
What’s inside
Effective January 1, 2020
Walmar 401(k) Plan effective February 1, 2020
Medical plan
Pharmacy benefit
Dental plan
Vision plan
Life insurance and disability plans
Associate Stock Purchase Plan
Walmar 401(k) Plan
2021 Summaries of Material
Modifications
Version 4.5 | Nov. 2020
2020 Associate
Benefits Book
Summary Plan Descriptions with
2021 Summaries of Material
Modifications

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Table of contents
Information obtained during communications with Walmar Inc. or any
Plan service provider does not waive any provision or limitation of
the Plan. Information given or statements made through any form of
communication do not guarantee payment of benefits. In addition,
benefits quotes that are given by phone are based wholly on the
information supplied at the time. If additional relevant information is
discovered, it may affect payment of your claim. All benefits are subject
to eligibility, payment of premiums, limitations, and all exclusions outlined
in the applicable Plan documents, including any insurance policies. You
can request a copy of the documents governing these plans by writing to:
Custodian of Records, People Services, 508SW8thStreet, Bentonville,
Arkansas 72716-3500.
Atención Asociados Hispanos: Este folleto contiene un resumen
en inglés de los derechos y beneficios para todos losasociados bajo el
plan de beneficios de Walmar. Si Ud tienedificultades para entender
cualquier pare de este folletopuede dirigirse a la siguiente dirección:
PeopleServices, 508 SW 8th Street, Bentonville, Arkansas72716-3500.
O puede llamar para cualquier pregunta al 800-421-1362. Tenemos
asociados quienes hablan Español y pueden ayudarles a Ud comprender
sus beneficios de Walmar. El Libro de beneficios para asociados esta
disponible en Español. Si usted desea una copia en Español, favor de
ver su Representante de Personal.
Eligibility and enrollment 4
Eligibility and benefitsfor associatesin Hawaii 38
The medical plan 44
The pharmacy benefit 92
Health savings account(HSA) 98
The dental plan 106
The vision plan 116
COBRA 122
Resources for Living
®
130
Critical illness insurance 134
Accident insurance 140
Company-paid lifeinsurance 148
Optional associate life insurance 154
Optional dependent life insurance 160
Accidental death and dismemberment
(AD&D) insurance 166
Business travel accident insurance 174
Shor-term disability for full-time hourly associates 180
Salaried shor-term disability plan 190
Truck driver shor-term disabilityplan 198
Long-term disability 206
Truck driver long-termdisability 214
The Associate Stock Purchase Plan (ASPP) 222
The Walmar 401(k)Plan 234
Claims and appeals 260
Legal information 280
Glossary 294
2021 Summaries of Material Modifications 296
For more information 338

3
When you download the 2020 Associate Benefits Book from One.Walmar.com, you’ll
have answers to your benefit questions at your fingerips.
Just launch the PDF with Adobe Reader and click “Edit” on the toolbar. Then click “Find,”
and enter a word or phrase that describes what you’re looking for, like“preventive”
or “copay.” Easy!
This is also where you’ll find the 2021 Summary of Material Modifications to the
Associates’ Health and Welfare Plan and the 2021 Summary of Material Modifications
to the Walmar 401(k) Plan. The addition of these “SMMs” brings the 2020 Associate
Benefits Book up to date for another year. You’ll find the SMMs on page 296, along
with several imporant legal notices.
Throughout this book you’ll also see many spots where we have alered you to details
that have been updated in one of the SMMs—look for the page icon like the one to the
left. When you see that, you’ll know where to turn to find the most current information.
Lots of information.
So easy to find.
Welcome to your 2020
Associate Benefits Book
This is where you’ll find the Summary Plan Descriptions (SPDs) for the
Associates’ Health and Welfare Plan (the Plan), and the Walmar 401(k) Plan.
The prospectus for the Associate Stock Purchase Plan is here, too.
Check out the table of contents for a complete list of what you’ll find in
this book. It’s a great resource to help you understand your benefits.
Many of the terms used throughout the 2020 Associate Benefits Book may
beunfamiliar to you, or have specific meanings within the context of the Plans.
You’ll find many of them defined in the Glossary on page 294, and we have also
included imporant definitions at critical points throughout the text.
Key words

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Eligibility and
enrollment
The Associates’ Health and WelfarePlan 6
Associate eligibility 6
Par-time hourly and temporary associates: eligibility checks for medical benefits 7
Dependent eligibility 9
Legal documentation for dependentcoverage 10
Dependents who are not eligible 10
When your dependent becomesineligible 10
When you enroll for benefits 10
When coverage is effective 11
If you leave the company and arerehired 12
Effective dates for benefits under the Plan 12
Enrollment and effective dates by job classification 13
Paying for your benefits 18
Tobacco rates 19
Continuing benefit coverage if you go on a leave of absence 19
Continuing benefit coverage whiledisabled 20
Status change events 21
If your job classification changes 24
Transferring from one job classification to another 24
Qualified Medical Child Suppor Orders (QMCSO) 36
When your Plan coverage ends 36
If you have Medicare or will become eligible for Medicare in the next 12 months,
you have more choices for your prescription drug coverage. See page 287 in the
Legal information chapter for more details. See page 332

Eligibility and enrollment
5
Eligibility and enrollment
RESOURCES
Find What You Need Online Other Resources
• Enroll in Walmar benefits
• Notify People Services within 60
days of a status change event
Go to One.Walmar.com or
Workday for Jet associates
Call People Services at 800-421-1362
Notify People Services if you have
questions about the payroll deductions
for your benefits
Call People Services at 800-421-1362
Pay premiums for benefits while on a
leave of absence
See Continuing benefit coverage if you go on a leave of
absence in this chapter for detailed information. If you
are required to pay your premiums to keep coverage
current, you must pay the premiums to keep coverage
current. You may pay by credit or debit card with a Visa,
MasterCard, American Express, or Discover card by
calling 800-421-1362 and saying “make a payment.”
You may also send a check or money order payable to
the Associates’ Health and Welfare Trust to:
Walmar People Services
P.O. Box 1039
Deparment 3001
Lowell, Arkansas 72745
To ensure timely posting of your payment, be sure to
include your WIN (Walmar ID) number on the check.
What you need to know about eligibility and enrollment
• You can enroll for benefits during your initial enrollment period as a newly eligible associate, during Annual Enrollment,
or when you have a status change event.
• Your job classification (or changes to your job classification) determines when your initial enrollment period begins.
Ifyou are a Hawaii associate, see the Eligibility and benefits for associates in Hawaii chapter.
• Medical, dental, vision, critical illness, accident, and accidental death and dismemberment (AD&D) insurance benefits
cannot be changed except during Annual Enrollment or after you have a status change event.
• If you choose to enroll in the short-term disability enhanced, long-term disability, or truck driver long-term disability
benefits options, you may drop your coverage at any time, but you will only be able to add this coverage again during an
initial enrollment period, Annual Enrollment, or when you have a status change event.
• You may enroll in, drop, or change optional life insurance benefits at any time but if you enroll after your initial
enrollment period, you will have to provide Proof of Good Health.
See page 298
Eligibility and enrollment
6
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The Associates’ Health and
WelfarePlan
The Associates’ Health and Welfare Plan (the Plan) is
a comprehensive employee benefit plan that offers
medical, dental, vision, critical illness insurance, accident
insurance, AD&D, business travel accident insurance, life
insurance, disability, and Resources for Living (employee
assistance and wellness) benefits to eligible associates and
their eligible dependents. Eligibility for these benefits is
described in this chapter, and the terms and conditions for
these benefits are described in the applicable chapters of
this 2020 Associate Benefits Book. The Plan is sponsored by
Walmart Inc. (the company).
You are automatically enrolled for certain benefits under
the Plan on your date of hire or a later date. For other
benefits, however, you must enroll to have coverage. Refer
to the Enrollment and effective dates by job classification
section in this chapter for details about initial enrollment
periods and when coverage is effective, for all benefits
available under the Plan.
Associate eligibility
The benefits you are eligible for depend on a number
of factors, which may include your date of hire, average
weekly hours, and your job classification in the Walmart
Inc. payroll system. In addition, for most benefits, you
may be required to meet an eligibility waiting period. See
the Enrollment and effective dates by job classification
section in this chapter for a list of the benefits you are
eligible for and for your eligibility waiting period based on
your job classification.
Our expectation is that you will use correct and accurate
information when applying for or enrolling in benefits.
If you do not, you may be subject to the loss of benefits
and/or loss of employment. To review Walmart’s policy
about intentional dishonesty, refer to the Statement of
Ethics, which can be found on One.Walmart.com. See
Legal documentation for dependent coverage later in this
chapter for information about documents that may be
requested of you to verify dependent eligibility.
NOTE: Your eligibility for benefits is determined by the
eligibility rules detailed in this Associate Benefits Book. To
the extent that any information provided to you through
other sources conflicts with the Associate Benefits Book, the
eligibility rules in the Associate Benefits Book will control.
MANAGEMENT ASSOCIATE ELIGIBILITY
To be eligible for benefits as a management associate, you
must be classified in the company’s payroll system as a
management associate, management trainee, California
pharmacist, or full-time truck driver.
FULLTIME HOURLY ASSOCIATE ELIGIBILITY
To be eligible for benefits as a full-time hourly associate,
you must be classified in the company’s payroll system as a
full-time hourly associate.
PARTTIME HOURLY ASSOCIATE ELIGIBILITY
To be eligible for benefits as a part-time hourly associate,
you must be classified in the company’s payroll system as a
part-time hourly associate.
To be eligible to enroll in medical benefits, you must
workan average of at least 30 hours per week, with the
following exceptions:
• Part-time hourly pharmacists hired prior to
February1,2012, do not need to work a minimum
number of hours per week.
• Part-time hourly pharmacists hired on or after
February1,2012, must work an average of at least
24hours per week.
• Part-time hourly associates in the field supply chain
must work an average of at least 24 hours per week.
• Part-time hourly nurse practitioners must work an
average of at least 24 hours per week.
Part-time hourly associates are subject to the annual
eligibility check process described later in this chapter, with
the exception of part-time hourly pharmacists hired prior to
February 1, 2012. The annual eligibility check determines your
eligibility for medical benefits based on the number of hours
you work on average in the 52-week period preceding the
date of the annual eligibility check. For more information, see
the section titled Part-time hourly and temporary associates:
eligibility checks for medical benefits.
PARTTIME TRUCK DRIVER ELIGIBILITY
To be eligible for benefits as a part-time truck driver, you
must be classified in the company’s payroll system as a
part-time truck driver. You do not need to work a minimum
numbers of hours per week to be eligible to enroll in
medical benefits as a part-time truck driver.

Eligibility and enrollment
7
TEMPORARY ASSOCIATE ELIGIBILITY
To be eligible for benefits as a temporary associate, you
must be classified in the company’s payroll system as a
temporary associate.
To be eligible to enroll in medical benefits, you must work
an average of at least 30 hours per week, with the exception
of temporary associates in the field supply chain, who must
work an average of at least 24 hours per week.
Temporary associates are subject to the annual eligibility
check process described later in this chapter. The annual
eligibility check determines your eligibility for medical
benefits based on the number of hours you work on average
in the 52-week period preceding the date of the annual
benefits eligibility check. For more information, see the
section titled Part-time hourly and temporary associates:
eligibility checks for medical benefits.
ASSOCIATES WHO ARE NOT ELIGIBLE
You are not eligible for the Plan if you fall in any of the
following categories, even if you are reclassified by a court,
the IRS, or the Department of Labor as a common-law
employee of the company or any participating affiliate:
• A leased employee
• A nonresident alien (except for optional associate life
insurance, optional dependent life insurance, accidental
death and disability insurance, and business travel accident
insurance, and unless covered under a specific insurance
policy for expatriates or third-country nationals who are
employed by the company)
• An independent contractor
• A consultant
• An associate residing outside the United States
• Not classified as an associate of the company or its
participating affiliates
• An associate who is enrolled in Medicare Part D (applicable
only to eligibility for medical plan options, including HMOs
and the eComm PPO Plan), or
• An associate covered by a collective bargaining agreement,
to the extent that the agreement does not provide for
participation in the Plan.
ELIGIBILITY INFORMATION FOR ADDITIONAL
ASSOCIATE CATEGORIES
Associates in HMOs and eComm PPO Plans: HMO and
eComm PPO Plans are available for some work locations.
The policies and enrollment materials for the HMO and
eComm PPO Plans may describe different eligibility
requirements and waiting periods than those described in
this chapter. If there is any difference between the HMO’s
or eComm PPO Plan’s eligibility terms and the eligibility
terms of the Associates’ Medical Plan (AMP) as described in
this chapter, eligibility terms in this chapter will control.
In addition, some HMOs require participants to accept an
arbitration agreement, where permitted by law, before
coverage under the HMO will become effective. Your
agreement must be received by the HMO within 60 days of
your initial enrollment or your HMO coverage will not take
effect. If the HMO does not receive your agreement, you will
not have medical coverage under the Plan unless you have a
valid status change event, as described later in this chapter.
Hawaii associates: Special rules govern benefits eligibility
and enrollment in the state of Hawaii. If you are a full-time
hourly, part-time hourly, or temporary associate in Hawaii,
please refer to the chapter titled Eligibility and benefits
for associates in Hawaii. For management associates in
Hawaii, the eligibility and enrollment terms described in this
Eligibility and enrollment chapter apply.
Localized associates: If you have been approved by the
company as having localized status, you and your dependents
residing in the United States are eligible for the same
benefits under the Plan as associates who are United States
citizens residing and working in the United States. Any
applicable waiting period is waived. You are not eligible for
expatriate coverage under the Plan. If you are a localized
associate and an eligible dependent resides outside the
United States, medical claims will be processed as network
benefits regardless of the provider’s network status and paid
at the applicable copay or coinsurance rate for network
charges, subject to applicable limitations and exclusions
under the Plan. You or your enrolled dependents must file a
claim for reimbursement under thePlan’s claims procedures.
See page 298 for important information for part-time
hourly and temporary associates about eligibility checks.
Par-time hourly and temporary
associates: eligibility checks for
medical benefits
INITIAL ELIGIBILITY CHECK FOR
MEDICALBENEFITS
If you are a part-time hourly or temporary associate
(other than a part-time truck driver), your initial eligibility
for medical benefits is determined during your initial
measurement period. Your initial measurement period is the
52 consecutive weeks beginning on your date of hire, during
which your average hours worked per week are reviewed.
Eligibility and enrollment
8
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you work an average of at least 30 hours a week (24 hours
a week for part-time nurse practitioners, part-time hourly
pharmacists, part-time hourly and temporary associates
in the field supply chain) over the 52-week review period
without a break in employment greater than 13 weeks, you
will become eligible for medical benefits at the close of
your initial measurement period. Specifically, your eligibility
for medical benefits will begin on the first day of the
second calendar month following your one-year anniversary
date. For example, if your date of hire is April 16, 2019, your
average hours worked from that day through April 15, 2020
will be calculated. If you meet the average-hours-worked
requirement over this initial measurement period, your
coverage would begin June 1, 2020 (assuming you enroll in a
timely manner).
Initial medical coverage for associates who meet the
average-hours-worked requirement continues through
the end of the second calendar year following date of hire.
In the example above, your coverage (if you enroll in a
timely manner) would continue through the end of 2021.
You would then be subject to annual eligibility checks, as
described below.
ANNUAL ELIGIBILITY CHECK FOR
MEDICALBENEFITS
If you are classified as a part-time hourly or temporary
associate (other than a part-time truck driver or a part-time
hourly pharmacist hired before Feb. 1, 2012), you will be
subject to an annual eligibility check to establish your
eligibility for medical benefits for the next calendar year.
You will also be subject to the annual eligibility check if you
were originally hired as a management or full-time hourly
associate and were employed one year or more before
changing to part-time hourly or temporary status.
The measurement period for the annual eligibility check
will be the 52 weeks preceding an annually designated
date in early October prior to each calendar year’s
Annual Enrollment. For example, the annual eligibility
check occurring in fall 2020 (for the 2021 calendar year)
will review your hours worked from October 5, 2019,
through October4, 2020. If you meet the average hours
requirement (24or 30 hours per week, depending on job
classification) over the 52-week period, you will be eligible
to enroll in medical benefits during Annual Enrollment for
coverage during2021.
If you do not meet the average weekly hours requirement
in the annual eligibility check, your medical coverage may
continue for a period of time, as described below under If you
do not meet the annual eligibility check for medical benefits.
If you have questions about the annual eligibility check, call
People Services at 800-421-1362.
IF YOU MEET THE ANNUAL ELIGIBILITY CHECK
FOR MEDICAL BENEFITS
If you are currently a part-time hourly or temporary associate
who is enrolled for medical coverage and you meet the
annual eligibility check in October, you will remain enrolled
for medical coverage for the remainder of the current year.
You will receive Annual Enrollment materials and be eligible
to enroll for medical benefits for the following year.
You will be subject to the annual eligibility check each year
to determine your eligibility for medical benefits for the
following year.
IF YOU DO NOT MEET THE ANNUAL
ELIGIBILITY CHECK FOR MEDICAL BENEFITS
If you are currently a part-time hourly or temporary
associate who is enrolled for medical coverage, but you do
not meet the annual eligibility check in October, you will
remain enrolled for medical coverage for the remainder of
the current calendar year. You will not be eligible for medical
benefits for the following year unless your job classification
changes and you meet the eligibility requirements based on
your new classification. You will receive a letter describing
your options under the Consolidated Omnibus Budget
Reconciliation Act (COBRA) to continue your medical
coverage when the current calendar year ends. (See the
COBRA chapter for more information.)
You will be subject to the annual eligibility check each year
to determine your eligibility for medical benefits for the
following year.
IF YOU TAKE TIME OFF DURING THE
ANNUAL MEASUREMENT PERIOD FOR THE
ELIGIBILITY CHECK
If you take any type of unpaid time off that is not an
approved leave of absence, as described below, your
number of actual service hours will still be used in the
calculation of your average hours for the annual eligibility
check (even if it is zero).
If your absence is an approved leave (including for jury
duty, Family and Medical Leave Act of 1993 [FMLA] leave,
or military leave), your average-hours-worked calculation
will be based on the number of weeks during the 52-week
measurement period that you worked. For example, if you
take an approved leave during two weeks of the 52-week
measurement period, your average hours worked will be
calculated over 50 weeks rather than 52.

Eligibility and enrollment
9
Dependent eligibility
If you are a management or full-time hourly associate and are eligible for benefits under the Plan, you may also enroll all eligible
dependents as described below. If you are a part-time hourly or temporary associate or a part-time truck driver, and you are
eligible for benefits under the Plan, you may also enroll only your dependent child; you may not enroll any other dependent.
EMPLOYMENT CLASSIFICATION ELIGIBLE DEPENDENTS AS DEFINED BELOW
• Management
• Full-time hourly
Can elect to cover:
• Spouse/parner
• Dependent child(ren)
• Par-time hourly
• Temporary
• Par-time truck driver
Can elect to cover:
• Dependent child(ren)
But not spouse/parner
DEFINITIONS: ELIGIBLE DEPENDENTS
SPOUSE/PARTNER
• Your spouse, as long as you are not legally separated
• Your domestic parner (or “parner”), as long as you and your domestic parner:
– Are in an exclusive and committed relationship similar to marriage and have been for at least 12months
– Are not married to each other or anyone else
– Meet the age for marriage in your home state and are mentally competent to consent to contract
– Are not related in a manner that would bar a legal marriage in the state in which you live, and
– Are not in the relationship solely for the purpose of obtaining benefits coverage.
• Any other person to whom you are joined in a legal relationship recognized as creating some or all of the
rights of marriage in the state or country in which the relationship was created (also referred to as“parner”)
DEPENDENT
CHILD(REN)
• Your dependent children through the end of the month in which the child reaches age 26.
Yourdependent children are:
– Your natural children
– Your adopted children or children placed with you for adoption
– Your stepchildren or children of your eligible parner, provided however:
• Eligibility will end upon divorce or change in parner status, even if the child is under age 26
• Eligibility will end upon death of your spouse or parner, if the child is under age 18, or
• Eligibility will continue until age 26 in the event of the death of your spouse or parner, if at the time
of death: i) the child has attained age 18, and ii) the child is enrolled in the Plan.
– Your foster children
– Someone for whom you have legal custody or legal guardianship, provided he or she is living as a member
of your household and you provide more than half of his or her suppor
If an individual is your eligible dependent and subsequently
no longer satisfies the definition of eligible dependent, that
individual will no longer be eligible for coverage under the
Plan and you are required to report the change. See When
your dependent becomes ineligible later in this chapter for
information. If you fail to report the change, you may be
subject to the loss of benefits and/or loss of employment.
If a court order requires you to provide medical, dental,
and/or vision coverage for your child, the child must be an
eligible dependent as defined above. For more information
on how the Plan handles a Qualified Medical Child Support
Order (QMCSO), see the Qualified Medical Child Support
Orders (QMCSO) section later in this chapter.
If you are enrolled in a medical plan option that does not
offer out-of-network coverage and you have an eligible
dependent living outside the service area of your medical
plan, you may still enroll your eligible dependents, but
they will not have access to network providers in the
geographic area in which they live and may have access only
to emergency coverage. If you are unsure if your eligible
dependent lives outside your medical plan’s service area, call
your health care advisor at the number on your plan ID card.
IF YOUR CHILD IS INCAPABLE OF
SELFSUPPORT
If your child is enrolled for coverage under the Plan, you
may continue the child’s coverage beyond the end of the
month in which your child reaches age 26 if:
• The child is physically or mentally incapable of self-support
and primarily dependent on you for legal support, and
• The child’s doctor provides written medical evidence of
the child’s incapacity.

Eligibility and enrollment
10
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Additional coverage may be added if your child experiences
a valid status change event. For information regarding a
status change event, refer to the Status change events
section of this chapter.
Legal documentation for
dependentcoverage
The Plan reserves the right to conduct a verification audit of
dependent eligibility. You may be required to provide legal
documentation to prove the eligibility of your dependent. It
is your responsibility to provide the written documentation
if requested to do so by the Plan. If you do not provide
necessary documentation in a timely manner, the Plan has the
right to cancel your dependent’s coverage until the requested
documentation is received. It is your responsibility to notify
the Plan of any changes in your dependent’s eligibility.
Examples of valid documentation are as follows:
• Spouse: marriage certificate and jointly filed federal
taxreturn
• Domestic partner: domestic partner affidavit and joint
mortgage statement or rental agreement
• Children: state- or county-issued birth certificate or
signed court order
Dependents who are not eligible
Your dependent is not eligible for coverage under the Plan
if he or she is:
• Residing outside the U.S. (not applicable to optional
dependent life insurance, AD&D, critical illness, and
accident insurance, and not applicable if your dependent
isattending college full-time outside the U.S.)
• Covered under an expatriate plan
• An undocumented immigrant
• Not an eligible dependent as defined under Dependent
eligibility on the previous page
• A Walmart associate already enrolled in coverage under
the Plan (not applicable to optional dependent life
insurance, AD&D, critical illness, and accident insurance)
• A dependent of another Walmart associate and already
enrolled in coverage under the Plan (not applicable to
optional dependent life insurance, AD&D, critical illness,
and accident insurance)
• Enrolled in Medicare Part D (applicable only to eligibility
for medical plan options, including HMOs and the eComm
PPO Plan)
When your dependent
becomesineligible
If your dependent is enrolled in coverage under the Plan and
becomes ineligible for coverage, you must notify People
Services at 800-421-1362 within 60 days from the date your
dependent becomes ineligible. If you notify People Services
within this time frame, the Plan will send an election notice,
allowing you to elect Consolidated Omnibus Budget
Reconciliation Act (COBRA) continuation coverage. Your
dependent’s election to enroll in COBRA coverage must be
received within 60 days from the date your dependent loses
coverage or the date of the election notice, if later. See the
COBRA chapter for more information.
Failure to notify the Plan by calling People Services at
800-421-1362 when your dependent becomes ineligible for
coverage may be considered an intentional misrepresentation
of material facts, which may result in your coverage being
canceled. If your dependent becomes ineligible for coverage
and you fail to notify the Plan by calling People Services, you
may be responsible for any charges mistakenly paid by the
Plan after the date that your dependent became ineligible.
When you enroll for benefits
Once you have completed any applicable eligibility waiting
period, you can enroll for benefits during your initial
enrollment period, which is the first time you are eligible to
enroll. The timing of your initial enrollment period varies by
job classification and may change if your job classification
changes. For more information, see Enrollment and
effective dates by job classification later in this chapter and
refer to the chart that applies to your job classification. You
may also enroll for benefits at the following times:
• During Annual Enrollment, which generally occurs
in the fall of each year. Benefits you enroll in during
Annual Enrollment are generally effective January 1 of
the following year, but there are exceptions. See the
appropriate chart in the Enrollment and effective dates by
job classification section for important details.
• If you choose to enroll in the short-term disability
enhanced, long-term disability, or truck driver long-term
disability benefits options, you may drop your coverage at
any time, but you will only be able to add this coverage
again during an initial enrollment period, Annual
Enrollment, or when you have a status change event
See page 298
• At any time for optional associate life insurance and
optional dependent life insurance. If you are enrolling in
optional associate life insurance or optional dependent
life insurance during Annual Enrollment, your coverage
is effective upon the date of approval by Prudential (not
January 1 of the following year).

Eligibility and enrollment
11
If you do not enroll during your initial enrollment period,
you will not be able to enroll for the following benefits until
the next Annual Enrollment, unless you have a status change
event (see the Status change events section of this chapter
for additional details):
• Medical, including HMO plans and the eComm PPO Plan
(subject to the annual eligibility check described in the
Annual eligibility check for medical benefits section
earlier in this chapter)
• Dental
• Vision
• Critical illness insurance
• Accident insurance
• Short-term disability enhanced plan (see important
exception immediately below)
• Long-term disability (LTD) or truck driver LTD (see
important exception immediately below)
• Accidental death and dismemberment (AD&D)
There is an important exception that can delay the effective
date of the short-term disability enhanced plan or the
long-term disability plan. If you do not enroll in the
short-term disability enhanced plan or the long-term
disability plan, and you later choose to enroll during Annual
Enrollment or when you have a status change event, you will
be considered a late enrollee and will be required to
complete a 12-month waiting period before your coverage is
effective. If your late enrollment is due to a status change
event, your 12-month waiting period will begin as of the date
of the event. If your late enrollment is during Annual
Enrollment, your 12-month waiting period will begin as of
the date you enroll.
See page 298
See the Truck driver long-term disability chapter for
additional information about coverage effective dates for
late enrollees in that benefit.
CHOOSING A COVERAGE LEVEL
Your eligible dependents enrolled in the Plan must have
the same coverage you elect for yourself. You may change
your coverage during Annual Enrollment or if you have a
status change event. See the Status change events section
later in this chapter.
Under the medical, dental, and vision plans, and critical
illness and accident insurance, you may elect one of the
following coverage levels:
• Associate only
• Associate + spouse/partner (except for part-time
hourlyassociates, temporary associates, and part-time
truck drivers)
• Associate + child(ren), or
• Associate + family (except for part-time hourly associates,
temporary associates, and part-time truck drivers).
CONFIRMING YOUR ENROLLMENT
Once you enroll for coverage, you can view your confirmation
statement on One.Walmart.com or Workday for Jet associates.
If you see an error regarding the benefits you enrolled in,
immediately contact People Services at 800-421-1362.
YOUR PLAN ID CARD
When you enroll in any of the medical coverage options
available under the Associates’ Medical Plan (AMP),
you receive a plan ID card at your home address. If your
third-party administrator is BlueAdvantage of Arkansas,
Aetna, or HealthSCOPE Benefits, plan ID cards for
dependents whose address is different from yours are
sent directly to the dependent’s address. If your third-
party administrator is UnitedHealthcare, a plan ID card
for a dependent is sent to your home address even if the
dependent’s address is different from yours. Your plan
IDcard also serves as your pharmacy ID card.
If you enroll in any of the medical coverage options under
the AMP or the eComm PPO Plan (if applicable) and you
also enroll in the Associates’ Dental Plan (the “dental plan”)
and/or the Associates’ Vision Plan (the “vision plan”), your
plan ID card will also serve as your dental ID card and/or
your vision ID card.
If you enroll in an HMO and you also enroll in the dental plan
and/or the vision plan, you will receive separate ID cards for
the dental and/or vision plan.
If you enroll in the dental plan and/or the vision plan only,
you will receive separate ID cards for those plans. ID cards
will be mailed to your home address.
You can update your address or that of your dependents
who are under the age of 18 when you enroll online or at any
time on One.Walmart.com or Workday for Jet associates.
If your dependent is age 18 or over, they need to contact
People Services at 800-421-1362 to update their address.
When coverage is effective
See the Enrollment and effective dates by job classification
section of this chapter for more details about coverage
effective dates.
If you are not at work on the day your coverage becomes
effective (including for a leave of absence) for medical,
vision, dental, critical illness insurance, accident insurance,
accidental death and dismemberment (“AD&D”) insurance,
Resources for Living, business travel accident insurance, or
company-paid life insurance, your coverage is effective on
the first day you are “actively at work,” as defined on the next
page, as long as you are enrolled for the benefit and have
paid the applicable premiums. No enrollment is required for
Resources for Living, business travel accident insurance,
short-term disability basic, or company-paid life insurance.

Eligibility and enrollment
12
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you are not at work for any reason (including for a leave of
absence) other than scheduled paid time off (PTO) on the
day your coverage becomes effective for optional associate
life insurance, optional dependent life insurance, short-term
disability enhanced, long-term disability (LTD), or truck
driver LTD insurance, your coverage will be effective on the
first day you are “actively at work,” as defined below.
“ACTIVE WORK” OR “ACTIVELY AT WORK”
See page 300 for information replacing the following two
paragraphs.
For medical, dental, vision, critical illness insurance,
accident insurance, AD&D and Resources for Living
coverage, “active work” (or “actively at work”) means you
are on active status and have reported to your first day of
work at the company, even if you are not at work the day
coverage begins (for example, due to illness).
For company-paid life insurance, optional associate life
insurance, optional dependent life insurance, business travel
accident insurance, and all types of disability coverage, being
actively at work means you are at work with the company
on a day that is one of your scheduled work days and
performing all of the regular duties of your job on a full-time
basis or part-time basis according to your employment
classification. You are deemed to be actively at work on a day
that is not one of your scheduled work days only if you were
actively at work on the preceding scheduled work day.
AUTOMATIC REENROLLMENT
If you currently have coverage and are eligible for benefits
during the following calendar year, but do not actively enroll
for those benefits during Annual Enrollment, you and any
dependents you cover will be automatically reenrolled. You
will be reenrolled in the coverage options closest to what you
have currently. For more information, refer to the Annual
Enrollment materials provided to you and posted online at
One.Walmart.com or on Workday for Jet associates. Call
People Services at 800-421-1362 for information.
If you do not actively enroll during Annual Enrollment
and are automatically enrolled in coverage as described
above, you may not change this coverage except during
a subsequent Annual Enrollment, unless you experience a
status change event.
If you do not actively reenroll during Annual Enrollment, you will
be deemed to have consented to automatic reenrollment and
your payroll deductions will be adjustedaccordingly.
If you leave the company and
arerehired
MANAGEMENT AND FULLTIME
HOURLYASSOCIATES
If you are enrolled for medical benefits before you terminate
employment and you return to the company within 13 weeks,
you will be automatically reenrolled in your previous coverage
(or the most similar coverage offered under the Plan). If you
return within 30 days, your annual deductible and out-of-
pocket maximum under the AMP for the calendar year in
which you terminate will not reset. If you return after 30 days
but within 13 weeks, your annual deductible and out-of-pocket
maximum will reset and you will be responsible for meeting the
new deductible and out-of-pocket maximum in their entirety.
You will have 60 days after resuming employment to drop
or otherwise change the coverage in which you were
automatically reenrolled. If you return after 13weeks, you
will be treated as a new associate.
PARTTIME HOURLY AND
TEMPORARYASSOCIATES
If you return to employment as a part-time hourly or
temporary associate within 13 weeks after leaving during your
initial measurement period, you will be treated as if you had not
left, for the remainder of the measurement period. All hours
worked during the measurement period will be used in the
average-hours-worked calculation. For example, if you have a
four-week break in service during the 52-week measurement
period, your average hours will be calculated using the
48weeks during which you worked, rather than 52weeks.
If you terminate employment after the completion of a
measurement period and return to employment as a part-time
hourly or temporary associate within 13 weeks, you will retain
your previous status through the end of the calendar year.
If you are enrolled for medical benefits before you terminate
employment and you return to the company within 13weeks,
you will be automatically reenrolled in your previous coverage
(or the most similar coverage offered under the Plan). If you
return within 30 days, your annual deductible and out-of-
pocket maximum under the AMP for the calendar year in
which you terminate will not reset. If you return after 30 days
but within 13 weeks, your annual deductible and out-of-pocket
maximum will reset and you will be responsible for meeting the
new deductible and out-of-pocket maximum in their entirety.
You will have 60 days after resuming employment to drop
or otherwise change the coverage in which you were
automatically reenrolled. If you return after 13 weeks, you will
be treated as a new associate and will be subject to the initial
eligibility check for medical benefits before you will be eligible.
Effective dates for benefits under
the Plan
The following Enrollment and effective dates by job
classification charts provide your coverage effective dates
if you enroll during your initial enrollment period. If you
terminate employment before enrolling for benefits during
your initial enrollment period, you will not be eligible to enroll.
If you are an associate in Hawaii, see the chapter titled
Eligibility and benefits for associates in Hawaii.

Eligibility and enrollment
13
Enrollment and effective dates by job classification
FULLTIME HOURLY ASSOCIATES
Includes pharmacists (except California pharmacists*), field supply chain, field supervisor positions in stores and clubs;
excludesVision Center managers
Plan Enrollment periods and coverage effective dates
• Medical
• HMO plans
• Dental (enrollment is for two full
calendar years)
• Vision
• Critical illness insurance
• Accident insurance
• AD&D
Initial enrollment period:
You must enroll in coverage between the date of your
firstpaycheck and the day prior to the date your coverage
iseffective.
When coverage is effective:
Your coverage is effective the first day of the calendar
month during which your 89th day of continuous full-
timeemployment falls.
NOTE: IRS regulations
require that the pretax
benefit elections you
make stay in effect
through the full Plan
year (Jan. 1 – Dec.31)
unless you have a status
change event.
• Company-paid life insurance You are automatically enrolled on the first day of the calendar month during which your
89th day of continuous full-time employment falls.
• Resources for Living
• Business travel accident insurance
You are automatically enrolled on your date of hire.
• Shor-term disability basic plan (not
available to associates who work in
California, Hawaii, NewJersey, and
RhodeIsland; different coverage is
available in NewYork)
You are automatically enrolled on your 12-month anniversary.
• Optional associate life insurance
• Optional dependent life insurance
Initial enrollment period:
You must enroll in coverage between the date of your first paycheck and the day prior
to the date your coverage is effective.
When coverage is effective:
• If you enroll during your initial enrollment period:
– The guaranteed issue amount is effective on the later of your enrollment date or the
first day of the calendar month during which your 89th day of continuous full-time
employment falls.
– When you enroll for more than the guaranteed issue amount, you must provide
Proof of Good Health for yourself and/or your spouse/parner. Following Prudential’s
approval, your coverage is effective upon the later of the date of Prudential’s
approval or the first day of the calendar month during which your 89th day of
continuous full-time employment falls.
• If you enroll after your initial enrollment period: You may enroll or drop coverage
at any time during the year, but Proof of Good Health is required if you enroll
(or increase your coverage) at any time after your initial enrollment period. Your
coverage is effective upon the date of approval by Prudential.
• Shor-term disability enhanced plan
(not available to associates who work
in California, Hawaii, NewJersey, and
Rhode Island; NewYork shor-term
disability enhanced plan is available in
NewYork)
• Long-term disability (LTD) plan
• LTD enhanced plan
Initial enrollment period:
You must enroll in coverage between the date of your first
paycheck and the first day of the calendar month during
which your 89th day of continuous full-time employment falls.
When coverage is effective:
If you enroll during your initial enrollment period, coverage
is effective on your 12-month anniversary.
If you enroll after your
initial enrollment period,
your coverage is effective
12 months after the
date you enroll or, in the
event of a status change,
12months after the date
of the event.
See page 298
* If you are classified as a “California pharmacist” in payroll systems, you are eligible for the benefits listed in the char for
managementassociates.
NOTE: Some benefits require you to meet the definition of active work. See the “Active work” or “actively at work” section in
thischapter for information.

Eligibility and enrollment
14
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
FULLTIME HOURLY VISION CENTER MANAGERS
Plan Enrollment periods and coverage effective dates
• Medical
• HMO plans
• Dental (enrollment is for two full
calendar years)
• Vision
• Critical illness insurance
• Accident insurance
• AD&D
Initial enrollment period:
You must enroll in coverage between the date of your first
paycheck and prior to the 60th day after your date of hire.
When coverage is effective:
Your coverage is effective on your date of hire.
NOTE: IRS regulations
require that the pretax
benefit elections you
make stay in effect
through the full Plan
year (Jan. 1 – Dec. 31)
unless you have a status
change event.
• Resources for Living
• Company-paid life insurance
• Business travel accident insurance
• Shor-term disability basic plan
(not available to associates in
California, Hawaii, NewJersey, and
RhodeIsland; different coverage is
available in NewYork)
You are automatically enrolled on your date of hire.
• Optional associate life insurance
• Optional dependent life insurance
Initial enrollment period:
You must enroll in coverage between the date of your first paycheck and prior to the
60th day after your date of hire.
When coverage is effective:
• If you enroll during your initial enrollment period:
– The guaranteed issue amount is effective on your enrollment date.
– When you enroll for more than the guaranteed issue amount, you must provide Proof
of Good Health for yourself and/or your spouse/parner. Your coverage is effective
upon the date of Prudential’s approval.
• If you enroll after your initial enrollment period: You may enroll or drop coverage
at any time during the year, but Proof of Good Health is required if you enroll (or
increase your coverage) at any time after your initial enrollment period. Your coverage
is effective upon the date of approval by Prudential.
• Shor-term disability enhanced
plan (not available to associates
who work in California, Hawaii,
NewJersey, and RhodeIsland;
NewYork shor-term disability
enhanced plan is available in
NewYork)
• Long-term disability (LTD) plan
• LTD enhanced plan
Initial enrollment period:
You must enroll between the date of your first paycheck and
prior to the 60th day after your date of hire.
When coverage is effective:
If you enroll during your initial enrollment period, coverage is
effective as of your date of hire.
If you enroll after
your initial enrollment
period, your coverage is
effective 12 months after
the date you enroll or,
in the event of a status
change, 12 months after
the date of the event.
See page 298
NOTE: Some benefits require you to meet the definition of active work. See the “Active work” or “actively at work” section in
thischapter for information.

Eligibility and enrollment
15
PARTTIME HOURLY AND TEMPORARY ASSOCIATES
Plan Enrollment periods and coverage effective dates
• Medical*
• HMO plans
• Dental (enrollment is for two full
calendar years)
• Vision
• Critical illness insurance
• Accident insurance
• AD&D
Initial enrollment period: See page 300
You must enroll in coverage during the 60-day period
beginning with your 52-week anniversary date.
When coverage is effective:
Your coverage is effective the first day of the second
calendar month following your 52-week anniversary date.*
NOTE: IRS regulations
require that the pretax
benefit elections you
make stay in effect
through the full Plan
year (Jan. 1 – Dec. 31)
unless you have a status
change event.
* To be eligible for medical coverage, par-time hourly and temporary associates must work
the required number of hours and pass the initial or annual benefits eligibility check (as
applicable) described under Associate eligibility earlier in this section. Par-time hourly
pharmacists hired before February 1, 2012, are exempt from this requirement.
• Resources for Living
• Business travel accident insurance
You are automatically enrolled on your date of hire.
• Optional associate life insurance
• Optional dependent life insurance
Initial enrollment period: See page 300
You must enroll in coverage during the 60-day period beginning with your 52-week
anniversary date.
When coverage is effective:
• If you enroll during your initial enrollment period:
– Your guaranteed issue amount becomes effective on the later of your enrollment date
or the first day of the second calendar month following your 52-week anniversary date.
– When you enroll for more than the guaranteed issue amount, you must complete Proof
of Good Health. Your coverage is effective upon the later of the date of Prudential’s
approval or your benefits eligibility date.
• If you enroll after your initial enrollment period: You may enroll or drop coverage
at any time during the year, but Proof of Good Health is required if you enroll (or
increase your coverage) at any time after your initial enrollment period. Your coverage
is effective upon the date of approval by Prudential.
NOTE: Par-time hourly and temporary associates may only cover their eligible dependent children and may not cover their
spouse/parners. Disability coverage and company-paid life insurance are not available to par-time hourly and temporary associates.

Eligibility and enrollment
16
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
PARTTIME TRUCK DRIVERS
Plan Enrollment periods and coverage effective dates
• Medical
• HMO plans
• Dental (enrollment is for two full
calendar years)
• Vision
• Critical illness insurance
• Accident insurance
• AD&D
Initial enrollment period:
You must enroll in coverage between the date of your first
paycheck and the day prior to your effective date.
When coverage is effective:
Your coverage is effective the first day of the calendar month
during which your 89th day of continuous employment falls.
NOTE: IRS regulations
require that the pretax
benefit elections you
make stay in effect
through the full Plan
year (Jan. 1 – Dec. 31)
unless you have a status
change event.
• Resources for Living
• Business travel accident insurance
You are automatically enrolled on your date of hire.
• Optional associate life insurance
• Optional dependent life insurance
Initial enrollment period:
You must enroll in coverage between the date of your first paycheck and the day prior to
your effective date.
When coverage is effective:
• If you enroll during your initial enrollment period:
– The guaranteed issue amount is effective on your enrollment date or the first day of
the calendar month during which your 89th day of continuous employment falls.
– When you enroll for more than the guaranteed issue amount, you must provide
Proof of Good Health. Your coverage will be effective upon the later of the date of
Prudential’s approval or your benefits eligibility date.
• If you enroll after your initial enrollment period: You may enroll or drop coverage
at any time during the year, but Proof of Good Health is required if you enroll (or
increase your coverage) at any time after your initial enrollment period. Your coverage
is effective upon the date of approval by Prudential.
Par-time truck drivers are not subject to the benefits eligibility checks described earlier in this chapter.
NOTE: Par-time hourly and temporary associates may only cover their eligible dependent children and may not cover their
spouse/parners. Disability coverage and company-paid life insurance are not available to par-time hourly and temporary associates.

Eligibility and enrollment
17
MANAGEMENT ASSOCIATES
Includes management trainees, California pharmacists,* and full-time truck drivers
Plan Enrollment periods and coverage effective dates
• Medical
• HMO plans
• Dental (enrollment is for two full
calendar years)
• Vision
• Critical illness insurance
• Accident insurance
• AD&D
Initial enrollment period:
You must enroll between the date of your first paycheck
and prior to your 60th day after your date of hire.
When coverage is effective:
Your coverage is effective on your date of hire.
NOTE: IRS regulations
require that the pretax
benefit elections you
make stay in effect
through the full Plan
year (Jan. 1 – Dec. 31)
unless you have a status
change event.
• Resources for Living
• Company-paid life insurance
• Business travel accident insurance
• Shor-term disability plan**
You are automatically enrolled on your date of hire.
• Optional associate life insurance
• Optional dependent life insurance
Initial enrollment period:
You must enroll in coverage between the date of your first paycheck and prior to the
60th day after your date of hire.
When coverage is effective:
• If you enroll during your initial enrollment period:
– Your guaranteed issue amount is effective on your enrollment date
– When you enroll for more than the guaranteed issue amount, you must provide Proof
of Good Health for yourself and/or your spouse/parner. Your coverage is effective
upon the date of approval by Prudential.
• If you enroll after your initial enrollment period: You may enroll or drop coverage
at any time during the year, but Proof of Good Health is required if you enroll (or
increase your coverage) at any time after your initial enrollment period. Your coverage
is effective upon the date of approval by Prudential.
• Long-term disability (LTD) plan
• LTD enhanced plan
• Truck driver LTD plan
• Truck driver LTD enhanced plan
Initial enrollment period:
You must enroll between the date of your first paycheck and prior to the 60th day after
your date of hire.
When coverage is effective:
If you enroll during your initial enrollment period, coverage is effective as of your date
ofhire.
If you enroll after your initial enrollment period, coverage under the LTD plan is effective
after a 12-month wait from the date you enroll or, in the event of a status change, 12 months
after the date of the event. Under the truck driver LTD plan, you must provide Evidence of
Insurability and coverage is effective the first day of the pay period after People Services
receives approval from Lincoln.
See page 298
* Pharmacists who work in California and have the designation of “California pharmacist” in payroll systems are eligible for the benefits
listed here for management associates.
** The salaried and truck driver shor-term disability plans are not covered by ERISA and are not par of the Associates’ Health and
Welfare Plan.
NOTE: Some benefits require you to meet the definition of active work. See the “Active work” or “actively at work” in
thischapter for information.
Eligibility and enrollment
18
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Paying for your benefits
When you have enrolled for coverage, payroll deductions
for the premium amounts are withheld from your paycheck
to pay for your benefits coverage. The first paycheck after
your effective date generally reflects deductions for each
day you had coverage during that pay period. If a pay period
spans two calendar years, your deductions will reflect the
amount for the prior year through December 31 and the
new amount for the new year, prorated for the number of
days covered from January 1 until the end of the pay period.
Your payroll deductions reflect your cost for benefits for
the payroll period stated on your paycheck. So, if you are
paid biweekly (every other week), your deductions pay for
coverage for the previous two weeks. Deductions are based
on biweekly pay periods (except in Rhode Island, which has
weekly pay periods).
If your payroll deductions are not sufficient to pay any
portion of a premium due, you are responsible for paying
any unpaid premiums to the extent the premiums would
have been paid if withheld as a payroll deduction. If you
owe premiums for benefits coverage, any check issued by
the company (e.g., paid time off, incentive, etc.), including
during or after a leave of absence, will have premiums
deducted on an after-tax basis, as permitted by law.
Be sure to check your statement of earnings and
deductions on your pay stub to verify that the proper
deductions are being taken. You can view your paycheck
stub the Monday before payday by going to Online Paystub
on One.Walmart.com or Workday for Jet associates. If
you believe the coverage or deductions are not correct
on your pay stub, call People Services immediately at
800-421-1362. Requests for a review of premiums paid are
considered if submitted within one year from the date of
a possible overpayment. A premium reconciliation up to a
maximum of one year will be completed.
Many of your Plan benefits are paid for with pretax dollars,
which means your payroll deductions for coverage are
deducted from your paycheck before federal and, in most
cases, state taxes are withheld. Because Social Security
taxes are not withheld on any pretax dollars you spend for
benefits, amounts you pay for benefits with pretax dollars
are not counted as wages for Social Security purposes.
As a result, your future Social Security benefits may be
reducedsomewhat.
If you are enrolled in the Saver Plan, you may also be eligible
to contribute to a health savings account on a pretax basis.
See the Health savings account chapter for information.
Deductions for premiums or contributions that are past due
or for retroactive elections generally must be made on an
after-tax basis.
WHEN SPECIAL ARRANGEMENTS ARE
NECESSARY TO MAINTAIN COVERAGE
If your payroll deductions are not sufficient to pay any portion
of a premium due, you are responsible, regardless of your job
status, for making arrangements to pay any unpaid premiums
to the extent the premiums would have been paid if withheld as
payroll deductions. These terms apply to the following benefits:
• Medical
• Dental
• Vision
• Critical illness insurance
• Accident insurance
• Optional associate life insurance
• Optional dependent life insurance
• Accidental death and dismemberment (AD&D)
Your premium payments for coverage during a pay period
are due by the close of that pay period and will be made
on an after-tax basis. Your failure to make your premium
payments by the due date may result in your coverage being
canceled due to nonpayment of premiums.
To avoid interruption or cancellation of coverage, premium
payments can be made in advance through the automated
system with a VISA, MasterCard, American Express, or
Discover credit or debit card by logging into the payment
portal on One.Walmart.com. You can also call People
Services at 800-421-1362 and say “make a payment.” To
confirm the premium amount owed, call People Services.
Payments of premiums may also be made by check or
money order and should be made payable to Associates’
Health and Welfare Trust and mailed to:
Walmart People Services
P.O. Box 1039
Department 3001
Lowell, Arkansas 72745
To ensure proper credit when you send payment, include
your name and WIN number on your payment. Please allow
10–14 days for processing.
If you have a break in coverage as the result of a
coveragecancellation:
• If you are an active associate, you will not be able to enroll
again until the next Annual Enrollment or until you have a
valid status change event.
• If you are on a leave of absence and return to active work
within one year of the leave, you will be enrolled for the
same coverage (or the most similar coverage offered
under the Plan). Your coverage will be effective the first
day of the pay period that you return to active work.

Eligibility and enrollment
19
• If you are on a leave of absence and return to active
work after one year of the leave, you will be considered a
newly eligible associate and will be required to meet any
applicable eligibility requirements before you may enroll
for coverage.
TAX CONSEQUENCES OF PARTNER BENEFITS
Partners generally do not qualify as spouses or dependents
for federal income tax purposes. Therefore, the value of
company-provided medical (including the HRA) coverage
that relates to your partner, or your partner’s children, is
generally considered imputed income and taxable to you.
This value is subject to change from year to year as the
underlying benefit values change. Tax and other withholdings
are made from your paycheck and the value of those
benefits is included in your Form W-2. During any period
in which partner benefits that have an imputed income are
maintained by you but you are not receiving a paycheck from
the company, the company reserves the right to collect your
portion of FICA tax liability directly from you.
These rules do not apply if your partner satisfies the
requirements to be considered your tax dependent under
the Internal Revenue Code.
Tobacco rates
You can receive lower tobacco-free rates for medical
and prescription drug coverage, optional associate life
insurance, optional dependent life insurance for a spouse,
and critical illness insurance if:
• You and/or a covered spouse/partner do not use tobacco
and are considered to be “tobacco free,” or
• You and/or a covered spouse/partner use tobacco and
you complete participation in a quit-tobacco program of
your choice between the time of Annual Enrollment and
December 31, 2020. Alternatively, if you call Walmart’s
Quit Tobacco program at 866-577-7169, the program
will work with you (and, if you wish, your doctor) to find
aprogram that is right for you.
“Tobacco free” means that you (and/or your covered
spouse/partner) do not use tobacco in any form —
cigarettes, cigars, pipes, snuff, or chewing tobacco. For
purposes of establishing tobacco-free rates, being “tobacco
free” also means that you do not use e-cigarettes or any
such nicotine-delivery devices.
You will be asked to attest to your tobacco use at your
initial enrollment, to determine your eligibility for tobacco-
free rates for your initial eligibility period, and each year
at Annual Enrollment, to determine your eligibility for
tobacco-free rates for the next calendar year.
The statement below is shown on the screen when you enroll
for benefits and answer the questions regarding tobacco use:
“Our expectation is that you will use correct and accurate
information when applying for or enrolling in benefits. If you
do not, you may be subject to the loss of benefits and/or loss
of employment.”
To review the company’s policy about intentional
dishonesty, please refer to the Statement of Ethics, which
can be found on One.Walmart.com. If we receive a report of
abuse, we will conduct an ethics investigation.
Please note that your eligibility for tobacco-free rates can
be established only at your initial enrollment and at Annual
Enrollment. If you become tobacco-free during the year,
you will not become eligible for tobacco-free rates until the
following calendar year.
The company offers the Quit Tobacco program at no cost to
all associates. For information, see Quit Tobacco program in
The medical plan chapter.
IMPORTANT
If you are a first-time enrollee, you must
actively complete an online enrollment session
at One.Walmart.com or on Workday for Jet
associates to receive tobacco-free rates.
Continuing benefit coverage if you
go on a leave of absence
While you are on a Family Medical Leave Act (FMLA) leave,
personal leave, or military leave, you retain any medical,
dental, vision, critical illness insurance, accident insurance,
optional associate life, optional dependent life, AD&D, and
Resources for Living coverage that you had on the day
immediately preceding the first day of the leave. Coverage
generally is maintained on the same terms and conditions as
if you had continued to work during the leave.

Eligibility and enrollment
20
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
During your leave, you are responsible for paying any unpaid
premiums to the extent the premiums would have been
paid if withheld as a payroll deduction. See When special
arrangements are necessary to maintain coverage earlier in
this chapter for details.
If you cancel your coverage during your FMLA, personal or
military leave and return to work, you may contact People
Services at 800-421-1362 within 60 days of returning to
work to reinstate your coverage. See the If you go on a
leave of absence section in the respective chapters for each
of the above-named benefits to learn more.
Decisions about leaves of absence are made by the
company, not the Plan.
Contact a member of your management team or Sedgwick
for additional information about FMLA, personal or military
leave, or refer to the company’s Leave of Absence Policy on
One.Walmart.com for specific information. You may also
contact your personnel representative if you have questions
about the FMLA, personal or military leave policy.
PAYING FOR BENEFITS WHILE ON
ALEAVEOFABSENCE
To continue benefit coverage while on a leave of absence,
you must pay your premiums on an after-tax basis. For
details on making payments while on a leave of absence,
refer to When special arrangements are necessary to
maintain coverage earlier in this chapter.
If you are on a leave of absence and you owe premiums for
benefits coverage, any check issued by the company (e.g.,
paid time off, incentive, etc.) will have premiums deducted
on an after-tax basis, as permitted by law.
Continuing benefit coverage
whiledisabled
If you are a salaried associate or truck driver receiving
short-term disability benefits, please see the Salaried short-
term disability plan or the Truck driver short-term disability
plan chapter for information about continuing benefit
coverage while disabled.
If you are receiving disability benefits and wish to continue
your coverage under other benefits offered under the Plan,
this chart describes how your coverage costs are handled:
TO MAINTAIN COVERAGE UNDER THESE BENEFITS
• Medical
• Dental
• Vision
• Critical illness insurance
• Accident insurance
• Optional associate life
• Optional dependent life
• AD&D
WHILE YOU ARE RECEIVING…
Shor-term
disability benefits
for full-time hourly
associates (except
for those who work
in CA, HI, NJ, NY,
and RI)
Your premiums for the coverage
listed above will be deducted from
your short-term disability benefit
checks (issued through the company
payroll system).
NOTE: You are not required to pay
shor-term disability enhanced plan
or long-term disability plan premiums
from any shor-term disability benefit
payments you receive.*
Shor-term
disability benefits
for full-time hourly
associates who
work in CA, HI, NJ,
NY, or RI
Your premiums for the coverage
listed above will not be deducted
from your shor-term disability
benefit checks because they are not
issued through the company payroll
system. You must make premium
payments each pay period or risk
cancellation of your benefits.
NOTE: You are not required to pay
shor-term disability enhanced plan
or long-term disability plan premiums
from any shor-term disability benefit
payments you receive.*
• Long-term
disability benefits
• Truck driver
long-term
disability benefits
Your premiums for the coverage
listed above will not be deducted
from your long-term disability
benefit checks because they are not
issued through the company payroll
system. You must make premium
payments each pay period or risk
cancellation of your benefits.
NOTE: You are not required to pay
shor-term disability enhanced plan
or long-term disability plan premiums
from any long-term disability benefit
payments you receive.*
* If you receive any other earnings, including bonuses, through
the company payroll systems while you are receiving disability
benefits, your applicable disability premiums will be withheld
from those payments.

Eligibility and enrollment
21
Status change events
Certain benefits can be changed at any time during
the year, but others can be changed only during Annual
Enrollment or if you have a status change event, as follows:
• Optional associate life insurance and optional dependent
life insurance can be added or dropped at any time.
• The AMP, HMO plans, the eComm PPO Plan, dental,
vision, AD&D, critical illness insurance, and accident
insurance can be changed only during Annual Enrollment
unless you have a status change event.
• Short-term disability enhanced, long-term disability, and
truck driver long-term disability can be dropped at any
time. (The change becomes effective the day after you
drop coverage.) They can be added only at Annual
Enrollment unless you have a status change event.
See page 298
Federal tax law generally requires that your pretax benefit
choices remain in effect for the entire calendar year for
which the choice was made. This does not apply to pretax
contributions to a health savings account, which can be
changed at any time.
You may make certain coverage changes if you experience
a status change event. A status change event is an event
that allows you to make changes to your coverage outside
of annual or initial enrollment. Any change you make must
be directly related to the impact of the event on your
benefits or eligibility. In other words, there must be a logical
relationship between the event and the change you request.
For example, if you (the associate) and your spouse divorce,
you can only drop coverage for your spouse. Changing
another dependent’s coverage due to this event would not
be permitted.
When you have a status change event (including the loss or
gain of other coverage as described below), any changes to
your coverage must be made within 60 days from the date
of the event.
Status change events include:
• Events that change your marital status:
– Marriage
– Death of your spouse
– Divorce (including the end of a common-law marriage
in states where a divorce decree is required to end a
recognized common-law marriage)
– Annulment, or
– Legal separation.
• Events that change your domestic partnership status:
– Commencement of domestic parnership
– Termination of domestic parnership, or
– Death of your domestic parner.
• Events that change the status of a legal relationship with
a person other than a spouse or domestic partner, as
specified in the definition of partner:
– Commencement of legal relationship
– Termination of legal relationship, or
– Death of the other person to whom you are joined in
legal relationship.
• Events that change the number of your dependents:
– Birh
– Adoption
– Placement for adoption
– Death of a dependent
– Gain of legal custody of a dependent
– Loss of legal custody of a dependent for whom you have
previously been awarded legal custody or guardianship
by a judge
– Your paternity test result
– A dependent loses eligibility, such as at the end of the
month in which the dependent reaches age 26, or
– You receive valid documentation establishing the
eligibility of a dependent previously deemed ineligible.
• Employment changes experienced by you, your spouse/
partner or your dependent:
– Going on or returning from an approved leave
ofabsence
– Gain or loss of coverage due to staring or ending
employment
– A change in work location that affects your medical
coverage. If the change affects your medical
coverage options (such as if a new HMO, local plan,
or the eComm PPO Plan is offered), you will have
60 calendar days from your transfer to submit a
request to change your coverage. If you transfer work
locations where your medical benefits are affected
and do not submit a request, you will automatically be
enrolled in a predetermined plan
– Gain or loss of coverage under any other employer
plan,or
– If you are a par-time hourly or temporary associate and
your hours are reduced such that you work an average
of less than 30 hours per week (regardless of whether
the reduction in hours affects your eligibility for medical
benefits) and you intend to enroll in another plan that
provides minimum essential coverage that is effective
no later than the first day of the second month following
the month that your medical coverage under the Plan
would end, you may drop coverage in the AMP or an
HMO plan or the eComm PPO Plan.
Eligibility and enrollment
22
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
LOSS OF COVERAGE
• You may add medical, dental, or vision coverage for you
and/or your eligible dependents if:
– You originally declined coverage because you and/or
your dependents had COBRA coverage and that
COBRA coverage has ended (nonpayment of premiums
is not sufficient for this purpose)
– You and/or your dependents had non-COBRA medical
coverage and the other coverage has terminated due to
your loss of eligibility, or
– Employer contributions toward other coverage
haveterminated.
• A change may also be allowed if there is a significant loss
of coverage under the benefits available at the company,
such as if an HMO plan in your area discontinues service.
The Plan determines when a significant loss of coverage
has occurred.
• If you or your eligible dependents lose coverage under a
governmental plan including Medicaid or a state children’s
health insurance plan, an educational institution’s plan,
or a tribal government plan, you can add coverage under
the AMP, an HMO plan, the eComm PPO Plan, accident
insurance, or critical illness insurance within 60 days of the
loss of coverage. (This does not apply to loss of coverage
under a Health Insurance Marketplace plan.)
• A change may also be allowed pursuant to a court order.
GAIN OF OTHER COVERAGE
• If an order resulting from a divorce, legal separation,
annulment, or change in legal custody (including a
Qualified Medical Child Support Order — See Qualified
Medical Child Support Orders (QMCSO) later in this
chapter) requires you to provide medical, dental, and/or
vision coverage for your eligible dependent child, you
may add coverage for your eligible dependent child (and
yourself, if you are not already covered). If the order
requires your spouse, former spouse, or other person
to provide medical, dental, and/or vision coverage for
your dependent child, and that other coverage is in fact
provided, you may drop coverage for the dependent child.
• If you are eligible for a Special Enrollment Period to enroll
in a qualified health plan through a Marketplace, or you seek
to enroll in a qualified health plan through a Marketplace
during the Marketplace’s annual enrollment, as described
on the next page in Changes in your coverage following a
status change event, you can drop coverage in the AMP, an
HMO plan, or the eComm PPO Plan in accordance with
rules set forth by the Department of Health and Human
Services. You and any dependent who cease coverage
under the Plan must provide evidence of your enrollment
rights and state that you intend to enroll in a qualified
health plan through a Marketplace effective no later than
the day immediately following the last day of your coverage
under the AMP, HMO plan, or eComm PPO Plan.
• If you or your eligible dependents are enrolled in the AMP,
an HMO plan, the eComm PPO Plan, accident insurance,
or critical illness insurance, you can drop that coverage
if you or your dependents become entitled to Medicare
or Medicaid benefits or coverage under a state children’s
health insurance plan.
NOTE: If you or your eligible dependents gain eligibility
under a governmental plan (other than Medicare, Medicaid,
TRICARE, or a state children’s health insurance plan), you
cannot drop the AMP, an HMO plan, the eComm PPO Plan,
accident insurance, or critical illness insurance coverage
except during Annual Enrollment.
ADDITIONAL CIRCUMSTANCES IN WHICH YOU
MAY CHANGE YOUR BENEFITS
In addition to the circumstances under which you may
change your benefits, as listed on the previous page, there
are additional circumstances, including cost changes,
reduction of coverage, and/or additions/improvements of
a benefit option, in which the Plan may allow you to make
mid-year changes to your elections.
If you or your eligible dependents become eligible for
assistance under Medicaid or a state children’s health
insurance plan to help you pay for Plan coverage, you
must request coverage under the Plan within 60 days of
becoming eligible for assistance.
For information about circumstances in which you may change
your benefits, contact People Services at 800-421-1362.
CHANGES IN YOUR COVERAGE FOLLOWING A
STATUS CHANGE EVENT
When you have a status change event, you must request
your change within 60 days from the date of the event.
Unless otherwise provided in the Plan, if you add a spouse or
partner or other eligible dependent due to a status change
event, each person must individually meet any applicable
benefit waiting period (for example, for transplant coverage
or weight loss surgery) and will be subject to applicable
Plan limitations. If you change medical plans due to a status
change event, your annual deductible and out-of-pocket
maximum will reset, and you will be responsible for meeting
the new deductible and out-of-pocket maximum in their
entirety. If you change from the Contribution Plan to another
plan, your HRA balance under the Contribution Plan will be
forfeited. See The medical plan chapter for information.
If you are covered as a dependent and move to coverage as an
associate during the Plan year, you will generally not receive
credit under the AMP for expenses incurred prior to the date
of the change. However, if you are covered as a dependent
and you experience a qualifying event that affects your
status as a dependent and makes you eligible for your own
continuation coverage under COBRA, you will receive credit
Eligibility and enrollment
23
toward your deductibles and out-of-pocket maximum under
the AMP for expenses incurred as a covered dependent. You
will also receive credit toward any waiting periods.
The Plan reserves the right to request additional necessary
documentation to show proof of a status change event.
HIPAA SPECIAL ENROLLMENT FOR
MEDICALCOVERAGE
Under the Health Insurance Portability and Accountability
Act of 1996 (HIPAA), you also may have a right to a special
enrollment in medical coverage under the Plan if you lose
other coverage or acquire a dependent. These events are
described in the list of status change events and include:
• If you decline enrollment for yourself or your dependents
because of other health insurance or group health
plan coverage, you may be able to enroll yourself, and
if you choose, your dependents in this Plan if you or
your dependents lose eligibility for that coverage (or if
the employer stops contributing toward your or your
dependents’ other coverage). You must request enrollment
within 60 days after your or your dependents’ other
coverage ends (or after the employer stops contributing
toward the other coverage).
• If you have a new dependent as a result of marriage, birth,
adoption, or placement for adoption, you may be able to
enroll yourself and/or your eligible dependents. You must
request enrollment within 60 days.
• If you or a dependent is no longer eligible for coverage
under Medicaid or a state children’s health plan, or you
or a dependent becomes eligible for assistance for Plan
coverage under Medicaid or a state children’s health
plan, you must request enrollment within 60 days of the
prior coverage terminating or your becoming eligible for
assistance. Such coverage will be effective upon the date
you enroll in the Plan.
• To request special enrollment or obtain more information,
refer to the information earlier in this chapter regarding
status change events or contact People Services at
800-421-1362.
HOW TO CHANGE YOUR ELECTIONS DUE TO
ASTATUS CHANGE EVENT
You can make changes online within 60 days of the event
on One.Walmart.com or Workday for Jet associates for
statuschanges due to:
• Adoption
• Birth
• Commencement of domestic partnership
• Commencement of legal relationship with a person other
than your spouse or domestic partner
• Death of spouse/partner
• Divorce or legal separation
• Gain or loss of legal custody
• Gain or loss of coverage by you, your dependent(s), or your
eligible spouse/partner
• Going on leave of absence
• Marriage
• Returning from leave of absence
• Special enrollment period
• Termination of domestic partnership, or
• Termination of legal relationship with a person other than a
spouse or domestic partner.
For all other types of status changes, call People Services at
800-421-1362.
If your status change event is the birth of a dependent, the
Plan will accept provider billing charges related to the birth
as notice that the newborn is to be added as a dependent
under your coverage, so long as the charges are submitted
within 60 days of the birth.
If you are seeking to add a dependent as a result of
marriage, commencement of a domestic partnership, or
commencement of a legal relationship with a person other
than a spouse or domestic partner, but the individual to be
added as a dependent dies before you have provided notice
of the status change event, the individual will not be added
to your coverage as a dependent.
Changes to your coverage are effective on the event date
or on the day after the status change event date. If a change
is made due to your unpaid leave of absence, the change is
effective as of the effective date of your leave of absence.
This does not apply to optional associate life insurance,
optional dependent life insurance, short-term disability
enhanced plan coverage, long-term disability, or truck
driver long-term disability; see the respective chapters for
information about effective dates.
If your status change results in an increase in your coverage
costs, such as if you change from associate-only coverage
to associate + dependent coverage, the increased charge
will be deducted from your pay after you notify People
Services of your status change event and will be retroactive
to the effective date of your new coverage. These
retroactive deductions are made on an after-tax basis.
If you do not notify People Services or go online and make a
change within 60 days of the status change event, you cannot
add or drop coverage until the next Annual Enrollment or
until you have a different status change event.
Also, if the status change event is due to your dependent
losing eligibility, your dependent will lose the right to elect
COBRA coverage for medical, dental, and/or vision benefits if
you do not notify People Services of the event within 60 days.
Similarly, if the status change event is due to your divorce, the

Eligibility and enrollment
24
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
termination of a domestic partnership, or the termination of
a legal relationship with a person other than your spouse or
domestic partner, your former spouse/partner will lose the
right to elect COBRA coverage for medical, dental, and/or
vision benefits if People Services is not notified of the event
within 60 days. See the COBRA chapter for more information.
If your job classification changes
Transitioning from one job classification to another may
affect your eligibility for certain benefits.
If you are classified as a part-time hourly or temporary
associate and your classification is changed to full-time,
you will be eligible for full-time benefits, as described in
thechart below.
If your job classification changes from full-time associate to
part-time or temporary associate or part-time truck driver,
your spouse/partner will no longer be eligible for medical,
dental, vision, dependent life insurance, AD&D, critical
illness, or accident coverage. You will no longer be eligible
for company-paid life or disability coverage. If this change
results in your spouse/partner or other dependent losing
coverage, see the COBRA chapter to learn how you and/or
your eligible dependents may be able to continue medical,
dental, and vision coverage.
NOTE: If your job classification changes to part-time hourly
or temporary associate, see the earlier section of this
chapter titled Part-time hourly and temporary associates:
eligibility checks for medical benefits.
Transferring from one job classification to another
PARTTIME HOURLY OR TEMPORARY ASSOCIATES TRANSFERRING TO A FULLTIME HOURLY POSITION CONTINUED
Your status at transition Coverage effective dates and details
You have been continuously
employed for more than
52weeks and were eligible for
medical coverage under the
Plan as a par-time hourly or
temporary associate immediately
prior to your transition
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective either the first day of the pay period in which your transition
occurs or the date of your enrollment, depending on your choice and on the manner in
which you enroll:
– If you enroll online, coverage is effective the date you enroll.
– If you enroll by phone call to People Services, you may choose for coverage to be effective
either the first day of the pay period in which your transition occurs or the date you
enroll. Once you enroll, premiums are deducted from your paycheck on an after-tax basis
retroactively to your effective date.
• You are enrolled automatically in the shor-term disability basic plan effective the first day
of the pay period in which your transition occurs, and are eligible to enroll in the shor-term
disability enhanced plan at the same time, unless you work in the states of California,
Hawaii, New Jersey, or Rhode Island, which have legally mandated disability plans.
(Associates in New York can enroll in the NY shor-term disability enhanced plan.)
• You are enrolled automatically in company-paid life insurance on the first day of the pay
period in which your transition occurs.
• You are eligible to enroll in optional dependent life insurance for your spouse/parner:
– If you enroll during the enrollment period following your transition in status, your
guaranteed issue amount becomes effective on your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must complete Proof of Good
Health for your spouse/parner. Your coverage becomes effective upon the date of approval
by Prudential.
• You are eligible to enroll in long-term disability (LTD) plan coverage.
• If you are currently enrolled in medical, dental, vision, AD&D, critical illness, and/or
accident insurance, you can increase your coverage type to associate + spouse/parner or
associate + family as a result of your change in job classification. If you are not currently
enrolled in medical, dental, vision, AD&D, critical illness, and/or accident insurance, you
may enroll only in associate + spouse/parner or associate + family coverage as a result of
your change in job classification, until the next Annual Enrollment or until you have a valid
status change event. You may not select associate-only or associate + child(ren) coverage as
a result of your change in job classification, as you were already eligible for those coverage
types as a par-time hourly or temporary associate.
(Continued on the next page)

Eligibility and enrollment
25
PARTTIME HOURLY OR TEMPORARY ASSOCIATES TRANSFERRING TO A FULLTIME HOURLY POSITION CONTINUED
Your status at transition Coverage effective dates and details
You have been continuously
employed for more than
52weeks and were not eligible
for medical coverage under
the Plan as a par-time hourly
associate immediately prior to
your transition
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective either the first day of the pay period in which your transition
occurs or the date of your enrollment, depending on your choice and on the manner in
which you enroll:
– If you enroll online, coverage is effective the date you enroll.
– If you enroll by phone call to People Services, you may choose for coverage to be effective
either the first day of the pay period in which your transition occurs or the date you
enroll. Once you enroll, premiums are deducted from your paycheck on an after-tax basis
retroactively to your effective date.
• You become eligible to enroll in medical coverage. See The medical plan chapter
forinformation.
• You are enrolled automatically in the shor-term disability basic plan effective the first day
of the pay period in which your transition occurs, and are eligible to enroll in the shor-term
disability enhanced plan at the same time, unless you work in the states of California,
Hawaii, New Jersey, or Rhode Island, which have legally mandated disability plans.
(Associates in New York can enroll in the NY shor-term disability enhanced plan.)
• You are enrolled automatically in company-paid life insurance on the first day of the pay
period in which your transition occurs.
• You are eligible to enroll in optional dependent life insurance for your spouse/parner:
– If you enroll during the enrollment period following your transition in status, your
guaranteed issue amount becomes effective on your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must complete Proof of Good
Health for your spouse/parner. Your coverage becomes effective upon the date of approval
by Prudential.
• You are eligible to enroll in long-term disability (LTD) plan coverage.
• If you are currently enrolled in dental, vision, AD&D, critical illness, and/or accident
insurance, you can increase your coverage type to associate + spouse/parner or associate
+ family as a result of your change in job classification. If you are not currently enrolled
in dental, vision, AD&D, critical illness, and/or accident insurance, you may enroll only in
associate + spouse/parner or associate + family coverage as a result of your change in job
classification, until the next Annual Enrollment or until you have a valid status change event.
You may not select associate-only or associate + child(ren) coverage as a result of your
change in job classification, as you were already eligible for those coverage types as a par-
time hourly or temporary associate.
(Continued on the next page)

Eligibility and enrollment
26
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
PARTTIME HOURLY OR TEMPORARY ASSOCIATES TRANSFERRING TO A FULLTIME HOURLY POSITION CONTINUED
Your status at transition Coverage effective dates and details
You have been continuously
employed for more than 90 days
but less than 52 weeks
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective (with the exception of shor-term and long-term disability)
either the first day of the pay period in which your transition occurs or the date of your
enrollment, depending on your choice and on the manner in which you enroll:
– If you enroll online, coverage is effective the date you enroll.
– If you enroll by phone call to People Services, you may choose for coverage to be effective
either the first day of the pay period in which your transition occurs or the date you
enroll. Once you enroll, premiums are deducted from your paycheck on an after-tax basis
retroactively to your effective date.
• You are eligible to enroll in medical, dental, vision, AD&D, optional associate and dependent
life insurance, critical illness, and accident insurance. See the respective chapters in this
Summary Plan Description for more information.
• You are enrolled automatically in company-paid life insurance on the first day of the pay
period in which your transition occurs.
• If you enroll for optional associate life insurance or optional dependent life insurance for
your spouse/parner during the enrollment period following your transition in status:
– Your guaranteed issue amount becomes effective on your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must provide Proof of Good
Health for you and/or your spouse/parner. Your coverage is effective upon the date of
approval by Prudential.
• You are automatically enrolled in company-provided shor-term disability basic coverage
effective on the 12-month anniversary of your date of hire, and are eligible to enroll in
the shor-term disability enhanced plan during the 60-day period beginning on the first
day of the pay period in which your transition occurs, unless you work in the states of
California, Hawaii, New Jersey, or Rhode Island, which have legally mandated disability
plans. (Associates in New York can enroll in the NY shor-term disability enhanced plan.)
You are also eligible to enroll in the long-term disability (LTD) plan during the 60-day period
beginning on the first day of the pay period in which your transition occurs. Your coverage
under the shor-term disability enhanced plan (if applicable) and LTD plan is effective on the
12-month anniversary of your date of hire. If you enroll in the shor-term disability enhanced
plan or LTD plan at any time after this enrollment period following your transition in status,
your coverage is not effective until after an additional 12-month waiting period from the
date you enroll. (If you enroll due to a status change event, the waiting period begins as of
the date of the event.)
See page 298
(Continued on the next page)

Eligibility and enrollment
27
PARTTIME HOURLY OR TEMPORARY ASSOCIATES TRANSFERRING TO A FULLTIME HOURLY POSITION CONTINUED
Your status at transition Coverage effective dates and details
You have been continuously
employed for less than 90days
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective (with the exception of shor-term and long-term disability)
asfollows:
– If you enroll online or by calling People Services during the 60-day period but before
the first day of the month during which your 89th day of continuous employment falls,
your effective date is the first day of the calendar month during which your 89th day of
continuous employment falls.
– If you enroll online during the 60-day period but after the first day of the month during
which your 89th day of continuous employment falls, your effective date is the date you
enroll. However, if you enroll by calling People Services you may choose to have your
benefits effective the first day of the month during which your 89th day of continuous
employment falls.
• Premiums may be deducted from your paycheck on an after-tax basis retroactively to your
effective date of coverage if you enroll after your 90th day of continuous employment.
• You are eligible to enroll in medical, dental, vision, AD&D, optional associate and dependent
life insurance, critical illness, and accident insurance. See the respective chapters in this
Summary Plan Description for more information.
• You are enrolled automatically in company-paid life insurance on the first day of the
calendar month during which your 89th day of continuous employment falls.
• If you enroll for optional associate life insurance or optional dependent life insurance for
your spouse/parner during your initial enrollment period:
– Your guaranteed issue amount becomes effective on your enrollment date or your eligibility
date, whichever is later.
– If you enroll for more than the guaranteed issue amount, you must provide Proof of Good
Health for you and/or your spouse/parner. Your coverage is effective upon the date of
approval by Prudential.
• You are automatically enrolled in company-provided shor-term disability basic coverage
effective on the 12-month anniversary of your date of hire, and are eligible to enroll in
the shor-term disability enhanced plan during the 60-day period beginning on the first
day of the pay period in which your transition occurs, unless you work in the states of
California, Hawaii, New Jersey, or Rhode Island, which have legally mandated disability
plans. (Associates in New York can enroll in the NY shor-term disability enhanced plan.)
You are also eligible to enroll in the long-term disability (LTD) plan during the 60-day period
beginning on the first day of the pay period in which your transition occurs. Your coverage
under the shor-term disability enhanced plan (if applicable) and LTD plan is effective on the
12-month anniversary of your date of hire. If you enroll in the shor-term disability enhanced
plan or LTD plan at any time after this enrollment period following your transition in status,
your coverage is not effective until after an additional 12-month waiting period from the
date you enroll. (If you enroll due to a status change event, the waiting period begins as of
the date of the event.)
See page 298

Eligibility and enrollment
28
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
PARTTIME HOURLY OR TEMPORARY ASSOCIATES TRANSFERRING TO MANAGEMENT CONTINUED
Your status at transition Coverage effective dates and details
You have been continuously
employed for more than
52weeks and were eligible
for medical coverage under
the Plan as a par-time hourly
associate immediately prior to
your transition
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective either the first day of the pay period in which your transition
occurs or the date of your enrollment, depending on your choice and on the manner in
which you enroll:
– If you enroll online, coverage is effective the date you enroll.
– If you enroll by phone call to People Services, you may choose for coverage to be effective
either the first day of the pay period in which your transition occurs or the date you
enroll. Once you enroll, premiums are deducted from your paycheck on an after-tax basis
retroactively to your effective date.
• You are enrolled automatically in company-paid life insurance on the first day of the pay
period in which your transition occurs.
• The maximum amount of optional associate life insurance coverage you can select increases
from $200,000 to $1,000,000. (If you increase your coverage, Proof of Good Health is
required; coverage is effective upon the date of approval by Prudential.)
• You are eligible to enroll in optional dependent life insurance for your spouse/parner.
• If you enroll for optional dependent life insurance for your spouse/parner during the
enrollment period following your transition in status:
– Your guaranteed issue amount becomes effective on your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must provide Proof of Good
Health for your spouse/parner. Your coverage is effective upon the date of approval by
Prudential.
• If you are currently enrolled in medical, dental, vision, AD&D, critical illness, and/or
accident insurance, you can increase your coverage type to associate + spouse/parner or
associate + family as a result of your change in job classification. If you are not currently
enrolled in medical, dental, vision, AD&D, critical illness, and/or accident insurance, you
may enroll only in associate + spouse/parner or associate + family coverage as a result of
your change in job classification, until the next Annual Enrollment or until you have a valid
status change event. You may not select associate-only or associate + child(ren) coverage as
a result of your change in job classification, as you were already eligible for those coverage
types as a par-time hourly or temporary associate.
• You are enrolled automatically in the salaried shor-term disability plan or truck driver
shor-term disability plan, as appropriate, effective the first day of the pay period in which
your transition occurs.
• You are eligible to enroll in the long-term disability (LTD) plan or truck driver LTD plan, as
appropriate. See the respective chapters in this Summary Plan Description for information.
(Continued on the next page)

Eligibility and enrollment
29
PARTTIME HOURLY OR TEMPORARY ASSOCIATES TRANSFERRING TO MANAGEMENT CONTINUED
Your status at transition Coverage effective dates and details
You have been continuously
employed for more than
52weeks and were not eligible
for medical coverage under
the Plan as a par-time hourly
associate immediately prior to
your transition
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective either the first day of the pay period in which your transition
occurs or the date of your enrollment, depending on your choice and on the manner in
which you enroll:
– If you enroll online, coverage is effective the date you enroll.
– If you enroll by phone call to the People Services Center, you may choose for coverage to
be effective either the first day of the pay period in which your transition occurs or the date
you enroll. Once you enroll, premiums are deducted from your paycheck on an after-tax
basis retroactively to your effective date.
• You are eligible to enroll in medical coverage and long-term disability (LTD) or truck driver LTD,
as appropriate. See the respective chapters in this Summary Plan Description for information.
• You are enrolled automatically in company-paid life insurance on the first day of the pay
period in which your transition occurs.
• The maximum amount of optional associate life insurance coverage you can select will
increase from $200,000 to $1,000,000. (If you increase your coverage, Proof of Good
Health is required; coverage is effective upon the date of approval by Prudential.)
• You are eligible to enroll in optional dependent life insurance for your spouse/parner:
– If you enroll during the enrollment period following your transition in status, your
guaranteed issue amount will become effective on your enrollment date.
–If you enroll for more than the guaranteed issue amount, you must complete Proof
of Good Health for your spouse/parner. Your coverage is effective upon the date of
approval by Prudential.
• If you are currently enrolled in dental, vision, AD&D, critical illness, and/or accident
insurance, you can increase your coverage type to associate + spouse/parner or associate
+ family as a result of your change in job classification. If you are not currently enrolled
in dental, vision, AD&D, critical illness, and/or accident insurance, you may enroll only in
associate + spouse/parner or associate + family coverage as a result of your change in
job classification, until the next Annual Enrollment or until you have a valid status change
event. You may not select associate-only or associate + child(ren) coverage as a result of
your change in job classification, as you were already eligible for those coverage types as
a par-time hourly or temporary associate.
• You are enrolled automatically in the salaried shor-term disability plan or truck driver
shor-term disability plan, as appropriate, effective the first day of the pay period in which
your transition occurs.
• You are eligible to enroll in the long-term disability (LTD) plan or truck driver LTD plan, as
appropriate. See the respective chapters in this Summary Plan Description for information.
(Continued on the next page)

Eligibility and enrollment
30
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
PARTTIME HOURLY OR TEMPORARY ASSOCIATES TRANSFERRING TO MANAGEMENT CONTINUED
Your status at transition Coverage effective dates and details
You have been continuously
employed for less than 52weeks
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective either the first day of the pay period in which your transition
occurs or the date of your enrollment, depending on your choice and on the manner in
which you enroll:
– If you enroll online, coverage is effective the date you enroll.
– If you enroll by phone call to the People Services Center, you may choose for coverage to
be effective either the first day of the pay period in which your transition occurs or the date
you enroll. Once you enroll, premiums are deducted from your paycheck on an after-tax
basis retroactively to your effective date.
• You are eligible to enroll in medical, dental, vision, AD&D, optional associate and dependent
life insurance, critical illness insurance, accident insurance, and long-term disability (LTD)
or truck driver LTD, as appropriate. See the respective chapters in this Summary Plan
Description for information.
• You are enrolled automatically in company-paid life insurance on the first day of the pay
period in which your transition occurs.
• If you enroll for optional associate life insurance or optional dependent life insurance during
the enrollment period following your transition in status:
– Your guaranteed issue amount becomes effective on your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must complete Proof of Good
Health for you and/or your spouse/parner. Your coverage becomes effective upon the date
of approval by Prudential.
• You are enrolled automatically in the salaried shor-term disability plan or truck driver
shor-term disability plan, as appropriate, effective the first day of the pay period in which
your transition occurs.
• You are eligible to enroll in the long-term disability (LTD) plan or truck driver LTD plan, as
appropriate. See the respective chapters in this Summary Plan Description for information.

Eligibility and enrollment
31
FULLTIME HOURLY ASSOCIATES TRANSFERRING TO MANAGEMENT
Your status at transition Coverage effective dates and details
You have been continuously
employed for 90 days or more
• The maximum amount of optional associate life insurance coverage you can select increases
from $200,000 to $1,000,000. (If you increase your coverage, Proof of Good Health is
required; coverage is effective upon the date of approval by Prudential.)
• The terms of your shor-term disability coverage change as follows:
– You are enrolled automatically in the salaried shor-term disability plan or truck driver
shor-term disability plan, as appropriate, effective the first day of the pay period in which
your transition occurs.
– Your eligibility for coverage under the shor-term disability plan for hourly associates
terminates, effective the first day of the pay period in which your transition occurs. (This
includes both shor-term disability basic and enhanced coverage, and applies whether you
were already covered under the plan or were awaiting the star of coverage.)
• If you elected long-term disability (LTD) or truck driver LTD during your initial enrollment
period, coverage is effective as of the first day of the pay period in which your transition occurs.
You have been continuously
employed for less than 90 days
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective either the first day of the pay period in which your transition
occurs or the date of your enrollment, depending on your choice and on the manner in
which you enroll:
– If you enroll online, coverage is effective the date you enroll.
– If you enroll by phone call to the People Services Center, you may choose for coverage to
be effective either the first day of the pay period in which your transition occurs or the date
you enroll. Once you enroll, premiums are deducted from your paycheck on an after-tax
basis retroactively to your effective date.
• You are eligible to enroll in medical, dental, vision, AD&D, optional associate and dependent
life insurance, long-term disability (LTD) or truck driver LTD insurance, critical illness
insurance, and accident insurance. See the respective chapters in this Summary Plan
Description for more information.
• If you enroll for optional associate life insurance or optional dependent life insurance during
your initial enrollment period:
– Your guaranteed issue amount becomes effective on your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must complete Proof of Good
Health for you and/or your spouse/parner. Your coverage becomes effective upon the date
of approval by Prudential.
• The terms of your shor-term disability coverage change as follows:
– You are enrolled automatically in the salaried shor-term disability plan or truck driver
shor-term disability plan, as appropriate, effective the first day of the pay period in which
your transition occurs.
– Your eligibility for coverage under the shor-term disability plan for hourly associates or
truck driver shor-term disability terminates, effective the first day of the pay period in
which your transition occurs. (This includes both shor-term disability basic and enhanced
coverage, and applies whether you were already covered under the plan or were awaiting
the star of coverage.)
FULLTIME HOURLY VISION CENTER MANAGERS TRANSFERRING TO MANAGEMENT
Coverage effective dates and details
• The terms of your shor-term disability coverage change as follows:
– You are enrolled automatically in the salaried shor-term disability plan effective the first
day of the pay period in which your transition occurs.
– Your eligibility for coverage under the shor-term disability plan for hourly associates
terminates, effective the first day of the pay period in which your transition occurs. (This
includes both shor-term disability basic and enhanced coverage, and applies whether you
were already covered under the plan or were awaiting the star of coverage.)

Eligibility and enrollment
32
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
MANAGEMENT ASSOCIATES TRANSFERRING TO FULLTIME HOURLY CONTINUED
Your status at transition Coverage effective dates and details
Within 60 days of your date
of hire and before you have
enrolled for benefits
You have 60 days to enroll from the date your transition in status occurs.
• The terms of your benefit plans as a full-time hourly associate are effective as of the
date of your transition in status. You can find details about benefits available to full-time
hourly associates in the Enrollment and effective dates by job classification chars earlier
in this chapter.
• Premiums are deducted from your paycheck on an after-tax basis retroactively to your
coverage effective date.
• Salaried shor-term disability or truck driver shor-term disability coverage is canceled
effective the first day of the pay period in which your transition occurs.
• You are automatically enrolled in shor-term disability enhanced coverage for hourly
associates as of the first day of the pay period in which your transition occurs, unless you
work in the states of California, Hawaii, New Jersey, or Rhode Island, which have legally
mandated disability plans. (Associates in New York are automatically enrolled in the NY
shor-term disability enhanced plan.) See the Shor-term disability for full-time hourly
associates chapter for more information.
• You are eligible to enroll in the long-term disability plan.
See page 300
• If you enroll for optional associate life insurance or optional dependent life insurance:
– Your guaranteed issue amount becomes effective on your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must provide Proof of Good
Health for you and/or your spouse/parner, as applicable. Your coverage is effective upon
the date of approval by Prudential.
Within 60 days of your date of
hire and after you have enrolled
for benefits
You have 60 days to enroll from the date your transition in status occurs.
• The terms of your benefit plans as a full-time hourly associate are generally effective as of
the date of your transition in status. You can find details about benefits available to full-time
hourly associates in the Enrollment and effective dates by job classification chars earlier in
this chapter.
• Premiums are deducted from your paycheck as of your coverage effective date for any new
benefit election you make. For benefit plans in which you were already enrolled, premiums
are adjusted to your full-time hourly status on an after-tax basis retroactively to the date of
your transition in status.
• Optional associate life insurance amounts selected over $200,000 are reduced to $200,000.
• If you were not previously enrolled in optional associate life insurance or optional
dependent life insurance and choose to enroll in either plan after your transition in status:
– Your guaranteed issue amount becomes effective as of your enrollment date.
– If you enroll for more than the guaranteed issue amount, you must provide Proof of Good
Health for you and/or your spouse/parner, as applicable. Your coverage is effective upon
the date of approval by Prudential.
• Salaried shor-term disability coverage or truck driver shor-term disability is canceled
effective the first day of the pay period in which your transition occurs.
• You are automatically enrolled in shor-term disability enhanced coverage for hourly
associates as of the first day of the pay period in which your transition occurs, unless
you work in the states of California, Hawaii, New Jersey, or Rhode Island, which have
legally mandated disability plans. (Associates in New York are automatically enrolled in the
NY shor-term disability enhanced plan.) See the Shor-term disability for full-time hourly
associates chapter for more information.
• You are eligible to enroll in the long-term disability plan.
See page 300
(Continued on the next page)
Eligibility and enrollment
33
MANAGEMENT ASSOCIATES TRANSFERRING TO FULLTIME HOURLY CONTINUED
Your status at transition Coverage effective dates and details
More than 60 days after your
date of hire
If you are currently enrolled for benefits, you have 60 days to make a new enrollment from
the date your transition occurs.
• The terms of your benefit plans as a full-time hourly associate are effective as of the date
of your transition in status. You can find details about benefits available to full-time hourly
associates in the Enrollment and effective dates by job classification chars earlier in this
chapter. You can make limited changes only in plans you’re already enrolled in. You cannot
add or drop benefits until the next Annual Enrollment or until you have a valid status change
event. If you are not currently enrolled for benefits, you cannot enroll until the next Annual
Enrollment or until you have a valid status change event.
• Optional associate life insurance amounts selected over $200,000 are reduced to $200,000.
• You may enroll in optional associate life insurance or optional dependent life insurance at
any time during the year, but Proof of Good Health will be required if you enroll or increase
coverage after your initial enrollment period has ended.
• Salaried shor-term disability coverage or truck driver shor-term disability is canceled
effective the first day of the pay period in which your transition occurs.
• You are automatically enrolled in shor-term disability enhanced coverage for hourly
associates as of the first day of the pay period in which your transition occurs, unless
you work in the states of California, Hawaii, New Jersey, or Rhode Island, which have
legally mandated disability plans. (Associates in New York are automatically enrolled in
the NY shor-term disability enhanced plan.) If you had not enrolled for benefits before
your transition in status, your coverage under the LTD plan will not be effective until the
12-month anniversary of your date of hire. See the Shor-term disability for full-time hourly
associates and Long-term disability chapters for more information.
See page 300
FULLTIME HOURLY ASSOCIATES TRANSFERRING TO PARTTIME HOURLY OR TEMPORARY
Your status at transition Coverage effective dates and details
You have met your eligibility
waiting period and were eligible
for coverage under the Plan
immediately prior to your
transition
• If you are enrolled in medical, dental, vision, AD&D, critical illness, and/or accident
insurance coverage, your coverage type is automatically adjusted to associate-only or
associate + child(ren) (depending on whether you have covered dependents) effective
thefirst day of the pay period after your transition occurs. Associate + spouse/parner
andassociate + family coverage are not available to par-time associates.
• Company-paid life, dependent life for your spouse/parner and disability coverage are
canceled effective the first day of the pay period after your transition occurs. You may be
able to conver your company-paid life insurance and your dependent’s life insurance to
individual policies.

Eligibility and enrollment
34
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
FULLTIME HOURLY ASSOCIATES TRANSFERRING TO PARTTIME HOURLY OR TEMPORARY
Your status at transition Coverage effective dates and details
You have NOT met your
eligibility waiting period
You have 60 days to enroll from the first day of the pay period in which your transition occurs.
• Your coverage is effective as follows:
– If you enroll online or by calling People Services during the 60-day period but before
the first day of the month during which your 89th day of continuous employment falls,
your effective date is the first day of the calendar month during which your 89th day of
continuous employment falls.
– If you enroll online during the 60-day period but after the first day of the month during
which your 89th day of continuous employment falls, your effective date is the date you
enroll. However, if you enroll by calling People Services, you may choose to have your
benefits effective the first day of the month during which your 89th day of continuous
employment falls.
• Premiums may be deducted from your paycheck on an after-tax basis retroactively to your
effective date of coverage if you enroll after your 90th day of continuous employment.
• You are eligible to enroll in medical, dental, vision, AD&D, optional associate life insurance
and dependent life insurance for your children, critical illness, and accident insurance. See
the respective chapters in this Summary Plan Description for more information.
• If you enroll for optional associate life insurance during your initial enrollment period:
– Your guaranteed issue amount becomes effective on your enrollment date or your
eligibility date, whichever is later.
– If you enroll for more than the guaranteed issue amount, you must complete Proof of Good
Health. Your coverage becomes effective upon the date of approval by Prudential.
• If you enrolled in the shor-term disability enhanced plan for full-time hourly associates
during your initial enrollment period but you have not reached the 12-month anniversary of
your date of hire, coverage under the plan will not take effect as of that date.
• If you enrolled in the LTD or LTD enhanced plan during your initial enrollment period,
coverage will not take effect.
• You are eligible to enroll in associate-only or associate + child(ren) coverage types.

Eligibility and enrollment
35
MANAGEMENT ASSOCIATES TRANSFERRING TO PARTTIME HOURLY OR TEMPORARY
Your status at transition Coverage effective dates and details
You are within 60 days of
your date of hire but have not
enrolled for benefits
You have 60 days to enroll from the date your transition in status occurs.
• You can find details about benefits for par-time hourly and temporary associates in the
Enrollment and effective dates by job classification chars earlier in this chapter.
• Premiums are deducted from your paycheck on an after-tax basis retroactively to your
coverage effective date.
• Company-paid life coverage and disability coverage are canceled effective the first day of
the pay period after your transition occurs. You may be able to conver your company-paid
life insurance to an individual policy.
You are within 60 days of your
date of hire and you have
enrolled for benefits
You have 60 days to make a new enrollment from the date your transition in status occurs.
• You can find details about benefits for par-time hourly and temporary associates in the
Enrollment and effective dates by job classification chars earlier in this chapter.
• Premiums will be adjusted to your new benefit elections on an after-tax basis retroactively
to your coverage effective date.
• Optional associate life insurance amounts selected over $200,000 will be reduced
to$200,000.
• Company-paid life, optional dependent life for your spouse/parner, and disability coverage
will be canceled effective the first day of the pay period after your transition occurs.
You may be able to conver your company-paid life insurance and your dependent’s life
insurance to individual policies.
More than 60 days have passed
since your date of hire
If you are currently enrolled for benefits, you have 60 days to make a new enrollment from
the date your transition occurs.
• The terms of your benefit plans as a par-time hourly or temporary associate are effective
as of the date of your transition. You can find details about benefits for par-time hourly
and temporary associates in the Enrollment and effective dates by job classification chars
earlier in this chapter. You can make limited changes only in plans you’re already enrolled in.
You cannot add or drop benefits until the next Annual Enrollment or until you have a valid
status change event.
• Optional associate life insurance amounts selected over $200,000 are reduced to $200,000.
• Company-paid life, optional dependent life for your spouse/parner, and disability coverage
are canceled effective the first day of the pay period after your transition occurs. You may
be able to conver your company-paid life insurance and your dependent’s life insurance to
individual policies.
If you are not currently enrolled for benefits, you cannot enroll until the next Annual Enrollment
or until you have a valid status change event.
You have 60 days from the date of your transition to a part-time hourly, temporary, or part-time truck driver position to
elect any other medical coverage option available to you and/or your dependents under the Plan. You may not drop medical,
dental, AD&D, critical illness, accident, or vision coverage for yourself and/or your dependent children during the Plan year. If
you do not elect to change your coverage option within the 60-day enrollment period, you will continue to be covered by the
same full-time medical option, but excluding spouse/partner coverage. You may change elections during any future Annual
Enrollment or as the result of a status change event.

Eligibility and enrollment
36
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Qualified Medical Child Suppor
Orders (QMCSO)
A QMCSO is a court or administrative agency order
requiring an associate or other parent or guardian to
provide health care coverage for eligible dependents after
a divorce or child custody proceeding. Federal law requires
the Plan to provide medical, dental, and/or vision benefits
to any eligible dependent of a Plan participant required by a
court order meeting the qualifications of a QMCSO.
You can obtain the written procedures for determining
whether an order meets the federal requirements, free
of charge, by contacting Medical Support Services at
877-930-5607.
Once the Plan determines an order to be a QMCSO,
coverage begins the first day of the pay period in which the
Plan receives the order, unless another date is specified in
the order. If you are eligible for the medical, dental, and/or
vision plan and did not elect coverage before the order was
received, you will be enrolled in the 2020 default Premier
Plan with associate + child(ren) coverage at the tobacco
rate, unless the QMCSO specifies otherwise. If you are in
the state of Hawaii, the default plan is Health Plan Hawaii
(HMSA). If you are in a location where the eComm PPO Plan
is offered, the default plan is the Saver Plan.
If you were enrolled for coverage before the order was
received, your child will be added under your existing
coverage, with the following exceptions:
• If you are enrolled in an HMO plan or one of the local
plans, your coverage will change to the Premier Plan,
under which the child would have coverage regardless of
where he or she lives.
• If you are enrolled in the eComm PPO Plan, your coverage
will change to the Saver Plan, under which the child would
have coverage regardless of where he or she lives.
• If you are in the state of Hawaii, your coverage will change
to HMSA.
You have 60 days to call Medical Support Services at
877-930-5607 to select an alternative medical plan.
If the Plan receives a QMCSO 61–90 days prior to you
satisfying your initial waiting period, the order will be put
into effect when your initial waiting period is satisfied. If
the Plan receives a QMCSO more than 90 days prior to
you satisfying your initial waiting period, the order will be
held until coverage takes effect. When the third-party
administrator enforces coverage for a court-ordered
dependent, information regarding the dependent is shared
only with the legal custodian. If you have questions, contact
Medical Support Services at 877-930-5607.
See page 301
DROPPING OR CHANGING QMCSO COVERAGE
You may drop the court-ordered QMCSO coverage if the
following applies:
• The QMCSO is terminated by a court or administrative
agency order — you must request your change within
60days.
• The QMCSO is rescinded by a court or administrative
agency order.
• A child who is the subject of the court order reaches the
age identified in the state issuing the court order for
termination of coverage. Contact your state child support
enforcement agency for details.
If the QMCSO is terminated or rescinded by court or
administrative agency order, the court-ordered coverage
will end on the date specified in the order or the first day
of the pay period in which the Plan receives the order. If
the order to rescind coverage is received, coverage will
be retroactively withdrawn and you will be returned to the
coverage status you had before the QMCSO was enforced,
to the extent permitted by law.
When a QMCSO terminates, you may drop medical, dental,
and/or vision coverage for the children named in the
QMCSO. However, you may not drop your own coverage
or coverage for any dependent voluntarily added after the
QMCSO became effective unless there is a change in status
for you or your child, or during Annual Enrollment. For
dental coverage, you may not drop associate-level coverage
at Annual Enrollment or due to a status change event unless
you have been covered for two full calendar years.
When your Plan coverage ends
Coverage under the Associates’ Health and Welfare Plan for
you and your dependents ends on the earliest of thefollowing:
• At termination of your employment
• The last day of coverage for which premiums were paid, if
you fail to pay your premiums within 30 days of the date
your premium is due
• On the date of your (the associate’s) death, for you and
your dependents
• On the date of death for a deceased dependent
• On the date you, a dependent spouse/partner, or child
loses eligibility
• When the benefit is no longer offered by Walmart
• Upon misrepresentation or the fraudulent submission of a
claim for benefits or eligibility
• Upon an act of fraud or a misstatement of a material fact, or
• The day after you drop coverage.
Premium deductions are withheld from your final paycheck
since your deductions pay for coverage for the previous
twoweeks.
Eligibility and enrollment
37

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Eligibility and
benefitsfor
associatesin Hawaii
Eligibility waiting periods for medicalcoverage 40
Medical coverage options for Hawaiiassociates 40
Paying premiums during a leave of absence for Hawaii associates 40
Enrollment and effective dates for Hawaii associates 41

Eligibility and benefitsfor associatesin Hawaii
39
Eligibility and benefits for associates in Hawaii
Because you work in Hawaii, there are some special rules about medical and shor-term disability
benefits. Those differences are described in this chapter. The rest of the information in this 2020
Associate Benefits Book applies to you.
RESOURCES
Find What You Need Online Other Resources
Health Plan Hawaii (HMSA) Go to hmsa.com 808-948-6372
Kaiser Foundation Health Plan Go to kaiserpermanente.org 800-966-5955
Enroll in Walmar benefits Go to One.Walmar.com Call People Services at 800-421-1362
Repor a claim under the legally mandated
state disability insurance program
Go to One.Walmar.com or directly to
MyLincolnPoral.com
Call Lincoln at 800-492-5678
Notify People Services within 60 days of a
status change event
Go to One.Walmar.com Call People Services at 800-421-1362
What you need to know as a Hawaii associate
• Associates in Hawaii have two medical coverage options: Health Plan Hawaii (HMSA) and the Kaiser Foundation Health Plan.
For information about these medical options, go to One.Walmart.com.
• Because Hawaii has a legally mandated disability plan, the company short-term disability plan for hourly associates is not
anoption for associates in Hawaii.
• Initial eligibility periods for coverage vary for Hawaii associates based on their employment status, as described in this chapter.
Eligibility and benefitsfor associatesin Hawaii
40
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Eligibility waiting periods for
medicalcoverage
MANAGEMENT ASSOCIATES
If you are a management associate in Hawaii, the eligibility
terms described in the Eligibility and enrollment chapter
apply to you; management associates and management
trainees in Hawaii are eligible for medical coverage on their
date of hire. For details on eligibility and enrollment in all
of the benefits available under the Associates’ Health and
Welfare Plan, refer to the chart for management associates
in the Enrollment and effective dates by job classification
section of the Eligibility and enrollment chapter.
FULLTIME HOURLY, PARTTIME HOURLY
ANDTEMPORARYASSOCIATES
If you are a full-time hourly associate (including full-time
hourly pharmacists and field supervisor positions in stores
and clubs) or a part-time hourly and temporary associate in
Hawaii, you are subject to legally mandated rules governing
eligibility for medical coverage. For benefits other than
medical, you follow the eligibility terms described in the
Eligibility and enrollment chapter. For details, refer to the
appropriate chart under Enrollment and effective dates for
Hawaii associates later in this chapter.
Medical coverage options for
Hawaiiassociates
Associates in Hawaii have two coverage options:
• Health Plan Hawaii (HMSA), and
• Kaiser Foundation Health Plan.
For details about these medical options, go to
One.Walmart.com.
Paying premiums during a leave of
absence for Hawaii associates
Because the associate portion of your medical premium
is wage-based, no premium is due from you if you are not
receiving wages during an approved leave of absence.
The only premium due for medical coverage while you
are on an approved leave of absence with no wages is the
dependent portion of your premium. All other coverage
options requirepayment as described in the Eligibility and
enrollment chapter.
Under Hawaii law, Walmart must contribute at least 50% of
the premium for your (associate only) medical coverage,
but not for dependent coverage. Associates are required to
pay the rest of the biweekly cost of the premium, but only
up to 1.5% of their wages or 50% of the biweekly cost of the
premium, whichever is less. For example: if your biweekly
wages are $1,000 and you qualify for tobacco-free rates, you
are not required to pay more than $15 biweekly for coverage
(assuming that the entire premium is at least $30 biweekly).

Eligibility and benefitsfor associatesin Hawaii
41
Enrollment and effective dates for Hawaii associates
FULLTIME HOURLY ASSOCIATES
Includes full-time hourly pharmacists and field supervisor positions in stores and clubs
Plan Enrollment Periods and Effective Dates
Medical Initial enrollment period:
You must enroll in coverage between the date of your first
paycheck and the day prior to your effective date.
When coverage is effective:
Your coverage is effective the earlier of:
• The first day of the pay period following a period of working at
least 20 hours per week for four consecutive weeks, or
• The first day of the calendar month during which your 89th day
of continuous full-time employment falls.
NOTE: The pretax
benefit elections
you make stay in
effect through
the full Plan year
(Jan.1 – Dec. 31)
unless you have a
status change event
recognized by IRS
regulations.
Dental (enrollment is for two full
calendar years)
Vision
Critical illness insurance
Accident insurance
AD&D
Initial enrollment period:
You must enroll in coverage between the date of your first
paycheck and the day prior to your effective date.
When coverage is effective:
Your coverage is effective the first day of the calendar
month during which your 89thday of continuous full-time
employmentfalls.
Company-paid life insurance You are automatically enrolled on the first day of the calendar month during which your
89th day of continuous full-time employment falls.
Resources for Living
Business travel accident insurance
You are automatically enrolled on your date of hire.
Optional associate life insurance
Optional dependent life insurance
Initial enrollment period:
You must enroll in coverage between the date of your first paycheck and the day prior to
your effective date.
When coverage is effective:
If you enroll during your initial enrollment period:
• The guaranteed issue amount is effective on the later of your enrollment date or the
first day of the calendar month during which your 89th day of continuous full-time
employment falls.
• When you enroll for more than the guaranteed issue amount, you must provide Proof
of Good Health for yourself and/or your spouse/parner. Following Prudential’s
approval, your coverage is effective upon the later of the date of Prudential’s approval
or the first day of the calendar month during which your 89th day of continuous
full-time employment falls.
If you enroll after your initial enrollment period: You may enroll or drop coverage at any
time during the year, but Proof of Good Health is required if you enroll (or increase your
coverage) at any time after your initial enrollment period. Your coverage is effective
upon the date of approval by Prudential.
Long-term disability (LTD) plan
LTD enhanced plan
Initial enrollment period:
You must enroll in coverage between the date of your first paycheck and the first day of
the calendar month during which your 89th day of continuous full-time employment falls.
When coverage is effective:
If you enroll during your initial enrollment period, coverage is effective on your 12-month
anniversary.
If you enroll after your initial enrollment period, your coverage is effective 12 months after
the date you enroll or, in the event of a status change, 12 months after the date of the event.
See page 298

Eligibility and benefitsfor associatesin Hawaii
42
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
PARTTIME HOURLY AND TEMPORARY ASSOCIATES
Plan Enrollment Periods and Effective Dates
Medical*
* Par-time hourly and temporary
associates in Hawaii are not subject
to the requirements described
under Par-time hourly and
temporary associates: eligibility
checks for medical benefits in the
Eligibility and enrollment chapter.
Initial enrollment period:
You must enroll in coverage between the date of your first
paycheck and the day prior to your effective date.
When coverage is effective:
Your coverage is effective the earlier of:
• The first day of the pay period following a period of working at
least 20 hours per week for four consecutive weeks, or
• The first day of the calendar month during which your 89th day
of continuous employment falls.
NOTE: The pretax
benefit elections
you make stay in
effect through
the full Plan year
(Jan.1 – Dec. 31)
unless you have a
status change event
recognized by IRS
regulations.
Dental (enrollment is for two full
calendar years)
Vision
Critical illness insurance
Accident insurance
AD&D
Initial enrollment period:
You must enroll in coverage between the date of your first
paycheck and the day prior to your effective date.
When coverage is effective:
Your coverage is effective the first day of the calendar month
during which your 89th day of continuous employment falls.
Resources for Living
Business travel accident insurance
You are automatically enrolled on your date of hire.
Optional associate life insurance
Optional dependent life insurance
Initial enrollment period:
You must enroll between the date of your first paycheck and the day prior to your
effective date.
When coverage is effective:
• If you enroll during your initial enrollment period:
– The guaranteed issue amount is effective on the later of your enrollment date or the
first day of the calendar month during which your 89th day of continuous full-time
employment falls.
– When you enroll for more than the guaranteed issue amount, you must provide
Proofof Good Health for yourself and/or your spouse/parner. Following Prudential’s
approval, your coverage is effective upon the later of the date of Prudential’s approval
or the first day of the calendar month during which your 89th day of continuous
full-time employment falls.
• If you enroll after your initial enrollment period: You may enroll or drop coverage
at any time during the year, but Proof of Good Health is required if you enroll (or
increase your coverage) at any time after your initial enrollment period. Your coverage
is effective upon the date of approval by Prudential.
NOTE: Part-time hourly and temporary associates may only cover their eligible dependent children and may not cover
theirspouses/partners. Disability coverage and company-paid life insurance are not available to part-time hourly and
temporary associates.
Management associates: Refer to the chart for management associates in the Enrollment and effective dates by job
classification section of the Eligibility and enrollment chapter.
Eligibility and benefitsfor associatesin Hawaii
43

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The Associates’ Medical Plan (AMP) 46
National plan options 46
Local plan options 50
HMO plan options 53
The eComm PPO Plan 53
The Walmar Premier Plan 54
The Walmar Contribution Plan 57
The Walmar Saver Plan 61
The local plans 65
Administration of the AMP 66
What is covered by the AMP 66
Your provider network 68
Alternate provider networks 69
Preventive care program 70
Prenotification 72
Preauthorization 73
Helping you manage your health 73
Walmar clinics 75
Centers of Excellence 76
When limited benefits apply to theAMP 81
What is not covered by the AMP 85
Filing a medical claim 87
If you have coverage under more than one medical plan 88
Break in coverage 89
When coverage ends 90
If you leave the company and arerehired 90
If you drop coverage and reenroll 90
Other information about the medicalplan 90
The medical plan

The medical plan
45
The medical plan
RESOURCES
Find What You Need Online
By Phone:
Health Care Advisor
Other Resources
Aetna Go to One.Walmar.com or
aetna.com
855-548-2387 Aetna
151 Farmington Avenue
Harford, Connecticut 06156
BlueAdvantage
Administrators of Arkansas
Go to One.Walmar.com or
blueadvantagearkansas.com
866-823-3790 BlueAdvantage Administrators
ofArkansas
P.O. Box 1460
Little Rock, Arkansas 72203-1460
Grand Rounds
(Administration in Norh
Carolina and South
Carolina for BlueAdvantage
Administrators of Arkansas)
855-377-2200
Personal Healthcare
Assistant
HealthSCOPE Benefits Go to One.Walmar.com or
healthscopebenefits.com
800-804-1272
877-385-8786
Expanded telehealth
in MN, CO, and WI
HealthSCOPE Benefits
P.O. Box 16367
Lubbock, Texas 79490-6367
UnitedHealthcare Go to One.Walmar.com or
myuhc.com
888-285-9255 UnitedHealthcare
P.O. Box 30555
Salt Lake City, Utah 84130-0555
Request a paper copy of this
2020 Associate Benefits Book
Call People Services
at 800-421-1362
What you need to know about medical benefits
• If you are eligible for coverage under the Associates’ Medical Plan (AMP), you can choose one of various national
plans or locally available plans. This chapter describes these plan options and where they are available.
• Eligible preventive care services are paid at 100% with no deductible, when received from any network provider.
• Planoptions have no annual or lifetime maximum dollar limits and have no limitations on pre-existing conditions.
• All plan options provide access to a network of providers. Depending on your plan and work location, some options
offer out-of-network coverage.
• Depending on the medical option you choose, you may be eligible for funds in the form of a Health Reimbursement
Account (HRA), which you can use for eligible medical expenses, or a company match to your own tax-free
contributions to a health savings account (HSA), which you can save or use for eligible medical expenses.
• HMO plans are offered in select areas. Refer to your personnel representative to find out if an HMO is available in
your area and to request HMO plan information.
• The eComm PPO Plan is offered in some locations. If the eComm PPO Plan is available at your work location, the
plan benefits are described in materials provided separately by Aetna, the Plan’s third-party administrator.
• The AMP provides prescription drug coverage through the pharmacy benefit. For information, see The pharmacy
benefit chapter.
• If you enroll in the Premier Plan and you have a balance in the Health Reimbursement Account (HRA) associated with
the former HRA Plan option, you can use the remaining funds for limited purposes through the end of 2021, provided
you remain enrolled in the Premier Plan option.

The medical plan
46
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The Associates’ Medical Plan (AMP)
If you are eligible to enroll in the AMP, you may choose from
among several options available under the AMP. The specific
options available to you depend on your work location.
Generally, there are three options available nationwide: the
Walmart Premier Plan, the Walmart Contribution Plan, and
the Walmart Saver Plan. Terms for these national options
vary in specified geographic areas, as described below.
Local plan options are also available in certain regions. All
options available to you are described in this chapter.
If you work in Hawaii, see the chapter titled Eligibility and
benefits for associates in Hawaii.
CHOOSING A COVERAGE LEVEL
When you enroll in the AMP, you also select your coverage
level depending on which, if any, of the eligible dependents
you wish to cover:
• Associate only
• Associate + spouse/partner (except for part-time hourly
associates, temporary associates, or part-time truck drivers)
• Associate + child(ren), or
• Associate + family (except for part-time hourly associates,
temporary associates, or part-time truck drivers).
For information on dependent eligibility and when
dependents can be enrolled, see the Eligibility and
enrollment chapter.
National plan options
The charts on the following pages summarize the coverage
offered under the AMP coverage options.
The national plan options under the AMP are the Premier
Plan, the Contribution Plan, and the Saver Plan. Under each
of these options, plan terms in most areas nationwide are
summarized in the left-hand charts on the following pages.
If you participate in the Premier Plan, Contribution Plan,
or Saver Plan and your work location is within certain
geographic areas, as listed below, these national plans have
slightly different terms from the terms of the national plan
options available in most areas nationwide. These different
terms apply if you work in one of the following areas:
• Central Florida (including Orlando and Tampa)
– Counties within this area are Brevard, Citrus, Hernando,
Hillsborough, Lake, Manatee, Marion, Orange, Osceola,
Pasco, Pinellas, Polk, norhern Sarasota (Sarasota area
only), Seminole, Sumter, and Volusia
• Dallas/Fort Worth
– Counties within this area are Collin, Dallas, Denton, Ellis,
Hunt, Johnson, Kaufman, Parker, Rockwall, Tarrant,
andWise
• Northwest Arkansas
– Counties within this area are Benton, Madison,
andWashington
References throughout this chapter to “central Florida,
Dallas/Fort Worth, and northwest Arkansas” are references
to these listed counties, respectively.
Terms of the national plan options available in central
Florida, Dallas/Fort Worth, and northwest Arkansas are
summarized in the right-hand charts on the following pages.
See page 301 for information replacing the text above
headed National plan options, and the charts on pages 47,
48, and 49.

