
A report from the Health Impact Project
Aug 2017
10 Policies to Prevent
and Respond to
Childhood Lead
Exposure
An assessment of the risks communities face and key federal, state, and local solutions
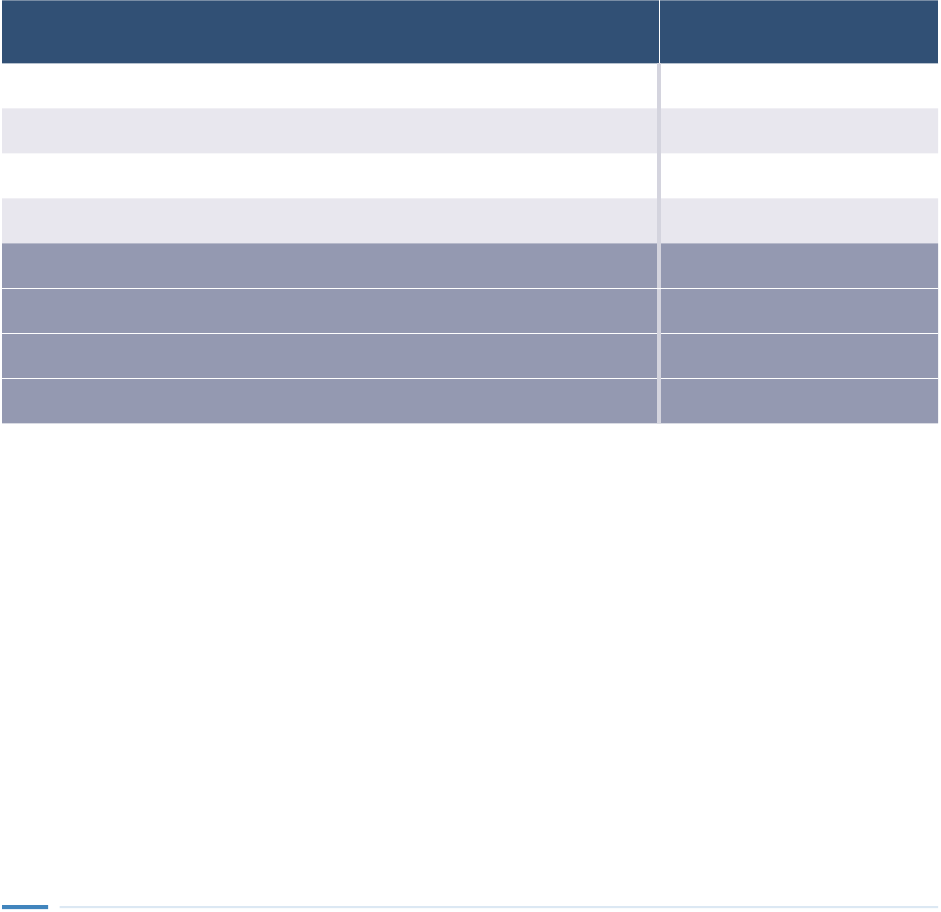
Contents
1 Overview
5 The history of lead in the United States
Lead and the brain 8
Disproportionate Risks and Related Health Disparities 9
12 Methods
Quantitative methods 12
Qualitative methods 14
Study limitations 15
17 Total prevention of lead poisoning
Lead is ubiquitous; past and present uses challenge eradication eorts 17
Lead in Everyday Items 18
Modeling total prevention 20
23 Drinking water
Lead in Water and Infant Health 23
Drinking Water in Schools and Child Care Facilities 25
Residential lead service line replacement 28
Policy in Action: Strategies to Promote Lead Service Line Replacement 29
Policy in Action: Replacing Lead Service Lines 36
38 Lead paint hazards
Residential remediation 38
Policy in Action: Local Lead Paint Laws 40
Policy in Action: State Lead Paint Hazard Control Laws 42
Policy in Action: Financing Lead Paint Hazard Control 46
Lead Paint Hazards and Contaminated Soil at Schools and Child Care Facilities 49
Safe renovation, repair, and painting enforcement 52
57 Air emissions and soil contamination
Lead smelting and battery recycling facilities 58
Superfund sites 59
Policy in Action: Superfund Cleanup 60
Policy in Action: Imposing a Fee on Emitters to Fund Public Lead Remediation Programs 62
Leaded aviation gas 63
Policy in Action: Safe Soil for Schools and Child Care 66
67 Addressing data gaps
69 Supporting children with a history of lead exposure
Blood lead testing 69
Academic and behavioral interventions 70
Policy in Action: Serving Children With a History of Lead Exposure 73
Nutrition 74
Policy in Action: Healthy Diets for Better Long-Term Outcomes 74
79 Recommendations
Priority sources 79
Additional sources 82
Poisoning response 83
Data and research 84
86 Conclusion
87 Glossary
90 Appendix: Methodology
Policy screening process 91
Literature review 92
Case studies 95
Listening sessions 96
Parent conversations 96
Focus groups 96
Quantitative methods 98
Assumptions for modeled policies 106
Uncertainty in modeling lead impacts and remediation policies 109
Qualitative description of uncertainty 110
Bounding exercises to measure uncertainty in eect sizes 112
Quantitative sensitivity analyses 113
118 Endnotes
Figures and tables
Figure 1: Exposure Prevention Eectively Lowers Children’s Lead Levels 6
Figure 2: All Children Face Some Exposure Risk, but Racial and Ethnic Disparities Persist 10
Table 1: Keeping Blood Lead Levels of Children Born in 2018 at Zero Would Generate
$84 Billion in Benefits 20
Figure 3: Most Benefits of Exposure Prevention Accrue for Children Whose Blood Lead Would Otherwise
Be Below 2 μg/dL 21
Table 2: Keeping Blood Lead Levels at Zero Among Children Born in 2018 Would Improve Educational
and Social Outcomes 22
Table 3: Every Dollar Invested in Full Lead Service Line Replacement Would Generate $.42 to $1.33
in Benefits 34
Table 4: Targeting Lead Paint Hazard Control to Older Low-Income Housing Oers the Greatest
Per-Dollar Benefits 45
Table 5: Lead-Safe Renovation Could Yield $3.10 Per $1 Invested 55
Figure 4: Piston Engine Aircraft and Industrial Processes Make Up the Majority of Lead Emissions 57
Table 6: Removing Lead From Aviation Fuel Could Prevent a 5.7% Increase in Children’s Blood Lead 65
Table 7: Providing Both Early and Middle Childhood Interventions Could Yield the Greatest Benefits 77
Table A.1: Summary of Research Methods 90
Table A.2: Strength of Evidence Criteria for Literature Review Used in Quantitative Models 94
Table A.3: Focus Group Participant Demographics and Other Characteristics 97
Table A.4: Summary of Eects of Selected Lead-Exposure Prevention Policies 100
Table A.5: Value of Prevention Tool Sensitivity Analysis Results 114
External experts and reviewers
This report was reviewed by Morri E. Markowitz, M.D., the Children’s Hospital at Montefiore, and professor
of pediatrics, Albert Einstein College of Medicine; and Steven Teutsch, M.D., M.P.H., senior fellow, Leonard D.
Schaeer Center for Health Policy and Economics, University of Southern California, senior fellow, Public
Health Institute, and adjunct professor, UCLA Fielding School of Public Health. Although they found the approach
and methodology to be sound, neither they nor their organizations necessarily endorse the report’s findings
or conclusions.
Robert Wood
Johnson Foundation
Giridhar Mallya, senior policy ocer
Pamela Russo, senior program ocer
Study partners
Child Trends
Vanessa Sacks, research scientist
Kristin Moore, senior scholar and youth development
director
Fadumo Abdi, research analyst
Altarum Institute
George Miller, fellow
Paul Hughes-Cromwick, co-director, Center for
Sustainable Health Spending
Corwin Rhyan, health care research analyst
The Pew Charitable
Trusts
Susan K. Urahn, executive vice president
Allan Coukell, senior director
Health Impact Project
Rebecca Morley, director
Amber Lenhart, senior associate
Gabriela Illa, associate
Mary Jean Brown, consultant
Urban Institute
Steven Martin, senior research associate
Gregory Acs, director, Income and Benefits Policy Center
Trust for America’s Health
Rich Hamburg, executive vice president and chief
operating ocer
Albert Lang, senior communications ocer
National Center for Healthy Housing
David Jacobs, chief scientist
Acknowledgments
The team thanks the following people for their contributions to this report as partners, subject matter experts,
and case study reviewers: Christine Stanik, Altarum Institute; Jonathan Schwabish, Urban Institute; Jonathan
Wilson and Amanda Reddy, National Center for Healthy Housing; Jonathan Cuppett, Water Research Foundation;
Maida Galvez, M.D., Mount Sinai; Todd Grindal, Ed.D., Abt Associates; Cheryl Johnson, People for Community
Recovery; Linda Kite, Healthy Homes Collaborative; Patrick MacRoy, M.A., Environmental Health Strategy Center;
Howard Mielke, Ph.D., Tulane University School of Medicine; Deborah Nagin, M.P.H., New York City Department
of Health and Mental Hygiene; Tom Neltner, J.D., and Ananya Roy, Sc.D., Environmental Defense Fund; Rick
Nevin, ICF International; Ruth Ann Norton and G. Wesley Stewart, Green & Healthy Homes Initiative; Janet
Phoenix, M.D., The George Washington University; Lisa Ragain, Metro Washington Council of Governments; Jay
Schneider, Ph.D., Thomas Jeerson University; Lynn Thorp, Clean Water Action/Clean Water Fund; Steven Via,
American Water Works Association; Kamillah Wood, M.D., Stewards of Aordable Housing for the Future; Laura
Brion, Childhood Lead Action Project; Valerie Charlton, M.D., Lauren Rice, and Rick Kreutzer, M.D., California
Department of Public Health; Julia Robey Christian and Lisa A. Gilmore, Government of the District of Columbia;
Dale Clarkson, Peoria City/County Health Department; Kara Eastman, M.S.W., Omaha Healthy Kids Alliance;
Angie Goodman, Lansing Board of Water and Light; Gary Kirkmire, City of Rochester Inspection and Compliance
Services; Elisabeth Long, Washington State Department of Health; Lisa Smestad, City of Minneapolis; Amber A.
Sturdivant, District of Columbia Department of Energy and Environment; Claire Barnett, M.B.A., Healthy Schools
Network; Don Farquhar, J.D., National Conference of State Legislatures; Perry Gottesfeld, M.P.H., Occupational
Knowledge International; Paul Haan, Healthy Homes Coalition of West Michigan; and Christina Hecht, Ph.D.,
Nutrition Policy Institute at the University of California.
Many thanks also to the concerned citizens, parents, community-based organizations, community health
professionals, landlords, and federal, state, and local agency sta who served as key sources of information
for this project.
Finally, the team thanks current and former Pew colleagues Dan Benderly, Gaby Bonilla, Stefanie Carignan, Erika
Compart, Jennifer V. Doctors, Richard Friend, Tami Holzman, Carol Hutchinson, Bronwen Latimer, Mary Markley,
Bernard Ohanian, Jennifer Peltak, and Peter Wu, as well as our fact check team, for their assistance in preparing
this document for publication.

Advisory Group
This report benefited from the guidance of a formal advisory group with diverse perspectives
and expertise. Although the research team gave substantial weight to the committee’s input
and advice, it retained final authority over and responsibility for the process, findings, and
recommendations. Additionally, although the committee members found the approach and
methodology to be sound, neither they nor their organizations necessarily endorse the findings
or conclusions.
Committee members
Nancy Andrews, M.S., president and chief executive ocer, Low Income Investment Fund
John Bartlett, executive director, Metropolitan Tenants Organization
Jeanne Brooks-Gunn, Ph.D., M.Ed., Virginia and Leonard Marx Professor of Child Development,
Columbia University
Mona Hanna-Attisha, M.D., M.P.H., director, Pediatric Residency Program, Hurley Medical
Center, Michigan State University
Mark Hayward, Ph.D., professor of sociology, The University of Texas at Austin
Ruth Katz, J.D., M.P.H., executive director, the Aspen Institute
Bruce Lanphear, M.D., M.P.H., professor, Simon Fraser University
Marie Lynn Miranda, Ph.D., M.A., provost, Rice University
Brenda Music, co-director, Iowa Parents Against Lead
Damon Music, co-director, Iowa Parents Against Lead
Michèle Prévost, Ph.D., professor, Department of Civil, Geological and Mining Engineering,
Polytechnique Montréal
Queen Zakia Shabazz, director, United Parents Against Lead
Steve Shabazz, parent advocate, United Parents Against Lead
Sara Rosenbaum, J.D., professor, George Washington University
Joshua Sharfstein, M.D., associate dean, Johns Hopkins University
Deborah Cory-Slechta, Ph.D., M.A., professor, Department of Environmental Medicine,
University of Rochester
Lauren Smith, M.D., M.P.H., managing director, Foundation Strategy Group
Alan Woolf, M.D., M.P.H., professor of pediatrics, Harvard Medical School

1
Overview
The ongoing lead contamination crises in Flint, Michigan, and East Chicago, Indiana, as well as the surge of news
reports about lead risks in communities across the country have shone a national spotlight on the problem of
childhood lead exposure. The increased public awareness and scientific evidence that lead poisoning is completely
preventable make this a critical moment for action to protect the nation’s children, enhance their opportunities to
succeed, and reduce costs to taxpayers.
With that background, the Health Impact Project convened a team of researchers to assess the implications of
childhood lead exposure and perform a cost-benefit analysis of various policies to prevent and respond to the
problem. The study team conducted a literature review, case studies, interviews, national listening sessions, focus
groups, and quantitative analyses using models developed by Altarum Institute and by the Brookings Institution,
Child Trends, and Urban Institute. The team included sta from Altarum, Child Trends, Urban Institute, Trust for
America’s Health, the National Center for Healthy Housing, and the Health Impact Project, a collaboration of the
Robert Wood Johnson Foundation and The Pew Charitable Trusts.
Lead’s adverse health impacts have been recognized since at least the second century B.C. Since then, thousands
of studies have concluded that lead has wide-ranging eects on the health of young children and significant costs
to taxpayers. Even at very low levels, lead exposure aects the brain’s ability to control impulses and process
information. Lead-poisoned children are more likely to struggle in school, drop out, get into trouble with the law,
underperform in the workplace, and earn less throughout their lives, independent of other social and economic
factors. The financial consequences of these outcomes include billions of dollars in public spending on special
education, juvenile justice, and other social services.
Despite the evidence, the U.S. lagged many European nations by nearly 50 years in reducing the sources of exposure
to lead. The delay resulted in greater quantities of lead in the environment, higher rates of childhood lead poisoning,
and the need for more resources for remediation. Various federal agencies have imposed restrictions on lead during
the past 40 years, yet lead persists in many places, mainly in drinking water and in existing paint in older homes
and the dust and soil contamination it generates. Many states and communities have implemented laws to address
lead exposure, but those eorts have been fragmented and underfunded. As a result, lead continues to adversely
aect millions of children, particularly those in low-income communities and those of color because of their
disproportionate risk of exposure to sources of lead in older homes and under-resourced neighborhoods.
The study team analyzed existing policies for their impacts on public health and health equity—the concept that
every person should have the same opportunity to be healthy. The eort was guided by a diverse group of advisers
and experts from fields including environmental and public health, child development, economics, housing, health
care, environmental and social justice, and drinking water engineering. In addition, input from stakeholders,
including families whose children have suered the toxic eects of lead, provided valuable insights.
Where economic benefits are estimated, they are referred to as “future benefits”—meaning they are discounted at
a rate of 3 percent per year to account for changes in the value of money over time. The cost-benefit analyses are
based on the lifelong impacts of interventions for a single cohort of U.S. children, those who will be born in 2018.
Where appropriate, the analysis includes benefits that would accrue for additional children born into the same
households within 10 years. In some cases, costs were unavailable so a cost-benefit ratio is not provided.

2
Key findings include:
• Removing leaded drinking water service lines from the homes of children born in 2018 would protect more
than 350,000 children and yield $2.7 billion in future benefits, or about $1.33 per dollar invested.
Of those benefits, about $2.2 billion in higher lifetime earnings, better health, and other gains would accrue
to 272,000 children born in the 2018 cohort, and $550 million would come from protecting the roughly
80,000 other children born into those homes over the next 10 years. The total includes $480 million for the
federal government and $250 million for states and municipalities from health and education savings and
increased tax revenue associated with higher earnings among the cohort. Replacing these lead pipes would
cost an estimated $2 billion.
• Eradicating lead paint hazards from older homes of children from low-income families would provide
$3.5 billion in future benefits, or approximately $1.39 per dollar invested, and protect more than
311,000 children. About $2.8 billion of those benefits would accrue to roughly 244,000 of the 4 million
children in the 2018 cohort. The other $670 million in benefits would accrue from protecting approximately
67,000 additional children born into those homes over the next 10 years. The total benefits include
$630 million in federal and $320 million in state and local health and education savings and increased
revenue. Controlling lead paint hazards would cost $2.5 billion for the 2018 cohort.
• Ensuring that contractors comply with the Environmental Protection Agency’s rule that requires lead-safe
renovation, repair, and painting practices would protect about 211,000 children born in 2018 and provide
future benefits of $4.5 billion, or about $3.10 per dollar spent. This includes $990 million in federal and
$500 million in state and local health and education savings and increased revenue. The eort would cost
about $1.4 billion.
• Eliminating lead from airplane fuel would protect more than 226,000 children born in 2018 who live
near airports, generate $262 million in future benefits, and remove roughly 450 tons of lead from the
environment every year.
• Providing targeted evidence-based academic and behavioral interventions to the roughly 1.8 million children
with a history of lead exposure could increase their lifetime family incomes and likelihood of graduating
from high school and college and decrease their potential for teen parenthood and criminal conviction.
No studies have specifically assessed the eectiveness of such programs for lead-exposed children. However,
research shows that for children at similar developmental risk from trauma, poverty, and other adverse
experiences, certain high-quality interventions can increase the likelihood of earning a high school diploma
and a four-year college degree and reduce the chance of becoming teen parents. The estimated benefits
presume comparable impacts on lead-exposed children.
The costs and benefits outlined in the bullets above are based on a targeted approach to implementing the
interventions, such as focusing on older homes with the highest probability of having lead hazards, and on
populations at greatest risk, including low-income families. These economic calculations do not include emotional
distress or other potentially large costs to families, such as time away from work.
Preventing childhood lead exposure will require significant policy and regulatory action, coordination across levels
of government, and public and private investments, but it has the potential to generate substantial economic
and public health gains in the short and long terms. The maximum potential future benefits of preventing all lead
exposure for the 2018 birth cohort, such that those children’s blood lead levels could be kept from rising above
zero, could reach $84 billion, not including the costs to achieve such total prevention. This figure includes nearly
$18.5 billion for the federal government and $9.6 billion for states in the form of increased revenue and savings to

3
the health care, education, and criminal justice systems. Calculating the cost of such hypothetical total prevention
was beyond the scope of this study, but as shown above, the models for the individual interventions, which together
could address a significant share of children’s exposure risk, do include cost estimates.
No recent conclusive epidemiologic evidence exists on the relative contribution of dierent sources to children’s
blood lead levels,
1
so based on the results of its research, the study team has prioritized policies that the research
literature strongly indicated could have the greatest positive population-wide eect on blood lead levels and could
protect the most children. Secondarily, the team proposes focusing on other sources that contribute to the overall
amount of lead, including nonessential uses of lead, which may cause individual acute cases of lead poisoning, but
account for a smaller proportion of lead in children’s blood overall. Concurrent with eorts to prevent exposure,
the team also encourages the adoption of policies for intervening with children already poisoned by lead and for
improving the data available to policymakers and the public.
The study team recommends:
Priority sources
• Reduce lead in drinking water in homes built before 1986 and other places children frequent. States and
municipalities, with support from federal agencies, should fully replace lead service lines, from street to
structure, that provide drinking water to homes built before the EPA banned their use. The EPA should
strengthen its requirements to reduce the corrosivity of drinking water, improve water sampling protocols,
and create a science-based household water lead action level—the amount that requires intervention—to
help families and communities assess their risks. States and localities should investigate and mitigate drinking
water hazards in schools and child care facilities.
• Remove lead paint hazards from low-income housing built before 1960 and other places children spend
time. According to the Department of Housing and Urban Development, about 3.6 million homes nationwide
that house young children have lead hazards such as peeling paint, contaminated dust, or toxic soil. HUD, the
EPA, and the Centers for Disease Control and Prevention should work with states and local governments to
support replacement of windows coated with lead paint, fix peeling paint, clean up contaminated dust, and
treat toxic soil in and around those homes. States should require school districts and child care facilities to
identify and remediate lead paint hazards.
• Increase enforcement of the federal renovation, repair, and painting rule. The EPA and its state agency
partners should conduct more investigations to ensure that contractors are in compliance with federal
regulations requiring training and certification to minimize dust and debris when working with lead-based
paint. The EPA and states should emphasize enforcement for work done at child care facilities and in housing
built before 1960.
Additional sources
• Reduce lead in food and consumer products. The federal government, through participation in the
international Codex Alimentarius Commission—a cooperative eort of the United Nations and World Health
Organization—should encourage expedited reduction of international limits on lead in foods, particularly those
that young children and babies are likely to consume. Further, where local data indicate that children are being
exposed to lead from sources such as candy, health remedies, or cosmetics, state and local agencies should
target education and outreach to at-risk neighborhoods; support cultural awareness among physicians; and
increase investigation and enforcement of small retailers.

4
• Reduce air lead emissions. The EPA and other federal agencies should collaborate to curtail new discharges by
reducing concentrations of lead into the environment, such as from aviation gas and lead smelting and battery
recycling facilities.
• Clean up contaminated soil. The EPA should collaborate with business to remediate dangerous conditions at
and near facilities that extract lead from batteries and other electronics.
Poisoning response
• Improve blood lead testing among children at high risk of exposure and find and remediate the sources
of their exposure. Federal and state health agencies should work with parents of lead-poisoned children,
providers, Medicaid, and the Children’s Health Insurance Program to remove barriers to blood lead testing and
reporting, and to reduce sources of lead in children’s home environments.
• Ensure access to developmental and neuropsychological assessments and appropriate high-quality
programs for children with elevated blood lead levels. The U.S. Departments of Health and Human Services
and Education and state and local health and education agencies should invest in education and care
programs, and the federal Centers for Medicare & Medicaid Services should increase children’s access to
developmental assessments and neuropsychological testing so that the services provided address each child’s
individual needs.
Data and research
• Improve public access to local data. Federal, state, and local authorities should work together to make lead-
risk data available to families, policymakers, and other stakeholders who need information about sources of
exposure, such as property-specific information on leaded drinking water pipes and lead in the water, dust,
paint, and soil at or near homes, schools, and child care facilities.
• Fill gaps in research to better target state and local prevention and response eorts. Federal, state, and
local agencies and philanthropic organizations should support new studies and conduct their own research to
identify sources of lead exposure and populations at greatest risk.
Policy initiatives such as these, while ambitious, are not without precedent, and this report includes illustrative
case studies from states and municipalities that have tackled significant lead-exposure problems.
The report begins with a brief history of lead in the U.S. and the policies enacted to address it, a discussion of
the impact of lead on children’s brains and the disproportionate risks to low-income children and children of
color, and a description of the study methods and limitations. It then examines policies to prevent exposure,
including interventions focused on lead in drinking water, paint, dust, air emissions, and soil, as well as research
gaps revealed during the study of those policy options. Later sections look at strategies for improving blood
lead testing in children and at nutritional, educational, and behavioral programs to help mitigate the eects of
lead in children already exposed. Each policy discussion includes literature review findings; case studies; input
from stakeholders; potential challenges; and, when possible, costs, benefits, and simulated eects on children’s
lifetime outcomes. The study concludes with a detailed list of actions federal, state, and local policymakers can
take to implement the above recommendations. (See Page 79.)

5
The history of lead in the United States
By the 20th century, lead had permeated every aspect of American life, from air in cities to windows and
plumbing of homes across the country. In 1900, “more than 70 percent of [the nation’s] cities with populations
greater than 30,000 used lead water lines.”
2
Then in 1923, leaded automobile gasoline entered the public market
and quickly surpassed other fuels, becoming one of the most important sources of lead exposure.
3
Further,
between 1900 and 1950, paint containing high concentrations of lead pigments replaced wallpaper as the
primary wall covering in homes.
4
Lead’s harmful eects on children were first documented in Australia during the 1890s, and by the 1920s, several
European nations had adopted laws limiting lead in paint.
5
For example, France, Belgium, and Austria banned
white-lead interior paint in 1909. Then, in 1921, the International Labour Organisation adopted a proposal to
prohibit the use of lead-based paint in all member countries, but the U.S. declined to adopt the rule.
6
During this
same period, public concern led some American towns and cities to prohibit the use of leaded drinking water
lines.
7
In the 1930s, the FDA recognized the need to control potential lead exposure from food and limited the use
of lead-containing substances, such as pesticides.
8
But despite the growing evidence of lead’s toxic eects on children, during the 20th century the Lead Industries
Association aggressively promoted lead as a superior product while downplaying public health risks and
undercutting larger-scale regulatory eorts.
9
Notably, the industry developed model building codes for lead in
plumbing and paint and successfully lobbied for their adoption by federal, state, and municipal governments.
10
Additional federal action lagged until the Clean Air Act of 1970, which regulated air pollution and required that
all cars manufactured in the U.S. after 1975 be built with catalytic converters—emission control devices that
turned out to be incompatible with leaded gas.
11
The 1971 Lead-Based Paint Poisoning Prevention Act, which
prohibited the use of lead paint in government-funded housing, was largely driven by the determined eorts of
the scientific community, whose work would help to shape the next 40 years of federal guidelines and policies
to protect children.
12
In 1973, the EPA announced a phase-out of lead in gasoline, although the process took
more than 20 years.
13
Thanks to key policy actions, including the elimination of leaded gasoline, reductions in
industrial emissions, limits placed on lead in residential paint in 1978, the 1974 Safe Drinking Water Act, the
1986 prohibition against use of lead pipes and plumbing, and a shift in the 1990s to welded (nonsoldered) food
cans, average blood lead levels among U.S. children have declined by about 94 percent from 15 micrograms
per deciliter (μg/dL) in 1976 to 0.86 μg/dL today.
14
(See Figure 1.) In the early 1970s, the U.S. Centers for
Disease Control and Prevention (CDC) called for public health action at a blood lead level of 40 μg/dL. Since
that time the agency has incrementally lowered the threshold for action. In October 2012, the CDC established
a reference value—the level at which a child’s blood lead level is much higher than most children’s and public
health interventions are recommended—of 5 μg/dL and declared, “No safe blood lead level in children has been
identified.”
15
The CDC’s scientific advisers recommended lowering the reference level to 3.5 μg/dL, and agency
ocials were considering the change as of the writing of this report.
16

6
2
4
6
8
10
12
14
16
18
Blood lead level (µg/dL)
1971 Lead-based paint restricted
in federally assisted housing
1973 Phase-out of leaded gasoline begins
2012 CDC updates
recommendations on children’s
blood lead levels
1992 Comprehensive law sets
national strategy for eliminating
lead paint hazards.
1995 Lead-soldered
food cans banned
1999-2001 Standards for lead
in paint, dust and soil created
2000 Federal plan targets
lead-paint hazards
1991 Rules restrict lead and
copper in drinking water
1986 Use of lead
in pipes, solder,
and flux limited
2008 Renovation contractors
required to have lead-paint
safety certification
15
2.7
1.9
1.7
1.8
1.6 1.5 1.5
.97
1.3
1974 1978 1982 1986 1990
1994 1998 2002 2006 2010 2014 2018
1970
1.17
0
1978
• Lead in household paint and
certain children’s products limited
• Air quality standards for lead set
• Protections from lead established
for industrial workers
2017 HUD updates
lead-paint regulations
0
3.6
2.2
1996 Known
lead-paint
hazards must
be disclosed at
sale or lease
of housing
1999 Lead-based
paint in federally
owned and assisted
housing regulated
Sources: Reproduced and modified from Mary Jean Brown & H. Falk, “Toolkit for Establishing Laws to Control the Use of Lead Paint.
Module C.iii. Conducting Blood Lead Prevalence Studies,” Global Alliance to Eliminate Lead Paint (2016); President’s Task Force on
Environmental Health Risks and Safety Risks to Children, “Key Federal Programs to Reduce Childhood Lead Exposures and Eliminate
Associated Health Impacts” (November 2016), https://ptfceh.niehs.nih.gov/features/assets/files/key_federal_programs_to_reduce_
childhood_lead_exposures_and_eliminate_associated_health_impactspresidents_508.pdf
© 2017 The Pew Charitable Trusts
Figure 1
Exposure Prevention Eectively Lowers Children’s Lead Levels
Average blood lead levels in children 1 to 5 and federal policies

7
2
4
6
8
10
12
14
16
18
Blood lead level (µg/dL)
1971 Lead-based paint restricted
in federally assisted housing
1973 Phase-out of leaded gasoline begins
2012 CDC updates
recommendations on children’s
blood lead levels
1992 Comprehensive law sets
national strategy for eliminating
lead paint hazards.
1995 Lead-soldered
food cans banned
1999-2001 Standards for lead
in paint, dust and soil created
2000 Federal plan targets
lead-paint hazards
1991 Rules restrict lead and
copper in drinking water
1986 Use of lead
in pipes, solder,
and flux limited
2008 Renovation contractors
required to have lead-paint
safety certification
15
2.7
1.9
1.7
1.8
1.6 1.5 1.5
.97
1.3
1974 1978 1982 1986 1990
1994 1998 2002 2006 2010 2014 2018
1970
1.17
0
1978
• Lead in household paint and
certain children’s products limited
• Air quality standards for lead set
• Protections from lead established
for industrial workers
2017 HUD updates
lead-paint regulations
0
3.6
2.2
1996 Known
lead-paint
hazards must
be disclosed at
sale or lease
of housing
1999 Lead-based
paint in federally
owned and assisted
housing regulated

8
Despite this progress, U.S. children remain at risk from lead exposure. The CDC found in 2016 that approximately
500,000 children ages 1-5 tested at or above the reference value.
17
Additionally, many federal limits on lead in the
environment have not been updated to reflect new evidence about the eects of low-level exposure, and most
agencies have not set standards to protect unborn babies and pregnant women.
18
For example, in 2016, during
the most recent such review, the EPA opted not to update the 2008 air standards for lead. Standards for paint,
dust, soil, water, and occupational hazards are 15 to 40 years old, despite calls to modernize them, such as from
the EPA’s Science Advisory Board.
19
For example, the EPA’s soil lead standard is 400 parts per million (ppm) for
areas where children play, while, by comparison, California’s guideline is 80 ppm.
Lead and the brain
Very high doses of lead, which are rarely seen in the U.S. today, can cause seizures, coma, and death.
20
However,
even much lower levels, between 3 and 5 μg/dL, can lead to neurologic damage, including impaired memory and
executive function,
21
which is the ability to plan, remember instructions, and juggle multiple tasks. Such levels can
lead to decreased IQ and academic performance and can also cause behavioral problems, such as impulsivity,
hyperactivity, and attention disorders.
22
Some studies suggest that lead exposure may also cause conduct
disorders, depression, anxiety, and withdrawn behavior
23
—the tendency to avoid the unfamiliar, either people,
places, or situations.
An advertisement for leaded paint from 1866.
Photo: Library of Congress

9
The mechanisms by which lead causes harm are complex and not completely understood, but one important
way it is known to aect children’s brains is by mimicking or competing with other metals such as calcium,
zinc, iron, and copper. Young children, particularly from birth to age 6, require large amounts of these essential
metals for growth and development, especially to build brain cells and send signals throughout the nervous
system. The passage of these metals from the blood into the brain is regulated by the blood-brain barrier—
a cellular membrane that selectively allows some substances, such as oxygen, immune cells, and nutrients, to
pass between the bloodstream and the brain.
24
Lead can masquerade as these essential metals, moving across
the barrier, taking the place of important metals in the brain and interfering with the growth of brain cells, which
can lead to changes in the way those cells communicate.
25
Disproportionate Risks and Related Health Disparities
Any child can be aected by lead, but exposure in the United States is unequal across
populations. (See Figure 2.) Race and ethnicity are particularly strongly associated with children’s
risk. A national survey found that African-American children’s average blood lead levels were
well above those of non-Hispanic white and Mexican-American children.
*
Although the survey
did not control for social and economic factors, other studies have shown that race and ethnicity
are associated with elevated blood lead levels in children regardless of family income. One study
of more than 1 million blood tests from Chicago collected between 1995 and 2013 found that,
after controlling for socioeconomic factors, children from predominantly black, and to a lesser
extent Hispanic, neighborhoods had higher rates of lead poisoning than their white counterparts,
even as blood lead levels fell dramatically citywide. (See the Glossary for the definition of lead
poisoning used throughout this report.) Another study of children from Rochester, New York,
found that, after adjusting for environmental exposures, behaviors, socioeconomic status,
and dietary intake, black children were at higher risk of elevated blood lead than their peers
of other races.
†
These findings reflect the disparate risk that minority communities face from older housing
with lead paint hazards, a condition that has its origins in unfair lending practices and social
policies, such as redlining—in which even well-qualified black applicants were treated as too
risky for federally backed mortgages—and racial covenants, which prohibited people of
color from moving into white neighborhoods.
‡
These practices contributed to the isolation
of impoverished communities and people of color in areas with poorer-quality housing,
infrastructure, and air.
§
One national survey found that the extent of serious lead paint hazards
in U.S. housing diered significantly by race and income: Twenty-eight percent of African-
American households and 29 percent of poorer households faced housing-related exposure risks,
compared with 20 percent of white and 18 percent of more auent families, respectively.
||
Continued on next page

10
Figure 2
All Children Face Some Exposure Risk, but Racial and
Ethnic Disparities Persist
Share and number of 1-5-year-olds with blood lead levels below and
above 2 μg/dL by race and ethnicity, 2011-14
Note: All numbers are rounded.
Sources: Altarum analysis of National Center for Health Statistics, “National Health and Nutrition Examination
Survey 2011-2012,” accessed May 26, 2017, https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.
aspx?BeginYear=2011; and National Center for Health Statistics, “National Health and Nutrition Examination
Survey 2013-2014,” accessed May 26, 2017, https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.
aspx?BeginYear=2013
© 2017 The Pew Charitable Trusts
Continued on next page
0% 20% 40% 60% 80%
100%
White
10,184,000
Hispanic
5,225,000
Black
2,787,000
Other
2,108,000
Below 2 µg/dL 2 µg/dL and above
Percentage of children
808,000
9,376,000
428,000
4,797,000
424,000
2,363,000
203,000
1,905,000
Further, American Indian and Alaska Native children are far more likely than other children to be
exposed to potentially lead-contaminated runo and other eects of former mining sites, and in a
2008 study from New York City, foreign-born children were five times as likely as their U.S.-born
counterparts to have elevated blood lead levels.
#
Certain ethnic groups also experience disproportionate risk from lead associated with health
remedies and consumer products. Lead and other heavy metals are sometimes added to
traditional medicines used to treat ailments such as arthritis, infertility, upset stomach, menstrual
cramps, teething, and colic. Lead has been found in some candies and spices, such as chili
powder and tamarind. In addition, traditional eye cosmetics are still made with ingredients, such
as kohl, that are high in lead, and the FDA does not allow importation or marketing of these
products in the U.S., though they are sometimes brought in by individual travelers.
**

11
Income also influences rates of lead exposure. According to the CDC, children living in poverty
had significantly higher average blood lead levels than their more auent peers.
††
This is in part
because low-income families tend to rent rather than own their homes, and renters are more
likely than owners to face issues associated with inadequate housing, such as lack of complete
plumbing facilities in the unit, have more serious constraints on funding for improvements, and
depend on landlords to make their homes lead-safe.
‡‡
In addition, some evidence suggests that rural communities may be exposed to contaminated
soil resulting from past use of lead in pesticides applied to orchards and other crops; however
published research on these risks is limited.
§§
* William Wheeler and Mary Jean Brown, “Blood Lead Levels in Children Aged 1-5 Years—United States, 1999—
2010,” Morbidity and Mortality Weekly Report 62, no. 13 (2013): 245–48, https://www.cdc.gov/mmwr/preview/
mmwrhtml/mm6213a3.htm.
† Robert J. Sampson and Alix Winter, “The Racial Ecology of Lead Poisoning: Toxic Inequality in Chicago
Neighborhoods, 1995-2013,” Du Bois Review: Social Science Research on Race 13, no. 2 (2016): 261–83, http://dx.doi.
org/10.1017/S1742058X16000151; Bruce Lanphear et al., “Environmental Lead Exposure During Early Childhood,”
Journal of Pediatrics 140, no. 1 (2002): 40–47, https://dx.doi.org/10.1067/mpd.2002.120513.
‡ Kirwan Institute for the Study of Race & Ethnicity, “History Matters: Understanding the Role of Policy, Race, and
Real Estate in Today’s Geography of Health Equity and Opportunity in Cuyahoga County” (February 2015), http://
kirwaninstitute.osu.edu/wp-content/uploads/2015/02/history-of-race-real-estate.pdf.
§ Ibid.; Alex F. Schwartz, “Housing Policy in the United States: An Introduction” (Routledge, Taylor and Francis
Group, 2006): 217–18; Russ P. Lopez, “Public Health, the APHA, and Urban Renewal,” American Journal of Public
Health 99, no. 9 (2009): 1605, http://dx.doi.org/10.2105/AJPH.2008.150136.
|| U.S. Department of Housing and Urban Development, “American Healthy Homes Survey: Lead and Arsenic
Findings” (2011), http://portal.hud.gov/hudportal/documents/huddoc?id=AHHS_Report.pdf.
# Lacey McCormick, “Honoring the River: How Hardrock Mining Impacts Tribal Communities,” National Wildlife
Foundation, news release, April 25, 2013, http://www.nwf.org/News-and-Magazines/Media-Center/News-by-
Topic/Wildlife/2013/04-25-13-Honoring-the-River-Press-Release.aspx; Parisa Tehranifar et al., “Immigration
and Risk of Childhood Lead Poisoning: Findings From a Case-Control Study of New York City Children,” American
Journal of Public Health 98, no. 1 (2008): 92–97, http://dx.doi.org/10.2105/AJPH.2006.093229.
** U.S. Food and Drug Administration, “Kohl, Kajal, Al-Kahal, Surma, Tiro, Tozali, or Kwalli: By Any Name, Beware
of Lead Poisoning,” accessed March 6, 2017, https://www.fda.gov/Cosmetics/ProductsIngredients/Products/
ucm137250.htm.
†† Wheeler and Brown, “Blood Lead Levels in Children Aged 1-5 Years—United States, 1999–2010.”
‡‡ Joint Center for Housing Studies of Harvard University, “The State of the Nation’s Housing 2016” (Cambridge, MA:
Harvard University, 2016): 5, 25, http://www.jchs.harvard.edu/sites/jchs.harvard.edu/files/jchs_2016_state_of_
the_nations_housing_lowres.pdf.
§§ Carol L. Hanchette, “The Political Ecology of Lead Poisoning in Eastern North Carolina,” Health and Place 14, no.
2 (2008): 214, http://dx.doi.org/10.1016/j.healthplace.2007.06.003; C. Marjorie Aelion et al., “Associations
Between Soil Lead Concentrations and Populations by Race/Ethnicity and Income-to-Poverty Ratio in Urban and
Rural Areas,” Environmental Geochemistry and Health 35, no. 1 (2013): 10, http://dx.doi.org/10.1007/s10653-012-
9472-0.

12
Recent news reports provide stark reminders that lead continues to aect American communities. In
September 2015, Dr. Mona Hanna-Attisha found significant blood lead increases among children in Flint,
Michigan, which elevated the city’s drinking water crisis to a national public health issue. Nearly a year later,
roughly 270 families in East Chicago, Indiana, were displaced from a public housing development built near
a former smelter and lead refinery, which is now a federally designated Superfund site.
26
Soil at the housing
complex had lead levels significantly above the EPA’s action level—the concentration of lead above which
regulatory or remedial intervention is needed.
27
Methods
The research team developed a list of more than 100 policies for analysis based on documents from a range of
organizations and agencies, including the 2000 President’s Task Force on Environmental Health Risks and Safety
Risks to Children, the U.S. Centers for Disease Control and Prevention, Earthjustice, the American Academy of
Pediatrics, the National Center for Healthy Housing, the National Safe and Healthy Housing Coalition, the Green
& Healthy Homes Initiative, the Healthy Schools Network, and the Lead Service Line Replacement Collaborative.
28
The research team selected policies for analysis based on interviews; focus groups; and a series of meetings
with experts, advocates, and community members. The team asked these stakeholders to identify policies for
inclusion in the study based on their public health and health equity value and, noting the urgency of action,
their potential to be implemented within 18-36 months. Additionally, the team chose policies with the
strongest evidence base.
Priority was placed on those that related most directly to preventing children from coming into contact with lead
and enabling those who have already been exposed to access services to help improve their lifelong outcomes.
29
The analysis included qualitative and quantitative research organized according to a modified Sequential
Explanatory approach, to develop an understanding of the relevant social, economic, and cultural contexts for
lead exposure in children.
30
Studies that use both qualitative and quantitative methods are strengthened by the
combination because they are able to present information from multiple perspectives. Qualitative data collection,
including focus groups, listening sessions, and interviews, was conducted first, followed by quantitative analyses
of costs and benefits.
See the appendix for an in-depth discussion of the methodology used for this report.
Quantitative models
Child Trends, a nonprofit research center focused on child development, led the quantitative work, in partnership
with Altarum Institute, a nonprofit health systems research organization, and the Urban Institute, a nonprofit
economic and policy research organization.
The study team quantitatively modeled only those prevention interventions for which data on the scope of
exposure and the eectiveness of the policy were readily available. For example, data exist on the extent of lead
paint, lead service lines, and contaminated dust in homes, as well as on the eectiveness of interventions to
address these hazards. However, similarly comprehensive information for these threats and policies to mitigate
them in schools and child care facilities was not available. Exposure from sources not tied to a specific structure,
such as consumer products and food, was also dicult to estimate, and data regarding the eectiveness of
interventions targeted at those sources were lacking. Despite these data constraints, in recognition of the reality
that many sources of lead contribute to childhood lead exposure, the team studied those hazards for which

13
quantitative data were not available using the qualitative methods described later in this chapter. The team
selected the inputs for the models from a literature search that identified 176 peer-reviewed articles related to the
policies analyzed. The team used the most rigorous literature available as the basis for the quantitative models.
Child Trends and the Urban Institute used the Social Genome Model (SGM), which examines how actions at
developmentally significant life stages reverberate through a person’s life, to predict the eects of policies to
prevent harmful blood lead levels and of interventions for lead-exposed children.
31
The SGM simulated the
eects of the prevention and response policies on educational attainment, grade point average, teen parenthood,
criminal convictions, and lifetime family income. Using a data set of 8,056 children, the SGM tracks lifelong
development starting at birth and employs statistical techniques to assess the relationships between children’s
early life circumstances and later outcomes. The studied eects build on one another over a child’s life:
Circumstances at birth influence early childhood, which in turn aects middle childhood circumstances, which
translate into a child’s situation in adolescence, and so on well into adulthood. For example, robust research
shows that, after controlling for other factors, children with lower blood lead levels have better early reading
scores than those with higher levels.
32
The SGM calculates how this better reading contributes to greater
educational attainment and higher income later in life.
The SGM does not include information on children’s blood lead levels, so the team used data from the
two most recent editions (2011-14) of the National Health and Nutrition Examination Survey (NHANES),
a national population-based survey, to assign blood lead levels to children based on their social and
demographic characteristics.
The modeling team used data from the literature to determine the change in children’s blood lead that could be
expected as a result of the policy interventions and how it would aect reading, math, and behavior. The team
then ran the SGM to estimate how those eects would, in turn, impact later life outcomes, such as graduation
rates, criminal convictions, and teen pregnancy. The SGM was used to examine five interventions for which
eect size estimates were available: lead service line replacement; lead paint hazard control; renovation, repair,
and painting rule enforcement; removal of lead from aviation gas; and programs for children with a history of
lead exposure. The SGM outputs for this final intervention are presented in the body of the report, while for
brevity, the findings from the first four analyses may be found in the appendix.
The analysis also employed Altarum Institute’s Value of Prevention (VP) tool, a spreadsheet-based application,
which synthesizes research findings and national data sets to quantify the financial and health impacts of various
preventive investments. The tool has been applied to investigating the value of smoking and obesity prevention,
and of early childhood education. For this study, the team synthesized four types of data to estimate the costs
and benefits of the four prevention policies. The tool integrated published findings on the eect of an intervention
on blood lead levels and information on the health and social impacts of lead exposure to infer later-life health
status, health care costs, and incarceration rates; and data on the eect of lead on IQ and on the relationship
between IQ and income to predict lifetime earnings.
The research team modeled the benefits for the cohort of children born in 2018, the next full year that most
closely approximates the blood lead level data from the 2011-14 NHANES. According to those data, the mean
blood lead level for the population of children 1-5 was 1.1 μg/dL.
These analyses provided an estimate of the benefits of each policy to society and to the federal and state
and local governments. These are referred to in the report as “future benefits” and are discounted at a rate of
3 percent per year to account for the changing value of money over time.

14
To better understand and describe any uncertainty within the findings, the modeling team conducted two
additional analyses. First, it modeled the eects of preventing blood lead levels from rising above 0 μg/dL as
a bounding exercise to provide an upper limit on the potential impacts of the intervention policies. Second, to
address uncertainties that could not be tested by that method, the team performed quantitative sensitivity
analyses to clarify how changes in the assumptions, coecients, and data points could aect the overall results.
(See the appendix for details.)
Qualitative methods
Through qualitative approaches, researchers can identify stakeholder concerns, explain why and how
phenomena occur, and gauge the range of eects. These methods also provide context for quantifiable
information and enable an examination of processes and experiences along with outcomes.
In addition to the research literature gathered for the quantitative models, the study team identified and reviewed
other studies across a range of methods and topics that could help with screening policies and formulating
recommendations. Across the two literature searches, the team identified roughly 700 peer-reviewed articles.
Through 16 focus groups held in Baltimore; Chicago; Flint; Indianapolis; Los Angeles; New Orleans; Philadelphia;
and Warren, Arkansas, the team collected feedback from at least 129 community members, including landlords
(16 participants), parents of children with high blood lead levels, and other concerned citizens (113 participants).
The team gathered basic demographic information from participants in the parents and concerned citizens
groups using a brief survey. (See Table A.3 for complete results.) The team also held two conference
calls with eight parents of lead-poisoned children to capture their experiences navigating the medical and
education systems.
The research team developed a list of themes from the discussion guides for the focus groups. The team
analyzed the field notes and transcriptions from each focus group to identify additional common themes and
keywords to add to the list and then summarized the findings and linked those to the quantitative results to
provide context for the economic information. Perhaps more importantly, the qualitative analysis allowed the
team to identify barriers to implementing the recommendations as well as steps to mitigate those challenges
and support eective remediation of lead exposure risks.
In addition, the research team gathered more insight into the eects of childhood lead exposure and potential
policy interventions through five national online listening sessions. (See the appendix for details on participants
and methodologies for these events.) Unstructured conversations with experts provided additional input for
the report.
Finally, the Trust for America’s Health and the National Center for Healthy Housing developed case studies to
highlight examples of policies in action and lessons learned from across the country. The team selected the case
studies based on their relevance to the policies analyzed and their applicability to other jurisdictions. (See the
“Policy in Action” listings in the Table of Contents.)

15
Study limitations
Qualitative data limitations
Obtaining input from all stakeholder groups that could be aected by the recommendations was beyond the
scope of the study. Eorts were made to broadly advertise the national listening sessions to ensure that the
study included diverse stakeholder perspectives, but in general, school administrators, the aviation industry, and
owners of secondary smelters did not respond and so are not as well represented as the public health community.
Further, although the team solicited feedback through the advisory committee and focus groups from several
representatives of water utilities, property management firms, renovation contractors, child care operators, and
rental property owners, fewer of these groups’ perspectives were included than of public health professionals and
community-based organizations. Finally, the focus group locations and project advisers were subject to selection
bias, because existing relationships and networks were leveraged during the selection process. When possible,
the team controlled for this by seeking input from a broad array of partners.
Quantitative model limitations
Blood lead data for the 2018 birth cohort
The team relied on the two most recent NHANES surveys (2011-14) to establish children’s baseline blood lead,
which, based on historical trends, may be higher than what will be seen among the 2018 birth cohort. However,
data from the CDC lead surveillance program indicate a leveling-o between 2009 and 2015 of the number of
children with blood lead levels above 10 μg/dL,
33
suggesting that using the NHANES data is appropriate to
predict 2018 blood lead levels.
Current exposure levels
Recent epidemiologic data on the relative contribution to blood lead levels of dierent environmental sources are
scarce. Therefore, the study team could not determine whether the proportion of exposure coming from dierent
sources has changed or what adjustments would be necessary to reflect such shifts.
Data on the impact of interventions
In light of today’s lower blood lead levels and the decreased amount of lead in the environment, the team took
several precautions to avoid overestimating the benefits of exposure prevention, including using multistep
processes to estimate the relationship between lead in the environment and in blood and the most recent data
available on the eectiveness of the interventions, relying on studies of children with lower mean blood lead
levels, and modeling dierent baseline levels of lead in the environment.
For the lead paint hazard control and drinking water interventions, instead of relying on older epidemiologic
studies of environmental and blood lead levels, the team used a two-part process to establish first the
relationship between the interventions and levels of lead in the environment and, second, the association
between those environmental levels and the amount of lead in a child’s blood. The team used an estimate from
a large national evaluation of the eect of lead paint hazard control on dust lead levels in the home and then
used corresponding blood lead level reductions from a 2009 study. In addition, the team modeled the benefits
of the intervention based on two starting levels of lead in dust on floors; 20 and 10 μg/sq ft.
The team used a similar process for determining the relationship between removing lead drinking water
lines, levels of lead in water, and lead in a child’s blood. The team also modeled two baseline water lead level
scenarios, 11.4 ppb and 5 ppb, to show a range of eects of replacing lead service lines depending on baseline
water lead levels.

