
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 1
Ohio
Medicaid
Pharmacy Benefit Management Program
Unified Preferred Drug
List
Medicaid Fee-for-Service
and Managed Care
Plans
Effective January 1,
2024

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 2
Helpful Links
Prior Authorization (PA)
Prior Authorization (PA) Information |
pharmacy.medicaid.ohio.gov
• General Prior Authorization Requirements
• PA and Step Therapy Frequently Asked Questions
(FAQ)
Drug Coverage
Drug Coverage Information | pharmacy.medicaid.ohio.gov
• Drug Lookup Tool
• UPDL Criteria
• Quantity Limits
• Preferred Diabetic Supply List
General Information
- The Statewide UPDL is not an all-inclusive list of drugs covered by Ohio Department of Medicaid.
- Medications that are new to market will be non-preferred, PA required until reviewed by the Ohio
Department of Medicaid Pharmacy and Therapeutics (P&T) Committee.
- The document is listed in sections defined by therapeutic class. Drugs are listed by generic name if a generic is
available unless the brand name of the drug is preferred. In most cases, when a generic for a brand-name
drug is available, the generic drug will be preferred, and the brand name will be non‐preferred. Some drugs
may also require a specific manufacturer or the brand to be dispensed.
- Ohio Department of Medicaid will only cover drugs that are part of the Medicaid Drug Rebate Program, with
limited exceptions. This document may not reflect the most current rebate status of a drug (i.e., a drug may
be listed on the document but is non-rebateable and therefore non-payable).
- Some therapeutic categories are grandfathered. These categories will be denoted with an “*” next to their
title on the table on contents and their place within the criteria document.
- Some therapeutic categories may have quantity limits on specific drugs detailed in the criteria document,
however this is not an all-inclusive list. For a list of the quantity limits on specific drugs, please reference the
Quantity Limit Document found here: Quantity Limits Document | pharmacy.medicaid.ohio.gov
Terminology/Abbreviations:
AR (Age Restriction) – An edit allowing claims for members within a defined age range to be covered without PA
BvG (Brand Preferred Over the Generic) – The brand name drug is preferred over the generic equivalent
PA (Clinical Prior Authorization) – A prior authorization (PA) is required before the drug will be covered
QL (Quantity Limit) – A limit on the quantity that will be covered within a given time frame
ST (Step Therapy) – Drug requires a trial with one or more preferred drugs before being covered

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 3
New UPDL Criteria Format
- Beginning January 2023 and with a few minor exceptions, all therapeutic categories have the same standardized
outline format. The design of this new format is intended to have a cumulative approach bottom-to-top.
Example Category
LENGTH OF AUTHORIZATIONS: X days or Initial: X days; Subsequent: X days (if different)
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically approved to continue
the drug. Patients who have taken the drug previously, but do not have claims history (e.g. new to Medicaid), will need
to submit a prior authorization in order to continue coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA (if applicable):
“DRUG” CRITERIA (if applicable):
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least X days with at least X preferred drugs
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient cannot be changed
to a preferred drug (i.e., allergies, drug-drug interactions, contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical necessity for why
patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least X days with X preferred drugs
o For non-preferred extended-release formulations: must provide documentation of an inadequate clinical
response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide documentation of an
inadequate clinical response or allergy to two or more generic labelers (if available)
ADDITIONAL “DRUG” CRITERIA (if applicable):
ADDITIONAL INFORMATION (if applicable):
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s response to treatment from baseline and/or attestation of clinical
stabilization
QL – Drug: X doses per X days
AR – a PA is required for patients X years and older OR younger than X years
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 4
Interpretation of New UPDL Criteria Format
- Beginning January 2023 and with a few minor exceptions, all therapeutic categories have the same standardized outline
format. The design of this new format is intended to have a cumulative approach bottom-to-top. The following
scenarios will aid in illustrating this point:
Scenario 1: Clinical PA drug
- All Authorizations
- Clinical PA Criteria
Scenario 2: Clinical PA drug with drug-specific criteria
- All Authorizations
- Drug-Specific Criteria
Scenario 3: Step-Therapy drug
- All Authorizations
- Clinical PA Criteria (if applicable)
- Step Therapy Criteria
Scenario 4: Non-Preferred drug
- All Authorizations
- Clinical PA Criteria (if applicable)
- Step Therapy Criteria (if applicable)
- Non-Preferred Criteria
Scenario 5: Non-Preferred drug with drug-specific criteria
- All Authorizations
- Clinical PA Criteria (if applicable)
- Step Therapy Criteria (if applicable)
- Non-Preferred Criteria
- Additional Drug-Specific Criteria

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 5
Table of Contents
Example Category ......................................................................................................................... 3
Analgesic Agents: Gout ......................................................................................................................... 8
Analgesic Agents: NSAIDS ...................................................................................................................... 8
Analgesic Agents: Opioids ..................................................................................................................... 8
Blood Formation, Coagulation, and Thrombosis Agents: Colony Stimulating Factors ............................... 9
Blood Formation, Coagulation, and Thrombosis Agents: Hematopoietic Agents ...................................... 9
Blood Formation, Coagulation, and Thrombosis Agents: Hemophilia Factor* .......................................... 9
Blood Formation, Coagulation, and Thrombosis Agents: Heparin-Related Preparations ........................ 10
Blood Formation, Coagulation, and Thrombosis Agents: Oral Anticoagulants........................................ 10
Blood Formation, Coagulation, and Thrombosis Agents: Oral Antiplatelet ............................................ 10
Cardiovascular Agents: Antiarrhythmics .............................................................................................. 12
Cardiovascular Agents: Lipotropics ...................................................................................................... 12
Cardiovascular Agents: Pulmonary Arterial Hypertension* ................................................................... 13
Central Nervous System (CNS) Agents: Alzheimer’s Agents* ................................................................. 13
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Cluster Headache ................................... 14
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Prophylaxis ............................................ 14
Central Nervous System (CNS) Agents: Anticonvulsants*...................................................................... 14
Central Nervous System (CNS) Agents: Anticonvulsants Rescue ............................................................ 14
Central Nervous System (CNS) Agents: Antidepressants* ..................................................................... 15
Central Nervous System (CNS) Agents: Attention Deficit Hyperactivity Disorder Agents ........................ 15
Central Nervous System (CNS) Agents: Fibromyalgia Agents ................................................................. 16
Central Nervous System (CNS) Agents: Medication Assisted Treatment of Opioid Addiction.................. 17
Central Nervous System (CNS) Agents: Movement Disorders ................................................................ 17
Central Nervous System (CNS) Agents: Multiple Sclerosis* ................................................................... 17
Central Nervous System (CNS) Agents: Narcolepsy ............................................................................... 17
Central Nervous System (CNS) Agents: Neuropathic Pain ..................................................................... 17
Central Nervous System (CNS) Agents: Parkinson's Agents ................................................................... 18
Central Nervous System (CNS) Agents: Restless Legs Syndrome ............................................................ 18
Central Nervous System (CNS) Agents: Sedative-Hypnotics, Non-Barbiturate ........................................ 18
Central Nervous System (CNS) Agents: Skeletal Muscle Relaxants, Non-Benzodiazepine ....................... 19
Central Nervous System (CNS) Agents: Smoking Deterrents ................................................................. 19
Dermatologic Agents: Oral Acne Products ............................................................................................ 19
Dermatologic Agents: Topical Acne Products ....................................................................................... 19
Endocrine Agents: Androgens .............................................................................................................. 20

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 6
Endocrine Agents: Diabetes – Hypoglycemia Treatments ..................................................................... 20
Endocrine Agents: Diabetes – Insulin ................................................................................................... 20
Endocrine Agents: Diabetes – Non-Insulin ............................................................................................ 21
Endocrine Agents: Endometriosis ........................................................................................................ 21
Endocrine Agents: Estrogenic Agents ................................................................................................... 22
Endocrine Agents: Osteoporosis – Bone Ossification Enhancers ............................................................ 22
Endocrine Agents: Progestin Agents .................................................................................................... 23
Endocrine Agents: Uterine Fibroids ...................................................................................................... 23
Gastrointestinal Agents: Anti-Emetics .................................................................................................. 23
Gastrointestinal Agents: Crohn’s Disease ............................................................................................. 23
Gastrointestinal Agents: Hepatic Encephalopathy ................................................................................ 24
Gastrointestinal Agents: Irritable Bowel Syndrome (IBS) with Diarrhea ................................................ 24
Gastrointestinal Agents: Pancreatic Enzymes ....................................................................................... 24
Gastrointestinal Agents: Proton Pump Inhibitors ................................................................................. 24
Gastrointestinal Agents: Ulcerative Colitis ........................................................................................... 24
Gastrointestinal Agents: Unspecified GI ............................................................................................... 25
Genitourinary Agents: Benign Prostatic Hyperplasia............................................................................. 25
Genitourinary Agents: Electrolyte Depleter Agents .............................................................................. 25
Genitourinary Agents: Urinary Antispasmodics .................................................................................... 25
Immunomodulator Agents: Systemic Inflammatory Disease ................................................................. 26
Infectious Disease Agents: Antibiotics – Cephalosporins ....................................................................... 26
Infectious Disease Agents: Antibiotics – Inhaled ................................................................................... 27
Infectious Disease Agents: Antibiotics – Macrolides ............................................................................. 27
Infectious Disease Agents: Antibiotics – Quinolones ............................................................................. 27
Infectious Disease Agents: Antibiotics – Tetracyclines .......................................................................... 27
Infectious Disease Agents: Antifungals................................................................................................. 27
Infectious Disease Agents: Antivirals – Hepatitis C Agents .................................................................... 27
Infectious Disease Agents: Antivirals – Herpes ..................................................................................... 28
Infectious Disease Agents: Antivirals – HIV* ......................................................................................... 28
Ophthalmic Agents: Antibiotic and Antibiotic-Steroid Combination Drops and Ointments .................... 29
Ophthalmic Agents: Antihistamines & Mast Cell Stabilizers .................................................................. 29
Ophthalmic Agents: Glaucoma Agents ................................................................................................. 30
Ophthalmic Agents: NSAIDs ................................................................................................................ 30
Ophthalmic Agents: Ophthalmic Steroids ............................................................................................. 30
Otic Agents: Antibacterial and Antibacterial/Steroid Combinations ...................................................... 31

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 7
Respiratory Agents: Antihistamines – Second Generation .................................................................... 31
Respiratory Agents: Epinephrine Auto-Injectors ................................................................................... 31
Respiratory Agents: Hereditary Angioedema ....................................................................................... 31
Respiratory Agents: Inhaled Agents ..................................................................................................... 31
Respiratory Agents: Leukotriene Receptor Modifiers & Inhibitors ........................................................ 32
Respiratory Agents: Monoclonal Antibodies-Anti-IL/Anti-IgE ................................................................ 32
Respiratory Agents: Nasal Preparations ............................................................................................... 32
Respiratory Agents: Other Agents ........................................................................................................ 33
Topical Agents: Antifungals ................................................................................................................. 33
Topical Agents: Antiparasitics .............................................................................................................. 33
Topical Agents: Corticosteroids ........................................................................................................... 33
Topical Agents: Immunomodulators .................................................................................................... 34

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 8
Analgesic Agents: Gout
PREFERRED
NON-PREFERRED
Allopurinol 100, 300mg
QL
Allopurinol 200mg
Colchicine Tab
PA QL
Febuxostat
Colcrys Tab
PA QL
Gloperba Susp
QL
Probenecid
QL
Mitigare
BvG
QL
Probenecid/Colchicine
QL
Link to Criteria: Analgesic Agents: Gout
Analgesic Agents: NSAIDS
PREFERRED
NON-PREFERRED
Celecoxib
QL
Diclofenac/Misoprostol
Diclofenac Sodium IR, DR, ER, Gel 1%
Diclofenac Gel 3%, Patch 1.3%, Soln 1.5%, 2%
Etodolac
Diclofenac Potassium
Fenoprofen 600mg
Diclotrex
Flurbiprofen
Elyxyb
Ibuprofen
Fenoprofen 400mg
Indocin
Ibuprofen/Famotidine
Indomethacin
Ketorolac Tromethamine Nasal Spray
Ketoprofen ER
Ketoprofen
Ketorolac
Licart Patch
Meclofenamate
Meloxicam Cap
Mefenamic Acid
Naproxen CR, DR, ER, EC
Meloxicam Tab
Naproxen/Esomeprazole
Nabumetone
Pennsaid
BvG
Naproxen IR
Qmiiz ODT
Naproxen Susp
AR
Relafen DS
Oxaprozin
Zorvolex
Piroxicam
Sulindac
Link to Criteria: Analgesic Agents: NSAIDS
Analgesic Agents: Opioids
PREFERRED
NON-PREFERRED
Acetaminophen/Codeine
QL
Acetaminophen/Caffeine/Dihydrocodeine
QL
Butalbital/Acetaminophen/Caffeine/Codeine
QL
Belbuca
QL
Butalbital/Aspirin/Caffeine/Codeine
QL
Benzhydrocodone/Acetaminophen
QL
Butorphanol
QL
Buprenorphine TD Patch Weekly
QL
Butrans
BvG PA QL
Codeine
QL
Butalbital/Acetaminophen/Caffeine/Codeine
50/300/40/30mg
QL
Hydrocodone/Acetaminophen
QL
Dsuvia
QL
Hydromorphone IR
QL
Fentanyl
QL
Morphine IR Tab, Sol
QL
Hydrocodone Bitartrate ER 12HR Cap
QL
Morphine ER Tab
PA QL
Hydrocodone Bitartrate ER 24HR Tab
QL
Nucynta IR
QL
Nucynta ER
PA QL
Hydrocodone/Acetaminophen 5-300, 7.5-300, 10-
300mg
QL
Oxycodone Cap, Sol, Tab
QL
Hydrocodone/Ibuprofen
QL
Oxycodone/Acetaminophen
QL
Hydromorphone ER
QL
Tramadol
QL
Levorphanol
QL

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 9
Analgesic Agents: Opioids
PREFERRED
NON-PREFERRED
Tramadol/Acetaminophen
QL
Meperidine
QL
Methadone
QL
Morphine ER 24HR Cap
QL
Oxycodone ER
QL
Oxycodone/Ibuprofen
QL
Oxymorphone IR, ER
QL
Link to Criteria: Analgesic Agents: Opioids
Blood Formation, Coagulation, and Thrombosis Agents: Colony Stimulating Factors
PREFERRED
NON-PREFERRED
Neupogen
PA
Fulphila
Nivestym
PA
Fylnetra
Nyvepria
PA
Granix
Ziextenzo
PA
Leukine
Neulasta
Releuko
Rolvedon
Stimufend
Udenyca
Zarxio
Link to Criteria: Blood Formation, Coagulation, and Thrombosis Agents: Colony Stimulating Factors
Blood Formation, Coagulation, and Thrombosis Agents: Hematopoietic Agents
PREFERRED
NON-PREFERRED
Epogen
PA
Aranesp
Mircera
PA
Procrit
Retacrit
PA
Link to Criteria: Blood Agents: Blood Formation, Coagulation, And Thrombosis Agents: Hematopoietic Agents
Blood Formation, Coagulation, and Thrombosis Agents: Hemophilia Factor*
PREFERRED
NON-PREFERRED
Advate
PA
Altuviiio
Adynovate
PA
Jivi
Afstyla
PA
Nuwiq
Alphanate
PA
Obizur
Alphanine SD
PA
Rebinyn
Alprolix
PA
Sevenfact
Benefix
PA
Vonvendi
Corifact
PA
Eloctate
PA
Esperoct
PA
Feiba
PA
Hemlibra
PA
Hemofil M
PA
Humate-P
PA
Idelvion
PA
Ixinity
PA

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 10
Blood Formation, Coagulation, and Thrombosis Agents: Hemophilia Factor*
PREFERRED
NON-PREFERRED
Koate
PA
Kogenate FS
PA
Kovaltry
PA
Mononine
PA
Novoeight
PA
Novoseven RT
PA
Profilnine
PA
Recombinate
PA
Rixubis
PA
Wilate
PA
Xyntha
PA
Link to Criteria: Blood Formation, Coagulation, and Thrombosis Agents: Hemophilia Factors
Blood Formation, Coagulation, and Thrombosis Agents: Heparin-Related Preparations
PREFERRED
NON-PREFERRED
Enoxaparin
Fondaparinux
Fragmin
Link to Criteria: Blood Formation, Coagulation, and Thrombosis Agents: Heparin-Related Preparations
Blood Formation, Coagulation, and Thrombosis Agents: Oral Anticoagulants
PREFERRED
NON-PREFERRED
Eliquis
Dabigatran Cap
Pradaxa Cap
BvG
Pellet Pak
AR
Savaysa
Warfarin
Xarelto Susp
AR
Tab
QL
Link to Criteria: Blood Formation, Coagulation, and Thrombosis Agents: Oral Anticoagulants
Blood Formation, Coagulation, and Thrombosis Agents: Oral Antiplatelet
PREFERRED
NON-PREFERRED
Aspirin
Yosprala
Aspirin/Dipyridamole ER
Zontivity
Brilinta
Clopidogrel
Prasugrel
QL
Link to Criteria: Blood Formation, Coagulation, and Thrombosis Agents: Oral Antiplatelet
Cardiovascular Agents: Angina, Hypertension and Heart Failure
PREFERRED
NON-PREFERRED
Acebutolol
QL
Aliskiren
Amlodipine
QL
Aspruzyo Sprinkle
Amlodipine/Benazepril
Camzyos
Amlodipine/Olmesartan
QL
Candesartan
Amlodipine/Valsartan
Candesartan/HCTZ
Amlodipine/Valsartan/HCTZ
Carospir
Atenolol
QL
Carvedilol ER
Atenolol/Chlorthalidone
Clonidine ER (generic of Nexiclon XR)
Benazepril
Corlanor
Benazepril/HCTZ
Diltiazem 24HR ER Tabs
QL

