
ACHI is a nonpartisan, independent, health policy center that serves as a catalyst to improve the health of Arkansans.
1401 W Capitol Avenue, Suite 300 ● Little Rock, Arkansas 72201 ● (501) 526-2244 ● www.achi.net
Copyright © 2018 by the Arkansas Center for Health Improvement
Arkansas Health Care Independence Program
(‘Private Option’)
Section 1115 Demonstration Waiver
Final Report
June 30, 2018

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
About the Evaluators
The Arkansas Center for Health Improvement (ACHI) is a nonpartisan, independent health policy center whose
vision is to be a trusted health policy leader committed to innovations that improve the health of Arkansans. This
vision is carried out through ACHI’s mission to be a catalyst for improving the health of Arkansans through
evidence-based research, public issue advocacy, and collaborative program development. In undertaking this
mission, ACHI has worked hard to develop and adhere to an important set of values that guide the Center.
ACHI’s core values are commitment, initiative, trust, and innovation. These are the fundamental principles that
guide the Center’s collective and individual decisions, strategies, and actions to advance the health of Arkansans.
These core values define what ACHI — the organization and its people — stands for throughout time, regardless
of changes in ACHI’s internal structure and leadership, or in response to external factors and environmental
conditions.
ACHI Team
Joseph W. Thompson, MD, MPH, Director
Anthony Goudie, PhD, Director of Research and Evaluation
Nichole Sanders, PhD, Assistant Director of Analytics
Kanna Lewis, PhD, Health Policy Data Architect
Vanessa White, BA, Project Coordinator
Stephen Lein, MS, Senior Data Analyst
Judy Bennett, MS, Senior Research Analyst
Pader Moua, MPH, Policy Analyst
Tim Holder, BA, Technical Editor
John Lyon, BA, Strategic Communications Manager
Vaishali Thombre, MBA, MS, Senior Research Analyst
Jeral Self, MPH, Senior Data Analyst
Kenley Money, MA, MFA, Director of Information Systems Architecture
University of Arkansas for Medical Sciences Evaluators
Anthony Goudie, PhD
Director of Research and Evaluation, Arkansas Center for Health Improvement
Assistant Professor, Center for Applied Research and Evaluation, Department of Pediatrics, College of Medicine,
University of Arkansas for Medical Sciences
Assistant Professor, Department of Health Policy and Management, Fay W. Boozman College of Public Health,
University of Arkansas for Medical Sciences

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
John “Mick” Tilford, PhD
Professor and Department Chair, Department of Health Policy and Management, Fay W. Boozman College
of Public Health, University of Arkansas for Medical Sciences
Professor, Department of Pharmaceutical Evaluation and Policy, College of Pharmacy, University of
Arkansas for Medical Sciences
Bradley Martin, PharmD, PhD
Professor, Division Head, Department of Pharmaceutical Evaluation and Policy, College of Pharmacy,
University of Arkansas for Medical Sciences
Comparative Effectiveness Research Program Co-Director, Translational Research Institute, University of
Arkansas for Medical Sciences
Teresa Hudson, PharmD, PhD
Associate Professor of Psychiatry and Director, Division of Health Services Research, College of Medicine,
University of Arkansas for Medical Sciences
Director, National Rural Evaluation Center, U.S. Department of Veterans Affairs
Associate Director, Center for Mental Healthcare and Outcomes Research, U.S. Department of Veterans Affairs
Jeffrey Pyne, MD
Professor, Department of Psychiatry and Behavioral Sciences, College of Medicine, University of Arkansas
for Medical Sciences
Associate Professor, Department of Pharmacy Practice, College of Pharmacy, University of Arkansas for
Medical Sciences
Associate Professor, Department of Epidemiology, College of Public Health, University of Arkansas for
Medical Sciences
Staff Physician, Central Arkansas Veterans Healthcare System
Associate Director for Research and Site Leader for Community Engagement, South Central (VISN 16)
Mental Illness Research, Education, and Clinical Center
Research Health Scientist and Core Investigator, Center for Mental Healthcare and Outcomes Research,
U.S. Department of Veterans Affairs
Chenghui Li, PhD
Associate Professor, Division of Pharmaceutical Evaluation and Policy, College of Pharmacy, University of
Arkansas for Medical Sciences
Nalin Payakachat, PhD
Associate Professor, Division of Pharmaceutical Evaluation and Policy, College of Pharmacy, University of
Arkansas for Medical Sciences

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
UAMS Research Support Team
Gary Moore, MS, Research Analyst
Xiaotong Han, MS, Biostatistician
Niranjan Kathe, MS, Graduate Research Assistant
Divyan Chopra, MS, Graduate Research Assistant
Naleen Raj Bhandari, MS, Graduate Research Assistant
Mahip Acharya, B Pharm, Graduate Research Assistant
Acknowledged Contributors
Heather L. Rouse, MSEd, PhD
Brady Rice, BS
Grayson Shelton, BS
Donald Poe, BS
Anuj Shah, PhD
Siqing Li, MS

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
Acknowledgements
Private Option Evaluation National Advisory Committee
The purpose of the National Advisory Committee (NAC) is to act as an external expert advisory group for the
Arkansas Section 1115 demonstration waiver evaluation. Members of the committee were asked to serve in the
capacity for the duration of the three-year evaluation period (2014-2017) and were selected based on their content
expertise and methodological experience. The committee is comprised of a diverse range of policy perspectives and
professional backgrounds.
Eduardo Sanchez, MD, MPH, Chief Medical Officer (CMO) for Prevention, American Heart Association National
Center
Darrell J. Gaskin, PhD, Deputy Director, Center for Health Disparities Solutions, Bloomberg School of Public
Health, Johns Hopkins University
Daniel Polsky, PhD, Executive Director, Leonard Davis Institute of Health Economics, University of Pennsylvania
Timothy S. Carey, MD, MPH, Sarah Graham Kenan Professor of Medicine, Departments of Medicine and Social
Medicine, School of Medicine, University of North Carolina at Chapel Hill
Correspondence concerning this report should be addressed to the Arkansas Center for Health Improvement
(ACHI).
Contributing ACHI authors include Joseph W. Thompson, MD, MPH, and Anthony Goudie, PhD.
Suggested Citation
Arkansas Center for Health Improvement. Arkansas Health Care Independence Program (‘Private Option’)
Section 1115 Demonstration Waiver Final Report. Little Rock, AR: Arkansas Center for Health Improvement, June
2018.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
Abbreviations
ACHI Arkansas Center for Health Improvement
AHA The Arkansas Hospital Association
AHRQ Agency for Healthcare Research and Quality
AID Arkansas Insurance Department
AV Actuarial Value
BNC Budget Neutrality Cap
CAHPS Consumer Assessment of Healthcare Providers and Systems
CAST Center for Advanced Spatial Technologies
CDC Centers for Disease Control and Prevention
CMS Centers for Medicare & Medicaid Services
CPT Current Procedure Terminology
CSR Cost-Sharing Reduction
CY Calendar Year
DCO Department of County Operations
DHS Arkansas Department of Human Services
EHB Essential Health Benefit
EPSD Early and Periodic Screening and Diagnostic
ER Emergency Room
FFM Federally Facilitated Marketplace
FFS Fee-For-Service
FPL Federal Poverty Level
FQHC Federally Qualified Community Health Center
GME Graduate Medical Education
HbA1c Hemoglobin A1c
HCIP Health Care Independence Program
HEDIS Healthcare Effectiveness Data and Information Set
HIA Health Independence Accounts
LATE Local Average Treatment Effect
LDL-c Lipoprotein
LSM Least Squares Mean

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
Marketplace Individual Health Insurance Marketplace
MDES Minimum Detectable (standardized) Effect Size
MEPS Medical Expenditure Panel Survey
MLR Medical Loss Ratio
NAC National Advisory Committee
NCQA National Committee for Quality Assurance
NEMT Non-Emergency Medical Transportation
NQF National Quality Forum
NYU New York University
PCCM Primary Care Case Management
PCP Primary Care Provider
PMPM Per Member Per Month
PMPY Per Member Per Year
PPACA Patient Protection and Affordable Care Act
PY Person-Years
PY1 Program Year 1
PY2 Program Year 2
PY3 Program Year 3
QHP Qualified Health Plan
Questionnaire Healthcare Needs Assessment Questionnaire
RCT Randomized Controlled Trial
RD Regression Discontinuity
RE Relative Efficiency
RUCA Rural-Urban Commuting Area Code
SIPTW Stabilized Inverse Probability of Treatment Weighting
SNAP Supplemental Nutrition Assistance Program
SSI Social Security Income
TEFRA Tax Equity and Fiscal Responsibility Act
UAMS University of Arkansas for Medical Sciences
UPL Upper Payment Limit

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
Table of Contents
Executive Summary ...................................................................................................................................................... i
Background ............................................................................................................................................................... i
Summary of Findings Based on Evaluation Hypotheses ........................................................................................... i
Conclusion ............................................................................................................................................................... vi
Introduction ................................................................................................................................................................. 1
Background .............................................................................................................................................................. 1
Arkansas Profile ....................................................................................................................................................... 1
Arkansas Structure of Commercial Premium Assistance ......................................................................................... 2
Arkansas Structure of PPACA Eligibility and Enrollment ......................................................................................... 3
Arkansas HCIP Program Experience ......................................................................................................................... 6
Arkansas HCIP Evaluation Strategy .......................................................................................................................... 8
Research Design and Approach ................................................................................................................................... 9
Goals and Objectives................................................................................................................................................ 9
Programmatic Timeline and Reporting Requirements .......................................................................................... 10
Theoretical Approach............................................................................................................................................. 11
Hypotheses ............................................................................................................................................................ 13
Data Sources and Analytic Comparison Groups .................................................................................................... 14
Methodological Approaches .................................................................................................................................. 16
The First Year Experience ....................................................................................................................................... 18
Year 2 and Year 3 Waiver Impact Findings ................................................................................................................ 24
Introduction to Analyses ........................................................................................................................................ 24
Geographic and Realized Access Differences and Provider Reimbursement Comparison
between Medicaid and QHP Programs .................................................................................................................. 27
Differences in Comparison Groups by Comparison Populations ........................................................................... 31
Special Populations and Topic Studies ................................................................................................................... 43
Program Costs ............................................................................................................................................................ 71
Overview ................................................................................................................................................................ 71
Cost-Effectiveness .................................................................................................................................................. 72
Program Impact Simulation ................................................................................................................................... 73
Appendices .............................................................................................................................................................. A-1
Appendix A – Arkansas Evaluation Hypotheses: Proposed and Original Test Indicators .................................... A-1
Appendix B – Arkansas Evaluation Hypotheses .................................................................................................... B-1
Appendix C – Data Processing of Carrier Data ...................................................................................................... C-1
Appendix D – Study Subjects: Analytical Sample Extraction ............................................................................... D-1

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
Appendix E – Statistical Modeling to Assess Effect Differences for Those Assigned to Medicaid and QHPs ....... E-1
Appendix F – Supplemental Payments, Claims Loading Process, and Per Member Per Month Logic ................. F-1
Appendix G – Geographic Information System (GIS) Processing ......................................................................... G-1
Appendix H – Weighted Average Price Calculations............................................................................................ H-1
Appendix I – Pregnancy Analytic Profile ................................................................................................................ I-1
Appendix J – Opioid Use Outcomes ...................................................................................................................... J-1
Appendix K – Consumer Assessment of Healthcare Providers and Systems (CAHPS) Sample Size
Calculation, Sampling Strategy, and Data Preparation ......................................................................................... K-1
Table of Figures
Figure 1. HCIP Premium and Cost-Sharing Reduction Breakdown ............................................................................... 3
Figure 2. Enrollment Pathways and Plan Assignment Process ..................................................................................... 4
Figure 3. HCIP Monthly Enrollment, January 2014–December 2016 ........................................................................... 6
Figure 4. Enrollment Age Demographics by Category .................................................................................................. 7
Figure 5. Premium and Cost-Sharing Reduction Breakdown, January 2014–December 2016 .................................... 8
Figure 6. Arkansas Demonstration Waiver Evaluation Logic Model............................................................................. 9
Figure 7. Arkansas Health Care Independence Program Period: System Evaluation ................................................. 10
Figure 8. Proportion of Medicaid and QHP Enrollees with a First Outpatient Care Visit, by Day .............................. 31
Figure 9. Health Care Independence Program Enrollment by Program and Month .................................................. 52
Figure 10. Charlson Comorbidity Index by Health Independence Account Non-Participants
(Made No Payment) vs. Participants (Made Payment) .............................................................................................. 56
Figure 11. Access Improvement Simulation Model Studying Scenario-Based Price Increases
to Medicaid Providers to Reach Commercial PMPM Payments ................................................................................. 75
Table of Tables
Table 1. Comparison Group Description and Analytical Data Populations ................................................................ 15
Table 2. Differences in General Population Geographic Access to Health Care between Medicaid and QHP
Enrollees ..................................................................................................................................................................... 28
Table 3. Differences in Higher Needs Population Geographic Access to Health Care between Medicaid and
QHP Enrollees ............................................................................................................................................................. 29
Table 4. Medicaid and Commercial Payer Price Differences for Outpatient Procedures by Provider Type .............. 30
Table 5. Differences in Perceived Access to Health Care between Medicaid and QHP Enrollees (Propensity
Score Matched Comparison) ...................................................................................................................................... 32
Table 6. Differences in Primary Preventive Health Care between Medicaid and QHP Enrollees (Propensity
Score Matched Comparison) ...................................................................................................................................... 32
Table 7. Differences in Secondary and Tertiary Preventive Health Care between Medicaid and QHP Enrollees
(Propensity Score Matched Comparison) ................................................................................................................... 33
Table 8. Differences in the Percentage of Medicaid and QHP Enrollees Receiving Recommended Disease
Management (Propensity Score Matched Comparison) ............................................................................................ 34
Table 9. Differences in the Use of Healthcare Services between Medicaid and QHP Enrollees (Propensity
Score Matched Comparison) ...................................................................................................................................... 35

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
Table 10. Differences in Rates of Preventable Hospitalizations and Readmissions between Medicaid and
QHP Enrollees (Propensity Score Matched Comparison) ........................................................................................... 36
Table 11. Differences in Utilization of Emergency Room Services between Medicaid and QHP Enrollees
(Propensity Score Matched Comparison) ................................................................................................................... 36
Table 12. Differences in Perceived Access to Health Care between Medicaid and QHP Enrollees (Regression
Discontinuity Comparison) ......................................................................................................................................... 37
Table 13. Differences in Primary, Secondary, and Tertiary Preventive Health Care between Medicaid and
QHP Enrollees (Regression Discontinuity Comparison ............................................................................................... 38
Table 14. Differences in Secondary and Tertiary Preventive Health Care between Medicaid and QHP Enrollees
(Regression Discontinuity Comparison) ...................................................................................................................... 39
Table 15. Differences in the Percentage of Medicaid and QHP Enrollees Receiving Recommended Disease
Management (Regression Discontinuity Comparison) ............................................................................................... 40
Table 16. Differences in the Use of Healthcare Services between Medicaid and QHP Enrollees (Regression
Discontinuity Comparison) ......................................................................................................................................... 41
Table 17. Differences in Rates of Preventable Hospitalizations and Readmissions between Medicaid and
QHP Enrollees (Regression Discontinuity Comparison) .............................................................................................. 42
Table 18. Differences in Utilization of Emergency Room Services between Medicaid and QHP Enrollees
(Regression Discontinuity Comparison) ...................................................................................................................... 43
Table 19. Maternal Pregnancy and Birth Outcomes, with Description ...................................................................... 44
Table 20. Maternal Pregnancy Differences between Medicaid and QHP Enrollees .................................................. 46
Table 21. Pregnancy Birth Outcomes between Medicaid and QHP Enrollees ........................................................... 46
Table 22. Differences in Non-Emergency Transportation between General Population Medicaid and QHP
Enrollees ..................................................................................................................................................................... 48
Table 23. Differences in Non-Emergency Transportation between Medicaid and QHP Enrollees (Propensity
Score Matched Comparison) ...................................................................................................................................... 48
Table 24. Differences in Non-Emergency Transportation between Higher Needs Population Medicaid and
QHP Enrollees ............................................................................................................................................................. 48
Table 25. Differences in Non-Emergency Transportation between Medicaid and QHP Enrollees (Regression
Discontinuity Comparison) ......................................................................................................................................... 49
Table 26. Health Insurance Carrier at 19 Years of Age for Medicaid Screened and Diagnosed Sickle Cell
Disease, Cystic Fibrosis, or Hemophilia (n=151) ......................................................................................................... 50
Table 27. Medicaid Enrollment History of QHP and 06 Medicaid Individuals Enrolled in June 2015 ........................ 53
Table 28. The Impact of Redetermination on QHP and 06 Medicaid Enrollees (Enrolled in July 2015) .................... 53
Table 29. HCIP Enrollment History of Individuals Enrolled in HCIP During 2016........................................................ 54
Table 30. Health Independence Account Eligible Population Demographic Profile................................................... 56
Table 31. Health Independence Accounts Cost-Sharing Expenditures....................................................................... 56
Table 32. Characteristics of Unmatched and Propensity Score Matched General Population .................................. 59
Table 33. Opioid Use Measures for Propensity Score Matched General Population Medicaid and QHP by
Assessment Period ...................................................................................................................................................... 60
Table 34. Comparison of Opioid Utilization for General Population Medicaid and QHP Enrollees ........................... 60
Table 35. Comparison of Number of Opioid Prescriptions by General Population Medicaid and QHP
(Reference) Enrollees .................................................................................................................................................. 61
Table 36. Characteristics of Higher Needs Population ............................................................................................... 62
Table 37. Opioid Use Measures for Propensity Score Matched Higher Needs Population Medicaid and QHP by
Assessment Period ...................................................................................................................................................... 62
Table 38. Comparison of Opioid Utilization for Medicaid and QHP Higher Needs Population Enrollees .................. 63

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report
Table 39. Change in Estimated Rate of Non-Emergent Emergency Room Visits per 100 Person-Years .................... 64
Table 40. Unadjusted Analysis of Urgent Care Facility Utilization and Cost ............................................................... 65
Table 41. Medicaid and QHP Enrollee General Population Propensity Score Matched Characteristics .................... 67
Table 42. Medicaid and QHP Enrollees General Population Propensity Score Matched Characteristics .................. 69
Table 43. Observed Utilization Rates (Per Member Per 100 Person-Years) for Medicaid and QHP Enrollees in
2014, 2015, and 2016 ................................................................................................................................................. 71
Table 44. Observed and Estimated PMPM Cost Scenarios for Medicaid and QHP Enrollees by Service
Category and Year ....................................................................................................................................................... 73

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report i
Executive Summary
Background
In 2013, like many other states across the country, Arkansas faced a complex series of political challenges
following the U.S Supreme Court decision on the Patient Protection and Affordable Care (PPACA) Act. Unlike any
other state in the South, however, Arkansas was able to successfully navigate these challenges to pursue a novel
approach to Medicaid expansion through the commercial sector. Through a Section 1115 demonstration waiver,
the state utilized premium assistance to secure private health insurance, offered on the newly formed individual
health insurance marketplace (the Marketplace), for individuals between 19 and 64 years of age with incomes at
or below 138 percent of the federal poverty level (FPL).
i
In 2014, Arkansas successfully established the Health Care Independence Program (HCIP),
ii
commonly referred to
as the “Private Option,” as designed under the terms and conditions of the Section 1115 demonstration waiver.
Through 2015, the estimated target-enrollment population of approximately 250,000 was met. Approximately
25,000 additional individuals eligible under the PPACA — and deemed to have exceptional healthcare needs —
were enrolled in the traditional Medicaid program. Finally, approximately 20,000 previously eligible but newly
enrolled individuals also obtained Medicaid coverage. By the end of 2016, the Private Option population totaled
approximately 280,000.
Arkansas’s healthcare providers have reported significant clinical and financial effects under the HCIP. In 2014,
federally qualified community health centers (FQHCs) reported increased success in attaining needed specialty
referrals for their clients.
iii
The Arkansas Hospital Association (AHA) reported significant annualized reductions in
uninsured outpatient visits (45.7 percent reduction), emergency room (ER) visits (38.8 percent reduction), and
hospital admissions (48.7 percent reduction).
iv
The state’s public teaching hospital reported a reduction in uninsured
admissions, from 16 percent to 3 percent, during the same time period.
v
These reductions persisted through 2016.
Competitiveness and consumer choice in the Marketplace have increased across the seven market regions in the
state with approximately 80 percent of the covered lives in the Marketplace enrolled through the Private Option.
In 2014, individuals in three out of the seven regions of the state — those marked by extreme poverty — only had
access to Arkansas Blue Cross and Blue Shield and Blue Cross Blue Shield Multi-State plans. By 2016, five carriers
were offering coverage across all seven market regions, with one market region having access to six carriers. A
sixth carrier operated in a single region restricted by Medicaid’s purchasing guidance limiting premium assistance
to those plans within 10 percent of the second-lowest cost silver plan in the market region. Over the three year
period, all plans experienced single digit rate increases.
For 2014, the estimated budget neutrality cap (BNC) was exceeded during the initial enrollment phase of the
program. The enrollment of younger individuals over time (affecting net premiums), the rebate of medical-loss
ratio (MLR) payments by one carrier not meeting the minimum MLR requirements in 2014, and inflationary
expectations brought cumulative program costs within the estimated BNC 2015 limit of $500.08 per member per
month (PMPM) and well under the 2016 limit of $523.58 PMPM.
Summary of Findings Based on Evaluation Hypotheses
The HCIP programmatic goals and objectives included successful enrollment, enhanced access to quality health
care, improved quality of care and outcomes, and enhanced continuity of coverage and care at times of re-
enrollment and during income fluctuations. These goals and objectives were to be achieved within a cost-effective

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report ii
framework for the Medicaid program, compared with what would have occurred if the state had provided
coverage to the same expansion group in Arkansas’s traditional Medicaid fee-for-service (FFS) delivery system.
The state’s required evaluation design under the terms and conditions of the Private Option waiver was
negotiated within 135 days of approval of the waiver on Sept. 27, 2013. The terms and conditions required the
evaluation to meet prevailing standards of scientific rigor, use the best available data, use controls and
adjustments for reporting limitations of the data, and discuss generalizability of results. Additional requirements
included a robust discussion of cost effectiveness. The state was required to submit a final Interim Evaluation
Report within 180 days of the end of the second year of the demonstration. That report is available
at www.achi.net.
The evaluation was conducted independently and with oversight of a National Advisory Committee consisting of
established leaders in major academic and medical centers around the country. The evaluation employed the
most current and well-established research design techniques to optimize confidence in observed findings. There
were two principle comparisons — the experiences of those with “Higher Needs” and that of the “General
Population.”
The Higher Needs population examined the approximately one-half of the newly eligible expansion population
who took a medical frailty screener to detect prior conditions and utilization. This information was used to
identify and compare similar individuals with higher needs that were placed in the traditional Medicaid program
versus those placed in QHPs through a quasi-experimental regression discontinuity approach.
The General Population consisted of the one-half of newly eligible that did not take the screener and were placed
in QHPs. They were paired with the approximately 40,000 newly enrolled adult Medicaid beneficiaries (woodwork
effect) and were matched using advanced propensity score techniques with appropriate statistical tests applied.
This report reflects the experience and findings from the three-year waiver for the Private Option, and major
findings are summarized below, grouped by questions of interest.
1. What were differences across access, quality, and outcomes between those enrolled in Medicaid and
those enrolled in commercial Qualified Health Plans (QHPs)?
A major assumption grounded in Arkansas’s use of premium assistance through the Marketplace was that
by utilizing the delivery system available to the privately enrolled individuals in the Marketplace, the
availability and accessibility of both primary care providers (PCPs) and specialists would be greater than
what would have been expected if Arkansas had utilized a traditional Medicaid expansion strategy. A
three-year enrollment comparison of Medicaid and commercial QHP beneficiaries in both the cohort with
Higher Needs and that in the General Population revealed:
The geographic proximity of available primary and specialty providers were similar for those
served by Medicaid and the QHP networks, and both met network adequacy requirements of the
Arkansas Insurance Department.
Initiation of care occurred more rapidly for enrollees in QHPs than for those in the Medicaid
program following enrollment.
In 2014, differences in the accessibility of both primary care and specialty providers were
reported, with QHP enrollees experiencing increased ability to get needed “care, tests, and
treatment” and receiving “an appointment for a check-up or routine care as soon as needed,”
compared to their Medicaid counterparts.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report iii
Perceived access differences improved after 18 months in the program for the General
Population. However, for individuals in the Higher Needs Population, Medicaid enrollees
continued to report more difficulty “receiving care when they needed it right away” and did not
always “find it easy to get the care, tests, and treatments they need,” compared to QHP enrollees
(range of differences 31-36 percent).
For Emergency Room (ER) use, differences were only observed within the General Population, in
which Medicaid enrollees experienced more ER visits in total, for both emergent and non-
emergent reasons, compared to QHP enrollees over the three years enrolled.
With the exception of QHP enrollees experiencing longer hospital stays compared to Medicaid
enrollees, there are no consistent differences across hospitalization measures.
For clinical services assessed for both populations — and for most measures studied — differences
in care and clinical service delivery were observed.
QHP enrollees were significantly more likely to receive individual clinical preventive services and
were more likely to receive all recommended screenings (a range of 24-94 percent relative
differences for the General Population).
QHP enrollees were significantly more likely to receive appropriate disease management services
and more likely to adhere to appropriate medication management than Medicaid enrollees (a
range of 31-55 percent relative differences for the General Population).
For pregnancy related care, no clinically significant differences were observed in the initiation of
prenatal services, complications of maternity care, or birth outcomes between QHP and Medicaid
enrollees.
With respect to non-emergency medical transportation, no differences were observed for the
General Population. However, for the Higher Needs Population, those in QHPs were 15 percent
less likely to miss a visit due to transportation issues.
Opioid use, while similar in the first year, diverged significantly in subsequent years, with
increasing numbers of prescriptions, high dose utilization, and concomitant benzodiazepine use in
the QHPs, compared to Medicaid enrollees.
With respect to Early Periodic, Screening, Diagnosis, and Treatment (EPSDT) services, we found no
indication that needed services were not available to individuals in premium assistance.
With respect to continuity of enrollment, both Medicaid and QHP enrollees experienced few
disruptions in coverage, with the exception being a mass eligibility redetermination undertaken in
the summer of 2015.
There were no statistically significant differences in mortality within the first three years of the
program.
2. What were the differences in costs between Medicaid and premium assistance?
The cost of providing coverage for Medicaid beneficiaries through premium assistance in QHPs was
expected to be greater than providing coverage through the traditional Medicaid FFS system. Exploration
and characterization of the contrasts between the two programs provided a better understanding of the
observed variations in access, utilization, and clinical impacts described above. In addition, dramatic

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report iv
differences in payment rates were observed, with QHP rates consistently exceeding those in the Medicaid
program:
Physician payment rates across outpatient services were approximately 95 percent higher in each
of the three years under study for enrollees in a QHP compared to their Medicaid counterparts
(e.g., In 2016, the weighted average per PCP visit was $94.03 for a QHP compared to $47.69 for
Medicaid);
For inpatient hospital stays, average QHP payments averaged $12,270 per discharge compared to
Medicaid payments of $7,778 (a 53 percent difference); and
In 2016, administrative costs were estimated to be $91.65 PMPM for QHPs and $64.33 PMPM for
Medicaid (a 29.8 percent difference).
Utilization differences were also observed, but not at the same magnitude as payment differentials.
Medicaid beneficiaries, under the traditional FFS system, experienced increased ER visits and
hospitalizations. Conversely, QHP beneficiaries received more outpatient visit contacts, and by 2016,
almost twice as many prescriptions.
3. What were the cost-effective aspects of premium assistance?
Cost-effectiveness for the purposes of this evaluation considered any benefits associated with care
delivered through QHPs at increased payment rates. To assess cost-effectiveness, total program costs for
enrolled individuals in QHPs were directly compared to their Medicaid counterparts. Ratios of
improvement in care to associated costs were developed (e.g., access improvements, clinical, and
utilization differentials compared to payment rate differentials).
In 2016, the weighted average payment to QHPs (premium and cost-sharing reductions) was $486 PMPM
or $5,832 per year, compared to Medicaid costs of $317 PMPM or $3,804 per year for each enrollee
(using existing Medicaid payment rates). Using the difference of $167 PMPM, select ratios of
improvement to access reflect the following:
For colorectal cancer screening in the General Population, the QHP cohort had a 94 percent
higher relative difference in screening rates. Thus, the marginal improvement is suggested to be
an increase of 5.6 percent per observed 10 percent increase in program costs associated with use
of premium assistance.
For the proportion who received all indicated clinical preventive services in the General
Population, the QHP relative difference of 25 percent greater than Medicaid suggests a 1.4
percent improvement in clinical performance per observed 10 percent increase in program costs.
For individuals with Higher Needs, QHP enrollees were 26 percent more likely to self-report
“always getting care when needed right away” and 18 percent more likely to find it “easy to get
the care, tests, and treatment needed.” This suggests a 1.1 percent improvement in access, per
observed 10 percent increase in program costs.
For individuals with Higher Needs, Medicaid enrollees experienced fewer outpatient events and a
concurrent higher rate of ER visits and hospitalizations. For each observed 10 percent increase in
program costs, QHPs were projected to achieve seven more physician office visits and avoid 2.5
ER visits per 100 person years.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report v
There were no clinical indicators in which Medicaid was favored.
Importantly, enrollees in QHPs received twice as many prescriptions than their Medicaid
counterparts. For each 10 percent increase in program costs, QHPs were projected to cover 78
additional prescriptions per 100 person years.
Over the three-year evaluation, PMPM claims costs for QHPs increased, a trend which was associated
with both increased utilization rates and provider rate increases. The established Medicaid rate schedule
does not incorporate inflationary adjustments, so no comparable increases were observed during the
evaluation. Continued divergence in experience, utilization, and payment rates will likely affect ratios of
improvement in care to associated program costs.
4. What would the Medicaid program have experienced if a traditional Medicaid expansion had been
adopted?
A core component of this demonstration evaluation is an examination of the hypothetical costs of
covering the entire expansion population through Arkansas’s traditional Medicaid program and
identifying the programmatic changes that would be necessary to achieve a similar outcome to that
experienced through premium assistance. In 2013, prior to the PPACA expansion, Arkansas had one of the
lowest Medicaid eligibility thresholds for non-disabled adults in the U.S., covering only 24,955 non-
disabled adults with a full benefits package.
In 2014, following PPACA expansion, an additional 267,482 individuals were covered:
approximately 17,300 (6.5 percent) previously eligible but newly enrolled;
approximately 25,000 (9.3 percent) PPACA eligible but with exceptional healthcare needs;
and 225,000 (84.2 percent) PPACA eligible with premiums purchased on the individual marketplace.
These 267,482 individuals represented 16.0 percent of the total 19- to 64-year-old population in the state.
In 2016, this number increased to 330,943 covered lives:
approximately 22,375 (6.8 percent) PPACA eligible but with exceptional healthcare needs;
32,427 (9.8 percent) interim status before enrollment in a QHP;
and 276,141 (83.4 percent) PPACA eligible with premiums purchased on the individual marketplace.
vi
These 330,943 individuals represent 19.1 percent of the working-aged adults within the state.
Thus, because of the high rates of uninsurance and low Medicaid eligibility prior to the PPACA, Medicaid
has experienced a 13-fold increase in coverage for the non-disabled 19- to 64-year-old population.
Traditional microeconomics principles would suggest that increased demand through the expansion of the
Medicaid program would place increasing price pressure on the rate structure of the existing Medicaid
program. The observed differences in payment rates between QHPs and Medicaid described above could
lead to unsustainable access differentials for Medicaid enrollees. Any potential increase in payment rates
would affect not only the new expansion population, but also enrollees under the same payment rate
schedule across the entire Medicaid program. To model the potential effects, a budgetary impact analysis
was conducted on increasing payment rates across the Medicaid program.
Three increasingly fiscally conservative scenarios were simulated for alternative expansion options
through the existing Medicaid FFS system, the counterfactual, to provide policymakers with
conditions under which necessary increases to achieve equitable access could be considered. They

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report vi
included: 1) claims potentially associated with wage-sensitive services; 2) restricted claims associated
with major medical services; and 3) restricted to claims associated only with physician billed services.
The budget impact analysis revealed that costs to the Medicaid program would exceed the increased
costs associated with premium assistance:
if wage-sensitive payment rates had increased by 29 percent;
if claim payments associated with clinical services had increased by 45 percent; or
if physician-only claim payments had increased by 64 percent;
Importantly, under the most conservative scenario of increases restricted to physician-only claims, the
physician rate increase at which the Medicaid program costs exceed those of premium assistance remains
36 percent below the commercial payment rates observed. This suggests the likelihood of continued
differential access despite increased payments.
These findings suggest that with the 13-fold increase in enrollment of 19- to 64-year-olds, plausible
required increases in Medicaid payment rates across the entire program would exceed the costs
associated with purchasing commercial coverage through premium assistance.
Conclusion
The three-year evaluation of the Private Option is the first direct comparison of commercial insurance with
Medicaid since Medicaid’s inception in 1965. Through Arkansas’s use of premium assistance, and as a
consequence of the rigorous CMS evaluation requirements of the waiver, previously unfeasible direct
comparisons of system performance have been enabled.
Arkansas Medicaid achieves comparable participation in its network, compared to QHPs, for both primary and
specialty providers. However, likely due to markedly higher provider payment rates and more active enrollee
management, the network adequacy and clinical performance of the QHPs exceeds that of Medicaid. These
differences have an impact on the uptake of clinical preventive services, appropriate disease management, and
utilization of emergency room services. For those with Higher Needs, perceived barriers to getting care when
needed and getting necessary tests and treatments are persistent for Medicaid.
For pregnancy, where Medicaid previously covered a majority of deliveries and had invested significant
performance improvement efforts, no advantage was observed for treatment in the commercial sector at higher
reimbursement rates. In addition, Medicaid achieved reduced opioid consumption compared to the commercial
sector, likely due to more assertive programmatic restrictions.
In the first three years of the program, no differences in mortality were observed between enrollees in Medicaid
and those in the commercial sector.
Systemic effects on the Arkansas healthcare landscape through the use of premium assistance was significant. By
guaranteeing purchase for over 250,000 individuals and establishing purchasing guidelines, at a time when
surrounding states were facing major challenges in the stability of their markets, the Arkansas Health Insurance
Marketplace experienced exceptional stability, marked increase in competition, and single-digit rate increases
across the three years. In addition, Arkansas has experienced no hospital closures — with service expansion in
some underserved areas — further distinguishing its overall system stability from neighboring states and from the
rest of the country.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report vii
Finally, while the costs of premium assistance exceed those modeled under a static Medicaid expansion scenario,
it is unlikely that Arkansas Medicaid would have been able to absorb a 13-fold increase in enrollees and meet the
federal equal access requirements, under which the state is subject to judiciary review, without considerable
adjustment to provider rates. Although political discourse has highlighted concerns about the differences in
absolute cost between commercial and Medicaid alternatives, Medicaid expansion scenarios under which similar
clinical experiences would be achieved suggest budgetary outcomes that may mitigate these concerns.
These findings may have limited applicability to other states. Few states had the restrictive Medicaid eligibility
threshold, resulting in dramatic increases in coverage through expansion. In addition, provider rate differentials
between Medicaid and commercial plans are also unlikely to exceed those in Arkansas.
However, these findings do support direct comparisons of both commercial and Medicaid costs and performance
across states. These differential payment rates and associated results raise questions regarding the ability of
Medicaid programs nationwide to meet the federal equal access requirements through delivery system strategies
that pay providers significantly lower rates.
The innovative use of premium assistance and the integrated relationship between the individual Marketplace
and the Arkansas Medicaid program merit continued observation. The demonstration waiver through which
Arkansas implemented the Private Option was extended in January of 2017, enabling the successor premium
assistance program, “Arkansas Works.” With work requirements, workforce training, and/or community service
for a subset of enrollees implemented in June 2018, further evaluation of the use of premium assistance and the
impact on upward social mobility is warranted.
i
The Centers for Medicare & Medicaid Services [Letter] to Andy Allison, Arkansas Department of Human Services. September
2013. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ar/Health-Care-
Independence-Program-Private-Option/ar-private-option-app-ltr-09272013.pdf.
ii
Ark. Code § 2-77-2405 (2014).
iii
Susan Ward-Jones, MD. Personal Communication. March 12, 2015.
iv
Arkansas Hospital Association. APO’s Hospital Impact Strong in 2014. The Notebook. 2015;22(22):1.
http://www.arkhospitals.org/archive/notebookpdf/Notebook_07-27-15.pdf.
v
Dan Rahn, M.D., Testimony before Health Reform Legislative Taskforce. August 20, 2015.
vi
Arkansas Department of Human Services (DHS). (2016, December 31). Arkansas Private Option 1115 Demonstration
Waiver. Quarterly Report October 1, 2016-December 31, 2016 [Report]. Retrieved from
https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ar/Health-Care-
Independence-Program-Private-Option/ar-works-qtrly-rpt-oct-dec-2016.pdf

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 1
Introduction
Background
The U.S. Supreme Court’s June 2012 ruling
1
allowed states to decide whether to extend Medicaid benefits to their
citizens who qualified under the Patient Protection and Affordable Care Act (PPACA) expansion. This amplified the
political polarization about the PPACA at the state level, resulting in varied decisions about expansion. Historically,
states have had the option to implement Medicaid coverage through direct provider reimbursement, Medicaid
managed care contracts, or the purchase of coverage with premium assistance through employer-sponsored
coverage.
The state of Arkansas, navigating the political barriers facing many states, pursued a novel approach to expansion
through the commercial sector. Through a Section 1115 demonstration waiver, the state utilized premium
assistance to secure private individual health insurance offered on the newly formed individual health insurance
marketplace (the Marketplace) to individuals between 19 and 64 years of age with incomes at or below 138
percent of the federal poverty level (FPL).
2
The Arkansas Health Care Independence Program (HCIP),
3
commonly
referred to as the “Private Option,” provided coverage to more than 225,000 low-income Arkansans through
2015. By the end of 2016, approximately 300,000 individuals were enrolled.
One component of the waiver’s terms and conditions is a required evaluation of differences in access, quality,
outcomes, and efficiencies achieved through the use of commercial coverage for the low-income expansion
population.
4
The interim evaluation
5
examined first-year programmatic differences in both effects and costs
through commercial premium assistance compared to the experience that would have been achieved through a
traditional Medicaid expansion as a principal outcome of interest for the demonstration. The final evaluation, and
content of this report, examines the three-year experience of individuals enrolled in the HCIP program.
Arkansas Profile
Arkansas is a largely rural state with approximately 3 million citizens, many of whom face significant healthcare
challenges. These include high health-risk burdens, low median-family income, high rates of uninsured individuals,
and limited provider capacity, particularly in non-urban areas of the state. The Health Resources and Services
Administration has designated 74 of Arkansas’s 75 counties as medically underserved.
6
Prior to the PPACA, 25
percent of adult Arkansans between 18 and 64 years of age were without health insurance.
7
Arkansas’s Medicaid program prior to the HCIP had one of the most stringent eligibility thresholds in the nation
for adults, largely limiting coverage to the aged, disabled, and parents with extremely low incomes and limited
assets. Eligibility for adults between 19 and 64 years of age was restricted to parents/caretakers earning at, or
below, 17 percent FPL. Prior to expansion, non-disabled adults with full benefits comprised 18 percent of
Medicaid beneficiaries.
8
Expansion of the program under the PPACA more than doubled the number of eligible
19- to 64-year-old beneficiaries.
The Arkansas Medicaid program is a Primary Care Case Management (PCCM) fee-for-service (FFS) based delivery
system. Individuals are assigned to a primary care provider (PCP) and providers may limit the number of Medicaid
beneficiaries assigned.
9
Medicaid provider reimbursement rates are significantly below their commercial
counterparts. Supplemental payments for select hospitals — critical access hospitals, public and private hospitals,
and state teaching hospitals — have been used to support delivery-system stability. Providers elect to join as a
qualified Medicaid provider, but may limit the number of Medicaid beneficiaries they serve.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 2
The commercial insurance marketplace has historically consisted of two carriers with statewide coverage,
including a dominant carrier with over 65 percent of private coverage penetration and other regional carriers. The
predominant network structure is preferred provider organizations with limited managed care and/or the
presence of restricted networks. This is, in part, due to Arkansas’s “any willing provider”
10
law, requiring insurers
to allow any provider willing to accept terms for the class of providers into their networks. Under the PPACA, the
state elected to utilize the Federally Facilitated Marketplace (FFM) partnership in which the state conducts plan
management and consumer outreach.
11
Proactive consumer outreach and advertising was limited to responsive
consumer support based upon state legislative restrictions.
Arkansas Structure of Commercial Premium Assistance
The Arkansas approach utilizing commercial premium assistance has several unique attributes that successfully
meet both Medicaid requirements and protections while enabling commercial sector independence. The state’s
approach was in large part based upon the hypotheses that Arkansas could not meet the equal access provision
requiring state Medicaid provider payments to be “consistent with efficiency, economy, and quality of care and
...sufficient to enlist enough providers so that care and services are available under the plan at least to the extent
that such care and services are available to the general population in the geographic area.”
12
Successful use of the
commercial plans offered on the Marketplace explicitly meet the equal access provision of Medicaid
requirements. However, several structural elements warrant acknowledgement and are described.
First, Medicaid’s purchase of individual commercial coverage via premium assistance is fundamentally different
from the historic use of Medicaid managed care. In premium assistance, the Medicaid program does not directly
contract with the private carrier but rather purchases plans offered on the individual marketplace. While a
memorandum of understanding was established between the state, Medicaid, the Arkansas Insurance
Department (AID), and each carrier to facilitate payments, plans are governed by AID through existing state law
and certification requirements (e.g., network adequacy). The Medicaid population is then integrated into the
privately insured risk pool, and provider payment rates are established by commercial carriers, not through
independent Medicaid contracts. Medicaid beneficiaries engage providers with commercial insurance cards and
are not separated into a Medicaid-specific program or plan.
Second, plans offered under the PPACA were utilized to meet a majority of the Medicaid cost-sharing protections.
For individuals at or below 100 percent FPL, the state utilized the 100 percent actuarial value (AV) plan required to
be available for Native Americans. For Medicaid beneficiaries between 101 and 138 percent FPL, the state utilized
the high-value silver 94 percent AV plan required to be offered on the Marketplace to individuals between 101
and 150 percent FPL. The remaining Medicaid-required cost-sharing protections were achieved through active
structuring of allowable deductibles and other cost sharing.
13
Importantly, these plans consist both of premiums
subject to medical-loss ratio (MLR) requirements of 80 percent and of cost-sharing reductions (CSRs) that are to
be fully reconciled (see Figure 1).
AID divided the state into seven geographic market regions, and carriers established age-specific premiums within
market regions (one carrier incorporated allowable tobacco use surcharges). The costs of premium assistance
through the individual marketplace was thus influenced by the premium variation based on age within each
market region, the age distribution of those deemed eligible, CSRs paid, and any subsequent repayments for
failure to meet MLR requirements or reconciliation of CSR.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 3
Figure 1. HCIP Premium and Cost-Sharing Reduction Breakdown
Finally, the impact of Medicaid’s guaranteed purchase in the individual insurance market had the potential to
convey stability to the individual marketplace and improve the actuarial profile of the risk pool. The HCIP Act
further extended potential benefits to the actuarial profile of the individual marketplace by requiring that
individuals who were medically frail or had exceptional healthcare needs requiring supplemental Medicaid
benefits would be retained in the traditional Medicaid program.
Arkansas Structure of PPACA Eligibility and Enrollment
As an FFM partnership with the state conducting plan management and consumer assistance combined with
Medicaid’s use of premium assistance, the Arkansas structure for PPACA eligibility and enrollment was complex.
Arkansas used three enrollment pathways for eligibility determination for beneficiaries: the Arkansas Department of
Human Services (DHS) Supplemental Nutrition Assistance Program (SNAP); an Arkansas eligibility web portal
(access.arkansas.gov); and the federal Healthcare.gov portal. Following eligibility determination, individuals were
directed to a separate enrollment portal (insureark.org) to facilitate a healthcare needs assessment and plan selection.
Additional cost-sharing reduction for
HCIP enrollees from 0% to 100% FPL
Deductible buy-down for HCIP enrollees
from 101% to 138% FPL
Cost-sharing reduction for enrollees
from 139% to 150% FPL
Premium
3.5%
2.5%
24.0%
70.0%
100%
PMPM cap including
wrap-around costs:
2014: $477.63
2015: $500.08
2016: $523.58
Audit Processes:
Subject to reconciliation
Subject to medical loss ratio
* Actual PMPM costs were $485.84 (186,950 enrollees) in 2014, $486.86 (200,703 enrollees) in 2015, and $478.61
(276,141 enrollees) in December 2016.
Source: “Arkansas Health Care Independence Program Annual Cap.” Arkansas Department of Human Services
and Arkansas Department of Human Services Final Private Option Report, 2016.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 4
The SNAP-facilitated eligibility determination strategy was a time-limited effort to reach out to and engage with
potentially eligible beneficiaries. Through prior income determination for SNAP benefits, DHS identified
individuals and notified them of their eligibility. Redetermination of income or family composition was not
conducted. Individuals who affirmed their desire for coverage in response to the notice were directed to the
enrollment website. The Arkansas eligibility portal was utilized by DHS county offices, outreach workers,
community and faith-based organizations, and insurance agents across the state. Individuals thought to be
Medicaid-eligible were directed to the portal, where eligibility applications and FPL determinations were
processed. The enrollment pathways and plan assignment process for 2014 enrollment is depicted in Figure 2.
Figure 2. Enrollment Pathways and Plan Assignment Process
As in other states, individuals and the state both experienced challenges in the first year of the federal
Healthcare.gov portal.
14
Individuals identified through the federal portal and deemed to be Medicaid eligible were
transferred to the state for determination. Frequently, unsuccessful transfer of information resulted in
incomplete enrollments, with similar experiences noted by commercial carriers for individuals above 138 percent
FPL. Over time, the volume of enrollees and accuracy of eligibility information improved.
Two categories of eligible individuals were observed. One category was comprised of individuals who had
previously been eligible for traditional Medicaid benefits but had not enrolled and then subsequently applied and
were determined to be eligible. These individuals were placed into the Medicaid program. The second category
included individuals newly eligible under the PPACA — parents/caretakers from 18 to 138 percent FPL and
childless adults from 0 to 138 percent FPL. These individuals were eligible for commercial premium assistance
under the demonstration waiver. Prior to commercial enrollment, however, individuals were asked to complete a
Enrollment Portals
SNAP
Eligible
PPACA
Newly
Eligible
≤ 138% FPL
Previously
Eligible
Newly Enrolled
Plan
Selected
> 138%
FPL
Auto
Assigned
Federally
Facilitated
Health Insurance
Marketplace
(healthcare.gov)
Arkansas
Eligibility &
Enrollment
System

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 5
Healthcare Needs Assessment Questionnaire (the Questionnaire) to retain those with exceptional healthcare
needs in the traditional Medicaid program.
As required in the HCIP Act, these retained individuals were to include those “…determined to be more effectively
covered through the standard Medicaid program, such as an individual who is medically frail
a
or other individuals
with exceptional medical needs for whom coverage through the Health Insurance Marketplace is determined to
be impractical, overly complex, or would undermine continuity or effectiveness of care.” No previously developed
and validated tool for this purpose was known to exist.
The Arkansas Center for Health Improvement (ACHI) and the Arkansas DHS Division of Medical Services
collaborated with experts at the University of Michigan and the Agency for Health Care Research and Quality
(AHRQ) to develop a screener to identify newly eligible Medicaid applicants who had exceptional healthcare
needs. A pooled subsample from the Household Component of the Medical Expenditure Panel Survey (MEPS),
2005-2010,
15
was used to develop the Questionnaire and scoring thresholds. Questionnaire responses grouped
individuals into one of three categories:
1) Exceptional healthcare needs (Frail): those who reported exceptional healthcare needs as represented by
deficits in their “activities of daily living,” having severe mental illness, and/or being dependent or homeless;
2) Exceptional healthcare needs (Threshold): those who reported high healthcare use in the prior six months
through hospitalization, emergency room, and/or outpatient visits who met the predetermined threshold; or
3) No exceptional healthcare needs: those completing the Questionnaire who did not meet any criteria
outlined in (1) or exceed the predetermined threshold.
Individuals completing the screener and deemed as not having exceptional healthcare needs proceeded to select
plans offered on the individual marketplace through the state’s enrollment portal. The predetermined threshold
target was selected to achieve 10 percent retention for PPACA-newly eligible within the Medicaid program as
operationalized from the HCIP contract.
Importantly, approximately 50 percent of those determined to be PPACA eligible did not proceed to the
enrollment portal and complete the Questionnaire. After a maximum of 45 days, these individuals entered an
auto-assignment process. Individuals were auto-assigned to carriers based upon previously determined ratios tied
to the number of carriers in each of the seven insurance market regions. Auto-assigned individuals had a time-
limited opportunity to take the Questionnaire and choose to change carriers. Individuals could either choose to
stay with their assigned plan or choose another plan during subsequent open-enrollment periods each year or for
qualifying family events.
Following selection or auto-assignment, DHS executed monthly premium payments to the carriers on behalf of
the individuals. Individuals in the commercial plans received a letter with their Medicaid Identification Number (to
receive services prior to commercial plan coverage start date) and, subsequently, a commercial insurance card
from their carrier. Medicaid-retained individuals received a Medicaid benefit card.
In the second half of 2015 and all of 2016, DHS opted not to use the threshold method to identify individuals who
had exceptional healthcare needs. However, DHS continued use of the question about deficits in activities of daily
living to identify individuals with exceptional healthcare needs. New individuals enrolling in these years who did
not take the Questionnaire were still assigned to a QHP.
a
Note that “Medically Frail” as defined in the HCIP Act and operationalized in the HCIP preceded the current definition of
“Medically Frail” as found in 42 CFR 440.315(f).