16
For renovation, repair, and painting, the team relied on a 2008 EPA model that estimated the eects of
preventing acute exposure from unsafe practices.
For aviation gas, the team relied on a study of Michigan children from 2001 to 2009 with a relatively low
mean blood lead level of 2.98 μg/dL.
The relationship between current blood lead levels and cognitive and behavioral outcomes
The models rely on estimates of the relationship between blood lead levels and outcomes such as IQ, cognition,
and behavior from older studies that were conducted when mean blood lead levels were higher. Although
few studies capture the relationship between IQ and blood lead levels below 2 μg/dL, several have found a
relationship at mean levels of 3 to 5 μg/dL.
34
Not only do low blood lead levels result in IQ changes, but evidence
suggests that IQ losses from lead exposure may be greater at lower blood levels.
35
An increase in blood lead
from less than 1 to 10 μg/dL is associated with a loss of 6 IQ points, compared with 2 points lost from a rise from
10 μg/dL to 20.
36
(See appendix for further discussion of the impacts of low-level lead exposure on IQ.)
To avoid potentially overstating the blood lead-to-IQ impact for today’s population of children, the team modeled
dierent eect sizes depending on the predicted blood lead level of a child. For the lowest blood lead category
of less than 5 μg/dL, the team relied only on studies with a mean level below 5 μg/dL. Although limited data exist
on the relative eect sizes on IQ of blood levels below 2 μg/dL, the team assumed that the linear relationship
established in the literature for levels between 5 and 2 μg/dL continued below 2 μg/dL. These strategies—
using studies with the closest possible mean to today’s blood lead levels and assuming a linear trend down to
0 μg/dL—are identical to those used by the EPA for its 2008 clean air regulations.
37
Similarly, the team considered 14 estimates of the relationship between blood lead and reading and math scores,
all but two of which were based on samples of children with mean blood lead levels of 5 μg/dL or lower.
38
Among
the studies, two found that the rate of decline in reading scores increased at lower blood lead levels, while the
others found a linear relationship, even in children with low blood lead levels. The team also reviewed eight
estimates of the eect size of blood lead on behavioral outcomes: five from study samples with mean blood levels
below 6 μg/dL, and three based on samples with higher mean levels.
39
Other limitations
Data for the numbers of children at risk from leaded aviation gas and living in homes with leaded drinking
water pipes as well as for those children’s blood lead levels were incomplete. The benefits only account for the
child residing in a treated home; they exclude children who might visit, except where otherwise noted. Further,
the NHANES, which was used to establish the baseline blood lead levels for children in the quantitative models,
estimates levels nationally rather than by smaller geographic areas such as neighborhoods, and the SGM is
based on a population with fewer immigrants than the current U.S. population. These dierences may mean
that predictions in this study may understate or overstate eects for certain communities.
In addition, the cost-benefit ratios exclude the cost of government administration for the studied interventions
because they could be operated by many levels of government or the private sector at widely varying
costs. Where available, information about program administration expenses is included in the discussion
of each intervention.
Further, outcome predictions assume complete implementation of each intervention, but, in reality, a portion
of targeted homes would probably not receive a given remediation because of refusal, financial barriers, or other
factors. As a result, total benefits, total costs, and net benefits would be lower, while cost-benefit ratios and
per-child benefits would remain the same.

17
Total prevention of lead poisoning
I guess there must have been some public health campaigning at one
point where they said paint chips are it! Because everybody got that
message. It was like Smokey the Bear. But they don’t understand that
it’s so much broader than that. … It’s in the soil. It’s [in] the air. It’s in
your pipes.”
—New Orleans resident
The team, with guidance from advisers and key stakeholders, selected policies for analysis that promised the
greatest public health and equity benefits and that could be adopted, though not necessarily fully implemented,
in 18 to 36 months, given the urgent need for action.
Lead is ubiquitous; past and present uses challenge eradication eorts
Many sources and pathways add to the amount of lead in a child’s blood, including releases from previous
exposure stored in a child’s bones. In addition, individual children’s exposures vary based on several factors,
including location, age, intake of food and water, mouthing behavior, and nutritional status. Evidence also
suggests that for children with blood lead levels below 10 μg/dL, “no single exposure source predominates,”
40
underscoring the need for a comprehensive response.
Kev Klopper/Getty Images

18
Lead in Everyday Items
To the surprise of many people, lead continues to be used in a variety of everyday consumer and
commercial goods. Although the team found no data to characterize the extent to which these
sources present a population-level health risk, dozens of case studies have documented acute
instances of child lead poisoning and even death from a range of products, including candies,
health remedies, cosmetics, and spices.
*
For example, one national survey found that imported
candy contributed 10 percent of dietary lead for 2- to 6-year-old children.
†
In addition, Greta,
a health remedy used in some Hispanic cultures to treat upset stomach, contains high levels
of lead and has accounted for several cases of lead poisoning;
‡
Tiro, an African eye cosmetic,
has been found to contain 82 percent lead and has sickened at least one child in the U.S.;
§
and
Litargirio (also known as litharge or lead monoxide), a Central American antiperspirant and
deodorant, poisoned two siblings in Rhode Island in 2003. Further, between 2010 and 2014,
six poisoning cases were attributed to lead-contaminated spices, including turmeric.
||
Lead compounds, such as lead oxide, also are sometimes used in pottery glazes because
they allow for a broader range of firing temperatures. However, when fired at inadequate or
uncontrolled temperatures, the lead may not be not fully incorporated into the glaze and can
leach into food.
#
Also, many commercially available food products contain small amounts of
lead, including some marketed for infants and toddlers.
**
The allowable amount of lead for many
foods is based on consultation with other countries and on what is achievable for members of
an international committee called the Codex Alimentarius General Standard for Contaminants
and Toxins in Food and Feed.
††
In focus groups, participants worried about lead contamination of food, including imported
spices, breast milk, toys, jewelry, and other products, wanted improved labeling, and expressed
concerns for refugees and a desire to ban lead from health remedies. They also identified a need
for culturally and linguistically appropriate education eorts to reach recent immigrants and
refugee families with information about sources of lead in consumer goods. According to one
Spanish-speaking participant from Flint, Michigan, “There isn’t any information about lead in
Spanish here.” In general, participants wanted increased testing and labeling of food products
containing lead and improved health communication about related risks.
California has led U.S. eorts to ban lead from a range of products beginning with a 1986 law,
known as Proposition 65, which requires manufacturers, retailers, and other businesses to notify
consumers when they are being exposed to toxic chemicals, including lead. More recently, the
state has enacted additional policies:
• The 2006 Lead-Containing Jewelry Law requires jewelry and components, such as dyes and
crystal, that is sold, shipped, or manufactured for sale in California to meet limits set by the
state under a 2004 consent judgment that applied to a number of manufacturers, retailers,
and distributors.
‡‡
Continued on next page

19
• A 2010 law restricted the use of heavy metals including lead in motor vehicle brake pads to
no more than 0.1 percent by weight. In January 2015, brake manufacturers agreed that all
brake pads sold in the United States will meet California standards.
§§
• The 2003 Toxics in Packaging Prevention Act, which limited harmful substances in
packaging, originally exempted lead in paint or applied ceramic decoration on glass bottles,
but a 2008 amendment banned such uses in excess of 600 ppm.
|| ||
• To protect wildlife, a 2013 law required that only lead-free ammunition be used for hunting
with a firearm.
##
* Centers for Disease Control and Prevention, “Childhood Lead Poisoning Associated With Tamarind Candy and Folk
Remedies—California, 1999–2000”; Whitney Cowell et al., “Ground Turmeric as a Source of Lead Exposure in the
United States,” Public Health Reports 132, no. 3 (2017): 289–93, http://dx.doi.org/10.1177/0033354917700109.
† S.K. Egan et al., “U.S. Food and Drug Administration’s Total Diet Study: Intake of Nutritional and Toxic Elements,”
Food Additives and Contaminants 19, no. 2 (2002): 103–25.
‡ Centers for Disease Control and Prevention, “Lead Poisoning Associated With Ayurvedic Medications—Five
States, 2000–2003.”
§ Centers for Disease Control and Prevention, “Infant Lead Poisoning Associated With Use of Tiro, an Eye Cosmetic
From Nigeria—Boston, Massachusetts, 2011,” Aug. 3, 2012, https://www.cdc.gov/mmwr/preview/mmwrhtml/
mm6130a3.htm.
|| Centers for Disease Control and Prevention, “Lead Poisoning Associated With Use of Litargirio—Rhode Island,
2003,” Morbidity and Mortality Weekly Report, March 11, 2005, https://www.cdc.gov/mmwr/preview/mmwrhtml/
mm5409a5.htm; Whitney Cowell et al., “Ground Turmeric as a Source of Lead Exposure in the United States.”
# U.S. Food and Drug Administration, “Guidance for Industry: The Safety of Imported Traditional Pottery Intended
for Use With Food and the Use of the Term ‘Lead Free’ in the Labeling of Pottery; and Proper Identification of
Ornamental and Decorative Ceramicware,” accessed Feb. 6, 2017, http://www.fda.gov/Food/GuidanceRegulation/
GuidanceDocumentsRegulatoryInformation/ucm214740.htm.
** U.S. Food and Drug Administration, “Total Diet Study, Elements Results Statistics, Market Baskets 2006 through
2011” (College Park, MD: U.S. Food and Drug Administration, 2014), https://www.fda.gov/downloads/food...
totaldietstudy/ucm184301.pdf.
†† Codex Alimentarius Commission, “Report of the Ninth Session of the Codex Committee on Contaminants in
Foods” (New Delhi, India, March 16–20, 2015), ftp://ftp.fao.org/codex/reports/reports_2015/REP15_CFe.pdf.
‡‡ California Department of Toxic Substances Control, “History of the Law,” accessed Jan. 12, 2017, http://www.dtsc.
ca.gov/PollutionPrevention/ToxicsInProducts/upload/History-of-the-Law1.pdf.
§§ California Department of Toxic Substances Control, “Brake Pad Legislation,” accessed Jan. 12, 2017, http://
www.dtsc.ca.gov/SCP/BrakePadLegislation.cfm; U.S. Environmental Protection Agency, “Copper Mitigation in
Watersheds and Waterways,” accessed Jan. 12, 2017, https://www.epa.gov/sites/production/files/2015-11/
documents/copper_brakepads_mou.pdf.
|| || California Department of Toxic Substances Control, “Senate Bill (SB) 774 and Changes to the Toxics in Packaging
Prevention Act,” accessed Jan. 12, 2017, https://www.dtsc.ca.gov/ToxicsInPackaging/upload/TIP_FS_SB-774_
Changes.pdf.
## California Fish and Game Commission, “Prohibition on the Use of Lead Projectiles and Ammunition Using
Lead Projectiles for the Take of Wildlife,” accessed Jan. 12, 2017, http://www.fgc.ca.gov/regulations/current/
mammalregs.aspx#250_1.
20
Modeling total prevention
The research team modeled interventions to prevent children’s blood lead levels from exceeding zero. Notably,
given the diverse sources of lead in the environment and the widely varied exposure risks across populations,
a zero blood lead level is aspirational. However, the team chose to model a zero level to establish the maximum
possible benefits that could be realized under a total prevention scenario. Using the VP Tool, the team
determined that the discounted future societal benefits of such hypothetical total prevention would be $84 billion
for the 2018 birth cohort. (See Table 1.)
Table 1
Keeping Blood Lead Levels of Children Born in 2018 at Zero Would
Generate $84 Billion in Benefits
Future savings and increased earnings by source and recipient
Benefit Value (in billions)
Increased lifetime earnings for entire 2018 cohort $77.2
Health savings $1.7
Education savings $1.9
Quality-adjusted life years benefits $3.1
Total future benefits $84.0
Share to the federal government $18.5
Share to state and local governments $9.6
Share to households, private sector, and other nongovernmental entities $55.9
Notes: Analysis is based on the 2018 birth cohort, estimated at approximately 4 million children. Future benefits are discounted at 3 percent
per year to account for the changing value of money over time. Quality-adjusted life years is the number of additional healthy years of life
resulting from an intervention, which the research team conservatively valued at $50,000 for each additional year of healthy life. Total future
benefits include small changes in incarceration costs, which are not itemized in the table.
Source: Altarum Institute Value of Prevention Tool calculation. See the appendix for details on the model methodology and underlying
data sources.
© 2017 The Pew Charitable Trusts
The benefits include earnings associated with greater employment and higher-paying jobs and lower public
spending on short- and long-term health care costs, such as for testing and treating lead-exposed children,
doctor visits, and hypertension and cardiovascular disease later in life. The benefits also include savings to the
education system, specifically, reduced spending on special education and grade repetition. The calculations also
capture benefits from quality-adjusted life years (QALYs)—the number of additional healthy years of life resulting
from an intervention—which the research team conservatively valued at $50,000 each.
41
Finally, the estimated
future benefits also include $13 million in savings from decreased incarceration based on a longitudinal study

21
that linked blood lead levels to arrest rates.
42
However, that study only documented eects for blood lead above
6 μg/dL, a level that few children experience today, so the predicted benefits associated with reduced criminal
involvement are relatively small. The model did not account for other potential cost reductions associated with
crime and criminal justice, such as from fewer arrests, so the benefit estimates may be conservative.
Of the $84 billion in future benefits for the 2018 birth cohort, about $77 billion comes from increased earnings,
most of which accrues to families and the private sector, with a portion also going to federal, state, and local
governments as increased tax revenue. Of the $19 billion federal share, nearly $15 billion is in the form of
increased tax collections, with the remaining $4 billion coming from reduced spending on education, health
care, and social support programs. The $10 billion for state and local governments includes about $4 billion from
increased tax revenue and roughly $6 billion in decreases in government expenditures. This analysis predicts that
increased employment and wages would reduce demand for government assistance, leading to lower spending
on social support programs, which is counted as a benefit for federal, state, and local governments. However,
because the savings result in a loss to the citizens who would receive payments, the reduced government
spending is not included in the $84 billion benefit total.
Further, assuming no changes to current programs and policies, NHANES data predict that without the
intervention, from ages 1-5, 90.8 percent of the cohort would have blood lead levels below 2 μg/dL; 8.0 percent
would be between 2 and 5; 0.9 percent between 5 and 10; and 0.3 percent above 10. (See Figure 3.)
Figure 3
Most Benefits of Exposure Prevention Accrue for Children Whose
Blood Lead Would Otherwise Be Below 2 µg/dL
Economic gains by avoided blood lead levels and number of children
Notes: Without intervention, the blood lead level distribution at ages 1-5 for the 2018 birth cohort would be 14,000 children with blood lead
levels greater than 10 μg/dL, 34,000 between 5 and 9.9 μg/dL, 318,000 between 2 and 4.9, and 3,612,000 between 0 and 1.9.
Source: Altarum Institute Value of Prevention Tool calculation
© 2017 The Pew Charitable Trusts
$2.6 B
10+ µg/dL
$3.8 B
5-9.9 µg/dL
$60.4 B
0-1.9 ug/dL
$17.1 B
2-4.9 µg/dL
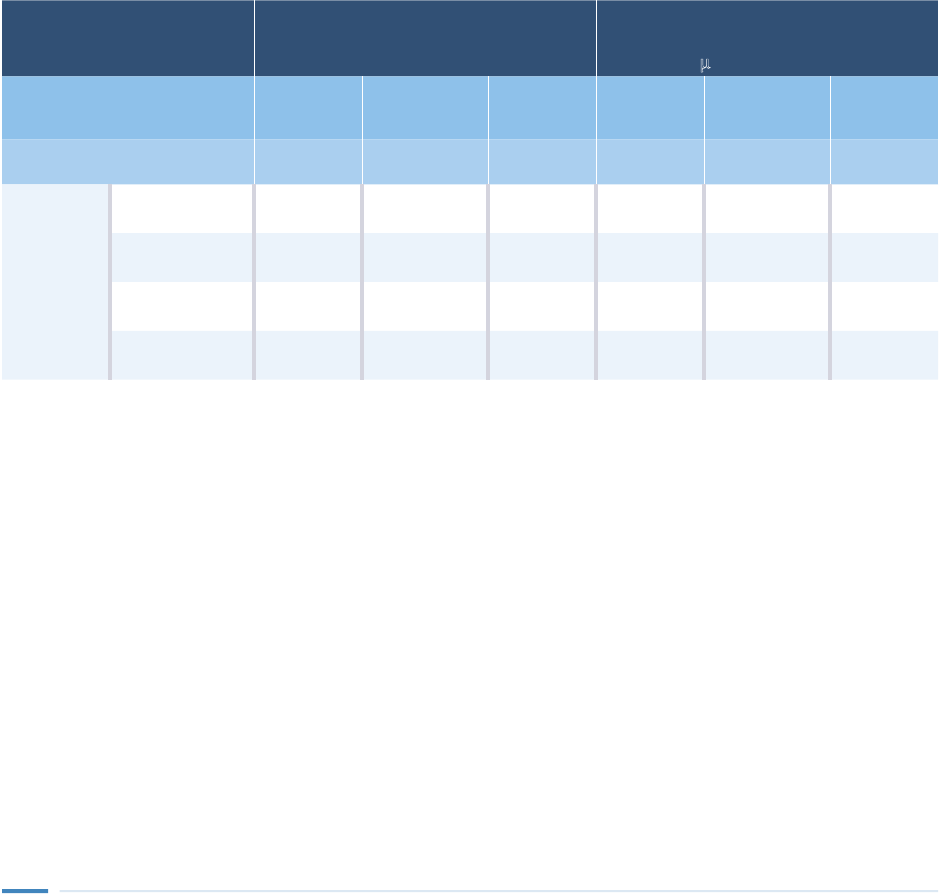
22
If federal investment of $80 billion was sucient to prevent the 2018 cohort’s blood lead from exceeding zero,
estimated societal benefits would be $1.05 per $1 invested; if the necessary investment proved smaller, the
cost-benefit ratio would be greater. Additionally, permanent removal of lead hazards would aect future cohorts,
and those benefits would be in addition to the estimates provided in this analysis.
Additionally, the research team used the SGM to explore the eects of full prevention on children’s educational
attainment and likelihood of risky behaviors, such as criminal activity. The model indicated that holding
blood lead levels at zero would improve high school and college graduation rates, and decrease rates of teen
parenthood and criminal conviction. (See Table 2.)
Outcome All children born in 2018
Children born in 2018 whose blood
lead levels would be expected to rise
above 2 μg/dL in early childhood
Baseline
conditions
Total
prevention
Children
benefiting
Baseline
conditions
Total
prevention
Children
benefiting
Average high school GPA 2.93 2.94 N /A 2.74 2.78 N/A
Percentage
and number
of children
Earn high school
diplomas
83.7% 84.0% 14,600 74.4% 75.6% 4,500
Become teen
parents
13.5% 13.3% 6,000 20.1% 19.6% 1,900
Be convicted
of crimes
17.2% 16.9% 15,500 22.0% 20.7% 4,700
Complete 4-year
college degrees
26.7% 27.1% 15,200 17.0% 18.3% 4,700
Notes: Analysis is based on the SGM’s sample of about 8,000 children, drawn from the Children of the National Longitudinal Survey of Youth
dataset. To arrive at the number of children positively aected, the research team applied the percentage point dierences between baseline
conditions and total prevention to the roughly 4 million children expected to be born in 2018 and to the roughly 365,000 of them whose
blood lead levels would probably exceed 2 μg/dL. See the appendix for information on the model and methodology.
Source: Social Genome Model analysis by Child Trends and the Urban Institute
© 2017 The Pew Charitable Trusts
Table 2
Keeping Blood Lead Levels at Zero Among Children Born in 2018
Would Improve Educational and Social Outcomes
Eects on education, teen parenthood, and crime
The modeling team examined the impact of the total prevention scenario on the IQs of children born between
2018 and 2023 using a similar methodology to that presented by Gilbert and Weiss and found that, on average,
preventing exposure would avoid the loss of 1.27 IQ points per child.
43
A 1.27-point dierence would be dicult to
discern between two children, but preventing lead exposure would reduce the number of intellectually challenged
children, those with IQs below 70, by about 101,000 or 18.5 percent and would increase the number of children
in the gifted category, above 130 IQ points, by about 119,000 or 22 percent across six birth cohorts. Findings from
a recent study suggest that the impact of childhood lead exposure on IQ persists into adulthood, which lends
support to the findings of these models that preventing exposure and mitigating the eects of lead for young
children would improve their outcomes later in life.
44

23
Drinking water
[Before the Flint, Michigan, case], I never thought we could get lead
poisoning from water. I was totally ignorant about that.”
—Flint focus group participant
Sources of contamination in drinking water include corrosion of lead service lines (LSLs), brass plumbing fixtures,
and lead solder installed before Congress limited the use of lead in plumbing and pipes in 1986.
45
Although indoor
plumbing fixtures and lead solder can also contribute to elevated lead levels in water, the research indicates that
LSLs account for the largest share of lead in water.
46
Importantly, observational studies show that U.S. residences
with LSLs are at even greater risk if the techniques used to manage the corrosivity of water are not eective.
A robust body of academic literature from the U.S. and Canada links lead in drinking water to increases in blood
lead levels.
47
For example, one cross-sectional study
48
of 183 children randomly selected from urban areas found
that an increase in water lead concentrations from background levels to 15 ppb was associated with a nearly
14 percent jump in the share of children with estimated blood lead over 10 μg/dL.
49
Participants in all 16 focus
groups said lead in drinking water at homes, schools, and child care facilities was a primary concern, and several
parents of lead-exposed children said water was the source of their children’s exposure.
Lead in Water and Infant Health
Infants can ingest lead through breast milk and water used to reconstitute powdered formula.
Lead stored in bones can release into a mother’s blood, and a fraction (up to 3 percent) of
that lead can transfer to breast milk.
*
Breastfeeding provides infants and mothers with many
health benefits, and weighing those against the adverse eects of lead exposure, the CDC
recommends mothers with blood lead levels below 40 μg/dL continue to breastfeed.
†
In
situations where breast milk is supplemented with or replaced by formula, caregivers should
take steps to avoid using water contaminated by lead to reconstitute formula, such as flushing
the tap or using bottled or filtered water, and never using water from the hot tap.
‡
* Centers for Disease Control and Prevention, “Guidelines for the Identification and Management of Lead Exposure
in Pregnant and Lactating Women” (Atlanta: U.S. Department of Health and Human Services, 2010), https://www.
cdc.gov/nceh/lead/publications/leadandpregnancy2010.pdf.
† Ibid.
‡ Ibid.

24
The EPA began requiring water utilities to manage lead under its 1991 Lead and Copper Rule.
50
The rule set forth
“corrosion control” as the primary method for reducing lead in water in the United States. This technique involves
treating water with chemicals, such as orthophosphates, that create a barrier between the pipes and the water
in them or adjusting the pH or hardness of water. Since the rule’s inception, corrosion control has dramatically
decreased water lead levels in the U.S., but the various methods can dier substantially in eectiveness, so the
EPA requires utilities to monitor selected water quality parameters, such as pH.
51
The rule also mandated that water utilities periodically test lead concentrations across a sample of customer taps
that are deemed more likely to have elevated levels based on the presence of LSLs, other lead pipes, or any pipes
with lead solder and to report the results to consumers. However, the rule does not require that all customer taps
be tested. Instead, systems are only obligated to sample 10 percent of their taps. The crisis in Flint shed light
on the shortcomings of the current approach to managing lead in water. The EPA acknowledged challenges in a
document concerning possible revisions to the Lead and Copper Rule, which cited issues including complexity,
sampling protocols, a lack of attention to specific areas such as schools, and too much flexibility regarding
corrosion control implementation and monitoring.
52
Jamie Grill/Blend Images

25
Water fountains in many public schools have not been tested for lead risks.
Drinking Water in Schools and Child Care Facilities
Millions of children spend significant time in school and child care facilities each day, making
these places important potential sources of exposure.
• About 50.4 million children attend public school and nearly 4.3 million children under 5 are
served annually by center- and home-based child care providers.
*
• Case studies of school drinking water have found dramatic variation: A 2015 study of
3,100 taps across 63 Seattle schools found lead levels from less than 1 ppb to 1,600 ppb; an
analysis of first-draw samples—those taken after water sat in the pipes overnight—from the
Los Angeles Unified School District revealed a range of 0.2 to 13,000 ppb; a 2004 study of
Philadelphia schools found that about 57 percent of buildings had water lead above the EPA
action level of 20 ppb, and 29 percent had water with mean levels over 50 ppb; and a report
determined that a third of Chicago schools tested (30 percent of taps) had at least one
sample above 15 ppb.
†
• The average age of U.S. public schools is 44 years, but many have undergone major
renovations, putting their “functional” age closer to 19 years on average. Despite the
upgrades, the American Society of Civil Engineers in 2017 rated school infrastructure and
drinking water quality as poor.
‡
Continued on next page
Damita Delimont/Getty Images

26
• About 10 percent (roughly 8,000) of the nation’s schools and child care facilities maintain
their own water supplies and are regulated under the Lead and Copper Rule, but because the
rule only requires a sampling of taps across the community, many schools may never have
been tested. Approximately 98,000 public schools and 500,000 child care facilities are
excluded from the federal Safe Drinking Water Act,
§
but in its 3Ts (training, testing, telling)
guidance, the EPA recommends testing and a standard of 20 ppb.
||
• The CDC School Health Policies and Practices Survey’s 2014 data show that
nationwide, fewer than half (46 percent) of schools test their drinking water for lead
and other contaminants.
#
In the absence of an overarching law or regulation governing drinking water in public schools
and licensed child care facilities, the 2010 Healthy, Hunger-Free Kids Act provides a possible
avenue to address lead risks. The act requires schools and child care programs that participate
in the National School Lunch (NSLP) and Child and Adult Care Food (CACFP) programs,
respectively, to provide children with free potable water.
**
The NSLP operates in more than
100,000 public and nonprofit private schools and residential child care institutions, and in
2012, it provided low- or no-cost lunches to more than 31 million children each school day.
CACFP supplied meals and snacks for more than 4.1 million children in child care settings each
day in 2015.
††
The U.S. Department of Agriculture (USDA), which oversees both programs, provides guidance
related to drinking water and has encouraged schools and child care facilities to follow the
EPA’s testing recommendations, but it has not defined the term “potable” to include safety from
the risks of lead above the EPA’s guidance of 20 ppb.
‡‡
The American Academy of Pediatrics
recommends a standard of 1 ppb lead in water from school drinking fountains, and in March
2017, Health Canada published for public comment a maximum allowable concentration of
lead in water for schools and child care providers of 5 ppb,
§§
either of which could serve as an
updated standard for the U.S.
Providing drinking water that meets such a health-based action level could help protect low-
income children served by these programs who are at increased risk of lead exposure.
Many focus group participants raised concerns that school drinking fountains were a potential
source of lead, but they also cited drawbacks to eorts to provide alternative sources of drinking
water, such as bottled water. For example, schools may need to provide cups, and in some cases
parents had to shoulder additional costs. Participants suggested adding filters to fountains or
installing filtered-water stations that allow students to refill personal water bottles.
Continued on next page

27
Concern over contaminated water in schools led to the introduction of 82 bills in 12 states and
the District of Columbia in 2016,
|| ||
and several school districts began testing tap water and
replacing or shutting down fountains with high lead levels:
• At least nine states and the district took action to test school drinking water at the tap,
including the Oregon Health Authority, which posted its results online.
##
• Governor Jerry Brown (D) of California issued an executive order requiring all public water
systems to oer free testing to schools in their service areas and included $9.5 million for
remediation in the state budget.
• Massachusetts appropriated $2 million for voluntary school testing.
• Illinois is developing rules for mandatory testing, notification, and mitigation in all licensed
child care homes and centers.
• New York, which requires testing and remediation of taps in schools and school-based child
care, has included funds for the eort in its state budget, and posts results online.
• Rhode Island’s General Assembly passed the Lead and Copper Drinking Water Protection
Act in June 2016, requiring schools, day care providers, public playgrounds, shelters and
foster homes with children under 6, and other state facilities to certify that drinking water
conduits are lead-safe. The act also directs state inspectors to conduct annual lead and
copper tests at these locations.
***
* National Center for Education Statistics, “Digest of Education Statistics” (2016), Table 105.20, https://nces.ed.gov/
programs/digest/d15/tables/dt15_105.20.asp?current=yes; U.S. Census Bureau, “Who’s Minding the Kids? Child
Care Arrangements: Spring 2011” (April 2013), https://www.census.gov/prod/2013pubs/p70-135.pdf.
† U.S. Environmental Protection Agency, “Seattle, WA: Arsenic in Public Schools” (Washington: U.S. Environmental
Protection Agency, September 2015), https://www.epa.gov/sites/production/files/2015-09/documents/
casestudy_seattle.pdf; Joel Grover and Matt Goldberg, “School Water Investigation—Part 2,” NBC Los Angeles,
Oct. 30, 2008, http://www.nbclosangeles.com/news/School_Water_Investigation_-_Part_2.html; S. Bryant, “Lead-
Contaminated Drinking Waters in the Public Schools of Philadelphia,” Journal of Toxicology: Clinical Toxicology 42, no.
3 (2004): 287–94; Juan Perez Jr., “CPS Is Testing Schools for High Lead Levels in Water: What You Should Know”
Chicago Tribune, June 19, 2016, http://www.chicagotribune.com/news/local/breaking/ct-chicago-schools-lead-
explainer-met-20160619-story.html.
‡ Debbie Alexander and Laurie Lewis, “Condition of America’s Public School Facilities: 2012-2013 (NCES 2014-
0222),” U.S. Department of Education (Washington: National Center for Education Statistics, 2014), https://nces.
ed.gov/pubs2014/2014022.pdf; American Society of Civil Engineers, “2017 Infrastructure Report Card,” accessed
May 19, 2017, https://www.infrastructurereportcard.org/americas-grades.
§ U.S. Environmental Protection Agency, “Controlling for Lead in Schools: A Summary of State Programs”
(Washington: EPA, Oce of Water, 2004), EPA-810-R-04-00, accessed Jan. 22, 2017, https://www.epa.gov/
sites/production/files/2015-09/documents/report_lcmr_schoolssummary.pdf; U.S. Environmental Protection
Agency, “Lead in Drinking Water in Schools and Childcare Facilities,” accessed June 5, 2017, https://www.epa.gov/
dwreginfo/lead-drinking-water-schools-and-childcare-facilities.
Continued on next page

28
|| U.S. Environmental Protection Agency, “3Ts for Reducing Lead in Drinking Water in Schools” (Washington:
EPA, 2006), https://www.epa.gov/sites/production/files/2015-09/documents/toolkit_leadschools_guide_3ts_
leadschools.pdf.
# Centers for Disease Control and Prevention, “School Health Policies and Practice Study: Results From the School
Health Policies and Practices Study, 2014” (Atlanta: Centers for Disease Control and Prevention, 2015): 119, http://
www.cdc.gov/healthyyouth/data/shpps/pdf/shpps-508-final_101315.pdf.
** Healthy, Hunger-Free Kids Act of 2010, Pub. L. No. 111-296, 124 Stat. 3183 (2010), Section 221 (u) 2.
†† U.S. Department of Agriculture, “Program Information Report (Key Data)” (Washington: USDA, 2016), http://www.
fns.usda.gov/sites/default/files/datastatistics/keydata-january-2016.pdf; U.S. Department of Agriculture, “Child
and Adult Care Food Program: Why CACFP Is Important,” accessed Feb. 4, 2017, http://www.fns.usda.gov/cacfp/
why-cacfp-important.
‡‡ U.S. Department of Agriculture, “Resources for Making Potable Water Available in Schools and Child Care
Facilities,” Memo Code SP 49—2016, CACFP 18—2016 (Alexandria, VA: USDA, Food and Nutrition Service, July 20,
2016), http://media.wix.com/ugd/9c073b_31708a4607294627a28777bc30668936.pdf.
§§ Health Canada, “Lead in Drinking Water” (October 2016), http://www.healthycanadians.gc.ca/health-system-
systeme-sante/consultations/lead-drinking-water-plomb-eau-potable/alt/lead-drinking-water-plomb-eau-
potable-03-01-2017-eng.pdf.
|| || National Conference of State Legislatures, “State Legislation on Lead, Lead in Water, Lead in Schools 2016-2017,”
February 2017.
## “Drinking Water Test Results: Oregon Schools,” Oregon Health Authority (2016), http://geo.maps.arcgis.com/apps/
MapSeries/index.html?appid=6a4f2b6001bd474ca7d0a7f0c2552f57.
*** State of Rhode Island, “An Act Relating to Waters and Navigation—Lead and Copper Drinking Water Protection
Act,” accessed Jan. 13, 2017; State of Rhode Island General Assembly, “Assembly Passes Rep. Naughton Bill to Test
Public Drinking Water for Lead, Copper Contamination,” accessed Jan. 13, 2017, http://webserver.rilin.state.ri.us/
BillText16/HouseText16/H8127.pdf.
Residential lead service line replacement
Under the Lead and Copper Rule, when testing finds lead concentrations that exceed the 15 ppb action level
in more than 10 percent of the samples, the utility must evaluate its corrosion control practices, conduct
public education, and initiate LSL replacement. Water systems removing LSLs must oer property owners the
opportunity to replace their portion of the line at the same time. But because owners cannot be compelled to pay
for replacement of their lines, the public portion is often all that gets updated.
However, research showing that lead concentrations increase during and after such partial remediation has
raised concerns about safety.
53
For example, one analysis based on an event in Washington, DC, found that
children living in homes with lead in at least some part of their service lines were twice as likely as those living
in homes without LSLs to have blood lead of 5 to 9 μg/dL and three times as likely to have levels at or above
10 μg/dL. The same study did not find a statistically significant dierence between blood lead levels of children
from homes with partial versus full LSLs,
54
indicating that partial replacements—in which only one portion of a
line is updated—are inadequate to protect children from exposure.

29
In 2011, an expert panel advising the EPA reviewed pilot studies and anecdotal reports from utilities and
concluded that partial LSL replacement does not reliably reduce water lead levels, at least in the short term,
and may result in more harm than benefit.
55
A recent field study monitoring partial replacement over
18 months found a short-term increase immediately following replacement and then slightly lower water
lead thereafter.
56
A Canadian study also showed a short-term (less than one month) increase but found no
improvement compared with no replacement after six months. These analyses confirm the limited benefits
of partial replacement for reducing water lead levels and conclude that full replacement is preferable.
The number of LSLs in use across the country is unknown, but estimates suggest that between 5.5 and 10 million
LSLs provide water to an estimated 15 to 22 million people. Similarly, no national data characterize the levels of
lead in U.S. drinking water, so as communities work to more clearly identify the number of LSLs in operation, the
estimates could prove low.
57
Policy in Action: Strategies to Promote Lead Service Line Replacement
Milwaukee requires full replacement of lead service lines with copper pipe if a leak or failure is
discovered or if the utility-owned portion is replaced on a planned or emergency basis. The city
is using $2.6 million in state grants to replace lines at 300 day care centers and 300 residences
as well as $3.6 million of its own funds to cover replacement of the city-owned portion of
600 other residential lines. The city’s total $3.9 million budget for the program also includes
funds to help pay for replacement of privately owned LSLs at the same time that the city
updates the public portions and to provide water filters and bottled water to property owners
during the work. Under the program, property owners are responsible for no more than one-
third of the cost of replacement up to $1,600 if the work is done by a city contractor, and they
can pay their share over 10 years. Previously, a property owner was responsible for the full cost,
which could be as much as $7,000.
Milwaukee Water Works will use customer water payments to cover the balance of the
cost to replace the city-owned portions, and property taxes will cover the dierence for the
private portion. The program is expected to take several decades to complete, reaching
about 600 properties a year until all 68,300 known residential LSL are replaced.
*
In 1986, Woonsocket, Rhode Island, adopted a policy requiring builders to replace the entire
lead service line when a structure is sold, demolished, or replaced.
†
The property owner is
responsible for the cost of the private side, and the city pays for its part at the same time, if
it has not already been replaced.
In November 2016, the Centers for Medicare & Medicaid Services (CMS) authorized an
amendment to allow Michigan’s Children’s Health Insurance Program (CHIP) to pay for
the replacement of water pipes and fixtures from the homes of low-income families with
children, marking the first such approval.
Continued on next page

30
The amendment was developed under a provision that allows a state to access special federal
CHIP matching funds for certain noncoverage-related expenditures that have a value of no
more than 10 percent of the state’s total amount paid for program benefits. Eligible activities
include initiatives targeted at improving the health of children, outreach, translation or
interpretation services, payments for other child health assistance such as specialty care not
included in the benefit package, and other reasonable administrative costs.
‡
Properties in Flint with contaminated water receive first priority, and any property in the state
with a resident under 19 who qualifies for Medicaid or CHIP is eligible. Under the initiative,
Michigan will spend $333,000 on the eort in fiscal year 2017, which will be matched by
$23.5 million in federal funds. Over five years, the state plans to spend $119 million. Lead
paint hazard control for eligible statewide residences is also an allowable expense under
the initiative.
§
* Don Behm, “Milwaukee Aldermen Approve Lead Pipe Replacement Plan,” Milwaukee Journal Sentinel, Dec. 13, 2016,
http://www.jsonline.com/story/news/local/milwaukee/2016/12/13/milwaukee-aldermen-approve-lead-pipe-
replacement-plan/95342526.
† Lead Service Line Replacement Collaborative, “State and Local Examples,” Requiring LSL Replacement When
Opportunities Arise, accessed May 25, 2017, http://www.lslr-collaborative.org/requiring-lsl-replacement.html.
‡ Cindy Mann, Kinda Serafi, and Arielle Traub, “Leveraging CHIP to Protect Low-Income Children From Lead”
(January 2017), https://www.manatt.com/getattachment/235604fe-5700-4ec1-a25e-7d51c4e347af/
attachment.aspx; U.S. Centers for Medicare & Medicaid Services, “Michigan Health Services Initiative,” 2016 Fact
Sheets, Nov. 14, 2016, https://www.cms.gov/newsroom/mediareleasedatabase/fact-sheets/2016-fact-sheets-
items/2016-11-14-3.html.
§ David Eggert for Associated Press, “Michigan Gets Federal OK to Spend $119 Million on Lead Abatement,” Crain’s
Detroit Business, Nov. 14, 2016, http://www.crainsdetroit.com/article/20161114/NEWS01/161119887/michigan-
gets-federal-ok-to-spend-119-million-on-lead-abatement; Kaiser Family Foundation, “Michigan’s Medicaid Section
1115 Waiver to Address Eects of Lead Exposure in Flint,” accessed Jan. 26, 2017, http://k.org/medicaid/fact-
sheet/michigans-medicaid-section-1115-waiver-to-address-eects-of-lead-exposure-in-flint.
Stakeholder input
Participants in the focus groups recognized that lead in water from fixtures, solder, and pipes is a potential
source of childhood exposure. Many community residents knew about steps they could take to reduce the
risk, such as flushing taps and using bottled or filtered water, but some expressed concerns that bottled
water could also be contaminated with lead or other chemicals. A few participants across multiple groups did
indicate some misperceptions about lead in drinking water, primarily that it would be visible as a brown tint
or particulate matter. A few believed that boiling water could protect against lead when, in fact, it can
actually increase the concentration.
58
Focus group participants in Flint emphasized the burden the city’s crisis has placed on small-business owners
and residents. For example, a woman who prepared and sold tamales from her home was forced to terminate her
business because of water contamination. Others described stress and strain on social relationships resulting
from worry and embarrassment over the quality of water in homes and said fear of unsafe water even led a

31
church to discontinue baptisms. One nursing mother explained that she had asked to have her blood tested for
lead to ensure that she could safely breastfeed her child. The discussions also highlighted the importance of
tailoring LSL replacement policies to local contexts; for example, a policy to replace pipes in Lansing, Michigan,
may not be successfully replicated in Flint because as participants explained, Flint’s water pipes are intricately
bent rather than straight as in Lansing. Community members also noted that Flint’s water system is underused
due to significant population declines after the closure of General Motors’ manufacturing plants.
Participants identified potential unintended eects of LSL removal, including trac issues and closed streets.
Others expressed concern about the cost of replacing private lines. Some also worried that the expense
associated with replacing public lines would present a barrier to decision-makers in their communities. One
Flint focus group participant said he “simply didn’t trust the water and couldn’t bear to drink it” despite having
received LSL replacement and filters.
Participants in the national listening sessions said policies aimed at eliminating lead in water should address
the risks of partial LSL replacement, consider the need for better sample collection and testing and reporting
methods, include remediation as part of federal infrastructure investments, and ensure that grant assistance
is available if abatement becomes a requirement of real estate transactions. They also pointed out that most
federal, state, and local laws regarding lead hazards in housing do not address drinking water. For example,
replacement of leaded pipes or plumbing is not an eligible expense under HUD’s lead paint hazard control
grant program because the relevant statute specified only paint, dust, and soil hazards.
These participants and expert advisers also expressed concern that consumers incorrectly interpret the EPA’s
action level of 15 ppb as addressing their individual tap, rather than the water system as a whole. Stakeholders
recommended that the EPA issue a separate tap action level to help customers know when they should take steps
to reduce the amount of lead in their water. The experts also pointed to a recent assessment by Health Canada
that proposed a maximum allowable concentration of 5 ppb, and they suggested the same level could serve as an
interim standard toward the goal of getting to 1 ppb over time.
Experts further expressed concern about the water sampling protocol used by utilities, specifically that too few
samples are drawn within each home and that the samples are not consistently taken after the water has sat in
the pipe (stagnated), so they may underestimate the risk to consumers. Many factors, including the materials
used to collect samples, water flow rates, and components at the tap also influence results, so typical testing may
not always be reliable. However, identifying a revised sampling protocol was beyond the scope of this study.
Experts recommended that the EPA develop a new protocol and partner with state agencies to assure that
utilities inform homeowners about appropriate test procedures. They also thought that the EPA should require
more widespread monitoring of lead in customers’ tap water rather than the current practice of sampling only
a percentage of taps.
Proposed solution
Full lead service line replacement (from street to structure) in the U.S. could take 20 to 30 years to complete,
and a large number of homes still have lead plumbing fixtures. The research suggests a multipronged approach is
the best option for reducing children’s exposure to lead in drinking water. First, the EPA should improve corrosion
control eorts by strengthening its Lead and Copper Rule to increase compliance monitoring, the use of corrosion
control, and the adoption of optimized corrosion control, a practice that can involve adjusting the pH of water and

32
adding chemicals to inhibit corrosion. Second, rather than treating LSL replacement as a last resort, municipalities
should proactively replace lead service lines. Finally, in light of the evidence of public health risks associated with
partial replacement, municipalities should replace the entire line during routine repairs that disturb LSLs.
Although corrosion control will remain an important component of lead management, particularly for addressing
risks associated with leaded plumbing fixtures and solder, because of concerns about the consistent eectiveness
of corrosion control practices, and to permanently remediate a key source of exposure, the research team
modeled the costs and benefits of removing LSLs from homes built before 1986 where children in the 2018 birth
cohort would reside.
Although the benefit of the intervention is broad—aecting hundreds of thousands of children, as discussed
earlier—children residing in low-income communities and localities with aging infrastructure would reap the
greatest benefits from the replacement of lead service lines.
Literature summary
Evidentiary support: Scientifically supported. Strategies have been tested in multiple robust studies with
consistently favorable results.
59
Population aected: Regional or national.
60
Modeling assumptions
• The number of LSLs used in this analysis relied in part on self-reported survey data collected from water
utilities and on input from industry representatives.
61
No data source was found to document how many
children are served by LSLs or their blood lead levels, so the team used a national survey of water systems
to first estimate that 6.84 percent of the U.S. population is served by a lead service line and then applied
that percentage to the roughly 4 million children estimated by the Current Population Survey to be in the
2018 cohort.
62
This calculation determined that the number of children born in 2018 who would be served
by a lead service line is 272,285.
63
• In the absence of national data to characterize the level of lead in drinking water in homes served by LSLs,
the research team used two water lead levels for reference. A mean concentration of 11.4 ppb was derived
from unpublished profiling samples from five Midwest utilities that were compliant with the Lead and Copper
Rule but were not considered to have optimized corrosion control, and a lower level of 5 ppb was taken from
profiling samples of an eastern U.S. utility viewed as using optimized corrosion control and from unpublished
data from the city of Ottawa.
64
These levels were selected to be indicative of systems in compliance with the
Lead and Copper Rule and to reflect the likely mean concentration of lead in water after stagnation. The team,
in consultation with members of the advisory committee, assumed that LSL replacement could reduce drinking
water lead levels to 2 ppb, rather than zero, because of remaining lead plumbing fixtures and solder in homes.
• To estimate baseline levels for children living in homes built before 1986 (the year the EPA banned lead in
drinking water pipes), the team used NHANES blood lead level data for children residing in homes built before
1990—the closest available year.
• Although two well-designed studies from the literature review provided an eect size for the relationship
between lead in water and children’s blood lead levels, both had limitations that made them inappropriate
for use in this study. Therefore the research team used the EPA’s Integrated Exposure Uptake and Biokinetic
(IEUBK) model estimates of 0.042 μg/dL change in blood lead per 1 ppb dierence water lead.
65
Applying this
estimate to the expected water lead changes, the team estimated that full residential LSL replacement would

33
prevent a 0.40 μg/dL and a 0.13 μg/dL increase in blood lead, for the 11.4 ppb and 5 ppb baseline water lead
levels, respectively, and then applied these estimates to children’s starting blood lead levels from NHANES.
(See the appendix for more details.)
• In the absence of national pricing data for full LSL replacement, the research team estimated a per-unit cost
of $6,000. A 2008 national survey of utilities found that typical replacement costs ranged widely from
$250 for the utility portion and $600 for the customer portion to $3,000 and $4,000, respectively.
66
A
recent informal survey of all systems known to be pursuing full LSL replacement suggested average costs of
roughly $7,500.
67
Given the cost variations across localities, the research team combined these estimates
to calculate the per-unit cost.
• The benefits include one child per home from the 2018 birth cohort as well as 80,000 additional children
born into the remediated homes in the subsequent 10 years. They do not account for children who visit but
do not reside in those homes.
Findings
The analysis, including the calculations of blood lead, cost, and children aected as well as the modeling, found
that full LSL replacement across all homes built before 1986 with resident children would:
• Protect 352,000 children, including 272,000 born in 2018 and 80,000 born into the same homes over the
next 10 years.
• Cost an estimated $2.0 billion for the 2018 cohort.
For homes with baseline water lead levels around 11.4 ppb, the intervention would:
• Prevent an increase of 0.40 μg/dL lead in the blood of children in the 2018 birth cohort.
• Produce total future benefits of $2.7 billion, including $480 million for the federal government and
$250 million for states and municipalities.
• Generate roughly $1.33 per $1.00 invested.
If, alternatively, baseline water lead levels were 5 ppb, replacing LSLs would:
• Prevent an increase of 0.13 μg/dl lead in the blood of children in the 2018 birth cohort.
• Yield future benefits of $860 million, including $150 million for the federal government and $80 million for
states and municipalities.
• Result in $0.42 in benefits for each $1 invested. (See Table 3.)

