCF Practice or KCF Nephrology
Professionals, or to induce them to receive or to continue to receive items or services from the KCF
Practice or KCF Nephrology Professionals. During a performance year, KCF Practices, KCF Nephrology
Professionals, and other individuals or entities performing functions or services related to KCF Practice
activities will be permitted to furnish certain in-kind incentives described below in accordance with
requirements set forth in the KCF Participation Agreement and applicable law. In addition, a KCF
Practice may elect to offer the Cost-Sharing Support for Face-to-Face Visits Beneficiary Engagement
Incentive, the Chronic Disease Management Reward Beneficiary Engagement Incentive, or both (each, a
“Beneficiary Engagement Incentive”) to certain KCF Beneficiaries subject to compliance with the KCF
Participation Agreement and applicable law.
In-kind Incentives
CMS believes that beneficiary engagement is an important part of encouraging more active participation
by
beneficiaries in their health care. Beneficiary engagement and coordination of care could be enhanced
by providing certain in-kind incentives to beneficiaries that would potentially encourage beneficiaries to
become actively involved in their care. Subject to compliance with all applicable laws and regulations and
the terms of the KCF Participation Agreement, KCF Practices, KCF Nephrology Professionals, and other
individuals or entities performing functions or services related to KCF activities will be permitted to
provide in-kind items or services to certain KCF Beneficiaries, if the following conditions are satisfied:
1. There is a reasonable connection between the in-kind items or services and the medical care of the
b
eneficiary;
2. The items or services are preventive care items and services or advance a one or more of the
f
ollowing clinical goals for the KCF Beneficiary: including adherence to a treatment regime
(including prescribed medication); adherence to a follow-up care plan; or management of a chronic
disease or condition;
3. The in-kind item or service is not a Medicare-covered item or service for the KCF Beneficiary on the
d
ate the in-kind item or service is furnished to that beneficiary (for purposes of this exception, an item
or service that could be covered pursuant to a Benefit Enhancement is considered a Medicare-covered
item or service, regardless of whether the KCF Practice selects to participate in such Benefit
Enhancement for a given Performance Year); and
KCF Practices and KCF Nephrology Professionals would pay for in-kind incentives from their own funds
a
nd at their discretion. Calculation of the KCF Practice’s benchmark and Performance Year expenditures
will not account for any of these items or services.
1. Cost-Sharing Support for Face-to-Face Visits Beneficiary Engagement Incentive
Subject to compliance with all applicable laws and regulations, the terms of the KCF Participation
Agreement, and CMS approval, a KCF practice may select to participate in the Cost-Sharing Support for
Face-to-Face Visits Beneficiary Engagement Incentive. Under the terms of the KCF Participation
Updated 03/06/2022 33
Agreement, a KCF Practice that selects and who has not been rejected by CMS for this option may offer
c
ost sharing support in the form of reduced or eliminated cost sharing for Medically Necessary Face-to-
Face Visits furnished by the KCF Practice under the KCC Model. The cost-sharing support must be
provided uniformly and consistently to certain KCF Beneficiaries by the KCF Practice. The KCF Practice
must not offer cost-sharing support to any KCF Beneficiary unless the beneficiary has no secondary
insurance that covers cost-sharing for the Face-to-Face visits and either: is experiencing documented
financial hardship, has documented evidence of high disease burden and Medically Necessary Face-to-
Face Visits may avoid hospitalization of the KCF beneficiary, or there is documented evidence of a recent
hospitalization or emergency department visit. KCF Practices that elect to offer cost-sharing support will
be required to submit an Implementation Plan detailing the procedures to be used to determine whether a
KCF beneficiary is eligible to receive the cost-sharing support.
The principal aim of allowing KCF Practices to offer this cost sharing support is to reduce financial
b
arriers so that certain beneficiaries may obtain needed care and better comply with treatment plans,
thereby improving their own health outcomes. In addition, permitting KCF Practices this flexibility will
provide a critical tool to engage aligned beneficiaries, promote the utilization of high-value services, and
incentivize aligned beneficiaries to continue receiving their care from KCF Practices.
The cost of providing the cost sharing support must not be shifted to Medicare or another federal health
car
e program. The KCF Practice shall note advertise or promote the availability of the Cost-Sharing
Support, except that the eligible KCF Beneficiary may be made aware of the availability of the benefit at
the time that KCF Beneficiary could reasonably benefit from it.
Participating KCF Practices will be
subject to monitoring and compliance activities in connection with the use of cost sharing support,
including all remedial actions in the Participation Agreement. To minimize possible abuse of this
Beneficiary Engagement Incentive, CMS will incorporate certain beneficiary protections and other
safeguards into the KCF Participation Agreement.
2. Chronic Disease Management Reward Beneficiary Engagement Incentive
Subject to compliance with all applicable laws and regulations, the terms of the KCF Participation
Agreement, and CMS approval, a KCF Practice may select to offer a Chronic Disease Management
Reward Beneficiary Engagement Incentive. Under this option, a KCF Practice, whose selection has not
been rejected by CMS, may provide gift cards to certain KCF Beneficiaries, up to an annual limit of $75,
for the purpose of incentivizing participation in a chronic disease management program. KCF Practices
will pay for the gift cards out of their own funds and at their discretion, subject to certain conditions. We
believe that allowing KCF Practices to incentivize beneficiary participation in a chronic disease
management program will promote beneficiary self-management, and ultimately improve quality and
reduce costs.
KCF Practices that elect to offer a Chronic Disease Management Reward Beneficiary Engagement
I
ncentive and whose election has not been rejected by CMS, will be required to submit an Implementation
Plan detailing how they will structure their program. KCF Practices will be permitted to offer programs
that focus on any KCF beneficiaries with a specific disease or chronic condition, as long as the program
does not discriminate against any KCF beneficiary who would otherwise qualify for participation. KCF
Practices that elect to offer a Chronic Disease Management Reward Beneficiary Engagement Incentive
will be required to maintain records of their reward program, including documentation of the amount and
type of each gift card awarded and the basis for beneficiary eligibility. Participating KCF Practices will be
subject to monitoring and compliance activities in connection with their reward program. To minimize
possible abuse of this Beneficiary Engagement Incentive, we will incorporate certain beneficiary
Updated 03/06/2022 34
protections and other safeguards into the KCF Participation Agreement and the Practice will be subject to
al
l applicable remedial actions for failure to comply with the terms of the Agreement.
I. Termination
CMS may immediately or with advance notice terminate a KCF Practice’s Participation Agreement if
gr
ounds for remedial action exist (including noncompliance with the terms of the participation agreement
or other program integrity issues), or as otherwise specified in the KCF Participation Agreement or
required by section 1115A(b)(3)(B) of the Social Security Act.
All KCF Practices will be expected to participate in the Model for at least two Performance Years.
However, a KCF Practice may terminate its Participation Agreement and exit the Model by providing
notice to CMS specifying an effective date of termination that is at least 30 days following the date of the
notice. KCF Practices may terminate the Participation Agreement without any financial liability by giving
notice to CMS by February 28, 2023 with an effective date of termination of the Participation Agreement
that is no later than March 30, 2023. A KCF Practice that submits a notice of termination for PY2023 to
CMS after February 28, 2023, or with an effective date of termination of the Participation Agreement that
is on or after March 31, 2023, will be subject to financial reconciliation for the full Performance Year,
and may be prohibited from participating in other Innovation Center Models.

Updated 03/06/2022 35
J. Application for KCF Option
1. Instructions
Practices interested in participating in the KCF Option must file an application by no later than March 25,
2022, at 11:59pm. To file an application, applicants must fill out and complete the Qualtrics form
available here.
CMS reserves the right to request additional information (interviews, site visits, or additional information
related to application responses) from applicants in order to assess their applications.
Applicants seeking to withdraw their application must submit an electronic withdrawal request to CMS
via
the following mailbox: KCF-CKCC-[email protected]. The request must be submitted as a PDF on
the organization’s letterhead and must be signed by a corporate official authorized to bind the applicant.
It should include: the applicant organization’s legal name; the organization’s primary point of contact; the
full and correct address of the organization; and a description of the nature of the withdrawal.
2. Application Template for KCF Option
Practices should include a description of the nephrology professionals that they will include in their KCF
appl
ication. However, there will be a later opportunity to submit detailed information about these
nephrology professionals.
Questions about the application should be directed to KCF-CKCC-[email protected].
Section A – Applicant Practice Information and Eligibility
1. Applicant is a(n):
Individual Nephrologist(s) Professional Corporation
Nephrology Physician Practice
2. Applicant Contact Information
• Applicant Practice Legal Business Name:
• Tax Identification Number (TIN)
• Mailing Address (Street, City, State, Zip Code):
You will now be asked to identify each individual or entity that has an ownership or investment interest in
the
Applicant practice. After entering the information for one individual or entity you will be asked if you
would like to identify additional individuals or entities.
3. Please identify each individual or entity that has an ownership or investment interest in the
App
licant practice. For each entity please include the following:
• Corporate Name:
• Corporate TIN:
• Corporate Street Address:
• Corporate County:
• Corporate State:
• Corporate Zip Code:
• Corporate Phone Number:
Updated 03/06/2022 36
4. Name of primary organizational contact for the individual or entity previously entered. We will
u
se this information to link practices within the same larger health care/parent organization.
o
First Name:
o Last Name:
o
Email:
o Phone Number:
5. Please describe the nature of the organization (e.g., another physician organization, public or
private hospital, health system, or foundation owned by a hospital, insurance company, health
plan or HMO, medical school or university, etc.):
6. Do you wish to identify another individual or entity that has an ownership or investment interest
in the Applicant practice?
Yes
No
7. If Applicant is not owned by an outside entity, who owns this practice? Select all that apply.
Physicians in the practice
Non-physician practitioners (nurse practitioners or physician assistants) in the practice
Other (Please describe) _________________________________________
8. Does your practice share a TIN for billing with other practices that are part of the same health
group or system?
Yes
No
9. Please provide the following contact information for the Applicant’s Executive Contact. Note
the executive contact must have the authority to act as the Applicant’s authorized corporate
official.
•
Name:
•
Organizational Title:
•
Phone Number:
•
E-mail Address:
10. Please provide the following contact information for the Applicant’s Primary Contact.
•
Name:
•
Organizational Title:
•
Phone Number:
•
E-mail Address:
11. Please provide the following contact information for the Applicant’s Secondary Contact.
•
Name:
•
Organizational Title:
•
Phone Number:
•
E-mail Address:
Updated 03/06/2022 37
12. Did any of your nephrology professionals participate in the Comprehensive ESRD Care Choices
(CEC) Model or are they currently participating in the KCC Model?
Yes
No
If so, please describe the nature of their participation in the CEC and/or KCC Model (ex. participant
owner or participant non-owner, etc.) ___________
13. Please indicate if any of the Applicant’s nephrology professionals have participated in or are
p
articipating in any of the following:
Accountable Health Communities
ACO Investment Model
Advance Payment ACO Model
Bundled Payments for Care Improvement
Bundled Payments for Care Improvement Advanced
Comprehensive Care for Joint Replacement
Comprehensive Primary Care Initiative
Comprehensive Primary Care Plus
Global and Professional Direct Contracting Model (GPDC)
Independence at Home Demonstration
Maryland All-Payer Model
Maryland Total Cost of Care Model
Medicare Care Choices Model
Medicare Shared Savings Program
Medicare ACO Track 1+ Model
Next Generation ACO Model
Oncology Care First
Oncology Care Model
Pioneer ACO Model
Private, For-Profit Demo Project for the Programs of All-Inclusive Care for the Elderly
(PACE)
State Innovation Models Initiative
Transforming Clinical Practice Initiative
Other (please specify)
Not Applicable
14. Please describe the nephrology professionals whom the Applicant expects will participate in the
KCF Option as a part of your KCF Practice, including the number of clinical and non-clinical
care providers and their roles. Please note that Applicant will have a later opportunity to provide
CMS with updated information regarding its nephrology professionals.
15. Please describe the Applicant’s performance under prior or current risk sharing arrangements, if
any. Risk sharing arrangements must include: (1) financial accountability; (2) evaluation of
patient experiences of care; and (3) substantial quality performance incentives. If applicable,
please include performance under CMS programs, demonstrations, and models that meet the
Updated 03/06/2022 38
definition of outcomes-based contracts. Provide an “N/A” response if no prior or current risk
sh
aring arrangements. Please keep responses to a maximum of approximately 500 words.
16. I certify that my organization is a recognized legal entity formed under applicable state, federal,
or
tribal law and authorized to conduct business in each state in which it operates or will be by
the time the Participation Agreement is signed. You must certify to proceed with the application.
Yes
Section B – Or
ganizational Structure, Leadership and Management, and Governance Structure
17. Please provide a paragraph summarizing your pr
actice. This may include: the practice’s history,
mission, and organization, including your practice’s affiliations; the practice’s composition,
geographic service area including where most of the practice's patients reside, if the service area
encompasses urban, suburban, and/or rural locations, if the area includes underserved
beneficiaries, and if the practice will work with other community-based organizations under the
KCF Option if selected to participate (e.g., care management organization, ESRD networks,
quality improvement organization, etc.). Please include any other applicable narrative
describing the practice. Please keep responses to a maximum of approximately 500 words
Section C –
Care Model Patient Centeredness
18. Please provide a narrative explanation of why the App
licant wishes to participate in the KCF
Model Option and how the Applicant will achieve the goals of better health and better care for
Medicare beneficiaries with CKD, ESRD, and kidney transplants. Please keep responses to a
maximum of approximately 500 words.
19. Please provide a narrative description of the App
licant’s plan for engaging with CKD and ESRD
beneficiaries and their caregivers. At a minimum, please address the following:
a. Managing the progression of CKD
b. Modality options and tr
ansition onto dialysis
c. Coordination of care with different providers and suppliers
d. Transplant process and mana
ging post-transplant care
e. Health I.T. and data sharing
f. Prescription drug utilization
g. Shared decision-m
aking, self-management and self-care skill development
Please keep responses to a maximum of approximately 1000 w
ords.
20. Please describe the App
licant’s historical and planned population health management and/or
population health tools. If applicable, please describe the metrics the Applicant has historically
used or plans to use to understand how to deploy clinicians, invest resources, and generally
improve health equity in managing the Applicant’s potential attributed beneficiary population.
At a minimum, please address the following:
a. Experience with social determinants of health and furnishing care to underserved
c
ommunities
b. Managing care for dually eligible beneficiaries
c. Metrics used for identifying health inequities in patients served

Updated 03/06/2022 39
d. Processes used to make improvements to address and mitigate identified health disparities
4
e. Decision support tools for use by providers/suppliers and/or patients/caregivers, and any tools
or approaches for fostering what might be termed “health literacy” in patients and their
families.
f. Processes for ensuring that the Applicant provides culturally-competent care
g. Approaches for providing high-quality-care to patients who do not speak English or for
whom English is a second language.
Please keep responses to a maximum of approximately 1000 words.
Section D – Community Engagement
21. Please describe the history of collaboration among major stakeholders in the community(ies)
being served and commitment from relevant community stakeholders to achieve seamless and
comprehensive care. Please include specific examples of community stakeholders with whom
the Applicant has a relationship and the nature of each relationship. Please keep responses to a
maximum of approximately 500 words.
Section E – Attestation and Signature
I have read the contents of this application. By my signature, I certify to the best of my knowledge,
information, and belief that the information contained herein is true, correct, and complete, that I am
authorized to sign this application on behalf of the applicant organization. I understand that the applicant
must not engage in anti-competitive practices, and if it has engaged in such practices, it may not get
accepted into the Model. If accepted into the Model, I understand that CMS can rescind the offering of a
Participation Agreement or terminate the Participation Agreement if it is determined that the applicant has
engaged in anti-competitive practices. I authorize the Centers for Medicare & Medicaid Services (CMS)
to verify this information. If I become aware that any information in this application is not true, correct, or
complete, I agree to notify CMS of this fact immediately and to provide the correct and/or complete
information.
____________
Printed Name of Applicant’s Authorized Corporate Official Date
____________
Signature of Applicant’s Authorized Corporate Official Date
4
Any race or ethnicity-conscious strategies must be supported by specific data or other information demonstrating a need for the
race or ethnicity-conscious strategy, and must demonstrate a close fit between disparities and the race or ethnicity-conscious
action that the Applicant intends to take. Additionally, any race or ethnicity-conscious strategies should be supported by
information demonstrating that alternative strategies that do not involve race or ethnicity will not be sufficient or effective to
address this disparity.
40
IV. Comprehensive Kidney Care Contracting (CKCC) Options
KCEs must be comprised of one or more nephrologists or non-physician clinicians who specialize in
nephrology (referred to collectively as “nephrology professionals”) and at least one transplant provider,
and may include other providers and suppliers that help to coordinate the care for beneficiaries with CKD
Stages 4 and 5, ESRD, and kidney transplants, such as dialysis facilities. KCEs will focus on improving
the quality of care, reducing total cost of care, delaying the progression of kidney disease, and increasing
the transplant rate.
The CKCC
Options include three options: the Graduated Option, the Professional, and the Global
Options. In all three Options, participants will receive capitated payments for care furnished to Medicare
beneficiaries with CKD Stages 4 and 5 and ESRD who are aligned to the KCE. The KCE will select a
risk sharing option, and will be accountable for quality outcomes.
KCEs will have the choice to move from a lower risk option to a higher risk option at the start of each
P
erformance Year beginning for their third Performance Year, but would not be able to move to a lower
risk option from a higher risk option. For instance, a KCE that is in the Professional Option in its second
performance year can move to the Global Option for its third Performance Year, but not vice versa.
A. Legal Entity and Governance Requirements
The KCE should be formed by one or more KCE Participants, which are Medicare-enrolled providers and
suppliers who have a participant agreement in place with the KCE and are identified on the KCE’s KCE
Participant List, as described further below. Each KCE must be identified by a single TIN and, unless
there is only one KCE Participant, must be a separate and unique legal entity that is recognized and
authorized to conduct business under applicable federal, state, or tribal law. The KCE may be an existing
legal entity if it conforms to all of the requirements set forth in this RFA and the CKCC Participation
Agreement (e.g., governance and composition requirements). To participate in the Model, the KCE must
be capable of:
•
Receiving and distributing shared savings payments or other payments received from CMS.
•
Collecting and repaying shared losses, if applicable.
•
Establishing reporting mechanisms and ensuring compliance with applicable Model requirements,
including but not limited to reporting on quality measures.
•
Securing a financial guarantee, if applicable.
KCEs must include as KCE Participants at least one nephrology professional, and at least one transplant
pr
ovider. Transplant providers can include: a transplant program (as defined in 42 CFR § 482.70) that
provides kidney transplants, a transplant hospital (as defined in 42 CFR § 428.70) that provides kidney
transplants, a transplant surgeon (as that term is used in 42 CFR § 482.98) who provides kidney
transplants, a transplant nephrologist, a transplant nephrology practice, an Organ Procurement
Organization (OPO), or another Medicare-enrolled provider or supplier who provides kidney transplant
related Covered Services to Medicare beneficiaries. Nephrology professionals may only participate in one
KCE, while transplant providers may participate in multiple KCEs. A transplant nephrologist would
participate in the KCE in their capacity as a transplant provider and could participate in multiple KCEs if
they do not identify themselves as an alignment eligible nephrologist. If the transplant nephrologist self-
identifies as an alignment eligible nephrologist, they may only participate in one KCE.
Most other providers and suppliers may participate in multiple KCEs and other CMS initiatives, if
co
nsistent with the rules governing the other initiative. Other Medicare-enrolled providers and suppliers