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 6
Arkansas HCIP Program Experience
Figure 3. HCIP Monthly Enrollment, January 2014–December 2016
Enrollment in the HCIP and for other newly eligible individuals, both within Medicaid and for those above 138
percent FPL in the individual marketplace, resulted in a reduction in the uninsured rate for adults from 22.5
percent to 9.6 percent in 2014, the largest reduction observed nationwide.
16
More than 250,000 Arkansans
enrolled, with approximately 45,000 occurring through the SNAP-facilitated eligibility. In 2014, approximately half
completed the Questionnaire. Of the total new enrollees, 10 percent were deemed to have exceptional
healthcare needs and were maintained in traditional Medicaid. In 2014, an additional 22,000 adults previously
eligible (but not enrolled) for traditional Medicaid became newly enrolled in the program. In the three years of
the program, Medicaid has purchased individual plans covering at least one month for 399,330 individuals and
276,081 were enrolled in December 2016 (see Figure 3) through the premium assistance mechanism.
17
Through 2016, HCIP enrollees represent approximately 80 percent of the covered lives on the individual
marketplace. They are younger than their counterparts above 138 percent FPL participating in the Marketplace
(see Figure 4 for Year 1 age demographic comparison).
18
,
19
0
50,000
100,000
150,000
200,000
250,000
300,000
Jan
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
HCIP Commercial Insurance Coverage
2014
2015
2016

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 7
Carrier participation, and thus
beneficiary choice, has increased in
each market region. In 2014, of the
seven market regions, only three
had more than two carrier options.
Statewide, in 2016, every region
had at least five participating
carriers, with one region having six.
Premiums for the benchmark silver
plan in the largest market region
dropped 2.3 percent in 2015 and
experienced an increase of 3.7
percent in 2016.
20
Because
insurance premiums external to the
Marketplace are tied to those on
the Marketplace, similar rate effects were seen in the non-Marketplace PPACA-compliant market.
Healthcare providers have reported both significant clinical and financial effects. Federally qualified community
health centers (FQHCs) have reported increased success in attaining needed specialty referrals for their clients.
21
The Arkansas Hospital Association (AHA) compared service use and uninsured volumes between 2013 and 2014.
They found a 5 percent increase in ER visits overall, and a reduction in outpatient visits (45.7 percent), ER visits
(38.8 percent), and hospital admissions for the uninsured population.
22
The University of Arkansas for Medical
Sciences (UAMS) has reported a reduction in uninsured admissions, from 16 percent to 3 percent, during a similar
time period.
23
The Section 1115 demonstration waiver required an estimated budget neutrality cap (BNC) represented as a per-
member per month (PMPM) cost for program expenditures.
4
These expenditures include premiums, CSRs, and
required Medicaid benefits (wrap-around costs associated with required benefits, such as non-emergency
transportation) not covered through premium assistance. Average program expenditures over the program years
have been within the estimated budget neutrality caps established within the conditions of the Section 1115
demonstration waiver with cumulative program expenditures at the beginning of Program Year 3 (PY3) (January
2016) equal to $489.01 PMPM, 7.1 percent below the PY3 — Calendar Year (CY) 2016 — federal cap of $526.58.
During Program Year 1 (PY1) — CY 2014 — cumulative program expenditures exceeded the BNC, but were under
the estimated cap by Program Year 2 (PY2) — CY 2015. The first months of 2016 saw the PMPM under the BNC
but eventually exceeded it by the end of the year. Early in 2017 there was a substantial differential between
PMPM and the 9 percent increase in BNC from 2016.
17
This includes the effects due to the enrollment of younger
individuals over time affecting net premiums, the rebate of MLR premiums by one carrier who did not meet the
MLR requirements, and inflationary expectations built into the BNC estimates. Importantly, this evaluation will
replace BNC estimates with realized experience.
41%
25%
23%
19%
22%
23%
15% 33%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
With Premium Assistance Without Premium Assistance
Percentage Enrolled Through the
Health Insurance Marketplace
Age 34 and Younger Age 35-44 Age 45-54 Age 55-64
Figure 4. Enrollment Age Demographics by Category

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 8
Figure 5. Premium and Cost-Sharing Reduction Breakdown, January 2014–December 2016
$477.63
$500.08
$523.58
$440
$450
$460
$470
$480
$490
$500
$510
$520
$530
0
50k
100k
150k
200k
250k
300k
J F M A M J J A S O N D J F M A M J J A S O N D J F M A M J J A S O N D
2014 2015 2016
Per Member Per Month
Enrollees
HCIP Monthly Enrollment and Total Costs
Enrollees PMPM Cost 2014 Budget Cap 2015 Budget Cap 2016 Budget Cap
(4.7% increase)
(4.7% increase)
Over the three years of the HCIP program, management has moved from a start-up to a steady-state phase. The
first six months of 2014 contained significant enrollment growth, followed by 12 months of relative steady-state
program performance. In the fall of 2014, income and eligibility redeterminations for Medicaid were delayed due
to information technology limitations on the eligibility and enrollment system. In July 2015, restarting these
determinations resulted in termination of coverage for approximately 10 percent of the covered lives.
24
Finally, in
2016, DHS implemented purchasing strategies through which premium assistance would only be available for
plans that were priced within 10 percent of the second lowest silver plan within the market region.
25
Arkansas HCIP Evaluation Strategy
The terms and conditions of the Section 1115 demonstration waiver state the requirements for submission of an
interim report following completion of the second programmatic year. Through a subsequent modification of the
waiver terms and conditions, a final summative report profiling the complete three-year HCIP experience using
fully adjudicated claims data was due by June 30, 2018. This document serves as the final summative report and
represents outcomes from the full three programmatic years of the HCIP. As expected, the Interim Report
reflected the start-up period in the first year and had certain limitations — quality metrics requiring enrollment
periods of 12 months or greater were problematic; continuity of care and coverage was not yet observable; and
steady state comparisons of system performance were premature. However, variations in experienced access,
utilization by types and location of services, and healthcare engagement opportunities to address unmet needs
were the focus of the Interim Report. Costs for the primary comparison of premium assistance to what would
have been experienced under a traditional Medicaid expansion were simulated in Year 1. We update these
simulations based on cost comparisons at the end of 2016. The CSR reconciliation for any of the three years of

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 9
HCIP have not been finalized and, hence, are not included in the financial description of the program in this
report. However, this final report presents quality metrics for up to three years of coverage in the program and
also includes a broader set of indicators.
In this report, we profile cost estimates covering the three years of the HCIP program; assess quality of care for
the Medicaid and QHP plans during a steady state period (2016); present an evaluation of continuity of care and
coverage following the redetermination period (July 2015–December 2015); conduct a comparison of Medicaid
and QHP pregnancy quality indicators; include a discussion of the EPSDT population that was eligible for QHP
enrollment; include a special section on opioid utilization; include a section on mortality difference between
Medicaid and QHP enrollees; and re-examine changes in the effectiveness and costs associated with the use of
premium assistance for Medicaid beneficiaries.
Research Design and Approach
Goals and Objectives
The HCIP programmatic goals and objectives included successful enrollment, enhanced access to quality health
care, improved quality of care and outcomes, and enhanced continuity of coverage and care at times of re-
enrollment and income fluctuation. These goals and objectives were to be achieved within a cost-effective
framework for the Medicaid program compared with what would have occurred if the state had provided
coverage for the same expansion group in Arkansas Medicaid’s traditional delivery system.
Figure 6. Arkansas Demonstration Waiver Evaluation Logic Model
Following the evaluation logic model (see Figure 6), this final report presents results from analyses that used
geographic travel time between enrollees and providers, enrollment information, and retrospective claims data,
and sampled survey responses. Using two different comparison groups and approaches, the evaluation team
Improved
Prevention and
Outcomes
Improved
Access to
Providers and
Healthcare
Services
Successful
Enrollment
Through
Marketplace,
State
Enrollment
Portal, and/or
Targeted
Outreach
Continuity of Enrollment and Reduced Churn
Cost-Effectiveness for Medicaid via
System Reform

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 10
empirically assessed whether QHP enrollees obtained better access to providers and healthcare services by using
commercial carrier networks and payment rates than comparable groups enrolled in traditional Medicaid. We
also assessed whether QHP enrollees received more appropriate care — including prevention, chronic disease
management, and therapeutic interventions potentially leading to better outcomes than their Medicaid
counterparts. This report also contains a profile of the effects of disruptions in continuous insurance coverage
(“churn”), highlighted by experiences after a universal eligibility redetermination in July 2015. Differences in
program costs between premium assistance and traditional Medicaid were determined and evaluated with
respect to differences in access, utilization, quality, and outcomes. In addition, the alternative of expansion solely
within the traditional Medicaid program was assessed by examining program impact and simulating alternative
payment scenarios with the goal of achieving similar outcomes.
Programmatic Timeline and Reporting Requirements
Under the terms of the Section 1115 demonstration waiver, two reports were required to be submitted that
characterize the experiences of individuals enrolled in Qualified Health Plans (QHPs) using premium assistance — the
Interim Report reflecting the first 12 months of programmatic experience, and the Final Report reflecting the three
years of the originally approved waiver. A key component of both required reports is a comparison of QHP enrollee
experiences to similar cohorts of new enrollees in traditional Medicaid. Another key component is a counterfactual
analysis through budget impact simulations of what it would have cost Medicaid through a traditional expansion to
achieve similar access, quality, and outcomes of the QHPs.
Efforts to optimize comparisons of care between that which is provided through commercial premium assistance
and that which is provided through the Medicaid program have been incorporated into this demonstration
evaluation. Program experience has included a significant uptake period during the initial six months of the
program followed by 12 months of steady state program enrollment due to delays in eligibility redeterminations
by DHS. Redeterminations in the summer of 2015 resulted in a number of previously enrolled individuals being
terminated (10 percent) from Medicaid and premium assistance programs, leading to a stimulus for discontinuity
of coverage and care. Finally, the state extended the HCIP premium assistance program (now called Arkansas
Works) through 2021,
26
which has continued the three-year HCIP demonstration into Year 4. As depicted in Figure 7
we have modified the original timing of evaluation components in response to these programmatic experiences.
Figure 7. Arkansas Health Care Independence Program Period: System Evaluation
This final report includes assessments of care using enrollment and claims data for the three program years of
2014 through 2016 and survey data from two enhanced Consumer Assessment Health Plan Surveys. Assessments

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 11
of quality and utilization data will reflect the steady state periods depicted, and continuity assessments will
evaluate the impact of redeterminations in 2015. In addition, cost-effectiveness and counterfactual simulations
will be reported by year, with 2016 being the first full year of steady state.
Theoretical Approach
The approach and content of this evaluation focuses on a comparison between access, quality, and outcomes
experienced by Arkansans enrolled in traditional Medicaid versus those enrolled in a QHP through premium
assistance. We also evaluate the cost-effectiveness of offering private health insurance by covering costs through
premium assistance, as opposed to expanding the Medicaid program, and assess the counterfactual experience
that would have been expected through the expansion of the traditional Medicaid program. Questions addressed
in this final report include (note that first year experience findings are summarized in this section, under
subsection g):
1. What were the differences associated with access, quality, and outcomes between those enrolled in
Medicaid and those enrolled in QHPs?
A major assumption grounded in Arkansas’s use of premium assistance through the Marketplace was that by
utilizing the delivery system available to the privately enrolled individuals in the Marketplace, the availability
and accessibility of both primary care providers and specialists would have exceeded that of a more
traditional Arkansas Medicaid expansion. By purchasing health insurance offered on the Marketplace and
utilizing private sector provider networks and their established payment rates, traditional barriers to
equitable health care, including limited specialist participation and provider availability, would be minimized.
In fact, through the use of commercial plans offered on the Marketplace, providers were not able to
differentiate between privately insured individuals supported by Medicaid premium assistance (e.g., those
earning less than 138 percent FPL), those supported by tax credits (139 to 400 percent FPL), and those earning
above 400 percent FPL who purchased from carriers offering plans in the Marketplace.
The PPACA required, through federal regulation, that QHPs “…maintain a network that is sufficient in
number and types of providers, including providers that specialize in mental health and substance abuse
services, to assure that all services will be accessible without unreasonable delay.”
27
AID has developed
network adequacy targets and data submission requirements to ensure adequacy of provider networks in
QHPs offered in the Marketplace. AID established network adequacy requirements to be reported by
participating carriers on an annual basis. This reporting requires data to be submitted, demonstrating a 30-
mile or 30-minute coverage radius from each general/family practitioner or internal medicine provider, and
each family practitioner/pediatrician. In addition, data/maps must be submitted demonstrating a 60-mile or
60-minute coverage radius from each category of specialist including, but not limited to, cardiologists,
endocrinologists, obstetricians, oncologists, ophthalmologists, psychiatric and state licensed clinical
psychologists, and pulmonologists. In addition to geographic access, perceived access indicators from
Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys and realized access from first
contact with new providers upon becoming insured will identify differences to providers of traditional
Medicaid enrollees to those in QHPs.
To assess quality and outcomes, measures were selected based on National Quality Forum (NQF) guidelines, and
peer reviewed studies that rate and compare health plans and providers. This included reviews of national
healthcare quality guidance, including AHRQ National Healthcare Quality Reports (Agency for Healthcare
Research and Quality, 2012 and 2013 National Healthcare Quality Reports), the U.S. Department of Health and

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 12
Human Services Annual Progress Report to Congress (“National Strategy for Quality Improvement: 2013 Annual
Progress Report to Congress,” July 2013) the Centers for Medicare and Medicaid Services (“Medicaid Core Set:
Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid: Technical Specifications and Resource
Manual for Federal Fiscal Year 2014 Reporting,” May 2014, CMS), CAHPS Reporting Guidance (CAHPS Reporting:
Reporting Measures for CAHPS® Health Plan Survey 4.0.), and National Committee for Quality Assurance (NCQA)
Healthcare Effectiveness Data and Information Set (HEDIS).
28
For this final report that spans individual healthcare coverage experience for up to three years, we used
validated quality, utilization, and outcome measures studied from the sources listed above to meet two
criteria. We chose measures that could be assessed efficiently by patient self-report or by administrative
claims data (measures requiring electronic medical/hospital records or provider reporting sources were
excluded), and that have been previously used to assess care for Medicaid and commercially insured patients.
Final measures for empirical testing were a priori, selected based on oversight from the National Advisory
Committee for this evaluation. The final listing of measures empirically tested to determine differences in
access, quality, and outcomes between Medicaid and QHP enrollees are contained in Appendix A.
2. What were the differences in costs between Medicaid and premium assistance?
Costs to the program were taken from the perspective of the Medicaid program as the payer. For commercial
costs, these included the PMPM premium payments made to commercial carriers on behalf of enrolled
individuals. These PMPM premiums were specific to market region, age, and for one carrier, tobacco status. In
addition to premiums, CSR payments to commercial carriers to achieve Medicaid out-of-pocket cost-sharing
limits were included. Medicaid expenditures for non-covered benefits in the commercial plans — e.g., non-
emergency medical transportation (NEMT) — were also included. Finally, while all MLR rebates were
included, CSR payments, as mentioned previously, have yet to be fully reconciled and are not reflected in cost
estimates presented in this report.
For Medicaid costs, the calculated PMPM expenditure was more complex. Medicaid claims were isolated for
those enrollees in the Medicaid comparison groups. Because Arkansas Medicaid incorporates several
supplemental payment strategies to select providers, allocation of these additional payments was necessary
to achieve a true claim-related expenditure. Hospitals in four categories — teaching, public, private, and
critical access — were eligible for supplemental payments up to the Medicare upper payment limit (UPL) for
both inpatient and outpatient services. In addition, critical access hospitals and UAMS were eligible for cost-
based reimbursement for select services. Total non-claims based payments to providers by Medicaid were
obtained annually for 2014 through 2016 and allocated proportionately to providers by service utilization to
achieve a loaded claims PMPM. Administrative costs were identified from DHS expenditure reports. Non-
changing costs (e.g., Disproportionate Share, Graduate Medical Education, facility costs) were not included in
PMPM estimates, as these would not have changed under alternative expansion approaches. For enrollee-
specific costs (e.g., enrollment, case-management, etc.) a per-enrollee estimate was generated from the
existing Medicaid program and applied to the loaded claims.
3. What were the cost-effective aspects of premium assistance?
Under the premise of the waiver authority, the cost of purchasing healthcare insurance through QHPs using
premium assistance was expected to be greater than purchasing care through the traditional Medicaid system
due to the compressed Medicaid rates publicly available (e.g., $850 per diem for hospitalizations). Concurrently,
the commercial care management strategies and differences in provider payments were hypothesized to
contribute to better access, more appropriate healthcare utilization, and better quality and outcomes.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 13
Effectiveness was assessed through access, utilization, quality, and outcome metrics described above. Costs
were assessed through two approaches. First, by direct comparison of experienced costs for newly enrolled
individuals between those in QHPs and those in the Medicaid program provided absolute differences in
program costs. Modeling efforts to estimate the experience of QHP enrollees and project a PMPM had they
been in traditional Medicaid is employed. In addition, PMPMs from newly eligible and enrolled 19- to 64-year-
old Medicaid beneficiaries are calculated.
Second, where plausible, ratios of improvement in care to associated costs are developed (e.g., access
improvements compared to rate differentials). While no single cost-effectiveness ratio is attainable, observed
effect differences can be interpreted with respect to differential costs between the two programs. If
differential effects on access, utilization, quality, and outcomes are observed, program effects will be
expected to lead to measureable health improvements over time. We will test this expectation by presenting
cost and outcome findings at Baseline (Year 1), Year 2, and Year 3 of the program. This will allow policymakers
to evaluate the potential trade-off of increased costs relative to important indicators focusing on access,
quality of care, and adverse event reduction consistent with health improvement.
4. What would the Medicaid program have experienced if a traditional Medicaid expansion had been adopted?
Examination of the hypothetical costs of covering the entire expansion population in Arkansas’s traditional
Medicaid program and the programmatic changes necessary to achieve a similar outcome to that experienced
through premium assistance is a core component of the demonstration evaluation. Consideration must be
given to the existing Medicaid program, its level of network participation, and the impact of existing payment
rates given differences identified through this evaluation. In addition, the price elasticity of the supply of
medical providers and their ability and/or willingness to provide for the healthcare needs of the expansion
population through the existing Medicaid program must be considered. Finally, if payment rate changes were
required to achieve access and quality outcomes, what would be the financial impact of those modifications
across the entire Medicaid program (e.g., rate changes would apply to all Medicaid rates, not only those
associated with PPACA newly eligible adults)? We provide a basis for this rationale and simulate results under
various pricing scenarios within this report.
Hypotheses
To address the theoretical questions on the previous pages, we tested hypotheses that aligned with the original
12 hypotheses outlined in the Section 1115 Demonstration Waiver Terms and Conditions, STC 70, No. 1 (see
Appendix B). Broadly, the original hypotheses fell into four categories:
1. HCIP beneficiaries will have equal or better access to health care compared with what they would have
otherwise had in the Medicaid system over time. Access will be evaluated using measures for geographic,
perceived, and realized access; use of ER services; potentially preventable ER and hospital admissions; and
non-emergency transportation services.
2. HCIP beneficiaries will have equal or better care and outcomes compared with what they would have
otherwise had in the Medicaid system over time. Quality and outcomes will be evaluated using measures of
preventive (primary, secondary, and tertiary) services and healthcare services, preventable medical events,
and health services utilization.
3. HCIP beneficiaries will have better continuity of care compared with what they would have otherwise had in
the Medicaid system over time. A thorough profile of the experience of churn following the universal
eligibility redetermination in July 2015 will be presented.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 14
4. Services provided to HCIP beneficiaries will prove to be cost-effective. Cost-effectiveness will be evaluated
using findings from testing the aforementioned hypotheses in combination with the following cost
determinations from the three programmatic years spanning 2014–2016:
a. For HCIP beneficiaries, fewer gaps in enrollment, improved continuity of care, and the resultant lower
Medicaid administrative costs would be experienced through premium assistance. Anticipated metrics
include cross-year carrier and Medicaid enrollment, cross-year continuity of primary care provider
engagement, and impact of administrative cost allocation to carriers compared to alternative
Medicaid administration.
b. Through HCIP use of premium assistance in the individual commercial marketplace, performance
characteristics of the Marketplace will be enhanced through increased carrier competition,
stabilization of the actuarial risk pool, and limited premium increases over time.
In this final report, we summarize first year program findings and study trends on premium effects over time.
We include enrollment information, carrier participation, market competition, and premium increases over
the three years of the HCIP. We also present a summary of an actuarial profile of the HCIP population in
comparison to other Arkansas enrollees in the individual marketplace.
c. Use of premium assistance in the individual commercial marketplace will prove to be cost-effective for
the program compared with what it would have cost to cover the same population in the Arkansas
Medicaid system.
Simulation of the counterfactual experience (if all of the PPACA expansion had occurred through the Medicaid
program), including the impact on non-PPACA Medicaid programmatic costs, will reflect one of the primary
outcomes of interest for this hypothesis.
Data Sources and Analytic Comparison Groups
For this final report, data were obtained from three primary data sources: Arkansas Medicaid enrollment files
from the DHS Division of County Operations, administrative claims data (Medicaid and QHPs), and two member
enrollment surveys (CAHPS). In order to construct variables of interest, additional data were obtained from the
Arkansas Department of Health (birth and death certificates from Vital Records), the Arkansas Health Data
Initiative, and the Medicaid-administered exceptional healthcare needs Questionnaire. In addition, enrollee and
network provider addresses were geocoded, allowing distances and drive times between enrollees and providers
to be calculated. Details on data processing can be found in Appendix C.
External claims data were assessed for consistency and integrity before being processed by the analytic data
team. Our team established a step-by-step logic flow to execute data exclusions and to create the final analytical
dataset. See Appendix D for a listing of exclusions and a flowchart of the process used to establish a final
analytical dataset which contains four non-overlapping subpopulations where Medicaid and QHP enrollees were
compared within two groups.
To assess the differences between the programmatic effects of commercial premium assistance to Medicaid, we
utilized two available comparison strategies: 1) a matched comparison group based upon the demographics of
Medicaid and QHP enrollees who did not complete the Questionnaire (the “General Population”); and 2) a
comparison between those who took the exceptional healthcare needs Questionnaire and reported higher
healthcare needs in the six months prior to enrollment (the “Screened Population”) and were subsequently
assigned to either Medicaid or QHP enrollment. For the General Population, we use Year 1 as a Baseline year to

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 15
obtain chronic-conditions history from claims data and follow quality and utilization differences across groups in
the second year (those enrolled in the program beginning in 2014 or 2015) and third year (those enrolled in the
program since 2014) of enrollment in the program.
Table 1 summarizes our comparison-group enrollee numbers by year and data source, followed by a description
of the comparison groups. Table 1 in Appendix D (Study Subjects) provides demographic profiles for Baseline/Year
1 for each comparison group by payer.
Table 1. Comparison Group Description and Analytical Data Populations
General Population,
Comparison Group 1
Screened Population,
Comparison Group 2
Year
Data Source
Traditional
Medicaid
(did not complete
the Questionnaire)
QHP
(did not complete the
Questionnaire)
Medicaid
(completed the
Questionnaire and met
the threshold)
QHP
(completed the
Questionnaire but did not
meet the threshold)
Baseline
(Year 1)
Claims
Matching variables from first year including
clinical need obtained
N = 9,037
N = 44,285
Year 2
Claims
N = 27,905
N = 92,940
N = 9,037
N = 44,285
CAHPS II
N = 241
N = 792
N = 985
N = 1,091
Year 3
Claims
N = 13,933
N = 56,874
N = 7,951
N = 37,752
Note: The second CAHPS survey was fielded approximately 18 months after the majority of respondents had enrolled in Medicaid or a
QHP. This was during the second year of insurance coverage in their respective programs. Enrollees in Comparison Group 2 were
oversampled for CAHPS, attributing to the higher number of responses.
Assessing Exceptional Healthcare Needs in Population Completing the Questionnaire (Screener)
A total of 108,690 HCIP enrollees completed a healthcare needs assessment screener. Select individuals who
reported deficits in activities of daily living, severe mental illness, or homelessness, were automatically assigned to
Medicaid and are not included in this evaluation. For the remainder, composite scores were compiled so that
everyone screened had a score on a continuum that ranged between 0.02 (no utilization) and 0.61 (extremely
high utilization). A “threshold” was established at 0.18, based on the assumption that 10 percent of those who
took the Questionnaire would demonstrate a higher need. Individuals with a composite score lower than 0.18 had
the option to choose a QHP or were auto-assigned to a QHP, while those with a composite score of 0.18 or higher
were deemed to have exceptional healthcare needs and were assigned to a Medicaid plan. Because those near
the threshold reported similar experiences in terms of higher utilization, programmatic assignment enables
application of quasi-experimental methods to test for differential program effects.
New Traditional Medicaid Enrollees/New Premium Assistance Commercial Enrollees Balanced on Key
Demographics
The original design to test low-income parents on the traditional Medicaid program (at or below 17 percent FPL)
to low-income parents in the QHPs (more than 17 percent FPL) and replicate quasi-experimental methods similar
to those described previously was not achievable. Fidelity of the income variable and parental status in the DHS
enrollment data violated the assumptions required for this methodological approach. Because of income
discrepancies identified related to eligibility determination, combined with the fact that income is determined at
the point of eligibility determination and varies substantially, the original approach was deemed infeasible.
However, because individuals previously eligible for Medicaid, but newly enrolled, were not screened for exceptional
healthcare needs, and because more than 116,000 of the 2014 newly eligible HCIP enrollees did not take the
screener, comparison of newly enrolled non-screened individuals within the two programs was possible. These

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 16
individuals represent the General Population in each program. They were balanced across programs on demographic
variables and, for those enrolled for at least two years, the first year clinical status was also used. This balancing
provided the ability to compare programmatic effects for the General (i.e., non-screened) Population.
Methodological Approaches
Regression Discontinuity
In evaluations such as this, when random assignment to treatment and control groups is not feasible, comparisons
can be performed by examining subgroups of individuals based on scores just below or above a cut-point value of
a predetermined variable. For the Screened population, this approach offered the opportunity to examine
individuals who took the Questionnaire but were assigned to Medicaid or QHP enrollment based upon their
responses and a predetermined composite-score threshold. The assumption is that individuals with very similar
scores on either side of the cut-point (threshold) should not differ significantly in terms of need, even though the
cut-point assigns the individuals into different groups. Regression discontinuity is a quasi-experimental design that
is increasingly being used in evaluation analyses to test differences attributable to group assignment.
29
,
30
In our evaluation, roughly one-half of the new enrollees to Medicaid and premium assistance plans completed a
healthcare needs assessment screener (described on the previous page). Those with a composite score of less
than 0.18 were assigned to a QHP, while those with a score of 0.18 or higher were assigned to a Medicaid plan. If
the regression line examining the association between composite score and an outcome variable of interest (e.g.,
number of ER visits to treat an emergent condition) passes continuously through the cut-point, we would not
expect to see a program effect. If we were to observe a sharp jump at the composite score cut-point where the
program assignment was made, we would have a strong indication that the jump was due to the program effect
and not attributable to individual demographics or traits. Further details on this methodological approach can be
found in Appendix E.
Propensity Score Matching
Enrollees were not randomly assigned to the traditional Medicaid plan or a QHP. Therefore, propensity scores can
be described as the probability of being assigned to a treatment group (here, our QHP group) given a set of
underlying characteristics (or observed covariates).
31
In our evaluation, for those newly eligible individuals in
either traditional Medicaid or the QHP who were not screened, we calculated the probability of being assigned to
a QHP treatment group (as opposed to the traditional Medicaid control group). This propensity score of
assignment to treatment is calculated based on incorporating age, gender, race/ethnicity, Charlson Comorbidity
Index, insurance region, and census block median income. We utilized first program year individual experience at
Baseline to develop the propensity scores with subsequent observations when individuals were in Years 2 and 3 of
the program. The goal was to balance the groups assigned to traditional Medicaid or a QHP by the underlying
characteristics included in the propensity score models. Using propensity scores in our empirical assessment of
group differences in access, quality, or healthcare outcomes has the potential to reduce biases associated with
imbalanced underlying characteristics across groups. We used a technique called greedy matching to closely
match individuals in Medicaid and QHPs for comparison. Further details on this methodological approach can be
found in Appendix E.
Direct Comparison of Programmatic Costs and Cost-Effectiveness Assessment
As described, while PMPM costs for premium assistance are reflected in the cumulative premiums paid to carriers
when combined with Medicaid payments for wrap-around services, including NEMT, no similar source of PMPM

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 17
costs for Medicaid existed. PMPM costs from both programs were constructed to enable program cost
comparisons. Allocation of non-claims related Medicaid payments (supplemental payments) were allocated and
Medicaid administrative costs associated with new enrollees (i.e., non-fixed costs) were identified and
incorporated as described in Appendix F.
We calculated PMPMs for observed Medicaid and QHP costs. To estimate a “what if QHP enrollees had been
enrolled in FFS Medicaid” scenario, we estimated the QHP experience using Medicaid costs with and without
across-program utilization adjustments. We provide direct program cost comparisons based upon actual
cumulative premiums paid; modeled PMPMs calculated from distribution of observed utilization experience
within the QHPs (inpatient, outpatient, ER, prescriptions filled, etc.); modeled projected PMPMs based upon
observed QHP utilization experience and estimated administrative costs within the QHPs adjusted for Medicaid
payment rates; modeled projected PMPMs based upon modeled QHP enrollee utilization in Medicaid with
Medicaid payment rates; and finally, actual Medicaid PMPM rates for newly eligible Medicaid enrollees.
To support policymakers’ decisions surrounding cost-effectiveness determination, we determined trade-offs for
incremental increases in access associated with identifiable payment increases. Specific provider payment
differentials (e.g., primary care outpatient rates) were determined, and observed differences in associated effects
(e.g., primary care accessibility, inappropriate ER use) facilitated the development of incremental cost-
effectiveness ratios for select indicators.
Counterfactual Medicaid Impact Simulation and Sensitivity Analyses
Examination of the hypothetical costs of covering the entire expansion population in Arkansas’s traditional
Medicaid program and the programmatic changes necessary to achieve a similar outcome to that experienced
through premium assistance is a core component of the demonstration evaluation. The price elasticity of the
supply of medical providers and their ability and/or willingness to provide for healthcare needs of the expansion
population through the existing Medicaid program was the central component of the simulation model.
To model the potential counterfactual Medicaid program impact, we examined the potential programmatic
impact on costs if increases in payment rates had been required to maintain provider access. Individuals whose
care would unlikely be exposed to the impact of rate adjustments were excluded (e.g., individuals 65 and older for
whom Medicare would be the primary payer on most medical services, children less than 1 year old covered on a
different payment rate schedule).
Differences observed for total Medicaid expenditures were calculated at incremental increases and expressed as a
total program cost effect. These were allocated onto enrollment month Medicaid PMPMs calculated previously
for the demonstration population. Summation of the experienced Medicaid PMPMs in our comparison groups
with the additional PMPM load caused by potential rate increases resulted in the generation of counterfactual
PMPMs, based upon underlying alternative rate increase scenarios. Importantly, for this simulation model,
increases in utilization due to increasing rates were not included.
Special Studies: Experience with Health Independence Accounts (2015–2016)
To assess the participation and impact of the Arkansas Health Independence Accounts, we examined individuals
required to participate (e.g., those between 101 and 138 percent FPL) and their respective experiences. Through
identified eligibility files, we categorized individuals into two groups: 1) those who received notification but did
not participate and 2) those who participated with at least one monthly contribution.
Comparisons were made between demographics and claims experiences for those who did and did not
participate. In addition, the frequency and duration of monthly contributions, the total contributions, and the

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 18
avoided cost-sharing received due to participation were characterized. Site of service for protected cost-sharing
was examined. Finally, net and individual cost-avoidance was compared to net and individual contributions and
assessment of exit payments for individuals from Arkansas DHS was also completed.
The First Year Experience
Overview
Arkansas successfully established the Health Care Independence Program (HCIP), commonly referred to as the
“Private Option,” in 2014, as designed under the Terms and Conditions of the Section 1115 demonstration waiver.
Through the end of 2015, the estimated target enrollment population of approximately 250,000 had been met.
Additionally, approximately 25,000 individuals eligible under the PPACA and deemed to have exceptional
healthcare needs were enrolled in the traditional Medicaid program, while approximately 22,000 previously
eligible, but newly enrolled individuals in 2014, had obtained Medicaid coverage.
After the first year, healthcare providers reported both significant clinical and financial effects. Federally qualified
community health centers (FQHCs) reported increased success in attaining needed specialty referrals for their
clients.
21
The Arkansas Hospital Association (AHA) reported annualized reductions in uninsured outpatient visits,
emergency department visits, and admissions — by 45.7 percent, 38.8 percent, and 48.7 percent, respectively.
22
The state’s teaching hospital reported a reduction in uninsured admissions from 16 percent to 3 percent,
attributable to HCIP.
23
The influence on the risk profile and competitiveness of the individual marketplace was substantive. Representing
84 percent of the covered lives within the individual health insurance marketplace, Medicaid’s premium
assistance lowered the average age of the risk pool(s) by approximately 10 years. The resulting more-favorable
risk within the Marketplace enabled stable premium prices not only in the first year, but across the first three
years of the HCIP. Competitiveness and consumer choice in the Marketplace increased across the seven market
regions in the state. In 2014, three regions had access to only Arkansas Blue Cross and Blue Shield and Blue Cross
Blue Shield Multi-State plans. By 2016, five carriers were offering coverage across all seven market regions, with
one market region having six carriers (the sixth restricted to a single market by Medicaid’s purchasing guidance
limiting premium assistance to those plans within 10 percent of the second lowest-cost silver plan within the
market region).
For 2014, the estimated budget neutrality cap (BNC) was exceeded during the initial enrollment phase of the
program. Enrollment of younger individuals over time affecting net premiums, the rebate of medical-loss ratio
(MLR) payments by one carrier not meeting the MLR requirements in 2014, and inflationary expectations built
into the BNC estimates brought cumulative program costs within the 2015 limit of $500.08 per member per
month (PMPM) and well under the 2016 limit of $523.58 PMPM. Importantly, the first year evaluation allowed
examination of BNC estimates compared to real experience.
Effect Comparison — Access
A key component in this evaluation is the comparison of QHP beneficiary experiences to similar cohorts of new
beneficiaries who were enrolled in traditional Medicaid. We employed two strategies: 1) a comparison of
individuals from a general population of new QHP enrollees or Medicaid (the General Population); and 2) a quasi-
experimental approach to individuals who had reported higher previous healthcare utilization and were assigned
to either QHPs or Medicaid (the Screened population). In general, findings observed in the two comparison

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 19
populations were consistent in direction, with the Screened population producing larger differences between
Medicaid and QHP enrollee experiences.
A key component of the demonstration was the degree to which Medicaid and QHP enrollees had access to
providers within their respective networks. Access was framed from three perspectives: 1) the geographic
presence of providers available to enrollees, 2) the experience of enrollees in attaining access at times of need,
and 3) variations in utilization observed between programs.
The location of providers in both the Medicaid and QHP network participation revealed high degrees of
geographic access and minimal variation between programs. Both Medicaid and commercial enrollees’ networks
contained providers who met network adequacy requirements (e.g., 30 minutes from a PCP, 60 minutes from a
specialist). More than 98 percent of enrollees in both Medicaid and QHPs had access to a PCP within a 30-minute
drive time. For specialists within the General Population comparison group, both programs achieved high levels of
geographic access, represented by more than 95 percent of enrollees having no more than a 60-minute drive time
from the enrollee’s home.
Two unexplained statistically significant access differences were observed with QHP enrollees having slightly
higher orthopedic access (98.3 percent of QHP versus 93.7 percent Medicaid enrollees within 60 minutes) and
Medicaid enrollees having slightly more oncological access (99.1 percent of Medicaid versus 95.0 percent of QHP
enrollees within 60 minutes). No meaningful differences were assigned to these statistical findings.
Geographic access assessments represent the Medicaid participating providers compared to commercial
participating providers for all carriers. Because of Arkansas’s “any willing provider” law,
10
requiring insurers to
allow any provider willing to accept terms for the class of providers into their networks, assessment across all
carriers was deemed appropriate.
By contrast, from the perspective of the beneficiary at times of need, significant differences were observed in
being able to access providers within the networks. Consistently across both the General Population and Screened
Population, enrollees reported improved access within QHPs. Responding to whether it was “always easy to get
care, tests, and treatment needed,” 64.5 percent of General Population QHP enrollees responded affirmatively
compared to 45.9 percent enrolled in Medicaid (a 40.5 percent relative difference). For individuals who
completed the screener, 57.9 percent of QHP enrollees compared to 48.4 percent of Medicaid enrollees
responded affirmatively (a 19.6 percent relative difference). With respect to getting “an appointment for a check-
up or routine care as soon as needed,” enrollees in QHPs reported more accessibility with a 12.1 percent relative
difference in the General Population. Improved accessibility was suggested for ease of appointment availability
for the General Population, with no differences observed for the Screened population.
Because this was the initiation year of the program and many of the newly enrolled lacked prior insurance
coverage, we examined the time to first outpatient visit in the General Population for Medicaid and QHP enrollees
and found significant differences. Within 30 days of enrollment, 21.2 percent of QHP enrollees had accessed an
outpatient visit compared to 8.2 percent of traditional Medicaid enrollees. By 90 days of enrollment, 41.8 percent
of QHP enrollees had accessed an outpatient visit compared to 29.6 percent of Medicaid enrollees. These
differences are dramatic and consistent with the perceived accessibility reported above from enrollees.
Finally, comparing utilization patterns for ER use and hospitalizations, the impact of access differences reported
previously are consistently observed for both the General Population and Screened Population. Examining the
rate of total ER visits per 12 months of enrollment, Medicaid enrollees experienced a 13.2 percent higher ER-visit
rate in the General Population and a 50.8 percent higher rate in the Screened Population.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 20
Differentiating between emergent and non-emergent ER visits by a modified NYU algorithm,
32
,
33
programmatic
differences were observed. QHP enrollees were much more likely to utilize ER services for emergent care — 122.1
percent for the General Population and 51.9 percent for the Screened Population. Conversely, non-emergent ER
services were much more likely to be utilized by the Medicaid enrollees — 58.1 percent higher for the General
Population and 63.6 percent higher for the Screened Population. These findings were highly statistically significant
across all ER comparisons. With respect to hospitalizations, the Screened Population demonstrated a 43.2 percent
higher hospitalization rate in the Medicaid program than in the QHP program, with no differences observed in the
General Population.
Considering network participation, self-reported perceived access, and patterns of utilization, a profile of the
differences between Medicaid and QHP program performance emerged. Enrollees were geographically located
near providers who have enrolled as a provider in Medicaid or contracted with a QHP to provide services.
Geographic access, however, does not equate to beneficiary accessibility. Published studies inclusive of Arkansas
providers during the time period reflected in this evaluation have found significant differences across multiple
states, and specifically Arkansas providers, in their acceptance of new patients privately covered by commercial
insurance compared to those with Medicaid coverage. In a 2013 study, Rhodes and colleagues estimated that
rates for new patient availability of appointments for commercial and Medicaid insurance scenarios in Arkansas
were 88.1 percent and 48.7 percent, respectively.
34
Survey information from this study indicated that fewer
practices were accepting patients with Medicaid coverage when compared with private payer sources. This
finding, combined with responses from practices indicating that their Medicaid patient population comprises less
than 10 percent of all patients, suggests that practices were likely limiting the number of patients with Medicaid
as the primary payer, particularly given that the Medicaid population comprises 26 percent of the state’s
population.
35
Combined with the time to first outpatient visit and non-emergent ER use rates, all of our findings
suggest individuals in the Medicaid program experience more difficulty accessing care when needed and
subsequently seek care in settings that are less likely to either address unmet needs or successfully establish
clinician-patient relationships to manage chronic conditions.
Effect Comparison — Care and Outcomes
Examination of quality indicators was undertaken in the first year to assess variations in healthcare quality or
outcomes. With a high proportion of the evaluation study population likely not having prior health insurance and
due to the time frame (first 12 months of coverage), assessments focused on the proportion of enrollees who
received appropriate clinical preventive screenings, the proportion of enrollees who received prophylaxis to
prevent influenza, and the proportion of individuals with diabetes who received appropriate management
screenings with an HbA1c and/or LDL-c screening test. Evaluation of a more robust set of quality indicators is
anticipated as person-time accumulates, which enables longer observation periods.
For receipt of preventive screenings, metrics were operationalized, both to compare between enrollee groups if
any clinical preventive screening was obtained and to compare if all recommended clinical preventive screenings
were obtained. In the first year, eligible screenings included the following: breast cancer, cervical cancer,
colorectal cancer, and cholesterol screenings. Across both comparison populations, enrollees in QHPs achieved
higher screening rates than their Medicaid counterparts. For any recommended screening event, the difference
was 29.6 percent to 25.8 percent in the General Population (a relative difference of 14.7 percent) and 66.0
percent to 41.2 percent (a relative difference of 60.2 percent) in the Screened Population. Although still
statistically significant, for those receiving all recommended screening events, the variation was less pronounced
with 16.8 percent versus 15.8 percent in the General Population and 23.2 percent versus 20.3 percent in the
Screened Population for QHP and Medicaid enrollees, respectively.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 21
With respect to receiving infection prevention through influenza prophylaxis (flu shot or spray), observed
differences in the Screened Population again favored enrollees in QHPs over those in Medicaid. A flu shot or nasal
spray was reported by 45.9 percent of enrollees in a QHP versus 38.5 percent in Medicaid (a 19.2 percent relative
difference). While directionally consistent, no statistically significant finding was present in the General
Population comparison.
Of importance, receiving a tertiary screening for HbA1c was more common among QHP enrollees than those
enrolled in Medicaid. In the General Population, QHP enrollees with diabetes received HbA1c assessments 79.1
percent of the time compared to 73.0 percent of the time for Medicaid enrollees with diabetes (an 8.4 percent
relative difference). Equally, in the Screened Population, QHP enrollees with diabetes received HbA1c
assessments 84.8 percent of the time compared to 80.4 percent of the time for Medicaid enrollees (a 5.5 percent
relative difference). No differences were observed for LDL-c screenings.
Ancillary findings reflecting the first year experience of individuals in both comparison groups included
assessments of experience with transportation needs and examination for longer-term health outcomes.
Significant findings were observed from reported transportation needs for individuals in the Screened Population.
QHP enrollees reported no transportation barriers to a personal doctor visit 89.4 percent of the time compared
with 80.4 percent of the time for Medicaid enrollees (an 11.2 percent relative difference). Transportation barriers
and access to specialty visits were not significantly different in the General Population. Preventable
hospitalizations, readmissions, and age-adjusted mortality showed no variation, likely due to this being the first
year of enrollee experiences.
In summarizing and interpreting care and outcomes, it appears that through more accessible and potentially
earlier engagement, the QHP enrollees experienced improved primary prevention (flu prophylaxis) and secondary
prevention (clinical screenings) compared with their Medicaid-enrollee counterparts.
First Year Program Observations
Differences between the costs of QHP enrollees and those managed through the Medicaid system were expected.
Exploration and characterization of cost differences were required to better understand their association with
effect differences in access, utilization, quality, and the outcomes described. Differences in payment rates and
utilization were also anticipated between Medicaid and the QHP carriers. Variations between QHP carriers are
also expected, but for the purpose of this evaluation, weighted averages of their experiences are utilized for the
commercial comparison.
From effect differences that were observed for comparable groups, overall program differences were suggested
and indeed observed. Examination of utilization rates for Medicaid and QHP enrollees with a minimum of six
months of coverage reinforced these findings.
Medicaid enrollees experienced fewer outpatient events and a concurrent higher rate of ER visits and
hospitalizations. Importantly, enrollees within QHPs received twice as many prescriptions than their Medicaid
counterparts. Because Medicaid utilizes different payment mechanisms and provider codes for select services
compared to their QHP counterparts, direct comparison of all services was not feasible. Volume and type of
service utilization have the potential to impact program costs and will be monitored over time to assess
convergence or divergence in experience.
While volume and type of service utilization is important, variation in payment rates and their potential impact on
access, care, and outcomes was a central component of the demonstration waiver justification. We examined
direct comparisons of payment differentials between that paid by Medicaid and by QHPs.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 22
Dramatic differences in payment rates were observed with commercial rates consistently exceeding those in the
Medicaid program. Physician rates for outpatient services were 90 percent higher when the enrollee was in a
QHP, as compared to their Medicaid counterparts. Primary care physicians had 90 percent higher payment rates
under commercial contracts than with the Medicaid payment schedule. Specialist payment differentials ranged
from 90 percent for obstetricians/gynecologists to 165 percent for ophthalmologists.
Higher payment rates for hospital services, as well as ER events, were also observed. For inpatient hospital stays,
average commercial payments were $11,894 per discharge compared to Medicaid payments (with supplemental
additions) of $7,778 — a 52.9 percent difference. For ER non-hospitalized visits, average commercial payments
were $598 per visit compared to Medicaid payments of $196 — a 205.1 percent difference.
Total program cost differences between that of the HCIP enrollees in QHPs and those managed through the
Medicaid system were expected. The cumulative weighted average premium that was paid during 2014 for
commercial premium assistance was $485.05 PMPM. For Medicaid expenditures inclusive of supplemental
payments and beneficiary-related administrative expenses, the observed Medicaid expenditures were $272.01
PMPM. This $213.04 PMPM difference represents a 78.3 percent difference between the commercial and
Medicaid PMPM. This difference largely reflects the variation in provider payments described, modified by
secondary variations in utilization. This is reflected in the modeling of Medicaid estimates based upon payment
rate differences alone ($244.96 PMPM) and in combination with utilization differences ($252.73 PMPM), resulting
in estimates within 9.9 percent and 7.1 percent of the observed, respectively.
The Counterfactual — Simulation of Traditional Medicaid Expansion in Arkansas
Examination of the hypothetical costs of covering the entire expansion population in Arkansas’s traditional
Medicaid program and the necessary programmatic changes necessary to achieve a similar effect outcome to that
experienced through premium assistance is a core component of the demonstration evaluation. Consideration
was given to the existing Medicaid program, its level of network participation, and impact of existing payment
rates given effect changes identified through this evaluation. In addition, the price elasticity of the supply of
medical providers and their ability and/or willingness to provide for healthcare needs of the expansion population
through the existing Medicaid program must be considered. Finally, if payment rate changes were required to
achieve access and quality outcomes, what would be the financial impact of those modifications across the entire
Medicaid program (e.g., rate changes would apply to all Medicaid rates and not only those associated with the
PPACA newly eligible)?
As previously described, Arkansas had one of the lowest Medicaid eligibility thresholds for non-disabled adults in the
United States (below 17 percent FPL for parent/caretakers only). This meant that the majority of the covered lives in
Medicaid were children, low-income Medicare beneficiaries receiving long-term services (not medical), Social
Security Income (SSI) disabled adults, and pregnant women and those with family-planning services with limited
benefit coverage. In 2013, prior to the PPACA expansion, Arkansas Medicaid covered 24,955 non-disabled adults with a
full benefit package. In 2014, following PPACA expansion, an additional 267,482 individuals were covered —
approximately 17,300 (6.5 percent) previously eligible but newly enrolled; approximately 25,000 (9.3 percent) PPACA
eligible but with exceptional healthcare needs; and 225,000 (84.2 percent) PPACA eligible with premiums purchased
on the individual marketplace. Thus, in 2014, Arkansas Medicaid expanded their non-disabled 19- to 64-year-old
population tenfold with 84 percent managed externally in the commercial marketplace. Effect comparisons
represented above draw on the experience of those newly eligible in either the Medicaid FFS or commercial
premium assistance programs during 2014.
Infusion of an additional 297,000 non-disabled 19- to 64-year-olds into the Medicaid system would likely have
resulted in widespread effects to the system. Traditional microeconomics suggests that increased demand