The medical plan
47
THE WALMART PREMIER PLAN
PREMIER PLAN BENEFITS
PREMIER PLAN BENEFITS (Associates with work locations
incentral FL, Dallas/For Worh, norhwest AR)
Annual deductible
(Individual/Family)
• Network
• Out-of-network
$2,750/$5,500
$5,500/$11,000
Annual deductible
(Individual/Family)
• Network
(Network benefits only)
$2,750/$5,500
Annual out-of-pocket maximum
(Individual/Family)
• Network
• Out-of-network
$6,850/$13,700
None
Annual out-of-pocket maximum
(Individual/Family)
• Network
(Network benefits only)
$6,850/$13,700
Eligible preventive care
• Network provider
• Non-network provider
100% (no deductible)
50% (no deductible)
Eligible preventive care
• Network provider
• Non-network provider
100% (no deductible)
No coverage
Doctor visits
Including routine same-day
diagnostic tests perormed in
doctor’s office
Primary care
• Network provider
• Non-network provider
Specialist
• Network provider
• Non-network provider
100% after $35 copay
50% after deductible
100% after $75 copay
50% after deductible
Doctor visits
Including routine same-day
diagnostic tests perormed in
doctor’s office
Primary care
• Network provider
• Non-network provider
Specialist
• Network provider
• Non-network provider
100% after $35 copay
No coverage
100% after $75 copay
No coverage
Telehealth video visits
Doctor On Demand
• Network provider
• Non-network provider
100% after $4 copay
N/A
Telehealth video visits
Doctor On Demand
• Network provider
• Non-network provider
100% after $4 copay
N/A
Urgent care
• Network provider
• Non-network provider
100% after $75 copay
50% after deductible
Urgent care
• Network provider
• Non-network provider
100% after $75 copay
No coverage
Diagnostic tests
All nonpreventive tests ordered or
perormed outside a doctor’s office
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Diagnostic tests
All nonpreventive tests ordered or
perormed outside a doctor’s office
• Network provider
• Non-network provider
75% after deductible
No coverage
Advanced imaging
MRI, CT scans
• Alternate network provider
• Network provider
• Non-network provider
75% after deductible
50% after deductible
50% after deductible
Advanced imaging
MRI, CT scans
• Alternate network provider
• Network provider
• Non-network provider
75% after deductible
50% after deductible
No coverage
Hospitalization
Inpatient & outpatient care
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Hospitalization
Inpatient & outpatient care
• Network provider
• Non-network provider
75% after deductible
No coverage
Behavioral health
Inpatient & outpatient (facility)
• Network provider
• Non-network provider
Outpatient (provider’s office)
• Network provider
• Non-network provider
75% after deductible
50% after deductible
100% after $35/visit copay
50% after deductible
Behavioral health
Inpatient & outpatient (facility)
• Network provider
• Non-network provider
Outpatient (provider’s office)
• Network provider
• Non-network provider
75% after deductible
No coverage
100% after $35/visit copay
No coverage
Emergency room visit
• Network provider
100% after deductible
and$300copay
Emergency room visit
• Network provider
100% after deductible
and$300copay
For non-network coverage, see The Premier Plan later in chapter. For non-network coverage, see The Premier Plan later in chapter.
Pharmacy
See The pharmacy benefitchapter.
Pharmacy
See The pharmacy benefitchapter.
Centers of Excellence
See the Centers of Excellence
section of this chapter.
Centers of Excellence
See the Centers of Excellence
section of thischapter.
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic
and Walmar Health section
ofthischapter.
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic
and Walmar Health section
ofthischapter.
No benefits are payable for services provided outside the network
except for emergency services.
See pages 302-305

The medical plan
48
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
THE WALMART CONTRIBUTION PLAN
CONTRIBUTION PLAN BENEFITS
CONTRIBUTION PLAN BENEFITS (Associates with work
locations in central FL, Dallas/For Worh, norhwest AR)
Annual deductible
(Individual/Family)
• Network
• Out-of-network
$1,750/$3,500
$3,500/$7,000
Annual deductible
(Individual/Family)
• Network
(Network benefits only)
$1,750/$3,500
Walmar-provided funds
(Individual/Family)
$250/$500
Maximum company
contributiontoHRA
Walmar-provided funds
(Individual/Family)
$250/$500
Maximum company
contributiontoHRA
Annual out-of-pocket maximum
(Individual/Family)
• Network
• Out-of-network
$6,850/$13,700
None
Annual out-of-pocket maximum
(Individual/Family)
• Network
(Network benefits only)
$6,850/$13,700
Eligible preventive care
• Network provider
• Non-network provider
100% (no deductible)
50% (no deductible)
Eligible preventive care
• Network provider
• Non-network provider
100% (no deductible)
No coverage
Doctor visits
Including routine same-day
diagnostic tests perormed in
doctor’s office
Primary care
• Network provider
• Non-network provider
Specialist
• Network provider
• Non-network provider
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Doctor visits
Including routine same-day
diagnostic tests perormed in
doctor’s office
Primary care
• Network provider
• Non-network provider
Specialist
• Network provider
• Non-network provider
75% after deductible
No coverage
75% after deductible
No coverage
Telehealth video visits
Doctor On Demand
• Network provider
• Non-network provider
100% after $4 copay
N/A
Telehealth video visits
Doctor On Demand
• Network provider
• Non-network provider
100% after $4 copay
N/A
Urgent care
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Urgent care
• Network provider
• Non-network provider
75% after deductible
No coverage
Diagnostic tests
All nonpreventive tests ordered or
perormed outside a doctor’s office
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Diagnostic tests
All nonpreventive tests ordered or
perormed outside a doctor’s office
• Network provider
• Non-network provider
75% after deductible
No coverage
Advanced imaging
MRI, CT scans
• Alternate network provider
• Network provider
• Non-network provider
75% after deductible
50% after deductible
50% after deductible
Advanced imaging
MRI, CT scans
• Alternate network provider
• Network provider
• Non-network provider
75% after deductible
50% after deductible
No coverage
Hospitalization
Inpatient & outpatient care
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Hospitalization
Inpatient & outpatient care
• Network provider
• Non-network provider
75% after deductible
No coverage
Behavioral health
Inpatient & outpatient (facility)
• Network provider
• Non-network provider
Outpatient (provider’s office)
• Network provider
• Non-network provider
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Behavioral health
Inpatient & outpatient (facility)
• Network provider
• Non-network provider
Outpatient (provider’s office)
• Network provider
• Non-network provider
75% after deductible
No coverage
75% after deductible
No coverage
Emergency room visit
• Network provider
100% after deductible
and$300copay
Emergency room visit
• Network provider
100% after deductible
and$300copay
For non-network coverage, see The Contribution Plan later in chapter. For non-network coverage, see The Contribution Plan later in chapter.
Pharmacy
See The pharmacy benefitchapter.
Pharmacy
See The pharmacy benefitchapter.
Centers of Excellence
See the Centers of Excellence
section of this chapter.
Centers of Excellence
See the Centers of Excellence
section of thischapter.
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic
and Walmar Health section
ofthischapter.
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic
and Walmar Health section
ofthischapter.
No benefits are payable for services provided outside the network
except for emergency services.
See pages 302-305

The medical plan
49
THE WALMART SAVER PLAN
SAVER PLAN BENEFITS
SAVER PLAN BENEFITS (Associates with work locations
incentral FL, Dallas/For Worh, norhwest AR)
Annual deductible
(Individual/Family)
• Network
• Out-of-network
$3,000/$6,000
$6,000/$12,000
Annual deductible
(Individual/Family)
• Network
(Network benefits only)
$3,000/$6,000
Walmar-provided funds
(Individual/Family)
$350/$700
Maximum company matching
contribution to HSA
Walmar-provided funds
(Individual/Family)
$350/$700
Maximum company matching
contribution to HSA
Annual out-of-pocket maximum
(Individual/Family)
• Network
• Out-of-network
$6,650/$13,300
None
Annual out-of-pocket maximum
(Individual/Family)
• Network
(Network benefits only)
$6,650/$13,300
Eligible preventive care
• Network provider
• Non-network provider
100% (no deductible)
50% (no deductible)
Eligible preventive care
• Network provider
• Non-network provider
100% (no deductible)
No coverage
Doctor visits
Including routine same-day
diagnostic tests perormed in
doctor’s office
Primary care
• Network provider
• Non-network provider
Specialist
• Network provider
• Non-network provider
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Doctor visits
Including routine same-day
diagnostic tests perormed in
doctor’s office
Primary care
• Network provider
• Non-network provider
Specialist
• Network provider
• Non-network provider
75% after deductible
No coverage
75% after deductible
No coverage
Telehealth video visits
Doctor On Demand
• Network provider
• Non-network provider
100% after deductible
and$4copay
N/A
Telehealth video visits
Doctor On Demand
• Network provider
• Non-network provider
100% after deductible
and$4copay
N/A
Urgent care
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Urgent care
• Network provider
• Non-network provider
75% after deductible
No coverage
Diagnostic tests
All nonpreventive tests ordered or
perormed outside a doctor’s office
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Diagnostic tests
All nonpreventive tests ordered or
perormed outside a doctor’s office
• Network provider
• Non-network provider
75% after deductible
No coverage
Advanced imaging
MRI, CT scans
• Alternate network provider
• Network provider
• Non-network provider
75% after deductible
50% after deductible
50% after deductible
Advanced imaging
MRI, CT scans
• Alternate network provider
• Network provider
• Non-network provider
75% after deductible
50% after deductible
No coverage
Hospitalization
Inpatient & outpatient care
• Network provider
• Non-network provider
75% after deductible
50% after deductible
Hospitalization
Inpatient & outpatient care
• Network provider
• Non-network provider
75% after deductible
No coverage
Behavioral health
Inpatient & outpatient (facility)
• Network provider
• Non-network provider
Outpatient (provider’s office)
• Network provider
• Non-network provider
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Behavioral health
Inpatient & outpatient (facility)
• Network provider
• Non-network provider
Outpatient (provider’s office)
• Network provider
• Non-network provider
75% after deductible
No coverage
75% after deductible
No coverage
Emergency room visit
• Network provider
100% after deductible
and$300copay
Emergency room visit
• Network provider
100% after deductible
and$300copay
For non-network coverage, see The Saver Plan later in chapter. For non-network coverage, see The Saver Plan later in chapter.
Pharmacy
See The pharmacy benefitchapter.
Pharmacy
See The pharmacy benefitchapter.
Centers of Excellence
See the Centers of Excellence
section of this chapter.
Centers of Excellence
See the Centers of Excellence
section of thischapter.
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic
and Walmar Health section
ofthischapter.
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic
and Walmar Health section
ofthischapter.
No benefits are payable for services provided outside the network
except for emergency services.
See pages 302-305

The medical plan
50
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Local plan options
Local plan options are available in designated regions, as listed here:
LOCAL PLAN
AVAILABLE FOR ASSOCIATES WITH WORK
LOCATIONS IN DESIGNATED AREAS
THIRDPARTY ADMINISTRATOR
Banner Local Plan Phoenix, Arizona metropolitan area Aetna
Emory Local Plan Atlanta, Georgia metropolitan area HealthSCOPE Benefits
Memorial Hermann Local Plan Houston, Texas metropolitan area HealthSCOPE Benefits
Mercy Arkansas Local Plan Porions of norhwest Arkansas and McDonald
County, Missouri
HealthSCOPE Benefits
Mercy Oklahoma Local Plan Oklahoma City metropolitan area, Ada, and
Ardmore areas
HealthSCOPE Benefits
Mercy Southwest Missouri
(SWMO) Local Plan
Springfield, southwest and east-central Missouri HealthSCOPE Benefits
Mercy St. Louis Local Plan St. Louis metropolitan area and porions of
eastern Missouri
HealthSCOPE Benefits
Ochsner Local Plan New Orleans and Baton Rouge, Louisiana
metropolitan areas
HealthSCOPE Benefits
St. Luke’s Local Plan Boise, Idaho metropolitan area Aetna
UnityPoint Local Plan Porions of Iowa, western Illinois and Peoria,
Illinois area
HealthSCOPE Benefits
Select Local Plan Designated regions nationwide Aetna
See page 306 for information on discontinued local plans.
The local plan options give you access to groups of providers that offer care specifically coordinated to your needs to ensure
that you receive the right high quality care at the right time. Agreements between the Plan and these providers may include
financial incentives to manage care. Additional information about the local plan options can be found under the The local
plans later in this chapter.
The following charts summarize the coverage available under the local plan options. With very limited exceptions, in the
designated areas where a local plan option is available, it will generally replace the Walmart Contribution Plan as a coverage
option for associates if your work location is in those areas. In other words, if a local plan is available in an area that includes
your work location, you will be able to choose coverage under the Walmart Premier Plan, the Walmart Saver Plan, or the
available local plan option, but in most areas you will not be able to choose the Walmart Contribution Plan.
The local plan options do not cover the services of doctors, hospitals, or other providers who are not in the local plan option’s
network, except in cases of emergency services.
For details about coverage under the local plan options, see the summary charts that follow and The local plans later in
this chapter.

The medical plan
51
BANNER LOCAL PLAN AND MERCY SOUTHWEST MISSOURI SW MO LOCAL PLAN
Network Benefits Only
No benefits for services provided outside the network except for emergency services
Annual deductible
Associate only
Associate + dependent(s)
Does not apply to eligible preventive care
$3,000
$6,000
Annual out-of-pocket maximum $6,850 Per person
$13,700 Per family
Eligible preventive care 100%
No deductible
Doctor visits*
Including routine same-day diagnostic x-rays and
tests perormed in the doctor’s office
Primary care physician (PCP) office visit
Specialist office visit*
Behavioral health office visit
Urgent care visit
$35 copay
$75 copay
$35 copay
$75 copay
Diagnostic tests
All nonpreventive tests ordered or perormed
outside a doctor’s office
75% after deductible
Hospitalization
Inpatient, outpatient 75% after deductible
Emergency room visit 100% after deductible and $300 copay
Behavioral health
Inpatient and outpatient
See above for doctor visits
75% after deductible
Telehealth video visits
Doctor On Demand $4 copay
Pharmacy See The pharmacy benefit chapter for details.
Centers of Excellence See the Centers of Excellence section of this chapter for details.
Walmar Care Clinic and Walmar Health See the Walmar Care Clinic and Walmar Health section of this chapter for details.
* The Mercy Southwest Missouri (SW MO) Local Plan offers limited coverage for chiropractic care office visits. There is a maximum of
10 visits per calendar year.

The medical plan
52
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
EMORY, MERCY ARKANSAS, MERCY OKLAHOMA, MERCY ST. LOUIS, ST. LUKE’S, UNITYPOINT, MEMORIAL HERMANN,
AND OCHSNER LOCAL PLANS
Network Benefits Only
No benefits for services provided outside the network except for emergency services
Annual deductible
Associate only
Associate + dependent(s)
Does not apply to eligible preventive care
$1,750
$3,500
Annual out-of-pocket maximum $6,850 Per person
$13,700 Per family
Eligible preventive care 100%
No deductible
Doctor visits*
Including routine same-day diagnostic x-rays and
tests perormed in the doctor’s office
Primary care physician (PCP) office visit
Specialist office visit*
Behavioral health office visit
Urgent care visit
$35 copay
$75 copay
$35 copay
$75 copay
Diagnostic tests
All nonpreventive tests ordered or perormed
outside a doctor’s office
75% after deductible
Hospitalization
Inpatient, outpatient 75% after deductible
Emergency room visit 100% after deductible and $300 copay
Behavioral health
Inpatient and outpatient
See above for doctor visits
75% after deductible
Telehealth video visits
Doctor On Demand $4 copay
Pharmacy See The pharmacy benefit chapter for details.
Centers of Excellence See the Centers of Excellence section of this chapter for details.
Walmar Care Clinic and Walmar Health See the Walmar Care Clinic and Walmar Health section of this chapter for details.
* The Mercy Local Plans for Arkansas, Oklahoma, and St. Louis offer limited coverage for chiropractic care office visits. There is a
maximum of 10 visits per calendar year.
See page 306 for information on discontinued local plans.

The medical plan
53
THE SELECT LOCAL PLAN
Network Benefits Only
No benefits for services provided outside the network except for emergency services
Annual deductible
Associate only
Associate + dependent(s)
Does not apply to eligible preventive care
$2,750
$5,500
Annual out-of-pocket maximum $6,850 Per person
$13,700 Per family
Eligible preventive care 100%
No deductible
Doctor visits
Including routine same-day diagnostic x-rays and
tests perormed in the doctor’s office
Primary care physician (PCP) office visit
Specialist office visit
Behavioral health office visit
Urgent care visit
$35 copay
$75 copay
$35 copay
$75 copay
Diagnostic tests
All nonpreventive tests ordered or perormed
outside a doctor’s office
75% after deductible
Hospitalization 75% after deductible
Emergency room visit 100% after deductible and $300 copay
Behavioral health
Inpatient and outpatient
See above for doctor visits
75% after deductible
Telehealth video visits
Doctor On Demand $4 copay
Pharmacy See The pharmacy benefit chapter for details.
Centers of Excellence See the Centers of Excellence section of this chapter for details.
Walmar Care Clinic and Walmar Health See the Walmar Care Clinic and Walmar Health section of this chapter for details.
HMO plan options
Health maintenance organization (HMO) plan options,
which are available in some locations, are offered under the
Associates’ Health and Welfare Plan, but are independent
of the AMP, including the national plans and local plans
offered under the AMP. To find out if an HMO is available at
your work location, contact your personnel representative.
If one is available, coverage details are described in
materials provided separately by the HMO. The HMO
may have different eligibility terms and waiting periods
than those described in the Eligibility and enrollment
chapter of this Associate Benefits Book, but if there is any
difference between the HMO’s eligibility terms and the
eligibility terms described in the Eligibility and enrollment
chapter, the eligibility terms described in the Eligibility and
enrollment chapter will control.
Some HMOs require participants to accept an arbitration
agreement, where permitted by law, before coverage under
the HMO can become effective. Your acceptance of this
agreement must be received by the HMO within 60 days of
your initial enrollment or your HMO coverage will not take
effect. If the HMO does not receive your agreement within
60 days of your initial enrollment, you will not have medical
coverage under the Plan unless you have a valid status change
event as described in the Eligibility and enrollment chapter.
The eComm PPO Plan
The eComm PPO Plan option, which is available in some
locations, is offered under the Associates’ Health and
Welfare Plan, but is independent of the AMP, including the
national plans and local plans offered under the AMP. To
find out if the eComm PPO Plan option is available at your
work location, contact your personnel representative. If
See page 306

The medical plan
54
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
it is available, coverage details are described in materials
provided separately by the eComm PPO Plan’s third-party
administrator. The eComm PPO Plan may have different
eligibility terms and waiting periods than those described
in the Eligibility and enrollment chapter of this Associate
Benefits Book, but if there is any difference between the
eComm PPO Plan’s eligibility terms and the eligibility terms
described in the Eligibility and enrollment chapter, the
eligibility terms described in the Eligibility and enrollment
chapter will control.
Over the next several pages you’ll find detailed
descriptions of the AMP options, as follows:
• The national plans, distinguishing between:
– those that apply to most
associatesnationwide
– those available to associates whose
work locations are in central Florida,
Dallas/For Worh, or norhwest
Arkansas(these sections are shaded)
• The local plans
Refer also to the summary charts at the
beginning of this chapter for cost-sharing
details for each plan.
The Walmar Premier Plan
PREMIER PLAN COVERAGE
If your work location is not in central Florida, Dallas/Fort
Worth, or northwest Arkansas
This section describes coverage under the
Premier Plan in all areas except specific
geographic areas of central Florida, Dallas/
Fort Worth, and northwest Arkansas. See
National Plan options earlier in this chapter
for the specific counties that make up these
areas. See Premier Plan coverage for work
locations in central Florida, Dallas/Fort
Worth, and northwest Arkansas later in
this chapter for details about Premier Plan
coverage if your work location is in those
specified geographic areas.
The Premier Plan offers you the ability to pay for doctor
visits with fixed amounts, called “copayments” or “copays,”
as explained below under Coinsurance, copays, and the out-
of-pocket maximum. If you were enrolled in the HRA Plan
in 2019 and have a balance in the Health Reimbursement
Account (HRA) associated with that plan, you can use the
remaining funds to pay for the copay required for doctor’s
office visits (primary care or specialist), Walmart Care Clinic
or Walmart Health, Doctor On Demand, or urgent care
through the end of 2021, provided you remain enrolled in
the Premier Plan option.
The annual deductible
Your annual deductible is the amount you must pay each
calendar year before the Premier Plan begins paying a
portion of the cost of covered services. Copays are in
addition to the annual deductible and do not count toward
the deductible. The Premier Plan has a separate annual
deductible for services provided by network providers and
services provided by non-network providers. Amounts you
pay toward the network annual deductible apply toward the
out-of-network annual deductible, and vice versa.
The amount of your annual deductible is based on whether
you are covering just yourself or any eligible dependents
as well. If you choose coverage for any dependents as
well as for yourself, the network annual deductible and
the out-of-network annual deductible can be met by any
combination of you and your covered dependents, but no
benefits are payable for any covered person until the entire
applicable annual deductible is met. The following expenses
do not count toward the network or out-of-network
annualdeductible:
• Copays for doctor office visits, Doctor On Demand,
urgent care, Walmart Care Clinic or Walmart Health, or
emergency room visits
• Pharmacy copays/coinsurance (including copay assistance
from a third party)
• Amounts in excess of the Plan’s maximum allowable charge
that you pay to non-network providers, including amounts
paid for emergency room services that are in excess of the
Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic
or Walmart Health that is a non-network provider (however,
amounts for covered diagnostic tests performed outside
the Walmart Care Clinic or Walmart Health will count toward
your deductible, subject to other exclusions in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for
network preventive services and certain Centers of
Excellence services, and
• Charges for out-of-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
After you meet your network annual deductible for covered
services that do not require a copayment, the Premier Plan
pays 75% of the cost of covered services from a network
provider and your share is 25% coinsurance. However, the
Plan will pay 100% of the cost of covered preventive services
from a network provider before you meet your network
deductible and no copayment will be required. For covered

The medical plan
55
services subject to a copayment, you must continue to pay
the copayment, even after your annual deductible has been
met, until you meet your annual out-of-pocket maximum.
After you meet your out-of-network annual deductible for
covered services that are subject to the deductible and
that do not require a copayment, the Plan pays 50% of the
maximum allowable charge of covered services from a
non-network provider and you pay the rest — i.e., you are
responsible for the other 50% coinsurance plus any amount
charged above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay is
in addition to your annual deductible and must be paid even
after you have met your annual deductible. The AMP will pay
only the maximum allowable charge for covered services and
only covered services will apply to the annual deductible. If
the third-party administrator determines that the emergency
room visit is an “emergency,” the AMP will pay 100% of the
maximum allowable charge after you have met your network
annual deductible, regardless of whether the facility is a
network facility. However, if it is a non-network facility, you
will still be responsible for any amount over the maximum
allowable charge. If the facility is a non-network facility, and
the third-party administrator determines that the emergency
room visit is not an “emergency,” the AMP will pay 50% of
the maximum allowable charge for covered services after
you have met your out-of-network deductible and you will be
responsible for paying the deductible, the other 50%, and any
amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted
to the hospital from an emergency room, or if the patient
dies prior to hospital admission. Note that the cost-sharing
details described above apply to all services provided in the
emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered
an “emergency” if an average prudent person with a basic
knowledge of health care and in the same situation would
have thought that not going to the emergency room would
result in their life or health being in serious jeopardy.
IMPORTANT TERMS
See the Glossary for definitions of
coinsurance and copayment.
After you meet the annual out-of-pocket maximum
for network services, the Plan pays 100% of the cost of
covered services from a network provider for the rest
of the calendar year. There is no annual out-of-pocket
maximum for services from non-network providers — you
are responsible for paying your share of these charges in full
throughout the year. The amounts you pay that apply toward
your network annual out-of-pocket maximum include:
• Network and out-of-network annual deductibles (including
amounts paid with remaining HRA funds)
• Copays for doctor office visits, Doctor On Demand,
urgent care, Walmart Care Clinic or Walmart Health, or
emergency room visits
• Coinsurance for services provided by a network provider
or by a non-network provider that the Plan pays as
in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any
combination of covered medical services. Certain expenses,
however, do not count toward the annual out-of-pocket
maximum, as listed here:
• Charges paid 100% by the AMP such as charges for
network preventive services and certain Centers of
Excellence services
• Charges for out-of-network preventive services
• Coinsurance when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge
that you pay to non-network providers, including amounts
paid for emergency room services in excess of the Plan’s
maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health will
count toward your deductible, subject to other exclusions
in this list)
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers or
pharmacies to assist you in purchasing prescription drugs
(including prescription drug discount/coupons provided to
pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Premier
Plan, you will have an individual out-of-pocket maximum
for network expenses of $6,850. If you add dependents to
your coverage, you will have an out-of-pocket maximum for
network expenses of $13,700 per family. Regardless of the
coverage level you choose, you and each of your covered
dependents have an individual out-of-pocket maximum of
$6,850. Once you or any of your covered dependents have
incurred charges for covered services up to that amount, that
individual’s eligible expenses are paid at 100% for the rest of
the calendar year. If your coverage includes dependents, you
have a family out-of-pocket maximum of $13,700, which is a
combination of all family members’ covered expenses. Any
combination of two or more family members can contribute
to meet the family out-of-pocket maximum. Once you meet
the total family out-of-pocket maximum, eligible network
expenses for your entire family are paid at 100% for the rest
of the calendar year, even if each individual has not met the
individual out-of-pocket maximum.
See pages 306-327 for information replacing the text from here until The local plans on page 65.

The medical plan
56
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
PREMIER PLAN COVERAGE FOR WORK
LOCATIONS IN CENTRAL FLORIDA, DALLAS/
FORT WORTH, AND NORTHWEST ARKANSAS
The Premier Plan offers you the ability to pay for doctor
visits with fixed amounts, called “copayments” or “copays,”
as explained below under Coinsurance, copays, and the out-
of-pocket maximum. If you were enrolled in the HRA Plan
in 2019 and have a balance in the Health Reimbursement
Account (HRA) associated with that plan, you can use the
remaining funds to pay for the copay required for doctor’s
office visits (primary care or specialist), Walmart Care Clinic
or Walmart Health, Doctor On Demand, or urgent care
through the end of 2021, provided you remain enrolled in
the Premier Plan option.
The annual deductible
Your annual deductible is the amount you must pay each
calendar year before the Premier Plan begins paying a portion
of the cost of covered services. Copays are in addition to the
annual deductible and do not count toward the deductible.
The amount of your annual deductible is based on whether
you are covering just yourself or any eligible dependents
as well. If you choose coverage for any dependents as well
as for yourself, the annual deductible can be met by any
combination of you and your covered dependents, but no
benefits are payable for any covered person until the entire
annual deductible is met.
The following expenses do not count toward the
annualdeductible:
• Copays for doctor office visits, Doctor On Demand,
urgent care, Walmart Care Clinic or Walmart Health, or
emergency room visits
• Pharmacy copays/coinsurance (including copay assistance
from a third party)
• Amounts in excess of the Plan’s maximum allowable charge
for services from a non-network provider that the Plan
pays as in-network, including for emergency room services
in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health with
a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for
network preventive services and certain Centers of
Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
After you meet your annual deductible for covered
services that do not require a copayment, the Premier
Plan pays 75% of the cost of covered services and your
share is 25% coinsurance. However, the Plan will pay 100%
of the cost of covered preventive services from a network
provider before you meet your network deductible, and no
copayment will be required. For covered services subject
to a copayment, you must continue to pay the copayment,
even after your annual deductible has been met, until you
meet your annual out-of-pocket maximum.
The emergency room copay is $300 per visit. This copay
is in addition to your annual deductible and must be paid
even after you have met your annual deductible. The AMP
will pay only the maximum allowable charge for covered
services and only covered services will apply to the annual
deductible. If the third-party administrator determines
that the emergency room visit is an “emergency,” the
AMP will pay 100% of the maximum allowable charge
after you have met your annual deductible, regardless of
whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any
amount over the maximum allowable charge. If the facility
is a non-network facility, and the third-party administrator
determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum
allowable charge for covered services after you have met
your deductible and you will be responsible for paying
the deductible, the other 50%, and any amount over the
maximum allowable charge.
The $300 copay is waived if the patient is directly admitted
to the hospital from an emergency room, or if the patient
dies prior to hospital admission. Note that the cost-sharing
details described above apply to all services provided in the
emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered
an “emergency” if an average prudent person with a basic
knowledge of health care and in the same situation would
have thought that not going to the emergency room would
result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the
Plan pays 100% of the cost of covered services for the rest
of the calendar year.
The amounts you pay that apply toward your annual out-of-
pocket maximum include:
• Annual deductible (including amounts paid with remaining
HRA funds)
• Copays for doctor office visits, Doctor On Demand,
urgent care, Walmart Care Clinic or Walmart Health, or
emergency room visits
• Coinsurance for services provided by a network provider
or by a non-network provider that the Plan pays as
in-network, and
• Pharmacy copays/coinsurance.

The medical plan
57
Your annual out-of-pocket maximum may be met by any
combination of covered medical services. Certain expenses,
however, do not count toward the annual out-of-pocket
maximum, as listed here:
• Charges paid 100% by the AMP such as charges for
network preventive services and certain Centers of
Excellence services
• Amounts in excess of the Plan’s maximum allowable charge
for services from a non-network provider that the Plan
pays as in-network, including for emergency room services
in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health with
a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers or
pharmacies to assist you in purchasing prescription drugs
(including prescription drug discount/coupons provided to
pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including
charges for services from non-network providers.
If you choose associate-only coverage under the Premier
Plan, you will have an individual out-of-pocket maximum of
$6,850. If you add dependents to your coverage, you will
have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and
each of your covered dependents have an individual out-
of-pocket maximum of $6,850. Once you or any of your
covered dependents have incurred charges for covered
services up to that amount, that individual’s eligible
expenses are paid at 100% for the rest of the calendar year.
If your coverage includes dependents, you have a family
out-of-pocket maximum of $13,700, which is a combination
of all family members’ covered expenses. Any combination
of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total
family out-of-pocket maximum, eligible expenses for your
entire family are paid at 100% for the rest of the calendar
year, even if each individual has not met the individual
out-of-pocket maximum.
The Walmar Contribution Plan
CONTRIBUTION PLAN COVERAGE
If your work location is not in central Florida, Dallas/Fort
Worth, or northwest Arkansas
This section describes coverage under the
Contribution Plan in all areas except specified
geographic areas of central Florida, Dallas/
Fort Worth, and northwest Arkansas. See
National plan options earlier in this chapter
for the specific counties that make up these
areas. See Contribution Plan coverage for
work locations in central Florida, Dallas/Fort
Worth, and northwest Arkansas later in this
chapter for details about Contribution Plan
coverage if your work location is in those
specified geographic areas.
The Contribution Plan includes a Health Reimbursement
Account (HRA). Each year, the company allocates money to
the HRA for you and any covered dependents to use toward
your portion of the cost of covered services (meaning those
expenses that are your responsibility), including the annual
deductible. You may not contribute your own money to
the HRA. The Plan automatically pays your share of eligible
medical expenses (except for prescription drug expenses,
which cannot be paid from the HRA) until the HRA funds
are exhausted. Amounts paid by the HRA count toward your
annual deductible (both network and out-of-network) as
well as your out-of-pocket maximum.
Any balance remaining in your HRA at the end of a calendar
year rolls over for use during the next year, provided you
remain enrolled in the Contribution Plan. However, your
HRA balance (including your allocated HRA funds for
the current year) cannot exceed your network annual
deductible under the Contribution Plan. Each new year’s
allocation of HRA funds may be used only for eligible
medical expenses for services rendered within that calendar
year. For example, if you enroll in the Contribution Plan and
receive an allocation of HRA funds for 2020, you would be
able to use those funds for eligible medical expenses for
services rendered in 2020 but not for services rendered
prior to 2020 (such as an expense incurred in 2019 but not
processed until 2020). The HRA funds that roll over from a
prior year can be used for any eligible medical expense for
services rendered while enrolled in the Contribution Plan.
If you cancel your coverage, lose eligibility, or change from
the Contribution Plan to a different coverage option, any
funds remaining in your HRA are forfeited. If you continue
coverage in the Contribution Plan through COBRA, your
HRA balance remains available to you under the terms
See pages 306-327 for information replacing the text from here until The local plans on page 65.

The medical plan
58
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
described above and the company will continue to allocate
money to your HRA. See the COBRA chapter for more
information about COBRA continuation coverage.
HRA allocations: midyear enrollments or changes
If you are hired midyear and enroll in the Contribution
Plan, the company prorates your initial HRA allocation on
a monthly basis; your annual deductible and out-of-pocket
maximums are not prorated.
If you have a qualifying event and change your coverage
level midyear, such as from associate-only to associate+
dependents coverage, the company adjusts your HRA
allocation, annual deductible, and annual out-of-pocket
maximum accordingly.
The annual deductible
Your annual deductible is the amount you must pay each
calendar year before the Contribution Plan begins paying
a portion of the cost of covered services. Copays are in
addition to the annual deductible and do not count toward
the deductible. You can meet your annual deductible with
your company-provided HRA funds from the current year
and any rollover HRA funds you may have from a previous
year. When you have used all your company-provided HRA
funds, you must use your own funds to meet the remainder
of your annual deductible.
The Contribution Plan has a separate annual deductible
for services provided by network providers and services
provided by non-network providers. Amounts you pay
toward the network annual deductible apply toward the out-
of-network annual deductible, and vice versa.
The amount of your annual deductible is based on whether
you are covering just yourself or any eligible dependents as
well. If you choose coverage for any dependents as well as
for yourself, the network annual deductible and the out-of-
network annual deductible can be met by any combination
of you and your covered dependents, but no benefits are
payable for any covered person until the entire applicable
annual deductible is met.
The following expenses do not count toward the network or
out-of-network annual deductible:
• Copays for Doctor On Demand, Walmart Care Clinic or
Walmart Health, or emergency room visits
• Pharmacy copays/coinsurance (including copay assistance
from a third party)
• Amounts in excess of the Plan’s maximum allowable charge
that you pay to non-network providers, including amounts
paid for emergency room services in excess of the Plan’s
maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health will
count toward your deductible, subject to other exclusions
in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for
network preventive services and certain Centers of
Excellence services, and
• Charges for out-of-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
After you meet your network annual deductible for covered
services that do not require a copayment, the Contribution
Plan pays 75% of the cost of covered services from a network
provider and your share is 25% coinsurance. However, the
Plan will pay 100% of the cost of covered preventive services
from a network provider before you meet your network
deductible and no copayment will be required. For covered
services subject to a copayment, you must continue to pay
the copayment, even after your annual deductible has been
met, until you meet your annual out-of-pocket maximum.
After you meet your out-of-network annual deductible
for covered services that are subject to the deductible
and that do not require a copayment, the Plan pays 50% of
the maximum allowable charge of covered services from a
non-network provider and you pay the rest — i.e., you are
responsible for the other 50% coinsurance plus any amount
charged above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay
is in addition to your annual deductible and must be paid
even after you have met your annual deductible. The AMP
will pay only the maximum allowable charge for covered
services and only covered services will apply to the annual
deductible. If the third-party administrator determines
that the emergency room visit is an “emergency,” the
AMP will pay 100% of the maximum allowable charge after
you have met your network annual deductible, regardless
of whether the facility is a network facility. However, if
it is a non-network facility, you will still be responsible
for any amount over the maximum allowable charge. If
the facility is a non-network facility, and the third-party
administrator determines that the emergency room visit is
not an “emergency,” the AMP will pay 50% of the maximum
allowable charge for covered services after you have met
your out-of-network deductible and you will be responsible
for paying the deductible, the other 50%, and any amount
over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted
to the hospital from an emergency room, or if the patient
dies prior to hospital admission. Note that the cost-sharing
details described above apply to all services provided in the
emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered
an “emergency” if an average prudent person with
a basicknowledge of health care and in the same

The medical plan
59
situationwould have thought that not going to the
emergency roomwould result in their life or health being
in seriousjeopardy.
IMPORTANT TERMS
See the Glossary for definitions of
coinsurance and copayment.
After you meet the annual out-of-pocket maximum, the Plan
pays 100% of the cost of covered services from a network
provider for the rest of the calendar year. There is no annual
out-of-pocket maximum for charges for services from non-
network providers — you are responsible for paying your
share of these charges in full throughout the year.
The amounts you pay that apply toward your network annual
out-of-pocket maximum include:
• Network and out-of-network annual deductibles (including
amounts paid with HRA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or
Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider
or by a non-network provider that the Plan pays as
in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any
combination of covered medical services. Certain expenses,
however, do not count toward the annual out-of-pocket
maximum, as listed here:
• Charges paid 100% by the AMP such as charges for
network preventive services and certain Centers of
Excellence services
• Charges for out-of-network preventive services
• Coinsurance when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge
that you pay to non-network providers, including amounts
paid for emergency room services that are in excess of the
Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health will
count toward your deductible, subject to other exclusions
in this list)
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers or
pharmacies to assist you in purchasing prescription drugs
(including prescription drug discount/coupons provided to
pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the
Contribution Plan, you will have an individual out-of-
pocket maximum for network expenses of $6,850. If
you add dependents to your coverage, you will have
an out-of-pocket maximum for network expenses of
$13,700 per family.
Regardless of the coverage level you choose, you and
each of your covered dependents have an individual out-
of-pocket maximum of $6,850. Once you or any of your
covered dependents have incurred charges for covered
services up to that amount, that individual’s eligible
expenses are paid at 100% for the rest of the calendar year.
If your coverage includes dependents, you have a family
out-of-pocket maximum of $13,700, which is a combination
of all family members’ covered expenses. Any combination
of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total
family out-of-pocket maximum, eligible network expenses
for your entire family are paid at 100% for the rest of the
calendar year, even if each individual has not met the
individual out-of-pocket maximum.
CONTRIBUTION PLAN COVERAGE FOR WORK
LOCATIONS IN CENTRAL FLORIDA, DALLAS/
FORT WORTH, AND NORTHWEST ARKANSAS
The Contribution Plan includes a Health Reimbursement
Account (HRA). Each year, the company allocates money
to the HRA for you and any covered dependents to use
toward your portion of the cost of covered services
(meaning those expenses that are your responsibility),
including the annual deductible. You may not contribute
your own money to the HRA. The Plan automatically
pays your share of eligible medical expenses (except for
prescription drug expenses, which cannot be paid from the
HRA) until the HRA funds are exhausted. Amounts paid by
the HRA count toward your annual deductible as well as
your out-of-pocket maximum.
Any balance remaining in your HRA at the end of a
calendar year rolls over for use during the next year,
provided you remain enrolled in the Contribution Plan.
However, your HRA balance (including your allocated
HRA funds for the current year) cannot exceed your
annual deductible under the Contribution Plan. Each
new year’s allocation of HRA funds may be used only for
eligible medical expenses for services rendered within
that calendar year. For example, if you enroll in the
Contribution Plan and receive an allocation of HRA funds
for 2020, you would be able to use those funds for eligible
medical expenses for services rendered in 2020 but not
for services rendered prior to 2020 (such as an expense
incurred in 2019 but not processed until 2020). The HRA
funds that roll over from a prior year can be used for
any eligible medical expense for services rendered while
enrolled in the Contribution Plan.
See pages 306-327 for information replacing the text from here until The local plans on page 65.

The medical plan
60
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you cancel your coverage, lose eligibility, or change from
the Contribution Plan to a different coverage option, any
funds remaining in your HRA are forfeited. If you enroll
in the Contribution Plan through COBRA coverage, your
HRA balance remains available to you under the terms
described above and the company will continue to allocate
money to your HRA. See the COBRAchapter for more
information about COBRA continuation coverage.
HRA allocations: midyear enrollments or changes
If you are hired midyear and enroll in the Contribution
Plan, the company prorates your initial HRA allocation on
a monthly basis; your annual deductible and out-of-pocket
maximums are not prorated.
If you have a qualifying event and change your coverage
level midyear, such as from associate-only to associate
+ dependents coverage, the company adjusts your HRA
allocation, annual deductible, and annual out-of-pocket
maximum accordingly.
The annual deductible
Your annual deductible is the amount you must pay each
calendar year before the Contribution Plan begins paying
a portion of the cost of covered services. Copays are in
addition to the annual deductible and do not count toward
the deductible. You can meet your annual deductible with
your company-provided HRA funds from the current year
and any rollover HRA funds you may have from a previous
year. When you have used all your company-provided HRA
funds, you must use your own funds to meet the remainder
of your annual deductible.
The amount of your annual deductible is based on whether
you are covering just yourself or any eligible dependents
as well. If you choose coverage for any dependents as well
as for yourself, the annual deductible can be met by any
combination of you and your covered dependents, but
no benefits are payable for any covered person until the
entire annual deductible is met.
The following expenses do not count toward the annual
deductible:
• Copays for Doctor On Demand, Walmart Care Clinic or
Walmart Health, or emergency room visits
• Pharmacy copays/coinsurance (including copay assistance
from a third party)
• Amounts in excess of the Plan’s maximum allowable
charge for services from a non-network provider that
the Plan pays as in-network, including for emergency
room services in excess of the Plan’s maximum
allowablecharge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests
performed outside the Walmart Care Clinic or Walmart
Health with a network provider will count toward your
deductible, subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for
network preventive services and certain Centers of
Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
After you meet your annual deductible for covered
services that do not require a copayment, the Contribution
Plan pays 75% of the cost of covered services and your
share is 25% coinsurance. However, the Plan will pay 100%
of the cost of covered preventive services from a network
provider before you meet your network deductible, and no
copayment will be required. For covered services subject
to a copayment, you must continue to pay the copayment,
even after your annual deductible has been met, until you
meet your annual out-of-pocket maximum.
The emergency room copay is $300 per visit. This copay
is in addition to your annual deductible and must be paid
even after you have met your annual deductible. The AMP
will pay only the maximum allowable charge for covered
services and only covered services will apply to the annual
deductible. If the third-party administrator determines
that the emergency room visit is an “emergency,” the AMP
will pay 100% of the maximum allowable charge after you
have met your annual deductible, regardless of whether the
facility is a network facility. However, if it is a non-network
facility, you will still be responsible for any amount over the
maximum allowable charge. If the facility is a non-network
facility, and the third-party administrator determines that
the emergency room visit is not an “emergency,” the AMP
will pay 50% of the maximum allowable charge for covered
services after you have met your deductible and you will be
responsible for paying the deductible, the other 50%, and
any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted
to the hospital from an emergency room, or if the patient
dies prior to hospital admission. Note that the cost-sharing
details described above apply to all services provided in the
emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered
an “emergency” if an average prudent person with a basic
knowledge of health care and in the same situation would
have thought that not going to the emergency room would
result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the
Plan pays 100% of the cost of covered services for the rest
of the calendar year.

The medical plan
61
The amounts you pay that apply toward your annual
out-of-pocket maximum include:
• Annual deductible (including amounts paid with HRA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or
Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider
or by a non-network provider that the Plan pays as
in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any
combination of covered medical services. Certain expenses,
however, do not count toward the annual out-of-pocket
maximum, as listed here:
• Charges paid 100% by the AMP such as charges for
network preventive services and certain Centers of
Excellence services
• Amounts in excess of the Plan’s maximum allowable charge
for services from a non-network provider that the Plan
pays as in-network, including for emergency room services
in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health with
a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers or
pharmacies to assist you in purchasing prescription drugs
(including prescription drug discount/coupons provided to
pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including
charges for services from non-network providers.
If you choose associate-only coverage under the Contribution
Plan, you will have an individual out-of-pocket maximum of
$6,850. If you add dependents to your coverage, you will have
an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and
each of your covered dependents have an individual
out-of-pocket maximum of $6,850. Once you or any
of your covered dependents have incurred charges for
covered services up to that amount, that individual’s eligible
expenses are paid at 100% for the rest of the calendar year.
If your coverage includes dependents, you have a family
out-of-pocket maximum of $13,700, which is a combination
of all family members’ covered expenses. Any combination
of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total
family out-of-pocket maximum, eligible expenses for your
entire family are paid at 100% for the rest of the calendar
year, even if each individual has not met the individual
out-of-pocket maximum.
The Walmar Saver Plan
SAVER PLAN COVERAGE
If your work location is not in central Florida, Dallas/Fort
Worth, or northwest Arkansas
This section describes coverage under
the Saver Plan in all areas except specific
geographic areas of central Florida, Dallas/
Fort Worth, and northwest Arkansas. See
National plan options earlier in this chapter
for the specific counties that make up these
areas. See Saver Plan coverage for work
locations in central Florida, Dallas/Fort
Worth, and northwest Arkansas later in this
chapter for details about Saver Plan coverage
if your work location is in those areas.
If you enroll in the Saver Plan and contribute to a Health
Savings Account (HSA), the company matches your payroll
deductions into your HSA, dollar-for-dollar up to $350 if you
have individual coverage or $700 if you have family coverage.
Combined contributions to your HSA (your own and the
company’s) cannot exceed the 2020 annual IRS limit of
$3,550 for individual coverage or $7,100 for family coverage,
plus a $1,000 catch-up contribution if you are age55 or over.
The annual deductible
Your annual deductible is the amount you must pay each
calendar year before the Saver Plan begins paying a portion
of the cost of covered services. Copays are in addition
to the annual deductible and do not count toward the
deductible. The Saver Plan has a separate annual deductible
for services provided by network providers and services
provided by non-network providers. Amounts you pay
toward the network annual deductible apply toward the
out-of-network annual deductible, and vice versa.
Preventive care services, as described in the Preventive
care program section later in this chapter, are covered even
if you have not met the annual deductible.
The amount of your annual deductible is based on whether
you are covering just yourself or any eligible dependents as
well. If you choose coverage for any dependents as well as
for yourself, the network annual deductible and the out-of-
network annual deductible can be met by any combination
of you and your covered dependents, but no benefits are
payable for any covered person until the entire applicable
annual deductible is met.
You can choose to use money in your HSA to pay expenses
that are subject to the annual deductible, or you can pay
them out of your own pocket and save your HSA money for
future expenses.
See pages 306-327 for information replacing the text from here until The local plans on page 65.

The medical plan
62
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you enroll in the Saver Plan, you generally must pay
full cost for prescriptions until you meet your network
annual deductible. The exception is medications on
the OptumRx list of approved preventive medications,
which are not subject to the Saver Plan’s network annual
deductible — you can purchase these medications at the
appropriate copay or coinsurance level even if you have
not met the network annual deductible. In addition, certain
over-the-counter drugs are available at 100% coverage if
you obtain a prescription, even if you have not satisfied
your deductible. See The pharmacy benefit chapter for
details. With the exception of these charges for approved
preventive medications, pharmacy charges under the
Saver Plan apply toward your network annual deductible
and out-of-pocket maximum.
The following expenses do not count toward the network or
out-of-network annual deductible:
• Copays for preventive medications not subject to the
annual deductible
• Discounts, coupons, pharmacy discount programs or
similar arrangements provided by drug manufacturers
orpharmacies to assist you in purchasing prescription
drugs (including any prescription drug charges paid
directly to pharmacies on your behalf through discount
programs/coupons)
• Amounts in excess of the Plan’s maximum allowable charge
that you pay to non-network providers, including amounts
paid for emergency room services in excess of the Plan’s
maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests
performed outside the Walmart Care Clinic or Walmart
Health will count toward your deductible, subject to other
exclusions in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for
network preventive services and certain Centers of
Excellence services, and
• Charges for out-of-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
After you meet your network annual deductible for covered
services, the Saver Plan pays 75% of the cost of covered
services from a network provider and your share is 25%
coinsurance. However, the Plan will pay 100% of the cost of
covered preventive services from a network provider before
you meet your network deductible and no copayment will be
required. For covered services subject to a copayment, you
must continue to pay the copayment, even after your annual
deductible has been met, until you meet your annual out-
of-pocket maximum. After you meet your out-of-network
annual deductible for covered services that are subject to
the deductible and that do not require a copayment, the
Plan pays 50% of the maximum allowable charge of covered
services from a non-network provider and you pay the rest
— i.e., you are responsible for the other 50% coinsurance plus
any amount charged above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay
is in addition to your annual deductible and must be paid
even after you have met your annual deductible. The AMP
will pay only the maximum allowable charge for covered
services and only covered services will apply to the annual
deductible. If the third-party administrator determines
that the emergency room visit is an “emergency,” the
AMP will pay 100% of the maximum allowable charge after
you have met your network annual deductible, regardless
of whether the facility is a network facility. However, if
it is a non-network facility, you will still be responsible
for any amount over the maximum allowable charge. If
the facility is a non-network facility, and the third-party
administrator determines that the emergency room visit is
not an “emergency,” the AMP will pay 50% of the maximum
allowable charge for covered services after you have met
your out-of-network deductible and you will be responsible
for paying the deductible, the other 50%, and any amount
over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted
to the hospital from an emergency room, or if the patient
dies prior to hospital admission. Note that the cost-sharing
details described above apply to all services provided in the
emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered
an “emergency” if an average prudent person with a basic
knowledge of health care and in the same situation would
have thought that not going to the emergency room would
result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum
for network services, the Plan pays 100% of the cost of
covered services from a network provider for the rest
of the calendar year. There is no annual out-of-pocket
maximum for services from non-network providers — you
are responsible for paying your share of these charges in full
throughout the year.
The amounts you pay that apply toward your network annual
out-of-pocket maximum include:
• Network and out-of-network annual deductibles (including
amounts paid with HSA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or
Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or
by a non-network provider that the Plan pays as in-network
• Pharmacy copays/coinsurance, and
• Pharmacy charges before your annual deductible is met.

The medical plan
63
Your network annual out-of-pocket maximum may be met
by any combination of covered medical services. Certain
expenses, however, do not count toward the annual out-of-
pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for
network preventive services and certain Centers of
Excellence services
• Charges for out-of-network preventive services
• Coinsurance when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge
that you pay to non-network providers, including amounts
paid for emergency room services in excess of the Plan’s
maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health will
count toward your deductible, subject to other exclusions
in this list)
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers or
pharmacies to assist you in purchasing prescription drugs
(including prescription drug discount/coupons provided to
pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Saver
Plan, you will have an individual out-of-pocket maximum
for network expenses of $6,650. If you add dependents to
your coverage, you will have an out-of-pocket maximum for
network expenses of $13,300 per family.
Regardless of the coverage level you choose, you and
each of your covered dependents have an individual out-
of-pocket maximum of $6,650. Once you or any of your
covered dependents have incurred charges for covered
services up to that amount, that individual’s eligible
expenses are paid at 100% for the rest of the calendar year.
If your coverage includes dependents, you have a family
out-of-pocket maximum of $13,300, which is a combination
of all family members’ covered expenses. Any combination
of two or more family members can contribute to meet
the family out-of-pocket maximum. Once you meet the
total family out-of-pocket maximum, eligible network
expenses for your entire family are paid at 100% for the
rest of the calendar year, even if each individual has not
met the individual out-of-pocket maximum.
SAVER PLAN COVERAGE FOR WORK
LOCATIONS IN CENTRAL FLORIDA, DALLAS/
FORT WORTH, AND NORTHWEST ARKANSAS
If you enroll in the Saver Plan and contribute to a Health
Savings Account (HSA), the company matches your payroll
deductions into your HSA, dollar-for-dollar up to $350 if you
have individual coverage or $700 if you have family coverage.
Combined contributions to your HSA (your own and the
company’s) cannot exceed the 2020 annual IRS limit of
$3,550 for individual coverage or $7,100 for family coverage,
plus a $1,000 catch-up contribution if you are age55 or over.
The annual deductible
Your annual deductible is the amount you must pay each
calendar year before the Saver Plan begins paying a
portion of the cost of your covered services. Copays are in
addition to the annual deductible and do not count toward
the deductible.
Preventive care services, as described in the Preventive
care program section later in this chapter, are covered even
if you have not met the annual deductible.
The amount of your annual deductible is based on whether
you are covering just yourself or any eligible dependents
as well. If you choose coverage for any dependents as well
as for yourself, the annual deductible can be met by any
combination of you and your covered dependents, but no
benefits are payable for any covered person until the entire
annual deductible is met.
You can choose to use money in your HSA to pay expenses
that are subject to the annual deductible, or you can pay
them out of your own pocket and save your HSA money for
future expenses.
If you enroll in the Saver Plan, you generally must pay
full cost for prescriptions until you meet your annual
deductible. The exception is medications on the OptumRx
list of approved preventive medications, which are not
subject to the Saver Plan’s annual deductible — you can
purchase these medications at the appropriate copay or
coinsurance level even if you have not met the annual
deductible. In addition, certain over-the-counter drugs
are available at 100% coverage if you obtain a prescription,
even if you have not satisfied your deductible. See The
pharmacy benefit chapter for details. With the exception
of these charges for approved preventive medications,
pharmacy charges under the Saver Plan apply toward your
annual deductible and out-of-pocket maximum.
The following expenses do not count toward the annual
deductible:
• Copays for preventive medications not subject to the
annual deductible
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers
orpharmacies to assist you in purchasing prescription
drugs (including any prescription drug charges paid
directly to pharmacies on your behalf through discount
programs/coupons)
• Amounts in excess of the Plan’s maximum allowable
charge for services from a non-network provider that
See pages 306-327 for information replacing the text from here until The local plans on page 65.

The medical plan
64
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
the Plan pays as in-network, including for emergency
room services in excess of the Plan’s maximum
allowablecharge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health with
a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for
network preventive services and certain Centers of
Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
After you meet your annual deductible for covered services,
the Saver Plan pays 75% of the cost of covered services
and your share is 25% coinsurance. However, the Plan
will pay 100% of the cost of covered preventive services
from a network provider before you meet your network
deductible, and no copayment will be required. For covered
services subject to a copayment, you must continue to pay
the copayment, even after your annual deductible has been
met, until you meet your annual out-of-pocket maximum.
The emergency room copay is $300 per visit. This copay
is in addition to your annual deductible and must be paid
even after you have met your annual deductible. The AMP
will pay only the maximum allowable charge for covered
services and only covered services will apply to the annual
deductible. If the third-party administrator determines
that the emergency room visit is an “emergency,” the
AMP will pay 100% of the maximum allowable charge
after you have met your annual deductible, regardless of
whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any
amount over the maximum allowable charge. If the facility
is a non-network facility, and the third-party administrator
determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum
allowable charge for covered services after you have met
your deductible and you will be responsible for paying
the deductible, the other 50%, and any amount over the
maximum allowable charge.
The $300 copay is waived if the patient is directly admitted
to the hospital from an emergency room, or if the patient
dies prior to hospital admission. Note that the cost-sharing
details described above apply to all services provided in the
emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered
an “emergency” if an average prudent person with a basic
knowledge of health care and in the same situation would
have thought that not going to the emergency room would
result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the
Plan pays 100% of the cost of covered services for the rest
of the calendar year.
The amounts you pay that apply toward your annual out-of-
pocket maximum include:
• Annual deductible (including amounts paid with HSA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or
Walmart Health, or emergency room visits
• Coinsurance for services provided by a network
provider or by a non-network provider that the Plan
pays as in-network
• Pharmacy copays/coinsurance, and
• Pharmacy charges before your annual deductible is met.
Your annual out-of-pocket maximum may be met by any
combination of covered medical services. Certain expenses,
however, do not count toward the annual out-of-pocket
maximum, as listed here:
• Charges paid 100% by the AMP such as charges for
network preventive services and certain Centers of
Excellence services
• Amounts in excess of the Plan’s maximum allowable charge
for services from a non-network provider that the Plan
pays as in-network, including for emergency room services
in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health with
a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers or
pharmacies to assist you in purchasing prescription drugs
(including prescription drug discount/coupons provided to
pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including
charges for services from non-network providers.
If you choose associate-only coverage under the Saver
Plan, you will have an individual out-of-pocket maximum of
$6,650. If you add dependents to your coverage, you will
have an out-of-pocket maximum of $13,300 per family.
Regardless of the coverage level you choose, you and
each of your covered dependents have an individual out-
of-pocket maximum of $6,650. Once you or any of your
covered dependents have incurred charges for covered
services up to that amount, that individual’s eligible
expenses are paid at 100% for the rest of the calendar year.
If your coverage includes dependents, you have a family
out-of-pocket maximum of $13,300, which is a combination
of all family members’ covered expenses. Any combination
of two or more family members can contribute to meet the

The medical plan
65
family out-of-pocket maximum. Once you meet the total
family out-of-pocket maximum, eligible expenses for your
entire family are paid at 100% for the rest of the calendar
year, even if each individual has not met the individual out-
of-pocket maximum.
The local plans
Local plan options are available in designated regions
nationwide. Your work location determines if a local plan
option is available to you. See the Local plan options chart
earlier in this chapter for a listing of the plans and the areas
they serve.
Under the local plan options, you must always use the
doctors, hospitals, and other providers in the plan’s network.
If you receive services from a provider outside the network,
or if you have dependents who live and seek care outside
the network coverage area, your expenses are not covered,
except in cases of emergency.
The annual deductible
Your annual deductible is the amount you must pay each
calendar year before the Plan begins paying a portion of
the cost of covered services. Copays are in addition to the
deductible and do not count toward the deductible.
The amount of your annual deductible is based on whether
you are covering just yourself or any eligible dependents
as well. If you choose coverage for any dependents as well
as for yourself, the annual deductible can be met by any
combination of you and your covered dependents, but no
benefits are payable for any covered person until the entire
applicable deductible is met.
The following expenses do not count toward the annual
deductible:
• Copays for doctor office visits, Doctor On Demand,
urgent care, Walmart Care Clinic or Walmart Health, or
emergency room visits
• Pharmacy copays/coinsurance (including copay assistance
from a third party)
• Amounts in excess of the Plan’s maximum allowable charge
for services from a non-network provider that the Plan
pays as in-network, including for emergency room services
in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health with
a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for
network preventive services and certain Centers of
Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
After you meet your annual deductible for covered services
that do not require a copayment, the Plan pays 75% of the
cost of covered services and your share is 25% coinsurance.
However, the Plan will pay 100% of the cost of covered
preventive services from a network provider before you
meet your network deductible, and no copayment will be
required. For covered services subject to a copayment,
you must continue to pay the copayment, even after your
annual deductible has been met, until you meet your annual
out-of-pocket maximum.
The emergency room copay is $300 per visit. This copay
is in addition to your annual deductible and must be paid
even after you have met your annual deductible. The AMP
will pay only the maximum allowable charge for covered
services and only covered services will apply to the annual
deductible. If the third-party administrator determines
that the emergency room visit is an “emergency,” the AMP
will pay 100% of the maximum allowable charge after you
have met your annual deductible, regardless of whether the
facility is a network facility. However, if it is a non-network
facility, you will still be responsible for any amount over the
maximum allowable charge. If the facility is a non-network
facility, and the third-party administrator determines
that the emergency room visit is not an “emergency,”
theservices provided will not be covered by the AMP.
The $300 copay is waived if the patient is directly admitted
to the hospital from an emergency room, or if the patient
dies prior to hospital admission. Note that the cost-sharing
details described above apply to all services provided in the
emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered
an “emergency” if an average prudent person with a basic
knowledge of health care and in the same situation would
have thought that not going to the emergency room would
result in their life or health being in serious jeopardy.
After you meet the out-of-pocket maximum, the Plan pays
100% of covered services for the rest of the calendar year.
The amounts you pay that apply toward your out-of-pocket
maximum include:
• Annual deductible
• Copays for doctor office visits, Doctor On Demand,
urgent care, Walmart Care Clinic or Walmart Health,
oremergency room visits
• Coinsurance for services provided by a network provider
or by a non-network provider that the Plan pays as
in-network, and
• Pharmacy copays/coinsurance.
See pages 306-327 for information replacing the text from here until The local plans on page 65.

The medical plan
66
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Your annual out-of-pocket maximum may be met by any
combination of covered medical services. Certain expenses,
however, do not count toward the annual out-of-pocket
maximum, as listed here:
• Charges paid 100% by the AMP such as charges for
network preventive services and certain Centers of
Excellence services
• Amounts in excess of the Plan’s maximum allowable charge
for services from a non-network provider that the Plan
pays as in-network, including for emergency room services
in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care
Clinic or Walmart Health that is a non-network provider
(however, amounts for covered diagnostic tests performed
outside the Walmart Care Clinic or Walmart Health with
a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or
similar arrangements provided by drug manufacturers or
pharmacies to assist you in purchasing prescription drugs
(including prescription drug discount/coupons provided to
pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including
charges for services from non-network providers.
If you choose associate-only coverage under a local plan,
you will have an individual out-of-pocket maximum of
$6,850. If you add dependents to your coverage, you will
have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and
each of your covered dependents have an individual out-
of-pocket maximum of $6,850. Once you or any of your
covered dependents have incurred charges for covered
services up to that amount, that individual’s eligible
expenses are paid at 100% for the rest of the calendar year.
If your coverage includes dependents, you have a family
out-of-pocket maximum of $13,700, which is a combination
of all family members’ covered expenses. Any combination
of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total
family out-of-pocket maximum, eligible expenses for your
entire family are paid at 100% for the rest of the calendar
year, even if each individual has not met the individual out-
of-pocket maximum.
Administration of the AMP
The AMP is self-insured, which means benefits are not
insured by an insurance company. Instead, participating
associates make contributions to cover a portion of the cost
of benefits, and the rest of the cost is paid from company
assets or through a Trust funded by the company.
The Plan contracts with third-party administrators
(TPAs) to handle administration of the options available
under the AMP: Aetna Life Insurance Company (Aetna),
BlueAdvantage Administrators of Arkansas, HealthSCOPE
Benefits, Inc., and UnitedHealthcare. The Plan also
contracts with Contigo Health (formerly Health Design
Plus) to serve as the TPA for certain procedures under
the Centers of Excellence program, as described under
Centers of Excellence later in this chapter. In some areas,
Grand Rounds and Doctor On Demand may provide care
management and similar services to assist the TPA. See
Helping you manage your health later in this chapter.
Your work location and the plan option you select determine
which TPA administers your AMP coverage. If you are a
remote worker or are receiving continuation coverage
under COBRA, you will be assigned to the nearest facility
and your coverage will be administered by a TPA at that
location. If you are a truck driver, your plan options and the
associated TPAs may be determined by your home location
rather than work location.
The TPA makes medical claim determinations and processes
claims based on the Plan’s terms and the TPA’s policies and
procedures. The TPA also provides a network of providers
that accept discounted rates for services they provide to
participants. See Your provider network later in this chapter
for details.
What is covered by the AMP
The AMP pays benefits for covered expenses, which are
charges for procedures, services, equipment and supplies
that are defined as:
• Not in excess of the maximum allowable charge, which is
determined by the third-party administrator
• Medically necessary
• Not excluded under the Plan (see What is not covered by
the AMP later in this chapter), and
• Not in excess of AMP limits.
MAXIMUM ALLOWABLE CHARGE
See page 327
The “maximum allowable charge” (MAC) is the maximum
amount the AMP covers or pays for any health care
services, drugs, medical devices, equipment, supplies, or
benefits covered by the Plan. The MAC applies both to
network and out-of-network services.
For covered network services, the MAC is that portion of
a provider’s charge covered by the AMP, as determined by
the provider’s contract with the third-party administrator. In
the case of BlueAdvantage Administrators of Arkansas, this
includes contracts with an independent licensee company
of the Blue Cross and Blue Shield Association; in the case
of UnitedHealthcare, this includes Harvard Pilgrim Health
The medical plan
67
Care, an independent licensee of UnitedHealthcare. For
information about the third-party administrator for your
medical plan coverage, see Your provider network later in
this chapter.
For covered out-of-network services, the MAC is
determined by each third-party administrator, as described
below. In certain circumstances, network benefits may be
paid for out-of-network services, as described under When
network benefits are paid for out-of-network expenses.
For out-of-network emergency services, the MAC will be the
greatest of the following: the median in-network rate; the
usual, customary, and reasonable rate; or the Medicare rate.
Aetna: The MAC is 125% of Medicare’s maximum allowable
charge for voluntary out-of-network services. For
involuntary out-of-network service, the MAC also is
125% of Medicare’s maximum allowable charge unless the
provider is in Aetna’s National Advantage Program (NAP).
NAP provider charges are paid at a discount. If a Medicare
maximum allowable charge is not published by the Center
for Medicare and Medicaid Services for a specific service,
Aetna uses a gap methodology to calculate the MAC that
is based on the Medicare maximum allowable charge.
Medicare’s allowable rate is based upon the geographic area
in which the service is furnished.
BlueAdvantage Administrators of Arkansas: The method for
establishing the MAC for covered out-of-network services
depends on whether the service is delivered by an individual
health care provider (e.g., a physician), an ambulance or air
ambulance service, or a hospital or facility. For services
of individual providers and ambulance and air ambulance
transport, the MAC is 125% of the Medicare allowed amount
for such services on the date administered. For hospital
and facility services or for other covered benefits (e.g.,
drugs, medical devices, products or implants, equipment, or
supplies), the MAC for covered out-of-network services is
limited to the allowance set by BlueAdvantage Administrators
of Arkansas in its discretion. If BlueAdvantage Administrators
of Arkansas does not have its own method or benchmark in a
given case, the MAC for covered out-of-network services is
limited to the pricing or allowance offered by the Blue Cross
and Blue Shield Plan in the state where services are provided.
For covered out-of-network services, the Plan pays the
lesser of MAC or the provider’s actual billed charges. If
the provider’s billed charges exceed the Plan’s MAC, you
are responsible for paying the difference. For additional
information, call your health care advisor at the number on
your plan ID card.
HealthSCOPE Benefits: There is no benefit for out-of-
network services sought voluntarily by participants in
local plans administered by HealthSCOPE Benefits. For
approved involuntary or emergency out-of-network
services, HealthSCOPE Benefits will use a discount
through a “wrap network,” if available and consistent with
the Affordable Care Act. (A wrap network is a group of
non-contracted providers who have arranged to provide
services to Plan participants at a discount.) If there is not
a discount available through a wrap network, the MAC
will be 125% of Medicare’s maximum allowable charge.
In cases where a Medicare maximum allowable charge is
not published by the Center for Medicare and Medicaid
Services for a specific service, HealthSCOPE Benefits will
use a gap methodology to calculate the MAC. There may
be some cases in which an individual agreement is reached
with the non-network provider.
UnitedHealthcare: The MAC is 125% of Medicare’s maximum
allowable charge for voluntary out-of-network services.
For involuntary out-of-network services, the MAC also
is 125% of Medicare’s maximum allowable charge unless
the provider is in UnitedHealthcare’s Shared Savings
Program (SSP). SSP provider charges are paid at a discount.
In cases where a Medicare maximum allowable charge is
not published by the Center for Medicare and Medicaid
Services for a specific service, UnitedHealthcare uses a gap
methodology to calculate the MAC.
MEDICALLY NECESSARY
”Medically necessary” (or “medical necessity”) generally
means the AMP has determined the procedure, service,
equipment, or supply to be:
• Appropriate for the symptoms, diagnosis, or treatment of
a medical condition
• Provided for the diagnosis or direct care and treatment of
the medical condition
• Within the standards of good medical practice within the
organized medical community
• Not primarily for the convenience of the patient or the
patient’s doctor or other provider, and
• The most appropriate procedure, service, equipment, or
supply that can be safely provided.
”Most appropriate” means:
• There is valid scientific evidence demonstrating that the
expected health benefits from the procedure, service,
equipment, or supply are clinically significant and produce
a greater likelihood of benefit, without disproportionately
greater risk of harm or complications, for the Plan
participant with the particular medical condition being
treated than other possible alternatives
• Generally accepted forms of treatment that are less
invasive have been tried and found ineffective or otherwise
unsuitable, and
• For hospital stays, acute inpatient care is necessary due
to the kind of services the participant is receiving or the
severity of the medical condition, and safe and adequate
care cannot be received as an outpatient or in a less
intensive medical setting.

The medical plan
68
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Aetna, UnitedHealthcare, BlueAdvantage Administrators
of Arkansas, HealthSCOPE Benefits, Precedence Inc. (with
respect to the UnityPoint Local Plan), and Mercy Health
Communities (with respect to all Mercy Local Plans) follow
policies in determining whether a procedure, service,
equipment, or supply is medically necessary. Your benefits
are subject to the terms of these policies, which vary by
third-party administrator.
You and your health care provider can access the coverage
policies of Aetna, UnitedHealthcare, and BlueAdvantage
Administrators of Arkansas at their respective websites,
listed in the Resources chart at the beginning of this
chapter. Access the coverage policies of HealthSCOPE
Benefits by calling 800-804-1272.
Your AMP benefits are subject to all terms, conditions,
limitations, and exclusions set forth in the coverage policies
administered by your third-party administrator regarding
medical necessity.
Your provider network
Depending on your work location and choice of medical
plan, your benefits under the AMP are administered by one
of the following third-party administrators:
• Aetna
• BlueAdvantage Administrators of Arkansas
• HealthSCOPE Benefits, or
• UnitedHealthcare.
The Plan contracts with each of the above third-party
administrators and also with Mercy Health Communities
(for all Mercy Local Plans), Emory, UnityPoint, Memorial
Hermann, and Ochsner to provide a network of health care
providers from whom you can receive medical services
covered under the AMP at discounted prices. Your provider
may include special networks, such as Centers of Excellence
and advanced imaging within its network. Network
providers accept an amount negotiated by the third-party
administrator for specific covered services as payment in
full (the maximum allowable charge for network services),
subject to the annual deductible and cost-sharing terms
applicable to the coverage you chose.
For provider listings, call the number on your plan ID card or
select the provider directory on One.Walmart.com.
See page 327
If your provider leaves the network, your benefit
is adjusted accordingly, based on the terms of your
medical plan. If you are covered under the Premier Plan,
Contribution Plan, or Saver Plan and your work location
is not in central Florida, Dallas/Fort Worth, or northwest
Arkansas, services provided by a provider who has left
the network are generally treated as an out-of-network
benefit; you may be required to pay any amount above the
maximum allowable charge, or choose another provider
in the network. If you are covered under a local plan, or
under the Premier Plan, Contribution Plan, or Saver Plan in
central Florida, Dallas/Fort Worth, or northwest Arkansas,
which provide no coverage for non-network providers
except in cases of emergency, your provider’s services are
not covered under the Plan.
The AMP does not furnish hospital or medical services and is
not liable for any act or omission of any provider or agent of
such provider, including failure or refusal to render services.
All medical decisions are between you and your provider.
The AMP makes no representations regarding the quality of
services rendered by any provider.
NOTE: The AMP, its third-party administrators, and network
providers may agree to certain incentive arrangements
(which may pay bonuses or withhold provider payments)
designed to reward high-quality and cost-effective
treatments. Some of the local plan contracts include such
arrangements. Contact your third-party administrator for
information regarding these arrangements.
WHEN NETWORK BENEFITS ARE PAID FOR
OUTOFNETWORK EXPENSES
A covered expense you incur with a non-network provider
may, in the following circumstances, be treated as a network
expense:
• If your dependent child under age 19 requires treatment at
a Children’s Miracle Network hospital
• If there are no network providers with the relevant
specialty within 30 miles of your home (not applicable to
local plan options)
• Services from a non-network provider involving a pregnant
participant are treated as network charges for up to six
weeks after delivery if services began when the provider
was a network provider and there is no interruption of the
doctor/patient relationship
• Services from a non-network provider, until the effective
date of the next Annual Enrollment, for a course of
treatment that began when the provider was a network
provider, where there is no interruption of the doctor/
patient relationship (for example, if you change third-party
administrators during the year because of a change in work
location and are in the middle of a course of treatment)
• Services for laboratory, anesthesia, radiology, or
pathology, if such services are received in connection with
care from a network provider or from a network hospital
• Services for treatment received while on vacation or
business travel in the U.S., where such treatment either
could not have reasonably been foreseen prior to the
travel or the course of treatment began prior to the travel
and for medical reasons must be continued during such
travel, or

The medical plan
69
• Until the next Annual Enrollment, when coverage under
the Plan is added and utilizing a non-network provider in a
course of treatment begun prior to effectivedate, where
there is no interruption of the doctor/patient relationship.
If your third-party administrator determines that any of
the above circumstances apply, services are covered at
the network coinsurance rate of 75%. You may have to
pay for treatment when you receive it and file a claim
for reimbursement, which will be based on the maximum
allowable charge. This means that the provider may bill you
for the difference between the maximum allowable charge
and the provider’s actual charge.
In addition, with respect to transport by ambulance or
air ambulance, out-of-network covered expenses may be
treated as network covered expenses. The amounts paid by
the AMP for ambulance or air ambulance are based on up to
200% of the maximum allowable charge if the participant is
directly admitted to the hospital from an emergency room
or if the participant dies prior to hospital admission.
Amounts in excess of 200% of the maximum allowable
charge are your responsibility and do not count toward your
annual deductible or out-of-pocket maximum. Exceptions
to the maximum allowable charge are not granted in
circumstances other than those described in this section.
For information about air ambulance coverage, call your
health care advisor at the number on your plan ID card.
Emergency room visits. The emergency room copay is
$300 per visit. This copay is in addition to your annual
deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the
maximum allowable charge for covered services and
only covered services will apply to the annual deductible.
If the third-party administrator determines that the
emergency room visit is an “emergency,” the AMP will
pay 100% of the maximum allowable charge after you
have met your applicable annual deductible, regardless
of whether the facility is a network facility. However, if it
is a non-network facility, you will still be responsible for
any amount over the maximum allowable charge. If you
participate in any local plan identified on page 50 of this
2020 Associate Benefits Book, the facility is a non-network
facility, and the third-party administrator determines
that the emergency room visit is not an “emergency,”
the services will not be covered by the AMP. For all other
participants, the AMP will pay 50% of the maximum
allowable charge for covered services after you have met
your deductible and you will be responsible for paying
the deductible, the other 50%, and any amount over the
maximum allowable charge. The $300 copay is waived if
the patient is directly admitted to the hospital from an
emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described
above apply to all services provided in the emergency
room(physician, facility, tests, etc.).
COVERAGE WHEN YOU TRAVEL TO A
FOREIGN COUNTRY
If you travel abroad, follow these steps:
• Before you begin your travel, contact
your third-party administrator (or your
HMO) for details about medical coverage
and emergency medical services when
traveling abroad. Coverage outside the
United States may vary.
• Always carry your plan ID card with you
when you travel and present it when you
receive medical services.
Alternate provider networks
In some locations and under certain circumstances, AMP
participants have access to alternate provider networks
that have coverage provisions differing in certain ways
from the medical plan provisions detailed on the preceding
pages. An alternate network is essentially a network within
a network, a subgroup of providers within the medical
plan’s larger network in a particular service area. In areas
where an alternate network operates, you must see the
alternate network providers to receive network terms
under the Plan — i.e., network annual deductibles and
network-level coinsurance.
If you seek services from medical providers who are within
the area served by the alternate network but have not agreed
to be providers within the alternate network, those services
are treated as out-of-network and covered accordingly.
General information about these special alternate
networksfollows.
ALTERNATE NETWORKS THROUGH
BLUEADVANTAGE ADMINISTRATORS
OFARKANSAS
If you have BlueAdvantage Administrators of Arkansas as
your third-party administrator, you may have access to
alternate networks of providers as listed below.
• Florida: NetworkBLUE
• Georgia: Blue Open Access POS
• Kansas City, Missouri: Preferred-Care Blue
• Maryland, Northern Virginia, District of Columbia:
BlueChoice Advantage Open Access
• Missouri: Blue Preferred POS
• New Hampshire: BlueChoice Open Access POS
• New Jersey: Horizon Managed Care Network
• Oklahoma: Blue Preferred

The medical plan
70
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• Pennsylvania: Community Blue Network
• Tennessee: Network S
• Wisconsin: Blue Preferred POS
For information about these alternate networks, go to
One.Walmart.com or call your health care advisor at the
number on your plan ID card.
ADVANCED IMAGING NETWORK
If you participate in the Premier Plan, Contribution Plan, or
Saver Plan options, at any location nationwide, an alternate
network of providers for advanced imaging services (i.e.,
MRI and CT scans) may be available to you. For information
about the alternate advanced imaging network, call your
health care advisor at the number on your plan ID card.
ADDITIONAL NETWORK THROUGH
UNITEDHEALTHCARE
If UnitedHealthcare is your third-party administrator and
you work in the following locations, you have access to
HPHC Insurance Company, an affiliate of Harvard Pilgrim
Health Care:
• Massachusetts
• Maine
• New Hampshire.
Preventive care program
See page 328 for clarifications of the preventive care
program and changes to the list of preventive services
effective Jan. 1, 2021.
Eligible preventive care services from network providers are
covered under the AMP at 100%.
If you are enrolled in the Premier Plan, Contribution Plan,
or Saver Plan and your work location is other than central
Florida, Dallas/Fort Worth or northwest Arkansas, the AMP
reduces the benefit to 50% if you use a non-network provider
for eligible preventive care services. Your out-of-pocket
costs do not apply toward your out-of-pocket maximum.
If you are enrolled in the Premier Plan, Contribution Plan,
or Saver Plan and your work location is in central Florida,
Dallas/Fort Worth or northwest Arkansas, or if you are
enrolled in one of the local plans, no benefits are provided if
you use a non-network provider for eligible preventive care
services. Your out-of-pocket costs do not count toward your
out-of-pocket maximum.
For a preventive care service to be eligible for 100%
coverage, it must be recommended by one of the agencies
responsible for maintaining U.S. preventive care guidelines,
as required under the Affordable Care Act. Many of these
guidelines are specific to gender, age, or risk factors
for a disease or condition. Check with your third-party
administrator for details.
Covered services include those listed below. Refer to your
third-party administrator for information on preventive
services not listed here. For the most up-to-date list of
covered preventive services, go to One.Walmart.com or
call your third-party administrator at the number on your
plan ID card.
COVERED PREVENTIVE SERVICES FOR ADULTS
• Abdominal aortic aneurysm one-time screening for men
of specified ages who have ever smoked
• Alcohol misuse screening and counseling
• Aspirin use for men and women of certain ages
(prescription required). See The pharmacy benefit for
more information.
• Blood pressure screening for all adults
• Colorectal cancer screening for adults over 50
• Depression screening for adults
• Diabetes (type 2) screening for adults age 40–70 who
are overweight or obese, and counseling for patients with
abnormal blood glucose
• Diet and physical activity counseling for adults at higher
risk for chronic disease
• Exercise or physical therapy for community-dwelling
adults age 65 and older who are at increased risk for falls
• Hepatitis B screening for adults at high risk
• Hepatitis C screening for adults at high risk
• HIV screening for all adults at higher risk
• Immunization vaccines for adults — doses, recommended
ages, and recommended populations vary:
– Haemophilus influenzae type b
– Hepatitis A
– Hepatitis B
– Herpes zoster
– Human papillomavirus
– Influenza (flu shot)
– Measles, mumps, rubella
– Meningococcal
– Pneumococcal
– Tetanus, diphtheria, perussis
– Varicella
Learn more about immunizations and see the latest vaccine
schedules at: cdc.gov/vaccines/schedules.
• Latent tuberculosis infection (LTBI) screening in
populations at increased risk
• Lung cancer screening for certain adults age 55–80 who
have a smoking history
• Obesity screening and counseling for all adults
The medical plan
71
• Sexually transmitted infection (STI) prevention counseling
for adults at higher risk
• Skin cancer counseling for young adults to age 24
• Syphilis screening for all adults at higher risk
• Tobacco use screening for all adults and cessation
interventions for tobacco users
COVERED PREVENTIVE SERVICES FOR
WOMEN, INCLUDING PREGNANT WOMEN
• Aspirin (low dose) for women 12 weeks pregnant who are
at high risk for preeclampsia (prescription required). See
The pharmacy benefit for more information.
• Bacteriuria urinary tract or other infection screening for
pregnant women
• BRCA counseling about genetic testing for women at
higher risk; and, if indicated after counseling, BRCA testing
• Breast cancer chemoprevention counseling for women at
higher risk
• Breast cancer mammography screenings every 1–2 years
for women over 40
• Breast cancer risk-reducing prescription medications
(such as Tamoxifen or Raloxifene) for certain women at
increased risk for breast cancer
• Breastfeeding comprehensive support and three
counseling visits from trained providers, as well as access
to breastfeeding supplies for pregnant and nursing women.
Check with your third-party administrator for details on
how to obtain a breast pump.
• Cervical cancer screening for women age 21–65
• Chlamydia infection screening for younger women and
other women at higher risk
• Contraception: Food and Drug Administration–approved
contraceptive methods, sterilization procedures
and patient education and counseling, not including
abortifacient drugs. See The pharmacy benefit for
information about contraception.
• Domestic and interpersonal violence screening and
counseling for all women and, when needed, initial
intervention services
• Folic acid supplements for women who may become
pregnant (prescription required). See The pharmacy
benefit for more information.
• Gestational diabetes screening for women 24–28weeks
pregnant and those at high risk of developing
gestationaldiabetes
• Gonorrhea screening for younger women and other
women at increased risk
• Hepatitis B screening for pregnant women at their first
prenatal visit
• Human immunodeficiency virus (HIV) screening
andcounseling
• Osteoporosis screening for women over age 65, and
younger postmenopausal women depending on risk factors
• Preeclampsia screening for pregnant women, with blood
pressure measurements throughout pregnancy
• Rh incompatibility screening for all pregnant women and
follow-up testing for women at higher risk
• Sexually transmitted infections (STI) counseling for
sexually active women
• Syphilis screening for all pregnant women or other women
at increased risk
• Tobacco use screening and interventions for all women,
and expanded counseling for pregnant tobacco users
• Well-woman visits to obtain recommended preventive
services for women
COVERED PREVENTIVE SERVICES
FORCHILDREN
• Anemia screening for children at 12 months
• Autism screening for children at 18 and 24 months
• Behavioral assessments for children of all ages
• Bilirubin screening for newborns
• Blood pressure screening for children of all ages
• Blood screening for newborns
• Cervical dysplasia screening for sexually active females
• Congenital hypothyroidism screening for newborns
• Critical congenital heart defect screening for newborns
• Depression screening for adolescents
• Developmental screening for children under age 3, and
surveillance throughout childhood
• Dyslipidemia screening for children at higher risk of
lipiddisorders
• Fluoride chemoprevention supplements for children
without fluoride in their water source and fluoride
varnish to the primary teeth of all infants and children
(prescription required)
• Gonorrhea preventive medication for the eyes of
allnewborns
• Hearing screening for all children
• Height, weight, length, head circumference, weight for
length and body mass index measurements for children
• Hemoglobinopathies or sickle cell screening for newborns
• Hepatitis B screening in adolescents at high risk
• HIV screening for adolescents

The medical plan
72
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• Immunization vaccines for children from birth to
age18 — doses, recommended ages, and recommended
populations vary:
– Diphtheria, tetanus, perussis (DTaP and Tdap)
– Haemophilus influenzae type b
– Hepatitis A
– Hepatitis B
– Human papillomavirus
– Inactivated poliovirus
– Influenza (flu shot)
– Measles, mumps, rubella
– Meningococcal
– Pneumococcal
– Rotavirus
– Varicella
Learn more about immunizations and see the latest vaccine
schedules at cdc.gov/vaccines/schedules.
• Lead screening for children at risk of exposure
• Medical history for all children throughout development
• Obesity screening and counseling
• Oral health risk assessment for young children, newborn
to 10 years
• Phenylketonuria (PKU) screening for this genetic disorder
in newborns
• Physical examination for children of all ages
• Sexually transmitted infection (STI) prevention counseling
and screening for adolescents at higher risk
• Skin cancer counseling for young adults to age 24 and
parents of young children
• Tobacco, alcohol, or drug use assessment for adolescents
at higher risk
• Tobacco use interventions in school-aged children
andadolescents
• Tuberculin testing for children at higher risk of tuberculosis
• Vision screening for all children.
FLU VACCINE PROGRAM
See page 328
An annual flu vaccination is covered under the AMP at 100%
during the September–March flu season when you receive
the vaccine from a network provider.
If you are enrolled in the Premier Plan, Contribution Plan,
or Saver Plan and your work location is other than central
Florida, Dallas/Fort Worth, or northwest Arkansas, the
AMP reduces the benefit to 50% of the maximum allowable
charge if you use a non-network provider for the vaccine,
and you are responsible for the other 50% plus any amount
above the maximum allowable charge. Your out-of-pocket
costs do not apply toward your out-of-pocket maximum.
If you are enrolled in the Premier Plan, Contribution Plan,
or Saver Plan and your work location is in central Florida,
Dallas/Fort Worth, or northwest Arkansas, or if you are
enrolled in one of the local plans, no benefits are provided
if you use a non-network provider for the vaccine. Your
out-of-pocket costs do not count toward your out-of-
pocket maximum.
The vaccine may also be provided in participating Walmart
and Sam’s Club pharmacies. If you are enrolled in the AMP,
you must show your plan ID card to receive the vaccine.
BEHAVIORAL HEALTH: MENTAL HEALTH AND
SUBSTANCE ABUSE PROGRAM
The AMP includes coverage for mental health and
substance abuse services in the same manner as other
medical and hospitalization benefits, including care at a
behavioral health facility.
Coverage is provided for:
• A behavioral health facility is one that provides 24-hour
inpatient care
• Residential treatment
• Partial hospitalization or outpatient care that requires six
to eight hours of service per day, five to seven days per
week, or
• Intensive outpatient care that requires two to four hours of
service per day, three to five days per week.
Refer to the medical plan summary charts earlier in this
chapter for details on how behavioral health services are
covered under the available plans.
Prenotification
You or your provider may voluntarily contact your third-party
administrator for information regarding coverage prior to your
obtaining most medical and behavioral health services by calling
the number on your plan ID card. If you choose to notify your
third-party administrator of a scheduled medical or behavioral
health admission, do so at least 24 hours prior to the admission.
For emergency services, third-party administrators should
be notified as soon as possible, but no later than 24 hours
after admission. Providing notification within 24 hours after
admission is not, however, required as a condition of coverage.
The third-party administrator’s responses to your inquiries in
a prior-notification call do not guarantee payment or ensure
coverage under the AMP, nor do any statements made by the
third-party administrator waive any AMP condition applicable
to your claim for benefits. The third-party administrator
cannot make a final claim determination on the phone or by
email. This means that any responses given by phone or email
are always subject to further review under the written terms,
conditions, limitations, and exclusions of the AMP.
The medical plan
73
Your coverage may be limited or denied if, when claims for
services are received, review shows that a benefit exclusion
or limitation applies, the covered participant was not eligible
for benefits on the date services were provided, coverage
lapsed for nonpayment of premiums, out-of-network
limitations apply, or any other basis exists for denial of the
claim under AMP terms.
Preauthorization
Network providers are required to obtain prior
authorization for certain services, including the following:
• Inpatient admissions (to hospital, hospice, and other
facilities) for medical benefits, including residential
treatment facilities
• Inpatient admissions (to behavioral health facilities) for
mental health and substance abuse benefits
• Maternity inpatient stays that exceed the third-party
administrator’s standard length of stay
• Home health care
• Outpatient surgery
• Outpatient radiology services, including MRI and CT scans
• Outpatient dialysis
• Outpatient services for mental health and substance
abuse, including:
– Detoxification
– Electroconvulsive therapy (ECT)
– Applied behavior analysis (ABA)
– Neuropsychological testing
– Parial hospitalization day treatment
– Intensive outpatient treatment
– Psychiatric home care
• Non-emergency ambulance (air or ground)
• Reconstructive procedures that may be considered cosmetic
• BRCA genetic testing
• Rehabilitation services (physical therapy, occupational
therapy, speech therapy)
• Certain prosthetic devices and durable medical equipment
• Clinical trials
• Specialty drugs issued by provider
• Services provided under the Centers of Excellence
program, including:
– Hear surgery
– Spine surgery
– Hip and knee replacement
– Transplants (including organ, stem cell, bone marrow,
and kidney)
– CAR T-cell therapy
– Ventricular assist devices (VADs) and total arificial hears
– Weight loss surgery
Prior authorization requirements vary based on third-party
administrator. For a complete list of services for which
preauthorization is required, call your health care advisor at
the phone number on your plan ID card.
Your network provider will seek preauthorization of
these services on your behalf. For non-network services,
you may need to seek preauthorization yourself. If your
preauthorization request is approved, the requested
services will be treated as covered services under the AMP
as long as you are otherwise eligible to receive benefits.
If your preauthorization request is denied, you and your
provider will be notified, and either you or your provider
may appeal the denial. If you proceed with a service that is
not preauthorized, you may be responsible for paying all of
your provider’s charges. For information on how to appeal
a denied request for preauthorization, see the Claims and
appeals chapter.
Helping you manage your health
YOUR HEALTH CARE ADVISOR
When you need to communicate with your third-party
administrator—to seek approval for a service, speak to a
registered nurse, ask about a claim or another matter—call
the number on your plan ID card. This connects you to
your health care advisor, your single point of contact for
all inquiries. Depending on the nature of your issue, the
health care advisor will answer your question or direct you
to the appropriate department. This process helps ensure
that you receive consistent information and guidance for
coverage-related inquiries.
CARE MANAGEMENT
If you are enrolled in a plan offered by the AMP, you have the
benefit of voluntary care management services, including a
personal medical team. These services are intended to bring
consistency to the full range of care and services provided
to AMP participants. Successful care management aims to
look at the whole individual rather than just the symptoms
orconditions being diagnosed; it can result in higher quality
of care, improvement in your experience with your providers
and third-party administrator, and potentially lower
out-of-pocket medical expenses.
Circumstances in which a nurse care manager may work
with you include the following:
• You are sick or injured and hospitalized
• You are scheduled for surgery
• You find out you have a chronic illness or are dealing with
an ongoing chronic illness
• You have a behavioral health/substance abuse condition
• You are prescribed multiple prescription drugs with
potential interactions
The medical plan
74
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• You simply have a question about your health
• You are home from the hospital and need help
understanding your discharge plan, or
• You are participating in the Life with Baby Maternity
Program, or comparable maternity program offered by
certain local plan options.
Your third-party administrator’s care management program,
working with your medical provider, can approve certain
medically necessary services that are not otherwise covered
by the AMP because they exceed a treatment limit (i.e.,
number of days or visits). The AMP’s rules regarding annual
deductibles and coinsurance continue to apply to any
additional benefits authorized by the care management
program. All such decisions are subject to your third-party
administrator’s determination of medical necessity.
Your medical team may also be able to assist you with
medical costs you may incur for “involuntary” out-of-
network services. These are costs you incur when you
cannot control your choice of provider (such as if you
have surgery in a network hospital but your anesthesia is
administered by an anesthesiologist who is a non-network
provider) or when you have no reasonable basis for believing
your provider is a non-network provider. In some cases,
out-of-network benefits may be paid as network benefits
(see When network benefits are paid for out-of-network
expenses earlier in this chapter). In other cases, your
third-party administrator may negotiate with non-network
providers before or after services are rendered to reduce
the billed charges for which you are responsible under the
Plan’s out-of-network benefit. There are no guarantees that
any reduction in your out-of-network costs will occur.
When you communicate with your third-party administrator,
depending on the nature of your inquiry, you may be routed
to your nurse care manager. On other occasions, your nurse
care manager may reach out to you, for example to invite
you to participate in a health management program.
To reach your medical team, call the phone number on your
plan ID card. Participation in the program is voluntary and
does not affect your eligibility to participate in the AMP.
QUIT TOBACCO PROGRAM
According to the National Institutes of Health, tobacco
use is a leading cause of preventable disease and death in
the United States. To help you kick the habit, the company
offers a free Quit Tobacco program for you and your
covered dependents age 18 and older who are enrolled in a
company-sponsored medical plan.
When you enroll in the program, a variety of services may
be available to you, including:
• Online support from coaches and other quitters.
• Phone-based coaching with a trained health coach.
• Email support with tips to help you quit and stay motivated.
• Over-the-counter (OTC) medications, including free
patches, gum, or lozenges. (You may hear these medications
referred to as “nicotine replacement therapy” or “NRT.”)
To enroll in a Quit Tobacco program call 866-577-7169.
If you are enrolled in an HMO, contact your provider to learn
what quit-tobacco programs are offered through your plan.
Learn more about the Quit Tobacco program at the Quit
Tobacco link at One.Walmart.com.
LIFE WITH BABY MATERNITY PROGRAM
Life with Baby is an exclusive prenatal care program offered at
no cost to you, your covered spouse/partner, and other covered
dependents. The program is available to you if you are enrolled
in the AMP with the exception of some local plans, which
provide comparable maternity programs for their participants.
(Call your health care advisor for more information.)
Whether you’re starting a family, adding to one, or just
thinking about it, Life with Baby can help you have a safe,
successful pregnancy. The program is offered at no cost,
but enrollment is not automatic. The program assists with
preconception, pregnancy, delivery (including three lactation
visits), and child development. Enroll in Life with Baby by
calling your health care advisor at the phone number on your
plan ID card. Once enrolled, you’ll have the opportunity to talk
confidentially with a registered nurse before, during, and after
your pregnancy. Participation in the program is voluntary and
does not affect your eligibility to participate in the AMP.
GRAND ROUNDS: PROVIDER RESEARCH AND
SECOND OPINIONS
Grand Rounds is a personalized tool that lets you
search for doctors and medical services online, view
quality information, obtain second opinions, and get
additional details about a provider’s charges. Register at
grandrounds.com/walmart or by calling Grand Rounds at
800-941-1384. There is no cost to you to use the Grand
Rounds tool, but any medical expenses you incur as a result
of your use of this tool will be subject to Plan rules.
Provider research: Participants and dependents age 18
and over who are enrolled in the Plan, with the exception
of participants in central Florida, Dallas/Fort Worth, and
northwest Arkansas, are eligible to use Grand Rounds’ provider
research functions. Register at grandrounds.com/walmart or
by calling Grand Rounds at 800-941-1384.
With Grand Rounds you can:
• Compare nearby doctors based on quality
• Learn about provider costs
• Review your Plan details, including your progress toward
meeting your deductible and out-of-pocket maximum

The medical plan
75
If your work location is in central Florida, Dallas/Fort Worth,
or northwest Arkansas, contact your health care advisor
at the number on your plan ID card to obtain information
on network doctors and Plan details. You can also find
information on network providers on One.Walmart.com.
Second opinions: Participants and dependents who are
enrolled in the Plan are eligible to obtain an expert second
opinion with Grand Rounds (for eligible dependents under
age 13, the service must be provided to a parent). Under
certain circumstances, when you have received a diagnosis
or been recommended for surgery or a certain treatment,
the AMP will cover second opinions provided online
through Grand Rounds.
Claims advocacy: Grand Rounds’ care team can assist you
with the financial aspects of medical claims. Specialized
claims experts can answer your questions regarding
medical bills or explanations of benefits, organize insurance
paperwork, audit provider and hospital charges, advocate
on your behalf to resolve billing inaccuracies, and negotiate
with providers and insurers as needed for claim denials.
TELEHEALTH VIDEO VISITS THROUGH
DOCTOR ON DEMAND
Under certain circumstances, the AMP covers doctor
consultations using telecommunication technologies such
as video visits. Participants enrolled in the AMP have access
to Doctor On Demand, a telehealth service offering video
medical and mental health visits. Doctor On Demand’s
contracted providers can diagnose, treat, and write
prescriptions for a wide range of non-emergency medical
issues. The service is available in all 50 states, 24 hours a
day, seven days a week by computer, tablet, or smartphone.
Doctor On Demand cannot provide treatment for medical
emergencies or for chronic conditions like diabetes.
Doctor On Demand submits claims for services directly
to covered participants’ third-party administrators. For all
eligible participants except for participants in the Saver
Plan option, telehealth consultations are subject to a $4
copay. For participants in the Saver Plan option, services
are subject to the same coverage terms as conventional
doctor visits (deductible, coinsurance, etc.) until you
meet the annual deductible, after which consultations are
subject to a $4 copay. For information about services and
technical requirements, visit Doctor On Demand online at
doctorondemand.com or call 800-997-6196.
See page 328 for information on new programs to help you
manage your health.
Walmar clinics
Walmart Care Clinic and Walmart Health are primary care
clinics found in select Walmart stores. They offer retail
primary care services including office visits, lab tests, and some
preventive care services, for individuals age two and older.
Office visits are offered to most covered associates at the
discounted price of a $4 copay, regardless of residency or
work location. Due to IRS rules governing health plans that
are used with health savings accounts, if you are enrolled in
the Saver Plan option you must pay the posted retail price
when using the Walmart Care Clinic or Walmart Health,
unless the clinic visit is limited to preventive services.
HSA dollars may be used as payment for qualified medical
expenses received at the clinics.
Lab tests and immunizations that are performed entirely
within the clinic setting but not covered as preventive care
under the AMP are available at a separate charge in addition
to the visit charge. Tests ordered within the Walmart Care
Clinic or Walmart Health but performed outside the clinic
setting are treated as covered network charges under the
AMP. These charges are subject to the AMP’s maximum
allowable charge and you would be responsible for any
difference between the AMP’s maximum allowable charge
and the provider’s actual charge.
Certain preventive services available at the Walmart Care
Clinic or Walmart Health are covered under all AMP options.
These preventive services are covered at no cost to you and
your dependents. See the Preventive care program section
earlier in this chapter for a list of services covered at 100% if
you are enrolled for medical coverage under the AMP.
NETWORK COVERAGE FOR CERTAIN
WALMART CLINICS
Your third-party administrator may contract with individual
Walmart Care Clinics and/or Walmart Healths to be
network providers, but not allWalmart clinics are network
providers. The manner in which the AMP treats your out-
of-pocket expenses at a Walmart clinic depends on the
clinic’s network status, as follows:
If the Walmart clinic is a network provider under your medical
plan option: The clinic will file insurance claims withyour
third-party administrator. Any eligible out-of-pocket costs
you incur in that clinic (after your $4 copay) will be subject to
your annual deductible and out-of-pocket maximum under the
same rules that apply toa network provider.
If the Walmart clinic is not a network provider under
yourPlan option: The clinic will not file insurance claims
with your third-party administrator. Out-of-pocket
costs you incur are not reimbursable under the AMP
and will not be credited against your annual deductible
or out-of-pocket maximum.
To find out whether a Walmart Care Clinic or Walmart
Health is a network provider, view your network provider
directory or contact your third-party administrator.

The medical plan
76
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Centers of Excellence
The Centers of Excellence program works with specific
facilities to provide medical services related to a range of
treatments and procedures. Through this program, you
and your covered dependents have access to specialized
providers and facilities selected for their expertise in
certain high-risk or high-cost procedures. The AMP offers
this program so that participants facing certain serious
medical conditions can receive high-quality care. The
Centers of Excellence program covers:
• Surgeries for certain heart conditions (age 18 and up)
• Surgeries for certain spine conditions (age limitations
apply to some spine conditions, such as scoliosis)
• Hip replacement surgery
• Knee replacement surgery
• Medical record review by a Centers of Excellence facility
for certain types of cancer (all ages) to determine if an on-
site evaluation is recommended
• Medical record review by a Centers of Excellence facility for
outpatient kidney dialysis or end-stage renal disease (ESRD)
(all ages) to determine if an on-site evaluation for kidney
transplant evaluation is recommended
• Liver, kidney, heart (including durable ventricular assist
devices [VADs] and total artificial hearts), lung (including
lung volume reduction surgery [LVRS]), pancreas,
simultaneous kidney/pancreas, multiple organ, and bone
marrow/stem cell transplants (including CAR T-cell
treatment), and
• Gastric bypass and gastric sleeve weight loss surgeries
(age18 and up).
This section describes the program in greater detail,
including important conditions and restrictions. The
Centers of Excellence chart below summarizes terms for
the medical services covered under the program. See also
the Transplant and Weight loss surgery sections later in this
chapter for details about those benefits.
As shown in the Centers of Excellence chart below, certain
eligible services performed at one of the medical centers
included in the program are covered at 100% with no annual
deductible (excluding weight loss surgery). However, if you
are enrolled in the Saver Plan, you must meet your annual
deductible before the Plan will make any payments, due to
federal tax laws.
See page 329
CENTERS OF EXCELLENCE
Centers of Excellence Program Your Medical Plan Network
Heart surgery
Cancer medical record review
with on-site evaluation if recommended
Eligible cancer types: breast, colorectal,
lung, prostate, blood (including myeloma,
lymphoma, leukemia)
Outpatient kidney dialysis or ESRD
medical record review with on-site kidney
transplant evaluation if recommended
100%
No deductible*
75%
After deductible
Hip and knee replacement
100%
No deductible*
Premier, Contribution, Saver Plans in areas other
than central FL, Dallas/Ft. Worh, and NW AR:
50% after out-of-network deductible
Premier, Contribution, Saver Plans in central FL,
Dallas/Ft. Worh, or NW AR:
50% after deductible
Local plans:
No coverage**
Spine surgery 100%
No deductible*
No coverage**
Transplant (Mayo Clinic only. Excludes
cornea and intestinal transplant)
100%
No deductible*
No coverage**
Weight loss surgery (Gastric bypass
andgastric sleeve)
75%
After deductible
No coverage**
* Due to federal tax law, paricipants in the Saver Plan must meet their annual deductible before 100% benefits can be provided.
** See the adjacent Centers of Excellence text for circumstances when exceptions may apply.

The medical plan
77
Additional program conditions and restrictions are
described in the adjacent Center of Excellence text.
If you believe you may be a candidate for Centers of
Excellence services, call your health care advisor at the
phone number on your plan ID card. To participate in the
Centers of Excellence program:
• Services must be scheduled and preauthorized by one
of the administrators for the Centers of Excellence
program. The particular administrators from whom
preauthorization must be obtained vary, depending on
the specific service to be provided and in certain cases
the associate’s medical coverage, as listed in the Centers
of Excellence administration chart below.
• If your request for preauthorization of a Centers
of Excellence service is denied, you have the right
to appeal. See the Claims and appeals chapter for
information. Note that services performed at a Centers
of Excellence facility that are not covered services under
the terms and conditions of the Centers of Excellence
program are subject to regular coverage and payment
terms under the AMP.
• For most eligible services, you must identify a
designatedcaregiver who is willing and able to meet
caregiver requirements.
• For most eligible services, you must be safe to travel for
medical care and must not require emergency care at the
time of travel.
• The medical center where you receive services is
determined by where you live and the indicated service.
• You acknowledge that the medical center must receive
necessary medical records prior to your acceptance into
the program.
• You must supply contact information for a local physician
who has agreed to manage your follow-up care after you
return home from the Centers of Excellence facility.
• After consultation with you, the third-party
administrator determines that your claim for benefits is
not subject to subrogation under terms of the Plan (see
The Plan’s subrogation and reimbursement rights in the
Claims and appeals chapter).
See page 329
Travel, lodging, and a daily allowance are provided for you
and a caregiver for all services covered under the Centers
of Excellence program except weight loss surgery. These
travel services must be preauthorized and scheduled
through the Centers of Excellence program. Payment is
subject to applicable limits. (Travel benefits may not be
available if you are enrolled in one of the local plan options.)
Specialized care benefit: In some cases, your third-party
administrator may consult with Grand Rounds to determine
whether services you need are available at a particular facility.
If Grand Rounds recommends that you be evaluated at a
specific facility based on your condition, even if the facility is
not a Centers of Excellence facility, the AMP will assist with
the same travel benefits as those paid for travel to a Centers of
Excellence facility. These travel services must be preauthorized
by Grand Rounds and scheduled by HealthSCOPE Benefits.
Reimbursement for medical treatment or services at the
facility are paid under otherwise applicable terms, and are
not reimbursed as Centers of Excellence services at the
rates listed in the chart on the previous page.
If you have a medical condition eligible for care under the
Centers of Excellence program and you choose to receive
treatment in a facility outside the Centers of Excellence
program, your care will not be covered at the Centers
of Excellence rates. Your care will instead generally be
subject to regular AMP coverage terms, as summarized in
the Centers of Excellence chart on the previous page and
in greater detail earlier in this chapter. Similarly, services
you receive prior to arrival or following discharge from a
Centers of Excellence facility, including services approved
by the Centers of Excellence program administrator, are
subject to regular AMP coverage terms.
NOTE: Under limited circumstances, the AMP covers out-
of-network coverage for certain Centers of Excellence
procedures. These exceptions apply only to participants in
the Premier Plan, Contribution Plan, or Saver Plan whose
work location is other than central Florida, Dallas/Fort Worth,
or northwest Arkansas. For such eligible AMP participants, if
you are a candidate for heart surgery, cancer medical record
review, hip or knee replacement, or outpatient kidney dialysis
review, and you choose to see a non-network provider,
services will be covered at a 50% coinsurance rate after you
meet your out-of-network deductible.
CENTERS OF EXCELLENCE ADMINISTRATION
NOTE: If you are enrolled in a local plan, call your health care advisor to be directed to the appropriate administrator.
Hear surgery Contigo Health (formerly Health Design Plus)
Cancer medical record review (On-site travel if recommended) HealthSCOPE Benefits
Outpatient kidney dialysis or ESRD medical record review HealthSCOPE Benefits
Spine surgery Contigo Health (formerly Health Design Plus)
Hip and knee replacement Contigo Health (formerly Health Design Plus)
Transplant (Mayo Clinic only. Excludes cornea and intestinaltransplant) HealthSCOPE Benefits
Weight loss surgery (Gastric bypass and gastric sleeve) Contigo Health (formerly Health Design Plus)

The medical plan
78
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
SPINE SURGERY AND HIP OR KNEE
REPLACEMENT
Spine surgery: If you are eligible for Centers of Excellence
benefits and you choose to receive treatment in a facility
outside the Centers of Excellence program, your treatment
will be considered out-of-network, even if the provider is a
network provider for other purposes. In such circumstances,
no benefits are payable except in cases of emergency.
Hip or knee replacement: If you are eligible for Centers of
Excellence benefits and you choose to receive treatment in
a facility outside the Centers of Excellence program, your
treatment will be considered out-of-network, even if the
provider is a network provider for other purposes. In such
circumstances, the AMP’s coverage terms are as follows:
• If you have coverage under the Premier Plan, Contribution
Plan, or Saver Plan and your work location is in central
Florida, Dallas/Fort Worth, or northwest Arkansas, and you
have your procedure performed by a network provider,
the AMP coinsurance is 50% and you will be subject to the
network deductible before benefits are payable.
• If you have coverage under the Premier Plan, Contribution
Plan, or Saver Plan and your work location is in an area
other than central Florida, Dallas/Fort Worth, or northwest
Arkansas, and you have your procedure performed by a
network provider, the AMP coinsurance is 50% and you will
be subject to the out-of-network deductible before
benefits are payable.
See page 329
• If you have coverage under any of the local plan options
and have your procedure performed by a provider outside
the Centers of Excellence program, no benefits are
payable except in cases of emergency.
Requests for exceptions to coverage terms for spine
surgery and hip and knee replacement
In cases of spine surgery and hip and knee replacement, you
may request an exception to the rules stated immediately
above, which describe how the AMP covers these procedures
when they are performed outside the Centers of Excellence
program. You may request an exception so that procedures
performed by a network provider that is not a Centers of
Excellence provider be covered at a coinsurance rate of 75%
of the network discounted rate; cost sharing will be applied
to your network deductible and network out-of-pocket
maximum. Depending on whether you have already received
treatment when you make your request, it will be treated as a
pre-service claim or post-service claim (as described below)
and decided under special rules for granting exceptions to
the AMP’s coverage terms for spine surgery and hip and knee
replacement under the Centers of Excellence program, as
described in the Claims and appeals chapter.
Pre-service exception request: If you have not yet received
treatment but are considering receiving services from a
non-Centers of Excellence provider, you may file a prior
authorization request (a pre-service claim). You can file a
pre-service claim if travel to the Centers of Excellence
provider would likely result in loss of life, paralysis, or
further injury. You can also file a pre-service claim if the
Centers of Excellence facility does not recommend spine
surgery or hip or knee replacement because it is not deemed
the appropriate medical course of treatment or you are
not an appropriate candidate for surgery. Your request
should be sent to Contigo Health (formerly Health Design
Plus) and will be considered by an Independent Review
Organization following the procedures described under
Special procedures for approval of exceptions to coverage
terms for spine surgery and hip and knee replacement in
the Claims and appeals chapter. If your request is granted,
coverage will be at the otherwise applicable network rate,
including any deductibles, coinsurance, or limitations. If your
request is denied because Contigo Health (formerly Health
Design Plus), through an Independent Review Organization,
determines that travel to a Centers of Excellence provider
is safe, based on the documentation received, coverage for
hip and knee joint replacement surgery at a non-Centers
of Excellence facility will be paid at 50%, as outlined earlier,
and no benefits will be payable in the case of spine surgery
performed at a non-Centers of Excellence facility, also as
outlined earlier.
See page 330
Decisions not to move forward with spine surgery or hip or
knee replacement by the respective Centers of Excellence
providers are not subject to review under this process if the
Centers of Excellence provider’s decision is based on a
determination that the procedure is not appropriate
because you refuse to comply with medical restrictions or
requirements, including weight loss, smoking cessation,
alcohol cessation, social support, or similar factors.
Post-service exception request: If you already have received
services from a non-Centers of Excellence provider,
you may file a post-service claim with your third-party
administrator, as described in the Claims and appeals
chapter. Your claim may be approved if:
• You experienced a traumatic injury resulting in the need
for immediate surgery or were in need of immediate
surgery, without which you would have likely incurred loss
of life or paralysis, or
• Services were provided by a network provider that began
a course of treatment prior to the effective date of this
provision and there has not been an interruption of the
doctor-patient relationship.
If your claim is approved, coverage will be at the otherwise
applicable network or non-network rate, depending on
your provider, including any deductibles, coinsurance, or
limitations. If your claim is denied, you may request an
appeal as described in the Claims and appeals chapter.
The medical plan
79
LIMITED COORDINATION OF BENEFITS
The AMP generally does not coordinate benefits with respect
to claims under the Centers of Excellence program, other than
coordination with Medicare in the case of certain transplant
benefits or as otherwise required by law. For all other
Centers of Excellence services, if any portion of a Centers
of Excellence benefit could have been paid by another
health plan, the AMP will not pay any amount of the claim.
TRANSPLANTS
To be eligible for transplant, lung volume reduction surgery
(LVRS), or CAR T-cell treatment benefits under the Centers
of Excellence program, you must be enrolled in the AMP for
at least 12 months. If you are enrolled in the eComm PPO
Plan or an HMO plan, you are not eligible for transplant
benefits, but if you later become covered under one of the
AMP options, your time enrolled in the eComm PPO Plan
or an HMO will count toward the 12-month waiting period.
If you are not enrolled in one of the AMP options, any time
enrolled in critical illness insurance or accident insurance
will not count toward the 12-month waiting period.
If you terminate coverage for any reason and reenroll,
your prior time enrolled for coverage will count toward the
12-month waiting period.
The 12-month waiting period does not apply to insertion of
durable ventricular assist devices (VADs) or artificial hearts,
regardless of whether the VAD is related to a transplant.
The 12-month waiting period applies to the associate
and, separately, to most covered dependents (except
as described on the following page) — i.e., the covered
associate and each covered dependent must meet his or
her own 12-month waiting period. If you add AMP coverage
for a new dependent through birth, or adoption of the
child as of the child’s date of birth, your new dependent’s
12-month waiting period will be waived.
The 12-month waiting period is waived for localized associates
and their covered dependents. The 12-month waiting period
may also be waived when your doctor certifies that in the
absence of a transplant, the covered participant’s death
is imminent within 48 hours. See the Claims and appeals
chapter for information on requesting a waiver.
If your doctor recommends a transplant, call HealthSCOPE
Benefits at 479-621-2830 or 800-421-1362.
Guidelines for covered transplants
• You must undergo a pretransplant evaluation at Mayo
Clinic. In performing this evaluation, Mayo Clinic is not
acting as an agent of the AMP. It is the AMP’s intent that
this evaluation be made pursuant to the doctor/patient
relationship between Mayo Clinic and the participant.
Travel, lodging, and a daily allowance will be provided for
you and a caregiver for required transplant evaluations at
Mayo Clinic.
• Liver, kidney, heart (including durable ventricular assist
devices [VADs] and total artificial hearts), lung (including
lung volume reduction surgery [LVRS]), pancreas,
simultaneous kidney/pancreas, multiple organ, and bone
marrow/stem cell transplants (including CAR T-cell
treatment) must be performed at Mayo Clinic or an
approved facility, or no benefits are paid, except when
a formal network exception request is reviewed and
approved in instances where there is a significant risk
that travel to Mayo Clinic could result in death, or the
Independent Review Organization approves coverage at a
different facility where Mayo Clinic determines that it will
not recommend and perform a transplant because it is
not the appropriate medical course of treatment, or the
individual is not an appropriate candidate (see Requests
for organ transplants at facilities other than Mayo Clinic
on the next page).
• Claims for eligible transplant services performed at
Mayo Clinic (including pediatric) should be filed with
HealthSCOPE Benefits and are covered at 100% with
no annual deductible. However, if you are enrolled in
the Saver Plan, you must meet your annual deductible
before the Plan will make any payments due to federal
tax laws. Additionally, travel, lodging, and a daily
allowance are provided for you and a caregiver, subject
to applicable limits.
• The AMP does not cover transplantation of body parts
(e.g., face, hands, feet, legs, arms, uterus) under any
circumstances. Experimental and/or investigational
transplant-related services are not covered unless those
services are recommended and performed by Mayo Clinic
or an approved facility.
• Benefits for a covered transplant procedure at Mayo
Clinic, and related expenses, including travel, lodging, and
a daily allowance, end one year post-transplant or after a
one-year post-transplant evaluation is performed.
• Coverage for procedures and devices unrelated to a
transplant, as determined by Mayo Clinic, are not covered
at 100% and are subject to applicable AMP terms and
limitations, including annual deductibles and coinsurance
(network and out-of-network). This includes certain
gastric-sleeve procedures performed at Mayo Clinic during
a liver transplant.
• Non-transplant services performed at Mayo Clinic are not
covered at 100% and are subject to applicable AMP terms
and limitations, including copays, annual deductible, and
coinsurance (network and out-of-network).
• Travel for transplant-related services must be arranged
by a transplant coordinator. For travel arrangements, call
HealthSCOPE Benefits at 479-621-2830 or 800-421-1362.

The medical plan
80
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• Claims for transplants and LVRS that are not performed in
accordance with the guidelines stated in this chapter and in
the Claims and appeals chapter will be denied.
• Coverage is limited to transplantation of human organs.
Requests for organ transplants at facilities other than
MayoClinic
• You may file a claim with an Independent Review
Organization to request an organ transplant at a facility
other than Mayo Clinic if:
– There is significant risk that travel to Mayo Clinic could
result in death, or
– Mayo Clinic determines that it will not recommend and
perorm a transplant because it is not the appropriate
medical course of treatment or you are not an
appropriate candidate for a transplant.
Your claim must be received by the Plan within 120
calendar days of the initial denial of the transplant by Mayo
Clinic. Your claim will be decided under the special rules
for transplant claims at a facility other than Mayo Clinic, as
described in the Claims and appeals chapter.
• The Independent Review Organization will be made
up of individuals appointed by the AMP administrator
and will not include any employee of the company,
Mayo Clinic, or a third-party administrator of the AMP.
The Independent Review Organization will review any
relevant medical files that were reviewed or generated
by Mayo Clinic, as well as any additional materials you
submit, and will consider various factors, including
alternative courses of treatment, scientific studies and
evidence, other medical professionals’ opinions, the
investigational or experimental nature of the proposed
procedures, and the potential benefit the transplant
would have.
• If the Independent Review Organization determines
that the transplant and related course of treatment are
medically necessary, the Independent Review Organization
will approve an exception to pursue a transplant outside of
Mayo Clinic, under regular medical benefits.
– Claims will be covered at 75% for network providers
after you meet the annual deductible.
– If you are enrolled in the Premier Plan, Contribution
Plan, or Saver Plan, and your work location is other
than central Florida, Dallas/For Worh, or norhwest
Arkansas, claims are covered at 50% of the maximum
allowable charge if you use a non-network provider,
even after you’ve reached your out-of-pocket maximum.
You are responsible for your 50% share plus any
charges above the maximum allowable charge. The
amount you pay for out-of-network services applies
toward your network deductible until it is met, and also
applies to your out-of-network annual deductible. Your
network deductible applies toward your annual out-
of-pocket maximum. (Note that services provided by
non-network providers are not covered in the Premier
Plan, Contribution Plan, or Saver Plan in central Florida,
Dallas/For Worh, or norhwest Arkansas, or in any of
the local plan options, except in cases of emergency.)
– The Plan does not cover the cost of travel or lodging or
provide a daily allowance for such transplants.
See page 330
Transplant denials by Mayo Clinic are not subject to review
under this process if Mayo Clinic’s decision is based on a
determination that the transplant is not appropriate because
you refuse to comply with medical restrictions or
requirements, including weight loss, smoking cessation,
alcohol cessation, social support, or similar factors.
Transplant-related claims where treatment has already been
rendered are decided under the regular medical claims and
appeals procedures found in the Claims and appeals chapter.
Pediatric transplant recipients under age 19
• Pediatric transplant recipients under age 19 (except for
cornea and intestinal transplants) must undergo a pre-
transplant review and, upon request by Mayo Clinic, an
evaluation by Mayo Clinic.
• Once a Mayo review or visit is complete, if transplant
services are sought at a facility other than Mayo Clinic,
transplant claims will be considered at 75% for network
providers after you meet the annual deductible.
• If your medical plan option provides coverage for non-
network providers, claims are covered at 50% of the
maximum allowable charge if you use a non-network
provider, even after you reach your out-of-pocket
maximum. You are responsible for your 50% share plus
any charges above the maximum allowable charge. The
amount you pay for out-of-network services applies
toward your network deductible until it is met, and also
applies to your out-of-network annual deductible. Your
network deductible applies toward your annual out-of-
pocket maximum. (Note that services provided by non-
network providers are not covered in the Premier Plan,
Contribution Plan, or Saver Plan in central Florida, Dallas/
Fort Worth, or northwest Arkansas, or in any of the local
plan options, except in cases of emergency.)
• Travel, lodging, and a daily allowance are provided only if
the transplant is performed at Mayo Clinic.
Transplant donor expenses
• Eligible transplant donor expenses with respect to a
living donor are covered when the recipient is an AMP
participant who is eligible for transplant coverage and the
living donor’s medical plan or insurance provider does not
pay for transplant donor charges or expenses.
• Eligible transplant donor expenses with respect to travel
and lodging benefits must be arranged by a transplant
coordinator. It is your responsibility to provide contact
information for the transplant benefit administrator to the
eligible transplant donor, prior to appointments.