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 11
Cardiovascular Agents: Angina, Hypertension and Heart Failure
PREFERRED
NON-PREFERRED
Betaxolol
QL
Edarbi
Bisoprolol
QL
Edarbyclor
Bisoprolol/HCTZ
Hydralazine/HCTZ
Bystolic
BvG
Innopran XL
Captopril
Inpefa
Captopril/HCTZ
Isradipine
Cartia XT
Kapspargo
Carvedilol
QL
Katerzia
Clonidine IR, Patch
Kerendia
Diltiazem
QL
Levamlodipine
Diltiazem 12HR ER Cap
QL
Nebivolol
Diltiazem 24HR ER Cap
QL
Nimodipine
Doxazosin
Nisoldipine
Dutoprol
Norliqva
Enalapril Tab
Nymalize
Enalapril/HCTZ
Qbrelis
Enalapril Sol
Sotylize
AR
Entresto
PA
Tekturna/HCTZ
Eplerenone
Telmisartan
Felodipine ER
QL
Telmisartan/HCTZ
Fosinopril
Verapamil 200, 300mg ER 24HR
QL
Fosinopril/HCTZ
Verquvo
Guanfacine
Hemangeol
PA
Hydralazine
Irbesartan
QL
Irbesartan/HCTZ
QL
Labetalol
QL
Lisinopril
Lisinopril/HCTZ
Losartan
QL
Losartan/HCTZ
Methyldopa
Methyldopa/HCTZ
Metoprolol Succinate
QL
Metoprolol Tartrate
QL
Metoprolol/HCTZ
QL
Minoxidil
Moexipril
Nadolol
QL
Nadolol/Bendroflumethiazide
Nicardipine
QL
Nifedipine
QL
Olmesartan
Olmesartan/Amlodipine/HCTZ
Olmesartan/HCTZ

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 12
Cardiovascular Agents: Angina, Hypertension and Heart Failure
PREFERRED
NON-PREFERRED
Propranolol
Propranolol/HCTZ
Quinapril
Quinapril/HCTZ
Ramipril
Ranolazine
Sotalol
QL
Spironolactone
Spironolactone/HCTZ
Telmisartan/Amlodipine
Terazosin
Timolol
QL
Trandolapril
Trandolapril/Verapamil
Valsartan
QL
Valsartan/HCTZ
QL
Verapamil IR, SR
QL
Link to Criteria: Cardiovascular Agents: Angina, Hypertension & Heart Failure
Cardiovascular Agents: Antiarrhythmics
PREFERRED
NON-PREFERRED
Amiodarone 200mg
QL
Amiodarone 100, 400mg
QL
Disopyramide
QL
Multaq
Dofetilide
Flecainide
QL
Mexiletine
QL
Norpace CR
QL
Propafenone IR, ER
QL
Quinidine IR, ER
QL
Link to Criteria: Cardiovascular Agents: Antiarrhythmics
Cardiovascular Agents: Lipotropics
PREFERRED
NON-PREFERRED
Atorvastatin
QL
Altoprev
Cholestyramine Regular, Light
Amlodipine/Atorvastatin
Colestipol Tab
Atorvaliq
Ezetimibe
Colesevelam
Fenofibrate 48, 145mg Tab
QL
Colestipol Granules
Gemfibrozil
QL
Ezallor
Lovastatin
QL
Ezetimibe/Simvastatin
Niacin IR, ER OTC
QL
Fenofibrate Cap
QL
Omega-3-Acid Ethyl Esters
Fenofibrate 40, 54, 120, 160mg Tab
QL
Praluent
PA
Fenofibric Acid
QL
Pravastatin
Fluvastatin
Prevalite
Juxtapid
Repatha
PA
Livalo
Rosuvastatin
QL
Nexletol

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 13
Cardiovascular Agents: Lipotropics
PREFERRED
NON-PREFERRED
Simvastatin
QL
Nexlizet
Niacin ER Tab
QL
Vascepa
BvG
Zypitamag
Link to Criteria: Cardiovascular Agents: Lipotropics
Cardiovascular Agents: Pulmonary Arterial Hypertension*
PREFERRED
NON-PREFERRED
Ambrisentan
PA
Adempas
Sildenafil
PA
Bosentan
Sildenafil Susp
AR PA
Epoprostenol
Tadalafil
PA
Liqrev
Tadliq
AR PA
Opsumit
Tracleer Tab
BvG PA
Orenitram
Tracleer Susp
Treprostinil
Tyvaso
Uptravi
Ventavis
Link to Criteria: Cardiovascular Agents: Pulmonary Arterial Hypertension
Central Nervous System (CNS) Agents: Alzheimer’s Agents*
PREFERRED
NON-PREFERRED
Donepezil 5, 10mg, ODT, Tab
AR QL
Adlarity
AR
Donepezil ODT
AR QL
Donepezil 23mg Tab
AR QL
Galantamine IR Tab, ER Cap
AR QL
Galantamine Sol
AR QL
Memantine Tab
AR
Memantine ER, Sol
AR
Rivastigmine Cap
AR QL
Namzaric
AR
Rivastigmine Patch
AR
Link to Criteria: Central Nervous System (CNS) Agents: Alzheimer’s Agents
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Acute
PREFERRED
NON-PREFERRED
Imitrex Nasal Spray
BvG QL
Almotriptan
Naratriptan
QL
Dihydroergotamine
Nurtec ODT
QL ST
Eletriptan
Rizatriptan
QL
Ergomar
Sumatriptan Inj, Tab
QL
Frovatriptan
Tosymra
BvG QL
Migergot
Onzetra Xsail
QL
Reyvow
Sumatriptan/Naproxen
Sumatriptan Nasal Spray
QL
Trudhesa
Ubrelvy
Zavzpret
Zolmitriptan

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 14
Link to Criteria: Central Nervous System (CNS) Agents: Anti-Migraine Agents, Acute
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Cluster Headache
PREFERRED
NON-PREFERRED
Verapamil
QL
Emgality
QL
Link to Criteria: Central Nervous System (CNS) Agents: Anti-Migraine Agents, Cluster Headache
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Prophylaxis
PREFERRED
NON-PREFERRED
Aimovig
QL
ST
Emgality
QL
Ajovy
QL ST
Nurtec ODT
QL
Cardiovascular Agents: Beta-Blockers
Qulipta
QL
CNS Agents: Anticonvulsants
CNS Agents: Serotonin-Norepinephrine Reuptake Inhibitors
CNS Agents: Tricyclic Antidepressants
Link to Criteria: Central Nervous System (CNS) Agents: Anti-Migraine Agents, Prophylaxis
Link to Criteria: Central Nervous System (CNS) Agents: Anticonvulsants
Central Nervous System (CNS) Agents: Anticonvulsants Rescue
PREFERRED
NON-PREFERRED
Diastat
Diazepam Gel
Central Nervous System (CNS) Agents: Anticonvulsants*
PREFERRED
NON-PREFERRED
Banzel Tab
BvG
Aptiom
Briviact
Briviact
Carbamazepine
Celontin
BvG
Clobazam
Clonazepam ODT
Clonazepam
Elepsia XR
Diacomit
PA QL
Felbamate
Divalproex IR, ER
Fintepla
Epidiolex
ST QL
Lamotrigine ER
Eprontia
AR
Levetiracetam ER Tab
Ethosuximide
Oxcarbazepine Susp
Fycompa
ST
Oxtellar XR
Gabapentin
QL
Peganone
Lacosamide
ST
Qudexy XR
BvG
Lamotrigine IR, ODT
Rufinamide Tab, Soln
Levetiracetam IR Tab, Sol
Spritam
Oxcarbazepine Tab
Sympazan
Phenobarbital
Tiagabine
Phenytoin
Topiramate Sprinkle Cap
Pregabalin
QL
Trokendi XR
BvG
Primidone
Vigabatrin
Topiramate
Vigabatrin Powder
AR
Trileptal Susp
BvG
Xcopri
Valproic Acid
Zonisade Susp
Zonisamide Cap
Ztalmy

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 15
Central Nervous System (CNS) Agents: Anticonvulsants Rescue
PREFERRED
NON-PREFERRED
Nayzilam
AR
Valtoco
AR
Link to Criteria: Central Nervous System (CNS) Agents: Anticonvulsants Rescue
Central Nervous System (CNS) Agents: Antidepressants*
PREFERRED
NON-PREFERRED
Bupropion
QL
Aplenzin
Bupropion SR (generic of Wellbutrin SR)
QL
Auvelity
Bupropion XL (generic of Wellbutrin XL)
QL
Brisdelle
Citalopram Tab, Soln
QL
Bupropion XL (generic of Forfivo XL)
QL
Duloxetine 20, 30, 60mg
QL
Citalopram Cap
Escitalopram
QL
Clomipramine
Fluoxetine 10, 20, 40mg
QL
Desvenlafaxine
Fluoxetine Sol
QL
Drizalma Sprinkle
Fluvoxamine
QL
Duloxetine 40mg
QL
Mirtazapine
QL
Emsam
Nefazodone
QL
Fetzima
Paroxetine IR Tab, Sol
QL
Fluoxetine 60mg, DR
QL
Sertraline Tab
Fluvoxamine ER
QL
Tranylcypromine
Marplan
Trazodone 50, 100, 150mg
QL
Paroxetine Cap, ER Tab
Venlafaxine IR Tab, ER Cap
QL
Pexeva
Phenelzine
Sertraline Cap
Trazodone 300mg
QL
Trintellix
Venlafaxine ER Tab
Viibryd
BvG
Link to Criteria: Central Nervous System (CNS) Agents: Antidepressants
Central Nervous System (CNS) Agents: Attention Deficit Hyperactivity Disorder Agents
PREFERRED
NON-PREFERRED
Amphetamine/Dextroamphetamine IR, ER
AR
QL
Adhansia XR
AR
Atomoxetine Cap
AR QL
Adzenys ER, XR ODT
Clonidine ER
Amphetamine Tab
Concerta
AR QL
Azstarys
AR
Dexmethylphenidate Tab
AR QL
Cotempla XR ODT
AR
Dexmethylphenidate ER (generic of Focalin XR)
AR QL
Daytrana
AR BvG
Dextroamphetamine IR Tab, ER Cap
AR QL
Evekeo ODT
Dextroamphetamine Sol
AR
Jornay PM
AR
Dyanavel XR
AR
Methamphetamine
Guanfacine ER
QL
Methylphenidate Chewable Tab
AR
QL
Methylphenidate ER Cap
AR QL
(generic of Metadate CD,
Ritalin LA)
Methylphenidate ER
AR QL
(generic of Aptensio XR, Relexxii)
Mydayis
QL
Methylphenidate ER Tab
AR QL
(generic of Concerta,
Methylin ER, Ritalin SR)
Vyvanse Chewable Tab
Xelstrym
AR
Zenzedi
AR QL
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 16
Central Nervous System (CNS) Agents: Attention Deficit Hyperactivity Disorder Agents
PREFERRED
NON-PREFERRED
Methylphenidate Sol
AR QL
Methylphenidate Tab
AR QL
Procentra
AR
Qelbree
ST
Quillichew ER
AR
Quillivant XR
AR
Ritalin LA
AR QL
Vyvanse Cap
QL
Link to Criteria: Central Nervous System (CNS) Agents: Attention Deficit Hyperactivity Disorder Agents
Central Nervous System (CNS) Agents: Atypical Antipsychotics*
PREFERRED
NON-PREFERRED
Abilify Maintena
QL
Abilify Asimtufii
Aripiprazole
QL
Abilify Mycite
Aristada
QL
Aripiprazole Sol
Aristada Initio
Asenapine
Clozapine
Caplyta
Fanapt
ST
Clozapine ODT Rapdis
Geodon
QL
Fluoxetine/Olanzapine
Invega Hafyera ER
PA
Lybalvi
Invega Sustenna
QL
Nuplazid
Invega Trinza
QL
Olanzapine ODT
Lurasidone
QL
Rexulti
Olanzapine
QL
Secuado
Paliperidone Tab
Uzedy
Perseris
Versacloz
Quetiapine IR, ER
QL
Vraylar
Risperdal Consta
QL
Zyprexa Relprevv
QL
Risperidone
QL
Saphris
BvG ST
Vraylar
ST
Ziprasidone
QL
Link to Criteria: Central Nervous System (CNS) Agents: Atypical Antipsychotics
Central Nervous System (CNS) Agents: Fibromyalgia Agents
PREFERRED
NON-PREFERRED
Pregabalin
QL
Savella
Link to Criteria: Central Nervous System (CNS) Agents: Fibromyalgia Agents

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 17
Central Nervous System (CNS) Agents: Medication Assisted Treatment of Opioid Addiction
PREFERRED
NON-PREFERRED
Buprenorphine/Naloxone
Buprenorphine
Clonidine
Lucemyra
QL
Sublocade
QL
Suboxone
Vivitrol
Zubsolv
Link to Criteria: Central Nervous System (CNS) Agents: Medication Assisted Treatment of Opioid Addiction
Central Nervous System (CNS) Agents: Movement Disorders
PREFERRED
NON-PREFERRED
Austedo
PA ST
Ingrezza
PA
Tetrabenazine
PA
Link to Criteria: Central Nervous System (CNS) Agents: Movement Disorders
Central Nervous System (CNS) Agents: Multiple Sclerosis*
PREFERRED
NON-PREFERRED
Aubagio
BvG
Bafiertam
Avonex
Extavia
Betaseron
Glatiramer
Copaxone
BvG
Glatopa
Dalfampridine
Kesimpta
Dimethyl Fumarate
Mavenclad
Fingolimod
Mayzent
Gilenya
Plegridy
Kesimpta
Ponvory
Rebif
Tascenso ODT
Teriflunomide
Teriflunomide
Vumerity
Zeposia
Link to Criteria: Central Nervous System (CNS) Agents: Multiple Sclerosis
Central Nervous System (CNS) Agents: Narcolepsy
PREFERRED
NON-PREFERRED
Amphetamine/Dextroamphetamine IR/ER
AR
Sunosi
Armodafinil
Wakix
Dextroamphetamine ER
AR
Xyrem
BvG
Methylphenidate ER
AR
Xywav
Methylphenidate Tab
AR
Modafinil
Link to Criteria: Central Nervous System (CNS) Agents: Narcolepsy
Central Nervous System (CNS) Agents: Neuropathic Pain
PREFERRED
NON-PREFERRED
Amitriptyline
Gralise
Carbamazepine
Horizant
Desipramine
Pregabalin ER