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 23
through the Medicaid program would place increasing price pressure on the rate structure of the existing
Medicaid program.
A recent study of appointment availability for Medicaid beneficiaries, inclusive of those in Arkansas, suggests that
increased Medicaid payments result in improved appointment availability.
36
In this 10-state study, an increase in
availability of primary care appointments of 1.3 percent was observed for each 10 percent increase in Medicaid
reimbursements. These findings are consistent with our first year findings internal to this evaluation, both for
ease of access for receiving needed care and for access with differential ease of receiving needed care, as well as
ease of appointment for routine care. Between Medicaid and QHP enrollees in the General Population, we
observed a 40.5 percent relative difference and for the Screened Population a 19.6 percent relative difference for
ease of access. Similarly, for ease in ability to get an appointment within the general population a 1.4 percent
difference was associated with a 10 percent increase in Medicaid reimbursements. Thus, theoretical, peer-
reviewed, and internal findings suggest upward price pressure on existing Medicaid payment rates in the
counterfactual that would be required to achieve comparable access and potential comparable outcomes to those
experienced in the commercial sector.
The observed differences in payment rates between Medicaid and QHPs described previously would plausibly
lead to increased access differences for Medicaid beneficiaries. As required by federal rule, it would be unlikely
that Arkansas could meet the equal access provision requiring state Medicaid provider payments to be
“consistent with efficiency, economy, and quality of care and ... sufficient to enlist enough providers so that care
and services are available under the plan at least to the extent that such care and services are available to the
general population in the geographic area.”
12
Importantly, any potential increase in Medicaid payment rates
would necessarily affect not only services for the new expansion population, but also services for beneficiaries
under the same payment rate schedule across the entire Medicaid program.
The simulated incremental effects of inflationary increases and the associated cost impacts were plausible. The
three increasingly conservative scenarios provide policymakers with conditions under which necessary increases
to achieve equitable access can be considered. They include: 1) claims associated with potentially wage-sensitive
services; 2) claims restricted only to those associated with major medical services; and 3) claims restricted to only
those associated with physician-billed services.
The base scenario utilized 2014 actual premiums paid for commercial coverage and observed Medicaid costs for
Medicaid coverage. Under the wage-sensitive scenario, the Medicaid program would achieve budget neutrality if
the Medicaid program experienced a 14.5 percent increase in costs. Under the major medical scenario, the
Medicaid program would achieve budget neutrality at a 24.7 percent increase in clinical-claims cost. Lastly,
restricting to a physician-only scenario, budget neutrality would be achieved at a 34.9 percent increase in
physician-claims costs. In actuality, the market would likely require payment modifications much more complex
than these scenarios. However, these scenarios provide policymakers with a comparison of budget neutrality
estimates based upon actual expenditures.
First year results should be viewed with caution for several reasons. First, cost-sharing reduction reconciliation
with carriers for 2014 had not been executed, and have still not been concluded. In addition, 2014 represented
the initiation phase of the program with significant transitions as reflected in enrollment growth. Future
assessments during steady state periods may provide more accurate reflections of both programmatic effects and
associated costs.
The subsequent sections in this report update findings over the second and third years of the HCIP that include a
period of programmatic steady state in 2016.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 24
Year 2 and Year 3 Waiver Impact Findings
Introduction to Analyses
Overview
While all individuals described in this section of the report are Medicaid-eligible individuals, the following groups
of individuals are categorized for the purposes of our findings:
i. Medicaid enrollees: Patient Protection and Affordable Care Act (PPACA) Medicaid expansion eligible
individuals with exceptional healthcare needs who are enrolled in the state’s fee-for-service Medicaid
program and are not a part of the Health Care Independence Program (HCIP) Section 1115 demonstration
waiver; and
ii. Qualified Health Plan (QHP) enrollees: PPACA Medicaid expansion eligible individuals who are enrolled in
QHPs through premium assistance and are a part of the HCIP Section 1115 demonstration waiver.
Provider Networks
Only providers who practiced within calendar year 2014 were included in these analyses. Medicaid and
commercial QHP enrollees and provider data (i.e., Blue Cross Blue Shield, Ambetter, and QualChoice) were used
to assess network adequacy and perform geographical information system (GIS) mapping. For the analysis,
“access” was defined as the distance (30 or 60 miles) or time of travel (30 or 60 minutes by passenger
automobile) from any enrollee’s location to the nearest provider, within an “access ring” offering any of the
eight categories of healthcare provider types (primary care, orthopedics, ophthalmology, OB/GYN, oncology,
surgical, psychology, and cardiology) under study. These “access rings” were created by computing a total of
four distinct travel distances and time-of-travel attributes from each unique provider location (latitude and
longitude coordinates) for each provider type. From each provider location a set of four miles traveled along
the existing (Environmental Systems Research Institute [ESRI], 2013) street centerline networks were computed
as “ringed-polygons” at the following distance rings: 0-15, 15-30, 30-45, and 45-60 miles. The percentage of
enrollees within a 30-minute travel time to an in-network primary care physician and a 60-minute travel time to
a specialist are compiled. A detailed description of the geospatial analysis is contained in Appendix G. Medicaid
in-network geographic access is compared to QHP in-network access where the three individual commercial
carriers have been aggregated.
Comparison Populations and Comparison Groups
Two comparison populations are available within the analytic framework. The first population compares traditional
Medicaid enrollees — who did not complete the exceptional healthcare needs Questionnaire — with QHP enrollees
who chose not to complete, or simply bypassed the Questionnaire upon applying to Medicaid. As previously stated,
enrollees in these insurance program groups are reflective of the General Population. For this comparison
population, we used enrollee first year program experience as a Baseline to ascertain a clinical needs background
(using the Charlson Comorbidity Index) and created individual propensity scores depicting the probability of being
assigned to a QHP given a set of demographic, clinical needs, and geographic covariates. Medicaid and QHP
enrollees with the same (or very similar) propensity scores were matched and differences in access, quality of care,
utilization, and other health outcomes across these matched pairs were empirically tested. For this population, the
first year program experience and comparison is contained in the Interim Report,
5
and this final report contains
Medicaid and QHP comparison group differences for coverage in Year 2 and Year 3 of enrollment.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 25
The second analytic population includes individuals who completed the Questionnaire. Those who were deemed
to have exceptional healthcare needs by virtue of attaining a composite score threshold cut-point were assigned
to Medicaid. All others completing the Questionnaire who did not attain the threshold were enrolled in a QHP.
Using a regression discontinuity approach, conclusions about differences between Medicaid and QHP enrollees in
this population were made within a model-derived optimal bandwidth around the threshold cut-point. Enrollees
with composite scores close together but on opposite sides of the cut-point, and thus assigned to different
coverage programs, are the focus of this comparison. Therefore, the comparison is reflective of a population who
completed the Questionnaire, and had at least a measure (close to and around the cut-point) of exceptional
healthcare needs. We called this a Higher Needs Population. For this population, the first year program
experience is a Baseline year and we present Medicaid and QHP comparison group differences for coverage in the
Baseline, and Years 2 and 3 of enrollment. The local average treatment effect (LATE) presented in the regression
discontinuity result tables represents the treatment effect at the discontinuity cut-point that was used to assign
enrollees to Medicaid or QHP programs.
In these analyses, there are two populations containing two comparison groups. Each of the four groups are
mutually exclusive and, in total, represent our complete analytical population (see Appendix D for inclusion and
exclusion criteria for each population over the three program years, 2014-2016).
For a more comprehensive description of the statistical designs used to determine the differences across
comparison groups in the two populations, as well as the technical details, please see the Methodological
Approaches section and Appendix E.
Analytic Approach to Access
For both comparison populations, access differences between the Medicaid and QHP programs were evaluated
using measures for geographic, perceived, and realized access. Other measures influenced by lack of primary care
physician access, including non-urgent emergency room utilization and potentially preventable hospital
admissions, are analyzed. Contributory factors to obtaining primary care physician appointments, and being able
to get to them when scheduled, are provider reimbursement rates and non-emergency transportation.
Differences in Medicaid and QHP reimbursement rates for office or other outpatient services by various provider
types and self-reported differences in the difficulty obtaining non-emergency transportation are highlighted in
this report.
Provider and enrollee populations did not incur any systematic changes in the second and third year of HCIP and,
thus, we present geographic access analyses compiled and presented in the Interim Report.
5
For the General
Population, this analysis was performed using a stabilized inverse probability of treatment weighting approach
and, for the Higher Needs Population, a regression discontinuity design was applied (see the description in
Appendix E).
For perceived access, there are new findings to present from responses to the second CAHPS survey (CAHPS II)
that was fielded in fall 2016. This survey elicited a perceived access perspective from individuals who were
continuously enrolled in Medicaid or a QHP for a period of approximately 18 months. In the Interim Report,
perceived access was framed based on an interpretation of access at program enrollment or shortly thereafter.
The interpretation in this report will shed light on whether perceived access differences persist after being in a
health insurance program for at least a year — when realized access of first contact with a provider should have
taken place and a familiar provider-patient relationship should have been established.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 26
Analytic Approach to Clinical Preventive Measures Outcomes
In the Interim Report, a series of clinical outcome differences was presented based on primary, secondary, and
tertiary screenings, as well as disease management outcomes that could be effectively measured within one year
of healthcare coverage. For this three-year synopsis of the HCIP program, we again report on these annual
screenings and disease management indicators. The three-year coverage period also allows us to compile
indicators that require more time to measure, such as cancer-screening indicators (i.e., breast, cervical, and
colorectal). A full list, descriptions, and operationalization of indicators included in these analyses can be found in
Appendix H.
Analytic Approach to Healthcare Services and Utilization Outcomes
We tested for differences in healthcare services outcomes (procedures) provided to Medicaid and QHP enrollees.
Not having a needed procedure performed could be an indication of poor quality of care, but at the same time, an
over-supply of unnecessary procedures could also be indicative of poor quality of care.
Based on age- and gender-appropriate inclusion, we present a series of healthcare services outcome rates across
Medicaid and QHP enrollee populations for abdominal hysterectomy, vaginal hysterectomy, cardiac
catheterization, percutaneous coronary intervention (PCI), coronary artery bypass graft, back surgery, open
cholecystectomy, laparoscopic cholecystectomy, prostatectomy, total hip replacement, total knee replacement,
carotid endarterectomy, lumpectomy, unilateral mastectomy, and bilateral mastectomy.
Quality utilization outcomes include not having preventable hospitalizations and non-emergent emergency room
visits. For those who do have hospitalizations, not having to be readmitted following discharge is another
indicator of quality healthcare delivery. We use an algorithm compiled by the Agency for Healthcare Quality and
Research to identify preventable hospitalizations and the modified New York University algorithm to identify non-
emergent emergency room visits.
37
,
38
Special Population and Topic Studies
In this section, we complement the access, clinical preventive measures outcomes, and healthcare services and
utilization program comparisons by studying areas of healthcare delivery where programs may differ in the
provision of quality health care.
The first special population under study was made up of pregnant women and looked at the care delivered in
each program. Women are not enrolled in a QHP if they are pregnant upon application — they are covered by the
traditional fee-for-service Medicaid. If they are diagnosed or become pregnant while enrolled in a QHP they
receive their perinatal care covered by the QHP. From 2014 onward, we have a reasonable population in which to
compare pregnancy and birth outcomes for Medicaid- and QHP-covered women.
In a low-income population, non-emergency transportation is an important factor contributing to gaining access
to the healthcare system. Using responses from the second CAHPS survey we present findings from a comparison
analyses of non-emergency transportation access.
Children who had been identified with chronic and persistent conditions through early and periodic screening,
diagnostic, and treatment benefits while in Medicaid were eligible for HCIP enrollment and a more
comprehensive set of healthcare benefits. In this study, we identify how many adolescents would have been
eligible to take advantage of HCIP enrollment and what level of care they received if they were enrolled in a QHP.
The availability and continuity of healthcare coverage is an important cornerstone to optimal health. Churn — or
gaps in healthcare coverage — has been demonstrated to have negative consequences on individual health,

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 27
especially for those with chronic conditions. We studied patterns of continuous enrollment, attrition, and churn
among those who enrolled in HCIP across various periods of the program.
Health Independence Accounts were introduced to the HCIP population, who were earning 101 to 138 percent of
the federal poverty level (FPL) in January 2015. A type of health savings account, the goal was to encourage
enrollees to pre-pay a small premium for next-month coinsurance protection. This study summarizes the buy-in,
impact, and overall effectiveness of the Healthcare Independence Account experience.
Utilization of urgent care clinics continues to increase in Arkansas. In this section, we test to see if emergency
room utilization has been substituted by urgent clinic care utilization to help explain changes in number and rates
of visits.
Given the high rates of opioid use observed in Arkansas statewide and the well documented risks associated with
high dose and long-term opioid use, we compared the rates of opioid analgesic use, high risk opioid use (high dose
opioid use or opioid use with a benzodiazepine), initial opioid use with >7 and >3 days supplied, and the extent of
naloxone use for those prescribed opioids between newly enrolled persons obtaining coverage in traditional
Medicaid and QHPs from 2014-16.
Finally, we present mortality comparison between Medicaid and QHP enrollee groups in both the General and
Higher Needs Populations.
Cost Comparison and Budget Impact Analyses
To determine what cost differentials were present to treat similar patients in Medicaid and QHPs, we identified
per member per month costs associated with the care provided to Medicaid and QHP enrollees. Using a budget
impact analysis simulation model, we used these estimates to present cost-enhancing scenarios to the
Medicaid reimbursement structure to identify how much Medicaid could have increased costs to stay within
HCIP budget neutrality. The goal was to increase Medicaid reimbursement to induce provider engagement to
accept more patients, and in a timelier manner, in order to improve access to care under a counterfactual
scenario that asked, in essence, “What would have happened if adult Medicaid expansion had proceeded in a
standard manner in Arkansas?”
Geographic and Realized Access Differences and Provider Reimbursement
Comparison between Medicaid and QHP Programs
Network Participation (Geographic Access)
Tables 2 and 3 contain findings from a geospatial analysis identifying the proportion of 2014 Medicaid and QHP
General and Higher Needs Population enrollees, respectively, who resided within a 30-minute drive to an in-
network primary care physician (PCP) or within a 60-minute drive to each of seven in-network specialists under
the study.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 28
Table 2. Differences in General Population Geographic Access to Health Care between Medicaid and
QHP Enrollees
Geographic Access Indicators
Comparison
Medicaid
QHP
Relative
Difference
(percent
3
)
Statistical
Difference
(p-value
4
)
Proportion of enrollees within 30 minutes
of a primary care physician
(source: GIS)
Crude (n, proportion)
9,604 (0.993)
61,918
(0.986)
1
Adjusted (LSM, StdErr)
0.994 (0.001)
0.986 (0.003)
- 0.8%
0.494
Proportion of enrollees within 60 minutes
of a cardiologist
(source: GIS)
Crude (n, proportion)
9,604 (0.994)
61,918
(0.977)
1
Adjusted (LSM, StdErr)
0.995 (0.001)
0.977 (0.001)
- 1.8%
0.116
Proportion of enrollees within 60 minutes
of an obstetrician/gynecologist
(source: GIS)
Crude (n, proportion)
6,541 (0.993)
34,852
(0.990)
1
Adjusted (LSM, StdErr)
0.994 (0.001)
0.990 (0.001)
- 0.4%
0.743
Proportion of enrollees within 60 minutes
of a psychiatrist
(source: GIS)
Crude (n, proportion)
9,604 (0.994)
61,918
(0.995)
1
Adjusted (LSM, StdErr)
0.995 (0.001)
0.995 (0.000)
0.0%
0.968
Proportion of enrollees within 60 minutes
of an orthopedist
(source: GIS)
Crude (n, proportion)
9,604 (0.937)
61,918
(0.983)
1
Adjusted (LSM, StdErr)
0.937 (0.003)
0.983 (0.001)
4.9%
<0.001
Proportion of enrollees within 60 minutes
of an ophthalmologist
(source: GIS)
Crude (n, proportion)
9,604 (0.993)
61,918
(0.979)
1
Adjusted (LSM, StdErr)
0.995 (0.001)
0.978 (0.001)
- 1.7%
0.140
Proportion of enrollees within 60 minutes
of an oncologist
(source: GIS)
Crude (n, proportion)
9,604 (0.990)
61,918
(0.950)
1
Adjusted (LSM, StdErr)
0.991 (0.001)
0.950 (0.009)
- 4.1%
<0.001
Proportion of enrollees within 60 minutes
of a general surgeon
(source: GIS)
Crude (n, proportion)
9,604 (0.994)
61,918
(0.995)
1
Adjusted (LSM, StdErr)
0.995 (0.001)
0.995 (0.000)
0.0%
0.984
Notes: Analysis derived from geospatial database containing travel time between patients and physicians. Relative percentage
calculated as (QHP – Medicaid)/Medicaid x 100. Due to lack of geographic access being a rare event, p-values for differences were
obtained using a Poisson regression.
Abbreviations: n=number of persons; StdErr=standard error of estimated mean.
Results contained in Table 2 assessing network adequacy through geographic proximity of providers reveal
minimal differences between providers accepting Medicaid enrollees and those participating in the
commercial QHP networks. There was no difference in the proportion of Medicaid and QHP enrollees in the
General Population within 30 minutes of a primary care physician and the proportion of enrollees within 60
minutes of most specialists. Minor, but statistically significant differences, were observed for orthopedists
and for oncologists. A higher proportion of QHP enrollees have access to orthopedists when compared to
Medicaid enrollees, with a relative difference of 4.9 percent. Conversely, a higher proportion of Medicaid
enrollees have access to oncologists when compared to QHP enrollees, with a difference of 4.1 percent.
Except for these minor differences, both the commercial and Medicaid networks met the geographic access
standards of AID.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 29
Table 3. Differences in Higher Needs Population Geographic Access to Health Care between Medicaid
and QHP Enrollees
Geographic Access Indicators
Comparison
Medicaid
QHP
Relative
Difference
(percent)
Statistical
Difference
(p-value
4
)
Proportion of enrollees within 30 minutes
of a primary care physician
(source: GIS)
Crude (n, proportion)
4,487 (0.996)
25,023
(0.976)
1
Adjusted (LSM, StdErr)
0.998 (0.001)
0.971 (0.007)
- 2.7%
0.578
Proportion of enrollees within 60 minutes
of a cardiologist
(source: GIS)
Crude (n, proportion)
4,489 (0.996)
24,214
(0.944)
1
Adjusted (LSM, StdErr)
0.997 (0.002)
0.953 (0.009)
- 4.4%
0.100
Proportion of enrollees within 60 minutes
of an obstetrician/gynecologist
(source: GIS)
Crude (n, proportion)
4,491 (0.997)
24,947
(0.973)
1
Adjusted (LSM, StdErr)
0.998 (0.001)
0.976 (0.003)
- 2.2%
0.466
Proportion of enrollees within 60 minutes
of a psychiatrist
(source: GIS)
Crude (n, proportion)
4,491 (0.997)
25,365
(0.989)
1
Adjusted (LSM, StdErr)
0.999 (0.001)
0.984 (0.006)
- 1.5%
0.771
Proportion of enrollees within 60 minutes
of an orthopedist
(source: GIS)
Crude (n, proportion)
3,886 (0.863)
24,778
(0.966)
1
Adjusted (LSM, StdErr)
0.867 (0.007)
0.965 (0.002)
11.3%
0.001
Proportion of enrollees within 60 minutes
of an ophthalmologist
(source: GIS)
Crude (n, proportion)
4,487 (0.996)
24,449
(0.953)
1
Adjusted (LSM, StdErr)
0.997 (0.001)
0.954 (0.004)
- 4.3%
0.147
Proportion of enrollees within 60 minutes
of an oncologist
(source: GIS)
Crude (n, proportion)
4,453 (0.989)
22,999
(0.897)
1
Adjusted (LSM, StdErr)
0.989 (0.002)
0.888 (0.006)
- 10.2%
0.001
Proportion of enrollees within 60 minutes
of a general surgeon
(source: GIS)
Crude (n, proportion)
4,491 (0.997)
25,415
(0.991)
1
Adjusted (LSM, StdErr)
0.998 (0.001)
0.993 (0.001)
- 0.5%
0.872
Notes: Analysis derived from geospatial database containing travel time between patients and physicians. Relative percentage
calculated as (QHP – Medicaid)/Medicaid x 100. Due to lack of geographic access being a rare event, p-values for differences were
obtained using a Poisson regression.
Abbreviations: n=number of persons; StdErr=standard error of estimated mean.
Geographic access differences for the Higher Needs Population are the same as what were identified within
the General Population. Notably, a higher proportion of QHP enrollees have access to orthopedists compared
to Medicaid enrollees, with a relative difference of 11.3 percent. Conversely, a higher proportion of Medicaid
enrollees have access to oncologists compared to commercial QHP enrollees, with a relative difference of
10.2 percent.
Provider Payment Differentials
Table 4 presents a summary of weighted average prices paid to different provider types in 2014, 2015, and
2016. The formal description of the aggregation and estimation of weighted average price is contained in
Appendix H.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 30
Table 4. Medicaid and Commercial Payer Price Differences for Outpatient Procedures by Provider Type
2014
2015
2016
Weighted
Average Price
Weighted
Average Price
Weighted
Average Price
Provider Type
MCD
QHP
Absolute
(Relative)
Diff
MCD
QHP
Absolute
(Relative)
Diff
MCD
QHP
Absolute
(Relative)
Diff
Primary Care
Physician
$48.13
$96.23
$48.10
(99.9%)
$47.61
$92.40
$44.79
(94.1%)
$47.69
$94.03
$46.33
(97.1%)
Advanced Practice
Nurses (APN)
$33.95
$63.45
$29.50
(86.9%)
$33.17
$65.41
$32.24
(97.2%)
$34.62
$65.62
$31.00
(89.5%)
Cardiologists
$44.68
$75.76
$31.08
(69.6%)
$66.61
$117.03
$50.42
(75.7%)
$64.68
$115.41
$50.73
(78.4%)
General Surgery
$58.74
$103.30
$44.56
(75.9%)
$57.83
$104.68
$46.85
(81.0%)
$58.65
$105.81
$47.16
(80.4%)
Obstetrician /
Gynecologist
$33.78
$87.59
$53.81
(159.3%)
$37.78
$90.92
$53.15
(140.7%)
$31.46
$100.94
$69.49
(220.9%)
Oncologist
$64.02
$108.32
($44.30)
(69.2%)
$62.56
$110.60
($48.04)
(76.8%)
$62.94
$109.14
$46.20
(73.4%)
Ophthalmologists
$84.04
$104.65
$20.61
(24.5%)
$57.12
$106.08
$48.96
(85.7%)
$57.37
$107.56
($50.19)
(87.5%)
Orthopedists
$53.50
$97.04
$43.54
(81.4%)
$51.21
$96.13
$44.92
(87.7%)
$51.51
$96.17
$44.66
(86.7%)
Psychologists /
Psychiatrists
$49.94
$83.91
$33.97
(68.0%)
$54.50
$88.95
$34.45
(63.2%)
$56.09
$92.46
$36.38
(64.9%)
Notes: Weighted Medicaid and QHP Average Prices were based on the most common CPT procedures billed for outpatient (non-ER)
services. Only CPT procedures that were represented both in Medicaid and QHP claims are included in the weighted averages. Relative
difference percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: MCD=Medicaid; QHP=Qualified Health Plans; Diff=Difference
For all provider types, QHPs reimburse identical procedures at higher dollar rates than Medicaid. In 2014, average
higher QHP remuneration relative differences ranged from 24.5 percent for ophthalmologists to 159.3 percent for
obstetrician/gynecologist providers. In 2015, average higher QHP remuneration relative differences ranged from
63.2 percent for psychologists/psychiatrists to 140.7 percent for obstetrician/gynecologist providers. In 2016,
average higher QHP remuneration relative differences ranged from 64.9 percent for psychologists/psychiatrists to
220.9 percent for obstetrician/gynecologist providers.
Time to First Visit at Program Initiation
In 2014, realized access differences in the time it took for those enrolled in Medicaid and QHPs to have their first
contact with the healthcare delivery system were identified from a Kaplan-Meier survival analysis (see Figure 8).
This is likely still the best representation of programmatic realized access, as the denominator included those who
were continuously enrolled from program start-up in January 2014 through the end of December 2014. Those
who enrolled after January 2014 may have had initial contact with the healthcare system that was confounded by
seasonal demand for health care.
In 2014, it was identified that more than twice as many QHP enrollees (21.2 percent) had a healthcare visit in the
first 30 days compared to new Medicaid enrollees (8.2 percent). By 90 days, 41.8 percent of those enrolled in a
QHP had at least one outpatient care visit, compared to 29.6 percent of those enrolled in traditional Medicaid.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 31
Figure 8. Proportion of Medicaid and QHP Enrollees with a First Outpatient Care Visit, by Day
Differences in Comparison Groups by Comparison Populations
General Population
Perceived Access
Table 5 presents a comparison of perceived access indicator differences between Medicaid and QHP enrollees in
the General Population. Responses are based on those who completed the CAHPS II survey and with a one-to-one
propensity score matched population of Medicaid and QHP enrollees.
Cumulative Probability of Outpatient Visit
Time to Event Duration: First Outpatient Visit (in Days)
Medicaid
Commercial QHP
% of Enrollees with Visit by
30 Days
Medicaid 8.2%
Commercial QHP 21.2%
% of Enrollees with Visit by
90 Days
Medicaid 29.6%
Commercial QHP 41.8%