34
Table 3
Every Dollar Invested in Full Lead Service Line Replacement Would
Generate $.42 to $1.33 in Benefits
Cost-benefit analysis, for two initial water lead levels
Baseline estimates
Number and percentage of children born
in 2018 into homes built before 1986 (1 child per unit)
2,352,000 (59%)
Percentage of those children in homes with potential lead
service lines (LSLs)
6.84%
Average blood lead level for children without intervention 1.19 μg /dL
Starting level of lead in water (ppb) 11.4 5
Predicted impacts
Homes receiving lead service line replacement 272,000
Children aected (including future cohorts) 352,000
Expected decrease in water lead (ppb) 9.4 3
Prevented blood lead level increase per child (μg/dL) 0.40 0.13
Gross future
benefits
Initial
cohort
Earnings $2.0 billion $640 million
Health savings $40 million $10 million
Education savings $50 million $20 million
Quality-adjusted life years benefits $80 million $30 million
Future cohorts (through year 10) $550 million $170 million
Total gross future benefits $2.7 billion $860 million
Share to federal government $480 million $150 million
Share to state and local governments $250 million $80 million
Share to households, the private sector, and other
nongovernmental entities
$2.0 billion $630 million
Continued on next page
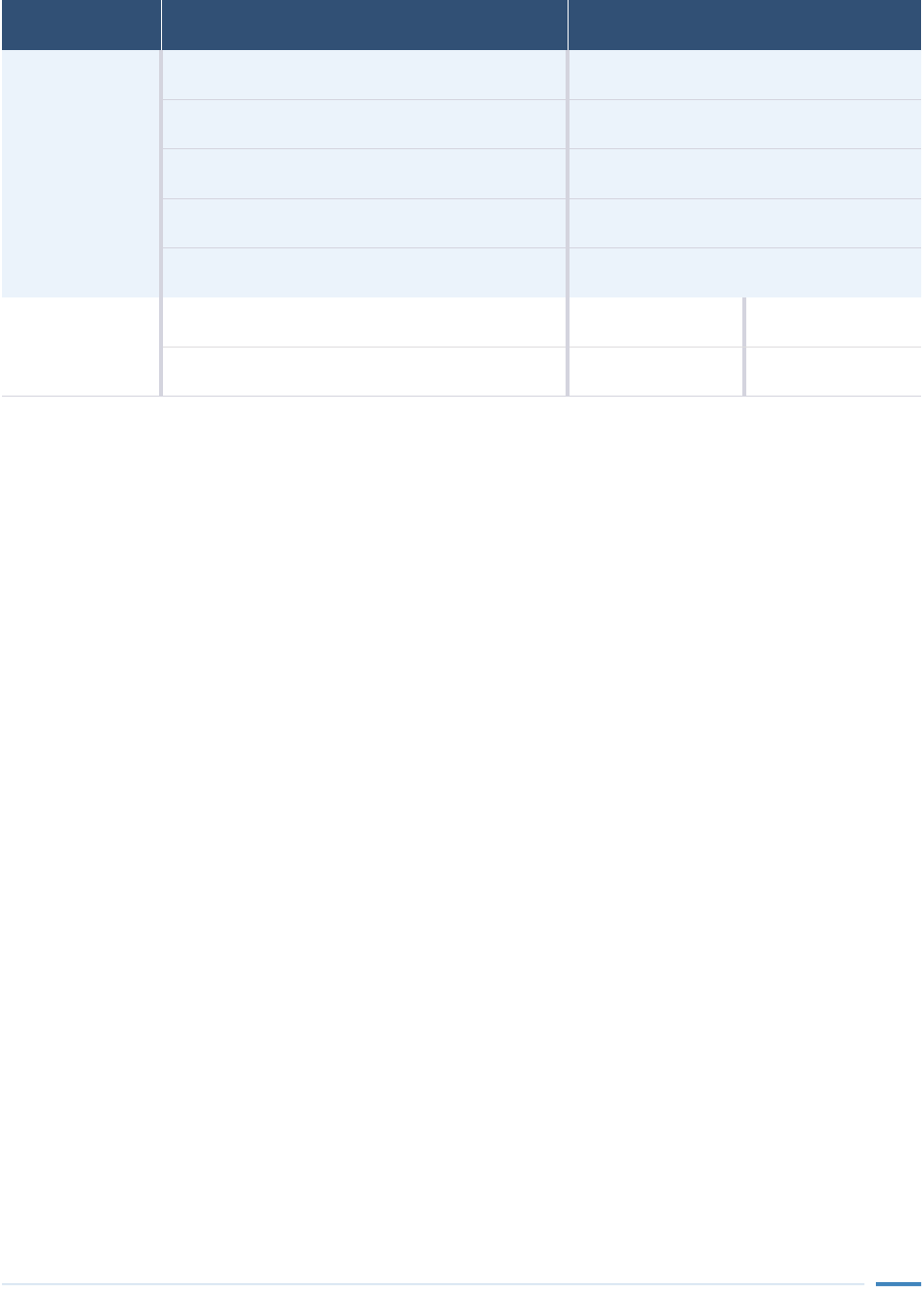
35
Costs
Testing cost per potential lead service line $175
Total testing cost $410 million
Full lead service line replacement cost per home $6,000
Full lead service line replacement cost for all homes $1.6 billion
Total costs $2.0 billion
Net
Net future benefits $680 million -$1.2 billion
Cost-benefit ratio 1.33 0.42
Notes: Analysis is based on the 2018 birth cohort, estimated at approximately 4 million children. Analysis includes benefits for future
cohorts. Total future benefits include small changes in incarceration costs not itemized in the table. Values may not add up to totals because
of rounding.
Source: Altarum Institute Value of Prevention Tool calculation
© 2017 The Pew Charitable Trusts

36
Policy in Action: Replacing Lead Service Lines
From 2004 through 2016, Lansing, Michigan, replaced 12,150 LSLs with copper lines at a cost of
$44.5 million through a program of the Lansing Board of Water and Light (BWL), a municipally
owned utility.
*
In 2004, then-Michigan State Senator Virg Bernero encouraged local ocials
to advocate with BWL Commissioners to accelerate the removal of Lansing’s LSLs. The BWL
funded the program as an infrastructure investment and utility customers shared the cost
through an increase in water rates.
†
BWL prioritized lines serving schools and licensed day care
centers, areas where testing showed that children had high blood lead levels, households with
pregnant women or children under 6, and other places with large concentrations of LSLs.
‡
BWL has developed a faster, more ecient method for replacing pipes: What had been a
nearly eight-hour, $9,000 job requiring a trench to be dug from the main to the foundation
of the house was streamlined to four hours and $3,600. Now, rather than trenching, BWL digs
a hole in the street and another at the shut-o valve and pulls a new pipe in behind the old
one.
§
Where possible, the program has followed planned street, sewer, and other infrastructure
projects to minimize street closures and reduce street reconstruction costs.
||
BWL water quality reports indicate a decrease in lead levels in the water over 10 years, with
90 percent of homes falling from 11.3 ppb in 2005 to no more than 7.8 in 2015.
#
Although BWL
has completed its LSL replacement program, it plans to continue corrosion control processes.
* Lansing Board of Water and Light, “Lead Service Advisory Information,” accessed Jan. 12, 2017, https://lbwl.com/
Community-Impact/Water-Quality/Lead-Service-Information; Lansing Board of Water and Light, “BWL 2015
Annual Water Quality Report,” accessed Jan. 12, 2017, http://lbwl.com/WaterQualityReport; Lorna Benson, “In
Battle to Keep Lead From Water, St. Paul Digs Deep,” MPR News, May 25, 2016, https://www.mprnews.org/
story/2016/05/25/water-stpaul-lead-pipes.
† Trent Gillies, “Flint Crisis Can Be Fixed With $55M in New Pipes: Lansing Mayor,” CNBC, April 24, 2016,
http://www.cnbc.com/2016/04/22/flints-crisis-can-be-fixed-with-55m-in-new-pipes-lansing-mayor.html.
‡ Lansing Board of Water and Light, “Lead Service Advisory Information.”
§ Faith Miller, “Lansing BWL Helping Flint Figure Out How to Replace Lead Pipes,” WILX 10, Feb. 9, 2016, http://www.
wilx.com/home/headlines/Lansing-BWL--368260751.html.
|| Lansing Board of Water and Light, “Lead Service Advisory Information.”
# Lansing Board of Water and Light, “BWL 2015 Annual Water Quality Report”; Lorna Benson, “In Battle to Keep Lead
From Water, St. Paul Digs Deep.”

37
Potential challenges
Although specifics vary across communities, service lines are typically jointly owned: The utility generally
owns the portion running from the water main at the street to the property line, while the section from the
property line into the home, as well as the household plumbing, belongs to the property owner. Also, some
cities assess substantial permitting fees; for example, Chicago reportedly charges $3,500 for city permits
to perform the work.
68
The concerns discussed above about partial LSL replacement risks have prompted some municipalities, such
as Lansing, Madison, and Milwaukee, to prohibit the practice and have driven others to authorize public water
utilities to replace the privately owned lines.
69
Promptly replacing LSLs would improve children’s health and
produce economic benefits, but it also would be costly and has the potential for unintended consequences.
In particular, avoiding excessive costs to taxpayers, utilities, and ratepayers; proactively planning for the safe
disposal of removed leaded lines; and minimizing trac issues, street closures, and disruption to residents would
all require significant planning, budgeting, and organizational capacity. In addition, investing in LSL removal could
constrain resources and limit expenditures for other drinking water-related priorities.
The EPA’s Drinking Water State Revolving Loan Fund (DWSRF) oers one potential means of osetting these
expenses. The fund was created in 1996 as an amendment of the Safe Drinking Water Act and is appropriated
annually by Congress.
70
The program provides infrastructure grants to the states, the District of Columbia, and
Puerto Rico for eligible projects, such as facility upgrades to improve drinking water quality and installation of
water storage tanks. Grant awards are based on the most recent Drinking Water Infrastructure Needs Survey and
Assessment, and states must provide 20 percent in matching funds. As water systems repay loans, the principal
and interest are directed back into the fund. In total, the DWSRF has provided over $32 billion to water systems
through nearly 13,000 grants.
Dale G. Young/The Detroit News
Lansing Board of Water and Light employees replace the last lead service line with copper pipes in Lansing, Michigan, on Dec. 14, 2016.

38
Lead paint hazards
I didn’t think about it. … We had repainted every surface of the house.
It looked clean. It looked neat. It looked ready. But there was still lead.”
—Baltimore resident
Lead-based paint and the contaminated dust it generates in homes and soil represent one of the most dangerous
and widespread sources of exposure aicting children.
71
The relationship between lead paint and blood lead has
been extensively studied.
72
More than half of homes built before 1978 have some lead-based paint, and the share
increases to 76 percent and 86 percent for homes built before 1960 and 1940, respectively.
73
The 2006 American
Healthy Homes Survey found that more than a third of the nation’s housing stock (an estimated 37 million
residences) contain lead paint, and more than 1 in 5 homes (roughly 23 million) have deteriorating lead paint or
dust or soil lead levels that exceed federal standards. Approximately 3.6 million homes with lead paint hazards
house young children, including those from roughly 1.1 million low-income households.
74
Residential remediation
Reducing lead paint hazards in homes involves testing paint, dust, and soil to determine whether levels are above
federal standards. Once a lead paint problem is identified, property owners typically choose from one of two
methods for dealing with it: Long-term “abatement” can last at least 20 years and involves either permanently
covering or removing lead paint,
75
while shorter-term “interim controls” include repairing flaking and peeling
paint and covering contaminated soil with mulch or grass. Windows have the highest levels of lead paint and
dust compared with other building components, and replacing windows with lead paint has been shown to
deliver large, sustained reductions in dust lead levels, including on floors that children are likely to contact more
frequently.
76
One barrier to replacing old windows coated with lead paint is provisions of the National Historic
Preservation Act, which along with state and local rules restricts replacement of features such as windows in
historic homes.
77
The preponderance of research evidence, including from multiple randomized-control trials and systematic
reviews, demonstrates the eectiveness of lead paint hazard control,
78
but a small body of research has
contradicted those findings. A few studies from the late 1980s and early 1990s found increased blood lead levels
after abatement, but those discordant findings were the result of unsafe practices such as using high heat to
remove paint, which created dangerous fumes and dust,
79
and which the federal government banned more than
20 years ago. In addition, some systematic reviews have found limited evidence to support lead paint abatement.
However, those studies focused on the ecacy of treatment measures in reducing elevated blood lead levels
in children,
80
which is an imperfect metric because blood lead can remain elevated for months or years after
exposure as lead is exchanged between blood and bone.
81
In children, bone lead represents about 70 percent of
total body lead,
82
so blood levels of lead-exposed children would not be expected to be statistically dierent one
year after their homes were treated. Therefore, not only do those findings not suggest that the intervention is
ineective, they in fact underscore the importance of actions, such as abatement, that can prevent exposure.

39
The primary federal law concerning lead paint hazards in housing is the Residential Lead-Based Paint Hazard
Reduction Act, also called Title X, to reflect the section of the Housing and Community Development Act of 1992
in which it was enacted.
83
Key features of the act include:
• Authorizing the HUD lead hazard control grant program, which is the federal government’s primary means of
assisting homeowners with control eorts. The program makes up less than 0.3 percent of the department’s
budget.
• Creating a certification system for individuals and businesses performing lead control activities.
• Requiring either interim controls or lead abatement for federally owned and assisted housing, such as public
and military housing.
• Establishing the federal lead disclosure rule, which requires property owners to reveal any known lead paint
hazards to prospective buyers or tenants before a property is sold or rented.
• Defining existing lead-based paint in housing as containing 5,000 ppm of lead or 1 mg/cm
2
.
• Requiring EPA to publish standards for lead in dust and bare soil at residential properties.
Title X led to a significant reduction in the number of homes with lead paint hazards. Specifically, more than
190,000 homes have been made lead-safe with HUD lead hazard control grants since the program’s inception in
1993. The program has a budget of about $90 million that supports lead-hazard reduction in roughly 7,000 units
each year, but the funding amount falls far short of the $230 million recommended by a federal lead poisoning
prevention task force in 2000.
84
About 12,000 low-income homes undergo lead paint hazard control annually
under HUD regulations authorized by Title X that apply to federally assisted housing. Additionally, HUD, the
EPA, and the Department of Justice enforce the federal lead disclosure rule which to date has yielded $31 million
in settlement funds from property owners, and under landlords’ agreements with HUD, the remediation of lead
paint hazards in more than 188,000 homes of low-income families.
Rental housing built before 1960 that is in poor condition and is occupied by low-income families carries the
greatest lead risks. States and local agencies can use available data to identify the neighborhoods and even
blocks or streets that have these characteristics and target resources to those areas.
85
One study found that
children from low-income families residing in federally assisted rental properties had lower blood lead levels than
comparable children living in housing without federal subsidies.
86
These results suggest that the former group’s
rental units may be in better condition because of federal requirements and that unsubsidized low-income
housing should be the primary focus for action in many states and localities. However, in communities that have
strong policies in place to prevent children from being exposed to lead in rental housing, low-income owner-
occupied homes, such as those handed down through generations, pose the more serious threat. Such variation
in risk profiles within and across communities underscores the need for neighborhood-level data to support
decision-making.
Forty-four states have adopted laws addressing lead paint hazards, and 38 require certification for contractors
that conduct lead inspections and abatement. EPA handles such licensing for the remaining states.
87
Several
municipalities also have taken action to address lead hazards in housing through code enforcement or public
health laws. Such local government action has the advantage of being targeted to communities’ immediate
situations. For example, the city of Rochester, New York, used neighborhood-level blood lead data to prioritize
enforcement of its local law. Municipal laws also are often more easily amendable than federal or state laws.
88

40
Frequently, a small number of rental units is responsible for poisoning many children in a given community. For
example, in Chicago, 67 high-risk buildings contributed to 994 cases of high lead levels, and in Jeerson County,
Kentucky (home to Louisville), 79 houses were home to 35 percent of the children with blood lead levels at or
above 20 μg/dl.
89
This is largely because most state and local laws permit property owners to re-rent units where
a child has been exposed to lead even if the hazards persist. Laws requiring inspection and treatment of units
with identified lead hazards can prevent multiple cases of lead poisoning at the same address. A study found that
Massachusetts and Ohio, which mandate inspection and treatment of units with hazards, were 79 percent less
likely than Mississippi, which lacks such a requirement, to have residential addresses that repeatedly contributed
to high lead levels in children.
90
Policy in Action: Local Lead Paint Laws
In Rochester, New York, 87 percent of homes were built before 1950, and 60 percent of
housing is tenant-occupied.
*
In December 2005, the City Council passed an ordinance requiring
regular inspections of most pre-1978 rental housing for lead paint hazards as part of the city’s
certificate of occupancy process for rental properties.
†
Housing inspections may be triggered by a new certificate of occupancy, renewal of an existing
certificate, a neighborhood survey, a referral by an outside agency, or a complaint. Single-family
and duplex rental units are inspected every six years with some exceptions, and buildings with
three or more units as well as mixed-use properties are inspected every three years.
To receive a certificate, property owners must correct identified lead hazard violations. The city
maintains an online database of all lead-safe units and properties granted a certificate.
‡
Experts describe Rochester’s law as one of the smartest in the nation.
§
In the decade since the
ordinance’s passage, the city has inspected more than 141,000 homes and the number and
proportion of children with high blood lead levels has decreased countywide. In 2004, 900
children tested for lead in Monroe County had levels above the CDC’s action level at the time of
10 μg/dL compared with 206 children in 2015.
||
Between 1997 and 2011, the number of children
with blood lead over 10 μg/dL decreased roughly twice as fast in Monroe County as it did in
New York state as a whole and nationwide.
#
Despite this significant progress in 2015, 988 of
14,283 children tested—enough to fill more than 40 kindergarten classrooms—had blood lead
levels at or above CDC’s current reference value of 5 μg/dL, indicating that additional eorts are
needed in Rochester.
**
The District of Columbia’s Lead Hazard Prevention and Elimination Act of 2008, amended in
2011, prohibits the presence of lead-based paint hazards in dwelling units, common areas of
multifamily properties, and day care and prekindergarten facilities constructed before 1978.
††
Before a purchaser or tenant is obligated under contract to buy or lease a unit, the property
owner must prove no lead-based paint hazards were present within the previous 12 months.
‡‡
Continued on next page

41
A related provision extends this requirement to units occupied or visited by a child or pregnant
woman. In addition, if owners discover lead-based paint in their properties, they must disclose
it to their tenants within 10 days.
* National Institutes of Health, “Rochester’s Lead Law: Evaluation of a Local Environmental Health Policy Innovation,”
accessed Jan. 13, 2017, http://www.cityofrochester.gov/article.aspx?id=8589936091.
† City of Rochester, “Article III: Lead-Based Paint Poisoning Prevention,” accessed Jan. 13, 2017, http://ecode360.
com/8677707; City of Rochester, “Lead Paint—Get Prepared,” accessed Jan. 13, 2017, http://www.cityofrochester.
gov/article.aspx?id=8589936091.
‡ Dan Telvock, “Rochester Leads on Lead While Bualo Dallies,” Investigative Post, accessed June 9, 2017, http://www.
investigativepost.org/2014/11/12/bualo-lacks-leadership-lead-poisoning-problem.
§ Rachel Dissell and Brie Zeltner, “How Rochester Responded to Its Lead Poisoning Problem: Toxic Neglect,” Cleveland
Plain Dealer, Oct. 23, 2015, http://www.cleveland.com/healthfit/index.ssf/2015/10/how_rochester_stopped_
using_ch.html.
|| Meaghan M. McDermott, “Lead Levels on the Rise in Monroe County,” Democrat & Chronicle, June 28, 2016,
http://www.democratandchronicle.com/story/news/2016/06/28/children-lead-levels-monroe-county/86471002.
# Byron Kennedy et al., “Declines in Elevated Blood Lead Levels Among Children, 1997-2011,” American Journal of
Preventive Medicine 46, no. 3 (2014): 259–64, http://dx.doi.org/10.1016/j.amepre.2013.11.007.
** McDermott, “Lead Levels on the Rise.”
†† D.C. Ocial Code § 8-231.01 et seq.
‡‡ D.C. Municipal Regulations and D.C. Register, “Regulation of Lead-Based Paint Activities.”
Stakeholder input
Regardless of race, ethnicity, and socioeconomic status, focus group participants worried about children coming
into contact with lead paint at home. Nearly all parents said they wished they had more information about
lead hazards in their homes before their children were exposed. Many also said that lead disclosure forms did
not suciently communicate the dangers, and that they would prefer to have access to property inspection
documents. Two homeowners admitted disregarding the lead disclosure information when they purchased their
homes to avoid seeming fussy or losing the sale. Renters suggested that fear of eviction might prevent them from
raising concerns about lead hazards with their landlords. Similarly, concerns about property devaluation keep
many property owners from testing for lead.
Community residents largely agreed that fining noncompliant landlords is inadequate because it does not
necessarily compel property owners to address the lead hazards. Families that moved to avoid continued
exposure worried that future renters could be in danger because of the landlord’s failure to comply or inability
to aord abatement or remodeling. Landlords, in turn, worried about lawsuits, even when the rental unit was
not confirmed as the primary source of exposure.

42
Not surprisingly, residents and landlords had dierent views on requiring inspections to identify lead hazards.
Some renters had experienced conflicts with landlords over lead hazards, while property owners worried that the
costs of addressing lead could cause financial strain and diculty selling homes that still required abatement.
Funding for abatement could mitigate some of these unintended harms. The cost of remediation and restrictions
on the type of modifications allowed to historic properties, such as window replacements, could make it dicult
for landlords meet lead requirements.
To reduce these burdens, some participants proposed prioritizing inspections for homes with young children
or units rented using housing vouchers, but targeting units with young children could mean lead paint hazards
in the homes of grandparents or other caregivers go undetected and could discourage landlords from renting
to families. Another suggestion was osetting the cost of window replacement and lead abatement through
tax credits and financing to minimize burdens and encourage landlords and homeowners to have properties
inspected. Some participants, however, identified citizenship requirements to receive financing and credits as a
barrier for some property owners to access such funding.
In interviews, stakeholders recommended that jobs generated to address lead paint hazards in housing, such as
inspectors and lead paint hazard control workers, be oered first to community members in lead-aected areas.
Policy in Action: State Lead Paint Hazard Control Laws
Maryland’s Reduction of Lead Risk in Housing Act, enacted in 1994 and amended in 2012,
requires owners of rental residences built before 1978 to annually register their properties with
the Maryland Department of the Environment indicating that they are free of chipping, peeling
paint, and lead-contaminated dust. To qualify for registration, owners must hire a certified
contractor to address any defective paint and have an accredited inspector verify compliance
before any change in occupancy. The department files between 500 and 800 violation notices
annually, and a team from the state’s attorney general’s oce is responsible for enforcing
actions against noncompliant owners. Since the law’s enactment, the rate of high blood lead
levels in Maryland children has declined by 98 percent: In 1993, 14,546 (23.9 percent) of the
60,912 children under 6 tested had blood lead levels of 10 μg/dl or higher, and by 2015, that
figure had declined to 377 children of 110,217 (0.3 percent).
*
Since 1993, New York state regulations have included a Notice and Demand component that
requires property owners to address lead hazards to prevent exposure. After inspecting a unit
for lead paint hazards, including deteriorated paint and contaminated dust and bare soil, the
local health department can issue a written notice, which outlines the hazards present and
requires owners to submit a corrective work plan within a fixed number of days.
†
Continued on next page

43
Proposed solution
According to HUD, roughly 23 million residences have lead hazards such as peeling paint, contaminated
dust, or toxic soil, and 3.6 million of these are home to young children.
91
Substantial evidence including from
randomized control trials indicates that remediating lead paint hazards reduces blood lead levels, and many
states and localities have undertaken successful lead hazard control eorts.
92
Given this diverse body of
evidence, the research team chose to analyze the impacts of testing and treating paint, dust, and soil, and
replacing old windows.
Literature summary
Evidentiary support: Scientifically supported. Strategies have been tested in multiple robust studies with
consistently favorable results.
93
Population aected: Regional or national.
94
Modeling assumptions
• Using published literature on the eects of lead paint hazard control on dust lead levels and studies of the
relationship between lead in dust and in blood, the team undertook a two-step process to estimate that
removing lead paint hazards from homes before those children are born would prevent a 40 percent increase in
their blood lead.
To establish the reduction in dust lead levels resulting from lead paint hazard control, the team used data from
a long-term follow-up of interventions in 189 nonrandomly selected homes from multiple regions of the country
that found an 89 percent decline in dust lead 12 years after treatment.
95
The study did not include a control
group for ethical reasons, but it is, nevertheless, the largest and longest national evaluation of lead hazard
control eorts, and its findings align with many smaller studies of lead paint hazard control eects.
96
Second,
the team used a national cross-sectional survey conducted from 1999 through 2004 to predict the eect of
decreased dust lead on child blood lead levels.
97
The data indicated that the above-referenced 89 percent
reduction in dust lead would prevent a 39.5 percent increase in children’s blood lead levels.
* Maryland Department of the Environment, “Lead Poisoning Cases Drop in Baltimore and in Maryland, Department
of the Environment Moves to Reduce Potential Exposures in More Homes,” accessed Jan.12, 2017, http://news.
maryland.gov/mde/2015/09/03/lead-poisoning-cases-drop-in-baltimore-and-in-maryland-department-of-the-
environment-moves-to-reduce-potential-exposures-in-more-homes; Maryland Department of the Environment,
“Childhood Blood Lead Surveillance, Statewide 1993-2014,” accessed June 14, 2017, http://www.mde.state.
md.us/programs/PressRoom/Documents/Childhood_Lead_Surveillance_Statewide_1993-2014.pdf; Maryland
Department of the Environment Lead Poisoning Prevention Program, “Childhood Blood Lead Surveillance in
Maryland: Annual Report 2015,” accessed May 25, 2017, http://www.mde.state.md.us/programs/land/documents/
leadreports/leadreportsannualchildhoodleadregistry/leadreportclr2015.pdf.
† New York State Department of Health, “NYS Regulations for Lead Poisoning Prevention and Control—NYCRR Title
X, Part 67,” accessed Jan. 13, 2017, https://www.health.ny.gov/regulations/nycrr/title_10/part_67/#sec67-2-6.

44
• The study team used the American Healthy Homes Survey to estimate that about 75 percent of pre-1960
homes and 50 percent of pre-1978 homes have lead-based paint and would require remediation.
98
• The per unit cost of remediation is estimated based on data from HUD’s Lead Hazard Control program which
includes costs for replacing some windows, treating deteriorated paint, remediating toxic soil, and repairing
other high-risk areas, such as doors. In addition, the cost estimates include $1,000 for testing of paint, dust,
and soil to identify hazards before work is initiated and to ensure the safety of the home before residents
return. The costs do not include expenses necessary to administer lead-hazard control programs, for which
HUD spends about $2.7 million. HUD also caps administrative costs for grantee states and municipalities at
10 percent, typically less than $300,000 for a three-year program.
• The benefits include one child per home from the 2018 birth cohort as well as 67,000 additional children likely
to be born into the remediated homes in the subsequent 10 years.
99
They do not account for children who visit
but do not reside in those homes.
100
The team modeled the implementation of lead paint hazard control under four scenarios. Specifically, the models
examined impacts for those living in homes built before 1978, the year that the CPSC restricted the use of lead-
based paint for residential use, and those built before 1960, because data suggest that the use of lead paint
tapered o after that date. Additionally, the team examined the eects of lead paint hazard control for the entire
population of children and for the population from families with incomes at or below 120 percent of the federal
poverty threshold. (See Table 4.)
Findings
The analysis determined that comprehensive lead paint hazard remediation for the children born in 2018,
would, on average:
• Protect 311,000 low-income children who live in homes built before 1960.
101
This includes 244,000 children
born in the initial 2018 cohort, with an additional 67,000 births estimated born into the same homes in the
following 10 years.
• Cost approximately $2.5 billion.
For homes with floor dust lead levels around 20 μg/sq. ft., the intervention would:
• Yield $3.5 billion in total discounted future benefits, including:
• $630 million for the federal government.
• $320 million for state and local governments.
• Generate $1.39 per $1 invested.
If, alternatively, baseline floor dust lead levels are 10 μg/sq. ft., the intervention would:
• Yield $2.8 billion in total discounted future benefits, including:
• $490 million for the federal government.
• $250 million for state and local governments.
• Produce $1.09 for every $1 invested. (See Table 4.)
The research found that targeting this intervention only to more at-risk populations—pre-1960 homes, and
low-income residents—generates a greater return and higher net benefits.

45
Pre-1960 homes Pre-1978 homes
All Low-income All Low-income
Baseline
estimates
Number and percentage of
children expected to live in older
housing (1 child per unit)
1,068,000
(26.8%)
321,000 (8.1%)
1,934,000
(48.6%)
600,000 (15.1%)
Percentage of those children
whose homes need lead hazard
control (LHC)
75.8% 52.4%
Average blood lead level
for children if no intervention
(μg/dL)
1.34 1.63 1.25 1.53
Starting level of lead in floor
dust (μg/sq. ft.)
10 20 10 20 10 20 10 20
Predicted
impacts
Homes remediated 809,000 244,000 1,014,000 315,000
Children aected (including
future cohorts)
1,033,000 311,000 1,295,000 402,000
Expected decrease in levels of
lead in house dust
76% 89% 76% 89% 76% 89% 76% 89%
Prevented increase in blood lead
levels per child
32% 40% 32% 40% 32% 40% 32% 40%
Gross future
benefits
Initial
cohort
Earnings
$6.1
billion
$7.7
billion
$2.0
billion
$2.6
billion
$7.2
billion
$9.0
billion
$2.5
billion
$3.2
billion
Health savings
$140
million
$170
million
$50
million
$60
million
$160
million
$200
million
$60
million
$80
million
Education savings
$140
million
$170
million
$50
million
$60
million
$170
million
$210
million
$60
million
$70
million
Quality-adjusted life
years benefits
$250
million
$310
million
$90
million
$110
million
$290
million
$360
million
$110
million
$140
million
Future cohorts (through year 10)
$1.6
billion
$2.0
billion
$530
million
$670
million
$1.8
billion
$2.3
billion
$650
million
$830
million
Total gross future
benefits
$8.2
billion
$10.3
billion
$2.8
billion
$3.5
billion
$9.6
billion
$12.1
billion
$3.4
billion
$4.3
billion
Share to the federal
government
$1.5
billion
$1.8
billion
$490
million
$630
million
$1.7
billion
$2.2
billion
$600
million
$770
million
Share to state and local
governments
$740
million
$940
million
$250
million
$320
million
$880
million
$1.1
billion
$310
million
$390
million
Share to households, the
private sector, and other
nongovernmental entities
$6.0
billion
$7.5
billion
$2.0
billion
$2.6
billion
$7.0
billion
$8.9
billion
$2.5
billion
$3.2
billion
Table 4
Targeting Lead Paint Hazard Control to Older Low-Income Housing
Oers the Greatest Per-Dollar Benefits
Cost-benefit analysis by income, age of housing, and floor dust lead level
Continued on next page

46
* Results are based on dust lead levels of 10 or 20 as shown on the previous page.
Notes: Analysis is based on the 2018 birth cohort, estimated at approximately 4 million children, and includes benefits for future cohorts.
Total future benefits include small changes in incarceration costs not itemized in the table. Values may not add up to totals because of
rounding.
Source: Altarum Institute Value of Prevention Tool calculation
© 2017 The Pew Charitable Trusts
Pre-1960 homes Pre-1978 homes
All Low-income All Low-income
Costs
Cost of inspection per home $1,000
Total inspection costs $1.1 billion $320 million $1.9 billion $600 million
Cost of LHC per home $9,043 $8,269
Total LHC costs $7.3 billion $2.2 billion $8.4 billion $2.6 billion
Total costs $8.4 billion $2.5 billion $10.3 billion $3.2 billion
Net*
Net future benefits
-$210
million
$1.9
billion
$230
million
$990
million
-$690
million
$1.8
billion
$200
million
$1.1
billion
Cost-benefit ratio 0.97 1.23 1.09 1.39 0.93 1.17 1.06 1.35
Policy in Action: Financing Lead Paint Hazard Control
Massachusetts’ lead law, enacted in 1971, is one of the oldest in the country and requires that
any property built before 1978 and occupied by a child under 6 be “deleaded” by removing
or covering lead paint hazards.
*
The state also prohibits property owners from discriminating
against families with young children when renting or selling. To help homeowners pay for
abating lead hazards, including replacement of windows, Massachusetts oers income tax
credits of $500 and $1,500, depending on a property’s needs, and administers a series of loan
programs to support compliance with the law.
†
Massachusetts imposes surcharges of $25 to $100 on the annual fees of certain professional
licenses, including for real estate brokers, property and casualty insurance agents, mortgage
brokers and lenders, small loan agencies, and individuals who perform lead inspections.
‡
The
collected revenue, roughly $2.5 million annually, is deposited into the Lead Paint Education and
Training Trust Account for use by the state’s Department of Public Health.
§
In 2016, testing
found that of more than 175,000 Massachusetts children tested, just 686 under age 6 had
blood lead levels of 10 μg/dL or greater, compared with 3,095 of about 194,000 children tested
in 2001, the earliest date for which data are available online.
||
Continued on next page

47
* “What Does the Massachusetts Lead Law Require,” Massachusetts Executive Oce of Health and Human Services,
accessed Jan. 13, 2017, http://www.mass.gov/eohhs/gov/departments/dph/programs/environmental-health/
exposure-topics/lead/lead/massachusetts-lead-law-requirement.html.
† Ibid.
‡ National Center for Healthy Housing, “Lead Education Trust Fund,” 2017, accessed June 14, 2017, http://www.nchh.
org/Portals/0/Contents/Alternative-Financing-Mechanism_Massachusetts_LETF.pdf.
§ National Center for Healthy Housing, “Lead Education Trust Fund”; Centers for Disease Control and Prevention,
“Building Blocks for Primary Prevention,” accessed Feb. 14, 2017, https://www.cdc.gov/nceh/lead/publications/
building_blocks_for_primary_prevention.pdf.
|| Massachusetts Department of Public Health Bureau of Environmental Health, Environmental Public Health
Tracking, accessed May 24, 2017, http://www.mass.gov/eohhs/docs/dph/environmental/lead/stats/screening-
and-prevalence-statistics-by-community-cy-2016.pdf; Massachusetts Department of Public Health Bureau of
Environmental Health, “Prevalence of Males and Females With Confirmed Elevated BLLs >= 10 μg/dL, Screened in
2001 That Were Between 0 - <72 Months of Age,” Environmental Public Health Tracking, accessed June 6, 2017, table
generated from https://matracking.ehs.state.ma.us/Health-Data/Childhood_Blood_Lead_Levels.html.
Potential challenges
Stakeholders pointed to cost as the single biggest barrier to widespread implementation of lead paint hazard
control and suggested several financing options, many of which are included in the recommendations. (See
Page 79.) At nearly $10,000 per unit, lead paint hazard control is unaordable for many low- and middle-
income Americans. Higher housing costs can have severe consequences for low-income residents if the cost of
replacement or abatement is passed on to them. Typical lower-income households spend 40 percent of their
income on housing,
102
suggesting many people are vulnerable to even small increases in rents or mortgages.
Unaordable housing can lead to evictions, foreclosures, and homelessness, which can have devastating eects
on the health of the family.
Stakeholders also highlighted many missed opportunities to inform renters and owners about potential risks. The
federal lead disclosure rule requires only that owners document known hazards before selling or renting a home,
not that they determine if lead is in fact present, and lead in water is not covered by the law. However, because
most homes in the country have not been inspected, most owners have nothing to disclose. States can expand
upon this federal law by requiring inspections during real estate transactions.
Remediating more than a million older low-income homes with children in the country will take time. Meanwhile,
preventive housing inspections can help identify hazards and compel action before a child becomes sick.
Although prevention is the most urgent and eective policy approach, when a child has already been poisoned,
environmental inspections are vital to identify the source and compel property owners to promptly fix hazards.
States could prevent the proliferation of repeat-oender units by requiring landlords to fix lead hazards before
re-renting a unit and could mandate inspections for all units in a building where one is found to have lead hazards.
This requirement would also create jobs because of increased demand for inspection and abatement, and those
jobs could be prioritized for low-income residents of the high-risk communities. According to one estimate,
addressing lead hazards in the highest-risk homes would create 50,000 to 75,000 jobs.
103

48
Chitose Suzuki/Associated Press
Stakeholders highlighted the lack of incentives and policies to encourage replacement of old windows as
another missed opportunity. For example, federal programs such as the Department of Energy’s (DOE)
Weatherization Assistance Program (WAP) uses a “savings to investment ratio” to prioritize possible upgrades,
but guidance regarding the calculation of this ratio does not typically rank window replacement high among
WAP priorities. States and the DOE could adjust their approaches to this ratio to promote lead paint hazard
controls within the WAP.
Another potential barrier to hazard-reduction eorts is that lead-based paint is not part of property value
calculations for mortgage and appraisal purposes. For example, the Federal Housing Administration (FHA)
states that, for single-family properties it insures, the “[m]ortgagee must confirm that the Property is free of
lead paint hazards.”
104
However, this determination is typically made based on a visual inspection, not a
determination by a licensed lead professional. Without mandatory inspections for lead paint and dust in pre-1978
units, appraisers cannot adjust the market price, provide buyers with important information, or encourage owners
to correct hazards, but state and federal home financing programs could update their requirements to include
lead inspections.
Luis Benitez (left) and Jose Diaz remove lead paint in a contaminated building in Providence, Rhode Island, in 2006.

49
Lead Paint Hazards and Contaminated Soil at Schools and Child
Care Facilities
The most common sources of lead exposure in and around schools and child care settings are
lead-based paint, dust, and contaminated soil. (See “Air emissions and soil contamination” on
Page 57 for additional information about lead in soil.) This is a particular concern for young
children, because of their frequent and extensive contact with soil outside and with floors,
carpets, windows, and other indoor areas where dust gathers, as well as their frequent hand-
to-mouth activity.
*
• Approximately 65 percent of school facilities were constructed before 1980.
†
A 2014
national survey of schools and classrooms found that only about a third (34 percent) had
been inspected for lead in cracked or peeling paint in the preceding 12 months, and another
29 percent had already been identified as having lead paint hazards and remediated.
‡
• Further, a 2003 study based on data from a nationally representative sample of licensed
U.S. child care facilities showed that 14 percent have one or more lead-based paint hazards,
including 26 percent of those located in buildings built before 1960 compared with 4 percent
in newer buildings.
§
• Painted metal or wood playground equipment may also contain high levels of lead,
which becomes a risk as it ages.
||
A 1996 Consumer Product Safety Commission (CPSC)
investigation of 26 older playgrounds in 13 cities across 11 states found that 20 had
equipment with lead paint levels above 600 ppm, the CPSC’s standard at the time. In
addition, nine states and 19 cities tested 223 additional playgrounds and reported that
125 exceeded the CPSC standard.
#
Many of these playgrounds have probably been
replaced in the intervening 30 years, so these data should be interpreted with caution.
• One cross-sectional study of four inner-city child care facilities in New Orleans, which
involved testing the hands of 40 children before and after they played outside, found that
greater outdoor lead dust levels were correlated with higher levels on the children’s hands.
**
Remediating lead hazards in schools and child care facilities is subject to barriers similar to
those identified for home environments. Older buildings tend to have more problems and to be
in poorer communities with fewer resources; public schools in these places often have many
competing priorities for limited dollars. Without new funding, the cost of removing lead paint,
dust, and soil hazards may be a hardship for some school districts, as well as state and local
governments.
††
Grants for capital improvements and maintenance, particularly for schools in
high-risk communities and that serve low-income children, could help oset this burden and
improve health equity for these disadvantaged populations.
Continued on next page

50
One possible model for addressing lead hazards in schools would be the USDA’s Equipment
Assistance Grants program, which provides federal funds to state child nutrition agencies that
then competitively award grants to individual schools for the purchase of kitchen equipment
necessary to meet National School Lunch Program (NSLP) nutrition standards.
‡‡
The program
also prioritizes high-need schools where at least half of enrolled students are eligible for free or
reduced-price meals.
§§
In addition, the 2014 reauthorization of the Child Care and Development Block Grant
Act included several changes to improve the health and safety of children in early care and
education settings that could provide a springboard for action on lead hazards. Specifically
it requires states to have health and safety regulations in place for providers serving
children funded by the grant and to include “building and physical premises safety” in
provider training.
|| ||
Focus group participants cited lead paint in child care facilities, especially those in historic
buildings, as a concern, reported diculty in finding information about lead risks in these
facilities, and recommended increased testing. In addition to citing cost as a potential burden
for child care providers, stakeholders pointed out that some people care for multiple children
but don’t have a license and so might not feel safe seeking help with identifying and abating
lead hazards.
According to a participant who worked at a child care center in a church, unlicensed providers
and facilities operated by religious institutions may also not be covered under existing
regulations, which could allow lead hazards to go unaddressed. Such unlicensed and “family and
friends” child care accounts for about half of all care provided to children
under 5.
##
Stakeholders in the national listening sessions suggested using local data to target information
to parents in high-risk areas. Schools also could be a good forum for reaching parents, including
expectant parents. Because of the legacy of lead paint, stakeholders also suggested engaging a
lead professional during the planning phase of school renovations.
* U.S. Environmental Protection Agency, “America’s Children and the Environment, Third Edition,” EPA 240-R-
13-001 (Washington: U.S. Environmental Protection Agency, January 2013): 289, https://www.epa.gov/sites/
production/files/2015-06/documents/ace3_2013.pdf; Ronnie Levin et al., “Lead Exposures in U.S. Children,
2008: Implications for Prevention,” Environmental Health Perspectives 116, no. 10 (2008): 1285–93, https://dx.doi.
org/10.1289%2Fehp.11241; Howard W. Mielke et al., “The Urban Environment and Children’s Health: Soils as an
Integrator of Lead, Zinc, and Cadmium in New Orleans Louisiana, USA,” Environmental Research 81, no. 2 (1999):
117–29, https://doi.org/10.1006/enrs.1999.3966.
Continued on next page

51
† National Center for Education Statistics, “Public-Use Data Files and Documentation (FRSS 105): Condition of Public
School Facilities: 2012-13,” accessed April 6, 2017, https://nces.ed.gov/surveys/frss/downloads.asp.
‡ Centers for Disease Control and Prevention, “School Health Policies and Practice Study: Physical School
Environment,” accessed June 6, 2017, https://www.cdc.gov/healthyyouth/data/shpps/pdf/2014factsheets/phy_
sch_env_shpps2014.pdf.
§ David Marker et al., “First National Environmental Health Survey of Child Care Centers: Final Report” (Rockville,
MD: Westat Inc., 2003), http://www.nmic.org/nyccelp/documents/HUD_NEHSCCC.pdf.
|| “Protect Your Family from Exposures to Lead,” U.S. Environmental Protection Agency, Oce of Pollution Prevention
and Toxics, accessed June 6, 2017, https://www.epa.gov/lead/protect-your-family-exposures-lead.
# Consumer Product Safety Commission, “CPSC Sta Recommendations for Identifying and Controlling Lead Paint
on Public Playground Equipment” (Washington: U.S. Consumer Product Safety Commission, October 1996), http://
www.state.nj.us/dca/divisions/dhcr/rec/pdf/recleadpaint.pdf.
** Latonia Viverette et al., “Environmental Health in Minority and Other Underserved Populations: Benign Methods
for Identifying Lead Hazards at Day Care Centres of New Orleans,” Environmental Geochemistry and Health 18 no.
1 (1996): 41–45, https://dx.doi.org/10.1007/BF01757218; Howard W. Mielke et al., “The Urban Environment and
Children’s Health: Soils as an Integrator of Lead, Zinc, and Cadmium in New Orleans Louisiana, USA.”
†† Rafael Guerrero, “Local Schools Have Mixed Reactions to Bill That Would Require Lead Testing,” Chicago Tribune,
Jan. 13, 2017, http://www.chicagotribune.com/suburbs/elgin-courier-news/news/ct-ecn-schools-lead-testing-st-
0115-20170113-story.html.
‡‡ The Pew Charitable Trusts, “U.S. Department of Agriculture Equipment Grants Improve School Kitchens,” Kids' Safe
and Healthful Foods Project (June 2016), http://www.pewtrusts.org/en/multimedia/data-visualizations/2016/
usda-school-kitchen-equipment-grants.
§§ U.S. Department of Agriculture, “2016 NSLP Equipment Assistance Grants,” Food and Nutrition Service (February
2016), https://www.fns.usda.gov/2016-nslp-equipment-assistance-grants.
|| || President’s Task Force on Environmental Health Risks and Safety Risks to Children, “Key Federal Programs to
Reduce Childhood Lead Exposures and Eliminate Associated Health Impacts” (November 2016), https://ptfceh.
niehs.nih.gov/features/assets/files/key_federal_programs_to_reduce_childhood_lead_exposures_and_eliminate_
associated_health_impactspresidents_508.pdf.
## U.S. Census Bureau, “Who’s Minding the Kids? Child Care Arrangements: Spring 2011” (2013), http://www.census.
gov/prod/2013pubs/p70-135.pdf.

52
Safe renovation, repair, and painting enforcement
We bought the house in March of this year, and after buying the
house we found out that it had been painted last year, and when
the house was painted they took no precautions when they were
scraping o the lead paint.”
—Indianapolis resident
As discussed above, residential remediation is the primary strategy for preventing chronic exposure to lead dust.
However, renovation, repair, and painting activities in older homes are also a major source of lead exposure. The
use of safe work practices is critical for avoiding acute exposures from highly toxic dust, debris, and fumes that
can be created when homes undergo routine maintenance and repair, including dry scraping, power sanding, and
the use of torches and heat guns to remove paint, which in older homes is often lead-based.
105
Children can be
exposed to these hazards if the family is not relocated during the work, if dust hazards remain when the family
returns to the home, and if a parent is a contractor who brings home dust-contaminated clothes or shoes.
Unsafe and unregulated remodeling and renovation of older housing that contains lead-based paint pose
significant hazards that can increase children’s blood lead levels by as much as 69 percent.
106
In a 2013 study,
276 children ranging in age from 6 months to 2 years whose housing underwent interior renovation had mean
blood lead levels at 2 years of age that were 12 percent higher than children whose homes were not renovated.
The study also found that the higher the lead paint content in the home, the more elevated the blood lead.
107
Studies have found that work done by parents and other do-it-yourselfers has been a factor in children’s high
blood lead levels.
108
For example, in 2006-07, a review of case records of children in New York state revealed
that 14 percent of children with blood lead levels at or above 20 μg/dL lived in homes that had undergone recent
renovations. Notably, residents performed 66 percent of these renovations, suggesting that while preventing
unsafe work by contractors is important, educating homeowners and renters about proper renovation practices
is also vital.
109
Although the 1992 Title X law directed EPA to require safe work practices similar to those for lead paint
abatement the agency did not finalize its rule for renovation activities until 2008.
110
The updated regulation went
into eect in April 2010 and set training requirements, standards, and enforcement mechanisms for renovations
that disturb paint in pre-1978 buildings.
The EPA supervises compliance with the rule through its 10 regional oces. The EPA is responsible for
enforcement in 36 states and has delegated this responsibility to 14 states. However, federal oversight is severely
underfunded. In its regulatory impact assessment, the EPA estimated that 11.4 million projects in pre-1978
homes and child care facilities would potentially fall under the scope of the rule each year, with about 4.4 million
required to follow its safe practices after subtracting minor maintenance projects and structures found not to
have lead.
111

53
Unfortunately, model codes which serve as the basis for many state and local housing regulations only require
any peeling paint in housing to be repaired. However, the codes do not explain how to perform the repairs
safely, nor do they reference the EPA’s requirements. Multiple eorts to fix the codes have been rejected by the
governing International Code Council because of unfunded mandates and concerns about code ocials being
responsible for enforcement that the EPA should handle. Several state and local governments have found ways
to encourage compliance:
• New York City has a system to identify potentially unsafe renovations and intervene to prevent lead exposure.
Health department inspectors who observe uncontained paint dust or debris must take samples and stop the
work. Owners or contractors must then post a “conspicuous” sign with a phone number to access additional
information, including inspection results, until they have completed cleanup and undergone additional
inspections to confirm that the source of potential lead exposure has been addressed.
112
When contractors
resume work, they must follow safe work practices that contain and minimize dust.
113
• In the District of Columbia, where an estimated 75 percent of housing was built before 1978, contractors
seeking permits for renovation must show proof of EPA-required training.
114
• Rhode Island requires contractors working in homes and child care facilities built before 1978 to hold a
Lead-Safe Remodeler/Renovator or higher certification.
115
To ensure compliance, the cities of Providence
and Pawtucket will not issue permits for construction work at properties covered by the law without proof
of such licensure.
116
Stakeholder input
In stakeholder conversations, parents of children with a history of lead exposure frequently cited renovation as
the culprit. One mother explained that she rented a historic home after the owners completed a do-it-yourself
remodel. Flaking paint on the windows and doors contributed to her child’s high lead levels. A few other parents
related similar stories of their children coming into contact with lead during home remodeling, including
renovations completed by the parents themselves as well as contractors who lacked proper certification.
One landlord pointed out that property owners who inherit buildings from family members may not know
about renovation, repair, and painting requirements and might attempt renovations without taking required
precautions, although most participants knew that they should seek out certified contractors. In some cases,
tenants distrusted the contractors hired by their landlords or felt that landlords hired the lowest bidder without
confirming proper certification. Residents and landlords alike suggested oering free certification classes for
contractors and encouraging the hiring of local builders. Landlords recommended providing and encouraging
training for property managers and smaller renovators on lead-safe practices and requirements.
Proposed solution
According to the EPA, an estimated 4.4 million older homes need repairs and updates that could generate lead-
contaminated dust, debris, and fumes of the sort that many robust studies show could cause sharp spikes in
children’s blood lead levels.
117
Several localities have successfully implemented programs and policies to increase
the use of these safe practices. Yet focus group participants identified home repairs as an ongoing concern.
Drawing upon findings from the literature, expert input, the experience of community members, and state and
local examples, the research team modeled enforcement of the EPA’s policy requiring that renovations, repair, and
painting in homes with children and child care facilities built before 1978 use lead-safe work practices.

54
Literature summary
Evidentiary support: Scientifically supported. Strategies have been tested in multiple robust studies with
consistently favorable results.
118
Population aected: Regional or national.
119
Modeling assumptions
• Using an EPA model which suggests that following lead-safe renovation practices would prevent a 1.08 μg/dL
increase in blood lead levels of children, the team modeled the eect of compliance with the renovation rule
enforcement on a single birth cohort, in terms of lifetime earnings, health and education expenditures, and
QALYs.
120
(See Table 5.)
• The costs and the number of renovation events are based on the EPA’s regulatory impact analysis for the rule.
The impact analysis included the costs of testing, increased training and education for renovators, government
certification and enforcement, and additional necessary supplies, such as plastic sheeting.
121
The study team
added costs associated with conducting full dust clearance testing after a renovation to ensure a home is
completely safe. The EPA analysis suggested that approximately 1.27 million children age 6 and younger would
be protected by the rule and assumed an achievable compliance rate of 75 percent.
122
The research team assumed, therefore, that a cohort of children born in the same year would be equal to that
figure divided by six, or approximately 211,000. The cost calculations also include clearance dust testing following
renovations, which the EPA does not require, because evidence indicates that it is necessary to confirm the safety
of a structure.
123
The team included the annual cost of compliance for all homes and child care facilities built
before 1978, but only counted benefits for children from the 2018 cohort living in those homes or visiting those
facilities. The calculations exclude benefits for children who may visit during a renovation activity or may move
into a remediated house in the future.
The federal estimates, and thus the models used in this study, exclude do-it-yourself renovations, which are not
regulated by the EPA. However, one analysis found that these projects accounted for most renovation-related
lead poisoning.
124
Findings
The analysis found that, for children born in 2018, rigorous enforcement of the EPA’s rule would:
• Protect 211,000 children from lead exposure in those settings.
• Cost about $1.4 billion.
• Provide positive net benefits of approximately $3 billion, including:
• $990 million for the federal government.
• $500 million for state and local governments.
• Return $3.10 for every dollar invested. (See Table 5.)