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 18
Central Nervous System (CNS) Agents: Neuropathic Pain
PREFERRED
NON-PREFERRED
Doxepin 10, 25, 50, 75, 100, 150mg
Ztlido
Doxepin Sol
Duloxetine
QL
Gabapentin
QL
Imipramine
Lidocaine Patch
Nortriptyline
Oxcarbazepine
Pregabalin
QL
Ztlido
ST
Link to Criteria: Central Nervous System (CNS) Agents: Neuropathic Pain
Central Nervous System (CNS) Agents: Parkinson's Agents
PREFERRED
NON-PREFERRED
Amantadine
Apokyn
Carbidopa
Carbidopa/Levodopa Dispersible Tab
Carbidopa/Levodopa
Carbidopa/Levodopa/Entacapone
Entacapone
Gocovri
Pramipexole
Inbrija
Ropinirole
Kynmobi
Selegiline
Neupro
Nourianz
Ongentys
Osmolex ER
Pramipexole ER
Rasagiline
Ropinirole ER
Rytary
Tolcapone
Xadago
Zelapar
Link to Criteria: Central Nervous System (CNS) Agents: Parkinson's Agents
Central Nervous System (CNS) Agents: Restless Legs Syndrome
PREFERRED
NON-PREFERRED
Pramipexole
Horizant
Ropinirole
Neupro
Link to Criteria: Central Nervous System (CNS) Agents: Restless Legs Syndrome
Central Nervous System (CNS) Agents: Sedative-Hypnotics, Non-Barbiturate
PREFERRED
NON-PREFERRED
Estazolam
QL
Belsomra
Temazepam 15, 30mg
QL
Dayvigo
Zaleplon
QL
Doxepin 3, 6mg
Zolpidem
QL
Eszopiclone
QL
Intermezzo
Quviviq
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 19
Central Nervous System (CNS) Agents: Sedative-Hypnotics, Non-Barbiturate
PREFERRED
NON-PREFERRED
Ramelteon
Temazepam 7.5, 22mg
QL
Zolpidem ER, SL
Link to Criteria: Central Nervous System (CNS) Agents: Sedative-Hypnotics, Non-Barbiturate
Central Nervous System (CNS) Agents: Skeletal Muscle Relaxants, Non-Benzodiazepine
PREFERRED
NON-PREFERRED
Baclofen Tab
Baclofen Solution
Chlorzoxazone 250, 500mg
QL
Carisoprodol
Cyclobenzaprine 5, 10mg
QL
Chlorzoxazone 375, 750mg
QL
Dantrolene
Cyclobenzaprine 7.5mg
QL
Methocarbamol
QL
Cyclobenzaprine ER
QL
Tizanidine Tab
QL
Fleqsuvy
BvG
Lyvispah
Metaxalone
Orphenadrine
Tizanidine Cap
Link to Criteria: Central Nervous System (CNS) Agents: Skeletal Muscle Relaxants, Non-Benzodiazepine
Central Nervous System (CNS) Agents: Smoking Deterrents
PREFERRED
NON-PREFERRED
Bupropion
QL
Chantix
QL
Nicotine
QL
Varenicline
QL
Link to Criteria: Central Nervous System (CNS) Agents: Smoking Deterrents
Dermatologic Agents: Oral Acne Products
PREFERRED
NON-PREFERRED
Accutane
PA
Absorica
Amnesteem
PA
Absorica LD
Claravis
PA
Isotretinoin
PA
Myorisan
PA
Zenatane
PA
Link to Criteria: Dermatologic Agents: Oral Acne Products
Dermatologic Agents: Topical Acne Products
PREFERRED
NON-PREFERRED
Adapalene Gel 0.1%
AR
Adapalene Cream, Sol 0.1%
AR
Benzoyl Peroxide
Adapalene Gel 0.3%
AR
Clindamycin Gel, Lot, Sol
Adapalene/Benzoyl Peroxide
AR
Clindamycin/Benzoyl Peroxide
Aklief
AR
Erythromycin
Altreno
AR
Erythromycin/Benzoyl Peroxide
Amzeeq
Neuac
Arazlo
AR
Sodium Sulfacetamide
Azelaic Acid Gel

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 20
Dermatologic Agents: Topical Acne Products
PREFERRED
NON-PREFERRED
Sodium Sulfacetamide/Sulfur Cream
Benzoyl Peroxide Foam
Sodium Sulfacetamide/Sulfur Wash Susp
Clindacin Kit
Tretinoin
AR
Clindamycin Foam, Swabs
Clindamycin/Tretinoin
AR
Dapsone Gel
Epsolay
Finacea Foam
Onexton Gel
Ovace Plus
Plixda
AR
Sodium Sulfacetamide/Sulfur Gel
Sodium Sulfacetamide Pads
Tazarotene Cream, Foam, Gel 0.1%
AR
Twyneo
AR
Winlevi
Link to Criteria: Dermatologic Agents: Topical Acne Products
Endocrine Agents: Androgens
PREFERRED
NON-PREFERRED
Androderm
AR PA
Jatenzo
AR
Testosterone Gel 1%
AR PA
Methyltestosterone
AR
Testosterone Gel 1% Pump
AR PA
Natesto
AR
Testopel
AR
Testosterone Cypionate
AR
Testosterone Gel 1.62%, 2%
AR
Testosterone Sol 30mg/ACT
AR
Tlando
AR
Xyosted
AR
Link to Criteria: Endocrine Agents: Androgens
Endocrine Agents: Diabetes – Hypoglycemia Treatments
PREFERRED
NON-PREFERRED
Baqsimi
QL
Glucagon Emerg Kit [Labeler 00548 & 63323]
QL
Glucagen Hypokit
QL
Glucagon Emerg Kit [Labeler 00002]
QL
Gvoke
QL
Zegalogue
QL
Link to Criteria: Endocrine Agents: Diabetes – Hypoglycemia Treatments
Endocrine Agents: Diabetes – Insulin
PREFERRED
NON-PREFERRED
Apidra
Admelog
QL
Humalog 50-50
Afrezza
Humalog 75-25
Basaglar
QL
Humalog U-100 Kwikpen, Vial
QL
Fiasp
QL
Humulin 70-30
Humalog U-100 Tempo Pen
Humulin R U-500
QL
Humalog U-200
QL

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 21
Endocrine Agents: Diabetes – Insulin
PREFERRED
NON-PREFERRED
Insulin Aspart
QL
Humulin N U-100
Insulin Aspart Protamine/Insulin Aspart
Humulin R U-100
Insulin Lispro
QL
Lyumjev
Lantus
BvG QL
Novolin 70-30
Levemir
Novolin N U-100
Novolog 70-30
Novolin R U-100
Novolog U-100
QL
Rezvoglar
Toujeo
Semglee
BvG
QL
Tresiba
BvG ST
Link to Criteria: Endocrine Agents: Diabetes – Insulin
Endocrine Agents: Diabetes – Non-Insulin
PREFERRED
NON-PREFERRED
Acarbose
QL
Adlyxin
Actoplus Met XR
Alogliptin
Byetta
Alogliptin/Metformin
Alogliptin/Pioglitazone
Farxiga
Bydureon Bcise
Glimepiride
QL
Glimepiride/Pioglitazone
Glipizide
QL
Glucophage
Glipizide/Metformin
QL
Glyxambi
Glyburide
QL
Invokamet XR
Glyburide/Metformin
QL
Jentadueto XR
Invokamet
Kombiglyze XR
BvG
Invokana
Metformin ER
QL
(Generic of Fortamet, Glumetza)
Janumet
Metformin Sol
Janumet XR
Mounjaro
Januvia
Onglyza
BvG
Jardiance
Ozempic
Jentadueto
Qtern
Metformin IR, ER
QL
(Generic of Glucophage XR)
Rybelsus
Miglitol
Segluromet
Nateglinide
QL
Soliqua
Pioglitazone
QL
Steglatro
Pioglitazone/Metformin
QL
Steglujan
Repaglinide
Symlinpen
Repaglinide/Metformin
Synjardy XR
Synjardy
Trijardy XR
Tradjenta
Xigduo XR
Trulicity
QL
Xultophy
Victoza
QL
Xigduo XR
Link to Criteria: Endocrine Agents: Diabetes – Non-Insulin
Endocrine Agents: Endometriosis
PREFERRED
NON-PREFERRED
Danazol
ST
Synarel

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 22
Endocrine Agents: Endometriosis
PREFERRED
NON-PREFERRED
Depo-Subq Provera 104
ST
Lupaneta Pack
ST
Lupron Depot
QL
ST
3.75, 11.25mg
Myfembree
QL ST
Orilissa
ST
Zoladex
ST
Link to Criteria: Endocrine Agents: Endometriosis
Endocrine Agents: Estrogenic Agents
PREFERRED
NON-PREFERRED
Climara Pro
QL
Angeliq
Combipatch
QL
Climara
QL
Dotti
QL
Divigel
BvG
Estradiol Cream, Tab
Duavee
Estradiol Patch
QL
Elestrin
BvG
Estring
QL
Estradiol 10mcg Vag Tab
Ethinyl Estradiol/Norethindrone Acetate
Estradiol/Norethindrone Acetate
Lyllana
QL
Estrogel
BvG
Menest
Evamist
Premarin
Femring
Premphase
Menostar
QL
Prempro
Minivelle
QL
Prefest
Vivelle-Dot
QL
Link to Criteria: Endocrine Agents: Estrogenic Agents
Endocrine Agents: Growth Hormone
PREFERRED
NON-PREFERRED
Genotropin
PA
Humatrope
Norditropin
PA
Nutropin
Zomacton
Omnitrope
Saizen
Serostim
Skytrofa
Sogroya
Zomacton
Link to Criteria: Endocrine Agents: Growth Hormone
Endocrine Agents: Osteoporosis – Bone Ossification Enhancers
PREFERRED
NON-PREFERRED
Alendronate Tab
Alendronate Susp
Calcitonin-Salmon
Fosamax Plus D
Forteo
PA QL
Risedronate
Hydroxyprogesterone Caproate
QL
Tymlos
QL
Ibandronate
Link to Criteria: Endocrine Agents: Osteoporosis – Bone Ossification Enhancers

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 23
Endocrine Agents: Progestin Agents
PREFERRED
NON-PREFERRED
Makena
QL
Medroxyprogesterone Acetate Tab
Megestrol
Norethindrone Acetate
Progesterone
Progesterone In Oil
Link to Criteria: Endocrine Agents: Progestin Agents
Endocrine Agents: Uterine Fibroids
PREFERRED
NON-PREFERRED
Lupron Depot
PA
3.75, 11.25mg
Myfembree
PA QL
Oriahnn
PA QL
Link to Criteria: Endocrine Agents: Uterine Fibroids
Gastrointestinal Agents: Anti-Emetics
PREFERRED
NON-PREFERRED
Aprepitant 40, 125mg
Aprepitant 80 mg
Diclegis
BvG
Aprepitant TriPac
Dimenhydrinate
Bonjesta
Diphenhydramine
Doxylamine/Pyridoxine
Emend 125mg Susp
Metoclopramide ODT
Emend 80mg
BvG
Sancuso
Emend TriPac
BvG
Zuplenz
Meclizine
Metoclopramide
Ondansetron
Phosphorated Carbohydrate
Prochlorperazine
Promethazine
Scopolamine
Trimethobenzamide
Link to Criteria: Gastrointestinal Agents: Anti-Emetics
Gastrointestinal Agents: Bowel Preparations
PREFERRED
NON-PREFERRED
Clenpiq
Moviprep
Gavilyte-C
PEG3350-SOD SUL-NACL-KCL-ASB-C 7.5-2.691G
Gavilyte-G
Plenvu
Golytely
SOD SULF-POTASS SULF-MAG SULF Soln
PEG-3350 and Electrolytes 236-22.7G, 420G
Suflave
Suprep
BvG
Sutab
Link to Criteria: Gastrointestinal Agents: Bowel Preparations
Gastrointestinal Agents: Crohn’s Disease
PREFERRED
NON-PREFERRED
Azathioprine
Ortikos ER

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 24
Gastrointestinal Agents: Crohn’s Disease
PREFERRED
NON-PREFERRED
Budesonide ER Cap
Mercaptopurine
Methotrexate
Sulfasalazine
Link to Criteria: Gastrointestinal Agents: Crohn’s Disease
Gastrointestinal Agents: Hepatic Encephalopathy
PREFERRED
NON-PREFERRED
Lactulose
Xifaxan
ST
Link to Criteria: Gastrointestinal Agents: Hepatic Encephalopathy
Gastrointestinal Agents: Irritable Bowel Syndrome (IBS) with Diarrhea
PREFERRED
NON-PREFERRED
Diphenoxylate/Atropine
Alosetron
Loperamide
QL
Viberzi
Xifaxan
ST
Link to Criteria: Gastrointestinal Agents: Irritable Bowel Syndrome (IBS) with Diarrhea
Gastrointestinal Agents: Pancreatic Enzymes
PREFERRED
NON-PREFERRED
Creon
Pancreaze
Zenpep
Pertzye
Viokace
Link to Criteria: Gastrointestinal Agents: Pancreatic Enzymes
Gastrointestinal Agents: Proton Pump Inhibitors
PREFERRED
NON-PREFERRED
Lansoprazole Cap
Aciphex
Nexium Granules
BvG
Dexilant
BvG
Omeprazole Cap
AR
Esomeprazole
Pantoprazole Tab
AR
Esomeprazole Granules
Protonix Pak
AR BvG
Konvomep
Lansoprazole ODT
Omeprazole Tab
AR
Omeprazole/Sodium Bicarbonate
Pantoprazole Packet
Prilosec Susp
Rabeprazole
Link to Criteria: Gastrointestinal Agents: Proton Pump Inhibitors
Gastrointestinal Agents: Ulcerative Colitis
PREFERRED
NON-PREFERRED
Balsalazide Disodium
Dipentum
Budesonide ER Tab
QL
Mesalamine DR Tab 800mg
Mesalamine DR Cap, Tab 1.2gm
Mesalamine Supp
Mesalamine Enema
Uceris Foam
BvG QL
Mesalamine ER Cap 0.375mg
Zeposia

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 25
Gastrointestinal Agents: Ulcerative Colitis
PREFERRED
NON-PREFERRED
Pentasa
BvG
Sulfasalazine
Link to Criteria: Gastrointestinal Agents: Ulcerative Colitis
Gastrointestinal Agents: Unspecified GI
PREFERRED
NON-PREFERRED
Amitiza
ST
Aemcolo
Bisacodyl
Gattex
Casanthranol/Docusate Sodium
Ibsrela
Dicyclomine
Linzess 72mcg
Diphenoxylate/Atropine
Motegrity
Lactulose
Mytesi
Linzess
ST
145, 290mcg
Relistor
Loperamide
Symproic
Lubiprostone
ST
Zorbtive
Movantik
ST
Polyethylene Glycol
Psyllium Fiber
Senna
Trulance
ST
Xifaxan
ST
Link to Criteria: Gastrointestinal Agents: Unspecified GI
Genitourinary Agents: Benign Prostatic Hyperplasia
PREFERRED
NON-PREFERRED
Alfuzosin
Cardura XL
Doxazosin
Dutasteride/Tamsulosin
Dutasteride
Entadfi
Finasteride
Silodosin
Prazosin
Tadalafil
PA
2.5, 5mg
Tamsulosin
Terazosin
Link to Criteria: Genitourinary Agents: Benign Prostatic Hyperplasia
Genitourinary Agents: Electrolyte Depleter Agents
PREFERRED
NON-PREFERRED
Calcium Acetate, Carbonate
Auryxia
Phoslyra
Lanthanum Carbonate
Sevelamer
Velphoro
Link to Criteria: Genitourinary Agents: Electrolyte Depleter Agents
Genitourinary Agents: Urinary Antispasmodics
PREFERRED
NON-PREFERRED
Gelnique
Darifenacin
QL
Myrbetriq Tab
Fesoterodine
Oxybutynin
QL
Gemtesa

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 26
Genitourinary Agents: Urinary Antispasmodics
PREFERRED
NON-PREFERRED
Oxytrol
Myrbetriq Granules
AR
Solifenacin
QL
Tolterodine
Toviaz
BvG
Trospium
QL
Vesicare LS
AR
Link to Criteria: Genitourinary Agents: Urinary Antispasmodics
Immunomodulator Agents: Systemic Inflammatory Disease
PREFERRED
NON-PREFERRED
Adbry
PA
Actemra
Dupixent
PA
Adalimumab-adaz (Generic of Hyrimoz)
Enbrel
PA
Adalimumab-fkjp (Generic of Hulio)
Humira
PA
Amjevita
Kineret
PA
Cibinqo
Otezla
PA
Cimzia
Taltz
PA ST
Cosentyx
Xeljanz IR
PA
Cyltezo
Hadlima
Idacio
Ilumya
Kevzara
Litfulo
Olumiant
Orencia
Rinvoq
Siliq
Simponi
Skyrizi
Sotyktu
Stelara
Tremfya
Xeljanz Sol, XR
Yuflyma
Yusimry
Link to Criteria: Immunomodulator Agents for Systemic Inflammatory Disease
Infectious Disease Agents: Antibiotics – Cephalosporins
PREFERRED
NON-PREFERRED
Cefaclor IR, ER
Cefixime Cap
Cefaclor Susp
AR
Cefixime Susp
AR
Cefadroxil
Cefpodoxime
Cefdinir
Cephalexin 750mg
Cefprozil
Suprax Chewable Tab
AR
Cefprozil Susp
AR
Cefuroxime
Cephalexin 250, 500mg
Link to Criteria: Infectious Disease Agents: Antibiotics – Cephalosporins

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 27
Infectious Disease Agents: Antibiotics – Inhaled
PREFERRED
NON-PREFERRED
Tobramycin
PA QL
Arikayce
Bethkis
QL
Cayston
Kitabis Pak
QL
Tobi Podhaler
QL
Link to Criteria: Infectious Disease Agents: Antibiotics – Inhaled
Infectious Disease Agents: Antibiotics – Macrolides
PREFERRED
NON-PREFERRED
Azithromycin
Eryped
Clarithromycin
Erythrocin Stearate
Erythromycin
Link to Criteria: Infectious Disease Agents: Antibiotics – Macrolides
Infectious Disease Agents: Antibiotics – Quinolones
PREFERRED
NON-PREFERRED
Ciprofloxacin
Baxdela
Ciprofloxacin Susp
AR
Ciprofloxacin ER
Levofloxacin
Moxifloxacin
Ofloxacin
Link to Criteria: Infectious Disease Agents: Antibiotics – Quinolones
Infectious Disease Agents: Antibiotics – Tetracyclines
PREFERRED
NON-PREFERRED
Doxycycline 50, 100mg
Demeclocycline
Doxycycline Syr
AR
Doxycycline 20, 40, 75, 150mg
Minocycline Cap
Doxycycline DR
Tetracycline
Minocycline IR, ER Tab
Vibramycin Susp
AR
Nuzyra
Link to Criteria: Infectious Disease Agents: Antibiotics – Tetracyclines
Infectious Disease Agents: Antifungals
PREFERRED
NON-PREFERRED
Fluconazole
Brexafemme
Flucytosine
Cresemba
Griseofulvin
Itraconazole
Ketoconazole
Noxafil Susp
Terbinafine
Oravig
Posaconazole
Tolsura
Vivjoa
Voriconazole
Link to Criteria: Infectious Disease Agents: Antifungals
Infectious Disease Agents: Antivirals – Hepatitis C Agents
PREFERRED
NON-PREFERRED
Mavyret
PA
Harvoni