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 32
Table 5. Differences in Perceived Access to Health Care between Medicaid and QHP Enrollees
(Propensity Score Matched Comparison)
Perceived Access Indicators
Matched N
Medicaid
Mean (StdErr)
QHP
Mean
(StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Percentage of enrollees who always received care when
it was needed right away
95
52.6 (5.1)
66.3 (4.8)
26.0
0.057
Percentage of enrollees who always got an appointment
for a check-up or routine care as soon as needed
149
57.7 (4.1)
59.7 (4.0)
3.5
0.702
Percentage of enrollees who always got an appointment
to a specialist as soon as needed
97
54.6 (5.1)
48.5 (5.5)
-9.4
0.474
Percentage of enrollees who always found it easy to get
the care, tests, and treatment needed
171
50.3 (3.8)
57.3 (3.8)
14.0
0.195
Notes: Data were obtained from CAHPS II responses. Adjusted analysis was performed using a propensity score matched sample.
Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: Matched N=number of Medicaid and QHP matched enrollee respondents; StdErr=standard error of estimated mean.
When Medicaid and QHP enrollees were matched by propensity score, no differences were observed across any
of the four perceived access indicators.
Primary Preventive Screenings
Receipt of a flu shot or spray is an indicator of quality primary preventive care. Table 6 shows results from
comparing all General Population Medicaid and QHP enrollees responding to CAHPS II and then restricting
analysis to a Medicaid and QHP propensity score matched population.
Table 6. Differences in Primary Preventive Health Care between Medicaid and QHP Enrollees
(Propensity Score Matched Comparison)
Primary
Preventive Healthcare
Indicators
Period
N
Medicaid
Mean (StdErr)
QHP
Mean (StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Percentage of enrollees
receiving flu shot or spray
(primary)
All
Respondents
241 (Medicaid)
792 (QHP)
33.7 (3.1)
36.1 (1.7)
6.9
0.240
Propensity
Score Matched
216
34.3 (3.2)
43.1 (3.4)
25.7
0.063
Notes: Receipt of flu shot or spray was obtained from CAHPS II responses. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: StdErr=standard error of estimated mean.
There were no differences in the percentages of Medicaid and QHP enrollees who received a flu shot or spray in
the year prior to completing the CAHPS II.
Secondary and Tertiary Preventive Screenings
Secondary and tertiary screenings for medical conditions are also a strong sign of quality preventive care.
Table 7 presents a series of screening comparisons between propensity score matched Medicaid and QHP
enrollees.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 33
Table 7. Differences in Secondary and Tertiary Preventive Health Care between Medicaid and QHP
Enrollees (Propensity Score Matched Comparison)
Secondary and Tertiary
Preventive Healthcare
Indicators
Time Period
Matched
N
Medicaid
Mean (StdErr)
QHP
Mean (StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Yearly Assessments
Percentage of chlamydia
screening (secondary)
Year 2
1,524
36.9 (1.2)
37.5 (1.2)
1.8
0.707
Year 3
610
44.4 (2.0)
45.2 (2.0)
1.8
0.773
Percentage of cholesterol
screening (secondary)
Year 2
9,463
18.8 (0.4)
28.3 (0.5)
50.6
<0.001
Year 3
4,741
17.1 (0.5)
30.8 (0.7)
80.0
<0.001
Percentage of enrollees with
diabetes with evidence of
HbA1C assessment (tertiary)
Year 2
1,156
62.7 (1.4)
82.5 (1.1)
31.6
<0.001
Year 3
1,118
32.9 (1.4)
51.2 (1.5)
55.4
<0.001
Periodic Assessments (if age and gender appropriate, eligible for at least one screening over 3 years)
Percentage of cervical cancer
screening (secondary)
3 years
6,771
27.9 (0.5)
34.9 (0.6)
25.1
<0.001
Percentage of breast cancer
screening (secondary)
3 years
984
16.6 (1.8)
24.2 (1.4)
46.6
<0.001
Percentage of colorectal
screening (secondary)
3 years
647
11.6 (1.3)
22.6 (1.6)
94.7
<0.001
Composite Assessments (if eligible for at least one screening)
Percentage of enrollees who
received at least one eligible
screening (secondary)
3 years
16,902
30.2 (0.4)
39.8 (0.4)
31.8
<0.001
Percentage of enrollees who
received at least half of eligible
screening (secondary)
3 years
16,902
19.9 (0.3)
26.1 (0.3)
30.9
<0.001
Percentage of enrollees who
received all eligible screenings
(secondary)
3 years
16,902
16.9 (0.3)
21.1 (0.3)
24.9
<0.001
Notes: All quality and screening indicators were derived from claims data. Adjusted analysis was performed using a propensity score
matched sample. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: Matched N=number of Medicaid and QHP matched enrollees; StdErr=standard error of estimated mean.
For every secondary and tertiary screening indicator presented in Table 7, with the exception of chlamydia
screening, QHP enrollees received higher rates of screening than Medicaid enrollees.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 34
Disease Management
Table 8 presents a propensity score matched Medicaid and QHP General Population comparison of treatments and
condition management consistent with quality of care delivery. Diabetic HbA1C assessment is included again in this
section because it is both a condition that is screened for, but also a quality indicator of disease management.
Table 8. Differences in the Percentage of Medicaid and QHP Enrollees Receiving Recommended
Disease Management (Propensity Score Matched Comparison)
Preventable Utilization
Indicators
Time Period
Matched
N
Medicaid
Mean (StdErr)
QHP
Mean (StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Percentage of enrollees with
diabetes with evidence of
HbA1C assessment (tertiary)
Year 2
1,156
62.7 (1.4)
82.5 (1.1)
31.6
<0.001
Year 3
1,118
32.9 (1.4)
51.2 (1.5)
55.4
<0.001
Anti-depressant management
3 years
866
43.2 (1.7)
58.2 (1.7)
34.8
<0.001
Rate of mental/behavioral
disorder inpatient
hospitalizations per 10,000
person-years
Year 2
27,822
193.4 (10.0)
202.4 (10.4)
4.7
0.461
Year 3
13,577
172.0 (15.0)
260.2 (17.4)
51.2
<0.001
Proportion of enrollees with any
re-engagement with outpatient
care per 100 discharges
Year 2
1,693
60.4 (1.6)
65.3 (1.6)
8.0
0.044
Year 3
625
58.6 (2.5)
65.8 (3.0)
12.4
0.054
Notes: All hospitalization indicators derived from claims data. Adjusted analysis was performed using a propensity score matched
sample. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: Matched N=number of Medicaid and QHP matched enrollees; StdErr=standard error of estimated mean.
QHP enrollees with diabetes had a higher relative percentage in Year 2 (31.6 percent) and in Year 3 (55.4 percent),
of having an HbA1c assessment compared to Medicaid enrollees in these coverage years.
Compared to Medicaid enrollees, 34.8 percent more QHP enrollees (58.2 percent compared to 43.2 percent)
received anti-depressant management over the course of the three years under study.
In the third year of health insurance coverage, compared to those covered by Medicaid, those covered by a
QHP had a higher rate of mental/behavioral disorder hospitalizations (260.2 compared to 172.0 per 10,000
person-years).
Compared to Medicaid enrollees at 60.4 percent in Year 2, 65.3 percent of QHP enrollees had re-engagement with
outpatient care following hospital discharge.
Use of Healthcare Services
Table 9 presents propensity score matched Medicaid and QHP healthcare services and procedure differences for
enrollees entered into the second and third years of coverage.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 35
Table 9. Differences in the Use of Healthcare Services between Medicaid and QHP Enrollees
(Propensity Score Matched Comparison)
Use of Healthcare Services
Indicators
Time Period
N
Medicaid
Mean (StdErr)
QHP
Mean (StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Rate of abdominal
hysterectomy per 10,000
person-years
Year 2
17,633
34.7 (4.5)
46.4 (5.2)
33.7
0.097
Year 3
8,706
30.5 (6.3)
48.8 (8.0)
60.1
0.079
Rate of vaginal hysterectomy
per 10,000 person-years
Year 2
17,633
32.4 (4.7)
42.8 (5.2)
32.4
0.120
Year 3
8,706
45.0 (8.4)
29.0 (6.5)
-35.6
0.108
Rate of cardiac catheterization
per 10,000 person-years
Year 2
27,822
69.2 (5.4)
63.3 (5.1)
-8.6
0.362
Year 3
13,577
75.2 (8.7)
82.3 (8.6)
9.4
0.584
Rate of PCI per 10,000 person-
years
Year 2
27,822
31.8 (4.8)
30.1 (4.2)
-5.3
0.678
Year 3
13,577
14.7 (4.4)
21.6 (4.7)
47.1
0.231
Rate of CABG per 10,000
person-years
Year 2
27,822
6.0 (1.5)
5.0 (1.4)
-17.2
0.599
Year 3
13,577
6.1 (2.3)
1.7 (1.2)
-72.5
0.103
Rate of back surgery per 10,000
person-years
Year 2
27,822
53.4 (4.7)
50.5 (4.9)
5.7
0.672
Year 3
13,577
46.7 (6.6)
53.2 (7.1)
14.0
0.501
Rate of open cholecystectomy
per 10,000 person-years
Year 2
27,822
3.7 (1.2)
1.5 (0.8)
-59.2
0.129
Year 3
13,577
1.7 (1.2)
2.5 (1.9)
44.2
0.700
Rate of laparoscopic
cholecystectomy per 10,000
person-years
Year 2
27,822
72.2 (5.4)
97.2 (6.3)
34.6
0.002
Year 3
13,577
66.6 (7.8)
90.6 (8.6)
36.1
0.036
Rate of total hip replacement
per 10,000 person-years
Year 2
27,822
7.9 (1.9)
8.4 (1.9)
6.8
0.844
Year 3
13,577
5.2 (2.4)
3.4 (1.7)
-35.9
0.482
Rate of total knee replacement
per 10,000 person-years
Year 2
27,822
16.1 (2.7)
12.6 (2.2)
-21.8
0.278
Year 3
13,577
10.4 (2.6)
13.1 (3.2)
36.2
0.425
Rate of lumpectomy per 10,000
person-years
Year 2
17,633
14.7 (3.1)
24.4 (4.0)
65.9
0.047
Year 3
8,706
21.2 (5.3)
23.7 (5.9)
11.9
0.743
Rate of unilateral mastectomy
per 10,000 person-years
Year 2
17,633
4.1 (1.8)
4.8 (1.9)
15.6
0.781
Year 3
8,706
5.3 (3.2)
4.0 (2.2)
-25.4
0.697
Notes: All healthcare service indicators derived from claims data. Adjusted analysis was performed using a propensity score matched
sample. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100. Prostatectomy, carotid endarterectomy, and bilateral
mastectomy indicators also tested with no significant differences between Medicaid and QHP enrollees.
Abbreviations: Matched N=number of Medicaid and QHP matched enrollees; StdErr=standard error of estimated mean.
With 97.2 procedures per 10,000 person-years in Year 2 of coverage and 90.6 procedures per 10,000 person-
years in Year 3 of coverage, second- and third-year enrollees in a QHP received more laparoscopic
cholecystectomies than Medicaid enrollees with 72.2 and 66.6 procedures per 10,000 person-years,
respectively, over the same coverage periods. Female QHP enrollees into Year 2 of coverage also have more
lumpectomies per 10,000 person-years (24.4) than Medicaid enrollees (14.7) covered for an equal period of
time. No other healthcare services rate differences were found between Medicaid and QHP enrollees in their
second or third year of coverage.
Table 10 shows hospital utilization differences between propensity score matched Medicaid and QHP enrollees
who were into Years 2 and 3 of insurance coverage with the programs.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 36
Table 10. Differences in Rates of Preventable Hospitalizations and Readmissions between Medicaid
and QHP Enrollees (Propensity Score Matched Comparison)
Preventable Utilization
Indicators
Time Period
Matched
N
Medicaid
Mean (StdErr)
QHP
Mean (StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Rate of medical/surgery
hospital discharges per 10,000
person-years
Year 2
27,822
757.7 (23.0)
643.0 (22.2)
-15.1
<0.001
Year 3
13,577
663.0 (28.3)
675.0 (34.2)
1.8
0.773
Rate of preventable
hospitalizations per 10,000
person-years
Year 2
27,822
102.5 (8.2)
97.6 (9.5)
-4.8
0.536
Year 3
13,577
91.6 (13.2)
104.7 (18.4)
14.3
0.325
Average length of stay in days
for all hospitalizations
Year 2
2,463
4.7 (0.2)
6.2 (0.2)
32.6
<0.001
Year 3
946
4.4 (0.2)
6.2 (0.4)
39.2
<0.001
Average length of stay in days
for medical/surgery
hospitalizations
Year 2
1,344
5.1 (0.3)
5.7 (0.3)
11.5
<0.001
Year 3
525
4.6 (0.2)
5.7 (0.4)
24.8
<0.001
Proportion of enrollees with any
all-cause 30-day readmission
per 100 hospitalizations
Year 2
1,593
11.8 (1.0)
13.7 (1.1)
15.7
0.085
Year 3
625
14.3 (2.8)
15.3 (2.5)
7.1
0.581
Notes: All hospitalization indicators derived from claims data. Adjusted analysis was performed using a propensity score matched
sample. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: Matched N=number of Medicaid and QHP matched enrollees; StdErr=standard error of estimated mean.
Compared to QHP enrollees, Medicaid enrollees in Year 2 of insurance coverage had 15.1 percent more
hospitalizations per 10,000 person-years (757.7 compared to 643.0 discharges per 10,000 person-years).
However, QHP enrollees who had hospitalizations spent more time, on average, in the hospital than Medicaid
enrollees. For those in the second year of insurance coverage, the difference was an average of 1.5 extra days, or
a 32.6 percent greater length of stay. For those in the third year of insurance coverage, the difference was an
average of 1.8 extra days, or a 39.2 percent greater length of stay. No differences between Medicaid and QHP
enrollees were observed for the rate of preventable hospitalizations or all-cause 30-day readmission rates.
Table 11 contains propensity score matched Medicaid and QHP enrollee difference for the rate of total, emergent,
and non-emergent emergency room (ER) utilization.
Table 11. Differences in Utilization of Emergency Room Services between Medicaid and QHP Enrollees
(Propensity Score Matched Comparison)
Emergency Room Indicators
Time Period
Matched
N
Medicaid
Mean (StdErr)
QHP
Mean (StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Rate of total emergency room
visits per 100 person-years
Year 2
27,822
82.4 (1.2)
73.5 (1.0)
-10.8
<0.001
Year 3
13,577
90.3 (1.9)
87.7 (1.7)
-2.9
0.041
Rate of emergent emergency
room visits per 100 person-
years
Year 2
27,822
14.5 (0.4)
12.7 (0.3)
-12.4
<0.001
Year 3
13,577
15.8 (0.6)
14.6 (0.4)
-7.5
0.020
Rate of non-emergent
emergency room visits per 100
person-years
Year 2
27,822
41.6 (0.7)
37.1 (0.6)
-10.8
<0.001
Year 3
13,577
45.5 (1.1)
44.2 (1.0)
-2.8
0.176
Notes: All emergency room indicators derived from claims data. Definitions for emergent and non-emergent care obtained from the
updated NYU algorithm (2017). Adjusted analysis was performed using a propensity score matched sample. Relative percentage calculated
as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: Matched N=number of Medicaid and QHP matched enrollees; StdErr=standard error of estimated mean.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 37
Medicaid enrollees in the second year of coverage had 10.8 percent more total ER visits than QHP enrollees. The
rate difference between Medicaid and QHP enrollees drops to 2.9 percent, but still significant, when comparing
those enrolled in the third year of coverage. When restricting analysis only to emergent emergency room visits,
Medicaid enrollees in the second and third years of coverage had 12.4 and 7.5 percent more visits, respectively,
than QHP enrollees. Compared to QHP enrollees in the second year of coverage, Medicaid enrollees experienced
10.8 percent more non-emergent ER visits. There is no Year 3 difference for non-emergent emergency room visits
between Medicaid and QHP propensity score matched enrollees.
Higher Needs Population
For the Medicaid and QHP statistical comparisons in this section, frequencies and rates for the full subgroup
populations are depicted along with the regression discontinuity local average treatment effects (LATE) for those
with an exceptional healthcare needs assessment composite score within a model-derived optimal bandwidth
around the threshold cut-point. The experience for those around the cut-point may differ from the comparison of
subgroup populations overall and hence effects may be reversed. Significant differences are concluded between
Medicaid and QHP subgroup populations for p-values associated with a LATE of 0.05 or less and the LATE
percentage is described in the results. Negative LATE values indicate that QHP enrollees had higher percentages
or rates compared to Medicaid enrollees.
Perceived Access
Table 12 presents a comparison of perceived access differences between Medicaid and QHP enrollees in the
Higher Needs Population. Responses are based on those who completed the CAHPS II survey.
Table 12. Differences in Perceived Access to Health Care between Medicaid and QHP Enrollees
(Regression Discontinuity Comparison)
Medicaid
QHP
Relative
Difference
(percent)
Average
Treatment
Effect
(percent)
Statistical
Difference
(p-value)
Perceived and Realized Access Indicators
N
Mean
(StdErr)
N
Mean
(StdErr)
Percentage of enrollees who always received care
when it was needed right away
537
52.9
(2.2)
505
72.3
(2.0)
36.7
-26.6
0.004
Percentage of enrollees who always got an
appointment for a check-up or routine care as
soon as needed
788
55.2
(1.8)
833
60.4
(1.7)
9.4
1.7
0.790
Percentage of enrollees who always got an
appointment with a specialist as soon as needed
564
52.5
(2.1)
581
55.4
(2.1)
5.6
6.2
0.346
Percentage of enrollees who always found it easy
to get the care, tests, and treatment needed
886
47.2
(1.7)
956
62.0
(1.6)
31.5
-18.7
0.003
Notes: Data were obtained from CAHPS II responses. Adjusted analysis was performed using regression discontinuity with a model-
derived optimal bandwidth around an exceptional healthcare needs composite score cut-point. Average treatment effect depicts
model-estimated difference at cut-point. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
Compared to Medicaid enrollees, an estimated 26.6 percent more QHP enrollees indicated that they always
received care when it was needed right away, and an estimated 18.7 percent more QHP enrollees indicated that
they always found it easy to get the care, tests, and treatment they needed.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 38
Primary Preventive Screenings
Receipt of a flu shot or spray is an indicator of quality preventive care. Table 13 presents the results from
comparing all Higher Needs Population Medicaid and QHP respondents to CAHPS II and then restricting to a
regression discontinuity model-derived optimal bandwidth around an exceptional healthcare needs composite
score cut-point.
Table 13. Differences in Primary, Secondary, and Tertiary Preventive Health Care between Medicaid
and QHP Enrollees (Regression Discontinuity Comparison
Primary/Secondary/Tertiary
Preventive Healthcare
Indicators
Medicaid
QHP
Relative
Difference
(Percent)
Average
Treatment
Effect
(Percent)
Statistical
Difference
(p-value)
Period
N
Mean
(StdErr)
N
Mean (StdErr)
Percentage of enrollees
receiving flu shot or spray
(primary)
CAHPS II
Crude
967
40.7 (1.6)
1,080
42.2 (1.5)
3.5
--
0.064
CAHPS II
RD
985
40.3 (1.6)
1,091
44.0 (1.5)
9.2
-22.2
0.001
Notes: Receipt of flu shot or spray, which was derived from CAHPS II. Adjusted analysis was performed using regression discontinuity
with a model-derived optimal bandwidth around an exceptional healthcare needs composite score cut-point. Average treatment effect
depicts model-estimated difference at cut-point. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; RD=Regression discontinuity; StdErr=standard error of estimated mean.
Using the full Higher Needs Population (Crude) who responded to the CAHPS II survey, there was no difference in
the percentages of Medicaid and QHP enrollees who received a flu shot or spray in the year prior to completing
the survey. When restricting the population to a regression discontinuity model-derived optimal bandwidth
around the exceptional healthcare needs composite score cut-point, 22.2 percent more QHP enrollees were
estimated to have received a flu shot or spray compared to Medicaid enrollees.
Secondary and Tertiary Preventive Screenings
Secondary and tertiary screenings for medical conditions are also a strong sign of qualit y preventive care.
Table 14 presents a series of screening comparisons between Medicaid and QHP enrollees in the Higher
Needs Population.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 39
Table 14. Differences in Secondary and Tertiary Preventive Health Care between Medicaid and QHP
Enrollees (Regression Discontinuity Comparison)
Primary/Secondary/Tertiary
Preventive Healthcare
Indicators
Medicaid
QHP
Relative
Difference
(percent)
Average
Treatment
Effect
(percent)
Statistical
Difference
(p-value)
Period
N
Mean
(StdErr)
N
Mean
(StdErr)
Yearly Assessments
Percentage of chlamydia
screening (secondary)
Baseline
253
40.7 (3.1)
1,806
34.9 (1.1)
-14.3
-2.1
0.673
Year 2
395
35.7 (2.4)
2,664
34.2 (0.9)
-4.1
-10.0
0.024
Year 3
224
48.7 (3.3)
1,617
47.1 (1.2)
-3.3
14.5
0.004
Percentage of cholesterol
screening (secondary)
Baseline
1,865
39.6 (0.7)
8,134
40.1 (0.3)
1.1
-17.2
<0.001
Year 2
4,947
31.6 (0.7)
21,354
37.9 (0.3)
20.2
-18.1
0.002
Year 3
4,455
33.3 (0.7)
18,958
41.0 (3.6)
23.4
-19.9
<0.001
Percentage of enrollees
with diabetes with evidence
of HbA1C assessment
(tertiary)
Baseline
978
75.1 (1.4)
2,353
89.1 (0.6)
18.7
-10.7
<0.001
Year 2
1,162
62. 2 (1.4)
2,958
83.7 (0.7)
34.5
-22.8
<0.001
Year 3
1,157
60.6 (1.4)
3,230
77.9 (0.7)
28.6
-21.5
<0.001
Periodic Assessments (if age and gender appropriate, eligible for at least one screening over 3 years)
Percentage of cervical
cancer screening
(secondary)
3 Years
1,313
29.5 (1.3)
5,777
45.8 (0.7)
55.5
-15.9
<0.001
Percentage of breast cancer
screening (secondary)
3 Years
885
44.1 (1.7)
3,721
51.7 (0.8)
17.2
-19.4
0.002
Percentage of colorectal
screening (secondary)
3 Years
1,286
27.3 (1.2)
5,950
28.7 (0.6)
5.0
3.0
0.382
Composite Assessments (if eligible for at least one screening)
Percentage of enrollees who
received at least one
eligible screening
(secondary)
3 Years
6,400
61.6 (0.6)
28,383
62.6 (0.3)
1.7
-15.3
0.007
Percentage of enrollees who
received at least half of
eligible screenings
(secondary)
3 Years
6,400
29.6 (0.6)
28,383
35.5 (0.3)
19.8
-16.2
0.002
Percentage of enrollees who
received all eligible
screenings (secondary)
3 Years
6,400
11.7 (0.4)
28,383
16.8 (0.2)
43.8
-6.9
<0.001
Notes: All quality and screening indicators were derived from claims data. Adjusted analysis was performed using regression
discontinuity with a model-derived optimal bandwidth around an exceptional healthcare needs composite score cut-point. Average
treatment effect depicts model-estimated difference at cut-point. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
All secondary and tertiary screening indicators presented in Table 14 with the exception of chlamydia screenings
in 2014 and colorectal screenings, show a higher percentage of QHP enrollees receiving screenings compared to
Medicaid enrollees.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 40
Disease Management
Table 15 presents a Medicaid and QHP Higher Needs Population comparison of treatments and condition
management that are consistent with quality of care delivery.
Table 15. Differences in the Percentage of Medicaid and QHP Enrollees Receiving Recommended
Disease Management (Regression Discontinuity Comparison)
Primary/Secondary/Tertiary
Preventive Healthcare
Indicators
Medicaid
QHP
Relative
Difference
(percent)
Average
Treatmen
t Effect
(percent)
Statistical
Differenc
e
(p-value)
Period
N
Mean
(StdErr)
N
Mean
(StdErr)
Percentage of enrollees with
diabetes with evidence of
HbA1C assessment (tertiary)
Baseline
978
75.1 (1.4)
2,353
89.1 (0.6)
18.7
-10.7
<0.001
Year 2
1,162
62. 2 (1.4)
2,958
83.7 (0.7)
34.5
-22.8
<0.001
Year 3
1,157
60.6 (1.4)
3,230
77.9 (0.7)
28.6
-21.5
<0.001
Anti-depressant
management
3 years
592
45.9 (2.1)
2,477
59.3 (1.0)
29.1
-15.8
0.002
Rate of mental/behavioral
disorder inpatient
hospitalizations per 10,000
person-years
Baseline
9,037
342.1 (20.2)
44,285
75.0 (4.3)
-78.1
304.1
0.003
Year 2
9,037
302.6 (20.0)
44,285
110.8 (5.7)
-63.4
157.5
0.179
Year 3
7,951
334.4 (24.7)
37,752
116.8 (6.5)
-65.1
167.8
0.245
Proportion of enrollees with
any re-engagement with
outpatient care per 100
discharges
Baseline
1,062
76.7 (2.0)
1,765
68.8 (1.3)
-10.3
2.9
0.316
Year 2
979
73.6 (2.9)
2,013
70.4 (1.4)
-4.4
-2.2
0.411
Year 3
905
69.2 (2.0)
1,809
70.1 (1.4)
1.2
-11.4
0.030
Notes: Adjusted analysis was performed using regression discontinuity with a model-derived optimal bandwidth around an
exceptional healthcare needs composite score cut-point. Average treatment effect depicts model-estimated difference at cut-
point. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
Compared to Medicaid enrollees with diabetes, a higher percentage of QHP enrollees with diabetes received an
HbA1C test during each of the three years under study. The difference was 10.7 percent at Baseline, 22.8 percent
in Year 2, and 21.5 percent in Year 3. QHP enrollees were also more likely to receive anti-depressant management
compared to Medicaid enrollees (15.8 percent).
Compared to QHP enrollees, those covered by Medicaid had a higher rate of mental/behavioral disorder
hospitalizations in each year of coverage. This effect was estimated to be a 304.1 percent, 157.5 percent, and
167.8 percent higher rate of hospitalizations per 10,000 person-years at Baseline, Year 2, and Year 3,
respectively.
In Year 3 (2016), QHP enrollees had a higher rate of re-engagement with outpatient care compared to Medicaid
enrollees (11.4 percent).
Use of Healthcare Services
The difference in medical procedure rates for Higher Needs Population Medicaid and QHP enrollees is presented
in Table 16.
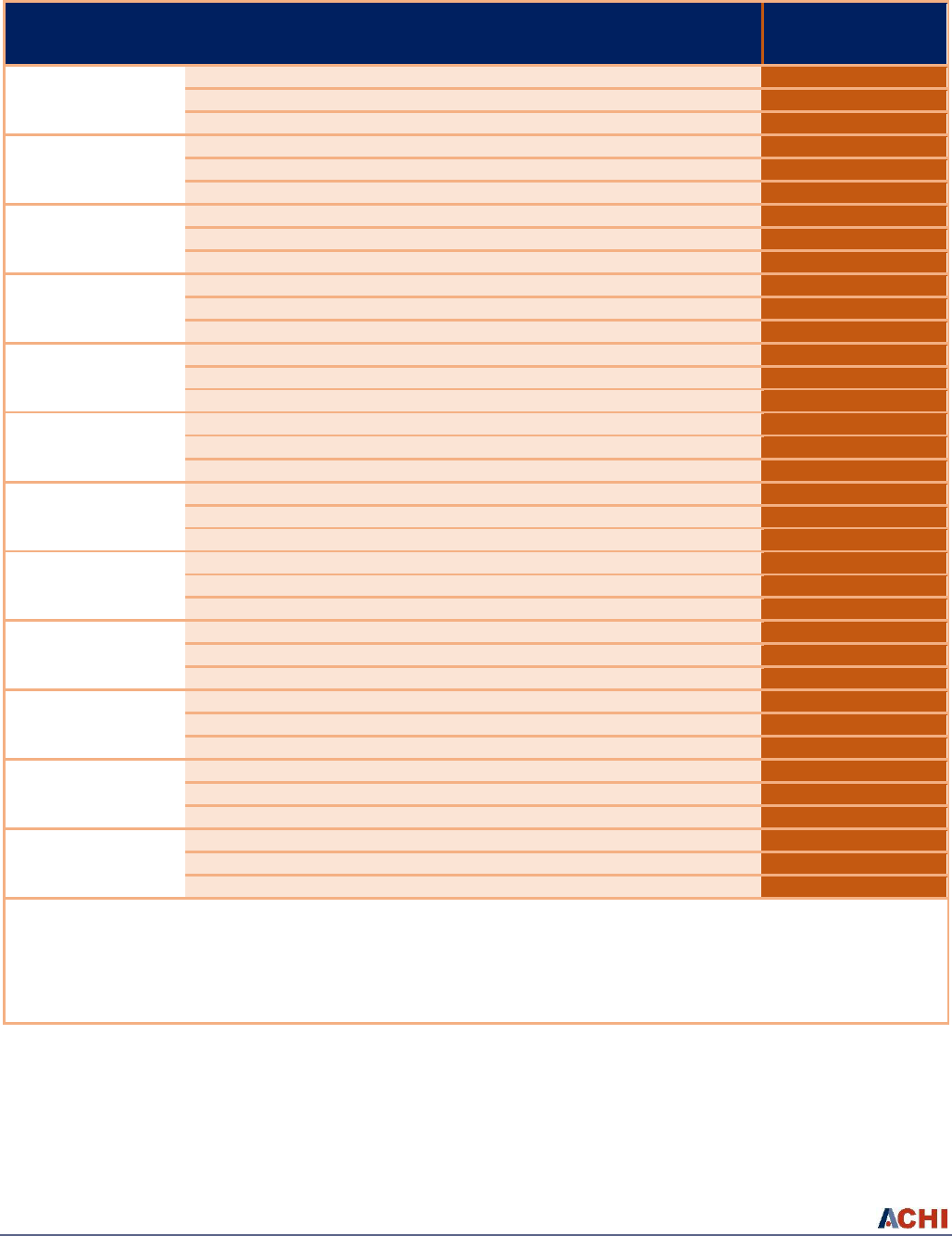
Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 41
Table 16. Differences in the Use of Healthcare Services between Medicaid and QHP Enrollees
(Regression Discontinuity Comparison)
Use of Healthcare
Services Indicators
Medicaid
QHP
Relative
Difference
(percent)
Average
Treatment
Effect
Statistical
Difference
(p-value)
Period
N
Mean (StdErr)
N
Mean
(StdErr)
Rate of abdominal
hysterectomy per
10,000 person-years
Baseline
5,763
46.4 (9.4)
26,469
57.6 (4.9)
24.1
-12.8
0.715
Year 2
5,763
103.3 (13.6)
26,469
51.7 (4.5)
-49.9
24.6
0.368
Year 3
5,168
42.2 (9.2)
23,241
37.5 (4.1)
-11.2
-11.8
0.655
Rate of vaginal
hysterectomy per
10,000 person-years
Baseline
5,763
79.2 (12.9)
26,469
78.6 (5.8)
-0.9
-57.7
0.011
Year 2
5,763
54.4 (10.2)
26,469
53.3 (4.6)
-2.0
-3.1
0.929
Year 3
5,168
34.1 (8.7)
23,241
51.3 (4.8)
50.2
20.3
0.249
Rate of cardiac
catheterization per
10,000 person-years
Baseline
9,037
280.0 (19.5)
44,285
109.1 (5.3)
-61.0
8.42
0.871
Year 2
9,037
207.2 (15.6)
44,285
100.6 (5.1)
-51.4
-45.3
0.448
Year 3
7,951
213.8 (18.0)
37,752
108.0 (5.6)
-49.5
-59.6
0.089
Rate of PCI per 10,000
person-years
Baseline
9,037
126.9 (19.3)
44,285
34.3 (3.3)
-73.0
35.5
0.337
Year 2
9,037
95.4 (15.7)
44,285
41.5 (3.9)
-59.5
-28.6
0.423
Year 3
7,951
63.0 (11.6)
37,752
31.1 (3.5)
-50.7
-4.6
0.871
Rate of CABG per
10,000 person-years
Baseline
9,037
23.7 (5.4)
44,285
10.9 (1.7)
-53.8
-6.3
0.609
Year 2
9,037
8.1 (3.1)
44,285
8.1 (1.4)
-0.5
-1.5
0.875
Year 3
7,951
15.7 (4.5)
37,752
9.1 (1.6)
-42.4
-5.6
0.661
Rate of back surgery
per 10,000 person-
years
Baseline
9,037
158.0 (15.8)
44,285
46.0 (3.5)
-70.9
27.6
0.199
Year 2
9,037
126.9 (13.4)
44,285
59.6 (4.0)
-53.0
-34.2
0.118
Year 3
7,951
95.7 (12.3)
37,752
75.3 (5.0)
-21.3
-49.1
0.202
Rate of open
cholecystectomy per
10,000 person-years
Baseline
9,037
11.2 (3.7)
44,285
4.1 (1.0)
-63.7
0.7
0.922
Year 2
9,037
7.0 (2.8)
44,285
2.6 (0.8)
-62.4
--
--
Year 3
7,951
5.2 (2.6)
37,752
3.0 (0.9)
-42.4
13.1
0.058
Rate of laparoscopic
cholecystectomy per
10,000 person-years
Baseline
9,037
215.2 (16.8)
44,285
123.8 (5.7)
-42.5
9.43
0.868
Year 2
9,037
111.7 (11.6)
44,285
106.1 (5.0)
-5.1
-63.1
0.013
Year 3
7,951
120.7 (12.8)
37,752
88.5 (5.0)
-26.6
-2.6
0.928
Rate of total hip
replacement per
10,000 person-years
Baseline
9,037
23.6 (6.5)
44,285
8.9 (1.6)
-62.4
--
--
Year 2
9,037
23.3 (5.7)
44,285
7.4 (1.4)
-68.3
4.2
0.530
Year 3
7,951
15.7 (5.2)
37,752
7.4 (1.4)
-52.8
-12.4
0.070
Rate of total knee
replacement per
10,000 person-years
Baseline
9,037
32.3 (7.1)
44,285
13.5 (2.0)
-58.3
-10.1
0.466
Year 2
9,037
40.7 (7.8)
44,285
22.9 (2.5)
-43.8
-23.1
0.214
Year 3
7,951
51.1 (9.0)
37,752
30.0 (3.3)
-41.4
-27.3
0.033
Rate of lumpectomy
per 10,000 person-
years
Baseline
5,763
38.7 (8.6)
26,469
43.7 (4.5)
13.0
4.8
0.773
Year 2
5,763
38.1 (8.7)
26,469
26.1 (3.3)
-31.5
3.0
0.872
Year 3
5,168
22.1 (6.4)
23,241
24.5 (3.4)
11.0
-36.6
<0.001
Rate of unilateral
mastectomy per
10,000 person-years
Baseline
5,763
9.7 (4.3)
26,469
10.1 (2.2)
4.3
-8.26
0.222
Year 2
5,763
10.9 (5.1)
26,469
9.9 (2.2)
-9.2
-25.0
0.214
Year 3
5,168
8.0 (4.9)
23,241
6.7 (1.7)
-16.7
--
--
Notes: All healthcare service indicators derived from claims data. Adjusted analysis was performed using regression discontinuity
with a model-derived optimal bandwidth around an exceptional healthcare needs composite score cut -point. Average treatment
effect depicts model-estimated difference at cut-point. Cells with “--” indicate insufficient data in vicinity of the cut-point to
calculate bandwidth. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100. Prostatectomy, carotid endarterectomy,
and bilateral mastectomy indicators also tested with no significant differences between Medicaid and QHP enrollees.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
Sporadic differences in healthcare services are evidenced between Medicaid and QHP enrollees. At Baseline,
there were 57.7 fewer vaginal hysterectomies per 10,000 person-years performed in the eligible female Medicaid
enrollee population compared to QHP enrollees. At Year 2 there were 63.1 fewer laparoscopic cholecystectomies
per 10,000 person-years performed in the Medicaid enrollee population compared to QHP enrollees. At Year 3

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 42
there were 36.6 fewer lumpectomies per 10,000 person-years performed in the Medicaid enrollee population
compared to QHP enrollees.
Hospital Utilization
Table 17 compares hospital utilization measures across Medicaid and QHP enrollees in the years that they were
enrolled in the respective programs.
Table 17. Differences in Rates of Preventable Hospitalizations and Readmissions between Medicaid
and QHP Enrollees (Regression Discontinuity Comparison)
Medicaid
QHP
Relative
Difference
(percent)
Average
Treatment
Effect
Statistical
Difference
(p-value)
Preventable Utilization
Indicators
Period
N
Mean (StdErr)
N
Mean (StdErr)
Rate of
medical/surgery
hospital discharges per
10,000 person-years
Baseline
9,037
1,663.3 (55.7)
44,285
528.0 (12.8)
-68.3
473.4
0.312
Year 2
9,037
1,478.0 (58.4)
44,285
557.3 (14.8)
-62.3
379.6
0.166
Year 3
7,951
1,506.9 (61.7)
37,752
602.2 (17.2)
-60.0
-27.98
0.903
Rate of preventable
hospitalizations per
10,000 person-years
Baseline
9,037
68.9 (4.1)
44,285
233.9 (24.8)
-70.5
22.0
0.845
Year 2
9,037
61.7 (4.7)
44,285
217.6 (21.0)
-71.6
57.3
0.508
Year 3
7,951
69.0 (5.1)
37,752
219.0 (20.6)
-68.5
-10.9
0.846
Average length of stay
in days for all
hospitalizations
Baseline
1,208
5.3 (0.2)
2,259
4.6 (0.2)
-12.5
0.001
0.999
Year 2
1,213
5.1 (0.2)
2,850
5.3 (0.2)
3.5
-0.233
0.640
Year 3
1,072
5.7 (0.2)
2,496
5.7 (0.2)
0.5
-3.012
0.006
Average length of stay
in days for
medical/surgery
hospitalizations
Baseline
952
4.9 (0.2)
1,679
4.4 (0.2)
-10.6
-0.186
0.756
Year 2
881
5.1 (0.2)
1,835
4.9 (0.2)
-5.1
-0.413
0.408
Year 3
796
5.6 (0.3)
1,647
5.3 (0.2)
-5.8
-2.315
0.033
Proportion of enrollees
with any all-cause 30-
day readmission per
100 hospitalizations
Baseline
1,062
12.0 (1.3)
1,765
8.3 (0.8)
-30.7
0.044
0.282
Year 2
979
13.0 (1.4)
2,013
9.1 (0.8)
-30.3
0.101
<0.001
Year 3
905
12.1 (1.5)
1,809
11.6 (1.0)
-4.4
-0.063
0.097
Notes: All hospitalization indicators derived from claims data. Adjusted analysis was performed using regression discontinuity with a
model-derived optimal bandwidth around an exceptional healthcare needs composite score cut-point. Average treatment effect depicts
model-estimated difference at cut-point. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
In the three years of program enrollment, no differences in hospital discharge or preventable hospitalization rates
were concluded between Medicaid and QHP enrollees. In addition, in Year 2, Medicaid enrollees had a higher rate
of all-cause 30-day readmission (0.101 readmissions per 100 hospitalizations) compared to QHP enrollees. One
strong difference in program effect is observed for average length of stay in Year 3, where compared to QHP
enrollees, Medicaid enrollees had a lower average length of stay of 3.0 days overall, and 2.3 days for those with
just medical/surgical related hospitalizations.
Emergency Room (ER) Utilization
Table 18 compares emergency room (ER) utilization measures across Medicaid and QHP enrollees in the years
that they were enrolled in the respective programs.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 43
Table 18. Differences in Utilization of Emergency Room Services between Medicaid and QHP Enrollees
(Regression Discontinuity Comparison)
Emergency Room
Indicators
Period
Medicaid
QHP
Relative
Difference
(percent)
Average
Treatment
Effect
Statistical
Difference
(p-value)
N
Mean
(StdErr)
N
Mean
(StdErr)
Rate of total
emergency room visits
per 100 person-years
Baseline
9,037
141.9 (2.9)
44,285
58.2 (0.7)
-59.0
80.5
0.085
Year 2
9,037
120.7 (2.7)
44,285
53.9 (0.7)
-55.3
40.8
0.219
Year 3
7,951
112.0 (2.6)
37,752
55.0 (0.7)
-50.8
33.9
0.343
Rate of emergent
emergency room visits
per 100 person-years
Baseline
9,037
27.5 (0.9)
44,285
10.1 (0.2)
-63.4
8.1
0.415
Year 2
9,037
24.6 (0.9)
44,285
10.0 (0.2)
-59.2
4.3
0.602
Year 3
7,951
23.2 (0.9)
37,752
10.7 (0.2)
-53.7
5.1
0.112
Rate of non-emergent
emergency room visits
per 100 person-years
Baseline
9,037
74.4 (1.7)
44,285
31.1 (0.4)
-58.2
41.8
0.109
Year 2
9,037
60.4 (1.5)
44,285
27.8 (0.4)
-54.0
29.3
0.042
Year 3
7,951
53.8 (1.5)
37,752
27.1 (0.4)
-49.7
11.2
0.536
Notes: All emergency room indicators derived from claims data. Adjusted analysis was performed using regression discontinuity with a
model-derived optimal bandwidth around an exceptional healthcare needs composite score cut-point. Average treatment effect depicts
model-estimated difference at cut-point. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
With the exception of Medicaid enrollees having a higher rate of non-emergent emergency room visits in Year 2
(29.3 visits per 100 person-years) compared to QHP enrollees, enrollees in the two programs do not differ in ER
utilization.
Special Populations and Topic Studies
Medicaid and QHP Maternal Pregnancy and Birth Outcomes
Overview
Historically, Arkansas Medicaid covered uninsured pregnant women with incomes up to 200 percent FPL,
increasing to 214 percent in 2014 with Modified Adjusted Gross Income calculations and income disregards.
Under the terms and conditions of the Health Care Independence Program (HCIP), all newly pregnant women
applying for Medicaid would continue to be covered through the traditional Medicaid program even if their
income levels (< 138 percent FPL) made them otherwise eligible for enrollment in a Qualified Health Plan (QHP)
covered by premium assistance under the HCIP. However, as QHP-enrolled women became pregnant, they would
remain under a premium assistance program and have their pregnancy care covered by the QHP commercial
carrier in which they were enrolled. There were a number of pregnant women who did enroll in HCIP early in 2014
and this was due to a systematic failure to collect pregnancy information from all new enrollees, or the new
enrollees were diagnosed as pregnant after enrolling in a QHP. The earliest normal full gestational delivery date
for a woman who conceived while a beneficiary of a QHP in HCIP is on, or around, Sept. 30, 2014.
The goal of this study is to compare pregnancy outcomes for women who were covered by traditional Arkansas
Medicaid to those who were covered in a QHP through premium assistance in HCIP.
There is a noteworthy factor with an important impact on this study. Perinatal and obstetrical care for both
Medicaid and the private carriers are bundled and paid a global fee to the delivering provider. As such,
encounters for individual physician visits or treatments received are not consistently available within claims. From

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 44
inquiry of both Medicaid and private carriers, routine quality assessments are performed, however claims-based
indicators (e.g., HEDIS) on prenatal and/or pregnancy services are neither generated nor, for Medicaid, reported
to CMS. Consequently, this study relied on pregnancy outcomes and prenatal care recorded in the 2014 and 2015
Arkansas birth certificate vital records.
Data Sources and Analytic Population
Birth certificate data for 2014 and 2015 were obtained from the Arkansas Department of Health (2016 data was
not available at the time of analysis). Mother’s personal identifying information contained on the birth certificate
was assigned a unique identifier using a match engine (described in Appendix C). The same identifier is included
on Medicaid and QHP enrollment files.
Birth certificate and enrollment data were matched by mother and produced information on 34,675 births from
mothers who were covered by Medicaid or an HCIP QHP. This population was then restricted to include only live
births in Arkansas that occurred between Sept. 1, 2014, and Sept. 30, 2015 (15,597). A further restriction required
mothers to be enrolled with Medicaid or an HCIP QHP coverage for a period of at least 43 days prior to the date of
birth and 56 days after date of birth. This minimum enrollment time was based on HEDIS methodology and
provides some assurance that the mother had access to coverage for at least a portion of their prenatal and
postnatal period. Pregnant women who switched from Medicaid to a QHP — or vice versa — were also excluded.
In total, 10,453 births were retained for analysis. Appendix J contains a detailed inclusion/exclusion flow chart to
depict those included in the analytic sample.
Maternal and Birth Outcomes
Table 19 contains a listing of the maternal and birth outcomes under study along with a description and the
unit/scale of the measure. All outcomes were derived from responses on the birth certificate, with the exception
of non-delivery related, preterm hospitalizations.
Table 19. Maternal Pregnancy and Birth Outcomes, with Description
Outcome
Description
Measure
Maternal
Time to First Prenatal Visit
Estimated time from conception to first prenatal visit
Days (continuous)
Number of Prenatal Visits
Self-reported number of prenatal visits
Prenatal visits (days)
Preterm Hospitalization
(Preeclampsia)
Hospitalization (from claims data) was due to a diagnosis
of preeclampsia and not labor/childbirth
Yes or No (dichotomous)
Preterm Hospitalization
(Gestational Diabetes)
Hospitalization (from claims data) was due to a diagnosis
of gestational diabetes and not labor/childbirth
Yes or No (dichotomous)
Preterm Hospitalization (Any
Reason)
Hospitalization (from claims data) was due to any
diagnosis not including labor/childbirth
Yes or No (dichotomous)
Cesarean Section
Delivery was performed by cesarean section
Yes or No (dichotomous)
Birth
Preterm Birth
Birth occurred at less than 38 weeks of gestation
Yes or No (dichotomous)
Low Birth Weight
Baby weighed less than 2,500 grams
Yes or No (dichotomous)
Abnormal Outcome
Combined measure of all abnormal indicators, excluding
meconium
Yes or No (dichotomous)
APGAR5 1
A systematic measure for evaluating the physical
condition of the infant at specific intervals following birth
Very abnormal category or
other category
(dichotomous)
APGAR5 2
A systematic measure for evaluating the physical
condition of the infant at specific intervals following birth
Any abnormal category or
other category
(dichotomous)
NICU Stay
Neonatal intensive care unit stay required following birth
Yes or No (dichotomous)