The medical plan
81
• Covered donor charges are paid at the same benefit level
as the recipient according to transplant guidelines, up to
120 days post-transplant.
• Cadaver organ acquisition and procurement expenses are
covered only when the expenses are part of the provider’s
contracted rate with the Plan’s third-party administrator.
CORNEA AND INTESTINAL TRANSPLANTS
Cornea and intestinal transplants are not
included in the Centers of Excellence
transplant program and can be performed at
the network facility of your choice, according
to these terms:
• Claims are covered at 75% for network
providers after you meet the annual
deductible.
• If your medical plan option provides
coverage for non-network providers,
claims are covered at 50% of the maximum
allowable charge if you use a non-network
provider, even after you’ve reached your out-
of-pocket maximum. You are responsible for
your 50% cost share plus any charges above
the maximum allowable charge. The amount
you pay for out-of-network services applies
toward your network deductible until it is
met, and also applies to your out-of-network
annual deductible. Your network deductible
applies toward your annual out-of-pocket
maximum. (Note that services provided by
non-network providers are not covered in
the Premier Plan, Contribution Plan, or Saver
Plan in central Florida, Dallas/Fort Worth,
or northwest Arkansas, or in anyof the local
plan options, except in cases of emergency.)
• No travel, lodging, or daily allowance is
provided for these transplants.
WEIGHT LOSS SURGERY BENEFIT
Certain weight loss surgeries are covered under the AMP
Centers of Excellence program, subject to specific criteria,
including but not limited to:
• Services must be provided by a physician and facility
designated by the AMP.
• If you wish to use the weight loss surgery benefit you must
be enrolled for medical benefits in the AMP for at least 12
months. If you are enrolled in the eComm PPO Plan or an
HMO, you are not eligible for weight loss surgery benefits,
but if you later become covered under one of the AMP
options, your time enrolled in the eComm PPO Plan or
an HMO will count toward the 12-month waiting period. If
you are not enrolled in one of the AMP options, any time
enrolled in critical illness insurance or accident insurance
will not count toward the 12-month waiting period. If you
terminate coverage for any reason and reenroll, your prior
time enrolled for coverage will count toward the 12-month
waiting period.
• You must be willing to travel to the designated facility at
your own expense (travel reimbursement is not provided).
• You must be at least 18 years of age.
• You must have either a body mass index (BMI) of 40 or
greater, or a BMI of 35 or greater and at least one obesity-
related comorbidity factor (type 2 diabetes, hypertension,
cardiovascular disease, etc.).
• You must agree to comply with all requirements for the
duration of the weight loss surgery treatment.
If you had a previous laparoscopic adjustable gastric band
procedure for weight loss purposes, and now need surgical
removal based on medical complications, you can apply
for the weight loss surgery benefit to be evaluated by a
Centers of Excellence facility to determine if you would
be an appropriate candidate for a conversion to a covered
weight loss surgery, during or in conjunction with the
removal of the gastric band. You will be required to provide
documentation demonstrating that you met the above-
mentioned clinical criteria for bariatric surgery prior to the
original lap band procedure.
Coverage for weight loss surgery is provided at the network
benefit level; after you meet your annual deductible for
eligible network expenses, the Plan pays 75% and you pay 25%.
If you meet the requirements stated above and your doctor
recommends weight loss surgery, call your health care advisor
at the number on your plan ID card to obtain a request form,
which must be completed by you and your physician. You must
send the completed request form to Contigo Health (formerly
Health Design Plus) at the address listed on the form. A claim is
considered filed when Contigo Health (formerly Health Design
Plus) receives the request form. The claim is determined under
the procedures for pre-service claims described in the Claims
and appeals chapter.
When limited benefits apply to
theAMP
Some services are subject to specific restrictions
and limitations in addition to annual deductible and
coinsurance/copayment requirements. If you have a
question on the coverage of a particular service, contact
the third-party administrator at the number on your plan
ID card.
The limitations and restrictions described below are
in addition to other AMP rules, including deductibles,
coinsurance/copayments, and exclusions. Consideration

The medical plan
82
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
may be given for additional coverage when authorized
by your nurse care manager, as described in the Care
management section.
Refer also to What is not covered by the Associates’
Medical Plan, later in this chapter.
Ambulance: Coverage of ambulance or air ambulance
transportation is limited to the nearest hospital or nearest
treatment facility capable of providing care, and only if such
transportation is medically necessary as compared to other
transportation methods of lower cost and safety.
The Plan covers ambulance or air ambulance transportation
between health care facilities if the treatment to be
provided at the second facility is medically necessary and
not available at the initial facility.
The Plan covers ambulance and air ambulance transportation
from a hospital to a hospice facility (including to a residence
where hospice care will be provided).
Ambulance charges for the sole convenience of the
participant, caregiver, or provider are not covered.
Birth control/contraceptives: Prescribed FDA-approved
contraceptive methods for women and female sterilization
are covered under women’s preventive care, including but
not limited to:
• Diaphragms: fitting and supply
• Cervical cap: fitting and supply
• Intrauterine device (IUD): fitting, supply, and removal
(including copper or with progestin)
• Birth control pills (including the combined pill, progestin-
only, and extended/continuous use)
• Birth control patch
• Vaginal ring
• Injection (e.g., Depo-Provera) given by a physician or nurse
every three months
• Implantable contraception (e.g., Implanon)
• Plan B, when prescribed
• Ella, when prescribed
• Female sterilization (including surgery and surgical
sterilization implant)
• Vaginal sponge, when prescribed
• Female condom, when prescribed
• Spermicide, when prescribed.
The AMP covers generic contraceptives only when
prescribed by a physician (and brand-name contraceptives
when medically necessary). If your attending physician
believes a brand-name contraceptive is medically
necessary, you may file a claim for coverage of the
brand-name drug.
Services and/or devices that are not included in the
contraceptive benefit are:
• Abortion
• Prescription abortifacient medication, including but not
limited to RU-486
• Male sterilization See page 330
• Over-the-counter birth control methods that are
not prescribed, including but not limited to Plan
B, spermicides, condoms, vaginal sponges, basal
thermometers, and ovulation predictor kits.
Clinical trials: Approved clinical trials are covered under
limited circumstances. Routine patient costs associated
with participation in Phases I–IV of approved clinical trials
to treat cancer or other life-threatening conditions, as
determined by the third-party administrator and required
by law. These costs are subject to the AMP’s applicable
deductibles and limitations and do not include costs of the
investigational item, device, or service, items provided
for data collection, or services that are inconsistent with
established standards of care.
Durable medical equipment (DME)/home medical supplies:
DME that satisfies all of the following criteria is covered,
except as stated under DME not covered on the next page.
DME is equipment that:
• Can withstand repeated use
• Is used mainly for a medical purpose rather than for
comfort or convenience
• Generally is not useful in the absence of an illness or injury
• Is related to a medical condition and prescribed by
aphysician
• Is appropriate for use in the home, and
• Is determined to meet medical criteria for coverage to
diagnose or treat an illness or injury, help a malformed
part of the body to work well, help an impaired part of the
body to work within its functional parameters, or keep a
condition from becoming worse.
Coverage is also provided for home medical supplies, such
as ostomy supplies, wound-care supplies, tracheotomy
supplies, and orthotics. Supplies must be prescribed by a
medical doctor (M.D.) or doctor of osteopathy (D.O.) to be
covered. Surgical stockings are limited to 12 stockings per
calendar year.
To be covered, a doctor must include a diagnosis, the
type of equipment needed, and expected time of usage.
Examples of DME include wheelchairs, hospital-type beds,
and walkers. If equipment is rented, the total benefit may
not exceed the purchase price at the time rental begins.
The medical plan
83
Repair of DME is covered when all the following are met:
• The patient owns the equipment
• The required repairs are not caused by the patient’s misuse
or neglect of the equipment
• The expense of repair does not exceed the expense of
purchasing new equipment, and
• The equipment is not covered by warranty.
If patient-owned DME is being repaired, up to one month’s
rental for that piece of DME is covered. Payment is based
on the type of replacement device provided, but will not
exceed the rental allowance for the equipment under repair.
DME not covered: Motor-driven scooters, invasive
implantable bone growth stimulators (except in the case of
spinal surgeries), sitz bath, seat lift, rolling chair, vaporizer,
urinal, ultraviolet cabinet, whirlpool bath equipment, bed
pan, portable paraffin bath, heating pad, heat lamp, steam/
hot/cold packs, devices that measure or record blood
pressure, and other such medical equipment or items
determined to be not medically necessary.
Foot care: For nonsurgical foot care in connection with
treatment for the following conditions, the AMP allows a
total of three provider visits per calendar year:
• Bunions
• Corns or calluses
• Flat, unstable or unbalanced feet
• Metatarsalgia
• Hammertoe
• Hallux valgus/claw toes, or
• Plantar fasciitis.
Services must be prescribed by a medical doctor (M.D.),
doctor of osteopathy (D.O.), or doctor of podiatric
medicine (D.P.M.).
Open-cutting surgical care (including removal of nail roots)
and nonsurgical care due to metabolic and peripheral
vascular disease are not subject to the calendar-year limit.
Orthotic devices for the feet may be covered if prescribed
by a qualified doctor and custom-molded under the doctor’s
supervision, subject to the calendar-year limit described
above. Orthopedic shoes prescribed by a doctor are limited
to two shoes per calendar year.
Gender dysphoria treatment: Medically necessary services
for treatment of gender dysphoria are covered:
• Gender reassignment surgery, including both male to
female surgery and female to male surgery
• Hormone replacement therapy, including laboratory
testing to monitor hormone therapy, and
• Psychotherapy visits.
Gender reassignment surgery is covered only if you are
age 18 or older. Cosmetic treatment of gender dysphoria
isnot covered.
Home nursing care: In-home private-duty professional
nursing services are covered if provided by a state-approved
licensed vocational nurse (L.V.N.), licensed practical nurse
(L.P.N.), or registered nurse (R.N.). Services cannot be
rendered by a relative or by someone in the same household
as the patient. Home nursing care benefits are payable up to
a maximum of 100 visits per calendar year. A visit is defined
as two hours or less.
Hospice care: Hospice care is an integrated program
providing comfort and support services for the terminally
ill. Hospice care is covered if you have an estimated
life expectancy of 12 months or less, as attested by the
physician treating the illness. Hospice care can be provided
on an inpatient or outpatient basis and includes physical,
psychological, social, spiritual, and respite care for the
terminally ill person, and support for immediate family
members, including partners, while the covered person is
receiving hospice care. Benefits are available only when
hospice care is received from a licensed hospice agency,
which can include a hospital.
Inpatient and outpatient hospice care are covered up to
365 days per illness. Participants may continue to receive
treatment and participate in approved clinical trials while
obtaining hospice services. Coverage for additional days
may be available if determined to be medically necessary.
Infertility treatment: Services for the diagnosis and
correction of an underlying condition of infertility are
covered. Refer to What is not covered by the Associates’
Medical Plan later in this chapter for a list of non-covered
infertility services.
International business travel medical coverage: The
company provides international business medical
insurance through an insurance policy from GeoBlue.
Ifyou participate in the Saver Plan you are not eligible to
make HSA contributions for any month in which you are
traveling on company business outside the U.S. and are
covered under the GeoBlue policy, which provides health
benefit coverage for associates traveling internationally
on business. You are encouraged to consult with your tax
advisor if you have questions about the amount to reduce
your contributions based on your individual circumstances.
Nutritional counseling: Nutritional counseling for children
is covered if it is medically necessary for a chronic disease
(e.g., PKU, Crohn’s disease, celiac disease, galactosemia,
etc.) in which dietary adjustment has a therapeutic role
when prescribed by a physician and furnished by a provider
(e.g., a registered dietician, licensed nutritionist, or other
qualified licensed health professional) recognized under the
AMP. Benefits are limited to three visits per condition per
The medical plan
84
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
year. See the Preventive care program section for additional
benefits related to nutritional and obesity counseling for
adults and children.
Off-label use of cancer chemotherapy injectable drugs:
These drugs are covered when medically necessary,
recommended by one of the following three drug
compendia, and not recommended against by one or more
of the same compendia (appropriate to the date of service):
• American Hospital Formulary Service (AHFS) Drug
Information
• Clinical Pharmacology Online, or
• National Comprehensive Cancer Network (consensus)
or category 1 (the recommendation is based on high-
level evidence and there is uniform NCCN consensus) or
category 2A (the recommendation is based on lower-level
evidence and there is uniform NCCN consensus).
If you or your physician are unsure about the Plan’s
coverage for any type of prescription drug, verify coverage
details by calling the third-party administrator of your
medical plan at the number on your plan ID card. You can
also call OptumRx at 844-705-7493.
Off-label use of non-cancer chemotherapy injectable
drugs: These drugs are covered when medically necessary
and recommended under one of the following drug
compendia (appropriate to the date of service):
• American Hospital Formulary Service (AHFS) Drug
Information, or
• Clinical Pharmacology Online.
The Plan does not cover any drug determined by the FDA
to be contra-indicated or not advisable. Coverage for
FDA-approved drugs is subject to the AMP’s applicable
requirements and limitations.
Oral treatment: Charges for care of teeth and gums are
covered when submitted by a doctor or dentist, including
but not limited to:
• Prescriptions
• Emergency room services for mouth pain
• Treatment of fractures/dislocations of the jaw resulting
from an accidental injury
• Accidental injury to natural teeth up to one year from the
date of the accident (does not include injuries resulting
from biting or chewing; those may be covered under the
dental plan)
• Dental procedures necessitated by either severe disease
(including but not limited to cancer) or traumatic event,
as long as the dental service is medically necessary and
the service is incidental to and an integral part of service
covered under AMP medical benefits. Examples of services
include, but are not limited to, the extraction of teeth
prior to or following chemotherapy or radiation therapy
of the head and neck. Treatment of oral tissues related to
chemotherapy must be supported by documentation of a
direct link between the destroyed bone or gums and the
chemotherapy.
• Non-dental cutting procedures in the oral cavity
• Medical complications that are the result of a dental
procedure, or
• Expenses for dental services performed in a hospital setting,
including facility and professional charges, for extensive
procedures that prevent an oral surgeon from providing
general anesthesia in an office setting, or for circumstances
that limit the ability of the oral surgeon to provide services
in an office setting. Such circumstances include, but are not
limited to, situations in which the covered person is:
– A child under age 4
– Between the age of 4 and 12, when either:
• Care in a dental office has been attempted
unsuccessfully and usual methods of behavior
modification have not been successful; or
• Extensive amounts of care are required, exceeding
fourappointments.
– An individual with one of the following medical
conditions, requiring hospitalization or general
anesthesia for dental treatment:
• Respiratory illness
• Cardiac conditions
• Bleeding disorders
• Severe disability (including but not limited to cerebral
palsy, autism, developmental disability)
• Other severe disease (including but not limited to
cancer or neurological disorder), or
• Compromised airway.
– An individual of any age whose condition requires
extensive procedures that prevent an oral surgeon from
providing general anesthesia in the office setting.
Outpatient physical/occupational therapy: Charges for
outpatient physical/occupational therapy are covered when
services are:
• Prescribed by a medical doctor (M.D.), doctor of
osteopathy (D.O.), or doctor of podiatric medicine
(D.P. M .), and
• Provided by a licensed physical therapy provider or
licensed occupational therapy provider or by one of the
types of doctors listed above.
This benefit is payable to a maximum of 20 visits for
physical therapy and 20 visits for occupational therapy per
calendar year. Additional visits may be covered if deemed
appropriate by the care manager.
Pregnancy benefits: Pregnancy expenses are covered the
same as any other medical condition. (Eligible prenatal
services are covered under the preventive care program.)

The medical plan
85
Benefits are paid for pregnancy-related expenses of
dependent children. The newborn is covered only if the
newborn is a covered dependent of the covered associate.
See How to change your elections due to a status change
event in the Eligibility and enrollment chapter for
information on enrolling a newborn for coverage.
Prostate-specific antigen (PSA) tests: Covered only when
conducted as part of a clinical diagnosis.
Prosthetics: Prosthetic devices (such as artificial limbs)
are covered if medically necessary and prescribed by
a physician, subject to the terms of the third-party
administrators. Replacement prostheses are allowed only
with a change of prescription. A licensed prosthetician must
perform replacements of artificial limbs.
Rehabilitative care: Inpatient and/or day rehabilitation is
covered to a maximum of 120 days per condition for the
following clinical groups if clinical criteria are met:
• Stroke
• Spinal cord injury
• Brain injury
• Congenital deformity
• Neurological disorders
• Amputation
• Severe or advanced osteoarthritis involving two or more
weight-bearing joints
• Rheumatoid, other arthritis
• Systemic vasculitis with joint inflammation
• Major multiple trauma, or
• Burns.
Specialty care: Medical care commonly provided at the
following types of facilities is covered if you are admitted
to this level of care subsequent to an eligible acute care
hospital confinement:
• Extended care facility
• Long-term acute care specialty facility
• Subacute care facility
• Skilled nursing facility, or
• Transitional care facility.
Benefits are limited to a maximum of 60 calendar days per
disability period. Successive periods of confinement due
to the same or related causes are considered one disability
period unless separated by a complete recovery.
Speech therapy: Therapy of up to 60 visits per calendar year
is covered when:
• Prescribed by a medical doctor (M.D.) or doctor of
osteopathy (D.O.), and
• Provided by a licensed speech therapist.
Initial and ongoing plans of treatment and progress reports
may be requested from the prescribing doctor. To be
covered, speech therapy must be for a residual speech
impairment resulting from:
• A cerebral vascular accident
• Head or neck injury
• Partial or complete paralysis of voice cords or larynx
• Head or neck surgery, or
• Congenital and severe developmental speech disorders.
Video visits: Video visits are covered for participants
enrolled in the AMP only when provided through the
Doctor On Demand service. See Telehealth video visits
earlier in this chapter for information.
See page 330
Vision services: Diagnosis and treatment of injury or
disease of the eye, including but not limited to diabetic
retinopathy, glaucoma, and macular degeneration, are
covered. Charges for routine eye care, including but not
limited to vision analysis, eye examinations, or eye surgeries
for nearsightedness or correction of vision, are not covered,
except for vision screening for children covered under
preventive care guidelines.
Weight loss treatment: Weight loss surgery is covered only
under the Centers of Excellence program when you meet
specific eligibility guidelines and clinical criteria. Weight
loss treatments, including but not limited to medications,
diet supplements, and surgeries outside the scope of the
Centers of Excellence program, are not covered. See
the Centers of Excellence section of this chapter for
information about weight loss surgery.
What is not covered by the AMP
In addition to the exclusions and limitations listed in the
When limited benefits apply to the AMP section of this
chapter, the following list represents services not covered by
the AMP. Network discounts do not apply to these services.
If you are enrolled in the Saver Plan, you may be able to
use your HSA funds for these and other qualified medical
expenses. For information, contact your HSA administrator.
If you have a question regarding whether a service is
covered under the Plan, call the third-party administrator
at the number on your plan ID card or see the inside back
cover of this book for contact information.
Acupuncture
Administrative services and interest fees: Charges for the
completion of claim forms, missed appointments, additional
charges for weekend or holiday appointments, interest fees,
collection fees, or attorney fees.
Alternative/nontraditional treatment (including
homeopathy, naturopathy, hypnosis, and massage therapy).
The medical plan
86
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Autopsy
Beyond the scope of licensure or unlicensed: Services
rendered by a non-credited or a non-licensed physician,
health care worker or institution, or services rendered
beyond the scope of such person or entity’s license.
Biofeedback
Breast reconstruction/reduction: Any expenses or charges
resulting from breast enlargement (augmentation),
including implant insertion and implant removal, whether
male or female, are not covered except when the implant
is removed as the result of implant damage or rupture.
Replacement of a damaged or ruptured implant is not
covered unless the original implant was placed for
conditions eligible to be paid by the Plan.
Any expenses or charges resulting from breast reductions,
implantations, or total breast removal, whether male
or female, are not covered, unless directly related to
treatment of a mastectomy, as provided by law (see
Women’s Health and Cancer Rights Act of 1998 later in this
chapter), or unless an AMP medical review determines the
procedure is medically necessary.
Chiropractic care: Spinal manipulation, joint manipulation,
or soft-tissue manipulation, regardless of the type of
provider performing the service, except that participants
enrolled in the Mercy Local Plans for Arkansas, Oklahoma,
Southwest Missouri, and St. Louis have limited coverage
when services are performed by a network provider.
Copays and/or discounts, deductibles and/or coinsurance
Cosmetic health services or reconstructive surgery: Except
for congenital abnormality, services covered by law (see
Women’s Health and Cancer Rights Act of 1998 later in this
chapter), or conditions resulting from accidental injuries,
tumors, or diseases.
Custodial or respite care: Care or services provided in
a facility or home to maintain a person’s present state
of health, which cannot reasonably be expected to
significantly improve.
Drugs, items, and equipment not FDA-approved
Educational services: Including any services for learning
and educational disorders (which include but are not
limited to reading disorders, alexia, developmental
dyslexia, dyscalculia, spelling disorders, and other learning
difficulties).
Elective inpatient and outpatient stays or services outside
the U.S.
Expenses related to missed appointments, review or
storage of your health care information or data
Experimental, investigational, and/or treatments and
services that are not medically necessary: Experimental
and/or investigational medical services are those defined as
experimental and/or investigational according to protocols
established by your third-party administrator. For Centers
of Excellence services, the Centers of Excellence third-
party administrator makes this determination.
Extracorporeal shock wave therapy: For plantar fasciitis and
other musculoskeletal conditions.
Government compensation: Charges that are compensated
for or furnished by local, state, or federal government, or
any agency thereof, unless payment is legally required.
Health and behavior assessment/intervention: Evaluation
of psychosocial factors potentially affecting physical
health problems and treatments, except for behavioral
assessments outlined under the preventive care program.
Hearing devices: Charges for routine hearing tests and
hearing aids, except for hearing screening for children,
covered under preventive care guidelines.
HMO copays
Illegal occupation, assault, felony, riot, or insurrection:
Charges for medical services, supplies, or treatments
that result from or occur while being engaged in an illegal
occupation, commission of an assault, felony, or criminal
offense (except for a moving violation), or participation in a
riot or insurrection.
Infertility services: Treatment by artificial means for the
purpose of creating a pregnancy. Assistive reproductive
technology (ART) and other non-covered services include
but are not limited to:
• Infertility prescription drugs
• Charges to reverse a sterilization procedure
• Charges for, or related to, the services of a surrogate
mother, egg donor, or sperm donor, and
• In-vitro fertilization, GIFT, ZIFT, IVC, gamete intra-
cryopreservation, frozen embryo transfer, and artificial
insemination, including all related charges.
Judgments/settlements
Late claims: Charges received more than 18 months past the
date of service. See Filing a medical claim later in this chapter
for information about coordination of benefits. In the event a
participant establishes that a claim was filed within the stated
time period, but the claim was mistakenly filed with the
company or any third-party administrator of the Plan, that
time shall not count toward the filing period above.
Marital, family, or relationship counseling: Or counseling
to assist in achieving more effective intra- or interpersonal
development.
Military-related injury or illness: Including injury or illness
related to, or resulting from, acts of war, declared or
undeclared.
The medical plan
87
Neurofeedback
Nonaccredited/nonlicensed providers or institutions
Non-covered services:
• Services not specifically included as a benefit in this
Summary Plan Description
• Services provided after exceeding the benefit maximum
for specified services
• Services for which you are responsible for payment, such
as non-covered out-of-network charges
• Charges for services above the contracted rates to
providers, or
• Charges for medical records.
Out-of-pocket expenses
Over-the-counter medications and equipment: Except for
specific preventive care medications. See The pharmacy
benefit chapter for more information.
Personal care items: Primarily for personal comfort or
convenience, including but not limited to diapers, bathtub
grabbers, handrails, lift chairs, over-bed tables, bedboards,
incontinence pads, ramps, snug seats, recreational items,
home improvements and home appliances, spas, wigs, and
knee braces for sports.
Services provided by a member of the patient’s family
Services provided by a government entity while incarcerated
Sexual dysfunction services and pharmaceuticals: Including
therapy, treatment, or pharmaceuticals for the treatment of
sexual dysfunction, except for sexual dysfunction resulting
from an accidental injury or treatment for an illness or
condition (e.g., erectile dysfunction resulting from a
prostatectomy or spinal cord injury).
Sports/school physicals: Charges for physical examinations
performed for the purpose of clearing an individual for
participation in a sport or school activity.
Surrogate parenting: Whether paying for another’s services
or serving as a surrogate.
Talking aids: Assistive talking devices, including special
computers or devices designed to assist in therapy
treatment to enhance motor and/or psychological abilities.
Termination of pregnancy: Charges for procedures,
services, drugs, and supplies related to abortions or
termination of pregnancy are not covered, except when the
health of the mother would be in danger if the fetus were
carried to term, the fetus could not survive the birthing
process, or death would be imminent after birth.
Travel and lodging, except as specified under Centers of
Excellence benefits
Vitamins: Charges for nonprescription vitamins (whether
oral or injectable), minerals, nutritional supplements, or
dietary supplements, except as outlined in the Preventive
care program section of this chapter.
Walmart Care Clinic/Walmart Health: Charges for
nonpreventive services, except where the Walmart Care Clinic
or Walmart Health is considered a network provider or for lab
services provided outside the clinic by an external vendor.
Work hardening or similar vocational programs
Workers’ compensation: Treatment of any compensable
injury, as defined by applicable workers’ compensation law,
regardless of whether or not you file a timely claim for
workers’ compensation benefits.
Filing a medical claim
If you use a network provider, the provider will generally file
the claim for you. If you see a non-network provider, you
may need to file a claim. If you need to file a claim, it should
include the following information:
• Patient’s name
• Provider’s name, address, and tax identification number
• Associate’s insurance ID (see your plan ID card)
• Date of service
• Amount of charges
• Medical procedure codes (these should be found on the
bill), and
• Diagnosis.
Claim forms are located on One.Walmart.com. You must file
within 18 months from date of service or your claim will be
denied. Claims are determined under the time frames and
requirements outlined in the Claims and appeals chapter.
See your plan ID card for the correct address to mail your
claim. Failure to mail your claim to the correct address may
result in the denial of your claim.
When you incur medical expenses and file a claim, or a
claim is filed on your behalf, benefits are paid directly to
the provider for network services. Payment to the provider
discharges the AMP’s obligation to you for the benefit.
If your plan provides coverage for non-network providers
and you use a non-network provider, payment may be made
directly to you upon your showing proof of payment in full
to the provider. You are responsible for your 50% share
of the maximum allowable charge, plus any amount above
the maximum allowable charge. As a convenience to you,
payment may also be made to a non-network provider
if you expressly authorize such payment. Your provider,
whether network or non-network, may not pursue appeals
on your behalf unless you designate your provider as your

The medical plan
88
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
authorized representative, as described in the Claims and
appeals chapter. The AMP prohibits the assignment of any
benefit or any legal claim or cause of action (whether known
or unknown). Note that any direct payment to a provider is
undertaken by the AMP solely for your convenience.
You have the right to appeal a claim denial, as described in
the Claims and appeals chapter.
If you have coverage under more
than one medical plan
The AMP has the right to coordinate with other plans under
which you are covered so the total medical benefits payable
do not exceed the level of benefits otherwise payable under
the AMP. “Other plans” refers to the following types of
medical and health care coverage:
• Coverage under a governmental program provided or
required by statute, including no-fault coverage to the
extent required in policies or contracts by a motor vehicle
insurance statute or similar legislation
• Group insurance or other coverage for a group of individuals,
including coverage under another employer plan or student
coverage obtained through an educational institution
• Any coverage under labor-management trusteed plans,
union welfare plans, employer organization plans, or
employee benefit organization plans
• Any coverage under governmental plans, such as
Medicare or TRICARE, but not including a state plan
under Medicaid or any governmental plan when, by law, its
benefits are secondary to those of any private insurance,
nongovernmental program, and
• Any private or association policy or plan of medical
expense reimbursement that is group or individual rated.
When you are covered by more than one plan, one of the
plans is designated the primary plan. The primary plan
pays first and ignores benefits payable under other plans
when determining benefits. Any other plan is designated
as a secondary plan that pays benefits after the primary
plan. A secondary plan reduces its benefits by the amount
of benefits payable under “other plans” and may limit the
benefits it pays.
You must follow the primary insurance terms in order for
the AMP to pay as secondary payer.
These rules apply whether or not a claim is made under the
other plan. If a claim is not made, benefits under the AMP
will be delayed or denied until an explanation of benefits is
received showing a claim made with the primary plan.
The AMP does not coordinate as a secondary payer for any
copays you pay with respect to another plan or with respect
to prescription drug claims or transplants (except where the
other plan is Medicare).
If you reside in a state where automobile no-fault coverage,
personal injury protection coverage, or medical payment
coverage is mandatory, that coverage is primary and the
AMP is secondary. The AMP reduces benefits for an amount
equal to the state’s mandatory minimum requirement.
• The Plan has first priority with respect to its right to
reduction, reimbursement, and subrogation.
• The Plan does not coordinate benefits with an HMO or
similar managed care plan where you pay only a copayment
or fixed dollar amount.
• The Plan does not coordinate with any other plan other
than Medicare with respect to a covered transplant.
HOW THE AMP COORDINATES WITH OTHER PLANS
Example 1 Example 2 Example 3
If another plan
pays primary at:
80% 80% 0%
And the AMP’s
payment is:
75% 100% 75%
The AMP’s total
benefit is:
0% 20% 75%
DETERMINING WHICH PLAN IS PRIMARY
A plan without a coordinating provision is always primary.
The AMP has a coordinating provision. If all plans have a
coordinating provision, the following provisions apply:
• The AMP always is the secondary payer to any motor
vehicle policy available to you, including personal
injury protection or no-fault coverage. If the AMP pays
benefits as a result of injuries or illnesses you sustain and
another party (e.g., an insurance company) bears primary
responsibility for your covered medical expenses, the AMP
has a legal right to reimbursement of benefits. See the
Claims and appeals chapter for more information.
• The plan covering the participant for whom the claim is
made, other than as a dependent, pays first and the other
plan pays second.
• If the plan participant is covered under a retiree medical
plan that includes a coordination of benefits provision, that
provision governs.
• For dependent children’s claims, the plan of the parent
whose birthday occurs earlier in the calendar year is primary.
• When the birthdays of both parents are on the same day,
the plan that has covered the dependent for the longer
period of time is primary.
• When the parents of a dependent child are divorced
or separated, or the domestic partnership or legal
relationship is terminated, and the parent with custody has
not remarried, that parent’s plan is primary.
The medical plan
89
• When the parent with custody has remarried, or entered
into a domestic partnership with another individual, that
parent’s plan is primary, the stepparent’s plan pays second
and the plan of the parent without custody pays last.
• When there is a court decree that establishes financial
responsibility for the health care expenses of the
child, the plan that covers the parent with financial
responsibility is primary.
• If these rules do not establish an order of benefit
determination, the plan that has covered the participant
for whom the claim is made for the longest period of
time is primary.
• If you are covered under a right of continuation coverage
pursuant to federal or state law (for example, COBRA)
and you are also covered under another plan that covers
you as an employee, member subscriber, or retiree (or as
that person’s dependent), the latter plan is primary and the
continuation coverage is secondary. If the other plan does
not have this rule, and the plans do not agree on the order
of benefits, this rule does not apply.
IF YOU OR A DEPENDENT IS COVERED
UNDER MEDICAID
If you or your dependent is a participant in the AMP and also
covered under Medicaid, the AMP pays before Medicaid.
The AMP does not take the Medicaid coverage into account
for purposes of enrollment or payment of benefits.
If, while you are covered under Medicaid, benefits are
required to be paid by the Plan, but are first paid by the
state plan, payment by the Plan will be made as required by
any applicable state law which provides that payment will be
made to the state.
IF YOU OR A DEPENDENT IS ELIGIBLE FOR
OR ENROLLED IN MEDICARE
If you are enrolled in Medicare Part D, you are not eligible
to enroll in the AMP. If your dependent is enrolled in
Medicare Part D and you are not, you are eligible to enroll
in a Walmart medical plan, but your dependent would not be
eligible for such coverage.
In general, the Social Security Act requires that AMP be
the primary payer if you or your dependent is eligible for or
enrolled in Medicare Part A, or Parts A and B, and meet one
of the following criteria:
• You are employed by the company and are age 65 or older
• You are employed by the company and your spouse/
partner is age 65 or older
• You are an active participant or COBRA participant
entitled to Medicare on the basis of end-stage renal
disease, but only for the first 30-month period of eligibility
for Medicare coverage (whether or not actually enrolled in
Medicare throughout this period)
• You are under age 65 and are entitled to Medicare due to
disability and are covered under the AMP due to being
employed by the company, or
• Your dependent is under age 65 and is entitled to Medicare
due to his or her disability and is covered under the AMP
due to your being employed by the company.
The AMP is secondary if you or your dependent is enrolled
in Medicare and meets one of the following criteria:
• You or your dependent is a COBRA participant, except
in the case of Medicare enrollment due to end-stage
renal disease, for which the AMP is primary for the first
30-month period of eligibility for Medicare coverage, or
• You or your dependent is an active participant or COBRA
participant enrolled in Medicare due to end-stage renal
disease, after the 30-month coordination period with
Medicare is exhausted.
IF YOU ARE AGE 65 OR OLDER AND AN ACTIVE
ASSOCIATE
If you are still working for the company, you may continue
your coverage under the AMP. If you also have Medicare,
the AMP is generally primary and Medicare is secondary.
File your claim with the AMP first.
You may also elect to end your coverage under the AMP and
choose Medicare as your primary coverage. If you choose
Medicare as your primary coverage, you may not elect the
AMP as your secondary plan.
LEGALLY MANDATED AUTOMOBILE PERSONAL
INJURY OR MEDICAL PAYMENT COVERAGE
If you reside in a state where automobile no-fault coverage,
personal injury protection coverage, or medical payment
coverage is mandatory, that coverage is primary and the
AMP takes secondary status. The AMP reduces benefits for
an amount equal to, but not less than, the state’s mandatory
minimum requirement.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your medical premiums to avoid a
break in coverage. These situations occur most commonly
if you are on a leave of absence or if your paycheck is not
sufficient to pay your full share of the cost of coverage
(such as after a reduction in hours). Depending on your
circumstances, failure to make your premium payments by
the due date may result in an interruption in the payment of
any benefit claims and/or a break in coverage.
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
The medical plan
90
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information about
making payments while on a leave of absence, see When
special arrangements are necessary to maintain coverage in
the Eligibility and enrollment chapter.
When coverage ends
Your coverage ends on your last day of employment,
or when you are no longer eligible under AMP terms.
Dependent coverage ends when your coverage ends or
when a dependent is no longer an eligible dependent (as
defined in the Eligibility and enrollment chapter). You
and/or your enrolled dependents may be eligible for
continued coverage through the Consolidated Omnibus
Reconciliation Act of 1985, as amended (COBRA). See the
COBRA chapter for details.
If you leave the company and
arerehired
If you terminate employment and return to work for
the company within 13 weeks, you will automatically be
reenrolled in your previous coverage (or the most similar
coverage offered under the AMP). If you return within 30
days, your annual deductible, out-of-pocket maximum and
HRA (if applicable) will not reset. If you return after 30 days
but within 13 weeks, your annual deductible, out-of-pocket
maximum and HRA (if applicable) will reset and you will be
responsible for meeting the new deductible and out-of-
pocket maximum in their entirety. You will have 60 days
after resuming employment to drop or otherwise change
the coverage in which you were automatically reenrolled.
If you return reenroll after 13 weeks, you will be treated
as a new associate and may enroll for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.
If you drop coverage and reenroll
If you drop coverage and reenroll within 30 days, you will
automatically be reenrolled in your previous coverage (or
the most similar plans offered under the AMP). The annual
deductible and waiting periods will not reset.
If you drop coverage and reenroll after 30 days, you will
be treated as a new associate and may enroll for coverage
under the time periods and conditions described in the
Eligibility and enrollment chapter.
IF A DEPENDENT IS DROPPED FROM
COVERAGE AND REENROLLED
If your dependent child is dropped from coverage and then
determined to be eligible for coverage within 30 days, the
dependent will automatically be reenrolled in the same
coverage you elect for yourself. The annual deductible and
waiting periods will not reset.
If your dependent regains eligibility and is reenrolled after
30 days, they will be treated as a newly eligible dependent.
The associate may enroll them for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.
Other information about the
medicalplan
THE WOMEN’S HEALTH AND CANCER RIGHTS
ACT OF 1998
The Women’s Health and Cancer Rights Act of 1998
requires that all group medical plans that provide medical
and surgical benefits with respect to mastectomy must
provide coverage for:
• All stages of reconstruction of the breast on which the
mastectomy has been performed
• Surgery and reconstruction of the other breast to produce
a symmetrical appearance, and
• Prostheses and physical complications of mastectomy,
including lymphedemas, in a manner determined in
consultation with the attending physician and the patient.
Such coverage will be subject to the otherwise applicable
annual deductibles and coinsurance/copayment provisions
under the Plan. Written notice of the availability of
such coverage shall be delivered to the participant
upon enrollment and annually thereafter. For additional
information, call People Services at 800-421-1362.
A NOTE ABOUT MATERNITY ADMISSIONS
Group health plans and health insurance issuers generally
may not, under federal law, restrict benefits for any hospital
length of stay in connection with childbirth for the mother
or newborn child to less than 48 hours following a vaginal
delivery or less than 96 hours following a cesarean section.
However, federal law does not prohibit the mother’s or
newborn’s attending provider, after consulting with the
mother, from discharging the mother or her newborn earlier
than 48 hours (or 96 hours, as applicable). In any case,
plans and issuers may not, under federal law, require that a
provider obtain authorization from the plan or the insurance
issuer for prescribing a length of stay not in excess of
48hours (or 96 hours, as applicable).
The medical plan
91

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The pharmacy benefit
The pharmacy benefit 94
How the pharmacy benefitworks 94
What is not covered by thepharmacybenefit 96
Pharmacy discounts for prescriptions not covered 97
Filing a pharmacy benefit claim 97
Privacy and security 97

The pharmacy benefit
93
The pharmacy benefit
Keep you and your eligible dependents in good health with your pharmacy benefit. It’s automatically
included with your medical plan.
RESOURCES
Find What You Need Online Other Resources
Find a Walmar or Sam’s Club pharmacy Go to One.Walmar.com or
OptumRx.com/Walmar
Find an OptumRx network pharmacy Go to OptumRx.com Call OptumRx at 844-705-7493
Get the list of covered brand-name drugs Go to One.Walmar.com or
OptumRx.com/Walmar
What you need to know about the pharmacy benefit
• You are covered under the pharmacy benefit if you are enrolled in any of the medical plan options available under the
Associates’ Medical Plan (AMP). If you are enrolled in an HMO plan or the eComm PPO Plan, your pharmacy benefits are
provided through your medical plan.
• Any reference to a “network pharmacy” refers to a Walmart or Sam’s Club pharmacy or OptumRx pharmacy, including
Walmart and OptumRx mail-order pharmacies.
• If your work location is five miles or less from a Walmart or Sam’s Club pharmacy, you must use a Walmart or Sam’s Club
pharmacy for pharmacy benefits to be paid. Benefits are generally not payable if you use another network pharmacy
(including an OptumRx network pharmacy).
• If your work location is more than five miles from a Walmart or Sam’s Club pharmacy and you have medical coverage
under the Premier Plan, Contribution Plan, or Saver Plan, you have the option to fill prescriptions at an OptumRx network
pharmacy, in addition to a Walmart or Sam’s Club pharmacy.
• If you have medical coverage under a local plan option, you must use a Walmart or Sam’s Club pharmacy (including
throughmail order) for benefits to be payable, regardless of the distance to a Walmart or Sam’s Club pharmacy from
yourwork location.
• If you have a chronic condition such as diabetes, asthma, or arthritis and require the same or similar prescriptions on a regular
basis, you may want to consider the mail-order option.
• Specialty drugs may be purchased from Walmart Specialty Pharmacy. Optum Specialty Pharmacy is also an option.
The pharmacy benefit
94
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The pharmacy benefit
The pharmacy benefits covers eligible prescriptions from
both retail and mail-order network pharmacies. You are
eligible for prescription coverage on the date your medical
coverage is effective.
To obtain eligible pharmacy benefits, simply present your
plan ID card at a Walmart or Sam’s Club pharmacy. If you are
covered under the Premier Plan, Contribution Plan, or Saver
Plan and your work location is more than five miles from a
Walmart or Sam’s Club pharmacy, you may also purchase
drugs at any OptumRx network pharmacy. When using
mail order, you can use Walmart or Sam’s Club mail-order
pharmacy regardless of your work location or medical plan.
A form is available on One.Walmart.com. OptumRx home
delivery pharmacy is also an option.
Under certain limited circumstances you can fill prescriptions
at an OptumRx network pharmacy even if your work location
is within five miles of a Walmart or Sam’s Club Pharmacy.
No pharmacy benefits are paid if you use a non-network
pharmacy, except as provided in this chapter.
Visit One.Walmart.com to find information about:
• Walmart or Sam’s Club pharmacies
• Pharmacies in the OptumRx network
• Mail-order network pharmacies
• Covered generic, brand-name, and specialty drugs, and
• Preventive medications.
You can also call OptumRx at 844-705-7493.
WHEN PRESCRIPTIONS CAN BE FILLED AT ANY
NETWORKPHARMACY
If you have medical coverage under the Premier Plan,
Contribution Plan, or Saver Plan and your work location
is more than five miles from a Walmart or Sam’s Club
pharmacy, you may use any network pharmacy to fill
your prescriptions. (If you have medical coverage under a
local plan option, you must use a Walmart or Sam’s Club
pharmacy, regardless of the distance to a Walmart or Sam’s
Club pharmacy from your work location.)
You may also have prescriptions filled at any OptumRx
network pharmacy in certain limited circumstances,
including:
• If a covered drug is out of stock and not available at a
Walmart or Sam’s Club pharmacy for an extended time (as
defined by the AMP)
• If a covered drug is unavailable at a Walmart or Sam’s Club
pharmacy
• If an emergency prescription fill is needed outside Walmart
or Sam’s Club pharmacy hours
NOTE: Certain restrictions apply to filling prescriptions for
narcotics and other controlled substances.
For information on other exceptions and steps you must
take, call OptumRx at 844-705-7493.
How the pharmacy benefitworks
The pharmacy benefit covers only prescription drugs
specifically listed on the pharmacy benefit’s formulary,
which is a list of generic and brand-name medications
maintained by OptumRx. You can view an abbreviated
list on One.Walmart.com or you can call OptumRx at
844-705-7493 for a full list. If you don’t see your drug on
the list, call OptumRx to see if it is on the formulary.
The pharmacy benefit provides discounted prices on
generic and brand-name drugs that are covered on the
formulary and filled at an eligible network pharmacy. If, at
the time your prescription is filled, the discounted price
available is lower than your copay, you will be charged the
lower amount, which may include a dispensing fee.
Premier Plan, Contribution Plan, and local plan participants:
You pay the required copay or coinsurance out of your own
pocket when you purchase your prescription drugs. See
the Pharmacy benefits chart on the next page for details
about copays and coinsurance. (If you are covered under the
Contribution Plan, HRA funds cannot be used to purchase
prescriptions.) Your copays are applied toward your medical
plan’s annual out-of-pocket maximum. Once you meet your
annual out-of-pocket maximum, eligible prescriptions are
paid at 100% for the rest of the calendar year.
Saver Plan participants: You pay the full price for your
prescription drugs until you meet the Saver Plan’s network
annual deductible. Once you meet your network annual
deductible, you pay the required copay or coinsurance
listed in the Pharmacy benefits chart. (The exceptions are
medications on the OptumRx list of approved preventive
medications, which are not subject to the Saver Plan’s
network annual deductible. See Preventive medications
not subject to the Saver Plan’s network annual deductible
later in this chapter for details.) Your copays are applied
toward the Saver Plan’s annual out-of-pocket maximum.
Once you meet your annual out-of-pocket maximum,
eligible prescriptions are paid at 100% for the rest of the
calendar year.
Refer to the Pharmacy benefits chart on the next page for
details about copays and coinsurance.

The pharmacy benefit
95
PHARMACY BENEFITS
See page 330 for updated terms replacing the char below.
Generic drugs
Up to 30-day supply
31- to 60-day supply
61- to 90-day supply
$4 copay
$8 copay
$12 copay
Filling your prescriptions
• Present your plan ID card at a Walmar or Sam’s Club
pharmacy.
• If you are covered under the Premier Plan, Contribution
Plan, or Saver Plan and your work location is more than 5
miles from a Walmar or Sam’s Club pharmacy, you may also
purchase drugs at an OptumRx network retail pharmacy.
(Note, however, that supplies of generic drugs for greater
than 30 days may be purchased only at a Walmar or Sam’s
Club pharmacy.)
• Prescription refills are available after 75% of your previous
prescription has been used.
• See When prescriptions can be filled at an OptumRx network
pharmacy on the previous page for additional information.
Brand-name drugs
Up to a 30-day supply
Greater of $50 or
25% of allowed cost
Specialty drugs
Available only at Walmar
Specialty Pharmacy or Optum
Specialty Pharmacy
Greater of $50 or
20% of allowed cost
Under the Saver Plan: The charges listed above apply after the Saver Plan’s network annual deductible has been met, with
the exception of medications that are on the OptumRx list of approved preventive medications, which are not subject to the
deductible. See Preventive medications not subject to the Saver Plan’s network annual deductible later in this chapter for details.
When purchasing mail-order drugs:
• You may purchase mail-order prescriptions through a Walmar/Sam’s Club mail-order pharmacy, regardless of yourwork
location or medical plan. OptumRx home delivery pharmacy is also an option.
• Your cost for a 90-day supply is three times the cost of a 30-day supply purchased at a Walmar or Sam’s Club pharmacy, as
listed above.
• For brand-name drugs, supplies of more than 30 days must be purchased through mail order.
Specialty drug: Specialty drugs are used to treat complex
conditions such as cancer, growth hormone deficiency,
hemophilia, hepatitis C, immune deficiency, multiple
sclerosis, and rheumatoid arthritis. Specialty drugs require
an enhanced level of service, whether administered by
a health care professional, self-injected, or taken orally.
(Medications used to treat diabetes are not considered
specialty medications.)
CONTRACEPTIVES FOR WOMEN
The AMP covers all FDA-approved contraceptive methods,
including over-the-counter (OTC) variations for women, as
required by the Affordable Care Act. The AMP covers
certain FDA-approved generic contraceptives (and
brand-name contraceptives when medically necessary) at
100%, with no deductible, for women who are capable of
bearing a child, when the drug is prescribed by a physician. If
your attending physician believes a brand-name
contraceptive is medically necessary, you may file a claim
for coverage of the brand-name drug. See Filing a
pharmacy benefit claim at the end of this chapter.
See page 330 for updates to the prescription drug benefit.
TYPES OF DRUGS
To be covered, prescription drugs must be on the
pharmacybenefit’s formulary, which is a list of generic
andbrand-name medications that have been tested
for quality and effectiveness and are believed to be
a necessary part of a quality treatment program. The
formulary is reviewed quarterly and can change.
The pharmacy benefit has a closed formulary. This means
that your prescription drugs, whether they fall under
thegeneric, brand-name or specialty drug category,
mustbe included on the formulary for pharmacy benefits
to bepaid.
Generic drug: A generic drug is a lower-cost equivalent of
a brand-name drug. When a generic equivalent becomes
available, the brand-name drug will no longer be covered.
Generic equivalents work like the brand-name drug in
dosage, strength, performance, and use, and must meet the
same quality and safety standards. All generic drugs must be
reviewed by the United States Food and Drug Administration
(FDA). For more information, visit One.Walmart.com.
Brand-name drug: A covered brand-name drug is a drug
manufactured by a single manufacturer that has been
evaluated for safety and effectiveness when compared to
similar drugs treating the same condition and identified for
inclusion on the covered brand-name drug list.

The pharmacy benefit
96
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
PREVENTIVE MEDICATIONS NOT
SUBJECTTOTHE SAVER PLAN’S
NETWORKANNUAL DEDUCTIBLE
For Saver Plan participants, certain preventive medications
are covered under the Saver Plan before you meet the
Plan’s network annual deductible. Prescription drugs that
can keep you from developing a health condition are called
“preventive medications.” If you are taking prescribed
drugs for certain health issues, such as high blood pressure,
high cholesterol, etc., you may be eligible to get these
medications at no cost before you meet your Saver Plan’s
network annual deductible.
PREVENTIVE OVERTHECOUNTER
MEDICATIONS
The AMP covers certain generic over-the-counter
(OTC) preventive care medications at 100% when they
are prescribed by a physician and purchased at network
pharmacies. You will need to present your plan ID card
and a prescription from your physician at the time of
purchase. Covered OTC preventive care medications
are those required under the Affordable Care Act. If
your physician believes a brand-name preventive OTC
medication is medically necessary rather than a generic,
the physician canfile an appeal with OptumRx for coverage
of the brand-name drug, or you can file a claim for the
brand-name drug under the procedures listed in the Filing
a pharmacy benefit claim section of this chapter.
Some common preventive OTC medications identified by
the United States Preventive Services Task Force (USPSTF)
are listed in the Preventive over-the-counter medications
chart below. For a current list of covered preventive care
OTC medications, go to One.Walmart.com or call OptumRx
at 844-705-7493.
PREVENTIVE OVERTHECOUNTER MEDICATIONS
Recommended by the U.S. Preventive Services Task Force
(USPSTF)
Oral fluoride By prescription when appropriate for
children 6 months to 6 years of age
Folic acid By prescription for all women planning or
capable of pregnancy
Generic aspirin By prescription for adults age 45 to
59 who have 10% or greater 10-year
cardiovascular disease risk, are not at
increased risk for bleeding, have life
expectancy of at least 10 years and are
willing to take low-dose aspirin for at least
10 years; low-dose aspirin (81mg/d) by
prescription after 12 weeks of gestation
in pregnant women at high risk for
preeclampsia
PREVENTIVE OVERTHECOUNTER MEDICATIONS
Recommended by the U.S. Preventive Services Task Force
(USPSTF)
Bowel prep
agents
By prescription when appropriate for a
screening colonoscopy for adults over
age 50
MEDICATIONS THAT REQUIRE
PRIORAUTHORIZATION
Prior authorization is required before some medications
canbe covered by the AMP. OptumRx may ask your
physician to provide additional information. This is called
a“coverage authorization.”
After OptumRx receives the required information, it will
notify you and your physician (usually within two business
days) to confirm whether coverage is authorized. If it is
determined that the prescription is not a covered benefit
under the AMP, it will not be paid. You may appeal this
decision, as described in the Claims and appeals chapter.
If you choose to fill the prescription without prior
authorization, you must pay the full retail cost, even if
the prescription would have been authorized if you had
waited. The amount paid will not be applied toward your
out-of-pocket maximum.
For questions about prior authorizations, call OptumRx at
844-705-7493.
MEDICATIONS WITH QUANTITY LIMITS
Certain medications have limits on the quantity you
can receive per prescription, based on FDA dosage
guidelines.Alist of these medications can be found
on One.Walmart.com.
Prescriptions for quantities greater than the FDA-approved
quantity are not covered under the AMP. If you choose to
fill the prescription, you must pay the full retail cost.
What is not covered by
thepharmacybenefit
Medications not covered by the pharmacy benefit include
but are not limited to:
• Compound medication, which consists of two or more
ingredients that are measured, prepared, or mixed
according to a prescription order. Select compounded
ingredients will not be covered. These may include
ingredients that are not approved by the FDA or are
available over-the-counter.
The pharmacy benefit
97
• Over-the-counter drugs (with the exception of insulin,
when a state does not require a prescription for it, and
those covered as part of the preventive care benefit
under the Affordable Care Act, when a prescription is
provided). See Preventive over-the-counter medications
earlier in this chapter for more information.
• Prescriptions filled at a pharmacy other than a Walmart
or Sam’s Club pharmacy (except as noted).
• Prescriptions filled by a pharmacy that is not an eligible
pharmacy for your medical plan option.
• Prescription drugs with over-the-counter equivalents.
• Prescription drugs purchased through a pharmacy
discount program.
• Drugs for which prior authorization has not been secured,
in cases where prior authorization is required.
• Prescription drug claims that are reduced, subsidized,
or paid by another health plan, insurance provider,
or pharmacy discount program. The AMP does not
coordinate benefits for pharmacy claims.
This list is not meant to be an all-inclusive list of excluded
benefits. For questions about excluded benefits, call
OptumRx at 844-705-7493.
Pharmacy discounts for prescriptions
not covered
If a prescription is covered by the pharmacy benefit, the
appropriate copay or coinsurance will apply. However, if the
prescription is covered under the AMP but ineligible for
coverage under the pharmacy benefit (e.g., it is being filled
too soon or is prescribed for off-label use), the prescription
will not be covered by the pharmacy benefit and the
pharmacy discount described in this section.
Discounts, coupons, pharmacy discount programs,
debit cards, or similar arrangements provided by drug
manufacturers or pharmacies to assist you in purchasing
prescription drugs (including any prescription drug
discounts/coupons provided to pharmacies when you fill a
prescription) do not count toward the medical plan’s annual
out-of-pocket maximum. In addition, if you have coverage
under the Saver Plan, such charges do not count toward
theSaver Plan’s network annual deductible.
If you are enrolled in the AMP, you are eligible for a
pharmacy discount on certain drugs not covered by the
pharmacy benefit. The discount varies depending on the
drug prescribed. Prescriptions purchased with the retail
pharmacy discount do not count toward your network
annual deductible or out-of-pocket maximum.
To use the pharmacy discount, present your plan ID card
to the pharmacy when you pick up your prescription. If
the prescription is not covered by the pharmacy benefit,
theretail pharmacy will automatically discount the cost
ofthe drug.
For information, contact OptumRx at 844-705-7493.
Filing a pharmacy benefit claim
When you fill a prescription at an eligible network pharmacy,
you do not need to file a claim. However, if you are unable
to use your card at a network pharmacy or if you disagree
with the amount you must pay, you can file a claim with
OptumRx. Your claim must be submitted in writing within
18 months of the date you had the prescription filled (or
attempted to have it filled). If the prescription is an eligible
prescription, it will be paid in accordance with the terms of
the pharmacy benefit.
Call OptumRx at 844-705-7493 for a claim form, or visit
One.Walmart.com. Claims are processed according to the
terms described in the Claims and appeals chapter.
If your claim is denied, you have a right to appeal. Appeals
are processed according to terms described in the Claims
and appeals chapter.
Privacy and security
When you purchase prescription drugs through a Walmart
or Sam’s Club pharmacy or an OptumRx network pharmacy,
your personal and medical information is kept confidential.
All network pharmacies are covered by and adhere to
applicable state and federal regulations, including the
Health Insurance Portability and Accountability Act of 1996
(HIPAA), which protects the privacy of personal health
information. Walmart values the trust that our associates
place in us. Earning that trust is in accordance with our core
value of respect for the individual. For more information,
see HIPAA notice of privacy practices in the Legal
information chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Health savings
account(HSA)
HSA advantages: tax breaks and Walmar contributions 100
HSA eligibility 100
Opening your HSA 101
Contributions to your HSA 102
Paying qualified medical expenses through your HSA 104
Investing your HSA 104
If you leave the company or are no longer enrolled in the Saver Plan 104
Closing your HSA 104

Health savings account(HSA)
99
Health savings account for Saver Plan paricipants
If you are enrolled in the Saver Plan and want to save money on qualified medical expenses, the
HSA is a great option. Your HSA contributions are tax-free and the company will match them
dollar-for-dollar, up to set limits. Your account balance earnings are also tax-free and, as the
money grows from year to year, you can use it to pay for current or future medical expenses.
RESOURCES
Find What You Need Online Other Resources
Establish an account or change your
contribution amount
Log on to One.Walmar.com or Workday
for Jet associates
Call People Services at 800-421-1362
Access your HSA Log on to MyHealthEquity.com
If you are logging in for the first time as a
member and have not already established
a user ID and password, click the “Begin
Now” button.
Call HealthEquity at 866-296-2860
HealthEquity is the HSA administrator
and custodian.
Get a list of qualified medical expenses
(I.R.C.§ 213(d))
Get information on contribution
limits, eligibility and tax reporing
responsibilities associated with an HSA
irs.gov Call HealthEquity at 866-296-2860 or
contact your tax advisor
What you need to know about the HSA
• You must be enrolled in the Saver Plan to open and contribute to an HSA through this program.
• Walmart will match on a pretax basis each dollar you contribute, up to the matching limit.
• The HSA allows you to pay for qualified medical expenses (as defined by the IRS) with tax-free dollars.
• If you accept the HSA’s terms and conditions, pass the customer identification process, and take the necessary steps
to open your account, you will receive a welcome kit at your home address. Your account will be considered open on
the effective date of your Saver Plan coverage.
• You are not eligible to make HSA contributions for any month in which you travel on Walmart business outside the U.S.
and are covered under the GeoBlue policy, which provides health benefits for associates traveling internationally on
business. Consult your tax advisor if you have questions about the amount to reduce your contributions based on your
individual circumstances.
• The health savings account is offered through HealthEquity.
Health savings account(HSA)
100
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
HSA advantages: tax breaks and
Walmar contributions
If you’re enrolled in the Saver Plan, the HSA offers you:
• Walmart contributions to your HSA to match your pretax
contributions, dollar-for-dollar up to the matching limit.
• The ability to contribute pretax dollars to the account
through payroll deductions.
• The ability to pay for qualified medical expenses with tax-
free dollars through the account, including easy access to
the money in your account using the debit card you will
receive. You can also access the funds in your account by
logging in to MyHealthEquity.com.
HealthEquity is the HSA administrator/custodian with which
Walmart has contracted to receive HSA contributions from
Walmart’s payroll. To receive the Walmart contribution to
your HSA or make pretax contributions through payroll
deduction, you must maintain an open account with
HealthEquity and continue medical coverage through the
Saver Plan. If you have an HSA with another custodian,
Walmart will not provide the Walmart contribution to your
account or allow you to make pretax contributions through
payroll deduction for that HSA.
Interest earnings and capital gains on the balance in your
account are not taxed during the period in which the funds
remain in your account. In addition, all HSA funds withdrawn
for qualified medical expenses are tax-free.
You have investment opportunities for your account balance
once that balance reaches a certain amount. Investments
are not guaranteed or FDIC-insured.
The balance in your HSA rolls over from year to year,
increasing your savings for future medical expenses. You
own the balance in your account, and can save it, invest
it in funds offered through your custodian, or spend it on
qualified medical expenses.
NOTE: State tax law with respect to HSAs may differ from
federal tax law in certain states, including California and
New Jersey. Please consult your tax advisor or HealthEquity
if you have questions about either the federal or state tax
implications of a health savings account.
HSA eligibility
You must be a Saver Plan participant to contribute to an
HSA through this program.
Even if you are enrolled in the Saver Plan, you cannot
contribute to an HSA if:
• You are covered under any other health plan that is not a
qualified high-deductible health plan, including a general
purpose health care flexible spending account (FSA)
or health reimbursement account (HRA). Exceptions
include some disease-specific coverage; dental, vision,
long-term care, and disability coverage; accident policies
such as critical illness insurance and accident insurance,
and others.
• You are enrolled in Medicare.
• You are enrolled in Medicaid.
• You are covered under TRICARE.
• You have received medical services from the U.S.
Department of Veterans Affairs during the preceding
three months, other than benefits for preventive care or a
service-connected disability. Mere eligibility for Veterans
Affairs benefits does not disqualify you from contributing
to an HSA.
• You have received medical services at an Indian Health
Service (IHS) facility during the preceding three months.
• You can be claimed as a dependent on another person’s
taxreturn.
Other restrictions may apply. For further information,
please call HealthEquity at 866-296-2860.
Your dependent’s status does not affect your ability
to contribute to an HSA. For example, your covered
spouse/partner’s Medicare status will not affect your
abilityto contribute to an HSA.
If you are a Saver Plan participant and also enrolled in
critical illness insurance, you’re not eligible for the major
organ transplant rider under that coverage due to IRS
guidance suggesting that such coverage would be viewed as
non-high-deductible plan coverage.
You are responsible for determining if you are eligible for
anHSA.
During the Plan year, you may be required to confirm
account eligibility to continue contributions (for example, if
you become Medicare-eligible because of your age, you may
be asked to verify that you have not enrolled in Medicare).
In certain cases, Medicare enrollment can be retroactive
(such as if you delay your enrollment past age 65) and, if that
occurs, you will also lose eligibility to make HSA contributions
retroactively. If you are eligible for, or are enrolling in,
Medicare, you should carefully evaluate your participation in
the HSA to avoid penalties for excess contributions.
The Saver Plan is a qualified high-deductible health plan
(HDHP) subject to ERISA and to requirements of federal
law that allow you to contribute to an HSA. Walmart does
not, however, insure the health savings account described
in this chapter. It is Walmart’s intention to comply with U.S.
Department of Labor guidance specifying that an HSA is
not subject to ERISA when the employer’s involvement with
the HSA is limited. Accordingly, the HSA is not established
or administered by Walmart or the Associates’ Health
Health savings account(HSA)
101
and Welfare Plan. Instead, the HSA is established by the
associate during the enrollment process and administered
by HealthEquity.
If you have non-high-deductible health plan coverage
through Walmart or any other employer (e.g., your
eligible spouse/partner’s employer), including a general
purpose flexible spending account (FSA) or a Health
Reimbursement Account (HRA), you are generally
ineligible to make HSA contributions (but you can enroll
in the Saver Plan). There are exceptions to this rule for
“limited purpose” FSAs/HRAs, which can be used for
dental or vision coverage only, or for “post-deductible”
FSAs/HRAs, which provide coverage only after you satisfy
the deductible under an HDHP. For information, contact
HealthEquity by phone at 866-296-2860 or online at
MyHealthEquity.com.
You are not eligible to make HSA contributions for any
month in which you are traveling on Walmart business
outside the U.S. and are covered under the GeoBlue policy,
which provides health benefit coverage for Walmart
associates traveling internationally on business. Consult your
tax advisor if you have questions about the amount to reduce
your contributions based on your individual circumstances.
If you make or receive an ineligible contribution to your
HSA, excise taxes may apply unless you remove the
contribution by certain deadlines. For more information
about Medicare, HSA eligibility, or how to correct
ineligible contributions, contact your tax advisor or review
IRS Publication 969, Health Savings Accounts and Other
Tax-Favored Health Plans. You can also call 800 Medicare
(800-633-4227), or visit Medicare.gov.
Opening your HSA
When you enroll online in the Saver Plan, you choose the
amount you want to contribute to your account through
payroll deductions. You may change your contribution
amount at any time. See Setting up or changing your
contribution amount later in this chapter.
You’ll receive a welcome kit at your home address directly
from HealthEquity, the HSA custodian, generally within the
following time frames:
• By the end of December if you enroll during Annual
Enrollment, or
• Within two to three weeks after your HSA is opened if you
enroll at any other time.
Your debit card will be included within the welcome kit.
Activate your debit card online at MyHealthEquity.com or
by calling HealthEquity at 866-296-2860.
No payroll withholding or employer contributions will be
deposited to your HSA until it is open. Your account will not
be considered open until you have successfully passed the
customer identification process required to open an HSA.
If HealthEquity requires additional information to complete
this process, it will contact you.
If any payroll withholding or employer contribution is made
before your account is open, the custodian will hold your
contribution and deposit it into your HSA when it is open.
If your account is not opened within a reasonable amount
of time, the funds withheld from your pay will be refunded
to you through your payroll check (less applicable payroll
taxes) and reported as wages on your Form W-2. The
employer contribution, if any, will be returned to Walmart.
For questions about your account status, welcome kit, or
debit card, call HealthEquity at 866-296-2860 or go online
to MyHealthEquity.com.
Once HealthEquity confirms that your account is open and
you have completed your HSA deductions selection online,
your contributions to the account and Walmart’s matching
contributions will begin the following pay period. See When
company contributions are made later in this chapter.
If you do not open your HSA by December 1 of the
Plan year, you will forfeit your right to the company’s
contributions for that year, even if you are covered by the
Saver Plan during that year.
For purposes of company funding and payroll deductions,
you must select HealthEquity as your HSA custodian when
you enroll. You may move your funds to another HSA
custodian at any time, but Walmart will provide company
funding and support ongoing payroll deductions only for
HSAs established with HealthEquity.
HSA FEES
The company pays the monthly maintenance fees if you
are enrolled in the Saver Plan and your HSA custodian is
HealthEquity.
The company does not pay overdraft fees, excess
contribution fees, or lost card fees. If you are enrolled
in COBRA, terminate employment with the company,
otherwise become ineligible for AMP coverage, or are
no longer enrolled in the Saver Plan, all associated fees
become your responsibility. These fees will be deducted
automatically from your HSA balance if any of these events
occur. Call HealthEquity at 866-296-2860 to learn about
the fees for various HSA services. It is your responsibility
to check your HSA balance prior to using funds to pay for
services. Current rate and fee schedules are available online
at MyHealthEquity.com. The fee schedule is also included in
the welcome kit.

Health savings account(HSA)
102
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Contributions to your HSA
Once you open your HSA, Walmart may make contributions
to your account as follows (as long as your account is open
and you are enrolled in the Saver Plan):
• Walmart matches your pretax contributions
dollar-for-dollar, up to the matching limit described
inthechart below.
• You may make pretax contributions to the account
through payroll deductions in any amount (of $5 or
more each pay period) up to the legal limit, taking into
account Walmart’s contributions. For administrative
purposes, contributions are generally based annually
on25 pay periods.
• In addition to making contributions by payroll deduction,
you can contribute money directly to your HSA by mailing
a check to HealthEquity, or by electronic funds transfer
(EFT) once you have linked a personal bank account on
the HealthEquity website. Any such contributions count
toward the contribution limit stated in the chart below.
These personal contributions are made on an after-tax
basis and are not eligible for the Walmart matching
contribution. Walmart does not track your after-tax HSA
contributions; you bear the responsibility of making sure
you do not exceed the annual contribution limit.
• If your requested HSA contribution for a specific pay
period exceeds the amount of your paycheck after
deductions, no contribution or company match will be
made to your HSA for that pay period.
• With respect to your final paycheck, your HSA salary
reductions and corresponding employer match may
be reduced because of state law restrictions on salary
reduction or because your requested HSA contribution
exceeds the net amount of your payroll check
afterdeductions.
If you experience a status change event and switch from
associate-only coverage to family coverage under the
Saver Plan during the year, Walmart will increase its
matching contribution to correspond with the matching
contribution limit for family coverage. If you switch from
family coverage to associate-only coverage during the year,
the matching contributions that the company made prior to
the change will not be reduced. If this results in your having
contributions in your account above the annual maximum
contribution allowed under IRS guidelines, the excess
contributions must be withdrawn bythe tax-filing deadline
to avoid additional taxes.
ANNUAL CONTRIBUTION LIMITS
By law, the maximum annual contribution that can be
made to your account, including both the company’s
contributions and your contributions (pretax and
after-tax), is:
• For 2020, $3,550 for individual coverage, or
• For 2020, $7,100 for family coverage.
See page 331
The annual maximum contribution is the total contribution
from all sources (payroll contributions by the associate
and/or the company and personal contributions).
These amounts are indexed annually by the federal
government and are subject to change each year.
YOUR CONTRIBUTIONS AND THE COMPANY’S CONTRIBUTIONS TO THE HSA
Your Saver Plan network
annualdeductible
Company matching contribution:
$1 for $1 up to
2020 maximum annual contribution
(associate and company contributions combined)*
$3,000 (associate-only coverage) $350 $3,550
$6,000 (family coverage) $700 $7,100
*If you are age 55 or over by December 31, 2020, you can contribute an
additional $1,000 in 2020.
See page 331 for 2021 contribution limits.
Health savings account(HSA)
103
SETTING UP OR CHANGING YOUR
CONTRIBUTIONAMOUNT
You may change your contribution amount online at any
time during the year on a going-forward basis.
To set up or change your contribution amount, log on to
One.Walmart.com or Workday for Jet associates and select
“OnlineEnrollment.” Contact People Services at 800-421-1362
if youneed help setting up your payroll deductions.
NOTE: Once you make the maximum annual contribution
(as stated in the chart on the previous page), your payroll
contributions automatically cease. It is your responsibility
to make a new contribution decision at the next Annual
Enrollment for the following calendar year.
IF YOU ARE AGE 55 OR OLDER
If you are age 55 or older, you can make additional “catch
up” contributions to your HSA by payroll deduction, just
like your regular contribution. For 2020, the catch-up
contribution limit is $1,000. Call HealthEquity at
866-296-2860 for information.
If you also cover your spouse under the Saver Plan and your
spouse is age 55 or older, he or she may also be eligible to
open a second HSA and contribute catch-up contributions.
The contribution limit for 2020 for both accounts combined
is based on the maximum amount that can be contributed
for a family: $7,100. If either you or your spouse is age 55 or
older in 2020, the total combined contribution is increased
by $1,000 for each participant age 55 or older. The company
does not contribute funds or pay any fees associated with an
HSA for your dependent spouse.
If you cover an eligible partner under the Saver Plan and
that individual is other than a spouse, you and your partner
are each eligible to contribute to individual HSAs up to the
maximum family contribution limit of $7,100 (provided that
neither party can be claimed as a tax dependent on any
individual’s federal tax return). If either associate or partner
is age 55 or older in 2020, the maximum contribution is
increased by $1,000 for each participant age 55 or older.
The company does not contribute funds or pay any fees
associated with an HSA for your dependent partner.
Call HealthEquity at 866-296-2860 for information on
opening an HSA for your eligible spouse/partner.
If two associates who are legally married are both eligible
to contribute to individual HSAs, the contribution limit for
2020 for both accounts combined is based on the maximum
amount that can be contributed for a family: $7,100. Note,
however, if either of the associates is age 55 or older in
2020, the total combined contribution is increased by
$1,000 for each associate age 55 or older.
If two associates are in a relationship that meets the
definition of eligible dependent but is other than a legal
marriage, and they have family coverage, each associate
is eligible to contribute to an individual HSA up to the
maximum family contribution limit of $7,100 (provided that
neither associate can be claimed as a tax dependent on any
individual’s federal tax return). If either associate is age 55
or older in 2020, the maximum contribution is increased by
$1,000 for each associate.
It’s important to monitor contributions to your HSA —
there are adverse tax consequences if your contributions
exceed the annual limit set by the federal government.
Changes in coverage during the year or enrollment after
the beginning of the year can affect your contribution
limits. If you become aware during the year that combined
contributions to your HSA exceed the annual limit, you can
withdraw the excess contribution and the related interest
earnings before your income tax return for the year is due
(including extensions). For assistance and information, call
HealthEquity at 866-296-2860.
EARNING INTEREST ON YOUR HEALTH
SAVINGSACCOUNT
The balance in your HSA earns interest. For interest rate
information on your account, contact HealthEquity at
866-296-2860 or go online to MyHealthEquity.com.
Your current interest earned along with the interest rate
schedule is available on your monthly statements.
WHEN COMPANY CONTRIBUTIONS ARE MADE
Walmart will match dollar-for-dollar the amount that you
contribute through payroll deduction each pay period, up to
the matching limit for your coverage, as shown in the chart
titled Your contributions and the company’s contributions to
the HSA. The company deposits this contribution, along with
any contribution you make through payroll deduction, into
your HSA shortly after each payroll deduction period ends.

Health savings account(HSA)
104
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Paying qualified medical expenses
through your HSA
See page 331 for updated information on eligible expenses.
When you have an eligible medical expense, you can decide
whether to pay out of your pocket or use the funds in your
HSA. Some people use their HSA for current expenses,
while others prefer to use the HSA as an account for future
health care expenses. Eligible expenses include health
plan deductibles and coinsurance, most medical care and
services, dental and vision care, and prescription drugs.
In addition, amounts paid for over-the-counter drugs
are qualified expenses if the drugs are prescribed by a
doctor. (This requirement does not apply to insulin.) These
expenses must not already be covered by your medical
plan, and health insurance premiums generally do not
qualify. Refer to IRS Publications 969 and 502 at irs.gov
for information about qualified medical expenses. You can
also find information about qualified medical expenses on
One.Walmart.com and MyHealthEquity.com.
THE HSA AND YOUR INCOME TAX RETURN
The funds in your HSA belong to you, but any money
used for nonqualified medical expenses is subject to
federal income tax as well as a 20% penalty if you are
under age 65. Make sure you save your receipts and other
records to show that you used your HSA funds for eligible
expenses. Remember that you are responsible for the
tax consequences associated with contributions to and
withdrawals from your HSA. Consult your tax advisor if
youhave questions about your HSA and taxes.
Investing your HSA
Once your account reaches a minimum balance of $1,000,
you can invest any amount over that balance in a selection
of over 20 investment funds available through HealthEquity.
Review the funds and learn more at MyHealthEquity.com
under “Investments.”
If you leave the company or are no
longer enrolled in the Saver Plan
The funds in your HSA belong to you as the account
holder, even if you enroll in COBRA, change medical plans,
change jobs, or leave the company. In these events, all fees
associated with the account become your responsibility.
Closing your HSA
All funds in your HSA belong to you. You may use these
funds for qualified medical expenses on a tax-free basis
now and in the future. If you do not choose to maintain the
account, call HealthEquity at 866-296-2860 for information
on closing your account.
Health savings account(HSA)
105

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Your dental plan 108
How the dental plan works 108
Filing a dental claim 109
What is covered under thedentalplan 110
Limited benefits 112
What is not covered under thedentalplan 112
Break in coverage 113
When dental coverage ends 113
If you leave the company and arerehired 114
If you drop coverage andreenroll 114
The dental plan

The dental plan
107
The dental plan
The dental plan covers a wide range of services, with no deductible for preventive or orhodontics.
Plus, when you use network dentists, you’ll save money while protecting one of your biggest
assets—your smile.
RESOURCES
Find What You Need Online Other Resources
Get a listing of Delta Dental
network dentists
Go to One.Walmar.com or
deltadentalar.com
Call Delta Dental at 800-462-5410
or People Services at 800-421-1362
Get answers to questions
about your dental claims
and to contact Delta Dental
Customer Service
Go to deltadentalar.com and select
“Login/Register” to create your account
Call Delta Dental at 800-462-5410
Get a claim form if you use a
nonparicipating dentist
Go to One.Walmar.com or
deltadentalar.com
What you need to know about the dental plan
• If you are an eligible associate, you may purchase dental coverage to assist with preventive, basic, and major dental care
as well as with orthodontia expenses. See the Eligibility and enrollment chapter for information on eligibility.
• Delta Dental administers the dental plan benefit.
• Once you meet the dental plan’s annual deductible, the dental plan pays benefits of up to $2,500 per covered person
per calendar year and a lifetime maximum orthodontia benefit of $1,500 per covered person. The annual deductible
does not apply for preventive and diagnostic services or orthodontia.
• Dental plan coverage must remain in effect for two full calendar years.
• Orthodontia is covered after a 12-month waiting period.
• If you have medical coverage with the Associates’ Medical Plan (AMP), both the dental and medical information are on
your plan ID card. If you are enrolled in an HMO or if you have dental-only coverage, you will receive a Delta Dental ID
card. Your ID cards will be mailed to your home address.

The dental plan
108
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Your dental plan
The dental plan is available to you if you are an hourly
or management associate. Coverage is also available
toyoureligible dependents, with the exception of
spouses/partners of part-time associates, temporary
associates, and part-time truck drivers. The dental plan
isadministered through Delta Dental.
Once you enroll in the dental plan, your coverage must
remain in effect for two full calendar years. You can add or
remove a dependent during Annual Enrollment or due to a
status change event, but you must maintain a minimum of
associate-only coverage for two full calendar years.
CHOOSING A COVERAGE LEVEL
When you enroll in the dental plan, you also select the
eligible family members you wish to cover:
• Associate only
• Associate + spouse/partner (except for part-time hourly
associates, temporary associates, or part-time truck drivers)
• Associate + child(ren), or
• Associate + family (except for part-time hourly associates,
temporary associates, or part-time truck drivers).
For information on dependent eligibility and when
dependents can be enrolled, see the Eligibility and
enrollment chapter.
The dental plan benefit is self-insured, which means benefits
are not paid by an insurance company. Claims are processed
by Delta Dental of Arkansas.
How the dental plan works
The dental plan covers four types of dental services:
• Preventive and diagnostic care coverage includes oral
examinations and cleanings and related services. You
do not have to meet the annual deductible before the
dental plan covers these services. Charges you incur for
preventive and diagnostic care, if any, do not apply toward
your deductible.
• Basic care coverage includes fillings, non-surgical
periodontics, and root canal therapy, and begins after you
meet the annual deductible.
• Major care coverage includes surgical periodontics,
crowns and dentures and begins after you meet the
annual deductible.
• Orthodontia coverage begins after an individual has been
covered under the dental plan for 12 months; you do not
have to meet the annual deductible before receiving
orthodontia benefits. Charges you incur for orthodontia
care do not apply toward your deductible.
NOTE: The 12-month waiting period for orthodontia
coverage is waived for localized associates and their
covered dependents.
COVERAGE UNDER THE DENTAL PLAN
Annual deductible
Waived for preventive and diagnostic care and
orhodontia care
$75 per person/$225 maximum per family
Maximum benefit
Does not apply to orhodontia care
$2,500 per covered person per calendar year
Delta Dental
PPO dentists
Delta Dental
Premier dentists
Non-network
dentists
Preventive and diagnostic care
Charges (if any) do not count toward
annualdeductible
100% covered; no annual
deductible applies
80% covered;* no annual
deductible applies
80% of maximum
plan allowance; no
annual deductible
* In areas served by an insufficient number of PPO
dentists, as determined by facility location, services are
covered at 100%. Go to One.Walmar.com for details.
Basic care
Including fillings, non-surgical periodontics, and
root canal therapy
80% of maximum plan allowance after annual deductible is met
Major care
Including surgical periodontics, crowns, and dentures
50% of maximum plan allowance after annual deductible is met
Orhodontia (12-month wait)
Charges do not count toward annual deductible
or maximum benefit
80% of maximum plan allowance up to $1,500 lifetime maximum orhodontia
benefit per person; no annual deductible applies

The dental plan
109
After you meet the annual deductible (if applicable) and
complete any applicable waiting period, the dental plan pays
a percentage of the maximum plan allowance (MPA) for
covered expenses.
MAXIMUM PLAN ALLOWANCE MPA
The MPA is the maximum amount the dental plan pays for
covered dental services. The MPA applies to network and
out-of-network dental services.
For covered network services, the MPA is that portion of a
provider’s charges covered by the dental plan as determined
by the provider’s contract with Delta Dental of Arkansas.
Network providers agree to accept an amount negotiated
by Delta Dental for covered services as payment in full,
subject to applicable deductible and coinsurance amounts.
For covered out-of-network services, the MPA is limited
to the allowance set by Delta Dental in its discretion and
utilizing such methods or benchmarks Delta Dental may
choose to employ. If you see an out-of-network dental
provider, the dental plan pays a percentage based on the
lesser of the MPA or the provider’s actual billed charges for
a covered procedure. If the provider’s billed charges exceed
the Plan’s MPA, you are responsible for paying 100% of the
difference. For additional information, call Delta Dental at
800-462-5410.
KNOW WHAT YOU’LL OWE:
GET A PRETREATMENT ESTIMATE
You are not required to get pre-approval of any dental
treatments. But by having your dentist submit a proposed
treatment plan, you can learn how much you can expect the
dental plan to pay for a procedure or course of treatment
before the work is done. It is recommended that a proposed
treatment plan be submitted for treatment expected to
cost $800 or more. Delta Dental will provide a pretreatment
estimate of the amount that will be covered and may
suggest an alternate treatment plan if part of your dentist’s
treatment plan is ineligible for coverage.
To get a pretreatment estimate, ask your dentist to
complete a regular dental claim form and check the
“predetermination” box. The form should be mailed to:
Delta Dental of Arkansas
P.O. Box 15965
Little Rock, Arkansas 72231-5965
Delta Dental’s pretreatment estimate is not a guarantee
of payment. You still must file a claim for the services
rendered, as set out in the Claims and appeals chapter.
SAVE MONEY BY USING NETWORK DENTISTS
As a dental plan participant, you can use any dentist and
receive benefits for covered expenses under the Plan.
You will save money and time, however, when you use
Delta Dental dentists. Providers contracted with Delta
Dental’s Premier and PPO networks agree to accept the
dental plan’s maximum plan allowance as payment in full
for a covered procedure, so you pay no more than the
dental plan’s applicable coinsurance percentage (after
you meet any applicable annual deductible). In addition,
Delta Dental’s network providers also provide participants
with discounted prices. When you see a Delta Dental PPO
provider, you may be able to save more because PPO
providers have agreed to accept reduced fees for covered
procedures when treating Delta Dental participants. You
may save time because network dentists will often file your
claims for you.
The Delta Dental PPO network is an extensive nationwide
network of dentists, but is not as widely available as the
Delta Dental Premier network. Refer to the chart entitled
Coverage under the dental plan earlier in this chapter for
details on how coverage terms for preventive and diagnostic
care may differ based on the availability of PPO dentists
in your area. To find a Delta Dental PPO or Delta Dental
Premier dentist, see Dental plan resources at the beginning
of this chapter.
IT PAYS TO USE NETWORK DENTISTS
Delta Dental
Premier dentists
and PPO dentists
Non-network
dentists
Dentist files claim
forms for you
Yes No
Dentist accepts
maximum plan
allowance as
payment in full,
subject to annual
deductible and
coinsurance
Yes No
Dentist offers
discounted prices
for Delta Dental
paricipants
Yes No
Filing a dental claim
If you use a Delta Dental network dentist, your dentist
will often file the claim for you. If you use a non-network
dentist, you may need to file a claim. The dentist may be
paid directly from the dental plan if the dentist is a Delta
Dental network dentist. If you use a non-network dentist,
the payment will be made to you.
Mail your claim to:
Delta Dental of Arkansas
P.O. Box 15965
Little Rock, Arkansas 72231-5965
The dental plan
110
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
You or your dental provider must file a claim in accordance
with the claims procedure within 18 months from date
of service or your claim will be denied. Not following the
claims procedure described in the Claims and appeals
chapter, such as failure to mail your claim to the correct
address, may result in the denial of your claim.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter. You
have the right to appeal a claim denial.
IF YOU HAVE COVERAGE UNDER MORE THAN
ONE DENTAL PLAN
If you or a family member have coverage under the
dental plan and are also covered under another dental
plan (for example, your spouse/partner’s company plan),
coordination of benefits may apply. The dental plan has the
right to coordinate with other plans you are covered under
so the total dental benefits payable will not exceed the
level of benefits otherwise payable under the dental plan.
Coordination of benefits procedures and plans referred to
as “other plans” are described in If you have coverage under
more than one medical plan in The medical plan chapter.
What is covered under
thedentalplan
The dental plan covers the services listed in this section,
subject to some limitations. If you have questions about
what is covered under the dental plan, call Delta Dental
at800-462-5410.
PREVENTIVE AND DIAGNOSTIC CARE
Preventive and diagnostic care are covered without having
to meet the annual deductible.
Bitewing X-rays: Limited to four per calendar year.
Combined with panoramic X-ray if done by same provider
on same day and processed as a full mouth series.
Cleaning (dental prophylaxis): One prophylaxis, including
cleaning, scaling and polishing of the teeth, is covered
twice during a calendar year. Two additional cleanings
are allowed during a pregnancy and up to three months
following delivery. Two additional cleanings are allowed for
heart disease, diabetes, and periodontal disease. Additional
periodontal maintenance allowed for periodontal disease.
Fluoride treatment: Covered once in any consecutive
12-month period for participants under age 19.
Full-mouth debridement: Limited to once per lifetime.
Full-mouth series or panoramic X-rays: Limited to
one procedure in any consecutive 60-month period.
A full-mouth series is any combination of 14 or more
periapical and/or bitewing X-rays taken on the same date.
If the combination of separately billed intraoral images
(i.e.,bitewings and periapicals) equals or exceeds the
number of films allowed for a full mouth series, the charges
for the images will be combined and deemed to comprise
a full mouth series. A benefit is paid only if no other full
mouth series or panoramic radiographic image has been
paid during the preceding 60 consecutive months.
Oral evaluations: Benefits are payable as follows:
• Routine oral evaluation: Two evaluations covered during
acalendar year.
• Comprehensive detailed oral evaluation or periodontal
evaluation: Initial comprehensive oral evaluation are
payable subject to the routine oral evaluation time
limitations. Subsequent oral evaluations submitted by the
same provider within three years are processed as routine
oral evaluations.
Emergency evaluations performed by dentists are not
subject to the calendar year restriction.
Periapical X-rays: Covered as needed.
Preventive resin restoration: Covered for first and second
permanent molars with unrestored occlusal surface for
participants under age 19. Limited to one treatment per
tooth every five years.
Pulp vitality tests: Covered if same provider does no other
definitive procedure the same day.
Risk assessment: Covered once every three-year period for
children age 3 through age 19.
Sealant repair: Covered for first and second permanent
molars with unrestored occlusal surface for participants
under age 16. Not covered during the first 24 months of the
initial placement of the sealant. Limited to one treatment
per tooth every 24 months. Not covered when the tooth has
previously received a preventive resin restoration.
Sealants: Covered for first and second permanent molars
with unrestored occlusal surface for participants under
age 16. Limited to one treatment per tooth per lifetime.
Not covered when the tooth has previously received a
preventive resin restoration.
Space maintainers: Covered for participants age 13 and
under. Limited to one appliance per space (quad/arch)
extraction site in any consecutive 60-month period. Repair
or replacement of a space maintainer is not covered.
BASIC CARE
After you meet the annual deductible, the Plan pays 80% of
the maximum plan allowance for basic care.
The dental plan
111
Amalgam and composite resin fillings: Benefits are payable
once per tooth surface in any consecutive 24-month period.
Endodontics: Includes pulp therapy and root canal therapy.
See Root canal therapy in Major care below.
Extractions: Nonsurgical extractions are covered once
pertooth.
Nonsurgical periodontics: Provided once per quadrant in
any consecutive 24-month period.
Occlusal orthotic device (TMJ appliance): Benefits are
payable once every five years. Adjustments within six
months are not covered. One adjustment covered per
yearthereafter.
Periodontal maintenance: Periodontal maintenance is
covered only if done 30 days or more after the completion
of surgical or nonsurgical periodontal treatment. Thereafter,
periodontal maintenance is allowed up to four times per
calendar year. This benefit is combined with any routine
cleanings performed during the same calendar year with a
combined limitation of four for that year.
MAJOR CARE
After you meet the annual deductible, the Plan pays 50% of
the maximum plan allowance for major care.
Anesthesia/general anesthetics and IV sedation: Covered
only when provided in the following circumstances:
• The patient suffers from a medical condition that prevents
him or her from holding still (including but not limited to
dystonia, Parkinson’s disease, autism)
• The patient is under age 4, or
• In connection with certain covered oral surgical procedures.
Complete and partial removable dentures and partial
fixed bridges: Covered when the denture or bridge is the
professionally accepted, standard course of treatment.
• Includes replacement or addition of teeth to dentures,
partials or fixed bridgework.
• When alternate treatment plans are available, the dental
plan covers the professionally accepted, standard course
of treatment. For example, a bridge is allowed only
when a partial denture will not suffice. See Alternative
treatment plans in Limited benefits later in this chapter.
• Complete and partial or removable dentures are not
payable for patients under the age of 16.
• A denture that replaces another denture or fixed bridge, or
a fixed bridge that replaces another fixed bridge, is covered
only if the existing denture, partial denture or fixed bridge
is at least five years old and cannot be repaired.
Crowns, cast restorations, inlays, onlays, and veneers:
Covered only when the tooth cannot be restored by
amalgam or composite resin filling.
• Replacement is not covered unless the existing crown, cast
restoration, inlay, onlay, or veneer is more than five years
old and cannot be repaired.
NOTE: Accidents as a result of biting or chewing are not an
exception to the five-year wait for crown replacements.
• For participants under age 12, benefits for crowns on vital
teeth are limited to resin or stainless steel crowns, unless
there is a history of root canal therapy or recession of
the pulp.
• Treatment is determined according to the alternate
treatment plan limitation. See Alternative treatment plans
in Limited benefits later in this chapter.
Implants: Surgical placement of an implant body is covered
once in every five-consecutive-year period.
• The abutment to support a crown is covered once in every
five-consecutive-year period.
• An implant or abutment-supported retainer is covered
once in every five-consecutive-year period.
• An implant maintenance procedure is covered once in any
12-consecutive-month period.
• Implant removal is covered once in a lifetime per tooth.
Implants are not payable for patients under the age of 16.
Occlusal adjustment (limited): Covered only if done
180 days or more after completion of initial restorative,
prosthodontic and implant procedures that include the
occlusal surface.
Oral surgery: Surgical extractions and extractions of
wisdom teeth, including preoperative and postoperative
care, except for those services covered under the
Associates’ Medical Plan. Oral sedation and/or nitrous oxide
(analgesia) are not covered. If oral surgery is performed in
a hospital setting, the dental plan covers oral surgeon fees
for such services for covered individuals not enrolled in the
Associates’ Medical Plan.
Outpatient or inpatient hospital costs and additional fees
charged by the dentist for hospital treatment: See Hospital
charges in What is not covered under the dental plan later
in this chapter.
Root canal therapy: Includes bacteriological cultures,
diagnostic tests, local anesthesia, and routine follow-up
care. Payable once per tooth.
• Therapeutic pulpotomy is payable once per tooth until
age21.
• Retreatment of a previous root canal is allowed once in a
consecutive 24-month period.
Surgical periodontics: Treatment of the gums — osseous
surgery/soft tissue graft, provided in the same area once in
any consecutive 36-month period.
The dental plan
112
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
ORTHODONTIA
After you have been a participant in the dental plan for
12 months, you are eligible for orthodontia assistance for
yourself (the associate). Each of your covered dependents
must also participate in the dental plan for 12 months
before becoming eligible for orthodontia assistance. If you
terminate coverage for any reason and reenroll, your prior
time enrolled for coverage will count toward the 12-month
waiting period. (The12-month wait is waived for localized
associates and their covered dependents.)
If the dentist submits a statement at the beginning of a period
of orthodontic treatment showing a single charge for the
entire treatment, benefits are paid in the following manner:
• The dentist receives an initial payment of up to $150
• A prorated portion of the remainder is paid every three
months based on the estimated period for treatment and
on continued eligibility, and
• The amount and number of payments are subject to
change if the charge or treatment period changes.
The dental plan covers only orthodontic treatment that
begins after the covered individual becomes eligible for
orthodontia assistance. Active orthodontic treatment is
deemed started on the date the active appliances are first
placed. Active orthodontic treatment is deemed completed
on the earlier of:
• The date on which treatment is voluntarily discontinued, or
• The date on which the active bands or appliances are
removed.
If an individual has had orthodontia treatment prior to
becoming eligible for orthodontia assistance under the
dental plan, treatment is available only if five years have
elapsed since the completion or discontinuance of that
orthodontic treatment plan.
Repair or replacement of an orthodontic appliance is
notcovered.
There are certain orthodontia assistance benefits that are
not covered. See What is not covered under the dental plan
later in this chapter.
Limited benefits
Alternative treatment plans: When alternative treatment
plans are available, the dental plan covers the professionally
accepted, standard course of treatment.
Transfer of treatment: If you transfer from the care of
one dentist to another during the course of treatment, or
if more than one dentist renders services for one dental
procedure, the dental plan pays no more than the amount it
would have paid if only one dentist had rendered services.
What is not covered under
thedentalplan
The dental plan does not pay benefits for all types of
services. To determine if a service is covered, call Delta
Dental or submit a pretreatment estimate of benefits form.
Services that are not covered by the plan include, but are
not limited to, the following:
Accidental injury to sound, natural teeth: Expenses for
treatment of accidental injury to sound, natural teeth may
be covered under the medical plan. This exclusion does not
apply to accidental injuries as a result of biting or chewing;
these charges may be covered under the dental plan.
Beyond the scope of licensure or unlicensed: Services
rendered by a dentist beyond the scope of their license, or
any services provided by an unlicensed dentist.
Bridgework: Repair or recementing of bridgework during
the first six-month post-delivery period, and such services
received more often than once every five years.
Cosmetic purposes: Services performed for cosmetic
purposes or to correct congenital, hereditary, or
developmental malformations. This exclusion does not apply
to orthodontic services for the correction of malposed teeth.
Dentures: Repair or relining of dentures during the first
six-month post-delivery period, and such services received
more often than once every five years for repairs and once
every three years for relines and rebases.
Elective non-emergency dental services outside the U.S.
Elective non-necessary services: Services that are
not dentally necessary or that do not meet generally
accepted standards of care for treating the particular
dental condition, including decoration, personalization or
inscription of any tooth, device, appliance, crown, or other
dental work.
Experimental or investigational: Charges for treatment
or services, including hospital care, that are experimental,
investigational, or inappropriate, under protocols
established by Delta Dental.
Governmental agency: Services provided or paid for by any
governmental agency or under any governmental program
or law, except charges for legally entitled benefits under
applicable federal laws.
Hospital charges: Services performed in a hospital or
outpatient hospital setting, including but not limited to
provider and facility charges. This exclusion does not apply
to oral surgeon fees for participants not enrolled in the
Associates’ Medical Plan, subject to terms of the dental plan.
The dental plan
113
Occlusal guards: Devices serving to minimize effects of
bruxism (grinding) or other occlusal factors. This exclusion
does not apply to occlusal orthotic devices to treat
TMJdisorders.
Oral sedation: Oral sedation and/or nitrous oxide (analgesia).
Orthodontia care: Services in connection with treatment
for the correction of malposed teeth during the first 12
consecutive months that a participant is covered under the
dental plan.
Periodontal splinting: Charges for complete occlusal
adjustments or stabilizing the teeth through the use of
periodontal splinting.
Permanent restorations: Charges for bases, liners,
and anesthetics used in conjunction with permanent
restorations (fillings).
Prescription drugs and medicines: Written for dental
purposes.
Prosthetics, duplicates: Duplicate prosthetic devices
orappliances.
Retainers: Separate charges for retainers (appliances
intended to retain orthodontic relationship) or habit
appliances to address harmful behaviors such as thumb-
sucking or tongue-thrusting.
Services undertaken prior to effective date or during
the waiting period for orthodontia services: Charges
for courses of treatment, including prosthetics and
orthodontics, which are begun prior to the effective date
of coverage or before you are eligible to receive benefits
for orthodontia services.
Surgical corrections: Charges for services related to the
surgical correction of:
• Temporomandibular joint dysfunction (TMJ)
• Orofacial deformities, and
• Specified oral surgery procedures covered by the
Associates’ Medical Plan.
Tooth structure: Services for restoring tooth structure lost
from wear, for rebuilding or maintaining chewing surfaces
due to teeth out of alignment or occlusion, or for stabilizing
the teeth.
OTHER CHARGES NOT COVERED
• Any procedure performed for a temporary purpose
• Charges in excess of the maximum plan allowance
• Extraoral grafts
• Hypnosis or acupuncture
• Oral hygiene instruction and dietary instruction
• Plaque control programs
• Services covered by the Associates’ Medical Plan
• Services for which there is no charge
• Teledentistry
• Any other services not specifically listed as covered
• Charges covered by workers’ compensation or employers’
liability laws
• Services provided by a member of the participant’s family,
or
• Charges incurred as a result of war.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your dental premiums to avoid a break
in coverage. These situations occur most commonly if you
are on a leave of absence or if your Walmart paycheck is
not sufficient to pay your full share of the cost of coverage
(such as after a reduction in hours). Depending on your
circumstances, failure to make your premium payments by
the due date may result in an interruption in the payment of
any benefit claims and/or a break in coverage.
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information about
making payments while on a leave of absence, see When
special arrangements are necessary to maintain coverage in
the Eligibility and enrollment chapter.
When dental coverage ends
Your coverage ends on your last day of employment or
when you are no longer eligible under the terms of the
Plan. Dependent coverage ends when your coverage ends
or when a dependent is no longer an eligible dependent
(as defined in the Eligibility and enrollment chapter). All
benefits cease on the date coverage ends, except for
completion of operative procedures in progress at the
time coverage ends. “Operative procedures” are limited
to individual crowns, dentures, bridges, and implants,
and are considered “in progress” only if all procedures
for commencement of lab work are completed and all
operative procedures are completed within 45 days of
termination. The dental plan does not pay benefits if you
or a covered dependent receive benefits for these post-
termination expenses from another plan. You and/or your
enrolled dependents may be eligible for continued coverage
through the Consolidated Omnibus Reconciliation Act of
1985, as amended (COBRA). See the COBRA chapter for
information regarding COBRA continuation coverage.
The dental plan
114
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you leave the company and
arerehired
If you return to work for the company within 13 weeks,
you will automatically be reenrolled for the same coverage
you had prior to leaving the company (or the most similar
coverage offered under the Plan). If your break is 30
days or less, the annual deductible and waiting period
for orthodontia assistance will not reset. If your break is
greater than 30 days, your annual deductible and waiting
period for orthodontia assistance will reset. If your break is
greater than 30 days but less than 13 weeks, and you have
already maintained coverage under the Plan for a minimum
of two years, you will have 60 days after resuming work to
drop or otherwise change the coverage in which you were
automatically reenrolled.
If you return to work after 13 weeks, you will be considered
newly eligible and may enroll for coverage under the time
periods and conditions described in the Eligibility and
enrollment chapter.
If you drop coverage andreenroll
If you drop coverage and reenroll within 30 days, you will
automatically be reenrolled for the same coverage you
had (or the most similar coverage offered under the Plan).
In this case, the annual deductible and waiting period for
orthodontia assistance will not reset.
If you drop coverage and reenroll after 30 days, you will be
considered newly eligible and may enroll for coverage under
the time periods and conditions described in the Eligibility
and enrollment chapter.
IF A DEPENDENT IS DROPPED FROM
COVERAGE ANDREENROLLED
If a dependent child is dropped from coverage and then
determined to be eligible for coverage within 30 days, the
dependent will automatically be reenrolled in the same
coverage you elect for yourself. The annual deductible and
waiting periods for orthodontia assistance will not reset.
If your dependent regains eligibility and is reenrolled after
30 days, they will be treated as a newly eligible dependent.
The associate may enroll them for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.
The dental plan
115

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The vision plan 118
How the vision plan works 118
How to use the plan 119
What is not covered 119
Breakage and loss of eyewear 119
Filing a vision claim 119
Break in coverage 120
When vision coverage ends 120
If you leave the company and arerehired 120
If you drop coverage and reenroll 120
The vision plan

The vision plan
117
The vision plan
The vision plan helps you pay for routine eye exams, lenses, frames, and contact lenses, so you can
see clearly for years to come.
RESOURCES
Find What You Need Online Other Resources
Locate a Walmar Vision Center or
Sam’s Club Optical provider
Go to One.Walmar.com
For detailed information about vision
plan coverage or to locate a VSP
network provider
Go to vsp.com and enter your member number Call VSP at 866-240-8390
Get the cost for vision plan coverage Go to One.Walmar.com Call People Services at
800-421-1362
What you need to know about the vision plan
• Coverage under the vision plan is separate from the medical plan, which generally does not cover charges for routine
eye care. If you are interested in coverage for vision services not covered by the medical plan, you must enroll
separately in the vision plan.
• You may see any Walmart Vision Center, Sam’s Club Optical, or VSP network provider for care and receive the same
level of benefits. No benefits are available if you see a non-network provider.
• You may purchase contact lenses online at WalmartContacts.com or SamsClubContacts.com. VSP coordinates the
amount of your purchase eligible for coverage. Go to vsp.com or call VSP at 866-240-8390 for details about the
contact lens benefit.
• If you have access to an HMO plan that offers vision coverage, compare the HMO’s benefits and the benefits
offered by the vision plan and decide which option best meets your needs.
• If you have medical plan coverage with the Associates’ Medical Plan (AMP), the VSP phone number will appear
on your plan ID card. If you are enrolled in an HMO or if you enroll for vision coverage only or dental and vision
coverage only, you will receive a VSP ID card, which will be mailed to your home address.

The vision plan
118
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The vision plan
Walmart offers the vision plan to help you pay for routine eye
care. The vision plan is administered through VSP. You may
access care under the vision plan through a Walmart Vision
Center or Sam’s Club Optical facility, or through a provider in
VSP’s nationwide network. Vision plan coverage is available to
you if you are an hourly or management associate. Coverage
is also available to your dependents, with the exception
of spouses/partners of part-time associates, temporary
associates, and part-time truck drivers.
CHOOSING A COVERAGE LEVEL
When you enroll in the vision plan, you also select the
eligible family members you wish to cover:
• Associate only
• Associate + spouse/partner (except for part-time hourly
associates, temporary associates, or part-time truck drivers)
• Associate + child(ren), or
• Associate + family (except for part-time hourly associates,
temporary associates, or part-time truck drivers).
For information on dependent eligibility and when
dependents can be enrolled, see the Eligibility and
enrollment chapter.
How the vision plan works
The vision plan covers a routine eye exam once every calendar
year, lenses once every calendar year, frames once every
calendar year, or contact lenses once every calendar year.
The vision plan pays benefits for prescription contact lenses
or prescription eyeglasses. If you choose contact lenses, you
will not be eligible for lenses or frames again until the next
calendar year. Benefits are paid as shown in the chart below.
Walmart providers and VSP network providers have agreed to
provide their services to covered associates for a prearranged
fee; all you pay is the applicable copay and the cost of any
non-covered or elective items. VSP pays the rest directly to
the provider. No benefits are paid for services at a provider
that is neither a Walmart/Sam’s Club provider nor a VSP
network provider.
Additional charges. Charges for any of the following items
are your responsibility. Call VSP at 866-240-8390 for more
information.
• Blended lenses
• Oversize lenses
• Photochromic or tinted lenses other than Pink 1 or 2
allowance
• Laminated lenses
• High-index lenses
VISION PLAN BENEFITS
Walmar Vision Center Sam’s Club Optical VSP network providers
Routine exam copay
Once every calendar year
$4
Limitations apply for low-vision testing or supplemental testing for individuals whose vision
problems are not correctable with regular lenses.
Materials copay $4
Applies with purchase of frames or lenses (but not contact lenses). Copay is charged only once
when frames and lenses are purchased together.
Progressive lens copay $55
Lenses
• Single vision
• Lined bifocal
• Lined trifocal
• Lenticular
• Progressive multifocal
100% covered after copay
Standard lenses are covered after applicable copay. Check with your optical team for lenses
offered under benefit.
Frames
Once every calendar year
$130 allowance
Charges above the frame allowance are your responsibility.
Contact lenses
Once every calendar year In lieu of
glasses
$130 contact lens allowance
Fitting and evaluation fee up to $60 may apply. Charges above the contact lens allowance are
your responsibility.
NOTE: Sales taxes may apply and will reduce the vision benefit.

The vision plan
119
compliance with laws or regulations enacted by any
federal, state, municipal, or other governmental body
– are paid for by another insurance plan (see If you have
coverage under more than one vision plan later in this
chapter), or
– are payable under any health care program suppored
in whole or in par by federal funds or any state or
political subdivision.
• Medical or surgical treatment or supplies
• Professional services or eyewear connected with
orthoptics, vision training, subnormal vision aids,
aniseikonic lenses and tonography, and other services/
materials not covered by the vision plan
• Replacement of broken lenses or frames after one year
from purchase
• Replacement of lost lenses or frames unless the patient
is otherwise eligible under the frequency provisions,
as detailed in the Vision plan benefits chart on the
previouspage
• Service contract fees
• Plano lenses (nonprescription lenses less than .50 diopter)
• Services from any non-network providers — i.e., any
provider that is not affiliated with a Walmart Vision Center
or Sam’s Club Optical, or that is not a VSP network provider.
Breakage and loss of eyewear
If you’re covered under the vision plan and you damage
your eyewear within one year of purchase, you can return
to your network provider for replacement or repair. Some
warranties on eyewear may be longer than one year; check
with your eyewear provider for details.
Lost eyewear is not covered under the vision plan.
Filing a vision claim
When you use the vision plan, claims for services are
generally not required; see How to use the plan for a
description of payment arrangements. When it’s necessary
to file a claim — for example, if you are newly enrolled in
the vision plan when you see a provider and your personal
information is not yet on file with VSP — return to the
provider after your information is in the system and ask
the provider to file the claim on your behalf. Claims are
processed according to the terms described in the Claims
and appeals chapter.
• Anti-reflective coating
• Color coating
• Mirror coating
• Optional cosmetic processes
• Low vision care
• Cosmetic lenses, and
• Frames or contacts that cost more than your allowance.
How to use the plan
Follow these steps for your vision care.
STEP 1 To find a Walmar Vision Center or Sam’s Club
Optical provider, go to One.Walmar.com;
to find a provider in the VSP network, call
866-240-8390 or go to vsp.com and enter your
member number.
STEP 2 When you make an appointment, identify
yourself as a VSP member and give the office
your name and date of birh, plus the patient’s
name (if different). The provider’s office
contacts VSP to verify your eligibility.
STEP 3 At your visit, pay your copay and any other
required amount directly to the Walmar
Vision Center or Sam’s Club Optical or VSP
network provider. The provider’s office arranges
for reimbursement and handles any other
administrative tasks required.
What is not covered
Some expenses are not covered under the vision plan,
including:
• Charges for eye exams, lenses, or frames that:
– you are not legally obligated to pay for or for which no
charge would be made in the absence of vision coverage
– exceed plan maximums
– are not necessary according to accepted standards of
ophthalmic practice, or not ordered or prescribed by
the attending physician or optometrist
– do not meet accepted standards of ophthalmic practice,
including charges for experimental or investigational
services or supplies
– are received as a result of eye disease, defect, or injury
due to an act of declared or undeclared war
– are for any condition, disease, ailment, or injury arising
out of and in the course of employment compensable
under a workers’ compensation or employers’ liability
law and were ordered before the patient became eligible
for coverage or after coverage ends
– are received free from any governmental agency by
The vision plan
120
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
IF YOU HAVE COVERAGE UNDER MORE THAN
ONEVISIONPLAN
If you or a family member have coverage under the vision
plan and are also covered under another vision plan (for
example, your spouse/partner’s company vision plan),
coordination of benefits may apply. The vision plan has the
right to coordinate with other plans under which you are
covered so the total vision benefits payable will not exceed
the level of benefits otherwise payable under the vision
plan. Under the vision plan, “other plans” refers only to
other plans administered by VSP. There is no coordination-
of-benefits provision with vision coverage providers other
than VSP. Plans referred to as “other plans” are described in
If you have coverage under more than one medical plan in
The medical plan chapter.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your vision premiums to avoid a break
in coverage. These situations occur most commonly if you
are on a leave of absence or if your Walmart paycheck is
not sufficient to pay your full share of the cost of coverage
(such as after a reduction in hours). Depending on your
circumstances, failure to make your premium payments by
the due date may result in an interruption in the payment of
any benefit claims and/or a break in coverage.
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information about
making payments while on a leave of absence, see When
special arrangements are necessary to maintain coverage in
the Eligibility and enrollment chapter.
If you have received covered vision services prior to your
leave, any applicable benefit frequency limitation under the
vision plan (i.e., eyeglass frames every calendar year) will
continue to apply after your return.
When vision coverage ends
Your coverage ends on your last day of employment or
when you are no longer eligible under the terms of the
Plan. Dependent coverage ends when your coverage ends
or when a dependent is no longer an eligible dependent
(as defined in the Eligibility and enrollment chapter).
You and/or your enrolled dependents may be eligible for
continued coverage through the Consolidated Omnibus
Reconciliation Act of 1985, as amended (COBRA). See
the COBRA chapter for information regarding COBRA
continuation coverage.
If you leave the company and
arerehired
If you return to work for the company within 13 weeks,
you will automatically be reenrolled for the same coverage
you had prior to leaving the company (or the most similar
coverage offered under the Plan). If your break is greater
than 30 days but less than 13 weeks, you will have 60 days
after resuming work to drop or otherwise change the
coverage in which you were automatically reenrolled.
If you return to work after 13 weeks, you will be considered
newly eligible and may enroll for coverage under the time
periods and conditions described in the Eligibility and
enrollment chapter.
If you drop coverage and reenroll
If you drop coverage and reenroll within 30 days, you will
automatically be reenrolled for the same coverage you had
(or the most similar coverage offered under the Plan).
If you drop coverage and reenroll after 30 days, you will be
considered newly eligible and may enroll for coverage under
the time periods and conditions described in the Eligibility
and enrollment chapter.
If you have received covered vision services prior to your
absence, any applicable benefit frequency limitation under
the vision plan (i.e., eyeglass frames once every calendar
year) will continue to apply after your return.
IF A DEPENDENT IS DROPPED FROM
COVERAGE ANDREENROLLED
If a dependent child is dropped from coverage and then
determined to be eligible for coverage within 30 days, the
dependent will automatically be reenrolled in the same
coverage you elect for yourself.
If your dependent regains eligibility and is reenrolled after
30 days, they will be treated as a newly eligible dependent.
The associate may enroll them for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.
The vision plan
121

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
COBRA continuation coverage 124
COBRA qualifying events 124
Paying for COBRA coverage 126
How long COBRA coverage may last 127
When COBRA coverage ends 129
COBRA

COBRA
123
COBRA
If you and/or your covered dependents lose medical, dental, or vision coverage because of a
qualifying event, a federal law known as “COBRA” may allow you to continue that coverage for
aset period of time at your own expense.
RESOURCES
Find What You Need Online Other Resources
Contact People Services within 60 calendar
days of a divorce, legal separation, termination
of a relationship with a parner, or ineligibility
of dependents
Call People Services at 800-421-1362 or
provide notification in writing to:
Walmar People Services
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Contact WageWorks, the COBRA
administrator, for questions regarding
eligibility, enrollment, premiums, and
notification of a second qualifying event
Go to
mybenefits.wageworks.com
Call 800-570-1863
What you need to know about COBRA
• “COBRA,” which stands for Consolidated Omnibus Budget Reconciliation Act of 1985, may apply if a “qualifying
event” occurs that would otherwise cause you or a covered dependent to lose medical, dental, or vision coverage.
Qualifyingevents are described in this chapter. The Plan extends COBRA continuation coverage to you and all your
covered dependents.
• For medical, dental, and vision benefits, COBRA continuation coverage can continue up to 18 or 36 months, depending
on the qualifying event. The 18 months can be extended to 29 months under certain circumstances when a disability
isinvolved.
• If you experience a qualifying event and become eligible for COBRA benefits, your Resources for Living benefits
automatically continue for 18 months from the date of the qualifying event (or the maximum duration for which you
would be eligible for COBRA coverage). You do not have to enroll in COBRA coverage to continue your Resources for
Living benefits.
• The Plan contracts with WageWorks, a third-party administrator, to administer COBRA. References to COBRA in this
section are to the Plan’s continuation coverage, which may be more favorable to participants and dependents than the
continuation coverage legally required under COBRA.
• There are strict notification rules and time limits for enrolling in COBRA continuation coverage, as described in this
chapter. Please read this chapter carefully—failure to adhere to these rules can result in the loss of your right to elect
COBRA continuation coverage. If you have any questions or need assistance with enrollment, please call 800-570-1863.
COBRA
124
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
COBRA continuation coverage
If medical, dental, or vision coverage under the Plan ends
for you or your eligible dependents, you and/or your eligible
dependents may be able to continue your coverage under
the Plan’s continuation coverage provisions, which comply
with the Consolidated Omnibus Budget Reconciliation Act
of 1985, as amended (COBRA).
An event that makes you and/or your eligible dependents
eligible for COBRA continuation coverage is called a
“qualifying event,” such as termination of employment or
loss of benefits eligibility. Under COBRA, each person who
would lose coverage after a qualifying event is considered
a “qualified beneficiary.” Each qualified beneficiary has an
independent right to elect COBRA continuation coverage.
You must have had medical, dental, or vision coverage
under the Plan on the day before the date of your
qualifying event to be eligible for COBRA coverage, unless
coverage ended during a leave of absence, as described
on this page. You may choose a lesser coverage level or
select an alternate medical plan, if applicable. COBRA
continuation coverage applies to medical, dental, and vision
coverage; it does not apply to other benefits described in
this Associate Benefits Book.
If you change medical plans when you elect COBRA
coverage, your annual deductible and out-of-pocket
maximum will reset, and you will be responsible for
meetingthe new deductible and out-of-pocket maximum
intheir entirety.
If you have HMO coverage at the time of your qualifying
event and the state where you live has more favorable
coverage continuation rules than federal COBRA, the
HMO generally follows state rules. For eComm PPO Plan
participants, the eComm PPO Plan also follows state rules.
For information on state continuation rights, contact your
HMO provider or the eComm PPO Plan, as applicable.
IF YOU ARE ON LEAVE OF ABSENCE
Generally, if your leave ends and you do not return to work,
you and any eligible dependents who were enrolled in
medical, dental, or vision coverage under the Plan during
your leave will be offered COBRA, which will run from the
date following your employment termination date.
If you and any eligible dependents were enrolled in medical,
dental, or vision coverage under the Plan on the day before
your leave began but you dropped coverage during your
leave or your coverage was canceled due to nonpayment
of premiums during the leave, you will still be offered
COBRA when your employment terminates. If you elect
COBRA coverage, it will run from the date following your
employment termination date. This means that if you or any
eligible dependent elects COBRA at the end of a leave of
absence during which coverage was dropped or canceled,
the elected COBRA coverage will not be effective
retroactive to the date coverage was dropped or canceled,
but will be effective on the date following your employment
termination date.
COBRA qualifying events
You are eligible for COBRA if your medical, dental, or vision
coverage ends because:
• Your employment with Walmart ends for any reason, or
• You are no longer eligible for medical coverage because
the number of hours you regularly work for Walmart
has decreased, making you ineligible for coverage under
thePlan.
Your spouse or partner is eligible for COBRA if coverage for
the spouse or partner ends for any of the following reasons:
• Your employment with Walmart ends for any reason
• Your spouse or partner is no longer eligible for medical,
dental, or vision coverage because the number of hours
you regularly work for Walmart has decreased, making
them ineligible for coverage under the Plan
• You and your spouse divorce or legally separate
• You and your partner no longer meet the definition of
having a “partnership” for purposes of the Plan (refer to
the Eligibility and enrollment chapter for the definition
of “partner”).
• You enroll in Medicare benefits Part D, causing your
medical coverage to terminate (you must contact People
Services by calling 800-421-1362 within 60 days of
enrolling in Medicare Part D), or
• You die.
Your eligible dependent other than a spouse or partner is
eligible for COBRA if coverage for the dependent ends for
any of the following reasons:
• Your employment with Walmart ends for any reason
• Your eligible dependent is no longer eligible for medical,
dental, or vision coverage because the number of hours
you regularly worked for Walmart has decreased, making
them ineligible for coverage under the Plan

COBRA
125
• You enroll in Medicare benefits Part D, causing your
medical coverage to terminate. (You or your eligible
dependent must contact People Services by calling
800-421-1362 within 60 days of enrolling in Medicare
Part D.)
• Your dependent child no longer meets eligibility
requirements (e.g., the end of the month in which a
dependent turns age 26), or
• You die.
NOTIFICATION
In general, Walmart will notify WageWorks, the Plan’s third-
party administrator for COBRA, if you or your dependents
become eligible for COBRA continuation coverage because
of your death, termination of employment, or a reduction in
hours of employment that makes you ineligible for coverage
under the Plan. Walmart will generally make this notification
to the COBRA administrator within 30 days after the
qualifying event.
Under the law, you or your eligible dependent is responsible
for notifying People Services of your divorce, legal
separation, termination of your relationship with a partner,
or a child becoming ineligible due to loss of dependent
status. You must also notify People Services if you enroll
in Medicare Part D. The notification must be made within
60 days after the qualifying event (or the date on which
coverage would end because of the qualifying event, if later).
You or your eligible dependent can provide notice on behalf
of yourself as well as any eligible dependent affected by the
qualifying event. Provide notice of the qualifying event to
People Services by calling 800-421-1362 or writing to:
Walmart People Services
508 SW 8th Street
Bentonville, Arkansas 72716-3500
The notice must include the following information:
• Name and address of the covered associate
• Type of qualifying event
• Date of qualifying event
• Name of dependent losing coverage, and
• Address of the dependent losing coverage (if different
from the covered associate’s address).
If you do not contact People Services within the 60-day
period, you will lose your right to elect COBRA continuation
coverage. To protect your family’s rights, let People
Services know about any changes in addresses of family
members. You should keep a copy of any notices you send to
People Services and/or WageWorks for your records.
Federal law places responsibility upon you
or your eligible dependent to notify People
Services within 60 calendar days after the
later of the date of a divorce, legal separation,
termination of your relationship with a
partner, or a child becoming ineligible due
to loss of dependent status, or the date on
which coverage under the Plan is terminated
as a result of one of these events. If you or
your eligible dependent do not notify People
Services within 60 days, your dependent will
not be eligible for COBRA.
You or your eligible dependent must also
notify the COBRA administrator by phone
or in writing of a second qualifying event or
Social Security disability in order to extend
the period of COBRA coverage. Other forms
of notice will not bind the Plan. If notice is not
provided by phone or in writing of a second
qualifying event or extension request within
60 days from the later of the date of the
second qualifying event or the date on which
you lost (or will lose) coverage as a result of a
second qualifying event, COBRA continuation
rights will expire on the date that your or your
eligible dependent’s initial COBRA coverage
period expires.
COBRA ENROLLMENT
Within 14 days after the COBRA administrator receives
notification that a qualifying event has occurred, the
COBRA administrator, on behalf of the Plan, will send a
COBRA election notice to you and your eligible dependent
at your last known address. The election notice describes
your right to continue medical, dental, or vision coverage
under COBRA. (If you do not receive this notification,
please contact People Services.) To receive COBRA
continuation coverage, you must elect such coverage
through the COBRA administrator within 60 calendar
days from the date you lose coverage or the date of the
election notice, if later. To enroll, you must complete
and mail your COBRA election notice or go online at
mybenefits.wageworks.com. If you elect COBRA, notify
the COBRA administrator of any change of address.
Refer to Paying for COBRA coverage on the next page
for information on making COBRA payments. If you need
assistance, call 800-570-1863.
NOTE: You may be asked to provide documentation of the
qualifying event.

COBRA
126
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
You and each of your eligible dependents have independent
election rights. You may elect COBRA coverage for all
of your family members who lose coverage because of
the qualifying event. A parent or legal guardian may elect
COBRA coverage on behalf of a minor eligible dependents.
A child born to or placed for adoption with you while you
are on COBRA also has COBRA rights.
COBRA is provided subject to the eligibility requirements
for continuation coverage for you and your eligible
dependents under the law and the terms of the Plan. To
the extent permitted by law, the Plan Administrator will
retroactively terminate your COBRA coverage if you are
later determined to be ineligible.
Instead of electing COBRA coverage, there
may be other coverage options for you and
your family through the Health Insurance
Marketplace or Medicaid. You may also be
eligible for a 30-day “special enrollment period”
in another group health plan for which you are
otherwise eligible (such as a plan sponsored by
your spouse’s employer). You may also have the
same special enrollment right at the end of your
COBRA coverage if you take COBRA coverage
for the maximum time available to you. Some
of these options may cost less than COBRA
continuation coverage. You can learn more
about your options at healthcare.gov.
STATUS CHANGE EVENTS WHILE ON COBRA
CONTINUATION COVERAGE
After the COBRA election period, you or your eligible
dependent may not change the elected COBRA coverage
without a status change event outside Annual Enrollment
or a subsequent qualifying event. For information about
status change events, see Status change events in the
Eligibility and enrollment chapter. If a status change
event occurs (such as if a child is born), you must notify
the COBRA administrator within 60 calendar days of the
event. Supporting documentation may be required. You
will have the right to make changes to your coverage
during any Annual Enrollment while you are on COBRA.
Unless otherwise provided in the Plan, if you add a spouse or
partner or other eligible dependent due to a status change
event while on COBRA, each person must individually meet
any applicable benefit waiting period (for example, for
transplant coverage or weight loss surgery) and is subject
to any applicable Plan limitations. If you change medical
plans due to a status change event, your annual deductible
and out-of-pocket maximum will reset, and you will be
responsible for meeting the new deductible and out-of-
pocket maximum in their entirety. If you change from the
Contribution Plan to another plan, your HRA balance under
the Contribution Plan will be forfeited.
If you are covered as a dependent and you experience a
qualifying event that affects your status as a dependent
and makes you eligible for your own continuation
coverage under COBRA, you will receive credit toward
your deductible and out-of-pocket maximum under
the Associates’ Medical Plan for expenses incurred as a
covered dependent, unless you change plan options as
described above. You will also receive credit toward any
waiting periods.
In the event of a status change, you or your eligible
dependent may change benefit coverage to another
benefit tier under the Plan only if the change in coverage is
consistent with the status change event.
If you move to a new location and this affects your medical
coverage (i.e., moving from an HMO area to a non-HMO
area), you will have 60 calendar days from the date you
notify the COBRA administrator of the address change to
select a different plan. If you do not submit your selections
within 60 days, you may automatically be enrolled in a
predetermined plan.
Paying for COBRA coverage
You and/or your eligible dependents are responsible for
both the associate portion of the premium and the portion
previously paid by the company, plus a 2% administrative fee
(50% administrative fee in cases of the 11-month disability
extension, as described later in this chapter). The letter sent
to you and your eligible dependents following notice of a
qualifying event will include the monthly premium cost for
COBRA coverage.
Initial COBRA premium: Your first payment is due 45 days
after you elect COBRA and must cover the cost of COBRA
coverage from the day following the qualifying event
through the end of the month before the month in which
you make your first payment. (For example, assume your
employment terminates on Sept. 30, and you lose coverage
on Sept. 30. You elect COBRA on Nov. 15. Your initial
premium payment should equal the premiums for October
and November and is due on or before Dec. 30, which is the
45th day after the date of your COBRA election. Ongoing
premiums are due the first day of each month, with a
30-day grace period. So your December payment must be
received no later than Dec. 31, the end of the 30-day grace
period for the December coverage period.)
If your initial premium payment is not made in the allowed
time frame, you will not be eligible for COBRA coverage.