Updated 03/06/2022
41
(other than durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) suppliers,
ambulance suppliers and drug/device manufacturers) are able to join a KCE as a KCE Participants, but
their participation is not mandatory for KCE eligibility.
KCE Governance Requirements
A KCE must maintain an identifiable governing body with sole and exclusive authority to execute the
functions and make the final decisions on behalf of the KCE. The KCE’s legal entity and governing body
must be separate and unique to the KCE, except that where the KCE is formed by a single KCE
Participant, the KCE’s legal entity and governing body may be the same as that of the KCE Participant.
The governing body may be a board of directors, board of managers or any other governing body
structure that provides a mechanism for shared governance and decision making. The KCE governing
body must:
•
Have authority to execute the functions of the KCE including defining the processes to promote
evidence-based medicine and patient engagement, reporting on quality and cost measures and
coordination of care, and the appointment and removal of an executive officer.
•
Have authority for final decision-making for the KCE, including responsibility for oversight and
strategic direction of the KCE and responsibility for holding the KCE management accountable
for the KCE’s activities.
•
Have a conflict of interest policy that applies to members of the governing body, requires
disclosure of all relevant financial interests and other conflicts of interest, identifies processes for
resolution of conflicts of interest, and sets forth remedial processes for non-compliance.
•
Have a transparent governing process.
•
Receive regular reports from the designated compliance official of the KCE, who is not legal
counsel to the KCE and who must report directly to the governing body.
Members of the governing body have a fiduciary duty to the KCE and are required to act consistent with
t
hat duty when engaging in governing body duties.
The KCE governing body must be structured as follows:
•
The governing body must ensure representation of patient interests by including an independent
Medicare beneficiary with CKD Stages 4 or 5 or ESRD who received nephrology services from a
KCE Participant at any time during the 15 months prior to the start of the Performance Year or an
experienced consumer advocate on the governing body. This representative must not have a
conflict of interest with the KCE or have an immediate family member with a conflict of interest
with the KCE. The representative must not be a participant in the KCE and not have a direct or
indirect financial relationship with the KCE or its KCE Participants, except that the person may
be reasonably compensated by the KCE for his or her duties as a member of the governing body
of the KCE.
•
Decision-making must be KCE participant-driven, as evidenced by KCE Participants or their
representatives having at least 75% control of the KCE’s governing body. The beneficiary
representative and/or consumer advocate shall not be included in either the numerator or
denominator when calculating percent control. The KCE may seek an exception from the 75
percent control requirement by submitting a proposal to CMS describing the current composition
of the KCE's governing body and how the KCE will involve KCE Participants in innovative ways
in KCE governance. Any exception to the 75 percent control requirement will be at the sole
discretion of CMS.
Updated 03/06/2022
42
• KCE Participants who are KCE Nephrology Professionals or KCE Nephrology Practices (or their
representatives) must represent at least 30% of the membership of the governing body. The
beneficiary representative and/or consumer advocate shall not be included in either the numerator
or denominator when calculating percent control.
• At least one governing body member must be a transplant provider or a representative a
transplant provider.
• KCE Participant Dialysis facility executives, employees or representatives may not exceed 50
percent control of the governing body. The beneficiary representative and/or consumer advocate
shall not be included in either the numerator or denominator when calculating percent control.
• The KCE governing body may not include any of the following: durable medical equipment,
prosthetics, orthotics, and supplies (DMEPOS) suppliers, ambulance suppliers, drug/device
manufacturers, or individual or entities that are excluded or otherwise prohibited from
participation in Medicare or Medicaid.
B. KCE Composition
A KCE must include at least one of each of the following as a KCE Participant in each Performance Year:
• A nephrology professional
• A transplant provider
Transplant providers may participate in multiple KCEs as KCE Participants or Preferred Providers.
Nephrologists, nephrology professionals, nephrology practices, and dialysis facilities may only participate
in a single KCE as a KCE Participants, a restriction that does not apply to other types of participants. In
addition to the required types of KCE Participants noted above, a KCE may include any of the following
optional Medicare-enrolled providers or suppliers as KCE Participants:
• Medicare-certified dialysis facilities, including facilities owned by large dialysis organizations
(LDOs), facilities owned by small dialysis organizations (SDOs), or independently-owned
dialysis facilities. LDOs may only participate in the Professional and Global options of CKCC.
• Other Medicare-enrolled providers and suppliers.
All types of providers and suppliers other than nephrology professionals and transplant providers, are
optional KCE Participants, including dialysis facilities, dieticians, and SNFs. DMEPOS suppliers,
ambulance suppliers, and drug/device manufacturers are prohibited from participating in a KCE. While
the KCE will not be required to be a Medicare-enrolled provider or supplier, KCE Participants under the
KCE must be a Medicare-enrolled provider or supplier by a date specified by CMS.
The KCE’s Market Area is the geographic area in which the main practice locations of the KCE’s
nephrology professionals are physically located. Generally, a KCE’s Market Area is defined as no more
than five CBSAs, which must be connected by no more than three rural counties and/or no more than one
CBSA. If the Market Area CBSAs are in more than one state, then those states must be contiguous. The
only exception to this requirement would be in the case of rural applicants whose locations are not
included in any Medicare CBSA. For rural applicants not located in any Medicare CBSA, the KCE
Market Area will be composed of the rural counties in a single state in which KCE nephrology
professionals have their main practice location.
In order to align beneficiaries, CMS will also need to determine a KCE’s Service Area. For a KCE, the
Service Area is defined as the KCE’s Market Area, and any CBSAs that are contiguous to the KCE’s
Market Area and any rural counties located in the same state(s) as the KCE’s Market Area in which
Updated 03/06/2022
43
participating nephrology professionals provide nephrology services (see Table 10) to beneficiaries with
CKD or ESRD .
If a KCE includes dialysis facilities, then all dialysis facilities that participate in that KCE must be owned
in w
hole or in part by the same dialysis organization., Additionally, at least 85% of the dialysis facilities
owned in whole or in part by that dialysis organization that are located within the KCE’s Market Area
must participate in the KCE. Furthermore, all dialysis facilities that participate in a KCE must be located
in the KCE’s Service Area.
Participating providers and suppliers other than nephrology professionals and dialysis facilities would not
be su
bject to Market Area or Service Area constraints.
The CKCC Options define categories of Medicare providers/suppliers and their respective relationships to
the
KCE. The two primary categories are KCE Participants and Preferred Providers in all three options:
•
KCE Participants are the core providers/suppliers in the Model. KCE Participants are Medicare-
enrolled providers or suppliers that bill for items and services they furnish to beneficiaries under a
Medicare billing number assigned to a TIN in accordance with the applicable Medicare
regulations and have agreed to participate in the Model. KCE Participants enter into a written
agreement with a KCE that satisfies the requirements of that KCE’s CKCC Participation
Agreement, and are identified on that KCE’s list of KCE Participants. In addition, a KCE
Participant cannot be a Preferred Provider (as described below) or a prohibited participant (i.e., a
DMEPOS supplier, an ambulance supplier, a drug or device manufacturer, or a provider/supplier
that is otherwise prohibited from participation in Medicare or Medicaid). The services furnished
by nephrology professionals that are KCE Participants are used for purposes of aligning
beneficiaries to the KCE.
•
Preferred Providers contribute to KCE goals by promoting better care for beneficiaries by
extending and facilitating valuable care relationships beyond the KCE. Preferred Providers are
Medicare-enrolled providers or suppliers that bill for items and services they furnish to
beneficiaries under a Medicare billing number assigned to a TIN in accordance with applicable
Medicare regulations, and have agreed to participate in the Model. Preferred Providers enter into
a written agreement with a KCE that satisfies the requirements of that KCE’s CKCC
Participation Agreement, and are identified on that KCE’s list of Preferred Providers. A Preferred
Provider cannot be a KCE Participant or a prohibited participant (as described above). Services
furnished by Preferred Providers will not be considered in beneficiary alignment. Nephrologists,
nephrology professionals, and nephrology practices cannot be Preferred Providers. Preferred
Providers are not considered participants in an Advanced Alternative Payment Model for the
purpose of the Quality Payment Program.
Both KCE Participants and Preferred Providers have the opportunity to participate in the Benefit
Enh
ancements selected by the KCE.
Individual providers and suppliers can be added to the Model as KCE Participants or Preferred Providers
only a
t the beginning of each Performance Year.
KCE Participants may not be KCE Participants in another KCE in the KCC Model, except as specified by
CMS,
or participate in the KCF Option. Likewise, KCE Participants are not permitted to participate in
the Medicare Shared Savings Program, other Medicare shared savings initiatives (except as expressly
permitted by CMS), the Independence at Home Demonstration (IAH), Primary Care First (PCF), ACO
Realizing Equity, Access, and Community Health (ACO REACH) Model (formerly known as the Global
Updated 03/06/2022
44
and Professional Direct Contracting (GPDC) Model, and Vermont Medicare ACO Initiative, or the
Maryland Primary Care Program (MDPCP) portion of the Maryland Total Cost of Care Model (MD
TCOC). For KCE Participants, overlaps are checked at the TIN level for the Medicare Shared Savings
Program and NPI-TIN level for the other models discussed above. The only exception is dialysis
facilities, for which overlaps are checked based on CCN for all initiatives except the Medicare Shared
Savings Program – which is checked based on TIN. Preferred Providers may overlap with the Medicare
Shared Savings Program and the other models discussed above.
C. Beneficiary Alignment
The patient population for the CKCC Options is Medicare beneficiaries with CKD Stages 4 and 5, ESRD,
a
nd kidney transplant recipients. CMS will prospectively align eligible beneficiaries to KCEs through a
claims-based alignment process. It is important to note that the alignment of beneficiaries to KCEs is for
Model test purposes only. Model activities for which beneficiary alignment under this Model is relevant
include expenditure calculations for KCEs, quality performance measurement, and CMS’ monitoring of
claims data. Beneficiary alignment to a KCE does not inhibit beneficiaries’ freedom to choose to receive
care from other Medicare providers and suppliers within Medicare FFS. Similar to other CMS programs
and models, the CKCC Options do not include provisions for beneficiaries that have been aligned to a
KCE to opt out of alignment, but they may opt out of certain data sharing with the KCE. Aligned
beneficiaries may obtain nephrology services from health care providers not participating in a KCE,
which could cause them to be de-aligned to a KCE retroactively during alignment reconciliation.
1. Beneficiary Eligibility
To be eligible for alignment and to remain aligned to a KCE during a Performance Year, a beneficiary
m
ust meet all of the following criteria, except where otherwise noted:
• Has either CKD Stages 4 or 5 or ESRD, or is a transplant recipient with a functioning kidney who
was previously aligned to the KCE while the beneficiary had CKD Stages 4 or 5 or ESRD;
•
Is enrolled in Medicare Parts A and B;
•
Is not enrolled in a Medicare Advantage plan, cost plan, or other non-Medicare Advantage
Medicare managed care plan;
•
Resides in the United States;
•
Receives greater than 50% of their nephrology services or MCP claims furnished in the KCE’s
Service Area;
•
Is 18 years of age or older;
•
Is alive;
•
Is not already aligned to a Medicare ACO or another participant in a Medicare
program/demonstration/model where overlap is not allowed;
•
Is not aligned to another KCE;
•
Does not have Medicare as a secondary payer;
•
Not received a kidney transplant in the last 13 months (initial alignment only);
•
Not in an active election period of hospice care at the time CMS conducts alignment, as
determined using Medicare enrollment data (initial alignment only); and
•
Not received hospice care at any time during the last three months of the 12-month period that
ends 3 months prior to the start of the quarter for which CMS is conducting initial alignment to
the KCE (“Alignment Lookback Period”) or during the period between the end of the Alignment
Lookback Period and the alignment run date (initial alignment only).

Updated 03/06/2022
45
If a beneficiary meets the alignment eligibility criteria described above, the beneficiary will be initially
aligned to the KCE if the beneficiary also meets the applicable criteria described in Table 9 below.
After each Performance Year, KCEs must have a have minimum of 750 aligned Medicare beneficiaries
wi
th CKD Stages 4 or 5 and 350 aligned Medicare beneficiaries with ESRD or else they will in most
cases have to aggregate their performance. CMS does not require that the KCE furnish services to a
minimum number of aligned transplant beneficiaries. Once an aligned beneficiary receives a kidney
transplant, they do not count towards a KCE’s minimum required number of aligned CKD or ESRD
beneficiaries. However, if the beneficiary was aligned to a KCE and had CKD Stages 4 or 5 or ESRD for
a period of time during the relevant Performance Year prior to receiving a kidney transplant, that period
of time may count towards the KCE’s applicable beneficiary minimum.
2. Alignment Process
Alignment to KCEs participating in the CKCC Options will occur through nephrology professionals that
ar
e KCE Participants for each stage of kidney care (CKD Stages 4 and 5, ESRD, or transplant recipient
who was previously aligned while they had CKD Stages 4 or 5 or ESRD) and will differ based on the
beneficiary’s kidney disease status. This is different than the CEC Model, where beneficiaries were
aligned through the dialysis facility.
CMS believes that aligning beneficiaries through participating nephrology professionals has the following
ad
vantages:
•
Prioritizes the nephrology professional relationship as the most important one for beneficiaries
with CKD Stages 4 or 5, ESRD, or kidney transplant.
•
Protects the continuity of care by aligning a beneficiary with CKD Stages 4 or 5 with the same
nephrology professional who might then be treating them for ESRD, although it does not have to
be the same nephrology professional.
•
Allows beneficiaries who only dialyze at nursing facilities, instead of outpatient dialysis facilities,
to be aligned to KCEs and included in the Model test if they receive care furnished by the KCE’s
nephrology professionals.
Initial and Quarterly Alignment
Alignment will be as prospective as is feasible given particular mechanisms, summarized in Table 9
below, and will be retrospectively finalized as part of a reconciliation process after each Performance
Year, allowing for a minimum of three months claims run-out. CMS will identify the final aligned
beneficiary population for the KCE following this reconciliation process. Beneficiaries will be de-aligned
from the KCE’s list of aligned beneficiaries if they do not receive certain health services from a
nephrology professional identified by the KCE as an aligning provider during the Performance Year, or
receive the majority of certain health services outside of the KCE’s Service Area.
KCEs will receive a list at the start of their first Performance Year with the aligned beneficiaries whose
car
e they will be accountable for based on visits in the past year. New eligible beneficiaries who satisfy
the alignment criteria described in Table 10 will be added to each KCE’s alignment list on a quarterly
basis. Once aligned, beneficiaries remain aligned to the KCE until they meet one of the criteria for de-
alignment.