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 45
Propensity Score Matching
A propensity scoring approach was implemented to match QHP mothers with traditional Medicaid mothers,
controlling for demographic and clinical characteristics prognostic for the maternal and infant outcomes assessed.
As a first step, a dichotomous variable indicating the assignment of a pregnant woman in a QHP (1) or Medicaid
(0) was used as an outcome variable in a logistic regression. Covariates obtained from the birth certificate data
used in the regression included mother’s age, race/ethnicity, insurance region, WIC (Women, Infants, and
Children) program status, body mass index category, education and marital status, urban/rural indicator, number
of previous live births, number of previous still births, single/multiple birth status, and number of days enrolled
during the perinatal period. Also included in the model as covariates were indicators for previous cesarean
section, pre-pregnancy diabetes and hypertension, preterm birth, and infections — chlamydia, gonorrhea,
syphilis, or hepatitis B/C — at time of birth. A propensity score was created for each observation to identify the
probability of a delivering mother covered by a QHP (1) or Medicaid (0).
Mothers covered by Medicaid and a QHP were matched, one to one, by their propensity score of program
assignment. Similar to the process used in the findings for the General Population, this was performed using a
greedy matching algorithm.
39
Crude covariate category values used in the matching and the subsequent matched
sample values are summarized in Appendix I, along with calculation of standardized differences between
Medicaid and QHP groups prior to and after matching. The bias reduction associated with matching is also
presented. In total, our analytic population contains 2,369 birth outcomes in each of the matched mother pairs
from Medicaid and QHP programs.
Statistical Approach
Prenatal visits were measured as a count outcome variable. Time to first visit was measured as a continuous
outcome variable. Frequency distributions for all outcomes under study are included in Appendix I.
Dichotomous maternal quality outcome measures of interest (yes/no responses) included pre-birth
hospitalization for preeclampsia, gestational diabetes, or any reason, and delivery by cesarean section.
Dichotomous birth quality outcome measures of interest (yes/no responses, unless otherwise indicated) included
preterm birth, low birth weight, abnormal outcomes (combined measure of all abnormal indicators, including
meconium), APGAR5 (very abnormal vs. other and any abnormal vs. other), and neonatal intensive care unit
(NICU) stay after birth.
Individual generalized linear models were fit regressing a Medicaid/QHP dichotomous primary independent
indicator on the outcomes of interest. A random variable indicating the matched Medicaid-QHP dyad was also
included. The distribution of the outcome determined the type of regression used. For dichotomous outcomes a
generalized logistic regression was utilized and adjusted odds ratios were reported for the differences between
matched Medicaid and QHP maternal and birth outcomes. For count variables, a generalized Poisson regression
model was utilized and incidence rate ratios reported. For continuous variable outcomes, generalized normal
regression models were utilized with marginal effect sizes reported.
Findings
Tables 20 and 21 contain the results of fitting generalized linear regression models on the matched Medicaid/QHP
data described above.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 46
Table 20. Maternal Pregnancy Differences between Medicaid and QHP Enrollees
Maternal Pregnancy Outcomes
Comparison of Programs
Continuous
Outcomes
Measure
Medicaid (N=2,369)
Mean (StdDev)
QHP (N=2,369)
Mean (StdDev)
Marginal Effect
(95 percent CI)
Time to First Prenatal
Visit
Days
90.81 (49.80)
81.89 (43.79)
-8.71 (-11.62 to -5.80)
Count Outcomes
Measure
Medicaid
Mean (StdDev)
QHP
Mean (StdDev)
Incidence Rate Ratio
(95 percent CI)
Prenatal Visits
Visits
10.55 (3.85)
11.00 (3.81)
0.420 (0.222-0.619)
Dichotomous
Outcomes
Category
Medicaid (N=2,369)
n (percent)
QHP (N=2,369)
n (percent)
Adjusted Odds Ratio
(95 percent CI)
Preterm Hospitalization
(preeclampsia)
Yes vs. No
69 (2.91)
77 (3.25)
1.121 (0.805-1.562)
Preterm Hospitalization
(gestational diabetes)
Yes vs. No
50 (2.11)
50 (2.11)
1.000 (0.667-1.498)
Preterm Hospitalization
(any reason)
Yes vs. No
225 (9.50)
201 (8.48)
0.885 (0.728-1.079)
Cesarean Birth
Yes vs. No
1,008 (35.17)
1,007 (35.14)
0.999 (0.897-1.111)
Notes: Marginal effect < 0 and confidence interval not containing 0 indicate less time to first visit for QHP. Incident rate ratio > 0
and confidence interval not containing 0 indicate higher number of visits for QHP. Adjusted odds ratios > 1 and confidence
interval not containing 1 indicate a higher rate for QHP.
Abbreviations: QHP=Qualified Health Plan; StdDev=Standard Deviation; CI=Confidence Interval
On average, pregnant women with QHP coverage had a prenatal visit 8.7 days sooner than similarly matched
women who were covered with Medicaid insurance. In addition, QHP-covered women had, on average, 0.4 more
prenatal visits than similarly matched women with Medicaid over the course of a pregnancy.
Table 21. Pregnancy Birth Outcomes between Medicaid and QHP Enrollees
Pregnancy Birth Outcomes
Comparison of Programs
Dichotomous
Outcomes
Category
Medicaid
N (percent)
QHP
N (percent)
Adjusted Odds Ratio
(95 percent CI)
Preterm Births
Preterm vs. Normal
183 (7.72)
214 (9.03)
1.189 (0.966-1.463)
Low Birth Weight
Yes vs. No
196 (8.16)
224 (9.33)
1.079 (0.882-1.321)
Abnormal Outcome
Yes vs. No
144 (6.00)
155 (6.46)
1.079 (0.851-1.369)
APGAR5 1
Very abnormal vs. other
33 (1.38)
36 (1.51)
1.096 (0.875-1.780)
APGAR5 2
Any abnormal vs. other
121 (5.04)
117 (4.88)
0.985 (0.756-1.283)
NICU
Yes vs. No
158 (6.58)
159 (6.63)
1.010 (0.799-1.276)
Notes: Adjusted odds ratios > 1 and confidence interval not containing 1 indicate a higher rate for QHP.
Abbreviations: QHP=Qualified Health Plan; CI=Confidence Interval
Based on matched Medicaid and QHP birth outcomes, our results did not detect any statistically significant
differences in rates of preterm births, low birth weight deliveries, abnormal outcomes, APGAR scores at any
abnormal cut-point, or NICU stays.
Discussion
Except for small differences in prenatal care — one additional visit with initiation approximately one week
earlier — no variation in maternal, delivery, or birth outcomes were observed between women in the
traditional Medicaid program and those with premium assistance in the QHPs.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 47
This finding may be reflective of Medicaid being the source of coverage for the majority of births within the
state — over 50 percent of births covered by Medicaid prior to 2014. In addition, the lack of variation in
chlamydia screening between Medicaid and QHPs — at least in the General Population, noted in Table 7, and in
favor of Medicaid in Year 3 for the Higher Needs Population, depicted in Table 14 — supports the influence of the
Medicaid quality improvement programs over time. These improvement projects and programs have included
focused efforts to increase prenatal visits and screening rates, care coordination and telemedicine support for
high-risk pregnancies, and value-based payment strategies shared with the private sector through the Arkansas
Healthcare Payment Improvement Initiative.
There are limitations to this study, including those previously mentioned involving the lack of detailed claims for
bundled provider payments. There is also not a perfect overlap in income eligibility across Medicaid and QHP
commercial programs. Medicaid covers previously uninsured women (or transition from pre-existing Medicaid aid
categories) with incomes up to 200 percent of FPL, while those receiving coverage in a premium-assisted QHP have
maximum incomes of 138 percent of FPL. To address this, we performed a sensitivity test on all maternal and birth
outcomes where the analytic population was restricted to just those who were WIC recipients during pregnancy.
WIC eligibility is capped at women who earn 185 percent of FPL, thus producing a slightly more balanced distribution
on income levels between Medicaid and QHP enrollees. There were no changes in the findings when analyses were
restricted to WIC beneficiaries (data not shown). On many demographic and geographic variables, the Medicaid and
QHP study populations are also already very similar, or balanced (Appendix I).
Non-Emergency Medical Transportation
Overview
As a required covered benefit within Medicaid, but not a component of the Essential Health Benefit (EHB) in QHP
coverage, non-emergency medical transportation (NEMT) was the most frequent wrapped service for QHP
enrollees. As required in the waiver, and subsequently stated in the research design, availability and accessibility
of NEMT services for QHP enrollees was a concern. Hypothesis 1e: HCIP beneficiaries will have equal or better
access to non-emergency transportation compared with what they would have otherwise had in the Medicaid fee-
for-service system over time.
In the Interim Report
5
— and based on self-reported responses to the first CAHPS survey — we found that within
the Higher Needs population, Medicaid enrollees had more problems accessing NEMT compared to QHP enrollees
during Program Year 1. There were no self-reported differences in access within the General population.
Data Source and Analytic Population
Using the results from a second CAHPS survey (CAHPS II) that elicited self-reported responses from respondents
who had approximately 18 months of continuous coverage, General Population and Higher Needs Population
results from CAHPS II are presented for Medicaid and QHP comparison group NEMT responses. Enrollees were
asked about transportation barriers for visits to both personal doctors and specialists.
Statistical Approach and Findings
Tables 22 and 23 present a statistical chi-square test of association, and a propensity score matched analysis for
Medicaid and QHP enrollees in the General Population for responses to each of the two non-emergency
transportation questions. Tables 24 and 25 present a statistical chi-square test of association, and a regression
discontinuity analysis for Medicaid and QHP enrollees in the Higher Needs Population for responses to each of the
two non-emergency transportation questions.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 48
Table 22. Differences in Non-Emergency Transportation between General Population Medicaid and
QHP Enrollees
Medicaid
QHP
Perceived Access Indicators
N
Mean
(StdErr)
N
Mean
(StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Percentage of enrollees who did not miss a visit to
a personal doctor due to lack of transportation
194
89.2 (2.2)
641
81.1 (1.5)
-9.1
0.002
Percentage of enrollees who did not miss a visit to
a specialist due to lack of transportation
89
89.9 (3.2)
340
88.4 (1.7)
-1.7
0.103
Notes: Data were obtained from CAHPS II responses. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100. Statistical
difference was concluded from a chi-square test of association.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
In a direct comparison of responses to NEMT questions, a higher percentage of Medicaid enrollees (89.2 percent),
compared to QHP enrollees (81.1 percent), indicated that they did not miss a visit to a personal doctor due to lack
of transportation.
Table 23. Differences in Non-Emergency Transportation between Medicaid and QHP Enrollees
(Propensity Score Matched Comparison)
Non-Emergency Transportation Indicators
Matched
N
Medicaid
Mean (StdErr)
QHP
Mean
(StdErr)
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Percentage of enrollees who did not miss a visit to a
personal doctor due to lack of transportation
181
90.1 (2.2)
87.8 (2.4)
-2.5
0.501
Percentage of enrollees who did not miss a visit to a
specialist due to lack of transportation
78
93.6 (2.8)
92.3 (3.0)
-1.4
0.295
Notes: Data were obtained from CAHPS II responses. Adjusted analysis was performed using a propensity score matched sample.
Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: Matched N=number of Medicaid and QHP matched enrollees; StdErr=standard error of estimated mean.
When General Population Medicaid and QHP enrollees are matched for the comparison of differences, the crude
results reported in Table 23 for personal doctors attenuate, and we find no evidence that access to NEMT is
different across enrollee groups.
Table 24. Differences in Non-Emergency Transportation between Higher Needs Population Medicaid
and QHP Enrollees
Medicaid
QHP
Relative
Difference
(percent)
Statistical
Difference
(p-value)
Non-Emergency Transportation Indicators
N
Mean
(StdErr)
N
Mean
(StdErr)
Percentage of enrollees who did not miss a visit to
a personal doctor due to lack of transportation
868
82.2 (1.3)
972
91.9 (0.9)
11.7
0.002
Percentage of enrollees who did not miss a visit to
a specialist due to lack of transportation
533
75.5 (1.9)
560
95.2 (0.9)
26.1
0.084
Notes: Data were obtained from CAHPS II responses. Adjusted analysis was performed using a chi-square test of association. Average
treatment effect depicts model-estimated difference at cut-point. Relative percent calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
In a direct comparison of responses to NEMT indicators, a higher percentage of QHP enrollees (91.9 percent),
compared to Medicaid enrollees (82.2 percent), indicate that they did not miss a visit a personal doctor due to
lack of transportation.
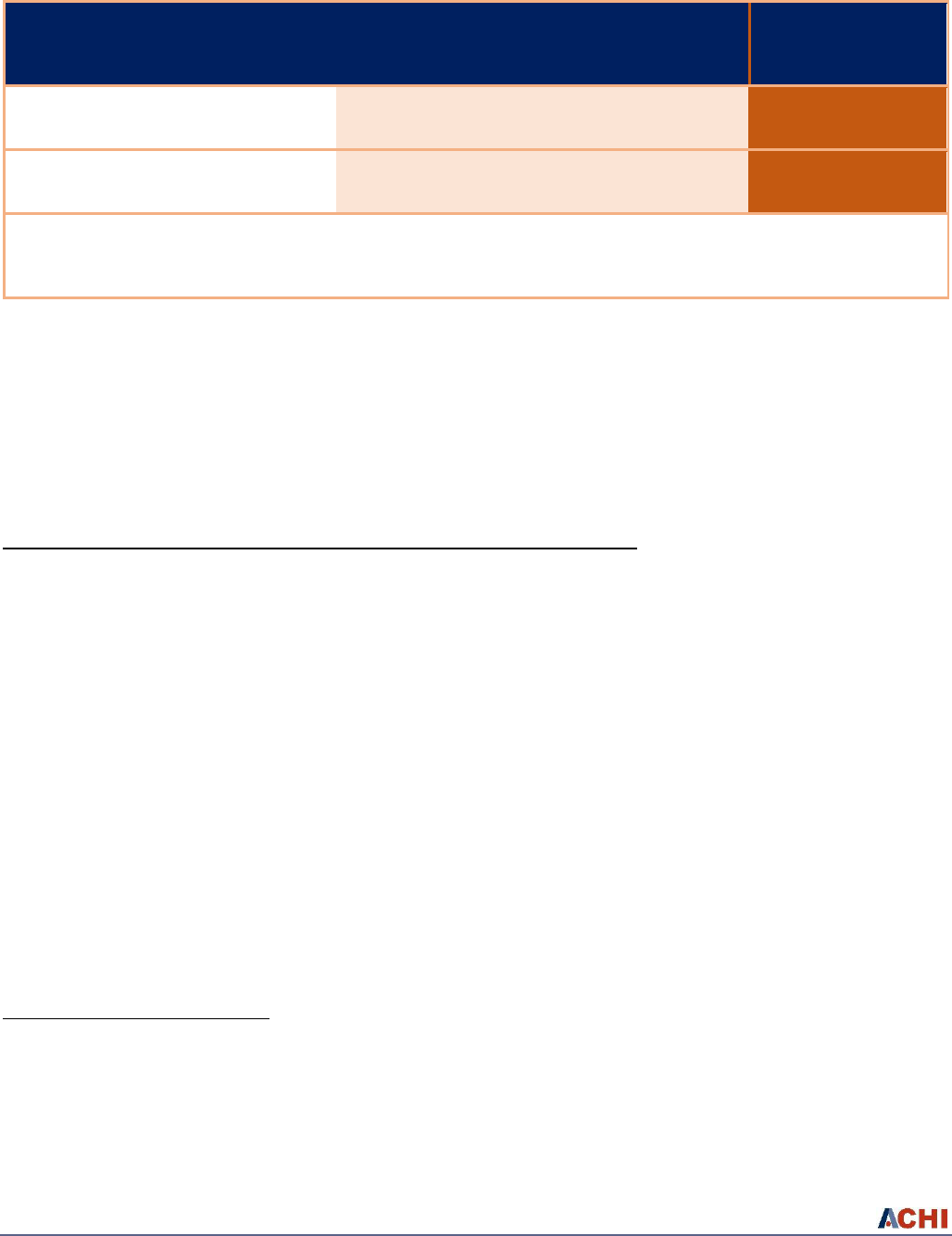
Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 49
Table 25. Differences in Non-Emergency Transportation between Medicaid and QHP Enrollees
(Regression Discontinuity Comparison)
Medicaid
QHP
Relative
Difference
(percent)
Average
Treatment
Effect
(percent)
Statistical
Difference
(p-value)
Non-Emergency Transportation Indicators
N
Mean
(StdErr)
N
Mean
(StdErr)
Percentage of enrollees who did not miss a
visit to a personal doctor due to lack of
transportation
884
83.0 (1.3)
983
87.9 (1.0)
5.9
-15.0
0.005
Percentage of enrollees who did not miss a
visit to a specialist due to lack of
transportation
544
87.1 (1.4)
564
90.4 (1.2)
3.8
-8.2
0.159
Notes: Data were obtained from CAHPS II responses. Statistical analysis was performed using regression discontinuity with a model-
derived optimal bandwidth around an exceptional needs screener cut-point. Average treatment effect depicts model-estimated
difference at cut-point. Relative percentage calculated as (QHP – Medicaid)/Medicaid x 100.
Abbreviations: N=number of Medicaid and QHP enrollees; StdErr=standard error of estimated mean.
Using a more robust evaluation design with regression discontinuity, we find evidence to confirm that 15.0 percent more
QHP enrollees, compared to Medicaid enrollees, did not miss a visit to a personal doctor due to lack of transportation.
Our findings from the second CAHPS survey indicate that for the Higher Needs population, lack of NEMT is still
more problematic for Medicaid enrollees than for QHP enrollees. This is evidenced even more for those around
the exceptional healthcare needs composite score cut-point, where we would expect no reasonable differences to
be caused by Medicaid or QHP program assignment.
Early and Periodic Screening, Diagnostic, and Treatment (Medicaid Benefit)
Overview
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) is a required benefit that provides comprehensive
and preventive healthcare services for children and adolescents under 21 who are enrolled in Medicaid. With
expansion, through premium assistance under the HCIP, 19- and 20-year-olds were placed in the QHP and received
the Essential Health Benefit (EHB). Examination of the structure of the EHB determined that the Early and Periodic
Screening and Diagnostic (EPSD) tests would be similarly covered. However, concern over the breadth of potential
treatments available under EPSDT and the definition of commercial coverage within the EHB was a component of
the waiver and the stated hypothesis in the research design. Hypothesis 1d: HCIP beneficiaries will have equal or
better access to EPSDT benefit access for young, eligible adults compared with what they would have otherwise had
in the Medicaid fee-for-service system over time (see Appendix B).
To approach this hypothesis, key informants who manage complex Medicaid-enrolled children and young adults
were consulted.
b
Concurrence on the overlap in EPSD services was provided and no recognized treatment deficits
in QHP coverage over the program’s initial three years was reported by our key informants.
b
Dr. Charles Field, former Division Director of Community Pediatrics and Professor in the Department of Pediatrics, University
of Arkansas, Arkansas Head Start Board Member, and clinician at Mid-Delta Community Health Center; Dr. Eldon Shultz, Eldon
G. Schulz, M.D., FAAP, Rockefeller Professor and Endowed Chair for Children with Special Needs, Section Chief, Developmental-
Behavioral and Rehabilitative Pediatrics, Medical Director, Arkansas Children’s Hospital Rehabilitative Services, and Medical
Director, Arkansas Developmental Disabilities Services; and Dan Knight, MD, Chairman of the Department of Family and
Preventive Medicine, and Associate Professor at the University of Arkansas for Medical Sciences.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 50
To further investigate the potential for treatment restrictions, we designed a pre- and post-enrollment
assessment comparing children enrolled in Medicaid as 17- and 18-year-olds, who were subsequently potentially
eligible for HCIP assignment to a QHP. To assess program treatment differences, we selected conditions that were
immutable and had the potential for intense medical treatment needs, as well as conditions and treatments that
would be traceable in both Medicaid and QHP claims. With support from our key informants, we selected sickle-
cell disease, cystic fibrosis, and hemophilia.
Data Source and Analytic Population
From Medicaid enrollment files, all 17- and 18-year-old children with Medicaid coverage in 2013 were identified. We
employed Medicaid claims files from 2013 to identify children who received health care in 2013 to treat a condition
of sickle cell disease, cystic fibrosis, or hemophilia. The premise was that these three conditions would require
specialized chronic care and disease management into young adulthood. We identified 151 Medicaid beneficiaries
who met one of these three conditions and were 17 or 18 years old. These individuals were then tracked to assess
coverage status as well as variations in treatment when they turned 19 and 20, in 2014 and 2015, respectively.
Findings
Efforts to track these 151 individuals into their nineteenth and twentieth year were largely successful. Through
Medicaid programmatic aid categories — including Supplemental Security Income (SSI) disability and the Tax Equity
and Fiscal Responsibility Act (TEFRA), otherwise known as “Katie Beckett options” — combined with the frailty screener
that directed expansion population members with higher needs into the traditional Medicaid-managed population, a
large majority (86.7 percent) of these individuals remained on Medicaid and were not assigned to a QHP.
Table 26 presents the number of beneficiaries who were still in Medicaid in the month following their nineteenth
birthday, as well as the associated aid category and a description of the program under which they were covered.
In total, 131 of the 151 adolescents (86.8 percent) were still enrolled in a Medicaid aid category with access to a
Medicaid in-network specialist provider.
Table 26. Health Insurance Carrier at 19 Years of Age for Medicaid Screened and Diagnosed Sickle Cell
Disease, Cystic Fibrosis, or Hemophilia (n=151)
Type of Health Insurance
Enrolled
Medicaid
131
SSI (aid category 43/45)
67
Adult Expansion (aid category 06 “Frail”)
49
Other, including AFDC Grant (aid category 20), Non-Medicaid (aid
category 04), Pregnant (aid category 61), TEFRA (aid category 49)
15
Not found in either Medicaid or QHP enrollment categories
<20
Enrolled in QHP
<5
Due to the scarcity of transition from Medicaid to QHP premium assistance, no comparative analyses were
achievable. Given the success of programmatic retention in existing aid categories for these individuals in
traditional Medicaid and the frailty screener’s sensitivity in identification of higher needs, this concern is
effectively non-existent. The established programmatic pathway for an individual to transition from QHP to
Medicaid management based on a medical assessment of frailty further allays concerns. However,
modification of the frailty screener to a single question at the time of application may warrant reassessment
in the future.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 51
Continuity of Care
Overview
One form of churn is through gaps in continuous health insurance coverage, when individuals go off coverage and
come back on after a short period of time. Churn can impact health from missed care during the time period when
the individual was uninsured. It can also leave individuals with high medical costs during the uncovered period.
As previously noted, under an alternative demonstration of the implementation of the ACA, the Arkansas adult
Medicaid expansion uses premium assistance to purchase commercial insurance in the Marketplace. Program
income eligibility in the Health Care Independence Program (HCIP) is up to 138 percent of the federal poverty
level. Shore-Sheppard
40
demonstrated that income can be highly variable from month to month in this low-
income range. Depending on eligibility and redetermination (a process through which income eligibility
determination to remain in the program is updated) periods, individuals eligible for coverage under state -
level Medicaid expansion earning at or less than 138 percent FPL in one month may cross the income
eligibility threshold in a subsequent month — strictly due to a temporary fluctuation in the number of hours
worked that month.
For low-income individuals, there are a number of programs through which they can churn eligibility on or off
simply by crossing a threshold. The traditional Medicaid eligibility in Arkansas is for parents earning at or less than
17 percent FPL; the HCIP threshold is up to 138 percent FPL; and individuals earning up to 400 percent FPL can
enter the Marketplace (with a number of gradients determining individual out-of-pocket premiums and tax
credits). Seamless churning between these programs requires careful application coordination. Another adult
Medicaid expansion population in Arkansas consists of those who were determined to have exceptional
healthcare needs (i.e., “Frail”) after completing a screener (06 Medicaid). Individuals can also churn in and out of
this program.
It was anticipated that churning within state-level ACA adult Medicaid expansions would be problematic, with
some estimates predicting that churn would affect 50 percent of enrollees during the first year.
41
,
42
One factor
that potentially limited the churn effect for the premium assistance HCIP expansion population in Arkansas, was
that commercial carriers received guaranteed monthly premiums to cover individuals enrolled in the HCIP. As
such, QHPs had a stake in retaining members through outreach during periods of redetermination or simply due
to upward-income mobility. Enrollees could also be retained with the same QHP coverage, but through a tax
credit-subsidized plan on the Marketplace. The result was a lower rate of churn for the insured ACA expansion
population.
More than 95 percent of those initiating premium assistance coverage in a QHP in 2014 maintained coverage
through December of that year.
5
In this report we follow the continuity of coverage, attrition, and churn for the
entire three-year period within the HCIP program. While the start-up period in 2014 included a number of system-
related challenges, those who enrolled during that year and the first six months of 2015 were not subject to
redetermination.
Due to current data limitations, we are unable to track the HCIP expansion population systematically into the
subsidized Marketplace if they leave the HCIP coverage. Therefore we cannot capture potential upward-income
mobility and subsequent insurance coverage into the Marketplace or into employer-sponsored insurance
programs. The Arkansas Center for Health Improvement (ACHI) is working on compiling a customized analytic
database from the Arkansas All-Payer Claims Database (APCD) to track individual insurance coverage across
insurance carriers and identify periods without insurance through machine learning.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 52
In this study, we profile those who enrolled and maintained enrollment in an HCIP QHP or were assigned to Aid
Category 06 of Medicaid coverage by virtue of being determined to have exceptional healthcare needs. We focus
on these two groups during three periods of distinct enrollment and retention processing by Arkansas Medicaid.
The first is an 18-month pre-redetermination period where income eligibility updating was not effectuated. This
was followed by a universal redetermination period that began in July 2015, when all QHP enrollees would have
been subjected to this process, likely for the first time. Finally, we study continuity of coverage, attrition, and
churn in 2016, when a regular monthly process of redetermining groups of enrollees based on individual
enrollment month for income eligibility was reinstated.
Data and Methodology
Data for these analyses came from the Arkansas Medicaid premium payment database. The data contained
indicators for the following: each member enrolled, each month a premium assistance premium was paid to a
QHP, and whether or not each individual was a member of the 06 Medicaid category for that month.
Program Enrollment History
Over the three-year course of HCIP, 399,330 individuals secured health insurance coverage in a QHP or through
the 06 Medicaid category for at least one month. Many who entered the program stayed on through December
2016, as evidenced by 247,579 individuals maintaining continuous coverage with a QHP and 18,660 individuals
maintaining continuous 06 Medicaid coverage from the point at which they enrolled in the program.
Figure 9 depicts enrollment in the start-up month of January 2014 and the steady growth in the number of those
insured over 36 months of the HCIP. The continuous growth in enrollment was only interrupted by the universal
redetermination in July 2015.
Figure 9. Health Care Independence Program Enrollment by Program and Month
Continuity of Coverage During Pre-Redetermination Months
As previously stated, approximately 95 percent of individuals who received health insurance through a QHP
retained continuous coverage in the first year of the program. From January 2014–June 2015, no systematic
redetermination of eligibility was conducted on adults enrolled in the HCIP program or in 06 Medicaid. In June
2015, prior to redetermination, 216,870 Arkansas adults were enrolled in a QHP, while an additional 25,733
expansion adults were retained in 06 Medicaid after being identified as having exceptional healthcare needs.
Table 27 profiles the pre-redetermination enrollment history of these two groups.
0
50,000
100,000
150,000
200,000
250,000
300,000
350,000
Enrolled
Enrollment Month
QHP 06 Medicaid

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 53
Table 27. Medicaid Enrollment History of QHP and 06 Medicaid Individuals Enrolled in June 2015
Enrolled in QHP in June 2015
N=216,870
Percent=100
Continuous Enrollment
213,879
98.6
Experienced at Least one QHP-to-QHP Gap Month
2,167
1.0
Experienced an 06-Medicaid-to-QHP Transition (Seamless)
470
0.2
Experienced an 06-Medicaid-to-QHP Transition (with Gap)
354
0.2
Enrolled in 06 Medicaid in June 2015
N=25,733
Percent=100
Continuous Enrollment
24,525
95.3
Experienced at Least one 06-Medicaid-to-06-Medicaid Gap Month
39
0.1
Experienced a QHP-to-06-Medicaid Transition (Seamless)
1,093
4.3
Experienced a QHP-to-06-Medicaid Transition (with Gap)
76
0.3
Overwhelmingly, in the absence of redetermination, those who were enrolled in a QHP in June 2015 did not
experience a gap in coverage (98.6 percent) since enrollment (up to 18 continuous months). Only 1.0 percent of
QHP enrollees enrolled in June 2015 had a gap in coverage of one or more enrollment months. A very small
number of enrollees churned between 06 Medicaid and a QHP (0.4 percent), with the majority having a seamless
transition without a gap in health insurance coverage.
For those determined to have exceptional healthcare needs and assigned to 06 Medicaid and were in the program in
June 2015, 95.3 percent experienced continuous coverage. Another 4.3 percent had seamless coverage — albeit
interrupted with a switch from a QHP to 06 Medicaid coverage.
There was a modest amount of attrition from the respective programs. A total of 9,907 individuals had been
enrolled in a QHP, and 2,364 individuals had been enrolled in 06 Medicaid, in one of the 17 months prior to June
2015, but were not enrolled in either program in June 2015. A small number of 82 individuals had experienced a
switch between programs and were not enrolled in either program in June 2015.
Impact of Redetermination
In this analysis, QHP and 06 Medicaid enrollees who received a notice of redetermination in July 2015 are profiled
to identify the impact on continuity of coverage within both programs. We focus on any gap in coverage during
the three months after July 2015. In July 2015, 222,282 Arkansas adults were enrolled in a QHP, while an
additional 25,930 expansion adults were retained in 06 Medicaid. Table 28 tracks the enrollment of these two
groups through the redetermination period.
Table 28. The Impact of Redetermination on QHP and 06 Medicaid Enrollees (Enrolled in July 2015)
Status of QHP Enrollees in November 2015
N=222,282
Percent=100
Continuous Enrollment
179,426
80.7
Gap Period of One to Three Months, Enrolled in QHP in November 2015
5,072
2.3
QHP-to-06-Medicaid Transition (Seamless), Enrolled in QHP in November 2015
<11
0.0
QHP-to-06-Medicaid Transition (with Gap), Enrolled in QHP in November 2015
<11
0.0
Not Enrolled in November 2015
37,765
17.0
Status of 06 Medicaid Enrollees in November 2015
N=25,930
Percent=100
Continuous Enrollment
20,590
79.4
Gap Period of One to Three Months, Enrolled in QHP in November 2015
776
3.0
06-Medicaid-to-QHP Transition (Seamless)
<11
0.0
06-Medicaid-to-QHP Transition (with Gap)
<11
0.0
Not Enrolled in November 2015
4,552
17.6
Redetermination affected 2.3 percent of QHP enrollees with a gap in coverage of one to three months. Very few
individuals were reassigned from a QHP to 06 Medicaid coverage. Of the 37,765 that were not back in a QHP by

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 54
November 2015, we were able to identify (data not shown) that 25,999 individuals (68.8 percent) were
subsequently not enrolled in a QHP or in 06 Medicaid during any period in 2016. Of the 11,766 individuals who
were re-enrolled with QHP or 06 Medicaid coverage in 2016, 6,559 individuals (55.7 percent) were back on in the
first six months of the year. The numbers are similar for the 4,552 06 Medicaid enrollees who lost coverage during
a month impacted by redetermination. A total of 3,293 individuals (72.3 percent) were not enrolled in a QHP or
with 06 Medicaid coverage in 2016.
Continuity of Care in the Post-Redetermination Period
Of the 399,330 individuals who were ever enrolled in a QHP or 06 Medicaid program during the first two HCIP
program years, only 45,387 individuals (11.4 percent) were not enrolled for any time period during 2016. This is a
strong indication of continuity in the program. Following the universal July 2015 redetermination, regular monthly
intervals of redetermination based upon month of birth were re-instituted. For this reason, it is expected that
more frequent gaps in coverage could be observed in 2016.
In 2016, a total of 353,943 individuals were covered in a QHP or in 06 Medicaid at some point in time. This
includes those who had been on the program continuously, those who re-enrolled in 2016 after a gap period of
being uninsured, and those who were covered by a non-HCIP program or were uninsured.
Table 29 presents continuity of coverage and transitions for those in the HCIP program in 2016.
Table 29. HCIP Enrollment History of Individuals Enrolled in HCIP During 2016
Enrolled in QHP in December 2016
N=327,739
Percent=100
Continuous Enrollment
269,091
82.1
Gap in 2016 Coverage, Still Enrolled in December 2016
6,457
2.0
06-Medicaid-to-QHP Transition (Seamless), Still Enrolled in December 2016
464
0.1
06-Medicaid-to-QHP Transition (Gap), Still Enrolled in December 2016
69
0.0
Not Enrolled in December 2016
51,658
15.8
Enrolled in 06 Medicaid in December 2016
N=26,204
Percent=100
Continuous Enrollment
20,781
79.3
Gap in Coverage, Still Enrolled in December 2016
486
1.8
QHP-to-06-Medicaid Transition (Seamless), Still Enrolled in December 2016
191
0.7
QHP-to-06-Medicaid Transition (Gap), Still Enrolled in December 2016
15
0.0
Not Enrolled in December 2016
4,731
18.1
The continuous monthly redetermination process did not change the percentage of enrollees maintaining
continuous coverage through 2016. We were unable to ascertain at this time if the attrition observed in 2016 was
due to enrollee-initiated action (i.e., obtaining employer-sponsored insurance) or as a result of redetermination.
Future Analyses
Of the 45,387 individuals (11.4 percent) enrolled in the first two years of the HCIP program, but who were not
enrolled in Program Year 3 (2016), it is unknown whether or not these individuals were eligible but failed to re-
enroll, out-migrated from the state, had an upward change in income status (enabling participation in the
Marketplace) or being employed and obtained insurance through their employer. Through the Arkansas All-Payer
Claims Database — with its unique “hashed” identifier — and the state’s hospital and emergency room discharge
databases, future studies tracking individuals’ longitudinal coverage status is possible. In addition, waiver requests
under consideration by CMS will offer quasi-experimental opportunities to test alternative coverage strategies
and their impact on churn.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 55
Health Independence Accounts
Overview
The Arkansas Health Care Independence Act of 2013 (Ark. Code Ann. § 20-77-2405 (j)) — known as the “Private
Option” — established authority for the state’s Section 1115 waiver for the Medicaid expansion population. The
Act contained language requiring the development and implementation of “health savings or independence
accounts” with required participation by non-aged, non-disabled program-eligible participants. Following waiver
approval and initiation of the Private Option in 2014, the state developed and received federal approval to
implement Health Independence Accounts (HIAs), named MyIndyCards, at the initiation of Program Year 2
(January 2015) for individuals between 100 and 138 percent of the federal poverty level (FPL).
Program Design
Design of the HIAs was to serve as a mechanism to provide protection from cost-sharing, promote appropriate
healthcare utilization, and offer a mechanism to enable savings for future potential premium exposure. All
individuals in qualified health plans (QHPs) between 100 and 138 percent FPL were required to participate and
contribute, or generate a debt to the state (i.e., $10 a month for those earning 100 to 117 percent FPL and $15 a
month for those earning 118 to 138 percent FPL).
Contribution to the HIA in one month resulted in state-funded cost-sharing protection for the following month.
Initial activation of an HIA gained two months’ cost-sharing protection before monthly contributions were
required to maintain cost-sharing coverage. The state debited the HIA balance for a failed payment in a given
month. The state matched the individual’s contribution up to $200, if timely payments were made, and balances
were allowed to roll over annually. Finally, funds were available for premium payments in the marketplace upon
exit from the HIA program.
Data Sources and Analytic Population
We profiled the programmatic experience of the Arkansas HIAs, assessed the characteristics of participating
individuals, and evaluated the financial impact of the HIAs on individuals and on the program.
Data from the 2014 enrollment files for Private Option beneficiaries between 100 to 138 percent FPL and claims
data from QHPs from 2014-2016 were used for this analysis. In addition, third-party HIA transactions for both
payment collection and distribution were employed.
In total, 57,079 individuals were eligible for HIA participation. Demographic characteristics, including age, gender,
race/ethnicity, and rural/urban status, were combined with 2014 claims experience for hospitalizations,
emergency room utilization, and the Charlson Comorbidity Index to profile eligible participants.
Statistical Approach
Outcomes assessed included: initiation of payments; contribution frequency and amounts; cost-sharing protection
received; relative contribution compared to cost-sharing protection of participants both in the aggregate and
individually; and participant contributions compared to programmatic administrative costs. Statistical significance
was assessed using chi-square assessments.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 56
Findings
Of eligible participants (N=57,079) during the 16-month program, only 7,072 individuals (14.1 percent)
contributed at least one valid monthly payment after receiving the card and received cost-sharing protection for
the following month. Table 30 presents a demographic profile of the Health Independence Accounts eligible
population by those who made no payments or made at least one payment.
Table 30. Health Independence Account Eligible Population Demographic Profile
Made No Payments
Made at Least One Payment
Category
N (Percent)
N (Percent)
Total
Age (Years)
19-34
24,154 (48.3)
1,508 (21.3)
25,664 (45.0)
35-49
14,279 (28.9)
1,954 (27.6)
16,233 (28.4)
50-64
11,572 (23.1)
3,610 (51.1)
15,182 (26.6)
Gender
Male
20,130 (40.3)
2,831 (40.0)
22,961 (40.2)
Female
29,877 (59.8)
4,241 (60.0)
34,118 (59.8)
Race / Ethnicity
White
32,073 (64.1)
4,400 (62.2)
36,473 (63.9)
Black
7,595 (15.2)
1,050 (14.9)
8,645 (15.2)
Hispanic
1,865 (3.7)
324 (4.6)
2,189 (3.8)
Other
8,474 (17.0)
1,298 (18.4)
9,772 (17.1)
Total
50,007 (85.9)
7,072 (14.1)
57,079 (100)
Those who made payments were disproportionately older
(Table 32) and have more comorbidities (Figure 10).
Compared to non-paying individuals, those making payments
were more likely to have prior hospitalizations (7.1 percent vs.
5.1 percent), but less likely to have had an emergency room
visit (25.7 percent vs. 27.7 percent; p0.0001, data not shown).
No differences in participation were observed for racial or
gender strata or for individuals in the 100-to-117 percent FPL
group ($10/month) compared to the 118-to-138 percent FPL
group ($15/month).
For the 7,072 who contributed, their monthly contributions
totaled $426,670 during the 18-month period — median of
$40 or four months’ payments (interquartile range $15, $90)
and mean of $60 (standard deviation $141) or six months of
payments. Cost-sharing protections totaled $476,843, with a
majority of the protection being for pharmaceutical
copayments (see Table 31).
Table 31. Health Independence Accounts Cost-Sharing Expenditures
Type
Transactions
Percent
Amount ($)
Pharmaceuticals
31,805
61.2
$289,522
Physician
9,198
17.7
$79,482
Non-MD Clinician
7,339
14.1
$59,095
Hospitals
2,884
5.6
$41,744
Other
710
1.4
$7,000
Total
51,936
100
$476,843
Figure 10. Charlson Comorbidity Index by Health
Independence Account Non-Participants (Made
No Payment) vs. Participants (Made Payment)

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 57
Cost-sharing protections exceeded HIA payments by $50,172. Cost-avoidance — an individual’s copayment
protections exceeding their payments — was realized by 23.4 percent of participants. Administrative costs to
maintain program and accounts were approximately $9 million throughout the program duration of 18 months.
Postlude
The HIAs were terminated by the Arkansas General Assembly in the 2
nd
Extraordinary Session of 2016. (Ark. Code
Ann. § 20-77-2408). There was no evidence of individuals directly utilizing account balances during the program
for private-sector premium payments. Upon termination of the program, individuals with account balances
(N=2,253) received program termination checks.
Medicaid and QHP Opioid Utilization Outcomes
Overview
Over the last decade, the United States has seen a significant rise in opioid overdose deaths and prescriptions — a
fivefold increase in prescription opioid overdose deaths and a fourfold increase in the sale of prescription
opioids.
43
Arkansas is no stranger to this epidemic. In 2016, Arkansas had the second highest rate of opioid
prescriptions nationally at 114.6 prescriptions per 100 persons.
44
While Arkansas has not yet seen the volume of
opioid overdose deaths seen in other states, trends indicate that Arkansas could soon approach those levels
absent intervention.
In an effort to address the issue, the Arkansas General Assembly has enacted legislation on multiple fronts.
1. In 2011, the state authorized a prescription drug monitoring program (PDMP) to enhance patient care by
ensuring legitimate use of controlled substances.
45
2. In 2015, the state established immunity for individuals seeking medical assistance during a drug overdose and
for healthcare professionals for administering, prescribing, or dispensing naloxone, which is used to treat a
narcotic drug overdose.
46
,
47
3. In 2017, Arkansas joined 38 other states that require prescribers to check the PDMP prior to prescribing
certain controlled substances.
48
In March 2016, the Centers for Disease Control and Prevention (CDC) issued guidelines
44
for primary care clinicians
for prescribing opioids for chronic pain outside of cancer treatment, palliative care, and end-of-life care. The
guidelines recommended non-opioid therapy as the preferred method for treatment of chronic pain. However,
when opioids are used, the CDC recommended that clinicians should prescribe the lowest effective dosage, assess
risks when considering increasing dosage to 50 morphine milligram equivalents (MMEs) or more per day, and
avoid concurrent opioids and benzodiazepines.
In response to a 2016 memo from the Centers for Medicare & Medicaid Services (CMS)
49
indicating that
“Medicaid beneficiaries are prescribed painkillers at twice the rate of non-Medicaid patients and are at three-to-
six times the risk of prescription painkillers overdose,” Arkansas Medicaid implemented best practices cited in the
memo as its new policy. Arkansas has also issued guidelines for emergency department opioid use, and, most
recently, the state has launched an effort to educate doctors on pain management in an effort to curb opioid
misuse and abuse.
Given the high rates of opioids prescribed in Arkansas, the well-documented risks associated with high-dose and
long-term opioid use, and the national and local responses to these issues, we compared the rates of opioid

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 58
analgesic use, high-risk opioid use (high dose opioid use or opioid use with a benzodiazepine), initial opioid use
with more than seven and more than three days supplied, and the extent of naloxone use for those prescribed
opioids between newly enrolled persons obtaining coverage in traditional Medicaid and QHPs from 2014-16.
Data Sources and Analytic Population
Data sources and study subjects included in the opioid analysis are the General and Higher Needs Populations
described in previous sections.
Opioid Utilization Outcome Measures
All opioid analgesic prescriptions were converted to morphine equivalent doses using standardized conversion
tables. Opioid-related differences between Medicaid and QHPs were assessed using five outcome measures,
including:
1. Any opioid use, which was calculated annually as a binary indicator whether an individual
received at least one opioid analgesic prescription in a calendar year. It should be noted that only
oral and transdermal opioid analgesics were examined, with opioid-containing cough and cold
preparations excluded.
2. High dose opioid use, which was defined as the receipt of at least one day of an opioid regimen
where the sum daily dose exceeded 90 Morphine Milligram Equivalents (MME).
3. Concomitant benzodiazepine and opioid use, which was defined as observing at least one claim
for both an opioid and a benzodiazepine in a calendar year.
4. Initial duration of the first opioid prescription received by individuals utilized a smaller sample of
new opioid users. In order to identify initial opioid use, this measure was assessed only in those
subjects who had six continuous months of enrollment without any opioid use prior to their first
opioid prescription. Based on the CDC guidelines, we used thresholds of three days and seven
days to identify initial opioid use that is more likely to lead to chronic opioid use.
5. We calculated the total number of opioid prescriptions dispensed per 100 person-years. Opioid
use was further stratified by Schedule III-V opioid use, short-acting Schedule II opioid use and any
long-acting Schedule II opioid use. The number of opioid prescriptions were calculated based on
the number of opioid prescriptions received by an individual in a calendar year and for descriptive
reporting this was converted to a rate by dividing total opioid use by the person-years observed in
each sample for each calendar year.
All measures were calculated annually, except for duration of initial opioid prescription measures, for which we
report use over all three study years.
General Population Propensity Score Matching
The General Population contains all newly enrolled individuals 19-64 years of age with at least 180 days of
continuous enrollment with either Medicaid or QHP coverage in two consecutive years between 2014 and 2016, and
who did not complete an exceptional healthcare needs assessment Questionnaire. In total, this analytic population
contains 120,845 individuals — 92,940 assigned to a QHP and 27,905 covered by Medicaid. A propensity score was
generated using variables from the first year in the program: age, sex, race/ethnicity, median household income
based on census block group residence, insurance market region, Charlson Comorbidity Index and duration of
enrollment. Enrollees were matched using a one-to-one greedy matching algorithm without replacement. A
summary of covariates for unmatched and matched samples are reported in Table 32.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 59
Table 32. Characteristics of Unmatched and Propensity Score Matched General Population
Unmatched (N=120,845)
PS Matched (N=55,676)
Medicaid
QHP
Medicaid
QHP
(N=27,905)
(N=92,940)
(N=27,838)
(N=27,838)
Continuous Variables
Unit
Mean
(StdErr)
Mean
(StdErr)
p-value
Mean
(StdErr)
Mean
(StdErr)
p-value
Age
Years
36.0 (0.07)
39.0 (0.04)
<0.001
36.0 (0.06)
36.0 (0.06)
0.795
Household Income
Dollars
40,876 (95)
38,973 (52)
<0.001
40,854 (99)
40,976 (99)
0.383
Enrollment Duration
Days
817 (1.2)
887 (0.7)
<0.001
817 (1.2)
813 (1.2)
0.010
Categorical Variables
Category
N (percent)
N (percent)
p-value
N (percent)
N (percent)
p-value
Sex
Male
1,015 (36.4)
4,375 (47.1)
<0.001
1,016 (36.5)
1,037 (37.3)
0.066
Female
1,775 (63.6)
4,918 (52.9)
1,767 (63.5)
1,746 (62.8)
Race/Ethnicity
Black
4,657 (16.7)
2,592 (27.9)
<0.001
4,663 (16.8)
4,389 (15.8)
<0.001
Hispanic
828 (3.0)
2,312 (2.5)
827 (3.0)
883 (3.1)
Others
7,092 (25.4)
1,316 (14.2)
7,011 (25.2)
6,646 (23.9)
White
1,532 (54.9)
5,154 (55.5)
1,533 (55.1)
1,592 (57.2)
Insurance Market Region
Central
8,517 (30.5)
2,667 (28.7)
<0.001
8,491 (30.5)
8,491 (30.5)
0.290
Northeast
5,309 (19.0)
1,886 (20.3)
5,303 (19.1)
5,395 (19.4)
Northwest
4,664 (16.7)
1,323 (14.2)
4,652 (16.7)
4,722 (17.0)
South
Central
1,639 (5.9)
6,207 (6.7)
1,638 (5.9)
1,722 (6.2)
Southeast
2,396 (8.6)
1,154 (12.4)
2,396 (8.6)
2,305 (8.3)
Southwest
2,303 (8.3)
8,378 (9.0)
2,301 (8.3)
2,196 (7.9)
West
Central
3,077 (11.0)
8,038 (8.7)
3,057 (11.0)
3,007 (10.8)
Charlson Comorbidity Index
0
1,823 (65.3)
5,681 (61.1)
<0.001
1,817 (65.3)
1,819 (65.4)
0.959
1-2
7,330 (26.3)
2,705 (29.1)
7,329 (26.3)
7,269 (26.1)
3-8
2,235 (8.0)
8,743 (9.4)
2,234 (8.0)
2,274 (8.2)
>=9
106 (0.4)
329 (0.4)
105 (0.4)
104 (0.4)
Note: Household income is compiled as the average overall census block group median household incomes.
Abbreviations: N=number of persons; QHP=qualified health plan; PS=propensity score; StdErr=standard error
Prior to propensity score matching (unadjusted), QHP enrollees were older, were more likely to be white, were
more likely to be male, and had fewer comorbidities than their Medicaid counterparts. After propensity score
matching, no differences between groups were observed with the exception of small differences in
race/ethnicity categories.
The opioid utilization measures for Medicaid and QHP propensity score matched populations are presented in
Table 33.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 60
Table 33. Opioid Use Measures for Propensity Score Matched General Population Medicaid and QHP
by Assessment Period
Medicaid
QHP
Measure
Period
Population
Number
Percent
Population
Number
Percent
Any Opioid Use
Baseline
27,838
9,698
34.8
27,838
8,834
31.7
Year 1
27,837
8,996
32.3
27,837
9,560
34.3
Year 2
12,657
4,097
29.4
12,657
4,832
38.2
Received High Opioid
Dose (>90 MME)
Baseline
27,838
213
2.2
27,838
589
6.7
Year 1
27,837
214
2.4
27,837
685
7.2
Year 2
12,657
103
2.5
12,657
361
7.5
Benzodiazepine and
Opioid Use
Baseline
27,838
2,947
30.4
27,838
2,855
32.3
Year 1
27,837
2,621
29.1
27,837
2,949
30.9
Year 2
12,657
1,039
25.4
12,657
1,389
28.8
Duration of First Opioid Prescription >3 days
6,926
5,112
73.8
6,926
4,479
64.7
Duration of First Opioid Prescription >7 days
6,926
1,711
24.7
6,926
1,571
22.7
Measure
Period
Person-
Years
Number
Dispensed
Rate
Person-
Years
Number
Dispensed
Rate
Opioid Prescriptions
Dispensed (per 100
person-years)
Baseline
23,726
32,658
137.7
24,383
38,274
157.0
Year 1
26,753
34,379
128.5
26,253
46,040
175.4
Year 2
11,820
14,605
123.6
11,333
24,371
215.1
Notes: Year 1 and Year 2 indicate follow-up years after baseline measurement. For those with enrollment beginning in 2014, follow-up
Year 1 is 2015 and follow-up Year 2 is 2016. For those with enrollment beginning in 2015, follow-up Year 1 is 2016, and no follow-up Year
2 is available.
Abbreviation: QHP=qualified health plan; MME=morphine milligram equivalent
Generalized linear models were fitted by regressing a Medicaid/QHP dichotomous primary independent indicator
on the outcomes of interest. For binary outcomes, generalized logistic regression models were used and adjusted
odds ratios (AOR) were reported. For count variables, generalized Poisson regression models were used and least-
square (LS) means were reported for each group. For the initial duration of an opioid prescription measure,
individuals having any opioid use with at least six months of prior enrollment without opioid use were matched.
Additional details about the propensity score approach are described in Appendix E.
A comparison of opioid utilization differences between Medicaid and QHP enrollees in the General Population is
presented in Table 34.
Table 34. Comparison of Opioid Utilization for General Population Medicaid and QHP Enrollees
Measure
(QHP is referent group)
Period
Adjusted
Odds Ratio
95% Confidence
Interval
p-value
Any Opioid Use
Baseline
1.151
1.111
1.193
<0.001
Year 1
0.912
0.881
0.945
<0.001
Year 2
0.682
0.648
0.718
<0.001
Received High Opioid Dose (>90 MME)
Baseline
0.356
0.304
0.417
<0.001
Year 1
0.307
0.263
0.358
<0.001
Year 2
0.281
0.226
0.350
<0.001
Benzodiazepine and Opioid Use
Baseline
1.036
0.981
1.094
0.201
Year 1
0.877
0.829
0.927
<0.001
Year 2
0.735
0.676
0.798
<0.001
Duration of First Opioid Prescription >3 Days
3 years
1.540
1.432
1.657
0.037
Duration of First Opioid Prescription >7 Days
3 years
1.119
1.034
1.210
0.005
Notes: Year 1 and Year 2 indicate follow-up years after baseline measurement. For those with enrollment beginning in 2014, Year 1 is
2015 and Year 2 is 2016. For those with enrollment beginning in 2015, Year 1 is 2016, and no Year 2 is available.
Abbreviations: QHP=qualified health plan; MME=morphine milligram equivalent

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 61
During the first year of enrollment (baseline) and compared to QHP enrollees, Medicaid enrollees were 1.15 times
as likely to have had at least one opioid prescribed. However, by the first and second follow-up years of
enrollment the effect reversed and Medicaid enrollees were only 0.91 and 0.68 times, respectively, to have any
opioid use compared to QHP enrollees. Medicaid enrollees were 0.36, 0.31, and 0.28 times as likely to receive a
high opioid dose at baseline and in follow-up years 1 and 2, respectively. Medicaid enrollees were 0.88 and 0.74
times as likely to have both benzodiazepine and opioid use in follow-up years 1 and 2, compared to QHP
enrollees. Compared to QHP enrollees, Medicaid enrollees were 1.54 times more likely to have a first opioid
prescription duration longer than three days and 1.12 times as likely to have a first prescription for duration
longer than seven days.
Table 35 presents analyses comparing the number of opioids prescribed to Medicaid and QHP enrollees.
Table 35. Comparison of Number of Opioid Prescriptions by General Population Medicaid and QHP
(Reference) Enrollees
Number of Opioid Prescriptions
Plan Type
Least Squares
Mean
Difference
Standard Error of
Difference
p-value
Baseline
Medicaid
1.120
0.122
0.008
<0.001
QHP
1.242
Year 1
Medicaid
1.080
0.306
0.007
<0.001
QHP
1.385
Year 2
Medicaid
0.982
0.431
0.011
<0.001
QHP
1.413
Notes: Year 1 and Year 2 indicate follow-up years after baseline measurement. For those with enrollment beginning in 2014,
follow-up Year 1 is 2015 and follow-up Year 2 is 2016. For those with enrollment beginning in 2015, follow-up Year 1 is 2016, and
no follow-up Year 2 is available.
Abbreviation: QHP=qualified health plan
For the General Population, Medicaid enrollees had a lower number of total opioid prescriptions, on average,
than QHP enrollees. There was an adjusted absolute difference of 0.122 prescriptions at baseline, 0.306 at follow-
up Year 1 and 0.431 at follow-up Year 2. Over the three measurement period years, the average number of total
opioids prescribed to Medicaid enrollees continuously declined (1.12, 1.08, 0.98) while there was a steady
increase for QHP enrollees (1.24, 1.39, 1.41).
Higher Needs Population Regression Discontinuity Analysis
The Higher Needs Population contains all newly enrolled individuals 19-64 years of age with at least 180 days of
continuous enrollment with either Medicaid or QHP coverage in two consecutive years from 2014 to 2016, and
who completed an exceptional healthcare needs assessment. For this population, enrollees were assigned to
Medicaid and QHP groups on the basis of responses to the assessment resulting in a continuous composite score
threshold cut-point. A descriptive demographic profile of the Higher Needs Population Medicaid and QHP enrollee
groups contained in these analyses is presented in Table 36.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 62
Table 36. Characteristics of Higher Needs Population
Medicaid (N=9,037)
QHP (N=44,285)
Continuous Variables
Measure
Mean (StdErr)
Mean (StdErr)
p-value
Age
Years
36.0 (0.07)
38.9 (0.04)
<0.001
Household Income
Dollars
40,704 (172)
41,327 (78)
<0.001
Enrollment Duration
Days
980 (2.0)
971 (0.9)
<0.001
Categorical Variables
Category
N (percent)
N (percent)
p-value
Sex
Male
3,274 (36.2)
1,781 (40.2)
<0.001
Female
5,763 (63.8)
2,646 (59.8)
Race/Ethnicity
Black
1,431 (15.8)
7,969 (18.0)
<0.001
Hispanic
130 (1.4)
853 (1.9)
Others
1,243 (13.8)
7,675 (17.3)
White
6,233 (69.0)
2,778 (62.8)
Insurance Market Region
Central
2,692 (29.8)
1,383 (31.3)
0.037
Northeast
1,800 (19.9
7,784 (17.6)
Northwest
1,471 (16.3)
8,259 (18.7)
South Central
651 (7.2)
3,430 (7.8)
Southeast
869 (9.6)
3,793 (8.6)
Southwest
670 (7.4)
3,094 (7.0)
West Central
884 (9.8)
4,087 (9.2)
Charlson Comorbidity Index
0
2,666 (29.5)
2,579 (58.2)
<0.001
1-2
4,178 (46.2)
1,468 (33.2)
3-8
2,104 (23.3)
3,699 (8.4)
>=9
89 (1.0)
109 (0.3)
Notes: Household income is compiled as the average overall census block group median household incomes.
Abbreviations: N=number of persons; QHP=qualified health plan; StdErr=standard error
In general, for the Higher Needs Population, Medicaid enrollees were younger, were more likely to be white, and
were more likely to have higher comorbidity burden than the QHP enrollees.
An unadjusted descriptive analysis of opioid utilization for Medicaid and QHP propensity score matched
populations is presented in Table 37.
Table 37. Opioid Use Measures for Propensity Score Matched Higher Needs Population Medicaid and
QHP by Assessment Period
Medicaid
QHP
Measure
Period
Population
Number
Percent
Population
Number
Percent
Any Opioid Use
2014
9,037
5,165
57.1
44,285
15,951
36.0
2015
9,037
4,653
51.5
44,285
16,600
37.5
2016
7,951
3,943
49.6
37,752
14,386
38.1
Received High Opioid Dose (>90
MME)
2014
9,037
188
3.6
44,285
917
5.8
2015
9,037
210
4.5
44,285
1,115
6.7
2016
7,951
195
5.0
37,752
1,065
7.4
Benzodiazepine and Opioid Use
2014
9,037
2,176
42.1
44,285
4,396
27.6
2015
9,037
2,036
43.8
44,285
4,801
28.9
2016
7,951
1,503
38.1
37,752
3,670
25.5
Duration of First Opioid Prescription >3 days
3,310
2,552
77.1
16,202
10,822
66.8
Duration of First Opioid Prescription >7 days
3,310
1,094
33.1
16,202
3,732
23.0
Measure
Period
Person-
Years
Number
Dispensed
Rate
Person-
Years
Number
Dispensed
Rate
Opioid Prescriptions Dispensed
(per 100 person-years)
2014
8,038
22,883
284.7
39,336
62,379
158.6
2015
8,593
23,549
274.1
41,953
74,393
177.3
2016
7,625
20,182
264.7
36,381
68,197
187.5
Abbreviations: QHP=qualified health plan; MME=morphine milligram equivalent

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 63
Appendix E contains the technical statistical details for the regression discontinuity approach. Using this approach,
a comparison of opioid utilization differences between Medicaid and QHP enrollees in the Higher Needs
Population is presented in Table 38.
Table 38. Comparison of Opioid Utilization for Medicaid and QHP Higher Needs Population Enrollees
Measure (QHP is referent group)
Period
Local Average
Treatment Effect
Standard
Error
p-value
Any Opioid Use
Year 1
-151.5
274.6
0.581
Year 2
-1,132.0
245.2
<0.001
Year 3
-929.7
210.3
<0.001
Received High Opioid Dose (>90 MME)
Year 1
-436.7
45.6
<0.001
Year 2
-442.4
50.5
<0.001
Year 3
-431.0
52.1
<0.001
Benzodiazepine and Opioid Use
Year 1
-21.4
115.5
0.853
Year 2
-182.9
93.3
0.049
Year 3
-323.0
48.8
<0.001
Duration of First Opioid Prescription >3 Days
3 years
0.011
0.026
0.687
Duration of First Opioid Prescription >7 Days
3 years
-0.002
0.037
0.962
Number of Opioid Prescriptions
Year 1
-1.569
0.237
<0.001
Year 2
-1.956
0.253
<0.001
Year 3
-1.662
0.184
<0.001
Notes: Local Average Treatment Effect is per 10,000 persons, with the exception of the duration and number of opioid prescription
measures, which are represented at the person level.
Abbreviations: QHP=qualified health plan; MME=morphine milligram equivalent
Compared to QHP enrollees, 1,132 and 930 fewer Medicaid enrollees per 10,000 persons in the Higher Needs
Population had at least one opioid prescribed in 2015 and 2016, respectively. Medicaid enrollees also had lower
rates of high dose opioid use than QHP enrollees by approximately 440 fewer recipients per 10,000 person-year
between in years 2014 through 2016. Medicaid enrollees also had fewer concomitant benzodiazepine users in
2015 and 2016.
No difference in the duration of first opioid prescription was detected between Medicaid and QHP enrollees. The
number of opioids prescribed was found to be significantly lower for Medicaid enrollees in each of the program
years: 1.57 fewer prescriptions per person-year in 2014; 1.96 fewer prescriptions per person-year in 2015; and
1.66 fewer prescriptions per person-year in 2016.
The adjusted finding in the Higher Needs Population is similar to those concluded in the General Population. More
detailed descriptive results, including schedule of opioids, hydrocodone, oxycodone, and tramadol prescriptions,
are presented in Appendix J.
Discussion
In both the General Population and the Higher Needs Population, especially past the first year of enrollment,
enrollees in QHPs had significantly higher opioid utilization. Of those prescribed opioids, QHP enrollees had higher
percentages of prescribed high doses and had more opioid prescriptions filled than those in Medicaid. Program
differences became more exaggerated the longer enrollees were covered.
These differences can largely be explained by higher levels of drug utilization management in Medicaid. Medicaid
policy allows a maximum of 93 units of any solid oral short-acting opioid per 31 days,
50
which would substantially
reduce the chances of someone exceeding 90 MME. Medicaid also limits short- and long-acting opioids in addition
to limits for benzodiazepine prescriptions for individuals with a prior diagnosis of poisoning from opioids,
narcotics, barbiturates, or benzodiazepine in the previous three months.
50
In terms of limiting initial opioid

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 64
prescribing to three or seven days, we found that the first opioid prescription for approximately two-thirds of
enrollees exceeds a three-day supply, and a fourth of enrollees receive a prescription for more than seven days
supplied. In the propensity score analysis, we also found that enrollees in Medicaid were more likely to have
opioid prescriptions with longer days supplied. The risk of long-term opioid use begins to increase on the third day
supplied,
51
and efforts to conform to the CDC guidelines
44
should be undertaken.
It appears that expanding coverage through a QHP strategy in which there are fewer restrictions to opioid
prescribing may be contributing to the state’s high prescribing rate. Some recent state policy efforts should
mitigate opioid misuse, including requirements for prescribers to check the prescription drug monitoring program
as per state legislative mandate, but this effort will likely only affect opioid use where misuse is suspected.
Strategies should be undertaken to reduce opioid prescribing in Medicaid and QHPs, but additional focus is
warranted in QHP plans. Limitations on dispensed opioids for initial prescriptions should be considered for both
Medicaid and QHPs. This is especially true with respect to high dose opioid use given the escalating opioid
utilization rate and the well-documented overdose risk associated with high dose opioid use.
Urgent Care Utilization
Overview
As shown in Table 39, there was a decrease in the rate of non-emergent emergency room visits between each
year of study in the Higher Needs Population. One possible explanation for this decrease in ER utilization for non-
emergent use might be explained by an increase in urgent care visits. To investigate this, we analyzed urgent care
clinic utilization, which would allow us to determine if there was an associated increase in urgent care utilization.
Table 39. Change in Estimated Rate of Non-Emergent Emergency Room Visits per 100 Person-Years
Baseline
Mean (StdErr)
Year 2
Mean (StdErr)
Year 3
Mean (StdErr)
Percent Change
Baseline to Year 2
Year 2 to Year 3
General Population (Propensity Score Matched Comparison)
Medicaid
--
41.6 (0.7)
45.5 (1.1)
--
9.4
QHP
--
37.1 (0.6)
44.2 (1.0)
--
19.1
Higher Needs Population (Regression Discontinuity Comparison)
Medicaid
74.4 (1.7)
60.4 (1.5)
53.8 (1.5)
-18.8
-10.9
QHP
31.1 (0.4)
27.8 (0.4)
27.1 (0.4)
-10.6
-2.5
Notes: Due to the manner in which we used Baseline clinical comorbidity to propensity score match, no General Population can be
made with Baseline.
Abbreviations: QHP=qualified health plan; StdErr=standard error
Approach
Both the General Population and the Higher Needs Population were included in this analysis. To determine
whether or not an individual utilized urgent care, we extracted claims based on the appropriate place of service
code (CMS Place of Service Code: 20 – Urgent Care Facility). Unfortunately, after the initial claim extraction, we
discovered that there were only two instances in the Medicaid samples of each population in which an urgent
care facility was listed as the place of service (Table 40).