55
Table 5
Lead-Safe Renovation Could Yield $3.10 Per $1 Invested
Benefits of EPA rule enforcement
Baseline estimates
Average blood lead level for children if no intervention 1.25 μg /dL
Number of children in homes with covered events 211,000
Total number of renovation events 11.4 million
Number of renovations requiring safe work practices 4.4 million
Predicted impacts Prevented increase in blood lead per child 1.08 μg /dL
Gross future benefits Earnings $4.1 billion
Health savings $90 million
Education savings $90 million
Quality-adjusted life years benefits $160 million
Total gross future benefits $4.5 billion
Share to the federal government $990 million
Share to state and local governments $500 million
Share to households, the private sector, and other
nongovernmental entities
$3.0 billion
Costs
Testing cost per renovation event $10
Total testing cost $110 million
Lead-safe work practices per renovation event $302
Total lead-safe work practices $1.3 billion
Total costs $1.4 billion
Net
Net future benefits $3.0 billion
Cost-benefit ratio 3.10
Notes: Analysis is based on the 2018 birth cohort, estimated at approximately 4 million children. Total future benefits include small changes
in incarceration costs not itemized in the table. Values may not add up to totals because of rounding.
Source: Altarum Institute Value of Prevention Tool calculation
© 2017 The Pew Charitable Trusts

56
Potential challenges
The modeled policy is unique among those studied in its simplicity and low cost, which is a primary driver of its
high cost-benefit ratio. Training for renovators in the EPA’s required protocol is widely available. However, the lack
of enforcement undercuts the rule’s protectiveness because contractors can avoid compliance without penalty.
Based on stakeholder feedback, consumer knowledge of the rule remains low. State and local governments
have the opportunity to codify EPA’s requirements or adopt their own laws and to conduct aggressive public
outreach about lead-safe renovation practices, but only a few have done so. Although all 4.4 million renovation
events undertaken each year in the U.S. probably do not require direct EPA or state oversight and supervising
every jobsite would be impractical, the large number of renovations that go unchecked are a missed opportunity
for protecting children. The EPA has only authorized 14 states to enforce the rule, but it could encourage more
states to apply for delegated authority. Additionally, the EPA could increase high-profile enforcement to promote
contractors’ awareness of the rule and adherence to its requirements.
Jessica Grin/PhillyNews.com
Jana Curtis and her children walk past a construction site next to their Philadelphia neighborhood park in April 2017. Curtis's 3-year-old
daughter was poisoned by lead in the soil in their backyard and from construction dust in the neighborhood.

57
Air emissions and soil contamination
I grew up in the country digging in the dirt and gardening and stu,
and that’s not a reality for my kid.”
—Baltimore resident
Even as the nation struggles to address the legacy of lead in homes, yards, and drinking water, more lead is being
introduced into the environment every day. Most emissions result from mobile sources such as the use of leaded
fuels in smaller piston-engine aircraft, followed by mining and smelting, factories that use lead, and electric power
plants that burn coal and other contaminated fuels.
125
(See Figure 4.)
In 2008, the EPA decreased the acceptable level of lead concentration in air—the primary National Ambient Air
Quality Standard (NAAQS)—from 1.5 to 0.15 μg /m
3
to better protect children and other at-risk populations. The
Children’s Health Protection Advisory Committee recommended a more significant reduction to 0.02 μg /m
3
because of the unique eects on children, particularly children of color.
126
Under current regulation, state and
environmental agencies that track lead in the air must place monitors at non-airport facilities that reported lead
emissions of a half-ton or more per year and at airports with documented emissions of 1 ton or more per year.
127
456.3
Piston engine
aircraft
5.0
Other
transportation
156.8
Industrial
processes
Fuel
combustion
Other
Waste
disposal
92.6
4.7
14.0
Notes: Other transportation includes locomotives, commercial marine vessels, diesel heavy-duty vehicles. Industrial processes include
activities involving ferrous (iron-containing) and nonferrous metals, mining, oil and gas production, pulp and paper production, cement
manufacturing, and petroleum refining. Fuel combustion includes electricity generation, the use of industrial boilers/internal combustion
engines, and the burning of residential oil, commercial natural gas, and coal. Waste disposal includes livestock waste and field burning.
Other includes dust, agriculture, gas stations, and solvents, comprising industrial surface coatings and degreasing agents.
Source: EPA, “2014 National Emissions Inventory Data” (2014), https://www.epa.gov/air-emissions-inventories/2014-national-emissions-
inventory-nei-data
© 2017 The Pew Charitable Trusts
Figure 4
Piston Engine Aircraft and Industrial Processes Make Up the
Majority of Lead Emissions
Lead emissions by source in tons, 2014

58
Lead in the air eventually makes its way into the top layer of soil, which children may ingest directly or be
exposed to if it contaminates toys or is tracked into homes.
128
The most recent nationally representative survey
of residential yards documented a mean soil lead level of 169 ppm, which is less than the EPA’s standard of
400 ppm for areas where children play, but this average can obscure significant site-specific contamination.
For example, a property near the East Chicago public housing development had levels of 54,900 ppm.
129
Importantly, the risks of lead in soil are not equally distributed. Two observational studies from New Orleans
suggest that children exposed to higher levels of lead in soil are more likely to be black, have low socioeconomic
status, and live in inner cities without safe outdoor play areas that are free from harmful lead.
130
The relationship between soil lead and children’s blood lead has been the subject of several analyses with
findings showing increases in blood lead of 0.12 to 1.4 μg/dL per 100 ppm lead in soil.
131
One study found that at
lower levels of lead in soil (i.e., below 100 ppm) the relationship between lead in soil and in blood is steeper than
at higher levels (i.e., above 300 ppm).
132
Despite the need for a cost-eective approach to soil lead remediation, the peer-reviewed studies evaluating
soil interventions are limited.
133
One randomized control trial study published in 1993 evaluated the dierence in
children’s blood lead levels before remediation and again 11 months after and found that among the group whose
homes received treatment, average blood lead was 1.28 μg/dL lower than the comparison group. The blood
lead decline associated with soil remediation ranged from 0.8 to 1.6 μg/dL after adjusting for other factors.
134
Conversely, one study found no reduction in blood lead after soil remediation, despite an average reduction in soil
lead from 501 to 34 ppm.
135
More recently, a case study review article assessed changes in blood lead and identified 13 relevant studies.
136
Twelve of those demonstrated decreases in blood lead or in the proportion of children with high levels after
treatment. The authors found that most soil remediation eorts have focused on Superfund sites or individual
neighborhoods with lead smelters that have aected nearby residences. They noted that low-cost solutions
are needed in cases where no “responsible party” is available to pay for cleanup, such as large residential
communities contaminated by past industry or gasoline emissions. Some options proposed by the authors
include the use of biosolid and compost-based soil products to build raised bed gardens; the use of biochar—
charcoal produced from plant or animal waste matter—which immobilizes lead in soil; and watering of lawns
to prevent soil resuspension in warm, dry months.
137
Lead smelting and battery recycling facilities
The production of lead, from mining and primary smelting—a process that uses high temperatures and chemical
oxidation to produce lead from ore—as well as from recycling of lead-containing products, such as car batteries
and electronic devices, referred to as secondary smelting, can cause widespread contamination of air and soil in
surrounding communities. According to the EPA, more than 80,000 people experienced elevated health threats
from 15 secondary lead smelters located in 10 states and Puerto Rico.
138
These communities typically have a
higher proportion of people of color (41 percent nonwhite) and more Latino and Hispanic residents (52 percent)
than the population as a whole (25 percent and 14 percent, respectively).
139
More recently, Exide plants in Vernon,
California (described later in this report); Frisco, Texas; and Baton Rouge, Louisiana, permanently closed, and one
was constructed in Florence, South Carolina, bringing the total number of active facilities at the time of this report
to 13.
140

59
Secondary smelting has increased as the value of lead has risen on international markets,
141
and no complete
account of current and historical secondary lead smelting sites in the U.S. exists. A 2001 study found that the
EPA’s centralized index of regulated facilities listed only 32 percent of existing sites.
142
Research indicates that
many are located in or near residential areas, suggesting that they have produced or are causing widespread
contamination of nearby neighborhood soil.
143
For example, between 2001 and 2009, 22 lead-emitting facilities
operated in Detroit.
144
These data highlight the need to monitor secondary smelter sites and identify and measure
lead concentrations in residential soils close to legacy sites.
A sign warns residents of the West Calumet Housing Complex in East Chicago, Indiana, to avoid playing in the dirt where high levels of lead
and arsenic were discovered in 2016.
Joshua Lott/Getty Images
Superfund sites
In 1992, the Agency for Toxic Substances and Disease Registry (ATSDR) ranked lead as the number one priority
hazardous substance at sites included on the EPA’s national priorities list (NPL), an inventory of the most
contaminated places in the country, known as Superfund sites. The Comprehensive Environmental Response,
Compensation and Liability Act (CERCLA), which is the Superfund law, typically requires identification of
a “principal responsible party” (e.g., smelter, mine, manufacturing plant, or other facility) that caused the
contamination and outlines steps to reduce hazards such as excavating and replacing contaminated soil, cleaning
up interior dust, and, in limited circumstances, stabilizing exterior paint to preserve soil treatment.
The EPA has documented lead contamination at 66 percent of the 1,300 Superfund sites across the country.
CERCLA does not apply to the many other facilities and communities with lead contaminated soil that do not
appear on the NPL, including more than 450 EPA-identified sites where lead was produced or used.
145
Lead dust
from industrial facilities can contaminate surrounding soil, creating a hidden source of exposure for communities.

60
In 2016, the EPA found that 800,000 children under 18 reside within roughly one mile of active Superfund sites.
146
A small but consistent set of local studies demonstrates an association between elevated blood lead in children
and residing near a Superfund site. One study of shuttered industrial facilities and the long-term risks they pose
determined that children living near one such abandoned factory in Philadelphia were more than four times as
likely as the general population to have elevated blood lead levels, but the investigators were not able to verify
that the facility was the source of the lead from the tested homes.
147
Similarly, children living near the Bunker Hill Superfund Site in northern Idaho were exposed to high levels of lead
in the mid-1970s; in 1974 more than 95 percent of children within 3 miles of the smelter had blood lead levels
over 40 μg/dL.
148
The Bunker Hill cleanup strategy included remediating nearby homes and soil. In 2001, only
3 percent of children in neighboring residential areas had blood lead levels over 10 μg/dL.
149
A 1999 observational study of four Superfund sites examined whether soil lead could be a predictor of blood lead
in children. Researchers evaluated blood lead measurements and environmental samples from soil, house dust,
interior paint, and tap water collected for the 1,015 children in the ATSDR’s multisite lead and cadmium study.
After adjusting for income, education of the parents, presence of a smoker in the household, gender, and dust
lead, the authors found a statistically significant association between lead in soil and in blood independent of
home dust lead levels; however, the model also had high levels of uncertainty and variability.
150
Policy in Action: Superfund Cleanup
In 1998, the Omaha, Nebraska, City Council requested assistance from the EPA after blood
tests conducted by the Douglas County Health Department revealed that nearly 10 percent
of tested children in the county had blood lead levels higher than 10 μg/dL.
*
The EPA began
investigating contamination from historic smelting and refining operations under its Superfund
authority, and in 2003, approximately 14 square miles of property in East Omaha was deemed
at high risk and added to the national priorities list.
†
Cleanup included soil testing at child care facilities, schools, playgrounds, parks, and homes;
removal and replacement of contaminated soil; and planting of new sod and grass seed. The
EPA funded an interior dust program to provide residents who had their soil remediated with
education and a free vacuum.
‡
To date, the EPA has tested nearly 40,000 properties, cleaned up
more than 12,000 that were polluted, and awarded $40 million to the city of Omaha through a
cooperative agreement to address the final phases of the work, including continued attempts to
collect soil samples and clean up remaining contaminated properties.
§
A lead-acid battery recycling plant in Vernon, California, which opened in 1922, contributed to
air pollution in the nearby Los Angeles neighborhood of Boyle Heights, for more than 90 years.
The plant logged at least 88 violations of emissions standards between 1996 and 2015.
||
The
facility, which was purchased by Exide Technologies in 2000, ran seven days a week, processing
25,000 batteries a day and emitting lead, arsenic, and other pollutants into the air.
#
Continued on next page

61
In 2013, after the South Coast Air Quality Management District found the plant “posed a higher
cancer risk to more people than any of 450 operations the agency has regulated in the last
25 years,” the state temporarily shut it down.
**
Exide was able to get the closure overturned
quickly, driving advocates to take further action. In 2014, the EPA found that Exide had violated
the Clean Air Act emissions standards more than 30 times and was subject to fines of up to
$37,500 a day for each violation. The ruling resulted in the plant’s second temporary closure.
††
At the same time, Exide was under criminal investigation and entered into an agreement with
the U.S. attorney’s oce to avoid prosecution in exchange for permanently closing the plant
and paying $50 million to tear it down and clean the site, including $9 million for removing
lead from nearby homes
.‡‡
In April 2016, California appropriated an additional $177 million to
clean up about a 2-mile radius surrounding the plant and intends to seek reimbursement from
the company.
§§
* Agency for Toxic Substances and Disease Registry , “ATSDR Releases Public Health Assessment Concerning Lead
for the Omaha Lead Site, Omaha, Neb.,” accessed Jan. 13, 2017, https://www.atsdr.cdc.gov/news/displaynews.
asp?PRid=1979.
† United States Environmental Protection Agency, “Site Information for Omaha Lead,” accessed Jan.13, 2017, https://
archive.epa.gov/region07/cleanup/npl-archive/web/pdf/record_of_decision.pdf.
‡ Environmental Protection Agency, “Site Information for Omaha Lead.”
§ The Chicago Tribune, “Violent Crime Part of Lead’s Toxic Legacy,” Omaha World-Herald, June 14, 2016, http://www.
omaha.com/eedition/sunrise/articles/violent-crime-part-of-lead-s-toxic-legacy/article_b4865302-fa82-5e76-
84a6-c1fe9b80e154.html; Brandon McDermott, “Where Does Omaha Stand After 15 Years of EPA Cleanup?,”
KNVO News, May 16, 2014, http://www.kvnonews.com/2014/05/omaha-stand-15-years-epa-cleanup; Steve
Kemp, “Going Home to Manage the Final Steps of Omaha’s Historic Lead Cleanup,” The EPA Blog, May 25, 2016,
http://blog.epa.gov/blog/2016/05/going-home-to-manage-the-final-steps-of-omahas-historic-lead-cleanup.
|| Molly Peterson, “State Toxic Regulators Give Exide 30 Days to Correct Permit Problems,” Southern California Public
Radio, June 17, 2014, http://www.scpr.org/news/2014/06/17/44788/state-toxics-regulators-give-exide-30-days-
to-corr/; Tony Barboza, “Exide’s Troubled History: Years of Pollution Violations but Few Penalties,” Los Angeles
Times, March 14, 2015, http://graphics.latimes.com/exide-battery-plant.
# Tony Barboza, “How a Battery Recycler Contaminated L.A.-Area Homes for Decades,” Los Angeles Times, Dec. 21,
2015, http://www.latimes.com/local/lanow/la-me-exide-cleanup-story-so-far-20151121-story.html.
** Jessica Garrison and Kim Christensen, “Vernon Plant Closed Over Toxics,” Los Angeles Times, April 25, 2013, http://
articles.latimes.com/2013/apr/25/local/la-me-exide-arsenic-20130425.
†† Ibid.; Tony Barboza, “How a Battery Recycler Contaminated L.A.-Area Homes for Decades.”
‡‡ Haley Branson-Potts, “Vernon Battery Recycler Cited by EPA for Excessive Lead Emissions,” Los Angeles Times,
May 23, 2014, http://www.latimes.com/local/la-me-0524-epa-exide-20140524-story.html; Environmental
Protection Agency, “Annual Air Quality Monitoring Network Plan,” July 2015, https://www3.epa.gov/ttn/amtic/
files/networkplans/CASCAQMDPlan2015.pdf.
§§ “$177 Million for Exide Cleanup Signed Into Law,” Southern California Public Radio, April 20, 2016, http://www.scpr.
org/news/2016/04/20/59806/177-million-for-exide-cleanup-signed-into-law.

62
Policy in Action: Imposing a Fee on Emitters to Fund Public Lead
Remediation Programs
In the mid-1980s, the California Legislature declared childhood lead poisoning to be the
state’s most significant environmental health problem and subsequently established a
prevention program within the Department of Public Health.
*
To help pay for the program, in
1993, California adopted an annual fee on manufacturers and other entities involved with the
production or sale of lead and lead-based products collected from businesses in the petroleum
and architectural coatings industries and from facilities reporting releases of lead into the air.
The department employs a “historical market share attributions” concept to estimate each
payer’s long-term contribution to environmental lead contamination and allocate fees. It then
deploys collected funds to support health care referrals, assessments of homes for hazards,
and educational activities. The fee generated $20.6 million in fiscal 2015.
†
* Californians for a Healthy and Green Economy, “California: The Leader in Lead Regulation,” accessed Jan. 12, 2017,
http://www.changecalifornia.org/2010/08/lead.html.
† California State Board of Equalization, “Supporting Our Communities: Funding a Better Quality of Life,” accessed
Jan. 12, 2017, http://www.boe.ca.gov/pdf/pub306.pdf.
Stakeholder input
Several focus group participants identified lead in soil as a concern, and a few parents said it was the source
of exposure for their children’s elevated blood lead. Los Angeles focus group participants expressed concerns
about children in a community near a smelter coming into contact with lead through soil at bus stops or while
playing in sprinklers. Community members in Baltimore said they kept their children from playing outside in the
dirt, digging, planting, climbing trees, or picking up worms. Other focus group participants reported gardening
in raised beds to avoid exposing their children to produce contaminated by lead, and in Chicago, one person
described a program where farmers brought fruits and vegetables to a school to give residents access to local
produce grown in safe soil.
Many participants wanted more transparency and better communications about lead hazards in their
neighborhoods. Residents in Philadelphia related how when the EPA came to their community to test soil and
children’s blood lead levels many people distrusted the researchers and didn’t answer their doors or participate
in the tests, suggesting a need for improved communication in the future. Others worried that residents who
participated in inspections would be unintentionally penalized and experience financial strain or diculty selling
their homes because of disclosure requirements. Participants also were concerned about lingering contamination
in their neighborhoods even after industrial sites had been cleaned up, and some called for safer handling of
Increasing the number of sites placed on the NPL and financing cleanup when no responsible industry party can
be identified are critical needs for scaling cleanup eorts. CERCLA initially gave the EPA authority to tax crude oil,
imported petroleum products, and hazardous chemicals and to use those funds for Superfund-related activities.
However, that provision of the law expired in 1996, severely reducing the resources available for cleaning up
contaminated sites.

63
industrial lead waste and disclosure of information about its location. A few individuals also worried about
exposure resulting from parents’ unintentionally carrying home lead from their workplaces on their clothing or
shoes. Participants discussed job loss as a potential disadvantage to increasing regulations on industry.
Proposed solution
Several policy interventions are available that could address industry-related lead soil contamination, such
as reducing emissions from secondary lead smelters, increasing public funding, and prioritization of cleanup,
particularly at sites where no responsible industry party exists to finance the work. To protect against lead risks
for food grown at home, the EPA has recommended practices for gardeners working in soil containing more
than 100 ppm lead (soil lead levels can be tested by private or university labs
151
), including building raised beds,
planting in containers, wearing gloves, using tools, restricting gardening by and for children, and selecting plants
with shallow roots.
152
Quantitatively modeling these strategies on a national basis was both beyond the scope of
this study and deemed by the team to present a significant chance of inaccuracy because soil exposure is highly
dependent on community context.
Literature summary
Evidentiary support: Some evidence. Strategies with this rating are likely to work, but further research is needed
to confirm eects. These strategies have been tested more than once and results trend favorable overall.
153
Population aected: Community.
154
Leaded aviation gas
Leaded fuel used by piston engine aircraft is the nation’s largest source of lead emissions into the air, with
approximately 167,000 aircraft emitting about 450 tons a year.
155
These planes constitute 71 percent of the
U.S. air fleet, and many of them require high-octane gasoline to avoid dangerous engine knocking. Lead is one
of the best known ingredients for raising octane, and eliminating its use would require modifications to a
Je Schultz/Getty Images
Lead levels in the ground and in the air can be higher near airports that serve piston engine aircraft, such as this one.

64
significant share of existing planes.
156
However, research suggests that most planes could safely make the
transition to unleaded fuel at little cost if airports provided appropriate alternatives to leaded gas, and most
new aircraft are certified to run on ethanol-free automobile gasoline.
157
In 2010, the EPA estimated that about half of lead emissions from aircraft remains in the vicinity of the airport,
and that approximately 16 million people live near the roughly 20,000 U.S. airports that serve aircraft running
on leaded fuel and 3 million children attend school near these airports.
158
Most of these are small, general
aviation facilities serving civilian, noncommercial flights, such as private or corporate planes, flying schools, and
sightseeing tours.
159
In one study, children who lived within 0.6 miles of an airport were found to have blood lead
levels that are 5.7 percent higher than those of children residing more than 2.5 miles from airports.
160
Stakeholder input
Community members in Los Angeles mentioned lead in aviation gas as a concern, and experts identified it as
an important contributor to air emissions. Additionally, the experts suggested that removing lead from the fuel
would decrease pilots’ and aircraft fuelers’ contact with lead, potentially reducing take-home exposure.
Proposed solution
The team modeled the eect on blood lead in children residing within about 0.6 mile of airports serving piston
engine aircraft of prohibiting the use of lead in aircraft fuel.
Literature summary
Evidentiary support: Some evidence. These strategies have been tested more than once and results trend
favorable overall.
161
Population aected: Community.
162
Assumptions
• The team used data from a cross-sectional study to determine that children living closer than 0.6 miles
from airports using leaded gas have blood lead levels that are 5.7 percent higher than those of children living
farther away.
163
• EPA data show that about 5.7 percent of the U.S. population resides within 0.6 miles of an airport that serves
piston engine aircraft, so the study team applied this percentage to the 2018 birth cohort to predict that
226,000 children would live within that radius of such airports.
164
• Baseline blood lead levels for children living in close proximity to airports serving piston engine aircraft were
based on NHANES 2011-14 data and mirror the national average.
Findings
Removing lead from aviation gas would:
• Prevent an increase in blood lead levels of 5.7 percent.
• Protect 226,000 children born in 2018.
• Provide positive benefits of approximately $262 million, including:
• $60 million for the federal government.
• $30 million for state and local governments. (See Table 6.)
In the absence of cost data, the team did not compute a cost-benefit ratio for this intervention.

65
Baseline estimates
Number and percentage of children expected to live within
0.6 miles of airports serving piston engine aircraft
226,000 (5.7%)
Average blood lead levels for children
if no intervention
1.11 μg /dL
Predicted impacts
Prevented increases in blood lead levels per child 5.7%
Children aected 226,000
Gross future benefits
Earnings $240 million
Health savings $6 million
Education savings $6 million
Quality-adjusted life years benefits $10 million
Total gross future benefits $262 million
Share to the federal government $60 million
Share to state and local governments $30 million
Share to households, the private sector, and other
nongovernmental entities
$170 million
Notes: Analysis is based on the 2018 birth cohort, estimated at approximately 4 million children total. Total future benefits include small
changes in incarceration costs not itemized in the table. Values may not add up to totals because of rounding.
Source: Altarum Institute Value of Prevention Tool calculation
© 2017 The Pew Charitable Trusts
Table 6
Removing Lead From Aviation Fuel Could Prevent a 5.7% Increase in
Children’s Blood Lead
Benefits, assuming about 230,000 children
Potential challenges
In 2012, the FAA estimated that phasing out leaded fuel would take 11 years.
165
According to a recent federal task
force report, the FAA is working to identify unleaded alternative fuels for most piston engine aircraft by 2018, and
under section 231 of the Clean Air Act, the EPA is evaluating whether lead emissions from aviation fuel “cause
or contribute to air pollution that may reasonably be anticipated to endanger public health or welfare.”
166
Based
on the results of its investigation, the EPA could help to expedite the elimination of lead in aviation fuel by using
its authority under the act to issue an “endangerment finding,” indicating that leaded aircraft fuel emissions are
polluting and harmful to public health. Such a ruling would trigger the FAA to issue standards.
Given the protracted timelines for federal action, however, states may wish to take steps to address the problem
by, for example, requiring all general aviation airports to provide unleaded gas or establishing fees or taxes on
airports serving piston engine aircraft to support the cleanup of the soil in parks and near homes, schools, and
child care facilities.
66
Policy in Action: Safe Soil for Schools and Child Care
In New Orleans, the use of leaded gasoline contributed significantly to elevated soil lead levels,
particularly in transit-heavy areas downtown. Research estimates that vehicles deposited more
than 10,000 metric tons of lead dust in New Orleans soil between 1950 and 1985.
*
In 2004, more than 40 percent of New Orleans soils exceeded the EPA’s cleanup standard.
†
But
a year later, storm surges and flooding from Hurricane Katrina deposited cleaner, less hazardous
surface soil over the high-lead topsoil, which, combined with citywide cleanup and remediation
eorts, reduced lead dust in homes and surrounding soil.
‡
Lead assessments conducted in
Katrina’s immediate aftermath found a 46 percent reduction in median soil lead levels.
§
And the
declines continued. Before the storm, 15 of the city’s 46 census tract neighborhoods exceeded
the EPA’s regulatory soil lead standards; by 2010, only six neighborhoods exceeded standards.
||
Inspired by the city’s unique natural experiment, researchers used a similar approach to clean
up soil at 10 child care centers in New Orleans, covering lead-contaminated surface soils with a
water-permeable barrier and 6-inch layer of low-lead soil.
#
Since 2005, nine of 10 federal public
housing projects in the city also were rebuilt using this process.
**
New Orleans expanded this
practice to all public parks and playgrounds that tested high for lead.
††
These eorts, combined
with the potential reduction of lead in soil from fresh topsoil deposited by the storm surge
during Hurricane Katrina, led to a decrease in the percentage of children from high-lead, largely
inner-city areas with blood lead of at least 5 μg/dL from 64 percent in 2005 to 19 percent
in 2015.
‡‡
* Howard W.Mielke et al., “Environmental and Health Disparities in Residential Communities of New Orleans: The
Need for Soil Lead Intervention to Advance Primary Prevention,” Environment International 51 (2013): 73-81, https://
doi.org/10.1016/j.envint.2012.10.013.
† Janet Pelley, “Lead a Hazard in Post-Katrina Sludge,” Environmental Science & Technology 40, no. 2 (2006): 414–15,
https://www.ncbi.nlm.nih.gov/pubmed/16468382.
‡ Howard W. Mielke et al., “Spatiotemporal Dynamic Transformations of Soil Lead and Children’s Blood Lead Ten
Years After Hurricane Katrina: New Grounds for Primary Prevention,” Environment International 94 (2016): 567–75,
https://doi.org/10.1016/j.envint.2016.06.017.
§ Sammy Zahran et al., “New Orleans Before and After Hurricanes Katrina/Rita: A Quasi-Experiment of the
Association Between Soil Lead and Children’s Blood Lead,” Environmental Science & Technology 44, no. 12 (2010):
4433–40, https://doi.org/10.1021/es100572s.
|| Ibid.
# Howard Mielke et al., “Soil Intervention as a Strategy for Lead Exposure Prevention: the New Orleans Lead-
Safe Childcare Playground Project,” Environmental Pollution 159 (2011): 2071–77, https://doi.org/10.1016/j.
envpol.2010.11.008.
** Mielke et al., “Spatiotemporal Dynamic Transformations of Soil Lead and Children’s Blood Lead Ten Years After
Hurricane Katrina.”
†† Ibid.
‡‡ Ibid.

67
Addressing data gaps
We need some data. We need to get children tested. Once we have
that data, we will have a game plan. If 80 percent of our kids have
lead, then we have an epidemic. We can raise our voices and perhaps
get something done.”
—New Orleans resident
Data play an important role in the nation’s ability to prevent and respond to childhood lead exposure by
helping to identify high-risk locations, assessing testing rates among high-risk groups, evaluating the impact
of remediation eorts, and detecting housing units responsible for multiple exposures over time. However,
inadequate investment in state and local technology and limited capacity for timely data collection, processing,
and sharing impede the ability of agencies at all levels of government to provide the public with transparent
data on the highest-risk areas and to protect privacy.
But even if these data were collected, no federal agency curates or integrates national blood lead and
environmental information into a single database. For example, the National Health and Nutrition Examination
Survey provides the best available blood lead data, and the American Healthy Housing Survey is the best
estimate of lead paint hazards, but because these are two separate databases, research on the issue is needlessly
complicated. Further, data are rarely available at a census tract level or finer, and county-level data obscure
neighborhood risks because exposure can vary block by block depending, for example, on the location of
industrial sources or the age of buildings and water infrastructure.
In addition to the need for better community-level information about lead, the research team identified several
significant research gaps during the course of this study. The questions include epidemiologic research to
establish the dose-response relationships between levels of lead in the environment and lower blood lead levels;
research on the eectiveness of prevention and response interventions; data on the geographic location of certain
lead risks and any populations that are at high risk of exposure; and information about valid testing methods.
Community members and landlords wanted more sharing of information about issues aecting their
neighborhoods. Spanish-speaking residents in Flint, for example, explained that the Latino community didn’t
learn about the water crisis until Univision reported on the issue four months after the story first broke. This
oversight speaks to the importance of cultural competency, that is the “ability to address [people’s] diverse
values, beliefs and behaviors,” in response programs to ensure that they promote equity by meeting the needs
of the populations at risk.
167
Some parents noted that messages about lead dangers tend to focus on specific populations, for example,
Medicaid-eligible children, at the risk of overlooking others, such as children from middle-income families
exposed to lead through home renovations.
Many community members expressed distrust in industries, inspectors, and the agencies that they feel should
be tracking information and protecting citizens. In Los Angeles, participants suspected that industry-hired
researchers manipulated data about blood lead levels in children from dierent neighborhoods to make the case
that a nearby battery facility hadn’t exposed children to harmful levels of lead.

68
Focus group participants suggested making neighborhood-level data publicly available to help community
members, policymakers, and the medical community detect possible sources of exposure and address high
lead levels in children. They felt that sharing these data by census tract or ZIP code could help pediatricians and
obstetricians identify patients at a high risk of lead exposure in their homes or yards. Participants also supported
community-based science and research, in which community members could be trained to collect samples from
their homes and neighborhoods and help with sharing data.
Some state laws may make it dicult to share data publicly or between responding agencies such as schools
and public health departments. Further, although cooperative agreements require states and cities to submit
blood lead surveillance data to the CDC, many states do not receive CDC funding and so are under no obligation
to submit data. Similarly, states and localities do not categorize lead as a reportable disease, which means that
laboratories across the country do not consistently convey all results of blood lead tests to health departments,
and even when those data are shared, considerable time typically elapses before the public is made aware of
neighborhood or other trends.
Future research could address the most pressing knowledge gaps, such as:
Water: Several municipalities, including Cincinnati, the District of Columbia, and Boston, have inventoried
their LSLs and made the information publicly available, and California and Ohio have passed laws requiring the
creation of such records.
168
However, no recent and rigorous national surveys have estimated the number of
LSLs in operation nationwide. Similarly, information on the extent of lead-leaching internal plumbing in homes
across the country is scarce. Finally, protocols for sampling water from homes and schools should be updated
and validated.
Housing: The evaluation of HUD’s lead hazard control program is the largest study of strategies to address lead
paint hazards in housing. Limitations of the study include that the units were not randomly selected, the omission
of a control or comparison group for ethical reasons, and that it was conducted when blood lead levels and the
amount of lead in the environment were higher. As a result, new assessments of this program are needed, as are
other studies to rigorously investigate the extent of lead paint hazards and resultant child exposures.
Epidemiology of blood and environmental lead levels: Declining blood lead levels and the technology to detect
lower amounts of lead in the environment create new research opportunities. New studies should include
epidemiologic research on the relationship between lead exposure and various sources such as food, water, soil,
air, dust, and paint, as well as better national and community-level data on risks by geography and population.
Future studies could examine the eect of blood lead levels below 2 μg/dL on IQ. Additionally, a longitudinal
study tracking IQ and lead exposure through childhood and adulthood could strengthen the evidence of the link
between lead exposure and lifetime earnings.
Educational interventions: No studies have measured the eectiveness of educational, social, or
behavioral interventions for children with a history of lead poisoning. Research is needed to identify practices
and pedagogies that can help children with elevated blood lead levels avoid or overcome cognitive and
behavioral challenges.

69
Supporting children with a history of lead exposure
Children aected by lead who can’t focus in class get separated from
the other students and labeled a trouble child.”
—Los Angeles resident
Prevention is the most critical and first approach to addressing childhood lead exposure, but those eorts
have come too late for many children. Children exposed to lead may demonstrate delays in development of
language skills, problems focusing, poor impulse control, and disruptive behavior. They are more likely to be
diagnosed with a learning disability, to struggle to pass achievement tests, and to have lower IQs and worse
academic achievement than other children.
169
Recent research has found that among young adults exposed to
lead as children, the areas of the brain important for language can reorganize to facilitate language; however
this reorganization does not necessarily compensate for the eects of lead on language function.
170
Research
suggests that exposure to lead has particularly detrimental eects on children's executive functioning, such as
working memory, mental flexibility, and self-control. These skills help children retain and manipulate information
over short periods; sustain or shift attention in response to dierent demands; set priorities; and resist impulsive
actions, responses, or judgments.
171
If children do not receive appropriate early interventions, lead-related deficits
can ripple through their lives. For example, attention deficit hyperactivity disorder, which is common among lead-
poisoned children, is a strong predictor of social isolation, which in turn can decrease school success and increase
risky behaviors.
172
All of these problems become risk factors for delinquency, criminal behavior, substance use,
and pregnancy in adolescence and young adulthood.
173
Fortunately, cognitive and behavioral developmental skills are malleable and can be built through high-quality
interventions, staed by engaged and skilled personnel who are supported by practice-based professional
development and provided in a safe setting with small child-to-adult ratios.
174
Research consistently finds that
strategic investments in children’s development can yield benefits for children and families.
175
However, the ability
to intervene early and eectively with at-risk children before problems compound begins with testing to ascertain
the extent of the exposure and then, through neuropsychological and developmental assessments, to determine
if developmental delay or cognitive or functional deficits have resulted.
Blood lead testing
A necessary precursor to getting children the interventions and care they need is determining the level of lead
in their bodies. Some state health departments encourage health care providers to use risk factor screening
questionnaires to identify children at a high risk of lead exposure based on housing and other conditions, but
one study found that many of these questionnaires do a poor job of predicting risk.
176
Providers often incorrectly
assume that if patients do not live in a poor neighborhood or a community of color then they are not at risk, and
clinicians are not always up to date on the latest CDC guidelines regarding harmful levels of lead in blood. For
example, some providers and laboratories still tell parents that blood lead test results are normal if levels are
below 10 μg/dL. Further, low blood lead levels can have lasting eects without any visible symptoms. For all of
these reasons, a blood test is the preferred way to determine if a child has been exposed to lead.

70
The CMS requires states to comply with the Early Periodic Screening Diagnostic and Testing (EPSDT) program,
a comprehensive preventive child health initiative that emphasizes early assessment of children’s health care
needs and requires that all children receiving Medicaid be tested for various health indicators, including receiving
a blood lead test, at 12 and 24 months of age, unless the state has been granted a waiver by the CMS. However,
despite these and other long-standing requirements, about 40 percent of Medicaid-enrolled children do not
receive tests.
177
State guidelines for children not covered by Medicaid range from universal testing to screening only high-risk
children.
178
Ten states plus the District of Columbia require testing of all children, eight mandate targeted testing,
and the rest either provide only recommendations or have no policy. Most of the states with universal testing
require it at ages 1 and 2 or at 3 years of age if no previous test was conducted, but even in these states, not all
children actually receive tests.
179
The CDC’s 2009 report on testing of Medicaid-eligible children recommends oering blood lead testing at sites
operated by the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) to increase the
percentage of children tested.
180
The report notes that collaboration with WIC has been eective for blood lead
testing of Native American children. Additionally, the CDC created lead poisoning prevention recommendations
for newly arrived refugee children, including testing within 90 days of entry to the U.S. for children ages 6 months
to 16 years, and six months after resettlement for children 6 years of age and younger.
181
Under EPSDT, Medicaid agencies are also required to cover diagnostic services and treatment to correct and
ameliorate defects, physical and mental illnesses, and other conditions for individuals up to age 21. To qualify for
coverage, school-based health programs must be primarily medical rather than educational in nature, medically
necessary for the child, and delivered by a qualified Medicaid provider to income-eligible families. Services can
include diagnosis and treatment of acute uncomplicated problems, monitoring and treatment of chronic medical
conditions, and provision of medical services to children with disabilities that are required by the Individuals with
Disabilities Education Act (IDEA). States and schools have flexibility in how they implement these services.
(See Special Education below.)
Academic and behavioral interventions
Many lead-poisoned children’s developmental and learning deficits are similar to those in children aected by
trauma and poverty. Within that broader population of at-risk children, certain high-quality, evidence-based
programs have demonstrated positive eects, for example on executive functioning.
182
In fact, research studies
consistently find that investments in high-quality child development interventions reap positive benefits for
children, families, and society.
183
Although no formal evaluations have measured the eectiveness of academic
and behavioral interventions for children with a history of lead exposure, robust evidence nevertheless shows that
various childhood interventions reduce deficits in the very same skills and behaviors most commonly aected by
lead exposure through injuries it causes to the brain. Further, although no high-quality programs were designed or
implemented specifically for children exposed to lead, they generally focus on children at similar developmental
risks from trauma, poverty, stress, and other adverse childhood experiences and therefore may provide benefits
for children aected by lead.

71
One such intervention is the federal Head Start and Early Head Start program for which the Administration
for Children and Families provides grants to states and communities to deliver high-quality early learning
opportunities to low-income infants, toddlers, and young children. Recipients then use the funding to provide
services for children from low-income families. Given the federal support and focus on high-risk populations,
Head Start could be a valuable entry point for reaching children who have been exposed to lead and could have
positive impacts on their academic and behavioral outcomes and executive functioning.
Early Head Start provides a range of comprehensive services for parents, including family support and coaching
oered in and outside the home. Such parent-focused interventions can build on the positive impacts of
early childhood education programs if they include regular, voluntary in-home family support and coaching—
commonly known as home visiting—to provide parents with opportunities to practice responsive interactions and
other activities that oer their children age-appropriate encouragement. A recent analysis of parent education
programs found that combining monthly in-home family support and coaching visits with parent education
resulted in the highest improvements in children’s cognitive and pre-academic skills, such as vocabulary
development, task persistence, reading, and counting.
184
If regularly provided, intensive, and focused on improving
the quality of interactions with young children, these programs might also represent a promising intervention for
lead-exposed children.
Still further, high-quality targeted academic and behavioral school-based, community-based, and caregiver and
parent training programs can provide children in elementary and middle school with opportunities and tools to
manage anger, aggression, and negative thoughts, which in turn can improve social and academic performance.
Some programs rely on cognitive therapy approaches, a type of talk therapy that builds awareness of negative
thinking and helps manage stress.
185
Behavioral interventions can engage parents to promote healthy emotional
management, improve attention, and reduce impulsiveness through meditation and computer trainings.
Rigorous research has demonstrated the positive eects of many high-quality early and middle childhood
interventions for children with some of the same deficits faced by lead-exposed children. For example:
• Nurse-Family Partnership (NFP) connects young, low-income, first-time expectant mothers with a public
health nurse, who meets with the woman in her home, starting during pregnancy and continuing until the baby
turns 2. The model has been shown to have a 54 percent return to the federal government on its investment,
lower enrollment in Medicaid, a 9 percent reduction in Medicaid costs, a decrease in emergency room visits
for poisonings, and fewer behavior and intellectual problems among children. A 2012 study found long-term
benefits of the program of almost $23,000 per participant.
186
At age 12, children who had received nurse visits
in early childhood out-performed their counterparts on standardized reading and math tests and were 70
percent less likely than children who did not participate to have used harmful substances, including cigarettes
and alcohol.
187
By age 15, participating children were half as likely to have behavioral problems and had half as
many arrests as those without visits.
188
• The Incredible Years training program consists of a range of activities that promote positive parenting
and teaching practices, interpersonal skills, academic competence, and general social skills and has been
shown, overall, to decrease harsh discipline practices, improve proactive parenting skills and the parent-child
relationship, enhance children’s academic and social competence, and decrease aggression.
189
In a randomized
controlled trial, researchers found reductions in antisocial behavior of up to 59 percent among children who
received training or whose parents or teachers were trained.
190

72
• Promoting Alternative Thinking Strategies (PATHS) fosters emotional and social competencies through the
development and strengthening of skills in emotional literacy, positive peer relations, and problem solving and
was found in an evaluation involving children in grades one to three to improve cognitive concentration and
reduce aggressive and antisocial behavior.
191
PATHS has also been found to improve academic skills. In a 2015
randomized evaluation of children from 24 elementary schools, those who participated in PATHS were 1.7 and
1.6 times more likely to attain proficiency in reading and math, respectively.
192
• Steps to Respect is a school-based bullying-prevention program that focuses on prosocial beliefs and social-
emotional learning. Students participate in a 12- to 14-week-long curriculum that uses literature-based
lessons, and parents receive information and updates about the program. Participating students demonstrated
fewer antisocial characteristics, such as aggression and bossiness, and by the end of the intervention, schools
saw a nearly 25 percent reduction in bullying behavior.
193
Only rigorously tested, culturally competent high-quality interventions have the potential to deliver benefits for
any children, including those exposed to lead. Policymakers and other stakeholders will need to investigate the
options with the needs of their communities in mind. The programs described above are illustrative of the many
high-quality interventions available. The resources below provide detailed descriptions of and information on
supporting research and evidence for these and many other interventions and can provide a starting point for
policymakers’ exploratory eorts:
• Blueprints for Healthy Youth Development, available at http://www.blueprintsprograms.com.
• Child Trends—What Works, available at https://www.childtrends.org/what-works.
• Home Visiting Evidence of Eectiveness, available at https://homvee.acf.hhs.gov.
• The Institute of Education Sciences’ What Works Clearinghouse, available at https://ies.ed.gov/ncee/WWC.
• The National Institute of Justice’s Crime Solutions, available at https://www.crimesolutions.gov/default.aspx.
• Pew-MacArthur Results First Clearinghouse Database, available at http://www.pewtrusts.org/en/multimedia/
data-visualizations/2015/results-first-clearinghouse-database.
Special education
The deficits associated with lead often do not become apparent until a child is older, such as in first grade when
children begin to acquire basic academic skills, and in sixth or seventh grade when executive functions such as
planning and organization skills are needed. For this reason, it is best not to wait until the eects of lead exposure
become a problem for the child, but rather begin intervention as early as possible once a child is identified as
having an elevated blood lead level.
The IDEA ensures that all children with disabilities receive a free appropriate public education. Part C of the
law serves infants and toddlers through age 2 with developmental delays or physical or mental conditions likely
to result in delays. Part B provides grants to states to partially fund special education and related services for
children and youth ages 3-21. Only eight states specify lead exposure as a condition that qualifies for IDEA,
12 others mention blood lead levels ranging from more than 10 to over 45 μg/dL as a criterion for eligibility, and
13 reference “toxic” exposures generally.
194
IDEA requires states to identify children with disabilities, determine
their eligibility, and make referrals to services via the comprehensive Child Find system.
195

73
Policy in Action: Serving Children With a History of Lead Exposure
Connecticut has a unique approach to providing educational interventions for lead-exposed
children. Under the Child Find program, the State Department of Education collaborates with
local school districts and the Connecticut Parent Advocacy Center to identify children with
a history of lead exposure or blood lead levels of 5 μg/dL or above, then notify the parent,
refer the family to medical providers and housing assistance, and obtain a health history from
the school nurse.
*
Based on a subsequent assessment, children then receive one of three
interventions:
• If the child has no noted or suspected developmental delays or other risk factors, the school team
develops a monitoring plan with annual review and refers the family to Head Start or a school
readiness or other enrichment program.
†
• If the child has a suspected or actual developmental delay or disability, the team determines
IDEA eligibility, conducts an evaluation, develops an individualized education program
identifying necessary services and supports, and places the child in district pre-kindergarten
or another enrichment program. For children with disabilities who do not qualify for IDEA,
the team completes evaluations as appropriate and investigates eligibility under Section 504
of the federal Rehabilitation Act of 1973, which requires schools to meet the needs of such
children.
‡
• If the child has other risk factors (e.g., poor housing condition, anemia, lack of enrichment) but no
noted or suspected delay, the team still assesses for services under Section 504 and, if the
child is eligible, develops an accommodation and monitoring plan and considers placement
in district or other enrichment programs in accordance with the federal provision. If the child
is not eligible, the team proceeds with an annual monitoring plan and referral to Head Start,
school readiness, or other enrichment programs. If the child does not qualify for Section 504,
the team proceeds with an annual monitoring plan and referral to Head Start or a school
readiness or other enrichment program.
* Connecticut Parent Advocacy Center, “Child Find,” accessed March 9, 2017, http://www.cpacinc.org/hot-topics/
child-find; U.S. Centers for Disease Control and Prevention, “Educational Interventions for Children Aected
by Lead” (Atlanta: U.S. Department of Health and Human Services, 2015), https://www.cdc.gov/nceh/lead/
publications/educational_interventions_children_aected_by_lead.pdf.
† U.S. Centers for Disease Control and Prevention, “Educational Interventions for Children Aected by Lead.”
‡ Ibid.
All states participate in IDEA, but state and local implementation and quality varies, resulting in some
dierences in policies, services, processes, and outcomes. One promising, but not yet rigorously evaluated,
strategy to accomplish this is Universal Design for Learning, an educational framework based on scientific
insight for improving teaching and learning for all students.

74
Nutrition
Nutritional measures have not yet been proven to have a clinically important impact on the blood lead levels
of children who have already been exposed.
196
However, nutritional interventions can support children’s
development in areas that lead exposure is known to cause impairment—particularly reading, math, and social-
emotional skills—and so may serve as a buer against lead’s deleterious eects. Multiple studies, including
randomized control trials, have found that healthy diets high in iron may improve children’s developmental
outcomes, including motor control, social interaction, and IQ later in life.
197
In a recent experiment in North Carolina, children with high blood lead levels received various health- and
nutrition-related services, such as WIC, and their parents were given advice about reducing lead in the home.
198
Children in the treated group had improved educational achievement and reduced adolescent antisocial behavior,
compared with the control group, which included children who did not have high blood lead levels and did not
receive interventions. The researchers observed and controlled for some dierences between the two groups,
such as children in the control group had more days absent from school and were suspended more than the
intervention group.
The USDA’s food programs, such as the Supplemental Nutrition Assistance Program (SNAP, previously known as
food stamps) and the National School Lunch Program (NSLP), must meet strong nutrition standards, including
providing meals that are high in iron, calcium, and other vital nutrients, but the research team did not find any
studies of the impact of these programs on children with elevated blood lead levels.
199
A few small studies,
however, have explored how these programs aect outcomes such as reading, math, and social-emotional
skills, which are areas that lead exposure tends to undermine. Specifically, these analyses found slight but not
statistically significant increases in reading and math scores and social-emotional outcomes among children
participating in WIC, while another study identified a positive relationship between participation in SNAP and
reading and math scores among elementary grade girls.
200
Policy in Action: Healthy Diets for Better Long-Term Outcomes
Michigan State University (MSU) and Hurley Children’s Hospital created the Pediatric Public
Health Initiative in January 2016 in response to Flint’s lead crisis. As part of the initiative,
university and hospital sta provide nutrition education.
*
Additionally, the Fair Food Network,
an organization committed to connecting families with healthy food, expanded its “Double-Up
Food Bucks” program to increase participants’ access to fruits and vegetables. This initiative
matches the value of federal food assistance that enrollees spend on produce at participating
farmers markets and grocery stores. For example, residents who buy $10 worth of fruit and
vegetables get another $10 in produce. Similarly, WIC beneficiaries can receive coupons to buy
locally grown fruit and vegetables through a program called WIC Project Fresh.
†
* Michigan State University, “About MSU-Hurley Children’s Hospital Pediatric Public Health Initiative,” accessed Jan.
25, 2017, http://humanmedicine.msu.edu/pphi/About.htm.
† Michigan State University, “Fight Lead With Nutrition,” accessed Feb. 18, 2017, http://msue.anr.msu.edu/uploads/
resources/pdfs/MSUE_Fight_Lead_With_Nutrition_WEB-4-22-16.pdf.

75
Stakeholder input
Parents of children with a history of exposure or who may be at risk strongly and consistently urged universal
blood lead testing.
201
Further, they advocated for blood tests to start early (e.g., 9 months) and be conducted
often, with some recommending annual tests. Parents of lead-exposed children thought having this information
sooner could have enabled them to seek appropriate follow-up treatment.
Some focus group participants explained that their children had blood lead tests as part of regular pediatric
checkups, but others said they had to ask their pediatricians for the tests. Participants in Flint noted that parents
without health insurance, especially immigrant families, might not have access to blood tests. Many participants
supported universal testing, though some said that positive tests set o a chain of negative events, including
visits from the health department, home inspections, doctor appointments, and requirements to abate or
remediate lead. Some participants reported receiving threats that Child Protective Services would remove their
children if they did not comply with health department requirements to remediate hazards.
Community members and parents emphasized the importance of prevention and improved awareness among
adult caregivers before children come into contact with lead, but many also commended the early interventions
their children received. Recommendations to improve these programs included professional development for
teachers, specialized curricula, and extension of certain services to older children.
Participants recommended employing community health and social workers to implement parent-focused
interventions and reinforced the need for neuropsychological assessments to ensure that interventions address
each child’s specific challenges. Other concerns included the cost of assessments and insurance coverage of
related expenses.
A small number of focus group participants mentioned healthy, nutritious food as a way to help protect children
from the eects of lead exposure. In Baltimore, a parent attributed her son’s decreasing lead levels to the diet
high in vegetables and fruits he received at school. Other participants in the same group referred to a connection
between diets rich in iron and low blood lead levels. In Chicago, a focus group participant explained that the
farm-to-school program described earlier in this report expanded to accept SNAP benefits, which allowed more
children to take advantage of the health benefits of fresh fruits and vegetables. In Indiana, the NAACP started
produce giveaways at two churches.
Experts from the national listening sessions and the advisory committee recommended including nutrition as
a policy to combat the eects of lead exposure. Listening session participants also considered whether special
education eligibility regulations should cite specific blood lead levels and inquired whether the Health Insurance
Portability and Accountability Act prohibits health care providers and health agencies from disclosing children’s
blood lead levels to schools; it does not in most cases.
202
Proposed solution
Although all children benefit from healthy diets, nutritional interventions cannot completely prevent the harms
associated with lead exposure.
203
However, based on the literature, expanding the services and outreach provided
by programs such as WIC, SNAP, Child and Adult Care Food Program (CACFP), and the NSLP helps improve
children’s academic and social outcomes.