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 28
Infectious Disease Agents: Antivirals – Hepatitis C Agents
PREFERRED
NON-PREFERRED
Pegasys
PA
Ledipasvir/Sofosbuvir
Ribavirin
PA
Sovaldi
Sofosbuvir/Velpatasvir
PA
Vosevi
Zepatier
Link to Criteria: Infectious Disease Agents: Antivirals – Hepatitis C Agents
Infectious Disease Agents: Antivirals – Herpes
PREFERRED
NON-PREFERRED
Acyclovir
Famciclovir
Valacyclovir
Sitavig
Link to Criteria: Infectious Disease Agents: Antivirals – Herpes
Infectious Disease Agents: Antivirals – HIV*
PREFERRED
NON-PREFERRED
Abacavir Sulfate
Abacavir Susp
Abacavir/Lamivudine
Abacavir/Lamivudine/Zidovudine
Apretude
Aptivus
Atazanavir Sulfate
Cimduo
Biktarvy
Darunavir
Cimduo
Didanosine
Complera
Edurant
Delstrigo
Efavirenz/Lamivudine/Tenofovir Disoproxil Fumarate
Descovy
Emtricitabine
Dovato
Fosamprenavir
Efavirenz
Fuzeon
Efavirenz/Emtricitabine/Tenofovir
Intelence
BvG
Emtricitabine/Tenofovir Disoproxil Fumarate
Lamivudine Tab
Emtriva
BvG
Lamivudine Sol
AR
Evotaz
Lamivudine/Zidovudine
Genvoya
Nevirapine IR, ER Tab
Isentress
Nevirapine Sol
AR
Isentress Chew Tab
AR
Norvir Powder, Sol
Juluca
Selzentry
BvG
Lopinavir/Ritonavir
Stavudine
Odefsey
Stribild
Pifeltro
Symfi
BvG
Prezcobix
Symfi Lo
BvG
Prezista
BvG
Tybost
Ritonavir Tab
Viracept
Rukobia ER
PA
Symfi
BvG
Symfi Lo
BvG
Symtuza
Temixys
Tenofovir Disoproxil Fumarate 300mg
Tivicay
Tivicay PD

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 29
Infectious Disease Agents: Antivirals – HIV*
PREFERRED
NON-PREFERRED
Triumeq
Triumeq PD
PA
Viread Tab, Powder
Zidovudine
Link to Criteria: Infectious Disease Agents: Antivirals – HIV
Ophthalmic Agents: Antibiotic and Antibiotic-Steroid Combination Drops and Ointments
PREFERRED
NON-PREFERRED
Bacitracin-Polymyxin
Azasite
Ciloxan
Bacitracin
Ciprofloxacin
Besivance
Erythromycin
Blephamide
Gentamicin
Gatifloxacin
Moxifloxacin
Levofloxacin
Neomycin/Polymyxin/Bacitracin
Moxifloxacin (Generic of Moxeza)
Neomycin/Polymyxin/Bacitracin/Hydrocortisone
Neomycin/Polymyxin/Hydrocortisone
Neomycin/Polymyxin/Dexamethasone
Pred-G
Neomycin/Polymyxin/Gramicidin
Sulfacetamide Sodium Ophth Oint 10%
Ofloxacin
Tobradex ST
BvG
Polymyxin/Trimethoprim
Zylet
Sulfacetamide Sodium Ophth Sol 10%
Sulfacetamide/Prednisolone
Tobramycin
Tobramycin/Dexamethasone 0.3/0.1%
Link to Criteria: Ophthalmic Agents: Antibiotic and Antibiotic-Steroid Combination Drops and Ointments
Ophthalmic Agents: Antihistamines & Mast Cell Stabilizers
PREFERRED
NON-PREFERRED
Azelastine
Alocril
Bepreve
BvG
Alomide
Cromolyn
Epinastine
Ketotifen
Zerviate
Olopatadine
Link to Criteria: Ophthalmic Agents: Antihistamines & Mast Cell Stabilizers
Ophthalmic Agents: Dry Eye Treatments
PREFERRED
NON-PREFERRED
Restasis Trays
BvG ST
Cequa
Xiidra
Eysuvis
Miebo
Restasis Multi-Dose
Tyrvaya
Xiidra
Link to Criteria: Ophthalmic Agents: Dry Eye Treatments

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 30
Ophthalmic Agents: Glaucoma Agents
PREFERRED
NON-PREFERRED
Alphagan P 0.1%
Apraclonidine
Alphagan P 0.15%
BvG
Betoptic S
Azopt
BvG ST
Bimatoprost
Betaxolol
Brimonidine 0.15%
Brimonidine 0.2%
Brinzolamide
Carteolol
Iopidine
Combigan
BvG ST
Istalol
Dorzolamide
Lumigan
Dorzolamide/Timolol
Timolol Maleate Droperette
Latanoprost
Travoprost
Levobunolol
Vyzulta
Metipranolol
Xelpros
Rhopressa
Zioptan
BvG
Rocklatan
Simbrinza
Timolol 0.5% Gel, Soln
Travatan Z
BvG ST
Link to Criteria: Ophthalmic Agents: Glaucoma Agents
Ophthalmic Agents: NSAIDs
PREFERRED
NON-PREFERRED
Diclofenac
Acuvail
Flurbiprofen
Bromfenac
Ketorolac
Bromsite
Ilevro
Nevanac
Prolensa
Link to Criteria: Ophthalmic Agents: NSAIDs
Ophthalmic Agents: Ophthalmic Steroids
PREFERRED
NON-PREFERRED
Alrex
BvG
Inveltys
Dexamethasone Sodium Phosphate
Lotemax SM
Difluprednate
Loteprednol
Durezol
Flarex
Fluorometholone
Fml Forte
Fml S.O.P.
Lotemax
BvG
Maxidex
Pred Forte
Pred Mild
Prednisolone Acetate
Prednisolone Sodium Phosphate
Link to Criteria: Ophthalmic Agents: Ophthalmic Steroids

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 31
Otic Agents: Antibacterial and Antibacterial/Steroid Combinations
PREFERRED
NON-PREFERRED
Cipro HC
Ciprofloxacin
Ciprodex
BvG
Ciprofloxacin/Dexamethasone
Cortisporin-TC
Ciprofloxacin/Fluocinolone
Neomycin/Polymyxin B/Hydrocortisone
Ofloxacin
Link to Criteria: Otic Agents: Antibacterial and Antibacterial/Steroid Combinations
Respiratory Agents: Antihistamines – Second Generation
PREFERRED
NON-PREFERRED
Cetirizine Syr, Tab
QL
Cetirizine Chewable
AR
Cetirizine/Pseudoephedrine
Clarinex-D
Loratadine Rapid Dissolve
QL
Desloratadine
Loratadine Syr, Tab
QL
Fexofenadine
Loratadine/Pseudoephedrine
Levocetirizine
Link to Criteria: Respiratory Agents: Antihistamines – Second Generation
Respiratory Agents: Cystic Fibrosis
PREFERRED
NON-PREFERRED
Kalydeco
PA QL
Bronchitol
Orkambi
PA QL
Symdeko
PA QL
Trikafta Pak
AR
, Tab
PA
Link to Criteria: Respiratory Agents: Cystic Fibrosis
Respiratory Agents: Epinephrine Auto-Injectors
PREFERRED
NON-PREFERRED
Epinephrine (labeler 49502)
Epipen
Symjepi
Epipen JR
Link to Criteria: Respiratory Agents: Epinephrine Auto-Injectors
Respiratory Agents: Hereditary Angioedema
PREFERRED
NON-PREFERRED
Haegarda
PA
Berinert
Ruconest
PA
Cinryze
Takhzyro
PA
Icatibant Acetate
Kalbitor
Link to Criteria: Respiratory Agents: Hereditary Angioedema
Respiratory Agents: Inhaled Agents
PREFERRED
NON-PREFERRED
Advair Diskus
BvG
Aerospan HFA
Advair HFA
BvG
Airduo Digihaler, Respiclick
Albuterol HFA
Alvesco
Albuterol Nebulizer Sol 0.021% (0.63mg/3mL),
0.042% (1.25mg/3mL)
AR
Arformoterol Nebulizer Sol
Armonair Digihaler, Respiclick
Albuterol Nebulizer Sol 0.083% (2.5mg/3mL), 0.5%
(5mg/mL) Conc
Arnuity Ellipta
Asmanex HFA
Albuterol Nebulizer Sol 0.083% (2.5mg/3mL), 0.5%
Bevespi Aerosphere

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 32
Respiratory Agents: Inhaled Agents
PREFERRED
NON-PREFERRED
Anoro Ellipta
Breo Ellipta
BvG
Asmanex Twisthaler
Breztri Aerosphere
Atrovent HFA
QL
Budesonide/Formoterol
QL
Budesonide Nebulizer Sol
AR QL
Duaklir Pressair
Combivent Respimat
Fluticasone/Salmeterol
Cromolyn Neb Sol
Formoterol Fumarate Nebulizer Sol
Dulera
Levalbuterol Nebulizer Sol
Flovent
BvG QL
Lonhala Magnair
Incruse Ellipta
Proair Digihaler, Respiclick
Ipratropium
Qvar
QL
Ipratropium/Albuterol Nebulizer Sol
QL
Tiotropium Inhaled Caps
Proair HFA
Trelegy Ellipta
Proventil HFA
Tudorza
Pulmicort Flexhaler
QL
Wixela Inhub
Serevent Diskus
Xopenex HFA
Spiriva
BvG QL
Yupelri
Stiolto
Striverdi Respimat
Symbicort
BvG QL
Ventolin HFA
Link to Criteria: Respiratory Agents: Inhaled Agents
Respiratory Agents: Leukotriene Receptor Modifiers & Inhibitors
PREFERRED
NON-PREFERRED
Montelukast
QL
Zileuton
Zafirlukast
ST
Zyflo
Link to Criteria: Respiratory Agents: Leukotriene Receptor Modifiers & Inhibitors
Respiratory Agents: Monoclonal Antibodies-Anti-IL/Anti-IgE
PREFERRED
NON-PREFERRED
Dupixent
PA
Nucala
Fasenra
PA
Tezspire
Xolair
PA
Link to Criteria: Respiratory Agents: Monoclonal Antibodies-Anti-IL/Anti-IgE
Respiratory Agents: Nasal Preparations
PREFERRED
NON-PREFERRED
Azelastine
Azelastine/Fluticasone Spray
Flunisolide
Beconase AQ
Fluticasone (Generic of Flonase)
Budesonide
Ipratropium
QL
Mometasone
Olopatadine
Omnaris
Qnasl
Ryaltris
Xhance
Zetonna
Link to Criteria: Respiratory Agents: Nasal Preparations

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 33
Respiratory Agents: Other Agents
PREFERRED
NON-PREFERRED
Roflumilast
Link to Criteria: Respiratory Agents: Other Agents
Topical Agents: Antifungals
PREFERRED
NON-PREFERRED
Alevazol
Butenafine
Ciclopirox
Ciclopirox Kit
Clotrimazole
Ertaczo
Clotrimazole/Betamethasone
Jublia
Econazole
Ketoconazole Foam
Ketoconazole
Luliconazole
Miconazole
Miconazole/Zinc Oxide/White Petrolatum Oint
Nystatin
Naftifine
Nystatin/Triamcinolone
Oxiconazole
Terbinafine
Tavaborole
Tolnaftate
Link to Criteria: Topical Agents: Antifungals
Topical Agents: Antiparasitics
PREFERRED
NON-PREFERRED
Natroba
BvG
Eurax
Permethrin
Ivermectin Lot
Piperonyl Butoxide/Pyrethrins
Malathion
Vanalice
Spinosad
Link to Criteria: Topical Agents: Antiparasitics
Topical Agents: Corticosteroids
PREFERRED
NON-PREFERRED
Amcinonide
Alclometasone
Betamethasone Dip/Calcipotriene Oint
Apexicon E
Betamethasone Valerate
Betamethasone Dipropionate
Clobetasol Propionate
Betamethasone Dipropionate/Calcipotriene Susp
Derma-Smoothe/FS
BvG
Betamethasone Valerate Aerosol Foam
Desonide Cream, Oint
Bryhali
Diflorasone Diacetate
Clocortolone Pivalate
Fluocinolone Acetonide 0.01% Cream, Sol, 0.05%
Cordran Tape
Flurandrenolide
Desonate Gel
Fluticasone Propionate Cream, Oint
Desonide Lotion
Hydrocortisone
Desoximetasone
Mometasone Furoate
Fluocinolone Acetonide 0.01% Oil
Prednicarbate
Fluocinolone Acetonide 0.025%, 0.1%
Triamcinolone Cream, Lotion, Oint
Fluticasone Propionate Lotion
Halcinonide Cream
Halobetasol Propionate
Halog
Hydrocortisone Butyrate, Valerate

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 34
Topical Agents: Corticosteroids
PREFERRED
NON-PREFERRED
Impeklo
Pandel
Triamcinolone Spray
Link to Criteria: Topical Agents: Corticosteroids
Topical Agents: Immunomodulators
PREFERRD
NON-PREFERRED
Elidel
AR BvG ST
Eucrisa
Tacrolimus
AR ST
Hyftor
Opzelura
Pimecrolimus
AR
Vtama
Zoryve
Link to Criteria: Topical Agents: Immunomodulators

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 35
Ohio
Medicaid
Pharmacy Benefit Management Program
Unified Preferred Drug
List
Medicaid Fee-for-Service
and Managed Care
Plans
Effective January 1, 2024

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 36
Helpful Links
Prior Authorization (PA)
Prior Authorization (PA) Information | pharmacy.medicaid.ohio.gov
• General Prior Authorization Requirements
• PA and Step Therapy Frequently Asked Questions
(FAQ)
Unified Preferred Drug List (UPDL)
Ohio Unified Preferred Drug List | pharmacy.medicaid.ohio.gov
• Unified Preferred Drug List (UPDL)
Terminology/Abbreviations:
AR (Age Restriction) – An edit allowing claims for members within a defined age range to be covered without PA
BvG (Brand Preferred Over the Generic) – The brand name drug is preferred over the generic equivalent
PA (Clinical Prior Authorization) – A prior authorization (PA) is required before the drug will be covered
QL (Quantity Limit) – A limit on the quantity that will be covered within a given time frame
General Information
- The Statewide UPDL is not an all-inclusive list of drugs covered by Ohio Department of Medicaid.
- Medications that are new to market will be non-preferred, PA required until reviewed by the Ohio Department of
Medicaid Pharmacy and Therapeutics (P&T) Committee.
- The document is listed in sections defined by therapeutic class. Drugs are listed by generic name if a generic is
available unless the brand name of the drug is preferred. In most cases, when a generic for a brand-name drug is
available, the generic drug will be preferred, and the brand name will be non‐preferred. Some drugs may also require
a specific manufacturer or the brand to be dispensed.
- Ohio Department of Medicaid will only cover drugs that are part of the Medicaid Drug Rebate Program, with limited
exceptions. This document may not reflect the most current rebate status of a drug (i.e., a drug may be listed on the
document but is non-rebateable and therefore non-payable).
- Some therapeutic categories are grandfathered. These categories will be denoted with an “*” next to their title on the
table on contents and their place within the criteria document.
- Some therapeutic categories may have quantity limits on specific drugs detailed in the criteria document, however
this is not an all-inclusive list. For a list of the quantity limits on specific drugs, please reference the Quantity Limit
Document found here: Quantity Limits Document | pharmacy.medicaid.ohio.gov

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 38
New UPDL Criteria Format
- With a few minor exceptions, all therapeutic categories have the same standardized outline format. The design of this
new format is intended to have a cumulative approach bottom-to-top.
Example Category
LENGTH OF AUTHORIZATIONS: X days or Initial: X days; Subsequent: X days (if different)
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically approved to continue the
drug. Patients who have taken the drug previously, but do not have claims history (e.g. new to Medicaid), will need to submit
a prior authorization in order to continue coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA (if applicable):
“DRUG” CRITERIA (if applicable):
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least X days with at least X preferred drugs
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient cannot be changed to a
preferred drug (i.e., allergies, drug-drug interactions, contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical necessity for why patient
cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least X days with X preferred drugs
o For non-preferred extended-release formulations: must provide documentation of an inadequate clinical
response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide documentation of an inadequate
clinical response or allergy to two or more generic labelers (if available)
ADDITIONAL “DRUG” CRITERIA (if applicable):
ADDITIONAL INFORMATION (if applicable):
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s response to treatment from baseline and/or attestation of clinical
stabilization
QL – Drug: X doses per X days
AR – a PA is required for patients X years and older OR younger than X years