COBRA
127
Continuing premiums: Monthly premiums are due on the
first day of each month following the due date of the initial
premium. If you make your payment on or before the first
day of each month, your COBRA coverage under the Plan
will continue for that month without any break.
You are allowed a 30-day grace period from the premium
due date before coverage is canceled. However, if you
make your payment later than the first day of the month,
your coverage will be suspended and any claims incurred,
including pharmacy benefits, will not be paid until coverage
is paid through the current month. If you do not pay this
premium, you will be responsible for claims incurred. If
the 30th day falls on a weekend or holiday, you have until
the first business day following to have your payment
postmarked or paid.
As a courtesy, the COBRA administrator will send you a
COBRA premium payment invoice, unless you make your
payments by Automated Clearing House (ACH) debit,
in which case you will not receive an invoice. Premium
payments are due regardless of your receipt of a payment
invoice. If you pay by mail, attach your payment to the
invoice and mail it to:
WageWorks
P.O. Box 660212
Dallas, Texas 75266-0212
To pay online, log on to mybenefits.wageworks.com. To pay
by phone, call 800-570-1863.
If your COBRA coverage is canceled due to nonpayment of
premiums, your COBRA coverage will end on the last day
for which you paid your full COBRA premium on time, and it
will not be reinstated.
If you do not want to continue coverage, you may cancel
COBRA coverage at any time by ceasing to pay the
premiums. No further action is required.
How long COBRA coverage may last
The maximum duration of your COBRA coverage depends
on the qualifying event making you eligible for COBRA
coverage, as shown in the chart below.
MAXIMUM DURATION OF COBRA COVERAGE
Event Associate Dependents
• Your employment with the company ends
for any reason
• You are no longer eligible for coverage
under the Plan due to a reduction in hours
18 months from the date of the event 18 months from the date of the event
• Your death
• Your marital
(or parnership) status changes
• Dependent(s) no longer meets eligibility
requirements
(e.g., turns age 26)
Not applicable 36 months from the date of the event
You enroll in Medicare less than 18 months
prior to your termination of employment or
reduction in hours
18 months from the date of termination
of employment or reduction in hours
Up to 36 months from the date the
associate enrolled in Medicare
You enroll in Medicare Par D Not applicable 36 months from the date the associate
enrolled in Medicare Par D
Disability extension is obtained 29 months from the date of the original
qualifying event
29 months from the date of the original
qualifying event
Second qualifying event — you must notify
the COBRA administrator within 60 days of
the second qualifying event or the date of
loss of coverage, if later
Not applicable Up to 36 months from the date of the
original qualifying event
COBRA
128
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
IF YOU ARE ENTITLED TO MEDICARE
If you are eligible for Medicare Parts A and/or B and
terminate employment with the company (or lose coverage
under the Plan), be aware that if you do not enroll in Medicare
Parts A and/or B during the Medicare special enrollment
period, you may have to wait until the next Medicare annual
enrollment period to enroll in Medicare Parts A and/or
B and may have to pay a higher Medicare premium when
you do enroll. The eight-month special enrollment period
runs from the date that you are no longer employed by
the company (orlose coverage under the Plan, whichever
occurs first), even if you elect COBRA continuation coverage
(e.g.,following termination of employment). For additional
information, refer to Medicare’s Medicare & You handbook,
published annually. The handbook can be obtained directly
from Medicare by calling 800-633-4227 or from the
Medicare website at medicare.gov.
Entitlement to Medicare means you are eligible for and
enrolled in Medicare. If you become entitled to Medicare
less than 18 months before a qualifying event due to
termination of employment or reduction in hours, your
eligible dependents can elect COBRA for a period of not
more than 36 months from the date you became eligible
for Medicare.
If you are entitled to Medicare prior to your COBRA
election date, you or your eligible dependents must
notify the COBRA administrator at 800-570-1863 of your
Medicare status in order to ensure your maximum coverage
period is properly calculated.
IF YOU OR AN ELIGIBLE DEPENDENT
ISDISABLED
If you’re a qualified beneficiary who has COBRA coverage
because of termination of employment or a reduction in
hours, you and each enrolled member of your family may
be entitled to an extra 11 months of COBRA coverage if
you or other enrolled members of your family become
disabled. (That is, you can get up to a total of 29 months of
COBRA coverage.) The 29-month COBRA coverage period
begins on the date after your termination of employment or
reduction in hours of employment that makes you ineligible
for coverage under the Plan. The disability extension applies
only if all of the following conditions are met:
• The Social Security Administration determines that you or
your eligible dependent is disabled
• The disability exists at any time within the first 60 calendar
days of COBRA coverage and lasts at least until the end of
18-month period of COBRA continuation coverage, and
• You and/or your eligible dependent notifies the COBRA
administrator of the Social Security Administration’s
disability determination by submitting a copy of the Social
Security Administration disability determination Notice
of Award letter to the COBRA administrator within your
initial 18-month COBRA period and within 60 days of the
later of:
– The date of your qualifying event
– The date of your Social Security Administration disability
determination Notice of Award, or
– The date on which you and/or your eligible dependent
loses coverage under the Plan as a result of the
qualifying event.
In the absence of an official Notice of Award from Social
Security, the Plan may accept other correspondence from
the Social Security Administration if that correspondence
explicitly includes all information the Plan needs to grant
the extension and is submitted to the COBRA administrator
within the time frames listed above.
If you and/or your eligible dependent qualify for the
disability extension, a new invoice will be mailed to you
and/or your eligible dependent before the end of the initial
18-month COBRA coverage period, unless you make your
payments by Automated Clearing House (ACH) debit, in
which case you will not receive an invoice. Contact the
COBRA administrator for details about paying premiums
during a disability extension.
The COBRA premium for the 19th through the 29th month
of COBRA coverage generally is the amount you were
paying before the qualifying event, plus the amount the
company was paying, plus a 50% administrative fee, or 150%
of the full premium amount.
However, if the disability extension applies, but the disabled
qualified beneficiary family member is not enrolled in
COBRA coverage, the COBRA premium for the covered
family members for the extended period is limited to 102%
of the full premium amount. You or your eligible dependent
must notify the COBRA administrator no later than 30 days
after the Social Security Administration determines that
you or your eligible dependent is no longer disabled.
IF YOU HAVE A SECOND QUALIFYING EVENT
WHILE ON COBRA
While you (the associate) cannot receive an extension of
COBRA coverage due to a second qualifying event, your
eligible dependent who has COBRA coverage due to your
termination of employment or reduction in hours may
receive COBRA coverage for up to a total of 36 months if a

COBRA
129
second qualifying event occurs during the original 18-month
continuation coverage period (or during the 29-month
coverage period, in the event of a disability extension).
The following can be second qualifying events:
• Your death
• Your divorce, legal separation, or termination of a
relationship with a partner
• Your child is no longer eligible for medical, dental, or vision
coverage (e.g., a dependent turns age 26), or
• Your enrollment in Medicare Part D.
If a second qualifying event occurs while your eligible
dependent has COBRA coverage, their COBRA coverage
may last up to 36 months from the date of the first
qualifying event that made you (the associate) eligible for
COBRA coverage.
To receive the extension of the COBRA
coverage period, you or your eligible
dependents must notify the COBRA
administrator of the second qualifying event
within 60 calendar days of the date of the
event or loss of coverage following the event,
if later. If the COBRA administrator is not
notified of the second qualifying event during
the 60-day period, your eligible dependents
cannot get the COBRA coverage extension
and the coverage will be terminated as of the
date your initial COBRA period expired.
When COBRA coverage ends
COBRA coverage usually ends after the 18-month,
29-month, or 36-month maximum COBRA coverage
period. See How long COBRA coverage may last in this
chapter to find out which maximum COBRA coverage
period applies to you.
COBRA coverage may be terminated before the end of the
18th, 29th, or 36th month if:
• The company no longer provides medical, dental, or vision
coverage to any associates
• After the initial 45-day payment period you do not make a
COBRA payment within 30 calendar days of the due date
(if the 30th day falls on a weekend or non-postal delivery
day, you have until the next business day to have your
payment postmarked or paid)
• You or your eligible dependent becomes covered by
another group health, dental, or vision plan after electing
COBRA coverage
• During a disability extension period, the disabled
qualified beneficiary is determined by the Social Security
Administration to be no longer disabled (COBRA coverage
for all qualified beneficiaries, not just the disabled qualified
beneficiary, terminates as of the later of (a) the first
day of the month that is more than 30 days after a final
determination by the Social Security Administration that
the qualified beneficiary is no longer disabled, or (b) the
end of the coverage period that applies without regard to
the disability extension), or
• You or your eligible dependent submits a fraudulent claim
or fraudulent information to the Plan.
FILING AN APPEAL
You have the right to appeal an enrollment or eligibility
status decision related to your COBRA coverage. See
Appealing an enrollment or eligibility status decision in the
Claims and appeals chapter for more information.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Using Resources for Living (RFL) 132
RFL counseling services 132
RFL legal and financial services 132
RFL daily life assistance 132
When RFL benefits end 133
Filing a claim for RFL benefits 133
Resources for Living
®

Resources for Living®
131
Resources for Living®
Resources for Living (RFL) gives you confidential counseling and well-being information. It’s
available at no cost to you and your family members from your date of hire. Call a professional
counselor anytime for help with stress management, family relationships, career issues, and other
daily challenges. RFL also has lots of information and help with childcare, eldercare, education,
finances, wellness, and more.
RESOURCES
Find What You Need Online Other Resources
Speak with a counselor or work-life specialist
to identify resources and solutions for
everyday needs
Call 800-825-3555
Access aricles, tools, and resources across a
wide range of topics
Go to One.Walmar.com or rl.com:
User ID: Walmar
Password: Associate
Access monthly healthy living tips and
webinars on a variety of topics
Go to One.Walmar.com or rl.com:
User ID: Walmar
Password: Associate
What you need to know about Resources for Living
• RFL is available 24 hours a day, seven days a week, 365 days a year.
• You and your household members can find counseling, information, and work-life assistance.
• There is no cost to you for RFL benefits. You are automatically enrolled in RFL as of your date of hire.
Resources for Living®
132
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Using Resources for Living (RFL)
If you are a U.S. associate, you, your household family
members, and your benefit-eligible dependents are
automatically enrolled in RFL as of your first day of
employment. You can call RFL any time at 800-825-3555
orlog into rfl.com to find tools for:
• Stress management
• Budgeting and saving money
• Legal assistance
• Relationships at home and in the workplace
• Emotional and physical well-being
• Family life and more
RFL provides access to services and support by telephone,
televideo, face-to-face counseling, videos, webinars, web-
based articles, and through a resource team that can help
support your everyday needs and well-being.
RFL counseling services
Whether you need help working through an issue or just
someone to talk to, RFL offers you support. You can call and
get help with:
• Managing stress
• Coping with depression, anxiety, or substance misuse
• Building healthy relationships with family, friends,
andco-workers
• Balancing the demands of work and home life
• Working through emotionally difficult situations
You or your eligible family members can talk to an RFL
counselor by telephone, televideo, or face-to-face. Just call
RFL toll-free at 800-825-3555 for support. If your situation
calls for face-to-face behavioral counseling, you can receive
up to three sessions per issue per year, at no cost.
RFL legal and financial services
RFL gives you access to legal and financial experts. Whether
you’re creating a budget or a will, RFL can help. RFL’s
specialists can help you:
• Meet your financial goals and save for the future
• Explore your options related to legal issues
• Create a personal budget
• Make your money go further
• Pay down debt
• Recover from identify theft, and more
You can receive a half-hour consultation for each legal or
financial issue or a one-hour consultation for each identity-
theft issue, at no cost to you. Note that this service does not
provide assistance in situations involving employment law.
RFL daily life assistance
You can reach out to RFL for help in meeting the demands
of work and home life. Call for help with everyday needs
such as:
• Care for your child or an older adult
• Military resources
• Pet care
• Adoption resources
• Home repair services
• Support groups
• Educational options and resources for children and adults
• Accessing tools to support your well-being, including
healthy eating, exercise, improved sleep, and stress
management
RFL’s work-life consultants can help you find options for
meeting your needs and research details like cost, services,
and availability.
Resources for Living®
133
CALLING RFL
Call 800-825-3555 for personalized support at any
time. Services are available in English and Spanish (other
languages available upon request). Calls are confidential,
except as required by law.
RFL ON THE WEB
Visit rfl.com for articles, webinars, tools, and resources on
a variety of topics to help you live well. To log on to rfl.com,
enter the following:
User ID: Walmart
Password: Associate
You can also access rfl.com by clicking on the single sign-on
link found on the RFL page of One.Walmart.com.
When RFL benefits end
If you experience a qualifying event and become eligible
for COBRA benefits, your Resources for Living benefits
automatically continue for 18 months from the date of the
qualifying event (or the maximum duration for which you
would be eligible for COBRA coverage). You do not have to
enroll in COBRA coverage to continue your Resources for
Living benefits.
Filing a claim for RFL benefits
You do not have to file a claim for RFL benefits. You may
access the RFL website or contact RFL by phone at any
time. However, if you have a question about your benefits,
or disagree with the benefits provided, you may contact
People Services at 800-421-1362 or file a claim by writing to
the following address:
People Services
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Claims and appeals are determined under the time frames
and requirements set out in the procedures for filing a
claim for medical benefits, as described in the Claims and
appeals chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Critical illness insurance 136
Critical illness benefits 136
When your critical illness insurance coverage begins 137
Naming a beneficiary 137
Filing a claim 138
When benefits are not paid 138
Break in coverage 138
When coverage ends 139
If you leave the company andarerehired 139
If you drop coverage and reenroll 139
This information is intended to be a summary of your benefits and may not include all policy provisions.
If there is a discrepancy between this document and the policy issued by Allstate Benefits regarding the
calculation of benefits and limitations under the policy, the terms of the policy will govern. You may obtain a
copy of this policy by contacting the Plan. Allstate Benefits is the marketing name used by American Heritage
Life Insurance Company, the underwriting company and subsidiary of The Allstate Corporation.
Critical illness
insurance

Critical illness insurance
135
Critical illness insurance
If you and your dependents sign up for critical illness insurance, you’ll be eligible for a direct lump-
sum cash benefit to help pay for expenses related to covered critical illnesses.
RESOURCES
Find What You Need Online Other Resources
Get detailed information Go to One.Walmar.com or
AllstateBenefits.com/Walmar
Call Allstate Benefits at 800-514-9525
What you need to know about critical illness insurance
• You may purchase critical illness insurance to assist you and your family in the event a covered individual is diagnosed
with certain serious illnesses.
• You may elect coverage amounts of $5,000, $10,000, $15,000, or $20,000.
• If a covered individual is diagnosed with a covered condition, critical illness insurance pays a percentage of the
coverage amount in a lump sum, based on the nature of the condition.
• Proof of Good Health is not required for any level of coverage.
• The Certificate of Insurance available online at One.Walmart.com or AllstateBenefits.com/Walmart provides detailed
information about critical illness insurance, in addition to the highlights available in this chapter.
Critical illness insurance
136
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Critical illness insurance
Critical illness insurance provides a direct benefit if you
or any covered dependents are diagnosed with a covered
illness or disease. The policy pays benefits regardless of,
and in addition to, any other insurance you may have.
Coverage is available in $5,000 increments up to a maximum
of $20,000 with no Proof of Good Health required.
Critical illness insurance is available to you if you are an
hourly or management associate. Coverage is also available
to your dependents, with the exception of spouses/partners
of part-time associates, temporary associates, and part-time
truck drivers.
CHOOSING A COVERAGE LEVEL
When you enroll for critical illness insurance, you also
select the eligible family members you wish to cover:
• Associate only
• Associate + spouse/partner (except for part-time
hourlyassociates, temporary associates, and part-time
truck drivers)
• Associate + child(ren), or
• Associate + family (except for part-time hourly associates,
temporary associates, and part-time truck drivers).
For information on eligibility and when you can enroll, see
the Eligibility and enrollment chapter.
The cost for coverage is based on the coverage amounts
you choose, the eligible dependents you choose to cover,
your age, and whether you (and/or your covered spouse/
partner) are eligible for tobacco-free rates.
If you have associate-only or associate + spouse/partner
coverage and you (or your spouse/partner) give birth to
a child, your newborn child will be automatically covered
for 60 days after birth. You must change your election
to associate + child(ren) or associate + family if you wish
to continue covering your child after 60 days. See the
Eligibility and enrollment chapter for information on when
and how you may change your election.
Critical illness benefits
Benefits are payable if you are diagnosed with one of the
conditions listed below. Coverage must be effective before
the date of diagnosis for an illness or disease to be covered
under the policy.
The following benefits are payable at 100% of the coverage
amount you elect:
• Invasive cancer
• Alzheimer’s disease (requires loss of three activities of daily
living [ADLs])
• Coronary artery bypass surgery
• End-stage renal failure
• Heart attack
• Stroke
• Parkinson’s disease (requires loss of two ADLs)
• Complete loss of hearing (due to illness)
• Loss of sight in one eye or both eyes (due to illness)
• Quadriplegia (due to illness)
• Paraplegia (due to illness)
• Loss of at least one foot, hand, arm, or leg (due to illness)
• Benign brain tumor
• Coma (lasting seven days) due to illness, or
• Major organ transplant (see note below).
If you undergo a major organ transplant, as specified in the
major organ transplant rider found in the Certificate of
Insurance, you will receive 100% of the coverage amount
you elect. If you are enrolled in the Saver Plan, you are not
eligible for the major organ transplant rider included in
critical illness insurance.
The following benefits are payable at less than 100% of the
coverage amount you elect:
• Carcinoma in situ: 25% of coverage amount
• Complete loss of one or more fingers and/or one or more
toes (due to illness): 25% of coverage amount
• Transient ischemic attacks (TIAs): 25% of coverage amount
• Aneurysm (ruptured or dissecting): 25% of coverage amount
• Specified diseases: 50% of coverage amount
– Addison’s disease
– Amyotrophic lateral sclerosis (Lou Gehrig’s disease)
– Cerebrospinal meningitis (bacterial)
– Cerebral palsy
– Cystic fibrosis
– Diphtheria
– Encephalitis
– Huntington’s chorea
– Legionnaires’ disease (confirmation by culture or sputum)
– Malaria
– Multiple sclerosis
– Muscular dystrophy
– Myasthenia gravis
– Necrotizing fasciitis
– Osteomyelitis
– Poliomyelitis
– Rabies
– Sickle cell anemia
– Systemic lupus
– Systemic sclerosis (scleroderma)
– Tetanus, or
– Tuberculosis.
Critical illness insurance
137
The benefits described above generally will be paid only
once, upon the initial occurrence of each critical illness
identified above (or, in the instance of invasive cancer,
for the particular form of cancer). However, if you have a
recurrence of heart attack, stroke, coronary artery bypass
surgery, invasive cancer, carcinoma in situ, rabies, ruptured
or dissecting aneurysm, benign brain tumor, or coma, the
plan will pay a recurrence benefit of 100% of the coverage
amount, provided the recurrence occurs 180 days after the
prior occurrence (or, in the case of a recurrence of the same
cancer, provided you were symptom-free and treatment-
free during the 180 days after the prior occurrence).
Other benefits payable include:
• Ambulance: $250 for ground ambulance or $2,000 for
air ambulance if a covered person requires ambulance
transportation to a hospital or emergency center due to a
covered illness.
• Post-traumatic stress disorder (PTSD): $100 for each day
a covered person receives counseling for PTSD; payable
once per day per covered person and limited to six days
per coverage year
• Skin cancer benefit: $500 upon positive diagnosis of
skin cancer (basal cell carcinoma and squamous cell
carcinoma) by a licensed Doctor of Medicine certified
by the American Board of Pathology to practice
pathological anatomy, or an osteopathic pathologist,
based on microscopic examination of skin biopsy samples.
This benefit is not paid for malignant melanoma (which is
covered under the invasive cancer benefit). It also does
not include any conditions which may be considered
precancerous, such as: leukoplakia; actinic keratosis;
carcinoid; hyperplasia; polycythemia; nonmalignant
melanoma; moles; or similar diseases or lesions. Payable
only once per covered person each calendar year.
• National Cancer Institute (NCI) evaluation and Walmart
Centers of Excellence evaluation: when evaluated for
determining the appropriate treatment of a previously
diagnosed covered illness, $500 for evaluation; $250 for
transportation and lodging if the center is more than
100 miles from your home. Payable once for each initial
occurrence or recurrence of a covered illness.
• Lodging benefit: $60 per day when you or a covered
family member receive treatment for a covered illness on
an outpatient basis at a treatment facility more than 100
miles from your or your covered family member’s home.
This benefit is limited to 60 days per calendar year and
is not payable for lodging occurring more than 24 hours
prior to treatment or for lodging occurring more than 24
hours following treatment.
• Transportation benefit: $0.50 per mile for personal
vehicle, up to $1,500, or up to $1,500 round-trip
transportation for coach fare on a common carrier.
Transportation must be required for treatment of
a covered critical illness at a hospital (inpatient or
outpatient), radiation therapy center, chemotherapy or
oncology clinic, or any other specialized freestanding
treatment facility. If the treatment is for a covered child
and common carrier travel is necessary, the benefit will
be paid for up to two adults to accompany the child. This
benefit will not be paid if the covered person lives within
100 miles of the treatment facility.
Your Certificate of Insurance will contain complete
information on the benefits payable. To obtain a copy, visit
One.Walmart.com or AllstateBenefits.com/Walmart. You
can also call Allstate Benefits at 800-514-9525 for a copy.
When your critical illness insurance
coverage begins
If you enroll during Annual Enrollment, your coverage
becomes effective on January 1 of the next year.
If you enroll outside of Annual Enrollment, your coverage
becomes effective on the date of your status change event
or the end of your eligibility waiting period, whichever is
later. No benefit is payable for any disease diagnosed before
your effective date of coverage. If you should die before
your effective date, no critical illness insurance benefit will
be paid to your beneficiary(ies).
Your critical illness insurance begins whether or not you are
actively at work, as long as you have reported for your first
day of work and enrolled for the benefit. See the Eligibility
and enrollment chapter for details.
Naming a beneficiary
If you die while covered under critical illness insurance, your
beneficiary(ies) will receive any benefits due at the time of
your death.
You must name a beneficiary(ies) to receive your critical
illness insurance benefit if you die. Do this by going to
One.Walmart.com or Workday for Jet associates. Note that
only beneficiary designations made online are accepted.
You can name anyone you wish. If the beneficiary(ies) you
list with Walmart differs from the beneficiary(ies) named in
your will, the list that Walmart has prevails.
The following information is needed for each beneficiary
you name:
• Name
• Current address and phone number
• Relationship to you
• Social Security number
• Date of birth, and
• The percentage you wish to designate per beneficiary,
upto 100%.
If two or more beneficiaries are designated and their
shares are not specified, they will share the insurance
benefit equally. If a named beneficiary dies before you,

Critical illness insurance
138
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
thatbeneficiary’s interest will end, and will be shared
equally by any remaining beneficiaries unless your
beneficiary form states otherwise.
You can name a minor as a beneficiary; however, Allstate
Benefits may not be legally permitted to pay the minor
untilthe minor reaches legal age. You may want to consult
an attorney or an estate planner before naming a minor as
abeneficiary.
You (the associate) are automatically assigned as the primary
beneficiary of your dependent’s critical illness coverage. If
you and your dependent die at the same time, benefits will
be paid to your dependent’s estate or at Allstate Benefits’
option to a surviving relative of the dependent.
CHANGING YOUR BENEFICIARY
You can change your beneficiary(ies) at any time on
One.Walmart.com or Workday for Jet associates. Any
change in beneficiary must be completed and submitted to
Walmart before your death and can be submitted only by
you, the covered associate.
IF YOU DO NOT NAME A BENEFICIARY
If no beneficiary is named or there is no surviving
beneficiary at the time of your death, payment will be made
to your surviving family member(s) in the following order:
1. Your spouse/partner; if not surviving, then
2. Your children, in equal shares; if not surviving, then
3. Your parents, in equal shares; if not surviving, then
4. Your siblings, in equal shares; if not surviving, then
5. Your estate.
Be sure to keep your beneficiary information
up to date. Proceeds go to whoever is listed
on your beneficiary form with Walmart,
regardless of your current relationship with
that person, unless state law says otherwise.
You can change your beneficiary(ies) at any
timeon One.Walmart.com or Workday for
Jetassociates.
Filing a claim
Within 60 days of the occurrence or commencement of any
covered critical illness, or as soon as reasonably possible,
send a notice of claim to:
Allstate Benefits
Attn: Walmart Claims Unit
P.O. Box 41488
Jacksonville, Florida 32203-1488
You may also provide notice of claim as follows:
Online: AllstateBenefits.com/mybenefits
By phone: 800-514-9525
By fax: 877-423-8804
Be sure to provide the following information for the
covered person:
• Name
• Social Security number, and
• Date the covered illness began.
You may request a claim form from Allstate Benefits or
visit One.Walmart.com, Workday for Jet associates, or
AllstateBenefits.com/Walmart to obtain a copy. If you do
not receive a claim form within 15 days of your request,
you may send a notice of the claim to Allstate Benefits by
providing Allstate Benefits with a statement of the nature
and extent of the loss.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter.
Youor your beneficiary has the right to appeal a claim
denial. See the Claims and appeals chapter for details.
When benefits are not paid
This policy does not pay benefits for any critical illness due
to or resulting directly or indirectly from:
• Any act of war, whether or not declared, or participation in
a riot, insurrection, or rebellion
• Intentionally self-inflicted injuries
• Engaging in an illegal occupation or committing or
attempting to commit a felony
• Attempted suicide, while sane or insane
• Being under the influence of narcotics or any other
controlled chemical substance, unless administered upon
the advice of a physician
• Participation in any form of aeronautics, except as a
fare-paying passenger in a licensed aircraft provided
by a common carrier and operating between definitely
established airports, or
• Alcohol abuse or alcoholism, drug addiction, or
dependence upon any controlled substance.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your critical illness insurance premiums
to avoid a break in coverage. These situations occur most
commonly if you are on a leave of absence or if your Walmart
paycheck is not sufficient to pay your full share of the cost
of coverage (such as after a reduction in hours). Depending
on your circumstances, failure to make your premium
payments by the due date may result in an interruption in the
payment of any benefit claims and/or a break in coverage.
Critical illness insurance
139
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information
about making payments while on a leave of absence, see
When special arrangements are necessary to maintain
coverage in the Eligibility and enrollment chapter.
When coverage ends
Your critical illness insurance coverage ends on the earliest
of the following:
• At termination of your employment
• Upon failure to pay your premiums
• On your date of death
• On the last day of an approved leave of absence (unless
you return to work), or
• When the benefit is no longer offered by the company.
Critical illness insurance coverage for your spouse/
partnerends:
• On the date your insurance coverage ends
• On the last day of the pay period when your job status
changes to part-time, temporary, or part-time truck
driver
• On the date your spouse/partner loses eligibility, such
as upon a valid decree of divorce or termination of
partnership, or
• On your spouse/partner’s death.
Critical illness insurance coverage for your dependent
child(ren) ends:
• On the date your insurance coverage ends
• On the date your dependent child loses eligibility, or
• On your dependent child’s death.
CONTINUATION OF COVERAGE
ATTERMINATION
If your coverage under critical illness insurance terminates as
described earlier in this section, you may continue to receive
critical illness insurance directly from Allstate Benefits
through portability coverage. To receive portability coverage,
you must notify Allstate Benefits that you wish to continue
coverage and send the first premium within 60 days of the
date your coverage under critical illness insurance terminates.
The premiums for portability coverage are due in advance
of each month’s coverage, on the first day of the calendar
month. The premiums are set at the same rate in effect
under critical illness insurance for active associates with the
same coverage.
For more information, please contact Allstate Benefits at
800-514-9525.
WHEN YOUR DEPENDENT BECOMES INELIGIBLE
Any eligible dependent covered under critical illness insurance
at the time such coverage terminates may also receive
portability coverage, under the terms described above.
Contact Allstate Benefits at 800-514-9525 for information.
If you leave the company
andarerehired
If you leave the company and then return to work within 13
weeks, you will automatically be reenrolled for the same
coverage plan you had prior to leaving the company (or the
most similar coverage offered under the Plan).
If your break is greater than 30 days but less than 13
weeks, you will have 60 days after resuming work to drop
or otherwise change the coverage in which you were
automatically reenrolled.
If you return to work after 13 weeks, you will be considered
newly eligible and may enroll for coverage under the time
periods and conditions described in the Eligibility and
enrollment chapter.
If you drop coverage and reenroll
If you drop coverage and reenroll within 30 days, you will
automatically be reenrolled for the same coverage you had
prior to dropping coverage (or the most similar coverage
offered under the Plan).
If you drop coverage and reenroll after 30 days, you will be
considered newly eligible and may enroll for coverage under
the time periods and conditions described in the Eligibility
and enrollment chapter.
IF A DEPENDENT IS DROPPED FROM
COVERAGE AND REENROLLED
If your dependent child is dropped from coverage and then
determined to be eligible for coverage within 30 days, the
dependent will automatically be reenrolled in the same
coverage you elect for yourself.
If your dependent regains eligibility and is reenrolled after
30 days, they will be treated as a newly eligible dependent.
The associate may enroll them for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Accident insurance 142
Accident insurance benefits 142
When your accident insurance coverage begins 145
Naming a beneficiary 145
Filing a claim 146
When benefits are not paid 146
Break in coverage 146
When coverage ends 147
If you leave the company and arerehired 147
If you drop coverage and reenroll 147
This information is intended to be a summary of your benefits and may not include all policy provisions.
If there is a discrepancy between this document and the policy issued by Allstate Benefits regarding the
calculation of benefits and limitations under the policy, the terms of the policy will govern. You may obtain a
copy of this policy by contacting the Plan. Allstate Benefits is the marketing name used by American Heritage
Life Insurance Company, the underwriting company and subsidiary of The Allstate Corporation.
Accident insurance

Accident insurance
141
Accident insurance
This insurance helps you if you’re in an accident away from work. If the accident is covered, this
can help you pay for things like immediate care treatment, hospitalization, physical therapy,
transporation, and lodging. Benefits are paid directly to you unless you want to have them paid to
the provider.
RESOURCES
Find What You Need Online Other Resources
Get detailed information Go to One.Walmar.com or
AllstateBenefits.com/Walmar
Call Allstate Benefits at 800-514-9525
What you need to know about accident insurance
• You may purchase accident insurance to assist you and your family if a covered individual has a covered accident
that requires medical care.
• Accident insurance pays a set benefit in a lump sum, based on the nature of the accident and the care required.
• Proof of Good Health is not required for any level of coverage.
• Coverage is provided through Allstate Benefits. The Certificate of Insurance available online at One.Walmart.com
or AllstateBenefits.com/Walmart provides detailed information about accident insurance, in addition to the
highlights available in this chapter.
Accident insurance
142
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Accident insurance
Accident insurance provides benefits to you if you or any
covered dependent receives covered treatment related to
an off-the-job accident. The benefits under this policy are
not reduced by any other benefits you may receive.
Accident insurance is available to you if you are an hourly or
management associate. Coverage is also available to your
dependents, with the exception of spouses/partners of
part-time associates, temporary associates, and part-time
truck drivers.
CHOOSING A COVERAGE LEVEL
When you enroll for accident insurance, you also select
theeligible family members you wish to cover:
• Associate only
• Associate + spouse/partner (except for part-time
hourlyassociates, temporary associates, and part-time
truck drivers)
• Associate + child(ren), or
• Associate + family (except for part-time hourly associates,
temporary associates, and part-time truck drivers).
For information on eligibility and when you can enroll,
seethe Eligibility and enrollment chapter.
The cost for coverage is based on the eligible dependents
you choose to cover.
If you have associate-only or associate + spouse/partner
coverage and you (or your spouse/partner) give birth to
a child, your newborn child will be automatically covered
for 60 days after birth. You must change your election
to associate + child(ren) or associate + family if you wish
to continue covering your child after 60 days. See the
Eligibility and enrollment chapter for information on when
and how you may change your election.
Accident insurance benefits
Accident insurance provides benefits if you or a covered
dependent seeks medical treatment or is hospitalized as a
result of a covered accident that happens off the job. An
accident generally is a covered accident if it occurs while
you (or your covered family member) are not working at
any job for pay or benefits and is the result of a sudden,
unforeseen, and unexpected event that results in injury
and occurs without the injured person’s intent. Certain
accidents are not covered. See When benefits are not paid
later in this chapter for more information.
For a complete list of benefits and the amounts payable,
visit One.Walmart.com or AllstateBenefits.com/Walmart.
Accident insurance will pay a benefit if you receive particular
services in connection with a covered off-the-job accident.
See the chart on the next page for details regarding services
for which accident insurance pays a benefit.

Accident insurance
143
SERVICE BENEFIT AMOUNT LIMITATIONS
Immediate care (physician fees,
x-rays, and emergency room)
$120 per covered accident Services must be received within 30 days of
covered accident.
Follow-up treatment (not
covered under physical
therapy)
$50 per follow-up treatment after
emergency treatment paid under
immediate care, up to 6 treatments
Follow-up visits must occur within 30 days of the
initial covered treatment. Benefit paid for only one
treatment per day.
Physical therapy (not covered
by follow-up treatment)
$50 per day, up to 10 days Therapy must begin within 30 days of covered
accident or discharge from hospital and be received
within six months of covered accident or discharge.
Initial hospitalization $1,500 payable the first time a covered
person is hospitalized for at least 24
hours; $2,250 if admitted directly to a
hospital intensive care unit
Hospitalization must begin within 30 days of
the covered accident. Payable only once per
hospitalization per calendar year.
Hospital confinement Daily benefit of $300 for a continuous
hospital confinement for at least 18 hours,
up to 365 days
Hospitalization must begin within 30 days of
covered accident. Not payable on same day
rehabilitation benefit is paid.
Intensive care unit (ICU)
confinement
$900 per day, up to 15 days Confinement must begin within 30 days of
covered accident.
Step-down ICU confinement $200 per day, up to 15 days Must be confined to step-down intensive care unit
for at least 18 hours.
Rehabilitation unit confinement
(after hospitalization)
$100 per day confined to rehabilitation
unit
Payable up to 30 days per continuous period of
confinement; maximum of 60 days. Not payable for
days in which hospital confinement benefit is paid.
Major diagnostic exams $400 for CT scan, MRI, or EEG One payment per calendar year.
Appliance to aid personal
locomotion or mobility
$200 for crutches, wheelchair, leg brace,
back brace, walker, and CAM boot walker
Payable once per covered accident.
Prosthesis $1,000 Payable once per covered accident. Not payable
for hearing aids, wigs, or dental aids (including
false teeth).
Ambulance $250 for ground ambulance or $2,000 for
air ambulance
Transporation by ambulance must occur within 72
hours of covered accident.
Blood, plasma, and/or platelets $100 Not payable for immunoglobulins. Payable once
per covered accident.
Transporation for treatment at
a non-local hospital
$400 per round trip; additional $400 if
dependent child is receiving treatment
Payable for up to three roundtrips per year. Not
payable for ambulance transporation.
Family lodging for confinement
at a non-local hospital
$100 per night for an immediate family
member of covered person, up to 30 days
Payable only during the days the covered person is
confined to the non-local hospital.

Accident insurance
144
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Accident insurance also pays a benefit if the following specific injuries are sustained in a covered accident:
INJURY BENEFIT AMOUNT LIMITATIONS
Dislocation $188–$3,750, depending on joint dislocated Payable for up to two dislocations per accident.
Cerain treatments may result in a lesser benefit.
Burns $100–$10,000 depending on degree of
burn and size of affected area
If proof of loss does not specify size of burn, the
lowest benefit amount will be paid. Treatment by a
physician must occur within 72 hours of the covered
accident.
Skin grafts 50% of benefit amount under burns Paid in addition to the burn benefit.
Eye injury $250 for surgical repair; $50 for removal of
foreign body
For services perormed by a physician.
Lacerations $25–$400, depending on the size of the
laceration
If proof of loss does not specify size of laceration, the
lowest benefit amount will be paid. Treatment must
occur within 72 hours of the covered accident.
Fractures $375–$3,750, depending on location
of fracture; 25% for chip fractures or
other fractures not corrected by open or
closedrepair
For fractures corrected by open or closed repair as a
result of covered accident. Payable for no more than
two fractures per covered accident.
Concussions (brain) $50 As a result of covered accident.
Emergency dental services $50 for broken teeth extracted; $150 for
broken teeth repaired with crowns
Payable once per covered accident.
Coma $10,000 Coma must persist at least seven days. Medically
induced comas are excluded.
Surgical procedures $350–$1,400, depending on
surgicalprocedure
Must be perormed within one year of covered
accident. Miscellaneous surgery is payable once per
24 hours even though more than one surgery or
procedure may be perormed.
Your Certificate of Insurance will contain complete information on the benefits payable. To obtain a copy, visit One.Walmart.com
or AllstateBenefits.com/Walmart. You can also call Allstate Benefits at 800-514-9525 for a copy, whichwill be provided at no
cost to you.

Accident insurance
145
When your accident insurance
coverage begins
If you enroll during Annual Enrollment, your coverage
becomes effective on January 1 of the next Plan year.
If you enroll outside of Annual Enrollment, your coverage
becomes effective on the date of your status change
event or the end of your eligibility waiting period,
whichever is later. If you should die before your effective
date, no accident insurance benefit will be paid to your
beneficiary(ies).
Your accident insurance begins whether or not you are
actively at work, as long as you have reported for your first
day of work and enrolled for the benefit. See the Eligibility
and enrollment chapter for details.
Naming a beneficiary
If you die while covered under accident insurance, your
beneficiary(ies) will receive any benefits due at the time of
your death.
You must name a beneficiary(ies) to receive your accident
insurance benefit if you die. You may do this by going to
One.Walmart.com or Workday for Jet associates. Note that
only beneficiary designations made online are accepted.
You can name anyone you wish. If the beneficiary(ies) you
list with Walmart differs from the beneficiary(ies) named in
your will, the list that Walmart has prevails.
The following information is needed for each beneficiary:
• Name
• Current address and phone number
• Relationship to you
• Social Security number
• Date of birth, and
• The percentage you wish to designate per beneficiary, up
to 100%.
If two or more beneficiaries are designated and their
shares are not specified, they will share the insurance
benefit equally. If a named beneficiary dies before you, that
beneficiary’s interest will end, and will be shared equally by
any remaining beneficiaries unless your beneficiary form
states otherwise.
You can name a minor as a beneficiary; however, Allstate
Benefits may not be legally permitted to pay the minor
until the minor reaches legal age. You may want to consult
an attorney or an estate planner before naming a minor
asabeneficiary.
Be sure to keep your beneficiary information up to date.
Proceeds go to whoever is listed on your beneficiary form
on file with Walmart, regardless of your current relationship
with that person, unless state law requires otherwise.
You (the associate) are automatically assigned as the
primary beneficiary of your dependent’s accident coverage.
If you and your dependent die at the same time, benefits
will be paid to your dependent’s estate or at Allstate
Benefits’ option to a surviving relative of the dependent.
CHANGING YOUR BENEFICIARY
You can change your beneficiary(ies) at any time on
One.Walmart.com or Workday for Jet associates. Any
change in beneficiary must be completed and submitted to
Walmart before your death and can be submitted only by
you, the covered associate.
IF YOU DO NOT NAME A BENEFICIARY
If no beneficiary is named or there is no surviving
beneficiary at the time of your death, payment will be made
to your surviving family member(s) in the following order:
1. Your spouse/partner; if not surviving, then
2. Children, in equal shares; if not surviving, then
3. Parents, in equal shares; if not surviving, then
4. Siblings, in equal shares; if not surviving, then
5. Your estate.
Be sure to keep your beneficiary information
up to date. Proceeds go to whoever is listed
on your beneficiary form with Walmart,
regardless of your current relationship with
that person, unless state law says otherwise.
You can change your beneficiary(ies) at any
timeon One.Walmart.com or Workday for
Jetassociates.
Accident insurance
146
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Filing a claim
Within 60 days of the occurrence or commencement of any
covered accident, or as soon as reasonably possible, send a
notice of claim to:
Allstate Benefits
Attn. Walmart Claims Unit
P.O. Box 41488
Jacksonville, Florida 32203-1488
You may also provide notice of claim as follows:
Online: AllstateBenefits.com/mybenefits
By phone: 800-514-9525
By fax: 877-423-8804
Provide the following information for the covered person:
• Name
• Social Security number, and
• Date the covered accident occurred.
You may request a claim form from Allstate Benefits or
visit One.Walmart.com or AllstateBenefits.com/Walmart
to obtain a copy. If you do not receive a claim form within
15 days of your request, you may send a notice of the claim
to Allstate Benefits by providing Allstate Benefits with a
statement of the nature and extent of the loss.
You will be required to provide written proof of your claim
to Allstate. Generally, you should provide written proof
related to your claim within 90 days of the service or loss,
or as soon as reasonably possible after the loss if it is not
possible to provide it within 90 days. In any event, you
generally must provide any required proof of the claim to
Allstate within 15 months, or your claim will be denied.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter. You
or your beneficiary has the right to appeal a claim denial.
When benefits are not paid
Benefits are not paid for a loss that is caused by or occurs as
a result of:
• An injury that results from an accident that occurs while
working at any job for pay or benefits
• An injury incurred prior to your effective date of coverage
• Any act of war, whether or not declared, or participation in
a riot, insurrection or rebellion
• Suicide, or any attempt at suicide, whether sane or insane
• Any injury sustained while you or your covered family
member are under the influence of alcohol or any narcotic,
unless administered upon the advice of a physician
• Dental or plastic surgery for cosmetic purposes, except
when such surgery is required to treat an injury or correct
a disorder of normal bodily function that was caused by
an injury
• Participation in any form of aeronautics, except as a
fare-paying passenger in a licensed aircraft provided
by a common carrier and operating between definitely
established airports
• Committing or attempting to commit an assault or felony
• Driving in any organized or scheduled race or speed test or
while testing an automobile or any vehicle on any racetrack
or speedway, or
• Any injury incurred while a covered person is an active
member of the military, naval, or air forces of any country
or combination of countries. Upon notice and proof of
service in such forces, Allstate Benefits will return the
prorated portion of the premium paid for any period of
such service.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your accident insurance premiums
to avoid a break in coverage. These situations occur most
commonly if you are on a leave of absence or if your
Walmart paycheck is not sufficient to pay your full share
of the cost of coverage (such as after a reduction in
hours). Depending on your circumstances, failure to make
your premium payments by the due date may result in an
interruption in the payment of any benefit claims and/or a
break in coverage.
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information about
making payments while on a leave of absence, see When
special arrangements are necessary to maintain coverage in
the Eligibility and enrollment chapter.
Accident insurance
147
When coverage ends
Your accident insurance coverage ends on the earliest of
the following:
• At termination of your employment
• Upon failure to pay your premiums
• On your date of death
• On the last day of an approved leave of absence (unless
you return to work), or
• When the benefit is no longer offered by the company.
Accident insurance coverage for your spouse/partner ends:
• On the date your accident insurance coverage ends
• On the last day of the pay period when your job status
changes to part-time, temporary, or part-time truck driver
• On the date your spouse/partner loses eligibility, such
as upon a valid decree of divorce or termination of
partnership, or
• On your spouse/partner’s death.
Accident insurance coverage for your dependent
child(ren)ends:
• On the date your accident insurance coverage ends
• On the date your dependent child loses eligibility, or
• On your dependent child’s death.
CONTINUATION OF COVERAGE
ATTERMINATION
If your coverage under accident insurance terminates
as described earlier in this section, you may continue to
receive accident insurance directly from Allstate Benefits
through portability coverage. To receive portability
coverage, you must notify Allstate Benefits that you
wish to continue coverage and send the first premium
within 60days of the date your coverage under accident
insuranceterminated.
The premiums for portability coverage are due in advance
of each month’s coverage, on the first day of the calendar
month. The premiums are set at the same rate in effect
under accident insurance for active associates with the
same coverage.
For more information, please contact Allstate Benefits
at800-514-9525.
WHEN YOUR DEPENDENT
BECOMESINELIGIBLE
Any eligible dependent covered under accident insurance
at the time such coverage terminated may also receive
portability coverage, under the terms described on the
previous page. Contact Allstate Benefits at 800-514-9525
for information.
If you leave the company and
arerehired
If you leave the company and then return to work within
13weeks, you will automatically be reenrolled for the same
coverage plan you had prior to leaving the company (or the
most similar coverage offered under the Plan).
If your break is greater than 30 days but less than
13weeks, you will have 60 days after resuming work to
drop or otherwise change the coverage in which you were
automatically reenrolled.
If you return to work after 13 weeks, you will be considered
newly eligible and may enroll for coverage under the time
periods and conditions described in the Eligibility and
enrollment chapter.
If you drop coverage and reenroll
If you drop coverage and reenroll within 30 days, you will
automatically be reenrolled for the same coverage you had
prior to dropping coverage (or the most similar coverage
offered under the Plan).
If you drop coverage and reenroll after 30 days, you will be
considered newly eligible and may enroll for coverage under
the time periods and conditions described in the Eligibility
and enrollment chapter.
IF A DEPENDENT IS DROPPED FROM
COVERAGE AND REENROLLED
If your dependent child is dropped from coverage and then
determined to be eligible for coverage within 30 days, the
dependent will automatically be reenrolled in the same
coverage you elect for yourself.
If your dependent regains eligibility and is reenrolled after
30 days, they will be treated as a newly eligible dependent.
The associate may enroll them for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information is intended to be a summary of your benefits and may not include all policy provisions. If
there is a discrepancy between this document and the policy issued by Prudential regarding the calculation
of benefits and limitations under the policy, the terms of the policy will govern. You may obtain a copy of
this policy by contacting the Plan.
Company-paid life insurance 150
Naming a beneficiary 150
When your company-paid life insurance coverage begins 150
Early payout due to terminal illness 150
Filing a claim 151
When benefits are not paid 151
When coverage ends 151
EstateGuidance® 151
Continuing your company-paid life insurance after you leave Walmar 152
If you leave the company and arerehired 152
Company-paid
lifeinsurance

Company-paid lifeinsurance
149
Company-paid life insurance
Life insurance is automatically provided by Walmar at no cost to you. So you can rest easy
knowing your loved ones will have financial help if the unthinkable happens.
RESOURCES
Find What You Need Online Other Resources
Change your beneficiary designation Go to One.Walmar.com or
Workday for Jet associates
Beneficiary changes cannot be made
over the phone
• Get more coverage details
• Request an accelerated benefit
• Get details about continuing
yourinsurance
Call Prudential at 877-740-2116
File a claim Call Prudential at 877-740-2116
What you need to know about company-paid life insurance
• If you are a full-time hourly or management associate, Walmart provides you with life insurance coverage at no cost to
you (for details about eligible job classifications, see the Enrollment and eligibility dates by job classification charts in
the Eligibility and enrollment chapter). No enrollment is necessary, and Proof of Good Health is not required.
• Your coverage amount is equal to your annualized rate of pay, including overtime and bonuses, during the one-year
period prior to your death, rounded to the nearest $1,000, to a maximum of $50,000.
• An early payout due to terminal illness is available.
• Coverage is provided through The Prudential Insurance Company of America (Prudential).
• This policy is term life insurance. It has no cash value.

Company-paid lifeinsurance
150
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Company-paid life insurance
If you are a full-time hourly or management associate,
Walmart provides you with life insurance coverage at no
cost to you (for details about eligible job classifications, see
the Enrollment and eligibility dates by job classification
charts in the Eligibility and enrollment chapter). No
enrollment is necessary.
Your company-paid coverage amount is equal to your
annualized rate of pay, including overtime and bonuses,
during the one-year period prior to your death, rounded to
the nearest $1,000, to a maximum of $50,000.
Naming a beneficiary
To ensure your company-paid life insurance benefit is paid
according to your wishes, you must name a beneficiary(ies).
You may do this by going to One.Walmart.com or Workday
for Jet associates. Note that only beneficiary designations
made online are accepted.
You can name anyone you wish. If the beneficiary(ies) you
list with Walmart differs from the beneficiary(ies) named in
your will, the list that Walmart has prevails. If you have not
designated a beneficiary(ies) under the company-paid life
insurance benefit, payment will be made to your surviving
family members as described under If you do not name a
beneficiary later in this chapter.
The following information is needed for each beneficiary:
• Name
• Current address and phone number
• Relationship to you
• Social Security number
• Date of birth, and
• The percentage you wish to designate per beneficiary,
upto 100%.
If two or more beneficiaries are designated and their
shares are not specified, they will share the insurance
benefit equally. If a named beneficiary dies before you, that
beneficiary’s interest will end, and will be shared equally
by any remaining beneficiaries unless your beneficiary
form states otherwise. If you and a beneficiary die in the
same event and it cannot be determined who died first, the
beneficiary will be treated as having died before you.
You can name a minor as a beneficiary; however, Prudential
may not be legally permitted to pay the minor until the minor
reaches legal age. You may want to consult an attorney or an
estate planner before naming a minor as a beneficiary. If you
name a minor as a beneficiary, funeral expenses cannot be
paid from the minor’s beneficiary proceeds.
CHANGING YOUR BENEFICIARY
You can change your beneficiary(ies) at any time on
One.Walmart.com or Workday for Jet associates. Any
change in beneficiary must be completed and submitted to
Walmart before your death and can be submitted only by
you, the covered associate.
IF YOU DO NOT NAME A BENEFICIARY
If no beneficiary is named or there is no surviving
beneficiary at the time of your death, payment will be made
to surviving family members in the following order:
1. Spouse or partner of the deceased; if not surviving, then
2. Children in equal shares; if not surviving, then
3. Parents in equal shares; if not surviving, then
4. Siblings in equal shares; if not surviving, then
5. Your estate.
Be sure to keep your beneficiary information
up to date. Proceeds go to whoever is listed
on your beneficiary form with Walmart,
regardless of your current relationship with
that person, unless state law says otherwise.
You can change your beneficiary(ies) at any
time on One.Walmart.com or Workday for
Jetassociates.
When your company-paid life
insurance coverage begins
Company-paid life insurance coverage begins on the
date specified in the Enrollment and effective dates by
job classification charts in the Eligibility and enrollment
chapter. You must be actively at work for your coverage
to become effective. You are considered actively at work
on a day that is one of your scheduled work days if you are
performing in the usual way all the regular duties of your
job. See the Eligibility and enrollment chapter for details.
Early payout due to terminal illness
If you are terminally ill, you may elect to receive an
“accelerated benefit” while you are still living of up to 50%
of the amount your beneficiary(ies) would have received
upon your death (measured on the date you provide proof
of your terminal illness). Payment may be made in a lump
sum or 12 equal monthly installments. Upon your death,
your beneficiary(ies) receive the greater of (a) 100% of
Company-paid lifeinsurance
151
your annual earnings, based on the most recent average
salary for the last 26 pay-periods, reduced by the amount
of any terminal illness proceeds paid under the option to
accelerate payment of death benefits, or (b) the amount of
insurance in effect prior to payment of any terminal illness
proceeds, reduced by the amount of any terminal illness
proceeds paid under the option to accelerate payment of
death benefits.
If you terminate from the company after you have received
(or begun to receive) the accelerated benefit, you will need
to convert the policy for your beneficiary(ies) to receive the
remaining balance upon your death. If you do not convert
the policy upon termination of your employment, no benefit
will be payable to your beneficiary(ies). See the Continuing
your company-paid life insurance after you leave Walmart
section in this chapter for details on conversion.
Under the policy, you are considered terminally ill if death
is expected within 12 months and a doctor can certify the
illness or injury as terminal.
There may be circumstances in which the accelerated
benefit is not paid. Contact Prudential at 877-740-2116
fordetails.
Please consult with a tax professional to assess the impact
of this benefit.
Filing a claim
The following information must be provided to Prudential
regarding the deceased associate:
• Name
• Social Security number
• Date of death, and
• Cause of death (if known).
An original or certified copy of the death certificate is
required as proof of death. The death certificate should be
mailed to:
The Prudential Insurance Company of America
Group Life Claim Division
P.O. Box 8517
Philadelphia, Pennsylvania 19176
The claim will not be finalized until Prudential receives the
death certificate. Acceptance of the death certificate is not
a guarantee of payment.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter.
Your beneficiary(ies) has the right to appeal a claim denial.
Benefits are paid according to the terms of the insurance
policy. For details, contact Prudential at 877-740-2116.
If your death occurs outside a 100-mile radius of your home,
there is a benefit for expenses incurred to return your body
to either a preferred location within the United States,
or to your residence at the time of death. The benefit
includes expenses for embalming, cremation, a coffin, and
transportation of your remains. The benefit is the lesser of
the cost to return your remains or $10,000.
When benefits are not paid
Benefits are not paid to any beneficiary(ies) who engaged
in an illegal act that resulted in the associate’s death.
The benefit in this circumstance would go to another
eligible designated beneficiary or, if there is no other
surviving beneficiary, to a beneficiary in the default list,
as specified under If you do not name a beneficiary earlier
in this chapter.
When coverage ends
Your company-paid life insurance coverage ends:
• At termination of your employment
• On the last day of the pay period when your job status
changes to part-time
• On the date of your death
• On the date that you lose eligibility
• On the last day of an approved leave of absence (unless
you return to work), or
• When the benefit is no longer offered by the company.
This policy is term life insurance. It has no cash value.
EstateGuidance®
EstateGuidance offers you the convenience of online
will preparation from your personal computer at no cost
to you. Wills ensure that your assets will be distributed
in accordance with your wishes and allow you to name
a guardian of your minor children. To complete the
online will questionnaire, log on to willguidance.com,
password:Walmart.
NOTE: Your will does not override the beneficiary
designation on a life insurance policy or retirement account
(such as a 401(k) plan). For this reason, be sure to review
your beneficiary designations, particularly after you have
created a will, to make sure your designations are consistent
and fully in line with your wishes. If the beneficiary(ies) you
have listed with Walmart differs from the beneficiary(ies)
named in your will, the list that Walmart has prevails.
Company-paid lifeinsurance
152
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Continuing your company-paid life
insurance after you leave Walmar
In most circumstances, you have two options to continue
your company-paid life insurance if your group life coverage
ends. The first option, called portability, allows you to
continue all or a portion of your coverage through a group
term policy with Prudential. The second option, called
conversion, allows you to convert all or a portion of your
coverage to a Prudential individual policy.
You must apply for portability or conversion within 31 days
of the date your company-paid coverage ends. If you die
within 31 days of a qualifying loss of coverage and before
electing portability or conversion of your life insurance
coverage, Prudential will pay a death benefit to your
beneficiary. The benefit will be paid based on the amount of
coverage in effect prior to the qualifying loss of coverage,
even if you did not apply for portability or conversion of
your coverage.
Portability enables you to maintain similar term life
insurance with Prudential after your employment ends,
if certain conditions are met. Proof of Good Health is
required to “port” your coverage. If you do not pass or do
not submit Proof of Good Health, you will be eligible to
convert your company-paid life insurance to an individual
policy, as described in the next column.
You can apply for term life coverage under the portability
feature if you meet all of these conditions:
• Your company-paid life coverage ends for any reason
otherthan:
– you leave the company due to a disability, or
– Walmar changes group life insurance carriers and you
are, or become, eligible within the next 31 days.
• You are actively at work on the day your company-paid
insurance ends.
• You are less than age 80.
• Your amount of insurance is at least $20,000 on the day
your company-paid insurance ends.
If you meet these conditions, you will have 31 days from
your termination date to contact Prudential and enroll.
Conversion is a required Plan provision that allows you
to convert your life insurance coverage to an individual
policy if coverage would end due to your termination
of employment or transfer from an eligible class. Proof
of Good Health is not required. Rates are based on your
age and amount converted. You have 31 days from the
termination date of coverage to request to convert your
coverage to an individual policy. If your death occurs during
the 31-day conversion period, the death benefit will be
payable up to the amount that could have been converted.
If you are a resident of Minnesota, you have a continuation
right instead of a conversion right when you lose coverage
due to a reduction in your hours or termination of
employment (other than for gross misconduct). You may
elect to continue coverage at your expense until you obtain
coverage under another group life insurance policy; however,
the maximum period that coverage may be continued is 18
months. If you continue coverage, at the expiration of the
continuation period you may convert your life insurance
coverage to an individual policy, as described above.
To request information on portability or conversion, call
Prudential at 877-740-2116.
If you leave the company and
arerehired
If you return to work for the company as a full-time
hourly or management associate within 13 weeks, you will
automatically be reenrolled for coverage.
If you return to work after 13 weeks, you will be considered
newly eligible and will be required to complete the
applicable eligibility waiting period. See the Eligibility and
enrollment chapter for details.
Company-paid lifeinsurance
153

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information is intended to be a summary of your benefits and may not include all policy provisions. If
there is a discrepancy between this document and the policy issued by Prudential regarding the calculation
of benefits and limitations under the policy, the terms of the policy will govern. You may obtain a copy of
this policy by contacting thePlan.
Optional associate life insurance 156
Naming a beneficiary 156
When your optional associate life insurance coverage begins 157
Early payout due to terminal illness 157
Filing a claim 157
When benefits are not paid 158
Break in coverage 158
When coverage ends 158
Continuing your optional associate life insurance after youleaveWalmar 158
If you leave the company and arerehired 159
If you drop or decrease your coverage and reenroll 159
Optional associate
life insurance

Optional associate life insurance
155
Optional associate life insurance
Optional associate life insurance takes care of your family by giving them extra financial
protection during a difficult time.
RESOURCES
Find What You Need Online Other Resources
Change your beneficiary designation Go to One.Walmar.com or Workday for
Jet associates
Beneficiary changes cannot be made
over the phone
• Get more details
• Request an accelerated benefit
• Get details about continuing your
insurance
Call Prudential at 877-740-2116
File a claim Call Prudential at 877-740-2116
What you need to know about optional associate life insurance
• If you are an hourly or management associate, you can enroll in optional associate life insurance when you are
eligible, as described in the Eligibility and enrollment chapter.
• Depending on the amount of coverage you choose and when you enroll, you may be required to provide Proof of
Good Health.
• You can enroll in, change, or drop optional associate life insurance at any time, but if you enroll at any time other
than your initial enrollment period, you will have to provide Proof of Good Health.
• An early payout due to terminal illness is available.
• Coverage is provided through The Prudential Insurance Company of America (Prudential).
• This policy is term life insurance. It has no cash value.

Optional associate life insurance
156
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Optional associate life insurance
Optional associate life insurance protects your family if you
die while coverage is in effect. If you become terminally ill, a
benefit may be payable to you while you are still living.
If you are an hourly or management associate you can enroll
in optional associate life insurance when you are eligible, as
described in the Eligibility and enrollment chapter.
Your coverage choices for optional associate life insurance
depend on your job classification, as reflected in the
company’s payroll system. The coverage amounts you can
choose are shown in the chart below.
HOURLY ASSOCIATES AND
PARTTIME TRUCK DRIVERS
MANAGEMENT
ASSOCIATES
$25,000 $100,000 $25,000 $200,000
$50,000 $150,000 $50,000 $300,000
$75,000 $200,000 $75,000 $500,000
$100,000 $750,000
$150,000 $1,000,000
For details about eligible job classifications, see the Enrollment
and eligibility dates by job classification section in the
Eligibility and enrollment chapter
If you die, your beneficiary(ies) may receive a lump sum
payment for the coverage amount you select.
The cost of optional associate life insurance is based on the
coverage amount you select, your age, and whether you
are eligible for tobacco-free rates. Premiums from optional
associate life coverage do not subsidize coverage under
company-paid life insurance.
If you are an hourly associate, part-time truck driver, or
management associate, you can enroll in optional associate
life insurance at any time once you are eligible. Proof of
Good Health may be required when you enroll, depending
on the coverage amount you choose and when you enroll.
You can change or drop coverage at any time. However, you
will be required to provide Proof of Good Health if you want
to increase your coverage or reenroll for any amount of
coverage after dropping coverage.
See the Company-paid life insurance chapter
for information about other life insurance
coverage available to full-time hourly and
management associates.
PROOF OF GOOD HEALTH
Proof of Good Health is required for optional associate life
insurance if:
• The coverage amount selected is above $25,000 during
your initial enrollment period
• You enroll after your initial enrollment period for any
amount, or
• You increase your coverage after your initial
enrollmentperiod.
Proof of Good Health includes completing a questionnaire
regarding your medical history and possibly having a
medical exam. The Proof of Good Health questionnaire is
made available when you enroll.
Naming a beneficiary
To ensure that your life insurance benefit is paid according
to your wishes, you must name a beneficiary(ies) to receive
your optional associate life insurance benefit if you die.
You may do this by going to One.Walmart.com or Workday
for Jet associates. Any change in beneficiary must be
completed and submitted to Walmart before your death
and can be submitted only by you, the covered associate.
Note that only beneficiary designations made online
areaccepted.
You can name anyone you wish. If the beneficiary(ies) you
list with Walmart differs from the beneficiary(ies) named in
your will, the list that Walmart has prevails. If you have not
designated a beneficiary(ies) under the optional associate
life insurance benefit, payment will be made to your
surviving family members as described under If you do not
name a beneficiary later in this chapter.
The following information is needed for each beneficiary:
• Name
• Current address and phone number
• Relationship to you
• Social Security number
• Date of birth, and
• The percentage you wish to designate per beneficiary, up
to 100%.
If two or more beneficiaries are designated and their
shares are not specified, they will share the insurance
benefit equally. If a named beneficiary dies before you, that
beneficiary’s interest will end and will be shared equally
by any remaining beneficiary(ies), unless your beneficiary
form states otherwise. If you and a beneficiary die in the
same event and it cannot be determined who died first, the
beneficiary will be treated as having died before you.

Optional associate life insurance
157
You can name a minor as a beneficiary; however, Prudential
may not be legally permitted to pay the minor until the minor
reaches legal age. You may want to consult an attorney or an
estate planner before naming a minor as a beneficiary. If you
name a minor as a beneficiary, funeral expenses cannot be
paid from the minor’s beneficiary proceeds.
CHANGING YOUR BENEFICIARY
You can change your beneficiary(ies) at any time on
One.Walmart.com or Workday for Jet associates. Any
change in beneficiary must be completed and submitted to
Walmart before your death and can be submitted only by
you, the covered associate.
Be sure to keep your beneficiary information
up to date. Proceeds will go to whoever is
listed on your beneficiary form with Walmart,
regardless of your current relationship with
that person, unless state law says otherwise.
You can change your beneficiary(ies) at
any time on One.Walmart.com or Workday
forJet associates.
IF YOU DO NOT NAME A BENEFICIARY
If no beneficiary is named or there is no surviving
beneficiary at the time of your death, payment will be made
to surviving family members in the following order:
1. Spouse or partner of the deceased; if not surviving, then
2. Children in equal shares; if not surviving, then
3. Parents in equal shares; if not surviving, then
4. Siblings in equal shares; if not surviving, then
5. Your estate.
When your optional associate life
insurance coverage begins
When Proof of Good Health is required (as described on the
previous page), your coverage becomes effective the day
the company receives approval from Prudential or at the
end of your eligibility waiting period, whichever is later.
If you should die before Prudential approves coverage, no
optional associate life insurance benefit will be paid to your
beneficiary(ies).
When Proof of Good Health is not required, your coverage
becomes effective on the date you enroll or at the end of
your eligibility waiting period, whichever is later.
In either case, you must be actively at work for your coverage
to become effective. You are considered actively at work
on a day that is one of your scheduled work days if you are
performing in the usual way all the regular duties of your job.
See the Eligibility and enrollment chapter for details.
Early payout due to terminal illness
If you are terminally ill, you may elect to receive an
“accelerated benefit” while you are still living of up to 50%
of the coverage amount your beneficiary(ies) would have
received upon your death, up to a $250,000 maximum.
Payment may be made in a lump sum or 12 equal monthly
installments. Upon your death, your beneficiary(ies)
receive the total amount of coverage in effect at your
death minus the amount of early payouts you received
before your death).
If you terminate from the company after you have
received (or begun to receive) the accelerated
benefit, you will need to convert the policy for your
beneficiary(ies) to receive the remaining balance upon
your death. If you do not convert the policy upon
termination of your employment, no benefit will be
payable to your beneficiary(ies). See the Continuing your
optional associate life insurance after you leave Walmart
section later in this chapter for details on conversion.
Under the policy, you are considered terminally ill if death
is expected within 12 months and a doctor can certify the
illness or injury as terminal.
There may be circumstances in which the accelerated
benefit is not paid. Contact Prudential at 877-740-2116
fordetails.
Please consult a tax professional to assess the impact of
thisbenefit.
Filing a claim
The following information must be provided to Prudential
regarding the deceased associate:
• Name
• Social Security number
• Date of death, and
• Cause of death (if known).
An original or certified copy of the death certificate is
required as proof of death. The death certificate should be
mailed to:
The Prudential Insurance Company of America
Group Life Claim Division
P.O. Box 8517
Philadelphia, Pennsylvania 19176
Optional associate life insurance
158
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The claim will not be finalized until Prudential receives the
death certificate. Acceptance of the death certificate is not
a guarantee of payment.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter.
Your beneficiary has the right to appeal a claim denial.
Benefits are paid according to the terms of the insurance
policy. For more details, contact Prudential at 877-740-2116.
When benefits are not paid
No benefits are paid to your beneficiary(ies) if you die as
a result of suicide while sane or insane during the first two
years of coverage. If you increase your coverage and you
die as a result of suicide within two years of the date you
increase your coverage, your beneficiary(ies) will receive
the prior coverage amount.
If your beneficiary(ies) files a claim within the first two
years of your approval date, Prudential has the right to
re-examine your Proof of Good Health questionnaire. If
material facts about you are found to have been stated
inaccurately, the true circumstances will be used to
determine what amount of coverage should have been in
effect, if any, and:
• The claim may be denied, and
• Premiums paid may be refunded.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your optional associate life insurance
premiums to avoid a break in coverage. These situations
occur most commonly if you are on a leave of absence or
if your Walmart paycheck is not sufficient to pay your full
share of the cost of coverage (such as after a reduction in
hours). Depending on your circumstances, failure to make
your premium payments by the due date may result in an
interruption in the payment of any benefit claims and/or a
break in coverage.
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information about
making payments while on a leave of absence, see When
special arrangements are necessary to maintain coverage in
the Eligibility and enrollment chapter.
When coverage ends
Your optional associate life insurance coverage ends:
• At termination of your employment
• Upon failure to pay your premiums
• On the date of your death
• On the last day of an approved leave of absence (unless
you return to work)
• When the benefit is no longer offered by the company, or
• On the day after you drop coverage.
This policy is term life insurance. It has no cash value.
Continuing your optional
associate life insurance after
youleaveWalmar
In most circumstances, you have two options to continue
your optional associate life insurance if your group life
coverage ends. The first option, called portability, allows
you to continue all or a portion of your current coverage
through a group term policy with Prudential. The second
option, called conversion, allows you to convert all or a
portion of your coverage to a Prudential individual policy.
You must apply for portability or conversion within 31 days
of the date your coverage ends. If you die within 31 days of
a qualifying loss of coverage and before electing portability
or conversion of your life insurance coverage, Prudential
will pay a death benefit to your beneficiary. The benefit will
be paid based on the amount of coverage in effect prior to
the qualifying loss of coverage, even if you did not apply for
portability or conversion of your coverage.
Portability enables you to maintain similar term life
insurance with Prudential after your employment ends if
certain conditions are met. Proof of Good Health is not
required to “port” your coverage. You can, however, receive
preferred rates similar to the rates you paid while an active
associate if you submit and pass Proof of Good Health. If
you do not pass or do not submit Proof of Good Health, your
rates will be based on Prudential’s standard portability rates.
You can apply for term life coverage under the portability
feature if you meet all of these conditions:
• Your optional associate life coverage ends for any reason
other than:
– your failure to pay premiums while an active associate
– you leave the company due to a disability, or
– Walmar changes group life insurance carriers and you
are, or become, eligible within the next 31 days.
• You meet the active work requirement on the day your
insurance ends.
Optional associate life insurance
159
• You are less than age 80.
• Your amount of insurance is at least $20,000 on the day
your insurance ends.
If you meet these conditions, you will have 31 days from
your termination date to contact Prudential and enroll.
Prudential will notify you of the amount of portability
coverage offered. The amount of insurance coverage
offered will not be more than the amount of coverage you
elected under the plan (and not more than five times your
annual earnings), and will not be less than $20,000.
Conversion is a required Plan provision that allows you
to convert your life insurance coverage to an individual
policy if coverage would end due to your termination
of employment or transfer from an eligible class. Proof
of Good Health is not required. Rates are based on your
age and amount converted. You have 31 days from the
termination date of coverage to request to convert your
coverage to an individual policy. If your death occurs during
the 31-day conversion period, the death benefit will be
payable up to the amount that could have been converted.
If you are a resident of Minnesota, you have a continuation
right instead of a conversion right when you lose coverage
due to a reduction in your hours or termination of
employment (other than for gross misconduct). You may
elect to continue coverage at your expense until you
obtain coverage under another group life plan; however,
the maximum period that coverage may be continued is 18
months. If you continue coverage, at the expiration of the
continuation period you may convert your life insurance
coverage to an individual policy, up to the amount of
coverage in effect at that time. You have 31 days from the
date continuation coverage would end to request to convert
your coverage to an individual policy.
To request information on portability or conversion, call
Prudential at 877-740-2116.
If you leave the company and
arerehired
If you return to work for the company within 13 weeks,
you will automatically be reenrolled for the same coverage
in effect prior to leaving the company (or the most
similar coverage offered under the Plan). You can drop or
otherwise change your coverage at any time.
If you return to work after 13 weeks, you will be considered
newly eligible and will be required to complete the
applicable eligibility waiting period. Proof of Good Health
is required for coverage plans above $25,000 (or for any
amount if you enroll after your initial enrollment period).
See the Eligibility and enrollment chapter for details.
If you drop or decrease your
coverage and reenroll
If you drop or decrease your coverage and reenroll within
30 days, you may reenroll for the same coverage in effect
prior to dropping or decreasing coverage.
If you reenroll more than 30 days after dropping or
decreasing your coverage, Proof of Good Health will
berequired.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information is intended to be a summary of your benefits and may not include all policy provisions. If
there is a discrepancy between this document and the policy issued by Prudential regarding the calculation
of benefits and limitations under the policy, the terms of the policy will govern. You may obtain a copy of
this policy by contacting the Plan.
Optional dependent life insurance 162
When your optional dependent life insurance coverage begins 162
Additional benefits 163
Filing a claim 163
When benefits are not paid 163
Break in coverage 163
When coverage ends 164
Continuing spouse/parner coverage after you leave Walmar 164
If you leave the company and arerehired 165
If you drop or decrease your coverage and reenroll 165
Optional dependent
life insurance

Optional dependent life insurance
161
Optional dependent life insurance
Optional dependent life insurance can help ease your financial situation if you lose someone close
to you, like a spouse, parner, or child.
RESOURCES
Find What You Need Online Other Resources
Get more details Go to One.Walmar.com
or Workday for Jet associates
Call Prudential at 877-740-2116
File a claim Call Prudential at 877-740-2116
What you need to know about optional dependent life insurance
• If you are an hourly or management associate, you can enroll your eligible dependents in optional dependent
life insurance when you are eligible, as described in the Eligibility and enrollment chapter. Full-time hourly and
management associates can enroll their spouse/partners and/or their children; part-time hourly associates and part-
time truck drivers can enroll their children but not their spouse/partners.
• Proof of Good Health for your spouse/partner is required if you enroll for a coverage amount above $5,000 during
your initial enrollment period, or for any coverage amount if you enroll at any other time. Proof of Good Health is not
required for your children.
• Coverage is provided through the Prudential Insurance Company of America (Prudential).
• This policy is term life insurance. It has no cash value.

Optional dependent life insurance
162
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Optional dependent life insurance
Optional dependent life insurance pays you a financial
benefit if you are an enrolled associate and your dependent
dies while coverage is in effect. If you are an hourly
or management associate, you can enroll in optional
dependent life insurance when you are eligible, as described
in the Eligibility and enrollment chapter.
All full-time hourly and management associates can enroll
their spouses/partners and/or children. All part-time
hourly associates, part-time truck drivers, and temporary
associates can enroll their children but cannot enroll their
spouses/partners.
For details about eligible job classifications, see the
Enrollment and eligibility dates by job classification charts
in that chapter.
When you enroll in optional dependent life insurance, if your
covered spouse/partner and/or legal dependent dies, you
may receive a lump sum payment for the coverage amount
you select. The coverage choices for optional dependent
life insurance are as follows:
SPOUSE/PARTNER COVERAGE* CHILD COVERAGE
$5,000 $75,000 $5,000
$15,000 $100,000 $10,000
$25,000 $150,000 $20,000
$50,000 $200,000
* Not available for par-time hourly associates, temporary
associates, or par-time truck drivers
Depending on the coverage amount you choose and when
you enroll, your spouse/partner may be required to provide
Proof of Good Health.
You (the associate) are automatically assigned as the
primary beneficiary of your dependent’s life insurance
coverage. If you and your covered dependent or
dependents die at the same time, benefits are paid to your
dependent’s estate or, at Prudential’s option, to a surviving
relative of the dependent.
The cost of optional dependent life insurance for your
spouse/partner is based on the coverage amount you select,
your (the associate’s) age, and whether your spouse/partner
is eligible for the tobacco-free rates. The cost of coverage
for your children is based on the coverage amount you
select. Premiums from optional dependent life coverage do
not subsidize coverage under company-paid life insurance.
You can enroll in optional dependent life insurance at any time.
Proof of Good Health is required for your spouse/partner if
you enroll after your initial enrollment period. Also, you can
change or drop coverage at any time. However, if you want
to increase your spouse/partner’s coverage or reenroll after
dropping coverage, you will be required to provide Proof of
Good Health for your spouse/partner.
PROOF OF GOOD HEALTH
Proof of Good Health is required for your spouse/partner’s
optional dependent life insurance coverage if:
• The coverage amount selected is above $5,000
duringyourinitial enrollment period
• You enroll after your initial enrollment period for
anyamount, or
• You increase your coverage after your initial
enrollmentperiod.
However, within 60 days of marriage, you may elect to
cover your spouse or change the amount of insurance for
your spouse. In this instance, even though you are outside
your initial enrollment period, your spouse is not required
toprovide Proof of Good Health unless you select a
coverage amount greater than $5,000.
Proof of Good Health includes completing a questionnaire
regarding your spouse/partner’s medical history and
possibly requiring your spouse/partner to have a medical
exam. The Proof of Good Health questionnaire is made
available when you enroll your spouse/partner. Proof of
Good Health is not required for children.
When your optional dependent life
insurance coverage begins
When Proof of Good Health is required (as described above),
coverage for your spouse/partner becomes effective the
day the company receives approval from Prudential or at
the end of your eligibility waiting period, whichever is later.
Proof of Good Health is not required for children.
If your spouse/partner should die before Prudential
approves coverage, no optional dependent life insurance
will be paid to you.
When Proof of Good Health is not required, coverage for
your spouse/partner or child becomes effective on the date
you enroll or at the end of your eligibility waiting period,
whichever is later.
Optional dependent life insurance
163
If your spouse/partner or dependent child is confined
for medical treatment (at home or elsewhere), coverage
is delayed until the spouse/partner or child has a medical
release (does not apply to a newborn child).
You must be actively at work for your dependent coverage
to become effective. You are considered actively at work
on a day that is one of your scheduled work days if you are
performing in the usual way all the regular duties of your
job. See the Eligibility and enrollment chapter for details.
Additional benefits
Benefits also are payable under the following
circumstances:
• If a dependent child is born alive and dies within 60 days
of birth and was eligible but not enrolled in optional
dependent life insurance prior to the loss — with a live birth
certificate and a death certificate — Prudential will pay a
$5,000 benefit only.
• If a dependent child is stillborn, Prudential will pay a
$5,000 benefit to associates who have met the eligibility
waiting period for dependent life insurance. See the
Eligibility and enrollment chapter for details. A stillborn
child is defined as an eligible associate’s natural-born
child whose death occurs before expulsion, extraction,
or delivery and whose fetal weight is 350 grams or more;
or, if fetal weight is unknown, whose duration in utero
was 20 or more complete weeks of gestation. If both the
mother and father of the stillborn child work at Walmart,
each associate is eligible to submit a claim for this benefit
separately, for a total of $10,000.
Filing a claim
The following information must be provided to Prudential
regarding the deceased dependent:
• Name
• Social Security number
• Date of death, and
• Cause of death (if known).
An original or certified copy of the death certificate is
required as proof of death. Mail the death certificate to:
The Prudential Insurance Company of America
Group Life Claim Division
P.O. Box 8517
Philadelphia, Pennsylvania 19176
The claim will not be finalized until Prudential receives the
death certificate. Acceptance of the death certificate is not
a guarantee of payment.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter.
Youhave the right to appeal a claim denial.
Benefits are paid according to the terms of the insurance
policy. For more details, contact Prudential at 877-740-2116.
When benefits are not paid
No benefits are paid to you if your spouse/partner dies as
a result of suicide while sane or insane during the first two
years of coverage. If you increase your spouse/partner’s
coverage and your spouse/partner dies as a result of suicide
within two years of the increase in coverage, you will receive
the prior coverage amount.
If you file a claim for your spouse/partner within the first
two years of your approval date, Prudential has the right to
re-examine your spouse/partner’s Proof of Good Health
questionnaire. If material facts about your spouse/partner
are found to have been stated inaccurately, the true
circumstances will be used to determine what amount of
coverage should have been in effect, if any, and:
• The claim may be denied, and
• Premiums paid may be refunded.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your optional dependent life insurance
premiums to avoid a break in coverage. These situations
occur most commonly if you are on a leave of absence or
if your Walmart paycheck is not sufficient to pay your full
share of the cost of coverage (such as after a reduction in
hours). Depending on your circumstances, failure to make
your premium payments by the due date may result in an
interruption in the payment of any benefit claims and/or
abreak in coverage.
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information about
making payments while on a leave of absence, see When
special arrangements are necessary to maintain coverage in
the Eligibility and enrollment chapter.
Optional dependent life insurance
164
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
When coverage ends
Your optional dependent life insurance coverage ends:
• At termination of your employment
• Upon failure to pay your premiums
• On the date of your death
• On the date that you or a dependent spouse/partner
orchild loses eligibility (see the Eligibility and
enrollment chapter)
• On the last day of an approved leave of absence (unless
you return to work)
• When the benefit is no longer offered by the company, or
• The day after you drop your coverage.
In addition, if you have optional dependent life coverage for
your spouse/partner and your job status changes to part-time
hourly associate, temporary associate, or part-time truck
driver, your coverage for your spouse/partner will end on the
last day of the pay period when your job status changes.
This policy is term life insurance. It has no cash value.
Continuing spouse/parner coverage
after you leave Walmar
If you are a full-time or management associate and
carry optional dependent life insurance for your spouse
or partner, you have two options to continue your
spouse/partner coverage after your group life coverage
ends. The first option, called portability, allows you and
your spouse or partner to continue all or a portion of
your current coverage through a group term policy with
Prudential. The second option, called conversion, allows
you to convert all or a portion of your spouse/partner
coverage to a Prudential individual policy. These options
are not available to part-time hourly associates, temporary
associates, or part-time truck drivers.
You must apply for portability or conversion within 31 days of
the date your spouse/partner coverage ends. If your spouse
or partner dies within 31 days of a qualifying loss of coverage
and before electing portability or conversion of the life
insurance coverage, Prudential will pay a death benefit.
The benefit will be the amount of coverage your spouse or
partner could have converted, even if your dependent did
not apply for portability or conversion of coverage.
Portability enables you to maintain similar term life
insurance for your spouse or partner with Prudential after
your associate coverage ends or your spouse or partner
loses eligibility due to divorce or separation, if certain
conditions are met.
Proof of Good Health is not required to “port” your spouse/
partner coverage. You can, however, receive preferred rates
for spouse/partner coverage similar to the rates you paid
while an active associate if your spouse/partner submits and
passes Proof of Good Health. If you do not pass or submit
Proof of Good Health for your spouse/partner, your rates
will be based on Prudential’s standard portability rates.
You can apply for term life coverage under the portability
feature if you meet all of these conditions:
• The optional dependent life coverage ends because your
optional associate life coverage ends for any reason
otherthan:
– your failure to pay premiums while an active associate
– the end of your employment on account of your
retirement due to disability, or
– the end of the optional associate life coverage for all
associates when such coverage is replaced by group life
insurance from any carrier for which you are or become
eligible within the next 31 days.
• You apply and become covered for term life coverage
under the portability plan.
• With respect to a dependent spouse or partner, that
person is less than age 80.
• The dependent is covered for optional dependent
life coverage on the day your optional associate life
coverageends.
• The dependent is not confined for medical care or
treatment, at home or elsewhere, on the day your optional
associate life coverage ends.
Your spouse or partner may also apply for term life
coverage under the portability feature if they meet all of
these conditions:
• Your spouse or partner’s coverage ends due to divorce or
termination of partnership.
• Your spouse or partner is less than age 80.
• Your spouse or partner is not confined for medical care or
treatment, at home or elsewhere, on the day your optional
dependent life coverage ends.
Optional dependent life insurance
165
If you meet these conditions, you will have 31 days from
your termination date to contact Prudential and enroll.
Prudential will notify you of the amount of portability
coverage offered. The amount of insurance coverage
offered will not be more than the amount of spouse/
partner coverage you elected under the plan. However, if
your spouse or partner provides Proof of Good Health, and
Prudential accepts such proof, you may increase the amount
of your spouse or partner’s coverage by $20,000 (or, if less,
by your annual earnings amount).
Conversion is a required Plan provision that allows you to
convert your life insurance coverage to an individual policy
if coverage would end for any reason other than failure
to pay premiums or the end of dependent coverage for
all associates. Proof of Good Health is not required. Rates
are based on your dependent’s age and amount converted.
You have 31 days from the termination date of coverage to
request to convert your coverage to an individual policy. If
your dependent’s death occurs during the 31-day conversion
period, the death benefit will be payable up to the amount
that could have been converted.
If you are a resident of Minnesota, you have a continuation
right instead of a conversion right when you lose coverage
due to a reduction in your hours or termination of
employment (other than for gross misconduct). You may
elect to continue coverage at your expense until you
obtain coverage under another group life insurance policy;
however, the maximum period that coverage may be
continued is 18 months. If you continue coverage, at the
expiration of the continuation period, you may convert your
life insurance coverage to an individual policy, up to the
amount of coverage in effect at that time. You have 31 days
from the date continuation coverage would end to request
to convert your coverage to an individual policy. In addition,
if you lose coverage for any reason other than a reduction
in your hours or termination of employment (other than for
gross misconduct), you may convert up to the amount of
coverage that was in force under the plan.
To request information on portability or conversion, call
Prudential at 877-740-2116.
If you leave the company and
arerehired
If you return to work for the company within 13 weeks,
you will automatically be reenrolled for the same coverage
you had prior to leaving the company (or the most
similar coverage offered under the Plan). You can drop or
otherwise change this coverage at any time.
If you return to work after 13 weeks, you will be considered
newly eligible and will be required to complete the applicable
eligibility waiting period. Proof of Good Health is required
for spouse/partner coverage plans above $5,000 (or for any
amount if you enroll after your initial enrollment period). See
the Eligibility and enrollment chapter for details.
If you drop or decrease your
coverage and reenroll
If you drop or decrease your coverage and reenroll within
30 days, you may reenroll for the same coverage in effect
you had prior to dropping or decreasing coverage.
If you reenroll more than 30 days after dropping or
decreasing coverage, Proof of Good Health will be required
for spouse/partner coverage plans.
IF A DEPENDENT IS DROPPED FROM
COVERAGE AND REENROLLED
If your dependent child is dropped from coverage and then
determined to be eligible for coverage within 30 days, the
dependent will automatically be reenrolled in the same
coverage you elect for yourself.
If your dependent regains eligibility and is reenrolled after
30 days, they will be treated as a newly eligible dependent.
The associate may enroll them for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information is intended to be a summary of your benefits and may not include all policy provisions. If
there is a discrepancy between this document and the policy issued by Prudential regarding the calculation
of benefits and limitations under the policy, the terms of the policy will govern. You may obtain a copy of
this policy by contacting thePlan.
AD&D insurance 168
Naming a beneficiary 168
When your AD&D coverage begins 169
AD&D coverage amount 169
When AD&D benefits are paid 169
Additional AD&D benefits 170
Filing a claim 172
When benefits are not paid 172
Break in coverage 172
When coverage ends 172
If you leave the company and arerehired 173
If you drop or decrease your coverage and reenroll 173
Accidental death and
dismemberment
(AD&D) insurance

Accidental death and dismemberment (AD&D) insurance
167
Accidental death and dismemberment
(AD&D)insurance
AD&D benefits can help pay the cost of medical care, childcare, and education expenses if you’re
seriously injured or die in an accident.
RESOURCES
Find What You Need Online Other Resources
Change your beneficiary designation Go to One.Walmar.com
or Workday for Jet associates
Beneficiary changes cannot be made
over the phone
Get more details Call Prudential at 877-740-2116
File a claim Call Prudential at 877-740-2116
What you need to know about AD&D insurance
• If you are an hourly or management associate, you can enroll in AD&D insurance when you are eligible, as described
in the Eligibility and enrollment chapter.
• Proof of Good Health is not required for AD&D insurance, regardless of the coverage amount you choose.
• If you have a covered loss, AD&D insurance pays a lump sum benefit based on the nature of the loss and the coverage
amount you select. Additional benefits may be payable, depending on the circumstances of the covered loss.
• Coverage is provided through The Prudential Insurance Company of America (Prudential).

Accidental death and dismemberment (AD&D) insurance
168
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
AD&D insurance
AD&D insurance pays a lump sum benefit to you or your
beneficiary(ies) if you or a covered dependent experiences
a covered loss. The amount of your benefit depends on the
type of loss you experience, as described later in this chapter.
If you are an hourly or management associate, you can
enroll in AD&D insurance when you are eligible, as described
in the Eligibility and enrollment chapter. For details about
eligible job classifications, see the Enrollment and eligibility
dates by job classification charts in that chapter.
You have two AD&D coverage decisions. You choose whom
you want to cover and your coverage amount.
You can choose to cover:
• Associate only
• Associate + dependents
If you are a part-time hourly associate, temporary associate,
or part-time truck driver and you choose associate +
dependents coverage, you can cover your dependent
children but not your spouse/partner.
The coverage amount for your dependents will be a
percentage of the coverage amount you choose for
yourself (see AD&D coverage amount later in this chapter).
The amounts available for you to choose as your associate
coverage amount are:
• $25,000 • $100,000
• $50,000 • $150,000
• $75,000 • $200,000
Management associates may also choose the following
additional coverage amounts:
• $300,000 • $750,000
• $500,000 • $1,000,000
You can enroll in or make changes to your AD&D insurance
during your initial enrollment period, Annual Enrollment,
or when you have a status change event. For more
information, see the Eligibility and enrollment chapter.
The cost of AD&D insurance is based on the coverage
amount you select and whether you choose associate-only
or associate + dependents coverage.
Naming a beneficiary
To ensure that your AD&D benefit is paid according to your
wishes, you must name a beneficiary(ies). You may do this by
going to One.Walmart.com or Workday for Jet associates.
Note that only beneficiary designations made online are
accepted. You (the associate) will receive any benefits
payable for your covered dependents.
You can name anyone you wish. If the beneficiary(ies) you
list with Walmart differs from the beneficiary(ies) named
in your will, the list that Walmart has prevails. If you have
not designated a beneficiary(ies) under the AD&D benefit,
payment will be made to your surviving family surviving
family members as described under If you do not name a
beneficiary later in this chapter.
The following information is needed for each beneficiary:
• Name
• Current address and phone number
• Relationship to you
• Social Security number
• Date of birth, and
• The percentage you wish to designate per beneficiary,
upto 100%.
If two or more beneficiaries are designated and their shares
are not specified, they will share the insurance benefit equally.
If a named beneficiary dies before you, that beneficiary’s
interest will end, and it will be shared equally by any remaining
beneficiary(ies), unless your beneficiary form states otherwise.
You can name a minor as a beneficiary; however, Prudential
may not be legally permitted to pay the minor until the minor
reaches legal age. You may want to consult an attorney or an
estate planner before naming a minor as a beneficiary. If you
name a minor as a beneficiary, funeral expenses cannot be
paid from the minor’s beneficiary proceeds.
CHANGING YOUR BENEFICIARY
You can change your beneficiary(ies) at any time on
One.Walmart.com or Workday for Jet associates. Any
change in beneficiary must be completed and submitted to
Walmart before your death and can be submitted only by
you, the covered associate.
Be sure to keep your beneficiary information
up to date. Proceeds go to whoever is listed
on your beneficiary form with Walmart,
regardless of your current relationship with
that person, unless state law says otherwise.
You can change your beneficiary(ies) at any
time on One.Walmart.com or Workday for
Jetassociates.

Accidental death and dismemberment (AD&D) insurance
169
IF YOU DO NOT NAME A BENEFICIARY
If no beneficiary is named or there is no surviving
beneficiary at the time of your death, payment will be made
to surviving family members in the following order:
1. Spouse or partner of the deceased; if not surviving, then
2. Children in equal shares; if not surviving, then
3. Parents in equal shares; if not surviving, then
4. Siblings in equal shares, if not surviving, then
5. Your estate.
When your AD&D coverage begins
If you enroll during Annual Enrollment, your coverage
becomes effective on January 1 of the next year.
If you enroll outside of Annual Enrollment, your coverage
becomes effective on the date of the status change event or
the end of your eligibility waiting period, whichever is later.
Your AD&D coverage begins whether or not you are actively
at work, as long as you have reported for your first day of
work and enrolled for the benefit. See the Eligibility and
enrollment chapter for details.
AD&D coverage amount
When you enroll in AD&D insurance, the coverage amount
you select is the amount that applies to you, the associate.
If you enroll in associate + dependent(s) coverage, the
coverage amount for your dependent(s) is a percentage of
your associate coverage amount. The coverage amount for
your dependent(s) depends on the type of dependents you
are covering. See the Full benefit amount chart below for
information on the coverage amount for your familymembers.
When AD&D benefits are paid
If you have chosen associate + dependent(s) coverage and
you or your dependent sustains an accidental injury that is
the direct and sole cause of a covered loss, AD&D benefits
are paid when proof of the accidental injury and covered
loss have been properly provided to Prudential.
Prudential deems a loss to be the direct result of an
accidental injury if it results from unavoidable exposure
tothe elements.
“Direct and sole cause” means the covered loss occurs within
12 months of the date of the accidental injury and is a direct
result of the accidental injury, independent of other causes.
COVERED LOSSES PAID AT FULL BENEFIT
The following covered losses resulting from an accident are
payable at the full benefit:
• Loss of life: It will be presumed that you have suffered
a loss of life if your body is not found within one year of
disappearance, stranding, sinking, or wrecking of any
vehicle in which you were an occupant.
• Loss of both hands above the wrists; both feet above the
ankles; total and permanent loss of sight in both eyes; loss
of speech and hearing in both ears that lasts for at least six
consecutive months following the accident.
• Loss of one hand and one foot: Severance at or above the
wrist and ankle joints.
• Loss of one arm or one leg: Severance at or above the
elbow or above the knee.
• Loss of one hand or foot and sight in one eye: Severance at
or above the wrist or ankle joint, with total and permanent
loss of sight in one eye.
FULL BENEFIT AMOUNT
Associate coverage
amount
If a spouse/parner is the
only dependent covered
If both a spouse/parner and children are
covered dependents
If children are the
only dependents
Associate — 100% Spouse/parner — 50% Spouse/parner — 40% Children — 10% Children — 25%
$25,000 $12,500 $10,000 $2,500 $6,250
$50,000 $25,000 $20,000 $5,000 $12,500
$75,000 $37,500 $30,000 $7,500 $18,750
$100,000 $50,000 $40,000 $10,000 $25,000
$150,000 $75,000 $60,000 $15,000 $37,500
$200,000 $100,000 $80,000 $20,000 $50,000
Management associates only:
$300,000 $150,000 $120,000 $30,000 $75,000
$500,000 $250,000 $200,000 $50,000 $125,000
$750,000 $375,000 $300,000 $75,000 $187,500
$1,000,000 $500,000 $400,000 $100,000 $250,000
Accidental death and dismemberment (AD&D) insurance
170
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• Quadriplegia: Total paralysis of both upper and lower limbs.
• Paraplegia: Total paralysis of both lower limbs.
• Hemiplegia: Total paralysis of upper and lower limbs on one
side of the body.
50% OF FULL BENEFIT
The following covered losses resulting from an accident are
payable at 50% of full benefit:
• Brain damage: Brain damage means permanent and
irreversible physical damage to the brain, causing the
complete inability to perform all the substantial and
material functions and activities normal to everyday life.
Such damage must manifest itself within 30 days of the
accidental injury, require a hospitalization of more than
five consecutive days within 30 days of the accident, and
continue for 12 consecutive months.
• Loss of hand or foot: Severance at or above the wrist
orankle.
• Loss of sight in one eye: Total and permanent loss of sight
in one eye.
• Loss of speech or hearing in both ears: Total and
permanent loss of speech or hearing (i.e., continuing for at
least six consecutive months following the accident).
25% OF FULL BENEFIT
The following covered losses resulting from an accident are
payable at 25% of full benefit:
• Loss of hearing in one ear: Total and permanent loss of
hearing (i.e., continuing for at least six consecutive months
following the accident).
• Loss of thumb and index finger of the same hand:
Severance at or above the point at which they are attached
to the hand.
• Uniplegia: Total paralysis of one limb.
“Paralysis” means loss of use, without severance, of a limb.
A doctor must determine that the loss is complete and not
reversible. “Severance” means complete separation and
dismemberment of the limb from the body.
COMA BENEFIT
If you or a covered dependent is comatose or becomes
comatose within 365 days as the result of an accident, a
coma benefit equal to 1% of your full benefit amount is paid
for 11 consecutive months to you, your spouse/partner, your
children, or a legal guardian. The benefit is payable after
31 consecutive days of being comatose. If you or a covered
dependent remains comatose beyond 11 months, the full
sum of the coverage, less any AD&D benefit already paid, is
made to you or your designated beneficiary.
“Coma” means a profound state of unconsciousness from
which the comatose person cannot be aroused, even by
powerful stimulation, as determined by the person’s doctor.
Such state must begin within 365 days of the accidental
injury and continue for 31 consecutive days and is total,
continuous, and permanent at the end of the 31-day period.
The maximum amount that AD&D insurance will pay for all
covered losses of an individual resulting from a covered
accident is the full benefit amount.
Additional AD&D benefits
Additional benefits may be payable by the Plan:
• Seat belt benefit: If you and/or your covered dependents
suffer a loss of life as a result of a covered accident that
occurs while wearing a seat belt, an additional benefit
maybe payable.
• Safe motorcycle rider benefit: If you and/or your covered
dependents suffer a loss of life as a result of a covered
accident that occurs while wearing a helmet, an additional
benefit may be payable.
• Spouse/partner education benefit (full-time hourly and
management associates only): If you (the associate)
suffer a loss of life, a spouse/partner education benefit
maybepayable.
• Child education and care benefit: If you (the associate)
or your covered spouse/partner suffers a loss of life,
a childcare benefit and/or child education benefit
maybepayable.
• Home alteration and vehicle modification benefit: If
you or your covered dependents suffer a covered loss
that requires home alteration or vehicle modification,
anadditional benefit may be payable.
• COBRA monthly medical premium benefit: If you (the
associate) suffer a covered accidental bodily injury which
results in your death or a termination after a leave of
absence, an additional benefit may be payable to assist with
the continuation of medical benefits under the Associates’
Medical Plan.
• Monthly rehabilitation benefit: If you or your covered
dependents suffer a covered accidental bodily injury that
requires medically necessary rehabilitation, an additional
benefit may be payable.
• Common accident benefit: If you (the associate) or your
covered spouse/partner both suffer a loss of life due to the
same accident or accidents that occur within 48 hours of
each other, a common accident benefit may be payable.
All additional AD&D benefits are subject to eligibility
criteria established by Prudential. Contact Prudential for
information if any of these benefits might apply to you.

Accidental death and dismemberment (AD&D) insurance
171
ADDITIONAL BENEFITS
Benefit Benefit amount Limitations
Seat belt benefit $10,000 If it cannot be determined that the person was wearing a
seat belt at the time of the accident, a benefit of $1,000
will be paid.
Safe motorcycle
riderbenefit
$10,000 If it cannot be determined that the person was wearing
the necessary safety equipment at the time of the
accident, a benefit of $1,000 will be paid.
Education benefit
forspouse/parner
An amount equal to the least of:
• The actual tuition charged for the program;
• 10% of your (the associate’s) amount of
insurance; and
• $25,000
Payable for up to 4 years.
Full-time hourly and management associates only.
Education benefit
forchild
An amount equal to the least of:
• The actual annual tuition, exclusive of room
and board, charged by the school;
• 10% of the amount of insurance on the
person incurring the loss; and
• $25,000
Payable annually for up to 4 consecutive years, but not
beyond the date the child reaches age 26.
Childcare benefit An amount equal to the least of:
• The actual cost charged by a childcare
center per year;
• 10% of the amount of insurance on the
person incurring the loss; and
• $12,500
Payable annually for up to 5 consecutive years, but not
beyond the date the child reaches age 13.
Home alteration
and vehicle
modification
benefit
An amount equal to the least of:
• The actual cost charged for the alteration or
modification;
• 10% of the amount of insurance on the
person incurring the loss; and
• $10,000
Payable for an amount no greater than $10,000.
COBRA premium
benefit for
associate
An amount equal to the least of:
• The amount of the medical premium;
• 5% of your (the associate’s) amount of
insurance; and
• $500
Payable monthly until the first of these occurs:
• Your continued enrollment in the AMP ends
• You become covered under any other group medical plan
• The benefit has been paid for 36 consecutive months
COBRA premium
benefit for
dependent
An amount equal to the lesser of:
• The actual amount of the medical premium;
and
• $10,000
Payable yearly until the first of these occurs:
• Your dependent’s continued enrollment in the AMP ends
• Your dependent becomes covered under any other
group medical plan
• The benefit has been paid for 3 consecutive years.
A benefit for spouse/parner premiums is only available to
full-time hourly and management associates only.
Monthly
rehabilitation
benefit
An amount equal to the lesser of:
• 10% of the amount of insurance on the
person incurring the loss; and
• $250
Payable monthly until the first of these occurs:
• A doctor determines the person no longer needs
rehabilitation
• The person fails to furnish any required proof of a
continuing need for rehabilitation
• The person fails to submit to a required medical exam
• The benefit has been paid for 36 consecutive months
Common accident
benefit
An amount equal to the difference between:
• The amount of insurance payable under the
coverage for your loss of life; and
• The amount of insurance payable under
the coverage for your spouse or domestic
parner’s loss of life
Accidental death and dismemberment (AD&D) insurance
172
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Filing a claim
The following information must be provided to Prudential
regarding the claimant:
• Name
• Social Security number
• Date of death or injury, and
• Cause of death or injury (if known).
Prudential will send a claim packet to your address on file.
The required information must be completed and returned
with the claim forms and an original or certified copy of the
death certificate, when applicable, to:
The Prudential Insurance Company of America
Group Claim Life Division
P.O. Box 8517
Philadelphia, Pennsylvania 19176
Benefits are paid in a lump sum. If you or a covered
dependent sustains more than one covered loss due to an
accidental injury, the amount paid, on behalf of any such
injured person, will not exceed the full amount of the benefit.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter. You
or your beneficiary has the right to appeal a claim denial.
When benefits are not paid
AD&D benefits are not paid for any loss that occurs prior
to your enrollment in the Plan, nor any loss caused or
contributed to by the following:
• Suicide or attempted suicide, while sane or insane
• Intentionally self-inflicted injuries, or any attempt to inflict
such injuries
• Sickness, whether the loss results directly or indirectly
from the sickness
• Medical or surgical treatment of sickness, whether the loss
results directly or indirectly from the treatment
• Bacterial or viral infection, but not including:
– Pyogenic infection resulting from an accidental cut or
wound, or
– Bacterial infection resulting from accidental ingestion
ofa contaminated substance.
• Taking part in any insurrection
• War, declared or undeclared, or any act of war
• An accident that occurs while the person is serving on
full-time active duty for more than 30 days in any armed
forces (not including Reserve or National Guard active
duty for training)
• Travel or flight in any vehicle used for aerial navigation if
you are riding as a passenger in any aircraft not intended
or licensed for the transportation of passengers (including
getting in, out, on, or off such vehicle)
• Commission or attempted commission of an assault
orfelony
• Operating a land, water, or air vehicle while being legally
intoxicated, or
• Being under the influence of or taking any controlled
substance as defined in Title II of the Comprehensive
Drug Abuse Prevention and Control Act of 1970, and
all amendments, unless prescribed by and administered
inaccordance with the advice of the insured’s doctor.
Break in coverage
There may be occasions in which you must make special
arrangements to pay your AD&D insurance premiums to
avoid a break in coverage. These situations occur most
commonly if you are on a leave of absence or if your
Walmart paycheck is not sufficient to pay your full share
of the cost of coverage (such as after a reduction in
hours). Depending on your circumstances, failure to make
your premium payments by the due date may result in an
interruption in the payment of any benefit claims and/or
abreak in coverage.
For details on the impact a break in coverage may have,
and on how to make personal payments to continue your
coverage, see When special arrangements are necessary to
maintain coverage in the Eligibility and enrollment chapter.
IF YOU GO ON A LEAVE OF ABSENCE
You may continue your coverage up to the last day of an
approved leave of absence, provided that you pay your
premiums before or during the leave. For information
aboutmaking payments while on a leave of absence, see
When special arrangements are necessary to maintain
coverage in the Eligibility and enrollment chapter.
When coverage ends
Your AD&D coverage ends:
• At termination of your employment
• Upon failure to pay your premiums
• On the date of your death
• On the date you or a dependent spouse/partner or child
loses eligibility
• On the last day of an approved leave of absence (unless
you return to work), or
• When the benefit is no longer offered by the company.
AD&D coverage cannot be converted to individual
coverage after coverage ends.
Accidental death and dismemberment (AD&D) insurance
173
In addition, if you have chosen associate + dependent(s)
coverage and your job status changes to part-time hourly
associate, temporary associate, or part-time truck driver,
your coverage for your spouse/partner will end on the last
day of the pay period when your job status changes.
If you leave the company and
arerehired
If you return to work for the company within 13 weeks, you
will automatically be reenrolled for the same coverage in
effect prior to leaving the company (or the most similar
coverage offered under the Plan). If your break is greater
than 30 days but less than 13 weeks, you will have 60 days
after resuming employment to drop or otherwise change
the coverage in which you were automatically reenrolled.
If you return to work after 13 weeks, you will be considered
newly eligible and will be required to complete the
applicable eligibility waiting period.
See the Eligibility and enrollment chapter for details.
If you drop or decrease your
coverage and reenroll
If you drop or decrease your coverage and reenroll within
30 days, you may reenroll for the same coverage in effect
prior to dropping or decreasing coverage.
If you reenroll more than 30 days after dropping or
decreasing coverage, you may enroll for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.
IF A DEPENDENT IS DROPPED FROM
COVERAGE AND REENROLLED
If your dependent child is dropped from coverage and then
determined to be eligible for coverage within 30 days, the
dependent will automatically be reenrolled in the same
coverage you elect for yourself.
If your dependent regains eligibility and is reenrolled after
30 days, they will be treated as a newly eligible dependent.
The associate may enroll them for coverage under the
time periods and conditions described in the Eligibility and
enrollment chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information is intended to be a summary of your benefits and may not include all policy provisions. If
there is a discrepancy between this document and the policies issued by the applicable insurers under this
chapter regarding the calculation of benefits and limitations under the policies, the terms of the policies will
govern. You may obtain a copy of these policies by contacting the Plan.
Business travel accident insurance 176
Naming a beneficiary 176
Filing a claim 177
When benefits are paid 177
Additional benefits 178
When benefits are not paid 178
When coverage ends 179
If you leave the company and arerehired 179
International business travel medicalinsurance 179
Business travel
accident insurance

Business travel accident insurance
175
Business travel accident insurance
When you’re traveling on authorized company business, this insurance protects you and your
loved ones financially if you have an accident resulting in cerain types of injury or death.
RESOURCES
Find What You Need Online Other Resources
Change your beneficiary designation Go to One.Walmar.com
or Workday for Jet associates
Beneficiary changes cannot be made
over the phone
Get more details Call Prudential at 877-740-2116
File a business travel accident insurance claim Call Prudential at 877-740-2116
Get more details about international business
travel medical insurance through GeoBlue
Go to geo-blue.com Call GeoBlue at 888-412-6403
Outside the U.S. call 610-254-5830
What you need to know about business travel accident insurance
• Walmart provides all associates with business travel accident insurance. There is no cost to you and no enrollment
isnecessary.
• Business travel accident insurance pays a benefit for loss of life, limb, sight, speech, or hearing, or paralysis, due to an
accident you are involved in while traveling on authorized company business.
• Your coverage amount for accidents while traveling is three times your base annual earnings to a maximum of $1 million.
• This company-paid insurance is provided through The Prudential Insurance Company of America (Prudential).
• International business travel medical insurance is available for eligible business travelers through GeoBlue.

Business travel accident insurance
176
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Business travel accident insurance
To protect you while you travel on company business,
Walmart provides all associates with business travel accident
insurance. There is no cost to you and no enrollment is
necessary. Coverage is effective on your first day of active
work, as described in the Eligibility and enrollment chapter.
If you experience a covered injury resulting in loss or
death while traveling on authorized company business, a
lump-sum benefit is payable to you or your beneficiary(ies)
of upto three times your base annual earnings, with a
maximum of $1 million and minimum of $200,000 (unless
otherwisespecified).
Base annual earnings is defined as follows:
• For hourly associates: Annualized hourly rate as shown in
the Walmart payroll system as of date of loss or death.
• For management associates and officers: Base salary as
shown in the Walmart payroll system as of date of loss
ordeath.
• For truck drivers: Annualized average day’s pay as of date
of loss or death, as determined by Logistics Finance.
Note that any bonus you may receive is not included in base
annual earnings.
Naming a beneficiary
To ensure that your business travel accident insurance
benefit is paid according to your wishes, you must
name a beneficiary(ies). You may do this by going to
One.Walmart.com or Workday for Jet associates. Note that
only beneficiary designations made online are accepted.
You (the associate) will receive any benefits payable for the
injuries listed in When business travel accident insurance
benefits are paid later in thischapter.
You can name anyone you wish. If the beneficiary(ies) you
list with Walmart differs from the beneficiary(ies) named
in your will, the list that Walmart has prevails. If you have
not designated a beneficiary(ies) under the business travel
accident benefit, payment will be made to your surviving
family members as described under If you do not name a
beneficiary later in this chapter.
The following information is needed for each beneficiary:
• Name
• Current address and phone number
• Relationship to you
• Social Security number
• Date of birth, and
• The percentage you wish to designate per beneficiary,
upto 100%.
If two or more beneficiaries are designated and their
shares are not specified, they will share the insurance
benefit equally. If a named beneficiary dies before you, that
beneficiary’s interest will end, and it will be shared equally
by any remaining beneficiary(ies), unless your beneficiary
form states otherwise. If you and a beneficiary die in the
same event and it cannot be determined who died first, the
beneficiary will be treated as having died before you.
You can name a minor as a beneficiary; however, Prudential
may not be legally permitted to pay the minor until the
minor reaches legal age. You may want to consult an
attorney or an estate planner before naming a minor as a
beneficiary. If you name a minor as a beneficiary, funeral
expenses cannot be paid from the minor’s beneficiary
proceeds.
CHANGING YOUR BENEFICIARY
You can change your beneficiary(ies) at any time on
One.Walmart.com or Workday for Jet associates. Any
change in beneficiary must be completed and submitted to
Walmart before your death and can be submitted only by
you, the covered associate.
IF YOU DO NOT NAME A BENEFICIARY
If no beneficiary is named or there is no surviving
beneficiary at the time of your death, payment will be made
to your surviving family members in the following order:
1. Spouse or partner of the deceased; if not surviving, then
2. Children in equal shares; if not surviving, then
3. Parents in equal shares; if not surviving, then
4. Siblings in equal shares; if not surviving, then
5. Your estate.
Be sure to keep your beneficiary information
up to date. Proceeds will go to whoever is
listed on your beneficiary form with Walmart,
regardless of your current relationship with
that person, unless state law says otherwise.
You can change your beneficiary(ies) at any
time on One.Walmart.com or Workday for
Jetassociates.

Business travel accident insurance
177
Filing a claim
Within 12 months of the covered associate’s injury or death
or within 90 days after any periodic payment is due (such
as periodic payments for coma), the following information
must be provided regarding the associate:
• Name
• Social Security number
• Occurrence, character, and extent of the injury
• Date of injury or death, and
• Cause of injury or death (if known).
An original or certified copy of the death certificate is
required as proof of death. The death certificate should be
mailed to:
The Prudential Insurance Company of America
Group Life Claim Division
P.O. Box 8517
Philadelphia, Pennsylvania 19176
The claim will not be finalized until Prudential receives the
death certificate, where applicable. Acceptance of the
death certificate is not a guarantee of payment.
Benefits can be paid in a lump sum or, upon written request,
in monthly installments. Only one benefit, the highest, will
be paid if you suffer more than one loss resulting from a
single accident.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter.
Your beneficiary(ies) has the right to appeal a claim denial.
Benefits are paid according to the terms of the insurance
policy. For details, contact Prudential at 877-740-2116.
When benefits are paid
Benefits are paid if you sustain an accidental injury while
traveling on authorized company business or due to a
felonious assault while you are working; your injuries
are the direct and sole cause of a covered loss; and you
properly provide proof of the accidental loss and covered
loss to Prudential.
Traveling for business includes travel using a common
carrier or any means of transportation owned and operated
by the company. An accidental injury includes exposure to
the elements. “Direct and sole cause” means the covered
loss occurs within 12 months of the date of the accidental
injury and is a direct result of the accidental injury,
independent of other causes.
BENEFIT AMOUNT
COVERED INJURY OCCURS… BENEFIT AMOUNT
While traveling on authorized
company business
Three times your
base annual earnings
to a maximum of
$1,000,000
Minimum benefit:
$200,000
Due to a felonious assault while
you are working
Up to $10,000
COVERED LOSSES PAID AT FULL BENEFIT
• Quadriplegia: Total paralysis of both upper and lower limbs.
• Paraplegia: Total paralysis of both lower limbs.
• Hemiplegia: Total paralysis of upper and lower limbs on one
side of the body.
• Loss of both hands, both feet, or sight in both eyes:
Severance through or above both wrists or both ankle
joints, or total and irrecoverable loss of sight.
• Loss of one hand and one foot: Severance through or
above the wrist or ankle joint.
• Loss of speech and hearing in both ears: Total loss of
speech and hearing that lasts for at least six consecutive
months following the accident.
• Loss of hand or foot and sight in one eye: Severance
through or above the wrist or ankle joint, with total and
irrecoverable loss of sight in one eye.
50% OF FULL BENEFIT
• Loss of hand or foot: Permanent severance through
or above the wrist but below the elbow, or permanent
severance at or above the ankle but below the knee.
• Brain damage: Brain damage means permanent and
irreversible physical damage to the brain, causing the
complete inability to perform all of the substantial
and material functions and activities of everyday life.
Such damage must manifest itself within 30 days of the
accidental injury, require hospitalization of at least five
days and persist for 12 consecutive months.
• Loss of sight in one eye: Total and permanent loss of sight
in one eye.
• Loss of speech or hearing in both ears: Total loss of speech
or hearing that lasts for at least six consecutive months
following the accident.
Business travel accident insurance
178
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
25% OF FULL BENEFIT
• Loss of thumb and index finger of the same hand:
Severance of each through or above the joint closest to
the wrist.
• Uniplegia: Total paralysis of one limb.
“Paralysis” means loss of use, without severance, of a limb.
A doctor must determine that the loss is complete and not
reversible. (“Severance” means complete separation and
dismemberment of the limb from the body.)
COMA BENEFIT
If you are comatose or become comatose within 365 days
as the result of a covered accident, a monthly coma benefit
equal to the greater of 2% of your full benefit amount or
$100 is paid for up to 50 months. The benefit is payable
after 31 consecutive days of being comatose.
“Coma” means a profound state of unconsciousness from
which the comatose person cannot be aroused, even by
powerful stimulation, as determined by the person’s doctor.
Such state must begin within 365 days of the accidental
injury and continue for 31 consecutive days and is total,
continuous, and permanent at the end of the 31-day period.
The maximum amount the business travel accident
insurance will pay you for all covered losses resulting from
a covered accident is the full benefit amount. If more than
one associate suffers a loss as a result of the same accident,
the maximum the business travel accident insurance policy
will pay for all losses is $10 million per accident and, if
necessary, benefits will be prorated among the affected
associates suffering a loss in the accident. The maximum
total payment is increased to $20 million if the covered
accident occurs while you are traveling to or from, or while
you are attending, Walmart’s Annual Shareholders Meeting,
annual holiday meeting, or annual year beginning meeting.
Additional benefits
Business travel accident insurance provides these
additional benefits:
• Seat belt benefit: If you suffer a loss of life as a result of a
covered accident that occurs while wearing a seat belt, an
additional benefit of up to $10,000 may be payable.
• Airbag benefit: If you suffer a loss of life as a result of a
covered accident that occurs while you are wearing a seat
belt and a properly functioning airbag deploys in the seat
you were occupying, an additional benefit of up to $10,000
may be payable.
• Funeral expenses benefit: If you suffer a loss of life within
365 days of and as a result of a covered accident, an
additional benefit of up to $5,000 may be payable.
• Medical evacuation benefit: If, as a result of a covered
accident, you require medical evacuation and are at least
100 miles from your home, an additional benefit of up to
$15,000 may be payable.
• Family relocation and accompaniment: If your spouse or
partner or dependent child suffers a covered loss while
traveling with you on business (or while on their way to
meet you), an additional benefit of up to $100,000 may be
payable for losses sustained by your spouse or partner, and
$10,000 for losses sustained by each dependent child.
All of these additional benefits are subject to additional
eligibility criteria established by Prudential. Please
contact Prudential if any of these benefits might apply for
additional information.
When benefits are not paid
Business travel accident insurance benefits will not be paid
for for any loss that results from any of the following:
• Suicide or attempted suicide, while sane or insane
• Intentionally self-inflicted injuries, or any attempt to inflict
such injuries
• Sickness, whether the loss results directly or indirectly
from the sickness
• Medical or surgical treatment of sickness, whether the loss
results directly or indirectly from the treatment
• Any bacterial or viral infection, except a pyogenic
infection resulting from an accidental cut or wound or a
bacterial infection resulting from accidental ingestion of a
contaminated substance
• War or act of war (declared or undeclared), including
resistance to armed aggression or an accident while on
full-time active duty with the armed services for more than
30 days (this does not include Reserve or National Guard
active duty for training)
• Riding in an unlicensed aircraft
• Flying as a crew member of an airplane, except one owned
and operated by the company
• Commission or attempted commission of an assault
orfelony
• Operating a land, water, or air vehicle while being legally
intoxicated, or
• Being under the influence of or taking any controlled
substance as defined in Title II of the Comprehensive
Drug Abuse Prevention and Control Act of 1970, and all
amendments, unless prescribed by and administered in
accordance with the advice of the insured’s doctor.
Business travel accident insurance
179
When coverage ends
Your business travel accident insurance coverage ends on
your last day of employment.
If you leave the company and
arerehired
Your business travel accident insurance coverage
(orthemost similar coverage offered under the Plan)
willbereinstated.
International business travel
medicalinsurance
International business travel medical insurance is available
through a policy with GeoBlue for associates who travel
internationally for business.
GeoBlue provides travel assistance services to you and
your eligible dependents if you require emergency medical
treatment while traveling on company-authorized business.
Walmart pays for this coverage in full — there is no cost
to you and no enrollment is necessary. Coverage is valid
for a trip lasting up to 180 days. Coverage is not available
for personal travel even when you add personal travel to a
business trip.
You are not eligible to make health savings account
contributions for any month in which you are traveling
on Walmart business outside the U.S. and are covered
under the GeoBlue policy. If you have medical coverage
under the Saver Plan, you are encouraged to consult
with yourtax advisor if you have questions about the
amount to reduce your HSA contributions based on your
individualcircumstances.
GEOBLUE SERVICES
Business travel medical insurance through GeoBlue provides
coverage for emergency medical treatment including
hospitalization, doctor visits, and prescription drug
coverage (not including over-the-counter medication).
GeoBlue has a network of doctors, physicians, and
medical facilities in over 180 countries and can also make
appointments on your behalf and arrange for direct billing.
Associates are advised to contact GeoBlue Customer
Service at 888-412-6403 before obtaining medical
treatment to ensure that the treatment is covered.
GeoBlue provides the following services:
• Reimbursement for eligible medical expenses
• Assistance in location of physician, medical facilities, and
making medical appointments
• Direct billing and payment guarantees
• Coordination for emergency medical evacuation to the
nearest appropriate medical facility for the associate and
an accompanying family member(s), and
• Repatriation of remains.
If you incur eligible medical expenses, submit them to
GeoBlue for reimbursement. They should not be charged to
the corporate credit card or submitted for reimbursement
through the travel and expense system.
Associates are advised to register on geo-blue.com
before their business travel, using group access code
QHG99999WALM. By registering, you gain access to
services and benefits including:
• Ability to print out your insurance ID card in case yours
is lost
• Doctor/facility locator
• Symptom checker
• Translate medical terms and medications, and
• Information about health and security risks.
Downloading the GeoBlue app: Once you’ve registered,
download the GeoBlue app and log in with the email address
and password you create when you register on the website.
The app provides you with convenient access to your ID
card and GeoBlue’s self-service tools including mapping
to your nearest approved medical facility/provider, making
appointments, etc.
GeoBlue member ID cards: Cards carry the Blue Cross Blue
Shield logo and are available in your travel department.
Additional or replacement cards can be downloaded via
geo-blue.com.
Claims: Claim forms are generally not required for GeoBlue
services. However, if you have a question about your
benefits or disagree with the benefits provided, you may
contact GeoBlue or file a claim. To submit a claim via email
or fax, download a claim form and view detailed instructions
in the Member Hub at geo-blue.com. Submit your claim by
email to claims@geo-blue.com or by fax to 610-482-9623.
You may also submit claims by post. Download a claim form
from the Member Hub at geo-blue.com and send your
completed form to:
GeoBlue
Claims Department
P.O. Box 1748
Southeastern, Pennsylvania 19399-1748
Claims and appeals are determined under the time frames
and requirements set out in the GeoBlue policy. Contact
GeoBlue at any time by calling 888-412-6403. Outside the
U.S. call collect: 610-254-5830.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Shor-term disability for full-time hourly associates 182
How shor-term disability isadministered 182
Your shor-term disability benefit 183
When you qualify for benefits 183
Filing a claim 184
When benefits are not paid 184
When benefits begin 185
Calculating your benefit 185
When shor-term disability benefit payments end 187
Returning to work 187
Coverage during a leave of absence or temporary layoff 188
When coverage ends 188
If you leave the company and arerehired 188
If you lose and then regain eligibility 188
Shor-term disability
for full-time hourly
associates

Shor-term disability for full-time hourly associates
181
Shor-term disability for full-time hourly associates
If pregnancy, a scheduled surgery, or an unexpected illness or injury keeps you off the job for an
extended period, this plan for full-time hourly associates can protect par of your paycheck. When
you can’t work, the Walmar shor-term disability plan works for you.
RESOURCES
Find What You Need Online Other Resources
To request a leave Go to One.Walmar.com Call Sedgwick at 800-492-5678
To file a claim or get more information
(all states except California and
RhodeIsland)
If you work in California
If you work in Rhode Island
Go to One.Walmar.com
Go to edd.ca.gov
Go to dlt.ri.gov/tdi
Call Sedgwick/Lincoln at 800-492-5678
Call the state of California at 800-480-3287
Call the state disability carrier at 401-462-8420
If you work in Washington
(to file a state benefit claim)
Go to paidleave.wa.gov Call the state of Washington at 833-717-2273
What you need to know about shor-term disability for full-time
hourlyassociates
• Walmart offers its short-term disability basic plan to eligible full-time hourly associates at no cost to you. Eligible
associates are enrolled in the plan automatically after your 12-month waiting period. During your initial enrollment
period, you can also enroll in the short-term disability enhanced plan. For details about your enrollment period, see
the Eligibility and enrollment chapter.
• If you are an hourly full-time associate who works in California, Hawaii, New Jersey, or Rhode Island, which have
legally mandated plans, you are not eligible for Walmart’s short-term disability coverage.
• In addition to the states named above, certain other states and local governments (currently New York and
Washington) also have legally mandated plans, but Walmart extends its short-term disability coverage options
to full-time hourly associates in these other states and localities in order to supplement their state and local
government disability benefits.
• Walmart’s short-term disability basic plan replaces 50% of your income as an eligible associate up to a maximum
of $200 per week. The short-term disability enhanced plan replaces 60% of your income with no weekly maximum
(theNew York short-term disability enhanced plan has a maximum of $6,000 per week).
• If you are eligible to participate and enroll in the short-term disability enhanced plan during your initial enrollment
period, your coverage begins on your effective date, as described in the Eligibility and enrollment chapter. If you
enroll in the short-term disability enhanced plan at any time other than during your initial enrollment period, your
short-term disability enhanced plan coverage will not begin until you complete a 12-month waiting period.

Shor-term disability for full-time hourly associates
182
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Shor-term disability for full-time
hourly associates
If you are a full-time hourly associate (except for associates
in certain states and local governments with legally
mandated plans, as noted below), you are automatically
enrolled for coverage in the short-term disability basic plan
after your 12-month eligibility waiting period. During your
initial enrollment period, you also have the opportunity
to enroll in the short-term disability enhanced plan. For
details about your enrollment period, see the Eligibility and
enrollment chapter.
The short-term disability basic plan is provided by the
company at no cost to you. Your cost for the short-term
disability enhanced plan is based on your biweekly earnings
and your age.
See Legally mandated plans later in this chapter for details
about coverage options available to associates in states and
localities with legally mandated plans.
Except in certain states and localities (as noted in Legally
mandated plans below), Walmart’s short-term disability
coverage is self-insured. This means no insurance company
collects premiums and pays benefits. The company funds
benefits under the short-term disability basic plan by using
the company’s general assets, assets of the Plan or Trust,
or through a combination of these sources. No associate
contributions are required for the short-term disability
basic plan. If you participate in the short-term disability
enhanced plan, your contributions are intended to cover the
costs of benefits.
How shor-term disability
isadministered
Walmart’s short-term disability coverage is administered by
Sedgwick Claims Management Services, Inc. (Sedgwick) in all
states and localities except those with legally mandated plans.
Details follow regarding disability coverage available for
associates in states and localities with legally mandated plans.
LEGALLY MANDATED PLANS
For associates who work in states and localities with legally mandated plans, differences in state and local laws and administrative
procedures will affect your eligibility to paricipate in Walmar’s shor-term disability plans and the amount of your disability
benefit. General information can be found in the char below. Call the appropriate number listed in the Resources char at the
beginning of this chapter for details about benefits in these states.
Legally mandated and
administered plans
California
Rhode Island
Associates in these states are not eligible to paricipate in Walmar’s shor-term disability plans
for hourly associates. Their benefit is administered by the state.
Legally mandated plans,
administered by Lincoln
Financial Group (“Lincoln”)
Hawaii
New Jersey
Associates in these states are not eligible to paricipate in Walmar’s shor-term disability
plans for hourly associates. Their benefit is provided in accordance with the state program and
administered by Lincoln.
New York
Associates in New York are eligible to paricipate in Walmar’s shor-term disability basic plan
and New York shor-term disability enhanced plan to supplement their state benefit, which is
insured and administered by Lincoln.
Legally mandated plans,
administered by Sedgwick
See page 331
All other states
Associates in other states and localities with legally mandated benefits are eligible to paricipate
in Walmar’s shor-term disability plans to supplement their state or local benefits, which
areadministered by Sedgwick.
Associates who work in Washington will have the opporunity to enroll in the shor-term
disability enhanced plan to supplement their state benefits. To be eligible to receive benefits
under the Walmar shor-term disability plans, you must apply through the state or local
government for your legally mandated benefits, as permitted by law. The amount of the
benefit under Walmar’s shor-term disability plans will be reduced by the amount of the legally
mandated benefit. The total benefits payable under the Walmar shor-term disability plans will
not exceed the level of benefits otherwise payable under the plans.