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 65
Table 40. Unadjusted Analysis of Urgent Care Facility Utilization and Cost
N
Visits
Urgent Care Facility Visits per
100 person-years
Total Costs ($)
General Population
Medicaid
Year 1
27,905
0
0
--
Year 2
27,905
0
0
--
Year 3
13,933
2
0.02
273
QHP
Year 1
92,940
774
0.93
111,489
Year 2
92,940
1,886
2.11
269,346
Year 3
56,874
2,100
3.97
281,317
Higher Needs Population
Medicaid
Baseline
9,037
0
0.00
--
Year 2
9,037
0
0.00
--
Year 3
7,951
2
0.03
237
QHP
Baseline
44,285
459
1.17
62,683
Year 2
44,285
1,018
2.43
151,562
Year 3
37,752
2,086
5.73
286,167
Notes: Visit counts were derived from claims data where the place of service was listed as an urgent care facility. Visits were
defined as the same person on the same day at the same facility. Cells with “--” indicate no associated costs.
Abbreviations: N=number of eligible Medicaid and QHP enrollees per group; QHP=qualified health plan
Discussion
While we could not examine whether or not urgent care clinic utilization reflected the decrease in Medicaid
recipients, we did observe an increasing trend in urgent care facility usage under the QHPs. It may be that
providers are not submitting claims under a place of service code for urgent care because of a Medicaid policy.
However, it is also possible that most urgent care clinics do not take Medicaid because of a programmatic effect.
We did attempt to find claims for urgent care clinics using National Provider Identifier; however, this methodology
also proved to be problematic because it was difficult to identify distinct clinics from other types of providers that
may be associated with the clinics. It would be interesting to look deeper into urgent care use compared to non-
emergent ER use in Arkansas in general to determine if there is an association between the two among a broader
population. If there is, there may be cost benefits for Medicaid to encourage urgent care facilities to agree to take
Medicaid patients.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 66
Mortality
Overview
A clear association exists between having health insurance coverage and a reduced risk of death.
52
The uninsured
lack the coverage necessary to regularly obtain recommended preventive screenings and appropriate disease
management. The Institute of Medicine — using findings from 130 studies — concluded in 2002 that not having
health insurance was a pre-eminent factor in the increase of all-cause mortality risk.
53
By expanding Medicaid to low-income uninsured adults, the PPACA has likely improved the survival of those who
were formerly uninsured. Previously in this report, we documented the findings that QHP enrollees had
significantly higher screening and disease-management rates.
Following National Advisory Committee (NAC) review of Interim Report
5
findings, considered indicators were
modified to include 7.1. Crude and Age adjusted mortality rates (see Appendix A). These represent the ultimate
outcome indicator of differences between QHP- and Medicaid-administered healthcare services.
Data Source and Study Population
Mortality data for 2014–2016 were obtained from the mortality vital records at the Arkansas Department of
Health. A unique study ID was placed on the mortality data files using the same methodology and personal
identifier match engine that was used to generate identifiers on all enrollment and claims data files used in this
evaluation. For this study, we compared newly enrolled traditional Medicaid enrollees (in or later than January
2014) in aid category 20 or 25, with those enrolled in a QHP under the Private Option. We restricted our study
population to enrollees who did not complete the exceptional healthcare needs assessment Questionnaire. To
account for early program switching, we only included those with at least 90 consecutive days in a program and
studied enrollees in programs beginning on their 91st day of enrollment. Observation time for death events
started on day 91 of enrollment through date of death, termination of coverage, or Dec. 31, 2016 (the end of the
evaluation period), whichever occurred first. Any time after a post-91st day Medicaid-to-QHP switch, or vice
versa, was censored and not included.
In the General Population, 36,182 traditional Medicaid enrollees and 176,081 QHP enrollees were eligible for the
mortality assessment. Of those, 72 mortalities were observed among the traditional Medicaid enrollees (0.2
percent) through Dec. 31, 2016, and 827 mortalities were observed among QHP enrollees (0.5 percent).
Traditional Medicaid and QHP enrollees were one-to-one matched based on propensity scores derived from
modeling characteristics of enrollees in traditional Medicaid and QHPs. Table 41 presents enrollee characteristics
after propensity score matching. Characteristics with an absolute standardized difference of 0.10 or higher
indicate significant categorical differences between Medicaid and QHP enrollees. A standardized difference of less
than 0.10 indicates that traditional Medicaid and QHP enrollees are balanced on that characteristic. In total,
35,917 enrollees in each program were matched (99.3 percent of Medicaid enrollees) using a greedy matching
algorithm (see Appendix E for additional matching details).

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 67
Table 41. Medicaid and QHP Enrollee General Population Propensity Score Matched Characteristics
Characteristic
Category
Medicaid 20/25
N=35,917 (percent)
QHP
N= 35,917 (percent)
Standardized
Difference
Insurance Market Region
Central
10,646 (29.7)
10,756 (30.0)
0.06
Northeast
6,635 (18.5)
6,730 (18.7)
Northwest
6,464 (18.0)
6,509 (18.2)
South Central
2,087 (5.8)
1,997 (5.6)
Southeast
3,111 (8.7)
2,940 (8.2)
Southwest
3,108 (8.7)
3,023 (8.4)
West Central
3,873 (10.8)
3,962 (11.0)
RUCA
Urban
20,847 (58.0)
20,793 ( 57.9)
0.00
Any Rural
15,070 (42.0)
15,124 (42.1)
Median Household Income
Quintile
1
7,984(22.2)
8,023 (22.3)
0.00
2
7,579 (21.1)
7,710 (21.5)
3
7,053 (19.6)
7,075 (19.1)
4
6,863 (19.1)
6,851 (19.1)
5
6,438 (17.9)
6,258 (17.4)
Charlson Comorbidity Index
0
30,277 (84.3)
31,074 (86.5)
-0.06
1
3,646 (10.2)
3,254 (9.1)
2
1,365 (3.8)
1,118 (3.1)
3 or higher
629 (1.8)
471 (1.3)
Sex
Female
25,954 (72.3)
25,995 (72.4)
0.00
Male
9,963 (27.7)
9,922 (27.6)
Race/
Ethnicity
Black
7,478 (20.8)
7,057 (20.0)
0.08
Hispanic
1,423 (4.0)
1,217 (3.4)
Other
2,500 (7.0)
2,290 (6.4)
White
24,516 (68.3)
25,353 (70.6)
Enrollment
Quarter
2014 Q1
2,613 (7.3)
2,671 (7.4)
0.00
2014 Q2
6,132 (17.1)
6,183 (17.2)
2014 Q3
3,304 (9.2)
3,267 (9.1)
2014 Q4
3,462 (9.6)
3,489 (9.7)
2015 Q1
2,385 (6.6)
2,409 (6.7)
2015 Q2
1,774 (4.9)
1,741 (4.9)
2015 Q3
2,184 (6.1)
2,161 (6.0)
2015 Q4
1,751 (4.9)
1,660 (4.6)
2016 Q1
3,732 (10.4)
3,756 (10.5)
2016 Q2
2,484 (6.9)
2,469 (6.9)
2016 Q3
3,180 (8.9)
3,214 (9.0)
2016 Q4
2,916 (8.1)
2,896 (8.1)
Age (years)
18-24
5,566 (15.5)
5,552 (15.5)
0.00
25-29
8,268 (23.0)
8,138 (22.7)
30-34
7,618 (21.2)
7,645 (21.3)
35-39
6,272 (17.5)
6,431 (17.9)
40-44
4,047 (11.3)
4,057 (11.3)
45-49
2,239 (6.2)
2,164 (6.0)
50-54
1,196 (3.3)
1,162 (3.2)
55-59
540 (1.5)
575 (1.6)
60-64
171 (0.5)
193 (0.5)
Notes: If any RUCA classification indicated the enrollee was residing in a rural region, a rural designation was assigned. Median
household income quintiles were derived from assigning enrollees a median household income based on the census block group in
which they resided.
Abbreviations: QHP=Qualified health plan; RUCA=Rural-urban commuting area code; Q1-Q4=quarter that individuals enrolled.
After propensity score matching, the traditional Medicaid and QHP enrollee populations are well balanced over all
characteristics used in the creation of the propensity score.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 68
Statistical Approach and Findings
Proportional hazard models tested for differential time to event across variables. After adjusting for variables
(covariates) associated with variability in death (e.g., age, poor health), we hypothesized no difference in the
number, or timing of deaths experienced by both traditional Medicaid and QHP enrollees. Hazard ratios were
constructed as measures to identify the effect of being enrolled in traditional Medicaid or a QHP on mortality.
Fully adjusted Cox proportional hazards time to event models were estimated using enrollment in Medicaid or
QHPs as the exposure variable and enrollee characteristics as covariates, including: patient age (as of the 91st day
of enrollment), sex, rural/urban status of residence, Charlson comorbidity index based on the first 90 days claims
experience (prior to study start date), an indicator for year and quarter of enrollment date, census block group
median income quintile, and insurance market region.
Table 42 presents the results of the fitted, adjusted Cox proportional hazards model. In the model, the outcome is
all-cause mortality. The main variable under study was plan type and Medicaid enrollees were the
“reference/control group,” while QHP enrollees constituted the “treatment group.”
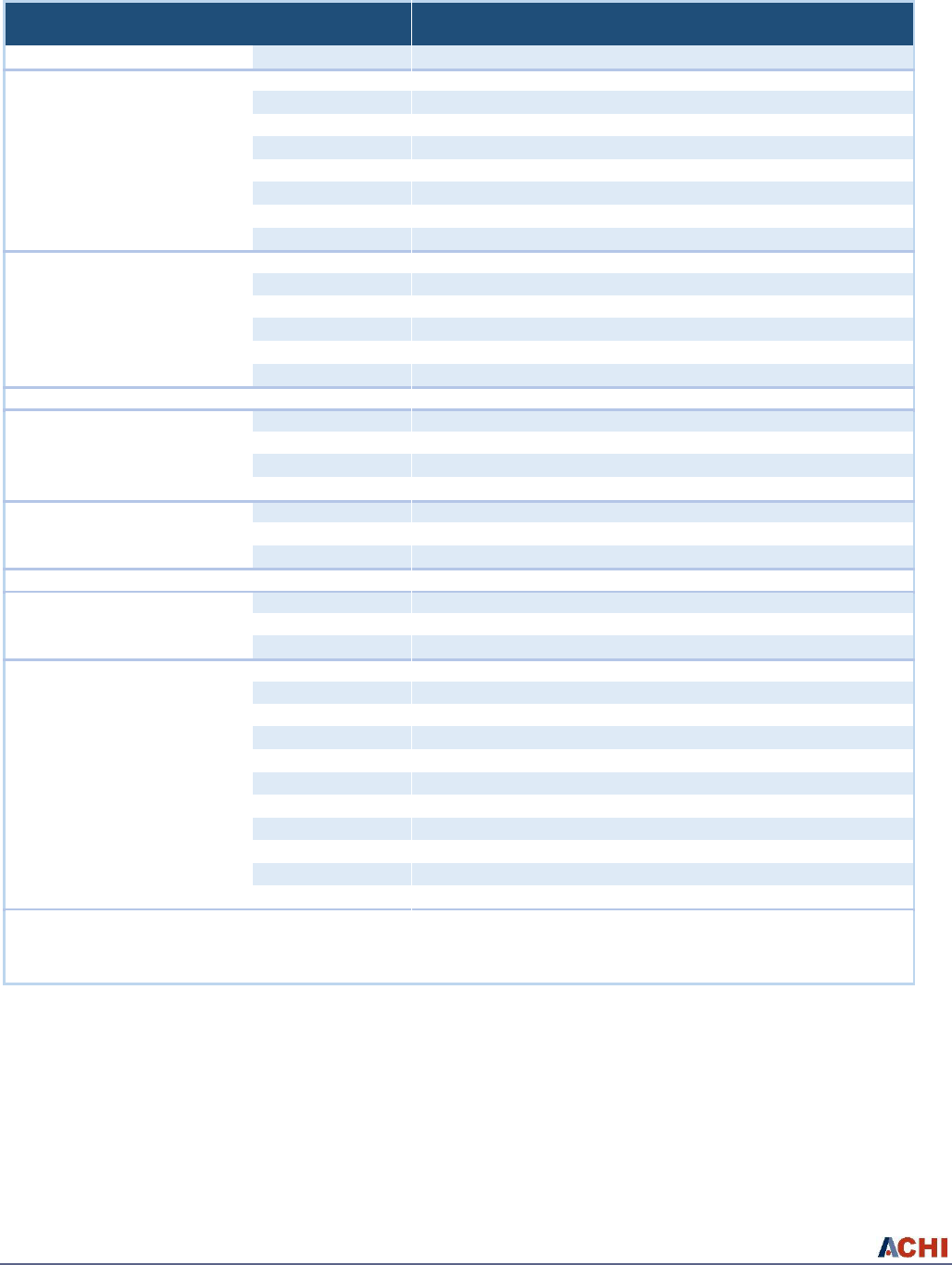
Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 69
Table 42. Medicaid and QHP Enrollees General Population Propensity Score Matched Characteristics
Characteristic
Category
Hazard Ratio
95% Confidence Interval
p-value
Plan Type (Reference = Medicaid)
QHP
1.256
0.913
1.728
0.162
AGE in Years (Reference = 18-24)
25-29
1.325
0.466
3.764
0.598
30-34
3.119
1.207
8.062
0.019
35-39
2.816
1.072
7.395
0.036
40-44
4.077
1.553
10.703
0.004
45-49
6.469
2.447
17.097
<0.001
50-54
7.149
2.589
19.738
<0.001
55-59
8.235
2.760
24.573
<0.001
60-64
9.404
2.458
35.984
<0.001
Region Code
(Reference = Northwest)
Central
1.433
0.86
2.386
0.167
Northeast
1.26
0.695
2.285
0.446
South Central
1.534
0.74
3.179
0.250
Southeast
2.934
1.567
5.493
<0.001
Southwest
1.589
0.754
3.349
0.223
West Central
1.111
0.571
2.16
0.756
RUCA (Reference = Urban)
Any rural
0.769
0.536
1.104
0.155
Income Quintile
(Reference = 1)
2
0.907
0.574
1.431
0.674
3
1.027
0.639
1.649
0.913
4
0.846
0.506
1.413
0.522
5
0.497
0.262
0.944
0.033
Charlson Comorbidity Index
(Reference = 0)
1
2.038
1.299
3.198
0.002
2
3.74
2.256
6.199
<0.001
3+
9.935
6.219
15.871
<0.001
Gender (Reference = Female)
Male
2.335
1.691
3.224
<0.001
Race/Ethnicity
(Reference = White)
Black
0.522
0.312
0.875
0.014
Hispanic
0.502
0.123
2.046
0.337
Other
0.669
0.31
1.444
0.306
Enrollment Quarter
(Reference = 2014 Q1)
2014 Q2
1.501
0.563
4.007
0.417
2014 Q3
1.091
0.422
2.819
0.857
2014 Q4
1.656
0.629
4.357
0.307
2015 Q1
1.621
0.605
4.346
0.337
2015 Q2
1.642
0.583
4.621
0.348
2015 Q3
1.357
0.429
4.289
0.603
2015 Q4
1.91
0.579
6.301
0.288
2016 Q1
1.329
0.415
4.254
0.632
2016 Q2
1.799
0.470
6.878
0.391
2016 Q3
2.318
0.593
9.064
0.227
2016 Q4
4.916
0.856
28.218
0.074
Note: Hazard ratio describes the mortality odds ratio of a patient belonging to a certain category relative to the reference case.
Abbreviations: QHP=Qualified health plan; RUCA=Rural-urban commuting area code; Q1-Q4=quarter that individuals enrolled.
After adjusting for individual characteristics (covariates), traditional Medicaid 20/25 enrollees were no more likely
to die than QHP enrollees at any given time between 2014 and 2016.
Increasing age, residing in the southeast region of the state, higher number of comorbidities, and being male were
associated with a higher likelihood of mortality. Of note, we observed that black enrollees were approximately
half as likely to die (52.2 percent) at any time over the study period, compared to white enrollees.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 70
Future Analyses
The finding of no increased mortality in Medicaid administered care compared to that in the QHPs is of significant
importance. The primary justification of the Section 1115 Waiver was the Federal Equal Access Requirements (42
U.S.C. §1396a(a)(30)(A)).
Documented perceived and realized access differences between QHP- and Medicaid-administered clinical
services, combined with less appropriate emergency room service utilizations by Medicaid administered
individuals, suggests differences in access may have resulted in differences in individual clinical outcomes — but
not mortality, as measured over the initial three years of enrollment in the program.
Of interest, the higher but not statistically significant mortality rate observed in the QHP General Population
suggests that mere exposure to the healthcare system for the average Arkansan may convey risk. The marked
reduction in mortality rates for African Americans suggest enhanced mortality benefits of coverage and also
warrants further exploration.
These findings require further exploration to account for additional unmeasured variables potentially contributing
to mortality (e.g., if applicable: smoking, obesity, job sector, and others) and a longer study period. This study may
be the first to formally test programmatic results for adults enrolled in traditional Medicaid and commercial
coverage. We will use the Arkansas All-Payer Claims Database to continue analysis of mortality in different insured
populations.
Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 71
Program Costs
Overview
In Table 4, the actual weighted average remuneration rates by Medicaid and QHPs for an identical basket of
services for different providers was presented. In this section, the focus is on program costs based on healthcare
visit type or services based on claims in the analytic population.
Utilization rates, as a component of differential cost, varied between Medicaid and QHP premium assistance.
While condition-specific comparisons were impractical due to variations in claim type and provider classifications
between the Medicaid and QHP programs, major categories of service utilization were categorized. Table 43
displays the utilization rates for Medicaid and QHP events including: hospitalizations, non-hospitalized ER visits,
physician’s office visits, outpatient visits, prescription medications, and other claims.
Table 43. Observed Utilization Rates (Per Member Per 100 Person-Years) for Medicaid and QHP
Enrollees in 2014, 2015, and 2016
2014
2015
2016
Visit Type
Medicaid Rate
1
QHP Rate
Medicaid Rate
1
QHP Rate
Medicaid Rate
1
QHP Rate
Hospitalization
0.154
0.097
0.135
0.111
0.120
0.117
Emergency Room
141.4
53.7
121.0
68.3
112.5
69.7
Physician’s Office
393.3
425.9
369.4
441.1
361.2
479.3
Outpatient
103.8
97.1
95.4
102.7
96.6
120.4
Prescription Medications
909.3
1,531.3
997.8
1,903.7
983.7
2,290.2
Other
2
638.3
499.4
608.5
541.8
605.8
613.5
Notes: The total person member-years used for all utilization metrics for the Medicaid population was 23,660 in 2014; 26,691 in 2015;
and 11,737 in 2016. The total person member-years used for all utilization metrics for the QHP population was 109,292 in 2014; 130,994
in 2015; and 88,954 in 2016.
1
The Medicaid rate includes individuals in traditional Medicaid and excludes 06 Medicaid (“Frail”).
2
Other
medical claims not classified above (excludes A6000/ARA6000 administrative claims — e.g., PCCM, Transportation — in Medicaid).
Abbreviation: QHP=qualified health plan
Clear and meaningful differences in utilization consistent with observed effects in the previous section are
demonstrated. Medicaid enrollees experienced fewer outpatient events and a concurrent higher rate of ER visits
and hospitalizations. Importantly, enrollees within QHPs received twice as many prescriptions than their Medicaid
counterparts. Because Medicaid utilizes different payment mechanisms and provider codes for select services
compared to their QHP counterparts, direct comparison of all services was not feasible.
The payment rates presented in the previous section and utilization differences depicted in Table 43 provide an
explanatory window into the effect differences observed between our comparison groups for access, quality, and
utilization indicators. Payments and utilization directly contribute to the absolute cost differences of the Medicaid
and commercial QHP programs and provide the quantitative basis to explore and simulate alternative scenarios of
payment and outcomes.
Using the matched payments from the primary care setting described in Table 4, we examined effect differences
in perceived access to determine the effect impact associated with payments.
Examining first year differences in access between individuals enrolled in Medicaid and those in QHPs (findings
contained in the Interim Report
5
), we noted a 13.2 percent increase in the number of QHP enrollees in the
General Population who reported that they “always get care when needed right away,” compared to Medicaid

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 72
enrollees. After approximately 18 months with coverage, the trend in perceived access difference between
Medicaid and QHP enrollees was greater, at 26.0 percent (bordering on, but not statistically significant at
p=0.057). In the Higher Needs Population, the self-reported differences were higher at both measurement
periods, with a difference of 16.9 percent during the first year, and a 36.7 percent difference at the second
measurement period, based on experience over the first 18 to 24 months with health insurance.
For every year of the HCIP program, QHPs reimbursed primary care physicians at nearly twice the rate as
Medicaid (99.9, 94.1, and 97.1 percent higher in 2014, 2015, and 2016, respectively — see Table 4). From the
observed 97.1 percent difference in payment rates to primary care physicians in 2016 and current access
differences, ratios of incremental access increase per payment difference were calculated. For the General
Population, a 2.68 percent improvement in access per 10 percent increase in payment rate could be expected. For
the Higher Needs Population, a 3.78 percent improvement in access per 10 percent increase in payment rate
could be expected.
Cost-Effectiveness
Based upon observed programmatic costs and utilization, PMPM rates for Medicaid and QHPs under alternative
scenarios were developed. Actual QHP premiums paid represented the cumulative PMPM average of premiums
paid to carriers during the first program year. Conversely, actual Medicaid expenditures paid for newly enrolled
previously eligible 19- to 64-year-old adults were calculated and expressed as a PMPM rate (supplemental
payments and estimates for marginal administrative costs were included — see Appendix F for details). Finally,
from observed utilization and payment differences, a model was generated to inform the counterfactual
assessment of what Medicaid would have experienced if a traditional expansion had been employed.
PMPM payments were calculated similarly for both Medicaid and QHP enrollees by summing adjudicated claims
for the different categories of services over 2014, 2015, and 2016 individually. Administrative costs (based on
medical loss ratio) were estimated to be an average of 18 percent for commercial carriers, while administrative
costs for traditional Medicaid were determined by examining spending across all Department of Human Services
categories that were eligible for matching federal funds. We also constructed an estimate to determine what the
QHP-enrolled individuals would have cost in the Medicaid program. The Estimated Medicaid PMPM cost are from
a model that calculates PMPM costs for QHP enrollees under the assumption that payments for services would be
at the prices paid in the Medicaid program. Under this methodology, prices for services were altered to reflect the
experience of the traditional Medicaid population, while holding utilization of services for the QHP enrollees
constant. Actual and estimated program cost numbers are contained in Table 44.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 73
Table 44. Observed and Estimated PMPM Cost Scenarios for Medicaid and QHP Enrollees by Service
Category and Year
2014
2015
2016
MCD
1
QHP
Estimated
MCD
MCD
1
QHP
Estimated
MCD
MCD
1
QHP
Estimated
MCD
Inpatient
$97.62
$96.90
$60.87
$100.73
$117.35
$81.39
$86.85
$123.99
$82.58
Emergency Room
$14.29
$40.25
$13.07
$13.27
$43.58
$12.54
$13.61
$44.16
$12.45
Physician’s Office
$35.28
$54.68
$43.13
$33.42
$58.67
$41.49
$31.36
$65.68
$37.27
Outpatient
$8.89
$9.89
$12.58
$8.52
$10.81
$12.04
$9.17
$11.63
$13.37
Prescription Medications
$35.53
$62.84
$41.46
$47.00
$94.37
$57.57
$40.27
$113.18
$48.15
Other
$71.20
$115.12
$67.66
$68.53
$129.40
$68.29
$64.44
$146.49
$62.83
Non-Emergency Transport Fees
$3.69
$4.92
$0.01
$3.30
$3.74
$0.01
$3.65
$4.04
$0.01
Total Claims PMPM
$266.50
$384.60
$238.78
$274.77
$457.92
$273.33
$249.35
$509.17
$256.66
Administrative PMPM
3,4
$67.96
$69.23
$68.28
$70.07
$82.43
$70.63
$63.58
$91.65
$63.58
Total PMPM
$334.46
$453.83
$307.06
$344.84
$540.35
$343.96
$312.93
$600.82
$320.24
QHP PMPM Premiums
2
$486.30
$486.98
$487.14
(Premium--Observed Variance)
6.7%
-9.9%
-18.9%
Notes:
1
Average PMPM represents loaded (i.e., cost-based reimbursement, supplemental payments, etc.) claims from Traditional Medicaid.
2
The
average PMPM payment made to QHP carriers includes cost-sharing and wrap services.
3
Includes PMPM Administrative costs for Observed QHP claims,
which were set at 18 percent of the total claims paid excluding copayments and deductibles.
4
Average PMPM represents claims costs based on average
Medicaid pricing.
5
Average PMPM paid represents claims costs based on average Medicaid pricing.
Abbreviations: MCD=Medicaid; QHP=qualified health plan; PMPM=per member per month
In 2014, the model estimate for commercial PMPMs developed from claims experience was $453.84, and 6.7 percent
lower than the actual average PMPM premium paid. In 2015, the model estimate for commercial PMPMs developed
from claims experience was $540.35, 9.9 percent more than the actual average PMPM premium paid. In 2016, the
model estimate for commercial PMPMs developed from claims experience was $600.82, 18.9 percent more than the
actual average PMPM premiums paid.
The estimated PMPM Medicaid cost of QHP enrollees in 2014 was $307.06 compared to $334.46 for actual
traditional Medicaid enrollees. In 2015, the estimated PMPM Medicaid cost of QHP enrollees was $343.96
compared to $344.84 for actual traditional Medicaid enrollees. In 2016, the estimated PMPM Medicaid cost of
QHP enrollees was $320.24 compared to $312.93 for actual traditional Medicaid enrollees. It is important to keep
in mind these modeled PMPMs reflect the estimated costs of care for QHP enrollees had they been managed
through the existing Medicaid system and experienced effects similar to those reported above. These PMPMs do
not account for potential utilization differences in the QHP enrollee population or reflect any modification of the
existing Medicaid program due to rate modifications to achieve necessary access.
Program Impact Simulation
One of the underlying justifications of Arkansas’s Section 1115 Waiver request to utilize premium assistance in the
new individual marketplace was that the network adequacy of the existing Medicaid program was insufficient to
meet anticipated demand. With Medicaid provider reimbursement rates approximately 50 percent of those in the
commercial sector (see Table 4), it was unlikely that Medicaid participating providers would be able or willing to
dramatically expand the volume of services provided without increases in reimbursement rates.
As previously noted, Arkansas had one of the lowest Medicaid eligibility thresholds for non-disabled adults in the
U.S. (below 17 percent FPL for parent/caretakers only). The result was that a majority of the covered lives were
for children, low-income Medicare beneficiaries for long-term services (not medical), pregnant women (limited
benefits for pregnancy and/or family planning services), and disabled adults (Social Security Income).
In 2013, prior to the Patient Protection and Affordable Care Act (PPACA) expansion, Arkansas Medicaid covered 24,955
non-disabled adults with a full benefits package representing 1.5 percent of the total 19- to 64-year-old population in

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 74
the state. In 2014, following PPACA expansion, an additional 267,482 individuals were covered — comprising
approximately 17,300 (6.5 percent) previously eligible but newly enrolled; approximately 25,000 (9.3 percent)
PPACA eligible but with exceptional healthcare needs; and 225,000 (84.2 percent) PPACA eligible with premiums
purchased on the individual marketplace. These 267,482 individuals represented 16.0 percent of the total 19- to
64-year-old population in the state.
In 2016, this number increased to 330,943 covered lives — approximately 22,375 (6.8 percent) PPACA eligible but
with exceptional healthcare needs; 32,427 (9.8 percent) interim status before enrollment in a QHP; and 276,141
(83.4 percent) PPACA eligible with premiums purchased on the individual marketplace.
54
These 330,943
individuals represent 19.1 percent of the working-aged adults within the state. Thus, because of the high rates of
uninsurance and low Medicaid eligibility prior to the PPACA, Medicaid has experienced a 13-fold increase in their
coverage for non-disabled 19- to 64-year-old population.
Infusion of an additional 330,943 non-disabled 19- to 64-year-olds into the Medicaid program is likely to have had
systemic effects. Traditional microeconomics suggests that increased demand through the Medicaid program
would place increasing price pressure on the rate structure of the existing Medicaid program. Medicaid could not
selectively raise provider rates solely for the expansion population. Thus, any potential increase in payment rates
would necessarily affect not only the new expansion population, but also beneficiaries under the same payment
rate schedule across the entire Medicaid program.
Though initial estimates of this potential systematic effects on the Medicaid program in 2014 were previously
calculated,
5
we have updated the estimates to reflect the more current environment in 2016.
In this program-impact simulation, we identified all claims paid within 2016 for Medicaid beneficiaries in the
system. We then restricted to individuals whose care would be under payment rates that might be affected (e.g.,
eliminating individuals age 65 and over, where Medicare would be the primary major medical payer, and children
younger than 1 because of a different rate structure in effect). Additionally, we eliminated payments by provider
types that were not likely to be subject to direct inflationary pressure (e.g., durable medical equipment providers,
transportation providers, etc.). Fixed costs for Medicaid, including Disproportionate Share payments and provider
supplemental payments to hospitals serving 19- to 64-year-olds were calculated by using the HP Financial
Transaction file provided by Medicaid.
From these expenses a total Medicaid expenditure of $2,490,804,452.76 for covered adults in the traditional (e.g.,
non-expansion) population was generated. The total member months for the traditional Medicaid population was
9,098,587 — resulting in a traditional Medicaid PMPM of $273.76. (Note that this is not the projected Medicaid
expansion PMPMs in Table 14.)
We then simulated, through a budget impact analysis, the incremental effect of potential inflationary increases in
payment rates and the net associated cost impact for the traditional Medicaid population under three alternative
scenarios:
1. Claims associated with potentially wage-sensitive services.
2. Then we restricted to claims associated with major medical services.
3. Then we further restricted to only claims associated with physician-billed services.
Within the budget impact analysis, increasing costs under the scenarios were applied to the total traditional
Medicaid expenditures. Claims were allocated according to each of the three scenarios. Increases for each
scenario were estimated based upon marginal five percentage payment increases and projected total traditional

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 75
Medicaid PMPMs were calculated. Results were plotted for each scenario. These Medicaid projections were then
compared to the actual premiums paid for commercial premium assistance to determine if, and at what
threshold, total Medicaid program costs would have exceeded the increased costs associated with using
commercial premium assistance.
Figure 11. Access Improvement Simulation Model Studying Scenario-Based Price Increases to Medicaid
Providers to Reach Commercial PMPM Payments
Note: PMPM expenditures observed for QHPs (premium assistance) and Medicaid with simulated Medicaid costs under incremental
increases under a scenario for all claims associated with wages, all claims restricted to major clinical services, and all claims restricted to
only physician services.
Figure 11 depicts the alternative scenarios when holding constant the actual commercial PMPM ($487.14) and
the actual traditional Medicaid PMPM ($265.75) in 2016. For each scenario, the budget impact analysis
demonstrated inflationary results and the thresholds where increases in the Medicaid program payment rates
would exceed the differential increase of expenditures associated with the use of premium assistance in the
expansion population.
Under the wage-sensitive scenario, if services for the traditional Medicaid beneficiaries experienced a 29.1
percent increase in wage-sensitive costs, Medicaid would have exceeded the costs associated with the use of
commercial premium assistance for the expansion population. Under the major medical scenario, the Medicaid
program would exceed expenditures at a 45.5 percent increase in clinical claims cost. Finally, restricting to the

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 76
physician-only scenario, the Medicaid program would exceed expenditures at a 64.2 percent increase in the cost
of physician claims.
While it is unknown to what degree Arkansas Medicaid would have experienced inflationary pressures on
provider payment rates, it is clear from comparison of access, utilization, and clinical performance between
Medicaid and QHP experiences that differences exist and are likely associated with provider payment
differentials. Had the approximately 330,000 newly covered individuals been placed in the traditional Medicaid
program, increases in payment rates would have been required to avoid potential legal challenges to the equal
access requirement and to assure attainment of needed services.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 77
References
1
National Federation of Independent Businesses v. Sebelius. 567 U.S. ___ (2012).
2
The Centers for Medicare & Medicaid Services [Letter] to Andy Allison, Arkansas Department of Human Services. September
2013. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ar/Health-
Care-Independence-Program-Private-Option/ar-private-option-app-ltr-09272013.pdf.
3
Ark. Code § 2-77-2405 (2014).
4
The Centers for Medicare & Medicaid Services. Arkansas Health Care Independence Program Special Terms and Conditions.
September 2013, 11-W-00287/6.
5
Arkansas Center for Health Improvement. Arkansas Health Care Independence Program (“Private Option”)
Section 1115 Demonstration Waiver Interim Report. Little Rock, AR: Arkansas Center for Health Improvement, March 2016.
6
Health Resources and Service Administration. Data Warehouse Medically Underserved Areas and Populations.
http://datawarehouse.hrsa.gov/tools/analyzers/muafind.aspx. Published 2016.
7
United States Census Bureau. Small Area Health Insurance Estimates (SAHIE), 2010 SAHIE Data.
https://www.census.gov/programs-surveys/sahie.html.
8
Arkansas Health Data Initiative. Report generated March 2016 by the Arkansas Center for Health Improvement.
9
The Centers for Medicare & Medicaid Services. Managed Care in Arkansas. https://www.medicaid.gov/medicaid-chip-
program-information/by-topics/delivery-systems/managed-care/downloads/arkansas-mcp.pdf. Published August 2014.
10
Ark. Code § 23-99-201.
11
Ark. Code § 23-61-801.
12
42 U.S.C. § 1396a(a)(30)(A)
13
Arkansas Insurance Department. Requirements for qualified health plan certification in the Arkansas federally facilitated
partnership exchange (marketplace) Bulletin No. 3B-2013. 2013
https://insurance.arkansas.gov/uploads/resource/documents/13b-2013.pdf
14
U.S. Government Accountability Office. CMS Has Taken Steps to Address Problems, but Needs to Further Implement
Systems Development Best Practices. March 2015. http://www.gao.gov/assets/670/668834.pdf.
15
Agency for Healthcare Research and Quality. The MEPS Data and Methods Manual. Medical Expenditure Panel Survey.
Rockville, MD. 2013. Available at http://meps.ahrq.gov/mepsweb/.
16
Witters D. Arkansas, Kentucky Set Pace in Reducing Uninsured Rate. Gallup, February 4, 2016.
http://www.gallup.com/poll/189023/arkansas-kentucky-set-pace-reducing-uninsured-rate.aspx.
17
Arkansas Department of Human Services. Private Option Enrollment and Premium Information. November 2017.
18
Calculated by the Arkansas Center for Health Improvement on March 22, 2016, based on enrollment and eligibility data
reported by the Arkansas Department of Human Services report run on April 14, 2015.
19
U.S. Department of Health and Human Services, Office of the Assistant Secretary of Planning and Evaluation. Profile of
Affordable Care Act Coverage Expansion Enrollment for Medicaid/CHIP and the Health Insurance Marketplace, 10-1-2013
to 3-31-2014, Arkansas. https://aspe.hhs.gov/sites/default/files/pdf/93416/ar.pdf. Published May 1, 2014. Accessed March
22, 2016.
20
Kaiser Family Foundation. Analysis of 2015 Premium Changes in the Affordable Care Act’s Health Insurance Marketplaces.
http://kff.org/health-reform/issue-brief/analysis-of-2015-premium-changes-in-the-affordable-care-acts-health-insurance-
marketplaces/. Published January 2015. Accessed March 21, 2016.
21
Susan Ward-Jones, MD. Personal Communication. March 12, 2015.
22
Arkansas Hospital Association. APO’s Hospital Impact Strong in 2014. The Notebook. 2015;22(22):1.
http://www.arkhospitals.org/archive/notebookpdf/Notebook_07-27-15.pdf.
23
Dan Rahn, M.D., Testimony before Health Reform Legislative Taskforce. August 20, 2015.
24
Lyon J. Despite elimination backlog, Medicaid re-determination process not quick. Arkansas News.
http://arkansasnews.com/news/arkansas/despite-elimination-backlog-medicaid-re-determination-process-not-quick
Published September 20, 2015.
25
Plan Management Frequently Asked Questions. https://static.ark.org/eeuploads/hbe/FAQs-3-13-15.pdf. Published March
5, 2015.
26
Arkansas Department of Health and Human Services. Arkansas 1115 Waiver-FINAL.
https://medicaid.mmis.arkansas.gov/Download/general/comment/ARWorksAppFinal.pdf. Accessed June 26, 2018.
27
45 CFR § 156.230

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report 78
28
National Committee for Quality Assurance. Healthcare Effectiveness Data and Information Set Technical Specifications for
Health Plans, 2015, Vol. 1-3.
29
Guo S, Fraser MW. Propensity Score Analysis: Statistical Methods and Applications. Los Angeles, CA: Sage; 2015.
30
Escanciano J. Regression Discontinuity Designs: Theory and Applications. Bingley, UK: Emerald Publishing Limited, 2017.
31
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. JASA.
1983;102:75-83.
32
New York University Center for Health and Public Service Research. NYU ED algorithm.
http://wagner.nyu.edu/faculty/billings/nyued-background. Published 2011. Accessed November 12, 2015.
33
Ballard DW, Price M, Fung V, et al. Validation of an algorithm for categorizing the severity of hospital emergency
department visits. Med Care. 2010;48(1):58-63. doi: 10.1097/MLR.0b013e3181bd49ad. PubMed PMID: 19952803.
34
Rhodes KV, Kenny GM, Friedman AB, et al. Primary Care Access for New Patients on the Eve of Health Care Reform. JAMA
Intern Med. 2014;174(6):861-869. doi:10.1001/jamainternmed.2014.20.
35
Arkansas Center for Health Improvement. Arkansas Health Care Workforce: A Guide for Policy Action. Little Rock, AR:
Arkansas Center for Health Improvement, March 2013.
36
Polsky D, Richards M, Basseyn S, et al. Appointment Availability after Increases in Medicaid Payments for Primary. N Engl J
Med 2015; 372:537-545. doi: 10.1056/NEJMsa1413299.
37
Agency for Healthcare Research and Quality, Prevention Quality Indicators.
http://qualityindicators.ahrq.gov/Modules/pqi_resources.aspx. Accessed March 14, 2018.
38
Kaskie B, Obrizan M, Cook E, et al. Defining emergency department episodes by severity and intensity: a 15-year study of
Medicare beneficiaries. BMC Health Services Research 2010, 10(1). doi:10.1186/1472-6963-10-173
39
Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques; 26th Annual SAS
Users Group International Conference; Long Beach, CA: 2001
40
Shore-Sheppard LD. Income Dynamics and Affordable Care Act. Health Services Research 2014; 46(6):2041-61.
41
Sinners BD, Rosenbaum S. Issues in Health Reform: How Changes in Eligibility May Move Millions Back and Forth between
Medicaid and Insurance Exchanges. Health Affairs (Millwood) 2011; 301(2):228-36.
42
Buettgens M, Nichols A, Dorn S. Churning under the ACA and state policy options for mitigation [Internet]. Urban Institute;
https://www.urban.org/research/publication/churning-under-aca-and-state-policy-options-mitigation
Published June 14, 2012. Accessed August 3, 2016.
43
Centers for Disease Control and Prevention. Prescription Opioid Overdose Data. 2017.
https://www.cdc.gov/drugoverdose/data/overdose.html. Accessed September 4, 2017.
44
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR
Recomm Rep. 2016;65(1):1-49.
45
Ark. Code Ann. § 20-7-601 (2011)
46
Ark. Code Ann. § 20-13-1701 (2015)
47
Ark. Code Ann. § 20-13-1801 (2015)
48
Ark. Code Ann. § 20-7-604 (2017)
49
Wachino V. Best Practices for Addressing Prescription Opioid Overdoses, Misuse and Addiction. CMCS Informational
Bulletin. 2016.
50
Arkansas Medicaid. Arkansas Medicaid Prescription Drug Program Prior Authorization Criteria. 2018.
https://arkansas.magellanrx.com/provider/docs/rxinfo/PACriteria.pdf. Accessed May 15, 2018.
51
Shah A, Hayes CJ, Martin BC. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use —
United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265-9.
52
Woolhandler S, Himmelstein DU. The Relationship of Health Insurance and Mortality: Is Lack of Insurance Deadly? Ann
Intern Medi. 2017; 167(6):424-431
53
Institute of Medicine; Committee on the Consequences of Uninsurance Care Without Coverage: Too Little, Too Late.
Washington, D.C., National Academies Press, 2002.
54
Arkansas Department of Human Services (DHS). (2016, December 31). Arkansas Private Option 1115 Demonstration
Waiver. Quarterly Report October 1, 2016-December 31, 2016 [Report]. Retrieved from
https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ar/Health-Care-
Independence-Program-Private-Option/ar-works-qtrly-rpt-oct-dec-2016.pdf