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 39
Interpretation of New UPDL Criteria Format
- Beginning January 2023 and with a few minor exceptions, all therapeutic categories have the same standardized outline
format. The design of this new format is intended to have a cumulative approach bottom-to-top. The following
scenarios will aid in illustrating this point:
Scenario 1: Clinical PA drug
- All Authorizations
- Clinical PA Criteria
Scenario 2: Clinical PA drug with drug-specific criteria
- All Authorizations
- Drug-Specific Criteria
Scenario 3: Step-Therapy drug
- All Authorizations
- Clinical PA Criteria (if applicable)
- Step Therapy Criteria
Scenario 4: Non-Preferred drug
- All Authorizations
- Clinical PA Criteria (if applicable)
- Step Therapy Criteria (if applicable)
- Non-Preferred Criteria
Scenario 5: Non-Preferred drug with drug-specific criteria
- All Authorizations
- Clinical PA Criteria (if applicable)
- Step Therapy Criteria (if applicable)
- Non-Preferred Criteria
- Additional Drug-Specific Criteria

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 40
Table of Contents
Example Category ....................................................................................................................... 38
Analgesic Agents: Gout ............................................................................................................... 43
Analgesic Agents: NSAIDs ........................................................................................................... 44
Analgesic Agents: Opioids ........................................................................................................... 45
Blood Formation, Coagulation, and Thrombosis Agents: Colony Stimulating Factors .................... 48
Blood Formation, Coagulation, and Thrombosis Agents: Hematopoietic Agents ........................... 49
Blood Formation, Coagulation, and Thrombosis Agents: Hemophilia Factors* .............................. 50
Blood Formation, Coagulation, and Thrombosis Agents: Heparin-Related Preparations ................ 51
Blood Formation, Coagulation, and Thrombosis Agents:
Or
al Anticoagulants ............................... 52
Blood Formation, Coagulation, and Thrombosis Agents:
Or
al Antiplatelet .................................... 53
Cardiovascular Agents: Angina, Hypertension & Heart Failure ...................................................... 54
Cardiovascular Agents: Antiarrhythmics ..................................................................................... 56
Cardiovascular Agents: Lipotropics ............................................................................................. 57
Cardiovascular Agents: Pulmonary Arterial Hypertension* .......................................................... 59
Central Nervous System (CNS) Agents: Alzheimer’s Agents* ....................................................... 60
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Acute ........................................... 61
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Cluster Headache .......................... 61
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Prophylaxis ................................... 62
Central Nervous System (CNS) Agents: Anticonvulsants* ............................................................ 64
Central Nervous System (CNS) Agents: Anticonvulsants Rescue .................................................. 66
Central Nervous System (CNS) Agents: Antidepressants*............................................................ 67
Central Nervous System (CNS) Agents: Attention Defic
it
Hyperactivity Disorder Age
nts
............... 69
Central Nervous System (CNS) Agents: Antipsychotics* .............................................................. 70
Central Nervous System (CNS) Agents: Fibromyalgia Agents ....................................................... 72
Central Nervous System (CNS) Agents: Medication
Assisted
Treatment of Opioid
Addiction
........ 73
Central Nervous System (CNS) Agents: Movement Disorders ....................................................... 75
Central Nervous System (CNS) Agents: Multiple Sclerosis*.......................................................... 76
Central Nervous System (CNS) Agents: Narcolepsy ..................................................................... 77
Central Nervous System (CNS) Agents: Neuropathic Pain ............................................................ 78
Central Nervous System (CNS) Agents: Parkinson's Agents .......................................................... 79
Central Nervous System (CNS) Agents: Restless
L
egs
Synd
rome ................................................... 80
Central Nervous System (CNS) Agents: Sedative-Hypnotics, Non-Barbiturate ............................... 81
Central Nervous System (CNS) Agents: Skeletal
Mus
cle Relaxants,
Non
-
Ben
z
odia
zep
ine
.............. 82
Central Nervous System (CNS) Agents: Smoking Deterrents ........................................................ 83
Dermatologic Agents: Oral Acne Products .................................................................................. 84
Dermatologic Agents: Topical Acne Products ............................................................................... 85
Endocrine Agents: Androgens ..................................................................................................... 86
Endocrine Agents: Diabetes – Hypoglycemia Treatments ............................................................ 87
Endocrine Agents: Diabetes – Insulin ......................................................................................... 88
Endocrine Agents: Diabetes –
Non
-
Insulin
.................................................................................. 89
Endocrine Agents: Endometriosis ................................................................................................ 91
Endocrine Agents: Estrogenic
A
gen
ts
......................................................................................... 92
Endocrine Agents: Growth Hormone .......................................................................................... 93

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 41
Endocrine Agents: Osteoporosis – Bone
Ossi
fic
ation
Enh
ancers .................................................. 95
Endocrine Agents: Progestin Agents ........................................................................................... 96
Endocrine Agents: Uterine Fibroids ............................................................................................ 97
Gastrointestinal Agents: Anti-Emetics ........................................................................................ 98
Gastrointestinal Agents: Bowel Preparations............................................................................... 99
Gastrointestinal Agents: Crohn’s Disease ................................................................................. 100
Gastrointestinal Agents: Hepatic Encephalopathy .................................................................... 101
Gastrointestinal Agents: Irritable Bowel Syndrome (IBS) with Diarrhea ..................................... 102
Gastrointestinal Agents: Pancreatic Enzymes ........................................................................... 103
Gastrointestinal Agents: Proton Pump
Inhibitors
...................................................................... 104
Gastrointestinal Agents: Ulcerative Colitis ................................................................................ 105
Gastrointestinal Agents: Unspecified GI ................................................................................... 106
Genitourinary Agents: Benign Prostatic Hyperplasia ................................................................. 107
Genitourinary Agents: Electrolyte Depleter Agents ................................................................... 108
Genitourinary Agents: Urinary Antispasmodics ........................................................................ 109
Immunomodulator Agents: Systemic Inflammatory Disease....................................................... 110
Infectious Disease Agents: Antibiotics – Cephalosporins ........................................................... 112
Infectious Disease Agents: Antibiotics – Inhaled ........................................................................ 113
Infectious Disease Agents: Antibiotics – Macrolides .................................................................. 114
Infectious Disease Agents: Antibiotics – Quinolones ................................................................. 115
Infectious Disease Agents: Antibiotics – Tetracyclines ................................................................ 116
Infectious Disease Agents: Antifungals ..................................................................................... 117
Infectious Disease Agents: Antivirals – Hepatitis C Agents ......................................................... 118
Infectious Disease Agents: Antivirals – Herpes .......................................................................... 119
Infectious Disease Agents: Antivirals – HIV* ............................................................................. 120
Ophthalmic Agents: Antibiotic and
Antibiotic
-
St
e
roid
Combination Drops and
Ointm
e
nts
......... 121
Ophthalmic Agents: Antihistamines & Mast Cell Stabilizers ....................................................... 122
Ophthalmic Agents: Dry Eye Treatments .................................................................................. 123
Ophthalmic Agents: Glaucoma Age
nts
..................................................................................... 124
Ophthalmic Agents: NSAIDs ..................................................................................................... 125
Ophthalmic Agents: Ophthalmic Steroids ................................................................................. 126
Otic Agents: Antibacterial and
Antibact
e
rial/Steroid Combinations
........................................... 127
Respiratory Agents: Antihistamines – Second Generation ......................................................... 128
Respiratory Agents: Cystic Fibrosis ............................................................................................ 129
Respiratory Agents: Epinephrine Auto-Injectors ........................................................................ 130
Respiratory Agents: Hereditary Angioedema ............................................................................. 131
Respiratory Agents: Inhaled Agents .......................................................................................... 132
Respiratory Agents: Leukotriene Receptor Modifiers & Inhibitors .............................................. 133
Respiratory Agents: Monoclonal Antibodies-Anti-IL/Anti-IgE ..................................................... 134
Respiratory Agents: Nasal Preparations .................................................................................... 135
Respiratory Agents: Other Agents ............................................................................................ 136
Topical Agents: Antifungals ..................................................................................................... 137
Topical Agents: Antiparasitics .................................................................................................. 138
Topical Agents: Corticosteroids ................................................................................................ 139

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 42
Topical Agents: Immunomodulators ........................................................................................ 140

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 43
Analgesic Agents: Gout
LENGTH OF AUTHORIZATIONS: 365 days except 180 days for Familial Mediterranean Fever
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must have had an inadequate clinical response with an NSAID and oral corticosteroid within
the last 30 days for acute gout diagnosis OR
• Must have had an inadequate clinical response of at least 30 days with the maximally
tolerated xanthine oxidase inhibitor dose for chronic gout diagnosis
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL COLCHICINE CAPSULE (MITIGARE) CRITERIA:
• Must have had an inadequate clinical response of 30 days with colchicine tablets
ADDITIONAL COLCHICINE SOLUTION (GLOPERBA) CRITERIA:
• Must be unable to swallow tablets or capsules for authorization of colchicine solution
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
QL – All colchicine products: 6 doses per claim for acute gout; 2 doses per day for 30 days for chronic
gout; 4 doses per day per 30 days for Familial Mediterranean Fever
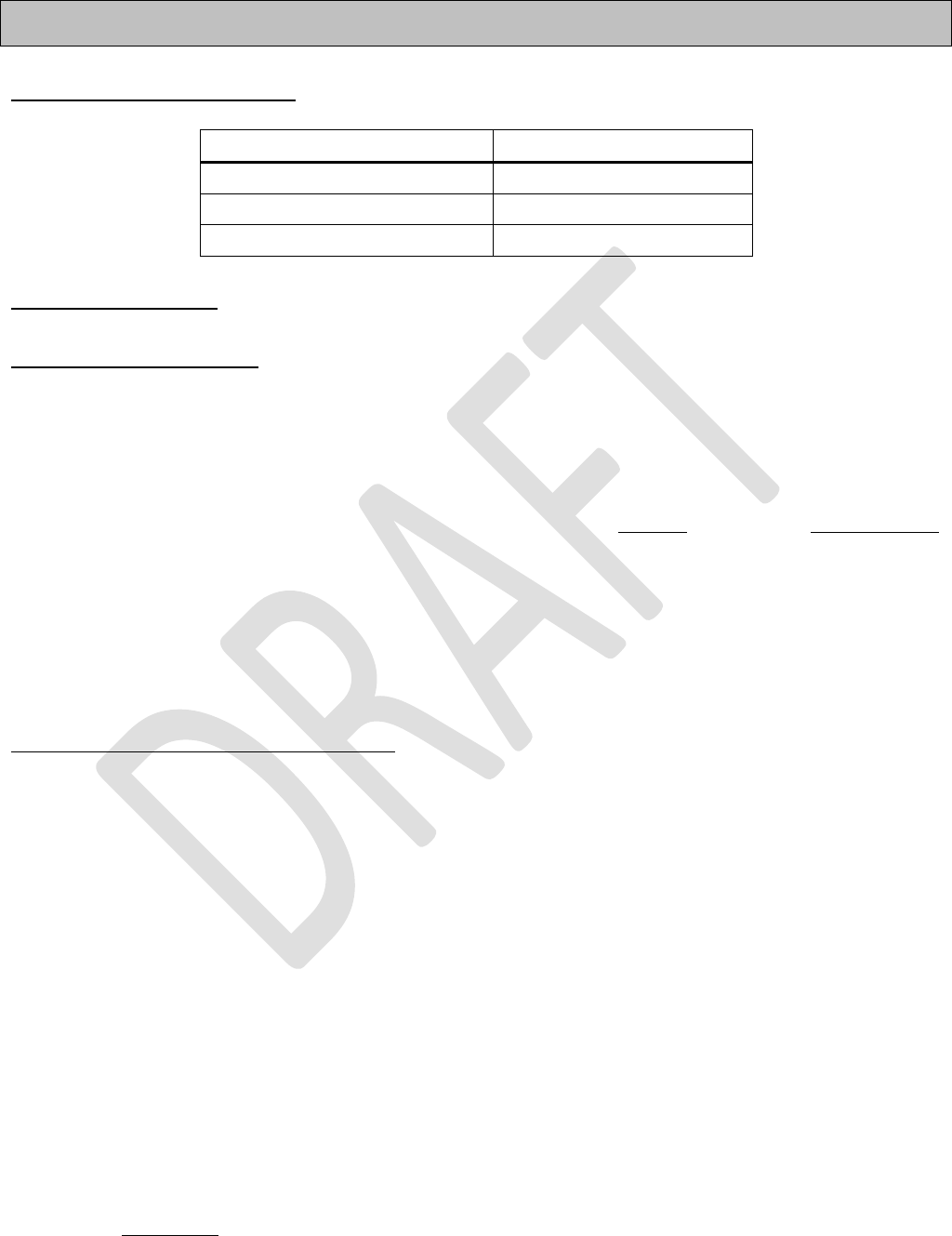
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 44
Analgesic Agents: NSAIDs
LENGTH OF AUTHORIZATIONS: Dependent upon the table below
Authorization Length
H. Pylori Treatment
30 days
Transdermal/Topical
90 days
All Other Treatments
365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Naproxen Suspension: a PA is required for patients 12 years old and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 45
Analgesic Agents: Opioids
**Ohio law requires prescribers to request and review an OARRS report before initially prescribing or personally
furnishing any controlled substance, such as an opioid analgesic or a benzodiazepine, and gabapentin**
LENGTH OF AUTHORIZATIONS: For the course of therapy, up to 180 days. Initial short-acting and
long-acting requests may only be authorized for up to 90 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
BUPRENORPHINE TOPICAL (BUTRANS) CRITERIA:
•
For doses greater than 5 mcg/hour must provide documentation of an
inadequate clinical response
with at least one opioid formulation taken for at
least 60 of the last 90 days
MORPHINE SULFATE ER (KADIAN, MS CONTIN) & TAPENTADOL ER (NUCYNTA) CRITERIA:
•
Unless receiving for cancer pain, palliative care, or end-of-life/hospice care,
must provide documentation of an inadequate clinical response with at least
one opioid formulation taken for at least 60 of the last 90 days
•
Must also meet
LONG-ACTING OPIOID CRITERIA
NON-PREFERRED CRITERIA:
•
Must provide documentation of medical necessity beyond convenience for why the
patient cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o
For any nonsolid oral dosage formulation: must provide documentation of
medical necessity for why patient cannot be changed to a solid oral dosage
formulation
•
Must have had
an inadequate clinical response of at least 7 days of at least two unrelated
preferred drugs of the same duration of action (SHORT-ACTING or LONG-ACTING)
o
For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more
generic labelers (if available)
•
Must also meet applicable SHORT-ACTING or LONG-ACTING OPIOID CRITERIA
ADDITIONAL SHORT-ACTING OPIOIDS CRITERIA:
•
The system defines an “initial request” as having no opioid claims in the previous 90 days
•
Initial short-acting requests can be authorized up to 90 days
o
Length of authorization is dependent on indication, previous patient utilization, and
requested length of therapy (could be more restrictive)
o
To exceed acute opioid limits, documentation of the following must be provided:
▪ Diagnosis code which must be for somatic type pain
▪ Prescriber attestation that the benefits and risks of opioid therapy have been

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 46
discussed with patient
o
Exemptions to the additional criteria:
▪ Patients receiving short-acting opioids for active cancer treatment, palliative
care, and end-of-life/hospice care, sickle cell, severe burn, traumatic
crushing of tissue, amputation, major orthopedic surgery
▪ Prescriber attestation that patient is opioid tolerant (i.e., new to Medicaid or
was on higher dose in hospital)
•
Subsequent short-acting requests can be authorized up to 180 days
o
Documentation of the following must be provided:
▪ Current treatment plan
▪ Demonstrated adherence to treatment plan through progress notes,
including pain and function scores, random urine screenings results
reviewed, concerns addressed, and no serious adverse outcomes observed
•
Dose escalation requests can be authorized up to 180 days
o
Documentation of the following must be provided:
▪ Prescriber attestation that dose escalation is likely to result in improved
function or pain control
▪ Requests for a cumulative daily dose > 80 MED must be prescribed by or in
consultation with a pain specialist, specialist in the area of the body
affected by pain, or anesthesiologist
Patients with initial prescriptions for opioid therapy, defined as no rx claims for opioids in the last 90
days, will be limited to 30 MED per
day and a maximum of 7 days per prescription. Prior
authorization will be required to exceed these limits.
ADDITIONAL LONG-ACTING OPIOIDS CRITERIA:
•
The system defines an “initial long-acting request” as having no opioid claims in the previous
90 days
•
Initial long-acting requests can be authorized up to 90 days
o
Documentation of the following must be provided:
▪ Request is a daily dose equivalent of ≤ 80 MED
▪ Inadequate clinical response to both non-opioid pharmacologic and non-
pharmacologic treatments
▪ Current use of opioids for ≥ 60 of the last 90 days
▪
Treatment plan including risk assessment, substance abuse history,
concurrent therapies, and requirements for random urine screenings
(baseline urine drug tests must be submitted)
▪ Pain and function scores at each visit
▪ Opioid contract required to be in place and submitted with PA form
o
Exemptions to the additional criteria:
▪ Patients receiving long-acting opioids for cancer pain, palliative care, or end-of-
life/hospice care