76
Additionally, a vast and robust body of literature demonstrates positive outcomes for children with deficits similar
to those that result from lead exposure who receive high-quality educational interventions. Experts in pediatrics
and project advisers agreed that providing access to developmental assessments and culturally appropriate
evidence-based programs is critical to responding to lead poisoning in children. Parents of lead-poisoned children
who participated in focus groups universally agreed that their children benefited from educational supports.
Giving children with elevated blood lead the best opportunity for success begins with ensuring that clinicians
follow blood lead testing guidelines; recommendations to improve blood lead testing for high-risk children are
included later in this report. Once a child is identified as having elevated levels of lead in his or her blood, any
ongoing source of exposure must be removed and neuropsychological assessments should be conducted to
identify the specific parts of the brain that have been aected. From there, caregivers need help navigating the
complicated system of potential educational and care interventions. Child Find is one program that can help
parents identify and enroll their children in appropriate programs. These are the ideal steps for children who
have been exposed to lead, but they are not in place in most communities in the U.S.
In the absence of this protocol, children with a history of elevated blood lead levels should be oered entry
into early and middle childhood development programs that are available in their communities. To quantify the
potential of doing so, the study team modeled the benefits of providing high-quality, culturally appropriate early
and middle childhood education and care programs for children known to have been exposed to lead.
Assumptions
• The team modeled the eect of high-quality interventions on later-life outcomes for children with blood lead
levels above 2 μg/dL. This blood lead level was selected because too few children in NHANES had blood lead
levels above other potential cut-points such as 3.5 or 5 μg/dl, which would lead to instability in the modeling,
and because, given that any lead in blood is harmful, it is the lowest practical level for which remediation
might be oered.
• The team drew eect sizes from a review of experimental evaluations and meta-analyses of programs
for children in early and middle childhood and then took the median eect size across the studies for
each outcome.
• Child Trends identified evidence-based interventions and determined their eect sizes for children with other
disadvantages, such as poverty and trauma. The relevant outcomes in the SGM include improved reading
and math scores and reduced antisocial behavior and hyperactivity, which are all areas of potential deficit in
lead-exposed children. To be included, interventions must have been rigorously evaluated, served children
in early or middle childhood, and reported on one or more of the outcome categories in the SGM: academic,
behavioral, or both. Assuming comparable benefits for children with lead-related deficits, those eect sizes
were used to predict impacts on children’s educational attainment, rates of teen parenthood and criminal
convictions, and family income later in life.
Findings
The Social Genome Model found possible benefits of high-quality early and middle education programs
for children with blood lead levels above 2 μg/dL (see Table 7), compared with having no such intervention,
including:
• Increases of roughly 4 and 3 percentage points, respectively, in the likelihood of earning a high school diploma
and a four-year college degree. Among the 2018 birth cohort, this would result in more than 13,000 additional
high school graduates.

77
• Decreases of 1.1 and 1.7 percentage points, respectively, in the likelihood of becoming a teen parent or being
convicted of a crime. This translates into 4,300 fewer teen parents and 6,200 fewer convictions among the
2018 birth cohort alone.
• Increased estimated lifetime family earnings of:
• $33,000 for children who receive only early interventions.
• $69,000 for children enrolled only in middle childhood interventions.
• $102,000 for children who receive both.
Table 7
Providing Both Early and Middle Childhood Interventions Could
Yield the Greatest Benefits
Eects on education, crime, and income
Notes: Analysis is based on the SGM’s sample of about 8,000 children drawn from the Children of the National Longitudinal Survey of
Youth dataset. To arrive at the number of children positively aected, the research team applied the percentage point dierences between
baseline conditions and total prevention to the roughly 365,000 children in the 2018 birth cohort whose blood lead levels would probably
exceed 2 μg/dL.
Source: Social Genome Model analysis by Child Trends and the Urban Institute
© 2017 The Pew Charitable Trusts
Outcome Baseline
Early childhood
programs
Middle childhood
programs
Both
With
intervention
Children
aected
With
intervention
Children
aected
With
intervention
Children
aected
At age 19
Average high school GPA 2.74 2.77 N/A 2.79 N/A 2.82 N/A
Percentage
of children
Earn a high
school diploma
74.4% 75.6% 4,100 76.9% 9,200 78.0% 13,300
Become a teen
parent
20.1% 19.9% 900 19.2% 3,500 19.0% 4,300
Be convicted of
a crime
22.0% 21.4% 2,500 21.0% 3,700 20.3% 6,200
At age 29
Earn a 4-year college degree 17.0% 18.1% 3,800 18.9% 6,800 19.9% 10,700
Income (in 2015 constant dollars)
Mean family at age 40 $62,300 $65,500 N/A $68,800 N /A $72,000 N /A
Estimated lifetime family $753,500 $786,700 N/A $822,000 N/A $855,300 N/A

78
Potential challenges
Dierences in guidelines for and implementation of blood lead testing and parents’ concerns about safety and
cost may pose barriers to identifying children exposed to lead. Requiring universal testing in communities at
high risk would push local clinicians to recognize the urgency of blood lead tests and ensure that lead-exposed
children receive needed follow-up services. Increasing environmental testing and public disclosure of results
could help parents make more informed choices about having their children tested.
The lack of studies investigating the eectiveness of educational interventions for children with a history of
elevated blood lead levels may present an obstacle to increasing availability of these programs. The unique
biological mechanisms by which lead contributes to behavior and attention deficits in children may mean that
interventions that support non-exposed children with similar deficits will not yield comparable benefits for
lead-exposed children. More research is needed to determine which specific types of interventions, if any, could
eectively help to mitigate the various impacts of lead on children’s brains.
Further, the cost of neuropsychological and developmental assessments may be a barrier to children being
evaluated and receiving needed services. States and the CMS could improve access by providing adequate
reimbursement for comprehensive follow-up services for children aected by lead, such as inspection and
reduction of hazards, family support and coaching programs, and remediation and developmental assessments.
In addition, school systems may not be in compliance with legal requirements to provide services such as special
education to children with a history of elevated blood lead levels because they have not allocated enough funding
or for other reasons. Without additional financial resources to increase access for these children, schools may
shift funding from one child in need to another. Similarly, schools and districts also may not have the capacity for
needed training and stang, and programs that require complete fidelity to a specific model may not be flexible
enough to adapt to local circumstances.
Finally, stakeholders worried about stigma associated with labeling children as having a disability, so care
would need to be taken to address the potential unintended harms of increasing enrollment in these programs.
Specifically, trauma-informed care, an approach now being used in schools that involves understanding,
recognizing, and responding to the eects of trauma, could be a useful model for lead-exposed children to
minimize stigma and enhance understanding among providers, caregivers, and children. To address stakeholders’
concerns about lack of support after children age out of programs, mental health and other services should
be made available to young people over the age of 18 with a history of childhood exposure to help reduce
interactions with the criminal justice system, diculties with job performance, and risky behaviors.

79
Recommendations
Children poisoned by lead may suer from impaired brain development and behavior problems, making them
more likely to struggle and drop out of school, get into trouble with the law, and underperform in the workplace.
It is not possible to quantify the emotional and psychological trauma these children and their families experience.
Eliminating lead exposure would avoid health and financial harms to families and future generations and could
yield $84 billion in discounted future benefits per birth cohort. The federal government would realize about
$19 billion, and states would gain approximately $10 billion, in the form of increased tax collections and lower
health care, education, and safety net expenditures for the children born in 2018 alone. In the absence of lead,
these children will have higher GPAs, a better chance of earning their high school diplomas and of graduating
from college, and they will be less likely to become teen parents or be convicted of a crime. Among children for
whom prevention eorts have come too late, comprehensive academic and behavioral interventions may help
overcome the challenges they will encounter and could help prevent the toxic eects of lead from diminishing
their lifelong health and potential for achievement.
Federal, state, and local organizations should coordinate to eectively align and target resources. In light
of the overwhelming evidence about the eects of lead at very low levels and the urgency of sending our
next generation of children to school ready and able to learn, the team developed the following 10 policy
recommendations and implementation tactics for various sources of lead exposure, such as housing and water.
At the national level, the success of these strategies depends on a comprehensive approach, rather than focusing
discretely on individual sources of lead, and demands collaboration across agencies and levels of government
to achieve full implementation within the next 36 months. At the state and local levels, data on community risk
factors can inform prioritization of the recommendations.
Priority sources
Based on the quantitative and qualitative findings the study team recommends prioritizing policies that address
sources of lead with which children are most likely to come into contact and in the places that they spend most
of their time.
Reduce lead in drinking water in homes built before 1986 and other places children frequent
• By 2019, the EPA and states should require water utilities to submit plans for full lead service line replacement
across their systems, including specific eorts by utilities to reduce the financial burden on low-income
customers. The plans should include strategies for ensuring customer safety following LSL replacement, such
as flushing, monitoring, and provision of water filters. For example, Lansing, Michigan; St. Paul, Minnesota; and
Madison, Wisconsin, have nearly completed replacement of their LSLs. (See Policy in Action on Page 36.)
• State or local governments should require all properties to be inspected for drinking water lead risks before
sale or lease.
• The EPA should develop an action level for lead in a home’s drinking water. Health Canada’s proposed
maximum allowable concentration of 5 ppb could serve as an interim level with the goal of getting to
1 ppb over time.
204

80
• The EPA should increase the number of household drinking water taps that are tested for lead under its Lead
and Copper Rule requirements.
• HUD and the EPA should require drinking water sampling as part of lead risk assessment procedures.
• The EPA and HUD should coordinate funding for addressing lead in low-income housing so it includes the
replacement of LSLs and plumbing as well as removal of paint hazards.
• Municipalities should require developers to conduct full LSL replacement when a structure is sold, demolished,
or rebuilt. Woonsocket, Rhode Island, has pursued this policy. (See Policy in Action on Page 29.)
• The EPA and states should require utilities to take immediate protective steps when partial LSL replacements
occur, including optimized corrosion control, flushing, monitoring, sampling, and clear and timely
communication to aected residents.
• The EPA should provide funding to train water system personnel to improve the consistency and eectiveness
of corrosion control across systems of dierent sizes and water chemistries.
• State Medicaid agencies should seek approval from the CMS to use CHIP funding for testing and remediation
of lead in water in children’s homes and child care facilities. (See Policy in Action on Page 30.)
• The USDA should provide supplemental benefits for SNAP and WIC participants whose home tap water
contains harmful levels of lead to purchase bottled water.
• The USDA should work with the EPA to define water quality for the National School Lunch Program (NSLP)
and the Child and Adult Care Food Program (CACFP).
• For schools and child care sites participating in NSLP and CACFP, respectively, the USDA should establish
a fund for testing and remediation costs. Such a program could be modeled after the NSLP Equipment
Assistance Grants program.
• The USDA should ensure that schools and child care facilities meet water quality standards through its NSLP
Administrative Reviews and CACFP Monitoring.
• Schools and licensed child care facilities should implement the EPA’s 3Ts recommendation to test water
for lead.
• States should require that schools and licensed child care providers test for lead in drinking water and release
the results publicly. California, New York, and Rhode Island already require testing at the tap in these facilities.
(See Policy in Action on Page 27.)
• To increase the number of water samples drawn from places where vulnerable children spend time, the
EPA’s Lead and Copper Rule should require utilities to collect and test water from schools and licensed child
care facilities in their service districts.
Remove lead paint hazards from low-income housing built before 1960 and other places children
spend time
• HUD should increase funding for replacement of windows coated with lead paint, fix peeling paint, clean up
contaminated dust, and treat toxic soil outside homes of low-income families built before 1960, while ensuring
that the homes remain aordable.

81
• The U.S. Department of Energy and states should encourage the replacement of lead-painted windows with
new energy-ecient ones by including the benefits of preventing lead exposure and government dollars spent
in the savings-to-investment ratio used to determine the cost eectiveness of energy upgrades.
• State and local governments should make lead paint hazard control financially accessible for property owners
by oering low-interest loans, tax credits and other incentives.
• States or localities should require housing inspections and remediation of lead paint hazards, including peeling
or chipped paint and contaminated soil and dust, before a home is sold, rented, or financed. Agencies should
seek to reduce costs for compliant rental property owners by, for example, requiring recertification only at
intervals that are demonstrated to protect health. Rental registries, such as those in Maryland and Rhode
Island, and systematic code enforcement, as in Rochester, New York, demonstrate various ways this can be
accomplished. (See Policy in Action on Page 40.)
• States and localities should prevent displacement of tenants in homes with lead hazards by freezing any
eviction proceeding initiated without just cause and within six months of a finding of a high blood lead level
or lead hazard in the home and should prohibit landlords from re-renting units that poisoned a child or where
lead has been found until hazards are addressed.
• States should mandate inspections of all apartments in buildings where one unit is found with hazards to
prevent other children from coming into contact with lead paint hazards. New York state’s notice and demand
authority provides a model for this approach. (See Policy in Action on Page 42.)
• State Medicaid agencies should pay for state and local health department testing of homes in high-risk
neighborhoods for environmental hazards, and states should establish additional permanent sources of
funding, other than Medicaid, for such investigations when aected children do not qualify for other state
or federal funds.
• The CMS and Title V Maternal and Child Health Services Block Grant Program should provide training to
enable home health care workers and other home-based aides to identify potential lead hazards in homes
with children.
• The EPA should update its standards for lead dust, soil, and paint based on evidence, and states should
adopt standards for lead in dust and on porches that are comparable to those covering HUD lead hazard
control grantees.
• The EPA and state and local governments should oer funding to schools and child care providers to support
lead paint hazard identification and mitigation.
Increase enforcement of the EPA’s renovation, repair, and painting rule
• The EPA should develop and implement a strategy for ensuring compliance with its renovation, repair, and
painting rule with an emphasis on older homes with children and child care facilities.
• Local governments should require proof of appropriate EPA-compliant lead-remediation training before issuing
a permit for work that is likely to disturb paint in housing built before 1978 and more broadly disseminate
information about the rule’s requirements. Providence, Rhode Island, and the District of Columbia and have
enacted such policies. (See Page 53.)
• The EPA should provide state and local agencies with funding to support compliance with the rule, including
educating businesses and consumers about the hazards of unsafe renovation and federal requirements.
• The EPA should require that contractors perform dust testing after completing renovation, repair, and painting
work to ensure that the home is safe for reoccupancy.

82
• The Occupational Safety and Health Administration should protect construction and renovation workers and
their children by updating its standards for occupational lead exposure to reduce both on-the-job risks and the
likelihood of dust and other hazards transferring from the jobsite to workers’ homes.
Additional sources
Although the top policy priority should be addressing sources of lead with which children are most likely to come
into contact, achieving total prevention also requires focusing on other sources that contribute to the overall
amount of lead in the environment and may cause individual serious cases of lead poisoning but account for a
smaller proportion of lead in children’s blood overall.
Reduce lead in food and consumer products
• The federal government, through participation in the Codex committee, should encourage expedited reduction
of international limits on lead in foods, particularly those that young children and babies are likely to consume.
Where local surveillance data indicate that children are being exposed to lead from sources such as candy,
health remedies, or cosmetics, state and local agencies should target education and outreach to at-risk
neighborhoods; support cultural awareness among physicians; and increase investigation and enforcement
of small retailers.
Reduce air lead emissions
• The EPA should implement the Children’s Health Protection Advisory Committee’s recommendation to reduce
the National Ambient Air Quality Standard for lead to 0.02 μg /m
3
and prioritize regulation of concentrations
around lead smelting and battery recycling facilities.
• The FAA should eliminate lead from aviation gas and identify alternative formulas that can minimize the cost
to airport and plane operators, and the EPA should issue an endangerment finding that lead emissions from
aircraft threaten public health and promulgate emissions limits, which would then require the FAA to adopt
regulations to ensure compliance with those standards.
• State and local governments should impose fees on airports serving piston engine aircraft that rely on leaded
gas and use the revenue to finance the cleanup of soil in surrounding residential neighborhoods, parks, and
school districts. California levies a fee on paint and petroleum. (See Policy in Action on Page 62.)
Clean up contaminated soil
• Congress should provide adequate funding for Superfund cleanup at lead-contaminated sites.
• The EPA and states should investigate lead levels in neighborhoods near former lead smelter sites and other
industrial and hazardous waste facilities and convey the information resulting from those studies in a culturally
competent manner and in partnership with organizations trusted by local communities.
• The EPA and HUD should coordinate Superfund eorts and lead hazard control activities so that when a
residence is treated for contaminated soil, the interior and exterior of homes are also made lead-safe. The
Omaha Superfund site provides an example of this approach. (See Policy in Action on Page 60.)
• State agencies should develop and fund a coordinated cleanup eort for contaminated neighborhoods.
• The EPA should adopt a health-based standard for lead in dust and soil and eliminate the distinction between
areas where children do and do not play in the soil.

83
Poisoning response
Prevention is the most critical and first approach to addressing childhood lead exposure, but those eorts have
come too late for many children. Policymakers should take concrete steps to ensure that children with elevated
blood lead levels are identified and receive the supportive services they need to minimize negative outcomes and
succeed later in life. Although no studies have specifically assessed the eect of education and care interventions
among children exposed to lead, high-quality programs have shown benefits for children at similar developmental
risk and might improve certain cognitive and behavioral outcomes among lead-exposed children.
Improve blood lead testing among children at high risk of exposure and find and remediate the sources
of their exposure
• The CDC should collaborate with the American Academy of Pediatrics and other professional
organizations, with input from concerned parents, to determine the factors that contribute to the persistent
lack of appropriate testing of high-risk children and should develop and implement strategies to address
identified barriers.
• HHS and the CDC should provide funding to upgrade and improve blood lead surveillance at the state and
local levels and to ensure that health agencies have the necessary resources to provide follow-up care for
children with elevated blood lead, including for finding the sources of exposures and connecting families to
remediation services and developmental and neuropsychological assessments.
• The CMS should work with state Medicaid agencies to increase the number of states that include blood lead
testing of Medicaid-enrolled children as one of its performance measures and should make publicly available
its annual estimates of Medicaid-enrolled children tested for lead by age 2, broken out by state and health
provider.
• State and local health departments should oer blood lead testing at clinics and schools and through mobile
health units to improve access for at-risk families; these sites can use simple, portable devices to check
blood lead levels at the point of care.
205
The results from blood lead tests should be shared with children’s
pediatricians and state agencies responsible for surveillance.
• The USDA should develop mechanisms to reimburse blood lead testing conducted at WIC sites in concert
with hemoglobin testing.
• State Medicaid agencies should only allow health care providers to receive an increased reimbursement
rate for Early and Periodic Screening, Diagnostic and Treatment services if required blood lead testing is
also conducted.
• State Medicaid agencies should use CHIP funding to increase inspections of the homes of lead-exposed
children and to remediate identified paint, dust, soil, and water hazards.
Ensure access to developmental and neuropsychological assessments and appropriate high-quality
programs for lead-exposed children
• The U.S. Departments of Health and Human Services and Education and state and local health and education
agencies should invest in high-quality early and middle childhood education programs for children with a
history of elevated blood lead levels.
• State education departments, through their Child Find programs, should collaborate with local health
departments to identify children with elevated blood lead levels and ensure that they receive needed supports
and services. Connecticut provides a model approach. (See Policy in Action on Page 73.)

84
• The CMS should provide adequate reimbursement for comprehensive follow-up services for children aected
by lead, including lead hazard remediation and developmental and neuropsychological assessments.
• State education agencies should modify their IDEA Part C programs so neurocognitive and developmental
deficits of lead exposure qualify for services and should presume that children with elevated blood lead levels
are eligible for services. States also should modify IDEA Part B programs to help local education agencies
identify and provide interventions and accommodations for children aected by lead.
• The USDA should increase funding for programs such as WIC and SNAP to expand their ability to improve
children’s nutrition.
Data and research
Decades of research have documented the extent of lead exposure and its impacts on children, but as policy
actions have helped curb exposures, research has not kept pace. As a result, more study of the eectiveness of
interventions on today’s lower blood lead and exposure levels is needed. In addition, local data, which play an
important role in helping public health ocials and community organizations identify and target treatment and
response eorts, are often not readily available to the agencies and groups that need them.
Improve public access to local data
• The CDC should, in partnership with community-based organizations, local health agencies, and private
philanthropy, collect census tract level data on blood lead level results; the presence of leaded drinking water
pipes; and lead in the water, dust, paint, and soil of homes, schools, child care facilities, and other places
children spend time.
• The CDC should use gathered data to produce culturally competent and accessible community lead reports
and broadly disseminate them to health care providers, school administrators, and child care operators. New
York City’s Environment & Health Data Portal is a good example.
• States should require laboratories to electronically submit all blood lead test results to local and state health
departments within a week of the result so the information can be aggregated to assist with prevention and
response eorts.
• States should be required to report blood lead surveillance data to the CDC.
• States should, in partnership with local health agencies and their municipalities, make property-specific
information on leaded drinking water pipes and lead in water, dust, paint, and soil of homes, schools, child care
facilities, and other places where children spend time easily available to the public.
Fill gaps in research to better target state and local prevention and response eorts
• The federal government should support an integrated national survey of children’s blood lead levels and
multiple sources of exposure, including food, water, soil, paint, house dust, and consumer products.
• HUD and the EPA should design and implement a study of water from a representative sample of U.S. housing
to collect data that can be used to estimate how much lead dierent sections of the house plumbing system
add to water. Samples should be drawn over time during cold and warm weather, from dierent parts of
the service lines, and under varying corrosion control and water source conditions. The study design should
produce exposure estimates for susceptible populations such as formula-fed babies and expectant mothers.
• The EPA should develop and validate a standardized method for sampling water for homes, schools, and child
care facilities that can be implemented in the field by environmental health professionals.

85
• The EPA should support an evaluation of the ecacy and eciency of water pipe liners and point-of-entry
water filters for prevention of lead leaching.
• The EPA should identify barriers to optimal corrosion control and methods to overcome them, including
widespread education of the public and water utilities.
• The EPA should develop field tools to identify LSLs.
• The EPA should evaluate the eectiveness of dierent periods of flushing in reducing dissolved and particulate
lead concentrations at household taps.
• HUD should research the eectiveness of various lead hazard control treatments in preventing blood lead
level increases.
• HUD and the EPA should undertake large-scale studies to test the eect of soil treatments over time to inform
cleanup programs.
• Federal, state, and local agencies and philanthropy should conduct small-area population-based studies to
identify relative risks among communities and subpopulations compared with the general population.
• The National Institute for Environmental Health Sciences should fund studies on the impacts of prenatal and
early childhood lead on high-prevalence adult conditions such as hypertension, cardiac disease, and stroke.
• The EPA and other agencies should conduct studies to understand the primary sources of children’s lead
intake, including dietary, residential, and neighborhood sources among the general population and newly
arrived immigrant groups.

86
Conclusion
Childhood lead poisoning is preventable. U.S. children’s blood lead levels have declined dramatically over the
past few decades as a result of successful policy interventions that have removed large amounts of lead from the
environment and reduced potential sources of exposure. However, current crises in Flint, East Chicago, and other
communities across the country demonstrate the need for continued attention and action to protect children
from the harmful eects of lead.
Eliminating lead hazards from the places where children live, learn, and play will pay dividends in terms of social
and educational outcomes, and this analysis found that it also could yield $84 billion in long-term benefits per
birth cohort. The federal government would reap about $19 billion, and states would gain approximately $10
billion for children born in 2018 alone. In the absence of lead, hundreds of thousands of children would be more
likely to realize their full potential thanks to higher GPAs, a better chance of earning high school diplomas and
graduating from college, and a reduced likelihood of becoming teen parents or being convicted of crimes.
Children spend dozens of hours each week in school and child care facilities, and dozens of case reports show
elevated levels of lead in the tap water of these facilities. Yet only scarce national data are available to indicate
how much lead children are coming into contact with in classrooms, from drinking fountains, or on playgrounds.
Uncovering and remediating the current sources of childhood exposure to lead both nationally and at the
community level, given the importance of contextual factors, should be a high priority.
And while prevention is the priority, addressing sources of lead does little to meet the needs of children once they
have been exposed. Children with a history of lead exposure can suer from impaired brain development and
behavior problems, making them more likely to struggle and drop out of school, get into trouble with the law, and
underperform in the workplace. And recent research confirms that the eects of early childhood exposure to lead
persist, undermining cognition and socioeconomic status well into adulthood.
206
Giving these children the best opportunity for success begins with ensuring that clinicians follow blood lead
testing guidelines. Although no studies have evaluated the eectiveness of childhood interventions for lead-
exposed children, the absence of these data should not prevent children from receiving evidence-based, high-
quality childhood interventions shown to reduce the same cognitive and behavioral deficits common among
lead-exposed children.
By taking steps to both address sources of lead aecting children and implement interventions to help lead-
exposed kids overcome the obstacles they face, federal, state, and local governments together with business
leaders can save billions of taxpayer dollars, generate thousands of good jobs, and improve the quality of life
for children and families across the nation.

87
Glossary
Abatement: Measures to permanently control (i.e., 20 years or more) lead-based paint or paint hazards,
including contaminated soil, dust, and deteriorated lead-based paint. EPA regulations exclude from the definition
“renovation, remodeling, landscaping or other activities, when such activities are not designed to permanently
eliminate lead-based paint hazards, but instead are designed to repair, restore, or remodel a given structure
or dwelling, even though these activities may incidentally result in a reduction or elimination of lead-based
paint hazards.”
207
Action level: Measurements used to express a health or physical hazard. They indicate the level of a harmful
or toxic substance or activity requiring medical surveillance, increased industrial hygiene monitoring, or
biological monitoring.
Blood lead test: Any draw of blood (capillary, venous, or unknown sample type) from a child that produces a
quantifiable lead level result and is analyzed by a certified facility or an approved portable device. A blood lead
test may be collected for use in screening, confirmation, or follow-up.
Community Development Block Grant (CDBG) program: A HUD program that issues grants to local government
and state entities to promote community development. Lead-based paint activities are an eligible expense under
the program.
Comprehensive Environmental Response, Compensation and Liability Act (CERCLA): A federal law enacted
in 1980, also known as Superfund, that granted federal agencies the authority to respond to public health and
environmental threats posed by the release of hazardous substances and levied a tax on the chemical and
petroleum industries to fund cleanup of waste sites. The funding provision has since expired, and the program is
now funded through regular appropriations.
Corrosion control: Treatment to minimize the dissolution of lead and/or copper in drinking water.
Cultural competency: The ability to address people’s diverse values, beliefs, and behaviors in public programs to
ensure they promote equity by meeting the particular needs of the population being served.
Early Periodic Screening Diagnostic and Testing (EPSDT) program: A comprehensive preventive child health
initiative that emphasizes early assessment of children’s health care needs and requires that all children receiving
Medicaid be tested for various health indicators, including blood lead at 12 and 24 months of age, unless the state
has been granted a waiver by the CMS.
Eect size: A quantitative measure of the magnitude of a dierence between or within groups over time. Eect
size is particularly useful in comparing the eects of interventions.
Elevated blood lead level (EBL): The CDC uses this term to refer to a blood lead level greater than or equal
to 5 μg/dL, which it defines as high and requiring public health intervention. (See also “reference value” and
“lead poisoning.”)
FIND: Filming Interactions to Nurture Development.
Healthy, Hunger-Free Kids Act (HHFKA): An update to the Child Nutrition Act passed in 2010 to improve child
nutrition through oversight of the USDA’s child nutrition programs, including the National School Lunch Program,
the School Breakfast Program, the Special Supplemental Nutrition Program for Women, Infants and Children
(WIC), the Summer Food Service Program, and the Child and Adult Care Food Program.

88
Integrated Exposure Uptake and Biokinetic model (IEUBK): Estimates lead in children using four interrelated
modules (exposure, uptake, biokinetic, and probability distribution) for children exposed to lead from water,
food, dust and soil, and through inhalation. The model allows the user to estimate, for a hypothetical child or
population of children at dierent ages, a distribution of blood lead concentrations based on information about
dierent sources of exposure to lead.
Individuals with Disabilities Education Act (IDEA): A law that was first enacted in 1975 to protect the rights of
children with disabilities to receive free appropriate education.
Interim controls: Set of measures to temporarily control lead-based paint hazards. Interim control methods
must be completed by qualified workers using safe work practices and followed by clearance testing. Follow-up
monitoring is needed.
Lead and Copper Rule (LCR): A regulation introduced by the EPA in 1991 to control lead and copper in the
drinking water distribution system. The EPA is currently considering new modifications to the rule, which has
been revised several times.
Lead-based paint: Defined by HUD and the EPA as existing paint or other surface coatings that contain lead
equal to or exceeding 5,000 parts ppm. In 1978, the CPSC banned residential use of new lead-based paint that
contained greater than or equal to 600 ppm of lead, which was later reduced by Congress to 90 ppm.
Lead-based paint hazards: Any condition that causes exposure to lead from dust-lead hazards, soil-lead hazards,
or lead-based paint that is deteriorated or present in chewable surfaces, friction surfaces, or impact surfaces, and
that would result in adverse human health eects.
Lead-Based Paint Hazard Control Grant Program (LBPHC): A HUD-administered program that assists elements
of local government in establishing programs to address lead-based paint hazards in privately owned residences.
Lead exposure: In toxicology, exposure is defined as any detectable level in blood; thus, lead exposure in this
document means any detectable level of lead in blood.
Lead poisoning: For the purposes of this report, a child is considered to have been poisoned by lead if he or she
has a single blood lead test (capillary or venous) at or above the Centers for Disease Control and Prevention’s
2012 reference value of 5 μg/dL even though some experts use the term to refer to a child who is at risk of a
blood lead concentration greater than 5 μg/dL.
Lead service line (LSL): The pipe that connects a home or other structure to the water main. Use of lead pipes in
all drinking water plumbing, including service lines, was banned by Congress eective 1986.
Microgram (μg): 1/1000th of a milligram (or 1 millionth of a gram). To put this unit into perspective, a penny
weighs 2 grams, so a microgram would be one of 2 million equal pieces of that penny.
National Health and Nutrition Examination Survey (NHANES): A set of representative national surveys
that measures the health and nutrition of adults and children in the United States using interviews, physical
examinations, and blood specimens. NHANES is the main government data source for estimating mean blood
lead levels for the U.S. population and the number of children with high blood lead levels.

89
National Ambient Air Quality Standards (NAAQS): EPA rules for concentrations of various pollutants in outdoor
air intended to minimize human health risks.
National Priorities List (NPL): The EPA’s list of locations with hazardous wastes eligible for cleanup
under CERCLA.
Parts per billion (ppb): Equivalent to μg/kilogram by weight, a part per billion is equal to the value of one penny
compared with $10 million. This unit is used to measure lead in water.
Parts per million (ppm): Equivalent to μg/gram (10,000 ppm = 1 percent) by weight, this unit is used to measure
lead in paint and soil.
Quality-adjusted life year (QALY): A generic measure of disease burden, including the quality and the quantity of
life lived that is used in economic evaluations to assess the monetary value of medical interventions. One QALY is
equal to one year of perfect health.
Reference value/level: A value used to identify children with blood lead levels that indicate an elevated source of
exposure in their environment. The value is based on the 97.5th percentile of blood lead concentrations from the
National Health and Nutrition Examination Survey. In 2011 this value was 5 μg/dL, and the CDC recommended
implementing interventions for individual children at this or higher blood lead concentrations. The CDC has not
made a recommendation for blood lead levels at the 2014 reference value of 3.5 μg/dL. The reference value is
calculated every four years based on the two latest years of NHANES data.
Risk assessment: A comprehensive evaluation, conducted by a certified assessor, to identify lead-based paint
hazards using paint testing, dust and soil sampling, and visual examination, and to recommend appropriate
reduction methods.
Savings to investment ratio (SIR): A measure that expresses the ratio of savings to costs.
Smelter: An industrial facility that extracts metals from ore (usually mixed with purifying and/or heat-generating
substances such as limestone and coke) at high temperature in an enclosed furnace. The process results in lighter
ore components (impurities called slag or tailing) rising to the top and floating on the molten metal.
Social Genome Model (SGM): A quantitative tool that combines two national longitudinal datasets to simulate
the eects of childhood interventions on outcomes at five life stages, from birth to age 40.
Soil remediation: The purification, covering, or removal of contaminated soil.
Value of Prevention (VP) Tool: A quantitative modeling system that synthesizes data from literature and national
datasets to characterize the financial and health impacts of investment in prevention from the perspectives of
dierent stakeholders.

90
Appendix: Methodology
Study methods included policy screening, literature review, case studies, interviews, national listening sessions,
focus groups, and quantitative modeling. (See Table A.1.) The models required several inputs, including the
number of children likely to be aected by a proposed policy, their baseline blood lead levels, and the expected
change in those levels as a result of each policy intervention.
To determine the number of children aected by a policy, the researchers sought information about the scope of
sources of exposure. For example, to determine the eect of replacing lead service lines, researchers needed to
know how many children live in homes with those lines, the level of lead in the water of their homes, their current
blood lead levels, and what the evidence suggests would happen to their blood lead levels with the replacement
of the lead lines. In the case of policy proposals for which those data were lacking, the team did not attempt
quantitative modeling and instead relied on qualitative research. Similarly, the team conducted cost-benefit
analyses only for policy solutions for which cost information was available. Details of the various methods are
included below.
Method Purpose Source
Policy screening
• Narrow the list of policies to be included in the
assessment
Literature review
• Identify potential policy interventions
• Document the relationship between blood lead
levels and parameters in the quantitative models
including IQ, earnings, and math and reading
scores
• Identify the eect sizes of potential policy
interventions on environmental lead levels,
blood lead levels, and educational and behavioral
outcomes for use in quantitative modeling
• Determine the populations aected by the
prospective policies
• Document known sources of exposure
for aected populations and vulnerable
subpopulations
Articles in medical, public health, education,
and child development publications, including
original papers, meta-analyses, syntheses,
and literature reviews
Case studies
• Illustrate if and how recommended policies have
been implemented at the state and local levels to
provide pragmatic information
Informant interviews
• Capture the perspectives of stakeholders,
such as parents of children with a history of lead
exposure, businesses that could be aected by
the policies, and environmental health and early
childhood experts and advocates
Table A.1
Summary of Research Methods
Continued on next page

91
Policy screening process
The Health Impact Project conducted policy screening between August and December 2016 using the
following criteria:
• Will Congress or a federal, state, or municipal agency likely consider the policy within the next 18-36 months?
• Does an authoritative document (i.e., a produced by a multidisciplinary task force, advisory committee,
professional organization, or government body) cite the policy as a recommendation?
• Is the policy a high priority for aected populations?
• What is the expected result of the policy intervention in terms of the number of children aected and eect
size of the intervention?
The timeframe criteria reflect the team’s desire to identify policies that can reasonably be advanced in time
to protect the next generation of children. The 18-36 month window assumes policy adoption, but not full
implementation. The team relied on authoritative documents to identify recommendations that addressed
stakeholder priorities and that experts and advocates had previously vetted. To avoid potential conflicts between
recommendations promoted by agencies and experts and those endorsed by community members, the team
specifically sought input from aected populations during the policy screening process.
The screening process began with an Aug. 5 meeting of advocates and experts from the fields of water, housing,
soil, consumer products, and early childhood to identify “best policy bets.” The research team used the findings
from the meeting, combined with recommendations developed by a wide range of organizations and agencies, to
generate a list of more than 100 policy options for consideration. (The full list is available upon request.)
The team then refined the list to include policies that would result in either reduced environmental sources of
lead (prevention) or the provision of a service for children at risk or with a history of exposure (response). This
screening led the team to initially exclude financing strategies, operational policies (e.g., task forces, job training),
and approaches to blood lead testing.
© 2017 The Pew Charitable Trusts
Method Purpose Source
National listening sessions
• Identify possible unintended benefits and
consequences of policy interventions
• Prioritize recommendations
Federal, state, and local ocials, industry
representatives, academics, and advocacy
organizations
Focus groups
• Prioritize recommendations
• Document community concerns and priorities
• Identify possible unintended benefits and
consequences of policy interventions
Landlords and property managers
Parents of children with a history of lead
exposure
People at high risk of exposure, and other
concerned community members
Quantitative models
• Quantify potential eects of policy interventions
on early childhood and adult outcomes, including
cognitive and social/emotional development,
academic achievement, and earnings
• Predict policies’ long-term economic impacts in
terms of potential cost and future savings
Social Genome Model and Value of
Prevention Tool

92
After the initial screening, about 50 policies remained for consideration. In October 2016, subject matter experts
helped the team further narrow the list to 28 for potential study. The experts subsequently identified several
underrepresented policy areas on the list, including schools, plumbing fixtures, wells, lead paint hazards created
through demolition, exposures associated with Superfund sites, lead in ambient air, occupational hazards,
blood lead testing, state and municipal policies, and early interventions for children exposed to lead. The team
conducted informant interviews and additional literature reviews to fill many of these gaps. For example, at the
recommendation of stakeholders, the team included several financing policies deemed critical to implementing
the prevention policies, as well as options related to blood lead testing, Superfund, early interventions, and
schools and child care facilities. In total, the team studied 10 high-level policy options and analyzed 70 tactics for
implementing those 10.
In November 2016, the Health Impact Project conducted a series of national virtual conversations to collect
stakeholder feedback on the interventions and tactics. Between December 2016 and January 2017, the team held
focus groups to document the concerns of communities across the country. Feedback from these events also
helped refine the list of policies considered for analysis.
Literature review
Researchers from Pew, with support from Child Trends and other experts, led the literature search to answer a
set of research questions on the eects of lead on young children and interventions to prevent and respond to
exposure. The initial research questions were:
1. To what extent do blood lead levels above 5 μg/dL aect cognition and academic achievement (i.e., IQ,
reading scores, math scores, high school drop-out/graduation rates, cognition, attention disorder, memory
impairment)?
2. To what extent do elevated blood lead levels aect lifetime earnings (i.e., lifetime earnings, employment,
income)?
3. To what extent do elevated blood lead levels aect criminal behavior (i.e., delinquency, violent crime)?
4. To what extent do elevated blood lead levels aect health (i.e., hypertension, cardiovascular health,
immunological health, endocrine health, child growth rates, hearing)?
5. To what extent does the replacement of lead service lines decrease or prevent elevated blood lead levels?
6. To what extent does lead hazard control prevent elevated blood lead levels?
7. How do nutritional interventions impact cognition and educational achievement for children exposed to lead
(i.e., IQ, reading scores, math scores, high school drop-out/graduation rates, cognition, attention disorder,
memory impairment)?
8. How do nutritional interventions impact cognition and educational achievement for children with blood
lead levels less than 5 μg/dL (i.e., IQ, reading scores, math scores, high school drop-out/graduation rates,
cognition, attention disorder, memory impairment)?
9. How do early childhood education interventions impact cognition and educational achievement for children
with blood lead levels greater than 5 μg/dL (i.e., IQ, reading scores, math scores, high school drop-out/
graduation rates, cognition, attention disorder, memory impairment)?
10. How do early childhood interventions impact cognition and educational achievement for children with blood
lead levels less than 5 μg/dL (i.e., IQ, reading scores, math scores, high school drop-out/graduation rates,
cognition, attention disorder, memory impairment)?

93
11. To what extent do detectable levels of lead in a pregnant woman’s blood aect her newborn’s health?
12. To what extent do the impacts of lead poisoning increase societal or taxpayer costs?
Pew searched PubMed, Cochrane, Campbell, ERIC, EBSCO, Google Scholar, and Google databases for systematic
reviews, experimental studies, and quasi-experimental studies conducted over the past 30 years. For searches
that yielded a large number of results, the team screened a minimum of 50 abstracts to determine relevance to
the research questions, and for those that produced fewer than five articles, the team employed a “snowball”
method to identify relevant peer-reviewed studies and gray literature from citations and bibliographies. The
search excluded articles published in languages other than English or that studied populations outside the
United States, except when no U.S. studies addressed a particular research question, in which cases the team
expanded the search to international articles published in English. For each study, the team documented the
target population, source name, article title, year of publication, authors, source type (e.g., peer-reviewed or gray
literature), analysis type (i.e., systematic review, experimental study, quasi-experimental), data sources and
measures, and key findings. The initial search included 100 articles in medical, public health, education, and child
development publications, including original papers, meta-analyses, syntheses, and literature reviews.
Concurrent with the literature search, the Health Impact Project commissioned five sector-specific white papers
to summarize the literature related to the prospective policies. Experts prepared papers on housing, water,
consumer products, early interventions, and schools and child care facilities and contributed additional references
to be included in the Pew literature review. Child Trends reviewed the sector-specific white papers to compare
the studies cited in those with other identified articles to ensure that no major research was omitted. Experts
recommended several international studies to fill gaps where U.S. data were lacking and the team eventually
included those in the search results. Pew, with assistance from Child Trends, the Urban Institute, and Altarum
Institute, conducted additional literature searches throughout the project based on input from key informants,
subject matter experts, and advisory committee members. The team ultimately reviewed well over 700 articles.
Of those, Child Trends reviewed 176 studies that provided information necessary to inform the inputs in the two
quantitative models. Child Trends, the Urban Institute, and Altarum Institute performed a third-party review of
these selected studies to establish eect sizes for interventions that would be included in the models. Using a five
category scale, Child Trends evaluated the strength of each study used to estimate eect sizes based on design,
sample size, attrition rate, intent-to-treat analysis, clarity of variable definitions, and whether or not the studies
adjusted for socio-economic status. (See Table A.2.)

94
Study type Lower quality Higher quality
Level 1: Meta-analysis
Design
Quasi Experimental Designs (QEDs) or mix
of randomized control trials and QEDs
Randomized control trials
Number of included studies Fewer than 10 10 or more
Inclusion/exclusion criteria
Unclearly defined, or inconsistently applied
across studies
Clearly defined, and consistently applied
across studies
Attrition
Attrition rate of included studies is 50% or
more and/or varies between treatment and
control group
Attrition rate of included studies is 49% or lower
Control variables
Included studies don’t control for
socioeconomic status
Included studies that control for at least one
measure of socioeconomic status, such as
mother’s education or free and reduced-price
meal eligibility
Intent-to-treat analysis Not used by included studies Used by included studies
Outcome measures
Unclearly defined, not valid and reliable, or
inconsistently applied across study participants
Clearly defined, valid, reliable, and implemented
consistently across study participants
Level 2: Randomized controlled trial
Sample size
No power analysis conducted, or, sample size
insucient to conduct all analyses as required
Sample size is sucient to conduct all analyses as
required. If suciency of sample size is not clear,
then a power analysis was conducted
Attrition
Attrition rate is 50% or more, and/or attrition rate
varies between treatment and control group
Attrition rate is 49% or lower
Control variables Doesn’t include SES
Includes at least one measure of SES such as
mother’s education or free and reduced price
meal eligibility
Intent-to-treat analysis Not used Used
Outcome measures
Unclearly defined, or not valid and reliable, or
inconsistently applied across study participants
Clearly defined, valid, reliable, and implemented
consistently across all study participants
Level 3: Controlled trial without randomization (Quasi-experimental design)
Sample size
No power analysis conducted, or, sample size
insucient to conduct all analyses as required
Sample size is sucient to conduct all analyses as
required. If suciency of sample size is not clear,
then a power analysis was conducted
Attrition
Attrition rate is 50% or more, and/or attrition rate
varies between treatment and control group
Attrition rate is 49% or lower
Control variables Doesn’t include SES
Includes at least one measure of SES such as
mother’s education or free and reduced price meal
eligibility
Intent-to-treat analysis ITT analyses not used ITT analyses used
Outcome measures
Unclearly defined, or not valid and reliable, or
inconsistently applied across study participants
Clearly defined, valid, reliable, and implemented
consistently across all study participants
Table A.2
Strength of Evidence Criteria for Literature Review Used in
Quantitative Models
Continued on next page

95
Study type Lower quality Higher quality
Level 4: Cohort study or case-control study
Sample size Insucient to conduct all analyses as intended Sucient to conduct all analyses as intended
Control variables Doesn’t include SES
Includes at least one measure of SES such as
mother’s education or free and reduced price meal
eligibility
Outcome measures
Unclearly defined, or not valid and reliable, or
inconsistently applied across study participants
Clearly defined, valid, reliable, and implemented
consistently across all study participants
Additional criteria for prospective cohort studies only
Attrition Attrition rate is 50% or more Attrition rate is 49% or lower
Additional criteria for retrospective cohort studies and case control studies
Potential for recall bias Data subject to bias (e.g., subjects asked to recall)
Data from administrative source or recorded prior
to start of study
Missing data 33% or more of cases are missing data Less than 33% of cases are missing data
Additional criteria for case control studies only
Sample selection Convenience sample
Sample selection method accounts for bias (e.g.,
matching, two or more control groups, random
sampling of cases and controls)
Level 5: Cross sectional study
Representativeness
Representative at state or local level; not
representative; representativeness unknown;
or, nationally representative but response rate
below 80%
Nationally representative, with a response rate of
80% or higher
Sample size Insucient to conduct all analyses as intended Sucient to conduct all analyses as intended
Control variables Doesn’t include a measure of SES
Includes at least one measure of SES such as
mother’s education or free and reduced price meal
eligibility
Outcome measures
Unclearly defined, or not valid and reliable, or
inconsistently applied across study participants
Clearly defined, valid, reliable, and implemented
consistently across all study participants
© 2017 The Pew Charitable Trusts
Case studies
Trust for America’s Health (TFAH) and the National Center for Healthy Housing (NCHH) received grants from
the Health Impact Project to create case studies (see the “Policy in Action” listings in the Table of Contents)
detailing successful prevention and response strategies at the state and local levels. To select the case study
subjects, NCHH reviewed literature and developed three criteria for policies and programs under consideration:
diversity of lead hazard exposures addressed (water, housing, consumer products, etc.), geographic diversity, and
impact (based on published evaluations or summaries of the policies and programs). NCHH contacted members
of the National Safe and Healthy Housing Coalition, a broad voluntary coalition of over 300 organizations, for
recommendations on possible case study locations. Based on the literature review and the responses from
coalition members, NCHH recommended 20 communities as models to include in the case studies. The Health
Impact Project made additions to the list using the same criteria. Ultimately, TFAH developed 22 case studies,
and the study team selected 15 for inclusion in the final report based on the above criteria and a determination of
relevance to the policies analyzed.

96
Listening sessions
The Health Impact Project held five national listening webinars to collect additional stakeholder feedback. The
topics of the web-based conversations included housing, schools and childcare, early childhood development,
and consumer products; one general session was also held. In total, more than 200 people registered for
the listening sessions and approximately 195 attended, including individuals from federal, state, and local
environmental, health, housing, water, and utilities agencies and tribal health departments as well as nonprofit
and advocacy organizations who work with policymakers. Stakeholders unable to participate through the
webinars had the opportunity to provide feedback through an online form. The team collected and stored under
password protection registrants’ names, email addresses, and organizations and summarized all feedback
provided in the session thematically.
Parent conversations
The Health Impact Project led two conference calls with a total of eight parents of lead-poisoned children and
guided the participants in open-ended discussions. The conversations focused primarily on interventions for
children with a history of lead exposure and parents’ experiences with various programs. The team summarized
parent feedback thematically and identified relevant quotes for inclusion in the report. The Health Impact
Project collected and stored under password protection participants’ names, cities and states of residence,
and email addresses.
Focus groups
The Health Impact Project held a total of 16 focus groups between December 2016 and January 2017 in
Baltimore; Chicago; Flint, Michigan; Indianapolis; Los Angeles; New Orleans; Philadelphia; and Warren, Arkansas,
with a diverse group of participants, including property owners and landlords, residents of communities aected
by lead exposure, parents of lead exposed children, and representatives from organizations supporting these
populations. (See Table A.3.) The team led the semi-structured, open-ended discussions to identify which
lead sources raised the greatest concern, obtain feedback on potential policies to prevent and respond to lead
exposure, and provide stakeholders with an opportunity to inform the policy development process.
The team sought Institutional Review Board (IRB) approval for the focus group methodology and the Chesapeake
board deemed the project exempt from IRB oversight on Dec. 7. Two to 15 individuals attended each focus group,
and participation was entirely voluntary. Focus group settings included a library, a church, and several facilities
operated by community organizations. Host site contacts chose the locations based on their convenience and
accessibility. Focus group participants received prepaid Visas in the amount of $25 as thank-you gifts. The team
recorded each participant’s city and state of residence. No other identifying information was collected. The team
summarized the findings, and identified key themes.