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report A-1
Appendices
Appendix A – Arkansas Evaluation Hypotheses: Proposed and Original Test
Indicators
Test Metrics for Incorporation into Year 1 HCIP Assessment
Note: This is an abridged list from hundreds of candidate indicators considered. Due to the short coverage period
of 12 months, observations did not meet the HEDIS indicator inclusion criteria. For others, there were too few
observed episodes to be able to detect significant differences across programs. This final listing was approved by
the National Advisory Committee as reasonable for presentation in this report.
1. Geographic Access
1.1. Was network participation in Medicaid equal to that of the qualified health plans (QHPs)?
1.1.1. Proportion of enrollees within 30 miles of at least one primary care provider (PCP)
1.1.2. Proportion of enrollees within 60 miles of the following specialists:
1.1.2.1. Cardiologist
1.1.2.2. Obstetrician/Gynecologist
1.1.2.3. Psychiatrist
1.1.2.4. Orthopedist
1.1.2.5. Internist
1.1.2.6. Ophthalmologist
1.1.2.7. Oncologist
1.1.2.8. General Surgeon
2. Realized Access – Differences in Utilization
2.1. Was time to engagement with a PCP in Medicaid equal to that in the QHP?
2.1.1. Proportion of enrollees with a PCP visit during first 12 months of continuous enrollment
2.1.2. Of those with a PCP visit, what were the number of days from enrollment date to first visit with a
PCP?
2.1.3. Reengagement with primary care following discharge:
2.1.3.1. Proportion of non-maternal discharges seen in outpatient setting within 10 days
2.1.3.2. Proportion of non-maternal discharges seen in outpatient setting within 30 days
2.2. Was utilization of frequent procedures in Medicaid equal to that in the QHP? Will require summary
indicator stratified by age and gender—HEDIS FSP frequency table
2.2.1. Percutaneous coronary intervention
2.2.2. Cardiac catheterization
2.2.3. Coronary artery bypass graft
2.3. Was inpatient utilization in Medicaid equal to that in the QHP? Reported separately by medical, surgical,
and maternity stratified by age and gender—HEDIS IPU frequency table
2.3.1. Discharges
2.3.2. Discharges per 1,000 member months
2.3.3. Days
2.3.4. Days per 1,000 member months
2.3.5. Average length of stay

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report A-2
3. Perceived Access – The Consumer’s Experience
3.1. Proportion of CAHPS respondents who report obtaining care as soon as needed
3.2. Primary care—Proportion of CAHPS respondents who report getting an appointment for checkup or
routine care as soon as needed
3.3. Specialty care—Proportion of CAHPS respondents who report getting an appointment for specialty care
as soon as needed
3.4. Proportion of CAHPS respondents who report ease of getting care
4. Transportation
4.1. CAHPS respondents who did not visit their personal doctor in the last six months because they could not
arrange acceptable transportation
4.2. CAHPS respondents who did not visit a specialist in the last six months because they could not arrange
acceptable transportation
5. Clinical Quality Process Measures
5.1. Were primary prevention efforts in Medicaid equal to that in the QHP?
5.1.1. CAHPS respondents who had a flu shot or nasal flu spray since July 1, 2014
5.1.2. CAHPS respondents who use tobacco and reported a cessation discussion with provider
5.2. Did secondary prevention efforts in Medicaid achieve equal results to those in the QHPs?
5.2.1. Combined screening indicator for age-appropriate screening tests—cervical cancer, breast cancer,
colorectal, cholesterol (note deviates from HEDIS):
5.2.1.1. Proportion of enrollees receiving one or more indicated screening tests
5.2.1.2. Proportion of enrollees receiving all indicated screening tests
5.3. Were indicators of chronic disease management (tertiary prevention) in Medicaid equal to those in the
QHP?
5.3.1. Diabetes
5.3.1.1. Proportion of enrollees with diabetes with evidence of HbA1c assessment
5.3.1.2. Proportion of enrollees with diabetes with evidence of two or more HbA1c assessments
5.3.1.3. Proportion of enrollees with diabetes with LDL-c screening
6. Clinical Quality Outcome Measures
6.1. Were preventable medical events in Medicaid equal to those in the QHPs?
6.1.1. Preventable emergency department visits
6.1.2. Preventable hospitalizations
6.2. Were avoidable readmissions in Medicaid equal to those in the QHPs?
6.2.1. Plan all-cause readmission (non-mental health)
7. Were Outcome Differences in Medicaid Equal to Those in the QHPs?
7.1. Crude and age-adjusted mortality rates

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report B-1
Appendix B – Arkansas Evaluation Hypotheses
Table 1 includes a description of each of the original 12 hypotheses outlined in STC 70 that have been reorganized
into the following four categories:
Table 1. Evaluation Hypotheses
Arkansas Evaluation Hypotheses
Arkansas Original Terms and Conditions Hypotheses (Section
8, STC 70, No. 1)
1 – Access
a. Use of PCP/specialist
i. Premium Assistance beneficiaries will have equal or
better access to care, including primary care and
specialty physician networks and services.
b. Non-emergent ER use
iii. Premium Assistance beneficiaries will have lower non-
emergent use of emergency room (ER) services.
c. Preventable ER use
vii. Premium Assistance beneficiaries will have lower rates of
potentially preventable emergency department and
hospital admissions.
d. EPSDT
ix. Premium Assistance beneficiaries who are young adults
eligible for EPSDT benefits will have at least as
satisfactory and appropriate access to these benefits.
e. Non-emergency
transportation
x. Premium Assistance beneficiaries will have appropriate
access to non-emergency transportation.
2 – Care/Outcomes
a. Preventive and healthcare
services
ii. Premium Assistance beneficiaries will have equal or
better access to preventive care services.
b. Experience
c. Non-emergent ER use*
d. Preventable ER use*
viii. Premium Assistance beneficiaries will report equal or
better experience in the care provided.
iii. Premium Assistance beneficiaries will have lower non-
emergent use of emergency room services.
vii. Premium Assistance beneficiaries will have lower rates
of potentially preventable emergency department and
hospital admissions.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report B-2
Arkansas Evaluation Hypotheses
Arkansas Original Terms and Conditions Hypotheses (Section
8, STC 70, #1)
3 – Continuity
a. Gaps in coverage
iv. Premium Assistance beneficiaries will have fewer gaps in
insurance coverage.
b. Continuous access to same
health plans
v. Premium Assistance beneficiaries will maintain
continuous access to the same health plans, and will
maintain continuous access to providers.
c. Continuous access to same
providers
4 – Cost Effectiveness
a. Administrative costs
vi. Premium Assistance beneficiaries, including those who
become eligible for Exchange Marketplace coverage, will
have fewer gaps in plan enrollment, improved continuity
of care, and resultant lower administrative costs.
b. Reduce premiums
xi. Premium Assistance will reduce overall premium costs in
the Exchange Marketplace and will increase quality of
care.
c. Comparable costs
xii. The cost for covering Premium Assistance beneficiaries
will be comparable to what the costs would have been for
covering the same expansion group in Arkansas Medicaid
fee-for-service, in accordance with STC 68 on determining
cost effectiveness and other requirements in the
evaluation design as approved by CMS.
* The outcomes of interest and evaluation approaches associated with hypotheses 2c and 2d are shared with 1b
and 1c.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report C-1
Appendix C – Data Processing of Carrier Data
Overview
Data were obtained from two primary data sources: administrative claims data from Medicaid and commercial
Qualified Health Plans (QHPs) and a member enrollment survey, Consumer Assessment of Healthcare Providers
and Systems (CAHPS). In order to construct variables of interest, these data were supplemented by files from the
Department of County Operations (DCO), Arkansas Department of Health (Birth/Death Certificates and Hospital
Discharges), and the Exceptional Health Care Needs Assessment Questionnaire. Administrative claims for
Medicaid and QHP enrollees contained enrollment and all reimbursed care provided by Medicaid and the three
commercial health plans from Jan. 1, 2014, through Dec. 31, 2016. The administrative claims data included
medical claims (provider and facility claims), pharmacy claims, member enrollment details, and provider files.
A survey of a sample of traditional Medicaid and QHP enrollees was fielded by the Arkansas Foundation for
Medical Care (AFMC) with measures derived from CAHPS, SF-12, and supplementary items. The survey was
administered between July and September of 2015 and questioned members about their plan experiences over
the prior six months. AFMC sent an initial survey, a reminder post card, a second survey for non-responses, and, if
no response after the second mailing, a follow-up phone survey.
A unique person identifier, called a POID, was generated using characters contained in the enrollee’s Social
Security number, first and last name, and date of birth. All data were linked by this encrypted identifier.
Data Specifications
i.
Program Enrollment and Eligibility Data
The Department of Human Services provided Medicaid enrollment data from Jan. 1, 2014, through March 31,
2017. This data was used to identify enrollees in the traditional Medicaid population and those assigned to
Medicaid with exceptional needs. Medicaid enrollment data was then integrated with enrollment data received
from each of the QHPs including Blue Cross Blue Shield, Ambetter, and QualChoice.
QHP assignment was validated using Department of Human Services fiscal expenditure data. This file included all
subsidized premiums paid by Medicaid for each QHP enrollee from January 2014 through March 2017.
ii.
Medical and Pharmacy Claims
Administrative claims for Medicaid and QHP enrollees were obtained from all reimbursed care provided by
Medicaid and the three QHPs from Jan. 1, 2014, through Dec. 31, 2016. The administrative claims data included
medical claims (provider and facility claims), pharmacy claims, member enrollment details, and provider files.
a.
Medicaid
Department of Human Services Medicaid medical and pharmacy claims files were used to assess utilization and
cost in the traditional Medicaid population and those assigned to Medicaid with exceptional needs. These data
were in Medicaid Management Information Systems standard format and layout. All claims included in the
analyses were adjudicated and non-voided.
b.
Qualified Health Plans (Blue Cross Blue Shield, Ambetter, and QualChoice)
QHP medical and pharmacy claims files for QHP enrollees were used to identify cost and utilization of services.
Each QHP was asked to provide this data in the Arkansas All-Payer Claims Database (APCD) layout. The APCD was

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report C-2
established pursuant to the Arkansas Healthcare Transparency Initiative of 2015. The Arkansas Insurance
Department (AID) established an APCD Data Submission Guide which defines file requirements for data
submissions (for the specific requirements please see the APCD Data Submission Guide here:
https://www.arkansasapcd.net/Resources/DataSubmissionGuideResources). All claims received were adjudicated
and non-voided.
iii. Arkansas Department of Health
The 2014-2016 Arkansas Inpatient Hospital Discharge data and 2013-2016 Arkansas Vital Statistics information,
including 2013-2016 birth and death certificate data, were made available through the Arkansas Center for Health
Improvement’s Arkansas Health Data Initiative health policy database, with approval from the Arkansas
Department of Health. Birth certificate data were used to assess pregnancy outcomes measures, differences in
low birth weight and very low birth weight, and the number of prenatal visits. Additionally, the birth certificate
data were used to capture pre-delivery covariates such as prior C-sections, mothers’ education, plurality, and
other measures. Mortality files were used to estimate death rates. Additionally, hospital discharge data was used
in calculations for cost effectiveness supplemental payment allocations.
iv. Income Eligibility Determination
Data was received from the Department of County Operations (DCO) containing all available eligibility and
enrollment data for Medicaid and QHPs covering the time period of Jan. 1, 2013, through Dec. 31, 2016. A key
feature of these data was the income determination levels of each enrollee at the time of application that was
used in survey sample strata creation and other analyses.
v. Consumer Assessment of Health Plans Survey (CAHPS) Data
Nationwide experience with CAHPS has led to important new insights into patient experiences regarding care for
both the Medicaid and the commercially insured populations. Various CAHPS surveys are available to gauge
consumer and patient experience with healthcare services and cover important topics including quality of care,
access to care, and experience with care. Surveys are available in the public domain.
The AFMC is the current contractor that collects CAHPS data for the Arkansas Medicaid program every two years.
In our evaluation, we contracted with AFMC to field a modified CAHPS survey in the third quarter of 2015. AFMC
sent an initial survey, a reminder post card, a second survey for non-responses, and, if no response after the
second mailing, a follow-up phone survey.
We included questions to be able to address access to and availability of services, consistency of care providers
and networks, use of primary and specialty care services, and experience with care. In addition, we included
questions from the 12-item Short Form Health Survey (SF12)
1
to determine physical and mental health
standardized scores.
In order to attain reasonable power to detect differences between Medicaid and QHP enrollees in responses to
CAHPS questions we oversampled sub-populations that formed comparison and distinct groups of interest. In
addition, we sampled a representative portion of the traditional Medicaid enrollees. The cooperation rate for the
survey was 26.4 percent and a representative response rate was received across sub-populations of interest.
Details on the CAHPS sampling strategy can be found in Appendix K.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report C-3
vi. GIS Processed Provider-Enrollee Distance Measures Data
To determine geographic access of Medicaid and HCIP enrollees to providers we contracted with the Center for
Advanced Spatial Technologies (CAST) at the University of Arkansas, J. William Fulbright College of Arts and
Sciences. Medicaid and QHP enrollee addresses were obtained as well as in-network provider address lists.
Enrollee and provider addresses were geocoded. Distances between enrollees and in-network providers were
measured in both 15-minute travel time increments and 15-mile distance increments. For enrollees in a QHP,
additional access metrics were calculated to determine if they had access to out-of-network, as well as in-network
providers.
For the purpose of this evaluation, we defined adequate access if an enrollee resided within a 30-minute travel
time for a primary care physician or within 60 minutes of a specialist. Specialty access was calculated for each of
the following: orthopedics, ophthalmology, obstetrician/gynecologist (OB/GYN), oncology, surgical, psychology,
and cardiology. More details on methods used by the CAST team can be found in Appendix H.
Reference
1
Burdine JN, Felix MR, Abel AL, Wiltraut CJ and Musselman YJ. The SF-12 as a population health measure: an exploratory
examination of potential for application. Health Services Research. 2000 Oct; 35(4): 885–904.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report D-1
Appendix D – Study Subjects: Analytical Sample Extraction
This analysis sought to compare the effects of the Health Care Independence Program (HCIP) versus traditional
Medicaid for subjects who had relatively stable coverage in their respective plans for at least two contiguous
calendar years. For the regression discontinuity (RD) sample, subjects had to have at least two years of coverage
starting in 2014, but could be followed until 2016. Additionally, the RD sample was restricted to those with a
health needs assessment (frailty) score recorded before the end of 2014. For the propensity score sample, a
subject’s first year of contiguous enrollment could start in 2014 or 2015, with the first year serving as the baseline
year to capture covariate history, and the subject had to have at least one year of contiguous enrollment the
following year, but could be followed for up to two years after their baseline year. Further, the propensity score
sample was restricted to persons who did NOT have a health needs assessment score.
Arkansas Medicaid enrollment files for calendar years 2013 and 2014 were used to exclude enrollees of non-
interest and identify the study population. Enrollees who did not meet each of the following criteria were
excluded:
At least 18 years of age on Jan. 1, 2014, and less than 65 years of age on Dec. 31, 2016;
Continuously enrolled in a Medicaid or HCIP category, which is defined as enrollment for at least
180 days with, at most, one gap of no more than 13 days in each of a subject’s first two calendar
years of enrollment.
o For the regression discontinuity sample, subjects had to be continuously enrolled
throughout 2014 and 2015.
o For the propensity sample, subjects had to have two consecutive years of continuous
enrollment, beginning in either 2014 or 2015.
Not dually enrolled with a Medicare benefit;
Not enrolled in a full-benefit Medicaid category between Jan. 1, 2013, and Oct. 15, 2013.
Figure 1 outlines the study population development starting from a base population of enrollees who had at least
one valid enrollment segment from Jan. 1, 2014, through Dec. 31, 2016. Two important exclusions should be
highlighted. First, members who switched between Medicaid and any of the commercial carriers after their first
90 days enrolled were excluded. Persons could switch between any of the commercial carriers after the 90 days
and still be retained, but could not make a transition to a traditional Medicaid enrollment category. Second,
enrollees with coverage discrepancies were also removed from analytical consideration. A majority of these
people were eligible for commercial qualified health plan (QHP) coverage, but never transitioned into a
commercial plan.
Figures 1 and 2 illustrate the application of the inclusion and exclusion criteria for the regression discontinuity and
propensity score samples, respectively. Once the samples were selected, an analyzable dataset was built, which
included, for each subject, rural/urban designation using rural-urban commuting area (RUCA) classifications,
1
healthcare services utilization variables, and constructed fields to represent access, experience, and outcomes
indicators. Selected demographics are shown in Table 1.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report D-2
Figure 1. Analytical Data Preparation Regression Discontinuity Sample — Final Report
Total newly covered 20/25/06 individuals in premium assistance
(regression discontinuity sample)
N = 765,026
N = 215,450
Exclude persons not enrolled for at least 180 days in 2014
and 2015 and those who died before the time frame of
analysis
N = 545,379
N = 207,484
Exclude persons enrolled in Medicaid prior to the
HCIP program (Oct. 15, 2013) other than Family
Planning
N = 7,966
Analyzable Study Population
N = 53,322
Exclude persons who were dually eligible or
institutionalized in 2014
N = 6,403
Exclude those who made a switch between Medicaid
and commercial plans after the first 91 days of
enrollment but before the beginning of the third year
N = 17,660
Exclude persons less than 18 years of age on Jan. 1, 2014
or older than 65 years of age on Dec. 31, 2016
N = 4,197
Exclude those with coverage discrepancies (i.e.
premium assistance members who never transitioned
to commercial coverage or were frail and placed in
commercial coverage)
N = 1254
Exclude persons with one day or more of pregnancy
coverage
N = 20
Exclude persons without a frailty score
N = 128,825
General Population
Traditional Medicaid
Baseline and Year 2
N = 9,037
General Population
Commercial QHP
Baseline and Year 2
N = 44,285
General Population
Commercial QHP
Year 3
N = 37,752
General Population
Traditional Medicaid
Year 3
N = 7,951

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report D-3
Figure 2. Analytical Data Preparation-Propensity Score Sample — Final Report
Total newly covered 20/25/06 individuals in premium assistance
(propensity score sample)
N = 765,026
N = 300,549
Exclude persons enrolled for less than 180 days in two
consecutive calendar years and those who died before the
time frame of analysis
N = 458,845
N = 255,182
Exclude persons enrolled in Medicaid, other than
Family Planning, prior to the HCIP program,
Oct. 15, 2013
N = 45,367
Analyzable Study Population
N = 120,845
Exclude persons who are severely developmentally disabled,
dually eligible or institutionalized in 2014
N = 5,210
Exclude those who made a switch between Medicaid and
commercial plans after the first 91 days of enrollment but
before the beginning of the third year
N = 54,501
Exclude persons less than 18 years of age on Jan. 1, 2014
or older than 65 years of age on Dec. 31, 2016
N = 5,632
Exclude those with coverage discrepancies
(I.e. overlapping coverage)
N = 1,193
Exclude persons with one day or more of pregnancy
coverage
N = 2,175
Exclude persons with a frailty score
N = 71,258
General Population
Traditional Medicaid
Baseline Year and Year 2
N = 27,905
Expansion Population
Baseline Year and Year 2
N = 92,940
General Population
Traditional Medicaid
Year 3
N = 13,933
Expansion Population
Year 3
N = 56,874

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report D-4
Table 1. Demographic Profiles of General Population and Higher Needs Population
General Population
(n=120,845)
Higher Needs Population
(n=53,322)
Medicaid
QHP
Medicaid
QHP
n
%
n
%
n
%
n
%
Age
<34
14,731
52.8
39,627
42.6
2,910
32.2
18,165
41.0
35-44
7,399
26.5
22,252
23.9
2,261
25.0
9,872
22.3
45-54
4,052
14.5
20,124
21.7
2,408
26.6
9,374
21.2
55-64
1,723
6.2
10,937
11.8
1,458
16.1
6,874
15.5
Gender
Male
10,155
36.4
43,756
47.1
3,274
36.2
17,816
40.2
Female
17,750
63.6
49,184
52.9
5,763
63.8
26,469
59.8
Race
White
19,645
70.4
58,711
63.2
7,026
77.7
31,776
71.8
Black
5,858
21.0
28,258
30.4
1,588
17.6
8,856
20.0
Hispanic
347
1.2
1,009
1.1
50
0.6
426
1.0
Other
1,288
4.6
1,440
1.5
152
1.7
900
2.0
Missing/Unknown
767
2.7
3,522
3.8
221
2.4
2,327
5.3
Region
Central
8,517
30.5
26,674
28.7
2,692
29.8
13,838
31.2
Northeast
5,309
19.0
18,867
20.3
1,800
19.9
7,784
17.6
Northwest
4,664
16.7
13,232
14.2
1,471
16.3
8,259
18.6
South Central
1,639
5.9
6,207
6.7
651
7.2
3,430
7.7
Southeast
2,396
8.6
11,544
12.4
869
9.6
3,793
8.6
Southwest
2,303
8.3
8,378
9.0
670
7.4
3,094
7.0
West Central
3,077
11.0
8,038
8.6
884
9.8
4,087
9.2
Household Median Income
$30k or less
6,985
25.0
27,215
29.3
2,213
24.5
10,380
23.4
$30k–$40k
7,589
27.2
25,684
27.6
2,558
28.3
12,310
27.8
$40k–$50k
7,059
25.3
22,319
24.0
2,306
25.5
11,496
26.0
$50k–$60k
3,268
11.7
9,580
10.3
1,019
11.3
5,123
11.6
Greater than $60k
3,004
10.8
8,142
8.8
941
10.4
4,976
11.2
Totals
27,905
92,940
9,037
44,285
Reference
1
United States Department of Agriculture, Economic Research Services. http://www.ers.usda.gov/data-products/rural-urban-
commuting-area-codes.aspx. Accessed 10/12/2017

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report E-1
Appendix E – Statistical Modeling to Assess Effect Differences for Those
Assigned to Medicaid and QHPs
In our evaluation plan, we proposed using regression discontinuity as the statistical method to assess the access,
quality, and utilization effect differences between beneficiaries assigned to the Medicaid plan and beneficiaries
assigned to the QHPs. We had two candidate variables on which to use regression discontinuity designs. One was
using the continuum of composite scores obtained from the exceptional healthcare needs assessment
Questionnaire. A threshold cut-point was established along the composite scores to identify those with higher risk
of exceptional healthcare needs, who were then assigned to the Medicaid plan.
In addition, the traditional programmatic assignment of beneficiaries into the traditional Medicaid fee-for-service
plan was based on being a parent earning 17 percent or less of the federal poverty level (FPL). We anticipated
using the programmatic income cut-point assignment for a parent subpopulation to be able to fit a series of
regression discontinuity models. Preliminary data analyses confirmed that nearly one in three enrollees (30.3
percent) in the traditional Medicaid fee-for-service plan (aid categories 20/25) were not parents. Also, many
parents who were assigned to a QHP indicated an income of less than 17 percent FPL, with many of these
indicating an income of zero dollars. For this reason, and lacking the ability to conform to accepted standards for
the use of a regression discontinuity design, we decided to pursue a different statistical method to compare
groups of people who did not complete an exceptional healthcare needs assessment Questionnaire but were
assigned into one of the Medicaid plans, or a QHP.
This document provides an outline of the statistical methods used in producing the results in this report.
Regression Discontinuity Design
Comparison Groups
We included beneficiaries completing the exceptional healthcare needs assessment Questionnaire and meeting
other inclusion criteria for claims-based metrics and for CAHPS respondents. This population is labeled as “Higher
Needs” and there was a sharp assignment into either the Medicaid or a QHP plan based on the exceptional
healthcare needs assessment composite score. Those completing the Questionnaire and receiving a composite
score of 0.18 or higher were all assigned to the Medicaid plan and those with a composite score less than 0.18
were assigned to a QHP. In total, our analytic claims file contained 9,037 assigned to the Medicaid plan and
44,285 assigned to a QHP (see Table 1 in the Final Report). For CAHPS II, where we oversampled populations that
were close to the threshold composite score value of 0.18, our analytic file contained 1,013 assigned to the
Medicaid plan and 1,119 assigned to a QHP.
Figures 1 and 2 depict the composite score frequencies in the Claims and CAHPS II analytic populations.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report E-2
0
5,000
10,000
15,000
20,000
25,000
30,000
35,000
0.02
0.07
0.08
0.10
0.13
0.15
0.17
0.18
0.19
0.20
0.21
0.22
0.23
0.24
0.26
0.27
0.28
0.29
0.31
0.32
0.33
0.34
0.35
0.37
0.38
0.40
0.42
0.43
0.44
0.45
0.46
0.49
0.50
0.51
0.56
0.61
Frequency of Enrollees
Exceptional Health Care Needs Composite Score
Figure 1. Claims Data - Exceptional Health Care Needs Composite Score (N=53,332)
0
50
100
150
200
250
300
350
0.02
0.07
0.08
0.10
0.13
0.15
0.17
0.18
0.19
0.20
0.21
0.22
0.23
0.24
0.26
0.27
0.28
0.29
0.31
0.32
0.33
0.34
0.35
0.37
0.38
0.40
0.42
0.44
0.45
0.46
0.50
0.51
0.61
Frequency of Enrollees
Exceptional Health Care Needs Composite Score
Figure 2. CAHPS II Data - Exceptional Health Care Needs Composite Score (N=2,132)

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report E-3
Theoretical Causal Determination of Program Effect
As stated in the report, regression discontinuity is a quasi-experimental design that is increasingly being used in
evaluation analyses to test differences attributable to group assignment. This approach is useful when random
assignment to groups is not feasible. We adhered to standards for regression discontinuity designs
1
which included:
1) Treatment assignments were based on a forcing variable (composite score); enrollee assignment to
Medicaid and QHP groups on the basis of a threshold cut-point from the composite score met
assumptions to conduct a regression discontinuity design analysis.
2) The forcing variable must be ordinal with a sufficient number of unique values (higher composite
scores indicated higher needs).
3) There must be no factor confounded with the forcing variable. Overall, those assigned to Medicaid with
higher needs were slightly older and tended to be female and white more often than those assigned to a
QHP. Locally around the cut-point, we did not see any differences across these confounders.
Modeling Strategy
Since our outcome variables are discrete — either counts (e.g., number of emergency room visits) or binary (e.g.
any readmission within 30 days of an indexed hospitalization) variables — we used the local linear regression
modeled as below.
) +
), where
is the outcome for individual and
is a dummy
variable for the treatment (1 = QHP, 0 = Medicaid),
is the composite score,
is the threshold (cut-off) for
assignment (0.18),
is the parameter for the effect of association between the outcome and being in a QHP
(treatment group) compared to Medicaid (comparison group). This model also incorporates an interaction
between treatment assignment and difference in composite score from the cut-off.
For the regression discontinuity models presented in the Final Report, we incorporated optimal bandwidths. An
Imbens-Kalyanaraman optimal bandwidth calculation
2
,
3
and heteroskedasticity-consistent (“HC1”) variance were
estimated.
4
Since the construction of frailty scores were discrete, standard errors were adjusted for clustering within
frailty scores.
5
Furthermore, triangular kernel weights were applied which gave observations closer to the threshold of
0.18 higher weights than those further away from the threshold within the optimal bandwidth around the threshold
and zero weights to those outside of the estimated optimal bandwidth.
We used the R statistical computing language (R Foundation for Statistical Computing, Vienna, Austria) to run the
regression discontinuity design (RDD) package developed by Drew Dimmery (2016) and fit the regression models
with the functional form above. For each model we reported linear average treatment effects and the p-value
corresponding to the bandwidth.
Models Using Stabilized Inverse Probability of Treatment Weighting (Geographic Access Models)
Comparison Groups
We included individuals not completing the exceptional healthcare needs assessment Questionnaire and meeting
other inclusion criteria detailed in Appendix D for claims-based metrics and Appendix G for CAHPS respondents,
contained in the Interim Report.
6
Individuals assigned to the traditional Medicaid fee-for-service plan were mostly
parents, and mostly with very low incomes, while those assigned to a QHP were, in general, a more equal mixture of
parents and individuals with no dependents, with many having higher income levels than those assigned to
Medicaid. Since the presumptive assumption of assignment to Medicaid and QHP did not hold to meet standards of
using a regression discontinuity design based on parenthood status and an income forcing variable we chose to

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report E-4
match the beneficiaries assigned to Medicaid and QHPs by using propensity scores. In total, our analytic claims file
contained 27,905 assigned to the General Population Medicaid plan and 92,940 assigned to a General Population
QHP. For CAHPS, our analytic file contained 275 assigned to the Medicaid plan and 835 assigned to a QHP.
Theoretical Association Determination of Program Effect
To test for the association of plan assignment and outcome, we mitigated differences in assignment that may
have been due to demographic or other factors attributing to the assignment (income was not used). Propensity
scores are the probability of being assigned to a treatment group (i.e., a QHP) given a set of underlying
characteristics.
Stabilized Inverse Probability of Treatment Weighting (SIPTW)
Following nomenclature outlined in Xu and colleagues,
7
we let z be a binary outcome where 1 indicates that a person
was assigned to a QHP and 0 as assignment to the Medicaid plan. X is a row vector of covariates (characteristics) and π
indicates for the probability of being assigned to a QHP (the propensity score).
For our claims analytic data the total number (N=80,505) was equal to the 11,006 assigned to Medicaid (n
0
) plus 69,499
assigned to a QHP (n
1
). The crude calculation of probability of treatment was p = n
1
/N = 69,499/80,505 = 0.86. The
probability of no treatment, or being assigned to Medicaid was 1-p = 1 – 0.86 = 0.14.
The propensity score associated with an individual (i) was estimated using a logistic regression with the functional
form of:
, where β is a vector of parameters to be fit in the model and associated with the
a row vector of
covariates for individual i (age, gender, race/ethnicity, and parent status for claims data and in addition education,
marital, employment, and obesity status for CAHPS data — no data on 2013 health status was available). We used a
class statement to produce dummy covariate categories. Inherent in the model is a parameter (β
0
) associated with
the intercept for the model. Our logistic regression model had a reasonably high coefficient of determination (c-
statistic) of 0.718 for claims data and 0.717 for CAHPS data.
The resulting estimated propensity scores were used to produce inverse proportional treatment weights (IPTW)
as follows:
, where
denotes the IPTW for individual i.
Weights for individuals assigned to a QHP (treatment group) with a low propensity score and those assigned to
Medicaid with a high propensity score for assignment into a QHP will be high and increase the risk of a Type I
error. To reduce this risk we adjusted, or stabilized, the increased pseudo-sample size that was created by using
large weights as follows:
, where is the crude probability of treatment without
considering covariates and
denotes the SIPTW for individual i.
effectively keeps sample sizes used in statistical models the same as if those weights had not been included
and had not artificially increased the risk of a Type I error.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report E-5
Statistical Models with Treatment Assignment as the Primary Predictor
Statistical models to fit access, quality, and utilization outcomes incorporated the distributional form of the
outcome that produced the best-fitting model. For example, for the number of total emergency room visits over
the course of 12 months, we used a negative binomial distribution after demonstrating that this distribution
provided a better model fit. The only covariate that was used in models testing for a treatment effect (primary
predictor) was urban/rural designation determined by a RUCA classification (see Appendix D).
General linear models were fit using SAS Enterprise Guide V7.1 HF1 (SAS Institute, Cary, NC). For outcomes that
were affected by duration of tenure with coverage (ranging from six to 12 months) we produced estimated rates
based on 12 months of coverage. We accomplished this by using an offset option in the model statement of the
proc genmod SAS procedure. The SAS statement to produce the results for total emergency room visits is
presented below. The stabilized inverse probability of treatment weights were labeled “siptw.”
proc genmod data = ps_data;
class treatment urban;
model num_poid_er_visits_total = treatment urban/dist = negbin link = log
offset = TotDur_POID_per_yr_ln type1 type3;
weight siptw;
lsmeans treatment/ilink cl alpha = 0.05;
run;
Models Using Propensity Score Matching
Comparison Groups
We included individuals not completing the exceptional healthcare needs assessment Questionnaire and meeting
other inclusion criteria detailed in Appendix D. Individuals assigned to the traditional Medicaid fee-for-service plan
were mostly parents, and mostly with very low incomes, while those assigned to a QHP were, in general, a more
equal mixture of parents and individuals with no dependents, with many having higher income levels than those
assigned to Medicaid. Since the presumptive assumption of assignment to Medicaid and QHP did not hold to
meet standards of using a regression discontinuity design based on parenthood status and an income forcing
variable, we chose to match the beneficiaries assigned to Medicaid and QHPs by using propensity scores. In total,
our analytic claims file contained 27,905 assigned to the General Population Medicaid plan and 92,940 assigned to
a General Population QHP. For CAHPS II, matching respondents meeting the new inclusion criteria produced an
analytic file containing 275 assigned to the Medicaid plan and 835 assigned to a QHP.
Theoretical Association Determination of Program Effect
Propensity score analysis is a post-hoc statistical method that estimates a treatment effect when subjects are not
randomly assigned to a treatment group. To test for the association of plan assignment and outcome, we
mitigated differences in assignment that may have been due to demographic or other factors attributing to the
assignment. Propensity scores are the probability of being assigned to a treatment group (i.e., a QHP) given a set
of underlying characteristics.
Propensity Score Matching
8
For claims and CAHPS II data separately, logistic regression models were fit modeling assignment to a QHP as the
treatment (1) and assignment to Medicaid as the control (0). Covariates used in the models included age, gender,
Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report E-6
race/ethnicity, Charlson comorbidity index (obtained from the complete first year experience in the program),
insurance region, and census block median income.
The propensity score associated with an individual (i) was estimated from the logistic regression with the
functional form of:
, where β is the vector of parameters to be fit in the model and associated with the vectors of
covariates listed above. The resulting propensity scores were matched using a greedy matching algorithm.
9
The
algorithm first attempts matches between Medicaid and QHP where the propensity score is identical to eight
decimal places. Unmatched treatment and controls are then attempted to be matched at a less restrictive seven
decimal places and this process continues until a caliper boundary of 0.005 is met. All remaining unmatched
treatment and controls are not entered in the analysis. For full population denominator indicators, we were able
to find matched one-to-one pairs of Medicaid and QHP enrollees in 99.7 percent of claims for Medicaid enrollees
and 94.2 percent of CAHPS II Medicaid enrollees. There were no standardized differences in any of the covariates
that were included in the logistic regression in claims, CAHPS II, and the special population pregnancy study.
The c-statistic of the claims data logistic regression model used to generate the propensity scores was 0.67, indicating a
moderate ability to differentiate between those assigned to a QHP and those with Medicaid coverage. The c-statistic
represents the discriminative power of the logistic regression model. The c-statistic of the CAHPS II data logistic
regression model was 0.63 and for the pregnancy study Medicaid and QHP match, the c-statistic was 0.87.
Matched pairs were accounted for in individual generalized linear models by using a random effect indicator for the
dyads. In reality, the number of matched pairs was too high for fitting a random effects model and we therefore
collapsed matched propensity scores into 100 groups (percentiles) and used this variable as a random effect.
References
1
Schochet P, Cook T, Deke J, Imbens G, Lockwood JR, Porter J, and Smith J. Standards for Regression Discontinuity Designs.
Retrieved from What Works Clearinghouse. Website http://ies.ed.gov/ncee/wwc/pdf/wwc_rd.pdf Accessed 8/6/2015.
2
McCrary, Justin. (2008) "Manipulation of the running variable in the regression discontinuity design: A density test," Journal
of Econometrics. 142(2): 698-714.
3
Guido Imbens & Karthik Kalyanaraman. Optimal Bandwidth Choice for the Regression Discontinuity Estimator. The
Review of Economic Studies. Vol. 79, No. 3 (July 2012), pp. 933-959.
4
MacKinnon JG, White H (1985). “Some Heteroskedasticity-Consistent Covariance Matrix Estimators with Improved Finite
Sample Properties.” Journal of Econometrics, 29, 305–325. doi:10.1016/0304-4076(85)90158-7.
5
Lee, D.S. and Card, D. (2008): “Regression discontinuity inference with specification error,” Journal of Econometrics, 142,
655–674.
6
Arkansas Center for Health Improvement. Arkansas Health Care Independence Program (“Private Option”) Section 1115
Demonstration Waiver Interim Report. Little Rock, AR: Arkansas Center for Health Improvement, March 2016.
7
Xu S, Ross C, Raebel MA, Shetterly S, Blachetter C, and Smith D. Use of stabilized inverse propensity scores as weights to
directly estimate relative risk and its confidence intervals. Value Health. 2010;13(2):273–277.
8
Guo S and Fraser MW. Propensity Score Analysis: Statistical Methods and Applications. Second edition. Thousand Oaks, CA:
Sage Publications, Inc; 2015.
9
Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques; 26th Annual SAS Users
Group International Conference; Long Beach, California: 2001.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report F- 1
Appendix F – Supplemental Payments, Claims Loading Process, and Per Member
Per Month Logic
The cost analysis focused on a comparison of health services provided to commercial qualified health plan (QHP)
enrollees in the Health Care Independence Program (HCIP) premium assistance program relative to health service
provision under a traditional Medicaid Fee-for-Service (FFS) program. The analysis required an assessment of the
costs of services provided under the two alternatives that can be compared to assessments of access,
effectiveness, and quality outcome measures. Our main hypothesis was that the provision of health services
through QHPs results in higher per member per month (PMPM) costs (payments) relative to traditional Medicaid,
but quality and access would be rated higher by enrollees in a QHP. Policymakers generally believe, and evidence
suggests, that access to healthcare services is improved within state Medicaid programs when payments for
primary care services increase.
1
,
2
If our hypothesis is confirmed, the findings provide information for policymakers to evaluate the trade-offs
between the cost of care, access to health services, and the quality of services provided. In all of our discussions of
cost, we follow the health services literature and define cost as the amount paid on behalf of beneficiaries by
insurance or Medicaid payers, plus the amount paid by the beneficiary.
In order to obtain a per member per month cost (PMPM) we used the claims data provided by Medicaid and QHPs
and incorporated in the Arkansas All-Payer Claims Database. As claims data are limited to claims paid, we had to
adjust claims for PMPM calculations to include important supplemental payments made by the Medicaid program
to providers. In Arkansas, providers receive payments based on upper payment limits (UPL) and cost-based
reimbursement from the state Medicaid program. We define supplemental payments as any payment made for
the utilization of services that were not paid through claims. Supplemental payments totaled $596,142,904.30 in
fiscal year 2016, including disproportionate share hospital payments (DSH). As these payments are made for
services provided, they should be incorporated into the costs of claims paid, rather than treated as an
administrative cost allocated across all beneficiaries. The process for measuring supplemental payments and
allocating them to claims is discussed below.
Both UPL payments and cost-based reimbursements for inpatient and hospital outpatient services were identified
for every hospital receiving them from the Division of Medicaid Services (DMS). As there is inconsistent use of
cost-reports and different resource pools for allocating supplemental payments to generate payment algorithms,
UPL and cost-based reimbursement were averaged across four categories of hospitals: academic (UAMS), private,
critical access, and public hospitals.
Specifics of this allocation are contained in Table 1. Allocation of inpatient supplemental payments was
straightforward as these payments are based on discharges and not days. However, allocation of outpatient
hospital supplemental payments proved difficult to identify and, as such, were also allocated with inpatient
hospitalizations. Sensitivity analyses were performed to test the effect of adding hospital outpatient to
inpatient claims.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report F- 2
Table 1. Allocation for 2016 Supplemental Payments by Hospital Category
Hospital Category
Inpatient
UPL/Discharge
Outpatient
UPL/Discharge
Cost-Based
Reimbursement
Total Supplement
Academic (UAMS)
$2,699.00
N/A
$1,148.00
$3,847.00
Private
$2,946.00
$983.00
$20.00
$3,949.00
Critical Access
$4,172.00
$2,419.96
$5,144.00
$11,735.00
Public
$6,621.00
$150.77
$0.00
$6,771.00
Average/Discharge
$3,093.00
$889.00
$309.00
$4,529.00
Total costs were calculated as the sum of claims costs plus administrative costs for both Medicaid and QHPs. For
Medicaid administrative costs as depicted in Table 2, we identified expenditures for services across all agencies
associated with Medicaid that received matching funds from the federal government. We also identified other
payments made by DMS that could not be included in claims such as physician payments for rate adjustments,
case management services, contracts, and payments for quality improvement initiatives.
Table 2. Administrative Costs for 2016
Administrative Cost
Non-Fixed
Fixed
Others
All Costs
64.10 Base and Waivers
$375,059,126.00
21. Children’s Health Insurance Program (CHIP)
$625,391.00
Inpatient Quality Incentive (IQI) Payment
N/A
64.10's Net
$7,774,710.00
Disproportionate Share to Hospitals (DSH)
N/A
Graduate Medical Education (GME)
$10,319,457.00
Physician Rate Adjustment (UAMS)
$35,954,166.00
Physician Services
N/A
Prescription Drug – Clawback
N/A
Case Management
N/A
Payment to Federally Qualified Health Center
(FQHC)
N/A
Total
$411,013,292.00
$18,719,558.00
$0.00
$429,732,850.00
PMPM Admin
$45.17
$2.06
$47.23
Note: We were unable to report $1,978,130 Total Cost of CQ/64.10B, line 2B (FFY16 Q1), Medicaid Management Information (MMIS)
related cost this quarter due to insufficient allotment available. There will be a PPA in FFY16 Q2. It is not included in this total.
Abbreviations: PMPM=total administrative cost/total enrollee months in Medicaid (excluding 06 commercial months).
Calculation of Per Member Per Month Payments
This section describes the calculation of per member per month (PMPM) payments made by the Arkansas
Medicaid program for services provided to people in one of our study groups — newly insured parents with
incomes at or below 17 percent of the federal poverty level (FPL). People in this group received traditional
Medicaid benefits that did not change as a result of Medicaid expansion. Given the benefit structure and
population, we report in this section actual service utilization and payment measures, including PMPM payments
for the 174,167 enrollees in our analytical sample — all of whom had at least six months of coverage. Payments
were categorized as inpatient, outpatient emergency room (ER) visits, outpatient physician visits, prescription
drugs, and other services that fell outside of these categories.
Utilization and payment of services are presented using the following measures: the percentage of enrollees
who use the service category, the amount of spending for the service category conditional on having positive
spending (or the probability of positive spending), the average spending on the category conditional on
having positive spending, and per person spending defined as total spending for the category divided by the

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report F- 3
number of enrollees in the group. PMPM payment was calculated by dividing average payment pe r person by
average member months. Per member per year (PMPY) payment was calculated by multiplying PMPM
payment by 12 months.
Table 3 provides observed payments for traditional Medicaid and QHP enrollees on a per member per month
basis by service category, administrative costs, and overall. Also, we present estimates of PMPM payments based
on an additional method. PMPM payments were calculated similarly for both traditional Medicaid and QHP
enrollees by summing adjudicated claims for the different categories of services and then summing the total
months of services for each enrollee. PMPM payments are defined as total payments divided by total months of
coverage. Service categories for both traditional Medicaid and QHP enrollees were defined as inpatient,
prescription drugs, outpatient ER visits, outpatient physician, and all other services including outpatient
ambulatory surgeries, labs, imaging, and other services that could not be assigned. Inpatient services include ER
services that resulted in an admission, as well as other labs, imaging, and other services that could be identified as
occurring during the inpatient hospitalization.
Table 3. Observed and Estimated Per Member Per Month Cost Scenarios for Traditional Medicaid and
QHP Enrollees by Service Category (2016)
Per Member Per Month (PMPM) Observed and Estimated Costs (2016)
Service Category
Observed Medicaid
Commercial
Premiums
Observed
Commercial
Estimated
Medicaid
Inpatient
$86.85
$123.99
$82.58
Emergency Room
$13.61
$44.16
$12.45
Physician’s Office
$31.36
$65.68
$37.27
Outpatient
$9.17
$11.63
$13.37
Prescription Medications
$40.27
$113.18
$48.15
Other
$64.44
$146.49
$62.83
Non-Emergency Transport Fees
$3.65
$4.04
$0.01
Total Claims PMPM
$249.35
$509.17
$256.66
Administrative PMPM
3,4
$63.58
$91.65
$63.58
Total PMPM
$312.93
1
$478.14
2
$600.82
3
$320.24
4
Notes:
1
Average PMPM represents loaded (i.e., cost-based reimbursement, supplemental payments, etc.) claims from Traditional Medicaid.
2
The average PMPM payment made to QHP carriers includes cost-sharing and wrap services.
3
Includes PMPM Administrative costs for
Observed QHP claims, which were set at 18 percent of the total claims paid excluding copayments and deductibles.
4
Average PMPM
represents claims costs based on average Medicaid pricing.
Column 1 (Observed Medicaid) provides PMPM payments for enrollees in traditional Medicaid that had
incomes below 17 percent of FPL. PMPM payments were much lower than for QHP enrollees because of the
differences in prices paid for services between the two programs. The largest difference in PMPM payments
were found in the “Other” category, suggesting the need for a greater understanding of spending in this
category across the two programs. Administrative costs for traditional Medicaid were based on an exhaustive
examination of spending across all Department of Human Services categories that were eligible for matching
funds from the federal government. Spending on disproportionate share adjustments and Graduate Medical
Education were included as these are paid by the Medicaid program to deliver services. Total administrative
spending was divided by total enrollee member months excluding QHP enrollees to generate PMPM payments
for administrative services ($63.58).