Shor-term disability for full-time hourly associates
183
Your shor-term disability benefit
If you become disabled as defined by the Plan, Walmart’s
short-term disability basic plan provides up to 50% of your
average weekly wage for up to 25 weeks of an approved
disability, after a waiting period of seven calendar days. The
maximum weekly benefit under the short-term disability
basic plan is $200. For more information about your average
weekly wage, see Calculating your short-term disability
benefit later in this chapter.
If you become disabled as defined by the Plan, the short-
term disability enhanced plan provides up to 60% of your
average weekly wage for up to 25 weeks after a waiting
period of seven calendar days, with no maximum weekly
benefit. For participants who work in New York, the New
York short-term disability enhanced plan provides up to
60% of your average weekly wage for up to 25 weeks after
a waiting period of seven calendar days if you become
disabled as defined by the Plan, and has a $6,000 maximum
weekly benefit.
ENROLLMENT FOR SHORTTERM
DISABILITYBENEFITS
You are automatically enrolled in the short-term disability
basic plan after your 12-month eligibility waiting period.
You must be actively at work for your coverage to become
effective. You are considered actively at work on a day that
is one of your scheduled work days if you are performing in
the usual way all the duties of your job. See the Eligibility
and enrollment chapter for details.
The date your short-term disability enhanced plan coverage
begins depends on when you enroll for coverage:
• If you enroll during your initial enrollment period, your
coverage begins on your effective date. See the Eligibility
and enrollment chapter for information on your initial
enrollment period and your effective date.
• If you enroll after transferring from one job classification
to another, your coverage begins on your effective date.
See the Eligibility and enrollment chapter for details about
your transition enrollment period and your effective date.
• If you enroll at any time after your initial enrollment period
as a late enrollee, you are required to finish a 12-month
waiting period before your coverage is effective. You are
not required to pay short-term disability enhanced plan
premiums during your 12-month waiting period.
– If your late enrollment is due to a status change event,
your 12-month waiting period begins as of the date of
the event.
– If your late enrollment is during an Annual Enrollment,
your 12-month waiting period begins as of the date
you enroll.
You may drop your short-term disability enhanced plan
coverage at any time; the change is effective the day after
you drop coverage. If you drop your short-term disability
enhanced plan coverage and later decide to reenroll, you will
be treated as a late enrollee with a 12-month waiting period.
See page 298
When you qualify for benefits
To qualify for short-term disability benefits through the
Plan, you must meet the following requirements:
• You must be actively at work at the time of your disability
(except in certain cases of leave of absence or layoff, as
described later in this chapter under Coverage during a
leave of absence or temporary layoff).
• You must submit medical evidence provided by a qualified
doctor that you are disabled as defined by the Plan
(qualified doctors are legally licensed physicians and
practitioners who are not related to you and who are
performing services within the scope of their licenses,
including medical doctors [M.D.], osteopaths [D.O.], nurse
practitioners, physician’s assistants, psychologists, or
other medical practitioners whose services are eligible
for reimbursement by the Associates’ Health and Welfare
Plan).
• You must receive approval by Sedgwick or Lincoln of
your claim.
These conditions apply whether you are covered under
the short-term disability basic plan, enhanced plan, or
New York short-term disability enhanced plan. Sedgwick
or Lincoln may require written proof of your disability or
additional information before making a decision on your
claim. A statement by your physician that you are unable to
work does not by itself qualify you for short-term disability
benefits. Approval of a medical leave of absence does not
constitute approval for short-term disability benefits.
As defined by the Plan, “disabled” or “disability” means
that you are unable to perform the essential duties of your
job for your normal work schedule, or a license required
for your job duties has been suspended due to a mental
or physical illness or injury, or pregnancy. Benefits are
payable during a loss of license only while you are disabled
and pursuing reinstatement of your license on a timely
basis. Timely pursuit of reinstatement means you apply
for reinstatement when your condition meets the criteria
and you provide information and forms requested by the
licensing agency on a timely basis until your license is
reinstated. The determination of whether you are disabled
is made by Sedgwick (or Lincoln, as applicable) on the basis
of objective medical evidence, which consists of facts
and findings, including X-rays, laboratory reports, tests,
consulting physician reports as well as reports and chart
notes from your physician. In addition, you must be under

Shor-term disability for full-time hourly associates
184
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
the continuous care of a qualified doctor and following the
course of treatment prescribed. Loss of license by itself is
not sufficient for meeting the definition of disability.
If Sedgwick or Lincoln requests that you be examined by an
independent physician or other medical professional, you
must attend the exam to be considered for benefits.
If your disability is the result of more than one cause, you
will be paid as if they were one. The maximum benefit for
any one period of disability is limited to 25 weeks, after the
initial waiting period of seven calendar days.
If your disability is due to pregnancy, you will be deemed
to meet the definition of disability, and Sedgwick (or
Lincoln, as applicable) will not require objective medical
evidence as a condition for approving your disability claim
for the short-term disability maternity benefit, except in
the following situations:
• You begin your leave of absence more than two weeks
before your estimated delivery date, or
• You do not begin your leave of absence immediately after
your delivery date.
The maternity benefit generally begins on the earlier
of two weeks before your estimated delivery date (as
determined by a qualified doctor) or no later than your
actual delivery date.
If your disability is caused by a mental illness
or substance abuse, you are encouraged
to seek treatment within 30 days from the
first date of absence from a psychologist,
psychiatrist, or clinical social worker who
holds a Master of Social Work (M.S.W.),
specializes in mental health and substance
abuse, and is licensed pursuant to state law.
Filing a claim
Claims for short-term disability benefits in Hawaii, New
Jersey, and New York must be submitted to Sedgwick within
30 days of the date your disability begins. Sedgwick will
notify Lincoln of your disability claim.
For all other states, you must submit your short-term
disability claim to Sedgwick within 90 days of the date your
disability begins. Claims filed later than 90 days after the
date of disability may be denied unless Sedgwick determines
you had good cause for filing late.
If you experience a disabling illness or injury, or are
scheduled to begin maternity leave, follow these steps:
STEP 1: Notify Sedgwick to apply for a leave of absence
and file a short-term disability claim as soon as you know
you will be absent from work due to an illness, injury or
pregnancy. Notify your manager if your illness or injury is
related to your Walmart work, so a workers’ compensation
claim can be initiated. Report your disability online
by going to One.Walmart.com > mySedgwick, or call
800-492-5678. Your claim cannot be processed until you
have stopped working.
STEP 2: Tell your doctor’s office that it will be contacted
and asked to complete an attending physician’s statement
and provide medical information, including:
• Diagnosis
• Disability date and expected duration of disability
• Restrictions and limitations
• Physical and/or cognitive exam findings and test results
• Treatment plan, and
• Doctor visit notes.
You must sign a form authorizing your doctor to release
this information. (If filing your claim online, an electronic
signature is accepted.)
STEP 3: Follow up with your doctor to ensure that
information was forwarded to the disability administrator.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter. You
have the right to appeal a claim denial. See the Claims and
appeals chapter for details.
You may be required to provide written proof of your
disability or additional medical information before your
benefit payments begin.
When benefits are not paid
Short-term disability benefits will not be paid for an illness
or injury that is:
• Not under the care of and being treated by a qualified
doctor
• Caused by taking part in an insurrection, rebellion or a riot,
or civil disorder
• Resulting from your commission of or attempt to commit
a crime (e.g., assault, battery, felony, or any illegal
occupation or activity)
• One for which workers’ compensation benefits are paid, or
may be paid, if properly claimed, or
• Sustained as a result of doing any work for pay or profit.

Shor-term disability for full-time hourly associates
185
When benefits begin
If you are approved for short-term disability benefits, the
benefit will begin, after a waiting period of seven calendar
days, on the eighth calendar day after your disability begins.
You may use up to 40 hours of available paid time off (PTO)
during the benefit waiting period. You must repay the
company for PTO taken beyond the benefit waiting period
of seven calendar days.
If you are receiving short-term disability at the end of the
PTO plan year, please refer to your location’s PTO policy
for payout and/or carryover information. You do not
accrue additional PTO while receiving short-term disability
benefits.
Calculating your benefit
The amount of your short-term disability benefit is based on:
• Your average weekly wage, and
• Whether or not you have enrolled in the short-term
disability enhanced plan.
AVERAGE WEEKLY WAGE
Length of
employment
How average weekly wage is
determined
Employed 12 months
or more
Total gross pay ÷ 52 weeks
For example, the average weekly
wage for an associate with a total
gross pay of $36,400 is $700
($36,400 ÷ 52)
Employed less than
12 months
Total gross pay ÷ number of
weeksworked
For example, the average weekly
wage for an associate with a total
gross pay of $8,400 for 12 weeks of
work is $700 ($8,400 ÷ 12)
If a weekly benefit is payable for less than a week, your
pay will be 1/7 of the weekly benefit for each day you
weredisabled.
Total gross pay includes:
• Overtime
• Bonuses
• PTO and other illness protection benefits (not including
any previously paid disability benefits), and
• Personal pay for the 26 pay periods prior to your last day
worked (or for the number of pay periods worked if less
than 26). Note that if you have any pay periods in which
you had no earnings, those pay periods are excluded and
the number of pay periods used for the calculation will
be decreased.
The maximum weekly benefit under the short-term
disability basic plan is $200. There is no maximum weekly
benefit under the short-term disability enhanced plan,
except in New York, where the maximum is $6,000 per
week. A hypothetical benefit calculation is shown below,
using an average weekly wage of $700.
YOUR SHORTTERM DISABILITY BENEFIT: AN EXAMPLE
If you have Your benefit is
Shor-term disability
basic plan coverage
50% of your average weekly wage to
a maximum of $200/week
Average weekly wage: $700
50% of $700: $350
Reduced to the maximum weekly
benefit: $200
Shor-term disability
enhanced plan
coverage
60% of your average weekly wage
Average weekly wage: $700
60% of $700: $420
There is no maximum weekly benefit
under the shor-term disability
enhanced plan, so this figure would
not be reduced (in New York, there
is a maximum weekly benefit of
$6,000).
NOTE: For associates who are eligible for legally mandated
benefits as well as benefits under Walmar’s shor-term
disability plans, the amount of the benefit under Walmar’s
shor-term disability plans will be reduced by the amount of
the legally mandated benefit.
MATERNITY BENEFIT
For full-time hourly associates, except for those who
work in California, Hawaii, New Jersey, and Rhode Island,
if your disability is due to pregnancy, and you begin your
short-term disability leave on your delivery date or up to
two weeks before your expected delivery date, you will
be deemed to meet the plan’s definition of disability and
eligible for maternity disability benefits. The short-term
disability plan for hourly associates pays a maternity benefit
of 100% of your average weekly wage for up to the first
nine weeks, after an initial waiting period of seven calendar
days. However, if you begin your leave later than your
actual delivery date, you must meet the plan’s definition of
disability and will be eligible for the non-maternity disability
benefits only.
If you are eligible for benefits and continue to meet the
definition of disability after the first nine weeks of disability
payments, the short-term disability basic plan will pay up to
50% of your average weekly wage to a maximum of $200
per week and the enhanced plan will pay up to 60% of your
average weekly wage, from week 11 up to 25 weeks.

Shor-term disability for full-time hourly associates
186
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Full-time hourly associates who work in California, Hawaii,
New Jersey, and Rhode Island generally are not eligible
for the Walmart short-term disability plan because these
states have legallymandated disability plans with their
own eligibility terms. If you work in one of these states and
your disability is due to pregnancy, you will be eligible for
maternity benefits under the short-term disability plan for
hourly associates, subject to the following:
• If you are eligible for legallymandated short-term
disability benefits, the short-term disability plan for hourly
associates supplements the legallymandated short-term
disability benefits, as shown in the chart below.
• If you are not eligible for legally mandated short-term
disability benefits, the short-term disability plan pays a
maternity benefit of 100% of your average weekly wage
up to the first nine weeks, after an initial waiting period of
seven calendar days. The short-term disability maternity
benefits will end after nine weeks.
If you begin your leave later than your actual delivery date,
you will not be eligible for maternity benefits under the
short-term disability plan for hourly associates.
Maternity benefits under the short-term disability plan for full-time hourly associates are as described here:
MATERNITY BENEFIT
Associate’s work location (state or locality) Up to 9 weeks* Beyond 9 weeks*
If you work in a state or locality with no
legally mandated benefit
100% of your average weekly wage
after an initial waiting period of 7
calendar days.
If you experience medical complications
during pregnancy or post-parum, benefits
may be payable under the shor-term
disability plan for hourly associates. Benefits
would be equal to 50% or 60% of your average
weekly wage, depending on your coverage
election, from week 11 up to 25weeks.
If you work in a state or locality with
legallymandated benefits and you are
eligible to receive the state or local
government benefit
Legally mandated benefits are
payable at the applicable state or
local government rate; the Walmar
shor-term disability maternity
benefit will make up the difference
between the legally mandated
benefit and 100% of your average
weekly wage after an initial waiting
period of 7calendar days.
Applicable state or local government benefits
If you work in a state or locality with
legallymandated benefits and you are
not eligible to receive the state or local
government benefit
100% of your average weekly wage
afteran initial waiting period of
7calendardays.
Walmar’s shor-term disability benefits are
not available; maternity benefits end after
the first 9 weeks.
If you work in Washington state Legallymandated benefits are
payable at the applicable state rate;
the Walmar shor-term disability
maternity benefit will make up
the difference between the state
benefit and 100% of your average
weekly wage after an initial waiting
period of 7 calendar days.
If you experience medical complications
during pregnancy or post-parum, benefits
may be payable under both Walmar’s shor-
term disability plan for hourly associates and
the state benefits. Benefits under Walmar’s
plans would be equal to 50% or 60% of your
average weekly wage, depending on your
coverage election, from week 11 up to 25
weeks. The amount of the benefit under
Walmar’s plans will be reduced by the
amount of the legally mandated benefit.
* You may also be eligible for additional parental pay equal to 100% of your average weekly wage under Walmar’s Parental Pay policy.
Formore information, refer to the parental pay policy on One.Walmar.com.
Shor-term disability for full-time hourly associates
187
TAXES AND YOUR SHORTTERM
DISABILITYBENEFIT
The taxation of benefits payable to you depends on
whether you are enrolled only in the short-term disability
basic benefit or in the enhanced benefit. If you are
enrolled in short-term disability basic, benefits payable
to you are subject to taxes. This is because you do not
make contributions to the short-term disability basic plan
or pay any tax on the coverage that Walmart provides. If
you are enrolled in short-term disability enhanced, only
a portion of your benefits will be taxed, because both
Walmart and you pay for the cost of the coverage through
a combination of Walmart pretax and associate after-tax
contributions. Walmart generally withholds federal, state,
local, and Social Security taxes from the portion of the
benefit that is taxable.
In Hawaii, New Jersey, and New York, benefits are partially
taxed. Please contact Lincoln for more information.
Associates in other states or localities with legally mandated
benefits should contact the state or locality for information
about the tax status of state or local government benefits.
The Plan has the right to recover from you, and you
must repay, any amount overpaid to you for short-term
disability benefits under this Plan. See The Plan’s right to
recover overpayment and Right to salary/wage deduction
in the Claims and appeals chapter. If you do not repay
overpaid amounts in a timely manner, the company may
treat the portion of such amounts that were not taxed
when paid as taxable wages to you (reportable on your
Form W-2) or, alternatively, deduct such amounts from
your paycheck or future disability benefit payments, to
the extent permitted by law.
When shor-term disability benefit
payments end
If you are receiving short-term disability benefits from the
Plan due to an approved disability, your benefit payments
from the Plan will end on the earliest of:
• The date you no longer meet the plan’s definition of disabled
• The date you fail to furnish required proof of disability
when requested to do so by Sedgwick or Lincoln
• The date you are no longer under the continuous care and
treatment of a qualified doctor
• The date you refuse to be examined, if Sedgwick or Lincoln
requires an examination
• The last day of the maximum period for which benefits
are payable (25 weeks or nine weeks for maternity
disability benefits)
• The date you are medically able and qualified to work in a
similar full-time position offered to you by Walmart, or
• The date of your death.
When your short-term disability benefits end, and for any
reason you do not return to work, you must request an
extension of your leave. Failure to do so may result in your
employment being terminated.
If you return to work within 30 days of the end of your
approved disability period, you will be reinstated to the
disability coverage you had prior to your disability. If you
do not return to work within 30 days of the end of your
approved disability period, your coverage will lapse until
youreturn to work and meet the active work requirement.
State and local government short-term disability
programs may have different end dates from Walmart’s
coverage.
Returning to work
Sedgwick will contact you before your expected return-to-
work date and advise you of steps you may need to take,
including getting a return-to-work certification completed
by your doctor. In some cases, your doctor may release
you to work with certain medical restrictions; any such
restrictions should be explicitly stated on your return-to-
work certification or written release. If you receive a return-
to-work certification containing medical restrictions, you
may be subject to a review to determine whether a job
adjustment or accommodation will help you return to work.
Notify Sedgwick when you physically return to work. If your
short-term disability benefits have ended and you have
not returned to work or communicated your intentions,
Sedgwick will notify you of your options, which include
requesting an extension of your leave or voluntarily
terminating employment. Failure to request an extension
may result in your employment being terminated.
IF YOU RETURN TO WORK AND BECOME
DISABLED AGAIN
If you return to work for 30 calendar days or less of active
full-time work (with or without medical restrictions) and
become disabled again from the same or a related condition
that caused the first period of disability, as determined by
Sedgwick or Lincoln, known as a “relapse/recurrent claim,”
your short-term disability benefits will pick up where
they left off before you came back to work. There will be
no additional waiting period of seven calendar days. The
combined benefit duration for both periods of disability will
not exceed 25 weeks.
If you have returned to active full-time work for more than
30 calendar days and then become disabled from the same
or a related cause, it will be considered a new disability, and
you may be able to receive up to 25 weeks of benefits. A
new benefit waiting period of seven calendar days will apply.

Shor-term disability for full-time hourly associates
188
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you return to active full-time work for any number of
calendar days and then become disabled from a new and
unrelated cause, it will be considered a new disability, and
you may qualify for up to 25 weeks of benefits. A new
benefit waiting period of seven calendar days will apply.
Coverage during a leave of absence
or temporary layoff
Once your short-term disability coverage is effective and
you are eligible to file a claim for benefits, if you are not
actively at work due to an approved non-disability leave of
absence or temporary layoff, you will continue to be eligible
for short-term disability benefits for 90 days from your last
day of work. Your eligibility for short-term disability benefits
ends on the 91st day after the beginning of your approved
non-disability leave or temporary layoff, but is reinstated if
you return to active work status within one year.
When coverage ends
Your short-term disability basic plan and enhanced plan
coverage ends:
• At termination of your employment
• On the last day of the pay period when your job status
changes from an eligible job status
• On the date you lose eligibility
• On the date of your death
• On the 91st day of an approved leave of absence (unless
you return to work), or
• When the benefit is no longer offered by the company.
In addition, coverage under the short-term disability
enhanced plan would end the day after you drop
yourcoverage.
If you leave the company and
arerehired
If you leave the company and return to full-time work for
the company within 13 weeks, you will automatically be
reenrolled for the same coverage plan you had prior to
leaving the company (or the most similar coverage offered
under the Plan). If you are automatically reenrolled in
short-term disability enhanced plan coverage and choose to
drop it after you return, you may do so at any time.
See page 298
If you return to full-time work after 13 weeks, you will be
considered newly eligible and may enroll for coverage under
the time periods and conditions described in the Eligibility
and enrollment chapter.
If you lose and then regain eligibility
If you lose eligibility and then regain eligibility within 30
days, you will automatically be reenrolled for the same
coverage you had prior to leaving the company (or the most
similar coverage offered under the Plan).
If you lose eligibility and then regain eligibility after 30 days,
you will be considered newly eligible and may enroll for
coverage under the time periods and conditions described
in the Eligibility and enrollment chapter.
Shor-term disability for full-time hourly associates
189

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information does not create an express or implied contract of employment or any other contractual
commitment. Walmar may modify this information at its sole discretion without notice, at any time,
consistent with applicable law.
Salaried shor-term disability 192
How salaried shor-term disability isadministered 192
When you qualify for benefits 192
Filing a claim 193
When benefits are not paid 193
Your pay after filing a claim 194
Benefits determination 194
When benefits begin 195
Calculating your benefit 195
When shor-term disability benefit payments end 196
Returning to work 197
Coverage during a leave of absence or temporary layoff 197
When coverage ends 197
If you leave the company and arerehired 197
Salaried shor-term
disability plan

Salaried shor-term disability plan
191
Salaried shor-term disability plan
If pregnancy, a scheduled surgery, or an unexpected illness or injury keeps you off the job for an
extended period, this plan for salaried associates can protect par of your paycheck. When you can’t
work, the Walmar salaried shor-term disability plan works for you.
RESOURCES
Find What You Need Online Other Resources
Get more details or file a claim
(provided to salaried associates in all
50 states)
Go to One.Walmar.com Call Sedgwick at 800-492-5678
If you work in Washington
(to file a state benefit claim)
Go to paidleave.wa.gov Call state of Washington at 833-717-2273
Request an appeal of a denied
shor-term disability claim
Go to One.Walmar.com/LOA
> mySedgwick
Call Sedgwick at 800-492-5678
What you need to know about salaried shor-term disability
• If you are a salaried (management) associate, you are automatically enrolled in the salaried short-term disability
plan. Coverage is effective as of your date of hire and there is no cost to you.
• If you become disabled and are eligible to receive short-term disability benefits, the salaried short-term disability
plan replaces 100% of your base pay for up to six weeks and 75% of your base pay for up to 19 additional weeks,
after an initial waiting period of seven calendar days. (Different rules may apply to work-related disabilities that
qualify for workers’ compensation through Walmart. See the chart titled Your salaried short-term disability plan
benefit for more information.)
• If your disability is due to pregnancy, the salaried short-term disability plan replaces 100% of your base pay for nine
weeks, after an initial waiting period of seven calendar days. Generally no medical evidence is required for this
short-term disability maternity benefit.
• The salaried short-term disability plan is not a benefit covered by ERISA and is not part of the Associates’ Health
and Welfare Plan.
• The claims and appeals procedures described in this chapter apply to the salaried short-term disability benefit
rather than the procedures in the Claims and appeals chapter.

Salaried shor-term disability plan
192
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Salaried shor-term disability
You are automatically enrolled for coverage in the salaried
short-term disability plan as of your date of hire if you are
a salaried/management associate (exempt). For details
about eligible job classifications, see the Enrollment
and eligibility dates by job classification section in the
Eligibility and enrollment chapter.
How salaried shor-term disability
isadministered
Salaried short-term disability coverage is administered by
Sedgwick Claims Management Services, Inc. (Sedgwick) and
is provided by the company at no cost to you.
If you become disabled and eligible to receive short-term
disability benefits, the salaried short-term disability plan
generally pays 100% of your base pay for up to six weeks
of an approved disability, after an initial waiting period of
seven calendar days of continuous disability. (Disabilities
that qualify for workers’ compensation through Walmart
are treated differently, as described in the chart titled
Your salaried short-term disability plan benefit.) If you
remain disabled and eligible for benefits after the first
six weeks of disability payments, the salaried short-term
disability plan will pay 75% of your base pay for up to
19additional weeks.
If your disability is due to pregnancy, you will be deemed to
meet the definition of disability, and the salaried short-term
disability plan pays a maternity benefit of 100% of your base
pay for the first nine weeks, after an initial waiting period of
seven calendar days.
For your pay to continue during the initial waiting period
of seven calendar days, you may use paid time off (PTO).
Salaried short-term disability benefits begin on the eighth
calendar day after your eligible disability begins.
LEGALLY MANDATED PLANS
Short-term disability benefits provided by individual states
and local governments generally have no impact on your
eligibility for the salaried short-term disability benefit
through Walmart, or the amount of the benefit you receive
under Walmart’s plan.
Exceptions to this policy apply to all eCommerce salaried
associates who work in California and all associates who
work in Washington. General information can be found in
the chart at the bottom of the page.
When you qualify for benefits
To qualify for short-term disability benefits through the
salaried short-term disability plan, you must meet the
following requirements:
• You must submit medical evidence provided by a
qualified doctor that you are disabled as defined by the
salaried short-term disability plan (qualified doctors are
legally licensed physicians and practitioners who are not
related to you and who are performing services within
the scope of their licenses, including medical doctors
[M.D.], osteopaths [D.O.], nurse practitioners, physician’s
assistants, psychologists, or other medical practitioners
recognized by the Associates’ Health and Welfare Plan).
• You must receive approval by Sedgwick of your claim.
If your disability is caused by a mental illness
or substance abuse, you are encouraged
to seek treatment within 30 days from the
first date of absence from a psychologist,
psychiatrist, or clinical social worker who
holds a Master of Social Work (M.S.W.),
specializes in mental health and substance
abuse, and is licensed pursuant to state law.
LEGALLY MANDATED PLANS
eCommerce salaried associates
who work in California
Associates are eligible to paricipate in Walmar’s salaried shor-term disability plan to
supplement their state benefits.
The amount of the benefit under Walmar’s salaried shor-term disability plan will be reduced
by the amount of the legally mandated benefit.
Associates who work in
Washington
Associates are eligible to paricipate in Walmar’s salaried shor-term disability plan to
supplement their state benefits.
To be eligible to receive benefits under the Walmar salaried shor-term disability plan, you
must apply through the state or local government for your legally mandated benefits, as
permitted by law. The amount of the benefit under Walmar’s salaried shor-term disability
plan will be reduced by the amount of the legally mandated benefit. The total benefits payable
under the Walmar shor-term disability plan will not exceed the level of benefits otherwise
payable under the plan.
See page 331 for updated terms replacing the chart above.

Salaried shor-term disability plan
193
Sedgwick may require written proof of your disability or
additional information before making a decision on your
claim. A statement by your physician that you are unable to
work does not by itself qualify you for short-term disability
benefits. Approval of a medical leave of absence does not
constitute approval for short-term disability benefits.
As defined by the salaried short-term disability plan,
“disabled” or “disability” means that you are unable to
perform the essential duties of your job for your normal
work schedule, or a license required for your job duties
has been suspended due to a mental or physical illness or
injury, or pregnancy. Benefits are payable during a loss of
license only while you are disabled or pursuing reinstatement
of your license on a timely basis. Timely pursuit of
reinstatement means you apply for reinstatement when your
condition meets the criteria and you provide information
and forms requested by the licensing agency on a timely
basis until your license is reinstated. The determination
of whether you are disabled is made by Sedgwick on the
basis of objective medical evidence, which consists of facts
and findings, including X-rays, laboratory reports, tests,
consulting physician reports as well as reports and chart
notes from your physician. In addition, you must be under
the continuous care of a qualified doctor and following the
course of treatment prescribed. Loss of license by itself is
not sufficient for meeting the definition of disability.
If Sedgwick requests that you be examined by an
independent physician or other medical professional, you
must attend the exam to be considered for benefits.
If your disability is the result of more than one cause, you
will be paid as if they were one. The maximum benefit for
any one period of disability is limited to 25 weeks, after the
initial waiting period of seven calendar days.
If your disability is due to pregnancy, you will be deemed
to meet the definition of disability, and Sedgwick will not
require objective medical evidence as a condition for
approving your disability claim for the short-term disability
maternity benefit, except in the following situations:
• You begin your leave of absence more than two weeks
before your estimated date of delivery, or
• You do not begin your leave of absence immediately after
the date of delivery.
The maternity benefit generally begins on the earlier
of two weeks before the estimated date of delivery (as
determined by a qualified doctor) or no later than the
actual date of delivery.
Filing a claim
If you experience a disabling illness or injury, or are planning
to begin maternity leave, follow these steps:
STEP 1: Notify Sedgwick to apply for a leave of absence and
file a short-term disability claim as soon as you know you will
be absent from work due to an illness, injury or pregnancy.
Sedgwick will send you an initial packet providing the
information you will need and describing any actions you will
need to take. Notify your manager if your illness or injury is
related to your Walmart work, so a workers’ compensation
claim can be initiated. Report your disability online by
going to One.Walmart.com/LOA > mySedgwick, or call
800-492-5678.
Processing of your claim cannot begin until you have stopped
working. All claims for benefits under Walmart’s salaried
short-term disability plan must be submitted to Sedgwick
within 90 days of the date your disability begins. Claims filed
later than 90 days after the date of disability may be denied
unless Sedgwick determines you had good cause for filing late.
STEP 2: Tell your doctor’s office that it will be contacted
and asked to complete an attending physician’s statement
and provide medical information, including:
• Diagnosis
• Disability date and expected duration of disability
• Restrictions and limitations
• Physical and/or cognitive exam findings and test results
• Treatment plan, and
• Doctor visit notes.
You must sign a form authorizing your doctor to release
this information. (If filing your claim online, an electronic
signature is accepted.)
STEP 3: Follow up with your doctor to ensure that
information was forwarded to the disability administrator.
If you become disabled, file your claim for
benefits promptly. A delay in filing could
result in delayed benefit payment, disruption
to your wages, or the denial of your claim.
When benefits are not paid
Short-term disability benefits will not be paid for an illness
or injury that is:
• Not under the care of and being treated by a qualified
doctor
• Caused by taking part in an insurrection, rebellion or a riot,
or civil disorder
• Resulting from your commission of or attempt to commit
a crime (e.g., assault, battery, felony, or any illegal
occupation or activity), or
• Sustained as a result of doing any work for pay or profit.
Salaried shor-term disability plan
194
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Your pay after filing a claim
Sedgwick will send you an initial packet when you file your
claim. You will have until the Medical Due Date, which is
stated in your initial packet, to provide the required medical
documentation. Your pay will continue until your Medical
Due Date; this pay is known as “provisional pay.” Your
pay will be suspended after your Medical Due Date if the
required medical documentation has not been approved.
Be sure to provide the required medical documentation at
your earliest opportunity. If you do not meet the Medical
Due Date deadline, your pay will be suspended effective
the first day of the pay period in which it falls. (In cases of
pregnancy, verification of your due date is the only medical
verification required for the short-term disability maternity
benefit, unless you begin your leave of absence more than
two weeks before your estimated date of delivery.) If your
claim is approved, the approval will be effective as of the
date of your disability, and the period of provisional pay will
count toward the duration of your disability benefit.
If your claim is denied before the Medical Due Date due
to your medical circumstances not meeting the salaried
short-term disability plan’s definition of disability, your pay
will be suspended and Walmart will commence efforts to
recover the amount paid to you for the period following
your illness or injury.
Provisional pay does not apply to relapse/recurrent claims.
Benefits determination
Sedgwick makes a decision within 45 days of receiving your
properly filed claim. The time for a decision may be extended
for up to two additional 30-day periods. You will be notified
in writing before any extension period that an extension is
necessary due to matters beyond Sedgwick’s control. Those
matters must be identified and you must be given the date by
which Sedgwick will make a decision. If your claim is extended
due to your failure to submit information Sedgwick deems
necessary to decide your claim, the time for decision will be
suspended as of the date on which the notification of the
extension is sent to you until the date Sedgwick receives your
response. If Sedgwick approves your claim, the decision will
contain information sufficient to inform you of that decision.
If Sedgwick denies your claim, you will be sent a written
notification of the denial, which will include:
• Specific reasons for the decision
• Specific reference to the policy provisions on which the
decision is based
• A description of any additional material or information
necessary for you to perfect the claim and an explanation
of why such material or information is necessary
• A description of the appeal procedures and time limits
applicable to such procedures, and
• If an internal rule, guideline, protocol, or other similar
criteria was relied upon in making the denial, either
– The specific rule, guideline, protocol, or other similar
criteria, or
– A statement that such a rule, guideline, protocol, or
other similar criteria was relied upon in making the
denial and that a copy will be provided free of charge to
you upon request.
APPEALING A DISABILITY CLAIM THAT HAS
BEEN FULLY OR PARTIALLY DENIED
If your claim for benefits is denied and you would like
to appeal, you must submit a written or oral appeal to
Sedgwick within 180 days of the denial. Your appeal should
include any comments, documents, records, or any other
information you would like considered.
You have the right to request copies, free of charge, of all
documents, records, or other information relevant to your
claim. Your appeal will be reviewed, without regard to your
initial determination, by someone other than the party who
decided your initial claim.
Sedgwick will make a determination on your appeal within 45
days of the receipt of your appeal request. This period may be
extended by up to an additional 45 days if it is determined that
special circumstances require an extension of time. You will be
notified prior to the end of the 45-day period if an extension
is required. If you are asked to provide additional information,
you will have 45 days from the date you are notified to provide
the information, and the time to make a determination will be
suspended until you provide the requested information (or the
deadline to provide the information, if earlier).
If your appeal is denied in whole or in part, you will receive a
written notification of the denial that will include:
• The specific reason(s) for the adverse determination
• Reference to the specific plan provisions on which the
determination was based
• A statement describing your right to request copies, free
of charge, of all documents, records, or other information
relevant to your claim
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination, and
• A statement describing any appeal procedures offered by
the Plan.

Salaried shor-term disability plan
195
YOUR SALARIED SHORTTERM DISABILITY PLAN BENEFIT
Duration of your
disability
Your benefit is:
If your disability does not qualify for
workers’ compensation through Walmar
If you have a work-related disability that qualifies for
workers’ compensation through Walmar
Up to 7 weeks After an initial waiting period of 7
calendar days, 100% of your base pay.
Benefits begin on the 8th calendar day.
You may use PTO during your first 7
calendar days of continuous disability.
100% of your base pay, with no initial waiting period. Benefits
are payable as of the date of your disability.
More than 7 weeks,
upto 26 weeks
75% of your base pay.
For example, if your base pay is $1,000,
75%of $1,000 is a $750 benefit.
Workers’ compensation benefits are payable at the
applicable state rate; shor-term disability benefits make up
the difference up to 75% of your base pay.
For example, if your base pay is $1,000 and workers’
compensation pays 66% for your disability, or $660, shor-
term disability will pay an additional $90, for a total benefit
of $750.
(If the legally mandated workers’ compensation rate exceeds
75% of your base pay, you will not receive any shor-term
disability benefit.)
NOTE: For associates who are eligible for legally mandated benefits (as noted in Legally mandated plans earlier in this chapter) as
well as benefits under Walmar’s salaried shor-term disability plan, the amount of the benefit under Walmar’s salaried shor-term
disability plan will be reduced by the amount of the legally mandated benefit.
If a benefit is payable for less than a week, your pay will be based on your base pay divided by your regular work schedule for
each day you are disabled.
NOTE: Workers’ compensation and short-term disability benefits are made as separate payments.
VOLUNTARY SECOND APPEAL OF A SALARIED
SHORTTERM DISABILITY CLAIM
If your appeal is denied, you may make a voluntary second
appeal of your denial orally or in writing to Sedgwick. You
must submit your second appeal within 180 days of the
receipt of the written notice of denial. You may submit any
written comments, documents, records, and any other
information relating to your claim. The same criteria and
response times that applied to your first appeal, as described
earlier, are generally applied to this voluntary second appeal.
All salaried short-term disability appeals should be sent to:
Walmart Disability and Leave Service Center at Sedgwick
National Appeals Unit
P.O. Box 14028
Lexington, Kentucky 40512
When benefits begin
If you are approved for short-term disability benefits, the
benefit will begin after a waiting period of seven calendar
days, on the eighth calendar day after your disability begins.
(There is no waiting period for work-related disabilities that
qualify for workers’ compensation through Walmart.)
In order for your pay to continue during the initial waiting
period of seven calendar days, you may use paid time
off (PTO). Salaried short-term disability benefits begin
on theeighth calendar day after your eligible disability
begins. PTO may not be used while receiving short-term
disabilitybenefits.
If you are receiving short-term disability at the end of the
PTO plan year, please refer to your location’s PTO policy for
payout and/or carryover information.
Calculating your benefit
The amount of your short-term disability benefit is based on:
• Your base pay as of your last day worked, and
• The duration of your disability.
Base pay, for purposes of the salaried short-term disability
benefit, is defined as follows:
ASSOCIATE TYPE BASE PAY
Exempt associates Gross biweekly salary
Non-exempt
associates
Hourly rate multiplied by hours
scheduled that pay period
If you become disabled and eligible to receive short-term
disability benefits, the salaried short-term disability plan
pays benefits as described below:

Salaried shor-term disability plan
196
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
MATERNITY BENEFIT
Maternity benefits under the salaried short-term disability plan are as described here:
MATERNITY BENEFIT
Duration of benefit Your benefit is: If you are eligible for legally mandated benefits in WA:
Up to 9 weeks* 100% of your base pay after an initial
waiting period of 7 calendar days.
Legallymandated benefits are payable at the applicable state
or local government rate; the Walmar salaried shor-term
disability maternity benefit will make up the difference
between the state or local government benefit and 100% of
your base pay after an initial waiting period of 7 calendar days.
Maternity benefits under the salaried shor-term disability plan begin on the 8th calendar day after your
eligible disability begins. You may use PTO during your first 7 calendar days of continuous disability.
* You may also be eligible for additional parental and family care pay equal to 100% of your base pay. For more information,
refer to the Parental and Family Care Pay policy on One.Walmart.com.
NOTE: For associates who are eligible for legally mandated benefits (as noted in Legally mandated plans earlier in this chapter) as
well as benefits under Walmar’s salaried shor-term disability plan, the amount of the benefit under Walmar’s salaried shor-term
disability plan will be reduced by the amount of the legally mandated benefit.
If you begin your short-term disability leave on your delivery
date or up to two weeks before your expected delivery date,
you will be deemed to meet the plan’s definition of disability
and eligible for maternity disability benefits.
If you begin your leave later than your actual delivery date,
you must meet the plan’s definition of disability and will be
eligible for the non-maternity disability benefits only.
If you experience medical complications during pregnancy
or post-partum, benefits may be payable under the salaried
short-term disability plan after the end of the nine-week
duration of maternity benefits if you continue to meet the
definition of disability. Benefits would be equal to 75% of
your base pay from week 11, up to 25 weeks.
TAXES AND YOUR SHORTTERM
DISABILITYBENEFIT
Benefits payable to you under Walmart’s salaried short-
term disability plan are company-provided, at no cost to
you. Because you do not make any contributions to the
salaried short-term disability plan, any benefits payable
to you are subject to taxes. Walmart generally withholds
federal, state, local, and Social Security taxes from the
amount of your benefits.
The salaried short-term disability plan has the right
to recover from you, and you must repay, any amount
overpaid to you for short-term disability benefits under
this plan. See The Plan’s right to recover overpayment and
Right to salary/wage deduction in the Claims and appeals
chapter. If you do not repay overpaid amounts in a timely
manner, the company may deduct such amounts from your
paycheck or future disability benefit payments, to the
extent permitted by law.
When shor-term disability benefit
payments end
If you are receiving short-term disability benefit payments
from the salaried short-term disability plan due to an
approved disability, your benefit payments from the plan
will end on the earliest of:
• The date you no longer meet the plan’s definition of disabled
• The date you fail to furnish the required proof of disability
when requested to do so by Sedgwick
• The date you are no longer under the continuous care and
treatment of a qualified doctor
• The date you refuse to be examined, if Sedgwick requires
an examination
• The last day of the maximum period for which benefits
are payable (25 weeks, or nine weeks for maternity
disability benefits)
• The date you are medically able and qualified to work in a
similar full-time position offered to you by Walmart
• The date your employment terminates, or
• The date of your death.
When your short-term disability benefits end and for any
reason you do not return to work, you must request an
extension of your leave; failure to do so may result in your
employment being terminated.
Salaried shor-term disability plan
197
Returning to work
Sedgwick will contact you before your expected
return-to-work date and advise you of steps you may need
to take, including getting a return-to-work certification
completed by your doctor. In some cases, your doctor
may release you to work with certain medical restrictions;
any such restrictions should be explicitly stated on your
return-to-work certification or written release. If you
receive a return-to-work certification containing medical
restrictions, you may be subject to a review to determine
whether a job adjustment or accommodation will help you
return to work.
Notify Sedgwick when you physically return to work.
If yourshort-term disability benefits have ended and
you have not returned to work or communicated your
intentions, Sedgwick will notify you of your options, which
include requesting an extension of your leave or voluntarily
terminating employment. Failure to request an extension
may result in your employment being terminated.
IF YOU RETURN TO WORK AND BECOME
DISABLED AGAIN
If you return to work for 30 calendar days or less of active
full-time work (with or without medical restrictions) and
become disabled again from the same or a related condition
that caused the first period of disability, as determined by
Sedgwick, known as a “relapse/recurrent claim,” your short-
term disability benefits will pick up where they left off
before you came back to work. There will be no additional
waiting period. The combined benefit duration will not
exceed 25 weeks.
If you return to active full-time work for more than 30
calendar days and then become disabled from the same or a
related cause, it will be considered a new disability, and you
may be able to receive up to 25 weeks of benefits. A new
benefit waiting period of seven calendar days will apply.
If you have returned to active full-time work for any number
of calendar days and then become disabled from a new
and unrelated cause, it will be considered a new disability,
and you may qualify for up to 25 weeks of benefits. A new
benefit waiting period of seven calendar days will apply.
Intermittent leave. If you are able to return to work after
a period of short-term disability and need to miss work
periodically for reasons related to your disability, notify
Sedgwick and your facility of your situation. Your treatment
may be covered under your prior short-term disability
claim for up to 12 months from the date you return to work
from your short-term disability claim. Salaried short-term
disability generally pays 100% of your base pay for the
duration of your approved intermittent leave. You will not
need to use PTO for the absences.
Coverage during a leave of absence
or temporary layoff
If you are not working due to an approved non-disability
leave of absence or temporary layoff, you will continue to
be eligible for short-term disability benefits for 90 days
from your last day of work. Your eligibility for short-term
disability benefits ends on the 91st day after the beginning
of your approved non-disability leave or temporary layoff,
but is reinstated if you return to work. See Benefits
continuation if you go on a leave of absence in the Eligibility
and enrollment chapter for more information, including
details on paying for benefits while on leave.
When coverage ends
Your short-term disability coverage ends:
• At termination of your employment
• On the last day of the pay period when your job status
changes from an eligible job status
• On the date you lose eligibility
• On the date of your death
• On the 91st day of an approved non-disability leave of
absence (unless you return to work), or
• When the benefit is no longer offered by the company.
If you leave the company and
arerehired
If you leave the company and return to work for the
company as a salaried associate, you will automatically be
reenrolled in the salaried short-term disability plan.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information does not create an express or implied contract of employment or any other contractual
commitment. Walmar may modify this information at its sole discretion without notice, at any time,
consistent with applicable law.
Truck driver shor-term disability 200
How truck driver shor-term disability is administered 200
When you qualify for benefits 200
Filing a claim 201
When benefits are not paid 201
Your pay after filing a claim 201
Benefits determination 202
When benefits begin 202
Calculating your benefit 203
When shor-term disability benefit payments end 204
Returning to work 204
Coverage during a leave of absence or temporary layoff 205
When coverage ends 205
If you leave the company and arerehired 205
Truck driver
shor-term
disabilityplan

Truck driver shor-term disabilityplan
199
Truck driver shor-term disability plan
If pregnancy, a scheduled surgery, or an unexpected illness or injury keeps you off the job for an
extended period, this plan for truck drivers can protect par of your paycheck. When you can’t
work, the Walmar truck driver shor-term disability plan works for you.
RESOURCES
Find What You Need Online Other Resources
Get more details or file a claim Go to One.Walmar.com Call Sedgwick at 800-492-5678
If you work in Washington
(to file a state benefit claim)
Go to paidleave.wa.gov Call state of Washington at 833-717-2273
Request an appeal of a denied
shor-term disability claim
Go to One.Walmar.com/LOA
> mySedgwick
Call Sedgwick at 800-492-5678
What you need to know about truck driver shor-term disability
• If you are a full-time truck driver, you are automatically enrolled in the truck driver short-term disability plan.
Coverage is effective as of your date of hire and there is no cost to you.
• If you become disabled and are eligible to receive short-term disability benefits, the truck driver short-term disability
plan replaces 75% of your average day’s pay for up to 25 weeks, after an initial waiting period of seven calendar days.
(Different rules may apply to work-related disabilities that qualify for workers’ compensation through Walmart. See
the chart titled Your truck driver short-term disability plan benefit for more information.)
• If your disability is due to pregnancy, the truck driver short-term disability plan replaces 100% of your average day’s
pay for up to nine weeks, after an initial waiting period of seven calendar days. Generally, no medical evidence is
required for this short-term disability maternity benefit.
• The truck driver short-term disability plan is not a benefit covered by ERISA and is not part of the Associates’ Health
and Welfare Plan.
• The claims and appeals procedures described in this chapter apply to the truck driver short-term disability benefit
rather than the procedures in the Claims and appeals chapter.

Truck driver shor-term disabilityplan
200
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Truck driver shor-term disability
You are automatically enrolled in the truck driver short-term
disability plan as of your date of hire if you are a full-time
truck driver. For details about eligible job classifications,
see the Enrollment and eligibility dates by job classification
section in the Eligibility and enrollment chapter.
How truck driver shor-term
disability is administered
Truck driver short-term disability coverage is administered
by Sedgwick Claims Management Services, Inc. (Sedgwick)
and is provided by the company at no cost to you.
If you become disabled and eligible to receive short-term
disability benefits, the truck driver short-term disability
plan generally pays 75% of your average day’s pay for up to
25 weeks of an approved disability, after an initial waiting
period of seven calendar days of continuous disability. The
waiting period begins on your next scheduled work day
after your total disability begins. (Disabilities that qualify
for workers’ compensation through Walmart are treated
differently, as described in the chart titled Your truck driver
short-term disability plan benefit.)
If your disability is due to pregnancy, you will be deemed
to meet the definition of disability, and the truck driver
short-term disability plan pays a maternity benefit of 100%
of your average day’s pay for the first nine weeks of an
approved disability, after an initial waiting period of seven
calendar days.
For your pay to continue during the initial waiting period of
seven calendar days, you may use paid time off (PTO). Truck
driver short-term disability benefits begin the day after the
initial waiting period ends.
LEGALLY MANDATED PLANS
Short-term disability benefits provided by individual states
and local governments generally have no impact on your
eligibility for the truck driver short-term disability benefit
plan through Walmart, or the amount of the benefit you
receive under Walmart’s plan.
An exception to this policy applies to associates who
work in the state of Washington. These associates are
eligible to participate in Walmart’s truck driver short-term
disability plan to supplement their state benefits. To be
eligible to receive benefits under the Walmart truck driver
short-term disability plan, you must apply through the state
or local government for your legally mandated benefits,
as permitted by law. The amount of the benefit under
Walmart’s plan will be reduced by the amount of the legally
mandated benefit. The total benefits payable under the
Walmart short-term disability plan will not exceed the level
of benefits otherwise payable under the plan.
When you qualify for benefits
To qualify for short-term disability benefits through the
truck driver short-term disability plan, you must meet the
following requirements:
• You must submit medical evidence provided by a qualified
doctor that you are disabled as defined by the truck
driver short-term disability plan (qualified doctors are
legally licensed physicians and practitioners who are not
related to you and who are performing services within
the scope of their licenses, including medical doctors
[M.D.], osteopaths [D.O.], nurse practitioners, physician’s
assistants, psychologists, or other medical practitioners
recognized by the Associates’ Health and Welfare Plan).
• You must receive approval by Sedgwick of your claim.
If your disability is caused by a mental illness
or substance abuse, you are encouraged
to seek treatment within 30 days from the
first date of absence from a psychologist,
psychiatrist, or clinical social worker who
holds a Master of Social Work (M.S.W.),
specializes in mental health and substance
abuse, and is licensed pursuant to state law.
Sedgwick may require written proof of your disability or
additional information before making a decision on your
claim. A statement by your physician that you are unable to
work does not by itself qualify you for short-term disability
benefits. Approval of a medical leave of absence does not
constitute approval for short-term disability benefits.
As defined by the truck driver short-term disability plan,
“disabled” or “disability” means that you are unable to
perform the essential duties of your job for your normal
work schedule, or a license required for your job duties
has been suspended due to a mental or physical illness
or injury, or pregnancy. Benefits will be payable during
a loss of license only while you are disabled or pursuing
reinstatement of your license on a timely basis. Timely
pursuit of reinstatement means you apply for reinstatement
when your condition meets the criteria and you provide
information and forms requested by the licensing agency
on a timely basis until your license is reinstated. The
determination of whether you are disabled is made by
Sedgwick on the basis of objective medical evidence, which
consists of facts and findings, including but not limited
to X-rays, laboratory reports, tests, consulting physician
reports as well as reports and chart notes from your
physician. In addition, you must be under the continuous
care of a qualified doctor and following the course of
treatment prescribed. Loss of license by itself is not
sufficient for meeting the definition of disability.

Truck driver shor-term disabilityplan
201
If Sedgwick requests that you be examined by an
independent physician or other medical professional, you
must attend the exam to be considered for benefits.
If your disability is the result of more than one cause, you
will be paid as if they were one. The maximum benefit for
any one period of disability is limited to 25 weeks, after the
initial waiting period.
If your disability is due to pregnancy, you will be deemed
to meet the definition of disability, and Sedgwick will not
require objective medical evidence as a condition for
approving your disability claim for the short-term disability
maternity benefit, except in the following situations:
• You begin your leave of absence more than two weeks
before your estimated date of delivery, or
• You do not begin your leave of absence immediately after
the date of delivery.
The maternity benefit generally begins on the earlier
of two weeks before the estimated date of delivery (as
determined by a qualified doctor) or no later than the
actual date of delivery.
Filing a claim
If you experience a disabling illness or injury, or are planning
to begin maternity leave, follow these steps:
STEP 1: Notify Sedgwick to apply for a leave of absence and
file a short-term disability claim as soon as you know you will
be absent from work due to an illness, injury, or pregnancy.
Sedgwick will send you an initial packet providing the
information you will need and describing any actions you will
need to take. Notify your manager if your illness or injury is
related to your Walmart work, so a workers’ compensation
claim can be initiated. Report your disability online by
going to One.Walmart.com/LOA > mySedgwick, or call
800-492-5678.
Processing of your claim cannot begin until you have
stopped working. All claims for benefits under Walmart’s
truck driver short-term disability plan must be submitted to
Sedgwick within 90 days of the date your disability begins.
Claims filed later than 90 days after the date of disability
may be denied unless Sedgwick determines you had good
cause for filing late.
STEP 2: Tell your doctor’s office that it will be contacted
and asked to complete an attending physician’s statement
and provide medical information, including the following:
• Diagnosis
• Disability date and expected duration of disability
• Restrictions and limitations
• Physical and/or cognitive exam findings and test results
• Treatment plan, and
• Doctor visit notes.
You must sign a form authorizing your doctor to release
this information. (If filing your claim online, an electronic
signature is accepted.)
STEP 3: Follow up with your doctor to ensure that
information was forwarded to the disability administrator.
If you become disabled, file your claim for
benefits promptly. A delay in filing could
result in delayed benefit payment, disruption
to your wages, or the denial of your claim.
When benefits are not paid
Short-term disability benefits are not paid for an illness or
injury that is:
• Not under the care of and being treated by a qualified
doctor
• Caused by taking part in an insurrection, rebellion or a riot,
or civil disorder
• Resulting from your commission of or attempt to commit
a crime (e.g., assault, battery, felony, or any illegal
occupation or activity), or
• Sustained as a result of doing any work for pay or profit.
Your pay after filing a claim
Sedgwick will send you an initial packet when you file your
claim. You will have until the Medical Due Date, which is
stated in your initial packet, to provide the required medical
documentation. Your pay will continue until your Medical
Due Date; this pay is known as “provisional pay.” Your
pay will be suspended after your Medical Due Date if the
required medical documentation has not been approved.
Be sure to provide the required medical documentation at
your earliest opportunity. If you do not meet this Medical
Due Date deadline, your pay will be suspended effective
the first day of the pay period in which it falls. (In cases of
pregnancy, verification of your due date is the only medical
verification required for the short-term disability maternity
benefit, unless you begin your leave of absence more than
two weeks before your estimated date of delivery.) If your
claim is approved, the approval will be effective as of the
date of your disability, and the period of provisional pay will
count toward the duration of your disability benefit.
If your claim is denied before the Medical Due Date due to
your medical circumstances not meeting the truck driver
short-term disability plan’s definition of disability, your pay
will be suspended and Walmart will commence efforts to
recover the amount paid to you for the period following
your illness or injury.
Provisional pay does not apply to relapse/recurrent claims.
Truck driver shor-term disabilityplan
202
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Benefits determination
Sedgwick makes a decision within 45 days of receiving your
properly filed claim. The time for a decision may be extended
for up to two additional 30-day periods. You will be notified
in writing before any extension period that an extension is
necessary due to matters beyond Sedgwick’s control. Those
matters must be identified and you must be given the date by
which Sedgwick will make a decision. If your claim is extended
due to your failure to submit information Sedgwick deems
necessary to decide your claim, the time for decision will be
suspended as of the date on which the notification of the
extension is sent to you until the date Sedgwick receives your
response. If Sedgwick approves your claim, the decision will
contain information sufficient to inform you of that decision.
If Sedgwick denies your claim, you will be sent a written
notification of the denial, which will include:
• Specific reasons for the decision
• Specific reference to the policy provisions on which the
decision is based
• A description of any additional material or information
necessary for you to perfect the claim and an explanation
of why such material or information is necessary
• A description of the appeal procedures and time limits
applicable to such procedures, and
• If an internal rule, guideline, protocol, or other similar
criteria was relied upon in making the denial, either
– The specific rule, guideline, protocol, or other similar
criteria, or
– A statement that such a rule, guideline, protocol, or
other similar criteria was relied upon in making the
denial and that a copy will be provided free of charge to
you upon request.
APPEALING A DISABILITY CLAIM THAT HAS
BEEN FULLY OR PARTIALLY DENIED
If your claim for benefits is denied and you would like
to appeal, you must submit a written or oral appeal to
Sedgwick within 180 days of the denial. Your appeal should
include any comments, documents, records or any other
information you would like considered.
You have the right to request copies, free of charge, of all
documents, records, or other information relevant to your
claim. Your appeal will be reviewed, without regard to your
initial determination, by someone other than the party who
decided your initial claim.
Sedgwick will make a determination on your appeal within
45days of the receipt of your appeal request. This period
may be extended by up to an additional 45 days if it is
determined that special circumstances require an extension
of time. You will be notified prior to the end of the 45-day
period if an extension is required. If you are asked to provide
additional information, you will have 45days from the date
you are notified to provide the information, and the time to
make a determination will be suspended until you provide
the requested information (or the deadline to provide the
information, if earlier).
If your appeal is denied in whole or in part, you will receive a
written notification of the denial that will include:
• The specific reason(s) for the adverse determination
• Reference to the specific plan provisions on which the
determination was based
• A statement describing your right to request copies, free
of charge, of all documents, records, or other information
relevant to your claim
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination, and
• A statement describing any appeal procedures offered by
the Plan.
VOLUNTARY SECOND APPEAL OF A TRUCK
DRIVER SHORTTERM DISABILITY CLAIM
If your appeal is denied, you may make a voluntary second
appeal of your denial orally or in writing to Sedgwick. You
must submit your second appeal within 180 days of the
receipt of the written notice of denial. You may submit any
written comments, documents, records, and any other
information relating to your claim. The same criteria and
response times that applied to your first appeal, as described
earlier, are generally applied to this voluntary second appeal.
All truck driver short-term disability appeals should be sent to:
Walmart Disability and Leave Service Center at Sedgwick
National Appeals Unit
P.O. Box 14028
Lexington, Kentucky 40512
When benefits begin
If you are approved for short-term disability benefits, the
benefit will begin after a waiting period of seven calendar
days. The waiting period begins on your next scheduled work
day after your disability begins. (Work-related disabilities
that qualify for workers’ compensation through Walmart
may have different waiting periods under state law.)
In order for your pay to continue during the initial waiting
period of seven calendar days, you may use paid time off
(PTO). Truck driver short-term disability benefits begin
after the initial waiting period. PTO may not be used while
receiving short-term disability benefits.
If you are receiving short-term disability at the end of the
PTO plan year, please refer to your location’s PTO policy for
payout and/or carryover information.
You do not accrue additional PTO while you are receiving
short-term disability benefits.

Truck driver shor-term disabilityplan
203
Calculating your benefit
The amount of your short-term disability benefit is based on your average day’s pay as of your last day worked. If you become
disabled and eligible to receive short-term disability benefits, the truck driver short-term disability plan replaces 75% of your
average day’s pay as of your last day before your disability for up to 25 weeks, after an initial waiting period of seven calendar
days. There is no maximum weekly benefit under the truck driver short-term disability plan.
YOUR TRUCK DRIVER SHORTTERM DISABILITY PLAN BENEFIT
Duration of your
disability
Your benefit is:
If your disability does not qualify for
workers’ compensation through Walmar
If you have a work-related disability that qualifies for workers’
compensation through Walmar
Up to 26 weeks
After an initial waiting period of
7calendardays, 75% of your average
day’s pay. The waiting period begins on
your next scheduled workday after your
total disability begins.
You may use PTO during your first
7calendar days of continuous disability.
For example, if your average day’s pay
over the week totals $1,000, 75% of
$1,000 is a $750 weekly benefit.
75% of your average day’s pay. Sedgwick will pay 75% during
the state workers’ compensation waiting period, then workers’
compensation will pay according to the state’s compensation
rate. Sedgwick will “top off” this pay to 75%. Ifthe state
compensation rate is greater than 75%, you will not receive
additional benefits from Sedgwick.
For example, if your workers’ compensation benefit or
anticipated benefit is 66%, the shor-term disability benefit
will provide 9% of your wages.
Workers’ compensation is not taxed, while shor-term
disability benefits are taxed.
Shor-term disability benefits are paid through your payroll
check, while workers’ compensation is paid through a
separatecheck.
NOTE: For associates who work in Washington and are eligible for legally mandated benefits as well as benefits under
Walmart’s truck driver short-term disability plan, the amount of the benefit under Walmart’s truck driver short-term
disability plan will be reduced by the amount of the legally mandated benefit.
If a benefit is payable for less than a week, your pay will be based on 75% of your average day’s pay multiplied by your program
for each day you were disabled.
NOTE: Workers’ compensation and short-term disability benefits are made as separate payments except in the states of
Texas and Wyoming, where the entire benefit is included in the payment you receive from Walmart.
MATERNITY BENEFIT
Maternity benefits under the truck driver short-term disability plan are as described here:
MATERNITY BENEFIT
Duration of benefit Your benefit is: If you are eligible for legally mandated benefits in WA:
Up to 9 weeks* 100% of your average day’s pay after an
initial waiting period of 7 calendar days
Legallymandated benefits are payable at the applicable state
or local government rate; the Walmar truck driver shor-term
disability maternity benefit will make up the difference between
the state or local government benefit and 100% of your average
day’s pay after an initial waiting period of 7 calendar days.
Maternity benefits under the truck driver shor-term disability plan begin on the 8th calendar day after
your eligible disability begins. You may use PTO during your first 7 calendar days of continuous disability.
* You may also be eligible for additional parental and family care pay equal to 100% of your average day’s pay. For more
information, refer to the Parental and Family Care Pay policy on One.Walmart.com.
If you begin your short-term disability leave on your delivery date or up to two weeks before your expected delivery date, you
will be deemed to meet the plan’s definition of disability and eligible for maternity disability benefits.
If you begin your leave later than your actual delivery date, you will be eligible for the non-maternity disability benefits only.
Truck driver shor-term disabilityplan
204
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you experience medical complications during pregnancy
or post-partum, benefits may be payable under the truck
driver short-term disability plan after the end of the nine-
week duration of maternity benefits if you continue to meet
the definition of disability. Benefits would be equal to 75%
of your average day’s pay from week 11, up to 25 weeks.
TAXES AND YOUR SHORTTERM
DISABILITYBENEFIT
Benefits payable to you under the truck driver short-term
disability plan are company-provided, at no cost to you.
Because you do not make any contributions to the truck
driver short-term disability plan, any benefits payable to you
are subject to taxes. Walmart generally withholds federal,
state, local and Social Security taxes from the amount of
your benefit payments.
The truck driver short-term disability plan has the right
to recover from you, and you must repay, any amount
overpaid to you for short-term disability benefits under
this plan. See The Plan’s right to recover overpayment and
Right to salary/wage deduction in the Claims and appeals
chapter. If you do not repay overpaid amounts in a timely
manner, the company may deduct such amounts from your
paycheck or future disability benefit payments, to the
extent permitted by law.
When shor-term disability benefit
payments end
If you are receiving short-term disability benefit payments
from the truck driver short-term disability plan due to an
approved disability, your benefit payments from the plan
will end on the earliest of:
• The date you no longer meet the plan’s definition of disabled
• The date you fail to furnish the required proof of disability
when requested to do so by Sedgwick
• The date you are no longer under the continuous care and
treatment of a qualified doctor
• The date you refuse to be examined, if Sedgwick requires
an examination
• The last day of the maximum period for which benefits
are payable (end of 25 weeks, or nine weeks for
maternity benefits)
• The date you are medically able and qualified to work in a
similar full-time position offered to you by Walmart
• The date your employment terminates, or
• The date of your death.
When your short-term disability benefits end and for any
reason you do not return to work, you must request an
extension of your leave; failure to do so may result in your
employment being terminated.
Returning to work
Sedgwick will contact you before your expected return-to-
work date and advise you of steps you may need to take,
including getting a return-to-work certification completed
by your doctor. In some cases, your doctor may release
you to work with certain medical restrictions; any such
restrictions should be explicitly stated on your return-to-
work certification or written release. If you receive a return-
to-work certification containing medical restrictions, you
may be subject to a review to determine whether a job
adjustment or accommodation will help you return to work.
Notify Sedgwick when you physically return to work. If your
short-term disability benefits have ended and you have
not returned to work or communicated your intentions,
Sedgwick will notify you of your options, which include
requesting an extension of your leave or voluntarily
terminating employment. Failure to request an extension
may result in your employment being terminated.
IF YOU RETURN TO WORK AND BECOME
DISABLED AGAIN
If you return to work for 30 calendar days or less of active
full-time work (with or without medical restrictions) and
become disabled again from the same or a related condition
that caused the first period of disability, as determined by
Sedgwick, known as a “relapse/recurrent claim,” your short-
term disability benefits will pick up where they left off
before you came back to work. There will be no additional
waiting period. The combined benefit duration will not
exceed 25 weeks.
If you have returned to active full-time work for more than
30 calendar days and then become disabled from the same
or a related cause, it will be considered a new disability, and
you may be able to receive up to 25 weeks of benefits. A
new benefit waiting period of seven calendar days will apply.
If you have returned to active full-time work for any number
of calendar days and then become disabled from a new
and unrelated cause, it will be considered a new disability,
and you may qualify for up to 25 weeks of benefits. A new
benefit waiting period of seven calendar days will apply.
Intermittent leave. If you are able to return to work after
a period of short-term disability and need to miss work
periodically for reasons related to your disability, notify
Sedgwick and your facility of your situation. Your treatment
may be covered under your prior short-term disability claim
for up to 12 months from the date you return to work from
your short-term disability claim. Truck driver short-term
disability generally pays 100% of your average day’s pay for
the duration of your approved intermittent leave. You will
not need to use PTO for the absences.
Truck driver shor-term disabilityplan
205
Coverage during a leave of absence
or temporary layoff
If you are not working due to an approved non-disability
leave of absence or temporary layoff, you will continue to
be eligible for short-term disability benefits for 90 days
from your last day of work. Your eligibility for short-term
disability benefits ends on the 91st day after the beginning
of your approved non-disability leave or temporary layoff,
but is reinstated if you return to work. See Benefits
continuation if you go on a leave of absence in the Eligibility
and enrollment chapter for more information, including
details on paying for benefits while on leave.
When coverage ends
Your short-term disability coverage ends:
• At termination of your employment
• On the last day of the pay period when your job status
changes from an eligible job status
• On the date you lose eligibility
• On the date of your death
• On the 91st day of an approved non-disability leave of
absence (unless you return to work), or
• When the benefit is no longer offered by the company.
If you leave the company and
arerehired
If you leave the company and return to work for the
company as a full-time truck driver, you will automatically
be reenrolled in the truck driver short-term disability plan.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
This information is intended to be a summary of your benefits and may not include all policy provisions.
Ifthere is a discrepancy between this document and the policy issued by Lincoln Financial Group (Lincoln)
regarding the calculation of benefits and limitations under the policy, the terms of the policy will govern.
Youmay obtain a copy of this policy by contacting Lincoln.
The LTD plans 208
When you qualify for LTD benefits 208
Filing an LTD claim 209
When benefits are not paid 209
When LTD benefits begin 209
Calculating your benefit 209
If you are disabled and working 211
When LTD benefit payments end 211
If you return to work and become disabled again 212
Coverage during a leave of absence or temporary layoff 212
When coverage ends 212
If you leave the company and arerehired 213
If you lose and then regain eligibility 213
Long-term disability

Long-term disability
207
Long-term disability
If you become disabled and can’t work, the company’s long-term disability plan can help. When
you enroll, the plan works with other benefits you get during a disability to replace par of your
paycheck.
RESOURCES
Find What You Need Online Other Resources
Get more details or file a claim Go to One.Walmar.com Call Lincoln at 800-492-5678
What you need to know about long-term disability
• Walmart offers a long-term disability (LTD) plan and also an LTD enhanced plan. If you are a full-time hourly or
management associate, you are eligible to enroll in either plan.
• The LTD plans work with certain other benefits you receive while disabled to replace 50% of your average
monthlywage under the LTD plan or 60% of your average monthly wage under the LTD enhanced plan.
• If you enroll in either plan after your initial eligibility period, your long-term disability coverage will not begin
untilyou complete a 12-month waiting period.
See page 298

Long-term disability
208
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The LTD plans
You are eligible to enroll in LTD coverage if you are a full-
time hourly or management associate. For details about
eligible job classifications, see the Enrollment and eligibility
dates by job classification section in the Eligibility and
enrollment chapter.
You can choose one of two available plans:
• The LTD plan. Provides up to 50% of your average monthly
wage up to a maximum monthly benefit of $15,000 after
your benefit waiting period if you become disabled as
defined by the plan.
• The LTD enhanced plan. Provides up to 60% of your
average monthly wage up to a maximum monthly benefit
of $18,000 after your benefit waiting period if you become
disabled as defined by the plan.
Both plans are insured by Lincoln. For information about
your waiting period, see When LTD benefits begin later in
this chapter. For information about your average monthly
wage, see Calculating your benefit later in this chapter.
The date your coverage begins depends on when you enroll
for coverage:
• If you enroll during your initial enrollment period, your
coverage begins on your effective date, as detailed in the
Eligibility and enrollment chapter.
• If you enroll upon transferring from one eligible job
classification to another, your coverage begins on your
effective date. See the Eligibility and enrollment chapter
for information on your transition enrollment period and
your effective date.
• If you enroll at any time after your initial enrollment
period, you will be considered a late enrollee and required
to finish a 12-month waiting period before your coverage
is effective, as described below. You are not required to
pay LTD plan or LTD enhanced plan premiums during your
12-month waiting period.
– If your late enrollment is due to a status change event,
your 12-month waiting period begins on the date of
theevent.
– If your late enrollment is during an Annual Enrollment,
your 12-month waiting period begin on the date
youenroll.
You may drop your LTD plan or LTD enhanced plan coverage
at any time; the change is effective the day after you drop
coverage. If you drop LTD coverage and later reenroll, you
will be treated as a late enrollee with a 12-month waiting
period, as described above.
See page 298
To receive benefits under the LTD plan or the LTD
enhanced plan, you must be actively at work at the time
ofyour disability.
THE COST OF LTD COVERAGE
Your cost for LTD coverage is based on your biweekly
earnings, your age, and whether you select the LTD plan
or the LTD enhanced plan. Premiums are deducted from
all wages, including bonuses. You are not required to pay
LTD premiums from any LTD benefit payments you receive.
If, however, you receive any other earnings, including
bonuses, through the Walmart payroll systems while you are
receiving LTD benefits, your premiums will be withheld from
those payments.
When you qualify for LTD benefits
Under the terms of the LTD plan and LTD enhanced plans,
“disability” or “disabled” means that, due to a covered
injury or sickness during the benefit waiting period and
forthe next 24 months of disability, you are unable to
perform the material and substantial duties of your own
occupation, and after 24 months of benefit payments, you
are unable to perform the material and substantial duties
of any occupation.
In determining whether you are disabled, Lincoln does
not consider employment factors, including interpersonal
conflict in the workplace, recession, job obsolescence, pay
cuts, job sharing, or loss of professional or occupational
license or certification.
To qualify for LTD benefits:
• You must be unable to return to work after the initial
benefit waiting period of disability.
• You must continue to be under the appropriate care of a
qualified doctor (qualified doctors include legally licensed
physicians and practitioners who are not related to you and
are performing services within the scope of their licenses).
• Lincoln must receive and approve certification with
accompanying medical documentation of a disability
from your qualified doctor before benefits are
considered for payment.
With respect to covered persons employed as pilots and
copilots of an aircraft: “disability” or “disabled” also means
that, as a result of an injury or sickness, you are unable
to perform the material and substantial duties of your
own occupation under the applicable Federal Aviation
Administration fitness standards.
PREEXISTING CONDITION EXCLUSION
You will not receive LTD benefits for any condition,
diagnosed or undiagnosed, for which you received
treatment during the 90-day period prior to your effective
date, unless you have not been treated for the same or
related pre-existing condition for more than 365 days while

Long-term disability
209
insured. Under the terms of the pre-existing condition
exclusion, you are receiving “treatment” when you are
consulting, receiving care or services provided by or under
the direction of a physician, including diagnostic measures;
being prescribed drugs or medicines, whether you choose
to take them or not; and taking drugs or medicines.
If you change from the LTD plan (50% benefit) to the LTD
enhanced plan (60% benefit), the pre-existing condition
exclusion will apply to the additional coverage amount. If
you had satisfied the pre-existing condition requirement
of the LTD plan (50% benefit) and then suffer a disability
before you satisfy the pre-existing condition exclusion of
the LTD enhanced plan (60% benefit), you will only receive
benefits under the LTD plan (50% benefit).
Filing an LTD claim
If you are on an approved short-term disability claim and are
eligible for LTD benefits, your claim will be automatically
transitioned from Sedgwick to Lincoln. You may also call
Lincoln at 800-492-5678 as soon as you know you will
need to use your LTD benefit. Lincoln will provide you with
additional information on how to complete your claim.
Associates receiving workers’ compensation benefits and
enrolled in the LTD plan or LTD enhanced plan may be
eligible for disability benefits after their benefit waiting
period has expired. Call Lincoln at 800-492-5678 to report
your LTD claim.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter. You
have the right to appeal a claim denial. See the Claims and
appeals chapter for details.
When benefits are not paid
Benefits are not paid for any LTD claim due to:
• War, declared or undeclared, or any act of war
• Active participation in a riot
• The committing of or attempting to commit a felony or
misdemeanor, or
• Cosmetic surgery, unless such surgery is in connection
with an injury or sickness sustained while you are a
coveredperson.
No benefit is payable during any period of incarceration.
When LTD benefits begin
If you are approved by Lincoln for LTD benefits, they will
begin after your waiting period: 26 weeks or the end of
yourshort-term disability benefits, whichever is longer.
Paid time off (PTO) may not be used while receiving LTD
benefits. If you are receiving LTD benefits at the end of the
PTO plan year, refer to your location’s PTO policy for payout
and/or carryover information. You do not accrue additional
PTO while receiving LTD benefits.
IF YOU RETURN TO WORK DURING
YOURWAITING PERIOD AND BECOME
DISABLED AGAIN
If you cease to be disabled and return to work full-time for
a total of 60 calendar days or less during a waiting period,
the waiting period will be suspended and you must meet the
balance of the waiting period if you become disabled again. If
you return to work for a total of more than 60 calendar days
while satisfying your benefit waiting period, you must satisfy
an entirely new benefit waiting period if you again become
disabled before you are eligible to receive LTD benefits.
Calculating your benefit
The amount of your LTD benefit is based on:
• Your average monthly wage, and
• If you are enrolled in the LTD plan or the LTD enhanced plan.
AVERAGE MONTHLY WAGE
Length of
employment
How average monthly wage is
determined
Employed 12
months or more
Prior annual pre-disability earnings
÷12months
For example, the average monthly
wage for an associate with prior annual
pre-disability earnings of $36,000 is
$3,000 ($36,000 ÷ 12).
Employed less
than 12 months
Prior annual pre-disability earnings
÷number of months worked
For example, the average monthly
wage for an associate with prior
annual pre-disability earnings of
$21,000 for seven months of work is
$3,000($21,000 ÷ 7).
Annual pre-disability earnings include:
• Overtime
• Bonuses
• Paid time off (not including any previous disability
benefits), and
• Personal pay for the 26 pay periods (52 if paid weekly)
prior to your last day worked. Any pay periods in which you
have no earnings are excluded, decreasing the number of
pay periods used for the calculation.

Long-term disability
210
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Commissions or any other extra compensation or fringe
benefits are not included.
If you have been employed less than 12 months, an
annualized average of earnings will be used.
Your LTD benefit is shown below:
YOUR LTD BENEFIT
If you are enrolled Your coverage is
In the LTD plan 50% of your average monthly wage
minus the amount of other benefits or
income you or your family are eligible
to receive (for example, Social Security
disability benefits*), up to a maximum
monthly benefit of $15,000
In the LTD
enhanced plan
60% of your average monthly wage
minus the amount of other benefits or
income you or your family are eligible
to receive (for example, Social Security
disability benefits*), up to a maximum
monthly benefit of $18,000
* See Other benefits or income that reduces LTD benefits
for more information.
Your benefit will be no less than $100 or 10% of your gross
benefit, whichever is greater, for any month that you are
eligible to receive LTD benefits. The total of your monthly
disability payment, plus all earnings, cannot exceed 100% of
your average monthly wage prior to your disability.
LTD benefits are paid biweekly, as long as you continue to be
disabled as defined by the LTD plans.
Lincoln has the right to recover, and you must repay, any
amount overpaid to you for LTD benefits under the LTD plan
or LTD enhanced plan.
TAXES AND YOUR LTD BENEFIT
You pay 100% of the costs of your LTD coverage with after-
tax contributions. As such, benefits payable to you under
the LTD plans are not subject to income taxes.
OTHER BENEFITS OR INCOME THAT REDUCES
LTD BENEFITS
Your LTD benefit amount is reduced, or offset, by other
benefits or income you or your family receives or are eligible
to receive. Examples include income from the following:
• Social Security disability insurance
• Social Security retirement benefits granted after the date
of disability
• Workers’ compensation
• Employer-related individual policies
• No-fault automobile insurance
• Any ongoing short-term disability benefits payable under
Walmart short-term disability coverage (i.e., relapse-
related benefits)
• An employer retirement plan that begins after the date of
the disability, or
• Settlement or judgment, less associated costs of a lawsuit
that represents or compensates for your loss of earnings.
If any of the benefits that reduce your LTD benefits are
subsequently adjusted by cost-of-living increases, your LTD
benefit will not be further reduced. Refer to the policy for
a complete list of offsets. You may obtain a copy of the LTD
policy by calling Lincoln at 800-492-5678.
EXAMPLE: REDUCTION OF LTD BENEFIT
Annual salary: $36,000 LTD Plan
(50%)
LTD
Enhanced
Plan (60%)
Average monthly wage $3,000 $3,000
Benefit amount
(percentageof average
monthly wage, subject to
themonthly maximum)
$1,500 $1,800
Less estimated Social
Securitydisability benefit
- $750 -$750
Less dependent’s estimated
Social Security benefit
- $375 - $375
LTD payment (monthly) $375 $675
APPLYING FOR SOCIAL SECURITY
DISABILITYBENEFITS
You may be eligible to receive Social Security disability
benefits after you have been disabled for five months.
If your disability has lasted 12 consecutive months, or is
expected to, the LTD policy terms may require you to apply
for Social Security disability benefits. If the Social Security
Administration denies your application for benefits, you will
be required to follow the Social Security Administration’s
appeal process.
Failure to file for Social Security disability benefits
could result in your Social Security retirement benefits
being reduced when you reach the age of retirement. If
you qualify for Social Security disability or retirement
benefits while you are receiving benefits under the LTD
plan and your Social Security disability claim is approved
retroactively, you must reimburse Lincoln for any LTD
benefits overpaid during the period covered by the
retroactive Social Security approval.
Lincoln may assist you in filing for Social Security disability
benefits. To be eligible for assistance, you must be receiving
a benefit from Lincoln.

Long-term disability
211
If you are disabled and working
You may be eligible to receive disability benefits if you
arepartially disabled. Under the Plan, “partial disability”
and “partially disabled” mean that, as a result of sickness
orinjury, you are able to:
• Perform one or more, but not all, of the material and
substantial duties of your own or any occupation on a
full-time or part-time basis, or
• Perform all of the material and substantial duties of your
own occupation on a part-time basis, and
• Earn between 20% and 80% of your indexed
pre-disability earnings.
“Pre-disability monthly earnings” means your regular
monthly rate of pay in effect for the 26 regular pay periods
(52 if paid weekly) immediately prior to your last day worked,
divided by 12. Pre-disability earnings include overtime,
bonuses, paid time off, vacation, illness protection, and
personal pay, but not commissions or other fringe benefits
or extra compensation. If you have worked for less than
12months with the company, your regular monthly rate of
pay will be based on the total earnings you actually received
while working for the company immediately prior to the date
you became disabled, annualized and divided by 12.
“Indexed pre-disability monthly earnings” means your
pre-disability earnings increased annually by 7% or
the percentage change in the Consumer Price Index,
whichever is less.
Lincoln offers a work incentive benefit for the first three
months that you are partially disabled and working. You will
continue to receive the full amount of your monthly benefit
for the first three months if you are partially disabled,
unless your benefit and current monthly earnings exceed
your pre-disability monthly earnings. Your monthly benefit
will be reduced by the excess amount so that the monthly
benefit plus your earnings do not exceed 100% of your pre-
disability monthly earnings.
After the first three months that you are partially disabled
and working, the following calculation is used to determine
your monthly benefit for a partial disability.
DISABLED AND WORKING BENEFIT CALCULATION
(A – B) x C
A
= D
A Your indexed pre-disability monthly earnings
B Your current monthly earnings
C
The monthly benefit payable if you were qualified
asdisabled
D The disabled and working benefit payable
IF YOU PASS AWAY WHILE RECEIVING
LTDBENEFITS
Coverage under the LTD plans ends upon your death.
However, if you pass away while receiving LTD benefits, a
lump-sum payment of $5,000 or three times your gross
monthly LTD benefit, whichever is greater, will be paid to
your surviving spouse/partner. If you are not survived by a
spouse/partner, the payment will be made to your surviving
children, including stepchildren and legally adopted
children, in equal shares. However, if any of these children
are minors or incapacitated, payment will be made on their
behalf to the court-appointed guardian of the children’s
property. If you are not survived by a spouse/partner or
children, the payment will be made to your estate.
When LTD benefit payments end
LTD benefit payments end on the earliest of:
• The date you fail to furnish proof of continued disability
and regular attendance of a doctor
• The date you fail to cooperate in the administration of your
claim. For example: providing information or documents
needed to determine whether benefits are payable and/or
determining the benefit amount
• The date you refuse to be examined or evaluated at
reasonable intervals
• The date you refuse to receive appropriate available
treatment
• The date you refuse a similar job with Walmart, paying
comparable wages, where workplace modifications or
accommodations are made to allow you to perform the
material and substantial duties of your job
• The date you are able to work in your own occupation on a
part-time basis but choose not to
• The date your partial disability monthly earnings exceed
80% of your indexed pre-disability earnings
• The date you no longer meet the plan’s definition
ofdisabled
• The last day of the maximum period for which benefits
arepayable (see charts on the next page), or
• The date of your death.

Long-term disability
212
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
MAXIMUM DURATION OF LTD BENEFITS
Age when you
becomedisabled
Benefits duration
(months of LTD benefits)
Prior to age 62 Until normal retirement age
(as listed below)
62 48 months
63 42 months
64 36 months
65 30 months
66 27 months
67 24 months
68 21 months
69 or older 18 months
SOCIAL SECURITY NORMAL RETIREMENT AGE
Year of birh Normal retirement age
1937 or before 65
1938 65 + 2 months
1939 65 + 4 months
1940 65 + 6 months
1941 65 + 8 months
1942 65 + 10 months
1943 through 1954 66
1955 66 + 2 months
1956 66 + 4 months
1957 66 + 6 months
1958 66 + 8 months
1959 66 + 10 months
1960 or after 67
IF THE DISABILITY IS DUE TO MENTAL
ILLNESS, ALCOHOLISM, OR DRUG ADDICTION
To receive LTD benefits for more than 24 months for the
following disabilities, you must be confined in a hospital or
other facility licensed to provide medical care:
• Mental illness (excluding demonstrable, structural
braindamage)
• Any condition that results from mental illness
• Alcoholism, and
• Non-medical use of narcotics, sedatives, stimulants,
hallucinogens, or similar substances.
When you are not confined to a hospital or other licensed
facility, there is a 24-month lifetime benefit for these
disabilities unless you are fully participating in an extended
treatment plan for the condition that caused the disability,
in which case the benefit is payable for up to 36 months.
If you return to work and become
disabled again
If you return to work for less than six months of active
full-time work and become disabled again from the same or a
related condition that caused the first period of disability, as
determined by Lincoln, known as a “relapse/recurrent claim,”
the recurrent disability will be part of the same disability.
Your LTD benefits will pick up where they left off before
you came back to work. There will be no additional waiting
period. The combined benefit duration for both periods of
disability will not exceed the maximum duration listed in the
chart to the left.
If you return to work as an active full-time associate for
six months or more, any recurrence of a disability will be
treated as a new disability. A new benefit waiting period
must be completed.
Coverage during a leave of absence
or temporary layoff
Once your LTD coverage is effective and you are eligible
to file a claim for benefits, if you are not actively at work
due to an approved non-disability leave of absence or
temporary layoff, you will continue to be eligible for LTD
benefits for 90 days from your last day of work. Your
eligibility for LTD benefits ends on the 91st day after your
approved non-disability leave or temporary layoff begins,
but is reinstated if you return to active work status within
one year. See Benefits continuation if you go on a leave of
absence in the Eligibility and enrollment chapter for more
information, including details on paying for benefits while
on leave.
When coverage ends
Your LTD coverage ends:
• At termination of your employment, unless you have
been absent due to disability during the 26-week benefit
waiting period and any period during which premium
payments are waived
• On the last day of the pay period when your job status
changes from an eligible job status
• Upon failure to pay your premiums
• On the date you lose eligibility
• If you do not return to work after the last day of an
approved leave of absence
• When the benefit is no longer offered by the company
• The day after you drop coverage, or
• On the date of your death.

Long-term disability
213
If you leave the company and
arerehired
If you leave the company and return to full-time work for
the company within 13 weeks, you will automatically be
reenrolled for the same coverage plan you had prior to
leaving the company (or the most similar coverage offered
under the Plan). If you are automatically reenrolled in LTD
plan or LTD enhanced plan coverage and choose to drop it
after you return, you may do so at any time.
See page 298
If you return to full-time work after 13 weeks, you will be
considered newly eligible and may enroll for coverage under
the time periods and conditions described in the Eligibility
and enrollment chapter.
If you lose and then regain eligibility
If you lose eligibility and then regain eligibility within
30days, you will automatically be reenrolled for the same
coverage you had prior to losing eligibility (or the most
similar coverage offered under the Plan).
If you lose eligibility and then regain eligibility after 30 days,
you will be considered newly eligible and may enroll for
coverage under the time periods and conditions described
in the Eligibility and enrollment chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The truck driver LTD plans 216
When you qualify for truck driver LTD benefits 216
Filing a truck driver LTD claim 217
When benefits are not paid 217
When truck driver LTD benefitsbegin 217
Calculating your benefit 218
If you are disabled and working 219
When truck driver LTD benefit payments end 220
If you return to work and become disabled again 221
Coverage during a leave of absence or temporary layoff 221
When coverage ends 221
If you leave the company and arerehired 221
If you lose and then regain eligibility 221
This information is intended to be a summary of your benefits and may not include all policy provisions. If
there is a discrepancy between this document and the policy issued by Lincoln Financial Group (Lincoln)
regarding the calculation of benefits and limitations under the policy, the terms of the policy will govern.
Youmay obtain a copy of this policy by contacting the Plan.
Truck driver
long-termdisability

Truck driver long-termdisability
215
Truck driver long-term disability
If a disability keeps you off the road and unable to work, this plan works with other benefits you
get to replace par of your paycheck. There are two long-term disability plans for truck drivers
that pay benefits for different lengths of time.
RESOURCES
Find What You Need Online Other Resources
Get more details or file a claim Go to One.Walmar.com Call Lincoln at 800-492-5678
What you need to know about truck driver long-term disability
• Walmart offers truck drivers a long-term disability (LTD) plan and also an LTD enhanced plan. If you are a full-time
truck driver, you are eligible to enroll in either plan. Each plan offers a choice of full-duration coverage or five-year
coverage.
• The truck driver LTD plans works with certain other benefits you receive while disabled to replace 50% of your
average monthly wage if you select the truck driver LTD plan or 60% of your average monthly wage if you select the
truck driver LTD enhanced plan.
• If you enroll in either plan after your initial eligibility period, you will have to submit Evidence of Insurability, and you
may be required to undergo a medical exam at your own expense before you can be approved for coverage.

Truck driver long-termdisability
216
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The truck driver LTD plans
You are eligible to enroll in truck driver LTD coverage if you
are a full-time truck driver. You can choose between two
coverage plans, each of which is available in two options:
• LTD plan
– Five-year coverage
– Full-duration coverage
• LTD enhanced plan
– Five-year coverage
– Full-duration coverage
The truck driver LTD plan options pay benefits as described
in the following chart.
Both plans are insured by Lincoln.
TRUCK DRIVER LTD
LTD PLAN LTD ENHANCED PLAN
Five-year
coverage
Pays 50% of average
monthly wage up to
a maximum monthly
benefit of $15,000
Pays 60% of average
monthly wage up to
a maximum monthly
benefit of $18,000
Both plans pay benefits for 60 months, unless
the longer of the following time periods is less
than 60 months, in which case the monthly
benefit will be payable for the longer period:
• The amount of time shown in the Maximum
duration of truck driver LTD char (later in
this chapter), or
• The amount of time between the date you
become disabled and your normal retirement
age under the Social Security Act, as shown
in the Social Security normal retirement age
char (later in this chapter).
LTD PLAN LTD ENHANCED PLAN
Full-
duration
coverage
Pays 50% of average
monthly wage up to
a maximum monthly
benefit of $15,000
Pays 60% of average
monthly wage up to
a maximum monthly
benefit of $18,000
Both plan options pay benefits for the longer of:
• The amount of time shown in the Maximum
duration of LTD benefits char (later in this
chapter), or
• The amount of time between the date you
become disabled and your normal retirement
age under the Social Security Act, as shown
in the Social Security normal retirement age
char (later in this chapter).
The date your coverage is effective depends on when you
enroll for coverage:
• If you enroll during your initial enrollment period, your
coverage will be effective on your date of hire.
• If you enroll at any time after your initial enrollment
period, you will be considered a late enrollee. Your
coverage will be effective the first day of the pay period
after People Services receives approval from Lincoln. You
will be required to provide Evidence of Insurability (you
must complete a medical history questionnaire and may be
required to undergo a medical exam at your own expense)
and may be denied coverage.
• If you enroll in the five-year coverage plan and
subsequently decide to enroll in the full-duration coverage
plan, you will be considered a late enrollee and required
to provide Evidence of Insurability before you can be
approved for coverage. Your coverage will be effective the
first day of the pay period after People Services receives
approval from Lincoln.
You may drop your truck driver LTD plan or truck driver LTD
enhanced plan coverage at any time; the change will be
effective the day after you drop coverage. If you drop LTD
coverage and later decide to reenroll in either plan, you will
be treated as a late enrollee, as described above.
See page 298
THE COST OF TRUCK DRIVER LTD COVERAGE
Your cost for truck driver long-term disability coverage is
based on your biweekly earnings and the type of truck driver
LTD coverage you select. Premiums are deducted from all
wages, including bonuses. You are not required to pay truck
driver LTD premiums from any truck driver LTD benefit
payments you receive. If, however, you receive any other
earnings, including bonuses, through the Walmart payroll
systems while you are receiving truck driver LTD benefits,
your premiums will be withheld from those payments.
When you qualify for truck driver
LTD benefits
Under the terms of the truck driver LTD plans, “disability”
or “disabled” means that, due to an injury or sickness during
the benefit waiting period and for the next 24 months
of disability, you are unable to perform the material and
substantial duties of your own occupation, or you lose
medical certification in accordance with the Federal Motor
Carrier Safety Regulations. After 24 months of benefit
payments, “disability” or “disabled” means that you are
unable to perform the material and substantial duties of
any occupation.
Truck driver long-termdisability
217
In determining whether you are disabled, Lincoln does
not consider employment factors, including interpersonal
conflict in the workplace, recession, job obsolescence, pay
cuts, job sharing, or loss of professional or occupational
license or certification for reasons other than a covered
injury or sickness.
To qualify for truck driver LTD benefits:
• You must be unable to return to work after the initial
benefit waiting period of disability.
• You must continue to be under the appropriate care of a
qualified doctor (qualified doctors include legally licensed
physicians and practitioners who are not related to you and
are performing services within the scope of their licenses).
• Lincoln must receive and approve certification with
accompanying medical documentation of a disability
from your qualified doctor before benefits are
considered for payment.
If you file a claim within the first two years of your approval
date, Lincoln has the right to re-examine your Evidence
of Insurability questionnaire. If material facts about you
are found to have been stated inaccurately, the true
circumstances will be used to determine if your coverage
should be in effect and for what amount, and your premium
may be adjusted.
PREEXISTING CONDITION EXCLUSION
You will not receive truck driver LTD benefits for any
condition, diagnosed or undiagnosed, for which you
received treatment during the 90-day period prior to
your effective date unless you have not been treated for
the same or related pre-existing condition for more than
365 continuous days while insured. Under the terms of
the pre-existing condition exclusion, you are receiving
“treatment” when you are consulting, receiving care or
services provided by or under the direction of a physician,
including diagnostic measures; being prescribed drugs or
medicines, whether you choose to take them or not; and
taking drugs or medicines.
If you change from the five-year duration coverage to the
full-duration coverage under either of the truck driver LTD
plans, the pre-existing condition exclusion will apply to the
additional duration. If you had satisfied the pre-existing
condition requirement of the five-year duration coverage
plan and then suffer a disability before you satisfy the pre-
existing condition exclusion of the full-duration coverage
plan, you will only receive benefits under the five-year
duration coverage plan.
Filing a truck driver LTD claim
If you are on an approved short-term disability claim and are
eligible for LTD benefits, your claim will be automatically
transitioned from Sedgwick to Lincoln. You may also call
Lincoln at 800-492-5678 as soon as you know you will need
to use your truck driver LTD benefit. Lincoln will provide you
with additional information on how to complete your claim.
Claims are determined under the time frames and
requirements set out in the Claims and appeals chapter. You
have the right to appeal a claim denial. See the Claims and
appeals chapter for details.
When benefits are not paid
Benefits are not paid for any truck driver LTD claim due to:
• War, declared or undeclared, or any act of war
• Active participation in a riot
• The committing of or attempting to commit a felony or
misdemeanor, or
• Cosmetic surgery, unless such surgery is in connection
with an injury or sickness sustained while the individual is a
covered person.
No benefit is payable during any period of incarceration.
When truck driver LTD
benefitsbegin
If you are approved by Lincoln for truck driver LTD
benefits, they will begin after your benefit waiting period:
26weeks or the end of your short-term disability benefits —
whichever is longer.
Paid time off (PTO) may not be used while receiving LTD
benefits. If you are receiving LTD benefits at the end of the
PTO plan year, refer to your location’s PTO policy for payout
and/or carryover information. You do not accrue additional
PTO while receiving LTD benefits.
IF YOU RETURN TO WORK DURING
YOUR WAITING PERIOD AND BECOME
DISABLEDAGAIN
If you cease to be disabled and return to work for a total of
60 calendar days or less during a waiting period, the waiting
period will be suspended and you must meet the balance
of the waiting period if you become disabled again. If you
return to work for a total of more than 60 calendar days
while satisfying your benefit waiting period, you must satisfy
an entirely new benefit waiting period if you again become
disabled before you are eligible to receive LTD benefits.

Truck driver long-termdisability
218
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Calculating your benefit
The amount of your truck driver LTD is based on:
• Your average monthly wage, and
• Which truck driver LTD plan you’re enrolled in.
AVERAGE MONTHLY WAGE
Length of employment How average monthly wage
isdetermined
Employed 12 months
ormore
Your activity pay, mileage rate,
and bonuses, paid in the 26 pay
periods prior to your last day
worked÷ 12months
Employed less than
12months
Your activity pay, mileage rate,
and bonuses ÷ the number of
months worked
Note that any pay periods in which you have no earnings are
excluded, decreasing the number of pay periods used for
the calculation.
Your truck driver long-term disability benefit is shown below:
YOUR TRUCK DRIVER LONGTERM DISABILITY BENEFIT
If you are enrolled Your coverage is
In the truck driver
five-year coverage LTD
plan or the truck driver
full-duration coverage
LTD plan
50% of your average monthly
wage minus the amount of other
benefits or income you or your
family are eligible to receive (for
example, Social Security disability
benefits*), up to a maximum
monthly benefit of $15,000
In the truck driver
five-year coverage
LTD enhanced plan
or the truck driver
full-duration coverage
LTD enhanced plan
60% of your average monthly
wage minus the amount of other
benefits or income you or your
family are eligible to receive (for
example, Social Security disability
benefits*), up to a maximum
monthly benefit of $18,000
* See Other benefits or income that reduces truck driver
long-term disability benefits for more information
Your benefit will be no less than $100 or 10% of your gross
benefit, whichever is greater, for any month that you are
eligible to receive truck driver LTD benefits. The total of
your monthly disability payment, plus all earnings, cannot
exceed your average monthly wage prior to your disability.
Truck driver LTD benefits are paid biweekly, as long as
you continue to be disabled as defined by the truck driver
LTDplans.
Lincoln has the right to recover from you any amount that
is overpaid to you for truck driver LTD benefits under the
truck driver LTD plan or the truck driver LTD enhanced plan.
TAXES AND YOUR LTD BENEFIT
You pay 100% of the costs of your LTD coverage with after-
tax contributions. As such, benefits payable to you under
the truck driver LTD plans are not subject to income taxes.
OTHER BENEFITS OR INCOME THAT REDUCES
TRUCK DRIVER LTD BENEFITS
Your truck driver LTD benefit amount is reduced, or offset,
by other benefits or income you or your family receive
orare eligible to receive. Examples include income from
the following:
• Social Security disability insurance
• Social Security retirement benefits that are granted after
the date of disability
• Workers’ compensation
• Employer-related individual policies
• No-fault automobile insurance
• Any ongoing short-term disability benefits payable under
Walmart short-term disability coverage (i.e., relapse-
related benefits)
• An employer retirement plan that begins after the date of
the disability, or
• Settlement or judgment, less associated costs of a lawsuit,
that represents or compensates for your loss of earnings.
If any of the benefits that reduce your LTD benefits are
subsequently adjusted by cost-of-living increases, your LTD
benefit will not be further reduced. Refer to the policy for a
complete list of offsets. You may obtain a copy of the truck
driver LTD policy by calling Lincoln at 800-492-5678.
EXAMPLE: REDUCTION OF TRUCK DRIVER LTD BENEFIT
LTD Plan
(50%)
LTD
Enhanced
Plan (60%)
Average monthly wage $3,000 $3,000
Benefit amount (percentage
of average monthly wage,
subject to the monthly
maximum)
$1,500 $1,800
Less estimated Social Security
disability benefit
- $750 - $750
Less dependent’s estimated
Social Security benefits
- $375 - $375
LTD payment (monthly) $375 $675

Truck driver long-termdisability
219
APPLYING FOR SOCIAL SECURITY
DISABILITYBENEFITS
You may be eligible to receive Social Security disability
benefits after you have been disabled for five months.
If your disability has lasted 12 consecutive months, or is
expected to, the truck driver LTD policy terms may require
you to apply for Social Security disability benefits. If the
Social Security Administration denies you benefits, you will
be required to follow the Social Security Administration’s
appeal process.
Failure to file for Social Security disability benefits could
result in your Social Security retirement benefits being
reduced when you reach the age of retirement. If you
qualify for Social Security disability or retirement benefits
while you are receiving benefits under any of the truck
driver LTD plan options and your Social Security disability
claim is approved retroactively, you must reimburse Lincoln
for any LTD benefits overpaid during the period covered by
the retroactive Social Security approval.
Lincoln may assist you in filing for Social Security disability
benefits. To be eligible for assistance, you must be receiving
a benefit from Lincoln.
If you are disabled and working
You may be eligible to receive disability benefits if you are
partially disabled. Under the truck driver LTD plans, “partial
disability” and “partially disabled” mean that, as a result of
sickness or injury, you are able to:
• Perform one or more, but not all, of the material and
substantial duties of your own or any occupation on a
full- time or part-time basis, or
• Perform all of the material and substantial duties of your
own occupation on a part-time basis, and
• Earn between 20% and 80% of your indexed pre-disability
earnings.
“Pre-disability monthly earnings” means your activity
pay, mileage rate, and bonus in effect for the 52 weeks
immediately prior to your last day worked, divided by 12.
“Indexed pre-disability monthly earnings” means your
pre-disability monthly earnings increased annually by 7%
or the percentage change in the Consumer Price Index,
whichever is less.
Lincoln offers a work incentive benefit for the first
threemonths that you are partially disabled and working.
You will continue to receive the full amount of your
monthly benefit for the first three months if you are
partially disabled, unless your benefit and current monthly
earnings exceed your pre-disability monthly earnings. Your
monthly benefit will be reduced by the excess amount so
that the monthly benefit plus your earnings do not exceed
100% of your pre-disability monthly earnings.
After the first three months that you are partially disabled
and working, the following calculation is used to determine
your monthly benefit for a partial disability.
DISABLED AND WORKING BENEFIT CALCULATION
(A – B) x C
A
= D
A Your indexed pre-disability monthly earnings
B Your current monthly earnings
C
The monthly benefit payable if you were qualified
asdisabled
D The disabled and working benefit payable
IF YOU PASS AWAY WHILE RECEIVING TRUCK
DRIVER LTD BENEFITS
Coverage under the truck driver LTD plans ends upon your
death. However, if you pass away while receiving truck
driver LTD benefits, a lump sum payment of $5,000 or
three times your gross monthly LTD benefit, whichever
is greater, will be paid to your surviving spouse/partner. If
you are not survived by a spouse/partner, the payment will
be made to your surviving children, including stepchildren
and legally adopted children, in equal shares. However, if
any of these children are minors or incapacitated, payment
will be made on their behalf to the court-appointed
guardian of the children’s property. If you are not survived
by a spouse/partner or children, the payment will be made
to your estate.
Truck driver long-termdisability
220
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
When truck driver LTD benefit
payments end
Truck driver LTD benefit payments end on the earliest of:
• The date you fail to furnish proof of continued disability
and regular attendance of a doctor
• The date you fail to cooperate in the administration of your
claim. For example: providing information or documents
needed to determine whether benefits are payable and/or
determining the benefit amount
• The date you refuse to be examined or evaluated at
reasonable intervals
• The date you refuse to receive appropriate available
treatment
• The date you refuse a similar job with Walmart, paying
comparable wages, where workplace modifications or
accommodations are made to allow you to perform the
material and substantial duties of your job
• The date you are able to work in your own occupation on a
part-time basis but choose not to
• The date your partial disability monthly earnings exceed
80% of your indexed pre-disability earnings
• The date you no longer meet the plan’s definition of
disabled
• The last day of the maximum period for which benefits are
payable (see charts on the right), or
• The date of your death.
FIVEYEAR COVERAGE
Five-year coverage pays benefits for 60 months unless the
longer of the following time periods is less than 60 months,
in which case the monthly benefit will be payable for the
longer period:
• The amount of time shown in the Maximum duration of
truck driver LTD char on the right; or
• The amount of time between the date you become
disabled and your normal retirement age under the Social
Security Act, as shown in the Social Security normal
retirement age char on the right.
FULLDURATION COVERAGE
Full-duration coverage pays benefits for the longer of:
• The amount of time shown in the Maximum duration of
truck driver LTD char on the right; or
• The amount of time between the date you become
disabled and your normal retirement age under the Social
Security Act, as shown in the Social Security normal
retirement age char on the right.
MAXIMUM DURATION OF LTD BENEFITS
Age when you
becomedisabled
Benefits duration
Prior to age 62 Until normal retirement age
(aslisted below)
62 48 months
63 42 months
64 36 months
65 30 months
66 27 months
67 24 months
68 21 months
69 or older 18 months
SOCIAL SECURITY NORMAL RETIREMENT AGE
Year of birh Normal retirement age
1937 or before 65
1938 65 + 2 months
1939 65 + 4 months
1940 65 + 6 months
1941 65 + 8 months
1942 65 + 10 months
1943 through 1954 66
1955 66 + 2 months
1956 66 + 4 months
1957 66 + 6 months
1958 66 + 8 months
1959 66 + 10 months
1960 or after 67
IF THE DISABILITY IS DUE TO MENTAL
ILLNESS, ALCOHOLISM, OR DRUG ADDICTION
To receive truck driver LTD benefits for more than
24months for the following disabilities, you must be
confined in a hospital or other place licensed to provide
medical care:
• Mental illness (excluding demonstrable, structural brain
damage)
• Any condition that results from mental illness
• Alcoholism, and
• Non-medical use of narcotics, sedatives, stimulants,
hallucinogens, or similar substances.

Truck driver long-termdisability
221
When you are not confined to a hospital or other licensed
facility, there is a 24-month lifetime benefit for these
disabilities unless you are fully participating in an extended
treatment plan for the condition that caused the disability,
in which case the benefit is payable for up to 36 months.
If you return to work and become
disabled again
If you return to work for less than six months of active
full-time work and become disabled again from the same or
a related condition that caused the first period of disability,
as determined by Lincoln, known as a “relapse/recurrent
claim,” the recurrent disability will be part of the same
disability. Your LTD benefits will pick up where they left off
before you came back to work. No additional waiting period
will be required. The combined benefit duration for both
periods of disability will not exceed the maximum duration
listed in the chart on the previous page.
If you return to work as an active full-time associate for
six months or more, any recurrence of a disability will be
treated as a new disability. A new benefit waiting period
must be completed.
Coverage during a leave of absence
or temporary layoff
Once your truck driver LTD coverage is effective and
you are eligible to file a claim for benefits, if you are not
actively at work due to an approved non-disability leave
of absence or temporary layoff, you will continue to be
eligible for truck driver LTD benefits for 90 days from
your last day of work. Your eligibility for truck driver LTD
benefits ends on the 91st day after your approved non-
disability leave or temporary layoff begins, but is reinstated
if you return to active work status within one year. See
Benefits continuation if you go on a leave of absence in the
Eligibility and enrollment chapter for more information,
including details on paying for benefits while on leave.
When coverage ends
Your truck driver LTD coverage ends:
• At termination of your employment, unless you have
been absent due to disability during the 26-week benefit
waiting period and any period during which premium
payments are waived
• On the last day of the pay period when your job status
changes from an eligible job status
• Upon failure to pay your premiums
• On the date you lose eligibility
• If you do not return to work after the last day of an
approved leave of absence
• When the benefit is no longer offered by the company
• On the day after you drop coverage, or
• On the date of your death.
If you leave the company and
arerehired
If you leave the company and return to full-time work for
the company within 13 weeks, you will automatically be
reenrolled for the same coverage you had prior to leaving
the company (or the most similar coverage offered under
the Plan). If you are automatically reenrolled in truck driver
LTD plan or LTD enhanced plan coverage and choose to
drop it after you return, you may do so at any time.
See page 298
If you return to full-time work after 13 weeks, you will be
considered newly eligible and may enroll for coverage under
the time periods and conditions described in the Eligibility
and enrollment chapter.
If you lose and then regain eligibility
If you lose eligibility and then regain eligibility within
30days, you will automatically be reenrolled for the same
coverage you had prior to losing eligibility (or the most
similar plans offered under the Plan).
If you lose eligibility and then regain eligibility after 30 days,
you will be considered newly eligible and may enroll for
coverage under the time periods and conditions described
in the Eligibility and enrollment chapter.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Associate Stock Purchase Planeligibility 224
Enrolling in the Associate Stock Purchase Plan 224
Walmar’s contribution to your company stock ownership 224
Selling stock through the Plan 225
Keeping track of your Computershare account 225
Ending your paricipation and closing your account 225
If you leave the company 225
PROSPECTUS 226
Introduction and overview 226
Plan administration; accountmanagement 227
Plan paricipation and eligibility 227
Plan contributions — Stock PurchaseProgram 228
Stock ownership, fees, and risks 229
Stock cerificate delivery and Stocksales 230
Termination of paricipation; accountclosure 231
Plan amendment and termination 232
Tax information 232
Available information 233
Electronic delivery of prospectuses and other documents 233
Documents incorporated byreference 233
The Associate Stock
Purchase Plan (ASPP)

The Associate Stock Purchase Plan (ASPP)
223
The Associate Stock Purchase Plan (ASPP)
The Associate Stock Purchase Plan (ASPP or Plan) allows you to buy Walmar stock conveniently
through payroll deductions and through direct payments to the Plan Administrator. You can have
any amount from $2 to $1,000 withheld from your biweekly paycheck ($1 to $500 if you are paid
weekly) to buy stock. Walmar matches $0.15 for every dollar that you contribute through payroll
deduction to purchase stock, up to the first $1,800 you contribute to the Plan in each Plan year
(April through March).
RESOURCES
Find What You Need Online Other Resources
Enroll in the Plan or change your
deduction amount
Complete an online enrollment session
on One.Walmar.com/ASPP or Workday
for Jet associates
• Access your account information
• Get your account statement
• Get a Form 1099
Go to the Computershare website at
computershare.com/walmar
Call Computershare at 800-438-6278
(hearing impaired: 800-952-9245) or get
the Associate Stock app (available for
Apple or Android devices)
Send money directly to Computershare Send check to:
Computershare
Attn: Walmar ASPP
P.O. Box 505042
Louisville, Kentucky 40233
(Company matching contributions will
not be made on money sent directly to
Computershare)
What you need to know about the Associate Stock Purchase Plan
• All eligible associates can purchase Walmart stock through convenient payroll deductions and direct payments
toComputershare.
• Walmart matches $0.15 for every $1 you put into the Plan through payroll deductions, up to the first $1,800 that
youcontribute in each plan year.
• There are no fees to purchase shares of Walmart stock through the Plan. You only pay a fee when you sell shares of stock.
• Your shares will be credited to an account that is maintained in your name at Computershare. You can access your
account online, by telephone, or app (see Resources chart above) to get your balance or sell stock held in your account.

The Associate Stock Purchase Plan (ASPP)
224
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Associate Stock Purchase
Planeligibility
You are eligible to enroll in the Associate Stock Purchase
Plan if you are:
• Not a member of a collective bargaining unit whose
benefits were the subject of good faith collective
bargaining.
• At least 18 years of age or the legal age of majority in your
payroll state to participate (19 is the legal age of majority in
Alabama and Nebraska). If you live in Puerto Rico, you must
be 21 years of age to participate. If you have questions
about the age requirement, review your state laws on legal
age of majority.
Enrolling in the Associate Stock
Purchase Plan
You can enroll in the Plan by completing an online benefits
enrollment session on One.Walmart.com/ASPP or Workday
for Jet associates. Before you enroll in this plan, you
should carefully review this Associate Stock Purchase Plan
brochure and the Plan Prospectus (a copy of which appears
on the following pages), as well as the reports and other
documents that the company has incorporated by reference
into the Plan Prospectus.
The decision to participate in the Plan and to purchase
company stock is an individual decision to be made solely
by you. The company is not recommending, endorsing,
or soliciting your participation in the Plan or purchase of
company stock. In making your decision, you should be
aware that the past performance of the company stock
is not an indication or prediction of future performance.
The value of company stock may be affected by many
factors, including those outside the company itself,
such as economic conditions. The company urges you to
consult with your financial and tax advisors regarding your
participation in the Plan and investment in company stock.
Walmar’s contribution to your
company stock ownership
The Associate Stock Purchase Plan allows all eligible
associates to buy Walmart stock conveniently through
payroll deductions. You can have any whole dollar amount
from $2 to $1,000 withheld from your paycheck to buy stock
($1 to $500 for associates with a weekly paycheck).
Walmart contributes to your stock purchase account by
matching $0.15 for every $1 you contribute to the Plan
through payroll deductions, up to your first $1,800 you
contribute in each Plan year. The Plan year runs from April
through March. The company match is reflected as income
on your check stub and on your Form W-2.
In addition to your payroll deductions, you can also contribute
to the Associate Stock Purchase Plan by sending money
directly to Computershare, the Plan’s administrator, at:
Computershare
Attn: Walmart ASPP
P.O. Box 505042
Louisville, Kentucky 40233
Money sent directly to Computershare will not receive the
Walmart matching contribution. The total of your payroll
deductions and money sent directly to Computershare
cannot exceed $125,000 per Plan year. Dividends paid on
the stock you hold as of each dividend record date are
automatically reinvested to buy additional shares of stock
for you, but do not count against the $125,000 maximum.
The value of the stock you purchase can fluctuate and may
decline. There is no way to guarantee that your stock will
have the same value in the future that it had when you made
the purchase or that the value of the stock will increase.
When making a decision about purchasing Walmart stock,
consider all your investments, including other Walmart stock
you may own. For investment questions, consult a financial
advisor. Investment in the stock is subject to certain risks
as described in the Plan Prospectus and Walmart’s most
recent Annual Report on Form 10-K that is incorporated by
reference in the Plan Prospectus.
WALMART’S CONTRIBUTION TO YOUR COMPANY STOCK OWNERSHIP
If you contribute
Your Plan year payroll deduction
contribution is
Walmar’s matching
contribution* is
Total amount used to purchase
Walmar stock
$10 biweekly $260 $39 $299
$20 biweekly $520 $78 $598
$70 biweekly $1,820
$270 (Walmar matches $0.15
forevery $1 up to $1,800)
$2,090
* Company contributions will be made only on stock purchased through payroll deductions. Company contributions will not be made on
money sent directly to Computershare.
The Associate Stock Purchase Plan (ASPP)
225
Selling stock through the Plan
No fees are charged to you for buying stock; however, when
you sell stock you will be charged a fee. The fees charged by
Computershare as described in this section are subject to
change from time to time.
If you choose to sell your stock, your stock will be sold
pursuant to a market order. Your stock will be sold as soon
as your request can reasonably be processed. Generally,
market orders are executed immediately after they are
placed. The price at which your order will be executed is
not guaranteed, and the Walmart stock price prior to the
execution of your order is not necessarily the price at which
your order will be executed.
Generally, any sales of your stock will be executed over the
New York Stock Exchange (NYSE). If the NYSE is closed
when your order is ready to be processed, your order will be
processed as early as possible on the next NYSE trading day.
The fee is $25.50 per sale plus $0.05 (five cents) per share
sold for each sell you execute.
You can sell stock from computershare.com/walmart, from
the Associate Stock app (available for Apple and Android
devices), or by calling Computershare at 800-438-6278.
You can choose to have your proceeds deposited to a bank
account on file or have a check mailed to the address on file
at Computershare. If you choose to deposit your proceeds
in a bank account, your funds are sent to the bank on the
share settlement date, which is two business days from
the date of sale. If you select to receive your proceeds via
check, you should receive your check within seven to 10
business days after you place an order to sell stock in your
Plan account.
The sell fee is automatically deducted from the amount
deposited or reported on your check for the net proceeds
of the sale. Each time you sell stock, you will receive a
transaction summary form. For tax reporting purposes,
you’ll receive appropriate tax documents (1099B and/or
1099DIV) enclosed with your annual statement in the first
quarter of the following year (January through March).
These documents will be mailed to your address on file with
Computershare and should be used when filing your taxes.
It’s important to understand the tax consequences of a
stock sale. If you have tax-related questions, please consult
a financial advisor or tax consultant.
Keeping track of your
Computershare account
You will receive a statement from Computershare at least
annually (first quarter) that shows the activity in your
account. However, if you opted to receive your statements
electronically, you will receive an email informing
you that your statement is ready and can be found on
computershare.com/walmart.
The annual statement you receive will contain important
tax information. It is very important that you keep your
statement so that you will know the difference between
your purchase price and sale price of any shares of stock you
sell. You will need this information for your income taxes.
You can access your account information online at
computershare.com/walmart, by the Associate Stock app
(available for Apple and Android devices), or by phone at
800-438-6278 (hearing impaired: 800-952-9245).
If you request replacement statements from
Computershare, there is a $5 charge per statement for
previous years’ statements. Or, you can obtain copies free of
charge through the website at computershare.com/walmart.
Ending your paricipation and
closing your account
To cancel your payroll deductions to the Associate Stock
Purchase Plan, complete an online benefit enrollment session
on One.Walmart.com/ASPP or Workday for Jet associates.
After you cancel your payroll deductions, you can close
your account by selling or transferring the remaining
stock in your account. To avoid paying a sales transaction
fee twice, cancel your payroll deductions before closing
your account. You also have the option to stop payroll
deductions and to continue to hold your shares through the
Plan at Computershare.
If you leave the company
If you leave the company, you will have several options
concerning the status of your account:
• You can keep your account open without the weekly or
biweekly payroll deduction and the company match. You
can make voluntary cash purchases and benefit from
having no broker’s fee. There is an annual maintenance fee
of $35 per year, which will be automatically deducted from
your account through the sale of an appropriate number
of shares or portion of a share of stock to cover the fee
during the first quarter of the year.
• You can close your account and transfer your shares to
another brokerage.
• You can close your account and sell some or all of the
shares in your account.
In order to prevent any residual balances and to avoid paying
a sales transaction fee twice, wait until you receive your
final paycheck before closing your account.
It is very important that you update Computershare if you
have an address change after you have left the company.