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 47
•
Subsequent long-acting requests can be authorized up to 180 days
o
Documentation of the following must be provided:
▪ Current treatment plan
▪ Demonstrated adherence to treatment plan through progress notes,
including pain and function scores, random urine screenings results
reviewed, concerns addressed, and no serious adverse outcomes observed
•
Dose escalation requests can be authorized up to 180 days
o
Documentation of the following must be provided:
▪ Prescriber attestation that dose escalation is likely to result in improved
function or pain control
▪ Requests for a cumulative daily dose > 80 MED must be prescribed by or in
consultation with a pain specialist, specialist in the area of the body
affected by pain, or anesthesiologist
ADDITIONAL TRANSMUCOSAL FENTANYL CRITERIA:
• Must be prescribed by an oncologist, pain specialist, or hospice/palliative prescriber
• Must be concurrently taking a long-acting opioid at a therapeutic dose of any of the
following for at least 7 days without adequate pain relief:
≥ 60 mg oral morphine/day
≥ 8 mg oral hydromorphone/day
≥ 25 mcg/hr transdermal fentanyl
≥ 25 mg oral oxymorphone/day
≥ 30 mg oral oxycodone/day
Equianalgesic dose of another opioid
BUPRENORPHINE BUCCAL FILM (BELBUCA) CRITERIA:
• Must meet ADDITIONAL LONG-ACTING OPIOID Criteria
QL – Transmucosal Fentanyl: 4 doses per day

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 48
Blood Formation, Coagulation, and Thrombosis Agents: Colony
Stimulating Factors
LENGTH OF AUTHORIZATIONS: Dependent upon diagnosis below
Diagnosis
Authorization Length
Acute Myeloid Leukemia (AML)
14 days or duration of
chemotherapy regimen
Malignancy at risk for febrile neutropenia or undergoing
myeloablative chemotherapy prior to allogeneic or autologous
bone marrow transplantation
14 days or duration of
chemotherapy regimen
Myeloid Engraftment for bone marrow transplant (BMT)
30 days
Severe, chronic neutropenia with absolute neutrophil count
(ANC) of less than 500/mm
3
and have symptoms associated
with neutropenia (e.g., fever, infections, oropharyngeal ulcers).
30 days
Hematopoietic radiation injury syndrome
30 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must provide documentation of diagnosis, patient’s weight, and duration of treatment
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least
14 days with
at least
one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 49
Blood Formation, Coagulation, and Thrombosis Agents:
Hematopoietic Agents
LENGTH OF AUTHORIZATIONS: Dependent upon diagnosis below
Authorization of epoetin alfa or darbepoetin:
Diagnosis
Hemoglobin
Level
Authorization Length
Anemia due to chronic renal failure, patient on dialysis
≤11
365 days
Anemia due to chronic renal failure, patient not on dialysis
≤10
365 days
Chemotherapy-induced anemia
≤10
90 days
Anemia in myelodysplastic syndrome
≤11
180 days
Authorization of epoetin alfa ONLY:
Diagnosis
Hemoglobin
Level
Authorization
Length
Autologous blood donation, patient will require blood
transfusions
>10 to ≤13
30 days
Anemia of prematurity, age ≤6 months
N/A
42 days
Anemia associated with chronic inflammatory disorders
(e.g., rheumatoid arthritis)
≤
11
180 days
Anemia associated with ribavirin combination therapy in
hepatitis C-infected patient
≤11
180 days
Anemia in zidovudine-treated HIV-infected patients
≤11
180 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least
14 days with
at least
one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 50
Blood Formation, Coagulation, and Thrombosis Agents: Hemophilia
Factors*
LENGTH OF AUTHORIZATIONS: 365 Days
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
authorized to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must provide documentation of patient’s body weight
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least
14 days with
at least
one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL EXTENDED HALF-LIFE FACTOR CRITERIA
• Must provide attestation that the patient is not a suitable candidate for treatment with a
shorter-acting half-life drug
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 51
Blood Formation, Coagulation, and Thrombosis Agents: Heparin-
Related Preparations
LENGTH OF AUTHORIZATIONS: Dependent upon criteria below
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:b
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least
14 days with
at least
one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION:
• For most indications: Guidelines from the American College of Chest Physicians limit duration
of therapy in the outpatient setting for most indications to less than 35 days and patients
should be transitioned to oral anticoagulant as soon as possible
• For requests over 35 days and/or the patient cannot be transitioned to an oral anticoagulant,
prescriber must submit additional documentation for reasoning:
o For patients with cancer – authorized up to 180 days
o For pregnant women – authorized up to 280 days
o For patients unable to take an oral anticoagulant – authorized up to 180 days
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 52
Blood Formation, Coagulation, and Thrombosis Agents:
Or
al
Anticoagulants
LENGTH OF AUTHORIZATION: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least
14 days with
at least
two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – All drugs: a PA is required for patients older than 12 years old

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 53
Blood Formation, Coagulation, and Thrombosis Agents:
Or
al
Antiplatelet
LENGTH OF AUTHORIZATION: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least
14 days with
at least
two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 54
Cardiovascular Agents: Angina, Hypertension & Heart Failure
LENGTH OF AUTHORIZATIONS: 365 days except nimodipine: 21 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
PROPRANOLOL ORAL SOLUTION (HEMANGEOL) CRITERIA:
• Must provide documentation of the patient’s weight
SACUBITRIL/VALSARTAN (ENTRESTO) CRITERIA:
• Must provide documentation of chronic heart failure classified as either NYHA Class II-IV or
ACC/AHA Stage B-D
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days of at least two preferred
drugs within the same class, if indicated for diagnosis
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL FINERENONE (KERENDIA) CRITERIA:
• Must be on a maximally tolerated dose of an angiotensin-converting enzyme inhibitor or
angiotensin receptor blocker
• Must provide documentation of an inadequate clinical response to a SGLT2 Inhibitor OR
provide documentation of medical necessity beyond convenience for why the patient cannot
try a SGLT2 inhibitor (i.e., chronic kidney disease diagnosis)
ADDITIONAL MAVACAMTEN (CAMZYOS) CRITERIA:
• Must be prescribed by or in consultation with a cardiologist
• Must provide documentation of NYHA Class II-III symptoms and left ventricular ejection
fraction ≥55%
ADDITIONAL SOTAGLIFLOZIN (INPEFA) CRITERIA:
• Must provide documentation of an inadequate clinical response to at least two SGLT2
Inhibitors

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 55
ADDITIONAL VERICIGUAT (VERQUVO) CRITERIA:
• Must provide documentation of ejection fraction
• Must have been hospitalized for the treatment of heart failure in the previous 180 days or
needs treatment with an outpatient intravenous diuretic in the previous 90 days
• Must be treated with an agent from ALL the following unless contraindicated:
o Angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, OR an
angiotensin receptor neprilysin inhibitor
o Beta-blocker
o Aldosterone antagonist and/or SGLT2 inhibitor as appropriate for renal function
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Sotylize Solution: a PA is required for patients 6 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 56
Cardiovascular Agents: Antiarrhythmics
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 57
Cardiovascular Agents: Lipotropics
LENGTH OF AUTHORIZATIONS: See below
Juxtapid (Initial)
180 days
Vascepa, Lovaza, ACL inhibitors (Initial)
84 days
All others (Initial and Subsequent)
365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must provide documentation of baseline labs AND have documented adherence to 90 days of
prescribed lipid lowering medications
• Must have had an inadequate clinical response of at least 90 days AND unable to reach goal
LDL-C (see below) despite treatment with maximally tolerated dose of high-potency statin
and ezetimibe (or a clinical reason that these drugs cannot be utilized)
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days (or 90 days for fibrates)
with at least one preferred drug in the same drug class
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL LOVASTATIN ER (ALTOPREV), PITAVASTATIN (LIVALO), FLUVASTATIN (LESCOL)
CRITERIA
•
Must have had an inadequate clinical response of at least 30 days with two preferred drugs
in the same drug class
ADDITIONAL COLESEVELAM (WELCHOL) CRITERIA:
• Must provide documentation of a Type 2 Diabetes diagnosis
ADDITIONAL ICOSAPENT ETHYL (VASCEPA) CRITERIA:

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 58
• Must provide documentation of baseline labs indicating triglyceride levels ≥500mg/dL after
an inadequate clinical response to fibrates, niacin, and diet/exercise
• Must provide documentation of discontinuation of drugs known to increase triglyceride
levels (i.e., beta blockers, thiazides, and estrogens), if clinically appropriate
ADDITIONAL LOMITAPIDE (JUXTAPID) & ATP CITRATE LYASE (ACL) INHIBITOR CRITERIA:
• Must provide documentation of baseline labs AND have documented adherence to 90 days of
prescribed lipid lowering medications
• Must have had
inadequate clinical response of
at least 90 days AND unable to reach goal LDL-
C with high-potency statin, ezetimibe and PCSK9 inhibitor (or a clinical reason that these
drugs cannot be utilized)
ADDITIONAL INFORMATION:
• High potency statins: atorvastatin (Lipitor) 40-80mg & rosuvastatin (Crestor) 20-40mg
• LDL goals for Familial Hypercholesterolemia (includes Heterozygous & Homozygous FH): LDL ≤
100mg/dL for adults or LDL ≤ 110mg/dL for those < 18 years of age
• LDL goals for Clinical Atherosclerotic Cardiovascular Disease (ASCVD): LDL ≤ 70mg/dL
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 59
Cardiovascular Agents: Pulmonary Arterial Hypertension*
LENGTH OF AUTHORIZATIONS: 365 Days
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
approved to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must provide documentation of NYHA Functional Class for Pulmonary Hypertension and
symptoms experienced by patient
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs, one of which must be a phosphodiesterase-5 inhibitor
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION:
• Patients who have class III or IV symptoms defined by the NYHA Functional Class for
Pulmonary Hypertension may be authorized for inhalation or intravenous agents
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR - Sildenafil Susp: a PA is required for patients 18 years and older
AR - Tadliq: a PA is required for patients younger than 18 years

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 60
Central Nervous System (CNS) Agents: Alzheimer’s Agents*
LENGTH OF AUTHORIZATIONS: 365 Days
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
approved to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – All drugs: a PA is required for patients younger than 40 years

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 61
Central Nervous System (CNS) Agents: Anti-Migraine Agents, Acute
LENGTH OF AUTHORIZATIONS: 180 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL UBROGEPANT (UBRELVY) CRITERIA
• Must have had
an inadequate clinical response of at least 14 days with at least one preferred
oral CGRP antagonist
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
QL - Nurtec ODT: 8 doses per 30 days for acute treatment
Central Nervous System (CNS) Agents: Anti-Migraine Agents,
Cluster Headache

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 62
LENGTH OF AUTHORIZATIONS: 180 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 60 days to at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION:
•
An inadequate clinical response to verapamil is defined as a titration to at least 480mg daily
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
QL – Emgality: 3 doses per 30 days
Central Nervous System (CNS) Agents: Anti-Migraine Agents,
Prophylaxis
LENGTH OF AUTHORIZATIONS: Initial: 180 days; Subsequent: 365 days

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 63
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 30 days with at least three
preferred controller migraine drugs
•
Must include
objective documentation of severity, frequency, type of migraine, and number
of headache days per month (preferably a headache diary)
ERENUMAB (AIMOVIG) CRITERIA:
• Must have had an inadequate clinical response of at least 60 days with the 70mg dose to
request a dose increase
FREMANEZUMAB (AJOVY) CRITERIA:
• Must have demonstrated efficacy for at least 90 days before quarterly administration will be
authorized
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least three
preferred controller migraine drugs
AND one step therapy drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION:
• Controller migraine drug classes include beta-blockers, anticonvulsants, tricyclic
antidepressants, or serotonin-norepinephrine reuptake inhibitors
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment (preferably a
headache diary or other objective documentation of severity, frequency, and number of
headache days per month).
QL – Nurtec ODT: 18 doses per 30 days for prophylactic treatment
QL – Aimovig, Ajovy: 1 dose per 30 days
QL – Emgality: 2 doses per 30 days (for initial loading dose only), then 1 dose per 30 days thereafter

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 64
Central Nervous System (CNS) Agents: Anticonvulsants*
LENGTH OF AUTHORIZATIONS: 365 days except Epidiolex and Diacomit – Initial: 180 days
GRANDFATHERING* (except Diacomit):
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
approved to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
CANNABIDIOL (EPIDIOLEX) CRITERIA
• Must have had an inadequate clinical response of at least 30 days with any two of the
following anticonvulsants: clobazam, levetiracetam, valproic acid, lamotrigine, topiramate,
rufinamide, or felbamate within the past 365 days (members who meet this criteria will not
require a PA)
STIRIPENTOL (DIACOMIT) CRITERIA
• Must be prescribed by or in consultation with a neurologist
• Must be concomitantly taking clobazam (Onfi)
• Must provide documentation of addressed comorbidities and baseline hematologic testing
(CBC)
o Patients with phenylketonuria (PKU) must provide evidence of total daily amount of
phenylalanine
o Prescribers must include management plans for patients with neutrophil counts <1,500
cells/mm
3
or platelet count <150,000/µL
• Must provide documentation of patient’s weight
o Maximum daily dose does not exceed: 50 mg/kg/day or 3,000mg/day
• Must provide baseline average number of seizure days per month (measured monthly or
quarterly)
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 65
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
• Prescriptions submitted from a prescriber who is credentialed as a neurology specialty with
Ohio Medicaid AND for drugs that are used only for seizures,
there must have been an
inadequate clinical response of at least 30 days
with one preferred drug. This provision
applies only to the standard tablet/capsule dosage form.
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring (i.e., documented reduction in average number of seizure days per month
[measured monthly or quarterly])
AR – Vigabatrin Powder: a PA is required for patients 3 years and older
AR – Eprontia Solution: a PA is required for patients 12 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 66
Central Nervous System (CNS) Agents: Anticonvulsants Rescue
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response with at least one preferred drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Valtoco: a PA is required for patients younger than 6 years old
AR – Nayzilam: a PA is required for patients younger than 12 years old

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 67
Central Nervous System (CNS) Agents: Antidepressants*
LENGTH OF AUTHORIZATIONS: 365 Days
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
approved to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
PSYCHIATRIST EXEMPTION:
Prescribers (as identified below) are exempt from prior authorization of any non-preferred
antidepressant, or step therapy of any preferred drug, in the standard tablet/capsule dosage forms.
Other dosage forms may still require prior authorization. The exemption will be processed by the
claims system when the pharmacy has submitted the prescriber on the claim using the individual
national provider identifier (NPI) for the prescriber.
Prescribers are defined as:
Physicians with a specialty in psychiatry, nurse practitioners certified in psychiatric mental health, or
clinical nurse specialists certified in psychiatric mental health, who are credentialed with the Ohio
Department of Medicaid.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL DEXTROMETHORPHAN/BUPROPION (AUVELITY) CRITERIA
• Must have an inadequate clinical response of at least 30 days with ALL of the following:
o ONE dopamine/norepinephrine reuptake inhibitor (DNRI)
o ONE selective norepinephrine reuptake inhibitor (SNRI)
o TWO selective serotonin reuptake inhibitors (SSRIs) (ONE of which must be either
vilazodone (Viibryd) OR vortioxetine (Trintellix))