Updated 03/06/2022
46
Table 10. Some Alignment Criteria by Beneficiary Type
Eligible Beneficiaries with
CKD
Eligible Beneficiaries with
ESRD
Eligible
Beneficiaries who
Receive Kidney
Transplants
Aligning
Participant
Nephrology professional Nephrology professional N/A – Must have
been previously
aligned by virtue of
CKD or ESRD
Criteria for
Alignment
Diagnosis of CKD Stages 4
or 5; No MCP claims; 2 or
more Nephrology Services
(Professional/Carrier claims)
within a 12-month period
with a KCE nephrology
professional; 50% or more
nephrology services within
the KCE Service Area;
Kidney disease status of
ESRD; 2 or more MCP claims
with a KCE nephrology
professional within a 3-month
period; 50% or more MCP
services within the KCE
Service Area.
Being previously
aligned to the KCE as
a CKD or ESRD
beneficiary and
receiving a kidney
transplant
Criteria for
De-alignment
Beneficiaries received the
majority of Nephrology
Services outside the KCE
Service Area; or did not
receive any Nephrology
Services from a KCE
nephrology professional
during the months of the
performance year in which
they were an eligible
beneficiary.
Beneficiaries received the
majority of MCP claims
outside the KCE Service
Area, did not receive any
MCP claims with a KCE
nephrology professional
during the months of the
performance year in which
they were an eligible
beneficiary, or did not receive
any maintenance dialysis
treatments during the
Performance Year.
Kidney transplant
failure (the
beneficiary may be
aligned as a CKD or
ESRD beneficiary
post-transplant
failure if the
applicable
requirements for
alignment are met); 3
years past their
transplant
The alignment lookback period is the 12-month period that ends 3 months prior to the start of quarter for
which CMS is conducting beneficiary alignment within which claims must occur in order to be
considered for the quarterly alignment process. For example, for PY2023 Quarter 1 (PY2023 Q1), the
lookback period is October 2021 to September 2022.
CMS will run beneficiary alignment for PY2023 Q1 in October 2022. CMS will then send beneficiary
al
ignment lists to KCEs in advance of the start of their first Performance Year (January 1, 2023).
Ineligibility and Dealignment
Beneficiaries aligned during one Performance Year will roll over to the next Performance Year , unless
they are de-aligned during the Annual Alignment Reconciliation that occurs at the end of the Performance
Year. If an aligned beneficiary no longer meets certain eligibility criteria during a Performance Year ,
they will remain aligned for the remainder of the Performance Year but CMS will assign to them an
eligibility status of “ineligible” and their expenditures will not be counted toward financial calculations

Updated 03/06/2022
47
for months in which they are ineligible. Aligned beneficiaries who become ineligible may be moved back
to eligible status again if they meet certain eligibility criteria again in the future.
When an aligned CKD or ESRD beneficiary receives a kidney transplant, they will remain aligned to the
KC
E for up to three years from the month of transplant in order for the KCE to be eligible to receive
Kidney Transplant Bonus payments, but the beneficiary’s expenditures will no longer be counted toward
financial calculations and the beneficiary will not be included in the quality performance sample for the
KCE. If the transplant fails within three years, the beneficiary will be de-aligned from the KCE. It is
possible for a kidney transplant beneficiary to become realigned (either to the original KCE or to a
different KCE) as a CKD or ESRD beneficiary in the event their transplant fails and they subsequently
meet the criteria required to be eligible for initial alignment. It is also possible for an aligned beneficiary
to progress from CKD to ESRD during the Performance Year . CMS reviews and updates each aligned
beneficiary’s kidney disease status (e.g., CKD, ESRD, or transplant recipient) on a quarterly basis. CMS
will also determine each aligned beneficiary’s final kidney disease status for each month that the
beneficiary was aligned to the KCE during a Performance Year after the end of the Performance Year.
De-alignment criteria, including de-alignment based on a beneficiary not receiving care from a
ne
phrology professional identified by the KCE as an aligning provider during the Performance Year or
receiving the majority of nephrology services or MCP claims outside the KCE’s Service Area, are
designed to ensure an accurate measure of the cost and quality of the beneficiary care in the model test.
The de-alignment criteria are intended to capture situations where there is no longer a care relationship
between the KCE nephrology professional and the aligned beneficiary. While there may be some
incentive for a KCE and its KCE Participants to refer aligned beneficiaries outside of the KCE Service
Area in order to take advantage of the de-alignment criteria – experience in the CEC Model has shown
that the market areas, as defined above, tend to be large enough that seeking care outside of the market
area truly represents a change in beneficiary residence rather than strategic referrals. This approach to de-
alignment balances predictability in beneficiary populations and accuracy in alignment, while reflecting
the unique way CKD and ESRD beneficiaries interact with the health care system.
Finalizing Alignment
Alignment will be retrospectively finalized as part of a reconciliation process after each Performance
Year. Through this reconciliation process, which will allow for a minimum of three months claims run-
out, CMS will identify the final aligned population for the KCE for the Performance Year, including each
beneficiary’s months of alignment within the Performance Year. In certain cases, a beneficiary may
become de-aligned from the KCE for the entire Performance Year at reconciliation if they meet the
Criteria for De-alignment described in Table 9 above:
•
Received the majority of their Nephrology Services or MCP claims outside of the KCE’s Service
Area;
•
Did not receive any Nephrology Services or MCP claims from one of the KCE’s aligning
providers; or
•
Did not receive any maintenance dialysis treatments during the Performance Year (ESRD
beneficiaries only).
3. Beneficiary Minimums and Aggregation
As previously noted, during each Performance Year, the KCE must have a minimum of 750 aligned
M
edicare beneficiaries with CKD Stages 4 or 5 and 350 aligned Medicare beneficiaries with ESRD. If a
KCE fails to meet either minimum threshold for a Performance Year, as determined by CMS during the
Updated 03/06/2022
48
annual alignment reconciliation process, CMS may take remedial actions, including requiring the KCE to
submit a Corrective Action Plan (CAP) explaining the steps it will take to meet the minimum threshold
for CMS’ review and approval, or termination of the KCE’s Participation Agreement.
In addition, a KCE that does not meet these minimum alignment thresholds at the end of the Performance
Y
ear, and does not include an LDO as a KCE Participant or KCE Preferred Provider, will generally be
required to aggregate its financial performance and quality performance with that of certain other KCEs
in the same option (referred to as the KCE’s aggregation partners). KCEs that may be required to
aggregate will have the opportunity to request one or more (up to 5) aggregation partners for the purposes
of creating a group of KCEs (an aggregation group) that collectively meet the minimum number of
aligned beneficiaries. The KCE must submit its preferred aggregation partner or partners for a given
Performance Year by a date specified by CMS. CMS will review any requests for preferred aggregation
partners and may accept, modify, or reject such requests at CMS’s sole discretion, using criteria specified
in the CKCC Participation Agreement. If a KCE that is required to aggregate does not submit a request
for its preferred aggregation partner(s), then CMS will assign an aggregation partner or partners based on
the KCE Service Area and geographic proximity of other KCEs in the same option that are also required
to aggregate. If at the end of the Performance Year one or more aggregation partners in an approved
aggregation group meet the minimum alignment thresholds and one or more other aggregation partners in
the same group do not, then the performance for the KCEs in the aggregation group will still be
aggregated. If all aggregation partners in an approved aggregation group meet the minimum alignment
thresholds at the end of the Performance Year, then the performance of the entities in the aggregation
group will not be aggregated.
However, if a KCE that includes dialysis facilities owned in whole or in part by an LDO does not meet
th
e minimum alignment thresholds at the end of the Performance Year, or if CMS determines that there
is not aggregation group available for a KCE that does not meet the minimum alignment thresholds at the
end of the Performance Year, the KCE will not be required to aggregate its quality performance or
financial performance with other KCEs. Rather, in these situations, the KCE’s financial performance for
the Performance Year will be subject to a Minimum Savings Rate or Minimum Losses Rate (MSR or
MLR). In order to start in the Model, KCEs must have at least 50% of the required minimum aligned
beneficiary thresholds. The required number of beneficiaries is at least 375 CKD Stages 4 or 5
beneficiaries and 175 ESRD beneficiaries. Entities that do not meet these requirements will be notified
and will not be offered a CKCC Participation Agreement for PY2023.
4. Beneficiary Notifications and Marketing Materials
All KCEs will be required to share with aligned beneficiaries certain details about their alignment to the
KC
E and the KCE’s participation in the Model. For KCEs’ ease, CMS will provide templates that
participants may use for aligned beneficiary notification purposes. If CMS provides a template to be used
for these notification requirements, such template will include all of the required information described
below and prior CMS review/approval of the template will not be needed. The KCE must also comply
with all applicable federal laws regarding interaction with Medicare FFS beneficiaries.
Specifically, KCEs will be required to ensure that their KCE Participants display materials in their office
or facility locations notifying beneficiaries that they are participating in the Model. KCEs are also
required to ensure that their KCE Participants distribute a paper copy of the informational materials to
each aligned beneficiary at the beneficiary’s first office visit with a KCE Participant after the KCE
Participant receives notice that the beneficiary is aligned to the KCE.

Updated 03/06/2022
49
The notification must include the following elements:
• A short description of the CKCC Option the KCE is participating in and what that means for their
care.
• The beneficiary’s option to opt out of certain data sharing, with instructions for how to modify his
or her data sharing preferences by calling 1-800-MEDICARE;
• Affirmation of beneficiary protections under Medicare, including beneficiary freedom of choice
5
;
and
• Instructions on whom to contact with concerns about beneficiary protections and the KCE
Participants’, as applicable, participation in the Model.
KCEs and their nephrology professionals must provide any KCE marketing materials and activities to
CMS upon request. If CMS requests such materials and activities, CMS will review them to ensure that
the materials comply with the terms of the CKCC Participation Agreement, including that they are not
inaccurate or misleading, are not discriminatory or used in a manner that is discriminatory, and make
clear that alignment to a KCE does not remove or otherwise affect a beneficiary’s freedom to choose a
provider or supplier. Additional requirements concerning this review process will be provided in the
CKCC Participation Agreement.
To ensure beneficiary freedom of choice, the KCE shall not, and shall require its KCE Participants and
Preferred Providers to not, commit any act or omission, nor adopt any policy that inhibits Medicare
beneficiaries from exercising their freedom to obtain health services from providers or suppliers who are
not KCE Participants or Preferred Providers.
5. Data Sharing
CMS will make historical and monthly claims data available to KCEs upon request, consistent with data
sharing practices in other comparable models and programs, and consistent with all applicable laws and
regulations, including HIPAA and the Part 2 regulations governing the disclosure and use of certain
substance use disorder patient records.
Upon a KCE’s request, CMS will make available several types of Medicare data for the purposes of the
health care operations work of the KCE, including developing and implementing activities related to care
coordination and quality assessment and improvement for beneficiaries aligned to the KCE under the
CKCC Options. Such data may include:
(1) individually identifiable demographic and Medicare eligibility status information about aligned
beneficiaries and various summary reports with data relevant to the KCE’s operations and performance in
the Model (such as data related to quality, expenditures, etc.); and (2) detailed claims data files that will
include individually identifiable claim and claim line data for services furnished by Medicare-enrolled
providers and suppliers to aligned beneficiaries. Historical data files for aligned beneficiaries will be
limited to three years of historical data, consistent with the approach under the CEC Model and other
shared savings models and programs.
The claims data provided to the KCE will not include individually identifiable data for aligned beneficiaries
who have opted out of data sharing. Moreover, CMS will honor the data sharing opt out decisions by
5
The beneficiary maintains the right to see any Medicare participating healthcare provider at any time under the traditional
Medicare FFS benefit structure. Example language may read “You still have the right to visit any dialysis facility, doctor,
hospital, or healthcare provider that accepts Medicare” and/or “This is not a Medicare Advantage Plan or any kind of managed
care plan.”

Updated 03/06/2022
50
beneficiaries who were previously given that choice while an aligned beneficiary in another Medicare ACO
initiative. KCEs are required to provide aligned beneficiaries who inquire about or wish to modify their
data sharing preferences with information regarding how to modify their data sharing preferences by calling
1-800-MEDICARE. The communications that the KCEs share with such beneficiaries must note that, even
if a beneficiary has elected to decline claims data sharing, CMS may still engage in certain limited data
sharing for care coordination and quality improvement activities for aligned beneficiaries, and population-
based activities relating to improving health or reducing health care costs, as well as claims data sharing
regarding claims subject to the CKD QCP Fee Reduction.
D. Finance and Payment
KCE
s will be eligible for the following payments:
•
CKD Quarterly Capitation Payment (CKD QCP)
•
Adjusted Monthly Capitation Payment (AMCP)
•
Kidney Transplant Bonus (KTB)
•
Shared savings/shared losses under one of the following Options:
o Graduated
o
Professional
o
Global
1. Payment Types
CKD Quarterly Capitation Payment (CKD QCP)
CMS will pay KCEs through an innovative per beneficiary CKD QCP, which combines payment for
several different outpatient E/M services and other care management services listed below, collectively
referred to as Nephrology Services, into a single capitated payment. The CKD QCP is intended to
provide an upfront payment to facilitate delivery of care for aligned beneficiaries with CKD Stages 4 or 5.
The CKD QCP replaces Medicare FFS payments for Nephrology Services when furnished to aligned
beneficiaries by nephrology professionals participating in the KCE. KCEs will be required to have
financial arrangements with these nephrology professionals to reimburse these practitioners for services
provided. Nephrology professionals will still be required to submit claims with the relevant codes for data
collection and quality purposes, but CMS will only pay the CKD QCP for Nephrology Services furnished
to aligned beneficiaries with CKD Stages 4 or 5. The CKD QCP is designed to allow flexibility in care
delivery and to give providers/suppliers a more stable payment stream to deliver advanced care for
aligned beneficiaries with CKD Stages 4 or 5. For the beneficiary, this may result in increased access to
nephrology care for their CKD, improved efficiency and coordination in addressing health issues, and
improved patient experience. The Model will test whether upfront, predictable revenue will help
nephrology professionals coordinate care for aligned beneficiaries with other specialists to better address
their renal needs.

Updated 03/06/2022
51
Table 11. Nephrology Services Included in the CKD QCP
Service Type CPT Codes
Office/Outpatient Visit E/M 99201-99205,
99211-99215,
Complex Chronic Care Coordination Services 99487
Home Care / Domiciliary Care E/M 99348-99349
Prolonged E/M 99354-99355
Transitional Care Management Services 99495-99496
Advance Care Planning 99497-99498
Welcome to Medicare and Annual Wellness Visits G0402, G0438, G0439
Chronic Care Management Services 99490
Prolonged non-face-to-face E/M Services 99358
6
Assessment/care planning for patients requiring CCM services G0506
Online digital E/M for an est. patient, for up to 7 days 99421 – 99423
Phone E/M phys/qhp 99441 – 99443
KCE Participants will continue to receive normal fee-for-service payments for services furnished to
aligned beneficiaries that are not included in the CKD QCP, such as inpatient visits, and services for
beneficiaries who have received transplants. KCE Participants will also continue to receive normal fee-
for-service payments, rather than CKD QCPs, for services furnished to beneficiaries not aligned to the
KCE. Beneficiary cost sharing for the services included in the CKD QCP will be set at the cost-sharing
amount which the beneficiary would have paid for the particular Nephrology Service furnished to the
beneficiary during a particular encounter, rather than the amount the beneficiary would have had to pay
based on the CKD QCP amount. The CKD QCP amount will be approximately one third of the amount
of the MCP that participating nephrology professionals are paid during the Performance Year for aligned
beneficiaries who are receiving dialysis services. The CKD QCP payment amount will be the same
amount for a beneficiary with CKD Stage 4 or CKD Stage 5. These payments will not be risk adjusted,
given very similar risk profiles in the CKD Stages 4 and 5 populations.
Because the CKD QCP is paid prospectively, KCEs may receive CKD QCPs for beneficiaries who are
deemed eligible at the time of alignment but are subsequently found ineligible for the period. As a result,
CMS will withhold a percentage of the CKD QCP amount paid each quarter to account for these changes
in alignment and will calculate alignment-based adjustments after the Performance Year to ensure CMS
did not overestimate the withhold. The withhold and adjustments ensure that the CKD QCP (and
corresponding FFS claims for services included in the CKD QCP) are paid accurately for services
6
The use of this code was discontinued in the CY 2020 PFS final rule. As this code is no longer used, it will not generate claims.
However, we are retaining the code for documentation purposes, as it was used in analyses supporting the development of the
CKD QCP methodology.

Updated 03/06/2022
52
provided. CMS will withhold 20 percent of CKD QCP amounts that would otherwise be paid to
participants during the Performance Year, and although this percentage is unlikely to change, CMS
maintains the right to increase or decrease the withhold percentage in subsequent Performance Years. We
refer to this withhold as the CKD QCP Alignment Withhold. After the end of each Performance Year,
CMS will reconcile the CKD QCP Alignment Withhold against the value of the KCE’s alignment
adjustments. Based on this analysis, CMS will return to the KCE any amounts owed by CMS to the KCE
but will not hold the KCE liable for recoupments beyond the amount of the withhold during the
Performance Year if the KCE is deemed to owe CMS.
CMS will also adjust the CKD QCP to account for “leakage,” meaning the dollar value of Medicare FFS
claim pa
yments for Nephrology Services furnished to aligned beneficiaries with CKD Stages 4 or 5 by
nephrology professionals who are not in the KCE that would have been subject to the CKD QCP fee
reduction if the services had been furnished by nephrology professionals in the KCE. This adjustment
incentivizes a sustained doctor-patient relationship. Increases in services delivered by nephrology
professionals outside of the KCE to aligned beneficiaries will lead to a reduction in the CKD QCP paid to
the KCE. CMS will determine actual leakage for each KCE following the end of each Performance Year ,
but CMS will use a prospective withhold to reduce the likelihood of recoupments for leakage. CMS will
withhold 10% of all CKD QCP payments to KCE to account for leakage. After the Performance Year,
CMS will reconcile the 10% withhold for leakage to the amount of leakage that occurred during the
Performance Year. CMS will either pay the KCE any excess leakage withheld if leakage is under the
amount withheld or recoup additional leakage from the KCE if leakage is over the amount withheld.
Consistent with PCF, to support continuous care, CMS may also share data with participants on
Nephrology Services delivered outside of the KCE to the KCE’s aligned beneficiaries.
Adjusted Monthly Capitation Payment (AMCP)
Currently, Medicare pays physicians and other practitioners who manage dialysis care for beneficiaries
receiving dialysis through the MCP. The per-patient-per-month MCP payment is for all routine
outpatient physicians’ services related to the dialysis patient’s renal condition. The amount of the MCP
varies based on several criteria:
• The location where the beneficiary dialyzes (at home or in center).
•
The number of face-to-face visits with the beneficiary for beneficiaries who dialyze in center (one
monthly visit, two- or three-monthly visits, or four or more monthly visits).
•
The age of the beneficiary.
Under the CKCC Options, CMS will modify the current MCP payment structure. Nephrology
pro
fessionals in the KCE will continue to bill the MCP as they ordinarily would and will receive the MCP
FFS amount from CMS that they would have received had they not been in the Model.
However, the current payment structure of the MCP creates a bias towards in-center hemodialysis
because
the highest MCPs are available for beneficiaries who dialyze in-center and receive four in-person
visits a month. According to a 2015 GAO report, equalizing nephrologist payments for home and in-
center dialysis removes the financial disincentive for prescribing home dialysis and supports beneficiaries
dialyzing at home.
The AMCP addresses this disincentive for prescribing home dialysis through the Home Dialysis True-Up,
which will standardize MCP reimbursement amounts for Nephrology Services regardless of where a
beneficiary dialyzes. The national average MCP for a nephrologist who visits a patient in-center 4 or
more times per month is $221 PBPM. The majority of MCP claims, over 70%, are billed at this 4+