97
Participant
demographics
n %
Race and ethnicity
American Indian and
Alaska Native
7 7%
Asian and Pacific
Islander
2 2%
Black, non-Hispanic 44 42%
Hispanic, any race 17 16%
White, non-Hispanic 25 24%
Other, including two
or more races
7 7%
No response 2 2%
Educational attainment
Some high school 8 8%
High school/GED 25 24%
Associate's degree 4 4%
Some college, no
degree
16 15%
College graduate or
above
47 45%
Other 2 2%
No response 2 2%
Annual household income
$19,999 or less 24 23%
$20,000 to $24,999 11 11%
$25,000 to $34,999 14 13%
$35,000 to $44,999 18 17%
$45,000 to $54,999 7 7%
$55,000 to $64,999 4 4%
$65,000 to $74,999 4 4%
$75,000 and over 16 15%
No response 6 6%
© 2017 The Pew Charitable Trusts
Housing characteristics n %
Type
Single-family 65 63%
Duplex 10 10%
Multiunit 17 16%
No response 12 12%
Age
Built before 1940 22 21%
Built between 1940
and 1959
20 19%
Built between 1960
and 1978
17 16%
Built after 1978 10 10%
Don’t know 23 22%
No response 12 12%
Ownership
Own 59 57%
Rent 33 32%
No response 12 12%
History of lead testing
Paint/dust 13 13%
Water 15 14%
Paint/dust and water 18 17%
Neither 40 38%
Don’t know 7 7%
No response 11 11%
Table A.3
Focus Group Participant Demographics and Other Characteristics

98
Quantitative methods
Social Genome Model
The Social Genome Model (SGM) is a lifecycle microsimulation model starting at birth and moving through five
subsequent life stages—early childhood, middle childhood, adolescence, transition to adulthood, adulthood—
through age 40. The version of the SGM used for this research (the SGM79) is constructed using two data sets
from the Bureau of Labor Statistics’ National Longitudinal Surveys: the Children of the National Longitudinal
Survey of Youth (CNLSY) and the National Longitudinal Survey of Youth 1979 (NLSY79). The CNLSY follows from
birth through age 19 a sample of children born to the women of the National Longitudinal Survey of Youth 1979
(NLSY79). Most of the children in the CNLSY were born in the 1980s or early 1990s. The second survey is the
NLSY79 itself, which follows a sample of people in the United States born between 1957 and 1964 from their first
interview (ages 14-22 in 1979) into mid-adulthood. Data are available for 25 rounds of data collection, through
2012 when respondents were 47-55 years of age.
To combine the two sources of information, SGM uses information about the children in the CNLSY from birth
through age 19 and then statistically matches them to comparable individuals in the NLSY79 sample based on
variables measuring circumstances at birth and adolescence common in the two data sets. The NLSY79 data are
then used to estimate outcomes at age 29 and age 40 for the children in the CNLSY. The overall model is based
on data on 8,056 children. Lifetime income estimates are based on data from the 1998-2015 Current Population
Survey, which is the primary source of labor force statistics for the population of the United States.
208
The SGM uses CNLSY and NLSY data to track children’s development from birth onward and employs regression
models to assess the relationships between children’s early life circumstances and subsequent outcomes such
as educational attainment, grade point average, teen parenthood, criminal conviction, and lifetime family income.
The model enables researchers to assess how actions at developmentally significant life stages reverberate
through a person’s life. For example, circumstances at birth influence early childhood outcomes, which in turn
aect middle childhood. Those middle and early childhood conditions influence adolescent outcomes, and so
on through middle age. Using data on children to assess these eects over time allows the SGM to explore how
early changes may ripple through outcomes later in life. Thus, if lead reduction improves a child’s reading ability
in early childhood, the SGM can be used to see how that improvement in reading leads, for instance, to greater
educational attainment and higher income later in life.
Because lead is not a variable included in the surveys that underpin the model’s dataset, the Urban Institute
and Child Trends had to estimate the blood lead levels for the children in the sample by using blood lead data
from the 2011-12 and 2013-14 NHANES to predict the age 1-5 blood lead level of each child. In other words,
they created in the dataset a cohort of children with blood lead levels consistent with those of the national child
population based on regression models of the logarithm of blood lead as a function of race, ethnicity, gender,
family income, maternal education, and maternal marital status, using children age 1-5 in the combined NHANES
samples. The average blood lead level in the combined two surveys for children ages 1-5 was 1.1 μg/dL, which
may be higher than what will be seen among the 2018 birth cohort. One option to address this possibility was to
extrapolate the trend line from earlier years to predict 2018 levels, but this strategy would underestimate 2018
levels if the rate of decline is slower between 2014 and 2018. Data from the CDC lead surveillance program
indicate that the number of children with blood lead above 10 μg/dL leveled o between 2009 and 2015.
209
The potential for similar settling at lower levels in subsequent years makes the 2011-14 NHANES data the most
accurate approach to predicting 2018 blood lead levels.

99
The modeling team assigned a blood lead value to every person in the SGM cohort to identify whether that
person was part of the target population for a policy intervention. This blood lead variable was not used in the
SGM regression equations to predict later life outcomes, so the results cannot be biased by misclassifying a
person’s blood lead level. The team modeled the policy eects by directly altering the values of the early and
middle childhood outcome scores (reading, math, and behavior) to the degree that the literature suggests given
the change in blood lead levels resulting from a given policy intervention. For example, if a child in the SGM has
a blood lead level of 1.5 μg/dL and is in the target population to receive a policy intervention that prevents a
50 percent increase in blood lead, his or her blood lead should be 0.75 μg/dL lower than without the intervention.
Using the expected reading score eect size, estimated from the literature, of a 0.0405 standard deviation
increase in reading score for every 1 μg/dL decrease in blood lead, this child’s reading score would improve by
0.0304 (i.e., 0.75 x 0.0405) standard deviations. This change in reading score, in turn, aects the person’s later
outcomes, such as high school graduation and family income at age 40.
The modeling team identified the eect of blood lead levels on variables in the model’s dataset that the literature
review indicated are aected by blood lead levels. The model contains the following outcomes for which Child
Trends and the Urban Institute gathered eect sizes for children ages 5 and 11 from the literature:
• Peabody Individual Achievement Test (PIAT) reading scores.
• PIAT math scores.
• Behavior Problems Index (BPI) hyperactivity subscale.
• BPI antisocial behavior subscale.
No studies estimated an association between blood lead levels and the specific variables in the SGM, so the
modeling team relied on estimates from other similar standardized reading and math assessments and on indices
of antisocial and hyperactive behavior. For reading and math scores, Child Trends used the median eect size for
all the included studies. For hyperactivity and antisocial behavior, most studies included multiple measures of
behavior, so the team first calculated a mean eect size for each study, then used the median value of the study
means. For example, if a study examined parent and teacher reports of hyperactivity on one scale, Child Trends
took the mean of those two measures and then used the median of those means across all the studies. Significant
and insignificant eect sizes were included in the calculations. A summary of the basis for the eect size
calculations is available upon request and includes a list of the research used as well as eect sizes and average
blood lead levels reported in each study.
Table A.4 provides the results of the SGM modeling of the prevention interventions: lead service line
replacements, lead paint hazard control, lead-safe renovation practices, and the elimination of leaded aviation
fuel. Although the dierences in outcomes for children with and without interventions appear small, it is
important to bear in mind that these are the changes for the entire population of children targeted for an
intervention (for example, all those who live in a house built before 1960), not just those who are at greatest risk
or have the highest blood lead levels. The eects for subpopulations with higher blood lead levels would be larger.
Additionally, improving outcomes such as high school graduation and the attainment of a college degree are
dicult to achieve with any one intervention since many factors play a role. Finally, the fact that blood lead levels
have declined rapidly as a result of the reduction of lead in the environment is evidence that policy interventions
make a dierence for the population—and the fact that disparities in exposure have shrunk over the last two
decades suggests that policies have been appropriately targeted. Intervening on lower levels of lead in blood
result in more modest improvements in later-in-life outcomes than in the recent past when blood lead levels were
much higher. But even modest outcomes when applied across a population of newborn children are meaningful,
both for individual children and for the entire cohort of school aged children.

100
Children living in pre-1978 homes
who experience a renovation,
repair, and painting (RRP) event
(N=211,167)
Lead paint hazard control (LHC)
for children living in pre-1960 low-
income housing (N=321,182)
Unsafe RRP Safe RRP
Children
benefiting
Without LHC With LHC
Children
benefiting
Outcomes at age 19
Average high school GPAs 2.86 2.87 N/A 2.79 2.80 N /A
Earn high school diplomas 81.6% 82.0% 900 72.1% 72.4% 1,000
Become teen parents 15.4% 15.2% 500 28.0% 28.0% 100
Be convicted of crimes 18.0% 17.7% 700 23.8% 23.6% 600
Outcomes at age 29
Complete 4-year degrees 23.5% 23.8% 800 15.0% 15.1% 400
Income
Mean family income at
age 40 (2015$)
$69,100 $70,000 N/A $58,300 $58,900 N /A
Estimated lifetime family income
(2015$)
$838,300 $848,700 N/A $701,300 $707,200 N/A
Notes: Analysis is based on the SGM’s sample of about 8,000 children drawn from the Children of the National Longitudinal Survey of
Youth dataset. To arrive at the number of children positively aected, the research team applied the percentage point dierences between the
baseline conditions and total prevention to the estimated number of children in the 2018 birth cohort who would receive the intervention.
Source: Social Genome Model analysis by Child Trends and the Urban Institute
© 2017 The Pew Charitable Trusts
Table A.4
Summary of Eects of Selected Lead-Exposure Prevention Policies
Impacts on education, income, teen parenthood, and crime

101
Full lead service line (LSL)
replacement for children living
in homes built before 1986 with
baseline water lead levels of 11.4
ppb (N=272,285)
Full lead service line replacement
for children living in homes built
before 1986 with baseline water
lead levels of 5 ppb (N=272,285)
Children ages 1-5 living within
0.6 miles of an airport serving
planes using leaded aviation gas
(N=226,530)
With an LSL
Without an
LSL
Children
benefiting
With an LSL
Without an
LSL
Children
benefiting
Without
removing
lead from
aviation gas
Removing
lead from
aviation gas
Children
benefiting
2.90 2.90 N/A 2.90 2.90 N/A 2.83 2.83 N /A
82.8% 82.9% 300 82.8% 82.9% 0 80.8% 80.9% 0
14.0% 13.9% 200 14.0% 13.9% 100 15.9% 15.9% 0
17.7% 17.6% 100 17.7% 17.7% 100 17.8% 17.8% 0
24.6% 24.8% 600 24.7% 24.8% 200 23.0% 23.0% 100
$70,700 $71,100 N /A $70,700 $70,800 N/A $67,500 $67,600 N /A
$855,400 $859,500 N/A $855,400 $857,000 N /A $823,700 $824,400 N /A

102
Value of Prevention Tool
Using data from the literature and national datasets, the Value of Prevention Tool predicts the financial and health
eects of investments in social determinants of health, such as access to early education. The tool can assess the
potential cost and future savings associated with various policies that would accrue to the federal government,
states, and society at large based on the intervention’s predicted impact on mortality, morbidity, future earnings
and health care and incarceration costs, and noneconomic impacts such as educational attainment.
The tool tracks impacts on the federal government, specifically those related to spending on Medicaid, CHIP,
Medicare, and other medical costs, such as exchange subsidies and care for veterans and military families;
safety net expenditures; Social Security spending; incarceration costs; and tax revenue. State eects may
include Medicaid and other medical spending, safety net expenditures, and incarceration costs. The tool also
tracks impacts on the federal, state, and local governments in the form of changes in tax receipts resulting from
dierences in lifetime earnings.
The tool provides an assessment of the QALYs that could be gained by the aected population as well as the
predicted impact of each intervention on health-adjusted life expectancy, both of which account for the amount
of time lived in less than perfect health. QALYs are the number of additional healthy years of life resulting
from an intervention measured on a scale of 0 to 1, where 0 and 1 correspond to the worst and best possible
health outcomes.
For this project, Altarum used the tool to estimate the benefits of policies that reduce exposure to lead for an
annual cohort of children (about four million births) over their lifetimes. These benefits consist of increased
lifetime earnings, reduced health expenditures, decreased education spending, and a lower risk of mortality;
are measured in 2015 constant dollars; and are discounted at 3 percent. When cost estimates of a policy were
available, the tool reported the cost-benefit ratio of an investment.
Reductions in incarceration costs were estimated but not depicted in the tables because they were very
small compared with the other outcomes measured. The benefits of decreased incarceration are based on a
longitudinal study that linked blood lead levels to arrest rates. However, that study only documented eects
for blood lead above 6 μg/dL,
210
a level that few children experience today, so the predicted benefits associated
with reduced criminal involvement are relatively small. The Value of Prevention Tool is designed to measure
incarceration costs so the team converted arrests to incarceration using FBI data to predict both the probability
and length of incarceration given an arrest for a nonviolent and violent crime. The model did not account for other
potential criminal justice-related cost reductions, such as those associated with arrests.
Importantly, the costs and benefits Altarum calculated are for a single annual cohort of children. Many of these
policies could and probably would be implemented over a longer period, but the results are reported only for a
single cohort to ensure consistency across policies and so readers can compare these simulations to previous
work.
211
Further, estimating benefits beyond the first cohort introduces greater uncertainty because it requires the
prediction of cohorts’ blood lead levels and other characteristics further into the future. The tool models lifetime
earnings benefits by estimating changes in IQ from lead exposure and their downstream impact on earnings
potential, health savings by approximating lead exposure’s short-term health costs (testing, oce and emergency
room visits) and long-term impacts (increased risk of cardiovascular disease, hypertension, and associated
costs), and education savings by estimating the decreased need for special education and repeated grades
associated with avoided IQ losses.

103
The QALY benefits are estimated through reductions in mortality risk associated with lifetime cardiovascular
disease, which puts a dollar value on increased healthy years of life and is included in many regulatory analyses of
environmental hazards. In this report the value of a gained QALY unit is $50,000, a conservative estimate when
compared with similar analyses.
212
The team’s estimates were restricted to benefits associated with reduced
cardiovascular disease because it is the only increased risk of mortality shown to occur down to blood lead levels
of zero, an important consideration given the lower levels of lead in children’s blood today.
The tool modeled the impacts of lead paint hazard control and lead service line replacement in homes for the
estimated 3,978,038 children who will be born in 2018. However, lead paint hazard control has been shown to
make changes in home dust lead levels that persist for at least 12 years, and lead service line replacement should
make permanent improvements to home water lead levels. Therefore, future children born into remediated
homes would see benefits. The modeling team approximated the number of such children using data on the
housing stock and the size of future birth cohorts from the American Community Survey. This analysis showed
that in the next 10 years, about 0.25 future children on average will be born into an already remediated home.
When possible, conservative assumptions were used and only some benefits were included as quantifiable in
the Value of Prevention Tool results. Therefore, interventions with a positive cost-benefit ratio have a beneficial
impact, but may have even greater positive eects not included in the results.
The tool tracks and distinguishes among benefits that accrue to dierent stakeholders, including the federal
government, state and local governments, and the remainder of society, including households and businesses.
Therefore, the future benefits reported are societal and include discounted benefits to all entities, not a particular
stakeholder or investor. When possible, Altarum breaks out individual benefits by the level of government to
which they would accrue. Many of these benefits occur far in the future, so the results are highly sensitive to the
3 percent discount rate and 1 percent real-earnings growth assumptions.
213
Altarum models evaluated changes in health care costs in two pieces. The first is short-term costs associated
with increased use of medical services, such as lead testing, oce visits, environmental investigations, and
chelation therapies. The medical procedures recommended for various blood lead levels were taken from the
American Academy of Pediatrics recommendations for children above the 5 μg/dL cuto,
214
which, in turn, were
revised from the previous guidance which recommended care beginning at 10 μg/dL.
215
Cost estimates for
medical procedures were derived from Gould’s 2009 study and inflated to 2015 dollars using Altarum’s health
care prices index.
216
The second piece of health outcomes are long-term risks associated with lead exposure, which has a large
research base. In addition to the cognitive impacts discussed above, evidence has found harmful eects of lead
exposure on hypertension; cardiovascular, immunological, and endocrine health; child growth rates; and hearing.
However, much of this research has been done in children and adults at blood lead levels much higher than
5 μg/dL, and the strongest evidence of impacts on individuals with levels at or below 5 μg/dL is for hypertension
and cardiovascular disease. The model, therefore, included only increased mortality risk and long-term health
care expenditures associated with cardiovascular disease and hypertension.
Further, to simplify the process of estimating long-term health impacts of childhood exposure and avoid the need
for engineering models to approximate changes in blood and bone lead over time, the analysis assumes that
children’s blood lead levels persist throughout their lives. This approach is reasonable because, although blood
lead levels are likely to fluctuate during a lifetime as a result of changing exposures, childhood levels are one of
the best predictors of lifetime average blood lead levels, particularly given the relationships between blood lead
and lead stored in bones.

104
The first long-term health outcome measured was increased mortality risk through likelihood of fatal
cardiovascular disease. Initial, nonexposed mortality risks were drawn from the Underlying Cause of Death data
from the CDC.
217
The model then used research on hazard ratios to represent the increased mortality risk.
218
To
calculate increased mortality rates, the team identified cardiovascular and noncardiovascular mortality from the
CDC Underlying Cause of Death data and then used a linearized hazard ratio to find the increased annual risk of
cardiovascular mortality associated with a 1 μg/dL increase in blood lead.
219
Additionally, for hypertension the model uses American Heart Association data from 2015 on hypertension
risks for baseline nonexposed risks,
220
and then other published data to calculate the increased risk of
hypertension associated with a 1 μg/dL increase in blood lead.
221
The higher prevalence of hypertension is then
used as a predictor for increased cardiovascular and health care costs through published data showing that
people with hypertension spend $5,755 in 2007 dollars more on average each year for medical expenditures.
222
Altarum then inflated these costs to 2015 dollars using its health care prices index and aggregated to produce
the cohort-level estimates.
IQ
The eect size of early childhood blood lead levels on IQ has been well studied, although researchers have
produced a wide range of estimates. The emphasis for this analysis was on the IQ impacts for young children with
blood lead levels less than 10 μg/dL because this is the range for most U.S. children. Strong evidence in the recent
literature suggests that the relative impacts of blood lead on IQ are much larger at lower levels.
223
Therefore, the
team estimated the impact of lead on IQ for three separate categories: children in the <5 μg/dL range, the
5-9.9 μg/dL range, and the 10+ μg/dL range.
The team identified four distinct studies of IQ in U.S.-based cohorts of young children with blood lead levels
in the <5μg/dL range
224
and standardized their estimated impacts to a 1 μg/dL increase in blood lead, measured
in IQ points.
When studies produced multiple estimates from subsamples of dierent blood lead level ranges, the research
team included all those estimates. The IQ estimates for the <5 μg/dL group ranged from a 0.19 to 2.53 decrease
in IQ points per 1 μg/dL increase in blood lead depending on study and methodology. Of the five estimates
included, the median result for the <5 μg/dL category was 0.77 IQ points lost per 1 μg/dL of additional blood lead
and the mean was 1.15 points. Altarum used the mean result of -1.15 in IQ per 1 μg/dL increase in blood level for
the <5 μg/dL analysis. The estimate is slightly more conservative than the eect size used by the EPA in its 2008
NAAQS final rule, which was based on four studies with a median result of -1.75,
225
but is slightly more aggressive
than the -0.83 estimate found by the European Food Safety Authority in its literature review.
226
For the 5-10 μg/
dL category, the mean result was 0.51 IQ points lost, and for the 10+ μg/dL category, the mean result was 0.18
points. A summary of the basis for the eect size calculations is available upon request and includes a list of the
research used as well as eect sizes and average blood lead levels reported in each study.
Lifetime earnings
The team used a similar methodology to determine the eect of IQ changes on lifetime earnings. The team
performed a literature search of relevant studies and supplemented the results using a survey article
227
because
the universe of available data on lifetime earnings is smaller than the data on IQ and blood lead levels. The team
found no literature directly connecting blood lead levels to lifetime earnings and therefore employed a two-step
approach commonly used in the field, first linking blood lead levels to IQ as described above and then linking
IQ to earnings.

105
Altarum further restricted the estimates of IQ eects on earnings to studies that analyzed males and females
together because the evidence suggests that IQ impacts on earnings for women are larger than those for men,
so studies that only report the eect size for males would underestimate the total. Additionally, Altarum
focused on studies that included in lifetime earnings not only hourly or annual wages but also likelihood of
labor force participation, because studies that consider just wage eects underestimate the impact of IQ on
lifetime earnings.
In addition, the team excluded studies that analyzed the impacts of IQ on lifetime earnings while controlling for
educational attainment because increased education is a probable pathway through which higher IQ increases
earnings, and controlling for education creates a “blocking variable” that results in an underestimate of the
impact of IQ on earnings.
228
Further, some studies attempted to approximate the lifetime value of blood lead
reduction through willingness-to-pay analyses for certain lead remediation and treatment,
229
but Altarum
deemed them inappropriate and excluded them because of the probable information asymmetries related to
the eectiveness of lead-related treatment.
The result of the above work is three estimates. Two focus on the NLSY79 cohort and a third incorporates
some evidence from literature that drew on the NLSY’s 1997 cohort, a nationally representative sample of
approximately 9,000 youths who were 12 to 16 years old as of Dec. 31, 1996. One finds an overall impact of a
single IQ point on lifetime earnings of 1.43 percent in the NLSY79 sample and similar eects in the NLSY97
data. The second estimates an earnings impact of 2.56 percent, and the third estimates a 2.82 percent eect.
230
Taking the mean of these three estimates, Altarum used an eect size of a 2.27 percent increase in earnings per
IQ point for this analysis.
Some researchers in this field view these estimates of IQ impacts on earnings as aggressive because of the
inability to control for other noncognitive variables, such as self-control and conscientiousness.
231
Others suppose
that 1.1 percent may be more appropriate, but the team found only one study that included noncognitive controls
in a lifetime earnings regression analysis.
232
Furthermore, because the Value of Prevention Tool does not include
noncognitive eects, the estimated eect size of 2.27 percent best aligns with the data incorporated into the tool.
Economic benefits
The quantifiable benefits of reducing child lead exposure are dominated by the expected increases in future
lifetime incomes as a result of improved cognitive and noncognitive ability, increased educational attainment,
and greater labor force participation. However, the Value of Prevention Tool also includes benefits associated
with reductions in special education and lifetime health spending and increases in expected lifespans as a result
of lower blood lead levels. Although the Value of Prevention and Social Genome models are structured dierently
and draw on dierent types of information, when considering a common outcome, such as the discounted
present value of lifetime income, they would reach conclusions within the same order of magnitude.
Education
Education impacts are estimated through expected changes in IQ as described above. Previous lead modeling
literature approximated the additional educational costs associated with children with blood lead levels above
20 μg/dL. One study estimated that 20 percent of those children would require an additional three years of
special education.
233
Altarum instead modeled possible increases in special education spending for all children
exposed to lead. This was done by approximating the number of children whose IQs would decline below the
70 point threshold as a result of lead exposure and assuming that all those children would require special
education interventions. The analysis also assumed a standard normal IQ distribution and used the IQ-to-blood

106
lead level eect sizes described above to estimate the number of children aected. For example, children in the
5 to 10 μg/dL blood lead category were predicted to lose 6.2 IQ pts as a result of their full lead exposure, so the
model estimated that any child within this blood lead level range and the post-intervention distribution between
76 and 70 IQ points (3.6 percent of children) would fall below the 70 point threshold absent elimination of blood
lead and would require additional special education. The analysis then assumed that special education spending
for these children would persist throughout their primary school years.
The expected additional cost of a year of special education was estimated for the 1999-2000 school year to
be $8,040 per student.
234
This number was inflated using the CPI to 2015 dollars. Total educational spending
was estimated by multiplying the number of aected children by the per-year per-student cost and then by the
number of primary education years.
Assumptions for modeled policies
Lead service line replacement
• Because of a lack of data for most of the inputs, the models had to rely on a range of available information
sources. For the number of LSLs in the country, this analysis relied in part on self-reported survey data
collected from water utilities and on input from industry representatives.
235
No data source was found that
could document how many children are served by those lines or their blood lead levels. The team used a
2016 study to estimate that 6.84 percent of the population is served by a lead service line and then applied
that percentage to the roughly 4 million children in the 2018 cohort to determine the number of children who
would be served by a lead service line (272,285).
236
• Limited data connect lead levels in water to blood lead levels in children so the research team assumed that
replacing an LSL prevents a 0.40 μg/dL increase in blood lead. This estimate is derived from proposed IEUBK
model coecients.
237
An alternative to the IEUBK estimate would have been to use findings from one study
that found a 20 percent reduction in blood lead levels for children exposed to less than 5 ppb of lead in water
compared with those exposed to greater than 5 ppb.
238
However, that report used data from a 2005 pooled
analysis, which drew water samples in such a way that they may not have accurately depicted the exposure
risk. Alternatively, a Canadian study showed a 35 percent decrease in blood lead for every 1 ppb decline
in water lead levels.
239
Assuming that LSL replacement reduces water lead levels from 11.4 to 2.0 ppb, the
Canadian findings suggest a resulting 98 percent decrease in blood lead levels, which seems implausible
given that children are also at risk from other sources of exposure. Ultimately, the research team used recently
proposed parameters for the IEUBK model that suggest a 0.5 μg/dL change in mean blood lead level is caused
by a 11.8 ppb increase in water lead. The team converted this to a 0.04 μg/dL increase in blood lead for every 1
ppb increase in water lead.
240
• In the absence of national data to characterize the level of lead in drinking water in homes served by LSLs, the
research team used two water lead levels for reference: 11.4 ppb lead based on unpublished sampling data
from five utilities in the Midwest and 5 ppb from unpublished Canadian data.
241
These levels were selected to
represent a system in compliance with the Lead and Copper Rule, and to reflect the upper bound amount of
lead in water for a system using optimized corrosion control, respectively.
• About 59 percent of the U.S. population lives in pre-1986 homes according to the American Community
Survey, so this analysis assumed the same percentage for the approximately 4 million children in the 2018
birth cohort to arrive at 2,351,498 children residing in homes built before 1986.

107
• The team assumed that children served by LSLs would have starting blood lead levels similar to the average
across children living in all homes built before 1990, specifically 1.16 μg/dL, with 9.2 percent of the cohort
having levels of at least 2 μg/dL.
• The team assumed that replacing the LSL in one home would aect one child in the initial cohort (i.e., that one
child, rather than multiple children, per cohort will be born into each home).
• The number of children born into homes with replaced LSLs in the next 10 years was estimated separately
from the initial cohort. First the percent of the housing stock that each intervention would remediate was
calculated by dividing the number of remediated homes by the total housing stock using data from the
American Community Survey.
242
This percentage was then used as the likelihood a future child will be born
into a remediated home. For example, in the LSL replacement intervention for pre-1986 housing, an estimated
0.3 percent of the housing stock would be remediated. Therefore each future child has a 0.3 percent chance
of living in a remediated home. This is likely a conservative estimate because it assumes births are evenly
distributed across the housing stock and ignores that children cluster in families and certain styles of homes.
The team also conservatively assumed that the impacts would persist for only the next 10 birth cohorts.
• In the absence of national pricing data for full LSL replacement, the research team estimated a per-unit cost of
$6,000. A 2008 national survey of utilities found that typical replacement costs ranged widely from $250 for
the utility portion and $600 for the customer portion to $3,000 and $4,000, respectively.
243
A recent informal
survey of all systems known to be pursuing full LSL replacement suggested that current costs averaged roughly
$7,500. The real cost varies greatly across regions, states, and even local providers and by the length of the
line, so the research team combined these estimates to calculate a rough $6,000 per unit cost.
244
Lead paint hazard control
• Using published literature on the eects of lead paint hazard control on dust lead levels and studies of the
relationship between levels in dust and those in blood, the team assumed that removing lead paint hazards
from homes before children are born would cut their expected blood lead levels by 39.5 percent. This involved
a two-step process. First, the team used data from a long-term follow up of lead hazard control interventions,
which found an 89 percent decline in dust lead levels 12 years after treatment.
245
The study was conducted in
189 nonrandomly selected homes from multiple regions of the country and did not include a control group for
ethical reasons. It is, nevertheless, the largest national evaluation of lead hazard control eorts and its findings
align with many smaller studies of lead paint hazard control eects.
246
• Second, the team used a an analysis of a national cross-sectional survey to predict the eect of decreased
dust lead on child blood lead levels.
247
The study was based on blood lead levels from 1999 to 2004.
(See “Uncertainty in modeling lead impacts and remediation policies” below.) The data indicated that the
above-referenced 89 percent reduction in dust lead would prevent a 39.5 percent increase in children’s
blood lead levels.
• The team provided an alternative baseline of 10 μg/sq. ft. to illustrate the benefits of the intervention at lower
floor dust lead levels.
• The analysis used the American Healthy Homes Survey to estimate that about 75 percent of pre-1960 homes
and 50 percent of pre-1978 homes have lead-based paint and would require remediation.
248
• The team calculated children’s baseline blood lead levels based on NHANES data from 2011-14.

108
• The benefits include one child per home from the 2018 birth cohort as well as additional children likely
to be born into the remediated homes in the subsequent 10 years. To calculate the number of children
born into a remediated home the team used the same methodology described under “Lead service line
replacement” above.
Renovation, repair, and painting
• The team consulted an EPA study which used the Leggett model to determine that following lead-safe
renovation practices would prevent a 1.08 μg/dL increase in blood lead levels of children and then used that
estimate to model the impact of compliance with the renovation rule enforcement on a single birth cohort,
in terms of lifetime earnings, health and education expenditures, and QALYs.
249
The Leggett model enables
estimates of blood lead levels and the probability of a child's concentration exceeding levels of concern based
on dierent exposure scenarios.
• Although the EPA does not require clearance dust testing following renovations, these tests were included in
this study’s cost calculations because they are necessary to confirm the safety of a home or child care facility
before children are allowed to re-enter.
• The team included the annual cost of compliance for all homes and child care facilities built before 1978 so
that it could use cost information from the EPA’s regulatory impact assessment. However, to be consistent
with all of the interventions modeled in this report, the team only counted benefits for children from the 2018
cohort living in those homes or visiting those facilities. As discussed, some limited benefits would also accrue
to homes without children, but those impacts were excluded from the modeling.
Aviation gas
• The team used published research to determine that children living closer than 0.6 miles from airports using
leaded gas have blood lead levels that are 5.7 percent higher than those living further away.
250
• The team used EPA’s estimated number of people living within 0.6 miles from airports serving piston engine
aircraft and assumed based on the NHANES 2011-14 blood lead distribution that the children living within that
proximity had baseline blood lead levels similar to the national average.
• Other researchers have found larger benefits than those shown in this report or studied the eects of aviation
emissions to the population of children living farther (up to 2.5 miles) from an airport serving piston engine
aircraft.
251
However, the research team found no published data on the number of such children nationwide
and so only modeled the distance for which data were available: 0.6 miles.
Early and middle childhood education and care
To estimate the potential impact of early and middle childhood care and education interventions on children
who have high blood lead levels, Child Trends identified evidence-based interventions and determined their eect
size on outcomes for children with other disadvantages, such as poverty and trauma, in the SGM, specifically,
reading and math scores, antisocial behavior, and hyperactivity, which are all areas of potential deficit in lead-
exposed children. Child Trends evaluated the early childhood literature to identify specific programs that have
been rigorously evaluated and demonstrated to improve outcomes for children at risk for or displaying cognitive
and behavioral deficits. Programs selected for the modeling eort have been the subject of previous meta-
analyses (reviews that compared multiple studies to determine typical eects), randomized controlled trials,
and quasi-experimental evaluations. In addition, research shows that addressing such disadvantages has strong
economic benefits, which are not included in this analysis.
252

109
To develop the list of programs to be considered, Child Trends reviewed high-quality interventions recommended
by subject matter experts, meta-analyses, and the following additional resources:
• Blueprints for Healthy Youth Development’s compendium of evidence-based program evaluations of
interventions for children and youth.
253
• The Nurture Eect: How the Science of Human Behavior Can Improve Our Lives and Our World. Oakland, CA:
New Harbinger.
254
• Child Trends’ LINKS Compendium of random assignment intent-to-treat evaluations of social interventions
for children.
255
• Early Childhood Roots of Bullying: Early Childhood Investigations Webinar. Child Trends.
256
To be included, interventions must have been subject to a randomized evaluation and an intent-to-treat analysis.
In addition, the program had to have served children in either early or middle childhood and reported on one or
more outcome categories included in the SGM, academic, behavioral, or both.
To determine the eect size of the interventions on academic and behavioral outcomes, Child Trends initially
categorized programs into either early childhood (0-5 years old) or middle childhood (6-11 years old). Because
some were implemented over a period of time, which resulted in data being collected in waves, Child Trends
only included the final outcome measures for those interventions. In cases when a program evaluation measured
multiple aspects of a behavioral or academic outcome, Child Trends calculated the mean eect size for each
outcome in that evaluation. Finally, to determine the overall eect size of early childhood and middle childhood
interventions, the research team used the median value across all of the program evaluations for reading,
math, and behavior, including significant and insignificant findings. A summary of the basis for the eect size
calculations is available upon request and includes a list of the research used as well as eect sizes and average
blood lead levels reported in each study.
Uncertainty in modeling lead impacts and remediation policies
Modeling the long-term impacts, costs, and benefits of early childhood focused lead remediation and prevention
policies is complex and involves high levels of uncertainty. Given available data, an analysis cannot generate
wholly accurate estimates of the eects of specific policies in reducing future blood lead levels in children and
mitigating the various eects of lead exposure, but rather is most useful to provide more insight into which
policies would most likely be eective and cost-beneficial and how policies might best be structured to help
ensure their usefulness. The long-term nature of the harms resulting from lead exposure and data limitations
in quantifying these harms necessitates a multistage modeling process that can compound the eects of
uncertainties from dierent sources.
Strong evidence indicates that early childhood lead exposure is statistically correlated with intermediate
outcomes, such as IQ, reading, math, and behavior, and that they, in turn, are statistically related to lifetime
outcomes, particularly earnings and educational attainment.
However, the modeling team has found neither data that directly links primary prevention interventions or blood
lead exposure to lifetime earnings outcomes nor studies designed to prove causality in an early childhood lead
exposure and earnings relationship. Therefore, for this project the modeling team used studies that measured
the impact of lead exposure on IQ (Value of Prevention Tool) and reading scores, math scores, and behavioral
outcomes (Social Genome Model) as intermediate outcomes to predict lifetime outcomes. As a result, defining
traditional statistical levels of uncertainty or “confidence intervals” in the results is not possible. Statistical

110
measurements of uncertainty are driven by standard errors and are designed to measure the relationship of
multiple variables taken from data analyzing a single sample of participants.
As a substitute, the modeling team performed three separate analyses to address concerns about the uncertainty
of the estimates of the lifetime benefits of reducing childhood lead exposure via policy interventions. The first
was a qualitative exploration and the second was a set of “bounding exercises” to frame possible upper and
lower limits on the impact of certain model results. Assuming appropriate data were used in other modeling
steps, these exercises show the maximum possible benefit (the prevention of any lead exposure, and therefore
the complete elimination of lead in children’s blood) that might be achieved through various policy interventions.
Finally, the modeling team used the VP Tool to perform sensitivity analyses on key areas of uncertainty.
Sensitivity analyses do not estimate statistical uncertainty, but they do provide descriptive, quantitative evidence
on how the dependent outcomes of a modeling process change depending on the inputs. The analyses chosen to
run were prioritized because either the parameter values were believed to be particularly uncertain (e.g., there are
a wide range of values in the literature) or parameter values for which even small changes in input values result in
large changes in the final results.
Qualitative description of uncertainty
The estimation of lifetime benefits of lead abatement policies is a multistage process, with uncertainties at each
step. To address these, the team developed a brief qualitative description of the modeling details relevant to each
step and of how each eect size might be larger or smaller in the real world.
Step 1: Impact of a policy intervention on lead in the environment and in children’s blood
The ability to quantify the magnitude of the eect of intervention policies on environmental and childhood blood
lead levels varies depending on the data available for each intervention. Whenever possible, the modeling team
used real-world risk and eect-size data from controlled evaluations of lead interventions; other types of studies
were also employed as needed. In some cases, no one clear eect size was evident, and the modeling team relied
on subject matter experts’ guidance to select an input for the model.
For example, for the first intervention examined, the replacement of residential LSLs, as discussed previously,
because of a lack of data the modeling team estimated water lead levels before and after a lead service line
replacement intervention. To address the uncertainty, the team modeled two starting water levels: 11.4 μg /dL
and 5 μg/dL.
The second intervention, residential lead hazard control, has been more extensively studied, and the data have
shown robust eects over long periods. The study used in this analysis to generate the eect size for lead paint
hazard control was conducted between 2008 and 2009.
257
If lead hazard control abatement and interim control
techniques and standards have improved since then, the data may underestimate the impact of lead hazard
control implemented today. Whether dust lead levels are higher or lower than those in the underlying study
is unknown, and as pre-1960 housing continues to age, dust lead levels attributed to deteriorated paint may
increase. The modeling team presented two baseline floor dust lead scenarios to examine the impact of varying
dust lead levels on the predicted benefits.
Modeling lead paint hazard control required a second step of predicting the eect of lower dust lead levels on
childhood blood lead. The modeling team considered a mix of evidence for this eect size. Although the range
was much tighter than the lead service line eect sizes, the team similarly relied on bounding assumptions

111
that the intervention could prevent some but not all lead exposure. However, whether the assumed eect size
accurately states, overstates, or understates the impact is unclear.
As with lead service line replacement, the third intervention, improved renovation and repair standards, has
a limited evidence base regarding impact. Some previous work explored the eect of a renovation on raising
child blood lead levels when compared to no renovation, but the modeling team could not find any analyses
that specifically compared the eects of safe versus unsafe practices on blood lead levels. However, one study
looked at the impact of following the EPA rule requirements on dust lead levels,
258
and strong anecdotal evidence
and expert opinion indicate that renovations pose some of the most acute risks because they disturb and
spread lead dust.
As a result, the modeling team relied heavily on previous work by the EPA for this intervention. Because this
model is looking at the prevention of a spike in blood lead levels, it is not as well bounded as the previous
interventions. Additionally, renovation activities are likely to cause short-term spikes in blood lead rather than
prolonged exposure as from lead in soil or water, and because the comparative eects of short- vs. long-term
exposure are not well studied, the model may overstate the impacts of the improved standards.
The final intervention, removal of lead from aviation gas, was modeled dierently. No data are available on the
prohibition of leaded aviation fuel because it has not been done. So the modeling team attempted to estimate the
eect of childhood exposure to aviation gas through the dierential of blood lead between children living near
airports (within 0.6 miles) compared with those living farther away (more than 2.5 miles). Then, using that figure,
the modeling team was able to predict the amount of blood lead that might be prevented by eliminating leaded
aviation gas. This approach may understate the impacts because it assumes that children living more than
2.5 miles from an airport are not exposed to lead from aviation emissions, which is probably untrue and leads
to a conservative estimate.
Step 2: Impact of childhood blood lead levels on intermediate outcomes
After predicting the impact on childhood blood lead levels of the four policy interventions, the modeling team
used a more comprehensive set of literature to estimate the impact on intermediate childhood outcomes. These
analyses primarily rely on regression modeling, which derives the relationship between blood lead levels and
childhood IQ, reading, math, and behavioral outcomes from data for a sample of children. These regression-based
approaches bring specific uncertainties into the modeling process. First, they are not designed to demonstrate
causal links between exposure and outcomes—that is, they are not random-assignment studies—which could
result in eect sizes that overstate the relationship. Because these are not random-assignment studies, they
instead must use control variables to account for other characteristics, such as socioeconomic status, related to
lead exposure and outcomes. These models could be missing key variables, which could also result in overstated
eect sizes. Alternatively, these models might over-control for certain variables and therefore understate the
relationship between lead and later outcomes.
Extrapolating results from this literature also includes some level of uncertainty. These studies may include
sampling errors, although many, such as those that explore the relationship between blood lead and reading
and math scores, have large sample sizes and probably low error levels. Nevertheless, sampling errors could
understate or overstate the true impacts. More concerning is the ability to apply the findings to children with very
low blood lead levels because most of these studies do not address that population and instead looked at children
with levels between 2 and 10 μg/dL. However, the majority of children today in the U.S. fall well below these
levels. The modeling team therefore extrapolated results for blood lead levels greater than 2 μg/dL to children

112
below that level and assumed linear relationships, which may over- or understate the eect sizes at lower levels.
If lead exposure below a certain threshold does no biological harm, then the linear extrapolations would overstate
the true relationship, but if, as suggested by some experts, a supralinear relationship continues at very low levels,
this analysis could be understating the eect. (Note that the VP tool used dierent eect sizes for blood lead
levels below 5 μg/dl, 5-10 μg/dl, and above 10 μg/dl to reflect the nonlinear relationship found in the literature).
Finally, uncertainty persists about the cumulative impacts of lead exposure, and the studies used for this analysis,
which look only at point-in-time relationships, may understate the true relationship between blood lead and IQ,
reading, math, and behavioral outcomes.
Step 3: Eect of intermediate outcomes on lifetime outcomes
Similar to the above steps connecting blood lead levels to intermediate outcomes, the relationships between
those intermediate outcomes and lifetime earnings and educational attainment are based on previous regression
models and literature. The SGM’s and VP Tool’s approaches to estimating earnings diverge somewhat in this
step, with the former relying on its well-tested and established microsimulation model, and the latter using
previous literature on the relationship between IQ and lifetime earnings.
The SGM is a regression-based model which raises concerns similar to those outlined in Step 2 above, in that it
might overstate the relationship if it misses important control variables or because it cannot show a causal link
between the regression-generated results. Additionally, the SGM process does not produce a direct calculation of
standard errors; hence, it does not provide a range around the estimated eects into which the true eect will fall.
Nevertheless, the eects shown represent the model’s best estimates.
The final uncertainty concern in the SGM results from the use of data on past children to predict eects for
future children. The cohorts from which the samples were drawn entered adulthood as long ago as the early
1980s and grew up with much higher levels of childhood lead exposure than exist today, which could be reflected
in their outcome measures. Therefore, applying their childhood and adult experiences to children born in 2018
and later could cause the modeling to understate or overstate the relationship between intermediate and lifetime
outcomes, but given the increasing importance of cognitive skills for life success, they are more likely
to understate the eect sizes.
In contrast, the VP Tool uses academic literature to connect intermediate childhood IQ to lifetime earnings.
The greatest amount of uncertainty in this relationship involves IQ measurements collected at dierent points in
time. In particular, the IQ that is connected to childhood blood lead comes from tests of children at younger ages
(5-10), but the IQ measurements used to estimate impacts on lifetime earnings are from older children (around
age 18). If childhood IQ is not perfectly predictive of adolescent IQ, this process may understate or overstate the
eect of childhood blood lead on lifetime earnings. Further, these relationships are estimated through regression
models, which are subject to the same concerns listed above regarding the use of regression in the SGM process,
except for those related to older samples and to direct standard error calculations.
Bounding exercises to measure uncertainty in eect sizes
A useful process to measure and constrain uncertainty in the estimation of eect sizes is to run the models
assuming a complete elimination of blood lead. Although this process still contains uncertainty surrounding
the blood lead-to-lifetime outcome eect sizes described in Steps 2 and 3 above, it provides a useful upper
bound on the potential impacts of a given policy. In this analysis, the modeling teams ran the models measuring
the impacts of preventing blood lead levels from rising above 0 μg/dL. Although this is an impossible real-life
scenario, it represents a maximum bound on achievable benefits for all policies.

113
The results of the bounding runs are available in Tables 1 and 2 of the report.
Quantitative sensitivity analyses
To address uncertainties that could not be tested in the bounding exercises, particularly those described in Steps
2 and 3 above, the modeling team performed quantitative sensitivity analyses using the VP Tool on the “Prevent
all Lead Exposure” hypothetical modeling scenario. (See Table 1.) These analyses help to better understand and
describe the sensitivity of the findings to changes in the input assumptions, coecients, and data points.
Inputs and coecients were selected for sensitivity analyses based on their likelihood of having substantial
impacts on the final results or if the published values in the literature varied substantially. Alternative values
for each coecient were chosen through literature reviews and typically had been used in previous analyses by
other authors. Details on how each alternative value was selected can be found below in the detailed discussion
of each result.
Although the sensitivity analyses were run on the hypothetical “total prevention” scenario, the results are
relevant to all four interventions modeled in the report. In general, the relative change in benefits would be similar
in the other modeling results. For example, an alternative input that reduced the total benefits in this sensitivity
analysis by 50 percent would probably have close to the same eect on any of the four policy cost-benefit
analyses. (See Table A.5.)

114
Total discounted
benefits
Benefit per child
Results using original inputs $84 billion $21,000
Input tested Original value Alternative value
Alternative total
discounted benefits
Alternative benefit
per child
Blood lead level (BLL)
to IQ eect size
(<5 μg/dL)
1.15 2.53 $174 billion $44,000
BLL to IQ eect size
(<5 μg/dL)
1.15 0.51 $42 billion $11,000
IQ to lifetime earnings
eect size
2.27% 1.10% $45 billion $11,000
Population BLL
distribution
1.11 0.95 $74 billion $16,000
Real wage growth 1% 0% $57 billion $14,000
Gross domestic
product multiplier
1.00 1.92 $155 billion $39,000
Valuation of QALYs $50k $0k $81 billion $20,000
Discount rates 3%
1% $208 billion $52,000
5% $38 billion $9,000
7% $19 billion $5,000
© 2017 The Pew Charitable Trusts
Table A.5
Value of Prevention Tool Sensitivity Analysis Results

115
Blood lead level-to-IQ eect size
The modeling team reviewed the available research to ensure that its estimates of the eect size on IQ of
lead in blood were appropriate. The literature included several prospective and cross-sectional epidemiologic
studies conducted in diverse populations with adjustment for socioeconomic variables as well as parental
intelligence, education, and caregiving quality and stimulation. The studies provide strong support of the loss of
neurocognition among young children with blood lead concentrations.
259
The research literature also included
a pooled analysis of children ages 4.8-10 who participated in seven prospective studies conducted in Boston,
Cincinnati, Cleveland, and Rochester, New York, in the U.S. as well as Mexico City; Port Pirie, Australia; and
Kosovo, Yugoslavia, which found associations between blood lead levels and deficits in full-scale intelligence
quotient (FSIQ), infant mental development, memory, learning, and executive function in children ages 2-17 with
mean blood levels (measured at various life stages and time periods) of 5 to 10 μg/dL. As discussed above,
when using this pooled analysis only study estimates of children with the lowest peak blood lead (<7.5 μg/dL
and <10 μg/dL) were included for the <5μg/dL eect size. The range of concurrent blood lead levels from these
categories was 0.9 to 7.4 μg/dL and 0.1 to 9.8 μg/dL.
The team was particularly interested in whether the relationship between blood lead and IQ persisted at blood
levels less than 5 μg/dL. Although few studies extend this relationship below 2 μg/dL, several found IQ deficits in
children ages 2-10 with lower mean blood lead levels of 3 to 5 μg/dL.
260
Specifically, in analyses of the Boston and
Rochester cohorts and of data pooled across all seven cohorts but restricted to children in the lower blood lead
range (e.g., up to 10 μg/dL), associations were observed in children with mean levels of 3 to 4 μg/dL.
261
The mean
blood lead levels in these subsets of children were 3.3 μg/dL (Rochester) and 3.8 μg/dL (Boston), which are
closer to those of current U.S. children compared with other prospective studies. Further, the Rochester cohort
study considered the eects of several variables, including gender, family income, maternal education, race,
prenatal maternal smoking, birth weight, and maternal IQ.
262
The modeling team, with input from members of the advisory committee, made separate estimates for the blood
lead-to-IQ eect size depending on starting blood level (<5 μg/dL, 5-10 μg/dL, and 10+ μg/dL), as described
above. The estimate for levels below 5 μg/dL had by far the greatest impact on the final results because based on
data from NHANES 2011-14, more than 90 percent of children in the U.S. fall into this group.
For the <5 μg/dL category, five estimates from the literature produced an average eect size of 1.15 IQ points per
1 μg/dL blood lead, which was used in the original analyses for this report. This result is somewhat smaller than
previous EPA estimates used in regulatory studies (1.75 in the NAAQS final rule and 2.94 in the 2015 cost-benefit
analysis on the Steam Electric Power Standards) but somewhat larger than the 0.51 coecient used in previous
research.
263
The 2.94 and 0.51 values are both based on a 2005 pooled analysis, which also was among the
studies used to derive the original assumptions for this report.
264
The 2.94 is based on the linear relationship of
children below 7.5 μg/dL, and the 0.51 is from the log-linear relationship of children between 2.4 and 10 μg/dL.
The team performed two sensitivity analyses on the blood lead-to-IQ eect size using alternate estimates of
2.53 and 0.51. The team selected these values because 2.53 is corrected from a re-analysis of the 2005 study’s
<7.5 μg/dL subsample (previously 2.94) and 0.51 is commonly used in other lead remediation studies.
265
As seen
in Table A.5, both alternate values had a substantial impact on the final results, changing the total discounted
benefits from $84 billion to $174 billion and $42 billion, respectively.

116
Lifetime earnings-to-IQ eect size
As previously discussed, the modeling team used an average of studies on the relationship between IQ and
earnings, while excluding studies that over-controlled for educational attainment or failed to calculate eect
sizes for both males and females. The 2.27 percent increase in earnings per IQ point was calculated from the
mean of three studies. Some additional literature, which the team excluded for the reasons stated above, favors
a value closer to 1.1 percent.
266
The team therefore selected 1.1 percent for the sensitivity analysis, and similar
to the IQ-to-blood lead eect size, this change had a large impact on the results, reducing total discounted
benefits to $45 billion.
Starting blood lead levels
The modeling team defined population blood lead levels using the two most recent samples from NHANES data
(2011-12 and 2013-14), as explained above. The team used a combined sample to provide demographic breakouts
of lead exposure as well as a larger dataset, which reduces uncertainty. However, given the persistent downward
trend in child blood lead levels since the start of NHANES data collection, the mixture of the two samples could
overestimate population blood lead concentrations. To account for this possibility, the team ran a sensitivity
analysis using only the 2013-14 distribution, which has a slightly lower mean (0.95 μg/dL vs. 1.1 μg/dL) and
a smaller percentage of children above important thresholds (2 μg/dL and 5 μg/dL). The sensitivity analysis
revealed relatively small impacts of the alternate data set on the results.
Real wage growth
The benefit calculations were particularly sensitive to assumptions about the labor market and future
earnings. Real wage growth was estimated to be 1 percent, which has been used in previous work on childhood
lead exposure and is similar to estimates used in other economic projections.
267
An alternative assumption
of 0 percent real wage growth had a significant impact on the results, reducing the benefits from $84 billion
to $57 billion.
Gross domestic product
The team did not include in the original model gross domestic product (GDP) multiplier eects of the increased
income resulting from reduced childhood lead exposure. Some previous work in this area does include such
impacts, which result from the assumption that an individual who gains $1 in income will spend some of that
dollar, increasing GDP by more than $1.
268
This concept is debated among economists, though most generally
agree that the real-world multiplier is greater than 1.0 and that the eect is larger when the economy is not at
full employment. The modeling team made a conservative assumption by not including a multiplier eect for this
work. Not using a GDP multiplier makes the results more consistent with previous work that also did not include
this eect.
269
An alternative multiplier value of 1.92 was derived using data from the Bureau of Economic Analysis and the ratio
of GDP to earned income,
270
which have been relatively consistent over the past 10 years, ranging from about 1.86
to 1.92. Altering this assumption to 1.92 had a significant impact on the results, increasing the total benefits from
$84 to $155 billion.