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 68
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 69
Central Nervous System (CNS) Agents: Attention Defic
it
Hyperactivity Disorder Age
nts
LENGTH OF AUTHORIZATIONS: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 30 days with atomoxetine OR at
least two preferred stimulants ADHD agents.
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least three
preferred drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Requests for non-preferred immediate-release formulations must have all required trials with
preferred immediate-release drugs, and requests for non-preferred extended-release
formulations must have all required trials with preferred extended-release drugs
• For patients established on drugs that change from preferred to non-preferred on January 1,
a prior authorization is NOT required until after June 30
th
of that year.
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Adderall, Dexedrine, & Zenzedi IR: a PA is required for patients younger than 3 years
AR – Adderall XR, Atomoxetine, Cotempla XR-ODT, Daytrana, Dexedrine ER, Dexmethylphenidate,
Methylphenidate IR & ER, & Xelstrym: a PA is required for patients younger than 6 years
AR – Dextroamphetamine Solution & Dyanavel XR: a PA is required for patients 12 years and older
AR – Methylphenidate solution/suspension: a PA is required for patients younger than 6 years and 12 years
and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 70
Central Nervous System (CNS) Agents: Antipsychotics*
LENGTH OF AUTHORIZATIONS: 365 Days
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
approved to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
PSYCHIATRIST EXEMPTION:
Prescribers (as identified below) are exempt from prior authorization of any non-preferred second-
generation antipsychotic, or step therapy of any preferred drug, in the standard tablet/capsule and long-
acting injectable dosage forms. Other dosage forms may still require prior authorization. The exemption
will be processed by the claims system when the pharmacy has submitted the prescriber on the claim
using the individual national provider identifier (NPI) for the prescriber.
Prescribers are defined as:
Physicians with a specialty in psychiatry, nurse practitioners certified in psychiatric mental health, or
clinical nurse specialists certified in psychiatric mental health, who are credentialed with the Ohio
Department of Medicaid.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
PALIPERIDONE PALMITATE (INVEGA HAFYERA) CRITERIA:
• Must have had 4 months of treatment with Invega Sustenna or 3 months with Invega Trinza
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 71
ADDITIONAL ARIPIPRAZOLE (ABILIFY MYCITE) CRITERIA:
• Must be prescribed by or in consultation with a psychiatrist following an aripiprazole serum
blood level draw indicating need for further investigation of adherence
ADDITIONAL OLANZAPINE/SAMIDORPHAN (LYBALVI) CRITERIA:
• Must provide documentation that patient is not using opioids or undergoing acute opioid
withdrawal
ADDITIONAL PIMAVANSERIN (NUPLAZID) CRITERIA:
• For Parkinson-related Hallucinations & Delusions ALL of the following must be met:
o Psychotic symptoms are severe and frequent enough to warrant treatment with an
antipsychotic AND are not related to dementia or delirium
o The patient’s other Parkinson’s Disease drugs have been reduced or adjusted and
psychotic symptoms persist OR patient is unable to tolerate adjustment of these other
drugs
o Must have been inadequate clinical response or contraindication to at least 30 days of
either quetiapine or clozapine
• An exemption to the criteria will be authorized for prescribers with a neurology specialty to a
patient with a history of the related condition
ADDITIONAL FLUOXETINE/OLANZAPINE (SYMBYAX) CRITERIA
• Must provide documentation for patient’s inability to use the individual drugs
ADDITIONAL INFORMATION
• Long-acting injectable antipsychotics may be billed by the pharmacy if they are not dispensed
directly to the patient. If not administered by the pharmacist, the drug must be released only
to the administering provider or administering provider’s staff, following all regulations for a
Prescription Pick-Up Station as described by the Ohio Board of Pharmacy
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 72
Central Nervous System (CNS) Agents: Fibromyalgia Agents
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs in different classes (see Additional Information section below)
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Drugs and drug classes include gabapentin, pregabalin, short- and/or long-acting opioids,
skeletal muscle relaxants, SNRIs, SSRIs, trazodone, and tricyclic antidepressants
• The P&T Committee does not recommend the use of opioids for treatment of fibromyalgia
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 73
Central Nervous System (CNS) Agents: Medication
Assisted
Treatment of Opioid
Addiction
LENGTH OF AUTHORIZATIONS: 180 days except 14 days for Lucemyra
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL LOFEXIDINE (LUCEMYRA) CRITERIA
• May be authorized if ALL of the following criteria are met:
o Must provide medical justification supporting why an opioid taper (such as with
buprenorphine or methadone) cannot be used
o Must have had an inadequate clinical response or contraindication to clonidine
• Must provide documentation that the drug was initiated in an inpatient setting to be exempt
from the above criteria
BUPRENORPHINE SAFETY EDITS AND DRUG UTILIZATION REVIEW CRITERIA:
• Prescribing for buprenorphine products must follow the requirements of Ohio Administrative
Code rule 4731-33-03 Office based treatment for opioid addiction.
• In favor of eliminating prior authorization for all forms of oral short acting buprenorphine-
containing products, ODM and the Managed Care Plans will implement safety edits and a
retrospective drug utilization review process for all brand and generic forms of oral short acting
buprenorphine-containing products. Safety edits are in place for dosages over 24mg of
buprenorphine equivalents/day.
• Buprenorphine sublingual tablets (generic Subutex) will be restricted to pregnancy,
breastfeeding, or contraindication to preferred products
• Buprenorphine injection (Sublocade) dosing schedule will be limited to 300mg/30 days
ADDITIONAL INFORMATION

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 74
•
Vivitrol and Sublocade may be billed by the pharmacy if it is not dispensed directly to the
patient. If not administered by the
pharmacist, the drug must be released only to the
administering provider or administering provider's staff, following all regulations for a
Prescription Pick-Up Station as described by the Ohio Board of Pharmacy.
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 75
Central Nervous System (CNS) Agents: Movement Disorders
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must be prescribed by or in consultation with a neurologist or psychiatrist
STEP THERAPY CRITERIA:
• Must have an inadequate clinical response of at least 90 days to a maximally tolerated dose
of tetrabenazine for Huntington’s Disease only
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 76
Central Nervous System (CNS) Agents: Multiple Sclerosis*
LENGTH OF AUTHORIZATIONS: 365 Days
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
approved to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL SIPONIMOD (MAYZENT) CRITERIA:
• Must provide documentation of genotype, liver function tests (LFTS) complete blood count
(CBC), ophthalmic examination, varicella zoster virus antibodies, and electrocardiogram (ECG)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 77
Central Nervous System (CNS) Agents: Narcolepsy
LENGTH OF AUTHORIZATIONS: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
• Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs - either (1) at least 30 days of modafinil or armodafinil; or (2) at least 7 days of a
preferred methylphenidate or amphetamine drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL OXYBATE SALTS (XYWAV) CRITERIA:
• Must have documented adherence to sodium restricted diet
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Adderall IR: a PA is required for patients younger than 3 years
AR – Adderall XR, Dexedrine ER: a PA is required for patients younger than 6 years
AR – Methylphenidate: a PA is required for patients younger than 6 years

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 78
Central Nervous System (CNS) Agents: Neuropathic Pain
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
• Must have had an inadequate clinical response of at least 30 days with generic Lidocaine
patch
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs in different drug classes
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 79
Central Nervous System (CNS) Agents: Parkinson's Agents
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL APOMORPHINE (APOKIN/KYNMOBI), LEVODOPA INHALATION (INBRIJA), &
ISTRADEFYLLINE (NOURIANZ) CRITERIA:
• Must have had inadequate clinical response to at least 30 days with one other drug for the
treatment of “off episodes” (dopamine agonist, COMT inhibitor, or MAO-B inhibitor)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 80
Central Nervous System (CNS) Agents: Restless
L
egs
Synd
rome
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 81
Central Nervous System (CNS) Agents: Sedative-Hypnotics, Non-
Barbiturate
LENGTH OF AUTHORIZATIONS: 180 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 10 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Non-controlled medications may be authorized if the prescriber indicates the patient has a
history of addiction
•
The P&T Committee does not recommend the use of flurazepam (Dalmane) or triazolam
(Halcion)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 82
Central Nervous System (CNS) Agents: Skeletal
Mus
cle Relaxants,
Non
-
Ben
z
odia
zep
ine
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions, contraindications,
or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics, requests must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL BACLOFEN SOLUTION CRITERIA:
• Must provide documentation of trial with baclofen tablets or justification why a non-solid oral
dosage form is indicated
ADDITIONAL CARISOPRODOL (SOMA) CRITERIA:
• Must provide medical justification that no other muscle relaxant or agent to treat
fibromyalgia, or any musculoskeletal condition would serve the clinical needs of the
patient
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 84
Dermatologic Agents: Oral Acne Products
LENGTH OF AUTHORIZATIONS: 150 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must have had an inadequate clinical response of at least 90 days with at least one preferred
topical AND one preferred oral antibiotic for acne
• Must be absent of oral tretinoin in the past 56 days
• Patient must be Prescriber attests that patient is registered and meets all of the requirements
of the iPLEDGE program
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 90 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Authorization length will be for no more than 150 days at a time then must take 56 days off
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 85
Dermatologic Agents: Topical Acne Products
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days or (90 days for retinoids) of
at least three preferred drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL TRETINOIN/BENZOYL PEROXIDE (TWYNEO) CRITERIA
• Must provide documentation for patient’s inability to use the individual drugs
ADDITIONAL INFORMATION
• All retinoids - May be authorized with a diagnosis of skin cancer
• Tazarotene (Tazorac) - May be authorized with a diagnosis of psoriasis
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR - All topical retinoids: a PA is required for patients 24 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 86
Endocrine Agents: Androgens
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must provide documentation of lab work to support the need for testosterone
supplementation
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 90 days with ALL preferred drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring (i.e., testosterone and hematocrit)
AR: All drugs: a PA is required for patients younger than 18 years

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 87
Endocrine Agents: Diabetes – Hypoglycemia Treatments
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least two one preferred drugs OR the
inability of the member and/or caregiver to administer a preferred glucagon product in a
timely fashion
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
QL – All glucagon products: 2 doses per 34 days

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 88
Endocrine Agents: Diabetes – Insulin
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 120 days with at least one
preferred drug
having a similar duration of action
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 120 days with at least two
preferred drugs
having a similar duration of action
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an
inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL TEMPO PEN CRITERIA
• Must have had an inadequate clinical response or documentation of medical necessity
beyond convenience for why the patient cannot use the corresponding FlexPens or Kwikpens
ADDITIONAL INHALED INSULIN (AFREZZA) CRITERIA:
• Must provide documentation of spirometry testing prior to initiation with a predicted FEV1
≥70% - Will not be authorized for patients with asthma or COPD
• Must provide documentation of being nicotine-free for at least 180 days
ADDITIONAL INFORMATION
• An
inadequate clinical response
is defined as the inability to reach A1C goal after at least 120
days of current regimen with documented adherence and appropriate dose escalation.
•
Requests may be authorized for patients with a condition that is difficult to
control (i.e., prone
to ketoacidosis, hypoglycemia)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 89
Endocrine Agents: Diabetes –
Non
-
Insulin
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 120 days with at least three
preferred drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL ORAL AND INJECTABLE COMBINATION DRUGS CRITERIA
•
Must have had a trial of at least 120 days with
the individual drugs OR must provide
documentation of medical necessity beyond convenience for patient’s inability to use the
individual drugs
ADDITIONAL INFORMATION
•
An inadequate clinical response is dened as the inability to reach A1c goal aer at least 120
days of current regimen, with use of mulple drugs concomitantly per ADA guidelines,
documented adherence, and appropriate dose escalaon (must achieve maximum
recommended dose or document that maximum recommended dose is not tolerated or is
clinically inappropriate).
o
Must document A1c goal per ADA guidelines and baseline A1c.
•
Requests may be authorized for patients with a condition that is difficult to
control (i.e., prone
to ketoacidosis, hypoglycemia)
• For non-preferred drugs that have preferred drugs in the same drug class: must provide
documentation that there was at least one inadequate clinical response with a drug in same
drug class
SUBSEQUENT AUTHORIZATION CRITERIA:
•
Must provide documentaon of paent’s clinical response to treatment and ongoing safety
monitoring
o
Must document A1c goal per ADA guidelines and A1c trends including current value
(within last 6 months).
•
Must meet all inial clinical criteria for subsequent authorizaons.

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 91
Endocrine Agents: Endometriosis
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 84 days with at least one preferred
NSAID and one preferred oral contraceptive
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 84 days with at least one preferred
NSAID, one preferred oral contraceptive, AND one preferred step-therapy drug
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 92
Endocrine Agents: Estrogenic
A
gen
ts
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of
an
inadequate clinical response with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION:
• Requests for non-preferred drugs must have
an inadequate clinical response
with preferred
drugs with the same delivery method
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 93
Endocrine Agents: Growth Hormone
LENGTH OF AUTHORIZATIONS: Initial: 180 days; Subsequent: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
Pediatric Approvals (under 18 years of age):
• Must be treated and followed by a pediatric endocrinologist, nephrologist, clinical
geneticist, endocrinologist, or gastroenterologist (or as appropriate for diagnosis)
• Must provide documentation to justify criteria being met, including height, weight, bone
age (children), date and results of most current x-ray, stimulus test results, IGF-1 levels,
and a growth chart (children)
• Must not being used in combination with another somatropin agent
Adult Approvals (18 years of age or older):
• Must be treated and following by an endocrinologist
• Must provide documentation of growth hormone deficiency by means of a negative response
to an appropriate stimulation test (clonidine test is not acceptable for adults)
• Must provide documentation of baseline evaluation of the following clinical indicators: (1)
insulin-like growth factor (IGF-1); (2) fasting lipid profile; (3) BUN; (4) fasting glucose; (5)
electrolytic levels; (6) evaluation of any new osteoarthritis and joint pain; (7) bone density test
• Must have had other hormonal deficiencies addressed with adequate replacement therapy
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 90 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring (i.e., height, weight gain, improved body composition)

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 94
For adults:
must provide documentation by endocrinologist that discontinuing agent would
have a detrimental effect on body composition or other metabolic parameters

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 95
Endocrine Agents: Osteoporosis – Bone
Ossi
fic
ation
Enh
ancers
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
TERIPARATIDE (FORTEO™) CRITERIA:
• Must have had an inadequate clinical response of at least 365 days with one bisphosphonate
• A total lifetime duration of therapy of 730 days will be authorized between any parathyroid
analog
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 365 days with at least one
preferred drug within the same class
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
A
DDIT
I
O
NAL ABAL
OPAR
A
T
I
D
E
(T
YMLOS™) CRIT
ERIA
:
• Must have had an inadequate clinical response of at least 365 days with one bisphosphonate
• A total lifetime duration of therapy of 730 days will be authorized between any parathyroid
analog
ADDITIONAL INFORMATION
• Patients should only be on ONE of the therapeutic classes (bisphosphonates, calcitonin-
salmon)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 97
Endocrine Agents: Uterine Fibroids
LENGTH OF AUTHORIZATIONS: Up to 180 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must have had an inadequate
clinical response of at least 90 days with at least one preferred
oral contraceptive
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 90 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION:
• A total lifetime duration of therapy of 730 days between Oriahnn and Myfembree or 180 days
for Lupron Depot will be authorized
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 98
Gastrointestinal Agents: Anti-Emetics
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 7 3 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 99
Gastrointestinal Agents: Bowel Preparations
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any solid oral dosage formulation: must provide documentation of medical necessity
for why patient cannot be changed to a non-solid oral dosage formulation
•
Must have had an inadequate clinical response with at least one preferred drug
o For non-preferred brand names that have preferred generics: must provide
documentation of
an inadequate clinical response
or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 100
Gastrointestinal Agents: Crohn’s Disease
LENGTH OF AUTHORIZATIONS: 365 Days; Ortikos ER – based on indication
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 101
Gastrointestinal Agents: Hepatic Encephalopathy
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 14 days with at least one preferred
drug
RIFAXAMIN (XIFAXAN) CRITERIA:
• Must have had an inadequate clinical response of at least 14 days to lactulose to be
authorized for monotherapy or add on therapy
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 102
Gastrointestinal Agents: Irritable Bowel Syndrome (IBS) with
Diarrhea
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 103
Gastrointestinal Agents: Pancreatic Enzymes
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 104
Gastrointestinal Agents: Proton Pump
Inhibitors
LENGTH OF AUTHORIZATIONS: 180 days, except as listed under additional criteria
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL CRITERIA FOR PPI DOSES GREATER THAN ONCE DAILY
• For H. Pylori diagnosis: Must provide documentation of diagnosis
o Authorization length: 30 days
• For any of the following diagnoses: carcinoma of GI tract, COPD, Crest Syndrome, dyspepsia,
esophageal varices, gastritis, gastroparesis, scleroderma, symptomatic uncomplicated Barret’s
Esophagus, systemic mastocytosis, or Zollinger Ellison Syndrome: Must provide
documentation of diagnosis AND must have failed once-daily dosing of the requested drug
o Authorization length: 365 days
ADDITIONAL INFORMATION
•
Request may be authorized If the drug was initiated in the hospital for the treatment of a
condition such as a GI bleed or the presence of a gastrostomy and/or jejunostomy
(G, GJ, J-
tube)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR - Protonix Pak/Pantoprazole Packet: a PA is required for patients 6 years and older
AR – Omeprazole & Pantoprazole Tab/Cap/ODT: a PA is required for patient 21 years and older
requesting more than once daily dosing

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 105
Gastrointestinal Agents: Ulcerative Colitis
LENGTH OF AUTHORIZATIONS: 365 Days; except Uceris foam – based on indication
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
QL – Budesonide ER 9mg tablets: 56 tablets per 90 days

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 106
Gastrointestinal Agents: Unspecified GI
LENGTH OF AUTHORIZATIONS: 365 days except 3 days for Aemcolo
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response to at least 14 days with at least two preferred
drugs
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least three
preferred drugs, if indicated for diagnosis
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL METHYLNALTREXONE (RELISTOR) AND NALDEMEDINE (SYMPROIC) CRITERIA:
• Must have a history of chronic pain requiring continuous opioid therapy for ≥84 days
ADDITIONAL RIFAMYCIN DELAYED-RELEASE (AEMCOLO) CRITERIA:
• Must have the inability to take, or failure of ALL of the following: azithromycin,
ciprofloxacin, levofloxacin, ofloxacin, or rifaximin
ADDITIONAL SOMATROPIN INJECTION (ZORBTIVE) AND TEDLOGLUTIDE (GATTEX) CRITERIA:
• Must have evidence of specialized parenteral nutritional support
• Must have documentation of appropriate lab assessment (bilirubin, alkaline phosphatase,
lipase, and amylase) at least 180 days prior to initiation
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring (i.e., decreased frequency of specialized nutrition support or improvement in
symptoms)