The Associate Stock Purchase Plan (ASPP)
226
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Prospectus
This document below constitutes a prospectus covering securities that have been registered
under the Securities Act of 1933.
50,000,000 Shares
WALMART INC.
Common Stock
($.10 par value per share)
WALMART INC.
2016 Associate Stock Purchase Plan
(formerly, the Wal-Mart Stores, Inc. 2016 Associate Stock Purchase Plan,
the Wal-Mart Stores, Inc. 2004 Associate Stock Purchase Plan,
and the Walmart Stores, Inc. Associate Stock Purchase Plan of 1996)
This prospectus relates to the purchase of the number of shares of the common stock, $0.10 par value per share, of Walmart
Inc. (“Walmart,” the “Company” or “we”) shown above under the Walmart Inc. 2016 Associate Stock Purchase Plan (the
“Plan”) by eligible Walmart associates who elect to participate in the Plan.
These securities have not been approved or disapproved by the Securities and Exchange Commission or any state securities
commission nor has the Securities and Exchange Commission or any state securities commission passed upon the accuracy
or adequacy of this prospectus. Any representation to the contrary is a criminal offense.
No one is authorized to give any information or to make any representations other than those contained in this Prospectus
and, if given or made, you should not rely on them. This Prospectus is not an offer to sell or a solicitation of an offer to buy
any of the securities referred to in this Prospectus in any state or other jurisdiction where such an offer or solicitation would
be unlawful. Neither the delivery of this Prospectus nor acquisition of securities described in this Prospectus implies that no
change in the affairs of the company has occurred since the date of this Prospectus.
Investment in shares of the Common Stock offered hereby involves certain risks. See “Part I, Item 1A. Risk Factors” in
Walmart’s Annual Report on Form 10-K most recently filed with the Securities and Exchange Commission for a discussion of
certain risks that may affect our business, operations, financial condition, results of operations and cash flows. See “Stock
Ownership, fees and risks” below.
The date of this Prospectus is September 1, 2019
Introduction and overview
The Plan is an amendment and restatement of the Wal-
Mart Stores, Inc. 2004 Associate Stock Purchase Plan
which had previously amended and restated the Wal-Mart
Stores, Inc. Associate Stock Purchase Plan of 1996. The
Plan was most recently approved by the stockholders of
Walmart at our Annual Stockholders’ Meeting held on June
3, 2016. As of June 30, 2019, up to 59,423,969 shares of
the company’s common stock, par value $.10 per share (the
“Stock”), were available for purchase from the company
or on the open market under the Plan; 20,000,000 shares
of Stock were available for purchase from the company
PROSPECTUS
under the Plan; and 30,000,000 shares of Stock were
available for purchase on the open market under the
Plan. On November 30, 2018, 50,000,000 shares were
registered with the United States Securities and Exchange
Commission for offer and sale on Registration Statements
on Form S-8. Shares of the Stock are listed for trading on
the New York Stock Exchange. Participating associates may
be referred to as “you” in this Prospectus.
The Plan has two parts — the Stock Purchase Program and
the Outstanding Performance Award Program. The Stock
Purchase Program gives eligible associates an opportunity
to share in company ownership by allowing them to purchase

The Associate Stock Purchase Plan (ASPP)
227
which) associates of non-U.S. Participating Employers
should be eligible to participate in the Plan; (vi) make all
determinations deemed necessary or advisable for the
administration of the Plan; (vii) make, amend, waive and
rescind rules and regulations for the administration of the
Plan; and (viii) exercise any powers, perform any acts and
make any determinations it deems necessary or advisable to
administer the Plan. All decisions made by the Committee
under the Plan are final and binding on all persons, including
the company and its affiliates, any associate, any person
claiming any rights under the Plan from or through any
participant, and shareholders of the company. The members
of the Committee do not act as the trustees of the
participants or hold the Stock credited to the participants’
Plan accounts, any funds contributed to the Plan by any
associate or the proceeds of any sale of shares of stock in
trust for the benefit of the participants.
Plan paricipation and eligibility
If you are eligible to participate in the Plan, you can
become a participant in the Plan by enrolling online at
One.Walmart.com to authorize payroll deductions to be
taken from your regular compensation and contributed to
the Plan for the purchase of Stock to be held in your Plan
account. You can also become a participant in the Plan if
the Committee grants you an award of Stock under the
Outstanding Performance Award Program.
All associates of the company and approved affiliates of
the company (“Participating Employers”) are eligible to
participate in the Plan, except:
• If you are restricted or prohibited from participating in the
Plan under the law of your state or country of residence,
you may not participate in the Plan or your participation in
the Plan may be limited. It is your responsibility to ensure
there are no such restrictions or prohibitions on your
participation in the Plan.
• You must have attained the age of majority in your state
of residence or employment to participate. It is your
responsibility to ensure you are of sufficient age to
participate. The company may terminate your participation
if it discovers you are not of legally sufficient age to
participate in the Plan.
• If you are a member of a collective bargaining unit
whose benefits were the subject of good faith collective
bargaining, you are excluded from participation in the Plan.
• If your employer is a non-U.S. Participating Employer,
you may participate only if you are an approved associate
(listed by group, category or by individual).
• If you are an officer of Walmart subject to subsection
16(a) of the Securities Exchange Act of 1934, or otherwise
subject to our Insider Trading Policy, your ability to acquire
or sell shares of Stock may be restricted.
shares of Stock by payroll deduction. In addition, if they make
or have made purchases through such payroll deductions
under the Plan, they may also purchase shares of Stock by
making voluntary contributions to the Plan out of their other
funds. Under the Outstanding Performance Award Program,
the company may reward associates for exceptional job
performance by awarding shares of Stock to them.
We believe that the Plan is not subject to any provisions of
the Employee Retirement Income Security Act of 1974, as
amended. The Plan is not qualified under Section 401(a) or
423 of the Internal Revenue Code of 1986, as amended.
Plan administration;
accountmanagement
The Plan provides that the Compensation and Management
Development Committee of our Board of Directors (the
“Committee”) has the overall authority for administering
the Plan. The Committee may delegate (and revoke the
delegation of) some or all aspects of Plan administration to
the officers or managers of the company or of a wholly-
owned or majority-owned subsidiary of the company (which
subsidiaries are referred to in this Prospectus as “affiliates”),
subject to terms as it deems appropriate. The members
of the Committee are selected by Walmart’s Board of
Directors. The Board of Directors may remove a member
from the Committee at its discretion, and a member will
cease to be a Committee member if he or she ceases to be
a director of Walmart for any reason. At the date of this
Prospectus, the members of the Committee were Mr. Steve
Reinemund, Mr. Steve Easterbrook, Ms. Carla Harris, and
Ms. Marissa Mayer.
The Committee has selected a third-party administrator,
currently Computershare Trust Company, N.A.
(“Computershare”), to establish and maintain accounts
under the Plan. Computershare also serves as the
company’s stock transfer agent and provides other stock-
related services to the company and its shareholders.
The Committee, as administrator of the Plan, or its delegate,
must follow the terms of the Plan, but otherwise has full
power and discretion to administer the Plan, including, but
not limited to, the power to: (i) determine when, to whom
and in what types and amounts contributions should be
made; (ii) authorize the company to make contributions to
eligible associates in any number and to determine the terms
and conditions applicable to each such contribution; (iii) set
a minimum and maximum dollar, share or other limitation
on the various contributions permitted under the Plan;
(iv) determine whether an entity of which we own more
than 50% or otherwise control, directly or indirectly (an
“affiliate”) should become (or cease to be) a Participating
Employer (as defined below); (v) determine whether (and
PROSPECTUS

The Associate Stock Purchase Plan (ASPP)
228
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you are on a bona fide leave of absence from the company
or a Participating Employer, you will continue to be eligible
to make contributions to the Plan during your leave of
absence, but you will not be eligible for company matching
contributions during that time. If you are on a military
leave of absence from the company or a Participating
Employer, please contact the Benefits Department to
seewhether you are eligible to receive company matching
contributions during your leave. Please note that you must
make contributions from your own funds if you are not
receiving a paycheck while you are on a leave of absence, as
payroll deduction would not be available as an option. Any
other circumstances which would permit you to continue to
participate in the Plan while on a leave must be approved by
the Committee.
Plan contributions — Stock
PurchaseProgram
To make payroll deduction contributions, you need
to complete an online benefits enrollment session at
One.Walmart.com. Once you have properly enrolled in
thePlan, your payroll deduction contributions will continue
in accordance with your most recent payroll deduction
authorization (subject to any restrictions imposed by the
Plan) as long as you are employed by the company or a
Participating Employer, unless you change or terminate
your payroll deduction authorization or the Plan itself
isterminated.
Please note that no deduction will be drawn from any
paycheck in which your payroll deduction contribution
exceeds your net pay after taxes are withheld. You can
change or terminate your payroll deduction authorization
by completing an online benefits enrollment session at
One.Walmart.com. Your request will be processed as soon
as practicable. Your enrollment or request may be delayed
or rejected if your enrollment or requested change is
prohibited at the time of the attempted enrollment or the
request by any company policy, including the company’s
Insider Trading Policy.
Note that payroll deduction contributions are generally
taken from your last paycheck as an associate. If you do not
want to have payroll deduction contributions taken from
your last paycheck, it is important that you timely terminate
your payroll deduction authorization. If you work in a state
that requires your last paycheck to be paid outside of the
normal payroll cycle, payroll deduction contributions will
not be taken out of your last paycheck.
Payroll deductions can be as little as $2 or as much as
$1,000 per biweekly payroll period. Payroll deductions
for associates paid on a weekly basis can be as little as
$1 or as much as $500 per weekly payroll period. The
amount of any biweekly or weekly deduction in excess of
the minimum must be in $1 increments. The Company or
your Participating Employer will make a matching cash
contribution on your behalf to your Plan account when you
make contributions to the Plan by payroll deduction. The
matching contribution is currently 15 percent of the first
$1,800 you contribute to the Plan by payroll deduction,
or up to $270 per Plan year. The company’s matching
contribution will be used to buy Stock for your Plan account.
If you participate or have participated in payroll deductions
under the Plan and your Plan account has not been closed
as described below, you can also voluntarily contribute
cash (in U.S. dollars) from your other resources to fund
the purchase of Stock under the Plan to be held in your
Plan account, including after your employment with
the Company or any Participating Employer has been
terminated. Any voluntary contributions must be made
directly to Computershare. Instructions for making such
voluntary contributions are available from Computershare.
Neither the Company nor your Participating Employer will
make matching contributions on amounts you contribute
directly to Computershare. In addition, you may also deposit
shares of Stock that you hold outside of the Plan (whether
you originally acquired those shares through the Plan or
otherwise) to your Plan account by making arrangements
directly with Computershare.
The total of your payroll deductions and voluntary cash
contributions to the Plan cannot exceed $125,000 per Plan
year (April 1 through March 31). Dividends credited to your
Plan account will not count against the maximum.
The Committee establishes and may change the maximum
and minimum contributions, may change the conditions for
voluntary cash or Stock contributions, and may change the
amount of the matching contributions of an employer at
any time.
OUTSTANDING PERFORMANCE
AWARDPROGRAM
Under the Outstanding Performance Award component,
you can be granted an award of Stock for demonstrating
consistently outstanding performance in your job over
the period of a month, a quarter or a year. The Committee
approves all Outstanding Performance Awards and sets
maximum dollar limitations on these awards from time
totime.
Your Stock under the Outstanding Performance Award
component will be given to you through an account
maintained for your benefit by Computershare.
PROSPECTUS

The Associate Stock Purchase Plan (ASPP)
229
STOCK PURCHASES
Your employer will send all of your payroll deductions along
with any matching contributions to Computershare as soon
as practicable following each pay period. Computershare
will purchase Stock for your Plan account no later than
five business days after it receives the funds. If you make a
voluntary cash contribution outside of payroll deductions,
Computershare will purchase your Stock with that voluntary
cash contribution no later than five business days after it
receives the funds.
Computershare may purchase Stock for the Plan accounts
on a national stock exchange, from the company, or from
a combination of these places. However, the Committee
reserves the right to direct Computershare to purchase from
a particular source, consistent with applicable securities rules
and the applicable rules of any national stock exchange.
Typically, when Computershare purchases Stock for the
Plan on a national stock exchange, the shares are purchased
as part of a bundled group rather than individually for
each participant. In some instances, the shares of Stock
for a bundled group must be purchased for the Plan over
more than one day. When shares of Stock are purchased
for you as part of a bundled group, your purchase price for
each share of Stock will be equal to the average price of all
shares of Stock purchased for that group as determined by
Computershare. A participant is not permitted to direct an
order for Computershare to purchase shares of Stock solely
for himself or herself that are part of the bundled group.
If Computershare buys shares of Stock from the company,
whether authorized but unissued shares or treasury shares,
the per-share price paid to the company for those shares
of Stock will be equal to the Volume Weighted Average
Price (VWAP) as reported on the New York Stock Exchange
– Composite Transactions on the date of purchase. The
VWAP is the weighted average of the prices at which all
trades of the company’s Stock are made on the NYSE on
the date of the Stock is purchased from the company.
While the Plan permits the Committee to designate
another methodology for valuing Stock purchased from
the company, as of the date of this Prospectus no other
methodology has been designated.
The number of shares allocated to your Plan account in
connection with any purchase of Stock will equal the total
amount of the contributions and dividends available for your
Plan account and used to fund such purchases, divided by
the purchase price for each share of Stock attributable to
those purchases as discussed above.
Non-U.S. Participants Please Note: All amounts contributed
to the Plan by payroll deduction, all matching contributions,
and any contributions made pursuant to the Outstanding
Performance Award component will be converted from
your local currency to U.S. dollars prior to the time the
shares of Stock are purchased. Generally, the exchange
rate used is the one for the business day immediately prior
to the day the funds are sent to Computershare, but that
may not be practicable in all circumstances. All voluntary
cash contributions must be converted to U.S. dollars before
being sent to Computershare to purchase shares of Stock.
Stock ownership, fees, and risks
STOCK OWNERSHIP
From the time that shares of Stock are credited to your
Plan account, you will have full ownership of those shares
(including any fractional shares) of Stock. The shares
of Stock held in your Plan account will be registered in
Computershare’s name until you request to have your
Stock certificates delivered to you from the Plan account
or you sell the shares credited to your Plan account. You
may not assign or transfer any interest in the Plan before
shares are credited to your account. However, you may
sell, transfer, assign or otherwise deal with your shares of
Stock credited to your Plan account once they are credited
to your Plan account, just like any other stockholder of the
company. You may not transfer or assign your Plan account
to another person who is not an eligible participant in the
Plan. There is no automatic lien or security interest on the
shares of Stock held in your Plan account, and the terms
of the Plan do not provide for anyone to have or to have
the ability to create a lien on any funds or shares of Stock
credited to your Plan account. However, you may pledge,
hypothecate or deal with the shares of Stock credited to
your Plan accounts in the same manner as you may do with
other shares of Stock you may own, subject to compliance
with our Insider Trading Policy.
For example, you may pledge the shares of Stock credited to
your Plan account as collateral in connection with a loan. If
you pledge shares of Stock credited to your Plan account to
secure a loan under the Stock Secured Line of Credit Program
maintained by USBancorp (prior to September 30, 2018) or
any other loan made available to you, the lender will have
a security interest in the shares of Stock held in your Plan
account. Neither Walmart nor any Participating Employer is
a sponsor of or will be responsible for any amounts owed by a
participant under the Stock Secured Line of Credit Program
or any loan. If you fail to repay the amounts you owe to the
lender for your loan, including the accrued interest and any
fees thereon, the lender may foreclose its lien on, and sell, the
number of shares pledged to secure the loan that will yield net
sales proceeds in an amount necessary to pay the amounts
you owe the lender. If the net proceeds from such a sale of
shares are less than the amount you owe the lender, you, and
not Walmart or a Participating Employer, will be responsible
for paying the deficiency from your other resources.
PROSPECTUS

The Associate Stock Purchase Plan (ASPP)
230
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
DIVIDENDS AND VOTING
Dividends on shares in your account will be automatically
reinvested in additional shares of Stock. You will be able to
direct the vote on each full share of Stock held in your Plan
account, but not fractional shares. You will receive at no
cost and as promptly as practicable (by mail or otherwise)
all notices of meetings, proxy statements, notices of
internet availability of proxy materials and other materials
distributed by the company to its stockholders. To vote the
shares of Stock held in your Plan account, you must deliver
signed voting instructions, also known as proxy instructions,
in a timely manner described in the company’s proxy
materials. If you do not provide properly completed and
executed voting instructions as described in the company’s
proxy materials, your shares will not be voted with respect
to any election of directors, any advisory vote on executive
compensation, or many other matters that may be subject
to a shareholder vote. However, in those circumstances,
your shares of Stock may be voted in the manner
recommended by the company in its proxy statement or as
directed by the Committee on matters defined by the New
York Stock Exchange as “routine,” such as the ratification of
the appointment of the company’s independent auditors,
provided that doing so would comply with applicable law and
any applicable listing standard of a national stock exchange.
FEES AND ACCOUNT STATEMENTS
The company pays all fees associated with the purchase of
Stock. Generally, no maintenance fees or other charges
will be assessed to your Plan account as long as you are
employed by the company or one of its affiliates (even if
that affiliate is not a Participating Employer). However,
you must pay any commissions or charges resulting from
other Computershare services you request, for example,
brokerage commissions and other fees applicable to the sale
of Stock. Computershare can tell you if a particular request
would cause you to incur a charge. The fees charged by
Computershare described in this Prospectus are subject to
change from time to time.
At least annually, you will receive a statement of your
account under the Plan, reflecting all activity with respect
to your Plan account for the period of time covered by the
statement. You may elect to receive your statements online.
If you elect to do so, you will receive an email informing
you that your statement is ready and can be found on
computershare.com/walmart. Your annual statement will
also contain important tax information. It is very important
that you keep your statement so that you will know the
difference between your purchase price and sales price of
any shares of Stock you sell. You will need this information
for your income taxes.
You may also access information regarding your account
at any time by logging on to computershare.com/walmart.
You can access your account information by phone at
800-438-6278 (hearing impaired 800-952-9245).
If you request replacement statements from
Computershare, there is currently a $5 charge per statement
for statements for years preceding the most recently
completed plan year. Or, you can obtain copies free of
charge through the website at computershare.com/walmart.
RISKS
Many of your risks of Plan participation are the same as
those of any other stockholder of the company, in that you
assume the risk that the value of the Stock may increase
or decrease. There are no guarantees as to the value of
a share of Stock. This means that you assume the risk of
fluctuations in the value or market price of the Stock.
Our latest Annual Report on Form 10-K filed with the SEC
and, as noted below, incorporated by reference in this
Prospectus, discusses, and other of our reports filed with
the SEC may discuss, certain risks relating to the company,
its operations and financial performance that can affect the
value, market price and liquidity of the Stock. The company
urges you to review those discussions in connection with
any determination to participate in the Plan, to change
the terms of your participation in the Plan, to terminate
your participation in the Plan or to make any voluntary
contributions under the Plan.
If you are a non-U.S. participant, you also assume the
risk of fluctuation in currency exchange rates. Also, your
payroll deductions (as well as the corresponding matching
contributions) are applied by Computershare to purchase
shares of Stock, such funds are considered general assets
of the company or the Participating Employer and, as such,
are subject to the claims of the company’s or Participating
Employer’s creditors. No interest will be paid on any
contributions to the Plan.
Stock cerificate delivery and
Stocksales
Computershare will send you, on request, a stock certificate
representing any or all full shares of Stock credited to
your Plan account at no cost to you. Your shares that are
represented by a stock certificate will no longer be credited
or otherwise related to any Plan account that you continue
to have in effect and the dividends those shares will not be
reinvested under the Plan.
You may also have Computershare transfer any or all of
the shares of Stock credited to your Plan account into your
name in the Direct Registration System. Such a transfer
PROSPECTUS

The Associate Stock Purchase Plan (ASPP)
231
means that you would hold your shares as “book-entry”
securities and your ownership would be shown on our stock
transfer records and represented by a statement which
shows your holdings of shares of Stock.
You may request that Computershare sell all or a portion
of the shares of Stock (including any fractional interests)
credited to your Plan account at any time, whether or not
you want to close your Plan account.
You will be charged a brokerage commission, as well as
any other applicable fees, if for any reason you have
Computershare sell shares of Stock held in your Plan account.
Any brokerage commission or fees will be at the rates
posted by Computershare from time to time. These rates
are available upon request from Computershare. A current
schedule of Computershare’s fees applicable to the Plan
can be found at computershare.com/walmart. The company
negotiated the amount of such fees with Computershare.
If you choose to sell your Stock, your Stock will be sold
pursuant to a market order. Although the Plan permits sales
of shares of Stock held in Plan accounts to be made through
batch orders and such sales have been made through batch
orders in the past, sales of shares of Stock under the Plan
are now made solely pursuant to market orders. As a result,
if you direct Computershare to sell any shares of Stock
credited to your Plan account, Computershare will sell
those shares in the open market at the then current best
available price. However, the price at which your order will
be executed is not guaranteed, and the last-traded price for
the Stock prior to the execution of your order to sell your
shares of Stock is not necessarily the price at which your
order will be executed. From time to time, we repurchase
shares of Stock in the open market under a stock repurchase
program adopted by our Board of Directors. As a result, if
Computershare sells shares credited to your Plan account in
the open market, we could be the purchaser of such shares.
However, we will typically not know if any of the shares
of Stock we purchase in the open market are purchased
from you. Your shares of Stock will be sold as soon as your
request can reasonably be processed. Generally, market
orders are executed immediately after they are placed.
We expect that any sales of your shares of Stock will be
executed over the New York Stock Exchange (the “NYSE”),
but orders for those sales need not be executed over the
NYSE. If the NYSE is closed when your order is ready to
be processed, your sale transaction will be processed as
early as practicable on the next NYSE trading day. Orders
for the sale of shares of Stock under the Plan may be
executed by or through an affiliate of Computershare
that is registered with the SEC as a broker-dealer under
the Securities Exchange Act of 1934. Sales of the Stock
will be made in U.S. dollars. If you are employed outside
the U.S. by a Participating Employer and if provided by
Computershare for your country, the proceeds from the
sale may be converted for a fee to another currency if you
request it when you request your Stock to be sold. If the
proceeds are converted to another currency, the exchange
rate that will be used is the exchange rate published in The
Wall Street Journal (or other similar source) on the date your
sale transaction is executed. You will assume the risk of any
fluctuations in currency exchange rates.
Termination of paricipation;
accountclosure
Once you become a participant in the Plan, you will remain
a participant until you elect to close your Plan account
and all Stock and sale proceeds credited to it have been
distributed out of your Plan account, or until all Stock
and sale proceeds have been distributed from your Plan
account after your employment with the company or one
of its affiliates has terminated.
If you terminate your payroll deduction authorization, or
your employment with the company and all its affiliates has
terminated, you may choose to continue your Plan account;
or you may close your Plan account if you specify this to
Computershare. Specifically:
• You may keep your Plan account open (without the
weekly or biweekly payroll deduction and your employer’s
matching contributions). If you keep your account open,
you may continue to make voluntary cash contributions
and no brokerage commissions will be charged on the
purchase of Stock. If you cease to be employed by the
company or one of its affiliates, an annual maintenance
fee will be charged to your account. Computershare has
the option to collect such maintenance fee either in the
form of quarterly installments, or in an annual lump sum
payment, which is due in the first quarter of each calendar
year and will be paid by means of the sale of an appropriate
number of shares or portion of a share of Stock by
Computershare. (If you are transferred to a company
affiliate that is not a Participating Employer, the company
may continue to pay the maintenance fee for you.)
• If you own at least one full share of Stock, you may close
your Plan account by moving your Stock into a “General
Shareholder” account maintained on your behalf by
Computershare. You may accomplish this move either by
receiving all full shares in certificate form with a check
for any fractional share ownership or by re-depositing
the shares in the General Shareholder account, or
Computershare can move the shares electronically at your
request. You should contact Computershare for more
information about the fees associated with a General
Shareholder account.
PROSPECTUS

The Associate Stock Purchase Plan (ASPP)
232
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• You may close your Plan account by having all shares
of Stock in your account sold and the proceeds paid to
you, or you can have certificates for full shares (and cash
proceeds of any fractional shares paid to you) delivered to
you instead. The proceeds of any sale of full or fractional
shares will be net of brokerage commissions, sales fees
and other applicable charges. Your account will be closed
automatically if you terminate employment and there are
no shares or fractional shares in your account.
If you die before your Plan account has been closed, your
Plan account will be distributed per the legal documentation
submitted to Computershare or to your estate, unless
you had previously arranged with Computershare to
have your stock held in a joint account. In the event you
have a joint account, the joint account holder may either
make arrangements with Computershare to move your
shares into a General Shareholder account maintained by
Computershare at his or her own expense or to have the
Stock (or proceeds from the sale thereof ) distributed, less
any applicable fees or commissions.
If you established a joint tenant account prior to April1,2018,
you may contact Computershare at 800-438-6278 to
remove a joint tenant from your account.
Plan amendment and termination
The Plan has no set expiration date. The Board of
Directors of the company, the Committee or any other
duly appointed committee of the Board of Directors may
amend or terminate the Plan at any time. However, if
stockholder approval of an amendment is required under
law or the applicable rules of a national stock exchange, the
amendment will be subject to that approval. No amendment
or termination of the Plan will cause you to forfeit: (1) any
funds you have contributed to the Plan or matching funds
the company has contributed that have not yet been used
to purchase shares of Stock; (2) any shares (or fractional
shares) of the Stock credited to your Plan account; or (3)any
dividends or distributions declared with respect to the Stock
after you have made a contribution to the Plan but before
the effective date of the amendment or termination.
Tax information
The following summary of the U. S. income tax
consequences of the Plan is based on the Internal Revenue
Code and any regulations thereunder as in effect as of the
date of this Prospectus. The summary does not cover any
state or local income taxes or taxes in jurisdictions other
than the United States. You should consult your tax advisor
regarding individual tax consequences before purchasing
Stock under the Plan.
STOCK PURCHASES UNDER THE STOCK
PURCHASE PLAN
You have no federal income tax consequences when you
enroll in the Plan or when shares of Stock are purchased
for you under the Stock Purchase Plan either by payroll
deduction or voluntary contribution. The amount of your
payroll deductions and any voluntary contributions under
the Plan are not deductible for purposes of determining your
federal taxable income. The amount of your wages that you
have deducted under the Plan and the full value of company
matching contributions are ordinary income to you in the
calendar year of deduction or the contribution, as the case
may be, and will be reported on your pay stub and your W-2.
The company deducts all applicable wage withholding and
other required taxes from your other compensation (by
increasing your payroll withholding and other tax deductions
for such purposes) with respect to the amount of your wages
deducted under the Plan and the matching contributions to
your Plan account, if any. Thecompany is entitled to a tax
deduction for the amount of the matching contribution in
the same year as you realize the income.
OUTSTANDING PERFORMANCE AWARDS
UNDER THE OUTSTANDING PERFORMANCE
AWARD PROGRAM
Stock grants under the Outstanding Performance Award
Program are taxable as ordinary income in the calendar year
of the award, regardless of whether the Stock certificates
are given directly to you or the Stock is awarded to your
Plan account. Your ordinary income will be the market value
of a share of Stock on the date the award is granted, times
the number of shares of Stock granted. The market value of
any Stock awarded will be reported to you on your W-2. The
company will deduct applicable wage withholding and other
required taxes from your other compensation (by increasing
your payroll deduction for such purposes). The company is
entitled to a tax deduction in the same amount and in the
same year as you realize the ordinary income.
STOCK SALES OR CERTIFICATE
DISTRIBUTIONS
You will not recognize any taxable income when you request
to have certificates delivered to you for some or all of the
shares of Stock held in your Plan account. However, when
you sell or otherwise dispose of your shares of Stock —
whether through Computershare or later after you have
received your Stock certificates — the difference between
the fair market value of the Stock at the time of sale and
the fair market value of the Stock on the date you acquired
it will be taxed as a capital gain or loss. The holding period
to determine whether the capital gain or loss is long-term
PROSPECTUS

The Associate Stock Purchase Plan (ASPP)
233
or short-term will begin on the date you acquire the Stock
(i.e., the date the Stock is credited to your Plan account).
The company will have no deduction as a result of your
disposition of shares of Stock and will not be liable for the
payment of any income or other taxes payable by you on
any gain you may realize on the sale of the shares of Stock
or imposed on or in connection with the sale transaction.
Available information
To obtain additional information about the Plan or
its administrators, please call People Services at
800-421-1362. You can also write to:
Walmart People Services
Walmart Inc.
508 SW 8th Street
Bentonville, Arkansas 72716-0295
Computershare may be contacted by calling
800-438-6278 (800GET-MART), online at
computershare.com/walmart, or by writing to the
following address for all correspondence, including
transactions, Stock certificate requests, Stock powers,
voluntary purchases and any customer service inquiries:
Computershare
Attn: Walmart ASPP
P.O. Box 505042
Louisville, Kentucky 40233
Electronic delivery of prospectuses
and other documents
To help reduce costs of operating the Plan and to help
with our sustainability efforts, we ask you to allow us
to deliver prospectuses and other documents related
to the Plan electronically and that you access the
prospectuses and documents we provide to participants
in the Plan over One.Walmart.com. Your enrollment in
the Plan will constitute your consent to receive or access
communications from us about the Plan and prospectuses
relating to the purchase of shares of Stock under the Plan
electronically through access on One.Walmart.com, unless
you affirmatively elect to receive paper copies of such
communications. At any time after enrollment you may
revoke that consent by sending a written revocation of the
consent to receive Plan documents electronically to the
Benefits Department at the address appearing below. In
addition, you may request a paper copy of the then current
prospectus relating to purchases of shares of Stock under
the Plan and of our most recent Annual Report on Form
10-K by writing the Benefits Department and those
documents will be provided to you free of charge.
Documents incorporated
byreference
The following documents filed by the company with the
Securities and Exchange Commission (the “Commission”)
(File No. 1-6991) are hereby incorporated by reference in
and made a part of this Prospectus:
• The company’s Annual Report on Form 10-K for the fiscal
year ended January 31, 2018;
• The company’s Quarterly Reports on Form 10-Q for the
fiscal quarters ended April 30, 2018 and July 31, 2018
• The company’s Current Reports on Form 8-K filed with
the Commission on June 5, 2018 and June 26, 2018;
• The company’s definitive Proxy Statement for the 2018
Annual Shareholders’ Meeting, filed with the Commission
on April 20, 2018; and
• Exhibit 99.1 to the Company’s Registration Statement on
Form S-8 (File No. 333-214060)
All documents filed by the company pursuant to Sections
13(a), 13(c), 14 and 15(d) of the Securities Exchange Act
of 1934 (the “Exchange Act”) on or after the date of this
Prospectus shall be deemed to be incorporated by reference
in this Prospectus and to be a part hereof from the date of
filing of such documents, except for information furnished to
the Commission that is not deemed to be “filed” for purposes
of the Exchange Act (such documents, and the documents
listed above, being hereinafter referred to as “Incorporated
Documents”). Any statement contained in an Incorporated
Document shall be deemed to be modified or superseded
for purposes of this Prospectus to the extent that a
statement contained herein or in any other subsequently
filed Incorporated Document modifies or supersedes such
statement. Any such statement so modified or superseded
shall not be deemed, except as so modified or superseded,
to constitute a part of the Section 10(a) prospectus of the
company relating to purchases under the Plan of the shares
of Stock described on the cover page of this Prospectus. This
document and the documents incorporated by reference
herein constitute such Section 10(a) prospectus.
These documents and the company’s latest Annual Report
to Stockholders and any other documents required to be
delivered to you under Rule 428(b) under the Securities Act
of 1933, as amended, are available to you without charge
upon written or oral request. Please direct your requests
for documents to:
Walmart Inc.
Benefits Department
508 SW 8th Street
Bentonville, Arkansas 72716-0295
Or you may call People Services at 800-421-1362.
PROSPECTUS

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Walmar 401(k) Plan eligibility 236
Enrolling in the Plan 236
Your Walmar 401(k) Plan accounts 237
Making a rollover from a previous employer’s plan or IRA 237
Making contributions to your account 238
Walmar’s contributions to your Company Match Account 240
Investing your account 241
More about owning Walmar stock 242
Account balances and statements 243
Receiving a payout while working forWalmar 243
If you die: your designated beneficiary 244
If you get divorced 245
If you leave Walmar 246
If you leave and are rehired byWalmar 247
The income tax consequences ofapayout 248
Filing a Walmar 401(k) Plan claim 249
Administrative information 250
Special tax notice addendum 252
Special tax notice addendum: Rothcontributions 256
The legal name of the Plan is the Walmar 401(k) Plan. This document is being provided solely by your
employer. No affiliate of Bank of America Corporation has reviewed or paricipated in the creation of the
information contained herein.
The Walmar
401(k)Plan

The Walmar 401(k)Plan
235
The Walmar 401(k) Plan
RESOURCES
Find What You Need Online Other Resources
Enroll in or change your pretax contribution and/oryour
catch-up contribution
Go to One.Walmar.com or
Workdayfor Jet associates or the
Plan’s website at benefits.ml.com
Call the Customer Service
Center at 888-968-4015
• NEW for February 1, 2020: you can make Roth contributions
• Enroll in or change your pretax, Roth, and/or your catch-
up contributions
• Request a rollover packet to make a rollovercontribution
• Get a fee disclosure sheet
• Get information about your Plan accounts
• Get a copy of your quarerly statement
• Request a hardship withdrawal or a withdrawal after you
reach age 59½
• Change your investment fund choices
• Request a payout when you leave Walmar
• Get information about your Plan investmentoptions
• Request a withdrawal of your rollovercontributions
• Request a loan from your Plan account
Go to benefits.ml.com Call the Customer Service
Center at 888-968-4015
Designate a beneficiary Go to One.Walmar.com or
Workdayfor Jet associates
What you need to know about the Walmar 401(k) Plan
• You are eligible to make your own contributions to the Plan as soon as administratively feasible after your hire date.
You can contribute from 1% to 50% of your eligible pay each pay period.
• You can elect to make pretax salary deferral contributions and, beginning February 1, 2020, Roth salary deferral
contributions. Pretax salary deferral contributions (and earnings thereon) are not subject to current federal income
tax and, in most cases, state or local taxes, until distributed from the Plan. Roth salary deferral contributions are
made on an after-tax basis, but the contributions and, in most cases, the earnings thereon are not subject to federal
income tax when distributed to you (as long as the distribution meets certain requirements).
• If you are credited with at least 1,000 hours of service in your first year and contribute to your account, you
begin receiving matching contributions on the first day of the calendar month following your first anniversary
ofemployment.
• After you become eligible for matching contributions, Walmart matches each dollar you contribute, up to 6%
of your eligible annual pay. (Contributions you make before you become eligible for matching contributions are
notmatched.)
• You are always 100% vested in the money you contribute and the money Walmart contributes to your Company
Match Account.
• You choose how to invest all contributions to your Plan account.
• If you do not specify how your contributions will be invested, they are automatically invested in the Plan’s default
investment option, the myRetirement Funds.
• The Plan accepts rollover contributions from other eligible retirement plans. You can withdraw your rollover
contributions at any time.
• You may request a loan from your Plan account, subject to Plan rules.
This is a summary of benefits offered under the Plan as of October 1, 2019. Should any questions arise about the nature and
extent of your benefits, the formal language of the Plan document, not the informal wording of this summary, will govern.
The Walmar 401(k)Plan
236
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Walmar 401(k) Plan eligibility
ASSOCIATES WHO ARE ELIGIBLE TO
PARTICIPATE IN THE PLAN
All associates of Walmart Inc. or a participating subsidiary
are eligible to participate in the Plan, except:
• Leased employees; nonresident aliens with no income from
U.S. sources; independent contractors or consultants
• Anyone not treated as an employee of Walmart or its
participating subsidiaries
• Associates covered by a collective bargaining agreement,
to the extent that the agreement does not provide for
participation in this Plan
• Associates represented by a collective bargaining
representative after Walmart has negotiated in good faith
to impasse with the representative on the question of
benefits, and
• Certain other associates who may be jointly employed by
Walmart and an affiliate that is not a participating affiliate
in the Plan.
For purposes of this Summary Plan Description, all
participating subsidiaries are referred to as “Walmart.”
WHEN PARTICIPATION BEGINS
For purposes of your contributions. If you are an eligible
associate, you may begin contributing to the Plan as soon as
administratively feasible after your date of hire is entered
into the payroll system. See Enrolling in the Plan later in this
summary for details about the enrollment process.
For purposes of matching contributions. If you are an
eligible associate, you will begin receiving matching
contributions on the first day of the calendar month
following your first anniversary of employment with
Walmart if you are credited with at least 1,000 hours of
service during your first year and are contributing your
own contributions (both pretax contributions and Roth
contributions) to the Plan. (Matching contributions are not
made with respect to contributions you make before you
become eligible for matching contributions.) For example,
if your date of hire was December 15, 2018 and you are
credited with 1,095 hours by December 15, 2019 (your
first anniversary), then you will begin receiving matching
contributions on January 1, 2020, with respect to any
contributions you make to the Plan on or after that date.
If you are not credited with 1,000 hours of service during
your first year, your eligibility for the matching contributions
will be determined on hours worked during the Plan year,
which runs from February 1 to January 31. You will be eligible
to receive matching contributions on any contributions
you make to the Plan on or after the February 1 that
follows the Plan year in which you are credited with at least
1,000 hours of service. For example, if your date of hire is
December 15, 2018, and you are credited with only 595 hours
by December 15, 2019 (your first anniversary), but you work
1,095 hours during the February 1, 2019–January 31, 2020
Plan year, you will begin receiving matching contributions on
February 1, 2020 with respect to any contributions you make
to the Plan on or after that date.
HOW HOURS OF SERVICE ARE CREDITED
UNDER THE PLAN
If you are an hourly associate, the hours counted toward the
1,000-hour requirement are credited as follows:
• Hours, including overtime hours, you work for Walmart or
any subsidiary are counted.
• Hours for which you receive paid leave or personal time off
are also counted.
• When a payroll period overlaps two Plan years, hours
arecredited toward the Plan year in which they are
actuallyworked.
If you are a salaried associate or truck driver, the hours
counted toward the 1,000-hour requirement are credited
asfollows:
• You are credited with 190 hours per month for each month in
which you work at least one hour for Walmart or a subsidiary.
• In general, you must work at least six months of the Plan
year to have 1,000 hours credited for the year. (Vacation
paid to you in cash after you leave Walmart does not give
you additional service for this purpose.)
If you become an associate of Walmart or any subsidiary as
the result of the acquisition of your prior employer, special
service crediting rules may apply to you.
Under the Uniformed Services Employment and
Reemployment Rights Act of 1994 (USERRA), veterans
who return to Walmart or a subsidiary after a qualifying
deployment may be eligible to have their qualified military
service considered toward their hours of service under the
Plan. Call People Services at 800-421-1362 for more details.
Enrolling in the Plan
Shortly after you become eligible to contribute to the Plan,
(i.e., shortly after your date of hire), you will receive an
enrollment packet at your home address on file. This packet
tells you how you can make contributions from your pay into
your 401(k) Account or Roth Account and explains how you
can direct the investment of your Plan funds by choosing
from among a menu of investment options with varying
investment objectives and associated risks. Because the
Plan is intended to be an important source for your financial
security at retirement, you should read all information
pertaining to the Plan carefully, and consult with your family,
tax and financial advisors before making any decisions.
The Walmar 401(k)Plan
237
Once you satisfy the eligibility requirements for receiving
matching contributions, Walmart will match all of your
subsequent contributions dollar-for-dollar up to 6%
of eligible annual pay, as explained in the Walmart’s
contributions to your Company Match Account section.
To begin contributing to the Plan, enroll online at
One.Walmart.com, Workday for Jet associates, or
benefits.ml.com. You can also call the Customer Service
Center at 888-968-4015. Note, however, that if you wish
to make Roth contributions to the Plan, you must enroll
at benefits.ml.com. You can enroll at any time after you
become eligible.
When you enroll, you can choose:
• The percentage of your pay that you want to contribute
on a per-pay-period basis and, after February 1, 2020,
whether your contributions will be pretax contributions
or Roth contributions (see Making contributions to your
account later in this summary), and
• How to invest your accounts among the Plan’s investment
options. The Plan’s investment options and procedures are
described in your enrollment packet.
After you enroll, a confirmation notice will be mailed to your
home address, or, if you have chosen electronic delivery of
Plan materials, you will receive an email notification when
the confirmation is available. The confirmation will show the
percentage of your pay that you have chosen to contribute
from each check, whether you elected to make pretax
contributions or Roth contributions, and the investment
options you have elected. Review the confirmation to make
sure your enrollment information is correct.
Your contributions to the Plan will start as soon as
administratively feasible, normally within two pay periods
after you enroll. No contributions are taken from your
pay before you become an eligible participant in the Plan.
Only participants who contribute their own funds to the
Plan will have those contributions matched by Walmart,
subject to eligibility requirements outlined in the Walmart’s
contributions to your Company Match Account section.
It is your responsibility to review your paychecks to confirm
that your election is implemented correctly. If you believe
your election has not been implemented correctly, notify
the Customer Service Center at 888-968-4015 in a
timely manner so that corrective steps can be taken. Your
notification will not be considered timely if it is made more
than six months after the date you make your election.
Your Walmar 401(k) Plan accounts
The Walmart 401(k) Plan consists of several accounts. You
will have some or all of the following accounts:
• Pretax Account: This account holds your pretax
contributions to the Plan (including your catch-up
contributions, if any), as adjusted for earnings or losses on
those contributions.
• Roth Account: This account holds your Roth contributions
to the Plan on or after February 1, 2020 (including your
Roth catch-up contributions, if any), as adjusted for
earnings or losses on those contributions.
• Company Match Account: This account holds Walmart’s
matching contributions, as adjusted for earnings or losses
on those contributions.
• Pretax Rollover Account: This account holds any
contributions that you rolled over to this Plan from
another eligible retirement plan, as adjusted for earnings
or losses on those contributions.
• Roth Rollover Account: This account holds any amounts
you rolled over to this Plan from your designated Roth
salary deferral account in another eligible retirement plan.
• Company Funded 401(k) Account: This account holds the
discretionary Walmart contributions to the 401(k) portion
of the Plan made for Plan years ended on or before
January 31, 2011, as adjusted for earnings or losses on
those contributions.
• Company Funded Profit Sharing Account: This account
holds the discretionary Walmart contributions to the
profit-sharing portion of the Plan made for Plan years
ended on or before January 31, 2011, as adjusted for
earnings or losses on those contributions.
The chart on the following page provides a summary of some
of the differences between these accounts. These differences
are discussed in more detail throughout this summary.
Note that if you become an associate of Walmart or any
subsidiary as the result of the acquisition of your prior
employer, and you participated in your prior employer’s
401(k) plan, you may have other accounts in this Plan that
hold amounts you contributed to your prior employer’s plan.
Making a rollover from a previous
employer’s plan or IRA
When you come to work for Walmart, you may have funds
owed to you from a previous employer’s retirement plan
(including a 401(k) plan, a profit-sharing plan, a 403(b)
plan of a tax-exempt employer or a 457(b) plan of a
governmental employer). If so, you may be able to roll over
that money to this Plan. You may also roll over pretax funds
you have in an individual retirement account (IRA). You may
directly roll into the Plan amounts from a designated Roth
salary deferral account in another qualified retirement plan.
If you roll over funds to this Plan, keep these points in mind:
• Once you roll funds into the Walmart 401(k) Plan, those
funds are subject to the rules of this Plan, including payout
rules, and not the rules of your former employer’s plan or
your IRA
• Your rollover contribution will be placed in your Rollover
Account and will be 100% vested, and
• You may withdraw all or any portion of your rollover
contributions at any time.

The Walmar 401(k)Plan
238
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
If you’re interested in making a rollover contribution to the
Plan, contact the Customer Service Center at 888-968-4015
or visit benefits.ml.com to obtain a rollover packet.
Making contributions to your account
After you become a participant in the Plan, you may
generally choose to contribute from 1% up to 50% of
each paycheck to your Pretax Account and/or your Roth
Account. Your contributions (including both pretax
contributions and Roth contributions) in any calendar year,
however, may not exceed a limit set by the IRS. For 2020,
the limit is $19,500. This amount will be increased from time
to time by the IRS.
The IRS also limits the amount of annual compensation
that can be taken into account under the Plan for any
participant. For 2020, this limit is $285,000.
On and after February 1,2020, you can choose whether
your contributions will be “pretax contributions” and/or
“Rothcontributions.” Together, these contributions
are called your “401(k) contributions” in this summary.
(BeforeFebruary1,2020, all 401(k) contributions are
pretax contributions.)
• Pretax contributions are deducted from your pay before
federal income taxes are withheld. This means that
you don’t pay federal income taxes on amounts you
contribute to the Plan. Earnings on these contributions
accumulate tax-free and are not taxed until your Pretax
Account is actually distributed to you from the Plan. You
may also save on state and local taxes as well, depending
on your location. Please note that your contributions are
subject to Social Security taxes in the year the amount
is deducted from your pay. Distributions from the Plan,
however, are not subject to Social Security taxes.
• Roth contributions are deducted from your pay after
federal income taxes are withheld. This means that
you pay federal and state income taxes, and also Social
Security taxes, on amounts you contribute to the Plan
in the year the amount is deducted from your pay. Roth
contributions, and earnings on those contributions,
are normally not subject to federal and state income
tax when your Roth Account is distributed to you
from the Plan. In order for the earnings to be tax-free,
the distribution must be a “qualified” distribution, as
explained later. (Note that income limitations applicable
to Roth IRAs are not applicable to Roth contributions to
the Plan. You may choose to make Roth contributions
regardless of your income.)
In addition, if you make contributions to the Plan, you
may be eligible for a “Saver’s Credit.” If you are a married
taxpayer who files a joint tax return and you have a modified
adjusted gross income (MAGI) of $65,000 or less (for 2020)
or a single taxpayer with $32,500 or less (for 2020) in MAGI
on your tax return, you are eligible for this tax credit, which
can reduce your taxes. For more details, your tax preparer
may refer to IRS Announcement 2001-106.
PROFIT SHARING AND 401K ACCOUNT DIFFERENCES
Source of
contributions
May paricipants
choose
investments?
Vesting
percentage
Are hardship
withdrawals
available?
Are in-service
withdrawals available
after age59½?
Pretax Account/
Roth Account
(including catch-up
contributions)
You Yes 100% Yes Yes
Company Match
Account
Walmar Yes 100% Yes, beginning
Feb. 1, 2020
Yes
All Rollover Accounts You Yes 100% Yes Yes
Company Funded
401(k) Account
Walmar Yes 100% Yes, beginning
Feb. 1, 2020
Yes
Company Funded
Profit Sharing
Account
Walmar (except
for rollovers you
made to the Profit
Sharing Plan)
Yes 2 years — 20%
3 years — 40%
4 years — 60%
5 years — 80%
6 years — 100%
(Rollovers are
immediately
100%vested)
Yes, beginning
Feb. 1, 2020
Yes
(to the extent vested)
The Walmar 401(k)Plan
239
HOW YOUR 401k CONTRIBUTION
ISDETERMINED
The percentage of pay you elect to contribute to the Plan is
applied to the following types of pay:
• Regular salary or wages, including bonuses and any
pretax dollars you use for your pretax contributions or
to purchase benefits available under the Walmart Inc.
Associates’ Health and Welfare Plan
• Overtime, paid time off (used and paid out), bereavement,
jury duty, and premium pay
• Most incentive plan payments
• Holiday bonuses
• Special recognition awards, such as the Outstanding
Performance Award
• Differential wage payments you receive from Walmart
while you are on a qualified military leave. This means that
the contribution you have in effect when you go on the
leave will continue to be applied to your differential wage
payments while you are on the leave unless you change
your election, and
• Transition pay designated as relating to a WARN Act event.
The percentage of pay you elect to contribute to the Plan
will not be applied to the following types of pay:
• The 15% Walmart match on the Associate Stock
PurchasePlan
• Reimbursement for expenses like relocation
• Approved disability pay
• Equity income, including income from stock options or
restricted stock rights, or
• Upon your termination of employment, a final paycheck
paid prior to the end of a normal pay cycle (unless it is
administratively practicable to withhold your contribution
from that paycheck).
CHANGING YOUR 401k
CONTRIBUTIONAMOUNT
You can increase, decrease, stop, or begin your contributions
at any time by logging on to One.Walmart.com, Workday
for Jet associates, or benefits.ml.com. You may also call the
Customer Service Center at 888-968-4015. Your change will
be effective as soon as administratively feasible, normally
within two pay periods. If you change your contribution
amount, a confirmation notice will be sent to your home
address or, if you have chosen electronic delivery of Plan
documents, you will receive an email notification when the
confirmation is available. It is your responsibility to review
your paychecks to confirm that your election is implemented
correctly. If you believe your election has not been
implemented correctly, notify the Customer Service Center
at 888-968-4015 in a timely manner, so that corrective steps
can be taken. Your notification will not be considered timely
if it is more than six months after the date you make your
election. If you do not notify the Customer Service Center in
a timely manner, the amount that is being withheld from your
paycheck will be treated as your deferral election.
IF YOU ARE AGE 50 OR OLDER
CATCHUPCONTRIBUTIONS
If you are age 50 or older (or will be age 50 by the end of
the applicable calendar year) and you are contributing up to
the Plan or legal limits, you are allowed to make additional
contributions. These are called “catch-up contributions”
and are made by payroll deduction just like your other
contributions. You can choose whether your catch-up
contributions will be either pretax contributions or Roth
contributions. For 2020, your catch-up contributions may be
any amount up to the lesser of $6,500 or 75% of your eligible
annual pay. This amount may be adjusted from time to time
by the IRS. Your catch-up contributions will be credited to
your Pretax Account or your Roth Account, depending on
which type of contributions you elect to make. Remember,
Roth contributions can be made only at benefits.ml.com.
For example, if you elect to contribute the maximum
amount of $19,500 in the 2020 calendar year, or if you
elect to contribute the maximum percentage of your
eligible annual pay allowed under the Plan, you could elect
to contribute up to an additional $6,500 during the 2020
calendar year. If you are interested in making catch-up
contributions, you can enroll online at One.Walmart.com,
Workday for Jet associates, or benefits.ml.com, or by
calling the Customer Service Center at 888-968-4015.
CONTRIBUTING TO MORE THAN ONE PLAN
DURING THE YEAR
The total amount you can contribute (including pretax
contributions and Roth contributions) to this Plan and to
any other employer plan (including 403(b) annuity plans,
simplified employee pensions or other 401(k) plans) is
$19,000 for the 2019 calendar year, or $25,000 if you are
eligible for catch-up contributions. This amount may be
increased from time to time by the IRS. If you contribute to
more than one plan during the year, it is your responsibility
to determine if you have exceeded the legal limit.
If your total contributions go over the legal limit for a
calendar year, you should request that the excess amount be
refunded to you. The excess amount (except as noted below
with respect to Roth contributions) must be included in your
income for that year and will be taxed. In addition, if the
excess amount is not refunded to you by April 15 following
the year the amount was deferred, you will be taxed a second
time when the excess amount is distributed to you. To request
that excess contributions be returned to you from this Plan,
contact People Services at 800-421-1362 no later than April 1
following the calendar year in which the excess contributions

The Walmar 401(k)Plan
240
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
were made. The Administrator will establish procedures for
determining whether your pretax contributions or Roth
contributions will be returned to you, if you contributed both
types of contributions during the calendar year. To the extent
excess amounts are distributed from your Roth contributions,
the Roth contributions will not be taxable to you, but related
earnings that are distributed will be taxable to you. Any
matching contributions related to refunded contributions
willbe forfeited.
IF YOU HAVE QUALIFIED MILITARY SERVICE
If you miss work because of qualified military service, you
may be entitled under the Uniformed Services Employment
and Reemployment Rights Act of 1994 (USERRA) to make
up contributions you miss during your military service
(that is, to make contributions equal to the amount you
would have been eligible to make if you were working for
Walmart). For more information, contact People Services
at800-421-1362.
Walmar’s contributions to your
Company Match Account
Once you are eligible to receive matching contributions,
Walmart will make matching contributions to your
Company Match Account equal to 100% of your subsequent
contributions (including pretax, Roth, and catch-up
contributions), up to 6% of your eligible annual pay. Matching
contributions are not made with respect to contributions
you make before you become eligible for matching
contributions. After you become eligible for matching
contributions, the company matching contribution will be
made to your Company Match Account each pay period
until you reach the full amount of the company matching
contribution for which you are eligible for that Plan year.
Your eligible annual pay for this purpose is the same as
outlined above for determining your 401(k) contributions to
the Plan, but does not include amounts paid to you before
you become eligible to receive matching contributions.
As previously noted, if you miss work because of qualified
military service, you may be entitled under USERRA to
make up 401(k) contributions that you missed during your
military service. If you do make up any 401(k) contributions,
Walmart is required to make up matching contributions you
would have received with respect to those contributions.
Ifyou think this rule applies to you, contact People Services
at800-421-1362.
VESTING IN YOUR COMPANY MATCH ACCOUNT
You are always 100% vested in Walmart’s matching
contributions to your Company Match Account.
VESTING IN YOUR COMPANY FUNDED PROFIT
SHARING ACCOUNT
If you have a Company Funded Profit Sharing Account (see
Your Walmart 401(k) Plan accounts earlier in this summary),
the vested percentage of your Company Funded Profit
Sharing Account is the portion that you are entitled to
receive if you leave Walmart. Your account statements show
your vested percentage.
You become vested in your Company Funded Profit Sharing
Account (other than rollovers in that account, which are
always 100% vested) depending on your years of service
with Walmart as follows:
PROFIT SHARING VESTING SCHEDULE*
Years of service Vested percentage
Less than two 0%
2 20%
3 40%
4 60%
5 80%
6 or more 100%
* Applies to paricipants actively employed on or after
January 31, 2008.
NOTE: If you terminated employment before
February 1, 2007, your payout was based on the prior
vesting schedule and not the vesting schedule shown above.
A year of service for this purpose is a Plan year
(February1–January 31) in which you are credited with at
least 1,000 hours of service under the hours of service
rules (see How hours of service are credited under the Plan
earlier in this summary). If you are credited with less than
1,000 hours in a Plan year, your vesting does not increase
for that year. (Note that years of service for this purpose
are not determined by your anniversary date.)
If you leave Walmart because of retirement (at age 65
or older) or death, your Company Funded Profit Sharing
Account will be 100% vested, regardless of your years of
service. Your Company Funded Profit Sharing Account will
also be 100% vested if the Plan is ever terminated.
VESTING IN YOUR COMPANY FUNDED
401kACCOUNT
You are always 100% vested in Walmart’s contributions to
your Company Funded 401(k) Account.
The Walmar 401(k)Plan
241
Investing your account
YOUR INVESTMENT OPTIONS
You decide how your accounts will be invested. You
canchoose:
• The myRetirement Funds. The myRetirement Funds are a
series of customized investment options created solely for
Plan participants by the Benefits Investment Committee,
and are commonly known as “target retirement date”
funds. The myRetirement Funds are diversified investment
options that automatically change their asset allocation
over time to become more conservative as you get closer
to retirement. This is done by shifting the amount of
money invested in more aggressive investments, such as
stocks, and allocating those amounts to more conservative
investments, such as bonds, as you near retirement.
• From among a menu of investment options made available
under the Plan. Note that Walmart stock is an investment
option only for your Company Funded Profit Sharing
Account. Walmart stock is not available for investment
through any of your other Plan accounts (although to the
extent these other accounts hold Walmart stock, you may
always sell such shares, but no future purchases of Walmart
stock are allowed).
You may choose one of the investment options or you may
spread your money among the various investment options.
The investment gains or losses on your accounts depend on
the performance of the investments you choose.
If you do not make an investment choice for current
contributions to your account, they will be invested in one
of the myRetirement Funds based on your age. For more
information, refer to the Qualified Default Investment
Alternative (QDIA) notice and your enrollment packet.
These documents can both be obtained by going to
benefits.ml.com or by calling the Customer Service Center
at 888-968-4015.
Because the Company Funded Profit Sharing Account
is an Employee Stock Ownership Plan, all or a significant
portion of Walmart’s profit-sharing contribution was
invested in Walmart stock for Plan years ending prior to
January 31, 2006. If you were a participant in the Plan
prior to that date, you may have Walmart stock in your
Company Funded Profit Sharing Account. For Plan years
ending January31,2007 or later, Walmart’s profit-sharing
contribution was not invested in Walmart stock.
A description of all investment options, including the
myRetirement Funds, is included in the enrollment packet
you receive when you are eligible to enroll. You also may
obtain additional information for each investment option
by reviewing the Annual Participant Fee Disclosure
Notice. Youmay obtain a copy free of charge by accessing
your account online at benefits.ml.com or by calling the
Customer Service Center at 888-968-4015.
Please note that this Plan is intended to be an “ERISA
Section 404(c) plan.” This means that you assume all
investment risks connected with the investment options
youchoose in the Plan, or in which your funds are invested
if you fail to make investment selections, including the
increase or decrease in market value. Walmart Inc., the
Benefits Investment Committee, and the trustee are not
responsible for losses to your accounts which are the direct
and necessary result of investment decisions you make or,
if you fail to make an affirmative investment decision, as a
result of your accounts being invested in a default fund.
If you have a Company Funded Profit Sharing Account (see
Your Walmart 401(k) Plan accounts earlier in this summary)
and you choose to invest some or all of your Company
Funded Profit Sharing Account in Walmart stock or retain
Walmart stock in your other accounts, be aware that since
this option is a single stock investment, it generally carries
more risk than the options offered through the Plan.
HOW TO OBTAIN MORE INVESTMENT
INFORMATION
It is also important to periodically review your investment
portfolio, your investment objectives, and the investment
options under the Plan to help ensure that your
investments are in line with your objectives and your risk
tolerance. For more sources of information on individual
investing and diversification, visit the website of the
Department of Labor’s Employee Benefits Security
Administration at www.dol/agencies/ebsa and type
“investing and diversification” in the search field.
You may obtain more specific information regarding your
investment rights and investment options under the Plan at
benefits.ml.com or by calling the Customer Service Center
at 888-968-4015.
CHANGING YOUR INVESTMENT CHOICES
You can change your investment choices at any time online
at benefits.ml.com or by calling the Customer Service
Center at 888-968-4015. If you make an investment
change, a confirmation notice will be sent to your home
address or you will receive an email notification when the
confirmation is available if you have chosen electronic
delivery of your Plan materials. It is your responsibility to
make sure your change is made. If you do not receive a
confirmation notice or you do not see that your change
has been applied, contact the Customer Service Center
at888-968-4015.
If you call the Customer Service Center prior to 3:00 p.m.
Eastern time, your investment change generally will be
processed on the day you call. Depending on the investment
change, there may be up to a three-day settlement period
before your funds are invested in your new election.
The Walmar 401(k)Plan
242
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
DIVERSIFICATION
To help you diversify your retirement savings, the Plan
offers a variety of investment options with different levels
of risk and potential for increase in value. To “diversify”
means that you spread your assets among different types of
investments. To help achieve long-term retirement security,
you should give careful consideration to the benefits of a
well-balanced and diversified investment portfolio. This
strategy can help reduce risk and may provide consistent
returns because a decline in the value of one investment
may potentially be offset by an increase in the value of
another. If you invest more than 20% of your retirement
savings in any one stock, such as Walmart stock, or any
one industry, your savings may not be properly diversified.
Although diversification cannot ensure a profit or protect
against loss, it can be an effective strategy to help you
manage investment risk.
When deciding how to invest your retirement savings, you
should take into account all of your assets, including any
retirement savings outside of the Plan. For example, you
may own Walmart stock through other means. No single
approach is right for everyone because, among other
factors, individuals have different financial goals, different
time horizons for meeting their goals, and different
tolerances for risk. Keep in mind your rights to diversify
your Plan account and carefully consider how you choose
to invest your Plan account. For information about your
right to diversify your account and all of the investment
options available under the Plan, access your account online
at benefits.ml.com or call the Customer Service Center at
888-968-4015. It is also important to periodically review
your investment portfolio, your investment objectives, and
the investment options under the Plan to help ensure that
your investments remain appropriate for your retirement
goals and your tolerance for investment risk. For more
sources on individual investing and diversification, visit the
website of the Department of Labor’s Employee Benefits
Security Administration at www.dol/agencies/ebsa and type
“investing and diversification” in the search field.
More about owning Walmar stock
VOTING
If any of your account is invested in Walmart stock through
the Plan, each year you will receive all of the materials
generally distributed to the shareholders of Walmart,
including an instruction card telling the trustee how you
would like the shares in your Plan account to be voted.
The materials are mailed to your home address or sent
electronically, based on your online elections.
You can instruct the trustee, through the company’s
transfer agent, to vote Walmart stock held in your Plan
accounts. This usually occurs in May of each year. Your
instructions to the transfer agent and the trustee are kept
confidential at all times. You send your voting instructions
directly to the transfer agent, who compiles the votes
and notifies the Benefits Investment Committee of the
total votes cast. The Benefits Investment Committee then
notifies the Plan trustee of the total votes to be cast.
If you do not provide instruction to the trustee on how
you would like your shares voted, the Benefits Investment
Committee will vote those shares at its discretion. If neither
you nor the Benefits Investment Committee exercise voting
rights, the trustee or an independent fiduciary appointed by
the trustee may vote the unvoted shares.
CONFIDENTIALITY
Procedures have been designed to protect the confidentiality
of your rights with respect to shares of Walmart stock held
under the Plan, including the right to purchase, sell, hold,
or vote on proxy matters. For example, procedures with
the Company’s transfer agent for Walmart stock have been
implemented that prevent Walmart Inc. and the Benefits
Investment Committee from finding out how any individual
participant or beneficiary voted (except as necessary to
comply with securities laws) and from having access to your
individual proxy cards or proxy card shareholder comments.
In addition, access to information about your decisions to
buy, sell, or hold Walmart stock generally is limited to those
assisting in the administration of the Plan. The Benefits
Investment Committee is responsible for ensuring that these
procedures are sufficient to protect the confidentiality of
this information and that the procedures are being followed.
If the Benefits Investment Committee determines that a
situation has potential for undue influence by the Walmart
with respect to your rights as shareholder (through your
Plan Account), the Benefits Investment Committee will
appoint an independent party to perform activities that are
necessary to prevent undue influence.
DIVIDENDS ON YOUR WALMART STOCK
If you have Walmart stock in your accounts, your accounts
will be credited with any dividends paid by Walmart Inc.
with respect to its stock. Dividends allocated to your
Pretax Account, your Company Funded 401(k) Account,
or your 401(k) Rollover Account will be automatically
reinvested in Walmart stock. Dividends allocated to your
Company Funded Profit Sharing Account (and Profit
Sharing Rollover Account) will also be reinvested in
Walmart stock, except as noted below.
If you are an active participant (excludes beneficiaries
and alternate payees, as defined in the If you get divorced
section) with six or more years of service, you have an option
to take a cash payout of any dividends paid on Walmart stock
held in your Company Funded Profit Sharing Account or

The Walmar 401(k)Plan
243
Profit Sharing Rollover Account. Also, if you are a terminated
participant who had more than six years of service when you
terminated and you continue to maintain your accounts in
the Plan after you leave, you will have the option to elect a
cash payout of dividends paid on Walmart stock held in your
Company Funded Profit Sharing Account or Profit Sharing
Rollover Account. If you do not opt for the cash payout, your
dividends will be reinvested in Walmart stock.
You may make an election any time by calling the Customer
Service Center at 888-968-4015. Your most recently filed
election will apply to all subsequent dividends until you
change your election. (You may change your election only
once each business day.) Keep in mind that your election
must be made no later than the close of business on the
day prior to the record date for the dividend in order to be
effective for that dividend. You will not be able to make any
elections or election changes during the period from the
record date of the dividend through the dividend pay date
(which is usually three to four weeks after the record date).
Each year, Walmart Inc. releases the quarterly record dates
for dividend payouts. You can find this information on
walmart.com. You may also contact the Customer Service
Center at 888-968-4015 if you need information about
upcoming record dates for dividends. Keep in mind that a
dividend payout is taxable to you.
Note that if you request a hardship payout from your 401(k)
Account within five business days of the record date for a
dividend and you have the right to elect a cash distribution
of the dividend, tax laws require that the dividend be
automatically paid to you in cash.
Account balances and statements
At least once a year, you’ll receive a statement on your
accounts showing contributions made by you and by
Walmart, if any, the performance of your investment
options, the values of your accounts, and fees assessed to
your account. You can easily get information about your
accounts, including a quarterly statement, at any time
online at benefits.ml.com or by calling the Customer
Service Center at 888-968-4015. You can also request a
paper copy of any quarterly statement at any time free of
charge by calling the Customer Service Center.
FEES CHARGED TO YOUR ACCOUNT
Administrative and investment fees may be assessed to
youraccounts. Information on fees can be found in the
Annual Participant Fee Disclosure Notice and online
atbenefits.ml.com.
Receiving a payout while working
forWalmar
Generally, you are not entitled to a payout from the
Walmart 401(k) Plan until you stop working for Walmart.
However, in the following limited situations you may be
entitled to receive a payout or loan of some or all of your
accounts while you’re still working:
• In the case of a financial hardship or after you reach age 59½.
• Rollovers can be withdrawn at any time.
• You may request a loan from your Plan account.
It’s important to understand how any type of payout or loan
from the Walmart 401(k) Plan affects your tax situation. For
more information, see The income tax consequences of a
payout later in this summary.
FINANCIAL HARDSHIP WITHDRAWALS
You may withdraw some or all of your vested Account
as necessary to meet a “financial hardship.” (Prior to
February1, 2020, you may only withdraw your 401(k)
Account, other than earnings on those contributions, and
your 401(k) Rollover Account.)
Under IRS guidelines, a financial hardship may exist if the
request is for:
• Payment of medical care expenses not covered by
insurance for you, your spouse, your dependents, or your
affirmatively designated primary beneficiary
• Costs directly related to the purchase of your primary
residence
• Payment of tuition, fees, and room and board expenses for
up to the next 12 months of post-high school education for
you, your spouse, your dependents, or your affirmatively
designated primary beneficiary
• Payments necessary to prevent eviction from, or
foreclosure on, your primary residence
• Payment for burial or funeral expenses for your deceased
parent, spouse, children, dependent, or your affirmatively
designated primary beneficiary, or
• Expenses for the repair of damage to your principal
residence that would qualify for a casualty deduction
under federal income tax rules (determined without
regard to whether the casualty was a federally-declared
disaster and whether the loss exceeds 10% of your
adjusted gross income).
See page 296
Federal tax law requires that you must have already
obtained all in-service payouts available (including in-service
withdrawals of rollover contributions, withdrawals after
age 59½, and, prior to February 1, 2020, any nontaxable
participant loans available to you under this Plan) before you
can request a financial hardship payout. Also, please note

The Walmar 401(k)Plan
244
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
that if you request a financial hardship payout within five
business days of the record date of a dividend and you are
entitled to elect a cash payout of that dividend, the dividend
will automatically be distributed to you in cash. For payouts
on or after January 1, 2020, you will also be required to
certify that you have insufficient cash or other liquid assets
to satisfy the need.
Note that if your payout is processed before January 1, 2020,
you will not be allowed to contribute to this Plan and certain
other retirement or stock purchase plans (including the
Associate Stock Purchase Plan) for six months after the date
of your financial hardship payout. If you are a management
associate with stock options, you may not exercise options
during this six-month period. If your payout is processed on or
after January 1, 2020, however, these restrictions do not apply.
A financial hardship payout is immediately taxable to
you (other than Roth contributions and, if the payout is a
qualified distribution, earnings on your Roth contributions),
including a 10% penalty tax if you are under age 59½ or if
the payout is not for certain medical purposes. For more
information, see The income tax consequences of a payout
later in this chapter.
You can make a request for a financial hardship payout
online at benefits.ml.com or by calling the Customer
Service Center at 888-968-4015.
WITHDRAWALS AFTER YOU REACH AGE 59½
Any time after you reach age 59½, you may elect to
withdraw all or any portion of your Plan accounts, to
the extent vested, even though you are still working for
Walmart. You can make a request for a withdrawal online at
benefits.ml.com or by calling the Customer Service Center
at 888-968-4015.
WITHDRAWALS OF ROLLOVER
CONTRIBUTIONS
You may withdraw all or any portion of your 401(k) Rollover
Account and your Profit Sharing Rollover Account at any time
even if you are still working for Walmart or its subsidiaries.
PLAN LOANS
You may apply for a loan from the vested portion of your
Plan account while you are still working for Walmart. The
Administrator has established a written loan program
explaining the Plan’s loan requirements in detail. You can
request a copy of the loan program or make a request for
aloan online at benefits.ml.com or by calling the Customer
Service Center at 888-968-4015.
Generally, the rules for loans include the following:
• The maximum loan amount is limited by IRS rules, which
generally limit your total loan balances to the lesserof
(1) 50% of the total of your vested Plan account or
(2)$50,000 (reduced by the excess, if any, of your highest
outstanding loan balance during the one-year period prior
to the date of the loan over your current outstanding
balance of loans). The minimum loan amount is $1,000.
• All loans must be secured by a pledge of up to one-half of
your vested Plan account.
• A fee will be charged to process your loan application.
Additional fees may be accessed for residential loans.
(Feeamounts may change from time to time.)
• All loans bear a commercially reasonable rate of interest
set by the Administrator from time to time.
• Loans must be repaid in regular installments over a one-
tofive-year period, unless you are using the loan proceeds
to buy a house for yourself, in which case the repayment
period may be longer as set forth in the written loan
program from time to time.
• You may have only one general purpose loan and one
residential loan outstanding at any time.
• All loans are considered a directed investment from your
account under the Plan. Your payments of principal and
interest on the loan are credited to your Plan accounts.
• If you fail to make payments when due under the loan,
you will be considered to be in default. Under certain
circumstances, a loan that is in default may be considered
a distribution from the Plan. The significance of the loan
balance being treated as a distribution is that the amount
of this distribution (other than Roth contributions) is
taxable to you as ordinary income and could be subject to
excise taxes. A Form 1099-R will be issued to you and the
total amount of the distribution will be reported to the IRS.
When you are on an authorized unpaid leave of absence, you
may be excused from making scheduled loan repayments
for a period of up to one year. If you have an outstanding
loan when you are called to qualified military service, special
rules under USERRA may apply. Call the Customer Service
Center at 888-968-4015 for more details.
See page 296
If you die: your designated beneficiary
In the event of your death, your entire Plan balance will be
paid out to your beneficiary. It is very important for you to
keep your beneficiary information up to date. Beneficiary
choices must be made at One.Walmart.com or Workday for
Jet associates. Starting February 1, 2020, only beneficiary
designations made online will be accepted. (Note that
your spouse’s consent must still be completed on Form
B, as explained below.) Since your spouse or partner has
certain rights in the death benefit, you should immediately
update your beneficiary election if there is a change in your
relationship status.
If you have a spouse and wish to name someone other than
your spouse as your designated beneficiary, your spouse
The Walmar 401(k)Plan
245
must consent to that designation. You must complete
the Alternate Beneficiary Form for Married Participants
FormB and your spouse must complete the Spousal Consent
portion of that form. The Spousal Consent form must be
notarized and must accompany the Form B in order to be
valid. Form B and the Spousal Consent form can be found on
One.Walmart.com. Any beneficiary designation you make
will be effective for all of your Plan accounts.
If you do not designate a beneficiary, your death benefit
will be distributed in accordance with the Plan’s default
provisions in the following order, as stated below:
• Spouse or partner (as defined below); if none, then
• Living children (stepchildren are not included); if none, then
• Living parents; if none, then
• Living siblings; if none, then
• Your estate.
Please note that if you designate your spouse as your
beneficiary and you later divorce, your beneficiary
designation will not be effective after the divorce unless
you complete a new beneficiary designation form. Similarly,
if you do not have a spouse and you later marry, your prior
beneficiary designation will not be effective after the
marriage unless you complete a new designation form with
your spouse’s consent.
Also, note that if you designate a beneficiary and your
beneficiary dies before the benefit check is issued, the
benefit will be paid to your contingent beneficiary or, if
none, under the default rules above. If your beneficiary dies
after the benefit check has been issued, the benefit will
be paid to your beneficiary’s estate. Note, however, that
if your spouse or partner is your beneficiary, the benefit
will always be paid to the spouse’s or partner’s estate if
he or she dies after you but before the benefit is paid.
Again, it is very important for you to keep your beneficiary
information up to date. Beneficiary choices should be made
at One.Walmart.com or Workday for Jet associates.
NOTE: Effective June 26, 2013, your same-sex spouse is
treated in the same manner as an opposite-sex spouse for
Plan purposes. Keep in mind that if you had a same-sex
spouse on that date, any beneficiary designation you had in
effect which designated someone other than your spouse as
your beneficiary became invalid on that date. Your spouse
will automatically be your beneficiary unless you make a
new beneficiary designation with your spouse’s consent.
Effective January 1, 2014, if you have a “partner” and you
have not made an affirmative beneficiary designation, your
partner will be your beneficiary unless you affirmatively
designate a different beneficiary (regardless of whether
the designation occurred before or after your partnership
began). Your “partner” for Plan purposes means:
• Your domestic partner, as long as you and your
domesticpartner:
– Are in an ongoing, exclusive and committed relationship
similar to marriage and have been for at least 12 months
and intend to continue indefinitely;
– Are not married to each other or to anyone else;
– Meet the age for marriage in your home state and are
mentally competent to consent to contract in that state;
– Are not related in a manner that would bar a legal
marriage in the state in which you live, and
– Are not in the relationship solely for the purpose of
obtaining benefits coverage, or
• Any other person to whom you are joined in a legal
relationship recognized as creating some or all of the
rights of marriage in the state or country in which the
relationship was created.
You should take action to ensure that your beneficiary
under the Plan reflects your current intent. Beneficiary
choices should be made at One.Walmart.com or Workday
for Jetassociates.
BENEFICIARY DESIGNATIONS MADE BEFORE
OCTOBER 31, 2003
If you made a beneficiary designation under the 401(k)
Plan on or before October 31, 2003, that designation
will continue to apply to your Pretax Account, your Roth
Account, your Company Funded 401(k) Account, your
Company Match Account, and your Rollover Accounts.
Similarly, if you made a beneficiary designation under the
Profit Sharing Plan on or before October 31, 2003, that
designation will continue to apply to your Company Funded
Profit Sharing Account and Profit Sharing Rollover Account.
If you change your beneficiary designation after October
31, 2003, it will apply to all Plan accounts and any prior
designations will be ineffective.
Note that changes in your relationship status may affect
your beneficiary designation, as explained above.
Again, it is very important for you to keep your beneficiary
information up to date. Beneficiary designations should be
made at One.Walmart.com or Workday for Jet associates.
If you get divorced
If you go through a divorce, all or part of your Plan balance
may be awarded to an “alternate payee” in the court order,
called a “qualified domestic relations order” (QDRO). An
alternate payee may be your spouse or former spouse,
child or other dependent. (Federal law at this time does
not permit the recognition of a QDRO for a partner
unless the partner is also a dependent of the participant.)
Because there are very strict requirements for these
The Walmar 401(k)Plan
246
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
cases, you should contact the QDRO Administrator at
877-MER-QDRO (877-637-7376) for a free copy of the
procedures your attorney should use in drafting the court
order. After the court order is received by the QDRO
Administrator, it must be reviewed to determine if it meets
legal requirements for this type of order and will take a
period of time to be processed. The administrative fee for
processing your QDRO will be charged to your account or
as directed in the Order.
If you leave Walmar
When you stop working for Walmart, you are entitled to
receive a payout of all of your vested accounts in the Plan.
It is important to understand how any type of payout from
the Walmart 401(k) Plan affects your tax situation. For more
information, see The income tax consequences of a payout
later in this summary.
You may elect to receive your payout 30 calendar days after
your termination is entered into the payroll system. For
example, if your termination is entered into and processed
by the payroll system on July 19, 2020, you may elect your
payout on or after August 18, 2020.
A notice informing you that you are entitled to payment
will normally be mailed to your home address or sent
electronically, based on your delivery elections, after
you leave Walmart and its subsidiaries. Please make sure
that your address is correct on your payroll check when
you leave Walmart and its subsidiaries or that you give a
forwarding address during your exit interview. If you have
not received any information regarding your payout within
60 days of your termination date, contact the Customer
Service Center at 888-968-4015. To request your payout,
you will need to access your account on benefits.ml.com or
by calling the Customer Service Center at 888-968-4015.
Your consent to the payout is not required and your payout
will automatically be made to you:
• If your total vested Plan balance (excluding your 401(k)
Rollover Account) is $1,000 or less at any time. This
automatic payout will be made as soon as possible after the
last business day of the third calendar month following the
calendar month in which your termination date is entered
into the payroll system, unless you consent to an earlier
payout, as described above. In the example above, if your
account is eligible for automatic payout and you do not
consent to payout on or after August 19, 2020, your payout
will automatically be made to you as soon as possible after
October 31, 2020, or
• If you are over age 70, regardless of the amount of your
total vested Plan balance. This automatic payout will be
made as soon as possible after the last business day of the
second calendar month following the calendar month in
which you turn age 70, unless you consent to an earlier
payout, as described above. For instance, if you turn age
70 in July 2020 and your account is eligible for automatic
payout, and you do not consent to payout, your payout
would automatically be made on the first scheduled date
after September 30, 2020, according to Plan provisions.
If your total vested Plan balance is more than $1,000 and
you are under age 70, you must consent to your payout.
Payout will be made as soon as possible after the Customer
Service Center receives your consent, but no earlier than
30 calendar days after your termination is entered into the
payroll system.
If your total vested Plan balance is more than $1,000, you can
choose to delay your payout until any date up to age 70, but
your Plan balance will be subject to an annual maintenance
fee and possibly other expenses. For information regarding
these charges, refer to the Annual Participant Fee Disclosure
Notice. If you choose to delay your payout, you will be able to
continue to make changes in your investment choices just as
you did while you were an active participant in the Plan.
If you return to work with Walmart before your payout is
completed, the payout will be canceled and no payout will
be made from your account.
THE AMOUNT OF YOUR PAYOUT
The entire value of your Pretax Account, your Roth
Account, your Company Funded 401(k) Account, your
Rollover Accounts, and the Company Match Account will
be paid out to you (alternatively, partial distributions will
be available effective February 1, 2020, as explained on
the next page). In addition, if you have a Company Funded
Profit Sharing Account (see Your Walmart 401(k) Plan
accounts earlier in this summary), you will also be paid the
value of the vested portion of your Company Funded Profit
Sharing Account. You will forfeit (give up) the nonvested
portion of your Company Funded Profit Sharing Account,
as explained in the Vesting in your Company Funded Profit
Sharing Account earlier in this summary.
The amount you will receive will be based on the value of
your accounts as of the date the payout is processed. If a
cash payout is made directly to you rather than rolled over
to an IRA or other employer plan, applicable taxes will be
withheld from your check.
A check processing fee will be applied to your Plan balance
when it is paid out to you.
HOW YOU RECEIVE YOUR PAYOUT
You have several options for receiving your payout.
Your accounts will normally be paid to you in cash. However,
you may elect to have your Company Funded Profit Sharing
Account (and Profit Sharing Rollover Account) distributed
to you in the form of Walmart stock (even if it is not invested
The Walmar 401(k)Plan
247
in Walmart stock at the time your payout is processed) or
partly in cash and partly in Walmart stock. You may also elect
to have your Pretax Account, your Company Funded 401(k)
Account, and your Rollover Accounts paid to you in Walmart
stock to the extent those accounts are invested in Walmart
stock at the time your payout is processed. Any part of those
accounts not invested in Walmart stock at the time of your
payout will be distributed in cash.
If the total of your vested accounts is $1,000 or less, or
if you are over age 70 (regardless of the amount of your
vested accounts), your payout will be made directly to you in
a single cash payout. If you wish to take any of your payout
in the form of Walmart stock or if you wish to roll over your
payout to an IRA or other employer plan, you must contact
the Customer Service Center at 888-968-4015 with your
payout instructions within the time period shown in your
payout notice. If you fail to contact the Customer Service
Center in a timely manner, your payout will be made in a
single cash payment to you.
If the total of your vested accounts in the Plan is more than
$1,000, your payout will not be made until you make an
election regarding the form of payout and consent to the
distribution, or until you reach age 70.
Beginning February 1, 2020, you can choose to take all or
any portion of your vested account. (Note, however, that if
you take a partial payout of your account and the amount
remaining in your account drops to $1,000 or less, it will
be cashed-out as explained above.) To obtain your payout,
contact the Customer Service Center at 888-968-4015.
Your accounts normally will be distributed directly to you,
unless you elect to roll them over to an IRA or to another
employer’s retirement plan.
If you leave and are rehired
byWalmar
If you leave Walmart and its subsidiaries and are later rehired as
an eligible associate, you will be immediately eligible to make
your own contributions to the Plan on your date of rehire.
If you leave Walmart and its subsidiaries after you became
eligible to receive matching contributions and are later
rehired by Walmart, you will automatically be eligible
to receive matching contributions on your rehire date.
Similarly, if you leave Walmart and its subsidiaries after
you have met the 1,000-hour requirement for matching
contribution eligibility but before your actual participation
date, you will be eligible to receive matching contributions
beginning on the later of the date you would have initially
become a participant or your rehire date (with respect
to contributions you make after that date). If you were
not a participant when you left, or had not satisfied the
1,000-hour requirement, you will be treated as a new
associate when you are rehired and will be required
to complete the eligibility requirements (see When
participation begins earlier in this summary) in order to be
eligible to receive matching contributions under the Plan.
THE NONVESTED PORTION OF
YOUR COMPANY FUNDED PROFIT
SHARINGACCOUNT
When you terminate employment, the portion of your
Company Funded Profit Sharing Account that is not vested
(if any) will not be paid to you. This nonvested amount is
called a “forfeiture.”
• If you receive a total payout of your vested Plan balance
after your termination of employment and while your
Company Funded Profit Sharing Account is partially
vested, the nonvested portion of your Company Funded
Profit Sharing Account will be forfeited on the date of
your payout.
• If you do not receive a total payout of your vested Plan
balance after your termination of employment, the
nonvested portion of your Company Funded Profit
Sharing Account will not be forfeited until you have five
consecutive “breaks in service.” A break in service is a Plan
year (February 1–January 31) in which you are credited with
500 hours of service or less. If you are absent from work
due to an FMLA leave and have worked 500 hours or less
in the Plan year, you will be credited with enough hours to
bring you up to 500.01 hours so that you will not incur a
break in service.
The nonvested portion of your Company Funded Profit
Sharing Account that was forfeited will be reinstated (at its
former value) if you are rehired by Walmart or subsidiary
before you have five consecutive breaks in service and you
pay back to the Plan the total amount of your payout within
five years after you are rehired. If you return to work with
Walmart or a subsidiary after five or more consecutive
breaks in service, or if you chose not to repay your payout
as discussed above, the nonvested portion of your Company
Funded Profit Sharing Account that was forfeited will not
be reinstated.
If you were zero percent vested in your Company Funded
Profit Sharing Account when you terminated employment,
your nonvested Company Funded Profit Sharing Account
will automatically be reinstated if you are rehired prior to
five consecutive breaks in service.
Forfeitures of nonvested Company Funded Profit Sharing
Accounts of terminated participants generally are used to
pay Plan expenses and for certain other purposes, such as to
restore account balances as discussed above.
When you are rehired, your years of service with Walmart
before you left will be counted for purposes of determining
your vesting in Walmart’s contributions to your Company
Funded Profit Sharing Account.
The Walmar 401(k)Plan
248
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The income tax consequences
ofapayout
The tax consequences of your participation in the Plan
are your responsibility. This explanation is only a brief
description of the U.S. federal tax consequences related
to your participation in the Plan. This description is based
on current law and current interpretations of the law by
the Internal Revenue Service. Because the law is subject
to change and because the application of the law may
vary depending on your particular circumstances, this
description is general in nature and you should not rely on
it in determining your tax consequences. You are strongly
urged to consult a tax advisor.
Walmart is entitled to a deduction on the amount of its
contributions, as well as your contributions, to the Plan.
Your pretax contributions and Walmart’s contributions
to the Plan, as well as earnings on those contributions,
generally are not subject to federal income taxes until they
are paid to you. You are taxed on your Roth contributions
when you contribute them to the Plan. Earnings on Roth
contributions are not taxed unless you take a distribution
that is not a qualified distribution. (See Taxation of payouts
of Roth contributions below.)
POSTPONE PAYING TAXES ON PAYOUTS
THROUGH A ROLLOVER OTHER THAN A
ROTH ACCOUNT
Although payouts from the Plan (other than from your Roth
Account) are subject to federal income taxes, the Internal
Revenue Code provides favorable tax treatment to payouts
in certain circumstances. For example, you can postpone
paying taxes on your payout if you direct the Plan to issue
your payout directly to an IRA or to another employer’s
qualified retirement plan, a 403(b) plan, or a governmental
457 plan. This is called a direct rollover. (The check will be
made payable to the IRA or other plan trustee and will be
delivered to you or your IRA or rollover institution. If the
check is mailed to you, you will be responsible for delivering
it to the IRA or other plan trustee within 60 days.)
If you elect this method for your payout, no taxes will be
withheld from the amount you are rolling over. It will not
be taxed until you later receive a payout from the IRA or
other plan.
If you do not elect to have your payout directly rolled over,
federal law requires that Walmart withhold 20% of the
payout for federal taxes, in addition to any required state
withholding. In some cases, 20% withholding may not be
enough, which could mean that you will owe additional taxes
when you file your income tax return.
If you do not elect a direct rollover (and instead receive an
actual payout from the Plan), you may still roll over those
funds to an IRA or an employer’s qualified retirement plan,
403(b) plan, or governmental 457 plan, as long as you do so
within 60 calendar days after you received the distribution.
The amount rolled over will not be subject to federal income
tax until you take it out of the IRA or other plan. If you want
to roll over 100% of your payout to an IRA or other plan,
however, you will have to use other money to replace the
20% that was withheld from your payout. If you roll over
only the 80% that you received, you will be taxed on the
20% that was withheld.
NOTE: You may roll over all or any portion of your account
that is eligible for rollover to a Roth IRA. Any amount rolled
over that would have been taxable if not rolled over will be
taxable at the time of the rollover to the Roth IRA. (Note
that you may voluntarily choose to have taxes withheld from
amounts at the time you roll over to a Roth IRA.)
For more information regarding these rollover rules,
reviewthe Special tax notice addendum that follows.
Retainthis addendum for review when you are eligible to
take adistribution.
TAXATION OF PAYOUTS OF
ROTHCONTRIBUTIONS
Your Roth contributions and earnings on those
contributions are not taxed when distributed from the
Plan as long as the distribution is a “qualified” distribution.
A“qualified” distribution is a distribution that is made:
(1)on account of your death, disability, or after you attain
age 59½, and (2)after you have completed a five-year
participation period. The five-year participation period is
the five-year period beginning with the first calendar year
in which in which you first make a Roth contribution to
the Plan (or to another 401(k) plan or 403(b) plan, if such
amount was rolled over to this Plan) and ending on the last
day of the fourth calendar year thereafter. For instance, if
you make your first Roth contribution in July 2020, your
five-year participation period will end on December 31,
2024. It is not necessary that you make a Roth contribution
in each of the five years.
If you receive a distribution from your Roth contributions
and earnings on those contributions that is not a “qualified”
distribution, the earnings on your Roth contributions will
be taxable to you at the time of distribution (unless you roll
over the distribution to a Roth IRA or a designated Roth
account in another employer plan). If you do roll over your
Roth contributions and earnings, you will not have to pay
taxes currently on the earnings and you will not have to pay
taxes later on payouts that are qualified distributions.
Your Roth contributions may be rolled over only to a Roth
IRA or a designated Roth account in another employer plan.
If the rollover is to a designated Roth account in another
employer plan, the rollover generally must be a direct
rollover (unless the amount being rolled over includes only
amounts that would have been taxable if distributed to you).
The Walmar 401(k)Plan
249
For more information regarding these rollover rules, review
the Special tax notice addendum: Roth contributions that
follows. Retain this addendum for review when you are
eligible to take a distribution.
EARLY WITHDRAWAL PENALTY
If you take a payout prior to age 59½ rather than rolling
it over, in most cases you will be subject to a 10% early
withdrawal penalty by the IRS on the taxable portion of your
payout. Thus, Roth contributions and, if they are distributed
in a “qualified” distribution, earnings on those contributions,
are not subject to the 10% early withdrawal penalty. There
are some exceptions to the penalty, such as death, disability,
retirement after age 55, and payouts for certain medical
expenses. Special rules also apply to distributions made to
reservists who are called to active military duty.
TAXATION OF PAYOUTS OF WALMART STOCK
There are also special rules for distributions of Walmart
common stock. If you receive cash (in excess of $200) in
addition to Walmart stock and the cash is not directly rolled
over, some withholding may apply, but the withheld amount
will not be greater than the amount of cash you receive.
Generally, if you receive Walmart common stock as part of
your payout that is not rolled over, you are taxed only on the
value of the stock at the time it was purchased by the Plan.
Keep in mind that if you elect cash payouts of dividends
paid on Walmart stock held in your Company Funded
Profit Sharing Account, the dividend is taxable to you
and is not eligible for rollover. The dividend is also taxable
if you request a financial hardship payout from your
account within five business days of the record date for
a dividend and the dividend is automatically paid out to
you in cash. The dividend payout is not subject to the 10%
early withdrawal penalty discussed above. In some cases,
Walmart Inc. will be entitled to deduct dividends paid on
shares subject to this election.
TAXATION OF PAYOUTS TO BENEFICIARIES
AND ALTERNATE PAYEES
The tax treatment discussed above applies only to payouts
to participants. Different rules may apply to payouts to
beneficiaries of deceased participants. In general, if your
spouse is your beneficiary, he or she will have the same
federal income tax treatment and rollover options that you
would have had. Other beneficiaries, including partners, will
only be entitled to a direct rollover to an inherited IRA or
Roth IRA. The 10% early withdrawal penalty does not apply
to payouts to your beneficiary.
The spouses or former spouse of a participant who receives
a payout from the Plan under a qualified domestic relations
order (QDRO) generally have the same federal income tax
treatment and options as the participant would have had. In
some cases, however, a payout on behalf of a non-spouse
dependent, including a partner, pursuant to a QDRO (e.g.,
state-ordered child support) may result in federal income
taxation to the participant even though the payout is made
to or on behalf of the dependent alternate payee.
TAXATION OF LOANS
Under current tax law, loans made from the Plan,
regardless of their purpose, are not considered taxable
income to the participant unless a default occurs. If you
default on a loan from the Plan (as discussed above), your
tax statement will show the amount of income to report
for the year of the default. You may also be subject to 10%
early withdrawal penalty.
Filing a Walmar 401(k) Plan claim
If you think you are entitled to a benefit beyond that
processed by the Plan’s recordkeeper (Merrill Lynch), you
may file a claim with the Administrator or its delegate at:
Walmart Inc.
Attn: Financial Benefits
508 SW 8th Street
Bentonville, Arkansas 72716-0295
For questions about filing a claim, contact People Services
at 800-421-1362.
If your claim is partially or fully denied, you will receive
written notice of the decision within a reasonable time, but
no later than 90 days after the Administrator receives your
claim. The Administrator or its delegate can extend this
period for up to an additional 90 days if it determines that
special circumstances require an extension. You will receive
notice of any extension before the expiration of the original
90-day period. The written notice you receive will state
the specific reasons for the denial of your claim, a specific
reference to the provisions of the Plan upon which the denial
is based, and a description of the review procedures and the
time limits applicable to such procedures, including your
right to bring a court action following a denial on appeal.
If you do not agree with the decision of the Administrator
or its delegate, you can request a review of the decision
by the Administrator. The Administrator has discretionary
authority to resolve all questions concerning administration,
interpretation, or application of the Plan. Your request must
be made in writing and sent to the Administrator at:
Walmart Inc.
Attn: Financial Benefits
508 SW 8th Street
Bentonville, Arkansas 72716-0295
The Walmar 401(k)Plan
250
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Your request must be made within 60 calendar days of the
denial. Your written request must contain all additional
information that you wish the Administrator to consider. If
you do not request a review within this time period, you will
be deemed to have waived your right to a review.
The Administrator will promptly conduct the review.
Written notice of the Administrator’s decision on review
will be provided to you within 60 calendar days after the
receipt of your request, unless special circumstances
require an extension of up to 60 additional days. In those
circumstances where the review is delayed to allow you
to provide additional information necessary for a proper
review, the length of the delay will not be included in the
calculation of the 60-day deadline and extension periods
set forth above. The written notice of the Administrator’s
decision will include specific reasons for the decision and
will refer to the specific provisions of the Plan on which the
decision is based.
You must exhaust these procedures before you can file
a lawsuit with respect to your Plan benefits. If you file
a lawsuit, it must be filed within one year from the date
of your payout or, if no payout is made, the date your
request for benefits is denied, in whole or in part, by
the Administrator on appeal (or, if earlier, the date the
Administrator fails to respond to your claim or appeal within
the time periods provided above).
Administrative information
PLAN NAME
The legal name of the Plan is the Walmart 401(k) Plan.
PLAN SPONSOR AND ERISA
PLANADMINISTRATOR
Walmart Inc. is the Plan Sponsor. Its contact information for
matters pertaining to the Plan is:
Walmart Inc.
Attn: Financial Benefits
508 SW 8th Street
Bentonville, Arkansas 72716-0295
800-421-1362
As the ERISA Plan Administrator, Walmart Inc. is responsible
for reporting and disclosure obligations under the Employee
Retirement Income Security Act of 1974 (ERISA) and
all other obligations required to be performed by plan
administrators under the Internal Revenue Code and
ERISA, except for those obligations delegated to the
Administrator, the Benefits Investment Committee or the
trustee of the Trust. ERISA is the federal law that imposes
certain responsibilities on Walmart Inc., the Administrator,
the Benefits Investment Committee, and the trustee with
respect to your retirement benefits.
Subsidiaries of Walmart Inc. are permitted to participate
in the Plan. You may obtain a list of subsidiaries currently
participating in the Plan by contacting People Services.
PLAN SPONSOR’S EMPLOYER
IDENTIFICATIONNUMBER
71-0415188
NAMED ADMINISTRATIVE FIDUCIARY
The individual from time to time holding the position
of Senior Vice President, Global Benefits Division, of
Walmart is the Administrator. The Administrator is the
named administrative fiduciary of the Plan. As the named
administrative fiduciary of the Plan, the Administrator is
generally responsible for the management, interpretation,
and administration of the Plan, including but not limited
to eligibility determinations, benefit payments, and other
functions required, necessary or advisable to carry out the
purpose of the Plan.
You may contact the Administrator at the following address:
Senior Vice President, Global Benefits Division/Administrator
Walmart Inc.
508 SW 8th Street
Bentonville, Arkansas 72716-0295
NAMED INVESTMENT FIDUCIARY
The Benefits Investment Committee is the named
investment fiduciary of the Plan. The Committee is
responsible for the Plan’s investment policies, including
selection of investment options to be made available under
the Plan and the selection of the default investment option.
You may contact the Benefits Investment Committee at the
following address:
Benefits Investment Committee
Walmart Inc.
508 SW 8th Street
Bentonville, Arkansas 72716-0295
PLAN TRUSTEE
Northern Trust Company
50 S. LaSalle Street
Chicago, Illinois 60603
One or more trusts hold all Plan assets, such as
contributions by participants and Walmart’s contributions.
As trustee of the Trust, Northern Trust Company receives
and holds contributions made to the Plan in trust and invests
those contributions according to the policies established
under the Plan.
The Walmar 401(k)Plan
251
AGENT FOR SERVICE OF LEGAL PROCESS
Corporation Trust Company
1209 Orange Street
Corporation Trust Center
Wilmington, Delaware 19801
Service of legal process may also be made on the ERISA
Plan Administrator or the trustee.
PLAN NUMBER
003
PLAN YEAR
February 1 through January 31
TYPE OF PLAN
The Walmart 401(k) Plan is a defined contribution plan
(401(k), profit sharing, and employee stock ownership plan).
ASSIGNMENT
Because this is a retirement plan governed by ERISA and
other federal laws, your accounts cannot be assigned or
used as collateral for a loan, nor can your accounts be
garnished or be subject to bankruptcy proceedings. They
can, however, be part of a divorce settlement, as explained
in the If you get divorced section earlier in this summary.
NO PBGC COVERAGE
ERISA created a governmental agency called the Pension
Benefit Guaranty Corporation (PBGC). One of the purposes
of the PBGC is to insure the benefits payable under defined
benefit plans. The PBGC does not, however, provide
coverage for defined contribution plans. Because the Plan
is a defined contribution plan, it is not eligible for coverage
by the PBGC.
PLAN AMENDMENT OR TERMINATION
Walmart reserves the right to amend or terminate the Plan
at any time. Amendments are made by Walmart’s Board of
Directors or by its Executive Vice President, Global People
Division. Neither the Plan nor the benefits described in
this summary may be orally amended. All oral statements
and representations have no force or effect, even if the
statements and representations are made by a management
associate of Walmart or a participating subsidiary, by the
Administrator, by any member of the Benefits Investment
Committee, or by Merrill Lynch.
You may obtain a copy of the formal Plan document by
writing to:
Walmart Inc.
Attn: People Services
508 SW 8th Street
Bentonville, Arkansas 72716-0295
You can also contact the Customer Service Center at
888-968-4015.
MISTAKEN PAYOUTS
If any payout is made under the Plan to the wrong party,
or if a payout is made to the right party but in the wrong
amount, the Administrator can recover the mistaken
payout from the recipient by either reducing his or her
Plan account or future payouts due to the recipient, or may
demand that the recipient promptly repay the Plan.
STATEMENT OF ERISA RIGHTS
As a participant in this Plan, you are entitled to certain
rights and protections under ERISA. ERISA provides that all
Plan participants shall be entitled to:
• Examine, without charge, at the ERISA Plan
Administrator’s office and at other specified facilities,
all documents governing the Plan, including insurance
contracts and collective bargaining agreements, and
a copy of the latest annual report (Form 5500 series)
filed by the Plan with the U.S. Department of Labor and
available at the Public Disclosure Room of the Employee
Benefits Security Administration.
• Obtain, upon written request to the ERISA Plan
Administrator, copies of documents governing the
operation of the Plan, including insurance contracts and
collective bargaining agreements, and copies of the latest
annual report (Form 5500 series) and updated Summary
Plan Description. The ERISA Plan Administrator may make
a reasonable charge for the copies. Your request must be
mailed to:
Walmart Inc. — ERISA Section 104(b) Request
Attn: People Services
508 SW 8th Street
Bentonville, Arkansas 72716-0295
• Receive a summary of the Plan’s annual financial report.
The ERISA Plan Administrator is required by law to
furnish each participant with a copy of the summary
financial report.
• Obtain a statement telling you the current balance
of your account and the portion of your account that
is nonforfeitable (vested). This statement must be
requested in writing and is not required to be given more
than once every 12 months. The Plan must provide the
statement free of charge.
The Walmar 401(k)Plan
252
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
In addition to creating rights for Plan participants, ERISA
imposes duties upon the people who are responsible for the
operation of the Plan. The people who operate the Plan,
called “fiduciaries” of the Plan, have a duty to do so prudently
and in your interest and in that of other Plan participants and
beneficiaries. No one, including your employer or any other
person, may fire or otherwise discriminate against you in
any way to prevent you from obtaining a pension benefit or
exercising your rights under ERISA.
If your claim for a benefit is denied or ignored in whole or in
part, you have a right to know why this was done, to obtain
copies of documents relating to the decision without charge,
and to appeal any denial, all within certain time schedules.
Under ERISA, there are steps you can take to enforce the
above rights. For instance, if you request materials from
the Plan and do not receive them within 30 days, you may
file suit in a federal court. In such a case, the court may
require the ERISA Plan Administrator or the Administrator
to provide the materials and pay you up to $110 a day until
you receive the materials, unless the materials were not sent
because of reasons beyond the control of the ERISA Plan
Administrator or the Administrator. If you have a claim for
benefits that is denied or ignored, in whole or in part, you
may file suit in a state or federal court. In addition, if you
disagree with the Plan’s decision or lack thereof concerning
the qualified status of a domestic relations order, you may
file suit in a federal court.
If it should happen that Plan fiduciaries misuse the Plan’s
money, or if you are discriminated against for asserting your
rights, you may seek assistance from the U.S. Department
of Labor, or you may file suit in a federal court. The court
will decide who should pay court costs and legal fees. If you
are successful, the court may order the person you have
sued to pay these costs and fees. If you lose, the court may
order you to pay these costs and fees, for example, if it
finds your claim is frivolous.
If you have any questions about the Plan, you should
contact the ERISA Plan Administrator or the Administrator.
If you have any questions about this statement or about
your rights under ERISA, you should contact the nearest
regional office of the Employee Benefits Security
Administration, U.S. Department of Labor, listed in your
telephone directory, or the Division of Technical Assistance
and Inquiries, Employee Benefits Security Administration,
U.S. Department of Labor, 200 Constitution Avenue
NW, Washington, DC 20210. You may also obtain certain
publications about your rights and responsibilities under
ERISA by calling the publications hotline of the Employee
Benefits Security Administration.
Special tax notice addendum
YOUR ROLLOVER OPTIONS
The law requires that participants receive this notice before
receiving a distribution from the Plan that is eligible to
be rolled over to an IRA or an employer plan. You may or
may not currently be eligible to receive a distribution from
the Plan. If you are eligible for a distribution, however,
you should review this notice carefully before you elect
a distribution from the Plan. This notice is intended to
help you decide whether to elect a rollover. If you are not
currently eligible for a distribution, you should retain this
notice and review it when you are eligible for a distribution.
Rules that apply to most payments from the Plan are
described in the General information about rollovers
section. Special rules that only apply in certain
circumstances are described in the Special rules and
options section.
This notice describes the rollover rules that apply to payouts
from the Plan, other than those from a designated Roth
account. If you also receive a payment from your Roth
Account in the Plan (or any Roth amounts that were merged
into or rolled over to the Plan from your prior employer’s
plan), see the Special tax notice: Roth contributions
addendum that follows this notice.
GENERAL INFORMATION ABOUT ROLLOVERS
How can a rollover affect my taxes? You will be taxed on a
payment from the Plan if you do not roll it over. If you are
under age 59½ and do not do a rollover, you will also have
to pay a 10% additional income tax on early distributions
(unless an exception applies, as explained below). If you do
a rollover, however, you will not have to pay tax until you
receive payment later and the 10% additional income tax will
not apply if the payment is made after you are age 59½ (or if
an exception applies).
Where may I roll over the payment? You may roll over the
payment to either an IRA (an individual retirement account
or individual retirement annuity, including a Roth IRA) or
an employer plan (a tax-qualified plan, section 403(b) plan,
or governmental section 457(b) plan) that will accept the
rollover. The rules of the IRA or employer plan that holds
the rollover will determine your investment options, fees,
and rights to payment from the IRA or employer plan (for
example, no spousal consent rules apply to IRAs and IRAs
may not provide loans). Further, the amount rolled over will
become subject to the tax rules that apply to the IRA or
employer plan.
The Walmar 401(k)Plan
253
How do I do a rollover? There are two ways to do a rollover.
You can do either a “direct rollover” or a “60-day rollover.”
If you do a “direct rollover,” the Plan will make the payment
directly to your IRA or an employer plan. Contact the IRA
sponsor or the administrator of the employer plan for
information on how to do a direct rollover.
If you do not do a direct rollover, you may still do a “60-
day rollover” by making a deposit into an IRA or eligible
employer plan that will accept it. You will have 60 days
after you receive the payment to make the deposit. If you
do not do a direct rollover, the Plan is required to withhold
20% of the payment for federal income taxes (up to the
amount of cash received). This means that, in order to roll
over the entire payment in a 60-day rollover, you must use
other funds to make up for the 20% withheld. If you do not
roll over the entire amount of the payment, the portion
not rolled over will be taxed and will be subject to the 10%
additional income tax on early distributions if you are under
age 59½ (unless an exception applies).
How much may I roll over? If you wish to do a rollover, you
may roll over all or part of the amount eligible for rollover.
Generally, any payment from the Plan is eligible for
rollover, except:
• Required minimum distributions after age 70½ (or after
death)
• Hardship distributions
• ESOP dividends
• Corrective distributions of contributions that exceed tax
law limitations
• Loans treated as deemed distributions (for example,
loans in default due to missed payments before your
employment ends)
The Plan Administrator or the payer can tell you what
portion of a payment is eligible for rollover.
If I don’t do a rollover, will I have to pay the 10% additional
income tax on early distributions? If you are under age
59½, you will have to pay the 10% additional income tax on
early distributions for any payment from the Plan (including
amounts withheld for income tax) that you do not roll over,
unless one of the exceptions listed below applies. This tax
is in addition to the regular income tax on the payment not
rolled over.
The 10% additional income tax does not apply to the
following payments from the Plan:
• Payments made after you separate from service if you will
be at least age 55 in the year of the separation
• Payments made due to disability
• Payments after your death
• Payments of ESOP dividends
• Corrective distributions of contributions that exceed
taxlaw limitations
• Payments made directly to the government to satisfy a
federal tax levy
• Payments made under a qualified domestic relations
order(QDRO)
• Certain payments made while you are on active duty if
you were a member of a reserve component called to duty
after September 11, 2001 for more than 179 days
If I do a rollover to an IRA, will the 10% additional income
tax apply to early distributions from the IRA? If you receive
a payment from an IRA when you are under age 59½, you
will have to pay the 10% additional income tax on early
distributions from the IRA, unless an exception applies.
In general, the exceptions to the 10% additional income
tax for early distributions from an IRA are the same as the
exceptions listed above for early distributions from a plan.
However, there are a few differences for payments from an
IRA, including:
• There is no exception for payments after separation from
service that are made after age 55.
• The exception for qualified domestic relations orders
(QDROs) does not apply (although a special rule applies
under which, as part of a divorce or separation agreement,
a tax-free transfer may be made directly to an IRA of a
spouse or former spouse).
• An exception for payments made at least annually in equal
or close to equal amounts over a specified period applies
(without regard to whether you have had a separation from
service).
• There are additional exceptions for (1) payments for
qualified higher education expenses, (2) payments up
to $10,000 used in a qualified first-time home purchase,
and (3) payments after you have received unemployment
compensation for 12 consecutive weeks (or would have
been eligible to receive unemployment compensation but
for self-employed status).
Will I owe state income taxes? This notice does not
describe any state or local income tax rules (including
withholding rules).
SPECIAL RULES AND OPTIONS
If your payment includes after-tax contributions: If you
have after-tax contributions that were merged into the
Walmart 401(k) Plan, those contributions are subject
to special tax rules when they are distributed from the
Walmart 401(k) Plan. (See below if you have made Roth
contributions to the Plan.)
In general, after-tax contributions included in a payment
are not taxed. If a payment is only part of your benefit,
an allocable portion of your after-tax contributions is
The Walmar 401(k)Plan
254
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
included in the payment, so you cannot take a payment of
only after-tax contributions. However, if you have pre-1987
after-tax contributions maintained in a separate account, a
special rule may apply to determine whether the after-tax
contributions are included in a payment. In addition, special
rules apply when you do a rollover, as described below.
You may roll over to an IRA a payment that includes
after-tax contributions through either a direct rollover or
a 60-day rollover. You must keep track of the aggregate
amount of the after-tax contributions in all of your IRAs (in
order to determine your taxable income for later payments
from the IRAs). If you do a direct rollover of only a portion
of the amount paid from the Plan and at the same time the
rest is paid to you, the portion directly rolled over consists
first of the amount that would be taxable if not rolled
over. For example, assume you are receiving a distribution
of $12,000, of which $2,000 is after-tax contributions. In
this case, if you directly roll over $10,000 to an IRA that is
not a Roth IRA, no amount is taxable because the $2,000
amount not directly rolled over is treated as being after-
tax contributions. If you do a direct rollover of the entire
amount paid from the Plan to two or more destinations at
the same time, you can choose which destination receives
the after-tax contributions.
If you do a 60-day rollover to an IRA of only a portion of
a payment made to you, the after-tax contributions are
treated as rolled over last. For example, assume you are
receiving a distribution of $12,000, of which $2,000 is
after-tax contributions, and no part of the distribution is
directly rolled over. In this case, if you roll over $10,000
to an IRA that is not a Roth IRA in a 60-day rollover, no
amount is taxable because the $2,000 amount not rolled
over is treated as being after-tax contributions.
You may roll over to an employer plan all of a payment that
includes after-tax contributions, but only through a direct
rollover (and only if the receiving plan separately accounts
for after-tax contributions and is not a governmental
section 457(b) plan). You can do a 60-day rollover to an
employer plan of part of a payment that includes after-tax
contributions, but only up to the amount of the payment
that would be taxable if not rolled over.
If you miss the 60-day rollover deadline: Generally, the
60-day rollover deadline cannot be extended. However,
the IRS has the limited authority to waive the deadline
under certain extraordinary circumstances, such as
when external events prevented you from completing
the rollover by the 60-day rollover deadline. To apply
for a waiver, you must file a private letter ruling request
with the IRS. Private letter ruling requests require
the paymentof a nonrefundable user fee. For more
information, see IRS Publication 590, Individual Retirement
Arrangements (IRAs).
If your payment includes employer stock that you do
not roll over: If you do not do a rollover, you can apply a
special rule to payments of employer stock that are paid
in a lump sum after separation from service (or after
age 59½, disability, or the participant’s death). Under the
special rule, the net unrealized appreciation on the stock
will not be taxed when distributed from the Plan and will
be taxed at capital gain rates when you sell the stock. Net
unrealized appreciation is generally the increase in the
value of employer stock after it was acquired by the Plan.
If you do a rollover for a payment that includes employer
stock (for example, by selling the stock and rolling over the
proceeds within 60 days of the payment), the special rule
relating to the distributed employer stock will not apply to
any subsequent payments from the IRA or employer plan.
The Plan Administrator can tell you the amount of any net
unrealized appreciation.
If you have an outstanding loan that is being offset: If you
have an outstanding loan from the Plan, your Plan benefit
may be offset by the amount of the loan, typically when
your employment ends. The loan offset amount is treated as
a distribution to you at the time of the offset. Generally, you
may roll over all or any portion of the offset amount. Any
offset amount that is not rolled over will be taxed (including
the 10% additional income tax on early distributions, unless
an exception applies). You may roll over offset amounts to
an IRA or an employer plan (if the terms of the employer
plan permit the plan to receive plan loan offset rollovers).
How long you have to complete the rollover depends
on what kind of plan loan offset you have. If you have a
qualified plan loan offset, you will have until your tax return
due date (including extensions) for the tax year during which
the offset occurs to complete your rollover. A qualified
plan loan offset occurs when a plan loan in good standing is
offset because your employer plan terminates, or because
you sever from employment. If your plan loan offset occurs
for any other reason, then you have 60 days from the date
the offset occurs to complete your rollover.
If you were born on or before January 1, 1936: If you were
born on or before January 1, 1936 and receive a lump sum
distribution that you do not roll over, special rules for
calculating the amount of the tax on the payment might
apply to you. For more information, see IRS Publication 575,
Pension and Annuity Income.
If you roll over your payment to a Roth IRA: If you roll
over a payment to a Roth IRA, a special rule applies under
which the amount of the payment rolled over will be
taxed. However, the 10% additional income tax on early
distributions will not apply (unless you take the amount
rolled over out of the Roth IRA within five years, counting
from January 1 of the year of the rollover). If you roll
over the payment to a Roth IRA, later payments from
the Roth IRA that are qualified distributions will not be
The Walmar 401(k)Plan
255
taxed (including earnings after the rollover). A qualified
distribution from a Roth IRA is a payment made after
you are age 59½ (or after your death or disability, or as
a qualified first-time homebuyer distribution of up to
$10,000) and after you have had a Roth IRA for at least
five years. In applying this five-year rule, you count from
January 1 of the year for which your first contribution was
made to a Roth IRA. Payments from the Roth IRA that are
not qualified distributions will be taxed to the extent of
earnings after the rollover, including the 10% additional
income tax on early distributions (unless an exception
applies). You do not have to take required minimum
distributions from a Roth IRA during your lifetime. For more
information, see IRS Publication 590, Individual Retirement
Arrangements (IRAs).
If you are not a plan paricipant
Payments after death of the participant. If you receive a
distribution after the participant’s death that you do not
roll over, the distribution will generally be taxed in the same
manner described elsewhere in this notice. However, the
10% additional income tax on early distributions does not
apply, and the special rule described under the section If
you were born on or before January 1, 1936 applies only if
the participant was born on or before January 1, 1936.
If you are a surviving spouse: If you receive a payment from
the Plan as the surviving spouse of a deceased participant,
you have the same rollover options that the participant
would have had, as described elsewhere in this notice. In
addition, if you choose to do a rollover to an IRA, you may
treat the IRA as your own or as an inherited IRA.
An IRA you treat as your own is treated like any other IRA
of yours, so that payments made to you before you are age
59½ will be subject to the 10% additional income tax on early
distributions (unless an exception applies) and required
minimum distributions from your IRA do not have to start
until after you are age 70½.
If you treat the IRA as an inherited IRA, payments from the
IRA will not be subject to the 10% additional income tax on
early distributions. However, if the participant had started
taking required minimum distributions, you will have to
receive required minimum distributions from the inherited
IRA. If the participant had not started taking required
minimum distributions from the Plan, you will not have to
start receiving required minimum distributions from the
inherited IRA until the year the participant would have
been age 70½.
If you are a surviving beneficiary other than a spouse:
If you receive a payment from the Plan because of the
participant’s death and you are a designated beneficiary
other than a surviving spouse, the only rollover option you
have is to do a direct rollover to an inherited IRA or Roth
IRA. Payments from the inherited IRA or Roth IRA will
not be subject to the 10% additional income tax on early
distributions. You will have to receive required minimum
distributions from the inherited IRA or Roth IRA.
Payments under a qualified domestic relations order: If
you are the spouse or former spouse of the participant
who receives a payment from the Plan under a qualified
domestic relations order (QDRO), you generally have the
same options the participant would have (for example, you
may roll over the payment to your own IRA or an eligible
employer plan that will accept it). Payments under the
QDRO will not be subject to the 10% additional income tax
on early distributions.
If you are a nonresident alien: If you are a nonresident
alien and you do not do a direct rollover to a U.S. IRA or
U.S. employer plan, instead of withholding 20%, the Plan
is generally required to withhold 30% of the payment for
federal income taxes. If the amount withheld exceeds the
amount of tax you owe (as may happen if you do a 60-day
rollover), you may request an income tax refund by filing
Form 1040NR and attaching your Form 1042-S. See Form
W-8BEN for claiming that you are entitled to a reduced
rate of withholding under an income tax treaty. For more
information, see also IRS Publication 519, U.S. Tax Guide
for Aliens, and IRS Publication 515, Withholding of Tax on
Nonresident Aliens and Foreign Entities.
OTHER SPECIAL RULES
If your payments for the year are less than $200, the Plan is
not required to allow you to do a direct rollover and is not
required to withhold for federal income taxes. However, you
may do a 60-day rollover.
You may have special rollover rights if you recently served
in the U.S. Armed Forces. For more information on special
rollover rights related to the U.S. Armed Forces, see IRS
Publication 3, Armed Forces’ Tax Guide. You also may have
special rollover rights if you were affected by a federally
declared disaster (or similar event), or if you received a
distribution on account of a disaster. For more information
on special rollover rights related to disaster relief, see the
IRS website at www.irs.gov.
FOR MORE INFORMATION
You may wish to consult with the Plan Administrator or
payer, or a professional tax advisor, before taking a payment
from the Plan. Also, you can find more detailed information
on the federal tax treatment of payments from employer
plans in IRS Publication 575, Pension and Annuity Income;
IRS Publication 590, Individual Retirement Arrangements
(IRAs); and IRS Publication 571, Tax-Sheltered Annuity Plans
(403(b) Plans). These publications are available from a
local IRS office, on the web at www.irs.gov, or by calling
800-TAX-FORM.

The Walmar 401(k)Plan
256
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Special tax notice addendum:
Rothcontributions
YOUR ROLLOVER OPTIONS
The law requires that participants receive this notice before
receiving a distribution from the Plan from your Roth
Account (or any Roth amounts that were merged into to the
Plan from your prior employer’s plan). You may or may not
currently be eligible to receive a distribution from the Plan.
If you are eligible for a distribution, however, you should
review this notice carefully before you elect a distribution
from the Plan. This notice is intended to help you decide
whether to elect a rollover. If you are not currently eligible
for a distribution, you should retain this notice and review it
when you are eligible for a distribution.
Rules that apply to most payments from your Roth
Account (or any Roth amounts that were merged into or
rolled over to the Plan from your prior employer’s plan,
referred to collectively in this addendum as your “Roth
Account”) are described in the General information about
rollovers section. Special rules that only apply in certain
circumstances are described in the Special rules and
options section.
Rules that apply to payments from the Plan, other than
from your Roth Account (or any Roth amounts that were
merged into or rolled over to the Plan from your prior
employer’s plan) are described in the separate Special tax
notice addendum above.
GENERAL INFORMATION ABOUT ROLLOVERS
How can a rollover affect my taxes? After-tax contributions
included in a payment from your Roth Account are not
taxed, but earnings might be taxed. The tax treatment of
earnings included in the payment depends on whether the
payment is a qualified distribution. If a payment is only part
of your Roth Account, the payment will include an allocable
portion of the earnings in your Roth Account.
If the payment from the Plan is not a qualified distribution
and you do not do a rollover to a Roth IRA or a designated
Roth account in an employer plan, you will be taxed on the
earnings in the payment. If you are under age 59½, a 10%
additional income tax on early distributions (generally,
distributions made before age 59½) will also apply to the
earnings (unless an exception applies). However, if you
do a rollover, you will not have to pay taxes currently on
the earnings and you will not have to pay taxes later on
payments that are qualified distributions.
If the payment from the Plan is a qualified distribution, you will
not be taxed on any part of the payment even if you do not
do a rollover. If you do a rollover, you will not be taxed on the
amount you roll over and any earnings on the amount you roll
over will not be taxed if paid later in a qualified distribution.
A qualified distribution from your Roth Account in the
Plan is a payment made after you are age 59½ (or after
your death or disability) and after you have had a Roth
Account in the Plan for at least 5 years. In applying the
5-year rule, you count from January 1 of the year your first
contribution was made to the Roth Account. However,
if you did a direct rollover to a Roth Account in the Plan
from a designated Roth account in another employer plan,
your participation will count from January 1 of the year
your first contribution was made to the Roth Account in
the Plan or, if earlier, to the designated Roth account in
the other employer plan.
What types of retirement accounts and plans may accept
my rollover? You may roll over the payment to either a
Roth IRA (a Roth individual retirement account or Roth
individual retirement annuity) or a designated Roth
account in an employer plan (a tax-qualified plan, section
403(b) plan, or governmental section 457 plan) that will
accept the rollover. The rules of the Roth IRA or employer
plan that holds the rollover will determine your investment
options, fees, and rights to payment from the Roth IRA
or employer plan (for example, no spousal consent rules
apply to Roth IRAs and Roth IRAs may not provide loans).
Further, the amount rolled over will become subject to the
tax rules that apply to the Roth IRA or the designated Roth
account in the employer plan. In general, these tax rules
are similar to those described elsewhere in this notice, but
differences include:
• If you do a rollover to a Roth IRA, all of your Roth IRAs will
be considered for purposes of determining whether you
have satisfied the 5-year rule (counting from January 1 of
the year for which your first contribution was made to any
of your Roth IRAs).
• If you do a rollover to a Roth IRA, you will not be required
to take a distribution from the Roth IRA during your
lifetime and you must keep track of the aggregate
amount of the after-tax contributions in all of your Roth
IRAs (in order to determine your taxable income for later
Roth IRA payments that are not qualified distributions).
• Eligible rollover distributions from a Roth IRA can only be
rolled over to another Roth IRA.
How do I do a rollover? There are two ways to do a rollover.
You can either do a direct rollover or a 60-day rollover.
If you do a direct rollover, the Plan will make the payment
directly to your Roth IRA or designated Roth account in an
employer plan. You should contact the Roth IRA sponsor or
the administrator of the employer plan for information on
how to do a direct rollover.