117
Valuation of QALYs
Another impact of reducing childhood lead exposure is greater longevity resulting from reduced risk of disease,
the benefits of which are captured in the model in multiple ways: reductions in health spending, increases in
lifetime earnings, and QALYs, a calculation of the “implicit value” of added years of life. QALYs is a somewhat
intangible benefit but one that is commonly included in regulatory analyses.
271
The modeling team used a
conservative valuation of $50,000 per QALY, and a sensitivity analysis to omit this variable (e.g., valuing a QALY
at zero) produced a very similar final result of $81 billion.
Discount rate
In an economic analysis, the rate at which the value of future benefits decreases relative to present-day dollars
has a substantial impact on the results. Because many of the benefits from reducing childhood lead exposure
come from earnings many years in the future, the discount rate has a very large impact on the findings in this
study. A discount rate of 3 percent has become relatively standard in regulatory analyses, though, in the past,
the Oce of Management and Budget and the Congressional Budget Oce have advocated for using both
7 percent and 3 percent. To address this variation in the field, the modeling team conducted a sensitivity analysis
at the 7 percent discount rate. The results were a substantially smaller present value, $19 billion rather than
$84 billion.
Although government cost-benefit analyses tend to use 3 percent and 7 percent, some economists suggest
that discount rates over longer time horizons should be much lower. In particular, they have argued that when
analyzing intergenerational transfers (interventions paid for today that benefit future generations), discount rates
closer to zero percent are more appropriate.
272
Conducting the sensitivity analysis using a smaller discount rate
of 1 percent yielded far greater total discounted benefits of $208 billion.

118
Endnotes
1 Ronnie Levin et al., “Lead Exposures in U.S. Children, 2008: Implications for Prevention,” Environmental Health Perspectives 116, no. 10
(2008): 1285–93, http://dx.doi.org/10.1289/ehp.11241; Susan M. Bernard and Michael A. McGeehin, “Prevalence of Blood Lead Levels >5
μg/dL Among U.S. Children 1 to 5 Years of Age and Socioeconomic and Demographic Factors Associated With Blood of Lead Levels 5 to
10 μg/dL, Third National Health and Nutrition Examination Survey, 1988–1994,” Pediatrics 112, no. 6 (2003): 1308 –13, http://pediatrics.
aappublications.org/content/112/6/1308.
2 Richard Rabin, “The Lead Industry and Lead Water Pipes: A Modest Campaign,” American Journal of Public Health 98, no. 9 (2008):
1584–92, http://dx.doi.org/10.2105/AJPH.2007.113555.
3 U.S. Environmental Protection Agency, “Phasing Down Lead in Gasoline,” Environmental Protection Agency Journal 11, no. 4 (1985), https://
nepis.epa.gov/Exe/ZyPURL.cgi?Dockey=93000E80.txt.
4 Gerald Markowitz and David Rosner, Lead Wars: The Politics of Science and the Fate of America’s Children, 2013 (Berkeley, CA: University of
California Press, 2013).
5 National Research Council Committee on Measuring Lead in Critical Populations, Measuring Lead Exposure in Infants, Children, and Other
Sensitive Populations; International Labour Organisation, “White (Painting) Convention,” 1921 (No. 13), accessed March 20, 2017, http://
www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_INSTRUMENT_ID:312158.
6 International Labour Organisation, “White (Painting) Convention”; David E. Jacobs, “Lead Poisoning: Focusing on the Fix,” Journal of
Public Health Management & Practice 22, no. 4 (2016): 326, http://dx.doi.org/10.1097/PHH.0000000000000430; Gerald E. Markowitz
and David Rosner, Deceit and Denial: The Deadly Politics of Industrial Pollution (Berkeley: University of California Press, 2002).
7 David E. Jacobs, “Lead Poisoning: Focusing on the Fix”; Richard Rabin, “The Lead Industry and Lead Water Pipes: A Modest Campaign.”
8 Lead-Soldered Food Cans, 60 Fed. Reg. 33106 (June 27, 1995), https://www.gpo.gov/fdsys/granule/FR-1995-06-27/95-15593.
9 David E. Jacobs, “Lead Poisoning: Focusing on the Fix”; Gerald E. Markowitz and David Rosner, Deceit and Denial.
10 David E. Jacobs, “Lead Poisoning: Focusing on the Fix”; Gerald E. Markowitz and David Rosner, Deceit and Denial, 58.
11 U.S. Environmental Protection Agency, “Phasing Down Lead in Gasoline.”
12 U.S. Food and Drug Administration, “Lead-Based Paint Poisoning Prevention Act,” accessed April 14, 2017, https://www.fda.gov/
RegulatoryInformation/LawsEnforcedbyFDA/ucm148755.htm; Randolph K. Byers and Elizabeth E. Lord, “Late Eects of Lead Poisoning
on Mental Development,” American Journal of Diseases of Children 66, no. 5 (1943): 471–94, http://rachel.org/files/document/Late_
Eects_of_Lead_Poisoning_on_Mental_devel.pdf; Gerald E. Markowitz and David Rosner, Deceit and Denial, 58.
13 U.S. Environmental Protection Agency, “EPA History: Lead,” accessed April 12, 2017, https://www.epa.gov/history/epa-history-lead; U.S.
Energy Information Administration, “Gasoline Explained: Gasoline and the Environment,” accessed Feb. 7, 2017, http://www.eia.gov/
energyexplained/?page=gasoline_environment.
14 Man-Fung Tsoi et al., “Continual Decrease in Blood Lead Level in Americans: United States National Health Nutrition and Examination
Survey 1999-2014,” American Journal of Medicine 129, no. 11 (2016): 1213–18, http://dx.doi.org/10.1016/j.amjmed.2016.05.042; William
Wheeler and Mary Jean Brown, “Blood Lead Levels in Children Aged 1-5 Years—United States, 1999-2010,” Morbidity and Mortality
Weekly Report 62, no. 13 (2013): 245–48, https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6213a3.htm.
15 Centers for Disease Control and Prevention, “What Do Parents Need to Know to Protect Their Children?” accessed Jan. 27, 2017, https://
www.cdc.gov/nceh/lead/acclpp/blood_lead_levels.htm.
16 National Center for Environmental Health/Agency for Toxic Substances and Disease Registry (meeting of the Lead Poisoning Prevention
Subcommittee of the NCEH/ATSDR Board of Scientific Advisors, record of the proceedings, Atlanta, Sept. 19, 2016), https://www.atsdr.
cdc.gov/science/lpp/docs/lead_subcommittee_minutes_9_19_2016_508.pdf.
17 Ibid.
18 Centers for Disease Control and Prevention, “Guidelines for the Identification and Management of Lead Exposure in Pregnant and
Lactating Women” (Atlanta: U.S. Department of Health and Human Services, Nov. 2010), https://www.cdc.gov/nceh/lead/publications/
leadandpregnancy2010.pdf. During pregnancy and lactation, lead stored in bones can release into a mother’s blood.

119
19 U.S. Environmental Protection Agency, “Review of the National Ambient Air Quality Standards for Lead,” Fed. Reg. 81, no. 201, Oct. 18,
2016, https://www.gpo.gov/fdsys/pkg/FR-2016-10-18/pdf/2016-23153.pdf; U.S. Environmental Protection Agency, “Lead; Identification
of Dangerous Levels of Lead; Final Rule,” 40 CFR Part 745, Fed. Reg. 66, no. 4 (2001): 1206–40, https://www.gpo.gov/fdsys/pkg/FR-
2001-01-05/pdf/01-84.pdf; Code of Federal Regulations, Protection of Environment, Title 40, Part 141 (1991), http://www.ecfr.gov/cgi-
bin/text-idx?SID=531617f923c3de2cbf5d12ae4663f56d&mc=true&node=sp40.23.141.i&rgn=div6; Department of Health and Human
Services, National Institute for Occupational Safety and Health, “Occupational Safety and Health Guideline for Inorganic Lead,” accessed
April 17, 2017, https://www.cdc.gov/niosh/docs/81-123/pdfs/0368.pdf; “Citizen Petition to EPA Regarding the Paint and Dust Lead
Standards” (Aug. 10, 2009): http://www.nchh.org/Portals/0/Contents/EPA_Lead_Standards_Petition_Final.pdf.
20 U.S. Environmental Protection Agency, “What Are the Health Eects of Lead?” Learn About Lead (March 2017), https://www.epa.gov/
lead/learn-about-lead#eects.
21 Ibid.; Bruce Lanphear et al., “Low Level Environmental Lead Exposure and Children’s Intellectual Function: An International Pooled
Analysis,” Environmental Health Perspectives 113, no. 7 (2005): 894–99, https://dx.doi.org/10.1289/ehp.7688; email from David
Bellinger, Harvard Medical School, to Jee-Young Kim, EPA (2008)—subject: request for additional information on Bellinger
and Needleman (2003) (EPA-HQ-OAR-2006-0735-5156), U.S. Environmental Protection Agency, http://www.regulations.
gov/#!documentDetail;D=EPA-HQ-OAR-2006-0735-5156; email from Dr. Richard Canfield, Cornell University, to Jee-Young Kim,
USEPA (2008)—subject: request for additional information on Canfield et al. (2003) (EPA-HQ-OAR-2006-0735- 5811), U.S.
Environmental Protection Agency, http://www.regulations.gov/#!documentDetail;D=EPAHQ-OAR-2006-0735-5811; email from
Richard Hornung, Cincinnati Children's Hospital Medical Center (CCHMC), to Jee-Young Kim, USEPA (2008)—subject: request for
additional information on Lanphear et al. (2005) (EPA-HQ-OAR-2006-0735-5814), U.S. Environmental Protection Agency, http://
www.regulations.gov/#!documentDetail;D=EPA-HQ-OAR-2006-0735-5814; email from Martha Tellez-Rojo, Center of Investigation in
Evaluation and Polls, National institute of Public Health, to Jee-Young Kim, USEPA (2008)—subject: questions on the Tellez-Rojo et al.
(2006) paper (EPAHQ-OAR-2006-0735-5123).
22 U.S. Environmental Protection Agency, “Integrated Science Assessment for Lead” (2013), https://www.epa.gov/isa/integrated-science-
assessment-isa-lead.
23 U.S. Environmental Protection Agency, “Integrated Science Assessment for Lead.”
24 Atmaram Yarlagadda et al., “Blood-Brain Barrier: The Role of Calcium Homeostasis,” Psychiatry (Edgmont) 4, no. 12 (2007): 55–59,
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2861516; Elizabeth Prado and Kathryn Dewey, “Nutrition and Brain Development in
Early Life,” Nutrition Reviews 72, no. 4 (2014): 267–84, https://doi.org/10.1111/nure.12102.
25 U.S. Environmental Protection Agency, “Air Quality Criteria for Lead—Volume I” (October 2006), http://ofmpub.epa.gov/eims/
eimscomm.getfile?p_download_id=459555; Talia Sanders et al., “Neurotoxic Eects and Biomarkers of Lead Exposure: A Review,”
Environmental Health 24, no. 1 (2009): 14, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2858639/pdf/nihms190515.pdf.
26 U.S. Environmental Protection Agency, “West Calumet Housing Complex—East Chicago, Ind.,” accessed Jan. 27, 2017, https://www.
epa.gov/uss-lead-superfund-site/west-calumet-housing-complex-east-chicago-ind; Agency for Toxic Substances and Disease Registry,
“Public Health Assessment for U.S. Smelter and Lead Refinery Inc. (USS Lead) East Chicago, Indiana” accessed Feb. 14, 2017, https://
www.atsdr.cdc.gov/HAC/pha/USSmelterandLeadRefinery/USSLeadPHABlue01272011.pdf.
27 U.S. Environmental Protection Agency, “West Calumet Housing Complex—East Chicago, Ind.”
28 Council on Environmental Health, “Prevention of Childhood Lead Toxicity,” Pediatrics 138, no. 1 (2016), http://dx.doi.org/10.1542/
peds.2016-1493; National Center for Healthy Housing, “Find It, Fix It, Fund It: A Lead Elimination Action Drive,” accessed Jan. 27,
2017, http://www.nchh.org/Portals/0/Contents/Find-It-Fix-It-Fund-It.pdf; Ruth Ann Norton, “Strategic Plan to End Childhood
Lead Poisoning,” Green & Healthy Homes Initiative Blog, accessed Jan. 27, 2017, http://www.greenandhealthyhomes.org/
StrategicPlanforEndingLeadPoisoning; Earthjustice, “Health, Environment & Children’s Groups Call for National Strategy to End Lead
Poisoning and Lead Exposure,” Oct. 24, 2016, http://earthjustice.org/news/press/2016/health-environment-children-s-groups-
call-for-national-strategy-to-end-lead-poisoning-and-lead-exposure; President’s Task Force, “Federal Strategy”; Centers for Disease
Control and Prevention, “Preventing Lead Poisoning in Young Children” (August 2005), https://www.cdc.gov/nceh/lead/publications/
prevleadpoisoning.pdf; Nick Farr and Cushing N. Dolbeare, “Childhood Lead Poisoning: Solving a Health and Housing Problem” Cityscape
2, no. 3 (1996): 167–81, https://www.huduser.gov/periodicals/cityscpe/vol2num3/farr.pdf; Centers for Disease Control and Prevention,
“Preventing Lead Exposure in Young Children: A Housing-Based Approach to Primary Prevention of Lead Poisoning” (Atlanta: CDC,
2004), https://www.cdc.gov/nceh/lead/publications/primarypreventiondocument.pdf; U.S. Environmental Protection Agency, “Report
of the Lead and Copper Rule Working Group to the National Drinking Water Advisory Council” (2015), https://www.epa.gov/sites/
production/files/2016-01/documents/ndwaclcrwgfinalreportaug2015.pdf; Educational Services for Children Aected by Lead Expert
Panel, “Educational Interventions for Children Aected by Lead” (2015), https://www.cdc.gov/nceh/lead/publications/educational_
interventions_children_aected_by_lead.pdf; Centers for Disease Control and Prevention, “Guidelines for the Identification and
Management of Lead Exposure in Pregnant and Lactating Women” (Atlanta: U.S. Department of Health and Human Services, November
2010), https://www.cdc.gov/nceh/lead/publications/leadandpregnancy2010.pdf.

120
29 The models include impacts for the 2018 birth cohort up to age 100 and estimate the number of children alive at each age using CDC
Underlying Cause of Death data. A decreasing percentage of the cohort is predicted to be alive and receiving the benefits of lead
reduction at older ages. For example, at age 100 approximately 4 percent of individuals are projected to still be alive.
30 A.C. Klassen et al., “Best Practices for Mixed Methods for Quality of Life Research,” Quality of Life Research 21, no. 3 (2012): 377–80,
https://doi.org/10.1007/s11136-012-0122-x; Sachiko Ozawa and Krit Pongpirul, “10 Best Resources on … Mixed Methods Research in
Health Systems,” Health Policy and Planning 29 (2014): 323–27, https://doi.org/10.1093/heapol/czt019.
31 Isabel V. Sawhill and Richard V. Reeves, “Modeling Equal Opportunity,” The Russell Sage Foundation Journal of the Social Sciences 2, no.
2 (2016): 60–97; Gregory Acs et al., “The Social Genome Model: Estimating How Policies Aect Outcomes, Mobility and Inequality
Across the Life Course,” Journal of Social Issues 72 (2016): 656–75, http://dx.doi.org/10.1111/josi.12188.
32 Lisa Chiodo et al., “Blood Lead Levels and Specific Attention Eects in Young Children,” Neurotoxicology and Teratology 29, no. 5 (2007):
538–46, https://doi.org/10.1016/j.ntt.2007.04.001; Marie Lynn Miranda et al., “The Relationship Between Early Childhood Blood Lead
Levels and Performance on End-of-Grade Tests,” Environmental Health Perspectives 115, no. 8 (2007): 1242–47, https://doi.org/10.1289/
ehp.9994; Michael J. Blackowicz et al., “The Impact of Low-Level Lead Toxicity on School Performance Among Hispanic Subgroups
in the Chicago Public Schools,” International Journal of Environmental Research and Public Health 13, no. 8 (2016): 774, https://dx.doi.
org/10.3390%2Fijerph13080774; Anne Evens et al., “The Impact of Low-Level Lead Toxicity on School Performance Among Children
in the Chicago Public Schools: A Population-Based Retrospective Cohort Study,” Environmental Health 14, no. 24 (2015): 21, https://doi.
org/10.1186/s12940-015-0008-9; Katarzyna Kordas et al., “Deficits in Cognitive Function and Achievement in Mexican First-Graders
With Low Blood Lead Concentrations,” Environmental Research 110, no. 3 (2006): 371–86, https://doi.org/10.1016/j.envres.2005.07.007;
Bruce Lanphear et al., “Cognitive Deficits Associated With Blood Lead Concentrations <10 microg/dL in U.S. Children and Adolescents,”
Public Health Reports 115, no. 6 (2000): 521–29, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1308622; David Bellinger, Karen Stiles,
and Herbert Needleman, “Low-Level Lead Exposure, Intelligence and Academic Achievement: A Long-Term Follow-Up Study,” Pediatrics
90, no. 6 (1992): 855–61, https://www.ncbi.nlm.nih.gov/pubmed/1437425.
33 U.S. Centers for Disease Control and Prevention, National Center for Environmental Health, Division of Emergency and Environmental
Health Services, “National Surveillance Data (1997–2015),” last updated Oct. 28, 2016, https://www.cdc.gov/nceh/lead/data/national.
htm.
34 Bruce Lanphear et al., “Low Level Environmental Lead Exposure and Children’s Intellectual Function: An International Pooled Analysis,”
Environmental Health Perspectives 113, no. 7 (2005): 894–99, https://dx.doi.org/10.1289/ehp.7688; email from David Bellinger, Harvard
Medical School, to Jee-Young Kim, EPA (2008)—subject: request for additional information on Bellinger and Needleman (2003)
(EPA-HQ-OAR-2006-0735-5156), U.S. Environmental Protection Agency, http://www.regulations.gov/#!documentDetail;D=EPA-
HQ-OAR-2006-0735-5156; email from Dr. Richard Canfield, Cornell University, to Jee-Young Kim, USEPA (2008)—subject: request
for additional information on Canfield et al. (2003) (EPA-HQ-OAR-2006-0735-5811), U.S. Environmental Protection Agency, http://
www.regulations.gov/#!documentDetail;D=EPAHQ-OAR-2006-0735-5811; email from Richard Hornung, Cincinnati Children's Hospital
Medical Center (CCHMC), to Jee-Young Kim, USEPA (2008)—subject: request for additional information on Lanphear et al. (2005)
(EPA-HQ-OAR-2006-0735-5814), U.S. Environmental Protection Agency, http://www.regulations.gov/#!documentDetail;D=EPA-
HQ-OAR-2006-0735-5814; email from Martha Tellez-Rojo, Center of Investigation in Evaluation and Polls, National Institute of Public
Health, to Jee-Young Kim, USEPA (2008)—subject: questions on the Tellez-Rojo et al. (2006) paper (EPAHQ-OAR-2006-0735-5123).
35 Bruce Lanphear et al., “Cognitive Deficits”; Lisa Chiodo et al., “Blood Lead Levels and Specific Attention Eects in Young Children,”
Neurotoxicology and Teratology 29, no. 5 (2007): 538–46, https://doi.org/10.1016/j.ntt.2007.04.001; Pamela Surkan et al.,
“Neuropsychological Function in Children With Blood Lead Levels < 10μg/dL,” Neurotoxicology 28, no. 6 (2007): 1170–77, https://dx.doi.
org/10.1016/j.neuro.2007.07.007; Meeyoung Min et al., “Cognitive Development and Low-Level Lead Exposure in Poly-Drug Exposed
Children,” Neurotoxicology and Teratology 31 no. 4 (2009): 225–31, https://dx.doi.org/10.1016/j.ntt.2009.03.002.
36 Richard L. Canfield et al., “Intellectual Impairment in Children With Blood Lead Concentrations Below 10 μg per Deciliter,” New England
Journal of Medicine 348 (2003): 1517–26, http:/dx.doi.org/10.1056/NEJMoa022848.
37 U.S. Environmental Protection Agency, “Benefit and Cost Analysis for the Euent Limitations Guidelines and Standards for the Steam
Electric Power Generating Point Source Category” (October 2015), https://www.epa.gov/sites/production/files/2015-10/documents/
steam-electric_benefit-cost-analysis_09-29-2015.pdf.

121
38 Marie Lynn Miranda et al., “The Relationship Between Early Childhood Blood Lead Levels and Performance on End-of-Grade Tests,"
Environmental Health Perspectives 115 (2007): 1242–47, http://www.jstor.org/stable/4626860?seq=1#page_scan_tab_contents;
Michael J. Blackowicz et al., “The Impact of Low-Level Lead Toxicity on School Performance Among Hispanic Subgroups in the Chicago
Public Schools,” International Journal of Environmental Research and Public Health 13, no. 8 (2016): 774, doi: 10.3390/ijerph13080774;
Chiodo et al., "Blood Lead Levels and Specific Attention Eects in Young Children," Neurotoxicology and Teratology 29, no. 5 (2007):
538–46, https://doi.org/10.1016/j.ntt.2007.04.001; David C. Bellinger, Karen M. Stiles, and Herbert L. Needleman, "Low-Level Lead
Exposure, Intelligence and Academic Achievement: a Long-Term Follow-Up Study," Pediatrics 90, no. 6 (1992): 855–61, http://pediatrics.
aappublications.org/content/90/6/855.short; Evans et al., “The Impact of Low-Level Lead Toxicity on School Performance Among
Children in the Chicago Public Schools: a Population-Based Retrospective Cohort Study,” Environmental Health 14, no. 21 (2015), https://
doi.org/10.1186/s12940-015-0008-9; Kordas et al., “Deficits in Cognitive Function and Achievement in Mexican First-Graders With Low
Blood Lead Concentrations,” Environmental Research 100, no. 3 (2006): 371–86, https://doi.org/10.1016/j.envres.2005.07.007; Lanphear
et al., "Cognitive Deficits Associated With Blood Lead Concentrations< 10 microg/dL in U.S. Children and Adolescents,” Public Health
Reports 115, no. 6 (2000): 521–29, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1308622.
39 J.M. Burns et al., “Lifetime Low-Level Exposure to Environmental Lead and Children's Emotional and Behavioral Development at
Ages 11-13 Years: The Port Pirie Cohort Study,” American Journal of Epidemiology 149, no. 8 (1999): 740–49, https://www.academia.
edu/25223826/Lifetime_Low-Level_Exposure_to_Environmental_Lead_and_Childrens_Emotional_and_Behavioral_Development_at_
Ages_11-13_Years_The_Port_Pirie_Cohort_Study; Aimin Chen et al., “Lead Exposure, IQ, and Behavior in Urban 5- to 7-Year-Olds: Does
Lead Aect Behavior Only by Lowering IQ?” Pediatrics 119, no. 3 (2007): e650–58, http://pediatrics.aappublications.org/content/119/3/
e650.short; Lisa M. Chiodo, Sandra W. Jacobson, and Joseph L. Jacobson, “Neurodevelopmental Eects of Postnatal Lead Exposure at
Very Low Levels,” Neurotoxicology and Teratology 26, no. 3 (2004): 359–71, doi: 10.1016/j.ntt.2004.01.010; Lisa M. Chiodo et al., "Blood
Lead Levels and Specific Attention Eects in Young Children," Neurotoxicology and Teratology 29, no. 5 (2007): 538–46, doi: 10.1016/j.
ntt.2007.04.001; Joel T. Nigg et al., “Low Blood Levels Associated With Clinically Diagnosed Attention-Deficit/Hyperactivity Disorder
and Mediated by Weak Cognitive Control,” Biological Psychiatry 63, no. 3 (2008): 325–31, doi: 10.1016/j.biopsych.2007.07.013.
40 S.M. Bernard and M.A. McGeehin, “Prevalence of Blood Lead Levels ≥5 μg/dL Among U.S. Children 1 to 5 Years of Age and
Socioeconomic and Demographic Factors Associated With Blood Lead Level 5 to 10 μg/dL, Third National Health and Nutrition
Examination Survey, 1988–1994,” Pediatrics 112, no. 6 (2003): 1308–13.
41 Peter J. Neumann, Joshua T. Cohen, and Milton C. Weinstein, “Updating Cost-Eectiveness—The Curious Resilience of the
$50,000-per-QALY Threshold,” New England Journal of Medicine 371, no. 9 (2014): 796–97, http://dx.doi.org/10.1056/NEJMp1405158.
42 John Paul Wright et al., “Association of Prenatal and Childhood Blood Lead Concentrations With Criminal Arrests in Early Adulthood,”
PLoS Medicine 5, no. 5 (2008): e101, https://doi.org/10.1371/journal.pmed.0050101.
43 Steven G. Gilbert and Bernard Weiss, “A Rationale for Lowering the Blood Lead Action Level from 10 to 2 μg/dL,” Neurotoxicology 27,
no. 5 (2006): 693–701, https://dx.doi.org/10.1016%2Fj.neuro.2006.06.008; Tanya E. Froelich et al., “Association of Tobacco and Lead
Exposures With Attention-Deficit/Hyperactivity Disorder,” Pediatrics 124, no. 6 (2009): e1054–63, https://doi.org/10.1542/peds.2009-
0738.
44 Aaron Reuben et al., “Association of Childhood Blood Lead Levels With Cognitive Function and Socioeconomic Status at Age 38 Years
and With IQ Change and Socioeconomic Mobility Between Childhood and Adulthood,” The Journal of the American Medical Association
317, no. 12 (2017): 1244–51, http://dx.doi.org/10.1001/jama.2017.1712.
45 U.S. Environmental Protection Agency, “Basic Information About Lead in Drinking Water,” accessed Dec. 12, 2016, https://www.epa.gov/
ground-water-and-drinking-water/basic-information-about-lead-drinking-water; “Safety of Public Water Systems,” The Public Health
and Welfare, U.S. Code 42 § 300f, accessed May 24, 2017, https://www.gpo.gov/fdsys/pkg/USCODE-2010-title42/pdf/USCODE-
2010-title42-chap6A-subchapXII.pdf. A later amendment to the SDWA that went into eect in 2014 banned lead plumbing fixtures in
homes and redefined the term “lead free.”
46 Anne Sandvig et al., “Contribution of Service Line and Plumbing Fixtures to Lead and Copper Rule Compliance Issues” (Denver: AWWA
and EPA, 2008), https://archive.epa.gov/region03/dclead/web/pdf/91229.pdf.
47 Simoni Triantafyllidou and Marc Edwards, “Lead (Pb) in Tap Water and in Blood: Implications for Lead Exposure in the United States,”
Critical Reviews in Environmental Science and Technology 42, no. 13 (2012): 1297–1352, http://dx.doi.org/10.1080/10643389.2011.55655
6; Mary Jean Brown and Stephen Margolis, “Lead in Drinking Water and Human Blood Lead Levels in the United States,” Morbidity and
Mortality Weekly Report 61 (2012), https://www.cdc.gov/mmwr/pdf/other/su6104.pdf; Marc Edwards, Simoni Triantafyllidou, and Dana
Best, “Elevated Blood Lead in Young Children Due to Lead-Contaminated Drinking Water,” Environmental Science and Technology 43, no.
5 (2009), http://dx.doi.org/10.1021/es802789w; G. Ngueta et al., “Use of a Cumulative Exposure Index to Estimate the Impact of Tap
Water Lead Concentration on Blood Lead Levels in 1- to 5-Year-Old Children (Montreal, Canada),” Environmental Health Perspectives 124
(2016): 388–95; http://dx.doi.org/10.1289/ehp.1409144.
48 A cross-sectional study is an analysis of observed data collected from a population at a specific point in time.
49 Bruce P. Lanphear et al., “Environmental Exposures to Lead and Urban Children’s Blood Lead Levels,” Environmental Research 76, no. 2
(1998): 120–30, https://doi.org/10.1006/enrs.1997.3801.

122
50 “National Primary Drinking Water Regulations,” Code of Federal Regulations, title 40, part 141 (June 7, 1991), http://www.ecfr.gov/cgi-
bin/text-idx?SID=531617f923c3de2cbf5d12ae4663f56d&mc=true&node=sp40.23.141.i&rgn=div6.
51 U.S. Environmental Protection Agency, “Lead and Copper Rule Revisions White Paper” (Washington: U.S. Environmental Protection
Agency, 2016), https://www.epa.gov/sites/production/files/2016-10/documents/508_lcr_revisions_white_paper_final_10.26.16.pdf.
52 Ibid.
53 An observational study is an analysis in which individuals are monitored or certain outcomes are measured. No attempt is made to
aect the outcome (for example, no treatment is given). Well-designed observational studies have been shown to provide results similar
to randomized controlled trials. Cohort and case-control studies are two primary types of observational studies that aid in evaluating
associations between diseases and exposures.
54 Mary Jean Brown et al., “Association Between Children’s Blood Lead Levels, Lead Service Lines, and Water Disinfection, Washington,
DC, 1998–2006,” Environmental Research 111 (2011): 67–74, https://doi.org/10.1016/j.envres.2010.10.003.
55 U.S. Environmental Protection Agency, “SAB Evaluation of the Eectiveness of Partial Lead Service Line Replacements” (2011), https://
www.epa.gov/sites/production/files/201509/documents/sab_evaluation_partial_lead_service_lines_epa-sab-11-015.pdf.
56 Élise Deshommes et al., “Monitoring-Based Framework to Detect and Manage Lead Water Service Lines,” Journal of the American
Waterworks Association 108, no. 11 (2016): 555–70, http://dx.doi.org/10.5942/jawwa.2016.108.0167.
57 David A. Cornwell, Richard A. Brown, and Steve H. Via, “National Survey of Lead Service Line Occurrence,” Journal of the American Water
Works Association 108, no. 4 (2016): E187–92, http://dx.doi.org/10.5942/jawwa.2016.108.0086; U.S. Environmental Protection Agency,
“Drinking Water Action Plan” (Washington: U.S. Environmental Protection Agency, November 2016), https://www.epa.gov/sites/
production/files/2016-11/documents/508.final_.usepa_.drinking.water_.action.plan_11.30.16.v0.pdf.
58 Michael W. Shannon and John W. Graef, “Lead Intoxication in Infancy,” Pediatrics 89, no. 1 (1992): 87–90, http://pediatrics.
aappublications.org/content/89/1/87?sso=1&sso_redirect_count=1&nfstatus=401&nftoken=00000000-0000-0000-0000-
000000000000&nfstatusdescription=ERROR%3a+No+local+token.
59 County Health Rankings, “Our Ratings,” accessed May 5, 2017, http://www.countyhealthrankings.org/roadmaps/what-works-for-
health/our-ratings. Scientifically supported is defined by County Health Rankings as interventions for which there are 1 or more
systematic review(s), or at least three experimental studies, or three quasi-experimental studies with matched concurrent comparisons.
Studies have strong designs and statistically significant favorable findings, see http://www.countyhealthrankings.org/roadmaps/what-
works-for-health/our-methods.
60 Alaska Department of Health and Social Services, “Technical Guidance for Health Impact Assessment In Alaska,” accessed May 12,
2017, http://dhss.alaska.gov/dph/Epi/hia/Documents/AlaskaHIAToolkit.pdf.
61 Cornwell et al., “National Survey of Lead Service Line Occurrence.”
62 U.S. Census Bureau, Population Division, “Annual Estimates of the Resident Population by Single Year of Age and Sex for the United
States: April 1, 2010 to July 1, 2015” (Washington: U.S. Census Bureau, June 2016), https://factfinder.census.gov/faces/tableservices/
jsf/pages/productview.xhtml?src=bkmk.
63 Ibid.
64 Michèle Prévost and Élise Deshommes. “Calculation of Reference Water Levels for Lead Service Line Replacement Intervention,” http://
altarum.org/our-work/lead-exposure-mitigation; S. Triantafyllidou et al., "Low Contribution of Pb02-Coated Lead Service Lines to Water
Lead Contamination at the Tap," Environmental Science & Technology 49, no. 6 (2015): 3746–54, doi: 10.1021/es505886h.
65 U.S. Environmental Protection Agency, “Proposed Modeling Approaches for a Health-Based Benchmark for Lead in Drinking Water”
(Washington: U.S. Environmental Protection Agency, 2017), https://www.epa.gov/sites/production/files/2017-01/documents/
report_proposed_modeling_approaches_for_a_health_based_benchmark_for_lead_in_drinking_water_final_0.pdf; U.S. Environmental
Protection Agency, Integrated Exposure Uptake Biokinetic Model for Lead in Children, EPA 9285.7-42540-K-01-005, IEUBK win 32Lead
Model Version 1.1 Build 11 (May 2007) https://www.epa.gov/superfund/lead-superfund-sites-software-and-users-manuals. IEUBK uses
site-specific data and biokinetic modeling.
66 Anne Sandvig et al., “Contribution of Service Line and Plumbing Fixtures to Lead and Copper Rule Compliance Issues” (Denver: AWWA
and EPA, 2008), https://archive.epa.gov/region03/dclead/web/pdf/91229.pdf.
67 Personal communication with Steve Via, “Informal Survey of Estimated Lead Service Line Replacement Costs,” unpublished dataset,
cited with permission, March 2017.
68 Pam Zekman, “2 Investigators: Cost of Replacing Lead Service Lines Is on Chicago Home Owners,” CBS Chicago, Dec. 8, 2016, http://
chicago.cbslocal.com/2016/12/08/2-investigators-cost-of-replacing-lead-service-lines-is-on-chicago-home-owners.

123
69 Michael Hawthorne and Peter Matuszak, “As Other Cities Dig Up Pipes Made of Toxic Lead, Chicago Resists,” Chicago Tribune, Sept. 21,
2016, http://www.chicagotribune.com/news/watchdog/ct-lead-water-pipes-funding-20160921-story.html; Environmental Protection
Agency Science Advisory Board, “SAB Evaluation of the Eectiveness of Partial Lead Service Line Replacements.”
70 U.S. Environmental Protection Agency, “How the Drinking Water State Revolving Fund Works,” accessed March 21, 2017, https://www.
epa.gov/drinkingwatersrf/how-drinking-water-state-revolving-fund-works.
71 Ronnie Levin et al., “Lead Exposures in U.S. Children, 2008: Implications for Prevention.”
72 David E. Jacobs, “Lead-Based Paint as a Major Source of Childhood Lead Poisoning: A Review of the Evidence,” in Lead in Paint, Soil
and Dust: Health Risks, Exposure Studies, Control Measures and Quality Assurance, ed. Michael E. Beard and S.D. Allen Iske (Philadelphia:
American Society for Testing and Materials, 1995), 175–87.
73 U.S. Department of Housing and Urban Development, “American Healthy Homes Survey: Lead and Arsenic Findings” (2011), http://
portal.hud.gov/hudportal/documents/huddoc?id=AHHS_Report.pdf.
74 Ibid.
75 40 CFR 745.223.
76 HUD, “American Healthy Homes Survey” (2011); David E. Jacobs et al., “Replacing Windows Reduces Childhood Lead Exposure: Results
From a State-Funded Program,” Journal of Public Health Management and Practice 22, no. 5 (2016): 482–91, https://doi.org/10.1097/
PHH.0000000000000389.
77 Caroline Alderson, “Technical Preservation Guidelines: Upgrading Historic Building Windows” (Washington: U.S. General Services
Administration, April 2009), https://www.gsa.gov/graphics/pbs/Windows.pdf; Advisory Council on Historic Preservation, “The
National Historic Preservation Program: Overview,” accessed Feb. 17, 2017, http://www.achp.gov/overview.html.
78 David E. Jacobs, “Lead-Based Paint as a Major Source of Childhood Lead Poisoning”; Sherry Dixon et al., “Window Replacement
and Residential Lead Paint Hazard Control 12 Years Later,” Environmental Research 113 (2012): 14–20, https://doi.org/10.1016/j.
envres.2012.01.005; David E. Jacobs et al., “Replacing Windows Reduces Childhood Lead Exposure”; Rick Nevin et al., “Monetary
Benefits of Preventing Childhood Lead Poisoning With Lead-Safe Window Replacement,” Environmental Research 106, no. 3 (2008):
410–19, http://doi.org/10.1016/j.envres.2007.09.003; Lead Safe Illinois, “CLEAR-WIN Comprehensive Lead Elimination and Reduction—
Through Window Replacement” (2010), http://www.leadsafeillinois.org/uploads/documents/CLEARWINfactsheet62010.pdf; Illinois
Department of Public Health, “Clear-Win Program: Pilot Phase Evaluation” (December 2014), http://www.dph.illinois.gov/sites/default/
files/publications/publications-ohp-clear-winreport-042016.pdf.
79 Yona Amitai et al., “Residential Deleading: Eects on the Blood Lead Levels of Lead-Poisoned Children,” Pediatrics 88, no. 5 (1991):
893–97, http://pediatrics.aappublications.org/content/88/5/893.
80 Walter J. Rogan et al., “The Eect of Chelation Therapy With Succimer on Neuropsychological Development in Children Exposed to
Lead,” The New England Journal of Medicine 344 (2001): 1421–26, http://dx.doi.org/10.1056/NEJM200105103441902;Hilary Thomson
et al., “Housing Improvements for Health and Associated Socio-Economic Outcomes,” Cochrane Database of Systematic Reviews 2
(Feb. 28, 2013), https://doi.org/10.1002/14651858.CD008657.pub2; Barbara Nussbaumer-Streit et al., “Household Interventions
for Preventing Domestic Lead Exposure in Children (Review),” Cochrane Database of Systematic Reviews 10 (2016): 2–3, http://dx.doi.
org/10.1002/14651858.CD006047.pub5.
81 Roberto Gwiazda, Carla Campbell, and Donald Smith, “A Noninvasive Isotopic Approach to Estimate the Bone Lead Contribution to
Blood in Children: Implications for Assessing the Efficacy of Lead Abatement,” Environmental Health Perspectives 113, no. 1 (2005):
104–10, http://www.jstor.org/stable/3435755.
82 P.S. Barry, “A Comparison of Concentrations of Lead in Human Tissues,” British Journal of Industrial Medicine 32, no. 2 (1975): 119–39,
https://www.ncbi.nlm.nih.gov/pubmed/1131339; Michael B. Rabinowitz, “Toxicokinetics of Bone Lead,” Environmental Health Perspectives
91 (1991): 33–37, http://dx.doi.org/10.2307/3430979; Howard Hu et al., “The Epidemiology of Lead Toxicity in Adults: Measuring
Dose and Consideration of Other Methodologic Issues,” Environmental Health Perspectives 115, no. 3 (2007): 455–62, https://dx.doi.
org/10.1289%2Fehp.9783; Pam Factor-Litvak et al., “The Yugoslavia Prospective Study of Environmental Lead Exposure,” Environmental
Health Perspectives 107, no. 1 (1999): 9–15, http://dx.doi.org/10.2307/3434284; Mary Jean Brown et al., “Determinants of Bone and
Blood Lead Concentrations in the Early Postpartum Period,” Occupational and Environmental Medicine 57, no. 8 (2000): 535–41, https://
dx.doi.org/10.1136%2Foem.57.8.535;Hung-Yi Chuang et al., “Interrelations of Lead Levels in Bone, Venous Blood, and Umbilical Cord
Blood With Exogenous Lead Exposure Through Maternal Plasma Lead in Peripartum Women,” Environmental Health Perspectives 109, no.
5 (2001): 527–32, http://dx.doi.org/10.2307/3454713; P.S. Barry, “Concentrations of Lead in the Tissues of Children,” British Journal of
Industrial Medicine 38, no. 1 (1981): 61–71, http://www.jstor.org/stable/27723491.
83 Residential Lead-Based Paint Hazard Reduction Act of 1992, Pub. L. No. 102-550 (as amended through April 21, 2005), https://www.
hud.gov/oces/lead/library/lead/Title_X.pdf.

124
84 President’s Task Force on Environmental Health Risks and Safety Risks to Children, “Key Federal Programs to Reduce Childhood Lead
Exposures and Eliminate Associated Health Impacts” (November 2016), https://ptfceh.niehs.nih.gov/features/assets/files/key_federal_
programs_to_reduce_childhood_lead_exposures_and_eliminate_associated_health_impactspresidents_508.pdf.
85 U.S. Department of Housing and Urban Development, “American Healthy Homes Survey: Lead and Arsenic Findings.”
86 Katherine A. Ahrens et al., “Housing Assistance and Blood Lead Levels: Children in the United States, 2005–2012,” American Journal of
Public Health 106, no. 11 (2016): 2049–56, http://dx.doi.org/10.2105/AJPH.2016.303432.
87 National Conference of State Legislatures, “Lead Hazards Project” (Washington: NCSL, Aug. 3, 2016), http://www.ncsl.org/research/
environment-and-natural-resources/lead-hazards-project.aspx.
88 Katrina S. Korfmacher and Michael L. Hanley, “Are Local Laws the Key to Ending Childhood Lead Poisoning?” Journal of Health Politics,
Policy and Law 38, no. 4 (2013): 757–813, http://dx.doi.org/10.1215/03616878-2208603.
89 Nimia L. Reyes et al., “Identifying Housing That Poisons: A Critical Step in Eliminating Childhood Lead Poisoning,” Journal of Public Health
Management and Practice 12, no. 6 (2006): 563–69, http://journals.lww.com/jphmp/Abstract/2006/11000/Identifying_Housing_
That_Poisons__A_Critical_Step.10.aspx; Dori B. Reissman et al., “Use of Geographic Information System Technology to Aid Health
Department Decision Making About Childhood Lead Poisoning Prevention Activities,” Environmental Health Perspectives 109, no. 1
(2001): 89–94, http://dx.doi.org/10.2307/3434926.
90 Chinaro Kennedy et al., “Primary Prevention of Lead Poisoning in Children: A Cross-Sectional Study to Evaluate State Specific
Lead-Based Paint Risk Reduction Laws in Preventing Lead Poisoning in Children,” Environmental Health 13 (2014): 93. http://dx.doi.
org/10.1186/1476-069X-13-93.
91 U.S. Department of Housing and Urban Development, “American Healthy Homes Survey: Lead and Arsenic Findings” (2011), http://
portal.hud.gov/hudportal/documents/huddoc?id=AHHS_Report.pdf.
92 David E. Jacobs, “Lead-Based Paint as a Major Source of Childhood Lead Poisoning”; Sherry Dixon et al., “Window Replacement
and Residential Lead Paint Hazard Control 12 Years Later,” Environmental Research 113 (2012): 14–20, https://doi.org/10.1016/j.
envres.2012.01.005; David E. Jacobs et al., “Replacing Windows Reduces Childhood Lead Exposure: Results From a State-
Funded Program,” Journal of Public Health Management and Practice 22, no. 5 (2016): 482–91, https://doi.org/10.1097/
PHH.0000000000000389; Rick Nevin et al., “Monetary Benefits of Preventing Childhood Lead Poisoning With Lead-Safe Window
Replacement,” Environmental Research 106, no. 3 (2008): 410–19, http://doi.org/10.1016/j.envres.2007.09.003; Lead Safe Illinois,
“CLEAR-WIN Comprehensive Lead Elimination and Reduction—Through Window Replacement” (2010), http://www.leadsafeillinois.
org/uploads/documents/CLEARWINfactsheet62010.pdf; Illinois Department of Public Health, “Clear-Win Program: Pilot Phase
Evaluation” (December 2014), http://www.dph.illinois.gov/sites/default/files/publications/publications-ohp-clear-winreport-042016.
pdf.
93 County Health Rankings, “Our Ratings.” Scientifically supported is defined by County Health Rankings as interventions for which
there are one or more systematic review(s), or at least three experimental studies, or three quasi-experimental studies with matched
concurrent comparisons. Studies have strong designs and statistically significant favorable findings.
94 Alaska Department of Health and Social Services, “Technical Guidance for Health Impact Assessment in Alaska.”
95 Sherry Dixon et al., “Window Replacement and Residential Lead Paint Hazard Control 12 Years Later,” Environmental Research 113 (2012):
14–20, https://doi.org/10.1016/j.envres.2012.01.005.
96 Mark Farfel et al., “An Extended Study of Interim Lead Hazard Reduction Measures Employed in the Baltimore Clinical Center of the
Treatment of Lead-Exposed Children (TLC)—Clinical Trial” (Washington: U.S. Department of Housing and Urban Development, April
2000), http://www.nmic.org/nyccelp/medical-studies/Farfel-extended-study-interim-controls-4-00.pdf; Farfel et al. 1997, “Lead Based
Paint Abatement and Repair and Maintenance Study” (Washington: U.S. Environmental Protection Agency, December 1997), EPA-
747-R-97-005, https://www.epa.gov/sites/production/files/documents/24folup. pdf. Several variables would aect the applicability of
this study to the prevention scenario. Techniques and standards may have improved since the study was conducted in 2008 and 2009,
so its data may underestimate the impact of lead hazard control undertaken today. Because the prevalence of contaminated dust in
older homes may have changed since these data were collected the team modeled two dierent baseline dust lead levels, 20 and 10 μg/
sq. ft.
97 Sherry L. Dixon et al., “Exposure of U.S. Children to Residential Dust Lead, 1999–2004: II. The Contribution of Lead-Contaminated Dust
to Children’s Blood Lead Levels,” Environmental Health Perspectives 117, no. 3 (2009): 468–74, https://dx.doi.org/10.1289/ehp.11918.
98 U.S. Department of Housing and Urban Development, “American Healthy Homes Survey: Lead and Arsenic Findings” (April 2011),
http://portal.hud.gov/hudportal/documents/huddoc?id=AHHS_Report.pdf.

125
99 To determine the number of children born into a remediated home in the next 10 years, the team first calculated the percent of the
housing stock that would receive the intervention by dividing the number of remediated homes by the total number of homes in the
U.S. as shown in the American Community Survey. The team then used this percentage as the likelihood that a future child would be
born into a remediated home. For example, for the pre-1960, lead hazard control intervention, the team estimated that 2.1 percent of the
housing stock would receive the intervention and therefore each future child would have a 2.1 percent chance of living in a remediated
home. The team then assumed conservatively that these eects would persist for the next 10 birth cohorts.
100 Mark Farfel et al., “An Extended Study of Interim Lead Hazard Reduction Measures Employed in the Baltimore Clinical Center of the
Treatment of Lead-Exposed Children (TLC)—Clinical Trial” (Washington: U.S. Department of Housing and Urban Development, April
2000), http://www.nmic.org/nyccelp/medical-studies/Farfel-extended-study-interim-controls-4-00.pdf; Mark Farfel et al., “Lead
Based Paint Abatement and Repair and Maintenance Study in Baltimore: Findings Based on Two Years of Follow-Up” (Washington: U.S.
Environmental Protection Agency, December 1997), https://www.epa.gov/sites/production/files/documents/24folup.pdf.
101 The maximum number children born in 2018 from low-income families expected to reside in pre-1960 housing is 321,000. A subset of
these children—311,000—are expected to reside in homes with lead-based paint.
102 The Pew Charitable Trusts, “Household Expenditures and Income: Balancing Family Finances in Today’s Economy” (March 2016), http://
www.pewtrusts.org/en/research-and-analysis/issue-briefs/2016/03/household-expenditures-and-income.
103 National Center for Healthy Housing, “Find It, Fix It, Fund It.”
104 Federal Housing Administration, “FHA Single Family Housing Policy Handbook” (Washington: U.S. Department of Housing and Urban
Development, Aug. 27, 2014), https://portal.hud.gov/hudportal/documents/huddoc?id=sfh_poli_appr_prop.pdf.
105 U.S. Environmental Protection Agency, Economic Analysis for the TSCA Lead Renovation, Repair, and Painting Program Final Rule
for Target Housing and Child-Occupied Facilities, §402(c) (2008): 3 39–41, http://www.nchh.org/Portals/0/Contents/EPA-HQ-
OPPT-2005-0049-0916_Final_Economic_Analysis_3-08.pdf.
106 Michael Rabinowitz, Alan Leviton, and David Bellinger, “Home Refinishing, Lead Paint and Infant Blood Lead Levels,” American Journal of
Public Health 75, no. 4 (1985): 403–04, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1646251/pdf/amjph00280-0093.pdf.
107 Adam J. Spanier et al., “The Contribution of Housing Renovation to Children’s Blood Lead Levels: A Cohort Study,” Environmental Health
12, no. 1 (2013): 72, http://dx.doi.org/10.1186/1476-069X-12-72.
108 E.M. Franko et al., “Children With Elevated Blood Lead Levels Related to Home Renovation, Repair, and Painting Activities—New York
State, 2006-2007,” Morbidity and Mortality Weekly Report 58, no. 3 (2009): 55–58, https://www.cdc.gov/mmwr/preview/mmwrhtml/
mm5803a3.htm; Rabinowitz, Leviton, and Bellinger, “Home Refinishing, Lead Paint and Infant Blood Lead Levels.”
109 E.M. Franko et al., “Children With Elevated Blood Lead Levels.”
110 U.S. Environmental Protection Agency, Lead Renovation, Repair and Painting Rule, 40 CFR 745, Federal Register 73, no. 78 (2008):
21691–769, https://www.gpo.gov/fdsys/pkg/FR-2008-04-22/html/E8-8141.htm.
111 U.S. Environmental Protection Agency, Economic Analysis for the TSCA Lead Renovation, Repair, and Painting Program Final Rule for
Target Housing and Child-Occupied Facilities, 3 39–41.
112 National Center for Healthy Housing, “New York’s Childhood Lead Poisoning Primary Prevention Program: Year 8 Grantee Impact
Summaries (Draft),” accessed Feb. 3, 2017, http://www.nchh.org/Portals/0/Contents/NYSDOH_Yr8_Appendix_Final.pdf; City of New
York, “Health Department Launches New Lead Dust Notification Procedures,” accessed Feb. 3, 2017, https://www1.nyc.gov/site/doh/
about/press/pr2015/pr021-15.page.
113 National Center for Healthy Housing, “New York’s Childhood Lead Poisoning Primary Prevention Program: Year 8 Grantee Impact
Summaries (draft),” accessed Feb. 3, 2017, http://www.nchh.org/Portals/0/Contents/NYSDOH_Yr8_Appendix_Final.pdf.
114 District of Columbia Department of Energy and Environment, “All About Lead,” accessed Jan. 13, 2017, http://doee.dc.gov/lead.
115 Rhode Island Department of Health, “Lead Safe Renovation, Repair, and Painting,” accessed Jan. 13, 2017, http://www.health.ri.gov/
healthrisks/poisoning/lead/about/renovationrepairandpainting.
116 Lead Safe Kids, “Working Lead-Safe in Providence: What Does This Mean for Me?” accessed Jan. 13, 2017, http://www.leadsafekids.org/
en/news/77-providence-rrp.
117 U.S. EPA, Economic Analysis for the TSCA Lead Renovation, Repair, and Painting Program, 3-39–41; Spanier et al., “The Contribution of
Housing Renovation to Children’s Blood Lead Levels: A Cohort Study”; Rabinowitz, Leviton and Bellinger, “Home Refinishing, Lead Paint
and Infant Blood Lead Levels”; Franko et al., “Children With Elevated Blood Lead Levels.”
118 County Health Rankings, “Our Ratings.” Scientifically supported is defined by County Health Rankings as interventions for which
there are one or more systematic review(s), or at least three experimental studies, or three quasi-experimental studies with matched
concurrent comparisons. Studies have strong designs and statistically significant favorable findings.