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 107
Genitourinary Agents: Benign Prostatic Hyperplasia
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
TADALAFIL (CIALIS) CRITERIA:
• Must have had
an inadequate clinical response of
at least 30 days with at least one alpha-1
adrenergic blocker. and If prostate volume of > 30cc on imaging, a prostate specific antigen
(PSA) > 1.5ng/dL, or palpable prostate enlargement on digital rectal exam (DRE), then a trial of
at least 90 days of finasteride is required.”
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL DUTASTERIDE/TAMSULOSIN (JALYN) & FINASTERIDE/TADALAFIL (ENTADFI) CRITERIA
• Must provide documentation for patient’s inability to use the individual drugs
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 108
Genitourinary Agents: Electrolyte Depleter Agents
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 7 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 109
Genitourinary Agents: Urinary Antispasmodics
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs with different active ingredients
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Vesicare LS: a PA is required for patients younger than 2 years old AND 5 years and older
AR – Myrbetriq Granules: a PA is required for patients younger than 3 years old AND 5 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 110
Immunomodulator Agents: Systemic Inflammatory Disease
LENGTH OF AUTHORIZATIONS: Initial: 90 days; Subsequent: 365 days
ALL AUTHORIZATIONS:
• Must be
prescribed in accordance with FDA approved labeling
• First line treatment can vary based upon the severity of disease for certain diagnoses.
Documentation of the patient’s disease state and the criteria used to classify the severity is
required.
CLINICAL PA CRITERIA:
• Must have been an inadequate clinical response of at least 90 days with
at least
two
applicable first-line drugs indicated for diagnosis – provide documentation of the trialed
drugs, dosages, dates, and durations
• Authorization of dosing regimens (loading/maintenance) will be based upon diagnosis.
Document the requested loading and maintenance dosing on PA form, if applicable
• Must not have a current, active infection
• Must provide evidence of negative TB test prior to initiation of biologic therapy, if required by
labeling
STEP THERAPY CRITERIA:
•
Must had had an inadequate clinical response of at least 90 days with at least one preferred
TNF inhibitor indicated for diagnosis
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 90 days with at least two preferred
drugs, if indicated for diagnosis
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL ALOPECIA AREATA CRITERIA:
• Must be prescribed by or in consultation with a specialist (i.e., dermatologist,
rheumatologist)
• Must provide documentation of an inadequate clinical response of at least 90 days with a
topical steroid

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 111
ADDITIONAL ATOPIC DERMATITIS CRITERIA:
• Must have at least 10% body surface area (BSA) involvement with
two of the following:
topical corticosteroids or topical calcineurin inhibitors [e.g., Elidel] unless atopic dermatitis is
severe and involves >
25% BSA
ADDITIONAL CROHN’S DISEASE CRITERIA:
• Must provide documentation of Crohn's Disease Activity Index (CDAI) score of 220 or
higher to be considered moderate to severe disease
ADDITIONAL HIDRADENTIS SUPPURATIVA CRITERIA:
• Must provide documentation of Hurley Stage III to be classified as severe disease
ADDITIONAL PLAQUE PSORIASIS CRITERIA:
• For patients currently receiving phototherapy, initial authorization for preferred drugs
requires an inadequate clinical response to at least 90 days of phototherapy
• To classify as severe disease patient must present at least two of the following: Psoriasis
Area and Severity Index (PASI) score ≥ 11, BSA ≥ 10%, and Static Physician's Global
Assessment (sPGA) ≥ 3
ADDITIONAL ULCERATIVE COLITIS CRITERIA:
• If an inadequate clinical response after 90 days with one TNF inhibitor, further TNF inhibitors
will not be authorized
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 112
Infectious Disease Agents: Antibiotics – Cephalosporins
LENGTH OF AUTHORIZATIONS: Based on indication
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 3 days with at least one preferred
antibiotic
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Requests may be authorized if:
o The infection is caused by an organism resistant to ALL preferred
antibiotics
(must
provide diagnosis and any culture/sensitivity results)
o The patient is completing a course of therapy that was started in the hospital or other
similar location or was started before Medicaid eligibility, only the remaining course will
be authorized
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment, ongoing safety
monitoring, AND medical necessity for continued use
AR - Cefaclor Suspension: a PA is required for patients 12 years and older
AR - Cefixime Suspension: a PA is required for patients 12 years and older
AR - Cefprozil Suspension: a PA is required for patients 12 years and older
AR - Suprax Chewable Tablet: a PA is required for patients 12 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 113
Infectious Disease Agents: Antibiotics – Inhaled
LENGTH OF AUTHORIZATIONS: Initial: 180 days; Subsequent: 365 days
ALL REQUESTS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must provide documentation of cultures demonstrating drug is prescribed in alignment with
approved indication
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 28 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring (i.e., culture conversion, symptom improvement)
QL – Tobramycin drugs: 56 doses in 56 days

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 114
Infectious Disease Agents: Antibiotics – Macrolides
LENGTH OF AUTHORIZATIONS: Based on indication
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 3 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Requests may be authorized if:
o The infection is caused by an organism resistant to ALL preferred
antibiotics
(must
provide diagnosis and any culture/sensitivity results)
o The patient is completing a course of therapy that was started in the hospital or other
similar location or was started before Medicaid eligibility, only the remaining course will
be authorized
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment, ongoing safety
monitoring, AND medical necessity for continued use

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 115
Infectious Disease Agents: Antibiotics – Quinolones
LENGTH OF AUTHORIZATIONS: Based on indication
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 3 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Requests may be authorized if:
o The infection is caused by an organism resistant to ALL preferred
antibiotics
(must
provide diagnosis and any culture/sensitivity results)
o The patient is completing a course of therapy that was started in the hospital or other
similar location or was started before Medicaid eligibility, only the remaining course will
be authorized
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment, ongoing safety
monitoring, AND medical necessity for continued use
AR - Ciprofloxacin Suspension: a PA is required for patients 12 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 116
Infectious Disease Agents: Antibiotics – Tetracyclines
LENGTH OF AUTHORIZATIONS: Based on indication for acute infections or 365 days for acne
ALL REQUESTS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 3 days with at least one preferred
drug for acute infections OR at least 90 days with at least one preferred oral drug for acne
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Requests may be authorized if:
o The infection is caused by an organism resistant to ALL preferred
antibiotics
(must
provide diagnosis and any culture/sensitivity results)
o The patient is completing a course of therapy that was started in the hospital or other
similar location or was started before Medicaid eligibility, only the remaining course will
be authorized
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment, ongoing safety
monitoring, AND medical necessity for continued use
AR – Vibramycin Suspension: a PA is required for patients 12 years and older
AR – Doxycycline Syrup: a PA is required for patients 12 years and older
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 117
Infectious Disease Agents: Antifungals
LENGTH OF AUTHORIZATIONS: Based on indication
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 7 days with at least one two
preferred drugs, if indicated for the diagnosis
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL OTESECONAZOLE (VIVJOA) CRITERIA:
• Must provide documentation of at least three symptomatic episodes of vulvovaginal candidiasis
in the past 12 months
• Must provide documentation of non-reproductive potential (i.e., post-menopausal)
• Must have had an inadequate clinical response of at least 180 day maintenance course with
oral fluconazole shown by documentation of more than one breakthrough infection
ADDITIONAL INFORMATION:
• Requests may be authorized if:
o The infection is caused by an organism resistant to ALL preferred
antifungals
(must
provide diagnosis and any culture/sensitivity results)
o The patient is completing a course of therapy that was started in the hospital or other
similar location or was started before Medicaid eligibility, only the remaining course will
be authorized
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment, ongoing safety
monitoring, AND medical necessity for continued use

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 118
Infectious Disease Agents: Antivirals – Hepatitis C Agents
LENGTH OF AUTHORIZATIONS: Dependent upon authorized course
ALL REQUESTS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Only regimens recommended by the American Association for the Study of Liver Diseases
(AASLD) will be authorized
• Please see the Hepatitis C Direct Acting Antiviral Prior Authorization Form for criteria
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response defined as not achieving SVR with guideline-
recommended preferred drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION:
• Requests for patients established on current therapy with prior payer (i.e., Commercial,
Fee-for-Service, Managed Care Plan, etc) will be authorized with documentation
• Requests for regimens including pegylated Interferons must include close monitoring
with periodic clinical and laboratory evaluations
• Requests for regimens including ribavirins must include documentation of at least two
reliable forms of contraception being used during therapy

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 119
Infectious Disease Agents: Antivirals – Herpes
LENGTH OF AUTHORIZATIONS: For the duration of the prescription (up to 180 days)
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 3 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 120
Infectious Disease Agents: Antivirals – HIV*
LENGTH OF AUTHORIZATIONS: 365 Days
GRANDFATHERING*:
Patients who have a claim for a non-preferred drug in the previous 120 days will be automatically
approved to continue the drug. Patients who have taken the drug previously, but do not have claims
history (e.g., new to Medicaid), will need to submit a prior authorization in order to continue
coverage.
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
ABACAVIR/DOLUTEGRAVIR/LAMIVUDINE (TRIUMEQ PD) CRITERIA:
• Must provide documentation of patient’s weight (only authorized for those 10 – 25 kg)
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug.
If applicable, the request must address the inability to use the individual components.
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Isentress chewable tablet: a PA is required for patients 12 years and older
AR – Lamivudine solution: a PA is required for patients 3 years and older
AR – Nevirapine solution: a PA is required for patients 3 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 121
Ophthalmic Agents: Antibiotic and
Antibiotic
-
St
e
roid
Combination
Drops and
Ointm
e
nts
LENGTH OF AUTHORIZATIONS: 30 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 3 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL INFORMATION
• Requests may be authorized if:
o The infection is caused by an organism resistant to ALL preferred
antibiotics
(must
provide diagnosis and any culture/sensitivity results)
o The patient is completing a course of therapy that was started in the hospital or other
similar location or was started before Medicaid eligibility, only the remaining course will
be authorized

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 122
Ophthalmic Agents: Antihistamines & Mast Cell Stabilizers
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 123
Ophthalmic Agents: Dry Eye Treatments
LENGTH OF AUTHORIZATIONS: 14 Days for Eysuvis; 365 Days for all other drugs
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 14 days with one artificial tear or
OTC dry eye drop in the previous 120 days
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 124
Ophthalmic Agents: Glaucoma Age
nts
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug in the same class, if available
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs in the same class, if available
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 125
Ophthalmic Agents: NSAIDs
LENGTH OF AUTHORIZATIONS: 30 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 3 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 126
Ophthalmic Agents: Ophthalmic Steroids
LENGTH OF AUTHORIZATIONS: 30 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 127
Otic Agents: Antibacterial and
Antibact
e
rial/Steroid Combinations
LENGTH OF AUTHORIZATIONS: 30 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least
7 days with
at least
one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 128
Respiratory Agents: Antihistamines – Second Generation
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two different
preferred drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR – Cetirizine Chewables: a PA is required for patients 6 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 129
Respiratory Agents: Cystic Fibrosis
LENGTH OF AUTHORIZATIONS: Initial: 90 days; Subsequent: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must be prescribed by or in consultation with a pulmonologist or infectious disease specialist
• Must provide documentation of the genetic mutation
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL BRONCHITOL CRITERIA:
• Must be used as an add-on maintenance therapy
• Must provide documentation of a completed Bronchitol Tolerance Test
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment (adherence to
treatment demonstrated by claims history AND one or more of the following: FEV1, weight
gain, sweat chloride, pulmonary exacerbations, etc.) and ongoing safety monitoring
AR – Trikafta Pak: a PA is required for patients 6 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 130
Respiratory Agents: Epinephrine Auto-Injectors
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response to at least one preferred drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 131
Respiratory Agents: Hereditary Angioedema
LENGTH OF AUTHORIZATIONS: Initial: 90 days; Subsequent: 180 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must provide documentation of diagnosis (i.e., C1-INH deficiency or dysfunction (Type I or II
HAE)) and whether the drug will be used for prophylaxis or treatment
• Must provide documentation of at-home administration
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 60 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 132
Respiratory Agents: Inhaled Agents
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs
within the same class and duration of action
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL STEROID-CONTAINING INHALER CRITERIA
• May be authorized if documentation of one of the following is provided:
o Patient is 12 years or younger OR is disabled and is unable to use a preferred inhaler
o Patient has been non-compliant on a preferred inhaler due to taste, dry mouth, or
infection
o Patient is clinically unstable, as defined by current guidelines in terms of oral steroid
use or patient’s current symptomatology
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR - Albuterol Nebulizer Solution 0.021% (0.63mg/3mL), 0.042% (1.25mg/3mL): a PA is required for
patients 13 years and older
AR - Budesonide Nebulizer Solution: a PA is required for patients 7 years and older

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 133
Respiratory Agents: Leukotriene Receptor Modifiers & Inhibitors
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 90 days with at least one preferred
drug
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 90 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 134
Respiratory Agents: Monoclonal Antibodies-Anti-IL/Anti-IgE
LENGTH OF AUTHORIZATIONS: Initial: 180 days; Subsequent: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
CLINICAL PA CRITERIA:
• Must be prescribed by or in consultation with an applicable specialist (i.e., allergist/
immunologist, pulmonologist, or otolaryngologist)
• For Asthma – Must have had uncontrolled asthma symptoms and/or exacerbations despite at
least 30 days with:
o Medium dose preferred ICS/LABA inhaler for 6 years and older OR medium dose
preferred ICS/LABA inhaler with tiotropium or high dose ICS/LABA inhaler if 12 years
and older
• For Chronic Rhinosinusitis with Nasal Polyposis – Must have had an inadequate clinical
response of at least 30 days to
at least
one oral corticosteroid AND one nasal corticosteroid
spray
• For Chronic Urticaria – Must have had an inadequate clinical response to at least 14 days
with
at least
two different antihistamines
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions, contraindications,
or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
• Must have had an inadequate clinical response of at least 90 days with
at least
one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics, requests must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring (i.e., PFT improvement, reduced affected BSA)

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 135
Respiratory Agents: Nasal Preparations
LENGTH OF AUTHORIZATIONS: 365 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least two preferred
drugs in the same class, if available
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 136
Respiratory Agents: Other Agents
LENGTH OF AUTHORIZATIONS: Initial: 90 days; Subsequent: 180 days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 90 days with at least one preferred
long
-acting beta agonist AND
one preferred
long-acting muscarinic antagonist-containing
inhalers
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL ROFLUMILAST (DALIRESP) CRITERIA:
• Must be used in addition to a long-acting beta agonist AND a long-acting muscarinic
antagonist-containing inhalers
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment, adherence to
maintenance inhaler per pharmacy claims, and ongoing safety monitoring
AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 137
Topical Agents: Antifungals
LENGTH OF AUTHORIZATIONS: Up to 180 days for all agents except 365 days for Jublia
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs, if indicated for diagnosis
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
ADDITIONAL EFINACONAZOLE (JUBLIA) CRITERIA:
•
Must have had an inadequate clinical response of at least 365 days with at least one preferred
topical drug AND at least 84 days with at least one preferred oral drug indicated for diagnosis
ADDITIONAL INFORMATION
• Requests may be authorized if:
o The infection is caused by an organism resistant to preferred
antibiotics
drugs (note
diagnosis and any culture/sensitivity results)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 138
Topical Agents: Antiparasitics
LENGTH OF AUTHORIZATIONS: 14 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 139
Topical Agents: Corticosteroids
LENGTH OF AUTHORIZATIONS: 365 days for low/med potency; 90 days for high/very high potency
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 14 days with at least two preferred
drugs
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring

AR = Age Restriction
QL = Quantity Limit
ST = Step Therapy Required
PA = Clinical Prior Authorization Required
BvG = Brand Preferred Over Generic
Ohio Medicaid Unified PDL effective January 1, 2024 140
Topical Agents: Immunomodulators
LENGTH OF AUTHORIZATIONS: 365 Days
ALL AUTHORIZATIONS: Must be
prescribed in accordance with FDA approved labeling
STEP THERAPY CRITERIA:
•
Must have had an inadequate clinical response of at least 30 days with at least two topical
corticosteroids
NON-PREFERRED CRITERIA:
• Must provide documentation of medical necessity beyond convenience for why the patient
cannot be changed to a preferred drug (i.e., allergies, drug-drug interactions,
contraindications, or intolerances) OR
o For any nonsolid oral dosage formulation: must provide documentation of medical
necessity for why patient cannot be changed to a solid oral dosage formulation
•
Must have had an inadequate clinical response of at least 30 days with at least one preferred
drug
o For non-preferred extended-release formulations: must provide documentation of an
inadequate clinical response
with its immediate release formulation (if available)
o For non-preferred brand names that have preferred generics: must provide
documentation of an inadequate clinical response or allergy to two or more generic
labelers (if available)
SUBSEQUENT AUTHORIZATION CRITERIA:
• Must provide documentation of patient’s clinical response to treatment and ongoing safety
monitoring
AR - pimecrolimus and tacrolimus: a PA is required for patients younger than 2 years old