The Walmar 401(k)Plan
257
If you do not do a direct rollover, you may still do a rollover
by making a deposit (generally within 60 days) into a Roth
IRA, whether the payment is a qualified or nonqualified
distribution. In addition, you can do a rollover by making a
deposit within 60 days into a designated Roth account in an
employer plan if the payment is a nonqualified distribution
and the rollover does not exceed the amount of the
earnings in the payment. You cannot do a 60-day rollover
to an employer plan of any part of a qualified distribution. If
you receive a distribution that is a nonqualified distribution
and you do not roll over an amount at least equal to the
earnings allocable to the distribution, you will be taxed on
the amount of those earnings not rolled over, including the
10% additional income tax on early distributions if you are
under age 59½ (unless an exception applies).
If you do a direct rollover of only a portion of the amount
paid from the Plan and a portion is paid to you at the
same time, the portion directly rolled over consists first
of earnings. If you do not do a direct rollover and the
payment is not a qualified distribution, the Plan is required
to withhold 20% of the earnings for federal income taxes
(up to the amount of cash and property received other than
employer stock). This means that, in order to roll over the
entire payment in a 60-day rollover to a Roth IRA, you must
use other funds to make up for the 20% withheld.
How much may I roll over? If you wish to do a rollover, you
may roll over all or part of the amount eligible for rollover.
Any payment from the Plan is eligible for rollover, except:
• Required minimum distributions after age 70½ (or
afterdeath);
• Hardship distributions;
• ESOP dividends;
• Corrective distributions of contributions that exceed tax
law limitations; and
• Loans treated as deemed distributions (for example,
loans in default due to missed payments before your
employment ends).
The Administrator or the payor can tell you what portion of
a payment is eligible for rollover.
If I don’t do a rollover, will I have to pay the 10% additional
income tax on early distributions? If a payment is not
a qualified distribution and you are under age 59½, you
will have to pay the 10% additional income tax on early
distributions with respect to the earnings allocated to
the payment that you do not roll over (including amounts
withheld for income tax), unless one of the exceptions listed
below applies. This tax is in addition to the regular income
tax on the earnings not rolled over.
The 10% additional income tax does not apply to the
following payments from the Plan:
• Payments made after you separate from service if you will
be at least age 55 in the year of the separation;
• Payments made due to disability;
• Payments after your death;
• Payments of ESOP dividends;
• Corrective distributions of contributions that exceed tax
law limitations;
• Payments made directly to the government to satisfy a
federal tax levy;
• Payments made under a qualified domestic relations
order(QDRO);
• Certain payments made while you are on active duty if
you were a member of a reserve component called to duty
after September 11, 2001 for more than 179 days; and
• Payments for certain distributions relating to certain
federally declared disasters.
If I do a rollover to a Roth IRA, will the 10% additional
income tax apply to early distributions from the IRA? If you
receive a payment from a Roth IRA when you are under age
59½, you will have to pay the 10% additional income tax on
early distributions on the earnings paid from the Roth IRA,
unless an exception applies or the payment is a qualified
distribution. In general, the exceptions to the 10% additional
income tax for early distributions from a Roth IRA listed
above are the same as the exceptions for early distributions
from a plan. However, there are a few differences for
payments from a Roth IRA, including:
• The exception for payments made after you separate
from service if you will be at least age 55 in the year
of the separation (or age 50 for qualified public safety
employees) does not apply.
• The exception for qualified domestic relations orders
(QDROs) does not apply (although a special rule applies
under which, as part of a divorce or separation agreement,
a tax-free transfer may be made directly to a Roth IRA of a
spouse or former spouse).
• An exception for payments made at least annually in equal
or close to equal amounts over a specified period applies
without regard to whether you have had a separation
from service.
• There are additional exceptions for (1) payments for qualified
higher education expenses, (2) payments up to $10,000 used
in a qualified first-time home purchase, and (3) payments
for health insurance premiums after you have received
unemployment compensation for 12 consecutive weeks
(or would have been eligible to receive unemployment
compensation but for self-employed status).
The Walmar 401(k)Plan
258
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Will I owe state income taxes? This notice does not
describe any state or local income tax rules (including
withholding rules).
SPECIAL RULES AND OPTIONS
If you miss the 60-day rollover deadline: Generally, the
60-day rollover deadline cannot be extended. However, the
IRS has the limited authority to waive the deadline under
certain extraordinary circumstances, such as when external
events prevented you from completing the rollover by the
60-day rollover deadline. Under certain circumstances,
you may claim eligibility for a waiver of the 60-day rollover
deadline by making a written self-certification. Otherwise,
to apply for a waiver from the IRS, you must file a private
letter ruling request with the IRS. Private letter ruling
requests require the payment of a nonrefundable user
fee. For more information, see IRS Publication 590-A,
Contributions to Individual Retirement Arrangements (IRAs).
If you have an outstanding loan that is being offset: If you
have an outstanding loan from the Plan, your Plan benefit may
be offset by the outstanding amount of the loan, typically
when your employment ends. The offset amount is treated
as a distribution to you at the time of the offset. Generally,
you may roll over all or any portion of the offset amount. If
the distribution attributable to the offset is not a qualified
distribution and you do not roll over the offset amount, you
will be taxed on any earnings included in the distribution
(including the 10% additional income tax on early distributions,
unless an exception applies). You may roll over the earnings
included in the loan offset to a Roth IRA or designated Roth
account in an employer plan (if the terms of the employer plan
permit the plan to receive plan loan offset rollovers). You may
also roll over the full amount of the offset to a Roth IRA.
How long you have to complete the rollover depends
on what kind of plan loan offset you have. If you have a
qualified plan loan offset, you will have until your tax return
due date (including extensions) for the tax year during which
the offset occurs to complete your rollover. A qualified
plan loan offset occurs when a plan loan in good standing is
offset because your employer plan terminates, or because
you sever from employment. If your plan loan offset occurs
for any other reason, then you have 60 days from the date
the offset occurs to complete your rollover.
If you receive a nonqualified distribution and you were
born on or before January 1, 1936: If you were born on or
before January 1, 1936, and receive a lump sum distribution
that is not a qualified distribution and that you do not roll
over, special rules for calculating the amount of the tax
on the earnings in the payment might apply to you. For
more information, see IRS Publication 575, Pension and
AnnuityIncome.
If you are not a Plan paricipant
Payments after death of the participant. If you receive a
distribution after the participant’s death that you do not
roll over, the distribution will generally be taxed in the
same manner described elsewhere in this notice. However,
whether the payment is a qualified distribution generally
depends on when the participant first made a contribution
to the designated Roth account in the Plan. Also, the
10% additional income tax on early distributions and the
special rules for public safety officers do not apply, and the
special rule described under the section “If you receive a
nonqualified distribution and you were born on or before
January 1, 1936” applies only if the participant was born on
or before January 1, 1936.
If you are a surviving spouse: If you receive a payment from
the Plan as the surviving spouse of a deceased participant,
you have the same rollover options that the participant would
have had, as described elsewhere in this notice. In addition, if
you choose to do a rollover to a Roth IRA, you may treat the
Roth IRA as your own or as an inherited Roth IRA.
A Roth IRA you treat as your own is treated like any other
Roth IRA of yours, so that you will not have to receive any
required minimum distributions during your lifetime and
earnings paid to you in a nonqualified distribution before
you are age 59½ will be subject to the 10% additional income
tax on early distributions (unless an exception applies).
If you treat the Roth IRA as an inherited Roth IRA,
payments from the Roth IRA will not be subject to the 10%
additional income tax on early distributions. An inherited
Roth IRA is subject to required minimum distributions.
If the participant had started taking required minimum
distributions from the Plan, you will have to receive required
minimum distributions from the inherited Roth IRA. If
the participant had not started taking required minimum
distributions, you will not have to start receiving required
minimum distributions from the inherited Roth IRA until the
year the participant would have been age 70½.
If you are a surviving beneficiary other than a spouse: If you
receive a payment from the Plan because of the participant’s
death and you are a designated beneficiary other than a
surviving spouse, the only rollover option you have is to
do a direct rollover to an inherited Roth IRA. Payments
from the inherited Roth IRA, even if made in a nonqualified
distribution, will not be subject to the 10% additional income
tax on early distributions. You will have to receive required
minimum distributions from the inherited Roth IRA.
Payments under a qualified domestic relations order: If
you are the spouse or a former spouse of the participant
who receives a payment from the Plan under a qualified
domestic relations order (QDRO), you generally have
The Walmar 401(k)Plan
259
the same options and the same tax treatment that the
participant would have (for example, you may roll over the
payment as described in this notice).
If you are a nonresident alien: If you are a nonresident
alien and you do not do a direct rollover to a U.S. IRA or
U.S. employer plan, instead of withholding 20%, the Plan
is generally required to withhold 30% of the payment for
federal income taxes. If the amount withheld exceeds the
amount of tax you owe (as may happen if you do a 60-day
rollover), you may request an income tax refund by filing
Form 1040NR and attaching your Form 1042-S. See Form
W-8BEN for claiming that you are entitled to a reduced
rate of withholding under an income tax treaty. For more
information, see also IRS Publication 519, U.S. Tax Guide
for Aliens, and IRS Publication 515, Withholding of Tax on
Nonresident Aliens and Foreign Entities.
OTHER SPECIAL RULES
If your payments for the year (only including payments from
the designated Roth account in the Plan) are less than $200,
the Plan is not required to allow you to do a direct rollover
and is not required to withhold federal income taxes.
However, you can do a 60-day rollover.
You may have special rollover rights if you recently served
in the U.S. Armed Forces. For more information on special
rollover rights related to the U.S. Armed Forces, see IRS
Publication 3, Armed Forces’ Tax Guide. You also may have
special rollover rights if you were affected by a federally
declared disaster (or similar event), or if you received a
distribution on account of a disaster. For more information
on special rollover rights related to disaster relief, see the
IRS website at www.irs.gov.
FOR MORE INFORMATION
You may wish to consult with the Plan Administrator or
payor, or a professional tax advisor, before taking a payment
from the Plan. Also, you can find more detailed information
on the federal tax treatment of payments from employer
plans in IRS Publication 575, Pension and Annuity Income; IRS
Publication 590-A, Contributions to Individual Retirement
Arrangements (IRAs); IRS Publication 590-B, Distributions
from Individual Retirement Arrangements (IRAs); and IRS
Publication 571, Tax-Sheltered Annuity Plans (403(b) Plans).
These publications are available from a local IRS office, on
the web at www.irs.gov, or by calling 800-TAX-FORM.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Deadlines to file a claim or bring legal action 262
Appealing an enrollment or eligibility status decision 262
Medical, pharmacy, Centers of Excellence, dental, and vision benefits claims process 262
Internal appeal process 265
External appeal process for medical, pharmacy, or CentersofExcellencebenefits 269
Rights related to medical, pharmacy, Centers of Excellence, dental, vision,
and shor-term disability benefits 269
The Plan’s subrogation and reimbursement rights 270
Claims for benefits and right to appeal reduction, reimbursement, and subrogation decisions 271
HMO plan claims and appealsprocedures 273
eComm PPO Plan claims and appeals procedures 273
Accident and critical illness insurance claims process 273
Company-paid life insurance, optional associate and dependentlife insurance,
business travel accident insurance, and AD&D claimsprocess 275
Claims and appeals process for disability coverage claims 276
Resources for Living benefits 278
International business travel medicalinsurance 278
Claims and appeals

Claims and appeals
261
Claims and appeals
As a paricipant in the Associates’ Health and Welfare Plan, you have the right to appeal a decision
regarding Plan eligibility and benefits. This chapter describes the process and the deadlines for
appealing a claim that has been parially or fully denied in the areas of eligibility, medical, pharmacy,
dental, vision, HMO plans, life insurance, AD&D, disability, or critical illness and accident insurance.
RESOURCES
Find What You Need
Submit a claim for benefits For medical, pharmacy, dental, and vision claims, see your plan ID card for the claims
address or call your health care advisor at the number on your plan ID card. Submit
Centers of Excellence claims to the administrator as shown in the char later in the
chapter. Submit all other claims to the Plan’s third-pary administrators as shown later in
this chapter.
Appeal a denied claim Submit appeals to the addresses provided in this chapter for the Plan’s third-pary
administrators and/or People Services, depending on the nature of your appeal. Your
initial denial letter will also specify where to file an appeal.
Appeal a decision on eligibility for
coverage or enrollment status
Write to:
Walmar People Services
Attn: Internal Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Or fax to 888-715-4154
Or for COBRA appeals, write to:
WageWorks (COBRA Appeals)
P.O. Box 226591
Dallas, Texas 75222-6591
Designate an authorized
representative to submit appeals on
your behalf
Call the number on your plan ID card or call People Services at 800-421-1362
What you need to know about claims and appeals
• You have the right to appeal an adverse eligibility decision affecting your coverage.
• You have the right to appeal an adverse preauthorization decision regarding your requested benefits.
• You must submit claims for benefits directly to the third-party administrator or provider of the Plan.
• You have the right to appeal a benefit claim that has been partially or fully denied.
• You can appoint another party to appeal on your behalf by completing the Plan’s authorized representative form.
• After a final decision of an appeal of a medical, pharmacy, or Centers of Excellence claim is made, you may have the
right to request an independent external review of the decision if your claim involves medical judgment.
• Decisions regarding enrollment, eligibility status, and questions related to eligibility waiting periods are not eligible
for external review, but are eligible for voluntary review under the Plan. In addition, for the medical, dental, and vision
plans, appeals denied for nonmedical administrative reasons (e.g., because you exceeded the Plan’s visit limits) are
eligible for voluntary review under the Plan.
• You have the right to bring legal action if a claim is denied on appeal, but only after you have exhausted the Plan’s
claims and appeals procedures.
Claims and appeals
262
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Deadlines to file a claim or bring
legal action
Unless otherwise specified in the chapter describing the
applicable benefit, initial claims for benefits under the Plan
must be filed within 18 months from the date of service.
Since procedures for filing a claim or an appeal are different
for different benefit plans and third-party administrators,
be sure to review the relevant section of this chapter for
detailed information. You must complete the required
claims and appeals process described in this Claims and
appeals chapter before you may bring legal action or, for
certain medical, pharmacy, dental, or Centers of Excellence
claims, pursue external review. You may not file a lawsuit for
benefits if the initial claim or appeal is not made within the
time periods set forth in the claims procedures of the Plan.
You must file any lawsuit for benefits within 180 days after
the final decision on appeal (whether by the Plan or after
external review). You may not file suit after the end of that
180-day period. You are not required to request a voluntary
review by the Plan or an external review of the decision on
appeal before filing a lawsuit. If you request a voluntary
review or an external review of the decision on appeal,
where applicable, the time taken by the voluntary review
or external review is not counted against the 180 days you
have to file a lawsuit.
BENEFITS MAY NOT BE ASSIGNED
You may not assign your legal rights or rights to any
payments under this Plan. However, the Plan may choose
to remit payments directly to health care providers with
respect to covered services, but only as a convenience to
you and only if you authorize the Plan to do so. Health care
providers are not, and shall not be construed as, either
“participants” or “beneficiaries” under this Plan and have no
rights to receive benefits from the Plan or to pursue legal
causes of action on behalf of (or in place of) you or your
dependents under any circumstances.
Appealing an enrollment or eligibility
status decision
This section describes the appeal process that applies to
enrollment and eligibility only.
If you disagree with the Plan Administrator’s determination
regarding your enrollment or eligibility status, you have
365 days from your eligibility enrollment event to appeal
in writing to People Services, attention Internal Appeals,
atthe address in the Resources chart at the beginning of
this chapter.
Eligibility decisions regarding the transplant and weight
loss surgery benefit waiting period are determined under
the claims and appeals time frames for medical claims, as
described in the section that follows.
COBRA participants should send the appeal, in writing,
to WageWorks at the address the Resources chart at the
beginning of this chapter.
Your appeal will be handled within 60 days from the date it is
received (30 days for COBRA appeals), unless an extension
is required.
The 60-day period may be extended if it is determined that
an extension is necessary due to matters beyond the Plan’s
control. You will be notified prior to the end of the 60-day
period if an extension or additional information is required.
Appeals of enrollment or eligibility decisions are not eligible
for external review but are eligible for voluntary review.
Medical, pharmacy, Centers of
Excellence, dental, and vision
benefits claims process
This section describes the claims process that will be used
for the following benefits only:
• Medical, pharmacy, and Centers of Excellence benefits
except for HMO Plans and the eComm PPO Plan; see
HMO plan claims and appeals procedures and eComm
PPO Plan claims and appeals procedures later in
thischapter
• Dental benefits (through Delta Dental)
• Vision benefits (through VSP), and
• A rescission of coverage, which is a cancellation of
coverage that has a retroactive effect, except where
cancellation of coverage is due to failure to pay required
contributions or premiums in a timely manner.
If you choose to prenotify the third-party administrator of a
scheduled medical service before you receive treatment or
file a claim for benefits, and prenotification is not otherwise
required under the Plan, the third-party administrator’s
response is nonbinding on the Plan and not subject to
appeal. However, if the third-party administrator requires
you or your provider to preauthorize services (including
under the Centers of Excellence program and local plans),
and your request for prior authorization is denied, that
decision is subject to appeal.
Refer to the respective chapters in this Summary Plan
Description for information on filing your initial claim. Initial
claims will be determined by Plan Administrators as listed in
the chart on the following page.

Claims and appeals
263
CLAIMS AND APPEALS ADMINISTRATION: ROUTINE MEDICAL, PHARMACY, DENTAL, AND VISION
Medical
(For Centers of Excellence claims, see below)
Your third-pary administrator (seeyour plan ID card)
Including services perormed at a Centers of Excellence facility
but not covered under theCenters of Excellence program and
transplant claims not required to be perormed atMayo Clinic.
If you are a paricipant in one of the Mercy local plans, Mercywill
handle prior authorizations and HealthSCOPE Benefits will
process claims. If you are a paricipant in the UnityPoint Local Plan,
Precedence Inc. will handle prior authorizations and HealthSCOPE
Benefits will process claims.
Pharmacy OptumRx
Dental Delta Dental
Vision VSP
CENTERS OF EXCELLENCE
NOTE: If you are enrolled in a local plan, please call your health care advisor to be directed to the appropriate administrator.
Hear surgery Contigo Health (formerly Health Design Plus)
Cancer medical record review HealthSCOPE Benefits
Outpatient kidney dialysis or ESRD medical record review HealthSCOPE Benefits
Spine surgery Contigo Health (formerly Health Design Plus)
Hip and knee replacement Contigo Health (formerly Health Design Plus)
Transplant HealthSCOPE Benefits
Weight loss surgery Contigo Health (formerly Health Design Plus)
maximum function, or, in the opinion of a physician with
knowledge of your medical condition, would subject you to
severe pain that could not adequately be managed without
the care or treatment that is the subject of the claim.
If you are filing a claim after you have already received
services, your claim is a post-service claim. If your claim
arises when there is a reduction in ongoing care, your claim
is a concurrent care claim.
The chart on the following page shows deadlines for claims
determinations for these types of claims.
The time period in which your claim is determined depends
on the type of claim. The Plan requires prior authorization
for all Centers of Excellence services and certain other
services, as described in the Preauthorization section
of The medical plan chapter. For these benefits, you or
your provider must file a claim for approval before you
receive treatment, or your claim may not be paid. These
are called “pre-service claims.” If your pre-service claim is
urgent, your claim will be decided under the time frames
applicable to urgent care. A claim is urgent where making a
determination under the normal time frames could seriously
jeopardize your life or health or your ability to regain

Claims and appeals
264
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
CLAIMS PROCESS AND TIMING
Urgent claims
Any claim for medical care or treatment where
making a determination under the normal time
frames could seriously jeopardize your life
or health or your ability to regain maximum
function, or, in the opinion of a physician with
knowledge of your medical condition, would
subject you to severe pain that could not
adequately be managed without the care or
treatment that is the subject of the claim.
Notice will be sent as soon as possible, taking into account the medical
circumstances, and in no case later than 72 hours after receipt of the claim.
You may receive notice orally, in which case a written notice will be provided within
threedays of the oral notice. If your urgent claim is determined to be incomplete,
you will receive a notice to this effect within 24 hours of receipt of your claim, at
which pointyou will have 48 hours to provide additional information.
If you request an extension of urgent care benefits beyond an initially determined
period and make the request at least 24 hours prior to the expiration of the original
determination, you will be notified within 24 hours of receipt of the request.
Pre-service claims
A claim for services that have not yet been
rendered and for which the Plan requires
prior authorization.
If your pre-service claim is filed properly, a claims determination will be sent
within a reasonable period of time appropriate to the medical circumstances, but
no later than 15days from receipt of the claim.
If an extension is necessary due to matters beyond the Plan’s control, this time may
be extended 15 days. You will receive notice prior to the extension that indicates
the circumstances requiring the extension and the date by which the Plan expects
to render a determination. If the extension is necessary to request additional
information, the extension notice will describe the required information, and you
will be given at least 45 days to submit the information. The Plan then will make its
determination within 15 days from the date the Plan receives your information, or, if
earlier, the deadline to submit your information.
If your pre-service claim is improperly filed, you will be sent notification within
five days of receipt of the claim.
Post-service claims
A claim for services that already have been
rendered, or where the Plan does notrequire
prior authorization.
A notice will be sent within a reasonable time period, but not longer than 30 days
from receipt of the claim.
If an extension is necessary due to matters beyond the Plan’s control, this time may
be extended 15 days. You will receive notice prior to the extension that indicates
the circumstances requiring the extension and the date by which the Plan expects
to render a determination. If the extension is necessary to request additional
information, the extension notice will describe the required information, and you
will be given at least 45 days to submit the information. The Plan then will make its
determination within 15 days from the date the Plan receives your information, or, if
earlier, the deadline to submit your information.
Concurrent care claims
A claim related to a reduction of
ongoingservices.
You will be notified in advance of any decision to reduce or terminate coverage
for ongoing care so that you will be able to appeal the decision before the
coverage is reduced or terminated, unless such a reduction or termination is due
to a Plan amendment or termination of the Plan.
If your claim is denied, the denial will include the
followinginformation:
• The specific reasons for the denial
• Reference to Plan provisions on which the denial was based
• Information regarding time limits for appeal
• A description of any additional information necessary to
consider your claim and why such information is necessary
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination
• If your denial is based on medical necessity or similar
limitation, an explanation of this rule (or a statement that it
is available upon request), and
• Notice regarding your right to bring legal action following
a denial on appeal.
For medical, pharmacy, Centers of Excellence, and vision
benefits, the denial also will include:
• Information sufficient to identify the claim involved,
including, as applicable, the date of service, health care
provider, and claim amount
– Upon written request, the Plan will provide you with the
diagnosis and treatment codes (and their corresponding
meanings) associated with any denied claim or appeal.
• The denial code and its meaning
• A description of the Plan’s standard for denying the claim
• Information regarding available internal and external
appeals, including how to initiate an appeal, and
• The availability of any contact information for an
applicable office of health insurance consumer assistance
or ombudsman to assist participants with the internal and
external appeals process.

Claims and appeals
265
Internal appeal process
APPEALING A CLAIM THAT HAS BEEN FULLY
OR PARTIALLY DENIED: MEDICAL, CENTERS
OF EXCELLENCE, PHARMACY, DENTAL, OR
VISION CLAIMS
You may request an appeal of the decision. In order for your
appeal to be considered, it must:
• Be in writing
• Be sent to the correct address
• Be submitted within 365 days of the date of the initial
denial (for medical, Centers of Excellence, and dental
claims) or 180 days (for pharmacy and vision claims), and
• Contain any additional information/documentation you
would like considered.
If your appeal involves an urgent claim, please contact your
third-party administrator for information about how to file
your claim orally.
Aetna and OptumRx allow two levels of review. The second
appeal must be submitted within 60 days of the date of the
first appeal denial. All other third-party administrators have
one level of appeal.
Send your written request for review of the initial claim to
the third-party administrator that administers your claims,
as listed in the chart that follows.
MAILING ADDRESSES FOR APPEALS
MEDICAL SERVICES
(Including services perormed at a Centers of Excellence facility but not covered under the Centers of Excellence program)
Refer to your plan ID card for the name of your third-pary administrator.
Aetna Aetna
Attn: National Account CRT
P.O. Box 14463, Lexington, Kentucky 40512 855-548-2387
BlueAdvantage Administrators of Arkansas BlueAdvantage Administrators
P.O. Box 1460, Little Rock, Arkansas 72203-1460 866-823-3790
HealthSCOPE Benefits HealthSCOPE Benefits
Attn: Appeals
P.O. Box 2359, Little Rock, Arkansas 72203 800-804-1272
UnitedHealthcare UnitedHealthcare
National Appeals Service Center
P.O. Box 30575, Salt Lake City, Utah 84130-0575 888-285-9255
CENTERS OF EXCELLENCE SERVICES
Note that there is a special claims and appeals process for cerain Centers of Excellence benefits. See details later in this chapter.
Contigo Health (formerly Health Design Plus)
• Hear, spine, and hip and knee replacement surgeries
• Weight loss surgery
Contigo Health
Centers of Excellence: Walmar
Attn: Appeals Coordinator
1755 Georgetown, Hudson, Ohio 44236
HealthSCOPE Benefits, Inc.
• Hear and weight loss surgery at Emory Local Plan
• Weight loss surgery at Mercy Local Plan
• Cancer care
• Mayo Clinic transplant appeals
HealthSCOPE Benefits, Inc.
Attn: Appeals Coordinator
27 Corporate Hill Drive, Little Rock, Arkansas 72205
PHARMACY
OptumRx OptumRx
Attn: Appeals Coordinator
P.O. Box 25184. Santa Ana, California 92799
DENTAL
Delta Dental of Arkansas Delta Dental of Arkansas Appeals Committee
P.O. Box 15965, Little Rock, Arkansas 72231-5965
VISION
VSP VSP
Member Appeals
3333 Quality Drive, Rancho Cordova, California 95670

Claims and appeals
266
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Your appeal will be conducted without regard to your initial
determination, by someone other than the party who
decided your initial claim. No deference will be afforded to
the initial determination. You will have the opportunity to
submit written comments, documents, or other information
in support of your appeal. You have the right to request
copies, free of charge, of all documents, records, or
other information relevant to your claim. The third-party
administrator, on behalf of the Plan, will provide you with
any new or additional evidence or rationale considered
in connection with your claim sufficiently in advance of
the appeals determination date to give you a reasonable
opportunity to respond.
If your claim involves a medical judgment question, the
Plan will consult with an appropriately qualified health
care practitioner with training and experience in the field
of medicine involved. If a health care professional was
consulted for the initial determination, a different health
care professional will be consulted on appeal. Upon request,
the Plan will provide you with the identification of any
medical expert whose advice was obtained on behalf of the
Plan in connection with your appeal.
A final decision on appeal will be made within the time
periods specified in the chart that follows, depending on
the type of claim:
APPEAL PROCESS AND TIMING
Urgent claims You will be notified of the determination
as soon as possible, taking into account
the medical circumstances, but not later
than 72 hours after receipt of the claim
(36 hours for Aetna appeals).
Pre-service
claims
You will be notified of the determination
within a reasonable period of time,
taking into account the medical
circumstances, but no later than 30 days
from the date your request is received
(15 days for Aetna appeals).
Post-service
claims
You will be notified of the determination
within a reasonable period of time, but
no later than 60 days from the date your
request is received (30 days for Aetna
appeals).
If your claim is denied on appeal, you will receive a denial
notice that includes:
• The specific reasons for the denial
• Reference to Plan provisions on which the denial was based
• A statement describing your right to request copies, free
of charge, of all documents, records, or other information
relevant to your claim
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination
• If your denial is based on a medical necessity or similar
limitation, an explanation of this rule (or a statement that it
is available upon request)
• A description of any voluntary review procedures available,
and
• Notice regarding your right to bring legal action following
a denial on appeal.
For medical, pharmacy, and Centers of Excellence benefits,
the denial will also include:
• Information sufficient to identify the claim involved,
including the date of service, health care provider, and
claim amount (if applicable)
– Upon written request, the Plan will provide you with the
diagnosis and treatment codes (and their corresponding
meanings) associated with any denied claim or appeal.
• The denial code and its meaning
• A description of the Plan’s standard for denying the claim
• Information regarding available internal and external
appeals, including how to initiate an appeal, and
• The availability of any contact information for an applicable
office of health insurance consumer assistance or
ombudsman to assist participants with the internal and
external appeals process.
SPECIAL PROCEDURES FOR APPROVAL OF
A TRANSPLANT LOCATION OTHER THAN
MAYOCLINIC
As described in The medical plan chapter, all eligible
transplant recipients under the Centers of Excellence
program must undergo a pre-transplant evaluation at
Mayo Clinic. For these transplants, Mayo Clinic will make
a recommendation regarding transplant services at Mayo
Clinic. You may file a prior authorization request to receive
a transplant at a facility other than Mayo Clinic if there
is significant risk that travel to Mayo Clinic could result
in death. In addition, if Mayo Clinic recommends that a
transplant is not an appropriate medical course of treatment
or the patient is not an appropriate candidate, you may file a
prior authorization request with the Plan.
These requests will be considered by an Independent
Review Organization appointed by the Plan Administrator,
which may approve the request for transplant services at a
different facility.
The Independent Review Organization will not include
any employee of Walmart, Mayo Clinic, or a third-party
administrator of the Plan. The Independent Review
Organization will review any pertinent medical files
reviewed or generated by Mayo Clinic, as well as any
additional materials you submit, and will consider your
condition, alternative courses of treatment, scientific
Claims and appeals
267
studies and evidence, other medical professionals’ opinions,
the investigational or experimental nature of the proposed
procedures, and the potential benefit of the transplant.
Send your written request for review of preauthorization
transplant claims to:
Walmart People Services
Attn: Internal Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
800-421-1362
Or fax to 888-715-4154
If you are filing a claim for services at a facility other
than Mayo Clinic because there is significant risk that
travel to Mayo Clinic could result in death, you should
file as soon as possible. If you are filing a claim because
Mayo Clinic has determined that the transplant is not an
appropriate medical course of treatment, your claim must
be received by the Plan within 120 calendar days of Mayo
Clinic’s initial denial of transplant treatment. If the claim
is urgent, the Independent Review Organization will make
its determination within 72 hours after receipt of the claim
(otherwise, the Independent Review Organization will make
its determination within 15 days of receipt of the claim).
If the urgent claim is determined to be incomplete, you will
receive a notice within 24 hours of receipt of the claim, and
you will have 48 hours to provide additional information.
For non-urgent claims, the deadline to decide the claim
may be extended 15 days, and the Independent Review
Organization will send a notice explaining the extension.
If the extension is necessary to request additional
information, the extension notice will describe the required
information and you will be given at least 45 days to submit
the information. The Plan will make a determination within
15 days from the date the Plan receives your information, or,
if earlier, the deadline to submit your information.
You will have 180 days to request internal review of a denial
by the Independent Review Organization. The Independent
Review Organization will decide a request for urgent review
within 72 hours and non-urgent review within 30 days after
receipt. You then may appeal a denial of an internal review
appeal under the external appeal process described in this
section if your claim involves medical judgment.
Cornea and intestinal transplants, and any other transplant
service or claim where treatment already has been
rendered, will be decided under the regular medical claims
and appeals procedures for post-service claims outlined
earlier in this chapter.
SPECIAL PROCEDURES FOR APPROVAL OF
EXCEPTIONS TO PLAN COVERAGE TERMS
FOR SPINE SURGERY AND HIP AND KNEE
REPLACEMENT
As described in The medical plan chapter, spine surgery and
hip and knee replacements that are eligible to be performed
at a Centers of Excellence facility must be pre-approved
by the administrator of the program and performed at
a Centers of Excellence facility in order for Centers of
Excellence benefits to be payable. You may file a prior
authorization request (a “pre-service” claim) to receive
services at a non-Centers of Excellence facility and receive
in-network benefits if there is significant risk that travel
could result in paralysis or death, or where a Centers of
Excellence facility determines that the procedure is not the
appropriate medical course of treatment or that you are not
an appropriate candidate for surgery.
In addition, if you have already received surgical treatment
because your circumstances called for immediate surgery,
without which you would likely have suffered paralysis or
loss of life, you may request that the services you received
at a non-Centers of Excellence facility be covered as in-
network services (a “post-service” claim).
Pre-service claims will be considered by Contigo Health
(formerly Health Design Plus), the administrator of
the Centers of Excellence for spine surgery and hip
and knee replacement, which may approve coverage
at the in-network level for spine surgery or hip or knee
replacement at a non-Center of Excellence facility.
Send your written request for a pre-service exception to
the Plan’s coverage terms for spine surgery or hip or knee
replacement to:
Centers of Excellence: Walmart
Attn: Appeals Coordinator
1755 Georgetown
Hudson, Ohio 44236
Contigo Health (formerly Health Design Plus) will utilize an
Independent Review Organization which will not include
any associate of Walmart or the Centers of Excellence
facility for spine surgery or hip or knee replacement. The
Independent Review Organization will review any pertinent
medical files that were reviewed or generated by the
Centers of Excellence facility, as well as any additional
materials you submit, and will consider your condition,
alternative courses of treatment, scientific studies and
evidence, other medical professionals’ opinions, the
investigational or experimental nature of the proposed
procedures, and the potential benefit the surgical
procedure would have.
Post-service claims will be considered by an Independent
Review Organization appointed by the Plan Administrator,
which may approve coverage at the in-network level for the
spine surgery or hip or knee replacement at a non-Centers
of Excellence facility.
Claims and appeals
268
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The Independent Review Organization will not include any
associate of Walmart, the Centers of Excellence facility
for spine surgery or hip or knee replacement, or a third-
party administrator of the Plan. The Independent Review
Organization will review any pertinent medical files that
were reviewed or generated by the Centers of Excellence
facility, as well as any additional materials you submit,
and will consider your condition, alternative courses of
treatment, scientific studies and evidence, other medical
professionals’ opinions, the investigational or experimental
nature of the proposed procedures, and the potential
benefit the surgical procedure would have.
Send your written request for a post-service exception
to the Plan’s coverage terms for spine surgery or hip or
kneereplacement to:
Walmart People Services
Attn: Internal Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
800-421-1362
Or fax to 888-715-4154
If you are filing a pre-service claim for services at a
non-Centers of Excellence facility because there is
significant risk that travel could result in paralysis or
death, you should file as soon as possible. If you are filing a
pre-service claim because a Centers of Excellence facility
determined that the surgery is not an appropriate medical
course of treatment, your claim must be received by the
Plan within 120 calendar days of the initial denial by the
Centers of Excellence facility. If you are filing a post-service
claim because you already received surgery elsewhere,
as described above, you must file your claim within 120
calendar days of the date of service.
If a pre-service claim is urgent, Contigo Health (formerly
Health Design Plus) will make its determination within 72
hours after receipt of the claim (otherwise, Contigo Health
(formerly Health Design Plus) will make its determination
within 15 days of receipt of a pre-service claim). If the urgent
claim is determined to be incomplete, you will receive a
notice within 24 hours of receipt of the claim, and you
will have 48 hours to provide additional information. For
non-urgent claims, the deadline to decide the claim may
be extended 15 days, and Contigo Health (formerly Health
Design Plus) will send a notice explaining the extension. If the
extension is necessary to request additional information, the
extension notice will describe the required information and
you will be given at least 45 days to submit the information.
Contigo Health (formerly Health Design Plus) will make a
determination within 15 days from the date Contigo Health
(formerly Health Design Plus) receives your information, or,
if earlier, the deadline to submit your information.
If you file a post-service claim, the Independent Review
organization will make its determination within 30 days of
receipt of the post-service claim. For post-service claims,
the deadline to decide the claim may be extended 15 days,
and the Independent Review Organization will send a notice
explaining the extension. If the extension is necessary to
request additional information, the extension notice will
describe the required information and you will be given at
least 45 days to submit the information. The Independent
Review Organization will make a determination within 15
days from the date the Independent Review Organization
receives your information, or, if earlier, the deadline to
submit your information.
You will have 180 days to request that an Independent
Review Organization conduct an internal review of a
denial of a pre-service claim by the Independent Review
Organization designated by Contigo Health (formerly
Health Design Plus), or a post-service claim of an
Independent Review Organization. The Independent Review
Organization will decide a request for urgent review of a
pre-service claim within 72 hours after receipt, non-urgent
review of a pre-service claim within 30 days after receipt,
and review of a post-service claim within 60 days of receipt.
You then may appeal a denial of an internal review appeal
under the external appeal process described in this section
if your claim involves medical judgment.
REQUESTING TO WAIVE THE ONEYEAR
WAITING PERIOD FOR TRANSPLANT BENEFITS
If the treating physician certifies that, absent the transplant,
the individual’s death is imminent within 48 hours, the
otherwise applicable 12-month waiting period for transplant
benefits may be waived. To request this waiver, the claimant
must file a prior-authorization request.
Send your request and supporting documentation to
Walmart People Services:
By email: ghappeal@wal-mart.com
By fax: 888-715-4154
By mail: Walmart People Services
Attn: Internal Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Your request will be treated as an urgent or pre-service
claim. See the Appeal process and timing chart earlier in
this chapter for details on the time frames under which the
Plan Administrator will notify you of its determination in
response to your request.
REQUESTING A VOLUNTARY REVIEW OF
A DENIED APPEAL: ENROLLMENT OR
ELIGIBILITY STATUS DETERMINATIONS
INCLUDING COBRA
If you have additional information that was not in your
appeal, you may ask for a voluntary review of the decision
on your appeal within 180 days of the date on the appeal
Claims and appeals
269
denial letter. The same criteria and response times that
applied to your appeal are generally applied to this
voluntary level of review.
Send a written request for a voluntary appeal for enrollment
or eligibility status to:
Walmart People Services
Attn: Voluntary Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Or fax to 888-715-4154
See Deadlines to file a claim or bring legal action earlier in
this chapter regarding the deadline to bring legal action.
REQUESTING A VOLUNTARY REVIEW OF
AN APPEAL DENIED FOR ADMINISTRATIVE
REASONS: MEDICAL, DENTAL, AND
VISIONAPPEALS
You may request a voluntary review of the decision on your
appeal of a denied medical, dental, or vision benefit claim if
your appeal was denied for an administrative reason, such
as if you exceeded the number of allowed visits, rather than
for a medical judgment reason. You must file your request
within 180 days of the date on the appeal denial letter. The
same criteria and response times that applied to your appeal
are generally applied to this voluntary level of review.
Send a written request for a voluntary appeal for
administrative denial to:
Walmart People Services
Attn: Voluntary Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Or fax to 888-715-4154
External appeal process
for medical, pharmacy, or
CentersofExcellencebenefits
If your internal appeal for medical, pharmacy, or Centers
of Excellence benefits under the Plan is denied based on
medical judgment, you may have the right to further appeal
your claim in an independent external review process.
Your external appeal will be conducted by an independent
review organization not affiliated with the Plan. If this
independent review organization overturns the Plan’s
decision, the independent review organization’s decision will
be binding on the Plan. Your internal appeal denial notice
will include information about your right to file a request for
an external review as well as contact information. You must
file your request for external review within four months of
receiving your final internal appeal determination. Filing a
request for external review will not affect your ability to
bring a legal claim in court. When filing a request for external
review, you will be required to authorize the release of any
medical records that may be required to be reviewed for the
purpose of reaching a decision on the external review.
Send a written request for an external medical appeal to:
Walmart People Services
Attn: External Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
800-421-1362
Or fax to 888-715-4154
Send a written request for an external pharmacy appeal to:
OptumRx
Attn: Appeals Coordinator
P.O. Box 25184
Santa Ana, California 92799
Rights related to medical, pharmacy,
Centers of Excellence, dental, vision,
and shor-term disability benefits
THE PLAN’S RIGHT TO REQUEST
MEDICALRECORDS
The Plan has the right to request medical records for any
associate or covered individual.
THE PLAN’S RIGHT TO RECOVER
OVERPAYMENT
Payments are made in accordance with the provisions of
the Plan. If it is determined that payment was made for an
ineligible charge or that other insurance was considered
primary, the Plan has the right to recover the overpayment.
The Plan (or the third-party administrator) will try to
collect the overpayment from the party to whom the
payment was made. However, the Plan reserves the right
to seek overpayment from any participant, beneficiary, or
dependent. In addition, the Plan has the right to engage an
outside collection agency to recover overpayments on the
Plan’s behalf if the Plan’s collection effort is not successful.
The Plan may also bring a lawsuit to enforce its rights to
recover overpayments.
If the overpayment is made to a provider, the Plan (or any
third-party administrator) may reduce or deny benefits,
in the amount of the overpayment, for otherwise covered
services for current or future claims with the provider on
behalf of any participant, beneficiary, or dependent in the
Plan. If a provider to whom an overpayment was made has
patients who are participants in other health and welfare
plans administered by the third-party administrator, the
third-party administrator may reduce payments otherwise
owed to the provider from such other health plans by the
amount of the overpayment.
Claims and appeals
270
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
YOUR RIGHT TO RECOVER OVERPAYMENT
If you overpay your contributions or premiums for any
coverage under the Plan (except COBRA), the Plan will
refund excess contributions or premiums to you upon
request. In this circumstance, any refunds you receive may
be offset by any benefits paid during this period by the Plan
if you or a dependent was not eligible for such coverage.
THE PLAN’S RIGHT TO AUDIT
The Plan has the right to audit your claims, including
claims of medical providers. The Plan (or the third-party
administrator) may reduce or deny benefits for otherwise
covered services for all current or future claims with the
provider made on your behalf or a participant in any other
health and welfare plan administered by the third-party
administrator based on the results of an audit. The Plan may
also reduce or deny benefits for otherwise covered services
for all current or future claims you file.
THE PLAN’S RIGHT TO
SALARY/WAGE DEDUCTION
To the extent that the Plan may recover from you or your
dependents all or part of benefits previously paid, you
shall be deemed, by virtue of your enrollment in any health
and welfare coverage under the Plan, to have agreed that
the company may deduct such amounts from your wages
or salary and pay the same to the Plan until recovery is
complete. If you enroll for coverage under the Plan, you
will be treated by the Plan as if you had consented to the
applicable payroll deductions for such coverage. In addition,
if you fail to affirmatively enroll or reenroll during Annual
Enrollment, you will be treated by the Plan as if you had
consented to the automatic reenrollment described in the
Eligibility and enrollment chapter, including the applicable
payroll deductions.
The Plan’s subrogation and
reimbursement rights
If you or a covered dependent is injured or otherwise harmed
due to the conduct of another party, the Plan Administrator
has the right to recover payments it makes on your behalf
from you or any party responsible for compensating you or
your dependent for your illnesses or injuries. The legal term
for this right of recovery is “subrogation.” The Plan shall have
a first-priority lien for the full amount of the benefits that
are paid to you and/or your covered dependents and against
future benefits due under the Plan in the amount of any
claims paid, should you seek to recover any monies from the
third party that caused the injuries.
The Plan has the right to:
• Reduce or deny benefits otherwise payable by the Plan, and
• Recover or subrogate 100% of the benefits paid or to be
paid by the Plan for covered persons, to the extent of any
and all of the following payments:
– Any judgment, settlement, or payment made or to be
made because of an accident or malpractice (except
for malpractice that results in paraplegia/quadriplegia,
severe burns, total and permanent physical or mental
disability, or death), including other insurance
– Any auto or recreational vehicle insurance coverage or
benefits, including uninsured/underinsured motorist
coverage
– Business medical and/or liability insurance coverage or
payments, and
– Attorney fees.
The Plan’s lien exists at the time the Plan pays any benefits.
If a covered person files a petition for bankruptcy, the
covered person agrees that the Plan’s lien existed prior to
the creation of the bankruptcy estate.
Also note that:
• “Covered person” means any participant (as defined by
ERISA) or dependent of a participant who is entitled to
benefits under the Plan
• The Plan has first priority with respect to its right to
reduction, reimbursement, and subrogation
• The Plan has the right to recover interest on the amount
paid by the Plan because of the accident
• The Plan has the right to 100% reimbursement in a
lumpsum
• The Plan is not subject to any state laws or equitable
doctrine, including the common fund doctrine, which
would purport to require the Plan to reduce its recovery by
any portion of a covered person’s attorney’s fees and costs
• The Plan is not responsible for the covered person’s
attorney’s fees, expenses, or costs
• The right of reduction, reimbursement, and subrogation
is based on the Plan language in effect at the time of
judgment, payment, or settlement
• The Plan’s right to reduction, reimbursement, and
subrogation applies to any funds recovered from another
party, by or on behalf of the estate of any covered
person, and
• The Plan’s right to first priority shall not be reduced due to
the participant’s own negligence.
The Plan will not pursue reduction, reimbursement, or
subrogation where the injury or illness that is the basis of
the covered person’s recovery from any party results in:
• Paraplegia or quadriplegia
• Severe burns
• Total and permanent physical or mental disability, or
• Death.
Claims and appeals
271
The Plan Administrator has the authority, in its sole
discretion, to determine not to pursue the Plan’s rights
to reduction, reimbursement, or subrogation. For more
information, contact the Plan Administrator.
Whether a covered person has a “total and permanent
physical or mental disability” will be determined based on
criteria developed and applied by the Plan Administrator
in its sole discretion. One way of demonstrating total and
permanent physical or mental disability is for a covered
person to show that the covered person has qualified
for Social Security disability income benefits. The Plan
Administrator will consider claims for physical and mental
disability, even if the covered person does not qualify for
Social Security disability income benefits, under criteria
developed by the Plan Administrator.
Even in circumstances where the Plan is not prohibited from
seeking reduction, reimbursement, or subrogation based
on the exceptions described previously, the Plan’s right to
reduction, reimbursement, or subrogation will be limited to
no more than 50% of the total amount recovered by or on
behalf of the covered person from any party (which shall
not be reduced for the covered person’s attorney’s fees
or costs). The Plan requires all covered persons and their
representatives to cooperate to guarantee reimbursement
to the Plan from third-party benefits. Failure to comply
will entitle the Plan to withhold benefits due to you
under the Plan. You and your representatives must not do
anything to hinder reimbursement of overpayment to the
Plan after benefits have been accepted by you or your
representatives.
The Plan’s rights to reduction, reimbursement, and
subrogation apply regardless of any allocation or
designation of your settlement (e.g., pain and suffering
or medical benefits). The Plan’s rights apply regardless of
whether you have been made whole or fully compensated
for your injuries.
Additionally, the Plan has the right to file suit on your
behalf for the condition related to the expenses to recover
benefits paid or to be paid by the Plan.
Claims for benefits and right to
appeal reduction, reimbursement,
and subrogation decisions
The Plan’s decision to seek reduction, reimbursement, or
subrogation is a determination of benefits under the Plan and
may be appealed in accordance with the procedures below.
For purposes of the claims procedures specified below,
a “claim for benefits” means a request by a participant,
beneficiary, or dependent (“claimant”) to have the
benefits provided under the Plan not reduced through the
application of the Plan’s right to reduction, reimbursement,
or subrogation.
INITIAL CLAIM FOR BENEFITS
If the Plan decides to seek reduction, reimbursement,
or subrogation, the claimant will be notified of the Plan’s
decision in a written notice from the Plan or a party acting
on behalf of thePlan.
If you receive a notice that your benefit is subject to
reduction, reimbursement, or subrogation and you
believe that your case falls within one of the exceptions or
limitations to the Plan’s right to reduction, reimbursement,
or subrogation, you may file a claim for benefits with the
Plan. You may also designate an authorized representative
to submit claims for benefits or appeals on your behalf.
For an initial claim for benefits to be considered, it must:
• Be in writing
• Be sent to the correct address
• Be submitted within 12 months of the date of the notice
that a benefit is subject to reduction, reimbursement, or
subrogation
• Identify the exception or limitation to the Plan’s right to
reduction, reimbursement, or subrogation that you believe
applies to your case, and
• Include documentation that will assist the Plan in making
its decision (e.g., medical and hospital records, physician
letters).
Send a written request for review of the initial claim for
benefits to:
Walmart People Services
Attn: Subrogation Review
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Within a reasonable time, but no later than 30 days after
your initial claim for benefits is made, the Plan will provide
written notice of its decision. If the claim for benefits is
partially or fully denied, the notice will include the following
information:
• The specific reasons for the denial
• Reference to provisions of the Plan on which the denial
was based
• A description of any additional material or information
necessary to perfect your claim for benefits and an
explanation of why such material or information is
necessary
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making the Plan’s determination
• A description of the Plan’s appeal procedures and the time
limits for appeal, and
• Notice regarding your right to bring a court action
following a denial on appeal.
Claims and appeals
272
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The 30-day period may be extended for 15 days if it
is determined that an extension is necessary due to
matters beyond the Plan’s control. The Plan will notify
you prior to the end of the 30-day period if an extension
or additional information is required. If asked to provide
additional information, you will have 45 days from the
date notified to provide the information. The time to make
a determination will be suspended until you provide the
requested information (or the deadline to provide the
information, ifearlier).
IF A CLAIM RELATED TO A REDUCTION,
REIMBURSEMENT, OR SUBROGATION
DECISION ISFULLY OR PARTIALLY DENIED
The claimant may request an appeal of the decision. For
your appeal to be considered, it must:
• Be in writing
• Be sent to the correct address
• Be submitted within 180 days of the date of the initial
denial, and
• Contain any additional information/documentation you
would like considered.
Send a written request for an appeal to:
Walmart People Services
Attn: Internal Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Or fax to 888-715-4154
The appeal will be conducted without regard to the initial
determination by someone other than the party who
decided the initial claim for benefits. You have the right to
request copies, free of charge, of all documents, records,
or other information relevant to the claimant’s claim
for benefits. You also have the right to submit written
comments, documents, records, and other information,
which the Plan will take into account in making its decision
on appeal. In deciding any claim for benefits that is based
in whole or in part on a medical judgment, the Plan’s claims
fiduciary will consult with a health care professional who
has appropriate training and experience in the field of
medicine involved in the medical judgment. The health care
professional will be an individual who is neither an individual
who was consulted in connection with the Plan’s decision
on the initial claim for benefits, nor the subordinate of
the health care professional. If the advice of a health care
professional is obtained in deciding an appeal, the name
of the health care professional will be provided to you
upon request, regardless of whether the Plan relied on the
advice. The Plan must provide you written notice of the
Plan’s decision on review within 60 days following the Plan’s
receipt of your appeal.
If the claim for benefits is denied on appeal, the Plan will
provide a denial notice to you that includes:
• The specific reason(s) for the denial
• Specific reference to provisions of the Plan on which the
denial was based
• A statement describing your right to request copies, free
of charge, of all documents, records, or other information
relevant to your claim for benefits
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination
• A description of available voluntary review procedures, if
any, and
• Notice regarding your right to bring a court action
following a denial on appeal.
The only method by which you can request the Plan not
to reduce benefits is to file a claim for benefits. An initial
claim for benefits must be filed within 12 months from the
date of the notice. You must complete the required claims
and appeals process described in these claims procedures
before bringing legal action. You may not file a lawsuit
for benefits if your initial claim for benefits or appeal is
not made within the time periods set forth in these claims
procedures. You must file any lawsuit for benefits within 180
days after the decision on appeal. You may not file suit after
that 180-day period expires.
YOUR RESPONSIBILITY REGARDING RIGHT OF
REDUCTION AND/OR RECOVERY
To aid the Plan in its enforcement of its right of reduction,
recovery, reimbursement, and subrogation, you or your
designated representative must, at the Plan’s request and at
its discretion:
• Take actions necessary to enable the Plan to exercise its
rights of recovery
• Give information, or
• Sign documents so required by the Plan.
Failure to aid the Plan and to comply with such requests
may result in the Plan’s withholding or recovering benefits,
services, payments, or credits due or paid under the Plan.
The Plan can seek reimbursement of 100% of medical
benefits paid from any judgment, payment, or settlement
that is made on behalf of the covered person for whom the
medical benefits were paid. Reimbursement to the Plan
of 100% of these charges shall be made at the time the
payment is received by you or your representative.
Claims and appeals
273
HMO plan claims and
appealsprocedures
In some facilities, Walmart offers health insurance coverage
through a health maintenance organization (HMO) as
part of the Associates’ Health and Welfare Plan. If you
participate in an HMO, the HMO will provide a benefit
booklet that, together with this document, will serve as the
Summary Plan Description for the HMO coverage and will
describe its claims and appeals procedures. Contact your
HMO for additional information.
eComm PPO Plan claims and appeals
procedures
In some facilities, Walmart offers the eComm PPO Plan
as part of the Associates’ Health and Welfare Plan. If you
participate in the eComm PPO Plan, Aetna, the Plan’s
third-party administrator, will provide a booklet that,
together with this document, will serve as the Summary
Plan Description for the eComm PPO Plan coverage and
describe its claims and appeals procedures. Contact Aetna
for additional information.
Accident and critical illness
insurance claims process
Accident and critical illness insurance claims should
be submitted within 60 days of the occurrence or
commencement of any covered accident or critical illness to:
Allstate Benefits
Walmart Claims Unit
P.O. Box 414848
Jacksonville, Florida 32203-1488
You may also provide notice of claim as follows:
Online: allstatebenefits.com/mybenefits
By phone: 800-514-9525
By fax: 877-423-8804
Be sure to provide the following information for the
covered person:
• Name
• Walmart identification number (WIN), and
• Date the covered illness or accident occurred or
commenced.
You may request a claim form from Allstate Benefits or
visit One.Walmart.com or AllstateBenefits.com/Walmart
to obtain a copy. If you do not receive a claim form within
15 days of your request, you may send a notice of the claim
to Allstate Benefits by providing Allstate Benefits with a
statement of the nature and extent of the loss.
CRITICAL ILLNESS
When you submit a claim to Allstate Benefits and your claim
is denied, a notice will be sent within a reasonable time
period, but no later than 30 days after Allstate Benefits
receives the claim (filed in accordance with the Critical
Illness Certificate of Insurance). In special circumstances, an
extension of time may be needed to make a decision. In that
case, Allstate Benefits may take a 15-day extension. You will
receive written notice of the extension before the end of
the 30-day period.
If your claim is denied, your denial will consist of a written
explanation, which will include:
• The specific reasons for the denial
• Reference to provisions of the Plan on which the denial
was based
• Information regarding time limits for appeal
• A description of additional material or information, if any,
needed to perfect the claim and the reasons such material
or information is necessary
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination
• If your denial is based on medical necessity or similar
limitations, an explanation of this rule (or a statement that
it is available upon request), and
• Notice regarding your right to bring a court action
following a denial on appeal.
APPEALING A CRITICAL ILLNESS CLAIM THAT
HAS BEEN FULLY OR PARTIALLY DENIED
You may appeal any denial of a claim for benefits by filing a
written request with Allstate Benefits. In connection with an
appeal, you may request, free of charge, all documents that
are relevant (as defined by ERISA) to your claim. You may also
submit with your appeal any comments, documents, records,
and issues that you believe support your claim, even if you
have not previously submitted such documentation. You may
have representation throughout the review procedure.
An appeal must be filed with Allstate Benefits in accordance
with the claim filing procedures described in your denial
letter within 180 days of receipt of the written notice of
denial of a claim. Allstate Benefits will render a decision no
later than 60 days after receipt of your written appeal. The
decision after your appeal will be in writing and will include:
• The specific reasons for the denial
• Reference to provisions of the Plan on which the denial
was based
• A statement that you have the right to receive, upon
request and free of charge, reasonable access to, and
copies of, all documents, records, and other information
relevant to the claim for benefits
Claims and appeals
274
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination
• If your denial is based on medical necessity or similar
limitations, an explanation of this rule (or a statement that
is available upon request)
• A description of any voluntary review procedures offered
by the Plan and your right to obtain information about such
procedures, and
• A statement regarding your right to bring court action
following a denial on appeal.
You also will receive a notice if the claim on appeal is
approved. If your claim is denied, you have the right to bring
action in federal court in accordance with ERISA Section
502(a), but only after you have followed the Plan’s claims
and appeals procedures.
ACCIDENT INSURANCE
When you submit a claim to Allstate Benefits and your claim
is denied, a notice will be sent within a reasonable time
period, but no later than 90 days after Allstate Benefits
receives the claim (filed in accordance with the Accident
Certificate of Insurance). In special circumstances, an
extension of time may be needed to make a decision. In that
case, Allstate Benefits may take a 90-day extension. You will
receive written notice of the extension before the end of
the 90-day period.
If your claim is denied, your denial will consist of a written
explanation, which will include:
• The specific reasons for the denial
• Reference to provisions of the Plan on which the denial
was based
• Information regarding time limits for appeal
• A description of additional material or information, if any,
needed to perfect the claim and the reasons such material
or information is necessary
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination
• If your denial is based on medical necessity or similar
limitations, an explanation of this rule (or a statement that
it is available upon request), and
• Notice regarding your right to bring a court action
following a denial on appeal.
You also will receive a notice if the claim on appeal
isapproved.
APPEALING AN ACCIDENT CLAIM THAT HAS
BEEN FULLY OR PARTIALLY DENIED
You may appeal any denial of a claim for benefits by filing a
written request with Allstate Benefits. In connection with an
appeal, you may request, free of charge, all documents that
are relevant (as defined by ERISA) to your claim. You may also
submit with your appeal any comments, documents, records,
and issues that you believe support your claim, even if you
have not previously submitted such documentation. You may
have representation throughout the review procedure.
An appeal must be filed with Allstate Benefits in accordance
with the claim filing procedures described in your denial
letter within 60 days of receipt of the written notice of
denial of a claim. Allstate Benefits will render a decision
no later than 60 days after receipt of your written appeal.
In special circumstances, an extension of time may be
necessary to make a decision. In that case, Allstate Benefits
may take a 60-day extension. The decision after your appeal
will be in writing and will include:
• The specific reasons for the denial
• Reference to provisions of the Plan on which the denial
was based
• A statement that you have the right to receive, upon
request and free of charge, reasonable access to, and
copies of, all documents, records, and other information
relevant to the claim for benefits
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination
• If your denial is based on medical necessity or similar
limitations, an explanation of this rule (or a statement that
is available upon request)
• A description of any voluntary review procedures offered
by the Plan and your right to obtain information about such
procedures, and
• A statement regarding your right to bring court action
following a denial on appeal.
You also will receive a notice if the claim on appeal is
approved. If your claim is denied, you have the right to bring
action in federal court in accordance with ERISA Section
502(a), but only after you have followed the Plan’s claims
and appeals procedures.
See Deadlines to file a claim or bring legal action earlier in
this chapter regarding the deadlines to bring legal action.
Claims and appeals
275
Company-paid life insurance,
optional associate and
dependentlife insurance,
business travel accident insurance,
and AD&D claimsprocess
Claims for company-paid life, optional associate and
dependent life, business travel accident, and AD&D
insurance can be initiated by calling Prudential at
877-740-2116.
See the applicable insurance chapter for details on the
information required to file each type of claim. When you
submit a claim to Prudential and your claim is denied, a
notice will be sent within a reasonable time period, but not
longer than 90 days from receipt of the claim. If Prudential
determines that an extension is necessary due to matters
beyond Prudential’s control, this time may be extended for
an additional 90-day period. You will receive notice prior
to the extension that indicates the circumstances requiring
the extension and the date by which Prudential expects to
render a determination.
If your claim is in part or wholly denied, you will receive
notice of an adverse benefit determination that will:
• State the specific reasons for the adverse benefit
determination
• Reference the specific plan provisions on which the
determination is based
• Describe additional material or information, if any, needed
to perfect the claim and the reasons such material or
information is necessary, and
• Describe Prudential’s claims review procedures and
the time limits applicable to such procedures, including
a statement of your right to bring a civil action under
Section 502(a) of ERISA following an adverse benefit
determination on review.
APPEALING A PRUDENTIAL CLAIM THAT HAS
BEEN FULLY OR PARTIALLY DENIED
If your claim for benefits is denied and you would like to
appeal, you must send a written appeal to Prudential at the
address below within 180 days of the denial. Your appeal
should include any comments, documents, records, or any
other information you would like considered.
Send your written appeal to:
Prudential Insurance Companies of America
Group Life Claim Division
P.O. Box 8517
Philadelphia, Pennsylvania 19176
You will have the right to request copies, free of charge, of
all documents, records, or other information relevant to your
claim. Your appeal will be reviewed without regard to your
initial determination by someone other than the party who
decided your initial claim. Prudential will make a determination
on your appeal within 45 days of the receipt of your appeal
request. This period may be extended by up to an additional
45 days if Prudential determines that special circumstances
require an extension of time. You will be notified prior to the
end of the 45-day period if an extension is required. If you are
asked to provide additional information, you will have 45 days
from the date you are notified to provide the information, and
the time to make a determination will be suspended until you
provide the requested information (or the deadline to provide
the information, if earlier).
If your appeal is denied in whole or in part, you will receive
a written notification from Prudential of the denial that
willinclude:
• The specific reasons for the adverse determination
• Reference to the specific plan provisions on which the
determination was based
• A statement describing your right to request copies, free
of charge, of all documents, records, or other information
relevant to your claim
• A description of Prudential’s review procedures and
applicable time limits
• A statement that you have the right to obtain, upon
request and free of charge, a copy of internal rules or
guidelines relied upon in making this determination, and
• A statement describing any appeals procedures offered by
the Plan and your right to bring a civil suit under ERISA.
If a decision on appeal is not furnished to you within the
time frames mentioned earlier, the claim shall be deemed
denied on appeal.
VOLUNTARY SECOND APPEAL OF LIFE
INSURANCE, AD&D, OR BUSINESS TRAVEL
ACCIDENT CLAIMS
If your appeal is denied or if you do not receive a response
to your appeal within the appropriate time frame (in which
case the appeal is deemed to have been denied), you or your
representative may make a voluntary second appeal of your
denial in writing to Prudential. You must submit your second
appeal within 180 days of the receipt of the written notice
of denial or 180 days from the date such claim is deemed
denied. You may submit any written comments, documents,
records, and any other information relating to your claim. The
same criteria and response times that applied to your first
appeal are generally applied to this voluntary second appeal.
See Deadlines to file a claim or bring legal action earlier in
this chapter regarding the deadline to bring legal action.

Claims and appeals
276
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Claims and appeals process for
disability coverage claims
NOTE: This section describes the claims and appeals
process for the short-term disability plan for full-time
hourly associates (basic and enhanced), the long-term
disability plan, and the truck driver long-term disability
plan. For claims and appeals information for the short-term
disability plans for salaried associates and truck drivers,
refer to the respective chapters.
FILING A CLAIM
Notify Sedgwick to apply for a leave of absence and
file a short-term disability claim as soon as you know
you will be absent from work due to an illness, injury, or
pregnancy. You may do this by visiting One.Walmart.com >
mySedgwick, or by calling 800-492-5678.
Claims under the short-term disability plan for full-time
hourly associates for all states except California and Rhode
Island should be submitted to:
Sedgwick Claims Management Services, Inc.
P.O. Box 14748
Lexington, Kentucky 40512-4748
For associates in states or localities with legally mandated
plans, such as California, Rhode Island, and Washington,
you should submit your claim directly to the state or local
government. For information, including filing timelines, call
the appropriate phone number listed in the Resources chart
at the beginning of the Short-term disability for full-time
hourly associates chapter.
Claims under the long-term disability and truck driver long-
term disability plans should be submitted to:
Group Benefits Claims
Lincoln Financial Group
Group — Charlotte WM See page 332
P.O. Box 7216
London, Kentucky 40742-7216
FILING DEADLINES
Claims for short-term disability benefits in Hawaii, New
Jersey, and New York must be submitted to Sedgwick within
30 days of the date your disability begins. Sedgwick will
notify Lincoln of your disability claim.
For all other states (with the exception of California and
Rhode Island, as noted above), you must submit your short-
term disability claim to Sedgwick within 90 days of the date
your disability begins in order to assure consideration for
benefits. Claims filed later than 90 days after the date of
disability may be denied unless Sedgwick determines you
had good cause for filing late.
If you are on an approved short-term disability claim and
are enrolled in long-term disability (LTD) or truck driver
LTD, your claim will automatically be transitioned to Lincoln
for consideration.
Once a claim has been filed, a decision will be made in no
more than 45 days after receipt of your properly filed
claim. The time for decision may be extended for up to
two additional 30-day periods, provided that, prior to
any extension period, you are notified in writing that an
extension is necessary due to matters beyond control, those
matters are identified, and you are given the date by which
a decision will be rendered. If your claim is extended due
to your failure to submit information necessary to decide
your claim, the time for decision may be tolled from the
date on which the notification of the extension is sent to
you until the date your response is received. If your claim is
approved, the decision will contain information sufficient to
reasonably inform you of that decision.
Any adverse benefit determination will be in writing and
willinclude:
• Specific reasons for the decision
• Specific reference to the Plan provisions on which the
decision is based
• A discussion of the decision, including an explanation of
the basis for disagreeing with or not following:
– The views presented by you to the Plan of health care
professionals treating you and vocational professionals
evaluated by you
– The views of medical or vocational expers whose
advice was obtained on behalf of the Plan in connection
with your adverse benefit determination, regardless
of whether the advice was relied upon in making the
benefit determination, and
– A disability determination regarding you made by the
Social Security Administration and presented by you to
the Plan.
• Either the specific internal rules, guidelines, protocols,
standards, or other similar criteria of the Plan relied upon
in making the adverse determination or, alternatively, a
statement that such rules, guidelines, protocols, standards,
or other similar criteria of the Plan do not exist
• If the adverse benefit determination is based on a medical
necessity or experimental treatment or similar exclusion
or limit, either an explanation of the scientific or clinical
judgment for the determination, applying the terms of
the Plan to your medical circumstances, or a statement
that such explanation will be provided free of charge
upon request
• A description of any additional material or information
necessary for you to perfect the claim and an explanation
of why such material or information is necessary
Claims and appeals
277
• A statement that you are entitled to receive, upon request
and free of charge, reasonable access to, and copies of,
all documents, records, and other information relevant to
your claim for benefits
• A description of the review procedures and time limits
applicable to such procedures, and
• A statement that you have the right to bring a civil action
under Section 502(a) of ERISA after you appeal the
decision if you receive a written denial on appeal.
APPEALING A DISABILITY CLAIM THAT HAS
BEEN FULLY OR PARTIALLY DENIED
If your claim for disability benefits is denied and you
wouldlike to appeal, you must submit a written or oral
appeal to Sedgwick or Lincoln (as applicable) within 180days
of the denial.
For associates in states or localities with legally mandated
plans, such as California, Rhode Island, and Washington,
you should submit your appeal directly to the state or local
government. For information, including filing timelines, call
the appropriate phone number listed in the Resources chart
at the beginning of the Short-term disability for full-time
hourly associates chapter.
Your appeal will be conducted without regard to your
initial determination by someone other than the party
who decided your initial claim or a subordinate of the
individual who decided your initial claim. No deference will
be afforded to the initial determination. You will have the
opportunity to submit written comments, documents, or
other information in support of your appeal. You have the
right to request copies, free of charge, of all documents,
records, or other information relevant to your claim. The
third-party administrator, on behalf of the Plan, will provide
you with any new or additional evidence or rationale
considered in connection with your claim sufficiently in
advance of the appeals determination date to give you a
reasonable opportunity to respond.
If your claim involves a medical judgment question, the
Plan will consult with an appropriately qualified health
care practitioner with training and experience in the field
of medicine involved. If a health care professional was
consulted for the initial determination, a different health
care professional will be consulted on appeal. Upon request,
the Plan will provide you with the identification of any
medical expert whose advice was obtained on behalf of the
Plan in connection with your appeal.
Sedgwick or Lincoln (as applicable) will make a
determination on your appeal within 45 days of the receipt
of your appeal request. This period may be extended by
up to an additional 45 days if it is determined that special
circumstances require an extension of time. You will
be notified prior to the end of the 45-day period if an
extension is required. If you are asked to provide additional
information, you will have 45 days from the date you are
notified to provide the information, and the time to make
a determination will be suspended until you provide the
requested information (or the deadline to provide the
information, if earlier).
If your appeal is denied in whole or in part, you will receive a
written notification of the denial that will include:
• The specific reasons for the adverse determination
• Reference to the specific Plan provisions on which the
determination was based
• A discussion of the decision, including an explanation of
the basis for disagreeing with or not following:
– The views presented by you to the Plan of health care
professionals treating you and vocational professionals
who evaluated you
– The views of medical or vocational expers whose
advice was obtained on behalf of the Plan in connection
with your adverse benefit determination, regardless
of whether the advice was relied upon in making the
benefit determination, and
– A disability determination regarding you made by the
Social Security Administration and presented by you to
thePlan.
• Either the specific internal rules, guidelines, protocols,
standards, or other similar criteria of the Plan relied upon
in making the adverse determination or, alternatively, a
statement that such rules, guidelines, protocols, standards,
or other similar criteria of the Plan do not exist
• If the adverse benefit determination is based on a medical
necessity or experimental treatment or similar exclusion
or limit, either an explanation of the scientific or clinical
judgment for the determination, applying the terms of
the Plan to your medical circumstances, or a statement
that such explanation will be provided free of charge
uponrequest
• A statement that you are entitled to receive, upon request
and free of charge, reasonable access to, and copies of,
all documents, records, and other information relevant to
your claim for benefits, and
• A statement that you have the right to bring a civil action
under Section 502(a) of ERISA (including a description of
any contractual limitation period that applies and the date
on which the contractual limitation period expires).
See Deadlines to file a claim or bring legal action earlier in
this chapter regarding the deadline to bring legal action.

Claims and appeals
278
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Appeals under the short-term disability plan for full-time
hourly associates for all states except California, Hawaii,
New Jersey, New York, and Rhode Island should be
submitted to:
Walmart Disability and Leave Service Center at Sedgwick
National Appeals Unit
P.O. Box 14028
Lexington, Kentucky 40512
For salaried associates and truck drivers, see the
Salariedshort-term disability plan chapter or the Truck
driver short-term disability plan chapter, as appropriate, for
detailed information on the appeals process for those plans.
Appeals for short-term disability benefits in Hawaii, New
Jersey, and New York, and long-term disability and truck
driver long-term disability appeals, should be sent to:
Group Benefits Claims Appeal Unit
Lincoln Financial Group
Group — Charlotte WM See page 332
P.O. Box 7216
London, Kentucky 40742-7216
VOLUNTARY SECOND APPEAL OF A CLAIM
FOR BENEFITS UNDER THE FULLTIME
HOURLY SHORTTERM DISABILITYPLAN
If you are a full-time hourly associate whose short-term
disability coverage is administered through Sedgwick and
your appeal is denied, you may make a voluntary second
appeal of your denial orally or in writing to Sedgwick. You
must submit your second appeal within 180 days of the
receipt of the written notice of denial. You may submit
any written comments, documents, records, and any
other information relating to your claim. The same criteria
and response times that applied to your first appeal, as
described earlier, are generally applied to this voluntary
second appeal.
Voluntary second appeals for short-term disability benefits
should be sent to:
Walmart Disability and Leave Service Center at Sedgwick
National Appeals Unit
P.O. Box 14748
Lexington, Kentucky 40512-4748
See Deadlines to file a claim or bring legal action earlier in
this chapter regarding the deadlines to bring legal action.
Resources for Living benefits
You do not have to file a claim or appeal for Resources for
Living benefits. You may access the Resources for Living
website or call Resources for Living at 800-825-3555 at
any time.
However, if you have a question about your benefits, or
disagree with the benefits provided, you may contact
People Services or file a claim or appeal by writing to the
following address:
Walmart People Services
Attn: Internal Appeals
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Any claims or appeals will be determined under the time
frames and requirements applicable to medical benefits.
International business travel
medicalinsurance
Claim forms are generally not required for GeoBlue
services. However, if you have a question about your
benefits or disagree with the benefits provided, you may
contact GeoBlue or file a claim. To submit a claim via email
or fax, download a claim form and view detailed instructions
in the Member Hub at geo-blue.com. Submit your claim by
email to claims@geo-blue.com or by fax to 610-482-9623.
You may also submit claims by post. Download a claim form
from the Member Hub at geo-blue.com and send your
completed form to:
GeoBlue
Claims Department
P.O. Box 1748
Southeastern, Pennsylvania 19399-1748
Any claims and appeals will be determined under the time
frames and requirements set out in the GeoBlue policy.
Contact GeoBlue at any time by calling 888-412-6403.
Outside the U.S. call collect: 610-254-5830.
Claims and appeals
279

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Associates’ Health and Welfare Plan 282
Plan amendment or termination 282
Your rights under ERISA 282
HIPAA notice of privacy practices 284
Medicare and your prescription drugcoverage 287
Premium assistance under Medicaid and the Children’s Health Insurance Program (CHIP) 289
Valued Plan Paricipant 292
Legal information

Legal information
281
Legal information
This document includes the Summary Plan Description (SPD) for the Associates’ Health and Welfare
Plan (the Plan). The SPD describes benefits offered to you by Walmar Inc. and the steps you need
to follow to take full advantage of the Plan. The previous chapters describe the most imporant
features of the Plan; in this chapter you’ll find imporant administrative information and facts about
your rights as a paricipant in the Plan.
RESOURCES
Find What You Need Online Other Resources
Contact the Plan Administrator Write to:
Walmar
Plan Administrator
Associates’ Health and Welfare Plan
508 SW 8th Street
Bentonville, Arkansas 72716-3500
Call 479-621-2058
Answers to questions about the
HIPAA Privacy Notice
Email your question to
AHWPrivacy@walmar.com
Call People Services at
800-421-1362
Answers to questions about
Medicare Par D
Visit medicare.gov 800-MEDICARE (800-633-4227)
TTY users should call 877-486-2048
Answers to your questions
about Medicaid/CHIP
Visit insurekidsnow.gov 877-KIDSNOW (877-543-7669)
What you need to know about the legal information for
the Associates’ Health and Welfare Plan
• As a participant in the Plan, you are entitled to certain rights and protections under the Employee Retirement Income
Security Act of 1974 (ERISA), as amended.
• The HIPAA privacy notice in this chapter describes how medical information about you may be used and disclosed and how
you can get access to this information.
• The Medicare and your prescription drug coverage section in this chapter explains the options you have under Medicare
prescription drug coverage, and can help you decide whether or not you want to enroll.
• The Medicaid/Children’s Health Insurance Program (CHIP) notice explains special enrollment and premium assistance rights
for individuals eligible for these programs.
Legal information
282
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Associates’ Health and Welfare Plan
The Plan is an employer-sponsored health and welfare
employee benefit plan governed by ERISA.
The terms and conditions of the Plan are set forth in this
SPD, in the Associates’ Health and Welfare Plan Wrap
Document (Wrap Document), and in the insurance policies
and other welfare program documents incorporated
into the Wrap Document (such as the Annual Enrollment
materials you are provided and the Summaries of Benefits
and Coverage). The Wrap Document, together with this
book and the other incorporated documents, constitutes
the written instrument under which the Plan is established
and maintained.
Plan Year: January 1 through December 31
Plan Number: 501
Type of Plan: Welfare, including medical, dental, vision,
short-term disability, long-term disability, business travel
accident insurance, accidental death and dismemberment
(AD&D) insurance, company-paid life insurance, optional
associate and dependent life insurance, accident
insurance, critical illness insurance, and Resources for
Living (the associate assistance program).
Type of Administration: The Plan Administrator (or its
delegates, including third-party administrators deciding
claims and appeals) has complete discretion to interpret
and construe the provisions of the Plan, make findings of
fact, correct errors, and supply omissions. All decisions and
interpretations of the Plan Administrator (or a delegate)
made pursuant to the Plan shall be final, conclusive and
binding on all persons, and may not be overturned unless
found by a court to be arbitrary and capricious. Benefits
will be paid only if the Plan Administrator (or a delegate)
determines in its sole discretion that the claimant is
entitled to them.
Plan Sponsor:
Walmart Inc.
702 SW 8th Street
Bentonville, Arkansas 72716-0295
Plan Administrator/Named Fiduciary:
Senior Vice President, Global Benefits Division,
Walmart Inc.
Associates’ Health and Welfare Plan
508 SW 8th Street
Bentonville, Arkansas 72716-3500
479-621-2058
Agent for Service of Legal Process:
Corporation Trust Company
1209 Orange Street Corporation Trust Center
Wilmington, Delaware 19801
Legal process may also be served on the Plan Administrator
or Trustee.
Plan Sponsor’s EIN: 71-0415188
FUNDING FOR THE PLAN
Walmart Inc. may fund Plan benefits out of its general
assets or through contributions made to the Walmart Inc.
Associates’ Health and Welfare Trust. Contributions also
may be required by employees, in an amount determined
by Walmart Inc. in its sole discretion. All assets of the Plan,
including associate contributions and any dividends or
earnings of the Plan, shall be available to pay any benefits
provided under the Plan or expenses of the Plan, including
insurance premiums.
Plan Trustee:
J. P. Morgan
4 New York Plaza, 15th Floor
New York, New York 10004-2413
Plan amendment or termination
Walmart reserves the right within its sole discretion to
amend or terminate any benefit or provision under the Plan,
at any time and for any reason, as it relates to any current,
past, or future participant or beneficiary under the Plan.
Neither the Plan nor the benefits described in this book can
be orally amended. All oral statements and representations
shall be without force or effect, even if such statements
and representations are made by the Plan Administrator or
by a management associate of the company. Only written
statements by the Plan Administrator shall bind the Plan.
Your rights under ERISA
As a participant in the Plan, you are entitled to certain rights
and protections under the Employee Retirement Income
Security Act of 1974 (ERISA), as amended. ERISA provides
that all Plan participants shall be entitled to:
RECEIVE INFORMATION ABOUT YOUR PLAN
AND BENEFITS
You have the right to:
• Examine, without charge, at the Plan Administrator’s
office and at other specified facilities, such as worksites
and union halls, all documents governing the Plan,
including insurance contracts and collective bargaining
agreements, and a copy of the latest annual report (Form
5500 Series) filed by the Plan with the U.S. Department of
Labor and available at the Public Disclosure Room of the
Employee Benefits Security Administration.
Legal information
283
• Obtain, upon written request to the Plan Administrator,
copies of documents governing the operation of the
Plan, including insurance contracts and collective
bargaining agreements, and copies of the latest annual
report (Form 5500 Series) and updated Summary Plan
Description. The Administrator may make a reasonable
charge for the copies.
• Receive a summary of the Plan’s annual financial report.
The Plan Administrator is required by law to furnish each
participant with a copy of this annual report.
CONTINUE GROUP HEALTH PLAN COVERAGE
You have the right to continue health care coverage for
yourself, your spouse, or your dependents if there is a loss
of coverage under the Plan as a result of a qualifying event.
You or your dependents may have to pay for such coverage.
Review this SPD and the documents governing the Plan on
the rules governing your COBRA continuation coverage
rights. (See the COBRA chapter for more information.)
You should be provided a certificate of creditable coverage,
free of charge, from the Plan or health insurance issuer
when you lose coverage under the Plan, when you become
entitled to elect COBRA continuation coverage, or when
your COBRA continuation coverage ceases, if you request it
before losing coverage or if you request it up to 24 months
after losing coverage.
Note that the Associates’ Medical Plan does not have a pre-
existing condition exclusion.
PRUDENT ACTIONS BY PLAN FIDUCIARIES
In addition to creating rights for Plan participants, ERISA
imposes duties upon the people who are responsible for
the operation of the Plan. The people who operate the
Plan, called “fiduciaries” of the Plan, have a duty to do
so prudently and in the interest of you and other Plan
participants and beneficiaries. No one, including your
employer, your union, or any other person, can fire you or
otherwise discriminate against you in any way to prevent
you from obtaining benefits or exercising your rights
under ERISA.
If your claim for a benefit is denied or ignored, in whole
or in part, you have the right to know why this was done,
to obtain copies of documents relating to the decision
without charge, and to appeal any denial, all within certain
time schedules.
Under ERISA, there are steps you can take to enforce the
above rights. For instance:
• If you request materials from the Plan and do not
receive them within 30 days, you can file suit in a federal
court. In such a case, the court may require the Plan
Administrator to provide the materials and pay you up
to $110 a day until you receive the materials, unless the
materials were not sent because of reasons beyond the
control of the Administrator.
• If you have a claim for benefits that is denied or ignored, in
whole or in part, you can file suit in a state or federal court.
Generally, you must complete the appeals process before
filing a lawsuit against the Plan. However, you should
consult with your own legal counsel in determining when it
is proper to file a lawsuit against the Plan.
• If you disagree with the Plan’s decision or lack thereof
concerning the qualified status of a domestic relations
order or a medical child support order, you can file suit in a
federal court.
• If it should happen that Plan fiduciaries misuse the Plan’s
money, or if you are discriminated against for asserting
your rights, you can seek assistance from the U.S.
Department of Labor, or you can file suit in a federal court.
The court will decide who should pay court costs and legal
fees. If you are successful, the court may order the person
you have sued to pay these costs and fees. If you lose,
the court may order you to pay these costs and fees; for
example, if it finds your claim is frivolous.
ASSISTANCE WITH YOUR QUESTIONS
If you have any questions about the Plan, you should contact
the Plan Administrator. If you have any questions about
this statement or about your rights under ERISA, or if you
need assistance in obtaining documents from the Plan
Administrator, you should contact the nearest office of the
Employee Benefits Security Administration, U.S. Department
of Labor, listed in your telephone directory or the:
Division of Technical Assistance and Inquiries
Employee Benefits Security Administration
U. S. Department of Labor
200 Constitution Avenue NW
Washington, DC 20210
You can also obtain certain publications about your rights
under ERISA by calling the Employee Benefits Security
Administration publications hotline at 866-444-3272 or by
going to dol.gov/ebsa.

Legal information
284
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
HIPAA notice of privacy practices
This notice was updated August 1, 2019
THIS NOTICE APPLIES TO THE ASSOCIATES’
MEDICALPLAN (AMP), DENTAL PLAN, AND
RESOURCES FOR LIVING (RFL), REFERRED TO
COLLECTIVELY AS THE “PLANS”
THIS NOTICE DESCRIBES HOW MEDICAL
INFORMATION ABOUT YOU MAY BE USED
AND DISCLOSED AND HOW YOU CAN GET
ACCESS TO THIS INFORMATION. PLEASE
REVIEW IT CAREFULLY. You have certain
rights under the Health Insurance Portability
and Accountability Act (HIPAA). HIPAA
governs when and how your medical health
information held by the AMP, dental plan, and
RFL may be used and disclosed and how you
can get access to this information. Please share
a copy of this notice with your family members
who are covered under the AMP, dental plan,
and RFL.
THE PLANS’ COMMITMENT TO YOUR PRIVACY
References to “we” and “us” throughout this notice mean the
Plans. Walmart also provides benefits for some associates
through a Health Maintenance Organization (HMO), a
fully insured PPO Plan and a fully insured international
business travel medical plan. For these benefit options, the
insurer of the HMO or PPO Plan or international business
travel medical plan is responsible to protect your health
information under the HIPAA rules, including providing you
with its own notice of privacy practices.
The Plans are dedicated to maintaining the privacy of your
health information for as long as the Plans hold your health
information or for fifty years after your death. In operating
the Plans, we create records regarding you and the benefits
we provide to you. This notice will tell you about the ways
in which we may use and disclose health information about
you. We will also describe your rights and certain obligations
we have regarding the use and disclosure of health
information. We are required by law to:
• Maintain the privacy of your health information, also
known as Protected Health Information (PHI)
• Provide you with this notice
• Comply with this notice, and
• Notify you if there is a breach of your unsecured PHI.
The Plans reserve the right to change our privacy practices
and to make any such change applicable to the PHI we
obtained about you before the change. If there is a material
revision to this notice, the new notice will be distributed to
you. You may obtain a paper copy of the current notice by
contacting the Plans using the contact information listed
at the end of this notice. The most current notice is also
available on One.Walmart.com.
HOW THE AMP, DENTAL PLAN, AND RFL MAY
USE AND DISCLOSE YOUR PHI
The law permits us to use and disclose your protected
health information (PHI) for certain purposes without your
permission or authorization. The following gives examples of
each of these circumstances:
1. For Treatment. We may use or disclose your PHI for
purposes of treatment. For example, we may disclose
your PHI to physicians, nurses, and other professionals
who are involved in your care.
2. For Payment. We may use or disclose your PHI to provide
payment for the treatment you receive under the Plans.
For example, we may contact your health care provider
to certify that you have received treatment (and for what
range of benefits), and we may request details regarding
your treatment to determine if your benefits will cover,
or pay for, your treatment. We also may use and disclose
your PHI to obtain payment from third parties that may
be responsible for such costs, such as family members or
other insurance companies.
3. For Health Care Operations. We may use or disclose
your PHI for our health care operations. For example,
our claims administrators in some states or the Plans may
use your PHI to conduct cost-management and planning
activities. Any information which we use or disclose for
underwriting purposes will not include any of your PHI
which is genetic information.
4. To the Plans’ Sponsor. The Plans may use or disclose your
PHI to Walmart, the Plan Sponsor. The Plans’ Sponsor
will only use your PHI as necessary to administer the
Plans. The law only permits the Plans to disclose your PHI
to Walmart, in its role as the Plans’ Sponsor, if Walmart
certifies, among other things, that it will only use or
disclose your PHI as permitted by the Plan, will restrict
access to your PHI to those Walmart employees whose
job it is to administer the Plan, and will not use PHI for
any employment-related actions.
5. For Health-Related Programs and Services. The Plans
may contact you about information regarding treatment
alternatives or other health-related benefits and services
that may be of interest to you.
6. To Individuals Involved in Your Care or Payment for Your
Care. The Plans may disclose your PHI to a third party
involved in your health care including a family member,
close friend, or a person you identified to the Plan as
involved in your health care, provided that you agree
to this disclosure. If you are not present or available to
Legal information
285
agree or disagree to disclose your PHI to a third person
requesting the PHI, then the Plans may use professional
judgment to determine if the disclosure of PHI is in your
best interests. If it is determined that a disclosure of PHI
is then in your best interest, the Plans may disclose the
minimum amount of PHI necessary to meet the need.
Additionally, you have the right to request that the Plans
limit any disclosure of PHI to specific individuals involved
in your health care.
OTHER USES OR DISCLOSURES OF YOUR PHI
WITHOUT AN AUTHORIZATION
The law allows us to disclose your PHI in the following
circumstances without your permission or authorization:
1. When Required by Law. The Plans will use and disclose
your PHI when we are required to do so by federal, state,
or local law.
2. For Public Health Risks. The Plans may disclose your
PHI for public health activities, such as those aimed at
preventing or controlling disease, preventing injury,
reporting reactions to medications or problems with
products, and reporting the abuse or neglect of children,
elders, and dependent adults.
3. For Health Oversight Activities. The Plans may disclose
your PHI to a health oversight agency for activities
authorized by law. These oversight activities, which are
necessary for the government to monitor the health
care system, include investigations, inspections, audits,
and licensure.
4. For Lawsuits and Disputes. The Plans may use or disclose
your PHI in response to a court or administrative order
if you are involved in a lawsuit or similar proceeding. We
also may disclose your PHI in response to a discovery
request, subpoena, or other lawful process by another
party involved in the dispute, but only if we receive
satisfactory assurances from the party seeking the
information that reasonable efforts have been made to
inform you of the request and given you the opportunity
to raise an objection to the court or obtain an order
protecting the information the party has requested.
5. To Law Enforcement. The Plans may release your PHI if
asked to do so by a law enforcement official in certain
circumstances, including but not limited to the following:
– Regarding a crime victim in cerain situations, if we
are unable to obtain the person’s agreement
– Concerning a death we believe might have resulted
from criminal conduct
– Regarding criminal conduct at our offices
– In response to a warrant, summons, cour order,
subpoena, or similar legal process
– To identify/locate a suspect, material witness, fugitive,
or missing person
– In an emergency, to repor a crime (including the
location or victim(s) of the crime or the description,
identity, or location of the person who committed the
crime), and
– In cases where a law enforcement agency has
requested PHI for purposes of identifying or locating
an individual, HIPAA permits that if cerain specific
situations are met, the Plans must disclose to the
law enforcement agency limited information such as
name, address, Social Security number, ABO blood
type, type of injury, date and time of treatment or
death, and distinguishing physical characteristics.
6. To Avert a Serious Threat to Health or Safety. The Plans
may use or disclose your PHI when necessary to reduce
or prevent a serious threat to your health and safety
or the health and safety of another individual or the
public. Under these circumstances, we will only make
disclosures to a person or organization able to help
prevent the threat.
7. For Military Functions. The Plans may use or disclose
your PHI if you are a member of the U.S. or foreign
military forces (including veterans), and if required to
assure the proper execution of a military mission if the
appropriate military authority has published the required
information in the Federal Register.
8. For National Security. The Plans may disclose your PHI
to federal officials for intelligence and national security
activities authorized by law. We also may disclose
your PHI to federal officials in order to protect the
president, other officials or foreign heads of state or to
conduct investigations.
9. Inmates. The Plans may disclose your health information
to correctional institutions or law enforcement officials
if you are an inmate or under the custody of a law
enforcement official. Disclosure for these purposes
would be necessary: for the institution to provide health
care services to you; for the safety and security of the
institution; and/or to protect your health and safety or
the health and safety of other individuals.
10. To Workers’ Compensation Programs. The Plans
may release your health information for workers’
compensation and similar programs.
11. For Services Related to Death. The Plans may disclose
your PHI upon your death to a coroner, funeral director,
or to tissue or organ donation services, as necessary to
permit them to perform their functions.
12. Research. HIPAA permits the Plans to disclose PHI for
government-approved research purposes. It is the policy
of the Plans not to disclose PHI for research purposes
and will not disclose your PHI for such purposes unless
the PHI is required to be disclosed under law.
13. Psychotherapy Notes. An authorization is always required
to use or disclose psychotherapy notes to a third person
unless the use or disclosure is permitted under HIPAA
Legal information
286
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
regulations. Permissible uses or disclosures include: use
for treatment, payment, or health care operations; use
by the originator of the notes for treatment; use by the
Plans to defend themselves in a lawsuit that you initiate;
when required by the Secretary of the Department
of Health and Human Services; when such disclosure
is required by law; for health oversight activities as
permitted under the regulations; disclosure to a person
who can reasonably prevent serious harm to an individual
or the public; and disclosure to a medical examiner
or coroner for the purpose of identifying a deceased
person, determining cause of death, or such other
purposes permitted by law. While the regulations permit
covered entities to use and disclose psychotherapy notes
for purposes of training health professionals or students,
the Plans do not engage in such training exercises and
cannot disclose the information for these purposes.
14. Victims of Abuse, Neglect, or Domestic Violence. The
Plans may disclose your PHI if there is reasonable belief
that you are a victim of abuse, neglect, or domestic
violence. Such disclosure is permitted under HIPAA only
if required by law or with your permission or to the extent
the disclosure is expressly authorized by statute and only if,
in the Plan’s best judgment, the disclosure is necessary to
prevent serious harm to you or other potential victims.
15. Health Oversight Activities and Joint Investigations. The
Plans must disclose PHI requested of health oversight
agencies for purposes of legally authorized audits,
investigations including joint investigations, inspections,
licensure, disciplinary actions, or other oversight activities
of authorized entities.
16. Disaster Relief Efforts. The Plans may use or disclose your
PHI to notify a family member or other individual involved
in your care of your location, general condition or death, or
to a public or private entity authorized by law or its charter
to assist in disaster relief efforts to make such notification.
USES AND DISCLOSURES REQUIRING
YOURAUTHORIZATION
The Plans will obtain your written authorization for any
other uses or disclosures of your PHI, including for most
uses and disclosures of psychotherapy notes (except in
situations noted above), uses and disclosures of PHI for
marketing purposes, and uses or disclosures that are a
sale of PHI. The Plan will not condition your eligibility to
participate in the Plan or payment of benefits under the
Plan upon your authorization, except where allowed by law.
If you give us written authorization for a use or disclosure of
your PHI, you may revoke that authorization at any time in
writing. If you revoke your authorization, we will no longer
use or disclose your PHI for the reasons described in the
authorization, except for where we have taken action in
reliance on your authorization before we received your
written revocation.
STRICTER STATE PRIVACY LAWS
Under the HIPAA Privacy Regulations, the Plan is required
to comply with state laws, if any, that also are applicable
and are not contrary to HIPAA (for example, where state
laws may be stricter). The Plan maintains a policy to ensure
compliance with these laws.
YOUR RIGHTS RELATED TO YOUR PHI
You have the following rights regarding your PHI that
wemaintain:
1. Right to Request Confidential Communications. You
have the right to request that the Plans communicate
with you about your health and related issues in a
particular manner or at a certain location if you feel
that your life may be endangered if communications
are sent to your home. For example, you may ask that
we contact you at work rather than home. In order to
request a type of confidential communication, you must
make a written request to the address at the end of this
section specifying the requested method of contact
or the location where you wish to be contacted. For
us to consider granting your request for a confidential
communication, your written request must clearly state
that your life could be endangered by the disclosure of
all or part of this information.
2. Right to Request Restrictions. You have the right to
request a restriction in our use or disclosure of your
PHI for treatment, payment, or health care operations.
We generally are not required to agree to your request
except in limited circumstances; however, if we do
agree, we are bound by our agreement except when
otherwise required by law, in emergencies, or when
the information is necessary to treat you. To request
a restriction in our use or disclosure of your PHI, you
must make your request in writing to the address at
the end of this section. Your request must describe in a
clear and concise fashion: (a) the information you wish
restricted; (b) whether you are requesting to limit the
Associates’ Medical Plan’s, dental plan’s, or RFL’s use,
disclosure, or both; and (c) to whom you want the limits
to apply.
3. Right to Inspect and Copy. Except for limited
circumstances, you have the right to inspect and copy
the PHI that may be used to make decisions about you.
Usually, this includes medical and billing records. To
inspect or copy your PHI, you must submit your request
in writing to the address listed at the end of this section.
The Plans must directly provide to you, and/or the
individual you designate, access to the electronic PHI
in the electronic form and format you request, if it is
readily producible, or, if not, then in a readable electronic
format as agreed to between you and the Plan. The Plans

Legal information
287
may charge a fee for the costs of copying, mailing, labor,
and supplies associated with your request. We may deny
your request to inspect and/or copy in certain limited
circumstances, in which case you may submit a request
to the Plan at the address in the next column that the
denial be reviewed.
4. Right to Request Amendment. You have the right to
request that we amend your PHI if you believe it is
incorrect or incomplete. To request an amendment,
you must submit a written request to the address listed
at the end of this section. You must provide a reason
that supports your request for amendment. We may
deny your request if you ask us to amend PHI that is: (a)
accurate and complete; (b) not part of the PHI kept by or
for the Plan; (c) not part of the PHI which you would be
permitted to inspect and copy; or (d) not created by the
Plan, unless the individual or entity that created the PHI
is not available to amend it. Even if we deny your request
for amendment, you have the right to submit a statement
of disagreement regarding any item in your record you
believe is incomplete or incorrect. If you request, it will
become part of your medical record and we will attach
it to your records and include it whenever we make a
disclosure of the item or statement you believe to be
incomplete or incorrect.
5. Right to an Accounting of Disclosures. You have the
right to request an accounting of disclosures. An
accounting of disclosures is a list of certain disclosures
we have made of your PHI, for most purposes other
than treatment, payment, health care operations, and
other exceptions pursuant to law or pursuant to your
authorization. To request an accounting of disclosures,
you must submit a written request to the address at the
end of this section. You must specify the time period,
which may not be longer than the six-year period prior
to your request. We will notify you of the cost involved
in complying with your request and you may choose to
withdraw or modify your request at that time.
6. Paper Notice. You have a right to request a paper copy
ofthis notice, even if you have agreed to receive this
notice electronically.
If you believe your privacy rights have been violated,
you may file a complaint with the Associates’ Medical
Plan, dental plan, or RFL, or with the Secretary of the
U.S. Department of Health and Human Services. To file
a complaint with us, you must submit it in writing to the
address listed at the end of this section. Neither Walmart
nor the Plans will retaliate against you for filing a complaint.
You will not be retaliated or discriminated against and no
services, payment, or privileges will be withheld from you
because you file a complaint with the Associates’ Medical
Plan, dental plan, or RFL, or with the U.S. Department of
Health and Human Services.
If you have questions about this notice or would like to
exercise one or more of the rights listed in this notice,
please contact:
Walmart People Services
Attn: HIPAA Compliance Team
508 SW 8th Street
Mail Stop #3500
Bentonville, Arkansas 72716-3500
Email your questions to: AHWPrivacy@walmart.com
Telephone: 800-421-1362
Medicare and your prescription
drugcoverage
Please read this notice about Medicare and your prescription
drug coverage carefully and keep it where you can find it.
This notice has information about your current prescription
drug coverage under the Associates’ Health and Welfare
Plan (the Plan) and your prescription drug coverage option
under Medicare. This information can help you decide
whether or not you want to join a Medicare drug plan. If you
are considering joining, you should compare your current
coverage, including which drugs are covered at what cost,
with the coverage and costs of the plans offering Medicare
prescription drug coverage in your area. It also tells you
where to find more information to help you make decisions
about your prescription drug coverage.
There are important things you need to know about your
current coverage and Medicare’s prescription drug coverage:
• Medicare prescription drug coverage became available
in 2006 to everyone with Medicare. You can get this
coverage if you join a Medicare prescription drug plan
or join a Medicare Advantage Plan (like an HMO or PPO)
that offers prescription drug coverage. All Medicare drug
plans provide at least a standard level of coverage set by
Medicare. Some plans may also offer more coverage for a
higher monthly premium.
• Some of the Walmart prescription drug plans (as described
later in this notice under the heading Which Walmart plans
are considered creditable coverage?) are, on average for
all Plan participants, expected to pay out as much as the
standard Medicare prescription drug coverage will pay
and are therefore considered creditable coverage. If you
are a participant in one of these plans, you may keep your
current coverage and not pay a higher premium (a penalty)
if you later decide to join a Medicare drug plan.
• Other Walmart plan options (as described later in this
notice under the heading Which Walmart plans are
considered non-creditable coverage?) are, on average for
all Plan participants, not expected to pay out as much as
the standard Medicare prescription drug coverage will pay.
If you are a participant in one of these plans, your coverage
is non-creditable coverage. This is important because for
See page 332

Legal information
288
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
most people enrolled in these plan options, enrolling in
Medicare prescription drug coverage means you will get
more help with drug costs than if you had prescription
drug coverage exclusively through the Plan. This is also
important because it may mean that you pay a higher
premium (a penalty) if you do not join a Medicare drug plan
when you first become eligible.
If you have non-creditable coverage under the Plan, it may
affect how much you pay for Medicare D drug coverage
in the future. When you become eligible for Medicare D,
you should compare your current coverage, including what
drugs are covered, with the coverage and cost of the plans
offered by Medicare prescription drug coverage in your
area. Read this notice carefully — it explains your options.
CREDITABLE AND NONCREDITABLE
COVERAGE
What is the meaning of the term “creditable coverage”?
Creditable coverage means that your current prescription
drug coverage is, on average for all Plan participants,
expected to pay out as much as the standard Medicare
prescription drug coverage will pay. Prescription drug
coverage that does not satisfy this requirement is not
creditable coverage.
WHICH WALMART PLANS ARE CONSIDERED
CREDITABLE COVERAGE?
Walmart has determined that the following Plans’
prescription drug coverages are considered creditable
according to Medicare guidelines:
• Premier Plan
• Contribution Plan
• Local Plans
• HMO Plans
• eComm PPO Plan
If your coverage is creditable, you can keep your existing
coverage and not pay extra if you later decide to enroll in
Medicare coverage.
If you are enrolled in any of the Plans listed above, you
can choose to join a Medicare prescription drug plan
later without paying extra because you have existing
prescription drug coverage that, on average, is as good as
Medicare’s coverage.
If you are enrolled in Medicare Part D, you are not eligible
to enroll in any of the Plans listed above. If your dependent
is enrolled in Medicare Part D and you are not, you are
eligible to enroll in a Walmart medical or HMO plan, but
your dependent would not be eligible for coverage.
If you drop your medical coverage with Walmart and enroll
in a Medicare prescription drug plan, you and your eligible
dependents will have the option of reenrolling in the
Walmart Plan during Annual Enrollment or with a valid status
change event. You should compare your current coverage,
including which drugs are covered, with the coverage and
cost of the plans offering Medicare prescription drug
coverage in your area.
WHICH WALMART PLANS ARE CONSIDERED
NONCREDITABLE COVERAGE?
The following Plan’s prescription drug coverage is considered
non-creditable according to Medicare guidelines:
• Saver Plan
If your coverage is non-creditable, you might want to
consider enrolling in Medicare prescription drug coverage
or a Walmart creditable Plan listed above because the
coverage you have is, on average for all participants, not
expected to pay out as much as the standard Medicare
prescription drug coverage will pay.
WHEN CAN I ENROLL FOR MEDICARE
PRESCRIPTION DRUG COVERAGE?
You can join a Medicare drug plan when you first become
eligible for Medicare and each year from October 15
through December 7.
If you have creditable prescription drug coverage and you
lose it through no fault of your own, you will be eligible
for a two-month Special Enrollment Period (SEP) to join a
Medicare drug plan.
If you have non-creditable prescription drug coverage and
you drop coverage under the Plan, because your coverage
is employer-sponsored group coverage, you will be eligible
for a two-month SEP to join a Medicare drug plan. However,
you may pay a higher premium (a penalty) because you did
not have creditable coverage under the Plan.
WHEN WILL I PAY A HIGHER PREMIUM A
PENALTY TO JOIN A MEDICARE DRUG PLAN?
If you have creditable coverage and drop or lose your
coverage under the Plan and do not join a Medicare drug
plan within 63 continuous days after your current coverage
ends, you may pay a higher premium (a penalty) to join the
Medicare drug plan later.
If you have non-creditable coverage, depending on how
long you go without creditable prescription drug coverage,
you may pay a penalty to join a Medicare drug plan.
Starting with the end of the last month that you were
first eligible to join a Medicare drug plan but didn’t join,
if you go 63 continuous days or longer without creditable
prescription drug coverage, your monthly premium may
go up by at least 1% of the Medicare base beneficiary
premium per month for every month that you did not have
that coverage. For example, if you go 19 months without
See page 332

Legal information
289
creditable coverage, your premium may always be at least
19% higher than the Medicare base beneficiary premium.
You may have to pay this premium (a penalty) as long as
you have Medicare prescription drug coverage. In addition,
you may have to wait until the following Medicare annual
enrollment period beginning in October to join.
WHAT HAPPENS TO YOUR CURRENT
COVERAGE IF YOU DECIDE TO JOIN A
MEDICARE DRUG PLAN?
If you decide to join a Medicare drug plan, your current
coverage under the Associates’ Medical Plan (AMP) will
be affected. Plan guidelines restrict you from enrolling
in the AMP if you are enrolled in Medicare Part D. If your
dependent is enrolled in Medicare Part D and you are not,
you are able to enroll in the AMP, but your dependent would
not be eligible for coverage.
If you decide to join a Medicare drug plan and drop your
coverage under the Walmart AMP, be aware that you and
your dependents will be able to get your AMP coverage
back, but only during Annual Enrollment or due to a status
change event.
If you enroll in a Medicare Part D plan and decide within 60
days to switch back to a plan under the Walmart AMP, you
will automatically be reenrolled for the same coverage you
had prior to the status change event. See the Eligibility and
enrollment chapter for further details.
FOR MORE INFORMATION ABOUT MEDICARE
AND YOUR PRESCRIPTION DRUG COVERAGE
• You will get this notice each year before your Medicare
enrollment period.
• If we make a plan change that affects your creditable
coverage, you will receive another notice.
• If you need a copy of this notice, you can request one from
People Services at 800-421-1362.
ADDITIONAL INFORMATION AVAILABLE
More detailed information about Medicare plans that
offer prescription drug coverage is available through the
Medicare & You handbook from Medicare. You may also be
contacted directly by Medicare-approved prescription drug
plans. You will get a copy of the handbook in the mail every
year from Medicare. You can also get more information
about Medicare prescription drug plans from these sources:
• Visit medicare.gov.
• Call your state health insurance assistance program for
personalized help. (See your copy of the Medicare & You
handbook for its telephone number.)
• Call 800-MEDICARE (800-633-4227). TTY users should
call 877-486-2048.
For people with limited income and resources, extra help
paying for the Medicare prescription drug plan is available.
For more information about this resource, visit the Social
Security Administration online at socialsecurity.gov, or call
800-772-1213 (TTY 800-325-0778).
REMEMBER
Keep this notice. If you enroll in one of the
Medicare prescription drug plans, you may
need to provide a copy of this notice when
you join to show whether or not you have
creditable coverage and therefore whether
ornot you are required to pay a higher
premium (a penalty).
Premium assistance under Medicaid
and the Children’s Health Insurance
Program (CHIP)
If you or your children are eligible for Medicaid or CHIP and
you’re eligible for health coverage from Walmart Inc., your
state may have a premium assistance program that can help
pay for coverage, using funds from their Medicaid or CHIP
programs. If you or your children aren’t eligible for Medicaid
or CHIP, you won’t be eligible for these premium assistance
programs but you may be able to buy individual insurance
coverage through the Health Insurance Marketplace. For
more information, visit healthcare.gov.
If you or your dependents are already enrolled in Medicaid
or CHIP and you live in a state listed on the following pages,
contact your state Medicaid or CHIP office to find out if
premium assistance is available.
If you or your dependents are NOT currently enrolled
in Medicaid or CHIP, and you think you or any of your
dependents might be eligible for either of these programs,
contact your state Medicaid or CHIP office or dial
877-KIDSNOW or insurekidsnow.gov to find out how to
apply. If you qualify, ask your state if it has a program that
might help you pay the premiums for the Plan.
If you or your dependents are eligible for premium
assistance under Medicaid or CHIP, as well as eligible
under the Walmart Inc. Plan, the Plan must allow you and
your dependents to enroll in the Plan if you aren’t already
enrolled. This is called a “special enrollment” opportunity,
and you must request coverage within 60 days of being
determined eligible for premium assistance. If you have
questions about enrolling in your employer plan, contact
the Department of Labor at askebsa.dol.gov or call
866-444-EBSA (3272).
See pages 332-334

Legal information
290
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
ALABAMA – Medicaid
Website: http://myalhipp.com
Phone: 855-692-5447
ALASKA – Medicaid
The AK Health Insurance Premium Payment Program
Website: http://myakhipp.com
Phone: 866-251-4861
Email: CustomerService@MyAKHIPP.com
Eligibility:
http://dhss.alaska.gov/dpa/Pages/medicaid/default.aspx
ARKANSAS – Medicaid
Website: http://myarhipp.com
Phone: 855-MyARHIPP (855-692-7447)
COLORADO – Health First Colorado (Colorado’s Medicaid
Program) & Child Health Plan Plus (CHP+)
Health First Colorado website:
https://www.healthfirstcolorado.com
Health First Colorado Member Contact Center:
800-221-3943 State Relay 711
CHP+:
https://www.colorado.gov/pacific/hcpf/child-health-plan-plus
CHP+ Customer Service: 800-359-1991 / State Relay 711
FLORIDA – Medicaid
Website: http://flmedicaidtplrecovery.com/hipp
Phone: 877-357-3268
GEORGIA – Medicaid
Website: https://medicaid.georgia.gov/health-insurance-
premium-payment-program-hipp
Phone: 678-564-1162 ext. 2131
INDIANA – Medicaid
Healthy Indiana Plan for low-income adults 19–64
Website: http://www.in.gov/fssa/hip/
Phone: 877-438-4479
All other Medicaid
Website: http://www.indianamedicaid.com
Phone: 800-403-0864
IOWA – Medicaid
Website: http://dhs.iowa.gov/Hawki
Phone: 800-257-8563
KANSAS – Medicaid
Website: http://www.kdheks.gov/hcf
Phone: 785-296-3512
KENTUCKY – Medicaid
Website: http://chfs.ky.gov
Phone: 800-635-2570
LOUISIANA – Medicaid
Website: http://dhh.louisiana.gov/index.cfm/subhome/1/n/331
Phone: 888-695-2447
MAINE – Medicaid
Website:
http://www.maine.gov/dhhs/ofi/public-assistance/index.html
Phone: 800-442-6003
TTY: Maine relay 711
MASSACHUSETTS – Medicaid and CHIP
Website:
http://www.mass.gov/eohhs/gov/deparments/masshealth
Phone: 800-862-4840
MINNESOTA – Medicaid
Website: http://mn.gov/dhs/people-we-serve/seniors/
health-care/health-care-programs/programs-and-services/
other-insurance.jsp
Phone: 800-657-3739
MISSOURI – Medicaid
Website:
http://www.dss.mo.gov/mhd/paricipants/pages/hipp.htm
Phone: 573-751-2005
MONTANA – Medicaid
Website:
http://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP
Phone: 800-694-3084
NEBRASKA – Medicaid
Website: http://www.ACCESSNebraska.ne.gov
Phone: 855-632-7633
Lincoln: 402-473-7000
Omaha: 402-595-1178
NEVADA – Medicaid
Medicaid website: https://dhcfp.nv.gov/
Medicaid phone: 800-992-0900
NEW HAMPSHIRE – Medicaid
Website: https://www.dhhs.nh.gov/oii/documents/hipp.htm
Phone: 603-271-5218
Toll-free for HIPP program: 800-852-3345 ext. 5218
NEW JERSEY – Medicaid and CHIP
Medicaid website:
http://www.state.nj.us/humanservices/dmahs/clients/medicaid
Medicaid phone: 609-631-2392
CHIP website: http://www.njfamilycare.org/index.html
CHIP phone: 800-701-0710
If you live in one of the following states, you may be eligible for assistance paying your employer health plan premiums.
Thefollowing list of states is current as of July 31, 2019. Contact your state for more information on eligibility.
See pages 334-335

Legal information
291
NEW YORK – Medicaid
Website: https://www.health.ny.gov/health_care/medicaid/
Phone: 800-541-2831
NORTH CAROLINA – Medicaid
Website: https://medicaid.ncdhhs.gov
Phone: 919-855-4100
NORTH DAKOTA – Medicaid
Website:
http://www.nd.gov/dhs/services/medicalserv/medicaid
Phone: 844-854-4825
OKLAHOMA – Medicaid and CHIP
Website: http://www.insureoklahoma.org
Phone: 888-365-3742
OREGON – Medicaid
Website: http://healthcare.oregon.gov/Pages/index.aspx
http://www.oregonhealthcare.gov/index-es.html
Phone: 800-699-9075
PENNSYLVANIA – Medicaid
Website:
http://www.dhs.pa.gov/provider/medicalassistance/
healthinsurancepremiumpaymenthippprogram/index.htm
Phone: 800-692-7462
RHODE ISLAND – Medicaid and CHIP
Website: http://www.eohhs.ri.gov
Phone: 855-697-4347
or 401-462-0311 (Direct RIte Share Line)
SOUTH CAROLINA – Medicaid
Website: https://www.scdhhs.gov
Phone: 888-549-0820
SOUTH DAKOTA – Medicaid
Website: http://dss.sd.gov
Phone: 888-828-0059
TEXAS – Medicaid
Website: http://gethipptexas.com
Phone: 800-440-0493
UTAH – Medicaid and CHIP
Medicaid website: https://medicaid.utah.gov
CHIP website: http://health.utah.gov/chip
Phone: 877-543-7669
VERMONT– Medicaid
Website: http://www.greenmountaincare.org
Phone: 800-250-8427
VIRGINIA – Medicaid and CHIP
Medicaid/CHIP website:
http://www.coverva.org/programs_premium_assistance.cfm
Medicaid phone: 800-432-5924
CHIP phone: 855-242-8282
WASHINGTON – Medicaid
Website: http://www.hca.wa.gov
Phone: 800-562-3022 ext. 15473
WEST VIRGINIA – Medicaid
Website: http://mywvhipp.com
Phone: 855-MyWVHIPP (855-699-8447)
WISCONSIN – Medicaid and CHIP
Website:
https://www.dhs.wisconsin.gov/publications/p1/p10095.pdf
Phone: 800-362-3002
WYOMING – Medicaid
Website: https://wyequalitycare.acs-inc.com
Phone: 307-777-7531
To see if any other states have added a premium assistance program since July 31, 2019, or for more information on special
enrollment rights, contact either:
U.S. Department of Labor
Employee Benefits Security Administration
dol.gov/ebsa
866-444-EBSA (3272)
U.S. Department of Health and Human Services
Centers for Medicare & Medicaid Services
cms.hhs.gov
877-267-2323, Menu Option 4, Ext. 61565

Legal information
292
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Valued Plan Paricipant
THE ASSOCIATES’ HEALTH AND WELFARE PLAN (AHWP) RESPECTS THE DIGNITY OF EACH INDIVIDUAL WHO
PARTICIPATES IN THE PLAN.
The AHWP does not discriminate on the basis of race, color, national origin, sex, age, or disability and strictly prohibits
retaliation against any person making a complaint of discrimination. Additionally, we gladly provide our participants
with language assistance, auxiliary aids, and services at no cost. We value you as our participant and your satisfaction is
important to us.
If you need such assistance or have concerns with your Plan services, please call the number on the back of your plan ID
card. If you have any questions or concerns, please use one of the methods below so that we can better serve you.
For assistance, call the number on the back of your plan ID card.
To learn about or use our grievance process, contact People Services at 1-800-421-1362.
To file a complaint of discrimination, contact the U.S. Department of Health and Human Services, Office of Civil Rights:
Phone: 1-800-368-1019 or 1-800-537-7697 (TDD)
Website:
https://ocrportal.hhs.gov/ocr/cp/wizard_cp.jsf
Email: OCRCompliant@hhs.gov
Interpreter services are available at no cost: 1-800-421-1362
Français
Des services d’interprètes sont disponibles sans frais.
1-800-421-1362.
kreyòl ayisye
Gen Sèvis entèprèt ki disponib gratis. 1-800-421-1362.
Polski
Usługi tłumacza dostępne są bez żadnych kosztów.
1-800-421-1362.
Português (Brasil)
Serviços de interprete estão disponíveis grátis.
1-800-421-1362.
Română
Serviciile de interpretariat sunt disponibile gratuit.
1-800-421-1362.
Af-Soomaali
Adeegyada Turjumaanka waxaa lagu heli karaa kharash la’aan.
1-800-421-1362.
Español
Los servicios de interpretación están disponibles de manera
gratuita. 1-800-421-1362.
Kiswahili
Huduma za tafsiri zipo bila malipo. 1-800-421-1362.
See page 336
Legal information
293

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Active work or actively at work: For medical, dental, vision,
Resources for Living, critical illness, accidental death and
dismemberment, and accident insurance coverage, “active
work” means you have reported to work for Walmart.
For company-paid life insurance, optional associate life
insurance, optional dependent life insurance, business
travel accident insurance, and all types of disability
coverage, “active work” means you are actively at work
with the company on a day that is one of your scheduled
work days and you are performing all of the regular
duties of your job on a full-time basis or a part-time basis
(depending on your classification as a full-time or part-time
associate). You will be deemed to be actively at work on a
day that is not one of your scheduled work days only if you
were actively at work on the preceding scheduled work day.
Annual Enrollment: The period, usually in the fall of each
year, during which associates make benefit elections for the
next Plan year.
Associates’ Health and Welfare Plan (the Plan): The
employer-sponsored health and welfare employee benefit
plan sponsored by Walmart Inc. and governed under the
Employee Retirement Income Security Act of 1974, as
amended (ERISA).
Associates’ Medical Plan (AMP): Refers to the medical plans
offered by Walmart (the Premier Plan, Contribution Plan,
Saver Plan, and local plans). See The medical plan chapter for
more information.
Behavioral health benefits: The benefits for mental health
and substance abuse, including alcohol and drug abuse.
Catch-up contributions: Additional contributions allowed
by the IRS to an associate’s health savings account if the
account holder is age 55 or older. Catch-up contributions
are also allowed by the IRS to an associate’s 401(k) plan if
the associate is age 50 or older.
COBRA: The Consolidated Omnibus Budget Reconciliation
Act, which allows associates and their eligible dependents
who experience a loss in coverage due to a qualifying event
to continue medical, dental, and vision coverage.
Coinsurance: The amount you pay for certain eligible
expenses after you’ve met your annual deductible. See
The medical plan and The dental plan chapters for specific
coinsurance details.
Company: Walmart Inc. and its participating subsidiaries.
Coordination of benefits: When two benefit plans insure the
same participant and coordinate coverage, the process of
designating one plan as primary and the other as secondary.
Copay or copayment: A fixed dollar amount required for
certain covered services or supplies. For details about
services subject to copays, see The medical plan, The
pharmacy benefit, and The vision plan chapters.
Covered expenses: Charges for procedures, supplies,
equipment, or services covered under the Associates’
Medical Plan that are:
• Medically necessary
• Not in excess of the maximum allowable charge
• Not excluded under the Plan, and
• Not otherwise in excess of Plan limits.
Deductible: The amount you pay each calendar year for
eligible charges before the AMP pays a portion of certain
covered expenses. For details, see The medical plan, The
pharmacy benefit, and The dental plan chapters.
Disability or disabled: Referring to a medical condition
or injury that impairs your ability to perform the duties
of your job. See the individual short-term and long-term
disability chapters for detailed definitions and related
terms and conditions.
Eligibility waiting period: The time between an associate’s hire
date and the date the associate is eligible to enroll forbenefits.
Eligible dependents: An eligible associate’s spouse, partner,
or child who satisfies the dependent eligibility requirements
listed in the Dependent eligibility section of the Eligibility
and enrollment chapter.
Evidence of Insurability: See Proof of Good Health.
Explanation of benefits (EOB): A document sent to Plan
participants explaining how a claim was paid or applied.
Health care advisor: For associates who enroll in the
Associates’ Medical Plan, a resource who serves as a single
point of contact for all inquiries and communication with
your third-party administrator.
Glossary
Glossary
295
Health Reimbursement Account (HRA): An “account” to
which the company allocates a specific sum of money to
help pay your eligible medical expenses before you have
topay toward the costs of covered medical expenses
(except prescriptions).
Health savings account (HSA): A tax-advantaged custodial
account you can open with HealthEquity, if you are enrolled
in the Saver Plan, which can be used to pay for qualified
medical expenses (as defined by the IRS), tax-free.
Initial enrollment period: The first time you are eligible
to enroll for benefits under the Plan. Initial enrollment
periods may vary by job classification. See the charts in the
Eligibility and enrollment chapter.
Leave of absence: Provides associates with needed time
away from work while maintaining eligibility for benefits and
continuity of employment. To accommodate situations that
necessitate absence from work, the company provides three
types of leave:
• Family and Medical Leave Act (FMLA)
• Personal, and
• Military.
The decision to grant a request for leave shall be based
on applicable laws, the nature of the request, the effect
on work requirements, and consistency with the policy
guidelines and procedures.
Maximum allowable charge (MAC): MAC is the maximum
amount the medical plan will cover or pay for any health
care services, drugs, medical devices, equipment, or
supplies covered by the AMP. For details, see The medical
plan chapter.
Maximum plan allowance (MPA): The MPA is the maximum
amount the dental plan will cover or pay for dental
services covered by the dental plan. For details, see The
dental plan chapter.
Network providers: Health care providers that have a
written agreement with third-party administrators to
provide services at discounted rates.
Non-network providers: Health care providers that do not
have a written agreement with third-party administrators to
provide services at discounted rates.
Out-of-network benefits: Payment for covered expenses
that are provided by a non-network provider and do not
meet the criteria outlined under When network benefits
are paid for out-of-network expenses in The medical plan
chapter. (Out-of-network benefits are not provided under
certain plan options available under the AMP except in cases
of emergency, as described in The medical plan chapter.)
Out-of-pocket maximum: The most you will pay each year
for eligible network services, including prescriptions.
Partner: For purposes of determining dependent eligibility,
an associate’s domestic partner or other person to whom
the associate is joined in a legal relationship recognized as
creating some or all of the rights of marriage, meeting the
eligibility requirements listed in the Dependent eligibility
section of the Eligibility and enrollment chapter.
Preauthorization or prior authorization: A notification that
may be required as a condition to coverage for certain
services by network providers. See the Preauthorization and
Centers of Excellence sections of The medical plan chapter
or contact the applicable administrator for more information.
Premium: The amount you pay for the benefits you choose,
generally out of each paycheck.
Prenotification: A notification voluntarily made by
enrollees/providers to advise third-party administrators of
any upcoming hospital admissions or outpatient services.
As described in the Prenotification section of The medical
plan chapter, responses by third-party administrator to
prenotification inquiries are not binding on the Associates’
Medical Plan.
Proof of Good Health or “Evidence of Insurability”:
Evidence of your health condition, which includes
completing a questionnaire regarding your medical history
and possibly having a medical exam.
Qualified medical expense: An expense that meets the
definition of medical expenses under Internal Revenue Code
Sec. 213(d). Examples are provided in IRS Publication 502,
Medical and Dental Expenses.
Qualified Medical Child Support Order (QMCSO): A final
court or administrative order requiring an associate to carry
health care coverage for eligible dependents under the
Associates’ Medical Plan, usually following a divorce or child
custody proceeding.
Status change event: An event that allows you to make
changes to your coverage outside of the initial enrollment
period or Annual Enrollment, and in accordance with
federal law. These events are listed in the Eligibility and
enrollment chapter.
Third-party administrator (TPA): A third party that provides
administrative services to the Plan, including making claims
and internal appeals determinations, pursuant to a contractual
arrangement with the Plan. Third-party administrators do not
insure any benefits under the Plan.
United States: For self-insured benefits, the 48 contiguous
states, Hawaii, Alaska, and the District of Columbia.
Walmart: Walmart Inc. and its participating subsidiaries.

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
2021 Summaries of
Material Modifications
This document contains the following benefits-related information:
• Summary of Material Modifications for the Walmart 401(k) Plan
• Summary of Material Modifications for the Associates’ Health and Welfare Plan including Additional Benefits/Extensions
During Covid-19 National Emergency
• Legal Notices for the Associates’ Health and Welfare Plan
This document contains the 2021 Summary of Material Modifications (“SMM”) to the Walmart 401(k) Plan and the 2021
SMM to the Associates’ Health and Welfare Plan. The 2020 Associate Benefits Book, which serves as the summary plan
description for each of these plans, has been revised. Please read each plan’s SMM, which explains these revisions. You will
not receive a new Associate Benefits Book for 2021. Instead, you should review your 2020 Associate Benefits Book, along
with these SMMs. The current summary plan description for each plan is comprised of the original printing of the 2020
Associate Benefits Book and this SMM.
2021 SUMMARY OF MATERIAL MODIFICATIONS TO THE WALMART 401k PLAN
February 1, 2020
The revisions and page numbers listed below refer to the initial printing of the 2020 Associate Benefits Book and the electronic version
distributed during the 2020 online Annual Enrollment session. Unless otherwise indicated, the revisions to the Walmart 401(k) Plan will be
effective as of February 1, 2021.
Page 243—RECEIVING A PAYOUT WHILE WORKING FOR WALMART: Effective April 20, 2020, add an additional bullet point to the list:
• Between the dates of April 20, 2020 and December 31, 2020, as part of the Coronavirus Aid, Relief, and Economic Security (CARES) Act,
participants eligible for a Coronavirus Relief Distribution may take up to $100,000 from all eligible accounts without incurring the usual 10%
early withdrawal penalty. Taxes related to Coronavirus Relief Distributions may also be spread over a three-year period. Also, remember that
you may repay some or all of your withdrawal within three years; repayments will be treated like a rollover contribution.
Page 243—FINANCIAL HARDSHIP WITHDRAWALS: Effective February 1, 2021, add an additional bullet point to the list:
• Expenses and losses (including loss of income) incurred by you on account of a disaster declared by the Federal Emergency Management Act
(FEMA) under the Robert T. Stafford Disaster Relief and Emergency Assistance Act, provided your principal residence or principal place of
employment at the time of the disaster was in an area designated for individual assistance with respect to disaster.
Page 244—PLAN LOANS: Add the following text to the end of the section:
Effective Apr. 20, 2020 as part of the Coronavirus Aid, Relief, and Economic Security (CARES) Act:
• You may be eligible to borrow up to 100% of your vested 401(k) plan account balance, not to exceed $100,000, subject to normal Plan rules
under the Walmart 401(k) Plan. To take advantage of the higher loan limits, this loan must be made within 180 days of March 27, 2020, when
the CARES Act was enacted. Loans must be requested by September 21, 2020.
• You are also able to delay loan payments that would otherwise be due through December 31, 2020. During this period, payments will be on hold,
but interest on the loan will continue to accrue. Repayments will commence as soon as administratively possible in 2021 and the original loan pay-
off date will be extended by 12 months. This may result in a different loan payment amount than the original loan payment.

2021 Summaries of Material Modifications
297
2021 SUMMARY OF MATERIAL MODIFICATIONS TO THE ASSOCIATES’ HEALTH AND WELFARE PLAN
January 1, 2021
The revisions and page numbers listed below refer to the initial printing of the 2020 Associate Benefits Book and the electronic version
distributed during the 2020 online Annual Enrollment session. Unless otherwise indicated, the revisions to the Associates’ Health and
Welfare Plan (“AHWP” or “Plan”) will be effective as of January 1, 2021. Coverage will continue to be subject to the Plan’s otherwise
applicable eligibility terms, exclusions, limitations, and cost-sharing as described in the 2020 Associate Benefits Book.
If you (and/or your dependents) have Medicare or will become eligible for Medicare in the next 12 months,
a federal law gives you more choices about your prescription drug coverage. Please see page 32 of this SMM
for more details.
ADDITIONAL BENEFITS/EXTENSIONS DURING COVID19 NATIONAL EMERGENCY
During the COVID-19 National Emergency, as defined by the U.S. Department of Labor (“DOL”) unless otherwise noted, the Plan will
provide additional COVID-related benefits or extensions as described below. For more information on the DOL COVID-19 National
Emergency declaration, see https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/covid-19.pdf.
Unless otherwise noted, these COVID-related changes apply from March 1, 2020 through the end of the COVID-19 National Emergency.
1. The period beginning March 1, 2020 and ending 60 days after the end of the COVID-19 public health emergency defined by the IRS will be
disregarded when determining the deadlines for making changes to Plan elections as the result of status change events, as described in the
Eligibility and enrollment chapter of the 2020 Associate Benefits Book, beginning under the subhead Status change events on page 21.
2. During the public health emergency declared by the President, the Plan will cover at 100%, without cost-sharing, a COVID-19 diagnostic
test when ordered by your attending health care provider, and services and diagnostic tests that result in an order for, or administration
of, a COVID-19 diagnostic test. This includes related diagnostic services and items furnished during network or non-network urgent care,
emergency room, or in-person or telehealth provider visits that result in an order for or administration of a COVID-19 diagnostic test.
3. The Plan will waive the $4 copay for Doctor On Demand visits.
4. If you are enrolled in the Saver Plan, the Plan will cover telehealth visits through Doctor On Demand, even if you have not yet met your
deductible. This provision will be in effect through December 31, 2021. If your telehealth visit is with a provider other than Doctor On Demand,
you will still need to meet your deductible, unless the visit results in the administration of a COVID-19 diagnostic test, as described above.
5. Certain Centers of Excellence requirements may differ based on travel safety during the COVID-19 National Emergency. Additionally, for
all programs, including weight loss surgery, additional funds will be provided per trip to the Centers of Excellence facility (regardless of the
number of travelers), intended for purchase of personal protective equipment. For updated Plan requirements and travel guidance, contact
Contigo Health (formerly Health Design Plus) for cardiac, spine, joint (hip and knee) replacement, and weight loss surgery programs, and
HealthSCOPE Benefits for cancer eReview, kidney eReview and transplant programs.
6. Certain pharmacy rules, such as being able to fill prescriptions for longer periods, may differ during the COVID-19 National Emergency.
These COVID-related rules may not extend through the end of the National Emergency. Contact OptumRx for current rules.
7. The deadlines to elect COBRA, provide required COBRA notifications, or pay COBRA premiums are extended, as required by law, for the
period from March 1, 2020 through 60 days after the end of the COVID-19 National Emergency. Contact the Plan’s COBRA administrator
for more information.
8. The deadlines to file claims and appeals or to request external review are extended, as required by law, for the period from March 1, 2020
through 60 days after the end of the COVID-19 National Emergency. Contact your third-party administrator for more information.
9. Effective March 1, 2020, if you are eligible for the short-term disability plan for full-time hourly associates, you will be “disabled” if you
are diagnosed with COVID-19, have exhausted all paid leave benefits under the Walmart Inc. COVID-19 Emergency Leave Policy, and are
unable to perform the essential duties of your job for your normal work schedule as a result of COVID-19 or major health complications
arising directly from COVID-19 (a “COVID-19 Disability”). If your disability is determined to be a COVID-19 Disability, then the initial seven-
day waiting period applicable to other disabilities is waived and benefits may be paid for up to 26 weeks (instead of 25 weeks). A second
occurrence of a COVID-19 Disability is treated as described in the section titled IF YOU RETURN TO WORK AND BECOME DISABLED
AGAIN in the Short-term disability for full-time hourly associates chapter. If you incur a COVID-19 Disability while you are disabled for
another reason, or you incur a disability for another reason while you are on a COVID-19 Disability, you will be paid as though they were a
single disability. If your COVID-19 diagnosis occurs during your seven-day waiting period, the remainder of the seven-day waiting period will
be waived. These terms will be effective through a date announced by Walmart, which may be earlier than the end of the COVID-19 National
Emergency. Benefits will end no later than 26 weeks after the earliest of your disability dates.
NOTE: These temporary terms also apply to the salaried short-term disability plan and truck-driver short-term disability plan. Those plans
are not benefits covered by ERISA and are not part of the Plan.