Updated 03/06/2022
53
monthly visit level. The national average MCP for a nephrologist who delivers care to a patient who
dialyzes at home is approximately $185 PBPM. The AMCP standardizes the MCP for home dialysis and
in-center dialysis patients by paying KCEs an additional $35 per MCP home dialysis claim for services
delivered to aligned ESRD beneficiaries. CMS will make this payment to KCEs at the end of the
Performance Year.
The total amount of the AMCP is the MCP, which is paid to the nephrology professional at current FFS
rates, plus the Home Dialysis True-Up, which is paid retrospectively to the KCE. As a result, the KCC
Model reduces the variance in reimbursement for ESRD dialysis services delivered to aligned
beneficiaries who dialyze in center compared to at home. Unlike the CKD QCP that CMS pays
prospectively to the KCE, CMS will pay the KCE the Home Dialysis True-Up component of the AMCP
in a lump sum at after the end of the Performance Year.
Kidney Transplant Bonus (KTB)
In addition to the payments described above, KCEs are eligible for up to three KTB payments for every
aligned beneficiary with CKD or ESRD who receives a kidney transplant, whether from a living or
deceased donor, provided the transplant remains successful. The KTB will create a direct incentive for
model participants to support beneficiaries through the transplant process, including continued care
management of transplant recipients to support graft success.
CMS recognizes the lack of supply of available kidneys and that nephrologists do not control access to
the transplant wait list. However, CMS believes that this payment could better incentivize providers and
suppliers to move beneficiaries onto the waitlist, assist beneficiaries with the living donation process, and
support beneficiaries after they receive a transplant in maintaining the health of the transplanted organ.
As stated, the purpose of the KTB is to incentivize KCEs to support beneficiaries during and after the
t
ransplant process through care coordination and other services – including patient engagement and
support – that are necessary to maximize the likelihood of long-term success for an organ transplant.
CMS does not intend that the KTB be used for, or imply that Model participants are permitted to, exert
inappropriate influence over the transplant process, or that Model participants can acquire, receive, or
otherwise transfer organs in exchange for valuable consideration. The exchange or transfer of valuable
consideration for a human organ for transplantation is in violation of section 301 of the National Organ
Transplant Act of 1984 (NOTA), as amended. Certain payments, including “reasonable payments
associated with the removal, transportation, implantation, processing, preservation, quality control, and
storage of a human organ,” are not valuable consideration for purposes of this criminal prohibition.
Inappropriate or illegal use of the KTB, in violation of NOTA or any other laws or regulations, would
result in removal from the Model and referral to the appropriate law enforcement organization.
CMS will make up to $15,000 in KTB payments per transplant, paid to the KCE at set intervals following
th
e transplant. In general, the KTB will be disbursed to the KCE in three installments as follows: $2,500
one year after transplant, $5,000 two years after the transplant, and $7,500 three years after the transplant.
In order to receive KTB installment payments, three criteria must be met at the time of disbursement, as
follows:
•
The beneficiary must remain alive.
•
The beneficiary’s kidney transplant has not failed (e.g., the beneficiary must not have returned to
maintenance dialysis).
•
The KCE must be participating in the Model.

Updated 03/06/2022
54
Payment of the KTB in installments over three calendar years introduces challenges for transplants that
occur in PY2025 and PY2026. Transplants during these Performance Years would result in KTB
payments being made after the performance period for the KCC Model ends in 2026 and settlement is
completed in 2027. Transplants that occur in PY2025 would require CMS make KTB payments in 2026 –
2028 and transplants that occur in PY2026 would require CMS make KTB payments in 2027 – 2029. To
address this dynamic, the KCC Model will alter both the amount and schedule of KTB installments for
transplants made in PY2025 and PY2026. Specifically, CMS will increase the proportion of the KTB paid
to participants in CY2027 for PY2025 and PY2026 transplants to ensure no payments need to be made
after CY2027.
At least 20 percent of KTB payments must be shared with KCE Participants who are transplant providers
(e.g., transplant surgeons, OPOs, etc.), and an additional 20 percent of the KTB payment must be shared
with KCE Participants who are nephrology professionals in order to ensure that the work of these KCE
Participants in the transplant process is recognized. The distribution of the remaining 60 percent of the
KTB payments is at the discretion of the governing body of the KCE, subject to the requirements of
applicable law.
Table 12. Schedule of KTB Installments
Installment
Transplants PY2022 – PY2024 Transplants PY2025 Transplants PY2026
Amount
per
Transplant
Date of Payment*
Amount
per
Transplant
Date of
Payment*
Amount
per
Transplant
Date of
Payment*
1
st
Installment
$2,500 1 year after
transplant
$2,500 1 year after
transplant
$2,500 1 year
after
transplant
2
nd
Installment
$5,000 2 years after
transplant
$5,000 2 years
after
transplant
$2,500 1 year
after
transplant
3
rd
Installment
$7,500 3 years after
transplant
$3,750 2 years
after
transplant
$3,750 1 year
after
transplant
Maximum
Total KTB
$15,000 $11,250 $8,750
*Provided transplant remains successful
2. CKCC Model Options
KCEs in the CKCC Options have two sources of income or losses from CMS. First, KCEs receive the
CKD QCP and AMCP and can be eligible to receive the KTB discussed earlier. Second, KCEs can be
eligible for shared savings or (with the exception of KCEs participating in Level 1 of the Graduated
Option) be liable for shared losses. CMS will calculate a prospective total cost of care benchmark based
on total Medicare Part A and Part B expenditures for aligned beneficiaries. CMS will reconcile the total
cost of care for the aligned beneficiaries during the Performance Year against the Performance Year
benchmark, giving KCEs the opportunity to be eligible to earn shared savings or be liable for shared

Updated 03/06/2022
55
losses depending on their expenditures compared to the benchmark. The amount that a KCE can retain or
will owe to CMS varies depending on the CKCC Option in which the KCE participates.
The CKD QCP and AMCP (and TCC if added to the CKCC Global Option in a future Performance Year)
coun
t as expenditures against the Performance Year benchmark, while the KTB does not. More details on
the financial methodology can be found below.
KCEs will have the option to select from among the following options:
•
CKCC Graduated Option: KCEs participating in this option will enter into a path that allows the KCE
to enter the Model at a lower level of risk and transition into a higher level of risk in future years.
Under the Graduated Option, KCEs may choose to begin participation under a lower-reward one-
sided option or a two-sided option with a lower level of risk and incrementally phase in risk and
additional potential reward. The Graduated Option is intended for KCEs with either no dialysis
facility participants or only dialysis facility participants with small dialysis organization ownership
(i.e., dialysis organizations with 500 or fewer dialysis facilities). KCEs with dialysis facility
participants owned by dialysis organizations that own, in whole or in part, more than 500 dialysis
facilities will not be allowed to participate in this option. KCEs entering into the Graduated Option
may select either level of risk (Level 1 or Level 2) at the start of their first Performance Year:
Level 1 – a one-sided arrangement where KCEs will share in up to 40% of savings in the total
cost of care for Medicare Part A and B services for aligned beneficiaries relative to a
benchmark calculated in the manner specified below. Level 1 is available only for the KCE’s
first Performance Year; and
Level 2 – a two-sided arrangement where KCEs will share in up to 50% of savings but only
30% of losses in the total cost of care for Medicare Part A and B services for aligned
beneficiaries relative to a benchmark calculated in the manner specified below.
If the KCE selects Level 1 for its first Performance Year, the KCE will automatically graduate to
Level 2
for its second Performance Year, and will then graduate to either Professional Option or the
Global Option for its third Performance Year. If the KCE selects Level 2 for its first Performance
Year, the KCE will automatically graduate to the Professional Option for its second Performance
Year.
•
CKCC Professional Option: KCEs participating in this option will share in 50% of savings or losses
in the total cost of care for Medicare Part A and B services for aligned beneficiaries relative to a
benchmark calculated in the manner specified below.
•
CKCC Global Option: KCEs participating in the Global Option will be at risk for 100% of the total
cost of care for all Medicare Part A and B services for aligned beneficiaries relative to a benchmark
calculated in the manner specified below.
While the payment methodology and degree of risk varies across CKCC options, a common
benchm
arking methodology will apply across all three options. In this section, the benchmarking
methodology will be described first, then the differences between the payment methodologies under the
three options will be discussed.
3. Benchmarking Methodology
Each option will use the same benchmark process, which will include the following steps:
1. Determine the baseline/historical expenditure
2. Apply trending and geographic adjustment factor (GAF)
3. Incorporate regional expenditures

Updated 03/06/2022
56
4. Risk adjust
5. Discount and quality adjustments
The benchmarks will be calculated prospectively and given to KCEs at the start of each Performance Year
and may be adjusted to account for CKD progression. Separate benchmarks will be calculated for CKD
and ESRD beneficiaries
7
and will cover all Medicare Part A and B costs, including those not related to
kidney disease, with a few exceptions. These exceptions are designed to avoid negative cost incentives
for behaviors CMS wishes to promote and include kidney transplant-related costs, such as: evaluation of
the recipient and donor, blood and tissue typing of the recipient and donor, organ acquisition, execution of
the transplant itself, and services following the transplant.
CMS reserves the right to change financial model provisions to respond to specific circumstances in a
particular market, such as a natural disaster or other emergency.
Step 1: Determine the baseline / historical expenditure
For all three CKCC options, the baseline period is a fixed three-year period for the duration of the KCC
Model: 2017, 2018, and 2019. These baseline years will be weighted to give additional weight to the
most recent base year (BY), recognizing that the population of base year-aligned beneficiaries for the
most recent base year is likely more comparable to the KCE’s Performance Year population of aligned
beneficiaries. The Model incorporates the weighting scheme used in the Shared Savings Program for
ACOs in their first agreement period (BY1 [2017] at 10%, BY2 [2018] at 30%, BY3 [2019] at 60%) in
determining a KCE’s CKD and ESRD Performance Year benchmarks. The baseline period will be static
across all of the Performance Years of the Model. However, the baseline expenditures will be updated
each year, as CMS will use a KCE’s most recent Participant List to identify the beneficiaries that would
have been aligned to the KCE for each of the base years and their associated expenditures. For example,
the baseline expenditures that will apply for purposes of calculating the PY2023 benchmarks will be
determined based on the KCE’s Participant List for PY2023. For PY2024, the same baseline period will
be used, but the baseline expenditures will be determined based on the KCE’s Participant List for
PY2024.
Step 2: Apply trending and Geographic Adjustment Factor (GAF)
Trending is determined by the year-over-year projected percent change in the U.S. Per Capita Cost
(USPCC). The USPCC is developed annually by the CMS Office of the Actuary and announced in the
annual Announcement of Calendar Year (CY) Medicare Advantage Capitation Rates and Medicare
Advantage and Part D Payment Policies. The CKCC Options will use the USPCC’s general FFS trend
rate for the CKD benchmarks and the USPCC’s ESRD trend rate for the ESRD benchmarks. CMS will
make adjustments to the USPCC, such as an adjustment based on a comparison of the projected USPCC
to the experience and trend for specific populations, to take into account differences in the expenditure
trend of the FFS population as a whole compared to the subset of FFS beneficiaries eligible to be aligned
to KCEs. Under limited circumstances, CMS may use an adjusted projected trend figure in response to
unforeseeable events that have a substantial impact on Medicare FFS expenditures. Any such adjustment
to the trend projections would be intended to prevent KCEs from being unfairly penalized or rewarded for
major payment changes beyond their control.
The USPCC growth trend will be adjusted to reflect the anticipated impact of changes in the regional
GAFs applied to payment amounts under the Medicare FFS payment systems. This GAF adjustment is
intended to prevent the benchmarks from being unfairly understated (or overstated) because of differences
7
No separate benchmark will be calculated for kidney transplant beneficiaries.
Updated 03/06/2022
57
in the local geographic price adjustments that Medicare uses to calculate provider and supplier payments
between the baseline period and the Performance Year. This process accounts for variations in the cost-
of-doing-business adjustments that Medicare applies under most of its FFS fee schedules (e.g., the
Medicare area wage index, the geographic practice cost index), which are typically updated annually.
Step 3: Incorporate regional expenditures
CMS incorporates regional expenditures into the historical baseline to generate the Performance Year
bench
marks. Incorporating regional expenditures will enable the Performance Year benchmarks to better
reflect the KCE’s regional environment while also providing a simple and predictable methodology
synchronized with other Medicare payment policies. To that end, CMS will test the use of county level
benchmarks from an ACO REACH/KCC Rate Book (previously known as the GPDC/KCC Rate Book),
modeled after the Medicare Advantage (MA) Rate Book to establish regional expenditures for KCEs
participating in the CKCC Options. These county level benchmarks will be established prospectively and
published in advance of the Performance Year . CMS will publish an updated ACO REACH/KCC Rate
Book prior to each Performance Year. CMS will blend the regional expenditures with the KCE’s
historical baseline expenditures, which have been trended forward to the Performance Year, in
determining the KCE’s Performance Year benchmarks.
Use of regional expenditures in the CKCC Options will depart from the use of regional expenditures in
pre
vious ACO initiatives, in that an ACO REACH/KCC Rate Book will be used to derive the regional
expenditures. This approach, which departs from the CEC methodology of developing an ESCO-specific
calculation of regional expenditures, is intended to be responsive to stakeholder feedback that the CEC
Model’s benchmarking methodology was too complex and gave rise to uncertainty throughout the
Performance Year. In making use of a rate book modeled after the MA Rate Book, CMS will be able to
capitalize on an existing rate setting methodology.
Despite sharing similarities with the MA Rate Book, CMS has made several deviations from the MA Rate
Book i
n constructing the ACO REACH/KCC Rate Book to ensure that the rates used for this Model serve
as an accurate representation of the regional costs for purposes of benchmarking.
1. Exclusion of adjustments based on health plan performance: CMS will remove the impact of
certai
n adjustments that are incorporated into the MA Rate Book for purposes of MA plan
payment, but that are not relevant to the CKCC Options, such as the Quality Bonus Payment
(QBP) percentage based on star ratings.
2. Removal of Quartile Adjustments: CMS will remove the MA quartile adjustments to the county
Aged
& Disabled rates from the ACO REACH/KCC Rate Book.
3. Reduction in Calendar Years Contributing to Rate Book: Whereas MA looks back 7 years to
establ
ish the MA rates (using an average of 5 years of claims data per county (or state for
ESRD) and with a 2 year gap for claims lag), the ACO REACH/KCC Rate Book for CKCC will
look back 4 years, using an average of 3 years of claims data with a single year gap between the
last year in the AC ACO REACH/KCC Rate Book and the Performance Year to account for
claims lag. For example, for the PY2023 ACO REACH/KCC Rate Book, claims for 2019,
2020, and 2021 will contribute to the ACO REACH/KCC Rate Book.
4. Removal from the Rate Book of Excluded Expenditures: CMS will make adjustments to account
for
differences in expenditure types that are included for purposes of the MA rate book but are
not relevant for purposes of the CKCC Options. CMS will make adjustments to account for
differences between the subset of FFS beneficiaries eligible to be aligned to KCEs and Medicare
FFS beneficiaries generally.