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report F- 4
Column 3 (Observed Commercial) of Table 3 shows that PMPM payments for enrollees in a QHP incurred $509.17
in payments per month with the majority of payments incurred for Inpatient and Other services. Total payments
included administrative loading costs that were estimated to be 18 percent of total claims paid ($91.65 PMPM)
resulting in total monthly payments of $600.82.
Column 4 (Estimated Medicaid) provides PMPM costs for QHP enrollees under the assumption that payments for
services would reflect the prices paid in the Medicaid program. Under this methodology, prices for services were
altered to reflect the experience of the traditional Medicaid population, while holding utilization of services for
the QHP enrollees constant. Allowing prices to change for the QHP enrollees substantially reduced estimated
PMPM expenditures with the largest change occurring for Inpatient and Other services. Administrative payments
were calculated by excluding payments that would not change irrespective of how the program was financed. DSH
payments and GME payments would not change with a difference in volume following the implementation of
HCIP and were considered fixed costs. In calculating administrative payments for only services associated with the
volume of the program, there was no change in administrative payments. Total payments were estimated to be
$320.24 PMPM.
References
1
Decker SL. Medicaid Physician Fees and the Quality of Medical Care of Medicaid Patients in the USA. Rev Econ Household
(2007). 5:95-112.
2
Pauly MV. Lessons to Improve the Efficiency and Equity of Health Reform. Hastings Center Report (2012). 42(5):21-24.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report G- 1
Appendix G – Geographic Information System (GIS) Processing
The Center for Advanced Spatial Technologies (CAST) was founded in September 1991 within the University of
Arkansas, J. William Fulbright College of Arts and Sciences by the Board of Trustees and the Arkansas Department
of Higher Education. Research efforts include multi-disciplinary projects from all around the world. CAST is funded
by competitive grants and research proposals from federal and state government offices, universities, nonprofit
groups, and other organizations.
Medicaid and commercial qualified health plan (QHP) enrollees and provider data (i.e., Blue Cross Blue Shield,
Ambetter, and QualChoice) were used to assess network adequacy and perform GIS mapping. For the analysis,
“access” was defined as the distance (30 or 60 miles) or time of travel (30 or 60 minutes by passenger automobile)
from any enrollee’s location to the nearest provider, within an “access ring” offering any of the eight categories of
healthcare provider types (primary care, orthopedics, ophthalmology, OB/GYN, oncology, surgical, psychology, and
cardiology). These “access rings” were created by computing four distinct travel distances and time-of-travel attributes
from each unique provider location (latitude and longitude coordinates) for each provider type. From each provider
location, a set of four miles traveled along the existing (ESRI, 2013) street centerline networks were computed as
“ringed-polygons” at the following distance rings: 0-15, 15-30, 30-45, and 45-60 miles.
Only providers that practiced within calendar year 2014 were included in the analyses. It is important to note that as
both enrollees and providers included out-of-state addresses, ACHI and CAST agreed, for this analysis, to compile travel
distances or travel-time polygons from any provider that was located within 70 miles of the Arkansas state boundary. It
was not uncommon for enrollees living near a state border to seek health care from a provider across the border.
De-identified data were sent to CAST for analysis. CAST returned to ACHI four provider-enrollee data tables
each — for Medicaid and the three QHPs. An additional data file combining all commercial enrollees and
providers was also prepared and returned. QHP enrollees were encouraged to seek care with a provider inside
a QHP, but were not pre-empted from going out-of-network. Within each enrollee dataset, fields containing
minutes and miles to each provider type were included, along with the geocoded locations for the enrollee. A
geocoded provider file listing was also returned to ACHI.
More specifics of the data processing steps used by CAST can be found on the following pages.
CAST was responsible for the development of the following products for the Arkansas Center for Health
Improvement (ACHI) between Oct. 20, 2015, and Feb. 15, 2016:
1. geocoded locations (latitude/longitude; WGS84) for all ENROLLEES and PROVIDERS of each of four
specified insurance programs,
2. “access zones” for each of the eight provider “specialties” for each of the four specified insurance
programs, based upon both drive-time (minutes) and distance (miles) criteria, plus the
3. updated tables for all geocoded ENROLLEES of each of the specified insurance providers,
indicating the time/distance zones that enrollees fall within for each PROVIDER specialty, and
4. delivery of GIS results as they were completed.
All work was performed on a physically and electronically secure computer, disconnected from any networks. The
specific methods for generating each of these products were as follows:
1. Geocoding and GIS data processing for four Arkansas-based healthcare PROVIDERS and their current
ENROLLEE tables obtained by ACHI and provided as .csv files (with schema descriptions) to CAST:

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report G- 2
a. CAST imported each provider and their enrollee tables (while maintaining ACHI-generated
unique IDs) into an ArcGIS File Geodatabase format.
b. Geo-locations for each providers’ facility address and each of their enrollee home
addresses were assigned using the best available Arkansas GIS locator(s) as the first-pass
for each provider (and their enrollee tables). The GIS locator used for Arkansas (“GeoStor
Composite” address locator, Arkansas GIS Office) leveraged our statewide 911 street
address datasets from 2015, which included street centerline AND address points (any
911 addressed structure), plus the fallback of the nine-digit zip code centroids (e.g.
73722-2356) located within the state of Arkansas. We set the minimum match score of
“65” (0-100) for these geocoded addresses. Any original misspellings or address issues
found within the source data tables were not corrected by CAST.
c. For the second-pass of geo-locating any remaining records that were not geocoded within
the first pass, we also re-ran the resulting “non-located” records against ESRI’s nationwide
street centerline network (updated in 2013), so that we could achieve a street-level
geocode for any remaining records that MAY have been missed within Arkansas OR that
were located outside of the state boundary.
d. The results of these two attempts to locate each and every record within all four provider
and enrollee tables were then MERGED into a common, single database table schema
grouped by healthcare provider. We maintained the original ACHI attributes contained
within each table and ADDED VALUE to each of these tables by providing the
latitude/longitude coordinates (WGS84), along with additional metadata references such
as: Locator Name, Status, Score, Match Type, and the resulting Matching Address from
the GeoLocator used to geocode each record. These additional attributes were appended
to each of the original data tables from ACHI, which also contained the original data table
“unique ID,” which was generated in-house by ACHI to help maintain anonymity for all
providers and their enrollees.
2. Determination of each healthcare enrollee’s “ACCESS” to each of the eight categories of provider-
specific services WITHIN and OUTSIDE OF each provider network:
a. ACHI originally defined “access” as the distance (30 or 60 miles) or time of travel (30 or 60
minutes by passenger automobile) from any enrollee’s location to the nearest provider
offering any of the eight categories of healthcare provider services (primary care,
orthopedics, ophthalmology, OB/GYN, oncology, surgical, psychological, and cardiology).
CAST proposed that ACHI compute a total of four distinct travel distances and time-of-travel
attributes from each unique provider location (latitude/longitude coordinates) for each
provider type. Therefore, from each provider location a set of four MILES-traveled along the
existing (ESRI, 2013) street centerline networks were computed as “ringed-polygons” at the
following distance rings: 0-15, 15-30, 30-45; 45-60 MILES.
b. The same provider locations and nationwide street network dataset (ESRI, 2013) was used
to ALSO compute a set of TIME-traveled (MINUTES) ringed-polygon buffers out from each
provider location — following the same street network dataset. The TIME-traveled was
computed using the ArcGIS Network Analyst extension for each provider location using
“typical” driving conditions for a passenger car traveling the posted speed limits along
each street segment as a hypothetical enrollee travels to or from each provider location
(geocoded latitude/longitude coordinate). These travel-time-in-minutes were created in

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report G- 3
sets of four from each provider and attributed as: 0-15, 15-30, 30-45, and 45-60 minute
ringed-polygon geometries.
c. It is important to note that ACHI and CAST agreed to ONLY compile travel distances or
travel-TIME polygons from any provider located within 70 miles of the Arkansas state
boundary. It was determined that it is very common for enrollees in a healthcare network
to travel across state lines to access any of the eight provider specialties as long as they
were “in-network” facilities.
d. The resulting set of provider polygon files enabled us to summarize the following
information for each provider.
e. Joining the original PROVIDER services-offered at each Unique Location enabled us to
select each “Services Provided” attribute and then “Merge Polygons” (actually, DISSOLVE)
by travel time or distance so that we would end up with 32 unique GIS data layers
(polygon geometry) for each provider specialty of the four unique providers (Blue Cross
Blue Shield, Medicaid, QualChoice, and Ambetter).
3. Once each of the four unique providers (Blue Cross Blue Shield, Medicaid, QualChoice, and Ambetter)
had their travel DISTANCE buffers (miles) and TIME-OF-TRAVEL (minutes) computed with four distinct
zones for each provider specialty, they could be used to leverage the spatial analysis of our
geographic information systems by using a “spatial selection” of the complete set of ENROLLEE
address locations (latitude/longitude geocodes) against each of their corresponding “in-network”
provider SPECIALITY with their travel distance/time merged buffers. We prepared each of the four
CAST geocoded provider-ENROLLEE tables with the eight provider services specified by ACHI within
this study and we processed all of those enrollee records using this methodology:
a. Add eight attribute columns needed to store each provider specialty (long integer).
b. Update any enrollee addresses that were NOT geocoded to the value “1111.”
c. Reverse the selection and then update all remaining records to the value “9999” within
EACH of the eight ACHI provider specialty columns.
d. We agreed that this value (“9999”) would represent any member located BEYOND our
cut-off of 60 miles or 60 minutes travel time from any of the eight provider specialty
columns. Therefore, we pre-populated those values before processing a series of “spatial
selections” between our ENROLLEE (point features) and the full-set of 32 travel polygons
grouped by distance and provider specialty (polygon feature classes).
e. For each ENROLLEE table we would methodically work through each of the eight provider
specialty TYPES using a SELECT BY LOCATION command and working our way from the
GREATEST distance or time; INWARD towards the nearest/shortest travel time. Each
enrollee record would be OVERWRITTEN or updated with ONE of these FOUR values (60,
45, 30, 15), which would indicate (depending upon the ENROLLEE table — MILES or
MINUTES — the quickest “level of access” each enrollee has to ANY provider within their
healthcare network for each of the eight specialty types.
4. Resulting Data Delivery: The four provider enrollee data tables were delivered as .csv and .xlsx
formats to ACHI using a secure FTP protocol and with AES-256 encryption applied. Within each
provider dataset a MINUTES and MILES-traveled table for each of the original enrollee records
were provided with a supporting CODE BOOK detailing the attribute columns and attribute values
contained within the delivery

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report H- 1
Appendix H – Weighted Average Price Calculations
To determine the average weighted price for Medicaid and Qualified Health Plans (QHPs), the paid amount listed
on the paid claims were rolled up on procedure codes for office visits for high utilization provider specialties. It
was anticipated that all payer/provider combinations were likely to have claims with office visits coded in a similar
manner regardless of provider specialty. This allows us to compare pricing across procedures and providers. One
limitation of these analyses is that not all payers used the same provider specialty codes to identify the different
provider types studied. In general, payers used provider specialty codes that were consistent with Medicare
coding. The only difference between payers was that the two smaller payers omitted the leading zero character
from the specialty code. Medicaid provider specialty codes are constructed with both typical Medicare provider
specialty codes and Medicaid specific provider specialty codes (See Table 1).
Table 145. Provider Specialty Codes Selected for Comparison
Provider Specialty
Medicaid
Centene/
QualChoice
BCBS
Primary Care Physician
01, 08, 11
1, 8, 11
01, 08, 11
Advanced Practice Nurse (APN)
N0, N6, N7
50
Cardiologist
06
6
06
General Surgeon
02
2
02
Obstetrician/Gynecologist (OB/GYN)
16, 19
16
Oncologist
X1
83, 90, 91, 98
Ophthalmologist
18
18
Orthopedist
X6
20, 57
Psychologist/Psychiatrist
26, 62
26, 62, 68
In order to calculate the weighted average price, claims were extracted from Medicaid medical and UB92 paid claims
and the medical paid claims from the QHP files if they contained any of the procedure codes listed in Table 2. These
claims were further reduced by extracting only those with the provider specialties listed in Table 1. The total and
average paid amounts, as well as claim counts were determined by procedure code for each provider specialty, for
each payer type (Medicaid and combined QHPs). For each provider specialty the Medicaid average paid amount was
multiplied by the number of commercial claims for procedure codes and summed, which gave a total cost for
Medicaid procedures at QHP reimbursement rates. It is important to note that only procedure codes that were
represented both in Medicaid and QHP claims were included in the weighted averages. This total was then divided
by the total number of QHP claims for the matching procedures to obtain a weighted average price.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report H- 2
Table 2. Procedure Codes and Their Descriptions
Code Ranges
Code Descriptions
CPT Codes
99201–99206
Office or other outpatient visit (New patient 10/20/30/45/60 minutes)
99211–99215
Office or other outpatient visit for the evaluation and management of an established
patient that may not require the presence of a physician or other qualified healthcare
professional (10/15/25/40 minutes)
99241–99245
Office consultation for a new or established patient
99343; 99347–99349
Home visit for the evaluation and management of a new/established patient
99384–99387
Office or other outpatient visit — preventive (new patient)
99394–99397
Office or other outpatient visit — preventive (established patient)
99401–99402
Preventive medicine counseling and/or risk factor reduction intervention(s) provided to
an individual (separate procedure); approximately 15/30 minutes
HCPCS Codes
G0438
Annual wellness visit, initial (AWV)
G0463
Hospital outpatient clinic visit for assessment and management of a patient
T1015
Clinic visit/encounter, all-inclusive
Note: Ranges of procedure codes for office visits are listed for simplicity. The difference within the codes in these ranges is
based on the level of care a patient would need for that visit.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report I- 1
Appendix I – Pregnancy Analytic Profile
This appendix contains additional technical and analytical information not presented in the body of the report,
including a detailed description and flow chart of the inclusion/exclusion criteria used to derive the analytical
sample, as well as the socioeconomic and health related demographics that were used to develop the propensity
scores.
Steps for inclusion / exclusion criteria in prenatal and post-partum visits:
1. All births in the birth certificate data having a mother participating in a QHP or in Medicaid were
selected (n = 34,675).
2. All births occurring on or between Sept. 1, 2014, and Sept. 30, 2015, were retained (n = 17,605).
3. Mothers and associated births which did not have delivery claims in the medical claims file were
removed (n = 15,734).
4. Infants must have been live-born according to the birth certificate (n = 15,597).
5. Mothers must have had continuous enrollment for 43 days prior to and 56 days after the date of
birth in any one of the following enrollment aid categories: 06, 20, 25, or 6X (except 69) (n =
14,502).
6. Mothers and associated births were excluded if:
a. The mother had enrollment segments other than 69 prior to Oct. 15, 2013 (n = 10,864).
b. The mothers had enrollment segments for dual eligibility, physical disability or mental
retardation (10, 11, 13, 14, 16, 17, 18, 31, 33, 34, 35, 36, 37, 38, 41, 43, 44, 45, 46, 47, 48,
49, 58, 78, 88) at any time during 2014/2015 (n = 10,862).
c. There were two or more claims more than 30 days apart any time during 2014/15 from
an institutionalized facility based on place of service codes (09 , 13, 14, 31, 34, 55, and
56) (n = 10,862).
7. Births with same mother and date of delivery were only counted once while births on different
dates were counted as separate births (n = 10,722).
8. Mother-birth pairs were excluded if the assigned Private Option identifier was associated with
multiple provider IDs (Medicaid or private) (n = 10,711).
9. Mothers with more than one switch between Medicaid coverage and commercial coverage were
removed (n = 10,692).
10. Mothers must have spent at least 50 percent of the prenatal time in the enrollment segment
closest to the delivery (n = 10,467).
11. Mothers who were missing data in the “Previous live births” or “Previous births now deceased”
were excluded (n = 10,453).
Subpopulation studied: Mothers who did not have continuous enrollment prior to delivery going back up to week
24 of gestation (n = 9,943).
To analyze the population, a propensity scored one-to-one matched sample with a caliper of 0.005 was created
and analyzed (matched n = 2,369). Medicaid beneficiaries were considered as the control group and compared
with those in the QHP.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report I- 2
Figure 1. Flow Diagram Depicting the Development of the Analyzable Study Population
Total prenatal and post-partum visits starting with all births found
in the birth certificate data having a mother POID
N = 34,674
N = 15,597
Exclude mother POIDs and associated births with no
delivery claims
N = 1,871
N = 10,864
Exclude persons not continually enrolled for 43 days
prior to date of birth and 56 days after date of birth
N = 1,095
Analyzable Study Population
N = 10,453
Exclude persons who are dually eligible, disabled or
institutionalized in 2014
N = 2
Exclude POIDS and births associated with coverage
discrepancies
N = 11
Exclude births prior to September 1, 2014, and after
September 30, 2015
N = 17,069
Exclude births with deceased status on the birth
certificate
N = 137
Exclude those who made more than one switch between
Medicaid and Commercial plans
N = 19
Deduplicated all births with same mother POID and and date
of delivery
N = 140
Exclude persons that had enrollment segments other
than “69" prior to October 15, 2013
N = 3,638
Exclude those who spent less than 50% of the prenatal time
in the enrollment segment closest to delivery
N = 225
Exclude those who had missing “previous live births” or
“previous births now deceased”
N = 14

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report I- 3
Table 1. Socio-Economic Demographics Selected as Covariates
Raw Sample
Matched Sample
Medicaid
N=7,583
QHP
N=2,870
Medicaid
N=2,369
QHP
N=2,369
Covariates
Category
N
Percent
N
Percent
N
Percent
N
Percent
Mother’s age
25 years old or less
3,749
49.4
1,067
37.2
986
41.6
999
42.2
25 ≤ 30 years old
2,218
29.3
1,037
36.1
830
37.4
812
34.3
30 ≤ 35 years old
1,149
15.2
569
19.8
397
16.8
411
17.4
35 ≤ 40 years old
397
5.2
163
5.7
134
5.7
121
5.1
40 and above
70
0.9
34
1.2
22
0.9
26
1.1
Mother’s
education
No high school
diploma
1,435
18.9
375
13.1
327
13.8
343
14.5
High school diploma
or GED
5,259
69.4
2,056
71.6
1,721
72.7
1,704
71.9
Some college
441
5.8
235
8.2
171
7.2
174
7.3
Bachelor’s degree
340
4.5
163
5.7
112
4.7
115
4.9
Graduate degree
57
0.8
28
1.0
29
0.9
27
0.9
Unknown
51
0.7
13
0.5
16
0.7
12
0.5
WIC
Yes
5,661
74.7
2,096
73.1
1,750
73.9
1,771
74.8
No
1,803
23.8
724
25.2
577
24.4
563
23.8
Unknown
119
1.6
49
1.7
42
1.8
35
1.7
Race
Hispanic
1,138
15.0
149
5.2
126
5.3
148
6.3
Non-Hispanic Black
1,635
21.6
898
31.3
647
27.3
630
26.6
Non-Hispanic White
4,605
60.7
1,790
62.4
1,570
66.3
1,558
65.8
Other
205
2.7
33
1.2
26
1.1
33
1.4
City Birth
Yes
5,880
77.5
2,157
75.2
1,778
75.1
1,781
75.2
No
1,530
20.2
656
22.9
678
23.7
656
22.9
Unknown
173
2.3
57
2.0
48
2.0
48
2.0
Region code
Central
2,383
31.4
922
32.1
747
31.5
758
32.0
Northeast
1,219
16.1
514
17.9
442
18.7
431
18.2
Northwest
1,502
19.8
463
16.1
392
16.6
397
16.8
South Central
471
6.2
190
6.6
152
6.4
147
6.2
Southeast
683
9.0
333
11.6
239
10.1
246
10.4
Southwest
379
5.0
162
5.6
130
5.5
130
5.5
West Central
917
12.1
282
9.8
263
11.1
256
10.8
Unknown
29
0.4
--
--
--
--
--
--
Marital Status
Currently married
2,709
35.7
1,010
35.2
825
34.8
826
34.9
Never married
1,985
26.2
722
25.2
634
26.8
604
25.5
Previously married
2,889
38.1
1,138
39.7
910
38.4
939
39.6
Notes: Cells with “--” indicate counts that are 10 or less. Percentages are rounded and may not add up to precisely 100 percent.
Abbreviation: QHP=qualified health plan

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report I- 4
Table 2. Health-Related Demographics Selected as Covariates
Raw Sample
Matched Sample
Medicaid
N=7,583
QHP
N=2,870
Medicaid
N=2,369
QHP
N=2,369
Covariates
Category
N
Percent
N
Percent
N
Percent
N
Percent
Enrollment duration during pregnancy
(in months)
219
63.4
275
18.2
274
21.1
274
19.9
Body Mass
Index (BMI)
underweight
279
3.7
84
2.9
71
3.0
80
3.4
normal
2,681
35.4
950
33.1
799
33.4
798
33.7
overweight
1,857
24.5
663
23.1
544
23.0
559
23.6
35 > BMI >= 30
1,252
16.5
470
16.4
424
17.9
403
17.0
40 > BMI >= 35
673
8.9
303
10.6
236
10.0
228
9.6
BMI 40 and above
596
7.9
327
11.4
236
10.0
243
10.3
not populated
245
3.2
73
2.5
59
2.5
58
2.5
Pre-pregnancy
diabetes
Yes
2,222
29.3
935
32.6
968
33.8
931
32.5
Previous
cesarean
Yes
1,242
16.4
545
19.0
438
18.5
432
18.2
Pre-pregnancy
hypertension
Yes
114
1.5
60
2.1
47
2.0
44
1.9
Preterm
birth risk
Yes
286
3.8
125
4.4
96
4.1
102
4.3
Chlamydia
Yes
270
3.6
94
3.3
73
3.1
77
3.3
Gonorrhea
Yes
32
0.4
16
0.6
12
0.5
11
0.5
Hepatitis B/C
Yes
38
0.4
22
0.7
12
0.5
13
0.6
Syphilis
Yes
17
--
--
--
--
--
--
--
Single/multiple
birth
One baby (single)
7,477
98.6
2,826
98.5
2,336
98.6
2,336
98.6
Multiples
106
1.4
44
1.5
33
1.4
33
1.4
Number of living children
1.26
1.32
1.35
1.32
1.34
1.31
1.31
1.29
Number of deceased children
0.03
0.2
0.04
0.2
0.03
0.2
0.04
0.2
Notes: Cells with “--” indicate counts that are 10 or less. Percentages are rounded and may not add up to precisely 100 percent.
Abbreviation: QHP=qualified health plan

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report J- 1
Appendix J – Opioid Use Outcomes
The tables contained in this Appendix complement the data and information presented in the special section
comparing the differences in opioid use between Medicaid and QHP enrollees. Type of opioid was stratified by
Schedule III to V opioid use, short-acting Schedule II opioid use, any long-acting Schedule II opioid use, and by
specific drug types. Only oral and transdermal opioid analgesics were examined — opioid-containing cough and
cold preparations were excluded.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report J- 2
Table 1: Schedule of Opioids and Specific Types by General Population Enrollees and Prescriptions
Baseline
Follow-Up Year 1
Follow-Up Year 2
QHP
Medicaid
QHP
Medicaid
QHP
Medicaid
Enrollees
N
Percent
N
Percent
Enrollees
N
Percent
N
Percent
Enrollees
N
Percent
N
Percent
Total Enrollees
27,838
100
27,838
100
Total Enrollees
27,838
100
27,838
100
Total Enrollees
12,657
100
13,937
100
No Opioid Use
19,004
68.3
18,140
65.2
No Opioid Use
18,278
65.7
18,842
67.7
No Opioid Use
7,825
61.8
9,840
70.6
Opioid Use
8,834
31.7
9,698
34.8
Opioid Use
9,560
34.3
8,996
32.3
Opioid Use
4,832
38.2
4,097
29.4
Opioid Schedule
Opioid Schedule
Opioid Schedule
III, IV, V Only
1,605
18.2
1,609
16.6
III, IV, V Only
2,141
22.4
1,748
19.4
III, IV, V Only
1,098
22.7
861
21.0
II SA Only
4,640
52.5
5,766
59.5
II SA Only
4,484
46.9
4,914
54.6
II SA Only
2,294
47.5
2,322
56.7
II LA Any
199
2.3
203
2.1
II LA Any
273
2.9
278
3.1
II LA Any
138
2.9
125
3.1
III, IV, V, II SA Only
2,390
27.1
2,120
21.9
III, IV, V, II SA Only
2,662
27.9
2,056
22.9
III, IV, V, II SA Only
1,302
27.0
789
19.3
Total
8,834
100.1
9,698
100.1
Total
9,560
100.1
8,996
100
Total
4,832
100.1
4,097
100.1
Specific Type
Specific Type
Specific Type
Hydrocodone
6,385
72.3
6,973
71.9
Hydrocodone
6,382
66.8
6,052
67.3
Hydrocodone
3,189
66.0
2,692
65.7
Oxycodone
1,945
22.0
2,078
21.4
Oxycodone
2,248
23.5
2,061
22.9
Oxycodone
1,137
23.5
876
21.4
Tramadol
3,092
35.0
2,609
26.9
Tramadol
3,545
37.1
2,598
28.9
Tramadol
1,699
35.2
1,084
26.5
Baseline
Follow-Up Year 1
Follow-Up Year 2
QHP
Medicaid
QHP
Medicaid
QHP
Medicaid
Prescriptions
N
Percent
N
Percent
Prescriptions
N
Percent
N
Percent
Prescriptions
N
Percent
N
Percent
II SA
26,645
69.6
23,852
73.0
II SA
29,240
63.5
23,738
69.1
II SA
15,563
63.9
10,071
69.0
II LA
1,016
2.9
949
2.9
II LA
1,601
3.5
1,418
4.1
II LA
859
3.5
576
3.9
III, IV, V
10,613
27.7
7,857
24.1
III, IV, V
15,199
33.0
9,223
26.8
III, IV, V
7,949
32.6
3,958
27.1
Total
38,274
100.2
32,658
100
Total
46,040
100
34,379
100
Total
24,371
100
14,605
100
Specific Type
Specific Type
Specific Type
Hydrocodone
21,136
55.2
18,948
58.0
Hydrocodone
21,754
47.3
17,921
52.1
Hydrocodone
11,737
48.2
7,630
52.2
Oxycodone
5,131
13.4
4,533
13.9
Oxycodone
7,261
15.8
5,521
16.1
Oxycodone
3,696
15.1
2,406
16.5
Tramadol
7,844
20.5
5,466
16.7
Tramadol
10,305
22.4
5,999
17.5
Tramadol
5,286
21.7
2,519
17.3
Note: III, IV, V only=either Schedule III or Schedule IV or Schedule V prescription only; II SA only=use of Schedule II Short Acting only; II LA only=use of Schedule II Long Acting only; III, IV, V, II SA Only=use of
Schedule III or Schedule IV or Schedule V drugs with Schedule II Short Acting only. Percentages are rounded and totals may not add up to precisely 100 percent.
Abbreviations: N=number of persons; SA=short acting; LA=long acting; QHP=Qualified Health Plans.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report J- 3
Table 2: Schedule of Opioids and Specific Type by Higher Needs Population Enrollees and Prescriptions
2014
2015
2016
QHP
Medicaid
QHP
Medicaid
QHP
Medicaid
Enrollees
N
Percent
N
Percent
Enrollees
N
Percent
N
Percent
Enrollees
N
Percent
N
Percent
Total Enrollees
44,285
100
9,037
100
Total Enrollees
44,285
100
9,037
100
Total Enrollees
37,752
100
7,951
100
No Opioid Use
28,334
64.0
3,872
42.9
No Opioid Use
27,685
62.5
4,384
48.5
No Opioid Use
23,366
61.9
4,008
50.4
Opioid Use
15,951
36.0
5,165
57.2
Opioid Use
16,600
37.5
4,653
51.5
Opioid Use
14,386
38.1
3,943
49.6
Opioid Schedule
Opioid Schedule
Opioid Schedule
III, IV, V only
2,786
17.5
683
13.2
III, IV, V only
3,739
22.5
924
19.9
III, IV, V only
3,243
22.5
795
20.2
II SA only
9,132
57.3
3,095
59.9
II SA only
8,039
48.4
2,398
51.5
II SA only
7,124
49.5
2,061
52.3
II LA any
253
1.6
195
3.8
II LA any
358
2.2
225
4.8
II LA any
403
2.8
267
6.8
III, IV, V, II SA only
3,780
23.7
1,192
23.1
III, IV, V, II SA only
4,464
26.9
1,106
23.8
III, IV, V, II SA only
3,616
25.1
820
20.8
Total
15,951
100
5,165
100
Total
16,600
100
4,653
100
Total
14,386
100
3,943
100
Specific Type
Specific Type
Specific Type
Hydrocodone
11,850
74.3
3,976
77.0
Hydrocodone
11,081
66.8
3,053
65.6
Hydrocodone
9,489
66.0
2,563
65.0
Oxycodone
3,027
19.0
1,110
21.5
Oxycodone
3,658
22.0
1,172
25.2
Oxycodone
3,193
22.2
963
24.4
Tramadol
5,259
33.0
1,500
29.0
Tramadol
6,001
36.2
1,466
31.5
Tramadol
4,968
34.5
1,119
28.4
2014
2015
2016
QHP
Medicaid
QHP
Medicaid
QHP
Medicaid
Prescriptions
N
Percent
N
Percent
Prescriptions
N
Percent
N
Percent
Prescriptions
N
Percent
N
Percent
II SA
44,620
71.5
17,824
77.9
II SA
46,973
63.1
16,535
70.2
II SA
43,201
63.4
14,210
70.4
II LA
1,102
1.8
957
4.2
II LA
2,306
3.1
1,401
6.0
II LA
2,624
3.9
1,350
6.7
III, IV, V
16,657
26.7
4,102
17.9
III, IV, V
25,114
33.8
5,613
23.8
III, IV, V
22,372
32.8
4,622
22.9
Total
62,379
100
22,883
100
Total
74,393
100
23,549
100
Total
68,197
100
20,182
100
Specific Type
Specific Type
Specific Type
Hydrocodone
37,190
59.6
14,161
61.9
Hydrocodone
35,895
48.3
11,729
49.8
Hydrocodone
32,643
47.9
10,273
50.9
Oxycodone
6,933
11.1
3,344
14.6
Oxycodone
10,535
14.2
4,467
19.0
Oxycodone
10,134
14.9
3,862
19.1
Tramadol
13,216
21.2
3,223
14.1
Tramadol
17,731
23.8
3,737
15.9
Tramadol
15,976
23.4
2,978
14.8
Note: III, IV, V only=either Schedule III or Schedule IV or Schedule V prescription only; II SA only=use of Schedule II Short Acting only; II LA only=use of Schedule II Long Acting only; III, IV, V, II SA Only=use of
Schedule III or Schedule IV or Schedule V drugs with Schedule II Short Acting only. Percentages are rounded and totals may not add up to precisely 100 percent.
Abbreviations: N=number of persons; SA=short acting; LA=long acting; QHP=Qualified Health Plans

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 1
Appendix K – Consumer Assessment of Healthcare Providers and Systems
(CAHPS) Sample Size Calculation, Sampling Strategy, and Data Preparation
Sample Size Calculation for CAHPS I
The sample size calculation is based on the algorithm described in Lee and Munk (2008).
1
The calculation assumed
a linear regression as follows:
where T
i
is an indicator for receiving coverage under the Private Option and τ therefore estimates the effect of the
Private Option at the cut-point compared to traditional Medicaid. g(Xi) is a function of the rating variable and can
accommodate the nonlinear terms of X (such as quadratic or cubic of X) and interactions with T. The sample size
calculation is based on detecting a significantly better experience in those enrolled in Private Option plans
compared to Medicaid as expected with the Arkansas Private Option.
The sample size n can be calculated as follows:
where:
n is the overall sample size of the study;
is the proportion of variation in the outcome (Y) predicted by the rating and other covariates included in the
regression discontinuity (RD) model;
is the proportion of variation in treatment status (T) predicted by the rating and other covariates included in
the RD model;
P is the proportion of sample members in the treatment group;
MDES is the minimum detectable (standardized) effect size, calculated as τ/, where is the standard deviation
of Y;
α is the desired statistical significance level; and
1- β is the desired power level.
Under the regression discontinuity (RD) design, treatment assignment is highly correlated with the rating variable
because treatment is determined based on rating variable crossing a threshold. Therefore, it is less efficient than a
randomized controlled trial (RCT) if everything is the same except the assignment strategy.
2
The relative efficiency
(RE) of RCTs compared to a RD design is given by:

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 2
This ratio varies from 2.75 to 4 depending on the distribution of the rating variable around the cut-point.
1
For our
sample size calculation, we assumed RE=3, which means the RD design would need three times as large a sample
size as the RCT to be able to detect the same MDES. This implies that
=2/3. We calculated the sample size at a
significant level of 0.05 (α=0.05), and a power of 80 percent (β=0.2), and assumed the RD model can explain 20
percent of the variation in Y (
). To account for the non-response rates and missing patterns, we used
those obtained from a previous 2013 Arkansas Medicaid CAHPS survey.
Sample size calculations were estimated for the global rating of specialist care. The maximum sample size
needed to detect a significant MDES from 0.2 to 0.4 for all items is shown below. We chose to focus on this
item to generate a more conservative sample size estimate because only about 35 percent had visited a
specialist in the previous six months in the 2013 Arkansas Medicaid CAHPS survey. The last column reports the
number of individuals needed to sample after accounting for the potential loss due to non-response. The
results presented assumed a balanced design with equal number of individuals in each group (p=0.5).
Sensitivity analyses were conducted using imbalanced design and the overall sample size needed is generally
larger. For the subsequent sampling, we chose the sample size required to detect a significant MDES of 0.25 as
the target sample size (i.e., n=9,324).
Table 1. Sample Size Requirement for Rating of Specialist Care
MDES
Assumed
Standard
Deviation
Assumed
Mean
Difference
Assumed
Mean of
Medicaid
Expected
Mean of
QHP
Assumed
Missing (no
visit and /
or no
response)
Overall Rate
of Complete
Surveys
Sample
Size
Adjusted for
Non-
Response
0.2
2.20
0.44
8.54
8.98
65%
29%
1,484
14,568
0.25
2.20
0.55
8.54
9.09
65%
29%
950
9,324
0.3
2.20
0.66
8.54
9.20
65%
29%
659
6,475
0.35
2.20
0.77
8.54
9.31
65%
29%
485
4,757
0.4
2.20
0.88
8.54
9.42
65%
29%
371
3,642
Notes: alpha=0.05, power=0.8, R²m=0.20, RT-sq=2/3
Sampling Strategy for CAHPS I
The above sample calculation is based on a parametric approach using all available data. Including all data may
increase bias if observations far away from the cut-point are included and they are significantly different from
those around the cut-point. Although the local linear regression approach is preferred, sample size determination
prior to data acquisition is difficult to assess because the existing methods are largely data driven.
The two procedures recommended for estimating “optimal bandwidth” described in the statistical analysis section
are data driven and cannot be used to determine the optimal bandwidth prior to data acquisition. A “rule of
thumb of bandwidth” has been proposed by Imbens and Kalyanaraman (2012)
1
that is based on a rectangular
kernel. This calculation requires only an estimate of the variance of the rating variable as follows:
where X is the rating variable of interest,
and N is the total number of observations
in the data set.
For this calculation, we estimated standard deviations using all available data on income and exceptional
healthcare needs assessment Questionnaire scores from the sampling cohort of Medicaid and commercial

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 3
qualified health plan (QHP) enrollees prepared by ACHI. Within this cohort, there were 36,434 available
exceptional healthcare needs scores from enrollees who satisfied the inclusion and exclusion criteria and had an
exceptional healthcare needs score that was greater than 0.023 and less than 1. To utilize all available
information, for this calculation, we did not exclude individuals with missing gender, race, or market regions if
they had valid scores. Figure 1 shows the distribution of the scores. The estimated standard deviation of the score
was 0.1121. Based on this, we estimated the
to be 0.0252.
A similar calculation was made for the income criteria comparison. Within the sampling cohort, there were 43,844
individuals who satisfied the inclusion and exclusion criteria and had valid household income and family size
information. Income was reported as monthly household income at eligibility determination, allowing for negative
values. We then extrapolated this information to 12 months to get the yearly household income. Using family size
information, we calculated the household income as the 2014 percentage of the federal poverty level (FPL). Figure
2 shows the distribution of the family income as a percentage of 2014 FPL. The estimated standard deviation of
the household income as a percentage of FPL was 0.3973. Based on this, we estimated the
to be 0.0862.
0%
5%
10%
15%
20%
25%
30%
0.07
0.08
0.1
0.13
0.15
0.17
0.18
0.19
0.2
0.21
0.22
0.23
0.24
0.26
0.27
0.28
0.29
0.31
0.32
0.33
0.34
0.35
0.37
0.38
0.4
0.42
0.43
0.44
0.45
0.46
0.49
0.5
0.51
0.56
0.61
Percent of Enrollees
Exceptional Healthcare Needs Score
Figure 1. Exceptional Healthcare Needs Scores (N=36,434)

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 4
It is important to note that
is proposed as the initial estimate for the calculation of optional bandwidth in
Imbens and Kalyanaraman (2012)
2
and can underestimate the bandwidth needed.
Based on the rule of thumb bandwidth calculation, we surveyed all who are within 2*
around the cut-point to
allow potential underestimation of the bandwidth. Therefore, our targeted value range for each comparison was
as following:
For exceptional healthcare needs threshold criteria, we sampled all individuals with a score in this
range: (0.1294, 0.2304).
For income criteria, we sampled all individuals with family income as percentage of poverty in this
range: (0 percent, 34.24 percent).
Our strategy was to sample enrollees as close to the threshold as possible. We first sampled within the specified
ranges. If there were more enrollees than the targeted sample size within these ranges, we randomly sampled to
obtain the target sample size. However, if there were insufficient numbers of individuals within the specified
ranges, we included all individuals with values within these ranges and further sampled from individuals with
values just outside of these ranges. This process was repeated until we reached our target sample size.
Table 2 summarizes our sampling strategy for the two comparisons.
0%
2%
4%
6%
8%
10%
12%
14%
16%
0%
5%
10%
15%
17%
20%
25%
30%
35%
40%
45%
50%
55%
60%
65%
70%
75%
80%
85%
90%
95%
100%
105%
110%
115%
120%
125%
130%
135%
138%
Percentage of Individuals
Family Income as a Percentage of FPL
Figure 2. Family Income as a Percentage of 2014 Federal Poverty Level (FPL)
(N=43,844)

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 5
Table 2. Summary of CAHPS Sampling Strategies for Income and Exceptional Healthcare Needs Criteria
Comparisons
Exceptional Healthcare Needs Sample
Required sample size for MDES = 0.25
9,324
Per group (1:1)
4,662
ROT optimal bandwidth
0.1294
0.2304
Below 0.1799
n
Sampling
Method
0.15-0.17
3,775
3,775
All
Random sampling from 0.07-0.13
17,317
1,000
Random
Subtotal
4,775
Above 0.1799
n
Sampling
Method
0.18-0.23
3,785
3,785
All
Random sampling from 0.24-0.29
3,823
1,000
Random
Subtotal
4,785
Total
9,560
Income Sample
Required sample size for MDES = 0.25
9,324
Per group
4,662
ROT optimal bandwidth
0
0.3424
17% FPL or less
n
Sampling
Method
0
5,611
4,500
Random
0-17%
420
420
All
Subtotal
4,920
18% FPL or more
n
Sampling
Method
18-35%
2,669
2,669
All
35-50%
3,432
2,300
Random
Subtotal
4,969
Total
9,889

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 6
Data Preparation for CAHPS I
Arkansas Medicaid enrollment files for calendar years 2012, 2013, and 2014, which included HCIP enrollees, were
examined to determine those who were eligible for the survey. In order to be eligible for the survey, enrollees had
to have the following:
Be continuously enrolled in Medicaid or a QHP plan from July 2014 through November 2014.
Because enrollment data at the time the CAHPS sample was created was only available through
November 2014, the last five months of enrollment were used based on the premise that the vast
majority of those continuously enrolled in the last five months of the year would have maintained
coverage through the end of the year. A minimum of six months of enrollment was required
based on the CAHPS methodology for Medicaid enrollees, which asks beneficiaries about their
experience with healthcare services received over the preceding six months.
Be at least 19 years old and less than 65 years old on Nov. 15, 2014.
Have full coverage under traditional Medicaid or a QHP for at least six months in 2014 in Medicaid
Aid categories, 06, 20, and 25.
Not have had any prior coverage in aid coverage 06, 20, or 25 in 2013.
Not be determined to be auto-frail (score>=1).
Not have missing information on gender, race, or market region.
Received exceptional healthcare needs assessment screening but were not in aid category 06.
Have a valid mailing address.
The resulting subset of enrollees eligible for mailing was 188,213. A random sample of 5,000 enrollees were
selected from Medicaid and QHP enrollees separately. Further sampling steps were applied to these samples of
enrollees in order to obtain proper income and exceptional healthcare needs groups for comparison.
The final sample used for CAHPS survey distribution was 29,164. Of those surveyed, 6,568 were completed and
valid for analysis. The cooperation rate for the survey was 26.4 percent and a representative response rate was
received across populations of interest. Details of this calculation are contained in Table 3.
Table 3. Calculation of CAHPS Cooperation Rate
Sample
Size
No. of
Pieces
Received
(by Mail)
Complete
and Valid
Surveys
Received
by Mail
(M10)
Complete
and Valid
Surveys
Received
in Phone
Follow-Up
(T10)
Ineligibles
Excluded from
Analysis (Mail
Only) (M21 +
M22 + M24)
Ineligibles
Excluded from
Analysis
(Phone Only)
(T21 + T22 +
T24)
Total
Complete
and Valid
(M10 +
T10)
No
Forwarding
Addresses
and/or
Invalid
Phone
Numbers
(M23 + T23)
Cooperation
Rate*
29,164
6,438
6,404
164
25
28
6,568
4,228
26.4%
*Cooperation rate = (M10 + T10) / (Total Sample - (M21 + T21 + M22 + T22 + M23 + T23 + M24 + T24))
Figure 3 outlines the overall CAHPS study population development. The general comparison sample groups used
in the stabilized inverse probability of treatment weighting methodology are in boxes highlighted in blue. The
Higher Needs Population used in the regression discontinuity models comparing those who were assigned to
Medicaid or a QHP based on the medical needs assessment screener score are in boxes highlighted in pink. The
groups contained with the CAPHS sample will overlap with those contained within our analytical study population
for comparison.

Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 7
Figure 3. CAPHS Analytical Data Preparation
Total Cohort
N = 225,168
Exclude those not continuously enrolled in
the last 6 months of 2014
N = 8,945
Exclude those age 65 or older as of
November 15, 2014, with missing
demographic information, or were frail and
placed in commercial coverage
N = 18,904
Exclude those with prior Medicaid coverage
in Aid Categories 06, 20, or 25
N = 2,124
Exclude those auto-frail (Frailty score >= 1)
N = 6,982
Final Overall Cohort
N = 188,213
Exclude those with invalid addresses
N = 7,007
Final Eligible Cohort for Mailing
N = 181,206
Medicaid Cohort
N = 26,544
HCIP Cohort
N = 154,662
General Population
Traditional Medicaid
N = 648
High Needs
Medicaid
N = 1,569
Commercial Coverage
N = 2,809
High Needs
Commercial QHP
N = 1,914
General Population
Commercial QHP
N = 895
Total Surveys Complete and Valid for Analysis
N = 6,568
Expansion Population
“06”
Sample Size for CAPHS survey distribution
N = 29,164
Copyright © 2018 by the Arkansas Center for Health Improvement. All rights reserved.
Arkansas Health Care Independence Program (‘Private Option’) Final Report K- 8
Sampling Strategy for CAHPS II
The sampling strategy for the second CAHPS survey used a pragmatic design that included four distinct
subpopulations, all following on the sampling universe used in CAHPS I. All 5,026 respondents for CAHPS I were
included in the sampling frame for CAHPS II. In addition, 5,000 participants assigned to a QHP and 5,000 assigned
to Medicaid, by virtue of exceeding a composite score threshold on the exceptional healthcare needs assessment
Questionnaire, were randomly selected from the 154,662 HCIP cohort with a valid mailing address. A further
5,000 were randomly selected from the Medicaid 20/25 aid category CAHPS I cohort (26,544). In total, 19,999
participants (excluding duplicates) were sent a CAHPS II survey that was fielded during September through
December 2016.
Data Preparation for CAHPS II
The final sample used for CAHPS survey distribution was 19,999. Of those surveyed, 4,338 were completed and
valid for analysis. The cooperation rate for the survey was 24.7 percent and a representative response rate was
received across all populations of interest. Of note, there was no telephone follow-up pursued in CAHPS II. Details
of this calculation are contained in Table 4.
Table 4. Calculation of CAHPS II Cooperation Rate
Sample Size
No. of Pieces
Received (by
Mail)
Complete and
Valid Surveys
Received by
Mail (M10)
Ineligibles
Excluded from
Analysis (Mail Only)
(M21 + M22 + M24)
Total
Complete and
Valid (M10 +
T10)
No Forwarding
Addresses (M23)
Cooperation Rate*
19,999
4,356
4,338
18
4,338
2,738
25.2%
*Cooperation rate = (M10) / (Total Sample - (M21 + M22 + M23 + M24)
References
1
Lee M and Munk T. Using Regression Discontinuity Design for Program Evaluation. Journal of the American Statistical
Association Joint Statistical Meetings, Section on Survey Research Methods. Denver, CO. 2008
2
Imbens GW and Kalyanaraman K. Optimal Bandwidth Choice for the Regression Discontinuity Estimator. Review of
Economics and Statistics. 2012;79(3): 933-959.