2021 Summaries of Material Modifications
298
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Changes affecting multiple locations in the 2020 Associate Benefits Book
If you are a full-time hourly associate enrolled in the shor-term disability enhanced plan or the New York shor-term disability
enhanced plan, you will no longer be able to drop your coverage at any time; you will be able to drop coverage only at Annual
Enrollment or after a status change event.
Similarly, if you are enrolled in the long-term disability plan, the long-term disability enhanced plan, the truck driver long-term
disability plan, or the truck driver long-term disability enhanced plan, you will no longer be able to drop your coverage at any time;
you will be able to drop coverage only at Annual Enrollment or after a status change event.
THE FOLLOWING
SECTIONS ARE
AFFECTED:
ELIGIBILITY AND ENROLLMENT (pp. 4-37): pp. 5, 10, 21
SHORT-TERM DISABILITY FOR FULL-TIME HOURLY ASSOCIATES (pp. 180-189): pp. 183, 188
LONG-TERM DISABILITY (pp. 206-213): pp. 208, 213
TRUCK DRIVER LONG-TERM DISABILITY (pp. 214-221): pp. 216, 221
Effective October 1, 2020, if you are a full-time hourly or management associate and you do not enroll in the long-term disability
plan or the long-term disability enhanced plan when first eligible but later enroll during Annual Enrollment or after a status
change event, you will no longer be required to complete a 12-month waiting period before your coverage is effective. However,
you will be required to submit Evidence of Insurability and may be required to undergo a medical exam at your own expense
before you can be approved for coverage. If approved, your coverage will be effective the first day of the following pay period
after approval is received from Lincoln. If you are not approved, you will only be eligible to enroll in the long-term disability plan
during the next Annual Enrollment or after a status change event.
THE FOLLOWING
SECTIONS ARE
AFFECTED:
ELIGIBILITY AND ENROLLMENT (pp. 4-37): pp. 11, 13, 14, 17, 26, 27
ELIGIBILITY AND ENROLLMENT FOR ASSOCIATES IN HAWAII (pp. 38-43): p. 41
LONG-TERM DISABILITY (pp. 206-213): pp. 207, 208
Effective August 1, 2020, all references to “Health Design Plus,” the third-pary administrator for cerain services under the
Centers of Excellence program, are changed to Contigo Health.
THE FOLLOWING
SECTIONS ARE
AFFECTED:
THE MEDICAL PLAN (pp. 44-91): pp. 66, 77, 78, 81
CLAIMS AND APPEALS (pp. 260-279): pp. 263, 265, 267, 268
ELIGIBILITY AND ENROLLMENT
Pages 4-37 of the 2020 Associate Benefits Book
Page 7—60-day eligibility checks for benefits: Effective January 1, 2021, the following section is added before the section titled Part-time
hourly and temporary associates: eligibility checks for medical benefits:
Par-time hourly and temporary associates: 60-day eligibility checks for benefits
during the first 52 weeks of employment
PREINITIAL CHECK FOR PARTTIME ASSOCIATES DURING FIRST 52 WEEKS OF EMPLOYMENT
MEDICAL BENEFITS
If you are a part-time hourly or temporary associate (other than a part-time truck driver), your hours worked will be measured to determine
whether you are eligible for benefits described in the chart on page 15 of the 2020 Associate Benefits Book before the end of your first 52 weeks
of employment. Your hours worked per week will be measured on the 59th day following your date of hire (the 60th day of employment) and on
every 60th day thereafter until you have been employed for 52 weeks (six total pre-initial checks during your first year of employment). No 60-
day check will be performed after the date on which you reach the end of your initial measurement period, as described later in this chapter.
If you work an average of at least 30 hours a week during your first 60-day measurement cycle, without a break in employment of greater than 30
days, you will become eligible for benefits at the close of that measurement cycle. Specifically, your eligibility for benefits described in the chart
on page 15 of the 2020 Associate Benefits Book will begin on the first day of the month in which your 89th day of employment occurs.
2021 Summaries of Material Modifications
299
If you do not work an average of at least 30 hours a week during your first 60-day measurement cycle, but you do work an average of at least 30
hours a week during any subsequent 60-day measurement cycle, without a break in employment of greater than 30 days, you will become eligible
for benefits described in the chart on page 15 of the 2020 Associate Benefits Book at the close of that measurement cycle. Specifically, your
eligibility for benefits described in the chart on page 15 of the 2020 Associate Benefits Book will begin on the first day of the month in which your
89th day of employment occurs after the successful 60-day measurement cycle began.
For example, if your date of hire is April 16, 2021, your average hours worked from that day through June 14, 2021 will be measured on your 60th
day of employment, June 15. If you worked an average of at least 30 hours a week over this 60-day measurement cycle, your coverage would
begin July 1, 2021 (assuming you enroll in a timely manner), the first day of the month in which your 89th day of employment occurs.
If you work an average of at least 30 hours a week during any 60-day measurement cycle and are offered benefits but do not enroll, you will not
be included in future 60-day measurement cycles and the next time your hours will be measured is at the end of the initial measurement period,
which is described later in this chapter.
If you meet the average-hours-worked requirement, eligibility for medical coverage continues through the end
of the second calendar year following the date that coverage is first offered and and eligibility for all other benefits described in the chart on
page 15 of the 2020 Associate Benefits Book will continue as long as you remain a part-time or temporary associate. However, if you do not elect
coverage when first eligible, you will only be able to elect coverage during Annual Enrollment or if a qualifying event occurs.
In the example above, if you elect medical coverage, your medical coverage (if you enroll in a timely manner) would continue through the end of
2022. For years after 2022, you would be subject to annual eligibility checks, as described later in this chapter.
IF YOU TAKE TIME OFF DURING ANY 60DAY MEASUREMENT CYCLE
If you take any type of unpaid time off that is not an approved leave of absence, as described later in this chapter, your number of actual
service hours will still be used in the calculation of your average hours for the 60-day measurement cycle (even if it is zero) in which the
absence occurs.
If your absence is an approved leave (including for jury duty, Family and Medical Leave Act of 1993 [“FMLA”] leave, or military leave),
your average-hours-worked calculation will be based on the number of days during the 60-day measurement cycle that you worked. For
example, if you take an approved leave during five days of the 60-day measurement cycle, your average hours worked will be calculated
over 55 days rather than 60.
TRANSITION RULE FOR ASSOCIATES WHO WERE EMPLOYED ON OR BEFORE NOVEMBER 2, 2020
If you were employed as a part-time hourly or temporary associate on or before November 2, 2020, there will be a one-time eligibility
check of hours worked from November 2, 2020 through December 31, 2020 to determine whether you worked an average of 30 hours
per week during that period. If you meet the average-hours-worked requirement, eligibility for medical coverage continues through the
end of 2022 and eligibility for all other benefits described in the chart on page 15 of the 2020 Associate Benefits Book will continue as long
as you remain a part-time or temporary associate. However, if you do not elect coverage when first eligible, you will only be able to elect
coverage during Annual Enrollment or if a qualifying event occurs.
For years after 2022, you would be subject to annual eligibility checks for medical benefits, as described later in this chapter.
If you did not work an average of 30 hours a week during that period, ongoing 60-day eligibility checks will resume, based on your original
hire date under the rules described above.
IF YOU LEAVE THE COMPANY AND ARE REHIRED
PART-TIME HOURLY AND TEMPORARY ASSOCIATES
If you return to employment as a part-time hourly or temporary associate within 30 days after leaving during the first 52 weeks of
employment, you will be treated as if you had not left.
If you were enrolled in medical coverage before you left, you will still be enrolled in medical coverage with a break in coverage for
the time coverage was not paid. The medical coverage will continue through the end of the second calendar year following date that
coverage is first offered.
If you are rehired and re-enrolled in the same calendar year, your annual deductible and out-of-pocket maximum under the AMP for the
calendar year in which you terminate will not reset.
If you are rehired in a different calendar year, your annual deductible and out-of-pocket maximum will reset and you will be responsible
for meeting the new deductible and out-of-pocket maximum in their entirety. You will have 60 days after resuming employment to drop
or otherwise change the coverage in which you were automatically re-enrolled.
If you were eligible for medical coverage before you left but did not elect coverage, you will still be eligible to enroll in medical coverage
when you return (assuming you enroll in a timely manner). Your eligibility continues through the end of the second calendar year
2021 Summaries of Material Modifications
300
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
following the date that coverage is first offered. You will be able to elect coverage during this period during Annual Enrollment or if a
qualifying event occurs. If you do not enroll in a timely manner, you will not be included in future 60-day measurement cycles and the
next time your hours will be measured is at the end of the initial measurement period, which is described later in this chapter.
If you were in a 60-day measurement cycle when you left and you return during that same measurement cycle, your hours will continue
to be measured until the end of that measurement cycle. All hours worked during that measurement cycle will be used in the average-
hours-worked calculation. For example, if you have a 10-day break in service during the 60-day measurement cycle, your average hours
will be calculated using the 50 days during which you worked, rather than 60 days.
If you return to employment as a part-time hourly or temporary associate more than 30 days after leaving during your first 52 weeks of
employment, you will be treated as a new hire. The 60-day measurement cycles will resume, with your date of rehire being the first day of
the first 60-day measurement cycle that occurs after you are rehired. The 60-day measurement cycles will continue until the end of the
initial measurement period, which is explained later in this chapter.
Page 12—“Active work” or “actively at work”: Effective January 1, 2020, the two paragraphs following this subhead are replaced with the following:
For medical, dental, vision, critical illness insurance, accident insurance, AD&D and Resources for Living coverage, “active work” (or “actively at
work”) means you are on active status and have reported to your first day of work at the company, even if you are not at work the day coverage
begins (for example, due to illness).
For company-paid life insurance, optional associate life insurance, optional dependent life insurance, and business travel accident insurance, being
actively at work means you are on active status and not on a leave of absence.
For all types of disability coverage, being actively at work means you have worked hours in the immediately preceding pay period if you are an
hourly associate or have earned wages if you are a member of management.
Page 15—PART-TIME HOURLY AND TEMPORARY ASSOCIATES: The following text replaces the text under the heading “Initial enrollment
period”: You must enroll in coverage during the 60-day period beginning with the earlier of 1) the date on which you are first notified that you
have passed a 60-day eligibility check described in the new section titled Part-time hourly and temporary associates: 60-day eligibility checks for
benefits during the first 52 weeks of employment, or 2) your 52-week anniversary date.
The following text replaces the text under the heading “When coverage is effective”: Your coverage is effective the earlier of 1) the first day of
the month in which your 89th day of employment occurs after the successful 60-day measurement cycle began, as described in the new section
titled Part-time hourly and temporary associates: 60-day eligibility checks for benefits during the first 52 weeks of employment, or 2) the first day of
the second calendar month following your 52-week anniversary date.*
Page 32—MANAGEMENT ASSOCIATES TRANSFERRING TO FULL-TIME HOURLY: The following text replaces the bullet point reading “You
are eligible to enroll in the long-term disability plan,” which appears in the top row of the chart (as labeled “Within 60 days of your date of hire and
before you have enrolled for benefits”):
• You are eligible to enroll in the long-term disability (“LTD”) plan during the 60-day period beginning on the first day of the pay period in which your
transition occurs. Your coverage under the LTD plan is effective on your date of hire.
• If you do not enroll in LTD during the 60-day period following your transition, you will only be able to enroll or make changes during Annual
Enrollment or after a status change event and will be required to submit Evidence of Insurability (EOI), which may include undergoing a medical
exam at your own expense before you can be approved for coverage.
– If you are within 12 months of your date of hire and are approved through EOI, your coverage will be effective on the 12-month anniversary
of your date of hire.
– If you are not within 12 months of your date of hire and are approved through EOI, your coverage will be effective the first day of the
following pay period after approval is received from Lincoln.
In addition, the following text replaces the bullet point reading “You are eligible to enroll in the long-term disability plan,” which appears in the
bottom row of the chart (as labeled “Within 60 days of your date of hire and after you have enrolled for benefits”):
• You are eligible to enroll in the long-term disability (“LTD”) plan. If you are enrolled in LTD coverage, you will maintain your benefit coverage.
• If you have not enrolled in LTD coverage, you are eligible to enroll in the LTD plan during the 60-day period beginning on the first day of the
pay period in which your transition occurs. Your coverage under the LTD plan is effective on your date of hire.
• If you do not enroll in LTD coverage during the 60-day period following your transition, you will only be able to enroll or make changes during
Annual Enrollment or after a status change event and will be required to submit Evidence of Insurability (EOI), which may include undergoing a
medical exam at your own expense before you can be approved for coverage.
– If you are within 12 months of your date of hire and are approved through EOI, your coverage will be effective on the 12-month anniversary
of your date of hire.
– If you are not within 12 months of your date of hire and are approved through EOI, your coverage will be effective the first day of the
following pay period after approval is received from Lincoln.
Page 33—MANAGEMENT ASSOCIATES TRANSFERRING TO FULL-TIME HOURLY (CONTINUED): The following text replaces the fifth bullet
point in the chart (as labeled “More than 60 days after your date of hire):
2021 Summaries of Material Modifications
301
• You are eligible to enroll in the long-term disability (“LTD”) plan. If you are enrolled in LTD coverage, you will maintain your benefit coverage.
• If you have not enrolled in LTD coverage, you are eligible to enroll in LTD during the 60-day period beginning on the first day of the pay period in
which your transition occurs.
– If you are within 12 months of your date of hire, your coverage will be effective on the 12-month anniversary of your date of hire.
– If you are not within 12 months of your date of hire, your coverage will be effective as of the date of your transition.
• If you do not enroll in LTD coverage during the 60-day period following your transition, you will only be able to enroll or make changes during
Annual Enrollment or after a status change event and will be required to submit Evidence of Insurability (EOI), which may include undergoing a
medical exam at your own expense before you can be approved for coverage.
– If you are within 12 months of your date of hire and are approved through EOI, your coverage will be effective on the 12 month anniversary of
your date of hire.
– If you are not within 12 months of your date of hire and are approved through EOI, your coverage will be effective the first day of the
following pay period after approval is received from Lincoln.
Page 36—Qualified Medical Child Support Orders (“QMCSO”): The following text replaces the paragraph at the bottom of the first column:
When the Plan receives a QMCSO, it will apply the following rules:
• If the Plan receives a QMCSO when you are eligible but prior to you satisfying your initial waiting period for medical coverage, the order will be
put into effect when your initial waiting period is satisfied.
• If you are ineligible for coverage when the Plan receives a QMCSO, the order will be rejected.
• If you are ineligible for coverage when the plan receives a QMCSO but subsequently become eligible, the Plan requires a new QMCSO before
coverage for your dependent can take effect.
• If you are eligible for coverage when the Plan receives a QMCSO and you lose eligibility, and then subsequently regain eligibility, the Plan
requires a new QMCSO before coverage for your dependent can take effect.
• If you are eligible for coverage when the Plan receives a QMCSO, then become ineligible and then subsequently regain eligibility, the Plan
requires a new QMCSO before coverage for your dependent can take effect.
• If you are eligible for coverage and have a QMCSO in effect, then terminate, then are rehired and become eligible again, the Plan requires a new
QMCSO before coverage can take effect.
When the third-party administrator enforces coverage for a court-ordered dependent, information regarding the dependent is shared only with the
legal custodian. If you have questions, contact Medical Support Services at 877-930-5607.
See also the section titled Changes Affecting Multiple Locations in the 2020 Associate Benefits Book, earlier in this SMM, for additional changes in the
Eligibility and enrollment chapter.
THE MEDICAL PLAN
Pages 44-91 of the 2020 Associate Benefits Book
Page 46—Changes to Plan Options Available in Certain Regions: Plan terms are changed in certain medical plan options available in three
geographic areas. The section titled National plan options is replaced with the following:
National plan options
The charts on the following pages summarize the coverage offered under the AMP coverage options.
The national plan options under the AMP are the Premier Plan, the Contribution Plan, and the Saver Plan. Under each of these national plan options,
plan terms in most areas nationwide are summarized in the first chart that immediately follows, titled Walmart plans offered nationwide.
If you participate in one of the national plan options and your work location is within one of three geographic areas, as detailed below, each
national plan option available to you has terms that are different from the same national plan option available to associates with work locations
outside of these three areas. Different terms apply if you work in one of the following areas:
• Central Florida (including Orlando and Tampa)
– Counties within this area are Brevard, Citrus, Hernando, Hillsborough, Lake, Manatee, Marion, Orange, Osceola, Pasco, Pinellas, Polk,
norhern Sarasota (Sarasota area only), Seminole, Sumter, and Volusia
• Dallas/Fort Worth
– Counties within this area are Collin, Dallas, Denton, Ellis, Hunt, Johnson, Kaufman, Parker, Rockwall, Tarrant, and Wise (the Contribution Plan
is available only in limited work locations in this area)
• Northwest Arkansas
– Counties within this area are Benton, Madison, and Washington
References throughout this chapter to central Florida, Dallas/Fort Worth, or northwest Arkansas are references to these listed counties, respectively.
The terms of the Premier Plan, Contribution Plan, and Saver Plan options available in central Florida, Dallas/Fort Worth, and northwest Arkansas are
summarized in the charts titled, respectively, Central Florida, Dallas/Fort Worth, and Northwest Arkansas, which follow the chart on the next page.
Page 47-49—Medical plan summary charts: Replace the charts on page 47, 48, and 49 with the following:

2021 Summaries of Material Modifications
302
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
WALMART PLANS OFFERED NATIONWIDE
If your work location is in central Florida, Dallas/For Worh, or norhwest Arkansas, refer to the chars on the following pages.
Premier Plan Contribution Plan Saver Plan
Annual deductible
(Individual/Family)
• Network
• Out-of-network
$2,750/$5,500
$5,500/$11,000
$1,750/$3,500
$3,500/$7,000
$3,000/$6,000
$6,000/$12,000
Walmar-provided funds
(Individual/Family)
N/A
$250/$500
Maximum company
contribution to HRA
$350/$700
Maximum company matching
contribution to HSA
Annual out-of-pocket maximum
(Individual/Family)
• Network
• Out-of-network
$6,850/$13,700
None
$6,850/$13,700
None
$6,650/$13,300
None
Eligible preventive care
• Network
• Non-network
100% (no deductible)
50% (no deductible)
100% (no deductible)
50% (no deductible)
100% (no deductible)
50% (no deductible)
Doctor visits (provider’s office or telehealth)
Including routine same-day diagnostic tests
perormed in doctor’s office
Primary care
• Network
• Non-network
Specialist
• Network
• Non-network
100% after $35 copay
50% after deductible
100% after $75 copay
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Telehealth video visits through
Doctor On Demand
100% after $4* copay 100% after $4* copay
100% after deductible
and $4* copay
*The $4 Doctor On Demand copay is waived for the duration of the COVID-19 National Emergency. In addition, Saver Plan paricipants will not be
required to first meet their annual deductible before utilizing Doctor On Demand services throughout 2021.
Urgent care
• Network
• Non-network
100% after $75 copay
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Diagnostic tests
All nonpreventive tests ordered or perormed
outside a doctor’s office
• Network
• Non-network
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Advanced imaging
MRI, CT scans
• Alternate network
• Network
• Non-network
75% after deductible
50% after deductible
50% after deductible
75% after deductible
50% after deductible
50% after deductible
75% after deductible
50% after deductible
50% after deductible
Hospitalization
Inpatient & outpatient care
• Network
• Non-network
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Behavioral health
Inpatient & outpatient (facility)
• Network
• Non-network
Outpatient (provider’s office or telehealth)
• Network
• Non-network
75% after deductible
50% after deductible
100% after $35 copay
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Emergency care through emergency room visit
• Network
• Non-network
100% after deductible and $300 copay
For information regarding non-network emergency room coverage, see later in chapter.
Pharmacy See The pharmacy benefit chapter
Centers of Excellence See the Centers of Excellence section of this chapter
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic and Walmar Health section of this chapter

2021 Summaries of Material Modifications
303
CENTRAL FLORIDA
Premier Plan Contribution Plan Saver Plan
Annual deductible
(Individual/Family)
• Network preferred & nonpreferred
• Out-of-network
$2,750/$5,500
$5,500/$11,000
$1,750/$3,500
$3,500/$7,000
$3,000/$6,000
$6,000/$12,000
Walmar-provided funds
(Individual/Family)
N/A
$250/$500
Maximum company
contribution to HRA
$350/$700
Maximum company matching
contribution to HSA
Annual out-of-pocket maximum
(Individual/Family)
• Network preferred & nonpreferred
• Out-of-network
$6,850/$13,700
None
$6,850/$13,700
None
$6,650/$13,300
None
Eligible preventive care
• Network preferred
• Network nonpreferred & non-network
100% (no deductible)
50% (no deductible)
100% (no deductible)
50% (no deductible)
100% (no deductible)
50% (no deductible)
Doctor visits (provider’s office or telehealth)
Including routine same-day diagnostic tests
perormed in doctor’s office
Primary care
• Network preferred
• Network nonpreferred & non-network
Specialist
• Network preferred
• Network nonpreferred & non-network
100% after $35 copay
50% after deductible
100% after $75 copay
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Telehealth video visits through
Doctor On Demand
100% after $4* copay 100% after $4* copay
100% after deductible
and $4* copay
*The $4 Doctor On Demand copay is waived for the duration of the COVID-19 National Emergency. In addition, Saver Plan paricipants will not be
required to first meet their annual deductible before utilizing Doctor On Demand services throughout 2021.
Urgent care
• Network preferred
• Network nonpreferred & non-network
100% after $75 copay
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Diagnostic tests
All nonpreventive tests ordered or perormed
outside a doctor’s office
• Network
• Non-network
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Advanced imaging
MRI, CT scans
• Alternate network
• Network
• Non-network
75% after deductible
50% after deductible
50% after deductible
75% after deductible
50% after deductible
50% after deductible
75% after deductible
50% after deductible
50% after deductible
Hospitalization
Inpatient & outpatient care
• Network
• Non-network
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Behavioral health
Inpatient & outpatient (facility)
• Network
• Non-network
Outpatient (provider’s office or telehealth)
• Network
• Non-network
75% after deductible
50% after deductible
100% after $35 copay
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
75% after deductible
50% after deductible
Emergency care through emergency room visit
• Network
• Non-network
100% after deductible and $300 copay
For information regarding non-network emergency room coverage, see later in chapter.
Pharmacy See The pharmacy benefit chapter
Centers of Excellence See the Centers of Excellence section of this chapter
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic and Walmar Health section of this chapter

2021 Summaries of Material Modifications
304
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
DALLAS/FORT WORTH
The Contribution Plan is available in limited locations in the Dallas/For Worh area.
Premier Plan Contribution Plan Saver Plan
Annual deductible
(Individual/Family)
• Network preferred & nonpreferred
(Network benefits only)
$2,750/$5,500 $1,750/$3,500 $3,000/$6,000
Walmar-provided funds
(Individual/Family)
N/A
$250/$500
Maximum company
contribution to HRA
$350/$700
Maximum company matching
contribution to HSA
Annual out-of-pocket maximum
(Individual/Family)
• Network preferred & nonpreferred
(Network benefits only)
$6,850/$13,700 $6,850/$13,700 $6,650/$13,300
Eligible preventive care
• Network preferred
• Network nonpreferred
• Non-network
100% (no deductible)
50% (no deductible)
No coverage
100% (no deductible)
50% (no deductible)
No coverage
100% (no deductible)
50% (no deductible)
No coverage
Doctor visits (provider’s office or telehealth)
Including routine same-day diagnostic tests
perormed in doctor’s office
Primary care
• Network preferred
• Network nonpreferred
• Non-network
Specialist
• Network preferred
• Network nonpreferred
• Non-network
100% after $35 copay
50% after deductible
No coverage
100% after $75 copay
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
Telehealth video visits through
Doctor On Demand
100% after $4* copay 100% after $4* copay
100% after deductible
and $4* copay
*The $4 Doctor On Demand copay is waived for the duration of the COVID-19 National Emergency. In addition, Saver Plan paricipants will not be
required to first meet their annual deductible before utilizing Doctor On Demand services throughout 2021.
Urgent care
• Network preferred
• Network nonpreferred
• Non-network
100% after $75 copay
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
Diagnostic tests
All nonpreventive tests ordered or perormed
outside a doctor’s office
• Network
• Non-network
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
Advanced imaging
MRI, CT scans
• Alternate network
• Network
• Non-network
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
Hospitalization
Inpatient & outpatient care
• Network
• Non-network
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
Behavioral health
Inpatient & outpatient (facility)
• Network
• Non-network
Outpatient (provider’s office or telehealth)
• Network
• Non-network
75% after deductible
No coverage
100% after $35 copay
No coverage
75% after deductible
No coverage
100% after $35 copay
No coverage
75% after deductible
No coverage
100% after $35 copay
No coverage
Emergency care through emergency room visit
• Network
• Non-network
100% after deductible and $300 copay
For information regarding non-network emergency room coverage, see later in chapter.
Pharmacy See The pharmacy benefit chapter
Centers of Excellence See the Centers of Excellence section of this chapter
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic and Walmar Health section of this chapter

2021 Summaries of Material Modifications
305
NORTHWEST ARKANSAS
Premier Plan Contribution Plan Saver Plan
Annual deductible
(Individual/Family)
• Network
(Network benefits only)
$2,750/$5,500 $1,750/$3,500 $3,000/$6,000
Walmar-provided funds
(Individual/Family)
N/A
$250/$500
Maximum company
contribution to HRA
$350/$700
Maximum company matching
contribution to HSA
Annual out-of-pocket maximum
(Individual/Family)
• Network
(Network benefits only)
$6,850/$13,700 $6,850/$13,700 $6,650/$13,300
Eligible preventive care
• Network
• Non-network
100% (no deductible)
No coverage
100% (no deductible)
No coverage
100% (no deductible)
No coverage
Doctor visits (provider’s office or telehealth)
Including routine same-day diagnostic tests
perormed in doctor’s office
Primary care
• Network
• Non-network
Specialist
• Network
• Non-network
100% after $35 copay
No coverage
100% after $75 copay
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
Telehealth video visits through
Doctor On Demand
100% after $4* copay 100% after $4* copay
100% after deductible
and $4* copay
*The $4 Doctor On Demand copay is waived for the duration of the COVID-19 National Emergency. In addition, Saver Plan paricipants will not be
required to first meet their annual deductible before utilizing Doctor On Demand services throughout 2021.
Urgent care
• Network
• Non-network
100% after $75 copay
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
Diagnostic tests
All nonpreventive tests ordered or perormed
outside a doctor’s office
• Network
• Non-network
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
Advanced imaging
MRI, CT scans
• Alternate network
• Network
• Non-network
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
75% after deductible
50% after deductible
No coverage
Hospitalization
Inpatient & outpatient care
• Network
• Non-network
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
Behavioral health
Inpatient & outpatient (facility)
• Network
• Non-network
Outpatient (provider’s office or telehealth)
• Network
• Non-network
75% after deductible
No coverage
100% after $35 copay
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
75% after deductible
No coverage
Emergency care through emergency room visit
• Network
• Non-network
100% after deductible and $300 copay
For information regarding non-network emergency room coverage, see later in chapter.
Pharmacy See The pharmacy benefit chapter
Centers of Excellence See the Centers of Excellence section of this chapter
Walmar Care Clinic and
Walmar Health
See the Walmar Care Clinic and Walmar Health section of this chapter

2021 Summaries of Material Modifications
306
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Page 50-53—Changes in local plans options: Certain local plan options are discontinued.
• The following local plans are eliminated from the chart listing all plans by name on page 50:
– Emory Local Plan
– Mercy Oklahoma Local Plan
– Mercy St. Louis Local Plan
– St. Luke’s Local Plan
– Select Local Plan
• The plan names Emory, Mercy Oklahoma, Mercy St. Louis, and St. Luke’s are removed from the top row in the chart on page 52.
• The entire chart on page 53, The Select Local Plan, is removed.
Pages 54-65—Detailed descriptions of the AMP options: The following replaces the text on pages 54-65, starting with The Walmart Premier
Plan on page 54 and concluding immediately before The local plans on page 65:
The Walmar Premier Plan
PREMIER PLAN COVERAGE
If your work location is not in central Florida, Dallas/For Worh, or norhwest Arkansas
This section describes coverage under the Premier Plan in all areas except specific geographic areas of central Florida, Dallas/Fort Worth,
and northwest Arkansas. See National Plan options earlier in this chapter for the specific counties that make up these areas. Descriptions
of Premier Plan coverage for each of those areas follow later in this chapter.
The Premier Plan offers you the ability to pay for doctor visits with fixed amounts, called “copayments” or “copays,” as explained below
under Coinsurance, copays, and the out-of-pocket maximum. If you were enrolled in the HRA Plan in 2019 and have a balance in the Health
Reimbursement Account (“HRA”) associated with that plan, you can use the remaining funds to pay for the copay required for doctor’s in-
person or telehealth visits (primary care or specialist), Walmart Care Clinic or Walmart Health, Doctor On Demand, or urgent care through
the end of 2021, provided you remain enrolled in the Premier Plan option.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Premier Plan begins paying a portion of the cost of covered
services. Copays are in addition to the annual deductible and do not count toward the deductible. The Premier Plan has a separate annual
deductible for services provided by network providers and services provided by non-network providers. Amounts you pay toward the network
annual deductible apply toward the out-of-network annual deductible, and vice versa.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the network annual deductible and the out-of-network annual deductible can be met by
any combination of you and your covered dependents, but no benefits are payable for any covered person until the entire applicable annual
deductible is met. The following expenses do not count toward the network or out-of-network annual deductible:
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency
room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services that are in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health will count toward your deductible, subject to other exclusions
in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for network preventive services and certain Centers of Excellence services, and
• Charges for non-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your applicable annual deductible has been
met, until you meet your annual out-of-pocket maximum. See the WALMART PLANS OFFERED NATIONWIDE chart earlier in this chapter for
information about the copayment required for specific covered services.
2021 Summaries of Material Modifications
307
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
applicable annual deductible. The WALMART PLANS OFFERED NATIONWIDE chart shows the percentage that the Plan will pay for each covered
service, which varies depending on whether the services are provided by a network provider or a non-network provider. The remaining portion,
which is your coinsurance, is the share that you are responsible for. If you receive covered services from a non-network provider, you are also
responsible for any amount above the maximum allowable charge. After you meet your out-of-pocket maximum, no coinsurance will be required
for covered services from a network provider. There is no out-of-pocket maximum for covered services from a non-network provider.
The Plan will pay all or a portion of the cost of covered preventive services before you meet your applicable deductible and with no
copayment. If services are provided by a network provider, the Plan will pay 100% of the cost of covered preventive services. If services are
provided by a non-network provider, the Plan will pay 50% of the cost of covered preventive services. The remaining portion, which is your
coinsurance, is the share that you are responsible for. If covered preventive services are provided by a non-network provider, you are also
responsible for any amount above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply
to the annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay
100% of the maximum allowable charge after you have met your network annual deductible, regardless of whether the facility is a network
facility. However, if it is a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility
is a network facility, the Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator
determines that the visit is an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the
emergency room visit is not an “emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have
met your out-of-network deductible and you will be responsible for paying the deductible, the other 50%, and any amount over the maximum
allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and in
the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum for network services, the Plan pays 100% of the cost of covered services from a network
provider for the rest of the calendar year. There is no annual out-of-pocket maximum for services from non-network providers—you are
responsible for paying your share of these charges in full throughout the year. The amounts you pay that apply toward your network annual
out-of-pocket maximum include:
• Network and out-of-network annual deductibles (including amounts paid with remaining HRA funds)
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency
room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for network preventive services and certain Centers of Excellence services
• Charges for non-network preventive services
• Coinsurance when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health will count toward your deductible, subject to other exclusions
in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Premier Plan, you will have an individual out-of-pocket maximum for network expenses of
$6,850. If you add dependents to your coverage, you will have an out-of-pocket maximum for network expenses of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
2021 Summaries of Material Modifications
308
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible network expenses for your entire family are
paid at 100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum. There is no out-of-
pocket maximum for out-of-network expenses.
PREMIER PLAN COVERAGE FOR WORK LOCATIONS IN CENTRAL FLORIDA
The Premier Plan offers you the ability to pay for doctor visits with fixed amounts, called “copayments” or “copays,” as explained below
under Coinsurance, copays, and the out-of-pocket maximum. If you were enrolled in the HRA Plan in 2019 and have a balance in the Health
Reimbursement Account (“HRA”) associated with that plan, you can use the remaining funds to pay for the copay required for in-person or
telehealth doctor’s visits (primary care or specialist), Walmart Care Clinic or Walmart Health, Doctor On Demand, or urgent care through the
end of 2021, provided you remain enrolled in the Premier Plan option.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Premier Plan begins paying a portion of the cost of covered
services. Copays are in addition to the annual deductible and do not count toward the deductible. The Premier Plan has an annual deductible
for network services (preferred and nonpreferred network providers) and a separate annual deductible for non-network services. Amounts
you pay toward the network annual deductible apply toward the out-of-network annual deductible, and vice versa.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered
dependents, but no benefits are payable for any covered person until the entire annual deductible is met.
The following expenses do not count toward the network annual deductible or to the out-of-network annual deductible:
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency
room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for preferred network preventive services and certain Centers of Excellence services, and
• Charges for nonpreferred network preventive services and non-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your applicable annual deductible has been
met, until you meet your annual out-of-pocket maximum. See the CENTRAL FLORIDA chart earlier in this chapter for information about the
copayment required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet
your annual deductible. The CENTRAL FLORIDA chart shows the percentage that the Plan will pay for each covered service, which varies
depending on whether the services are provided by a network provider who is preferred or nonpreferred, or a non-network provider. The
remaining portion, which is your coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum.
If you receive covered services from a non-network provider, you are also responsible for any amount above the maximum allowable charge.
After you meet your out-of-pocket maximum, no coinsurance will be required for covered services from a network provider. There is no out-
of-pocket maximum for covered services from a non-network provider.
The Plan will pay all or a portion of the cost of covered preventive services before you meet your applicable deductible and with no copayment.
If services are provided by a network preferred provider, the Plan will pay 100% of the cost of covered preventive services. If services are
provided by a network nonpreferred provider or non-network provider, the Plan will pay 50% of the cost of covered preventive services. The
remaining portion, which is your coinsurance, is the share that you are responsible for. If covered preventive services are provided by a non-
network provider, you are also responsible for any amount above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the
annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the
maximum allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the
2021 Summaries of Material Modifications
309
Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is
an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be
responsible for paying the deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and
in the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum for network services, the Plan pays 100% of the cost of covered services for the rest of
the calendar year. There is no out-of-pocket maximum for services from non-network providers—you are responsible for paying your share of
these charges in full throughout the year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with remaining HRA funds)
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency
room visits
• Coinsurance for services provided by a network provider (preferred or nonpreferred) or by a non-network provider that the Plan pays as
in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for preferred network preventive services and certain Centers of Excellence services
• Charges for non-network preventive services.
• Coinsurance charges when using non-network providers.
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Premier Plan, you will have an individual out-of-pocket maximum of $6,850. If you add
dependents to your coverage, you will have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at
100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum. There is no out-of-pocket
maximum for out-of-network expenses.
PREMIER PLAN COVERAGE FOR WORK LOCATIONS IN DALLAS/FORT WORTH
The Premier Plan offers you the ability to pay for doctor visits with fixed amounts, called “copayments” or “copays,” as explained below
under Coinsurance, copays, and the out-of-pocket maximum. If you were enrolled in the HRA Plan in 2019 and have a balance in the Health
Reimbursement Account (“HRA”) associated with that plan, you can use the remaining funds to pay for the copay required for in-person or
telehealth doctor’s visits (primary care or specialist), Walmart Care Clinic or Walmart Health, Doctor On Demand, or urgent care through the
end of 2021, provided you remain enrolled in the Premier Plan option.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Premier Plan begins paying a portion of the cost of covered
services. Copays are in addition to the annual deductible and do not count toward the deductible.
2021 Summaries of Material Modifications
310
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered
dependents, but no benefits are payable for any covered person until the entire annual deductible is met.
The following expenses do not count toward the annual deductible:
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency
room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for preferred network preventive services and certain Centers of Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your annual deductible has been met,
until you meet your annual out-of-pocket maximum. See the DALLAS/FORT WORTH chart earlier in this chapter for information about the
copayment required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet
your annual deductible. The DALLAS/FORT WORTH chart shows the percentage that the Plan will pay for each covered service, which varies
depending on whether the services are provided by a network provider who is preferred or nonpreferred. The remaining portion, which is your
coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. Care provided by a non-network
provider is not covered under this plan, except in cases of emergency.
The Plan will pay all or a portion of the cost of covered preventive services provided by a network provider before you meet your network
deductible and with no copayment. If the network provider is preferred, the Plan will pay 100% of the cost of covered preventive services. If
the network provider is nonpreferred, the Plan will pay 50% of the cost of covered preventive services. Preventive services provided by a non-
network provider are not covered under this plan.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the
annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the
maximum allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the
Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is
an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be
responsible for paying the deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and
in the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the Plan pays 100% of the cost of covered services for the rest of the calendar year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with remaining HRA funds)
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider (preferred or nonpreferred) or by a non-network provider that the Plan pays as
in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for preferred network preventive services and certain Centers of Excellence services
2021 Summaries of Material Modifications
311
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including charges for services from non-network providers.
If you choose associate-only coverage under the Premier Plan, you will have an individual out-of-pocket maximum of $6,850. If you add
dependents to your coverage, you will have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at
100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum.
PREMIER PLAN COVERAGE FOR WORK LOCATIONS IN NORTHWEST ARKANSAS
The Premier Plan offers you the ability to pay for doctor visits with fixed amounts, called “copayments” or “copays,” as explained below
under Coinsurance, copays, and the out-of-pocket maximum. If you were enrolled in the HRA Plan in 2019 and have a balance in the Health
Reimbursement Account (“HRA”) associated with that plan, you can use the remaining funds to pay for the copay required for in-person or
telehealth doctor’s visits (primary care or specialist), Walmart Care Clinic or Walmart Health, Doctor On Demand, or urgent care through the
end of 2021, provided you remain enrolled in the Premier Plan option.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Premier Plan begins paying a portion of the cost of covered
services. Copays are in addition to the annual deductible and do not count toward the deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered
dependents, but no benefits are payable for any covered person until the entire annual deductible is met.
The following expenses do not count toward the annual deductible:
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for network preventive services and certain Centers of Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your annual deductible has been met, until you
meet your annual out-of-pocket maximum. See the NORTHWEST ARKANSAS chart earlier in this chapter for information about the copayment
required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
annual deductible. The NORTHWEST ARKANSAS chart shows the percentage that the Plan will pay for each covered service. The remaining
portion, which is your coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. Care provided by a
non-network provider is not covered under this plan, except in cases of emergency.
The Plan will pay 100% of the cost of covered preventive services provided by a network provider before you meet your network deductible,
and with no copayment. Preventive services provided by a non-network provider are not covered under this plan.
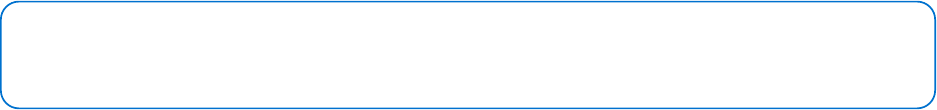
2021 Summaries of Material Modifications
312
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the
annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the
maximum allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the
Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is
an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be
responsible for paying the deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and
in the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the Plan pays 100% of the cost of covered services for the rest of the calendar year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with remaining HRA funds)
• Copays for in-person or telehealth doctor visits, Doctor On Demand, urgent care, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for network preventive services and certain Centers of Excellence services
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including charges for services from non-network providers.
If you choose associate-only coverage under the Premier Plan, you will have an individual out-of-pocket maximum of $6,850. If you add
dependents to your coverage, you will have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at
100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum.
The Walmar Contribution Plan
CONTRIBUTION PLAN COVERAGE
If your work location is not in central Florida, Dallas/For Worh, or norhwest Arkansas
This section describes coverage under the Contribution Plan in all areas except specified geographic areas of central Florida, Dallas/
Fort Worth, and northwest Arkansas. See National plan options earlier in this chapter for the specific counties that make up these areas.
Descriptions of Contribution Plan coverage for each of those areas follow later in this chapter.
The Contribution Plan includes a Health Reimbursement Account (“HRA”). Each year, the company allocates money to the HRA for you and any
covered dependents to use toward your portion of the cost of covered services (meaning those expenses that are your responsibility), including
the annual deductible. You may not contribute your own money to the HRA. The Plan automatically pays your share of eligible medical expenses
(except for prescription drug expenses, which cannot be paid from the HRA) until the HRA funds are exhausted. Amounts paid by the HRA
count toward your annual deductible (both network and non-network) as well as your out-of-pocket maximum.
2021 Summaries of Material Modifications
313
Any balance remaining in your HRA at the end of a calendar year rolls over for use during the next year, provided you remain enrolled in the
Contribution Plan. However, your HRA balance (including your allocated HRA funds for the current year) cannot exceed your network annual
deductible under the Contribution Plan. Each new year’s allocation of HRA funds may be used only for eligible medical expenses for services
rendered within that calendar year. For example, if you enroll in the Contribution Plan and receive an allocation of HRA funds for 2021, you
would be able to use those funds for eligible medical expenses for services rendered in 2021 but not for services rendered prior to 2021 (such
as an expense incurred in 2020 but not processed until 2021). The HRA funds that roll over from a prior year can be used for any eligible
medical expense for services rendered while enrolled in the Contribution Plan.
If you cancel your coverage, lose eligibility, or change from the Contribution Plan to a different coverage option, any funds remaining in your
HRA are forfeited. If you continue coverage in the Contribution Plan through COBRA, your HRA balance remains available to you under the
terms described above and the company will continue to allocate money to your HRA. See the COBRA chapter for more information about
COBRA continuation coverage.
HRA allocations: midyear enrollments or changes
If you are hired midyear and enroll in the Contribution Plan, the company prorates your initial HRA allocation on a monthly basis; your annual
deductible and out-of-pocket maximums are not prorated.
If you have a qualifying event and change your coverage level midyear, such as from associate-only to associate + dependents coverage, the
company adjusts your HRA allocation, annual deductible, and annual out-of-pocket maximum accordingly.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Contribution Plan begins paying a portion of the cost
of covered services. Copays are in addition to the annual deductible and do not count toward the deductible. You can meet your annual
deductible with your company-provided HRA funds from the current year and any rollover HRA funds you may have from a previous year.
When you have used all your company-provided HRA funds, you must use your own funds to meet the remainder of your annual deductible.
The Contribution Plan has a separate annual deductible for services provided by network providers and services provided by non-network
providers. Amounts you pay toward the network annual deductible apply toward the non-network annual deductible, and vice versa.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose coverage
for any dependents as well as for yourself, the network annual deductible and the non-network annual deductible can be met by any combination of
you and your covered dependents, but no benefits are payable for any covered person until the entire applicable annual deductible is met.
The following expenses do not count toward the network or non-network annual deductible:
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health will count toward your deductible, subject to other exclusions
in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for network preventive services and certain Centers of Excellence services, and
• Charges for non-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your applicable annual deductible has been
met, until you meet your annual out-of-pocket maximum. See the WALMART PLANS OFFERED NATIONWIDE chart earlier in this chapter for
information about the copayment required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
applicable annual deductible. The WALMART PLANS OFFERED NATIONWIDE chart shows the percentage that the Plan will pay for each covered
service, which varies depending on whether the services are provided by a network provider or a non-network provider. The remaining portion,
which is your coinsurance, is the share that you are responsible for. If you receive covered services from a non-network provider, you are also
responsible for any amount above the maximum allowable charge. After you meet your out-of-pocket maximum, no coinsurance will be required
for covered services from a network provider. There is no out-of-pocket maximum for covered services from a non-network provider.
The Plan will pay all or a portion of the cost of covered preventive services before you meet your applicable deductible and with no
copayment. If services are provided by a network provider, the Plan will pay 100% of the cost of covered preventive services. If services are
2021 Summaries of Material Modifications
314
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
provided by a non-network provider, the Plan will pay 50% of the cost of covered preventive services. The remaining portion, which is your
coinsurance, is the share that you are responsible for. If covered preventive services are provided by a non-network provider, you are also
responsible for any amount above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply
to the annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay
100% of the maximum allowable charge after you have met your network annual deductible, regardless of whether the facility is a network
facility. However, if it is a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility
is a network facility, the Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator
determines that the visit is an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the
emergency room visit is not an “emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have
met your out-of-network deductible and you will be responsible for paying the deductible, the other 50%, and any amount over the maximum
allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and
in the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the Plan pays 100% of the cost of covered services from a network provider for the rest
of the calendar year. There is no annual out-of-pocket maximum for charges for services from non-network providers—you are responsible for
paying your share of these charges in full throughout the year.
The amounts you pay that apply toward your network annual out-of-pocket maximum include:
• Network and out-of-network annual deductibles (including amounts paid with HRA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for network preventive services and certain Centers of Excellence services
• Charges for non-network preventive services
• Coinsurance when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services that are in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health will count toward your deductible, subject to other exclusions
in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Contribution Plan, you will have an individual out-of-pocket maximum for network expenses of
$6,850. If you add dependents to your coverage, you will have an out-of-pocket maximum for network expenses of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible network expenses for your entire family are
paid at 100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum. There is no out-of-
pocket maximum for out-of-network expenses.
CONTRIBUTION PLAN COVERAGE FOR WORK LOCATIONS IN CENTRAL FLORIDA
The Contribution Plan includes a Health Reimbursement Account (“HRA”). Each year, the company allocates money to the HRA for you and
any covered dependents to use toward your portion of the cost of covered services (meaning those expenses that are your responsibility),
2021 Summaries of Material Modifications
315
including the annual deductible. You may not contribute your own money to the HRA. The Plan automatically pays your share of eligible
medical expenses (except for prescription drug expenses, which cannot be paid from the HRA) until the HRA funds are exhausted. Amounts
paid by the HRA count toward your annual deductible as well as your out-of-pocket maximum.
Any balance remaining in your HRA at the end of a calendar year rolls over for use during the next year, provided you remain enrolled in
the Contribution Plan. However, your HRA balance (including your allocated HRA funds for the current year) cannot exceed your annual
deductible under the Contribution Plan. Each new year’s allocation of HRA funds may be used only for eligible medical expenses for services
rendered within that calendar year. For example, if you enroll in the Contribution Plan and receive an allocation of HRA funds for 2021, you
would be able to use those funds for eligible medical expenses for services rendered in 2021 but not for services rendered prior to 2021 (such
as an expense incurred in 2020 but not processed until 2021). The HRA funds that roll over from a prior year can be used for any eligible
medical expense for services rendered while enrolled in the Contribution Plan.
If you cancel your coverage, lose eligibility, or change from the Contribution Plan to a different coverage option, any funds remaining in your
HRA are forfeited. If you enroll in the Contribution Plan through COBRA coverage, your HRA balance remains available to you under the
terms described above and the company will continue to allocate money to your HRA. See the COBRA chapter for more information about
COBRA continuation coverage.
HRA allocations: midyear enrollments or changes
If you are hired midyear and enroll in the Contribution Plan, the company prorates your initial HRA allocation on a monthly basis; your annual
deductible and out-of-pocket maximums are not prorated.
If you have a qualifying event and change your coverage level midyear, such as from associate-only to associate + dependents coverage, the
company adjusts your HRA allocation, annual deductible, and annual out-of-pocket maximum accordingly.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Contribution Plan begins paying a portion of the cost of
covered services. Copays are in addition to the annual deductible and do not count toward the deductible. The Contribution Plan has an annual
deductible for network services (preferred and nonpreferred network providers) and a separate annual deductible for non-network services.
Amounts you pay toward the network annual deductible apply toward the out-of-network annual deductible, and vice versa.
You can meet your annual deductible with your company-provided HRA funds from the current year and any rollover HRA funds you may have from a
previous year. When you have used all your company-provided HRA funds, you must use your own funds to meet the remainder of your annual deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered
dependents, but no benefits are payable for any covered person until the entire annual deductible is met.
The following expenses do not count toward the network annual deductible or to the out-of-network annual deductible:
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for preferred network preventive services and certain Centers of Excellence services, and
• Charges for nonpreferred network preventive services and non-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your applicable annual deductible has been
met, until you meet your annual out-of-pocket maximum. See the CENTRAL FLORIDA chart earlier in this chapter for information about the
copayment required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
annual deductible. The CENTRAL FLORIDA chart shows the percentage that the Plan will pay for each covered service, which varies depending
on whether the services are provided by a network provider who is preferred or nonpreferred, or a non-network provider. The remaining
portion, which is your coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. If you receive
2021 Summaries of Material Modifications
316
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
covered services from a non-network provider, you are also responsible for any amount above the maximum allowable charge. After you
meet your out-of-pocket maximum, no coinsurance will be required for covered services from a network provider. There is no out-of-pocket
maximum for covered services from a non-network provider.
The Plan will pay all or a portion of the cost of covered preventive services before you meet your applicable deductible and with no copayment.
If services are provided by a network preferred provider, the Plan will pay 100% of the cost of covered preventive services. If services are
provided by a network nonpreferred provider or non-network provider, the Plan will pay 50% of the cost of covered preventive services. The
remaining portion, which is your coinsurance, is the share that you are responsible for. If covered preventive services are provided by a non-
network provider, you are also responsible for any amount above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the
annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the
maximum allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the
Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is
an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be
responsible for paying the deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests,
etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health
care and in the same situation would have thought that not going to the emergency room would result in their life or health being in serious
jeopardy.
After you meet the annual out-of-pocket maximum for network services, the Plan pays 100% of the cost of covered services for the rest of
the calendar year. There is no out-of-pocket maximum for services from non-network providers—you are responsible for paying your share of
these charges in full throughout the year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with HRA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider (preferred or nonpreferred) or by a non-network provider that the Plan pays as in-
network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for preferred network preventive services and certain Centers of Excellence services
• Coinsurance charges when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Contribution Plan, you will have an individual out-of-pocket maximum of $6,850. If you add
dependents to your coverage, you will have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at
100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum. There is no out-of-pocket
maximum for out-of-network expenses.
2021 Summaries of Material Modifications
317
CONTRIBUTION PLAN COVERAGE FOR WORK LOCATIONS IN DALLAS/FORT WORTH
The Contribution Plan is available in a limited number of work locations in the Dallas/Fort Worth area. The Contribution Plan includes a Health
Reimbursement Account (“HRA”). Each year, the company allocates money to the HRA for you and any covered dependents to use toward
your portion of the cost of covered services (meaning those expenses that are your responsibility), including the annual deductible. You may
not contribute your own money to the HRA. The Plan automatically pays your share of eligible medical expenses (except for prescription
drug expenses, which cannot be paid from the HRA) until the HRA funds are exhausted. Amounts paid by the HRA count toward your annual
deductible as well as your out-of-pocket maximum.
Any balance remaining in your HRA at the end of a calendar year rolls over for use during the next year, provided you remain enrolled in
the Contribution Plan. However, your HRA balance (including your allocated HRA funds for the current year) cannot exceed your annual
deductible under the Contribution Plan. Each new year’s allocation of HRA funds may be used only for eligible medical expenses for services
rendered within that calendar year. For example, if you enroll in the Contribution Plan and receive an allocation of HRA funds for 2021, you
would be able to use those funds for eligible medical expenses for services rendered in 2021 but not for services rendered prior to 2021 (such
as an expense incurred in 2020 but not processed until 2021). The HRA funds that roll over from a prior year can be used for any eligible
medical expense for services rendered while enrolled in the Contribution Plan.
If you cancel your coverage, lose eligibility, or change from the Contribution Plan to a different coverage option, any funds remaining in your
HRA are forfeited. If you enroll in the Contribution Plan through COBRA coverage, your HRA balance remains available to you under the
terms described above and the company will continue to allocate money to your HRA. See the COBRA chapter for more information about
COBRA continuation coverage.
HRA allocations: midyear enrollments or changes
If you are hired midyear and enroll in the Contribution Plan, the company prorates your initial HRA allocation on a monthly basis; your annual
deductible and out-of-pocket maximums are not prorated.
If you have a qualifying event and change your coverage level midyear, such as from associate-only to associate + dependents coverage, the
company adjusts your HRA allocation, annual deductible, and annual out-of-pocket maximum accordingly.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Contribution Plan begins paying a portion of the cost
of covered services. Copays are in addition to the annual deductible and do not count toward the deductible. You can meet your annual
deductible with your company-provided HRA funds from the current year and any rollover HRA funds you may have from a previous year.
When you have used all your company-provided HRA funds, you must use your own funds to meet the remainder of your annual deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered
dependents, but no benefits are payable for any covered person until the entire annual deductible is met.
The following expenses do not count toward the annual deductible:
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for preferred network preventive services and certain Centers of Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your annual deductible has been met,
until you meet your annual out-of-pocket maximum. See the DALLAS/FORT WORTH chart earlier in this chapter for information about the
copayment required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet
your annual deductible. The DALLAS/FORT WORTH chart shows the percentage that the Plan will pay for each covered service, which varies
2021 Summaries of Material Modifications
318
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
depending on whether the services are provided by a network provider who is preferred or nonpreferred. The remaining portion, which is your
coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. Care provided by a non-network
provider is not covered under this plan, except in cases of emergency.
The Plan will pay all or a portion of the cost of covered preventive services provided by a network provider before you meet your network
deductible and with no copayment. If the network provider is preferred, the Plan will pay 100% of the cost of covered preventive services. If
the network provider is nonpreferred, the plan will pay 50% of the cost of covered preventive services. Preventive services provided by a non-
network provider are not covered under this plan.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the
annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the
maximum allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the
Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is
an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be
responsible for paying the deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and in
the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the Plan pays 100% of the cost of covered services for the rest of the calendar year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with HRA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider (preferred or nonpreferred) or by a non-network provider that the Plan pays as in-
network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for preferred network preventive services and certain Centers of Excellence services
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including charges for services from non-network providers.
If you choose associate-only coverage under the Contribution Plan, you will have an individual out-of-pocket maximum of $6,850. If you add
dependents to your coverage, you will have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at
100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum.
CONTRIBUTION PLAN COVERAGE FOR WORK LOCATIONS IN NORTHWEST ARKANSAS
The Contribution Plan includes a Health Reimbursement Account (“HRA”). Each year, the company allocates money to the HRA for you and any
covered dependents to use toward your portion of the cost of covered services (meaning those expenses that are your responsibility), including
the annual deductible. You may not contribute your own money to the HRA. The Plan automatically pays your share of eligible medical expenses
(except for prescription drug expenses, which cannot be paid from the HRA) until the HRA funds are exhausted. Amounts paid by the HRA count
toward your annual deductible as well as your out-of-pocket maximum.
2021 Summaries of Material Modifications
319
Any balance remaining in your HRA at the end of a calendar year rolls over for use during the next year, provided you remain enrolled in the
Contribution Plan. However, your HRA balance (including your allocated HRA funds for the current year) cannot exceed your annual deductible
under the Contribution Plan. Each new year’s allocation of HRA funds may be used only for eligible medical expenses for services rendered within
that calendar year. For example, if you enroll in the Contribution Plan and receive an allocation of HRA funds for 2021, you would be able to use
those funds for eligible medical expenses for services rendered in 2021 but not for services rendered prior to 2021 (such as an expense incurred
in 2020 but not processed until 2021). The HRA funds that roll over from a prior year can be used for any eligible medical expense for services
rendered while enrolled in the Contribution Plan.
If you cancel your coverage, lose eligibility, or change from the Contribution Plan to a different coverage option, any funds remaining in your
HRA are forfeited. If you enroll in the Contribution Plan through COBRA coverage, your HRA balance remains available to you under the terms
described above and the company will continue to allocate money to your HRA. See the COBRA chapter for more information about COBRA
continuation coverage.
HRA allocations: midyear enrollments or changes
If you are hired midyear and enroll in the Contribution Plan, the company prorates your initial HRA allocation on a monthly basis; your annual
deductible and out-of-pocket maximums are not prorated.
If you have a qualifying event and change your coverage level midyear, such as from associate-only to associate + dependents coverage, the
company adjusts your HRA allocation, annual deductible, and annual out-of-pocket maximum accordingly.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Contribution Plan begins paying a portion of the cost of covered
services. Copays are in addition to the annual deductible and do not count toward the deductible. You can meet your annual deductible with your
company-provided HRA funds from the current year and any rollover HRA funds you may have from a previous year. When you have used all your
company-provided HRA funds, you must use your own funds to meet the remainder of your annual deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered dependents,
but no benefits are payable for any covered person until the entire annual deductible is met.
The following expenses do not count toward the annual deductible:
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Pharmacy copays/coinsurance (including copay assistance from a third party)
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for network preventive services and certain Centers of Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your annual deductible has been met, until you
meet your annual out-of-pocket maximum. See the NORTHWEST ARKANSAS chart earlier in this chapter for information about the copayment
required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
annual deductible. The NORTHWEST ARKANSAS chart shows the percentage that the Plan will pay for each covered service. The remaining
portion, which is your coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. Care provided by
a non-network provider is not covered under this plan, except in cases of emergency.
The Plan will pay 100% of the cost of covered preventive services provided by a network provider before you meet your network deductible, and
with no copayment. Preventive services provided by a non-network provider are not covered under this plan.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met your
annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the annual
deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the maximum
allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is a non-network
facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the Plan will pay 100%

2021 Summaries of Material Modifications
320
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is an “emergency.” If the
facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an “emergency,” the AMP
will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be responsible for paying the
deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and in
the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the Plan pays 100% of the cost of covered services for the rest of the calendar year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with HRA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network, and
• Pharmacy copays/coinsurance.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for network preventive services and certain Centers of Excellence services
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including charges for services from non-network providers.
If you choose associate-only coverage under the Contribution Plan, you will have an individual out-of-pocket maximum of $6,850. If you add
dependents to your coverage, you will have an out-of-pocket maximum of $13,700 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,850.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses are
paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,700, which
is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the family
out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at 100% for
the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum.
The Walmar Saver Plan
SAVER PLAN COVERAGE
If your work location is not in central Florida, Dallas/For Worh, or norhwest Arkansas
This section describes coverage under the Saver Plan in all areas except specific geographic areas of central Florida, Dallas/Fort Worth,
and northwest Arkansas. See National plan options earlier in this chapter for the specific counties that make up these areas. Descriptions
of Saver Plan coverage for each of those areas follow later in this chapter.
If you enroll in the Saver Plan and contribute to a Health Savings Account (“HSA”), the company matches your payroll deductions into your HSA,
dollar-for-dollar up to $350 if you have individual coverage or $700 if you have family coverage. Combined contributions to your HSA (your own
and the company’s) cannot exceed the 2021 annual IRS limit of $3,600 for individual coverage or $7,200 for family coverage, plus a $1,000 catch-
up contribution if you are age 55 or over.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Saver Plan begins paying a portion of the cost of covered
services. Copays are in addition to the annual deductible and do not count toward the deductible. The Saver Plan has a separate annual deductible
for services provided by network providers and services provided by non-network providers. Amounts you pay toward the network annual
deductible apply toward the out-of-network annual deductible, and vice versa.
2021 Summaries of Material Modifications
321
Preventive care services, as described in the Preventive care program section later in this chapter, are covered even if you have not met the
annual deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose coverage
for any dependents as well as for yourself, the network annual deductible and the out-of-network annual deductible can be met by any combination
of you and your covered dependents, but no benefits are payable for any covered person until the entire applicable annual deductible is met.
You can choose to use money in your HSA to pay expenses that are subject to the annual deductible, or you can pay them out of your own pocket
and save your HSA money for future expenses.
If you enroll in the Saver Plan, you generally must pay full cost for prescriptions until you meet your network annual deductible. The exception is
medications on the OptumRx list of approved preventive medications, which are not subject to the Saver Plan’s network annual deductible—you
can purchase these medications at the appropriate copay or coinsurance level even if you have not met the network annual deductible. In addition,
certain over-the-counter drugs are available at 100% coverage if you obtain a prescription, even if you have not satisfied your deductible. See The
pharmacy benefit chapter for details. With the exception of these charges for approved preventive medications, pharmacy charges under the Saver
Plan apply toward your network annual deductible and out-of-pocket maximum.
The following expenses do not count toward the network or out-of-network annual deductible:
• Copays for preventive medications not subject to the annual deductible
• Discounts, coupons, pharmacy discount programs or similar arrangements provided by drug manufacturers or pharmacies to assist you in purchasing
prescription drugs (including any prescription drug charges paid directly to pharmacies on your behalf through discount programs/coupons)
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health will count toward your deductible, subject to other exclusions
in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for network preventive services and certain Centers of Excellence services, and
• Charges for non-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your applicable annual deductible has been
met, until you meet your annual out-of-pocket maximum. See the WALMART PLANS OFFERED NATIONWIDE chart earlier in this chapter for
information about the copayment required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
applicable annual deductible. The WALMART PLANS OFFERED NATIONWIDE chart shows the percentage that the Plan will pay for each covered
service, which varies depending on whether the services are provided by a network provider or a non-network provider. The remaining portion,
which is your coinsurance, is the share that you are responsible for. If you receive covered services from a non-network provider, you are also
responsible for any amount above the maximum allowable charge. After you meet your out-of-pocket maximum, no coinsurance will be required
for covered services from a network provider. There is no out-of-pocket maximum for covered services from a non-network provider.
The Plan will pay all or a portion of the cost of covered preventive services before you meet your applicable deductible and with no copayment.
If services are provided by a network provider, the Plan will pay 100% of the cost of covered preventive services. If services are provided by a
non-network provider, the Plan will pay 50% of the cost of covered preventive services. The remaining portion, which is your coinsurance, is the
share that you are responsible for. If covered preventive services are provided by a non-network provider, you are also responsible for any amount
above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met your
annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the annual
deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the maximum
allowable charge after you have met your network annual deductible, regardless of whether the facility is a network facility. However, if it is a non-
network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the Plan will pay
100% after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is an “emergency.”
If the facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an “emergency,” the
AMP will pay 50% of the maximum allowable charge for covered services after you have met your out-of-network deductible and you will be
responsible for paying the deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
2021 Summaries of Material Modifications
322
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and in
the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum for network services, the Plan pays 100% of the cost of covered services from a network
provider for the rest of the calendar year. There is no annual out-of-pocket maximum for services from non-network providers—you are
responsible for paying your share of these charges in full throughout the year.
The amounts you pay that apply toward your network annual out-of-pocket maximum include:
• Network and out-of-network annual deductibles (including amounts paid with HSA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network
• Pharmacy copays/coinsurance, and
• Pharmacy charges before your annual deductible is met.
Your network annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not
count toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for network preventive services and certain Centers of Excellence services
• Charges for non-network preventive services
• Coinsurance when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health will count toward your deductible, subject to other exclusions
in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Saver Plan, you will have an individual out-of-pocket maximum for network expenses of
$6,650. If you add dependents to your coverage, you will have an out-of-pocket maximum for network expenses of $13,300 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,650.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,300,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible network expenses for your entire family are
paid at 100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum. There is no out-of-
pocket maximum for out-of-network expenses.
SAVER PLAN COVERAGE FOR WORK LOCATIONS IN CENTRAL FLORIDA
If you enroll in the Saver Plan and contribute to a Health Savings Account (“HSA”), the company matches your payroll deductions into your
HSA, dollar-for-dollar up to $350 if you have individual coverage or $700 if you have family coverage. Combined contributions to your HSA
(your own and the company’s) cannot exceed the 2021 annual IRS limit of $3,600 for individual coverage or $7,200 for family coverage, plus a
$1,000 catch-up contribution if you are age 55 or over.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Saver Plan begins paying a portion of the cost of your
covered services. Copays are in addition to the annual deductible and do not count toward the deductible. The Saver Plan has an annual
deductible for network services (preferred and nonpreferred network providers) and a separate annual deductible for non-network services.
Amounts you pay toward the network annual deductible apply toward the out-of-network annual deductible, and vice versa.
Preventive care services, as described in the Preventive care program section later in this chapter, are covered even if you have not met the
annual deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered
dependents, but no benefits are payable for any covered person until the entire annual deductible is met.
You can choose to use money in your HSA to pay expenses that are subject to the annual deductible, or you can pay them out of your own
pocket and save your HSA money for future expenses.
2021 Summaries of Material Modifications
323
If you enroll in the Saver Plan, you generally must pay full cost for prescriptions until you meet your annual deductible. The exception is
medications on the OptumRx list of approved preventive medications, which are not subject to the Saver Plan’s annual deductible—you can
purchase these medications at the appropriate copay or coinsurance level even if you have not met the annual deductible. In addition, certain
over-the-counter drugs are available at 100% coverage if you obtain a prescription, even if you have not satisfied your deductible. See The
pharmacy benefit chapter for details. With the exception of these charges for approved preventive medications, pharmacy charges under the
Saver Plan apply toward your annual deductible and out-of-pocket maximum.
The following expenses do not count toward the network annual deductible or to the out-of-network annual deductible:
• Copays for preventive medications not subject to the annual deductible
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in purchasing
prescription drugs (including any prescription drug charges paid directly to pharmacies on your behalf through discount programs/coupons)
• Amounts in excess of the Plan’s maximum allowable charge that you pay to non-network providers, including amounts paid for emergency
room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP
• Charges paid 100% by the AMP, such as charges for preferred network preventive services and certain Centers of Excellence services, and
• Charges for nonpreferred network preventive services and non-network preventive services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your applicable annual deductible has been
met, until you meet your annual out-of-pocket maximum. See the CENTRAL FLORIDA chart earlier in this chapter for information about the
copayment required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
annual deductible. The CENTRAL FLORIDA chart shows the percentage that the Plan will pay for each covered service, which varies depending
on whether the services are provided by a network provider who is preferred or nonpreferred, or a non-network provider. The remaining
portion, which is your coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. If you receive
covered services from a non-network provider, you are also responsible for any amount above the maximum allowable charge. After you
meet your out-of-pocket maximum, no coinsurance will be required for covered services from a network provider. There is no out-of-pocket
maximum for covered services from a non-network provider.
The Plan will pay all or a portion of the cost of covered preventive services before you meet your applicable deductible and with no copayment.
If services are provided by a network preferred provider, the Plan will pay 100% of the cost of covered preventive services. If services are
provided by a network nonpreferred provider or non-network provider, the Plan will pay 50% of the cost of covered preventive services. The
remaining portion, which is your coinsurance, is the share that you are responsible for. If covered preventive services are provided by a non-
network provider, you are also responsible for any amount above the maximum allowable charge.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met
your annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the
annual deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the
maximum allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is
a non-network facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the
Plan will pay 100% after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is
an “emergency.” If the facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an
“emergency,” the AMP will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be
responsible for paying the deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and
in the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum for network services, the Plan pays 100% of the cost of covered services for the rest of
the calendar year. There is no out-of-pocket maximum for services from non-network providers—you are responsible for paying your share of
these charges in full throughout the year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with HSA funds)
2021 Summaries of Material Modifications
324
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network
• Pharmacy copays/coinsurance, and
• Pharmacy charges before your annual deductible is met.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for preferred network preventive services and certain Centers of Excellence services
• Charges for non-network preventive services
• Coinsurance charges when using non-network providers
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP.
If you choose associate-only coverage under the Saver Plan, you will have an individual out-of-pocket maximum of $6,650. If you add
dependents to your coverage, you will have an out-of-pocket maximum of $13,300 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,650.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses
are paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,300,
which is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the
family out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at
100% for the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum. There is no out-of-pocket
maximum for out-of-network expenses.
SAVER PLAN COVERAGE FOR WORK LOCATIONS IN DALLAS/FORT WORTH
If you enroll in the Saver Plan and contribute to a Health Savings Account (“HSA”), the company matches your payroll deductions into your
HSA, dollar-for-dollar up to $350 if you have individual coverage or $700 if you have family coverage. Combined contributions to your HSA
(your own and the company’s) cannot exceed the 2021 annual IRS limit of $3,600 for individual coverage or $7,200 for family coverage, plus a
$1,000 catch-up contribution if you are age 55 or over.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Saver Plan begins paying a portion of the cost of your covered
services. Copays are in addition to the annual deductible and do not count toward the deductible.
Preventive care services, as described in the Preventive care program section later in this chapter, are covered even if you have not met the
annual deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered
dependents, but no benefits are payable for any covered person until the entire annual deductible is met.
You can choose to use money in your HSA to pay expenses that are subject to the annual deductible, or you can pay them out of your own pocket
and save your HSA money for future expenses.
If you enroll in the Saver Plan, you generally must pay full cost for prescriptions until you meet your annual deductible. The exception is
medications on the OptumRx list of approved preventive medications, which are not subject to the Saver Plan’s annual deductible — you can
purchase these medications at the appropriate copay or coinsurance level even if you have not met the annual deductible. In addition, certain
over-the-counter drugs are available at 100% coverage if you obtain a prescription, even if you have not satisfied your deductible. See The
pharmacy benefit chapter for details. With the exception of these charges for approved preventive medications, pharmacy charges under the
Saver Plan apply toward your annual deductible and out-of-pocket maximum.
The following expenses do not count toward the annual deductible:
• Copays for preventive medications not subject to the annual deductible
2021 Summaries of Material Modifications
325
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in purchasing
prescription drugs (including any prescription drug charges paid directly to pharmacies on your behalf through discount programs/coupons)
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network,
including for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible,
subject to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for preferred network preventive services and certain Centers of Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your annual deductible has been met, until you
meet your annual out-of-pocket maximum. See the DALLAS/FORT WORTH chart earlier in this chapter for information about the copayment
required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet
your annual deductible. The DALLAS/FORT WORTH chart shows the percentage that the Plan will pay for each covered service, which varies
depending on whether the services are provided by a network provider who is preferred or nonpreferred. The remaining portion, which is your
coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. Care provided by a non-network
provider is not covered under this plan, except in cases of emergency.
The Plan will pay all or a portion of the cost of covered preventive services provided by a network provider before you meet your network
deductible and with no copayment. If the network provider is preferred, the Plan will pay 100% of the cost of covered preventive services. If the
network provider is nonpreferred, the Plan will pay 50% of the cost of covered preventive services. Preventive services provided by a non-
network provider are not covered under this plan.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met your
annual deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the annual
deductible. If the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the maximum
allowable charge after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is a non-network
facility, you will still be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the Plan will pay 100%
after you have met your annual deductible, regardless of whether the third-party administrator determines that the visit is an “emergency.” If the
facility is a non-network facility, and the third-party administrator determines that the emergency room visit is not an “emergency,” the AMP
will pay 50% of the maximum allowable charge for covered services after you have met your deductible and you will be responsible for paying the
deductible, the other 50%, and any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and in
the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the Plan pays 100% of the cost of covered services for the rest of the calendar year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with HSA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network
• Pharmacy copays/coinsurance, and
• Pharmacy charges before your annual deductible is met.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count
toward the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for preferred network preventive services and certain Centers of Excellence services
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network, including
for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible, subject
to other exclusions in this list)
2021 Summaries of Material Modifications
326
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including charges for services from non-network providers.
If you choose associate-only coverage under the Saver Plan, you will have an individual out-of-pocket maximum of $6,650. If you add dependents
to your coverage, you will have an out-of-pocket maximum of $13,300 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,650.
Once you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses are
paid at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,300, which
is a combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the family
out-of-pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at 100% for
the rest of the calendar year, even if each individual has not met the individual out-of-pocket maximum.
SAVER PLAN COVERAGE FOR WORK LOCATIONS IN NORTHWEST ARKANSAS
If you enroll in the Saver Plan and contribute to a Health Savings Account (“HSA”), the company matches your payroll deductions into your HSA,
dollar-for-dollar up to $350 if you have individual coverage or $700 if you have family coverage. Combined contributions to your HSA (your own
and the company’s) cannot exceed the 2021 annual IRS limit of $3,600 for individual coverage or $7,200 for family coverage, plus a $1,000 catch-
up contribution if you are age 55 or over.
The annual deductible
Your annual deductible is the amount you must pay each calendar year before the Saver Plan begins paying a portion of the cost of your covered
services. Copays are in addition to the annual deductible and do not count toward the deductible.
Preventive care services, as described in the Preventive care program section later in this chapter, are covered even if you have not met the
annual deductible.
The amount of your annual deductible is based on whether you are covering just yourself or any eligible dependents as well. If you choose
coverage for any dependents as well as for yourself, the annual deductible can be met by any combination of you and your covered dependents,
but no benefits are payable for any covered person until the entire annual deductible is met.
You can choose to use money in your HSA to pay expenses that are subject to the annual deductible, or you can pay them out of your own pocket
and save your HSA money for future expenses.
If you enroll in the Saver Plan, you generally must pay full cost for prescriptions until you meet your annual deductible. The exception is medications on the
OptumRx list of approved preventive medications, which are not subject to the Saver Plan’s annual deductible — you can purchase these medications at
the appropriate copay or coinsurance level even if you have not met the annual deductible. In addition, certain over-the-counter drugs are available at 100%
coverage if you obtain a prescription, even if you have not satisfied your deductible. See The pharmacy benefit chapter for details. With the exception of these
charges for approved preventive medications, pharmacy charges under the Saver Plan apply toward your annual deductible and out-of-pocket maximum.
The following expenses do not count toward the annual deductible:
• Copays for preventive medications not subject to the annual deductible
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in purchasing
prescription drugs (including any prescription drug charges paid directly to pharmacies on your behalf through discount programs/coupons)
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network, including
for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible, subject
to other exclusions in this list)
• Charges for services not covered by the AMP, and
• Charges paid 100% by the AMP, such as charges for network preventive services and certain Centers of Excellence services.
Coinsurance, copayments, and the out-of-pocket maximum
For covered services subject to a copayment, you must continue to pay the copayment, even after your annual deductible has been met, until you
meet your annual out-of-pocket maximum. See the NORTHWEST ARKANSAS chart earlier in this chapter for information about the copayment
required for specific covered services.
For covered services not subject to a copayment, you will be required to share the cost of covered services with the Plan after you meet your
annual deductible. The NORTHWEST ARKANSAS chart shows the percentage that the Plan will pay for each covered service. The remaining
portion, which is your coinsurance, is the share that you are responsible for until you meet your annual out-of-pocket maximum. Care provided by
a non-network provider is not covered under this plan, except in cases of emergency.
2021 Summaries of Material Modifications
327
The Plan will pay 100% of the cost of covered preventive services provided by a network provider before you meet your network deductible, and
with no copayment. Preventive services provided by a non-network provider are not covered under this plan.
The emergency room copay is $300 per visit. This copay is in addition to your annual deductible and must be paid even after you have met your annual
deductible. The AMP will pay only the maximum allowable charge for covered services and only covered services will apply to the annual deductible. If
the third-party administrator determines that the emergency room visit is an “emergency,” the AMP will pay 100% of the maximum allowable charge
after you have met your annual deductible, regardless of whether the facility is a network facility. However, if it is a non-network facility, you will still
be responsible for any amount over the maximum allowable charge. If the facility is a network facility, the Plan will pay 100% after you have met your
annual deductible, regardless of whether the third-party administrator determines that the visit is an “emergency.” If the facility is a non-network
facility, and the third-party administrator determines that the emergency room visit is not an “emergency,” the AMP will pay 50% of the maximum
allowable charge for covered services after you have met your deductible and you will be responsible for paying the deductible, the other 50%, and
any amount over the maximum allowable charge.
The $300 copay is waived if the patient is directly admitted to the hospital from an emergency room, or if the patient dies prior to hospital
admission. Note that the cost-sharing details described above apply to all services provided in the emergency room (physician, facility, tests, etc.).
Generally, the emergency room visit will be considered an “emergency” if an average prudent person with a basic knowledge of health care and in
the same situation would have thought that not going to the emergency room would result in their life or health being in serious jeopardy.
After you meet the annual out-of-pocket maximum, the Plan pays 100% of the cost of covered services for the rest of the calendar year.
The amounts you pay that apply toward your annual out-of-pocket maximum include:
• Annual deductible (including amounts paid with HSA funds)
• Copays for Doctor On Demand, Walmart Care Clinic or Walmart Health, or emergency room visits
• Coinsurance for services provided by a network provider or by a non-network provider that the Plan pays as in-network
• Pharmacy copays/coinsurance, and
• Pharmacy charges before your annual deductible is met.
Your annual out-of-pocket maximum may be met by any combination of covered medical services. Certain expenses, however, do not count toward
the annual out-of-pocket maximum, as listed here:
• Charges paid 100% by the AMP such as charges for network preventive services and certain Centers of Excellence services
• Amounts in excess of the Plan’s maximum allowable charge for services from a non-network provider that the Plan pays as in-network, including
for emergency room services in excess of the Plan’s maximum allowable charge
• Charges for services provided at any Walmart Care Clinic or Walmart Health that is a non-network provider (however, amounts for covered
diagnostic tests performed outside the Walmart Care Clinic or Walmart Health with a network provider will count toward your deductible, subject
to other exclusions in this list)
• Discounts, coupons, pharmacy discount programs, or similar arrangements provided by drug manufacturers or pharmacies to assist you in
purchasing prescription drugs (including prescription drug discount/coupons provided to pharmacies when you fill a prescription), and
• Charges for services not covered by the AMP, including charges for services from non-network providers.
If you choose associate-only coverage under the Saver Plan, you will have an individual out-of-pocket maximum of $6,650. If you add dependents to
your coverage, you will have an out-of-pocket maximum of $13,300 per family.
Regardless of the coverage level you choose, you and each of your covered dependents have an individual out-of-pocket maximum of $6,650. Once
you or any of your covered dependents have incurred charges for covered services up to that amount, that individual’s eligible expenses are paid
at 100% for the rest of the calendar year. If your coverage includes dependents, you have a family out-of-pocket maximum of $13,300, which is a
combination of all family members’ covered expenses. Any combination of two or more family members can contribute to meet the family out-of-
pocket maximum. Once you meet the total family out-of-pocket maximum, eligible expenses for your entire family are paid at 100% for the rest of the
calendar year, even if each individual has not met the individual out-of-pocket maximum.
Pages 66-67—Clarification of maximum allowable charge: Clarifications are made in the MAXIMUM ALLOWABLE CHARGE section, beginning on
page 66. The following new paragraph is added immediately after the first complete paragraph on page 67:
From time to time, and notwithstanding any Plan provisions that state otherwise, the AMP may enter into an agreement with a non-network provider
(directly or indirectly through a third-party administrator) that sets the rate the AMP will pay for a service or supply. In these cases, the MAC will be the
rate established in the agreement with the non-network provider.
In addition, the paragraph in the second column of page 67 beginning “UnitedHealthcare” is replaced with the following:
UnitedHealthcare: The MAC is 125% of Medicare’s maximum allowable charge for voluntary and involuntary out-of-network services unless the provider is in
UnitedHealthcare’s Shared Savings Program (“SSP”). SSP provider charges are paid at a discount. In cases where a Medicare maximum allowable charge is not
published by the Center for Medicare and Medicaid Services for a specific service, UnitedHealthcare uses a gap methodology to calculate the MAC.

2021 Summaries of Material Modifications
328
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Page 68—If your provider leaves the network: In the section titled Your provider network, the paragraph at the bottom of the first column
(continuing to the second column) is replaced with the following:
If your provider leaves the network, your benefit is adjusted accordingly, based on the terms of the medical plan options you have elected. If you
are covered under the Premier Plan, Contribution Plan, or Saver Plan and your work location is not in Dallas/Fort Worth or northwest Arkansas,
services provided by a provider who has left the network are generally treated as non-network services; you may be required to pay any amount
above the maximum allowable charge, or choose another provider in the network. If you are covered under a local plan, or under the Premier
Plan, Contribution Plan, or Saver Plan in Dallas/Fort Worth or northwest Arkansas, no benefit is paid for services received from a non-network
provider, except in cases of emergency. In that case, services provided by a provider who has left the network are not covered under the Plan
except as described in the section titled WHEN NETWORK BENEFITS ARE PAID FOR OUT-OF-NETWORK EXPENSES, on page 68.
Page 70—Preventive care program: The first three paragraphs under Preventive care program are replaced with the following chart:
PLAN
Eligible preventive care services received
from a network provider
Eligible preventive care services received
from a non-network provider
National plan with work location outside of central
Florida, Dallas/For Worh and norhwest Arkansas Covered at 100% Covered at 50%
National plan with work location in norhwest Arkansas,
or
Local plans
Covered at 100%
Not covered
Out-of-pocket costs do not apply toward
your out-of-pocket maximum
National plan with work location in Dallas/For Worh When received from preferred provider:
covered at 100%
When received from nonpreferred
provider: covered at 50%
Out-of-pocket costs apply to out-of-pocket
maximum
Not covered
Out-of-pocket costs do not apply toward
your out-of-pocket maximum
National plan with work location in central Florida When received from preferred provider:
covered at 100%
When received from nonpreferred
provider: covered at 50%
Out-of-pocket costs apply to out-of-pocket
maximum
Covered at 50%
Out-of-pocket costs do not apply toward
your out-of-pocket maximum
Pages 70-72—Preventive care program: The following service is added to the list titled COVERED PREVENTIVE SERVICES FOR ADULTS,
on p. 70:
• Preexposure prophylaxis (“PrEP”) with effective antiretroviral therapy to persons who are at high risk of HIV acquisition.
The following items should be added to the list titled COVERED PREVENTIVE SERVICES FOR WOMEN, INCLUDING PREGNANT
WOMEN, on page 71:
• Aromatase inhibitors are added to the list of “breast cancer risk-reducing prescription medications” for certain women at increased risk of
breast cancer
• Anxiety screening in adolescent and adult women, including those who are pregnant or postpartum
• Diabetes screening for women with a history of gestational diabetes who are not currently pregnant and who have not previously been
diagnosed with type 2 diabetes
• Maternal depression screening for mothers at certain well-child visits
• Perinatal depression counseling interventions or referrals for pregnant and postpartum women who are at increased risk of perinatal
depression
• Urinary incontinence screening annually, and referral for further evaluation and treatment if indicated
Page 72—Flu vaccine: The first three paragraphs under FLU VACCINE PROGRAM are replaced with the following:
An annual flu vaccination is a preventive service and covered according to the terms detailed in the table inserted on page 70 in the section
titled The preventive care program.
Page 75—myAgileLife: The following new section is added following the section titled TELEHEALTH VIDEO VISITS THROUGH DOCTOR
ON DEMAND on page 75:
MYAGILELIFE
As part of myAgileLife, associates who are covered under the AMP will have access to lower copays for certain diabetes-related medications by
enrolling for the diabetes self-care program. This is a voluntary program where incentives for eligible individuals are based on participation in
myAgileLife programs, not based on achieving a health status.
2021 Summaries of Material Modifications
329
The program features a text messaging-based coaching curriculum designed to help participants develop behaviors that support stated
health objectives and outcomes (i.e., medication adherence, diet, exercise, self-monitoring, and provider engagement/interaction as part of
an effective diabetes self-management regimen to reduce A1C, improve quality of life, and avoid unnecessary healthcare utilization).
Eligible participants will include only participants who are current beneficiaries under the AMP, comply with the formulary and sourcing
requirements specified by the Plan, and are active participants in the program.
Page 75—New pilot programs: The following new sections are added immediately before Walmart clinics:
DIGITAL PHYSICAL THERAPY
Physera: Participants with work locations in Alabama and Tennessee have access to a digital physical therapy program through Physera. This app-based
approach offers guidance, treatment, and support from a licensed physical therapist. Whether you want to prevent an injury, recover from one, or just live
without pain, Physera is available as part of your Walmart medical plan and subject to copays, deductible, and coinsurance, as otherwise applicable to physical
therapy telehealth doctor’s visits.
IMC (Integrated Musculoskeletal Care): Participants utilizing the Walmart Centers of Excellence program, administered by Contigo Health (formerly
Health Design Plus), for spine surgery or joint (hip and knee) replacement, have access to digital physical therapy through IMC. This app-based approach
is designed to help participants prior to and after surgical procedures. Services provided by IMC for spine surgery or joint (hip and knee) replacement for
participants in the Centers of Excellence program will be covered at 100%. Due to federal tax law, participants in the Saver Plan must meet their annual
deductible before the 100% benefit can be provided. IMC is not available outside of Centers of Excellence program participation, including when a local
network exception may be granted.
AIRCARE
The Plan expects to add AiRCare care management services in 2021.
The following terms will apply only after AiRCare care management services are added to the AMP:
If you are enrolled in a plan offered by the AMP, you also have the benefit of voluntary care management services through AiRCare, in addition
to the other care management resources described in section titled Helping you manage your health. The goal of all care management resources
available to you under the AMP is to bring consistency to the full range of care and services provided to you as an AMP participant by looking at you
as a whole individual.
AiRCare is a clinical services company offering a data-driven, comprehensive clinical approach to the treatment of emotional and behavioral
health conditions. AiRCare reviews Plan data to identify participants in the AMP who could benefit from emotional and behavioral health support.
AiRCare’s licensed clinicians then proactively reach out to those participants to offer support and counseling, and connect participants with other
Plan benefits, including behavioral health services, and, as appropriate, community resources to augment care.
The AiRCare program will be available only to participants with work locations in Arkansas. You are not required to utilize the services of AiRCare or
engage with an AiRCare licensed clinician that reaches out directly to you. This care management resource is voluntary.
Page 76—Centers of Excellence: The chart at the bottom of page 76 is changed to reflect the following:
If you are enrolled in the Premier Plan, Contribution Plan, or Saver Plan and your work location is other than Dallas/Fort Worth or northwest
Arkansas, as defined in the 2020 Associate Benefits Book, the AMP benefit for hip or knee replacement surgery not performed through the Centers
of Excellence program will be 50% and you will be subject to the out-of-network deductible.
Page 77—Centers of Excellence: The following text is added to the end of the list of bullet points in the first column, following the paragraph
beginning “If you believe you may be a candidate for Centers of Excellence services...”:
• You acknowledge that you, your caregiver, and any visitors must abide by all rules and policies of the hotel and Centers of Excellence facility,
including those that apply to onsite conduct. Failure to do so may result in loss of eligibility for benefits under the Centers of Excellence program.
Page 77—Centers of Excellence out-of-network coverage: The paragraph at the bottom of the second column, beginning “NOTE,” is replaced
with the following:
NOTE: Under limited circumstances, the AMP provides out-of-network coverage for certain procedures otherwise available through the Centers of
Excellence program if you are enrolled in the Premier Plan, Contribution Plan, or Saver Plan and have a work location other than Dallas/Fort Worth or
northwest Arkansas. In this case, you will have a 50% coinsurance and will be subject to the out-of-network deductible. If you are enrolled in the Premier
Plan, Contribution Plan, or Saver Plan and your work location is in Dallas/Fort Worth or northwest Arkansas, or you are enrolled in a local plan, you have
no out-of-network coverage for these procedures.
Page 78—Centers of Excellence out-of-network coverage for hip or knee replacement: The second bullet point in the first column is replaced with the following:
If you have coverage under the Premier Plan, Contribution Plan, or Saver Plan and your work location is in an area other than Dallas/Fort Worth or
northwest Arkansas, and you have your procedure performed by a network provider, the AMP coinsurance is 50% and you will be subject to the
out-of-network deductible before benefits are payable.

2021 Summaries of Material Modifications
330
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
Page 78–Centers of Excellence pre-service exception request: The second paragraph in the second column is replaced with the following:
Decisions not to move forward with spine surgery or hip or knee replacement by the respective Centers of Excellence providers are not subject to
review under this process if the Centers of Excellence provider decides not to treat you based on your refusal to follow the terms and conditions of
the Centers of Excellence Program or determines that the procedure is not appropriate because you refuse to comply with medical restrictions or
requirements, including weight loss, smoking cessation, alcohol cessation, social support, or similar factors.
Page 80—Centers of Excellence requests for organ transplants at facilities other than Mayo Clinic: The first full paragraph in the second column is
replaced with the following:
Transplant denials by Mayo Clinic are not subject to review under this process if Mayo Clinic decides not to treat you based on your refusal to follow
the terms and conditions of the Center of Excellence Program or determines that the transplant is not appropriate because you refuse to comply
with medical restrictions or requirements, including weight loss, smoking cessation, alcohol cessation, social support, or similar factors. Transplant-
related claims where treatment has already been rendered are decided under the regular medical claims and appeals procedures found in the Claims and
appeals chapter.
Page 82—Male sterilization: In the second column, “male sterilization” is removed from the list of services and/or devices that are not included in
the contraceptive benefit. Male sterilization is no longer excluded and is covered under the otherwise applicable Plan terms for doctor visits (not as
preventive care).
Page 85—Video visits: The “video visits” paragraph in the second column on page 85 is replaced in its entirety with the following:
Telehealth visits: Except for Doctor On Demand, telehealth visits with your provider are covered under the same terms as in-person visits and are subject
to the same terms, including cost sharing and coverage based on network or non-network status of the provider.
THE PHARMACY BENEFIT
Pages 92-97 of the 2020 Associate Benefits Book
Page 95—PHARMACY BENEFITS: The summary chart at the top of the page is replaced with the following:
PHARMACY BENEFITS
Generic drugs
Up to 30-day supply
31- to 60-day supply
61- to 90-day supply
High-cost generic drugs are not covered when a
therapeutically equivalent, lower-cost generic is
available.
$4 copay
$8 copay
$12 copay
Filling your prescriptions
• Present your plan ID card at a Walmar or
Sam’s Club pharmacy.
• If you are covered under the Premier Plan,
Contribution Plan, or Saver Plan and your
work location is more than 5 miles from a
Walmar or Sam’s Club pharmacy, you may
also purchase drugs at an OptumRx network
retail pharmacy. (Note, however, that
supplies of generic drugs for greater than
30 days may be purchased only at a Walmar
or Sam’s Club pharmacy.)
• Prescription refills are available after 75% of
your previous prescription has been used.
• See WHEN PRESCRIPTIONS CAN BE
FILLED AT ANY NETWORK PHARMACY
on the previous page for additional
information.
Preferred brand-name drugs
Up to a 30-day supply
Greater of $50 or 25% of allowed cost
Non-preferred brand-name drugs Not covered
Specialty drugs
Available only at Walmar Specialty Pharmacy or
Optum Specialty Pharmacy
Greater of $50 or 20% of allowed cost
Under the Saver Plan: The charges listed above apply after the Saver Plan’s network annual deductible has been met, with the exception of
medications that are on the OptumRx list of approved preventive medications, which are not subject to the deductible. See PREVENTIVE
MEDICATIONS NOT SUBJECT TO THE SAVER PLAN’S NETWORK ANNUAL DEDUCTIBLE later in this chapter for details.
When purchasing mail-order drugs:
• You may purchase mail-order prescriptions through a Walmar/Sam’s Club mail-order pharmacy, regardless of your work location or medical
plan. OptumRx home delivery pharmacy is also an option.
• Your cost for a 90-day supply is three times the cost of a 30-day supply purchased at a Walmar or Sam’s Club pharmacy, as listed above.
• For brand-name drugs, supplies of more than 30 days must be purchased through mail order.
Page 95—HIV prevention: The following new text is added at the bottom of the page, following the section titled
CONTRACEPTIVES FOR WOMEN:
HIV PREVENTION
The AMP covers preexposure prophylaxis (“PrEP”) with effective antiretroviral therapy at 100%, with no deductible, when the
drug is prescribed by a physician to a person at high risk of becoming infected with HIV.

2021 Summaries of Material Modifications
331
HEATH SAVINGS ACCOUNT (HSA)
Pages 98-105 of the 2020 Associate Benefits Book
Pages 102-103—IRS contribution limits for 2021: New HSA contribution limits, set annually by the IRS, will be $3,600 for self-only (associate)
coverage and $7,200 for family coverage.
• Under ANNUAL CONTRIBUTION LIMITS on page 102, the references to $3,550 (individual coverage) and $7,100 (family coverage) are
changed to $3,600 and $7,200 respectively.
• In the chart titled YOUR CONTRIBUTIONS AND THE COMPANY’S CONTRIBUTIONS TO THE HSA on page 102, the references to
$3,550 (associate-only coverage) and $7,100 (family coverage) are changed to $3,600 and $7,200 respectively.
• On page 103, in multiple paragraphs referencing the family contribution limit, $7,100 is changed to $7,200.
Page 104—Eligible expenses: Effective January 1, 2020, the following replaces the paragraph under the heading Paying qualified medical
expenses through your HSA:
When you have an eligible medical expense, you can decide whether to pay out of your pocket or use the funds in your HSA. Some people
use their HSA for current expenses, while others prefer to use the HSA as an account for future health care expenses. Eligible expenses
include health plan deductibles and coinsurance, most medical care and services, dental and vision care, prescription drugs, and over-
the-counter drugs. In addition, amounts paid for certain menstrual care products such as tampons and pads are eligible medical expenses.
These expenses must not already be covered by your medical plan, and health insurance premiums generally do not qualify. Refer to IRS
Publications 969 and 502 at irs.gov for information about qualified medical expenses. You can also find information about qualified medical
expenses on One.Walmart.com and MyHealthEquity.com.
SHORTTERM DISABILITY FOR HOURLY ASSOCIATES
Pages 180-189 of the 2020 Associate Benefits Book
Page 182—Legally mandated plans: Delete the final paragraph in the LEGALLY MANDATED PLANS chart, in the row bearing the subhead
All other states, and replace it with the following:
Associates who work in Washington State, Washington, D.C., and Massachusetts will have the opportunity to enroll in the short-term
disability enhanced plan to supplement the benefits mandated by the state or locality. The amount of the benefit under Walmart’s short-
term disability plans will be reduced by the amount of the mandated benefit Sedgwick estimates you are eligible to receive from the state
or locality, regardless of whether you apply for that legally mandated benefit. The total benefits payable under the Walmart short-term
disability plan to supplement your state or locality benefit will not exceed the level of benefits otherwise payable under the plan. You will
be responsible for providing your award letter from the state or locality to Sedgwick. If Sedgwick overestimated what your mandated
benefit would be, meaning that you were paid less under the Walmart short-term disability plan than you were entitled to, you will be paid
the difference. If Sedgwick underestimated what your mandated benefit would be, meaning that you were paid more under the Walmart
short-term disability plan than you were entitled to, you must repay any amount overpaid to you. See THE PLAN’S RIGHT TO RECOVER
OVERPAYMENT and THE PLAN’S RIGHT TO SALARY/WAGE DEDUCTION in the Claims and appeals chapter. If you do not repay overpaid
amounts in a timely manner, the company may treat the portion of such amounts that were not taxed when paid as taxable wages to you
(reportable on your Form W-2) or, alternatively, deduct such amounts from your paycheck or future disability benefit payments, to the
extent permitted by law.
SALARIED SHORTTERM DISABILITY
Pages 190-197 of the 2020 Associate Benefits Book
Page 192—Legally mandated plans: Delete the LEGALLY MANDATED PLANS chart and replace it with the following:
LEGALLY MANDATED PLANS
eCommerce salaried associates who work in
California
Associates are eligible to paricipate in Walmar’s salaried shor-term disability plan to
supplement their state benefits.
The amount of the benefit under Walmar’s salaried shor-term disability plan will be reduced by
the amount of the legally mandated benefit.
(continued on next page)

2021 Summaries of Material Modifications
332
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
LEGALLY MANDATED PLANS
Associates who work in Washington State,
Washington, D.C., and Massachusetts
The amount of the benefit under Walmar’s salaried shor term disability plan will be reduced by
the amount of the legally mandated benefit Sedgwick estimates that you are eligible to receive
from the state or locality, regardless of whether you apply for that legally-mandated benefit. The
total benefits payable under the Walmar shor term disability plan to supplement your state or
locality benefit will not exceed the level of benefits otherwise payable under the plan. You will
be responsible for providing your award letter from the state or locality to Sedgwick. If Sedgwick
overestimated what your mandated benefit would be, meaning that you were paid less under the
Walmar shor-term disability plan than you were entitled to, you will be paid the difference. If
Sedgwick underestimated what your mandated benefit would be, meaning that you were paid
more under the Walmar shor-term disability plan than you were entitled to, you must repay
any amount overpaid to you. See THE PLAN’S RIGHT TO RECOVER OVERPAYMENT and THE
PLAN’S RIGHT TO SALARY/WAGE DEDUCTION in the Claims and appeals chapter. If you do not
repay overpaid amounts in a timely manner, the company may deduct such amounts from your
paycheck or future disability benefit payments, to the extent permitted by law.
CLAIMS AND APPEALS
Pages 260-279 of the 2020 Associate Benefits Book
The mailing address for Lincoln Financial Group is changed in two places, as shown here:
Page 276, first column: Page 278, first column
Group Benefits Claims
Lincoln Financial Group
Group - Charlotte WM
P.O. Box 2578
Omaha, Nebraska 68172-9688
Group Benefits Claims Appeals Unit
Lincoln Financial Group
Group - Charlotte WM
P.O. Box 2578
Omaha, Nebraska 68172-9688
LEGAL NOTICES FOR THE ASSOCIATES' HEALTH AND WELFARE PLAN
• Medicare and Your Prescription Drug Coverage
• Premium Assistance Under Medicaid and the Children’s Health Insurance Program (CHIP)
• Nondiscrimination Notice: Valued Plan Participant
• Availability of Summary of Health Information
• Women’s Health and Cancer Rights Act
Medicare and your prescription drug coverage
Please read this notice about Medicare and your prescription drug coverage carefully and keep it where you can find it.
This notice has information about your current prescription drug coverage under the Associates’ Health and Welfare Plan (the “Plan”) and
your prescription drug coverage option under Medicare. This information can help you decide whether or not you want to join a Medicare
drug plan. If you are considering joining, you should compare your current coverage, including which drugs are covered at what cost,
with the coverage and costs of the plans offering Medicare prescription drug coverage in your area. It also tells you where to find more
information to help you make decisions about your prescription drug coverage.
There are important things you need to know about your current coverage and Medicare’s prescription drug coverage:
• Medicare prescription drug coverage became available in 2006 to everyone with Medicare. You can get this coverage if you join a Medicare
prescription drug plan or join a Medicare Advantage Plan (like an HMO or PPO) that offers prescription drug coverage. All Medicare
drug plans provide at least a standard level of coverage set by Medicare. Some plans may also offer more coverage for a higher monthly
premium.
• Some of the Walmart prescription drug plans (as described later in this notice under the heading WHICH WALMART PLANS ARE
CONSIDERED CREDITABLE COVERAGE?) are, on average for all Plan participants, expected to pay out as much as the standard Medicare
prescription drug coverage will pay and are therefore considered creditable coverage. If you are a participant in one of these plans, you may
keep your current coverage and not pay a higher premium (a penalty) if you later decide to join a Medicare drug plan.
• Other Walmart plan options (as described later in this notice under the heading WHICH WALMART PLANS ARE CONSIDERED
NON-CREDITABLE COVERAGE?) are, on average for all Plan participants, not expected to pay out as much as the standard Medicare
prescription drug coverage will pay. If you are a participant in one of these plans, your coverage is non-creditable coverage. This is
2021 Summaries of Material Modifications
333
important because for most people enrolled in these plan options, enrolling in Medicare prescription drug coverage means you will get
more help with drug costs than if you had prescription drug coverage exclusively through the Plan. This is also important because it may
mean that you pay a higher premium (a penalty) if you do not join a Medicare drug plan when you first become eligible.
If you have non-creditable coverage under the Plan, it may affect how much you pay for Medicare D drug coverage in the future. When you
become eligible for Medicare D, you should compare your current coverage, including what drugs are covered, with the coverage and cost
of the plans offered by Medicare prescription drug coverage in your area. Read this notice carefully—it explains your options.
CREDITABLE AND NONCREDITABLE COVERAGE
What is the meaning of the term “creditable coverage”? Creditable coverage means that your current prescription drug coverage is, on
average for all Plan participants, expected to pay out as much as the standard Medicare prescription drug coverage will pay. Prescription
drug coverage that does not satisfy this requirement is not creditable coverage.
WHICH WALMART PLANS ARE CONSIDERED CREDITABLE COVERAGE?
• Premier Plan
• Contribution Plan
• Local Plans
• HMO Plans
• eComm PPO Plan
If your coverage is creditable, you can keep your existing coverage and not pay extra if you later decide to enroll in Medicare coverage.
If you are enrolled in any of the Plans listed above, you can choose to join a Medicare prescription drug plan later without paying extra because
you have existing prescription drug coverage that, on average, is as good as Medicare’s coverage.
If you are enrolled in Medicare Part D, you are not eligible to enroll in any of the Plans listed above. If your dependent is enrolled in Medicare
Part D and you are not, you are eligible to enroll in a Walmart medical or HMO plan, but your dependent would not be eligible for coverage.
If you drop your medical coverage with Walmart and enroll in a Medicare prescription drug plan, you and your eligible dependents will
have the option of re-enrolling in the Walmart Plan during Annual Enrollment or with a valid status change event. You should compare
your current coverage, including which drugs are covered, with the coverage and cost of the plans offering Medicare prescription drug
coverage in your area.
WHICH WALMART PLANS ARE CONSIDERED NONCREDITABLE COVERAGE?
The following Plan’s prescription drug coverage is considered non-creditable according to Medicare guidelines:
• Saver Plan
If your coverage is non-creditable, you might want to consider enrolling in Medicare prescription drug coverage or a Walmart creditable
Plan listed above because the coverage you have is, on average for all participants, not expected to pay out as much as the standard
Medicare prescription drug coverage will pay.
WHEN CAN I ENROLL FOR MEDICARE PRESCRIPTION DRUG COVERAGE?
You can join a Medicare drug plan when you first become eligible for Medicare and each year from October 15 through December 7.
If you have creditable prescription drug coverage and you lose it through no fault of your own, you will be eligible for a two-month Special
Enrollment Period (“SEP”) to join a Medicare drug plan.
If you have non-creditable prescription drug coverage and you drop coverage under the Plan, because your coverage is employer-sponsored
group coverage, you will be eligible for a two-month SEP to join a Medicare drug plan. However, you may pay a higher premium (a penalty)
because you did not have creditable coverage under the Plan.
WHEN WILL I PAY A HIGHER PREMIUM A PENALTY TO JOIN A MEDICARE DRUG PLAN?
If you have creditable coverage and drop or lose your coverage under the Plan and do not join a Medicare drug plan within 63 continuous
days after your current coverage ends, you may pay a higher premium (a penalty) to join the Medicare drug plan later.
If you have non-creditable coverage, depending on how long you go without creditable prescription drug coverage, you may pay a penalty to
join a Medicare drug plan.
Starting with the end of the last month that you were first eligible to join a Medicare drug plan but didn’t join, if you go 63 continuous days
or longer without creditable prescription drug coverage, your monthly premium may go up by at least 1% of the Medicare base beneficiary
premium per month for every month that you did not have that coverage. For example, if you go 19 months without creditable coverage,

2021 Summaries of Material Modifications
334
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
your premium may always be at least 19% higher than the Medicare base beneficiary premium. You may have to pay this premium (a penalty)
as long as you have Medicare prescription drug coverage. In addition, you may have to wait until the following Medicare annual enrollment
period beginning in October to join.
WHAT HAPPENS TO YOUR CURRENT COVERAGE IF YOU DECIDE TO JOIN A MEDICARE DRUG PLAN?
If you decide to join a Medicare drug plan, your current coverage under the Associates’ Medical Plan (“AMP”) will be affected. Plan
guidelines restrict you from enrolling in the AMP if you are enrolled in Medicare Part D. If your dependent is enrolled in Medicare Part D and
you are not, you are able to enroll in the AMP, but your dependent would not be eligible for coverage.
If you decide to join a Medicare drug plan and drop your coverage under the Walmart AMP, be aware that you and your dependents will be
able to get your AMP coverage back, but only during Annual Enrollment or due to a status change event.
If you enroll in a Medicare Part D plan and decide within 60 days to switch back to a plan under the Walmart AMP, you will automatically be
re-enrolled for the same coverage you had prior to the status change event. See the Eligibility and enrollment chapter for further details.
FOR MORE INFORMATION ABOUT MEDICARE AND YOUR PRESCRIPTION DRUG COVERAGE
• You will get this notice each year before your Medicare enrollment period.
• If we make a plan change that affects your creditable coverage, you will receive another notice.
• If you need a copy of this notice, you can request one from People Services at 800-421-1362.
ADDITIONAL INFORMATION AVAILABLE
More detailed information about Medicare plans that offer prescription drug coverage is available through the Medicare & You handbook
from Medicare. You may also be contacted directly by Medicare-approved prescription drug plans. You will get a copy of the handbook in the
mail every year from Medicare. You can also get more information about Medicare prescription drug plans from these sources:
• Visit medicare.gov.
• Call your state health insurance assistance program for personalized help. (See your copy of the Medicare & You handbook for its telephone number.)
• Call 800-MEDICARE (800-633-4227). TTY users should call 877-486-2048.
For people with limited income and resources, extra help paying for the Medicare prescription drug plan is available. For more information
about this resource, visit the Social Security Administration online at socialsecurity.gov, or call 800-772-1213 (TTY 800-325-0778).
REMEMBER: Keep this notice. If you enroll in one of the Medicare prescription drug plans, you may need to provide a copy of this
notice when you join to show whether or not you have creditable coverage and therefore whether or not you are required to pay a
higher premium (a penalty).
Premium assistance under Medicaid and the Children’s Health Insurance
Program (CHIP)
If you or your children are eligible for Medicaid or CHIP and you’re eligible for health coverage from Walmart Inc., your state may have a
premium assistance program that can help pay for coverage, using funds from their Medicaid or CHIP programs. If you or your children
aren’t eligible for Medicaid or CHIP, you won’t be eligible for these premium assistance programs but you may be able to buy individual
insurance coverage through the Health Insurance Marketplace. For more information, visit healthcare.gov.
If you or your dependents are already enrolled in Medicaid or CHIP and you live in a state listed below, contact your state Medicaid or CHIP
office to find out if premium assistance is available.
If you or your dependents are NOT currently enrolled in Medicaid or CHIP, and you think you or any of your dependents might be eligible for
either of these programs, contact your state Medicaid or CHIP office or dial 877-KIDS NOW or insurekidsnow.gov to find out how to apply.
If you qualify, ask your state if it has a program that might help you pay the premiums for the Plan.
If you or your dependents are eligible for premium assistance under Medicaid or CHIP, as well as eligible under the Walmart Inc. Plan, the
Plan must allow you and your dependents to enroll in the Plan if you aren’t already enrolled. This is called a “special enrollment” opportunity,
and you must request coverage within 60 days of being determined eligible for premium assistance. If you have questions about enrolling in
your employer plan, contact the Department of Labor at askebsa.dol.gov or call 866-444-EBSA (3272).
If you live in one of the following states, you may be eligible for assistance paying your employer health plan premiums. The following list of
states is current as of July 31, 2020. Contact your state for more information on eligibility.

2021 Summaries of Material Modifications
335
ALABAMA – Medicaid
Website: http://myalhipp.com
Phone: 855-692-5447
ALASKA – Medicaid
The AK Health Insurance Premium Payment Program
Website: http://myakhipp.com
Phone: 866-251-4861
Email: CustomerService@MyAKHIPP.com
Eligibility:http://dhss.alaska.gov/dpa/Pages/medicaid/default.aspx
ARKANSAS – Medicaid
Website: http://myarhipp.com
Phone: 855-MyARHIPP (855-692-7447)
COLORADO – Health First Colorado (Colorado’s Medicaid Program) & Child Health
Plan Plus (CHP+)
Health First Colorado website:
https://www.healthfirstcolorado.com
Health First Colorado Member Contact Center:
800-221-3943 State Relay 711
CHP+: https://www.colorado.gov/pacific/hcpf/child-health-plan-plus
CHP+ Customer Service: 800-359-1991 / State Relay 711
FLORIDA – Medicaid
Website: http://flmedicaidtplrecovery.com/hipp
Phone: 877-357-3268
GEORGIA – Medicaid
Website: https://medicaid.georgia.gov/health-insurance-premium-payment-program-
hipp
Phone: 678-564-1162 ext. 2131
INDIANA – Medicaid
Healthy Indiana Plan for low-income adults 19–64
Website: http://www.in.gov/fssa/hip/
Phone: 877-438-4479
All other Medicaid
Website: http://www.indianamedicaid.com
Phone: 800-403-0864
IOWA – Medicaid
Website: http://dhs.iowa.gov/Hawki
Phone: 800-257-8563
KANSAS – Medicaid
Website: http://www.kdheks.gov/hcf
Phone: 785-296-3512
KENTUCKY – Medicaid
Website: http://chfs.ky.gov
Phone: 800-635-2570
LOUISIANA – Medicaid
Website: http://dhh.louisiana.gov/index.cfm/subhome/1/n/331
Phone: 888-695-2447
MAINE – Medicaid
Website: http://www.maine.gov/dhhs/ofi/public-assistance/index.html
Phone: 800-442-6003
TTY: Maine relay 711
MASSACHUSETTS – Medicaid and CHIP
Website: http://www.mass.gov/eohhs/gov/deparments/masshealth
Phone: 800-862-4840
MINNESOTA – Medicaid
Website: http://mn.gov/dhs/people-we-serve/seniors/health-care/health-care-
programs/programs-and-services/other-insurance.jsp
Phone: 800-657-3739
MISSOURI – Medicaid
Website: http://www.dss.mo.gov/mhd/paricipants/pages/hipp.htm
Phone: 573-751-2005
MONTANA – Medicaid
Website:http://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP
Phone: 800-694-3084
NEBRASKA – Medicaid
Website: http://www.ACCESSNebraska.ne.gov
Phone: 855-632-7633
Lincoln: 402-473-7000
Omaha: 402-595-1178
NEVADA – Medicaid
Medicaid website: https://dhcfp.nv.gov/
Medicaid phone: 800-992-0900
NEW HAMPSHIRE – Medicaid
Website: https://www.dhhs.nh.gov/oii/documents/hipp.htm
Phone: 603-271-5218
Toll-free for HIPP program: 800-852-3345 ext. 5218
NEW JERSEY – Medicaid and CHIP
Medicaid website: http://www.state.nj.us/humanservices/dmahs/clients/medicaid
Medicaid phone: 609-631-2392
CHIP website: http://www.njfamilycare.org/index.html
CHIP phone: 800-701-0710
NEW YORK – Medicaid
Website: https://www.health.ny.gov/health_care/medicaid/
Phone: 800-541-2831
NORTH CAROLINA – Medicaid
Website: https://medicaid.ncdhhs.gov
Phone: 919-855-4100
NORTH DAKOTA – Medicaid
Website: http://www.nd.gov/dhs/services/medicalserv/medicaid
Phone: 844-854-4825
OKLAHOMA – Medicaid and CHIP
Website: http://www.insureoklahoma.org
Phone: 888-365-3742
OREGON – Medicaid
Website: http://healthcare.oregon.gov/Pages/index.aspx
http://www.oregonhealthcare.gov/index-es.html
Phone: 800-699-9075
PENNSYLVANIA – Medicaid
Website: http://www.dhs.pa.gov/provider/medicalassistance/
healthinsurancepremiumpaymenthippprogram/index.htm
Phone: 800-692-7462
RHODE ISLAND – Medicaid and CHIP
Website: http://www.eohhs.ri.gov
Phone: 855-697-4347
or 401-462-0311 (Direct RIte Share Line)
SOUTH CAROLINA – Medicaid
Website: https://www.scdhhs.gov
Phone: 888-549-0820
SOUTH DAKOTA – Medicaid
Website: http://dss.sd.gov
Phone: 888-828-0059
TEXAS – Medicaid
Website: http://gethipptexas.com
Phone: 800-440-0493
UTAH – Medicaid and CHIP
Medicaid website: https://medicaid.utah.gov
CHIP website: http://health.utah.gov/chip
Phone: 877-543-7669
VERMONT– Medicaid
Website: http://www.greenmountaincare.org
Phone: 800-250-8427
VIRGINIA – Medicaid and CHIP
Medicaid/CHIP website:
http://www.coverva.org/programs_premium_assistance.cfm
Medicaid phone: 800-432-5924
CHIP phone: 855-242-8282
WASHINGTON – Medicaid
Website: http://www.hca.wa.gov
Phone: 800-562-3022 ext. 15473
WEST VIRGINIA – Medicaid
Website: http://mywvhipp.com
Phone: 855-MyWVHIPP (855-699-8447)
WISCONSIN – Medicaid and CHIP
Website:
https://www.dhs.wisconsin.gov/publications/p1/p10095.pdf
Phone: 800-362-3002
WYOMING – Medicaid
Website: https://wyequalitycare.acs-inc.com
Phone: 307-777-7531

2021 Summaries of Material Modifications
336
2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
To see if any other states have added a premium assistance program since July 31, 2020, or for more information on special enrollment rights, contact either:
U.S. Department of Labor
Employee Benefits Security Administration
dol.gov/ebsa
866-444-EBSA (3272)
U.S. Department of Health and Human Services
Centers for Medicare & Medicaid Services
cms.hhs.gov
877-267-2323, Menu Option 4, Ext. 61565
Af-Soomaali
Adeegyada Turjumaanka waxaa lagu heli karaa kharash la’aan.
1-800-421-1362.
Español
Los servicios de interpretación están disponibles de manera
gratuita. 1-800-421-1362.
Kiswahili
Huduma za tafsiri zipo bila malipo. 1-800-421-1362.
Română
Serviciile de interpretariat sunt disponibile gratuit. 1-800-421-1362.
Poruguês (Brasil)
Serviços de interprete estão disponíveis grátis. 1-800-421-1362.
Polski Usługi tłumacza dostępne są bez żadnych kosztów.
1-800-421-1362.
Français
Des services d’interprètes sont disponibles sans frais.
1-800-421-1362.
kreyòl ayisye
Gen Sèvis entèprèt ki disponib gratis. 1-800-421-1362.
A Few More Things…
Here are some important legal documents that go with it. You’ll find a couple of notices that talk about your rights as a Plan participant.
You should also share these notices with any family members who are covered under your Plan. If they live in a different household, you can ask for
these notices to be sent to a different address. You and your family members can also ask for a free paper copy of these notices by calling People
Services at 800-421-1362.
Valued Plan Paricipant
THE ASSOCIATES’ HEALTH AND WELFARE PLAN AHWP RESPECTS THE DIGNITY OF EACH INDIVIDUAL WHO PARTICIPATES IN THE PLAN.
The AHWP does not discriminate on the basis of race, color, national origin,
sex, age, or disability and strictly prohibits retaliation against any person
making a complaint of discrimination. Additionally, we gladly provide our
paricipants with language assistance, auxiliary aids, and services at no cost.
We value you as our paricipant, and your satisfaction is imporant to us.
If you need such assistance or have concerns with your Plan services,
please call the number on the back of your plan ID card. If you have any
questions or concerns, please use one of the methods below so that we can
better serve you.
For assistance, call the number on the back of your plan ID card.
To learn about or use our grievance process, contact People Services at
1-800-421-1362.
To file a complaint of discrimination, contact the U.S. Deparment of
Health and Human Services, Office of Civil Rights:
• Phone: 1-800-368-1019 or 1-800-537-7697 (TDD)
• Website: https://ocrporal.hhs.gov/ocr/cp/wizard_cp.jsf
Interpreter Services are available at no cost. 1-800-421-1362.
AVAILABILITY OF SUMMARY OF HEALTH INFORMATION
As an associate, the health benefits available to you represent a significant
component of your compensation package. They also provide imporant
protection for you and your family in the case of illness or injury.
Your plan offers a series of health coverage options. Choosing a health
coverage option is an imporant decision. To help you make an informed
choice, your plan makes available a Summary of Benefits and Coverage
(SBC), which summarizes imporant information about any health coverage
option in a standard format, to help you compare options. The SBC is
available on One.Walmar.com/Benefits. A paper copy is also available, free
of charge, by calling 800-421-1362.
WOMEN’S HEALTH AND CANCER RIGHTS ACT
As required by the Women’s Health and Cancer Rights Act (WHCRA) of
1998, Walmar-provided medical plans provide coverage for:
1. All stages of reconstruction of the breast on which the mastectomy
has been perormed;
2. Surgery and reconstruction of the other breast to produce a
symmetrical appearance; and
3. Prostheses and physical complications of mastectomy, including
lymphedemas, in a manner determined in consultation with the
attending physician and the patient.
Such coverage may be subject to annual deductibles and coinsurance
provisions as may be deemed appropriate and are consistent with those
established for other benefits under the plan or coverage. Written notice
of the availability of such coverage shall be delivered to the paricipant
upon enrollment and annually thereafter.
2021 Summaries of Material Modifications
337

2020 Associate Benefits Book | Questions? Log on to One.Walmart.com or call People Services at 800-421-1362
IF YOU HAVE QUESTIONS ABOUT… WEBSITE PHONE
When you’re eligible for benefits or
howto enroll
One.Walmar.com/Benefits People Services: 800-421-1362
Medical benefits, medical claims, or
caremanagement
One.Walmar.com/Medical Aetna (including Select Local Plan, Banner
Local Plan, and St. Luke’s Local Plan) health
care advisor: 855-548-2387
BlueAdvantage Administrators of Arkansas
health care advisor: 866-823-3790
UnitedHealthcare health care advisor:
888-285-9255
HealthSCOPE Benefits (includes all other
Local Plans): 800-804-1272
Expanded telehealth in MN, CO, and WI:
877-385-8786
Finding a doctor, most areas:
Grand Rounds
Register at:
GrandRounds.com/Walmar
Download the app at App Store or
GooglePlay
Learn about Personal Healthcare
Assistant (NC, SC only):
GrandRounds.com/Walmar
Grand Rounds: 800-941-1384
Personal Healthcare Assistant (NC, SC only):
855-377-2200
Finding a doctor: Central Florida, Dallas/
Ft. Worh, and Norhwest Arkansas,
except the Mercy Arkansas Local Plan
Provider Guide:
One.Walmar.com/ProviderGuide
BlueAdvantage Administrators of Arkansas:
866-823-3790
Doctor On Demand DoctorOnDemand.com/Walmar 800-997-6196
Centers of Excellence One.Walmar.com/COE People Services: 800-421-1362 or your
health care advisor (see above)
Quit Tobacco One.Walmar.com/QuitTobacco Kick Buts: 855-955-1905
Craving to Quit: 866-577-7169
Pharmacy benefits One.Walmar.com/Prescriptions OptumRx: 844-705-7493
Health savings account (HSA)–Saver Plan learn.healthequity.com/walmar/hsa HealthEquity: 866-296-2860
Dental plan One.Walmar.com/Dental Delta Dental: 800-462-5410
Vision plan One.Walmar.com/Vision VSP: 866-240-8390
For more information

For more information
339
IF YOU HAVE QUESTIONS ABOUT… WEBSITE PHONE
Resources for Living One.Walmar.com/RFL 800-825-3555, 24/7
Accident and critical illness insurance One.Walmar.com/Accident
One.Walmar.com/Critical
Allstate Benefits: 800-514-9525
Life, accidental death and
dismemberment (AD&D), and business
travel accident insurance
One.Walmar.com/Life
One.Walmar.com/ADD
Prudential: 877-740-2116
Shor-term disability insurance One.Walmar.com/ShorTermDisability Sedgwick/Lincoln: 800-492-5678
Long-term disability insurance One.Walmar.com/LongTermDisability Lincoln: 800-492-5678
Walmar 401(k) Plan One.Walmar.com/401k
Benefits.ml.com
Bank of America Merrill Lynch:
888-968-4015
Associate Stock Purchase Plan One.Walmar.com/ASPP
ComputerShare.com/Walmar
ComputerShare: 800-438-6278

2020 Associate Benefits Book | Summary Plan Descriptions
Version 4.5 | © 2020 Walmar Inc.