Updated 03/06/2022
58
Once CMS makes its adjustments to the ACO REACH/KCC Rate Book for purposes of this Model, a
specified percent of the KCE’s regional expenditures would be “blended” into the KCE’s benchmarks.
The percentage of regional baseline expenditures and the KCE’s baseline expenditures for each
Performance Year of the Model is described in the Table 13, below.
Table 13. Regional and KCE Historical Blend for KCE Benchmarks by Performance Year
Benchmark Component PY2023 PY2024 PY2025 PY2026
Composition of the
KCE Benchmark
KCE’s Weighted Baseline
Expenditure
65% 60% 55% 50%
KCE’s Weighted Regional
Rate (derived from ACO
REACH/KCC Rate Book)
35% 40% 45% 50%
For purposes of incorporating regional expenditures into a KCE’s benchmarks, a KCE’s region will
include all counties (or states, for the ESRD population) where one or more beneficiaries aligned to the
KCE in the baseline period reside. Regional expenditures are calculated using a beneficiary-month
weighted average of county-level or state-level FFS expenditures for the KCE’s aligned beneficiaries in
each county or state. General MA rates for the Aged & Disabled (i.e. non-ESRD) population are
calculated at the county level, while ESRD MA rates are calculated at the state level. Specifically, CMS
will calculate a beneficiary month-expenditure weighted average of each county’s (or state’s, for ESRD)
ACO REACH/KCC rate for which the KCE has aligned beneficiaries; the weights will be the proportion
of the KCE’s beneficiaries residing in that county . Note that the “region” for purposes of the financial
benchmark methodology is separate and distinct from the KCE’s “service area” that is used for purposes
of alignment.
We will establish limits on the maximum upward and downward adjustment that can result from
i
ncorporating regional expenditures into the benchmarks. To align with the ACO REACH Model, we
will limit the overall upward adjustment from incorporating the regional expenditures to a flat dollar
amount equal to 5 percent of the FFS USPCC described above for the Performance Year (e.g., PY2023
will use the 2023 ACO REACH/KCC Rate Book USPCC Rate adjusted as described above). We will
limit the overall downward adjustment from incorporating the regional expenditures to a flat dollar
amount equal to 2 percent of the FFS USPCC for that Performance Year. For example, in a hypothetical
Performance Year in which the FFS USPCC rate for Aged and Disabled beneficiaries was $891.07, then
this rate would result in a maximum upward adjustment of +$44.55 (=$891.07 * 5%) PBPM to the
historical benchmark (Aged and Disabled) and a maximum downward adjustment of -$17.82 (=$891.07 *
-2%) PBPM to the historical benchmark (Aged and Disabled).
Limiting the impact of the regional expenditures in calculating the benchmarks accomplishes three goals.
F
irst, the upward limit serves as a buffer against excessive increases to the benchmarks that would stem
solely from the incorporation of regional expenditures. The regional expenditures can otherwise provide
overly inflated benchmarks for KCEs that are relatively low-spending compared to their region. Second,
the downward limit recognizes that higher-cost KCEs may be particularly sensitive to the inclusion of
regional expenditures into the baseline. KCEs with higher spending compared to the region may choose
not to participate in the Model when otherwise faced with significantly lower benchmarks. Third, the use
of a flat dollar cap, rather than a cap based on a percentage of benchmark, provides a relatively higher
adjustment for those lower spending KCEs and a relatively lower adjustment for higher spending KCEs.
Updated 03/06/2022
59
As we would expect most KCEs to be efficient relative to their region, this would have the effect of
providing a greater relative adjustment for low spending KCEs than higher spending KCEs.
Limitations on the maximum upward/downward adjustments to the Performance Year benchmarks
s
temming from inclusion of regional expenditures have previously been introduced in ACO
benchmarking, including in the Next Generation ACO Model and in the Shared Savings Program
benchmarking methodology as part of the December 2018 final rule.
Step 4: Risk adjustment
Risk adjustment is necessary in the CKCC Options to ensure that benchmarks account for differences in
t
he risk of beneficiaries aligned to the KCE in the base and Performance Years. Existing ACO risk
adjustment models used in current Medicare ACO initiatives are based on the prospective CMS
Hierarchical Condition Category (HCC) risk model, which relies on provider-supplied diagnostic codes
for a prior calendar year to predict costs in the Performance Year (e.g., diagnoses from 2018 to predict
2019 costs).
CMS will continue to use the CMS HCC risk model to risk adjust the benchmarks for the CKD Stages 4
and 5 population. Furthermore, for beneficiaries with ESRD, CMS will continue to use the same CMS-
HCC ESRD prospective model which is applied in Medicare Advantage. Internal analyses indicate that
these risk adjustment models yield benchmarks that effectively predict medical expenditures for eligible
beneficiaries.
Consistent with the Next Generation ACO Model, CMS will apply a Symmetric Risk Score Cap to the
KCE’s risk score growth (relative to a prior year) to mitigate against coding intensity. The cap will be
applied separately for the CKD Stages 4 or 5 (Aged/Disabled) and ESRD populations. For the CKD
Stages 4 and 5 population the Symmetric Risk Score Cap will be +/- 6%. The +/- 6% Symmetric Risk
Score Cap was set at a level such that approximately 30% of KCEs would be expected to have changes in
risk scores that meet or exceed the cap; based on analyses of CKD Stages 4 and 5 aligned beneficiary risk
scores in Next Generation ACO beneficiaries. For the ESRD population, the Symmetric Risk Score Cap
will be +/-3%; consistent with the Next Generation ACO Model.
Step 5: Apply discount and quality adjustments
CMS will incorporate a discount to the trended, risk adjusted ESRD benchmarks for KCEs participating
in
the Global Option. KCEs participating in the Global Option will retain 100% of savings in relation to
their Performance Year benchmarks, and as such, the discount to the ESRD benchmark represents the
only mechanism for CMS to obtain savings from this Model Option (e.g., CMS does not “share” in the
savings generated by the KCE). This discount effectively reduces the total benchmark expenditures by a
specified percentage, in an effort to ensure that savings accrue to CMS from the KCC Model. The
discount will only apply to the ESRD benchmark and not the CKD benchmark. The discount will be set at
3% of the ESRD benchmark for PY2023. Subsequently, the discount will increase by a percentage point
each year, subject to the adjustments described below, thereby requiring continuous improvement by
KCEs in the Global Option. No discount will apply to the benchmarks for KCEs participating in the
Graduated or Professional Options.
The discounts applied to the ESRD benchmark for KCEs that select the Global Option could be reduced
by
0.5% for the Performance Year if the KCE includes one or more dialysis facilities owned by a dialysis
organization as KCE Participants or Preferred Providers, and more than 90% of the dialysis facilities
owned in whole or in part by that dialysis organization are participating in one or more KCEs across the
country. The discount applied to the ESRD benchmark may also be reduced if the KCE participates in

Updated 03/06/2022
60
future multi-payer payment strategies still to be developed, if a multi-payer component is added to the
Model in future years. Because the majority of patients with CKD are not on Medicare, CMS believes
that coordination across multiple payers is important to fully address CKD.
Additionally, if an aligned beneficiary has remained in CKD Stages 4 and 5 for over two years and has
not
progressed to ESRD, CMS will apply an upward adjustment to the KCE’s CKD benchmark to reward
the KCE for keeping these beneficiaries off dialysis. To determine this adjustment, the proportion of
CKD Stages 4 and 5 beneficiary months contributed by CKD Stages 4 and 5 beneficiaries who have been
continuously aligned to the KCE for at least 24 months and have not progressed to ESRD will be
multiplied by 1%; and this product will be applied as an upward adjustment to the CKD PY benchmark.
For practical purposes, this adjustment cannot be made to benchmarks until PY2025 for KCEs that begin
participation in PY2023. CMS will begin measuring beneficiary alignment for the 24-month continuous
alignment requirement at the start of PY2023.
Finally, adjustments will be made to the benchmarks to account for the KCE’s performance on quality
m
easures. Most KCEs will be subject to a quality withhold, a reduction in their Performance Year
benchmarks. KCEs in Level 1 of the Graduated Option do not have a quality withhold, KCEs in Level 2
of the Graduated Option have a quality withhold of 2.5%, and KCEs in the Professional and Global
Options have quality withholds of 5%. KCEs can recoup a portion or all of their quality withhold based
on their performance on the quality measures. The determination of the portion of the quality withhold
that the KCE recoups is made at final reconciliation. High performing KCEs may also have the
opportunity to participate in the High Performers Pool, should they qualify. Additional details on the
quality program and its impact on the financial methodology are discussed in the quality section of this
RFA.
4. Features Specific to the
CKCC Graduated Option
Minimum Savings Rate (MSR)/M
inimum Loss Rate (MLR)
The MSR is the minimum percentage of the total Performance Year expenditure benchmark that the KCE
must have in preliminary savings to be able to receive shared savings. Conversely, to be required to pay
back shared losses, preliminary losses must exceed the minimum loss rate or the MLR.
For KCEs participating in Graduated Level 1 (under a one-sided risk arrangement), preliminary savings
m
ust exceed the MSR to be eligible to receive shared savings. CMS will use a sliding scale, based on the
number of beneficiaries aligned to the KCE to establish the MSR for the KCE.
For KCEs participating in Graduated Level 2 (which involves taking on downside risk under a two-sided
r
isk arrangement) no MSR or MLR will apply to aggregate savings or losses, and as such KCEs
participating in Graduated Level 2 will retain “first dollar” savings and be responsible for “first dollar
losses,” provided that the KCE meets the beneficiary minimums.
Aggregate Savings/Losses Cap (Risk Corridor)
For Graduated Level 1, shared savings will be capped at 10% of the KCE’s Performance Year
be
nchmark. In Graduated Level 2, the aggregate amount of shared savings that KCEs will be eligible to
receive if their actual Performance Year expenditures are lower than their Performance Year benchmark
will be limited, or “capped” using a series of caps that are set as a percent of the Performance Year
benchmark, as shown in Table 14. Similarly, in the event that KCEs generate shared losses, those shared
losses will also be capped.

Updated 03/06/2022
61
Table 14. Series of Shared Savings and Shared Losses Caps (Level 2 of the Graduated Option)
Shared savings/losses cap as a
% of the Performance Year
benchmark
Portion of savings/losses
above the cap accruing to the
KCE’s shared savings/losses
Portion of savings/losses
above the cap accruing to
CMS’ shared savings/losses
Gross Savings/Losses
Less than 5%
50% of Saving
30% of Losses
50% of Savings
70% of Losses
Gross Savings/Losses
Between 5% and 10%
35% of Savings
20% of Losses
65% of Savings
80% of Losses
Gross Savings/Losses
Between 10% and 15%
15% of Savings
10% of Losses
85% of Savings
90% of Losses
Gross Savings/Losses
Greater than 15%
5% of Savings
5% of Losses
95% of Savings and Losses
Truncation and Optional Stop-Loss
For KCEs participating in Graduated Level 1, for expenditure calculations, CMS will truncate annualized
expenditures at the 99th percentile for CKD and at the 95th percentile for ESRD beneficiaries aligned to
the KCE. For KCEs participating in Graduated Level 2 and through transition into the Professional
Option, a stop-loss arrangement will be available as an optional feature that may be selected by KCEs at
the start of each Performance Year.
The purpose of the stop-loss arrangement is to reduce financial uncertainty associated with infrequent, but
high-cost, expenditures at the level of the individual aligned beneficiary. Stop-loss protects KCEs from
financial liability on individual beneficiary expenditures that are above the stop loss “attachment points.”
An attachment point is the dollar threshold at which stop-loss protection begins. A portion of the
expenditures accrued above each attachment point and below the next highest attachment point will be
included in the KCE’s Performance Year expenditure calculations. The percent of expenditures for each
of the three attachment points will be 30%, 20%, and 10% respectively (See Table 16).
KCEs that choose the stop-loss arrangement are effectively charged for this protection. CMS will apply a
PBP
M stop loss “charge” to the KCE’s final Performance Year Benchmark, which will be based upon the
percent of expenditures above each of the KCE’s attachment points in the baseline period. Following
adjustments to PY expenditures and/or Performance Year Benchmarks to account for truncation or
selection of the stop-loss arrangement, CMS will reconcile the KCE’s Performance Year expenditures
against the KCE’s Performance Year benchmark to determine the amount of the KCE’s shared savings, as
applicable with retrospective reconciliation.
5. Features Specific to the
Professional Option
MSR/MLR
Provided that the KCE achieves the beneficiary minimums, no MSR or MLR will apply to aggregate
savings/losses for the Professional Option. As such, KCEs will retain “first dollar” savings and be
responsible for “first dollar” losses.

Updated 03/06/2022
62
Aggregate Savings/Losses Cap (Risk Corridor)
The aggregate amount of shared savings that KCEs will be eligible to receive if their actual Performance
Year expenditures are lower than their Performance Year benchmarks will be limited, or “capped” using
a series of caps that are set as a percent of the applicable Performance Year benchmark. Similarly, in the
event that KCEs generate shared losses, those shared losses will be capped, as shown in Table 15. KCEs
will be eligible to receive a portion of shared savings, or liable for a portion of shared losses, above each
threshold, with the portion decreasing with each threshold. The shared savings/shared losses caps will be
set at the following amounts:
Table 15. Series of Shared Savings and Shared Losses Caps (Professional Option)
Shared savings/losses cap as a
% of the Performance Year
benchmark
Portion of savings/losses
above the cap accruing to
the KCE’s shared
savings/losses
Portion of savings/losses above
the cap accruing to the CMS’
shared savings/losses
Gross Savings/Losses
Less than 5%
50% of savings/losses 50% of savings/losses
Gross Savings/Losses
Between 5% and 10%
35% of savings/losses 65% of savings/losses
Gross Savings/Losses
Between 10% and 15%
15% of savings/losses 85% of savings/losses
Gross Savings/Losses
Greater than 15%
5% of savings/losses 95% of savings/losses
Stop Loss Arrangement (Optional)
The purpose of the stop-loss arrangement is to reduce financial uncertainty associated with infrequent, but
high-cost, expenditures at the level of the individual aligned beneficiary. Stop-loss protects KCEs from
financial liability on individual beneficiary expenditures that are above the stop loss “attachment points.”
An attachment point is the dollar threshold at which stop-loss protection begins. A portion of the
expenditures accrued above each attachment point and below the next highest attachment point will be
included in the KCE’s Performance Year expenditure calculations. The percent of expenditures for each
of the three attachment points will be 30%, 20%, and 10% respectively (See Table 16).
KCEs that choose the stop-loss arrangement are effectively charged for this protection. CMS will apply a
P
BPM stop loss “charge” to the KCE’s final Performance Year benchmark, which will be based upon the
percent of expenditures above each of the KCE’s attachment points in the baseline period.
Additional details will be provided in future methodology papers.
Table 16. Series of Stop Loss Attachment Points (Graduated and Professional Options)
Attachment Point Percent of
expenditures
accruing to KCE
Percent of
expenditures
accruing to CMS
Below stop-loss attachment points 100% 0%
Above 1
st
attachment point 30% 70%
Above 2
nd
attachment point 20% 80%
Above 3
rd
attachment point 10% 90%

Updated 03/06/2022
63
6. Features of Payment Methodologies Specific to the Global Option
MSR/MLR
Provided that the KCE achieves the beneficiary minimums, no MSR or MLR will apply to aggregate
savings/losses for the Global Option. As such, KCEs will retain “first dollar” savings and be responsible
for “first dollar” losses.
Aggregate Savings/Losses Cap (Risk Corridor)
The aggregate amount of shared savings that KCEs will be eligible to receive if their actual Performance
Year expenditures are lower than their Performance Year benchmarks will be limited, or “capped” using a
series of caps that are set as a percent of the applicable Performance Year benchmark. Similarly, in the
event that KCEs generate shared losses, those shared losses will be capped, as shown in Table 17. KCEs
will be eligible to receive a portion of shared savings, or liable for a portion of shared losses, above each
threshold, with the portion decreasing with each threshold. The shared savings/shared losses caps will be
set at the following amounts:
Table 17. Series of Shared Savings and Losses Caps (Global Option)
Shared savings/loss cap as a %
of the Final Performance Year
Benchmark
Portion of savings/loss above
the cap accruing to the
KCE’s shared savings/losses
Portion of savings/loss above the
cap accruing to the CMS’
shared savings/losses
Under 25% of Benchmark 100% of savings/losses 0% of savings/losses
Gross Savings/Losses
Between 25% and 35%
50% of savings/losses 50% of savings/losses
Gross Savings/Losses
Between 35% and 50%
25% of savings/losses 75% of savings/losses
Gross Savings/Losses
Greater than 50%
10% of savings/losses 90% of savings/losses
Stop Loss Arrangement (Optional)
The purpose of the stop-loss arrangement is to reduce financial uncertainty associated with infrequent, but
high-cost, expenditures at the level of the individual aligned beneficiary. Stop-loss protects KCEs from
financial liability on individual beneficiary expenditures that are above the stop loss “attachment points.”
An attachment point is the dollar threshold in at which stop-loss protection begins. A portion of the
expenditures accrued above each attachment point and below the next highest attachment point will be
included in the KCE’s Performance Year expenditure calculations. The percent of expenditures for each
of the four attachment points will be 30%, 20%, and 10% respectively (See Table 18).
KCEs that choose the stop-loss arrangement are effectively charged for this protection. CMS will apply a
P
BPM stop loss “charge” to the KCE’s final Performance Year benchmark, which will be based upon the
percent of expenditures above each of the KCE’s attachment points in the baseline period.
Additional details will be provided in future methodology papers.

Updated 03/06/2022
64
Table 18. Stop Loss Attachment Points (Global Option)
Attachment Point Percent of
expenditures
accruing to KCE
Percent of
expenditures
accruing to
CMS
Below stop-loss attachment points 100% 0%
Above 1
st
attachment point 30% 70%
Above 2
nd
attachment point 20% 80%
Above 3
rd
attachment point 10% 90%
7. Aggregation
KCEs will generally have the opportunity to request one or more aggregation partners to form an
aggregation group for the purposes of meeting the minimum required numbers of aligned beneficiaries
with CKD Stages 4 or 5 and ESRD. If a KCE thinks it may be below the minimum beneficiary threshold
at the end of the Performance Year, then before the start of that Performance Year it may submit a request
identifying another KCE or KCEs of the same CKCC Option with which to aggregate its performance.
CMS will have sole discretion to approve, modify, or reject such requests. The process and requirements
for such aggregation groups are described in the Beneficiary Alignment section, above.
Beneficiaries who are aligned to KCEs in the same aggregation group will be grouped together for
pur
poses of calculating the financial performance and quality performance of the KCEs in the aggregation
group. For each KCE aggregation group, CMS will calculate aggregate Performance Year benchmarks
and Performance Year expenditures. CMS will compare the resulting aggregate performance
expenditures for a given aggregation group to its aggregate benchmarks to determine the overall savings
percentages for the aggregated group. For each KCE aggregation group, CMS will distribute aggregate
savings to each individual KCE based on its number of aligned beneficiaries contributing to the
aggregation group.
8. Final Reconciliation
The final reconciliation will take place following the end of the Performance Year, with a final settlement
t
arget date of July 31 of the calendar year following the Performance Year. This lag in the final
reconciliation is necessary in order to allow for claims run-out through March 31st of the calendar year
following the Performance Year and for CMS to incorporate final risk scores and to determine the KCE’s
quality score.
CMS will reconcile adjusted payments including the CKD QCP and AMCP, as part of final settlement, as
wel
l as any payments under the possible future optional TCC alternative payment mechanism (discussed
above).
9. Financial Assurances
KCEs participating in Graduated Level 2, Professional, and Global (i.e., those KCEs with downside risk)
m
ust establish one of the following financial guarantees in an amount and by a deadline specified by
CMS: an escrow account with an FDIC-insured institution, a surety bond from a company included on the