126
119 Alaska Department of Health and Social Services, “Technical Guidance for Health Impact Assessment In Alaska.”
120 U.S. Environmental Protection Agency, “The Approach Used for Estimating Changes in Children’s IQ From Lead Dust Generated
During Renovation, Repair and Painting in Residences and Child-Occupied Facilities” (Washington: EPA, March 28, 2008), https://
www.regulations.gov/document?D=EPA-HQ-OPPT-2005-0049-0930; Richard W. Leggett, “An Age-Specific Kinetic Model of Lead
Metabolism in Humans,” Environmental Health Perspectives 101, no. 7 (1993): 598–616, http://dx.doi.org/10.1289/ehp.93101598; U.S.
Environmental Protection Agency, “Revised Final Report on Characterization of Dust Lead Levels After Renovation, Repair, and Painting
Activities” (Washington: U.S. Environmental Protection Agency, Nov. 13, 2016), https://www.regulations.gov/document?D=EPA-HQ-
OPPT-2005-0049-0857.
121 U.S. EPA, Economic Analysis for the TSCA Lead Renovation, Repair, and Painting Program, ES-4.
122 U.S. EPA, Economic Analysis for the TSCA Lead Renovation, Repair, and Painting Program.
123 In its economic analysis, the EPA identified the cost of spot test kits as approximately $0.50 each, and assumed that testing four
samples would require about 15 minutes of a certified renovator’s time. Therefore, the estimated cost of using the kits would be $10 per
renovation event.
124 Franko et al., “Children With Elevated Blood Lead Levels.”
125 Environmental Protection Agency, “2014 National Emissions Inventory Data” (2014), https://www.epa.gov/air-emissions-
inventories/2014-national-emissions-inventory-nei-data.
126 Children’s Health Protection Advisory Committee, “National Ambient Air Quality Standards for Lead” (Jan. 8, 2015), https://www.epa.
gov/sites/production/files/2015-01/documents/naaqs_for_lead_letter.pdf.
127 Environmental Protection Agency, “Review of the National Ambient Air Quality Standards for Lead.”
128 Howard W. Mielke et al., “Environmental and Health Disparities in Residential Communities of New Orleans: The Need for Soil Lead
Intervention to Advance Primary Prevention,” Environment International 51 (2013) 73–81, http://dx.doi.org/10.1016/j.envint.2012.10.013;
U.S. Environmental Protection Agency, “America’s Children and the Environment, Third Edition,” EPA 240-R-13-001 (Washington: U.S.
Environmental Protection Agency, January 2013): 61, https://www.epa.gov/sites/production/files/2015-06/documents/ace3_2013.pdf.
129 Environmental Protection Agency, “Results of Lead and Arsenic Testing at West Calumet Housing Complex (Excel spreadsheet),”
accessed May 10, 2017, https://www.epa.gov/sites/production/files/2016-08/uss-lead-zone-1-action-data-redacted.xlsx.
130 Michael D. Lewin, Sara Sarasua, and Paul A. Jones, “A Multivariate Linear Regression Model for Predicting Children’s Blood Lead Levels
Based on Soil Lead Levels: A Study at Four Superfund Sites,” Environmental Research 81, no. 1 (1999): 52–61, https://dx.doi.org/10.1006/
enrs.1998.3952; Sammy Zahran et al., “Linking Source and Eect: Resuspended Soil Lead, Air Lead, and Children’s Blood Lead Levels
in Detroit, Michigan,” Environmental Science and Technology 47, no. 6 (2013), http://pubs.acs.org/doi/abs/10.1021/es303854c;
Howard W. Mielke et al., “The Urban Environment and Children’s Health: Soils as an Integrator of Lead, Zinc, and Cadmium in New
Orleans, Louisiana, USA,” Environmental Research 81, no. 2 (1999): 117–19, https://dx.doi.org/10.1006/enrs.1999.3966; Mielke et al.,
“Environmental and Health Disparities in Residential Communities of New Orleans.”
131 Howard Mielke et al., “Nonlinear Association Between Soil Lead and Blood Lead of Children in Metropolitan New Orleans, Louisiana:
2000-2005,” Science of the Total Environment 388, no. 1–3 (2007): 43–53, http://dx.doi.org/10.1016/j.scitotenv.2007.08.012; Jerey
Shire and John Villanacci, “Analysis of Risk Factors for Childhood Blood Lead Levels El Paso, Texas, 1997–2002,” prepared by the Texas
Department of Health for the Agency for Toxic Substances and Disease Registry (April 20, 2004), https://www.dshs.texas.gov/epitox/
consults/elppasblpbgisfinal4_23.pdf.
132 Howard Mielke et al., “Nonlinear Association Between Soil Lead and Blood Lead of Children in Metropolitan New Orleans, Louisiana:
2000–2005,” Science of the Total Environment 388, no. 1–3 (2007): 43–53, http://dx.doi.org/10.1016/j.scitotenv.2007.08.012.
133 Mark Laidlaw et al., “Case Studies and Evidence-Based Approaches to Addressing Urban Soil Lead Contamination,” Applied Geochemistry
(2017), http://dx.doi.org/10.1016/j.apgeochem.2017.02.015.
134 Mielke et al., “Environmental and Health Disparities in New Orleans”; Michael Weitzman et al., “Lead-Contaminated Soil Abatement
and Urban Children's Blood Lead Levels,” JAMA 263, no. 13 (1993): 1647–54.
135 Katherine Farrell et al., “Soil Lead Abatement and Children’s Blood Lead Levels in an Urban Setting,” American Journal of Public Health 88,
no. 12 (1998): 1837–39, http://dx.doi.org/10.2105/AJPH.88.12.1837.
136 Mark Laidlaw et al., “Case Studies and Evidence-Based Approaches to Addressing Urban Soil Lead Contamination.”
137 Ibid.
138 U.S. Environmental Protection Agency, National Emissions Standards for Hazardous Air Pollutants From Secondary Lead Smelting, 77
Fed. Reg. 3 (Jan. 5, 2012), https://www.gpo.gov/fdsys/pkg/FR-2012-01-05/pdf/2011-32933.pdf#page=2.

127
139 EC/R Inc., memo prepared for EPA Oce of Air Quality Planning and Standards, “Risk and Technology Review—Final Analysis of Socio-
Economic Factors for Populations Living Near Secondary Lead Smelting Facilities,” December 2011, http://earthjustice.org/sites/default/
files/Leadsmeltersocioeconomicanalysis.pdf.
140 U.S. Environmental Protection Agency, National Emissions Standards for Hazardous Air Pollutants From Secondary Lead Smelting, 77
Fed. Reg. 3; Jessica Garrison and Kim Christensen, “Vernon Plant Closed Over Toxins,” Los Angeles Times, April 25, 2013, http://articles.
latimes.com/2013/apr/25/local/la-me-exide-arsenic-20130425; Texas Commission on Environmental Quality, “Exide Frisco Batter
Recycling Center” (October 2014), https://www.tceq.texas.gov/remediation/sites/exide/exide; Amy Wold, “New Plan to Close Former
Exide Site Expected to Be Complete in Early 2016,” The Advocate, Jan. 5, 2016, http://www.theadvocate.com/baton_rouge/news/article_
e0375310-ed91-578d-9f77-aa3019a2efdd.html.
141 U.S. Geological Survey, “Historical Statistics for Mineral and Material Commodities in the United States” (2011), https://minerals.usgs.
gov/minerals/pubs/historical-statistics; International Lead Association, “Lead Industry Profile,” accessed March 28, 2017, http://www.
ila-lead.org/UserFiles/File/factbook/chapter4.pdf.
142 William P. Eckel, Michael B. Rabinowitz and Gregory D. Foster, “Discovering Unrecognized Lead-Smelting Sites by Historical Methods,”
American Journal of Public Health 91, no. 4 (2001), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1446633/pdf/11291377.pdf.
143 Ibid.
144 Sammy Zahran et al., “Linking Source and Eect: Resuspended Soil Lead, Air Lead, and Children’s Blood Lead Levels in Detroit,
Michigan,” Environmental Science and Technology 47, no. 6 (2013): 2839–45, http://dx.doi.org/10.1021/es303854c .
145 United States Environmental Protection Agency, Oce of Inspector General, “EPA Has Made Progress in Assessing Historical
Lead Smelter Sites but Needs to Strengthen Procedures” (June 2014), https://www.epa.gov/sites/production/files/2015-09/
documents/20140617-14-p-0302.pdf.
146 Environmental Protection Agency, “Superfund Remedial Annual Accomplishments: Fiscal Year 2016 Superfund Remedial
Program Accomplishments Report,” accessed May 10, 2017, https://www.epa.gov/superfund/superfund-remedial-annual-
accomplishments#metrics.
147 Agency for Toxic Substances and Disease Registry, “John T. Lewis Community Childhood Blood Lead Study: Findings,” accessed March
24, 2017, https://www.atsdr.cdc.gov/sites/jtlewis/findings.html.
148 Ian von Lindern et al., “Estimating Children’s Soil/Dust Ingestion Rates Through Retrospective Analyses of Blood Lead Biomonitoring
From the Bunker Hill Superfund Site in Idaho,” Environmental Health Perspectives 124, no. 9 (2016): 1462–70, http://dx.doi.org/10.1289/
ehp.1510144.
149 Ian von Lindern et al., “Assessing Remedial Eectiveness Through the Blood Lead: Soil/Dust Lead Relationship at the Bunker Hill
Superfund Site in the Silver Valley of Idaho,” Science of the Total Environment 303 no. 1–2 (2003): 139–70, http://doi.org/10.1016/S0048-
9697(02)00352-2.
150 Michael D. Lewin, Sara Sarasua, and Paul A. Jones, “A Multivariate Linear Regression Model for Predicting Children’s Blood Lead Levels
Based on Soil Lead Levels.”
151 University of Maryland, “Lead in Garden Soils,” accessed June 7, 2017, https://extension.umd.edu/hgic/lead-garden-soils.
152 U.S. Environmental Protection Agency, “Technical Review Workgroup Recommendations Regarding Gardening and Reducing Exposure
to Lead-Contaminated Soils” (Washington: U.S. Environmental Protection Agency, 2014), http://nepis.epa.gov/Exe/ZyPURL.
cgi?Dockey=P100JJS3.TXT.
153 County Health Rankings, “Our Ratings.” Some evidence is defined by County Health Rankings and Roadmaps as: one or more systematic
review(s), or at least two experimental studies, or two quasi-experimental studies with matched concurrent comparisons, or three
studies with unmatched comparisons or pre-post measures. Studies have statistically significant favorable findings. Compared with
“Scientifically Supported,” studies have less rigorous designs or limited eect(s). Although the removal of lead from aviation fuel has not
been tested, multiple studies have documented an association between blood lead levels and residence near an airport serving aircraft
using leaded fuel.
154 Alaska Department of Health and Social Services, “Technical Guidance for Health Impact Assessment in Alaska.”
155 Unleaded AVGAS Transition Aviation Rulemaking Committee, “FAA UAT ARC Final Report Part I: Unleaded AVGAS Findings &
Recommendations” (Washington: Federal Aviation Administration, U.S. Department of Transportation, Feb. 17, 2012), https://www.faa.
gov/regulations_policies/rulemaking/committees/documents/media/Avgas.ARC.RR.2.17.12.pdf; Control of Air Pollution from Aircraft
and Aircraft Engines, Code of Federal Regulations, title 40, part 87 (2013); Advance Notice of Proposed Rulemaking on Lead Emissions
From Piston-Engine Aircraft Using Leaded Aviation Gasoline 75 Fed. Reg. 81 (April 28, 2010): 22439–68, https://www.federalregister.
gov/documents/2010/04/28/2010-9603/advance-notice-of-proposed-rulemaking-on-lead-emissions-from-piston-engine-aircraft-
using-leaded.

128
156 Sammy Zahran et al., “The Eect of Leaded Aviation Gasoline on Blood Lead in Children,” Journal of the Association of Environmental
and Resource Economists 4, no. 2 (2017): 575–610, http://dx.doi.org/10.1086/691686; “U.S. Product Supplied of Aviation
Gasoline,” U.S. Energy Information Administration, accessed Jan. 29, 2017, http://www.eia.gov/dnav/pet/hist/Leafhandler.
ashx?n=PET&s=MGAUPUS1&f=A.
157 Ibid.
158 Proposed Rulemaking on Lead Emissions From Piston-Engine Aircraft, 75 Fed. Reg. 81 (April 28, 2010), https://www.gpo.gov/fdsys/pkg/
FR-2010-04-28/pdf/2010-9603.pdf.
159 Rebecca Kessler, “Sunset for Leaded Aviation Gasoline?” Environmental Health Perspectives 121, no. 2 (2013): 54–57, http://dx.doi.
org/10.1289/ehp.121-a54; Marie Lynn Miranda, Rebecca Anthopolos and Douglas Hastings, “A Geospatial Analysis of the Eects
of Aviation Gasoline on Childhood Blood Lead Levels,” Environmental Health Perspectives 119, no. 10 (2011): 1513–16, https://dx.doi.
org/10.1289%2Fehp.1003231; Zahran et al., “The Eect of Leaded Aviation Gasoline.”
160 Zahran et al., “The Eect of Leaded Aviation Gasoline.”
161 County Health Rankings, “Our Ratings.” Some evidence is defined by County Health Rankings and Roadmaps as: one or more systematic
review(s), or at least two experimental studies, or two quasi-experimental studies with matched concurrent comparisons, or three
studies with unmatched comparisons or pre-post measures. Studies have statistically significant favorable findings. Compared to
“Scientifically Supported,” studies have less rigorous designs or limited eect(s). Although the removal of lead from aviation fuel has not
been tested, multiple studies have documented an association between blood lead levels and residence near an airport serving aircraft
using leaded fuel.
162 Alaska Department of Health and Social Services, “Technical Guidance for Health Impact Assessment in Alaska,” accessed May 12,
2017, http://dhss.alaska.gov/dph/Epi/hia/Documents/AlaskaHIAToolkit.pdf.
163 Alaska Department of Health and Social Services, “Technical Guidance for Health Impact Assessment in Alaska,” accessed May 12,
2017, http://dhss.alaska.gov/dph/Epi/hia/Documents/AlaskaHIAToolkit.pdf.
164 Proposed Rulemaking on Lead Emissions From Piston-Engine Aircraft, 75 Fed. Reg. 81; Advance notice of proposed rulemaking on lead
emissions from piston-engine aircraft using leaded aviation gasoline, 75 Fed. Reg. 22440: 22440–68 (April 28, 2010).
165 Unleaded AVGAS Transition Aviation Rulemaking Committee, “FAA UAT ARC Final Report Part I” (February 2012).
166 President’s Task Force on Environmental Health Risks and Safety Risks to Children, “Key Federal Programs to Reduce Childhood Lead
Exposures and Eliminate Associated Health Impacts,” https://ptfceh.niehs.nih.gov/features/assets/files/key_federal_programs_to_
reduce_childhood_lead_exposures_and_eliminate_associated_health_impactspresidents_508.pdf.
167 Substance Abuse and Mental Health Services Administration, “Cultural Competence,” accessed April 20, 2017, https://www.samhsa.
gov/capt/applying-strategic-prevention/cultural-competence
168 Greater Cincinnati Water Works, “Lead Awareness” (2007), http://cincinnati-oh.gov/water/lead-information/; DC Water, “Service Map,
Lead” (2017), https://www.dcwater.com/servicemap; Boston Water and Sewer Commission, “Lead Service Map” (2017), http://www.
bwsc.org/COMMUNITY/lead/leadmaps.asp#TOP_PAGE; Lead Materials, California Health and Safety Code 104 Part 12, Ch. 5 Art 4,
http://leginfo.legislature.ca.gov/faces/codes_displayText.xhtml?lawCode=HSC&division=104.&title=&part=12.&chapter=5.&article=4.;
Ohio House of Representatives Bill 512, 131st General Assembly (Sept. 9, 2016), http://search-prod.lis.state.oh.us/solarapi/v1/general_
assembly_131/bills/hb512/EN/05?format=pdf.
169 U.S. Centers for Disease Control and Prevention, “Educational Interventions for Children Aected by Lead” (Atlanta: U.S. Department of
Health and Human Services, 2015), https://www.cdc.gov/nceh/lead/publications/educational_interventions_children_aected_by_lead.
pdf.
170 Weihong Yuan et al., "The Impact of Early Childhood Lead Exposure on Brain Organization: A Functional Magnetic Resonance Imaging
Study of Language Function,"Pediatrics118, no. 3 (2006): 971–77, https://doi.org/10.1542/peds.2006-0467.
171 Center on the Developing Child at Harvard University, “Building the Brain’s ‘Air Trac Control’ System: How Early Experiences Shape the
Development of Executive Function,” Working Paper No. 11 (2011), http://developingchild.harvard.edu/resources/building-the-brains-
air-trac-control-system-how-early-experiences-shape-the-development-of-executive-function.
172 T. Matthews et al., “Social Isolation and Mental Health at Primary and Secondary School Entry: A Longitudinal Cohort Study,” Journal of
the American Academy of Child and Adolescent Psychiatry 54, no. 3 (2015): 225–32, http://doi.org/10.1016/j.jaac.2014.12.008.
173 Jessica Wolpaw Reyes, “Lead Exposure and Behavior: Eects on Antisocial and Risky Behavior Among Children and Adolescents,”
Economic Inquiry 53, no. 3 (2015): 1580–1605, http://dx.doi.org/10.1111/ecin.12202.
174 Adele Diamond and Kathleen Lee, “Interventions Shown to Aid Executive Function Development in Children 4 to 12 Years Old,” Science
333, no. 6045 (2011): 959–64, https://dx.doi.org/10.1126%2Fscience.1204529.

129
175 Hirokazu Yoshikawa et al., “Investing in Our Future: The Evidence Base on Preschool Education” (Ann Arbor, MI: Society for Research in
Child Development, 2013), http://www.srcd.org/sites/default/files/documents/washington/mb_2013_10_16_investing_in_children.pdf.
176 Eric M. Ossiander, “A Systematic Review of Screening Questionnaires for Childhood Lead Poisoning,” Journal of Public Health Management
Practice 19, no. 1 (2013): E21–29, http://dx.doi.org/10.1097/PHH.0b013e3182249523. This report uses the term “screening” to refer to
questionnaires only, while “testing” includes any sampling of blood. Methods for analyzing blood tests range in price, accuracy, sample
size, diculty of use, and amount of time required to provide results. In the U.S., most laboratories cannot detect blood lead levels below
3 μg/dL. Factors such as the person performing the analysis and the care taken to ensure that the sample is not contaminated after
collection can also aect the results.
177 The Centers for Medicare & Medicaid Services, “Early and Periodic Screening, Diagnostic, and Treatment,” accessed June 7, 2017,
https://www.medicaid.gov/medicaid/benefits/epsdt/index.html; Joshua Schneyer and M. B. Pell, “Unsafe At Any Level,” Reuters, June 9,
2016, http://www.reuters.com/investigates/special-report/lead-poisoning-testing-gaps.
178 Anne M. Wengrovitz and Mary Jean Brown, “Recommendations for Blood Lead Screening of Medicaid-Eligible Children Aged 1-5 Years:
An Updated Approach to Targeting a Group at High Risk,” Morbidity and Mortality Weekly Report 58, no. RR-9 (2009): 1–11, https://www.
cdc.gov/mmwr/preview/mmwrhtml/rr5809a1.htm.
179 Jennifer Dickman, “Children at Risk: Gaps in State Lead Screening Policies” (Washington: Safer Chemicals, Healthy Families, January
2017), http://saferchemicals.org/sc/wp-content/uploads/2017/01/saferchemicals.org_children-at-risk-report.pdf.
180 Wengrovitz and Brown, “Recommendations for Blood Lead Screening of Medicaid-Eligible Children.”
181 Centers for Disease Control and Prevention, “CDC Recommendations for Lead Poisoning Prevention in Newly Arrived Refugee Children,”
accessed Feb. 22, 2017, https://www.cdc.gov/nceh/lead/publications/refugeetoolkit/pdfs/cdcrecommendations.pdf
182 Diamond and Lee, “Interventions Shown to Aid Executive Function Development in Children 4 to 12 Years Old.”
183 Hirokazu Yoshikawa et al., “Investing in Our Future: The Evidence Base on Preschool Education” (Ann Arbor, MI: Society for Research in
Child Development, 2013), http://www.srcd.org/sites/default/files/documents/washington/mb_2013_10_16_investing_in_children.pdf.
184 Todd Grindal et al., "The Added Impact of Parenting Education in Early Childhood Education Programs: A Meta-Analysis,"Children and
Youth Services Review70 (2016): 238–49, https://doi.org/10.1016/j.childyouth.2016.09.018.
185 Mayo Clinic, “Cognitive Behavioral Therapy,” accessed March 9, 2017, http://www.mayoclinic.org/tests-procedures/cognitive-
behavioral-therapy/home/ovc-20186868.
186 Nurse-Family Partnership, “A Rigorously Tested Program with Measureable Benefits,” accessed Feb. 23, 2017, http://www.
nursefamilypartnership.org/assets/PDF/Fact-sheets/NFP_Benefit_Cost.aspx.
187 Harriet J. Kitzman et al., “Enduring Eects of Prenatal and Infancy Home Visiting by Nurses on Children,” Archive Pediatric Adolescent
Medicine 164, no. 5 (2010): 412–18, https://dx.doi.org/10.1001/archpediatrics.2010.76.
188 David Olds et al., “Long-Term Eects of Nurse Home Visitation on Children’s Criminal and Antisocial Behavior: 15-Year Follow-Up of
a Randomized Controlled Trial,” Journal of American Medicine Association 280 no. 14 (1996): 1238–44, https://dx.doi.org/ 10.1001/
jama.280.14.1238.
189 Child Trends, “Incredible Years Series,” accessed December 2016, https://www.childtrends.org/programs/incredible-years-series.
190 M. Jamila Reid, Carolyn Webster-Stratton, and Mary Hammond, “Follow-Up of Children Who Received the Incredible Years Intervention
for Oppositional-Defiant Disorder: Maintenance and Prediction of 2-Year Outcome,” Behavior Therapy 34 (2003): 471–91, https://dx.doi.
org/ 10.1016/S0005-7894(03)80031-X.
191 Hugh F. Crean and Deborah B. Johnson, “Promoting Alternative Thinking Strategies (PATHS) and Elementary School Aged Children's
Aggression: Results From a Cluster Randomized Trial,” American Journal of Community Psychology 52, no. 1–2 (2013): 56–72, https://
dx.doi.org/10.1007/s10464-013-9576-4.
192 David J. Schonfeld et al., “Cluster-Randomized Trial Demonstrating Impact on Academic Achievement of Elementary Social-Emotional
Learning,” School Psychology Quarterly 30, no. 3 (2015): 406–20, http://dx.doi.org/10.1037/spq0000099.
193 Karin S. Frey et al., “Reducing Playground Bullying and Supporting Beliefs: An Experimental Trial of the Steps to Respect Program,”
Developmental Psychology 41, no. 3 (2005): 479–90, https://dx.doi.org/10.1037/0012-1649.41.3.479.
194 U.S. Centers for Disease Control and Prevention, “Educational Interventions for Children Aected by Lead,” 34.
195 Assistance to States for the Education of Children With Disabilities, “§ 300.111 Child Find,” Cornell University Law School, accessed April
20, 2017, https://www.law.cornell.edu/cfr/text/34/300.111.

130
196 U.S. Centers for Disease Control and Prevention, “Managing Elevated Blood Lead Levels Among Young Children: Recommendations
From the Advisory Committee on Childhood Lead Poisoning Prevention,” accessed May 1, 2017, https://www.cdc.gov/nceh/lead/
casemanagement/managingEBLLs.pdf.
197 Betsy Lozo, “Iron Deficiency and Child Development,” Food and Nutrition Bulletin 28 (2007): S560–71, http://journals.sagepub.com/doi/
pdf/10.1177/15648265070284S409.
198 Stephen Billings and Kevin Schnepel,“Life Unleaded: Eects of Early Interventions for Children Exposed to Lead” (Working Paper
No. 2015-18, Life Course Centre, Australian Research Council, August 2015), http://www.lifecoursecentre.org.au/wp-content/
uploads/2015/08/2015-18-LCC-Working-Paper-Billings-and-Schnepel2.pdf.
199 U.S. Department of Agriculture Food and Nutrition Service, “Women, Infants and Children (WIC): WIC Food Package Regulatory
Requirements,” accessed April 18, 2017, https://www.fns.usda.gov/wic/wic-food-package-regulatory-requirements.
200 Margot I. Jackson, “Early Childhood WIC Participation, Cognitive Development and Academic Achievement,” Social Science & Medicine
126 (2015): 145–53, https://dx.doi.org/10.1016/j.socscimed.2014.12.018; Abigail Arons et al., “Participation in the Special Supplemental
Nutrition Program for Women, Infants, and Children Is Not Associated With Early Childhood Socioemotional Development: Results
From a Longitudinal Cohort Study,” Preventive Medicine Reports 4 (2016): 507–11, https://dx.doi.org/10.1016/j.pmedr.2016.09.004;
Edward A. Frongillo, Diana F. Jyoti, and Sonya J. Jones, “Food Stamp Program Participation Is Associated With Better Academic Learning
Among School Children,” The Journal of Nutrition 136, no. 4 (2006): 1077–80, http://jn.nutrition.org/content/136/4/1077.full.pdf+html.
201 U.S. Preventive Services Task Force, “Final Recommendation Statement: Lead Levels in Childhood and Pregnancy: Screening” (2006),
https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/lead-levels-in-childhood-and-
pregnancy-screening. In 2006, the U.S. Preventive Services Task Force recommended against universal blood lead testing for children at
average risk of exposure. This guidance was designed to avoid potential harms, including false-positive results, anxiety, inconvenience,
absenteeism from work and school, and financial costs of repeated testing. However, the recommendations did not address testing for
high-risk children.
202 Anne Guthrie Wengrovitz et al., “Overcoming Barriers to Data-Sharing Related to the HIPAA Privacy Rule” (Washington: Alliance for
Healthy Homes, June 2004), https://www.cdc.gov/nceh/lead/policy/HIPAADoc.pdf.
203 Katarzyna Kordas, “The ‘Lead Diet’: Can Dietary Approaches Prevent or Treat Lead Exposure?” Journal of Pediatrics, in print (2017),
http://dx.doi.org/10.1016/j.jpeds.2017.01.069.
204 Health Canada, “Lead in Drinking Water” (Health Canada, the Federal-Provincial-Territorial Committee on Drinking Water, October
2016), http://www.healthycanadians.gc.ca/health-system-systeme-sante/consultations/lead-drinking-water-plomb-eau-potable/alt/
lead-drinking-water-plomb-eau-potable-03-01-2017-eng.pdf.
205 Dr. Pascal Haefliger, “Brief Guide to Analytical Methods for Measuring Lead in Blood,” World Health Organization (2011), http://www.
who.int/ipcs/assessment/public_health/lead_blood.pdf; The U.S. Centers for Disease Control and Prevention defines a blood lead
test as “any blood lead draw (capillary, venous or unknown sample type) on a child that produces a quantifiable result and is analyzed
by a Clinical Laboratory Improvement Amendments (CLIA)-certified facility or an approved portable device. A blood lead test may be
collected for screening, confirmation, or follow-up.”
206 Reuben et al., “Association of Childhood Blood Lead Levels With Cognitive Function and Socioeconomic Status at Age 38 Years and
With IQ Change and Socioeconomic Mobility Between Childhood and Adulthood.”
207 40 CFR 745.223.
208 Miriam King, Steven Ruggles, J. Trent Alexander, Sarah Flood, Katie Genadek, Matthew B. Schroeder, Brandon Trampe, and Rebecca
Vick. Integrated Public Use Microdata Series, Current Population Survey: Version 3.0. [Machine-readable database]. Minneapolis, MN:
Minnesota Population Center [producer and distributor], 2010.
209 U.S. Centers for Disease Control and Prevention, National Center for Environmental Health, “National Surveillance Data (1997–2015)”
(Atlanta: U.S. Department of Health and Human Services, 2016), https://www.cdc.gov/nceh/lead/data/national.htm.
210 John Paul Wright et al., “Association of Prenatal and Childhood Blood Lead Concentrations With Criminal Arrests in Early Adulthood,”
PLoS Medicine 5, no. 5 (2008): e101, https://doi.org/10.1371/journal.pmed.0050101.
211 Leonardo Trasande and Yinghua Liu, "Reducing the Staggering Costs of Environmental Disease in Children, Estimated at $76.6 Billion in
2008," Health Aairs 30, no. 5 (2011): 863–70, http://content.healthaairs.org/content/30/5/863.short.
212 P.J. Neumann, J.T. Cohen, and M.C. Weinstein, “Updating Cost-Eectiveness—The Curious Resilience of the $50,000-per-QALY
Threshold,” New England Journal of Medicine 371, no. 9 (2014): 796–97.
213 G.D. Sanders et al., “Recommendations for Conduct, Methodological Practices, and Reporting of Cost-Eectiveness Analyses,” JAMA
316, no. 10 (2016): 1093–1103; W. Max, “Present Value of Lifetime Earnings, 2007,” unpublished tables, Institute for Health and Aging,
University of California, San Francisco (2010).

131
214 Council on Environmental Health, “Prevention of Childhood Lead Toxicity,” Pediatrics (2016), http://dx.doi.org/10.1542/peds.2016-1493.
215 Elise Gould, “Childhood Lead Poisoning: Conservative Estimates of the Social and Economic Benefits of Lead Hazard Control,”
Environmental Health Perspectives 117, no. 7 (2009): 1162–67, http://dx.doi.org/10.1289/ehp.0800408.
216 Ibid.; Altarum Institute, “Health Sector Economic Indicators—Price Briefs,” available at http://altarum.org/our-work/cshs-health-sector-
economic-indicators-briefs.
217 U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics,
Underlying Cause of Death 1999-2015 on CDC WONDER Online Database, released 2016. Data are compiled from the 57 vital statistics
jurisdictions through the Vital Statistics Cooperative Program, accessed at http://wonder.cdc.gov/ucd-icd10.html. Data for 2015 are
compiled from the Multiple Cause of Death File 2015, Series 20, No. 2U, 2016.
218 Yutaka Aoki et al., “Blood Lead and Other Metal Biomarkers as Risk Factors for Cardiovascular Disease Mortality,” Medicine 95, no. 1
(2016): e2223, http://dx.doi.org/10.1097/MD.0000000000002223.
219 Ibid.
220 Dariush Mozaarian et al., “Heart Disease and Stroke Statistics—2015 Update: A Report From the American Heart Association,”
Circulation 131 (2015): e29–322, http://dx.doi.org/10.1161/CIR.0000000000000152.
221 Martin et al., “Association of Blood Lead and Tibia Lead With Blood Pressure and Hypertension in a Community Sample of Older Adults,”
American Journal of Epidemiology 163, no. 5 (2006): 467–78, https://doi.org/10.1093/aje/kwj060.
222 Guijing Wang et al., “Hypertension-Associated Expenditures for Medication Among U.S. Adults,” American Journal of Hypertension 26,
no. 11 (2013): 1295–1302, https://doi.org/10.1093/ajh/hpt079.
223 Bruce Lanphear et al., “Low-Level Environmental Lead Exposure and Children’s Intellectual Function: an International Pooled Analysis,”
Environmental Health Perspectives 113, no. 7 (2005): 894–99, https://dx.doi.org/10.1056/NEJM200307313490515; Todd Jusko et al.,
“Blood Lead Concentrations < 10 μg/dL and Child Intelligence at 6 Years of Age,” Environmental Health Perspectives 166 (2008): 243–48.
224 Jusko et al., “Blood Lead Concentrations”; Richard L. Canfield et al., “Intellectual Impairment in Children With Blood Lead Concentrations
below 10 μg per Deciliter,” New England Journal of Medicine 348 (2003): 1517–26, http:/dx.doi.org/10.1056/NEJMoa022848; David
Bellinger and Herbert Needleman, “Intellectual Impairment And Blood Lead Levels,” New England Journal of Medicine 349 (2003):
500–02, https://dx.doi.org/10.1056/NEJM200307313490515; Bruce Lanphear et al., “Low-Level Environmental Lead Exposure And
Children’s Intellectual Function: An International Pooled Analysis,” Environmental Health Perspectives 113, no. 7 (2005): 894–99, https://
dx.doi.org/10.1289%2Fehp.7688.
225 National Ambient Air Quality Standards for Lead, 73 Fed. Reg. 219 (Nov. 12, 2008): 66964.
226 European Food Safety Authority, “Scientific Opinion on Lead in Food: EFSA Panel on Contaminants in the Food Chain (CONTAM),” EFSA
Journal 8, no. 4 (2010): 1570, http://dx.doi.org/10.2903/j.efsa.2010.1570.
227 David S. Salkever, “Assessing the IQ-Earnings Link in Environmental Lead Impacts on Children: Have Hazard Eects Been Overstated?,”
Environmental Research 131 (2014): 219–30, http://dx.doi.org/10.1016/j.envres.2014.03.018.
228 Ibid.
229 Randall Lutter, “Valuing Children’s Health: A Reassessment of the Benefits of Lower Lead Levels,” Working Paper 00-02 (AEI-Brookings
Joint Center for Regulatory Studies, 2000), https://papers.ssrn.com/sol3/papers.cfm?abstract_id=243537.
230 Dajun Lin, Randall Lutter, and Christopher J. Ruhm, “Cognitive Performance and Labor Market Outcomes,” Working Paper 22470 (NBER,
2016), http://www.nber.org/papers/w22470; David Salkever, “Updated Estimates of Earnings Benefits From Reduced Exposure of
Children to Environmental Lead,” Environmental Research 70, no. 1 (1995): 1–6, https://dx.doi.org/10.1006/enrs.1995.1038; Derek A. Neal
and William R. Johnson, “The Role of Premarket Factors in Black-White Wage Dierences,” Journal of Political Economy 104, no. 5 (1996):
869–95, http://dx.doi.org/10.1086/262045.
231 Scott Grosse, “How Much Does IQ Raise Earnings? Implications for Regulatory Impact Analyses,” Research Letter, Association of
Environmental and Resource Economics, 27, no. 2 (2007). http://www.umsl.edu/~kosnikl/AERE%20Essay.pdf.
232 Ted Gayer and Robert W. Hahn, “Designing Environmental Policy: Lessons From the Regulation of Mercury Emissions,” Journal
of Regulatory Economics 30 (2006): 291–315, http://dx.doi.org/10.1007/s11149-006-9005-9; Lin, Lutter and Ruhm, “Cognitive
Performance.”
233 J. Schwartz, “Societal Benefits of Reducing Lead Exposure,” Environmental Research 66 (1994): 105–24, https://dx.doi.org/10.1006/
enrs.1994.1048.
234 Jay G. Chambers, Thomas B. Parish, and Jenifer J. Harr, “What Are We Spending on Special Education Services in the United States,
1999-2000?” (Washington: American Institutes for Research, 2004), http://www.csef-air.org/publications/seep/national/advrpt1.pdf.

132
235 David A. Cornwell, “National Survey of Lead Service Line Occurrence,” American Water Works Association 108, no. 4 (2016), http://dx.doi.
org/10.5942/jawwa.2016.108.0086.
236 David A. Cornwell, Richard A. Brown and Steven Via, “National Survey of Lead Service Line Occurrence,” Journal of the American Water
Works Association 13 (2016): E187–92, http://dx.doi.org/10.5942/jawwa.2016.108.0086.
237 U.S. Environmental Protection Agency, “Proposed Modeling Approaches for a Health-Based Benchmark for Lead in Drinking Water”
(2017), https://www.epa.gov/sites/production/files/2017-01/documents/report_proposed_modeling_approaches_for_a_health_based_
benchmark_for_lead_in_drinking_water_final_0.pdf.
238 Bruce P. Lanphear et al., “Environmental Exposures to Lead and Urban Children’s Blood Lead Levels,” Environmental Research 76 no.
2 (1998): 120–30, https://dx.doi.org/10.1006/enrs.1997.3801; Bruce P. Lanphear et al., “Environmental Lead Exposure During Early
Childhood,” Journal of Pediatrics 140, no. 1 (2002): 40–47, http://dx.doi.org/10.1067/mpd.2002.120513; Bruce P. Lanphear et al., “Low-
Level Environmental Lead Exposure And Children’s Intellectual Function: An International Pooled Analysis.”
239 Gerard Ngueta et al., “Use of a Cumulative Exposure Index to Estimate the Impact of Tap Water Lead Concentration on Blood
Lead Levels in 1- to 5-Year-Old Children (Montreal, Canada),” Environmental Health Perspectives 124 (2016): 388–95; http://dx.doi.
org/10.1289/ehp.1409144.
240 U.S. Environmental Protection Agency, “Proposed Modeling Approaches for a Health-Based Benchmark for Lead in Drinking Water.”
241 Michèle Prévost and Élise Deshommes. “Calculation of Reference Water Levels for Lead Service Line Replacement Intervention”;
S. Triantafyllidou et al., "Low Contribution of Pb02-Coated Lead Service Lines to Water Lead Contamination at the Tap."
242 U.S. Census Bureau, “American Community Survey,” U.S. Census Bureau’s American Community Survey Oce (2006), http://
factfinder2.census.gov.
243 Anne Sandvig et al., “Contribution of Service Line and Plumbing Fixtures to Lead and Copper Rule Compliance Issues” (Denver: AWWA
and EPA, 2008), https://archive.epa.gov/region03/dclead/web/pdf/91229.pdf.
244 Personal communication with Steve Via, “Informal Survey of Estimated Lead Service Line Replacement Costs,” unpublished dataset,
cited with permission, March 2017.
245 Sherry Dixon et al., “Window Replacement and Residential Lead Paint Hazard Control 12 Years Later,” Environmental Research 113 (2012):
14–20, https://doi.org/10.1016/j.envres.2012.01.005.
246 Mark Farfel et al., “An Extended Study of Interim Lead Hazard Reduction Measures Employed in the Baltimore Clinical Center of the
Treatment of Lead-Exposed Children (TLC)—Clinical Trial” (Washington: U.S. Department of Housing and Urban Development, April
2000), http://www.nmic.org/nyccelp/medical-studies/Farfel-extended-study-interim-controls-4-00.pdf; Farfel et al. 1997, “Lead Based
Paint Abatement and Repair and Maintenance Study” (Washington: U.S. Environmental Protection Agency, December 1997) EPA-
747-R-97-005, https://www.epa.gov/sites/production/files/documents/24folup.pdf.
247 Sherry L. Dixon et al., “Exposure of U.S. Children to Residential Dust Lead, 1999–2004: II. The Contribution of Lead-Contaminated Dust
to Children’s Blood Lead Levels,” Environmental Health Perspectives 117, no. 3 (2009):468–74, https://dx.doi.org/10.1289/ehp.11918.
248 U.S. Department of Housing and Urban Development, “American Healthy Homes Survey: Lead and Arsenic Findings” (Washington:
HUD, 2011), http://portal.hud.gov/hudportal/documents/huddoc?id=AHHS_Report.pdf; An alternative to this approach would
have been to use the percent of homes with lead-based paint hazards, defined as significantly deteriorated lead-based paint, or
dust or soil lead levels in excess of EPA standards, which is a subset of those with lead-based paint: The AHHS estimates that 52.5
percent of pre-1960 homes and 33.7 percent of pre-1978 homes have hazards. The study team chose to lead-based paint rather than
hazards for several reasons. First, homes with lead paint could develop hazards at any time if the paint deteriorates or is damaged.
Second, the AHHS definition of a lead-based paint hazard would exclude many units that by today’s standards would be considered
dangerous. For example, a home with a floor dust lead level under 40 μg/sq ft would not constitute a hazard under the survey, but
would far exceed HUD’s recently adopted floor dust standard of 10 μg/sq ft for grantees of the department’s lead paint hazard control
program. This variation in standards could result in an underestimation of high-risk units if only homes with hazards were considered.
Finally, by focusing on low-income older housing, which evidence suggests is in poorer condition than other homes, the models and
recommendations probably already isolated the units with the greatest likelihood of risk.
249 U.S. Environmental Protection Agency, “The Approach Used for Estimating Changes in Children’s IQ From Lead Dust Generated
During Renovation, Repair and Painting in Residences and Child-Occupied Facilities” (Washington: EPA, March 28, 2008), https://
www.regulations.gov/document?D=EPA-HQ-OPPT-2005-0049-0930; Richard W. Leggett, “An Age-Specific Kinetic Model of Lead
Metabolism in Humans,” Environmental Health Perspectives 101, no. 7 (1993): 598–616, http://dx.doi.org/10.1289/ehp.93101598; U.S.
Environmental Protection Agency, “Revised Final Report on Characterization of Dust Lead Levels After Renovation, Repair, and Painting
Activities” (Washington: U.S. Environmental Protection Agency, Nov. 13, 2016), https://www.regulations.gov/document?D=EPA-HQ-
OPPT-2005-0049-0857.

133
250 Sammy Zahran et al., “The Eect of Leaded Aviation Gasoline on Blood Lead in Children,” Journal of the Association of Environmental and
Resource Economists (In press).
251 Philip J. Wolfe et al., “Costs of IQ Loss From Leaded Aviation Gasoline Emissions,” Environmental Science and Technology 50 (2016):
9026–33, http://dx.doi.org/10.1021/acs.est.6b02910; Sammy Zahran et al., “The Eect of Leaded Aviation Gasoline on Blood Lead in
Children.”
252 Lynn A. Karolyn, M. Rebecca Kilburn, and Jill Cannon, “Early Childhood Interventions: Proven Results, Future Promise” (Santa Monica,
CA: RAND Corp., 2005), http://www.rand.org/content/dam/rand/pubs/monographs/2005/RAND_MG341.pdf.
253 Blueprints for Healthy Youth Development, “Blueprints Programs,” accessed November 2016, http://www.blueprintsprograms.com/
programs.
254 A. Biglan, The Nurture Eect: How the Science of Human Behavior Can Improve Our Lives & Our World (Oakland, CA: New Harbinger
Publications, 2015).
255 ChildTrends, Youth Development Outcomes Compendium (2001), https://www.childtrends.org/publications/youth-development-
outcomes-compendium.
256 Kristen E. Darling-Churchill, Laura Lippman, “Early Childhood Social and Emotional Development: Advancing the Field of Measurement,”
Journal of Applied Developmental Psychology 45 (2016): 1–7, http://dx.doi.org/10.1016/j.appdev.2016.02.002.
257 Sherry Dixon et al., “Window Replacement and Residential Lead Paint Hazard Control 12 Years Later,” Environmental Research 113 (2012):
14–20, https://doi.org/10.1016/j.envres.2012.01.005.
258 U.S. Environmental Protection Agency, “Revised Final Report on Characterization of Dust Lead Levels After Renovation, Repair,
and Painting Activities” (Washington: U.S. Environmental Protection Agency, Nov. 13, 2016), https://www.regulations.gov/
document?D=EPA-HQ-OPPT-2005-0049-0857.
259 U.S. Environmental Protection Agency, “Air Quality Criteria for Lead: Volume I of II [EPA Report, EPA/600/R-05/144aF]” (2006), http://
cfpub.epa.gov/ncea/CFM/recordisplay.cfm?deid=158823.
260 Bruce Lanphear et al., “Low Level Environmental Lead Exposure and Children’s Intellectual Function: an International Pooled Analysis,”
Environmental Health Perspectives 113, no. 7 (2005): 894–99, https://dx.doi.org/10.1289/ehp.7688; David Bellinger, email to Jee-Young
Kim, Feb. 13, 2008; Richard Canfield, email to Jee-Young Kim, Aug. 12, 2008; Richard Hornung, email to Jee-Young Kim, Aug. 19, 2008;
Martha Tellez-Rojo, email to Jee-Young Kim, Feb. 11, 2008.
261 David Bellinger, email to Jee-Young Kim, Feb. 13, 2008.
262 Ibid.; Richard Hornung, email to Jee-Young Kim, Aug. 19, 2008; Richard Canfield et al., “Intellectual Impairment in Children With Blood
Lead Concentrations Below 10 μg per Deciliter,” The New England Journal of Medicine 348 (2003): 1517–26, http://dx.doi.org/10.1056/
NEJMoa022848.
263 National Ambient Air Quality Standards for Lead, 73 Fed. Reg. 219 (Nov. 12, 2008): 66964; U.S. Environmental Protection Agency,
“Benefit and Cost Analysis for the Euent Limitations Guidelines and Standards for the Steam Electric Power Generating Point Source
Category” (2015), https://www.epa.gov/sites/production/files/2015-10/documents/steam-electric_benefit-cost-analysis_09-29-2015.
pdf; Elise Gould, “Childhood Lead Poisoning: Conservative Estimates of the Social and Economic Benefits of Lead Hazard Control,”
Environmental Health Perspectives 117, no. 7 (2009): 1162–67, http://dx.doi.org/10.1289/ehp.0800408; Leonardo Trasande and Yinghua
Liu, "Reducing the Staggering Costs of Environmental Disease in Children, Estimated at $76.6 Billion in 2008," Health Aairs 30, no. 5
(2011): 863–70, http://content.healthaairs.org/content/30/5/863.short.
264 Bruce Lanphear et al., “Low-Level Environmental Lead Exposure and Children’s Intellectual Function: an International Pooled Analysis,”
Environmental Health Perspectives 113, no. 7 (2005): 894–99, https://dx.doi.org/10.1056/NEJM200307313490515.
265 K.S. Crump et al., “A Statistical Reevaluation of the Data Used in the Lanphear et al. (2005) Pooled Analysis That Related Low Levels of
Blood Lead to Intellectual Deficits In Children,” Critical Reviews in Toxicology 43 (2013): 785–99.
266 Scott Grosse, “How Much Does IQ Raise Earnings? Implications for Regulatory Impact Analyses,” Research Letter, Association of
Environmental and Resource Economics 27, no. 2 (2007), http://www.umsl.edu/~kosnikl/AERE%20Essay.pdf; Ted Gayer and Robert W.
Hahn, “Designing Environmental Policy: Lessons From the Regulation of Mercury Emissions,” Journal of Regulatory Economics 30 (2006):
291–315, http://dx.doi.org/10.1007/s11149-006-9005-9; Lin, Lutter and Ruhm, “Cognitive Performance.”
267 Leonardo Trasande and Yinghua Liu, "Reducing the Staggering Costs of Environmental Disease in Children, Estimated at $76.6 Billion in
2008," Health Aairs 30, no. 5 (2011): 863–70, http://content.healthaairs.org/content/30/5/863.short; See economic assumptions
and methods in Social Security Administration, “The 2016 Annual Report of the Board of Trustees of The Federal Old-Age and Survivors
Insurance and Federal Disability Insurance Trust Funds” (2016), https://www.ssa.gov/OACT/TR/2016/tr2016.pdf.
268 Philip J. Wolfe et al., “Costs of IQ Loss From Leaded Aviation Gasoline Emissions,” Environmental Science and Technology 50 (2016):
9026–33, http://dx.doi.org/10.1021/acs.est.6b02910.

134
269 Elise Gould, “Childhood Lead Poisoning: Conservative Estimates of the Social and Economic Benefits of Lead Hazard Control,”
Environmental Health Perspectives 117, no. 7 (2009): 1162–67, http://dx.doi.org/10.1289/ehp.0800408; Leonardo Trasande and Yinghua
Liu, "Reducing the Staggering Costs of Environmental Disease in Children, Estimated at $76.6 Billion in 2008," Health Aairs 30, no. 5
(2011): 863–70, http://content.healthaairs.org/content/30/5/863.short.
270 U.S. Bureau of Economic Analysis, “Table 1.10. Gross Domestic Income by Type of Income,” accessed April 13, 2017, https://www.bea.
gov/iTable/iTable.cfm?ReqID=9&step=1#reqid=9&step=3&isuri=1&903=51.
271 U.S. Environmental Protection Agency, “Mortality Risk Valuation,” https://www.epa.gov/environmental-economics/mortality-risk-
valuation.
272 See, for example, the discussion of discount rates in N.H. Stern & Great Britain, The Economics of Climate Change: The Stern Review
(Cambridge, UK: Cambridge University Press, 2007).

The Health Impact Project, a collaboration of the Robert Wood Johnson Foundation and The Pew Charitable Trusts, is a national initiative
designed to reduce health inequities and improve the health of all people by ensuring that health is a valued and routine consideration in
decisions aecting them.
This report was funded by Robert Wood Johnson and Pew, with additional support from the Charles Stewart Mott Foundation. Any opinions
and conclusions expressed herein do not necessarily represent the views of the contributing individuals, organizations, advisory committee
members, or funders of the Health Impact Project.
Contact: Tami Holzman, ocer, communications
Phone: 202-552-2122
Email: [email protected]
For further information, please visit:
healthimpactproject.org