Updated 03/06/2022
65
U.S. Department of Treasury’s List of Certified Companies, or a line of credit at an FDIC-insured
institution. The amount of the financial guarantee varies by CKCC Option, as per the schedule below.
Table 19: Financial Guarantees by CKCC Option
CKCC Option Financial Guarantee Amount
(As a Percent of Performance Year
Benchmark)
CKCC Graduated
Level 1 N / A
Level 2 1.5%
CKCC Professional 2.5%
CKCC Global 3%
This guarantee should be in the form of funds placed in escrow, a line of credit, or a surety bond. To
permit CMS to recover funds using the guarantee, CMS will require the guarantee to remain in effect for
a period of time after final reconciliation is completed for each Performance Year. Specific requirements
for the financial guarantee will be specified in the CKCC Participation Agreement.
E. Quality Measures and Scoring
CMS will calculate Quality scores for KCEs based on their performance on a set of measures that indicate
ap
propriate clinical care and engagement for beneficiaries with CKD and ESRD aligned to KCEs. A
KCE’s overall Quality score will factor into the determination of payment under the Model.
Prior to the start of the Performance Year, CMS will identify relevant Quality measures, the patients to
which these respective measures will apply; data collection and reporting requirements; and the
methodologies for determining measure-specific scores and a KCE’s overall Quality score.
The measures currently included are:
•
Gains in Patient Activation (PAM) Scores at 12 Months; NQF #2483
•
Depression Remission at Twelve Months – Progress Towards Remission; NQF #1885
•
Optimal End Stage Renal Disease (ESRD) Starts; NQF #2594
CMS is engaged in develo
ping new performance measures specifically for the CKD and ESRD patient
population. If implemented, these measures – Standardized Mortality Ratio for Late Stage CKD and
ESRD and Delay in Progression of CKD – will be incorporated into KCEs’ quality scores starting in
PY2023 or in future Performance Years.
1. Performance Adjustments
The shared savings calculated for KCEs in Level 1 of the Graduated Option will reflect their quality
sco
re. KCEs in Graduated Level 1 will not be subject to a quality withhold.
For KCEs participating in Level 2 of the Graduated Option, 2.5% of the KCE’s trended, risk adjusted,
di
scounted Performance Year benchmarks will be withheld to incentivize strong quality measure
performance. For KCEs in the Professional or Global Options, 5% of the Performance Year benchmarks
will be withheld. The Performance Year benchmarks will be reduced but KCEs will have the opportunity
to earn back all or part of the amount withheld based on their quality score on the quality measure set for

Updated 03/06/2022
66
the applicable Performance Year. The amount of the quality withhold that the KCE earns back will be
calculated as a function of the KCE’s quality score on the quality measure set multiplied by the applicable
quality withhold percentage (e.g., a KCE in Professional Option with a 95% quality score will earn back
4.75% of its benchmark (= 95% quality score x 5% quality withhold). A KCE that achieves a full (100%)
quality score will earn back the entire quality withhold for the Performance Year.
Quality scores for KCEs participating as part of an aggregation group will be based on aggregated
measure performance across the KCEs in the group.
Additionally, we will test the use of a quality pool, the High Performers Pool, to further incentivize high
performance and continuous improvement on the quality measure set. KCEs in Graduated Level 2 and the
Professional and Global Options may earn a quality bonus if they meet a high level of performance on a
subset of quality measures. The High Performers Pool will be funded from 50% of the remaining amount
of the quality withhold that KCEs fail to earn back based on their performance on the quality measure set
in a given Performance Year. For example, a KCE in the Professional Option that earns back 4.75% of its
benchmarks contributes 0.125% of its benchmarks to the High Performers Pool (5% quality withhold
minus 4.75% earned back, divided by 2). As outlined in the CKCC Participation Agreement, a KCE’s
performance for purposes of the High Performers Pool will be based on meeting reporting requirements
for the survey measures, as well as achieving higher scores on a subset of the overall Quality measure set.
KCEs will be ranked on this High Performers score, with the top one-third qualifying for a bonus. The
total amount of the High Performers Pool will be allocated to these qualifying KCEs in accordance with
each KCE’s number of aligned beneficiaries.
F. Benefit Enhancements
Under section 1115A(d)(1) of the Act, the Secretary of Health and Human Services may waive such
requirements of Titles XI and XVIII and of sections 1902(a)(1), 1902(a)(13), 1903(m)(2)(A)(iii), and
certain provisions of section 1934 of the Act as may be necessary solely for purposes of carrying out
section 1115A with respect to testing models described in section 1115A(b). CMS has found that it is
necessary for purposes of testing the CKCC Options to waive certain provisions of the Medicare statute
and regulations. As a result of these waivers, participating KCEs can choose to make certain additional
benefits available to their aligned beneficiaries during the performance period of the Model. These
additional benefits are referred to as benefit enhancements. CMS anticipates that the following benefit
enhancements will be available for PY2023:
Table 20. Benefit Enhancements
Name Description
3-Day Skilled Nursing
Facility Rule
CMS will make available to qualified KCEs a conditional waiver of the
three-day inpatient hospital stay requirement prior to admission to a SNF
or acute-care hospital or Critical Access Hospital (CAH) with swing-bed
approval for SNF services (Swing-Bed Hospital). This benefit
enhancement will allow eligible beneficiaries to receive Medicare-covered
SNF services from qualified SNFs or Swing-Bed Hospitals that are KCE
Participants or Preferred Providers either directly or with an inpatient stay
of fewer than three days.

Updated 03/06/2022
67
Name Description
3-Day Skilled Nursing
Facility Rule (continued)
A beneficiary aligned to a KCE will be eligible to receive covered
services under the terms of this benefit enhancement if the beneficiary: (1)
is aligned to the KCE at the time of admission to a qualifying SNF or
Swing-Bed Hospital or within a specified grace period; (2) has Medicare
as the beneficiary’s primary payer; (3) is enrolled in the part of Medicare
FFS under which the SNF Services will be reimbursed at the time of
admission to the SNF or Swing-Bed Hospital; (4) does not reside in a SNF
or long-term care facility at the time of the admission to the SNF or
Swing-Bed Hospital; and (5) meets all other CMS criteria for SNF or
swing-bed hospital admission, including that the beneficiary must:
•
Be medically stable;
•
Has been evaluated by a physician or other practitioner licensed to
perform the evaluation within three days prior to admission to the
Eligible SNF;
•
Have confirmed diagnoses (i.e., , does not have conditions that require
further testing for proper diagnosis);
•
Not require inpatient hospital evaluation or treatment; and
•
Have an identified skilled nursing or rehabilitation need that cannot be
provided on an outpatient basis or through home health services.
KCEs will identify the SNFs and Swing-Bed Hospitals with which they
w
ill partner for purposes of this benefit enhancement. Partner SNFs and
Swing-Bed Hospitals may be either KCE Participants or Preferred
Providers. Through the application and an implementation plan, KCEs that
select to offer this benefit enhancement will be asked to describe how the
identified KCE Participants and Preferred Providers have the appropriate
staff capacity and necessary infrastructure to carry out proposed
coordination activities. In addition to the information the KCE includes in
its implementation plan, a SNF or Swing-Bed Hospital must have an
overall rating of three or more stars under the CMS 5-Star Quality Rating
System in at least seven of the previous twelve months, as reported on the
Nursing Home Compare website to furnish SNF services under this benefit
enhancement. This star standard is subject to change in response to
changes in the scoring methodology.

Updated 03/06/2022
68
Name Description
Kidney Disease
Education Benefit
Enhancement
Medicare currently covers up to six 1-hour sessions of KDE services for
beneficiaries that have CKD Stage 4. While the KDE benefit is intended
to ensure beneficiaries are informed about the effects and treatment of
kidney disease, diet and nutrition, transplantation, dialysis modalities, and
vascular access, the uptake of this service has been exceptionally low at
less than two percent of eligible patients. In the KCC Model, beneficiary
education is a crucial component of increasing rates of transplants and
home dialysis and delaying the onset of ESRD. Therefore, CMS will
make available to KCEs a conditional waiver of certain KDE requirements
as necessary to test ways to increase the provision of the KDE benefit
under the KCC Model.
The programmatic waivers would:
• Waive the requirement that the KDE be performed by a physician,
physician assistant, nurse practitioner, or clinical nurse specialist to
allow certain additional types of clinical staff to furnish KDE services
incident to the services of a nephrologist who is a KCE Participant or
Preferred Provider.
• Waive the requirement that a beneficiary have Stage 4 CKD in order
to test furnishing the KDE benefit to beneficiaries with CKD Stage 5
and those in the first 6 months of starting dialysis, who can also
benefit from KDE.
• Waive the requirement that the content of KDE services include the
management of comorbidities, including for the purpose of delaying
initiation of dialysis, to allow participating nephrologists to cover this
topic only where relevant to a beneficiary, as delaying dialysis would
not be relevant to beneficiaries with ESRD who have already begun
dialysis.
• Waive the requirement that an outcomes assessment designed to
measure beneficiary knowledge of chronic kidney disease and its
treatment be conducted during one of the KDE sessions, provided that
such an assessment is administered by a qualified person (as that term
is defined under 42 CFR 410.48(a)) within one month of a
beneficiary’s final KDE session.

Updated 03/06/2022
69
Name Description
Telehealth Benefit
Enhancement
CMS will make available to qualified KCEs a conditional waiver of the
interactive telecommunications system requirement under section
1834(m)(1) of the Act and 42 CFR 410.78(b) for otherwise covered
dermatology and ophthalmology services furnished using asynchronous
store and forward technologies. Asynchronous telehealth includes the
transmission of recorded health history (for example, retinal scanning and
digital images) through a secure electronic communications system to a
practitioner, usually a specialist, who uses the information to evaluate the
case or render a service outside of a real-time interaction. Asynchronous
telecommunication systems in single media format do not include
telephone calls, images transmitted via facsimile machines, and text
messages without visualization of the patient (electronic mail).
Photographs must be specific to the patients’ condition and adequate for
rendering or confirming a diagnosis or treatment plan.
Payment will be permitted for dermatology and ophthalmology services
fu
rnished to eligible beneficiaries using asynchronous telehealth in single
or multimedia formats that is used as a substitute for an interactive
telecommunications system. Distant site practitioners will bill for these
services using CMMI specific asynchronous telehealth codes. The distant
site practitioner must be a KCE Participant or Preferred Provider who has
elected to participate in this benefit enhancement.
CMS will also waive the rural geographic component of originating site
requirements, allow the originating site to include a beneficiary’s home,
and waive the originating site fee requirement when the beneficiary’s
home serves as the originating site for telehealth services furnished to an
eligible beneficiary by a Preferred Provider approved to participate in the
Benefit Enhancement.
The Bipartisan Budget Act of 2018 added Section 1899(l) of the Social
S
ecurity Act, which affords the same flexibilities with respect to the
originating site requirements for telehealth services furnished to an eligible
beneficiary by a physician or practitioner participating in an accountable
care organization in a two-sided model tested or expanded under section
1115A of the Act for which Medicare FFS beneficiaries are assigned to the
accountable care organization using a prospective assignment method.
KCEs in the Graduated Level 2 Option, Professional Option, or Global
Option will be considered accountable care organizations meeting these
criteria, meaning that that physicians and practitioners who are KCE
Participants in such KCEs may receive payment for telehealth services
furnished to the KCE’s aligned beneficiaries without the need for CMS to
issue a waiver of applicable Medicare requirements.

Updated 03/06/2022
70
Name Description
Telehealth Benefit
Enhancement (continued)
Because KCEs participating in the one-sided Graduated Level 1 Option
are not applicable ACOs for purposes of section 1899(l) of the Act, CMS
will also issue a conditional waiver of the originating site requirements for
synchronous telehealth services furnished to eligible beneficiaries by KCE
Participants in KCEs in the Graduated Level 1 Option that select and are
approved to offer the Telehealth Benefit Enhancement.
CMS will make available to qualified KCEs participating in the one-sided
Graduated Level 1 Option a conditional waiver of the following
requirements with respect to otherwise covered telehealth services
furnished by an Eligible Telehealth Provider to a KCE Beneficiary when
furnished in accordance with the CKCC PA :
1. Waiver of Originating Site Requirements. CMS waives the
requirements in Section 1834(m)(4)(C) of the Act and 42 CFR §
410.78(b)(3)–(4) with respect to telehealth services furnished in
accordance with the CKCC PA.
2. Waiver of Originating Site Requirement in the Eligible Telehealth
Individual Provision. CMS waives the requirement in Section
1834(m)(4)(B) of the Act that telehealth services be “furnished at
an originating site” when the services are furnished in accordance
with the CKCC PA.
3. Waiver of Originating Site Facility Fee Provision. CMS waives
the requirement in Section 1834(m)(2)(B)(ii) of the Act and 42
CFR § 414.65(b)(3) with respect to telehealth services furnished to
a Beneficiary at his/her home or place of residence when furnished
in accordance with the CKCC PA.

Updated 03/06/2022
71
Name Description
Post-Discharge Home
Visits Benefit
Enhancement
CMS will make available to KCEs a conditional waiver of certain
supervision requirements in order to allow payment for certain home visits
to eligible, non-homebound beneficiaries when such home visits are
furnished “incident to” a physician (or other practitioner’s) professional
services by “auxiliary personnel” as defined in 42 CFR §410.26(a)(1),
under the general supervision (instead of direct supervision) of a physician
or other practitioner who is a KCE Participant or Preferred Provider.
Payment for these home visits will only be allowed when the visits are
furnished following the beneficiary’s discharge from an acute inpatient
hospital, inpatient psychiatric facility, inpatient rehabilitation facility,
long-term care hospital, or skilled nursing facility. The beneficiary must
not qualify for Medicare coverage of home health services (or qualifies for
Medicare coverage of home health services on the sole basis of living in a
medically underserved area). Further, a beneficiary would not be eligible
to receive covered home visits under this Benefit Enhancement if they are
receiving services under the Home Health Homebound Waiver Benefit
Enhancement.
Also, under this benefit enhancement, a beneficiary is eligible to receive
up to nine post-discharge home visits within 90 days following discharge.
The nine home visits do not accumulate across multiple discharges; if the
beneficiary is admitted within 90 days of the initial discharge and before
receiving nine home visits, the beneficiary may receive only nine home
visits in connection with the subsequent discharge.

Updated 03/06/2022
72
Name Description
Home Health
Homebound Waiver
Benefit Enhancement
Currently, to receive Medicare reimbursement for home health care
services, a Medicare beneficiary must be homebound as required by
§1814(a)(2)(C) and §1835(a)(2)(a). CMS guidance (Medicare Benefit
Policy Manual, Chapter 7, Section 30.1.1) states that:
1) The beneficiary either (a) must need the assistance of a supportive
device, special transportation, or another person to leave their residence
OR (b) have a condition that makes leaving his or her home medically
contraindicated; and
2) There must be a normal inability to leave the home AND leaving
hom
e must require a considerable and taxing effort.
The current homebound requirement focuses on a beneficiary’s functional
l
imitations rather than the underlying health condition or comorbidities
often present in this population. Unless homebound status is certified,
skilled nursing care services in the home are not reimbursable by Medicare
for a beneficiary residing in their home.
This benefit enhancement targets those beneficiaries with multiple chronic
c
onditions who are at risk of an unplanned inpatient admission using
different criteria than in Medicare law today. Specifically, to qualify for
home health services under this waiver, beneficiaries must (1) otherwise
qualify for home health services under 42 C.F.R. § 409.42 except that the
beneficiary is not required to be confined to the home; and (2) meet the
eligibility criteria as defined by CMS, including having at least two
chronic conditions as well as one of the three following indicators:
inpatient service utilization, frailty, and/or social isolation. CMS will
provide the KCE with a template form for purposes of documenting these
criteria (“Home Health Homebound Waiver Form”). The KCE shall
ensure that a completed and certified “Home Health Homebound Waiver
Form” is maintained in the beneficiary’s medical records.
A beneficiary would not be eligible to receive covered home health
ser
vices under this benefit enhancement if they are receiving services
under the Post-Discharge Home Visits Benefit Enhancement. KCEs
participating in this benefit enhancement will identify home health
providers that are KCE Participants or Preferred Providers who would
offer these services to eligible beneficiaries. KCE Participants and
Preferred Providers will use the criteria described above, as well as their
own clinical judgement to determine if a beneficiary is eligible and would
benefit from receiving home health services under the benefit
enhancement. All other requirements regarding Medicare coverage and
payment for home health services would continue to apply. The services
would be furnished in the beneficiary’s home or place of residence during
the certified episode of care period.

Updated 03/06/2022
73
Name Description
Concurrent Care for
Beneficiaries that Elect
the Medicare Hospice
Benefit
CMS will make available to KCEs a conditional waiver of the requirement
that beneficiaries who elect the Medicare Hospice Benefit give up their
right to receive curative care (sometimes referred to as “conventional
care”) as a condition of electing the hospice benefit. All expenditures
incurred by Medicare on behalf of such beneficiaries, whether for hospice
or other non-hospice services would be included as part of expenditure for
the relevant Performance Year.
Similar to the operation of the 3-Day Skilled Nursing Facility Rule
Wa
iver, KCEs will identify the KCE Participants or Preferred Providers
with which they will partner in this Benefit Enhancement. Medicare will
retain its existing claims-based edits to prevent non-hospice claims from
processing while a beneficiary is under hospice election, except with
respect to services furnished by those hospice and non-hospice providers
and suppliers identified by the KCE as participating in this Benefit
Enhancement. Medicare FFS claims submitted by these organizations will
be paid by Medicare if they are otherwise appropriate for payment absent
the restrictions on paying claims for a beneficiary that has elected hospice.
For purposes of this payment waiver, a KCE may not partner with any
h
ospice that has existing condition level deficiencies that have not been
remediated, and all hospices an entity partners with must readily offer
beneficiaries access to the four levels of hospice consistent with clinical
need.
G. Beneficiary Engagement Incentives
General
Except as permitted by applicable law and the CKCC Participation Agreement, KCEs, KCE Participants,
Preferred Providers, and other individuals or entities performing functions and services related to KCE
activities are prohibited from providing gifts or other remuneration to beneficiaries to induce them to
receive items or services from the KCE, KCE Participants, or Preferred Providers, or to induce them to
receive or to continue to receive items or services from the KCE, KCE Participants, or Preferred Providers.
During a Performance Year , KCEs, KCE Participants, Preferred Providers, and other individuals or entities
performing functions or services related to KCE activities will be permitted to furnish certain in-kind
incentives described below in accordance with requirements set forth in the CKCC Participation
Agreement. In addition, a KCE may elect to offer the Cost-Sharing Support for Part B Services Beneficiary
Engagement Incentive, the Chronic Disease Management Reward Program Beneficiary Engagement
Incentive, or both (each, a “Beneficiary Engagement Incentive”).
In-kind Incentives
CMS believes that beneficiary engagement is an important part of encouraging more active participation
b
y beneficiaries in their health care. Beneficiary engagement and coordination of care could be enhanced
by providing certain in-kind incentives to beneficiaries that would potentially encourage beneficiaries to
become actively involved in their care. Subject to compliance with all applicable laws and regulations and
the terms of the CKCC Participation Agreement, KCEs, KCE Participants, Preferred Providers, and other
Updated 03/06/2022
74
individuals or entities performing functions or services related to KCE activities will be permitted to provide
in-kind items or services to beneficiaries, if the following conditions are satisfied:
1. There is a reasonable connection between the items or services and the medical care of the beneficiary;
2. The items or services are preventive care items and services or advance a clinical goal for the
b
eneficiary, including adherence to a treatment regime (including prescribed medication), adherence to
a follow-up care plan, or management of a chronic disease or condition;
3. The in-kind item or service is not a Medicare-covered item or service for the beneficiary on the date
th
e in-kind item or service is furnished to that beneficiary (for purposes of this exception, an item or
service that could be covered pursuant to a Benefit Enhancement is considered a Medicare-covered
item or service, regardless of whether the KCE selects to participate in such Benefit Enhancement for
a given Performance Year); and
4. The in-kind item or service is furnished to a Beneficiary directly by the KCE, a KCE Participant, or a
Preferred Provider.
KCEs, KCE Participants, and Preferred Providers would pay for in-kind incentives from their own funds
a
nd at their discretion. Calculation of the KCE’s benchmark and Performance Year expenditures will not
account for any of these items or services.
1. Part B Cost-Sharing Support Beneficiary Engagement Incentive
Subject to compliance with all applicable laws and regulations, the terms of the CKCC Participation
A
greement, and CMS approval, a KCE may select to participate in the Part B Cost-Sharing Support
Beneficiary Engagement Incentive. Under the terms of the CKCC Participation Agreement, a KCE that
selects this option must enter into a cost sharing support arrangement with its KCE Participants and
Preferred Providers, pursuant to which the KCE Participants and Preferred Providers would not collect
beneficiary cost sharing amounts (in whole or in part) from categories of aligned beneficiaries and for
categories of Part B services (excluding prescription drugs and durable medical equipment, prosthetics,
orthotics, and supplies) identified by the KCE. KCEs would then make payments to those KCE Participants
and Preferred Providers to cover some or all of the amount of beneficiary cost sharing not collected. The
principal aim of allowing KCEs to offer this cost sharing support is to reduce financial barriers so that
certain beneficiaries may obtain needed care and better comply with treatment plans, thereby improving
their own health outcomes. In addition, permitting KCEs this flexibility will provide a critical tool to engage
aligned beneficiaries, promote the utilization of high-value services, and incentivize aligned beneficiaries
to continue receiving their care from KCE Participants and Preferred Providers.
KCEs that select to offer cost sharing support for Part B Services will be required to enter into a cost sharing
support arrangement with those KCE Participants and Preferred Providers who will participate in this
Beneficiary Engagement Incentive. The KCE will also be required to identify the categories (e.g., subset)
of beneficiaries, types of Part B services, or both, for which cost sharing support will be provided in an
Implementation Plan that the KCE submits to CMS. KCEs will be permitted to specify both primary care
and specialty care services for this cost sharing support so that beneficiaries with specialty needs may also
be incented to obtain the care they need. To the extent the KCE will not be paying the cost of the cost
sharing support entirely, the KCE will also be required to specify in its Implementation Plan how it will
determine the relative contributions of the KCE and the KCE Participants and Preferred Providers. Cost
sharing support payments must come only from the KCE and, if applicable, its KCE Participants and
Preferred Providers. Participating KCEs will be subject to monitoring and compliance activities in
connection with the use of cost sharing support. To minimize possible abuse of this Beneficiary
Updated 03/06/2022
75
Engagement Incentive, CMS will incorporate certain beneficiary protections and other safeguards into the
CKCC Participation Agreement.
2. Chronic Disease Management Reward Beneficiary Engagement Incentive
Subject to compliance with all applicable laws and regulations, the terms of the CKCC Participation
Ag
reement, and CMS approval, an KCE may select to offer a Chronic Disease Management Reward
Beneficiary Engagement Incentive. Under this option, an KCE may provide gift cards to eligible aligned
beneficiaries, up to an annual limit of $75, for the purpose of incentivizing participation in a chronic disease
management program. Use of modest beneficiary incentives and rewards – such as gift cards – has been
widely adopted by a variety of payers to influence healthy behaviors. KCEs will pay for the gift cards out
of their own funds and at their discretion, subject to certain conditions. We believe that allowing KCEs to
incentivize beneficiary participation in a chronic disease management program will promote beneficiary
self-management, and ultimately improve quality and reduce costs.
KCEs that elect to offer a Chronic Disease Management Reward Beneficiary Engagement Incentive will
be
required to submit an Implementation Plan detailing how they will structure their program. KCEs will
be permitted to offer programs that focus on aligned beneficiaries with a specific disease or chronic
condition, as long as the program does not discriminate against any aligned beneficiary who would
otherwise qualify for participation. KCEs that elect to offer a Chronic Disease Management Reward
Beneficiary Engagement Incentive will be required to maintain records of their reward program, including
documentation of the amount and type of each gift card awarded and the basis for beneficiary eligibility.
Participating KCEs will be subject to monitoring and compliance activities in connection with their reward
program. To minimize possible abuse of this Beneficiary Engagement Incentive, we will incorporate certain
beneficiary protections and other safeguards into the CKCC Participation Agreement.
H. Termination
CMS reserves the right to terminate a KCE’s CKCC Participation Agreement at any point during the
Ag
reement performance period for reasons associated with poor performance, program integrity issues,
non-compliance with the terms and conditions of the CKCC Participation Agreement, or if otherwise
specified in the Participation Agreement or required by section 1115A(b)(3)(B) of the Social Security
Act.
To determine whether KCEs can succeed in improving quality and reducing costs over a longer period of
tim
e, KCEs will be expected to participate in the Model for at least two performance years. However,
KCEs may terminate their Participation Agreement and exit the Model by providing notice to CMS
specifying an effective date of termination that is at least 30 days following the date of the notice. KCEs
may terminate the Participation Agreement by giving notice to CMS by February 28, 2023 with an
effective date of termination of the Participation Agreement that is no later than March 30, 2023. A KCE
that submits a notice of termination for PY2023 to CMS after February 28, 2023, or with an effective date
of termination that is on or after March 31, 2023 will be subject to financial reconciliation for the full
Performance Year. Such KCEs will be responsible for shared losses but will not be eligible for shared
savings if their effective date of termination is on or before December 30, 2023. In order to incentivize
continued participation from PY2023 to PY2024, a KCE that voluntarily terminates its participation for
the second Performance Year before February 28, 2024 will be subject to a retention withhold in the
amount of an additional 1% discount applied to both the KCE’s CKD and ESRD Performance Year
Benchmarks. If the KCE’s Participation Agreement remains in effect by this date for PY2024, the 1%
retention withhold will not be applied to the KCEs CKD or ESRD benchmarks for PY2023.

Updated 03/06/2022
76
I. Application for CKCC Option
1. Instructions
Potential KCEs interested in participating in the CKCC Options must file an application by no later than
March 25, 2022 at 11:59pm. To file an application, applicants must fill out and complete the Qualtrics
Form available here.
CMS reserves the right to request additional information (interviews, site visits, or additional information
related to application responses) from applicants in order to assess their applications.
Applicants seeking to withdraw their application must submit an electronic withdrawal request to CMS
be
fore the distribution of the CKCC Participation Agreements via the following mailbox: KCF-CKCC-
RFA-[email protected].gov. The request must be submitted as a PDF on the organization’s letterhead and
must be signed by an authorized corporate official authorized to bind the applicant. It should include: the
applicant organization’s legal name; the organization’s primary point of contact; the full and correct
address of the organization; and a description of the nature of the withdrawal.
Applications will be screened to determine eligibility for further review. Screening will include the
c
riteria detailed in this RFA and applicable law and regulations, including 2 CFR Parts 180 and 376. In
addition, CMS may deny selection to an otherwise qualified applicant on the basis of information found
during a program integrity (PI) review of the applicant, its KCE Participants, Preferred Providers, or any
other relevant individuals or entities. CMS may also deny individual KCE Participants or Preferred
Providers or any other relevant individual or entity participation in the CKCC Options based on the
results of a PI review. Adverse results from PI review may relate to issues with Medicare billing
privileges, outstanding Medicare debt, or current administrative review or investigation by CMS or other
federal government agencies. (Please see Section II.C of this document for full details on adverse results.)
Applicants will be required to disclose any investigations of, or sanctions that have been imposed on the
a
pplicant or individuals in leadership positions within the applicant in the last three years by an
accrediting body or state or federal government agency. Individuals in leadership positions include key
executives who manage or have oversight responsibility for the organization, its finances, personnel, and
quality improvement, including without limitation, a CEO, CFO, COO, CIO, medical director,
compliance officer, or an individual responsible for maintenance and stewardship of clinical data.
2. Application Template for the CKCC Options
It is important to note that applicants to the CKCC Options will not be expected to have their legal entity
formed until after application selection and prior to the finalization of the CKCC Participation
Agreement. KCEs should include a description of the providers and suppliers that they will include in
their KCE application as potential KCE Participants and Preferred Providers. However, for accepted
applicants, there will be a later opportunity to submit detailed information about KCE Participants and
Preferred Providers.
Questions about the application should be directed to KCF-CKCC-RFA @cms.hhs.gov
.
Section A – Applicant Information and Eligibility
1. Applicant Information (Required)
•
KCE Applicant Legal Business Name:
•
KCE Applicant Tax Identification Number (TIN):
Updated 03/06/2022
77
• Dialysis Organization with ownership interest in participant dialysis facility/facilities (if
applicable):
• Mailing Address (Street, City, State, Zip Code):
2. What is the composition of Provider/Supplier types expected to participate in the KCE as KCE
Participants and Preferred Providers (select all that apply):
Nephrologist(s)/ Nephrology practice(s) (required)
Dialysis facilities
Hospital(s)
Transplant Center(s)
Transplant Surgeon(s)
Organ Procurement Organization(s)
Rural Health Clinic(s)
Nursing Home(s)
Other Medicare-enrolled provider(s) and supplier(s): (Please
specify)_________________________________________________________
3. Please provide the following contact information for the KCE Applicant’s Executive Contact. Please
note the Applicant’s Executive Contact must have the authority to act as the Applicant’s authorized
corporate official.
• Name
• Organizational Title
• Phone Number
• Email Address
4. Please provide the following contact information for the KCE Applicant’s Primary Contact.
• Name
• Organizational Title
• Phone Number
• Email Address
5. Please provide the following contact information for the KCE Applicant’s Secondary Contact.
• Name
• Organizational Title
• Phone Number
• Email Address
6. Did any of the individuals or entities expected to participate in the KCE as KCE Participants and
Preferred Providers participate in the Comprehensive ESRD Choices (CEC) Model or are any of
these individuals or entities currently participating in the KCC Model?
Yes
No
If so, please describe the nature of their participation (e.g. participant, participant owner, provider/supplier
etc.) ___________
Updated 03/06/2022
78
7. Please indicate if any of the individuals or entities expected to participate in the KCE as KCE
Participants and Preferred Providers have participated or are currently participating in any of the
following:
Accountable Health Communities
ACO Investment Model
Advance Payment ACO Model
Bundled Payments for Care Improvement
Bundled Payments for Care Improvement Advanced
Comprehensive Care for Joint Replacement
Comprehensive ESRD Care Model
Comprehensive Primary Care Initiative
Global and Professional Direct Contracting (GPDC) Model
Independence at Home Demonstration
Maryland All-Payer Model
Maryland Total Cost of Care Model
Medicare Care Choices Model
Medicare Shared Savings Program
Next Generation ACO Model
Oncology Care First
Oncology Care Model
Pioneer ACO Model
Private, For-Profit Demo Project for the Program of All-Inclusive Care for the Elderly
(PACE)
State Innovation Models Initiative
Transforming Clinical Practice Initiative
Other: (Please Specify)
Not Applicable
8. Please describe the Applicant’s performance under prior or current outcomes-based contracts, if any.
Outcomes-based contracts must include: (1) financial accountability; (2) evaluation of patient
experiences of care; and (3) substantial quality performance incentives. If applicable, please include
performance under CMS programs, and demonstrations, and models that meet the definition of
outcomes-based contracts. Please keep responses to a maximum of approximately 1000 words.
9. I certify that my organization is a recognized legal entity formed under applicable state, federal, or
tribal law and authorized to conduct business in each state in which it operates or will be by the time
the CKCC Participation Agreement is signed.
Yes
By selecting YES, you certify that your legal entity can, or will be able to:
a) Receive and distribute shared savings;
b) Repay shared losses or other monies determined to be owed to CMS;
c) Establish, report, and ensure provider compliance with health care quality criteria,
i
ncluding quality performance standards; and
10. Please provide an executive summary describing the Applicant. This includes: the Applicant’s
history, mission, and organization, including the Applicant’s affiliations; the Applicant’s:

Updated 03/06/2022
79
composition, including the number of hospitals, number of skilled nursing facilities, types of
providers/suppliers (primary care and types of specialists); the Applicant’s geographic service area,
including the geographic area where most of the Applicant's patients reside; whether the Applicant’s
service area encompasses urban, suburban, and/or rural locations; whether the Applicant’s service
area includes underserved beneficiaries; and whether the Applicant will contract with other
community-based organizations (e.g., care management organization, ESRD networks, quality
improvement organization, etc.). Please include any other applicable narrative describing the
Applicant. Please keep responses to a maximum of approximately 500 words.
11. Please describe the nephrologists and nephrology professionals whom the Applicant expects to
partner with your organization as KCE Participants under the CKCC Options, including the number
of clinical and non-clinical care providers and their roles. Please note that Applicant will have a
later opportunity to provide CMS with updated information regarding its KCE Participants and
Preferred Providers.
12. If applicable, please identify investments or credit lines from outside the Applicant organization or its
individual or corporate owners, and provide details about the funding relationship, including (1) the
individual or corporate identity of the funder; (2) the month and year the funding relationship was
established and how long the funding is secured or guaranteed; (3) a summary of the bankruptcy
history of the funders; and (4) the ownership interest, if any, between the Applicant organization or
any expected KCE Participant or Preferred Provider and each outside funder.
Mechanism Funder (LBN,
TIN)
Date established and
length
secured/guaranteed
Bankruptcy
history of
funder
Ownership
interest
Bank loan/credit
line
Blank Blank Blank Blank
Angel investor
Blank Blank Blank Blank
Private equity
Blank Blank Blank Blank
Venture capital
Blank Blank Blank Blank
IPO
Blank Blank Blank Blank
SPAC
Blank Blank Blank Blank
Other
Blank Blank Blank Blank
13. To assist the Federal Trade Commission (FTC) and the Antitrust Division of the Department of
Justice (DOJ) in their activities to protect competition in the regions in which the KCC Model will
be tested, CMS may provide certain information, including aggregate claims data regarding allowed
charges and fee-for-services payments for your organization, to FTC and the Antitrust Division of
DOJ to assist in their monitoring of the competitive effects of potential KCC Entities in these
regions. Please confirm that you understand and agree that CMS may also share a copy of your
application (including all information and documents submitted with the application) with the FTC
and the Antitrust Division of the DOJ. You must select ‘Yes’ in order to proceed with the
application.
o
Yes
o
No

Updated 03/06/2022
80
Section B – Organizational Structure, Leadership and Management, and Governance Structure
14. Please provide a proposed organizational chart for the Applicant. It should depict the legal structure
a
nd governing body, the proposed composition of the Applicant, and any relevant committees (2
pages maximum).
15. Please complete the table below with information specific to the Applicant’s proposed leadership
team. The leadership team may include, but is not limited to: key executives, finance, clinical
improvement, compliance officers, information systems leadership, and the individual responsible for
maintenance and stewardship of clinical data. If specific individuals have not yet been identified,
please note that in the Name column and provide an anticipated date by which the individual will be
identified. Please also include a brief description of the responsibilities associated with that each
position/role.
Name Practice/ Leadership Team
Position/Role
Responsibilities
Blank Blank Blank
Blank Blank Blank
16. By checking the box below, you attest that your compliance plan will identify a compliance officer,
who must not be legal counsel to the applicant, must not be in a direct reporting relationship to legal
counsel for the Applicant, and must report directly to the Applicant’s governing body, and that the
compliance plan will include a description of the following:
•
A quality assurance strategy that, at the very least, includes a peer review process to
investigate cases of potentially suboptimal care;
•
The internal process for addressing a request for corrective action plan (CAP) by CMS and a
description of the supplier termination circumstances;
•
The remedial processes that apply when participating nephrologists fail to comply with the
CKCC Participation Agreement, Medicare regulations, and/or internal procedures and
performance standards including correction action plans (CAPs) and circumstances for
termination; and,
•
An antitrust compliance plan sub-section that describes appropriate firewalls, or other
safeguards against, improper exchanges of prices or other competitively sensitive information
among competing participant that could facilitate collusion and reduce competition in the
provision of services outside the Applicant organization.
•
Compliance training programs for the KCE nephrology professionals.
•
A method for KCE nephrology professionals to anonymously report suspected problems
related to the Applicant organization to the compliance officer.
•
A requirement for the Applicant to report probable violations of law to an appropriate
law enforcement agency.
•
The Applicant’s compliance plan must be in compliance with all applicable laws and
regulations and be updated periodically to reflect changes in those laws and regulations.
I attest that my compliance plan will meet the listed criteria. I further certify that the
information contained within the compliance plan will be true and correct and that the
compliance plan will be in compliance with all applicable laws and regulations and be
updated periodically to reflect changes in those laws and regulations.
Updated 03/06/2022
81
Section C – Financial Payment Options, Financial Guarantee
17. Please identify the CKCC Option that the Applicant is selecting in this application.
The CKCC Graduated Option
The CKCC Graduated Option: Level 1 (one-sided model risk, i.e., shared
savings only; this option will automatically glide to the Level 2 of the
Graduated Option in the following Performance Year. Applicant may elect to
participate in a CKCC Option with increased risk (Professional or Global) in
subsequent performance years.)
The CKCC Graduated Option: Level 2 (transition to risk; two-sided risk; this
option will automatically glide to the Professional Option in the following
Performance Year. KCE may elect to participate in the Global Option in
subsequent performance years.)
The CKCC Professional Option (two-sided model risk; 50% symmetrical shared
savings/losses)
The CKCC Global Option (two-sided risk option; 100% shared savings/losses)
Section D – Community Engagement
18. Please describe the history of collaboration among major stakeholders in the community(ies) being
served and commitment from relevant community stakeholders to achieve seamless and
comprehensive care. Please include specific examples of community stakeholders with whom the
Applicant has a relationship and the nature of each relationship. Please keep responses to a
maximum of approximately 500 words.
Section E – Care Model Patient Centeredness
19. Please provide a narrative explanation of 1) why the Applicant wishes to participate in one of the
CKCC Op
tions and how the Applicant will achieve the goals of better health and better care for
Medicare beneficiaries with CKD, ESRD and kidney transplants? Please keep responses to a
maximum of approximately 500 words.
20. Please provide a narrative description of the Applicant’s plan for engaging with CKD and ESRD
beneficiaries and their caregivers. At a minimum, please address the following:
a. Managing the progression of CKD
b. Modality options and transition onto dialysis
c. Coordination of care with different providers and suppliers
d. Transplant process and managing post-transplant care
e. Health I.T. and data sharing
f. Prescription drug utilization
g. Shared decision-making, self-management and self-care skill development
Please keep responses to a maximum of approximately 1000 words.
21. Please describe the Applicant’s historical and planned population health management and/or
population health tools. If applicable, please describe the metrics the Applicant has historically or

Updated 03/06/2022
82
plans to use to understand how to deploy clinicians, invest resources, and generally improve health
equity in managing the Applicant’s attributed beneficiary population. At a minimum, please address
the following:
a. Experience with social determinants of health (e.g., access to transportation, housing stability,
food security, income) and furnishing care to underserved communities
b. Managing care for dually eligible beneficiaries
c. Metrics used for identifying health inequities in patients served
d. Processes used to make improvements to address and mitigate identified health disparities
8
e. Decision support tools for use by providers/suppliers and/or patients/caregivers, and any tools
or approaches for fostering what might be termed “health literacy” in patients and their
families.
f. Processes for ensuring that the Applicant provides culturally-competent care
g. Approaches for providing high-quality-care to patients who do not speak English or for
whom English is a second language.
Please keep responses to a maximum of approximately 1000 words.
Section F – Attestation and Signature
I have read the contents of this application. By my signature, I certify to the best of my knowledge,
information, and belief that the information contained herein is true, correct, and complete, that I am
authorized to sign this application on behalf of the Applicant. I understand that the applicant must not
engage in anti-competitive practices, and if it has engaged in such practices, it may not get accepted into
the Model. If accepted into the Model, I understand that CMS can rescind the offering of a Participation
Agreement or terminate the Participation Agreement if it is determined that the applicant has engaged in
anti-competitive practices. I authorize the Centers for Medicare & Medicaid Services (CMS) to verify this
information. If I become aware that any information in this application is not true, correct, or complete, I
agree to notify CMS of this fact immediately and to provide the correct and/or complete information.
____________
Printed Name of Applicant Executive Contact Date
____________
Signature of Applicant Executive Contact Date
8
Any race or ethnicity-conscious strategies must be supported by specific data or other information demonstrating a need for the
race or ethnicity-conscious strategy, and must demonstrate a close fit between disparities and the race or ethnicity-conscious
action that the Applicant intends to take. Additionally, any race or ethnicity-conscious strategies should be supported by
information demonstrating that alternative strategies that do not involve race or ethnicity will not be sufficient or effective to
address this disparity.

83
V. Appendix A: Glossary of Key Definitions
Term Definition
ACO Accountable Care Organization - ACOs are groups of doctors, hospitals, and other
health care providers, who come together voluntarily to give coordinated high-quality
care to their Medicare patients.
ACO REACH Accountable Care Organization Realizing Equity, Access, and Community Health
Model
Advanced APM An APM that CMS determines meets the criteria set forth in 42 CFR 414.1415.
AMCP Adjusted Monthly Capitation Payment
APM Alternative Payment Model - As defined in 42 CFR 414.1305, an APM is any of the
following: (1) a model under section 1115 of the Social Security Act (Act) (other than
a health care innovation award); (2) the shared savings program under section 1899 of
the Act; (3) a demonstration under section 1866(C) of the Act; (4) a demonstration
required by federal law. APMs can apply to a specific clinical condition, a care
episode, or a population.
Beneficiary A Medicare beneficiary who has been aligned to the KCF Practice or KCE according
to the alignment methodology detailed above.
BY Base year - The three years prior to the start of the CKCC Options. BY1, BY2, and
BY3 correspond to calendar years 2017, 2018, and 2019, respectively.
CAP Corrective Action Plan
CBSA Core-Based Statistical Area - A core-based statistical area is a U.S. geographic area
defined by the Office of Management and Budget that consists of one or more
counties anchored by an urban center of at least 10,000 people plus adjacent counties
that are socioeconomically tied to the urban center by commuting.
CEC Comprehensive ESRD Care Model - Payment model run by The Innovation Center
from 2015-2021 that tested coordinated kidney care for ESRD beneficiaries.
CI Component The continuous improvement (CI) component of the Performance Based Adjustment
in the KCF Option
CKCC Comprehensive Kidney Care Contracting
CKD Chronic Kidney Disease - Condition characterized by the gradual loss of kidney
function over time. May ultimately lead to ESRD.
CKD QCP
CKD Quarterly Capitation Payment
CMS Centers for Medicare & Medicare Services - Federal agency within the United States
Department of Health and Human Services (HHS) that administers the Medicare and
Medicaid programs and contains the Innovation Center

84
Term Definition
CMS-HCC
Model
CMS Hierarchical Condition Category Condition Model – A risk adjustment model
used by CMS to calculate risk scores, which are used in adjusting capitated payments
made for beneficiaries enrolled in Medicare Advantage (MA) and other plans.
CPC+ Comprehensive Primary Care Plus Model
Dialysis Facility An entity, as defined at 42 CFR § 494.10, that provides outpatient maintenance
dialysis services, or home dialysis training and support services, or both.”
ESRD End-Stage Renal Disease - Medical condition in which a person's kidneys cease
functioning on a permanent basis leading to the need for a regular course of long-term
dialysis or a kidney transplant to maintain life. Beneficiaries may become entitled to
Medicare based on ESRD.
FFS Fee-for-Service - A payment method under which doctors and other health care
providers are paid for each service performed.
GFR or eGFR Glomerular Filtration Rate - A test used to check how well the kidneys are working.
Specifically, it estimates how much blood passes through the glomeruli each minute.
Glomeruli are the tiny filters in the kidneys that filter waste from the blood.
Hemodialysis A modality of dialysis where a machine and a special filter called an artificial kidney,
or a dialyzer, are used to clean the blood through an access in your blood vessels.
Home Dialysis Peritoneal or hemodialysis performed by an appropriately trained beneficiary (and/or
the beneficiary’s caregiver) at the home of the beneficiary.
Home Dialysis
True-Up
Component of the AMCP, equal to $35 per home dialysis MCP claim for aligned
beneficiaries with ESRD furnished by a KCF or KCE nephrologist or nephrology
professional during the performance year.
Innovation
Center
Center for Medicare and Medicaid Innovation - Division of CMS that tests innovative
payment and service delivery models to reduce program expenditures under Medicare
and Medicaid while preserving or enhancing the quality of care furnished to
individuals.
KCE Kidney Contracting Entity– Entity made up of providers and suppliers coordinating
care in the CKCC Options for aligned beneficiaries with CKD or ESRD or kidney
transplant
KDE Kidney Disease Education Benefit - Medicare covers up to 6 sessions of kidney
disease education services if the beneficiary has Stage 4 chronic kidney disease that
will usually require dialysis or a kidney transplant.
KTB Kidney Transplant Bonus
LDO Large Dialysis Organization; An entity that owns, directly or indirectly, 500 or more
Dialysis Facilities.
MA Medicare Advantage

85
Term Definition
Marketing
Materials and
Activities
Marketing Materials and Activities are defined as general audience materials such as
brochures, advertisements, outreach events, letters to beneficiaries, Web pages,
mailings, social media, or other activities conducted by or on behalf of the KCF
Practice or KCE, or by KCF or KCE Participants, or Preferred Providers, when used
to educate, solicit, notify, or contact Beneficiaries regarding the KCC Model.
MCP Monthly Capitation Payment
MIPS Merit-Based Incentive Payment System - the performance-based incentive program
for eligible clinicians paid under the PFS, required by section 1848(q) of the Social
Security Act.
MIPS APM An APM that meets the following criteria as specified at 42 CFR 414.1367(b):
(1) APM Entities participate in the APM under an agreement with CMS or
through a
law or regulation; and
(2) The APM bases payment on cost/utilization and quality measures.
MLR Minimum Loss Rate - The minimum percentage of the Total Performance Year
Expenditure Benchmark that the KCE must incur in losses to be liable for Shared
Losses.
MSR Minimum Savings Rate - The minimum percentage of the Total Performance Year
Expenditure Benchmark that the KCE must achieve in savings to be eligible to
receive Shared Savings.
KCF CMS Kidney Care First
KCC Kidney Care Choices Model
Non-LDO Non-Large Dialysis Organization; An entity that owns, directly or indirectly, no more
than 500 Dialysis Facilities.
NQF The National Quality Forum - A United States-based non-profit membership
organization that promotes patient protections and healthcare quality through
measurement and public reporting.
OACT Office of the Actuary
OPO Organ Procurement Organization - A non-profit organization that is responsible for
the evaluation and procurement of deceased-donor organs for organ transplantation.
Participation
Agreement
Participation Agreement refers to the agreements that will outline the requirements
and conditions of participation in the KCC Model.
PBA Performance Based Adjustment
PBPM Per Beneficiary Per Month

86
Term Definition
PBPY Per Beneficiary Per Year - A measurement of expenditures calculated by dividing
expenditures by Beneficiary-Years. This differs from a per capita basis, which is
expressed in per beneficiary terms.
PCF The Innovation Center’s Primary Care First Model
Peritoneal
Dialysis
A modality of dialysis where the blood is cleaned through the lining of the patient’s
abdomen via a catheter.
PY Performance Year - The 12-month period beginning on January 1 of each year during
the term of the Participation Agreement.
QPP The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) amended the
Social Security Act to create the Quality Payment Program (QPP). There are 2 ways
clinicians can participate in the Quality Payment Program: the Merit-based Incentive
Payment System (MIPS) and Advanced Alternative Payment Models.
Quality Gateway A set of measures that includes and indicates appropriate clinical care and
engagement for the patient population, that are directly and indirectly related to the
beneficiary’s kidney disease, and that are applicable to both CKD Stages 4 and 5
patients and ESRD patients. The Quality Gateway is only applicable to the KCF
Option.
RFA Request for Applications
Risk Adjustment The process of adjusting for diagnoses and demographic factors that are expected to
affect Medicare Part A and Part B expenditures
RP Component The relative performance (RP) component of the Performance Based Adjustment in
the KCF Option.
Shared Losses
The amount owed to CMS by the KCE due to expenditures for Medicare Part A
and Part B items and services furnished to aligned beneficiaries during a
Performance Year in excess of the KCE’s Final Performance Year Benchmarks
for the applicable Performance Year.
Shared Savings The amount owed to the KCE by CMS due to expenditures for Medicare Part A and
Part B items and services furnished to aligned beneficiaries during a performance year
that are lower than the KCE’s Final Performance Year Expenditure Benchmarks for
the applicable Performance Year.
Shared Savings
Program
The Medicare Shared Savings Program – Medicare program established under section
1899 of the Act that aims to encourage coordination and cooperation among providers
and suppliers to improve the quality of care for Medicare Fee-For-Service (FFS)
beneficiaries and reduce the rate of growth in expenditures.
SNF Skilled Nursing Facility

87
VI. Appendix B. Applicant Selection Criteria and Scoring
Selection
D
omain
Applicant Selection Criteria
To earn full points in each domain, the applicant must:
KCE
Score
KCF
Score
Care Model
Patient
Centeredness
• Demonstrate the ability to engage beneficiaries and their
caregivers in shared decision making, taking into account
patient preferences and choice.
• Have a feasible plan to establish mechanisms to conduct
patient outreach and education on the benefits of care
coordination, renal transplantation, and care settings.
• Demonstrate the ability to effectively involve beneficiaries
in care transitions to improve the continuity and quality of
care across settings, e.g., medication lists; care plans co-
developed with the patient and embedded in the EHR; case
manager follow up.
• Demonstrate the ability to engage and activate beneficiaries
at home (through such modes as home visits or tele-
monitoring) to improve self-management.
• Have mechanisms to evaluate patient satisfaction with the
access and quality of their care, including choice of
providers, and choice in care settings.
• Have a plan that establishes an effective mechanism that
allows for open communication of key care management
processes among patients, their caregivers, and the
interdisciplinary participant team.
25 35
Organizational
Structure and
Leadership &
Management,
Organizational Structure (5)
• Demonstrate a history of collaboration between participating
providers/provider organizations and/or credible plan for
how the participants will work together in the model.
• Have an organizational structure that promotes patient
centered care and the goals of the model. In addition to
meeting the minimum eligibility requirements for
provider/supplier participation, the applicant organization is
made up of a diverse set of provider/suppliers that
demonstrates a clear commitment to providing high quality,
coordinated care to beneficiaries.
• Leadership and Management (5)
• Have identified, or demonstrate plans to identify, executives
and lead staff throughout the organization with
responsibility for clinical, financial, management, HIT, and
quality improvement functions.
• Demonstrate experienced, strong project leadership and a
project management structure and design that will enable
accountability for a patient population. Alternatively, the
applicant provides a clear and detailed plan for establishing
project leadership and management structure that meets this
criterion.
10 10

88
Selection
Domain
Applicant Selection Criteria
To earn full points in each domain, the applicant must:
KCE
Score
KCF
Score
Governance
Structure
(CKCC Only)
• Have a governance structure that is clearly defined and
demonstrates commitment to providing high quality care to
beneficiaries consistent.
• Have a multi-stakeholder governing body comprised of well
qualified individuals, including an independent Medicare
beneficiary representative with a diagnosis of CKD Stage 4
or 5 or ESRD and/or a trained and/or experienced non-
affiliated, independent consumer advocate, that adequately
and collectively represent the interests of beneficiaries and
providers. If the applicant has not yet formed a new legal
entity, the applicant must have a feasible and clearly defined
plan, including timeline, for the formation of a multi-
stakeholder governing body as described above.
• Provide a clear and detailed plan for governance structure to
identify, report, and remediate suspected fraud and abuse.
• Demonstrate an effective governance structure plan
including a governing body and/or organizational
mechanisms to make decisions, distribute payment, and
obtain resources necessary to achieve the goals of the model.
10 N/A

89
Selection
Domain
Applicant Selection Criteria
To earn full points in each domain, the applicant must:
KCE
Score
KCF
Score
Care
Coordination
Capabilities
and
Implementation
Plan
• Present a strong, credible, coordinated and feasible plan to
realize the goals of the model.
• Demonstrate existing capacity or plans to expand capacity to
coordinate care through an interdisciplinary team structure
that includes practitioners with the necessary areas of
expertise and appropriate staffing to meet the needs of
complex patients.
• Provide clear and detailed plan for a majority of eligible
professionals in the organization to meet EHR meaningful
use criteria and requirements.
• Have population-based management tools and functions or
concrete plans to develop and invest in such tools and
functions, e.g. registry/ability to aggregate and analyze
clinical data.
• Have the ability, or credible plans to develop the ability, to
electronically exchange patient records across participating
providers and other providers in the community to ensure
continuity of care.
• Have ability to, or credible plan to gain ability to, share
performance feedback on a timely basis with participating
providers.
• Demonstrate ability to coordinate care across full continuum
of CKD care to improve the physical health,
mental/behavioral health, and functional status of
beneficiaries.
• Provide credible plan for incorporating medication
management into care coordination approach.
• Demonstrate a history of collaboration among major
stakeholders in the community being served including
incorporation of relevant social services in care plans and
management.
• Demonstrate compelling plan to succeed in the areas of
quality improvement and care coordination.
• Demonstrate performance under prior or current outcomes-
based contracts that includes: (1) financial accountability;
(2) evaluation of patient experiences of care; and (3)
substantial quality performance incentives.
• Provide a care coordination plan that incorporates
mental/behavioral health and social services as appropriate.
40 40

90
Selection
Domain
Applicant Selection Criteria
To earn full points in each domain, the applicant must:
KCE
Score
KCF
Score
Care for
Vulnerable
Populations
• Include a diverse group of practitioners, and care settings to
meet the needs of CKD and ESRD patients.
• Include safety net providers that care for indigent
populations.
• Include practitioners, technology, and other resources that
enable access to quality care for populations in rural areas.
• Provide care to a large percentage of Medicare-Medicaid
Enrollees.
• Demonstrate clear understanding of unique needs of
beneficiaries with CKD and ESRD that includes a care
coordination approach that addresses those needs.
15 15
Total Points 100 100
